Technical Challenges in Addiction Neurocircuitry Analysis: From Foundational Models to Clinical Translation
This article provides a comprehensive analysis of the technical challenges in addiction neurocircuitry research, addressing the needs of researchers, scientists, and drug development professionals.
Technical Challenges in Addiction Neurocircuitry Analysis: From Foundational Models to Clinical Translation
Abstract
This article provides a comprehensive analysis of the technical challenges in addiction neurocircuitry research, addressing the needs of researchers, scientists, and drug development professionals. It explores the foundational framework of addiction neurocircuitry, particularly the three-stage cycle model encompassing binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation stages. The content examines methodological advances including computational modeling, neuroimaging, and neuromodulation techniques, while addressing troubleshooting challenges such as individual variability, model limitations, and technical barriers in brain stimulation. Finally, it evaluates validation approaches and comparative efficacy of different analytical methods, offering insights for future biomedical research and clinical application development.
Deconstructing the Addiction Cycle: Core Neurocircuitry Frameworks and Conceptual Challenges
FAQs: Core Neurocircuitry Framework
What is the three-stage addiction cycle and its associated neurocircuitry? The three-stage addiction cycle is a heuristic model that describes addiction as a chronic, relapsing disorder characterized by a spiral of impulsivity and compulsivity. The stages are binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. Each stage is mediated by specific, though overlapping, neurocircuits [1].
- Binge/Intoxication: This stage is focused on the pleasurable effects of the drug and is primarily associated with the ventral tegmental area (VTA) and the ventral striatum (including the nucleus accumbens), key components of the brain's dopamine system [1].
- Withdrawal/Negative Affect: This stage occurs when drug access is prevented and is characterized by a negative emotional state. It is primarily mediated by the extended amygdala [1].
- Preoccupation/Anticipation (Craving): This stage involves the craving for the drug and the loss of control over drug-seeking. It engages a distributed network including the orbitofrontal cortex-dorsal striatum, prefrontal cortex, basolateral amygdala, hippocampus, and insula [1].
What are the common functional connectivity findings across Substance Use Disorders (SUDs)? A 2025 meta-analysis of resting-state functional magnetic resonance imaging (rs-fMRI) studies identified consistent disruptions within the cortical-striatal-thalamic-cortical circuit across various SUDs [2]. Key findings are summarized in the table below.
Table 1: Common Resting-State Functional Connectivity (rsFC) Alterations in SUD [2]
| Seed Region | Hyperconnectivity Observed With | Hypoconnectivity Observed With |
|---|---|---|
| Anterior Cingulate Cortex (ACC) | Inferior Frontal Gyrus, Lentiform Nucleus, Putamen | — |
| Prefrontal Cortex (PFC) | Superior Frontal Gyrus, Striatum | Inferior Frontal Gyrus |
| Striatum | Superior Frontal Gyrus | Median Cingulate Gyrus |
| Thalamus | — | Superior Frontal Gyrus, dorsal ACC, Caudate Nucleus |
| Amygdala | — | Superior Frontal Gyrus, ACC |
What are the key dopaminergic alterations observed in human addiction? Positron Emission Tomography (PET) studies have consistently shown lower availability of striatal dopamine D2/3 receptors (D2/3R) in individuals with cocaine, methamphetamine, alcohol, and opioid use disorders compared to healthy controls [3]. This hypodopaminergic state is associated with negative affect, craving, and reduced motivation for natural rewards [3].
Troubleshooting Guides & Experimental Protocols
Protocol: Targeting Dissociable Neurocircuits with Deep TMS
This protocol details a method to modulate the two key prefrontal-striatal circuits implicated in AUD, providing a model for circuit-specific intervention [4].
- Objective: To examine the capacity of two distinct theta-burst dTMS protocols to recalibrate the weakened dlPFC (executive control) and heightened vmPFC (limbic control) pathways in individuals with Alcohol Use Disorder (AUD) [4].
- Design: Randomized, single-blind, sham-controlled crossover trial [4].
- Participants: 30 adults (aged 18-49) with moderate to severe AUD [4].
- Interventions:
- Active iTBS to dlPFC: Intermittent TBS is applied using an H-coil to increase neuronal excitability in the weakened dorsolateral prefrontal cortex pathway.
- Active cTBS to vmPFC: Continuous TBS is applied using an H-coil to decrease neuronal excitability in the heightened ventromedial prefrontal cortex pathway.
- Sham Control: A sham condition is used to control for non-specific effects of stimulation.
- Outcome Measures:
- Primary: Change in effective connectivity within targeted circuits, assessed via spectral Dynamic Causal Modeling (spDCM) of resting-state fMRI data [4].
- Secondary: Changes in cognitive tests of executive control and decision-making [4].
- Exploratory: Laboratory measures of craving, and longitudinal tracking of daily craving and alcohol consumption over 90 days [4].
Challenge: Inconsistent rs-fMRI Findings Across SUD Studies
Symptoms: Reported functional connectivity changes for the same seed region (e.g., striatum) vary significantly between studies, showing both increased and decreased connectivity with frontal regions [2].
Diagnosis & Solution: The inconsistency often stems from heterogeneity in study parameters. Table 2: Troubleshooting Inconsistent rs-fMRI Findings in SUD Research
| Potential Cause | Impact on Results | Recommended Solution |
|---|---|---|
| Heterogeneous SUD Populations | Varying substances of abuse, stages of addiction, and comorbidities introduce noise. | Implement strict participant stratification by primary substance, dependence severity, and abstinence duration. Conduct substance-specific meta-analyses [2]. |
| Small Sample Sizes | Underpowered studies produce unreliable and non-replicable findings. | Prioritize large-scale, collaborative studies. Use meta-analytic techniques (e.g., SDM-PSI) to pool data from multiple studies for increased power [2]. |
| Varied Analytical Methodologies | Differences in preprocessing pipelines, seed placement, and statistical thresholds affect outcomes. | Adopt and publish standardized, consensus-based preprocessing and analytical protocols. Use validated, anatomical or functional seeds. |
The Scientist's Toolkit
Table 3: Key Reagents and Resources for Addiction Neurocircuitry Research
| Resource / Reagent | Application / Function |
|---|---|
| Deep TMS (dTMS) H-coil | Enables non-invasive modulation of deeper cortical and subcortical nodes (e.g., vmPFC, striatum) compared to traditional figure-eight coils, allowing direct targeting of addiction-relevant circuits [4]. |
| Spectral Dynamic Causal Modeling (spDCM) | A computational method applied to fMRI data to infer the directed (effective) connectivity between brain regions, quantifying how one region influences another [4]. |
| Theta-Burst Stimulation (TBS) | A patterned form of rTMS that mimics endogenous brain rhythms. Intermittent (iTBS) increases cortical excitability, while continuous (cTBS) decreases it, allowing bidirectional circuit control [4]. |
| GLP-1 Receptor Agonists (e.g., Semaglutide) | A class of drugs emerging as a potential new therapeutic. Preclinical and early clinical trials suggest they modulate neurobiological pathways underlying addictive behaviors and may reduce alcohol use and craving [5]. |
| Ultrahigh-Resolution fMRI | An emerging technology capable of resolving activations in individual cortical layers, promising a more nuanced understanding of circuit-specific dopaminergic signaling [3]. |
| Neuromelanin-Sensitive MRI | A non-invasive proxy for measuring dopamine function and metabolism in the substantia nigra, providing insights into the integrity of the dopaminergic system in vivo [3]. |
Emerging Frontiers & Novel Signaling Pathways
The Role of GLP-1 in Addiction Glucagon-Like Peptide-1 Receptor Agonists (GLP-1RAs), used for diabetes and obesity, are under investigation for SUD. The pathway involves GLP-1R activation within the central nervous system, which is thought to curb addictive behaviors by modulating reward-related neurocircuitry. Early studies show:
- AUD: Low-dose semaglutide reduced alcohol self-administration and craving in a randomized controlled trial [5].
- Opioid Use Disorder (OUD): Rodent models show GLP-1RAs reduce self-administration of heroin, fentanyl, and oxycodone, and reduce reinstatement of drug-seeking [5].
- Tobacco Use Disorder: Preclinical data indicate reduced nicotine self-administration, with initial clinical trials suggesting potential for reducing cigarette use [5].
Frequently Asked Questions (FAQs)
Q1: What are the primary functions of the four key neural networks in addiction neurocircuitry? These regions form a interconnected circuit that drives different stages of the addiction cycle [6]. The Ventral Tegmental Area (VTA) is crucial for initial drug reward and reinforcement through dopamine release [7] [8]. The Ventral Striatum (particularly the Nucleus Accumbens) is the hub for integrating reward and motivation signals, mediating the acute reinforcing effects of drugs [9] [6]. The Extended Amygdala (including central amygdala, bed nucleus of stria terminalis) becomes critical during withdrawal, generating negative affect and stress via systems like CRF and norepinephrine [10] [6]. The Prefrontal Cortex (PFC), especially orbitofrontal, anterior cingulate, and dorsolateral regions, governs executive function; its dysfunction leads to loss of control over drug intake, compulsivity, and impaired decision-making [11] [6].
Q2: What rodent behavioral models are best for studying specific aspects of substance use disorder? Different models recapitulate specific behavioral criteria of Substance Use Disorder. The table below summarizes the primary application and neural substrates of common models.
Table 1: Rodent Behavioral Models for Substance Use Disorder Research
| Behavioral Model | Primary Addictive Phenomena Modeled | Key Neural Circuits Involved | Experimental Readout |
|---|---|---|---|
| Conditioned Place Preference (CPP) [7] | Contextual reward learning & relapse | VTA, Ventral Striatum [7] | Time spent in drug-paired context vs. neutral context |
| Drug Self-Administration [7] | Escalated intake, motivation, relapse | VTA, Ventral Striatum, Dorsal Striatum, PFC [7] [9] | Number of operant responses (e.g., lever presses) for drug infusion |
| Behavioral Sensitization [7] | Progressive neuroadaptations to repeated drug exposure | VTA, Ventral Striatum [7] | Increase in drug-induced locomotor activity over repeated injections |
| Cued Reinstatement [7] [6] | Drug relapse triggered by cues | Ventral Striatum, Basolateral Amygdala, PFC [6] | Resumption of drug-seeking in response to a conditioned cue |
Q3: How do dopamine circuits functionally diverge in addiction-like behaviors? Mesostriatal (VTA to Ventral Striatum) and nigrostriatal (SNc to Dorsal Striatum) dopamine circuits have dissociable roles. The table below outlines their distinct contributions.
Table 2: Functional Roles of Dopamine Circuits in Addiction-like Behaviors
| Circuit Feature | Mesostriatal Pathway (VTA → Ventral Striatum) | Nigrostriatal Pathway (SNc → Dorsal Striatum) |
|---|---|---|
| Primary Behavioral Role | Motivational "pull"; goal-directed behavior, cue-reward learning [8] | Behavioral "push"; habit formation, movement invigoration [8] |
| Role in Addiction | Initial drug reward, positive reinforcement, cue-induced craving [8] [6] | Transition to compulsive, habitual drug use [8] |
| Relevant SUD Criteria | Impaired control (escalated use) [8] | Risky use, social impairment (perseveration despite harm) [8] |
Troubleshooting Guides
Problem 1: Lack of Cell-Type Specificity in Circuit Manipulation
Issue: Traditional lesions or pharmacological manipulations affect multiple neuronal populations, confounding interpretation of results from dense, heterogeneous regions like the VTA [7].
Solution: Utilize modern, cell-type-specific tools.
- Recommended Technique: Optogenetics or Chemogenetics (DREADDs).
- Sample Protocol (DREADDs):
- Stereotaxic Injection: Inject a Cre-inducible viral vector (e.g., AAV-hSyn-DIO-hM3D(Gq)-mCherry) into the target region (e.g., VTA) of transgenic Cre-driver mice (e.g., DAT-Cre for dopamine neurons) [9].
- Incubation: Allow 3-4 weeks for viral expression.
- Administration: Administer the designer ligand (e.g., CNO, 1-3 mg/kg, i.p.) prior to behavioral testing.
- Validation: Confirm expression and functionality post-hoc via immunohistochemistry and/or in vivo electrophysiology.
Problem 2: Differentiating Direct vs. Indirect Pathway Activity in the Striatum
Issue: The striatum's direct (dMSNs) and indirect (iMSNs) pathway neurons are intermingled, making selective study difficult [9].
Solution: Leverage pathway-specific biomarkers and tools.
- Recommended Technique: Pathway-specific transgenic mice or FISH.
- Identification Guide:
- Experimental Application: Use ex vivo electrophysiology in brain slices from D1-Cre or D2-Cre mice to measure drug-induced synaptic plasticity specific to each pathway [12].
Problem 3: Measuring Compulsive-like Behavior in Rodents
Issue: Simple drug self-administration does not capture the core addiction criterion of "use despite adverse consequences" [7].
Solution: Implement progressive ratio or punishment-based schedules of reinforcement.
- Recommended Assay: Punished Drug Seeking.
- Detailed Protocol:
- Stable Self-Administration: Train rats to self-administer a drug (e.g., cocaine, 0.75 mg/kg/infusion, 2h sessions) on a fixed-ratio 1 (FR1) schedule until stable intake is achieved.
- Introduce Aversion: In subsequent test sessions, deliver a mild footshock (e.g., 0.2-0.3 mA, 0.5s duration) contingent upon drug infusion. This can be done on all infusions or on a subset.
- Quantify Compulsion: The proportion of animals that continue to self-administer the drug despite the footshock is considered to exhibit a compulsive, addiction-like phenotype [6]. Compare the number of infusions earned on punishment days to baseline.
Research Reagent Solutions
Table 3: Essential Research Reagents for Addiction Neurocircuitry Studies
| Reagent / Tool | Primary Function | Example Application |
|---|---|---|
| Cre-driver Mouse Lines (e.g., DAT-Cre, D1-Cre, D2-Cre) | Enables genetic access to specific neuronal populations [9] | Targeting dopamine neurons or specific striatal pathways for manipulation or imaging. |
| Chemogenetic Tools (DREADDs) | Chemically remote control of neuronal activity [9] | Manipulating specific circuit elements during behavioral tests without implanted hardware. |
| Channelrhodopsin (ChR2) & Archaerhodopsin (ArchT) | Precise optogenetic activation or inhibition of neurons with light [12] | Establishing causal links between circuit activity and behavior with millisecond precision. |
| AAV Vectors (e.g., AAV5, AAV9) | Efficient delivery of genetic constructs to the brain [9] | Expressing opsins, DREADDs, or sensors in a region- and cell-type-specific manner. |
| Fiber Photometry Systems | Recording population-level calcium or neurotransmitter dynamics in vivo [8] | Measuring real-time activity of a defined neural population during drug-related behaviors. |
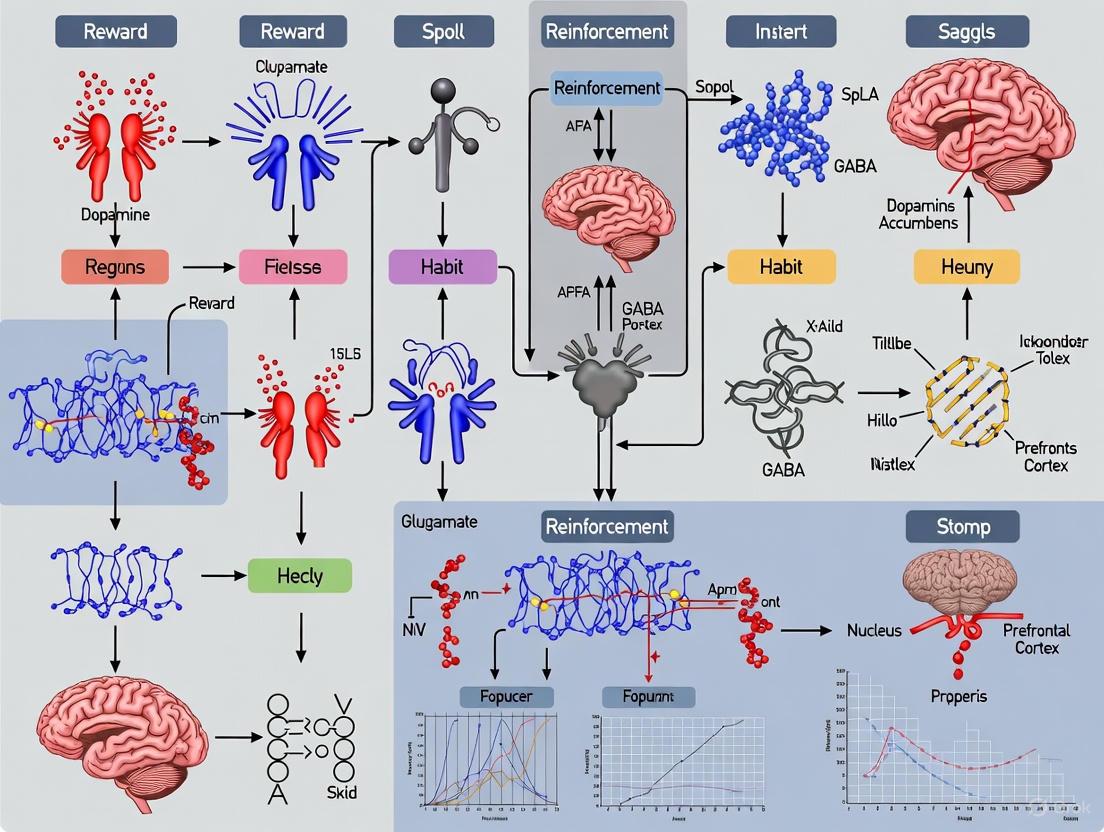
Visualizations: Key Addiction Neurocircuitry
The Three-Stage Addiction Cycle
Striatal Circuitry in Addiction
Prefrontal Cortex Dysfunction in Addiction (iRISA Model)
Addiction is a chronic relapsing disorder characterized by a compulsive pattern of drug seeking and use, which can be understood through the framework of a three-stage cycle: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation (craving) [13] [6]. Each stage is mediated by specific neurotransmitter systems acting within distinct brain circuits, and their dysregulation presents key technical challenges for researchers aiming to dissect these mechanisms [13] [14].
The core neurocircuitry involves the basal ganglia (critical for reward and habit formation in the binge/intoxication stage), the extended amygdala (central to the negative emotional state of withdrawal), and the prefrontal cortex (responsible for the executive function deficits and craving seen in the preoccupation/anticipation stage) [13]. The following diagram illustrates the interplay of these circuits and neurotransmitters across the addiction cycle.
Troubleshooting Guides: Key Neurotransmitter Systems
This section addresses common experimental challenges in studying the primary neurotransmitter systems implicated in addiction.
FAQ: Investigating the Mesolimbic Dopamine System
Q: What is the primary function of dopamine in addiction? A: Dopamine in the mesolimbic pathway (VTA to NAc) is crucial for the rewarding and reinforcing effects of drugs during the binge/intoxication stage. All major drugs of abuse directly or indirectly increase extracellular dopamine in the NAc, reinforcing drug-taking behavior [15] [16]. Fast and steep dopamine release is associated with the subjective "high" [13].
Q: My microdialysis data shows inconsistent dopamine release across different drug classes. Is this expected? A: Yes. While all addictive drugs increase NAc dopamine, they achieve this through distinct primary molecular targets [16]. For example, opioids do so by disinhibiting VTA dopamine neurons via GABA interneurons, while stimulants like cocaine directly block the dopamine transporter (DAT). Your results should align with the specific mechanism of the drug you are studying. Refer to Table 1 for details.
Q: How can I model the transition from goal-directed to habitual drug seeking? A: This transition involves a shift in the locus of dopaminergic control from the ventral striatum (NAc) to the dorsal striatum. Experimental designs should incorporate extended access self-administration protocols and use neural activity markers or receptor quantification to track this ventral-to-dorsal progression [13] [6].
FAQ: Probing the Opioid Peptide System
Q: Besides their own rewarding effects, how do opioid peptides influence other drug addictions? A: The endogenous opioid system, particularly mu-opioid receptors (MOR), critically modulates the rewarding properties of non-opioid drugs like alcohol, cocaine, and nicotine [16]. For example, alcohol consumption has been shown to induce endogenous opioid release in the human orbitofrontal cortex and NAc [13].
Q: Why does the opioid antagonist naltrexone show variable efficacy in clinical trials for alcoholism? A: This is a key translational challenge. Preclinical studies reliably show naltrexone reduces alcohol intake, but human clinical outcomes can be influenced by compliance issues and genetic variability in the opioid system [15]. Technical considerations for your research should include investigating individual differences in MOR expression or function.
FAQ: Analyzing the Brain Stress Systems (CRF and Dynorphin)
Q: What is the primary role of CRF and dynorphin in the addiction cycle? A: Corticotropin-releasing factor (CRF) and dynorphin are key mediators of the negative emotional state of withdrawal [13] [14]. During the withdrawal/negative affect stage, CRF systems in the extended amygdala become hyperactive, while dynorphin (a kappa-opioid receptor agonist) exerts aversive effects. This "dark side of addiction" drives negative reinforcement—taking the drug to relieve this dysphoric state.
Q: My CRF measurements in the amygdala are highly variable during withdrawal. What factors should I control for? A: Key factors include the duration of drug access (limited vs. extended), the time point of measurement after cessation, and environmental conditions like stress. The stress response is dynamic, and these factors significantly influence the magnitude of CRF and dynorphin system engagement [13].
FAQ: Assessing the Glutamate System and Executive Function
Q: How does glutamate contribute to craving and relapse? A: In the preoccupation/anticipation stage, glutamatergic projections from the prefrontal cortex to the NAc and extended amygdala become dysregulated [13] [14]. This is thought to underpin the intense craving and compromised executive control that can trigger relapse. A key mechanism is the incubation of craving, mediated by changes in AMPA receptor subunits in the NAc [6].
Q: What techniques can I use to study these prefrontal glutamate projections? A: Optogenetic or chemogenetic manipulation of specific prefrontal glutamatergic pathways during cue-induced reinstatement tests in animal models is a powerful approach. In humans, MR spectroscopy can measure glutamate levels, while functional connectivity MRI can assess the integrity of these circuits [13] [17].
The following tables consolidate key quantitative neurochemical changes and drug mechanisms to aid experimental design and data interpretation.
Table 1: Neurotransmitter Dynamics Across the Addiction Cycle [13]
| Addiction Stage | Neurotransmitter/Neuromodulator | Direction of Change |
|---|---|---|
| Binge/Intoxication | Dopamine | Increase |
| Opioid Peptides | Increase | |
| Serotonin | Increase | |
| GABA | Increase | |
| Withdrawal/Negative Affect | Corticotropin-Releasing Factor (CRF) | Increase |
| Dynorphin | Increase | |
| Norepinephrine | Increase | |
| Dopamine | Decrease | |
| Serotonin | Decrease | |
| Neuropeptide Y | Decrease | |
| Preoccupation/Anticipation | Glutamate | Increase |
| Dopamine | Increase | |
| Corticotropin-Releasing Factor (CRF) | Increase |
Table 2: Primary Neurotransmitter Mechanisms of Major Drugs of Abuse [15] [16]
| Drug Class | Primary Molecular Target | Net Effect on Reward Pathway |
|---|---|---|
| Opioids | Mu-Opioid Receptor (MOR) agonist | ↑DA in NAc (via disinhibition of VTA GABA neurons) |
| Stimulants | Cocaine: DAT blockerAmphetamines: DAT reversal/VMAT2 blocker | ↑DA in NAc (directly increases synaptic DA) |
| Alcohol | Multiple: enhances GABA-A, inhibits NMDA, ↑MOR | ↑DA in NAc (complex indirect modulation) |
| Nicotine | Nicotinic Acetylcholine Receptor (nAChR) agonist | ↑DA in NAc (direct activation of VTA DA neurons) |
| Cannabis | Cannabinoid CB1 Receptor agonist | Modulates GABA/Glu release, influencing VTA DA activity |
Standard Experimental Protocols
Protocol 1: Intracranial Self-Stimulation (ICSS) to Measure Brain Reward Function
- Purpose: To assess the hedonic state ("reward threshold") in animal models, particularly during drug withdrawal, which is a key marker of the withdrawal/negative affect stage [13].
- Methodology:
- Surgery: Implant a stimulating electrode into the medial forebrain bundle (MFB) in rats or mice.
- Training: Train subjects to press a lever to receive a brief electrical stimulus to the MFB.
- Threshold Determination: Use a psychophysical method (e.g., the "discrete-trial current-intensity" procedure) to determine the minimum current intensity required for the animal to perceive the stimulus as rewarding.
- Testing: Measure reward thresholds at baseline, during chronic drug administration, and at various time points during withdrawal. Elevated thresholds indicate a state of anhedonia (diminished reward function) [13].
- Technical Note: This model directly links to the human experience of dysphoria and anhedonia during abstinence.
Protocol 2: Drug Self-Administration and Reinstatement
- Purpose: The gold standard for modeling drug taking, seeking, and relapse in animals [6].
- Methodology:
- Surgery: Implant an intravenous catheter for drug delivery.
- Acquisition: Train animals to perform an operant response (e.g., nose-poke or lever-press) to receive a drug infusion, typically paired with a conditioned cue (light or tone).
- Extinction: Remove the drug and associated cues. The operant response no longer results in drug delivery.
- Reinstatement Test: Trigger drug-seeking behavior (measured as responses on the previously active lever) by:
- A priming dose of the drug (drug-induced reinstatement).
- Presentation of the drug-associated cue (cue-induced reinstatement).
- Exposure to a stressor (stress-induced reinstatement).
- Technical Note: This protocol effectively models the three stages of the addiction cycle and is ideal for testing potential anti-craving or relapse-prevention medications [13].
Key Signaling Pathways
The transition to addiction involves complex intracellular adaptations within the defined neurocircuitry. The diagram below outlines a generalized signaling cascade triggered by chronic drug exposure, leading to transcriptional changes that underlie long-term neuroplasticity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Addiction Neurobiology
| Reagent / Tool | Primary Function / Target | Example Application in Addiction Research |
|---|---|---|
| Dopamine Receptor Antagonists (e.g., SCH 23390 for D1, Eticlopride for D2) | Pharmacological blockade of dopamine receptors. | Used to dissect the role of specific DA receptor subtypes in drug reward and reinforcement in self-administration models [13]. |
| Opioid Receptor Antagonists (e.g., Naltrexone, Naloxone) | Broad opioid receptor blockade. | To test the involvement of endogenous opioid systems in the rewarding effects of alcohol, opioids, and other drugs [15] [16]. |
| CRF Receptor Antagonists (e.g., R121919, CP-154,526) | Blockade of CRF1 receptors. | Used to investigate the role of brain stress systems in withdrawal-induced anxiety and stress-induced reinstatement of drug seeking [13] [14]. |
| Kappa-Opioid Receptor Agonists/Antagonists (e.g., U50,488 (agonist), Nor-BNI (antagonist)) | Modulation of the dynorphin/KOR system. | To probe the aversive, stress-like effects of dynorphin during withdrawal and its impact on drug seeking [13]. |
| AMPA/NMDA Receptor Modulators (e.g., NBQX for AMPA, MK-801 for NMDA) | Glutamate receptor blockade. | To study the role of glutamatergic transmission in the prefrontal-striatal-amygdala circuits underlying craving and relapse [13] [6]. |
| DAT/SERT Inhibitors (e.g., GBR 12909 for DAT, Citalopram for SERT) | Selective blockade of monoamine transporters. | To isolate the effects of specific monoamine systems in psychostimulant reward and toxicity [16]. |
FAQs: Core Neurocircuitry Concepts
Q1: What is the fundamental neuroanatomical shift observed in the transition to addiction?
The transition is characterized by a ventral to dorsal striatal shift in control over drug-seeking behavior. Initially, goal-directed actions are driven by the ventral striatum (VS), particularly the nucleus accumbens, which processes reward and incentive salience. As addiction progresses, control shifts to the dorsal striatum (DS), which mediates habitual and compulsive behaviors. This represents a move from impulsive to compulsive drug use [1] [13] [18].
Q2: How are "impulsivity" and "compulsivity" defined in the context of addiction stages?
- Impulsivity: A predisposition toward rapid, unplanned reactions to stimuli without regard for negative consequences. This dominates the early stages of addiction and is largely associated with positive reinforcement mechanisms [1] [13].
- Compulsivity: The manifestation of perseverative, repetitive actions that are excessive and inappropriate. This dominates the later stages and is largely associated with negative reinforcement—performing the behavior to reduce a negative emotional state [1] [13].
Q3: What are the key neurotransmitter systems involved in this transition?
Different neurotransmitter systems are dysregulated across the three stages of the addiction cycle [13]:
Table: Key Neurotransmitter Changes in the Addiction Cycle
| Addiction Stage | Neurotransmitter | Direction of Change |
|---|---|---|
| Binge/Intoxication | Dopamine | Increase [13] |
| Opioid Peptides | Increase [13] | |
| Withdrawal/Negative Affect | Dopamine | Decrease [13] |
| Corticotropin-Releasing Factor (CRF) | Increase [13] | |
| Dynorphin | Increase [13] | |
| Preoccupation/Anticipation | Glutamate | Increase [13] |
Q4: What functional connectivity patterns distinguish ventral and dorsal striatum in addiction?
Resting-state functional connectivity (rsFC) studies reveal distinct patterns. In cocaine dependence, for example:
- Ventral Striatum (VS): Shows increased connectivity with the left inferior frontal cortex (IFC) and decreased connectivity with the hippocampus. These changes are correlated with higher impulsivity scores and recent cocaine use severity [19].
- Dorsal Striatum (DS): Shows increased connectivity with the orbitofrontal cortex (OFC), a pattern less directly correlated with impulsivity or recent use, potentially indicating a shift towards habitual processing [19].
Troubleshooting Guides & Experimental Protocols
Guide 1: Measuring Ventral-to-Dorsal Striatal Shifts Using Resting-State fMRI
Challenge: Inconsistent or weak findings when attempting to replicate ventral-to-dorsal shifts in human cohorts.
Solutions:
- Precise Seed Definition: Use well-validated, standardized atlases (e.g., Harvard-Oxford Subcortical Atlas) to define ventral (e.g., nucleus accumbens) and dorsal (e.g., caudate, putamen) striatal seeds for functional connectivity analysis. Avoid using small, arbitrary spherical seeds [19] [18].
- Cohort Stratification: Do not treat all individuals with a substance use disorder as a single group. Stratify your cohort based on addiction severity, duration of use, or behavioral measures of impulsivity/compulsivity to detect stage-specific connectivity changes [19].
- Control for Confounds: Rigorously account for age, sex, smoking status, and other substance use (e.g., alcohol) in your statistical models, as these can significantly influence functional connectivity measures [19].
Detailed Protocol: Seed-Based Functional Connectivity Analysis [19] [18]
- Data Acquisition: Acquire high-resolution T1-weighted anatomical and resting-state BOLD fMRI images on a 3T scanner (e.g., multi-band sequence to increase temporal resolution).
- Preprocessing: Process data using standard pipelines (e.g., fMRIPrep, CONN). Steps should include realignment, slice-time correction, normalization to standard space (e.g., MNI), and smoothing with an isotropic Gaussian kernel.
- Seed Placement: Define seed regions of interest (ROIs) for the Ventral Striatum and Dorsal Striatum.
- Time-Series Extraction: For each subject, extract the mean BOLD time series from each seed ROI.
- Connectivity Calculation: Compute the temporal correlation (e.g., Pearson's correlation) between the seed time series and the time series of every other voxel in the brain.
- Statistical Analysis: Convert correlation coefficients to Z-scores using Fisher's transformation. Compare Z-scores between patient and control groups using a general linear model (e.g., in SPM, FSL), including appropriate covariates.
Guide 2: Modeling the Transition in Animal Studies
Challenge: Designing an animal model that effectively captures the progression from voluntary, impulsive drug use to compulsive drug-seeking.
Solutions:
- Use Extended Access Models: Move beyond short-access (e.g., 1-2 hour) self-administration sessions. Implement "long-access" models (e.g., 6+ hours) which promote escalation of intake, a key feature of the transition to addiction [1] [13].
- Incororate Compulsion-Like Measures: Design protocols that measure drug-seeking despite adverse consequences. This can be done by pairing drug infusions with a punishing stimulus (e.g., a mild footshock) and observing which animals continue to self-administer, indicating compulsivity [13].
- Probe Cue-Induced Reinstatement: After extinction of drug-seeking behavior, re-present drug-associated cues. The degree of reinstatement is a model of craving and relapse, key elements of the "preoccupation/anticipation" stage [1] [13].
Guide 3: Targeting Specific Neurocircuits for Intervention
Challenge: Translating neurocircuitry findings into potential interventions.
Solutions & Protocol: Computational Modeling for Intervention Prediction [20] Recent research uses biophysical models of frontostriatal circuits to simulate "virtual interventions" and predict the most effective targets for restoring healthy dynamics.
- Model Construction: Develop a computational model of the interacting ventromedial (VS-OFC) and dorsolateral (DS-lateral PFC) circuits based on known anatomy and neurotransmitter actions.
- Parameter Estimation: Fit the model to empirical resting-state fMRI data from individuals with addiction (or OCD as a model of compulsivity) and healthy controls to identify disease-specific parameters (e.g., strengths of neural couplings) [20].
- Virtual Intervention Simulation: Systematically simulate changes to the model parameters (e.g., increasing dorsolateral cortico-striatal coupling while decreasing ventromedial coupling) to see which combination best restores the functional connectivity pattern observed in healthy controls [20].
- Validation: Test the model's predictions using longitudinal data, correlating simulated parameter changes with actual fluctuations in symptom severity over time. This approach can prioritize targets for neuromodulation therapies like TMS [20].
Signaling Pathways & Neurocircuitry Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Models for Investigating Striatal Transitions
| Item/Category | Function/Description | Example Application |
|---|---|---|
| Long-Access Self-Administration Model | An animal model where subjects have extended (6+ hrs) daily access to a drug, leading to escalated intake and compulsive-like seeking. | Modeling the transition from controlled to uncontrolled drug use; studying escalation neurobiology [13]. |
| Dopamine Receptor Antagonists | Pharmacological agents that block dopamine receptors (e.g., D1-like and D2-like receptor antagonists). | Local microinfusions to dissect the role of specific striatal subregion dopamine signaling in drug-seeking habits [13]. |
| Resting-State fMRI | A non-invasive neuroimaging technique that measures spontaneous brain activity to infer functional connectivity between regions. | Identifying hyper- and hypoconnectivity between ventral/dorsal striatum and cortical regions in human addiction [19] [18]. |
| Circuit-Specific Optogenetics | A technique using light to control the activity of genetically defined neurons in specific brain pathways. | Causally testing the role of specific VTA→VS or VTA→DS pathways in drug reward and relapse [1]. |
| Dynamic Causal Modeling (DCM) | A computational method for inferring effective connectivity (directed influence) between brain regions from fMRI data. | Modeling the directional influence between PFC and striatum and how it is altered in addiction [18] [20]. |
Troubleshooting Guides
Guide 1: Troubleshooting Target Identification in Addiction Neurocircuitry
Problem: Inconsistent results when trying to identify key brain targets for therapeutic neuromodulation in addiction.
Solution: Employ a connectivity-based approach, as lesion locations disrupting addiction map to a common brain circuit rather than a single region [21].
- Map Lesion Locations: Precisely map the anatomical locations of brain lesions from patients who experienced addiction remission onto a standard brain atlas.
- Compute Network Connectivity: Use a normative human connectome dataset (e.g., from 1,000 subjects) to calculate the functional connectivity network associated with each lesion location.
- Identify the Remission Network: Compare connectivity patterns of remission-associated lesions versus non-remission lesions. The resulting network shows positive connectivity to dorsal cingulate, lateral prefrontal cortex, and insula, and negative connectivity to medial prefrontal and temporal cortex [21].
Prevention: When designing neuromodulation trials, target hubs within this identified circuit (e.g., paracingulate gyrus, left frontal operculum) rather than a single anatomical structure.
Guide 2: Troubleshooting the Three-Stage Addiction Cycle Model in Preclinical Models
Problem: Difficulty in modeling the full, chronic-relapsing nature of human addiction in animal studies.
Solution: Deconstruct the addiction cycle into discrete, testable stages and employ behavioral paradigms specific to each [13] [6].
- Stage: Binge/Intoxication
- Core Dysfunction: Positive reinforcement and habit formation.
- Validated Protocol: Drug self-administration. Measure the escalation of intake with prolonged access to model the transition from controlled use to binge-like patterns [6].
- Stage: Withdrawal/Negative Affect
- Core Dysfunction: Reward deficits and stress surfeits.
- Validated Protocol: After chronic drug self-administration, impose abstinence and measure anxiety-like behaviors (e.g., elevated plus maze) and reward thresholds (e.g., intracranial self-stimulation) [6].
- Stage: Preoccupation/Anticipation (Craving)
- Core Dysfunction: Executive function deficits and craving.
- Validated Protocol: Cue-induced reinstatement of drug-seeking after extinction. This models relapse triggered by drug-associated cues [6].
Prevention: Use animal models that incorporate individual diversity, complex environments with alternative reinforcers, and the influence of stress to better model human vulnerability and resilience [13].
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary neurobiological circuits involved in addiction, and what are their core functions?
Addiction involves a dramatic dysregulation of three key motivational circuits [13] [6]:
- Basal Ganglia Circuit: Central to the
binge/intoxicationstage. It mediates the rewarding effects of drugs and the development of incentive salience and compulsive drug-seeking habits. - Extended Amygdala Circuit: Central to the
withdrawal/negative affectstage. It is responsible for the increases in negative emotional states (dysphoria, anxiety, irritability) and stress-like responses during drug withdrawal. - Prefrontal Cortex Circuit: Central to the
preoccupation/anticipationstage. It is involved in craving, deficits in executive function, and compromised inhibitory control, which contribute to relapse.
FAQ 2: How do neurotransmitter systems shift across the different stages of the addiction cycle?
The neurochemical landscape changes dramatically as an individual progresses through the addiction cycle. The table below summarizes key neurotransmitter alterations [13].
Table 1: Neurotransmitter Dynamics in the Addiction Cycle
| Stage | Neurotransmitter | Direction of Change |
|---|---|---|
| Binge/Intoxication | Dopamine | Increase [13] |
| Opioid Peptides | Increase [13] | |
| γ-aminobutyric acid (GABA) | Increase [13] | |
| Withdrawal/Negative Affect | Corticotropin-Releasing Factor (CRF) | Increase [13] |
| Dynorphin | Increase [13] | |
| Dopamine | Decrease [13] | |
| Endocannabinoids | Decrease [13] | |
| Preoccupation/Anticipation | Glutamate | Increase [13] |
| Hypocretin (Orexin) | Increase [13] | |
| Corticotropin-Releasing Factor (CRF) | Increase [13] |
FAQ 3: What is the key evidence for a shared neurocircuitry across different substance use disorders?
Human lesion studies provide causal evidence. Research shows that brain lesions resulting in remission of nicotine addiction are characterized by a specific pattern of functional connectivity. This same connectivity pattern is also associated with a reduced risk of alcoholism, suggesting a common network is disrupted [21]. This network involves positive connectivity to the dorsal cingulate, lateral prefrontal cortex, and insula, and negative connectivity to the medial prefrontal and temporal cortex [21].
FAQ 4: What are the main technical challenges in defining functional boundaries within addiction neurocircuitry?
- Spatial Overlap: The same brain structures (e.g., striatum, prefrontal cortex) are involved in multiple, distinct functions (reward, habit, executive control). Disentangling these roles is complex [13] [22].
- Temporal Dynamics: The neurocircuitry of addiction is not static. The dominant circuits and neuroadaptations shift from positive to negative reinforcement and from impulsive to compulsive behavior as the disorder progresses [13] [6].
- Individual Variability: Neurobiological factors underlying the transition from controlled use to addiction vary significantly between individuals, making it difficult to define a single "addicted brain" circuit map [13].
- Circuit Integration: These circuits do not operate in isolation. They form a complex, integrated network where dysfunction in one node can dysregulate the entire system, making it difficult to assign a specific behavior to a single region [22].
Experimental Protocols & Workflows
Protocol 1: Lesion Network Mapping to Identify Therapeutic Brain Targets
This methodology is used to identify brain circuits causally involved in addiction remission by analyzing lesions in patients who spontaneously recovered [21].
- Primary Materials: Database of patients with focal brain lesions and detailed behavioral history (e.g., smoking status); Normative human connectome dataset (e.g., from 1000 subjects); Standard brain atlas software.
- Step-by-Step Workflow:
- Patient Stratification: Identify two independent cohorts of patients who were daily smokers at the time of brain lesion. Stratify them into those who remitted (quit easily, no relapse, no craving) and those who did not.
- Lesion Mapping: Precisely trace each patient's lesion location and map it to a standard brain atlas (e.g., MNI space).
- Network Computation: For each lesion location, compute the functional connectivity pattern across the entire brain using the normative connectome data. This creates a "connectivity map" for every lesion.
- Statistical Comparison: Voxel-wise comparison of connectivity maps from the remission group versus the non-remission group to identify a common "addiction remission network."
- Validation: Test the generalizability of the identified network in an independent cohort (e.g., patients with alcohol addiction risk scores) and assess its specificity against other neuropsychological variables.
Protocol 2: Validating the Three-Stage Addiction Cycle in Rodent Models
This protocol outlines established methods for modeling the core stages of addiction in animals, allowing for the investigation of underlying neurocircuitry [13] [6].
- Primary Materials: Intravenous catheters for self-administration; Operant conditioning chambers; Microdialysis or fast-scan cyclic voltammetry equipment; Drugs of abuse (e.g., cocaine, heroin).
- Step-by-Step Workflow:
- Binge/Intoxication Stage:
- Procedure: Train rats to self-administer a drug (e.g., cocaine) by pressing a lever. Progress from short access (1-2 hours) to extended or intermittent long access (6+ hours) to promote escalation of intake.
- Measure: Number of infusions earned; breakpoint on a progressive ratio schedule.
- Withdrawal/Negative Affect Stage:
- Procedure: After stable escalation, impose a period of forced abstinence.
- Measure: Anxiety-like behaviors (e.g., time in open arms of an elevated plus maze); reward thresholds (intracranial self-stimulation); levels of stress neurotransmitters (e.g., CRF in the amygdala via microdialysis).
- Preoccupation/Anticipation (Craving) Stage:
- Procedure: After extinction of drug-seeking (lever presses no longer deliver drug), present previously drug-paired cues (e.g., light, tone).
- Measure: Number of non-reinforced lever presses during cue presentation (reinstatement of drug-seeking).
- Binge/Intoxication Stage:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials for Addiction Neurocircuitry Analysis
| Item | Function & Application |
|---|---|
| Normative Human Connectome Dataset | A large-scale map of human brain connectivity used as a reference to compute the network effects of focal brain lesions or stimulation sites [21]. |
| Animal Models of Addiction | Preclinical models (typically rodent) that recapitulate specific stages of addiction (binge, withdrawal, relapse) for controlled investigation of neurocircuitry and neuropharmacology [13] [6]. |
| Functional Magnetic Resonance Imaging (fMRI) | Non-invasive neuroimaging technique used in humans to measure brain activity (via BOLD signal) in response to drug cues or during rest, allowing for functional connectivity analysis [21] [23]. |
| Drug Self-Administration Apparatus | Operant conditioning chambers used in animal research where subjects perform an action (e.g., lever press) to receive intravenous infusions of a drug, modeling drug-taking behavior [6]. |
| Lesion Network Mapping Software | Computational tools for mapping brain lesions to a standard atlas and calculating their connectivity profiles using the connectome, enabling the identification of symptom-specific brain circuits [21]. |
| Neuromodulation Techniques (TMS / DBS) | Transcranial Magnetic Stimulation (TMS) and Deep Brain Stimulation (DBS) are used to test the causal role of specific brain circuits by modulating their activity, with potential therapeutic applications [21]. |
Advanced Methodologies in Circuit Analysis: From Computational Models to Neuromodulation
Frequently Asked Questions (FAQs)
General Framework Questions
Q1: What are the key differences between model-based and model-free reinforcement learning in the context of addiction research?
Model-based and model-free reinforcement learning represent two distinct computational approaches for understanding decision-making processes, which are often impaired in addiction.
Model-Free RL: This is a reflexive system where agents learn action values directly from experience without building an internal model of the environment. It associates actions with outcomes through trial and error, creating habitual behaviors. In addiction, this system becomes overactive, leading to compulsive drug-seeking behaviors even when outcomes are no longer desirable [24] [25].
Model-Based RL: This is a deliberative system where agents learn and utilize an internal model of the environment's dynamics to plan actions. It can simulate future states and outcomes before taking action. Addiction research suggests this system becomes compromised, reducing flexible, goal-directed behavior [24] [25].
The transition from model-based to model-free control represents a core computational mechanism in the development of compulsive habits in addiction [25].
Q2: How can Bayesian inference help address uncertainty in computational models of addiction neurocircuitry?
Bayesian inference provides a mathematical framework for updating beliefs (probability distributions) about model parameters as new data becomes available. This is particularly valuable in addiction research due to the high variability in patient responses and neural adaptations.
- Prior Distributions: Researchers can incorporate existing knowledge (e.g., from previous studies or theoretical constraints) as prior probabilities [26].
- Posterior Distributions: As new experimental data is collected (likelihood), Bayesian methods combine priors with data to form updated posterior distributions, which represent refined knowledge about neurocircuitry parameters [26].
- Quantifying Uncertainty: Unlike point estimates, posterior distributions naturally capture uncertainty, allowing researchers to make direct probability statements about parameters, such as the strength of a synaptic connection or the effect of a pharmacological intervention [26].
This approach is especially useful for modeling complex, multi-stage addiction processes and for integrating diverse data types within a single coherent framework [27].
Q3: What common computational challenges arise when fitting reinforcement learning models to human behavioral data in addiction studies?
Researchers often encounter several technical challenges when applying RL models to clinical populations:
- Parameter Identifiability: Different combinations of learning rates, discount factors, and inverse temperature parameters can produce identical choice patterns, making the true underlying mechanism difficult to discern.
- Model Misspecification: Standard RL models may not capture all relevant cognitive processes, such as attention or working memory deficits, which are often impaired in addiction.
- Exploration-Exploitation Dilemma: Addicted individuals often exhibit altered exploration strategies, which standard epsilon-greedy or softmax policies may not fully capture [24].
- Credit Assignment: Determining which actions led to rewarding or aversive outcomes is particularly challenging in complex environments with delayed consequences, a deficit that may be central to addiction [25].
Technical Implementation Questions
Q4: How do I choose an appropriate exploration strategy for my reinforcement learning agent in a novel behavioral task?
The choice of exploration strategy depends on your action space and research question:
- Discrete Action Spaces: Epsilon-greedy strategies are commonly used, where the agent selects a random action with probability ε (exploration) and the best-known action otherwise (exploitation). The ε parameter is typically high initially and decays over time [24].
- Continuous Action Spaces: Adding random noise to actions or using entropy regularization in the loss function encourages exploration by making the policy less certain about its choices [24].
- Advanced Methods: For more sophisticated exploration, intrinsic motivation methods like "curiosity" drive exploration by rewarding the agent for visiting novel states or for taking actions where outcomes are hard to predict [24].
Q5: What are the essential steps for implementing Markov Chain Monte Carlo (MCMC) methods for Bayesian model estimation?
Proper implementation of MCMC requires careful attention to several steps:
Algorithm Selection: Choose an appropriate sampling algorithm based on your model structure:
- Metropolis-Hastings: General-purpose algorithm applicable to many problems
- Gibbs Sampling: Efficient when conditional distributions are known and easy to sample from
- Hamiltonian Monte Carlo (HMC) & NUTS: More advanced algorithms that better explore complex, high-dimensional parameter spaces [26]
Convergence Diagnostics: Always assess whether your chains have properly converged to the target posterior distribution using:
- Trace Plots: Visual inspection should show stable fluctuation around a mean value ("fat hairy caterpillar" appearance)
- Gelman-Rubin Statistic (R-hat): Values should be close to 1 (typically <1.1) to indicate convergence
- Effective Sample Size (ESS): Should be sufficiently large to ensure reliable estimates [26]
Model Checking: Validate your model using posterior predictive checks to ensure it can generate data similar to your actual observations [26].
Troubleshooting Guides
Problem: RL Agent Fails to Learn Optimal Policy
| Symptoms | Potential Causes | Solutions | Related Addiction Context |
|---|---|---|---|
| Agent consistently chooses suboptimal actions | Poor balance between exploration and exploitation | Systematically decay exploration rate (ε); implement intrinsic curiosity rewards [24] | Models addictive behavior where exploration of alternatives diminishes |
| Unstable learning curves | Learning rate too high | Reduce learning rate; implement adaptive learning rate schedules | Analogous to maladaptive learning in addiction with heightened reward sensitivity |
| Agent fails to generalize | Incorrect state representation | Include task-relevant features in state space; consider feature engineering | Reflects impaired state representation in addiction neurocircuitry |
| Q-values diverge to infinity | Insufficient regularization | Apply gradient clipping; implement reward scaling | Models compulsive behavior where value representations become pathological |
Problem: Bayesian Model Estimation Issues
| Symptoms | Potential Causes | Solutions | Diagnostic Tools |
|---|---|---|---|
| MCMC chains fail to converge | Poor initialization; model misspecification | Run multiple chains from different starting points; simplify model structure | Gelman-Rubin statistic (R-hat >> 1.1) [26] |
| High autocorrelation in samples | Inefficient sampling algorithm | Switch to HMC/NUTS; reparameterize model | Effective Sample Size (ESS) diagnostic [26] |
| Poor model fit to data | Inappropriate likelihood function | Conduct posterior predictive checks; compare alternative models | Posterior predictive p-values [26] |
| Computational bottlenecks | High-dimensional parameter space | Implement variational inference approximations; use more efficient software (e.g., Stan) [26] | Memory usage and iteration time |
Problem: Translating Computational Models to Addiction Phenomena
| Challenge | Technical Issue | Potential Solutions | Theoretical Considerations |
|---|---|---|---|
| Modeling transition from goal-directed to habitual behavior | Determining relative contribution of model-based vs. model-free systems | Use two-step task designs with computational modeling to decompose contributions [25] | Addiction may involve a shift from model-based to model-free control dominance [25] |
| Capturing compulsive drug-seeking despite negative consequences | Standard RL agents avoid negative states | Implement asymmetric learning for positive vs. negative outcomes; alter baseline reward expectations [27] | Proposed models include raised reward thresholds in addiction [27] |
| Modeling craving and relapse | Standard RL frameworks poorly capture internal states | Incorporate interoceptive states into state representation; use active inference frameworks [25] | Craving may stem from incorrect beliefs about physiological states [25] |
Experimental Protocols & Methodologies
Protocol 1: Two-Step Task for Decomposing Model-Based and Model-Free Control
This behavioral task is widely used to quantify the relative contributions of model-based and model-free decision systems, which are often imbalanced in addiction [25].
Workflow Diagram: Two-Step Task Computational Analysis
Step-by-Step Methodology:
Task Structure: Participants make two sequential choices. The first choice leads to one of two second-stage states with probabilistic transitions (typically 70% common, 30% rare transitions).
Data Collection: Record choices and reaction times at both decision stages across multiple trials (typically 200-300 trials).
Computational Modeling: Fit hybrid RL models that include both model-based and model-free components:
- Model-Free Component: Updates action values based on reinforcement history using temporal difference learning
- Model-Based Component: Uses knowledge of the task structure (transition probabilities) to plan actions
Parameter Estimation: Estimate individual subject parameters using maximum likelihood or hierarchical Bayesian methods, focusing on:
- Learning rates for each system
- Relative weighting of model-based vs. model-free control
- Decision noise parameters
Clinical Correlation: Relate individual differences in computational parameters to addiction severity, craving measures, or neural activity [25].
Protocol 2: Hierarchical Bayesian Modeling of Addiction Longitudinal Data
This protocol describes how to implement Bayesian methods for analyzing longitudinal clinical data in addiction research, which often features multiple levels of variability (within-subject, between-subject, across time).
Workflow Diagram: Hierarchical Bayesian Modeling
Step-by-Step Methodology:
Model Specification:
- Define the hierarchical structure: individual-level parameters drawn from group-level distributions
- Specify appropriate likelihood functions for your data type (e.g., Bernoulli for binary outcomes, Gaussian for continuous)
- Choose weakly informative priors that regularize estimates without dominating the data
Computational Implementation:
- Code model in probabilistic programming languages like Stan, PyMC, or JAGS
- Implement appropriate MCMC sampling (NUTS is recommended for complex models)
- Run multiple chains from dispersed initial values
Convergence Diagnostics:
- Check R-hat statistics (<1.1 indicates convergence)
- Examine trace plots for good mixing
- Calculate effective sample size to ensure sufficient independent samples
Model Validation:
- Perform posterior predictive checks to assess model fit
- Compare with alternative models using information criteria (LOO, WAIC)
- Conduct sensitivity analyses to check prior influence
Result Interpretation:
- Report posterior means and credible intervals for key parameters
- Visualize posterior distributions to communicate uncertainty
- Make probabilistic statements about hypotheses (e.g., "There is 92% probability that the treatment reduces craving") [26]
The Scientist's Toolkit: Research Reagent Solutions
Computational Frameworks & Software
| Tool Name | Type | Primary Function | Application in Addiction Research |
|---|---|---|---|
| Stan | Probabilistic Programming | Bayesian inference using HMC/NUTS sampling | Hierarchical modeling of clinical trial data; dose-response modeling [26] |
| Python RLlib | Reinforcement Learning Library | Scalable RL implementation for various algorithms | Modeling decision-making processes at computational level [24] |
| MATLAB Computational Psychiatry Pack | Model Fitting Toolkit | Maximum likelihood and Bayesian estimation of cognitive models | Fitting RL models to behavioral data from addicted individuals |
| JAGS | Bayesian Analysis Tool | Gibbs sampling for Bayesian models | Alternative to Stan for models where conditional distributions are tractable [26] |
| AI Gym | RL Environment | Standardized environments for testing RL agents | Developing and validating novel RL models of addictive behavior |
Conceptual Frameworks for Addiction Modeling
| Framework | Key Components | Addiction Application | References |
|---|---|---|---|
| Model-Based vs Model-Free RL | Dual-system architecture of decision-making | Transition from goal-directed to habitual drug use [25] | [24] [25] |
| Active Inference | Bayesian belief updating with precision weighting | Compulsive drug seeking as faulty belief updating [25] | [25] |
| Reinforcement Learning Theory of Addiction | Temporal difference learning with dopamine | Drug-induced hijacking of natural reward learning [27] | [27] |
| Bayesian Brain Hypothesis | Predictive coding and precision estimation | Aberrant salience attribution in addiction [25] | [25] |
Quantitative Data Reference Tables
Table 1: Typical Parameter Ranges in RL Models of Addiction
| Parameter | Healthy Controls | Addicted Individuals | Computational Interpretation |
|---|---|---|---|
| Model-Based Weight | 0.5-0.8 | 0.2-0.5 | Reduced goal-directed control in addiction [25] |
| Learning Rate (Reward) | 0.2-0.4 | 0.3-0.6 | Heightened sensitivity to drug rewards [27] |
| Learning Rate (Punishment) | 0.3-0.5 | 0.1-0.3 | Reduced sensitivity to negative outcomes [27] |
| Inverse Temperature | 3-10 | 5-15 | Increased choice rigidity in addiction |
| Discount Factor (γ) | 0.8-0.95 | 0.5-0.8 | More steeply discounted future rewards [27] |
Table 2: Bayesian Model Comparison Metrics
| Metric | Formula | Interpretation | Advantages |
|---|---|---|---|
| Watanabe-Akaike Information Criterion (WAIC) | -2(log pointwise predictive density - effective number of parameters) | Lower values indicate better predictive accuracy | Fully Bayesian; works for singular models |
| Leave-One-Out Cross Validation (LOO) | Σ log p(yi|y{-i}) | Out-of-sample prediction accuracy | More robust than WAIC for influential observations |
| Bayes Factor | p(D|M1)/p(D|M2) | Relative evidence for one model over another | Direct Bayesian model comparison |
| Postior Model Probability | p(M|D) ∝ p(D|M)p(M) | Absolute probability of a model given data | Requires specifying prior model probabilities |
Troubleshooting Guides
Resting-State fMRI (rs-fMRI) Preprocessing and Analysis
Q1: How do I address common artifacts in rs-fMRI data, such as head motion and physiological noise? Excessive head motion and physiological noise (e.g., from cardiac and respiratory cycles) are major confounds in rs-fMRI, as they can mimic or obscure genuine neural signals in functional connectivity analysis [28].
- Head Motion: Implement rigorous motion correction during preprocessing. Scrub volumes with framewise displacement exceeding 0.2-0.5 mm. Include motion parameters as regressors in your general linear model.
- Physiological Noise: Use data-driven methods like ICA to identify and remove noise components related to physiological processes. If possible, record cardiac and respiratory rhythms during the scan and use them for retrospective correction.
- Low-Frequency Drift: Apply a high-pass filter (typically with a cutoff around 0.008-0.01 Hz) to remove slow scanner drifts that can dominate the BOLD signal.
Q2: What steps should I take if my functional connectivity matrices show poor test-retest reliability? Poor reliability can stem from insufficient data quality or suboptimal analytical choices [28].
- Increase Scan Duration: The reliability of functional connectivity estimates increases with scan length. Aim for at least 10-15 minutes of resting-state data.
- Ensure Sufficient Preprocessing: Verify that all standard preprocessing steps (motion correction, normalization, smoothing, band-pass filtering, and nuisance regression) have been correctly applied.
- Check Network Definitions: The reliability of connectivity matrices depends on the accurate definition of nodes (brain regions) and edges (connections). Use standardized, well-validated brain atlases for parcellation.
Effective Connectivity and Spectral DCM
Q3: How do I resolve model convergence issues or poor parameter identifiability in Spectral DCM? Spectral DCM infers effective connectivity by fitting a model to the cross-spectral density of the data [29]. Convergence issues often relate to model specification.
- Simplify the Model: Begin with a smaller network of brain regions (3-4 nodes). Large, overly complex models with many free parameters can be poorly identified and fail to converge.
- Check Priors: DCM uses Bayesian estimation with prior distributions on parameters. Ensure you are using appropriate priors. Very tight priors can prevent the model from fitting the data, while overly wide priors can lead to instability.
- Inspect Data Quality: As with all fMRI analyses, ensure your input time series are of high quality, with minimal artifacts. Noisy data can prevent the algorithm from finding a clear optimum.
Q4: What does it mean if a change in effective connectivity does not correlate with a change in functional connectivity? This is an expected scenario, not necessarily an error. Effective connectivity represents the directed, causal influence one neural region exerts over another, measured in Hz (rate of change) [29]. Functional connectivity is a measure of undirected, statistical dependence (e.g., correlation) between regions [30]. A single change in a directed effective connection can redistribute activity across the entire network, leading to complex changes in all pairwise correlations. Therefore, the brain region pairs showing the largest changes in functional connectivity may not be the same as those with the largest changes in effective connectivity [29].
General Technical Challenges
Q5: How can I programmatically generate reproducible and high-quality visualizations of my connectivity results? Relying on manual adjustments in GUI-based tools hinders replication and scalability [31].
- Adopt Code-Based Tools: Use well-documented software packages within programming environments like R (
cowplot,ggseg), Python (Matplotlib,Nilearn), or MATLAB. These allow you to generate publication-ready figures directly from code. - Leverage Templates: Utilize online resources and code-sharing platforms to find templates for brain connectivity visualizations, such as heat maps and connectomes.
- Enable Batch Processing: Code-based visualization allows you to easily iterate over multiple subjects or conditions, which is essential for quality control in large datasets [31].
Frequently Asked Questions (FAQs)
Q: What is the fundamental difference between functional and effective connectivity? A: Functional connectivity is a statistical description of "what" brain regions are synchronized. It quantifies temporal correlations or dependencies (e.g., using Pearson correlation) but does not imply direction or causality. Effective connectivity describes "how" and in "which direction" regions influence each other, modeling the causal impact one neural system exerts over another [30]. In essence, functional connectivity is a correlation, while effective connectivity is a causal estimate [29].
Q: When should I choose Spectral DCM over other effective connectivity methods like Granger Causality or Structural Equation Modeling? A: The choice depends on your data and research question. Spectral DCM is ideal for resting-state fMRI where there are no controlled experimental inputs, as it models endogenous neural fluctuations [29]. It is a state-space model that distinguishes between hidden neural states and observed BOLD signals. Granger Causality is a non-parametric method often applied to electrophysiological data like EEG with high temporal resolution [30]. Structural Equation Modeling (SEM) requires a pre-specified anatomical model to test the strength of connections between regions but is less flexible for exploring novel network dynamics [32].
Q: Can these neuroimaging techniques inform addiction treatment development? A: Yes. By mapping the neurocircuitry of addiction, these techniques can identify specific network dysfunctions as biomarkers and treatment targets. For example, addiction involves a three-stage cycle (binge/intoxication, withdrawal/negative affect, preoccupation/anticipation) mediated by dysregulation in specific circuits like the basal ganglia, extended amygdala, and prefrontal cortex [13]. Effective connectivity analysis with Spectral DCM could pinpoint the precise directional dysfunction within this circuit (e.g., weakened prefrontal control over the striatum), which can then be targeted with neuromodulation therapies or tracked as a biomarker of treatment response.
Q: What are the key limitations of fMRI for measuring neural activity? A: fMRI has two primary limitations [28] [33]:
- Indirect Measurement: fMRI measures the Blood-Oxygen-Level-Dependent (BOLD) signal, which is a hemodynamic response correlated with neural activity, not the electrical activity of neurons themselves.
- Temporal Resolution: The BOLD response is slow, unfolding over 1-5 seconds, which is much slower than the millisecond-scale dynamics of neural firing.
Data Presentation
Comparison of Neuroimaging Modalities
Table 1: Key characteristics of functional neuroimaging techniques relevant to connectivity analysis.
| Technique | Spatial Resolution | Temporal Resolution | Primary Use in Connectivity | Key Advantage |
|---|---|---|---|---|
| fMRI | Medium-High | Low (seconds) | Functional & Effective Connectivity | Whole-brain coverage; non-invasive; no radiation [33]. |
| EEG/QEEG | Low | Very High (milliseconds) | Functional Connectivity | Directly measures neural electrical activity; excellent for fast dynamics [30]. |
| MEG | Medium | Very High (milliseconds) | Functional & Effective Connectivity | Combines good spatial localization with high temporal resolution [30]. |
| SPECT | Medium | Very Low (minutes) | Functional Connectivity (broad) | Provides a broader overview of brain function over time [33]. |
Key Metrics for Connectivity Analysis
Table 2: Common metrics and their interpretations in functional and effective connectivity studies.
| Metric | Connectivity Type | Interpretation | Typical Use Case |
|---|---|---|---|
| Pearson Correlation | Functional | Linear, undirected statistical dependence between two time series. | Identifying nodes within a resting-state network (e.g., Default Mode Network) [28]. |
| Dynamic Causal Modeling (DCM) | Effective | A Bayesian framework to infer the directed influence between regions and how it is modulated by experimental conditions. | Testing how a cognitive task or drug challenge alters causal pathways in a pre-defined network [29]. |
| Granger Causality | Effective | A time-series-based measure where if past values of signal X improve the prediction of signal Y, then X "Granger-causes" Y. | Analyzing directed influences in high-temporal-resolution data like EEG [30]. |
| Structural Equation Modeling (SEM) | Effective | Tests the causal strength of connections within a pre-specified anatomical model. | Testing hypotheses about network interactions based on known neuroanatomy [32]. |
Experimental Protocols
Protocol 1: Conducting a Resting-State fMRI Experiment
Aim: To acquire data for estimating whole-brain functional connectivity networks at rest.
- Participant Preparation: Screen for MRI contraindications. Instruct the participant to lie still with their eyes open, fixating on a cross-hair, and to let their mind wander without falling asleep.
- Data Acquisition: Use a standard EPI sequence on a 3T MRI scanner. Acquisition parameters: TR = 2000 ms, TE = 30 ms, voxel size = 3x3x3 mm³, whole-brain coverage, ~10-15 minutes duration (300-450 volumes).
- Preprocessing Pipeline:
- Slice Timing Correction: Correct for acquisition time differences between slices.
- Realignment: Correct for head motion using a rigid-body transformation.
- Coregistration: Align the functional images to the participant's high-resolution T1-weighted anatomical scan.
- Normalization: Warp the images to a standard stereotaxic space (e.g., MNI).
- Spatial Smoothing: Apply a Gaussian kernel (e.g., 6-8 mm FWHM) to increase signal-to-noise ratio.
- Nuisance Regression: Regress out signals from white matter, cerebrospinal fluid, and the global signal, along with the 24 motion parameters.
- Band-Pass Filtering: Apply a filter (e.g., 0.008-0.09 Hz) to retain low-frequency fluctuations of interest.
Protocol 2: Applying Spectral DCM to rs-fMRI Data
Aim: To estimate the directed effective connectivity within a defined brain network during rest [29].
- Region of Interest (ROI) Selection:
- Based on your hypothesis (e.g., a reward network in addiction), select key ROIs (e.g., Ventral Striatum, Prefrontal Cortex, Amygdala).
- Extract the principal eigenvariate of the BOLD time series from each ROI.
- Model Specification:
- Define a model architecture (the "A" matrix) that specifies which regions are allowed to be connected.
- Set Bayesian priors on the strength and variance of these connections.
- Model Estimation:
- Use the spectral DCM algorithm (e.g., as implemented in SPM12) to fit the model. The algorithm optimizes the effective connectivity parameters to best explain the observed cross-spectral density of the ROI time series.
- Model Comparison & Inference:
- If you have multiple competing model architectures, use Bayesian model selection to identify the model that best explains the data.
- For the winning model, inspect the posterior parameter estimates to determine the strength and direction (excitatory/inhibitory) of the effective connections.
Signaling Pathways and Workflows
Diagram 1: Spectral DCM estimation from BOLD signal.
Diagram 2: Simplified addiction neurocircuitry model.
The Scientist's Toolkit
Table 3: Essential research reagents and computational tools for connectivity analysis.
| Item / Tool | Function / Purpose | Example / Note |
|---|---|---|
| fMRI Scanner | Acquires the BOLD signal by measuring changes in blood oxygenation related to neural activity. | Typically a 3T or 7T MRI scanner with appropriate head coils [28]. |
| Standardized Brain Atlas | Provides a parcelation of the brain into distinct regions for defining network nodes. | Automated Anatomical Labeling (AAL), Harvard-Oxford Atlas. |
| Preprocessing Software | Corrects for artifacts and standardizes data before analysis. | FSL, SPM, AFNI, fMRIPrep. |
| Spectral DCM Toolbox | Software implementation for performing Spectral DCM analysis. | Available within the SPM12 software package [29]. |
| Programmatic Visualization Library | Generates reproducible, high-quality figures of brain networks and connectivity matrices. | Nilearn (Python), ggseg (R), BrainNet Viewer (MATLAB) [31]. |
Frequently Asked Questions (FAQs) and Troubleshooting
This section addresses common technical and methodological questions researchers encounter when applying neuromodulation techniques to study addiction neurocircuitry.
Q1: What are the most effective cortical targets and parameters for reducing drug craving in substance use disorders (SUDs)?
A1: Targeting the dorsolateral prefrontal cortex (DLPFC) is most supported by evidence. A 2024 systematic review and meta-analysis found that repetitive Transcranial Magnetic Stimulation (rTMS) applied to the left DLPFC produced medium to large effect sizes in reducing substance use and craving [34]. For Transcranial Direct Current Stimulation (tDCS), protocols often use anodal stimulation of the right DLPFC (to enhance inhibitory control) or cathodal stimulation of the left DLPFC (to reduce reward-based motivation), also yielding medium effect sizes, though results are more variable [34]. The efficacy is significantly higher when multiple stimulation sessions are applied rather than single sessions [34].
Q2: A subject in our Deep TMS study experienced a seizure. What are the immediate steps and how should the incident be investigated?
A2: Although rare, seizures can occur. Immediate steps include [35]:
- Cease stimulation immediately.
- Ensure medical safety; manage the seizure following standard medical protocols (e.g., protecting from injury).
- Transport to emergency services if necessary.
- Report the event to your Institutional Review Board (IRB) and the device manufacturer.
A thorough investigation should review:
- Subject eligibility: Screen for pre-existing neurological conditions, brain injury, or history of seizures [35] [36].
- Concomitant medications: Review medications, particularly those known to lower the seizure threshold (e.g., high doses of antidepressants) [35].
- Substance use: Assess recent alcohol or drug consumption, as high alcohol intake the night before treatment has been linked to seizure occurrence during TMS [35].
- Device parameters: Verify that stimulation intensity and pattern were within recommended safety guidelines [36].
Q3: Our DBS system for addiction research is yielding suboptimal symptom relief. What is a systematic approach to troubleshooting?
A3: Suboptimal outcomes in DBS can arise from multiple factors. A systematic troubleshooting clinic model, as developed by the University of Florida, involves a comprehensive, multi-disciplinary evaluation [37]:
- Clinical Re-evaluation: Re-assess the patient's current status, including standardized rating scales in different medication and stimulation states. This can take 1-2 hours [37].
- Lead Placement Verification: Import post-operative MRI or CT imaging into a 3-D brain atlas to verify the location of the DBS lead. A misplaced or sub-optimally placed lead is a common cause of failure [37].
- Programming Optimization: Systematically test the thresholds for clinical benefit and side effects on every contact of the DBS lead. Based on this mapping, attempt to reprogram the patient with new parameters [37].
- Medication Adjustment: Review and adjust concomitant medications, as the interaction between stimulation and medication is critical [37].
- Surgical Re-evaluation: If the lead is confirmed to be misplaced and reprogramming is ineffective, surgical repositioning may be considered [37].
Q4: What are the critical safety contraindications for Deep TMS and TBS studies?
A4: The primary safety concern involves the interaction of the magnetic field with metal or implanted electronic devices [35] [36].
- Absolute Contraindications: The presence of ferromagnetic metal implants in or near the head, such as aneurysm clips or coils, stents, bullet fragments, or magnetic implants [35] [36]. Implanted electronic devices anywhere in the body, including pacemakers, implantable cardioverter defibrillators (ICDs), vagus nerve stimulators, or deep brain stimulators, are also absolute contraindications due to risk of malfunction [35] [36].
- Hearing Protection: The loud clicking sound generated by the TMS coil requires the use of earplugs with a rating of at least 30 dB noise reduction to prevent potential hearing loss [35].
Q5: How do I choose between rTMS and Theta-Burst Stimulation (TBS) protocols for an addiction study?
A5: The choice depends on the desired neurophysiological effect and practical considerations.
- Protocol Efficiency: Standard rTMS protocols for depression, which target the prefrontal cortex, can last 20-37 minutes per session [36]. In contrast, an intermittent TBS (iTBS) protocol can produce similar neuroplastic effects in just 3.5 minutes [36], offering a significant advantage for subject compliance and study throughput.
- Neurophysiological Target: Generally, high-frequency (≥5 Hz) rTMS and iTBS are used to increase cortical excitability, while low-frequency (≤1 Hz) rTMS and continuous TBS (cTBS) are used to induce cortical inhibition [34] [36]. For addiction, excitatory protocols over the left DLPFC or inhibitory protocols over the right DLPFC are common targets based on the hypothesis being tested [34].
The tables below summarize key quantitative findings from recent meta-analyses and clinical studies on neuromodulation for Substance Use Disorders (SUDs).
Table 1: Meta-Analysis of rTMS and tDCS Efficacy for Alcohol and Tobacco Use Disorders (2024)
| Parameter | rTMS (Hedge's g) | tDCS (Hedge's g) | Notes |
|---|---|---|---|
| Substance Use & Craving | Medium to Large (> 0.5) | Medium (highly variable) | rTMS effects are more robust [34] |
| Key Target | Left DLPFC | Right Anodal DLPFC | Right-sided anodal tDCS may help rebalance hemispheric asymmetry [34] |
| Session Number | Multiple sessions | Multiple sessions | Single sessions are significantly less effective [34] |
Table 2: Common Adverse Events in a Deep TMS Clinical Trial for Depression
| Adverse Event | Deep TMS Group (%) | Sham Group (%) | Likelihood Caused by TMS |
|---|---|---|---|
| Headache | 47% | 36% | No (Similar to sham) |
| Application Site Discomfort | 25%-29% | <1%-4.1% | Yes |
| Pain in Jaw | 10.2% | <1% | Yes [35] |
Experimental Protocols
This section provides detailed methodologies for key experiments cited in the literature.
Protocol 1: Standardized DBS Troubleshooting for Suboptimal Outcomes
This protocol is adapted from the University of Florida's DBS Failures Clinic [37].
- Objective: To systematically identify and correct the causes of suboptimal outcomes in Deep Brain Stimulation for movement or neuropsychiatric disorders.
- Materials: Standardized clinical rating scales, MRI/CT imaging suite, 3-D brain atlas software, DBS programming kit.
- Procedure:
- Comprehensive Clinical Assessment (1-2 hours): The patient undergoes standardized clinical rating scales (e.g., UPDRS for Parkinson's) in four potential states: ON-medication/ON-stimulation, ON-medication/OFF-stimulation, OFF-medication/ON-stimulation, and OFF-medication/OFF-stimulation [37].
- Imaging and Lead Localization: Post-operative MRI or CT images are imported into a 3-D brain atlas. The actual position of the DBS lead is co-registered with the preoperative surgical plan to verify placement [37].
- Systematic Programming & Thresholding: For each contact on the DBS lead, the thresholds for therapeutic benefit and for side effects (e.g., muscle contractions, paresthesia) are meticulously determined and recorded [37].
- Interdisciplinary Team Review: The patient's case is presented to a full team, including a neurologist, neurosurgeon, neuropsychologist, and rehabilitation therapists. Based on all data, a consensus decision is made on management: medication adjustment, new stimulation parameters, or surgical intervention [37].
Protocol 2: rTMS/tDCS for Craving Reduction in Substance Use Disorders
This protocol synthesizes methods from the 2024 meta-analysis [34].
- Objective: To assess the effect of multi-session non-invasive brain stimulation on cue-induced craving in participants with a specific SUD.
- Materials: rTMS or tDCS device with sham capability, EEG cap or measuring tape for 10-20 system positioning, validated craving scales (e.g., OCDS, VAS), substance-specific cues (e.g., images, paraphernalia).
- Procedure:
- Screening & Randomization: Participants meeting DSM-5 criteria for a SUD are screened for contraindications and randomly assigned to active or sham stimulation groups.
- Target Localization: The DLPFC target is identified using the 10-20 EEG system (F3 for left DLPFC, F4 for right DLPFC) or, preferably, neuronavigation based on the individual's MRI [34].
- Stimulation Protocol (Sample):
- rTMS: 10-20 sessions of high-frequency (e.g., 10 Hz) stimulation delivered to the left DLPFC. Intensity is set at 100-120% of the resting motor threshold [34].
- tDCS: 10-20 sessions of stimulation (e.g., 2 mA for 20 minutes) with the anode over the right DLPFC and the cathode over the left DLPFC or a supraorbital region [34].
- Outcome Measurement: Craving is assessed before and after each session using a visual analog scale (VAS). Cue-induced craving is measured before the first and after the last session by exposing participants to drug-related cues and rating craving intensity [34].
- Biochemical Verification: Substance use is verified through urine toxicology or breathalyzer tests at regular intervals [34].
Signaling Pathways and Experimental Workflows
The following diagrams, generated using DOT language, illustrate key neurocircuitry and methodological workflows.
DBS Troubleshooting Workflow
Addiction Cycle Neurocircuitry Framework
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and equipment essential for research in neuromodulation and addiction neurocircuitry analysis.
Table 3: Essential Research Materials for Neuromodulation Studies in Addiction
| Item | Function in Research | Example/Notes |
|---|---|---|
| Deep TMS H-Coil | Allows stimulation of deeper and broader brain structures (e.g., up to 3.2 cm) compared to figure-8 coils, potentially targeting insula and NAc circuits [34]. | Used in FDA-cleared protocols for smoking cessation [34]. |
| Theta-Burst Stimulation (TBS) Protocol | Enables rapid induction of neuroplasticity, mimicking natural brain rhythms. iTBS (excitatory) and cTBS (inhibitory) can be delivered in minutes [36]. | Significantly reduces protocol duration (e.g., 3.5 min vs. 20-37 min) [36]. |
| Neuronavigation System | Uses individual MRI data and infrared tracking to precisely position TMS/tDCS coils/electrodes over target brain regions, improving accuracy and reproducibility [34]. | Critical for targeting specific cortical areas like the DLPFC. |
| Validated Craving Scales | Quantifies the subjective experience of craving, a primary outcome in SUD trials. | Obsessive Compulsive Drinking Scale (OCDS), Visual Analog Scale (VAS) [34]. |
| Biochemical Verification Kits | Objectively verifies self-reported substance use and abstinence, reducing bias in study outcomes. | Urine drug screens, breathalyzers for alcohol, cotinine tests for smoking [34]. |
| High-Density EEG System | Measures brain activity and connectivity before, during, and after neuromodulation, helping to elucidate mechanisms of action and identify biomarkers of response. | Can be integrated with TMS (TMS-EEG) to directly assess cortical excitability and plasticity [38]. |
FAQ: Troubleshooting Common Experimental Challenges
1. We are observing inconsistent effects on drug-seeking behavior after dlPFC stimulation. What could be the cause? Inconsistent outcomes in dlPFC stimulation often relate to electrode placement and neuronal sub-population targeting. The dlPFC influences drug-seeking through an indirect pathway to the vmPFC. If your stimulation site is not optimally connected to this vmPFC pathway, effects may be weak or variable [39]. Furthermore, the behavioral context (e.g., active drug-seeking vs. extinction) is critical; the dlPFC's role can appear facilitatory or inhibitory depending on the experimental paradigm [40]. Ensure you are using neuronavigation systems based on individual subject anatomy and verify your target's connectivity to the vmPFC using tractography or other circuit-mapping techniques [41].
2. How can we definitively distinguish the causal roles of vmPFC sub-regions (e.g., PL vs IL) in our behavioral models? The prelimbic (PL) and infralimbic (IL) cortices have complex, sometimes overlapping roles. A simple "PL-seeks, IL-extinguishes" dichotomy does not always hold [40]. To troubleshoot, employ projection-specific manipulations. For example, use retrograde viruses to selectively target PL or IL neurons that project to a specific downstream target like the nucleus accumbens (NAc) or basolateral amygdala (BLA). In vivo calcium imaging reveals that these distinct pathways are differentially active during anxiety (mPFC→BLA) versus exploratory and positive social behaviors (mPFC→NAc) [42]. Your results may vary based on the specific downstream target of your manipulated neurons.
3. Our neuromodulation of the vmPFC leads to unexpected changes in risk-taking behavior. Is this relevant to addiction? Yes, this is highly relevant. The vmPFC is critically involved in valuation and decision-making processes that are fundamental to addiction. Inhibitory continuous Theta Burst Stimulation (cTBS) over the vmPFC has been shown to increase risk-taking behavior in a gambling task, an effect similar to that seen after inhibition of the right dlPFC [43]. This suggests that the vmPFC calculates the appeal or value of options, and disrupting this process can make riskier choices (like drug use) more likely. This behavioral assay can be a valuable tool for quantifying the cognitive effects of your vmPFC interventions.
4. What are the primary considerations when choosing a brain stimulation target for a new addiction therapeutic? Current frameworks recommend a three-phase approach [41]:
- Phase 1: Identify the Circuit. Use convergent approaches, including:
- Lesion Network Mapping: Identifying networks where lesions cause a symptom change (e.g., reduced addiction severity) can reveal effective neuromodulation targets.
- Retrospective Optimization: Analyze existing brain stimulation data to find sites where stimulation was most effective and map their connectivity.
- Neuroimaging Correlates: Use large-scale meta-analyses to find brain networks associated with addiction symptoms, but be cautious of the "causality gap" where correlations may not be therapeutic targets [41].
- Phase 2: Personalize the Target. Use individual neuroimaging to define the target based on the circuit identified in Phase 1.
- Phase 3: Choose the Modality. Select the appropriate technology (e.g., TMS, tDCS, DBS) based on its ability to modulate your chosen target.
Experimental Protocols & Methodologies
Protocol 1: Modulating dlPFC-vmPFC Circuitry with tDCS in Addiction
This protocol is based on a study demonstrating that bilateral tDCS over the dlPFC reduces drug craving and relapse, with effects mediated through increased activation of the vmPFC [39].
- Objective: To assess the effect of dorsolateral prefrontal cortex (dlPFC) transcranial direct current stimulation (tDCS) on ventral medial prefrontal cortex (vmPFC) activity and drug-seeking behavior.
- Subjects: Individuals with alcohol or crack-cocaine dependence.
- Stimulation Parameters:
- Type: Bilateral tDCS.
- Electrode Placement: Cathodal left dlPFC; Anodal right dlPFC.
- Current Intensity: 2 mA.
- Electrode Size: 35 cm².
- Session Schedule: Five daily sessions (repetitive stimulation).
- Outcome Measures:
- Craving: Self-report questionnaires and behavioral tasks.
- Relapse: Drug use confirmed by toxicology screens during and after treatment.
- vmPFC Activity: Measured via Low Resolution Electromagnetic Tomography (LORETA) analysis of Event-Related Potentials (ERPs), specifically the P3 segment (300-500 ms) under drug-related cue exposure.
- Structural Connectivity: Assessed via Diffusion Tensor Imaging (DTI) parameters (Fractional Anisotropy, Apparent Diffusion Coefficient) in the vmPFC to NAcc pathway.
- Troubleshooting Note: The vmPFC is the hypothesized target, but its activation is an outcome of dlPFC stimulation. Verify target engagement with concurrent fMRI or EEG if possible.
Protocol 2: Dissecting vmPFC Sub-Region Contributions with Projection-Specific Imaging
This protocol leverages modern circuit-tracing and imaging to delineate the functions of distinct mPFC descending pathways [42].
- Objective: To characterize the activity patterns of mPFC neurons projecting to the basolateral amygdala (BLA) vs. the nucleus accumbens (NAc) during emotional and exploratory behaviors.
- Subjects: Adult wildtype mice (~20 weeks old).
- Viral Vector Strategy:
- Inject retrograde AAV viruses carrying GCaMP6m into the BLA and NAc of the same subject.
- This results in GCaMP6m expression in the soma of mPFC→BLA and mPFC→NAc neurons within the medial prefrontal cortex.
- In Vivo Imaging:
- Use a portable miniaturized microscope to record calcium transients from the mPFC.
- Synchronize calcium imaging data with video recordings of behavior.
- Behavioral Assays:
- Open Field Test (OFT): To assess anxiety-like (corner-dwelling) and exploratory (center-dwelling, sniffing) behaviors.
- Social Competition Paradigm: To induce positive and negative emotional states.
- Data Analysis:
- Calculate Ca²⁺ transient rates for each neuronal population during specific behaviors.
- Perform Principal Component Analysis (PCA) on population activity to visualize and quantify how different behaviors are neurally encoded.
- Expected Results: mPFC→BLA neurons, particularly "center-ON" cells, will show heightened activity during anxiety-related behaviors. mPFC→NAc neurons will be more active during exploratory and socially rewarding behaviors [42].
Table 1: Comparative Effects of dlPFC and vmPFC Neuromodulation on Behavior
This table summarizes key findings from human and animal studies to guide hypothesis generation.
| Brain Target | Stimulation Type | Behavioral Effect | Proposed Mechanism | Source |
|---|---|---|---|---|
| dlPFC | Bilateral tDCS (cathodal L / anodal R) | ↓ Craving & relapse in addiction; ↑ vmPFC activation | Increased top-down control; enhanced activation of vmPFC to extinguish drug-seeking | [39] |
| vmPFC | Inhibitory cTBS | ↑ Risk-taking behavior | Reduced valuation of risky options, impairing cost-benefit analysis | [43] |
| Right dlPFC | Inhibitory cTBS | ↑ Risk-taking behavior; ↑ Response time | Reduced cognitive control over impulsive choices | [43] |
| Prelimbic (PL) mPFC | Chemogenetic/Optogenetic | Context-dependent ↑ or ↓ drug seeking | Drives drug-seeking via projections to NAc core; function is state-dependent | [40] [44] |
| Infralimbic (IL) mPFC | Chemogenetic/Optogenetic | Context-dependent ↓ or ↑ drug seeking | Suppresses drug-seeking after extinction; can drive seeking in other contexts | [40] [44] |
Table 2: Key Neurocircuitry Targets in the Three Stages of Addiction
This table aligns circuit elements with the widely used three-stage addiction cycle model [13] [6].
| Addiction Stage | Core Circuitry | Key Neurotransmitters | Potential Intervention Target |
|---|---|---|---|
| Binge/Intoxication | Ventral Tegmental Area (VTA) → Ventral Striatum (NAc) | Dopamine ↑, Opioid peptides ↑ | VTA dopamine neurons; NAc medium spiny neurons |
| Withdrawal/Negative Affect | Extended Amygdala | Corticotropin-releasing factor (CRF) ↑, Dynorphin ↑, Dopamine ↓ | Bed nucleus of the stria terminalis; Central amygdala |
| Preoccupation/Anticipation (Craving) | dlPFC, vmPFC/OFC, Basolateral Amygdala, Hippocampus | Glutamate ↑, Dopamine ↑ (in some areas) | dlPFC-vmPFC circuit; Corticostriatal projections from mPFC to NAc |
Research Reagent Solutions
A list of essential materials and their applications for studying PFC pathways.
| Reagent / Tool | Primary Function | Example Application |
|---|---|---|
| Transcranial Direct Current Stimulation (tDCS) | Non-invasive neuromodulation to increase (anodal) or decrease (cathodal) cortical excitability. | Bilateral dlPFC stimulation to treat addiction [39]. |
| Continuous Theta Burst Stimulation (cTBS) | A form of repetitive TMS that generally inhibits cortical activity. | Testing functional relevance of rDLPFC and vmPFC in risk-taking behavior [43]. |
| GCaMP6m / jGCaMP7s | Genetically encoded calcium indicators for monitoring neuronal activity in real-time. | In vivo calcium imaging of mPFC→BLA and mPFC→NAc neurons during behavior [42]. |
| Retrograde AAV Vectors (e.g., AAV2/Retro) | Viruses that travel backward across synapses to label or manipulate neurons based on their projection targets. | Specifically targeting mPFC neurons that project to the BLA or NAc for imaging or optogenetics [42]. |
| Low Resolution Electromagnetic Tomography (LORETA) | A computational method to localize the sources of electrical activity in the brain from EEG signals. | Source analysis showing vmPFC is activated by drug cues after effective dlPFC tDCS [39]. |
| Diffusion Tensor Imaging (DTI) | An MRI technique that maps white matter tracts by measuring water diffusion. | Quantifying structural integrity (Fractional Anisotropy) in the vmPFC-NAcc pathway [39]. |
Pathway & Workflow Diagrams
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My multimodal model's performance is worse than models using single data types. What could be the cause? This is typically caused by incorrect data alignment or failure to account for heterogeneity between modalities. Ensure temporal synchronization of time-series data (e.g., EEG) with other data streams and perform spatial registration for imaging data. The Ensemble Integration (EI) approach, which builds local models from each modality before combining them, often outperforms early integration methods that force data into a uniform representation [45].
Q2: How can I handle missing data points across different modalities in my addiction neurocircuitry dataset? Use late integration strategies like EI, which are inherently robust to missing modalities. EI trains separate predictive models on each complete data modality (e.g., fMRI, genomic sequences, clinical notes) and then aggregates their predictions. This allows the global model to function even if data for one modality is missing for a specific subject [46] [45].
Q3: What is the best way to integrate genomic data with neuroimaging data for addiction vulnerability studies? Given the semantic and structural differences between these modalities, employ a systematic late integration framework. Process the sequence-based genomic data and array-based neuroimaging data through separate, modality-appropriate algorithms. A heterogeneous ensemble method can then integrate these specialized local models into a unified predictor [45].
Q4: How can I make my complex multimodal ensemble model for addiction staging more interpretable for clinical audiences? Implement a post-hoc interpretation framework for your ensemble model. For example, after building an EI model to predict addiction stage or treatment outcome, you can identify and report the key features from each modality (e.g., specific clinical lab values, neuroimaging markers, or genetic variants) that most heavily influenced the predictions [45].
Q5: My dataset is relatively small. Can I still effectively use multimodal integration for addiction research? Yes, leverage transfer learning. Knowledge gained from analyzing one modality (e.g., structural MRI patterns) can be transferred to improve performance in another, reducing the data requirements for new applications. Furthermore, multimodal models are less likely to overfit to artifacts in any single data type [46].
Troubleshooting Experimental Protocols
Issue: Inconsistent Results from Multimodal Predictive Models
| Troubleshooting Step | Action | Example from Addiction Neurocircuitry |
|---|---|---|
| Verify Data Alignment [46] | Check and correct for temporal or spatial misalignment between data streams. | Synchronize cue-induced fMRI BOLD signals with simultaneously recorded physiological (EDA, ECG) data. |
| Audit Data Quality [46] | Assess quality, accuracy, and reliability for each modality; quality often varies. | In a model combining EEG and self-report, one modality (e.g., EEG) may be compromised by artifact. |
| Re-evaluate Integration Method [45] | If an early integration model is underperforming, switch to a late integration (EI) approach. | Separately model genetic, clinical, and neuroimaging data before ensemble aggregation to predict relapse risk. |
| Check for Information Redundancy [46] | Analyze whether modalities provide complementary information or are too similar. | Ensure that structural MRI (gray matter density) and DTI (white matter integrity) provide unique signals. |
Issue: Difficulty Visualizing or Interpreting Model Outputs for Addiction Staging
| Troubleshooting Step | Action | Example from Addiction Neurocircuitry |
|---|---|---|
| Implement a Visualization Framework [47] | Use a color-coded system to translate complex model outputs into 2D/3D renderings. | Generate a color-coded image from baseline data to visually represent predicted progression through addiction stages (binge, withdrawal, preoccupation). |
| Perform Feature Importance Analysis [45] | Use model interpretation methods to identify top predictive features from each modality. | In an EI model predicting transition to compulsion, identify key contributors: striatal fMRI activation, stress hormone levels, specific genetic polymorphisms. |
| Simplify for Communication [47] | Use established color palettes to represent different data types or prediction certainty levels. | Apply a severity color palette to highlight brain regions most implicated in the predicted addiction stage (e.g., basal ganglia, extended amygdala, prefrontal cortex). |
Experimental Protocols for Multimodal Integration
Protocol 1: Ensemble Integration for Predictive Modeling
Objective: To accurately predict a clinical outcome (e.g., mortality, treatment response, disease progression) by integrating heterogeneous data modalities [45].
Detailed Methodology:
- Data Preparation and Local Model Training:
- Process each data modality independently, applying appropriate preprocessing (normalization, feature scaling).
- For each modality, train multiple local predictive models using diverse algorithms (e.g., SVM, Random Forest, Logistic Regression). Handle class imbalance via techniques like random under-sampling of the majority class.
- Ensemble Construction:
- Use the base predictions from the local models as inputs for heterogeneous ensemble methods.
- Mean Aggregation: Calculate the mean of the base prediction scores.
- Iterative Ensemble Selection (CES): Start with an empty ensemble and iteratively add the local model that most improves performance.
- Stacking: Use the base predictions as features to train a second-level meta-predictor (e.g., XGBoost, Logistic Regression).
- Model Interpretation:
- Apply an interpretation framework to the final ensemble model to identify which features from which modalities were most influential in the predictions.
Protocol 2: Color-Coded Visualization of Disease Trajectory
Objective: To create an intuitive, visual representation of disease diagnosis and prognosis (e.g., staging in addiction) from baseline multimodal data [47].
Detailed Methodology:
- Input Tensorization:
- Assemble a feature vector from baseline multimodal measurements. Exclude target labels (e.g., CDR-SB in dementia) and highly correlated scores to avoid bias.
- Normalize each feature across the dataset.
- Model Architecture and Training:
- Employ a convolutional neural network (CNN) designed for image generation.
- The model takes the baseline feature vector as input and is trained to output a color-coded image that reflects the disease state at future time points.
- Visual Output and Evaluation:
- Generate the output images (e.g., 23x23 or 45x45 pixels). Different colors and strips in the image correspond to different aspects of the disease trajectory.
- Evaluate the model's diagnostic and prognostic accuracy using cross-validation and subjective ratings by human experts.
Table 1: Performance Comparison of Data Integration Methods on a Protein Function Prediction Task (Adapted from [45])
| Integration Method | Average AUC | Key Advantage |
|---|---|---|
| Early Integration | 0.72 | Simpler initial implementation |
| Intermediate Integration | 0.75 | Reinforces consensus among modalities |
| Ensemble Integration (EI) | 0.81 | Preserves exclusive local information from each modality |
Table 2: Performance of the ML4VisAD Visualization Model on Alzheimer's Disease Classification (Adapted from [47])
| Classification Task | Accuracy | Visual Rendering Speed |
|---|---|---|
| 3-way Classification (CN, MCI, AD) | 0.82 ± 0.03 | 0.08 msec (for 23x23 image) |
| 5-way Classification (More detailed stages) | 0.68 ± 0.05 | 0.17 msec (for 45x45 image) |
Signaling Pathways, Workflows & Logical Diagrams
Ensemble Integration Data Workflow
Addiction Neurocircuitry Framework
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Multimodal Data Integration in Addiction Research
| Tool or Resource | Function | Example Use in Addiction Neurocircuitry |
|---|---|---|
| Heterogeneous Ensemble Algorithms (Mean, Stacking, CES) [45] | Integrates predictions from local models trained on different data types into a final, robust prediction. | Combining predictions from genetic, fMRI, and clinical data models to forecast individual relapse risk. |
| Interpretation Framework for Ensemble Models [45] | Identifies key predictive features from each modality, making the complex ensemble model understandable. | Revealing that a specific stress biomarker (CRF), a prefrontal cortex activity pattern, and an OPRM1 genotype are top predictors of compulsive drug seeking. |
| Color-Coded Visualization Model (e.g., ML4VisAD) [47] | Translates complex, high-dimensional baseline data into an intuitive 2D/3D visual prognosis. | Generating a visual map from a patient's baseline data to show the predicted progression through the three stages of the addiction cycle. |
| Data Modality-Specific Algorithms (e.g., CNNs for imaging, RNNs for sequences) [48] | Provides the optimal architecture for building accurate local models on specific data types before integration. | Using CNNs to analyze structural MRI scans of the basal ganglia and RNNs to model longitudinal electronic health record data. |
| Standardized Color Palettes for Data Viz [49] | Ensures visualizations are clear, accessible, and consistently interpretable across different charts and outputs. | Applying a severity palette to a brain connectivity map to highlight the degree of functional impairment in the prefrontal cortex-executive control circuit. |
Addressing Analytical Hurdles: Individual Variability, Technical Limitations, and Optimization Strategies
FAQs: Addressing Core Challenges in Addiction Neurocircuitry Research
FAQ 1: Why do neurocircuitry findings in addiction research often fail to generalize across different study populations?
Individual variability is a fundamental property of neural systems, not merely experimental noise. This variability arises from a combination of genetic factors, environmental influences, and unique life experiences that shape each individual's brain connectivity and function [50] [51]. Furthermore, addiction is etiologically heterogeneous, meaning it encompasses multiple neurobiological subtypes (biotypes) that may present with similar behavioral symptoms but have distinct underlying neural circuit dysfunctions [52] [53]. Applying uniform neurocircuitry models without accounting for these subtypes dilutes statistical power and obscures clinically meaningful signals.
FAQ 2: What is a "biotype" in the context of addiction research, and how is it identified?
A biotype is a subgroup of individuals defined by distinct biological markers, rather than solely by behavioral symptoms. In addiction, biotypes are identified through data-driven approaches that integrate neuroimaging, clinical, and genetic data [52] [53]. For example, machine learning algorithms can partition individuals with Alcohol Use Disorder (AUD) based on their unique patterns of whole-brain functional connectivity (FC) derived from resting-state fMRI. These connectivity-based biotypes often correlate with specific clinical profiles, such as the presence of co-occurring anxiety and depression, and are associated with different genetic risk variants [52].
FAQ 3: How can we account for neural variability in experimental design and analysis?
Instead of averaging it out, researchers can harness neural variability by:
- Biotyping: Classifying participants into more homogeneous subgroups before comparing them to healthy controls [52] [53].
- State-Sensitive Protocols: Using non-invasive brain stimulation (NIBS) or other interventions that are calibrated to an individual's baseline neural state, moving toward a probabilistic framework for personalization [54].
- Advanced Modeling: Employing computational frameworks like active inference, which explicitly model how the brain represents and resolves different types of uncertainty (like novelty and variability) during decision-making [55].
FAQ 4: Which neural circuits are most frequently implicated in addiction biotypes?
Research has consistently highlighted dysfunction in several large-scale brain networks, though the specific nature of the dysfunction can vary by biotype. Key networks include:
- Default Mode Network (DMN): Often shows altered connectivity associated with self-referential thought and rumination.
- Salience Network (SN): Involved in detecting behaviorally relevant stimuli and switching between networks.
- Frontoparietal Network (FPN): Critical for cognitive control and executive function.
- Limbic Network (LN): Processes emotional and reward-related information.
- Cerebellar and Visual Circuits: Emerging evidence points to the importance of cerebellar connectivity and its interaction with visual processing circuits in distinguishing biotypes, particularly in comorbid AUD and Nicotine Use Disorder (NUD) [56] [52].
Troubleshooting Guides
Guide 1: Diagnosing and Addressing Poor Classifier Performance in Biotyping Studies
Problem: A machine learning model trained to distinguish individuals with a substance use disorder from healthy controls is performing at or near chance levels.
| Diagnostic Step | Evidence of the Issue | Recommended Solution |
|---|---|---|
| Check for Heterogeneity | High within-group variance in functional connectivity features; model fails to learn consistent patterns. | Shift from case-control to a biotyping paradigm. Use unsupervised clustering (e.g., k-means) on connectivity features to identify data-driven subgroups within the clinical population first [52] [53]. |
| Validate Biotypes | Clusters appear arbitrary and do not correlate with external clinical measures. | Ensure biotypes are clinically meaningful. Validate that the identified connectivity biotypes show significant differences in independent measures like drinking frequency, antisocial personality scores, or genetic markers [53]. |
| Refine Classification | Single-task classifier performance remains poor. | Implement a Multi-task Learning (MTL) artificial neural network. Jointly infer biotype membership and diagnosis, as this has been shown to achieve higher accuracy (AUC: 0.76 for AUD) than single-task models (AUC: 0.61) [52]. |
Guide 2: Managing Neural Variability in Non-Invasive Brain Stimulation (NIBS) Studies
Problem: Transcranial Magnetic Stimulation (TMS) produces highly variable motor-evoked potentials (MEPs) across trials in the same subject, complicating the measurement of cortical excitability.
| Diagnostic Step | Evidence of the Issue | Recommended Solution |
|---|---|---|
| Identify Variability Type | MEP amplitude and latency fluctuate significantly despite identical stimulation parameters [51]. | Classify the variability. It may be "genuine neutral" (degeneracy, where different neural activity patterns produce the same output) or "genuine useful" (the basis for neuroplasticity). It is rarely pure "noise" [51]. |
| Control for Known Factors | Variability is exacerbated by uncontrolled factors. | Systematically control for and document factors known to influence MEPs: stimulation intensity, voluntary muscle contraction, time of day, hormonal cycles, and participant anxiety levels [51] [54]. |
| Change the Framework | Viewing variability as a problem to be eliminated. | Harness the variability. Adopt a probabilistic framework that incorporates inter-individual and intra-individual variability as a feature. Adjust stimulation protocols to the individual's instantaneous brain state, measured with EEG or other real-time monitoring, to improve outcomes [54]. |
Experimental Protocols
Protocol 1: Identifying Addiction Biotypes Using Functional Connectivity and Machine Learning
This protocol is adapted from large-scale biotyping studies of AUD and NUD [52] [53].
1. Participant Selection & Clinical Assessment:
- Participants: Recruit individuals with the addiction phenotype (e.g., AUD) and healthy controls (HCs). Large samples are critical (e.g., N > 800).
- Clinical Measures: Collect detailed demographic data and standardized assessments of substance use, including frequency, quantity, and duration. Include measures of co-occurring psychopathology (e.g., depression, anxiety, antisocial personality traits) [53].
- Genotyping: Collect DNA samples for subsequent genetic association analysis.
2. fMRI Data Acquisition & Preprocessing:
- Acquisition: Acquire resting-state fMRI (rs-fMRI) data on a 3T scanner. A 6-minute eyes-open resting-state scan is typical (e.g., TR=0.735s) [52].
- Preprocessing: Process data using standard pipelines (e.g., with SPM12 or FSL). Steps include:
- Realignment and motion correction.
- Co-registration to high-resolution T1-weighted structural images.
- Normalization to a standard brain space (e.g., MNI).
- Smoothing with a Gaussian kernel.
- Regression of covariates (e.g., motion parameters, white matter, and CSF signals).
- Temporal band-pass filtering (e.g., 0.009–0.08 Hz) to focus on low-frequency fluctuations [53].
3. Feature Extraction:
- Functional Connectivity (FC): Parcellate the brain into defined regions (e.g., 268 regions from a predefined atlas). Calculate pairwise Pearson correlation coefficients between the time series of every region pair to create a subject-specific FC matrix. The unique correlations (e.g., 35,778 from 268 regions) serve as the feature set for machine learning [52].
4. Biotype Identification via Machine Learning:
- Feature Selection & Dimensionality Reduction: On the training set, regress out effects of age and sex from each FC feature. Apply feature selection (e.g., based on relationship to clinical metrics) and dimensionality reduction (e.g., Principal Component Analysis).
- Clustering: Apply an unsupervised clustering algorithm (e.g., k-means) to the reduced FC data from the clinical group (AUD/NUD) only to identify distinct biotypes.
- Validation: Validate the stability and clinical relevance of biotypes by demonstrating that they differ significantly on external clinical measures not used in the clustering (e.g., severity of use, antisocial personality scores) [53].
5. Genetic Association Analysis:
- Candidate Gene Analysis: Test for associations between the identified biotypes and specific single nucleotide polymorphisms (SNPs) in candidate genes previously linked to the addiction phenotype. A biotype-specific analysis can reveal genetic risk variants that are obscured in a heterogeneous case-control comparison [53].
Diagram: Functional Connectivity Biotyping Workflow
Protocol 2: Modeling Decision-Making Under Uncertainty with Active Inference
This protocol uses a computational framework to dissect the neural correlates of variability and novelty in decision-making, which is central to addictive behaviors [55].
1. Task Design: Contextual Two-Armed Bandit:
- Structure: On each trial, participants choose between a "Safe" option (constant reward) and a "Risky" option (variable reward).
- Key Manipulation: The reward distribution of the "Risky" option depends on an unobserved "context" (e.g., Context 1: high reward, Context 2: low reward).
- Critical "Cue" Option: Participants can choose to pay a cost to reveal the current context of the "Risky" option before making their choice. This allows them to actively resolve uncertainty ("novelty") about the environment [55].
2. Data Collection:
- Behavioral Data: Record all choices and outcomes.
- Neural Data: Simultaneously record high-density electroencephalogram (EEG) during task performance.
3. Computational Modeling:
- Model Comparison: Fit both an Active Inference model and a standard Reinforcement Learning model to the behavioral choice data.
- Parameter Estimation: The Active Inference model will estimate trial-by-trial computational variables, including:
- Expected Free Energy (G): The value of a policy, integrating both reward seeking and information seeking.
- Novelty: Uncertainty about the environment that can be reduced by sampling (e.g., using the "Cue").
- Variability: The inherent variance (risk) of a hidden state [55].
4. Neural Correlate Analysis:
- EEG Analysis: Link the trial-by-trial estimates of G, novelty, and variability from the winning model to the EEG data.
- Sensor-Level: Identify scalp topographies associated with high vs. low novelty and variability.
- Source-Level: Use source localization to identify the brain regions (e.g., frontal pole, middle frontal gyrus) where these computational variables are encoded [55].
Diagram: Active Inference in Decision-Making
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in Research |
|---|---|
| Resting-state fMRI (rs-fMRI) | A non-invasive imaging technique used to measure spontaneous, low-frequency brain activity while a participant is at rest. It is the primary method for deriving functional connectivity (FC) matrices, which serve as the core feature set for identifying addiction biotypes [52] [53]. |
| UK Biobank / Human Connectome Project (HCP) Data | Large-scale, publicly available datasets that include neuroimaging, genetic, and detailed behavioral phenotyping. These resources provide the statistical power necessary for robust biotype discovery and validation [52] [53]. |
| SPM12, FSL, CONN | Standard software packages for fMRI data preprocessing and analysis. They are used for critical steps including image realignment, normalization, smoothing, and the statistical extraction of functional connectivity metrics [52] [53]. |
| Unsupervised Clustering Algorithms (e.g., k-means) | Machine learning methods used to identify naturally occurring subgroups (biotypes) within a heterogeneous clinical population without pre-defined labels. They are applied to FC data to partition subjects based on similar connectivity profiles [52]. |
| Multi-task Learning (MTL) Artificial Neural Network | A machine learning architecture that improves classification accuracy by jointly learning multiple related tasks (e.g., inferring AUD and NUD diagnoses simultaneously). It leverages shared information across tasks and has been shown to outperform single-task classifiers in addiction biotyping [52]. |
| Active Inference Model | A computational framework that unifies perception, action, and learning under the principle of free energy minimization. It is used to model decision-making in uncertain environments and can dissociate the neural encoding of different uncertainty types (novelty vs. variability), which are aberrant in addiction [55]. |
| Transcranial Magnetic Stimulation (TMS) | A non-invasive brain stimulation technique. When combined with EMG, it is used to measure cortical excitability (via Motor Evoked Potentials). Understanding and harnessing the trial-to-trial variability in MEPs is a key challenge and opportunity for developing personalized neuromodulation therapies [51] [54]. |
Frequently Asked Questions
FAQ 1: What is the primary limitation of current computational models in addiction research? The primary limitation is that most computational models focus on simple drug-use behaviors rather than modeling the complex, multi-symptomatic nature of addiction itself. Many fail to capture the progression through different stages of addiction or the full range of clinical symptoms outlined in diagnostic criteria [27] [57].
FAQ 2: What are the two main categories of computational models used in this field? Computational models in addiction research generally fall into two broad categories [27]:
- Mathematically-based models: These operate at an algorithmic level, using computational theories to describe processes like learning and decision-making, without making precise mappings to neural circuits.
- Biologically-based models: These operate at an implementational level, linking computational processes to specific brain areas or circuits, such as the prefrontal cortex, basal ganglia, and the dopamine system.
FAQ 3: Which neurocognitive dysfunctions do computational models typically try to explain? Models often target specific dysfunctions to explain core addiction symptoms [57]:
- Impaired behavioral control: Often modeled through aberrant reinforcement learning algorithms or an imbalance between goal-directed ("model-based") and habitual ("model-free") behavioral control systems.
- Intense urge to use drugs (craving): Explained using neurocomputational models of incentive sensitization or behavioral economic theories that account for excessive valuation of drugs.
FAQ 4: How can I ensure my computational model is clinically relevant? To enhance clinical relevance, ensure that the model is informed by robust psychological theory, experimental data, and direct clinical observations. The model should aim to explain more than just drug consumption; it should address specific addiction symptoms, such as compulsive use despite punishment, craving, and relapse [27] [57].
Troubleshooting Guides
Problem: Model fails to capture the transition from casual use to addiction.
- Potential Cause: The model parameters or structure may be static and unable to account for the neuroadaptations and shifting behavioral control mechanisms that characterize the progression of addiction.
- Solution: Consider implementing a framework that allows for a transition of control from goal-directed to habitual systems. This can be linked to a computational shift from ventral to dorsal striatal control, reflecting established neurobiological theories [27].
Problem: Model simulations do not replicate key human behaviors or symptoms.
- Potential Cause 1: The experimental task or data used to develop and fit the model may not adequately engage the complex cognitive processes targeted (e.g., craving, impaired control).
- Solution 1: Re-evaluate your experimental design. A good experiment should first show signatures of the targeted processes in simple, model-independent analyses of behavior before computational modeling is applied [58].
- Potential Cause 2: The model may be incorrectly inferring the underlying psychological mechanisms from the behavioral data.
- Solution 2: Perform model comparison to determine which of a set of competing algorithms best describes the behavioral data. This helps identify the most likely mechanisms underlying the observed behavior [58].
Problem: Model parameters lack clear biological or psychological interpretation.
- Potential Cause: The model may be mathematically sound but not grounded in established theory or neural evidence.
- Solution: When designing the model, work in parallel with experimental design to ensure a clear theoretical hypothesis. Link model components to specific psychological constructs or neural circuits to improve interpretability [57] [58].
Comparative Analysis of Computational Approaches
Table 1: Key Computational Theories and Their Coverage of Addiction Characteristics
| Computational Approach | Primary Explanatory Focus | Addiction Stages Modeled | Key Symptoms Addressed | Biological Plausibility |
|---|---|---|---|---|
| Reinforcement Learning (e.g., Dezfouli et al., 2009) [27] | Compulsive drug use, Over-valuation | Early to late stage (no withdrawal/craving) | Compulsive use despite punishment | Algorithmic level (e.g., basal reward threshold) |
| Dual-System Control (e.g., Redish et al., 2008) [27] | Relapse, Impulsivity, Executive dysfunction | Yes | Withdrawal, Relapse, Incentive salience, Impulsivity | Algorithmic level (planning vs. habit systems) |
| Predictive Coding (e.g., Gu & Filbey, 2017) [27] | Craving, Subjective beliefs | Later work extends to abstinence | Craving, Effects of withdrawal | Algorithmic level (precision of beliefs) |
| Behavioral Economic (e.g., Bernheim & Rangel, 2004) [27] | Cue-triggered behavior, Relapse | Yes | Cue-triggered craving, Relapse | Inspired by dual-process ("hot"/"cold") systems |
Table 2: Quantitative Summary of Model Limitations from Literature Review
| Modeling Aspect | Number of Models Reviewed | Models Capturing Multiple Symptoms | Models Addressing Stages of Addiction | Models Supported by Human Data |
|---|---|---|---|---|
| Mathematical/Decision-Making | 7 | 4 | 4 | Limited / Not Specified |
| Predictive Coding | 3 | 0 | 0 | Limited / Not Specified |
| Brain-Based/Circuit | Information Not Provided | Information Not Provided | Information Not Provided | Information Not Provided |
Experimental Protocols for Model Validation
Protocol 1: Testing for Compulsive Drug Use Despite Punishment
- Objective: To validate models that propose mechanisms for compulsive behavior, a key diagnostic symptom of addiction.
- Methodology: Adapt paradigms from animal studies where self-administration of a drug is paired with an aversive consequence, such as a mild footshock. A model should be able to simulate the continued drug-seeking behavior despite punishment, as seen in studies by Vanderschuren & Everitt (2004) [27].
- Model Validation: The model parameters should correlate with the degree of compulsivity observed in the experimental data.
Protocol 2: Probing the Model-Based vs. Model-Free Balance
- Objective: To test computational theories suggesting addiction involves a shift from goal-directed (model-based) to habitual (model-free) control.
- Methodology: Use a two-step sequential decision-making task designed to dissociate contributions of model-based and model-free learning. This task has been successfully applied in human studies of addiction [27] [57].
- Model Validation: Fit the model to human choice data from the task. The parameter representing the balance or weight of model-based control should be significantly reduced in individuals with addiction compared to healthy controls.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application in Research |
|---|---|
| Gephi Software | An open-source platform for visual network analysis and exploration, useful for visualizing complex neurocircuitry or model relationships [59]. |
| Computational Modeling Frameworks (e.g., Python, R, MATLAB) | Provides the environment for simulating computational theories, performing parameter estimation, and conducting model comparison [58]. |
| Two-Step Decision Task | A behavioral paradigm used to dissociate and quantify the contributions of model-based and model-free learning systems in human participants [27] [57]. |
| dTMS (Deep Transcranial Magnetic Stimulation) | A non-invasive brain stimulation technique used to experimentally modulate targeted neurocircuitries (e.g., dlPFC, vmPFC) hypothesized to be dysfunctional in addiction, allowing for causal tests of circuit-based models [4]. |
Model Workflow and Signaling Pathways
Current Modeling Approaches and Identified Gaps
A Proposed Workflow for Clinically Relevant Modeling
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Motion Artifacts
Q1: What are the primary sources of motion artifacts in neuroimaging, and why are they a significant concern in addiction research?
Motion artifacts arise from both involuntary physiological processes and voluntary subject movement. In the context of addiction research, these artifacts are particularly problematic as they can confound the subtle neural signals associated with craving and withdrawal.
- Sources of Motion: Physiological motion includes cardiac pulsation, respiration, and tremors. Bulk subject motion, such as head movement, is a major source of artifact, especially in populations where withdrawal or anxiety may reduce compliance [60].
- Impact on Data: Motion causes a range of artifacts, including blurring, ghosting (replication of structures across the image), and signal loss [60]. These inconsistencies can be misinterpreted as neurobiological abnormalities, thereby compromising the validity of findings related to addiction neurocircuitry.
Q2: What practical steps can I take to minimize motion artifacts in my study?
A multi-faceted approach combining subject preparation, hardware, and acquisition protocols is most effective.
- Subject Preparation: Ensure participants are comfortable and use padding to restrict head motion. Clearly explain the importance of staying still. For addiction studies, scheduling sessions to avoid peak withdrawal periods may improve compliance.
- Stabilization Devices: Dedicated head stabilizers can be highly effective. A recent 2025 study demonstrated that the MR-MinMo head stabilisation device significantly reduced motion artifacts in both adult and pediatric cohorts during high-resolution 7T MRI, and crucially, it helped keep motion within a range that could be further corrected by software [61].
- Acquisition Strategies: Utilize prospective motion correction (PACE) or navigator echoes that track and correct for motion in real-time. Retrospective motion correction algorithms can be applied during image reconstruction. Furthermore, accelerated imaging sequences (e.g., parallel imaging, multiband EPI) shorten scan time, thereby reducing the window for motion to occur [60].
Q3: How does motion affect different k-space sampling trajectories?
The appearance of motion artifacts is heavily dependent on how k-space is acquired.
- Cartesian (Rectilinear) Sampling: This common method is sensitive to motion, particularly in the phase-encoding direction. Periodic motion (e.g., from pulsatile blood flow) synchronized with the TR can create coherent ghosting artifacts, while sudden motion leads to severe data inconsistency and intense ghosting [60].
- Non-Cartesian Sampling (Radial, PROPELLER, Spiral): These methods are generally more robust to motion because they oversample the center of k-space. For example, PROPELLER sequences acquire data in rotating blades, allowing for motion detection and correlation between segments during reconstruction [60].
Table 1: Motion Artifact Mitigation Techniques and Their Applications
| Technique Category | Specific Method | Principle of Operation | Best Use Case in Addiction Research |
|---|---|---|---|
| Physical Restraint | MR-MinMo Device [61] | Mechanical head stabilizer | Long-duration, high-resolution scans (e.g., 7T structural/functional) |
| Prospective Correction | PACE, Navigator Echoes | Real-time tracking and adjustment of scan plane | All session types, particularly with anxious or restless participants |
| Retrospective Correction | Image-based realignment, DISORDER [61] | Post-hoc realignment of acquired data or motion-estimated reconstruction | When motion is unavoidable; as a standard preprocessing step |
| Accelerated Acquisition | Parallel Imaging, Multiband EPI | Reduces acquisition time per volume | Functional MRI tasks measuring cue-reactivity or craving |
Signal-to-Noise Ratio (SNR)
Q4: What is SNR, and why is it a critical parameter in neuroimaging studies of addiction?
The Signal-to-Noise Ratio (SNR) describes the ratio between the intensity of the desired signal from the brain and the background noise. It is a fundamental determinant of image quality and data integrity.
- Impact on Data Analysis: Low SNR can obscure subtle neurobiological effects, such as small changes in BOLD signal during a craving task or fine structural differences in the prefrontal cortex or striatum between addicted and healthy individuals. In diffusion imaging, low SNR can lead to inaccurate estimation of fractional anisotropy and fiber pathways [60].
- Relation to Motion: Motion often manifests as structured noise, which is distinct from the random thermal noise typically measured for SNR. This structured noise can drastically reduce the effective SNR and complicate its measurement [62].
Q5: What are the standard methods for measuring SNR in MRI, and what are their caveats?
There is no universal method, but the National Electrical Manufacturers Association (NEMA) provides widely adopted standards.
- NEMA Method 1 (Background Noise):
- Procedure: Place a large Region of Interest (ROI) inside a uniform phantom to measure the mean Signal (S). Measure the standard deviation of the pixel intensity from multiple ROIs placed in the background air to represent Noise (N). The measured SNR is S/N. Because noise in magnitude images follows a Rayleigh distribution, a correction factor of approximately 0.66 must be applied to calculate the true SNR [62].
- Caveat: This method is less reliable for images reconstructed with parallel imaging, as the noise becomes spatially variant (non-stationary) [62].
- NEMA Method 2 (Difference Method):
- Procedure: Acquire two identical images in rapid succession. Signal (S) is the mean pixel value from an ROI in the first image. Subtract the second image from the first; the standard deviation within the ROI of this difference image represents the noise. A correction factor of 1/√2 ≈ 0.71 is required because the noise is calculated from a difference [62].
- Caveat: This method requires two sequential acquisitions and is sensitive to any system drift between them.
Table 2: Common SNR Measurement Methods and Corrections
| Method | Signal (S) Source | Noise (N) Source | Correction Factor | Key Consideration |
|---|---|---|---|---|
| NEMA (Background) | Mean value in phantom ROI | Std. Dev. in air-background ROIs | ~0.66 (Rayleigh) | Avoids structured noise from phantom |
| NEMA (Difference) | Mean value in first image | Std. Dev. in subtracted image ROI | ~0.71 (Difference) | Sensitive to system instability |
| Within-Object | Mean value in tissue ROI | Std. Dev. in "uniform" tissue ROI | Not standardized | Highly dependent on tissue heterogeneity |
Q6: How can I optimize SNR in my experimental protocol?
SNR is influenced by a multitude of factors, many of which involve trade-offs with scan time and resolution.
- Hardware: Scanning at higher magnetic field strengths (e.g., 3T vs. 7T) provides a fundamental increase in SNR. Using dedicated, multi-channel radiofrequency coils optimized for the head also dramatically improves SNR [62].
- Sequence Parameters:
- Voxel Size: Increasing voxel size (lowering resolution) boosts SNR at the cost of spatial detail.
- TR/TE: Using a longer repetition time (TR) allows for more longitudinal recovery, and a shorter echo time (TE) reduces T2* signal decay, both increasing SNR.
- Averaging: Increasing the number of excitations (NEX) averages out random noise, improving SNR by a factor of √NEX, at the cost of longer scan time.
- Reconstruction: Advanced reconstruction techniques, including denoising algorithms, can improve effective SNR post-acquisition.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Addressing Technical Barriers
| Item / Reagent | Function / Explanation | Example Use Case |
|---|---|---|
| MR-MinMo Stabilizer [61] | Physical head restraint device to minimize bulk motion | Enabling long, high-resolution 7T scans in challenging populations |
| Uniform Phantom | A standardized object for quality control, including SNR measurement | Calibrating scanner performance and monitoring SNR over time [62] |
| Multi-channel Head Coil | A radiofrequency coil array that increases signal reception | Boosting SNR for functional and structural imaging at all field strengths |
| DISORDER Reconstruction [61] | A retrospective motion correction algorithm | Correcting for residual motion in acquired k-space data |
| Computer Vision Software [63] | Tracks head orientation from video to characterize motion | Quantifying and classifying motion artifacts in fNIRS, with applications in MRI |
| Deep Brain-Machine Interface (DBMI) [64] | A system for closed-loop monitoring and modulation of deep brain circuits | A future tool for identifying craving biomarkers and delivering therapeutic stimulation in SUDs |
Experimental Protocols for Key Methodologies
Protocol 1: Evaluating a New Motion Reduction Device in an MRI Study
- Objective: To quantitatively assess the efficacy of a novel head stabilizer (e.g., MR-MinMo) in reducing motion artifacts.
- Design: A 2x2 factorial within-subjects design is recommended. Each participant is scanned under four conditions: (1) With device and standard sequence, (2) With device and motion-corrected sequence, (3) Without device and standard sequence, (4) Without device and motion-corrected sequence [61].
- Participants: Include both a control group and a target population (e.g., individuals with Substance Use Disorders) to test efficacy where it matters most.
- Image Acquisition: Use a high-resolution, motion-sensitive sequence (e.g., a 3D Multi-Echo Gradient Echo) with a long acquisition time to amplify motion effects.
- Analysis:
- Qualitative: Expert raters, blinded to the condition, score images for artifact severity using a standardized scale (e.g., 1=severe artifacts, 5=no artifacts).
- Quantitative: Calculate image sharpness metrics like the Normalized Gradient Squared (NGS). Lower NGS values indicate sharper images with less blurring [61]. Analyze data with a repeated-measures ANOVA to test for main effects of the device and its interaction with retrospective correction.
Protocol 2: Standardized SNR Measurement for Longitudinal Scanner Monitoring
- Objective: To establish a baseline SNR for an MRI scanner and track its performance over time.
- Phantom: Use a uniform, spherical phantom recommended by the scanner manufacturer.
- Scan Protocol: Implement a standard clinical structural sequence (e.g., T1-weighted MPRAGE) with parameters held constant for all future measurements.
- Measurement: Adopt a consistent NEMA method. The background method (NEMA 1) is often preferred for its simplicity [62].
- Acquire the phantom image.
- Signal: Draw a large circular ROI in the center of the phantom. Record the mean pixel value.
- Noise: Draw four square ROIs in the corners of the image, well outside the phantom. Calculate the average standard deviation of the pixel values in these ROIs.
- Calculation: Apply the appropriate correction factor: SNR = (Mean Signal / Average Noise) * 0.66.
- Documentation: Record the calculated SNR, all scan parameters, and the date in a dedicated quality control log. Investigate any significant deviations from the baseline.
Signaling Pathways and Experimental Workflows
Diagram 1: Motion Artifact Management Workflow
Diagram 2: Neurocircuitry of Addiction & Technical Barriers
Frequently Asked Questions
FAQ 1: What is the strongest predictor of effective seizure reduction in Vagus Nerve Stimulation (VNS)? Output current is the strongest predictor of seizure reduction. Increasing the output current by 1 mA more than doubles the probability of achieving a ≥75% seizure reduction, with effects peaking at around 2.70 mA. A target range of 1.5–2.25 mA is recommended for optimal treatment effectiveness, using a standard pulse width of 250 μs and frequency of 20 Hz. Higher currents should be attempted if tolerated by the patient [65].
FAQ 2: How do I approach optimizing Deep Brain Stimulation (DBS) for complex symptoms like gait in Parkinson's disease? Optimizing DBS for complex symptoms requires a structured, data-driven approach due to significant interindividual variability [66].
- Systematic Testing: Systematically vary stimulation parameters (amplitude, frequency, pulse width) within safe limits.
- Quantitative Metrics: Use a quantitative metric, such as a Walking Performance Index (WPI) that integrates key kinematics (stride velocity, arm swing, step variability), to objectively assess outcomes [66].
- Modeling: Apply computational models, like a Gaussian Process Regressor, to predict optimal patient-specific settings from a limited number of tests [66].
- Neural Biomarkers: Identify and target person-specific neural spectral biomarkers, such as reduced pallidal beta power during key gait phases [66].
FAQ 3: My DBS therapy isn't working for a specific symptom like Freezing of Gait (FoG). Should I only adjust intensity? No, for symptoms like FoG, adjusting the stimulation frequency and target site can be more critical. A randomized trial showed that while standard high-frequency subthalamic nucleus (STN) stimulation works for some, a comparable number of patients respond better to dual-site STN and substantia nigra (SNr) stimulation at different frequencies (e.g., 71 Hz or 119 Hz). Changes in kinematic gait parameters (stride length, swing time) are highly correlated with clinical improvement and can serve as digital biomarkers to guide this personalization [67].
FAQ 4: From a neurocircuitry perspective, why might the same stimulation parameters have different effects on individuals? Individual differences in underlying structural brain connectivity significantly influence how stimulation spreads and affects brain dynamics. Regions with high "average controllability" can impart large global changes in brain network activity with low energy input. The structural and functional variability between individuals means that a one-size-fits-all parameter set is unlikely to be effective; personalized parameter selection based on individual neurocircuitry is essential [68].
FAQ 5: What are the core stimulation parameters and their definitions? The core parameters for most neurostimulation therapies are [69]:
- Current Intensity: The amplitude or strength of the electrical pulse, measured in milliamperes (mA).
- Pulse Width: The duration of a single electrical pulse, measured in microseconds (μs).
- Frequency: The number of stimulation pulses delivered per second, measured in Hertz (Hz).
- Duty Cycle: The pattern of alternating stimulation (ON) and rest (OFF) periods.
Stimulation Parameter Tables
Vagus Nerve Stimulation (VNS) Parameters for Epilepsy
The following table summarizes key findings from a large cohort study on optimizing VNS for epilepsy [65].
| Parameter | Optimal Range / Value | Effect on Seizure Reduction | Clinical Recommendation |
|---|---|---|---|
| Output Current | 1.5 - 2.25 mA (Target); Peaks at ~2.70 mA | Strongest predictor; +1 mA more than doubles probability of ≥75% reduction | Primary focus for titration; increase if tolerated [65]. |
| Frequency | 20 Hz | Associated with the best effect | Use standard frequency [65]. |
| Pulse Width (PW) | 250 μs | Associated with the best effect | Use standard pulse width [65]. |
| Duty Cycle | Various | Changes may benefit patients unresponsive to current adjustment | Consider adjusting if current optimization fails [65]. |
| Treatment Duration | Long-term (Median 79 months) | Effectiveness improves over time | Maintain therapy; expect gradual improvements [65]. |
Deep Brain Stimulation (DBS) Parameters for Gait in Parkinson's Disease
This table synthesizes parameter effects and optimization strategies from recent studies on DBS for gait [66] [67].
| Parameter / Factor | Impact on Gait & Optimization Strategy | Key Consideration |
|---|---|---|
| Amplitude Tested ranges: ~2.8-5.5 mA [66]. | Directly modulates neural activity; systematic testing required within individual tolerance. | Higher amplitudes are not always better for gait; must be balanced with side effects. |
| Frequency Standard high (e.g., 119-130+ Hz) vs. Low (e.g., 30-71 Hz). | Effects are highly person-specific. Lower frequencies (e.g., 60, 71 Hz) can significantly improve gait in some patients [66] [67]. | A patient's optimal frequency for gait may differ from their optimal frequency for other symptoms [67]. |
| Stimulation Target Mono-site (STN) vs. Dual-site (STN+SNr). | Dual-target stimulation can improve freezing of gait where standard STN stimulation is insufficient [67]. | Requires a more complex implantation and programming strategy. |
| Personalization | Data-driven models (e.g., Gaussian Process Regressor) can efficiently identify optimal settings from limited trials [66]. | Essential due to significant inter-individual variability in response [66] [67]. |
Experimental Protocols
Protocol 1: Data-Driven DBS Optimization for Gait Enhancement
This protocol outlines the methodology for a personalized, model-based approach to optimizing DBS parameters for gait [66].
1. Participant Setup and Baseline Data Collection
- Implant participants with bidirectional neural stimulators (e.g., Medtronic Summit RC+S) allowing for chronic sensing and stimulation.
- Place DBS leads in the target structure (e.g., Globus Pallidus or STN/SNr) and electrocorticography (ECoG) paddles over the primary motor cortex.
- Record high-resolution time-domain neural data from both sites.
- Collect baseline gait kinematics using full-body Inertial Measurement Unit (IMU) sensors during overground walking.
2. Systematic Parameter Variation and Testing
- Define a safe parameter space for exploration, including amplitude, frequency, and pulse width.
- Test the clinically optimized settings alongside several novel configurations. For example [66]:
- Amplitude: Test clinical amplitude, a 25-30% reduction, and an upper limit (e.g., up to 5.5 mA).
- Frequency: Test clinical frequency, 60 Hz, and a higher frequency.
- For each parameter set, record neural data and gait kinematics simultaneously during a standardized walking task (e.g., 200 steps on a 6m loop).
3. Quantitative Gait Analysis and Modeling
- Calculate a composite Walking Performance Index (WPI) from the kinematic data. The WPI can include [66]:
- Stride velocity
- Arm swing amplitude
- Variability in step length
- Variability in step time
- Use a machine learning model (e.g., Gaussian Process Regressor) to learn the relationship between the tested DBS parameters and the WPI output.
- Use the model to predict the DBS parameter set that would maximize the WPI for that individual.
4. Validation and Neural Biomarker Identification
- Validate the model-predicted optimal settings by testing them in the participant and confirming improvement in the WPI.
- Analyze the recorded neural data (e.g., pallidal and motor cortical signals) to identify spectral biomarkers (e.g., reduced beta power) associated with improved walking performance.
Protocol 2: Framework for VNS Parameter Titration in Epilepsy
This protocol is based on findings from a large-scale registry study linking long-term outcomes to dosing parameters [65].
1. Establish Baseline and Initial Settings
- Document baseline seizure frequency and type.
- Initiate VNS therapy with standard parameters: Output current at a lower level (e.g., 0.5 mA), frequency at 20 Hz, pulse width at 250 μs, and a standard duty cycle.
2. Systematic Up-Titration of Output Current
- The primary focus should be on gradually increasing the output current.
- Increase the current in small increments (e.g., 0.25 mA) at regular intervals, based on patient tolerance.
- The target therapeutic range is 1.5 mA to 2.25 mA. If tolerated, currents up to ~2.7 mA can be attempted for maximum effect [65].
3. Evaluate and Optimize Other Parameters if Needed
- If a satisfactory response is not achieved after optimizing the current, consider adjusting the duty cycle.
- Maintain the standard frequency (20 Hz) and pulse width (250 μs), as these are associated with the best effect [65].
4. Long-Term Management
- Continue therapy and monitoring over the long term, as VNS effectiveness improves with time (median follow-up in studies was 79 months) [65].
- Be aware that the presence of intellectual disability may negatively impact treatment response [65].
Signaling Pathways and Workflows
Diagram 1: Neurocircuitry of Addiction and Stimulation Targets
Addiction Neurocircuitry and Stimulation Targets
Diagram 2: Stimulation Parameter Optimization Workflow
Parameter Optimization Workflow
The Scientist's Toolkit
Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Bidirectional Implantable Neurostimulator (e.g., Medtronic Summit RC+S) | Allows for simultaneous delivery of electrical stimulation and chronic streaming of high-resolution neural data (local field potentials, ECoG) in freely moving subjects [66]. |
| Inertial Measurement Unit (IMU) Sensors | Full-body wearable sensors to precisely capture kinematic gait parameters (stride velocity, step length variability, arm swing) for objective assessment of motor symptoms [66] [67]. |
| Computational Model (Wilson-Cowan Oscillators) | A biologically motivated, nonlinear mathematical model used to simulate mean-field dynamics of coupled neuronal populations and predict the system-wide impact of regional stimulation [68]. |
| Gaussian Process Regressor | A Bayesian machine learning model used to efficiently map the relationship between stimulation parameters and clinical outcomes, enabling prediction of optimal settings with limited experimental trials [66]. |
| Network Control Theory | A framework applied to structural brain networks (from DSI) to compute diagnostics like "average controllability," predicting which brain regions can impart large global changes when stimulated [68]. |
| Walking Performance Index (WPI) | A composite metric integrating multiple key gait parameters (stride velocity, arm swing, step length/time variability) into a single score to objectively quantify walking performance [66]. |
FAQs: Addressing Common Experimental Challenges
FAQ 1: What are the primary neurocircuitry domains disrupted in addiction, and how are they modeled across species?
Addiction can be conceptualized as a disorder affecting three key functional domains, mediated by specific brain circuits, which can be studied in both animals and humans [13].
- Binge/Intoxication Stage: This stage involves the rewarding effects of a substance and the development of incentive salience and habits. It primarily involves changes in dopamine and opioid peptides in the basal ganglia, including the nucleus accumbens and dorsal striatum. Animal models like drug self-administration and conditioned place preference (CPP) directly probe this circuit. Human neuroimaging studies show that intoxicating doses of alcohol and drugs release dopamine in the ventral striatum [13].
- Withdrawal/Negative Affect Stage: This stage is characterized by a negative emotional state when drug access is prevented. It involves decreases in dopamine function and recruitment of brain stress systems (e.g., corticotropin-releasing factor and dynorphin) in the extended amygdala. Dependence induction models in rodents and measurement of negative affective states in humans with AUD model this domain [13].
- Preoccupation/Anticipation (Craving) Stage: This stage involves craving and deficits in executive function. It is mediated by dysregulation of key afferent projections from the prefrontal cortex (PFC) and insula to the basal ganglia and extended amygdala, involving glutamate and other neurotransmitters. Reinstatement models in animals and cue-reactivity or cognitive testing in humans target this circuit [13].
FAQ 2: Why do some pharmacological treatments that are effective in animal models fail in human clinical trials for Alcohol Use Disorder (AUD)?
This failure often stems from limitations in the predictive validity of animal models and species differences [70].
- Lack of Syndrome Emulation: Animal models are designed to study specific behavioral endpoints (e.g., consumption, relapse) but do not fully emulate the entire human AUD syndrome, including its complex psychosocial dimensions [70].
- Genetic and Environmental Control: While precise genetic control in animals is a strength, genetically diverse outbred rat strains often do not readily consume alcohol, requiring experimental manipulations (e.g., stress, sweeteners) that limit generalizability to humans. Human laboratory studies serve as a critical "bridge" to validate targets and assess treatment efficacy in a controlled setting before costly clinical trials [70].
- Circuit Homology vs. Phenomenology: While core addiction neurocircuitry is conserved across species [71], the transition to addiction in humans involves higher-order cognitive processes that are difficult to fully capture in rodents. Ensuring that animal models demonstrate shared circuit abnormalities is critical for establishing face validity [70].
FAQ 3: How can we improve the translational validity of conditioned place preference (CPP) paradigms when studying cue-induced craving?
Improving the translational value of CPP requires addressing its limitations and aligning its application with human phenomena [72] [70].
- From Passive to Active: Standard CPP involves passive drug administration. To better model human behavior, CPP can be combined with operant self-administration paradigms to link cue-based motivation with goal-directed drug-seeking behavior [70].
- Modeling Heterogeneity: CPP can be used alongside dependence induction techniques to phenotype animals based on their level of incentive salience toward alcohol-paired cues. This helps model the individual variation seen in human AUD and can be aligned with research frameworks like the Alcohol Addiction Research Domain Criteria (RDoC) [70].
- Human Analogs: Virtual reality (VR) has been successfully used to create human analogs of the CPP paradigm, allowing for the conditioning of environmental contexts with rewards in a controlled but more ecologically valid setting [70].
FAQ 4: What are the technical considerations for using deep Transcranial Magnetic Stimulation (dTMS) to target specific neurocircuits in AUD?
Novel dTMS trials highlight specific methodological considerations for circuit-targeted neuromodulation [4].
- Coil Selection and Target Depth: Traditional figure-eight coils stimulate only superficial brain layers (~1.5 cm). In contrast, deep TMS (dTMS) with H-coils can modulate wider volumes of tissue and regions up to 5 cm beneath the skull. This is essential for directly targeting deeper nodes of addiction neurocircuitry, such as the ventromedial prefrontal cortex (vmPFC) and its subcortical connections [4].
- Stimulation Protocol: Different theta-burst stimulation protocols can be used to achieve opposing effects on neuronal excitability. For example, intermittent TBS (iTBS) can increase activity in a weakened pathway (e.g., targeting the dorsolateral PFC), while continuous TBS (cTBS) can decrease activity in a hyperactive pathway (e.g., targeting the vmPFC) [4].
- Outcome Validation: Proof of circuit engagement requires multimodal assessment. Combining dTMS with fMRI and spectral Dynamic Causal Modeling (spDCM) allows researchers to measure changes in effective connectivity within the targeted circuits, confirming that the stimulation is having the intended neurobiological effect [4].
Experimental Protocols & Methodologies
Conditioned Place Preference (CPP) Protocol
Objective: To measure the rewarding or aversive properties of a substance by assessing an animal's preference for an environment previously paired with that substance [72] [70].
Detailed Methodology:
- Apparatus: A box with at least two distinct compartments differing in visual, tactile, and/or olfactory cues (e.g., black vs. white walls, grid vs. mesh flooring). A neutral start zone may connect the compartments.
- Pre-Test (Baseline): The animal is allowed free access to all compartments for a set period (e.g., 15-20 minutes). The time spent in each compartment is recorded. Animals with a strong innate bias for one compartment are typically excluded.
- Conditioning (Training): This phase consists of multiple sessions (e.g., 4-8 sessions).
- On one day, the animal is confined to one compartment immediately after receiving the substance (e.g., alcohol, morphine). This is the "paired" compartment.
- On alternating days, the animal is confined to the other compartment after receiving a vehicle control (e.g., saline). This is the "unpaired" compartment.
- The order of pairing (paired vs. unpaired compartment first) should be counterbalanced across animals.
- Post-Test: Conducted exactly like the pre-test, with the animal in a drug-free state. The primary outcome measure is the difference in time spent in the paired compartment between the post-test and pre-test [70].
Human Laboratory Analog: Virtual Reality CPP
- Environment Design: Two distinct virtual environments are created using VR software.
- Conditioning: Participants explore one environment after administration of alcohol (or a rewarding stimulus). They explore the other environment after a control beverage.
- Post-Test: Participants choose which virtual environment to enter and spend time in. The preference for the alcohol-paired environment is measured [70].
Intermittent Access Two-Bottle Choice Protocol
Objective: To induce high, binge-like ethanol consumption in rodents, modeling the transition from moderate to excessive drinking seen in humans [70].
Detailed Methodology:
- Animals: Single-housed rodents (rats or mice) with free access to food.
- Fluid Access:
- The paradigm uses two bottles: one containing an ethanol solution (e.g., 20% v/v in water) and the other containing water.
- Animals have 24-hour access to both bottles for three sessions per week (e.g., Monday, Wednesday, Friday), with 24 or 48 hours of deprivation between sessions.
- Bottle positions are alternated at the start of each session to control for side preferences.
- Duration: This protocol is typically run for several weeks, during which ethanol intake gradually escalates.
- Key Measurements:
- Ethanol intake (g/kg/24h): Calculated by measuring the volume of ethanol solution consumed and the animal's body weight.
- Ethanol preference ratio: The proportion of total fluid consumed as ethanol (Ethanol intake / Total fluid intake) [70].
Deep TMS (dTMS) Protocol for AUD Neurocircuitry
Objective: To recalibrate disrupted neurocircuitry in AUD by applying targeted neuromodulation to the dorsolateral prefrontal cortex (dlPFC) and ventromedial prefrontal cortex (vmPFC) [4].
Detailed Methodology (as per a recent trial):
- Design: Randomized, single-blind, sham-controlled crossover trial.
- Participants: Adults (age 18-49) with moderate to severe AUD.
- dTMS Parameters:
- Coil: H-coil for dTMS.
- Target 1 - Weakened dlPFC Pathway: Intermittent Theta-Burst Stimulation (iTBS) is used to increase neuronal excitability.
- Target 2 - Heightened vmPFC Pathway: Continuous Theta-Burst Stimulation (cTBS) is used to decrease neuronal excitability.
- Control: A sham stimulation condition that mimics the sound and sensation of active TMS without delivering significant magnetic energy.
- Procedure: Participants receive two doses of active or sham dTMS (order counterbalanced), spaced 7 days apart.
- Outcome Measures:
- Primary: Stimulation-induced changes in effective connectivity within targeted circuits, measured via fMRI and spectral Dynamic Causal Modeling (spDCM).
- Secondary: Changes in cognitive tests of executive control and decision-making.
- Exploratory: Changes in craving-related emotions, daily craving experiences, and weekly alcohol consumption over a 90-day follow-up period [4].
Data Presentation
Table 1: Comparison of Common Preclinical Animal Models in Addiction Research
| Model | Key Readout | Advantages | Limitations / Translational Gaps |
|---|---|---|---|
| Conditioned Place Preference (CPP) [72] [70] | Time spent in drug-paired context | Drug-free testing; establishes rewarding/aversive properties; simple setup. | Lack of animal-driven drug-seeking behavior; not exclusive to drugs of abuse. |
| Behavioral Sensitization [72] | Potentiated locomotor response | Long-lasting; shared by most drugs; models incentive salience. | Poor face validity for full addiction syndrome; measures stereotypies at high doses. |
| Self-Administration (Short Access) [72] | Drug intake on a reinforcement schedule | Direct measure of drug-taking behavior; reliable for studying relapse. | Does not capture compulsive drug-taking; limited session length. |
| Self-Administration (Long Access) [72] | Escalation of drug intake | Models increased intake and motivation seen in addiction; higher breakpoints. | Long training sessions; can be resource-intensive. |
| Intermittent Access 2-Bottle Choice [70] | Ethanol consumption (g/kg) & preference | Good face validity for binge-like drinking; induces high voluntary intake. | Low consumption in some strains; may require initiation training. |
Table 2: Key Neurocircuits, Neurotransmitters, and Behavioral Domains in the Addiction Cycle
| Stage of Addiction Cycle | Core Neurocircuitry | Key Neurotransmitter Changes | Associated Behavioral Domain |
|---|---|---|---|
| Binge/Intoxication [13] | Basal Ganglia (Ventral Striatum, Dorsal Striatum) | Increase: Dopamine, Opioid peptides, GABA | Reward, Incentive Salience, Habit Formation |
| Withdrawal/Negative Affect [13] | Extended Amygdala | Increase: CRF, Dynorphin, NorepinephrineDecrease: Dopamine, Endocannabinoids | Negative Emotional State, Stress, Dysphoria |
| Preoccupation/Anticipation [13] | Prefrontal Cortex, Insula, Hippocampus | Increase: Glutamate, CRF | Craving, Executive Function Deficits, Relapse |
Table 3: Research Reagent Solutions for Addiction Neurocircuitry Studies
| Reagent / Material | Function & Application in Research |
|---|---|
| Deep TMS (dTMS) with H-Coil [4] | Non-invasive neuromodulation; allows direct targeting of deeper cortical nodes (e.g., vmPFC, insula) in addiction neurocircuitry in human trials. |
| Spectral Dynamic Causal Modeling (spDCM) [4] | A computational modeling technique applied to fMRI data; measures the valence (excitatory/inhibitory) and directionality of neural connections, providing insights into circuit-level changes. |
| Virtual Reality (VR) Environments [70] | Used in human laboratory studies to create immersive, contextual cues for conditioned place preference (CPP) and cue-reactivity paradigms, enhancing ecological validity. |
| Operant Self-Administration Chambers [72] [71] | Standardized chambers for rodents; allow for the study of drug-taking behavior (e.g., lever pressing, nose-poking) and reinstatement (relapse) in a controlled environment. |
Experimental Workflow and Neurocircuitry Diagrams
Diagram Title: Cross-Species Translational Research Workflow
Diagram Title: Key Neurocircuits in the Three-Stage Addiction Cycle
Validation Frameworks and Method Comparison: Assessing Analytical Approaches and Clinical Translation
Frequently Asked Questions
Q: My computational model fits my training data well but fails to predict novel behavioral outcomes. What should I investigate? A: This is a classic sign of overfitting. First, ensure you are using proper cross-validation (e.g., 5-fold or 10-fold) instead of testing your model on the same data it was trained on [73]. Second, simplify your model; a model with fewer parameters might generalize better to unseen data. Third, verify that your experimental design has enough trials and conditions to properly engage the cognitive processes you are modeling, as a poor design cannot be salvaged by modeling alone [58].
Q: When validating a model against neural data, what is a common pitfall in relating model parameters to brain activity? A: A major pitfall is assuming that a good behavioral fit automatically means the model's latent variables are represented in the brain. Always look for model-independent signatures of the cognitive process in the behavioral data first [58]. Furthermore, ensure that the neuroimaging data (e.g., fMRI, EEG) has sufficient temporal and spatial resolution to detect the neural signals corresponding to your model's computational variables.
Q: How can I determine the right machine learning algorithm for predicting clinical outcomes like addiction treatment response? A: There is no single "best" algorithm; performance depends on your specific dataset and clinical question [73]. Start with simpler, interpretable models like Logistic Regression or Support Vector Machines before moving to complex ones like Random Forests. Crucially, use a nested cross-validation approach to tune hyperparameters and avoid optimistic bias in your performance estimates [73].
Q: What does it mean if my neuroimaging data does not improve clinical outcome predictions over basic clinical variables? A: This is a common and valid finding. It suggests that the neuroimaging features you selected may not carry additional predictive power beyond what is captured by clinical variables (e.g., symptom severity, age) for your specific outcome. A study on OCD found that clinical data alone predicted therapy remission better than neuroimaging data [74]. This can help prioritize cost-effective predictors.
Troubleshooting Guide
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Model Generalization | Poor performance on test data/novel subjects. | Overfitting Inadequate cross-validation Sample size too small. | Use K-fold cross-validation [73]. Apply regularization techniques. Perform power analysis for sample size [73]. |
| Behavioral Validation | Model predictions deviate from actual behavior. | Model mis-specification Experiment doesn't engage target process [58]. Poor parameter estimability. | Compare against simpler alternative models [58]. Pilot task to confirm it elicits desired behavior. Simulate data to check parameter recovery. |
| Neural Correlates | No correlation between model states and brain activity. | Incorrect latent variables Neural data doesn't match model's temporal/spatial scale. The model is a poor description of the brain's algorithm. | Use model-based fMRI to regress latent variables against BOLD signal [58]. Align model timecourse with EEG/MEG metrics. |
| Clinical Prediction | Low accuracy in predicting treatment outcomes. | High patient heterogeneity Outcome measure is noisy/multi-factorial. Features lack predictive power. | Use algorithms robust to heterogeneity (e.g., SVM, Random Forests) [73]. Define clear, objective outcome measures (e.g., abstinence). Combine neurobiological, clinical, and demographic features [73]. |
Experimental Protocols for Key Validation Types
Protocol 1: Validating a Computational Model of Addiction Behavior
- Objective: To test whether a Reinforcement Learning (RL) model can accurately predict compulsive drug-seeking behavior in a simulated environment and identify its neural correlates.
- Methodology:
- Task Design: Administer a computer-based decision-making task (e.g., a probabilistic reversal learning task) to participants with Alcohol Use Disorder (AUD) and healthy controls. The task should involve learning which stimuli are associated with rewards (monetary or other) and adapting when these contingencies change [58].
- Behavioral Modeling: Fit a series of computational models (e.g., Q-learning models with varying learning rates, perseverance parameters) to the trial-by-trial choice data [58].
- Model Comparison: Use metrics like the Akaike Information Criterion (AIC) or Bayesian Information Criterion (BIC) to compare which model best accounts for the observed choices without overfitting [58].
- Parameter Validation: Examine if the estimated model parameters (e.g., a low learning rate) correlate with clinical measures of addiction severity, demonstrating the parameter's real-world relevance.
- Outcome Measures: Model fit indices (AIC, BIC), parameter recovery accuracy in simulations, correlations between model parameters and clinical scores.
Protocol 2: Cross-Validated Neuroimaging for Treatment Outcome Prediction
- Objective: To build a machine learning model that uses baseline brain function and clinical data to predict relapse in patients undergoing treatment for stimulant use disorder.
- Methodology:
- Participant & Data Acquisition: Recruit patients entering treatment. Acquire baseline clinical data (e.g., years of use, craving scores) and resting-state functional MRI (rs-fMRI) data [73].
- Feature Extraction: From the rs-fMRI data, extract features such as functional connectivity (FC) within known addiction neurocircuits (e.g., between the prefrontal cortex and basal ganglia as outlined in the addiction cycle [50]) or the fractional amplitude of low-frequency fluctuations (fALFF) [74].
- Model Training & Validation:
- Define a clear clinical outcome (e.g., "relapse" vs. "abstinence" at 3-month follow-up).
- Use a 5-fold or 10-fold cross-validation approach [73].
- Within each fold, train a classifier (e.g., Support Vector Machine) on the training set and test it on the held-out fold.
- For a more rigorous test, perform external validation by applying the final model to a completely independent cohort [73].
- Model Interpretation: Identify which features (e.g., specific functional connections, clinical variables) were most impactful in the model's predictions.
- Outcome Measures: Prediction accuracy, sensitivity, specificity, and Area Under the ROC Curve (AUC) [73].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Addiction Research |
|---|---|
| Reinforcement Learning Models | A class of computational models used to understand how individuals learn to associate actions (e.g., drug use) with rewards and punishments. They are key for simulating the "binge/intoxication" stage of addiction [50] [58]. |
| Support Vector Machines (SVM) | A machine learning algorithm used for classification and regression. It is often used to classify individuals into groups (e.g., treatment responder vs. non-responder) based on neurobiological or clinical features [73]. |
| Functional Magnetic Resonance Imaging (fMRI) | A neuroimaging technique that measures brain activity by detecting changes in blood flow. It is used to map addiction-related neurocircuitry, such as hyperactivity in the extended amygdala during withdrawal [50] [73]. |
| Electroencephalography (ERP-PCA) | Electroencephalography (EEG) measures electrical activity in the brain. Event-Related Potentials (ERP) analyzed with Principal Component Analysis (PCA) can identify neural signatures (e.g., N200, P3a) that predict treatment completion in addiction [73]. |
| Glucagon-Like Peptide-1 Receptor Agonists (GLP-1RAs) | A class of drugs for diabetes and obesity being investigated for addiction treatment. They may modulate neurobiological pathways underlying addictive behaviors, potentially reducing substance craving and use [5]. |
Quantitative Data on Predictive Modeling in Addiction
Table 1: Machine Learning Studies Predicting Addiction Treatment Outcomes. (FC = Functional Connectivity; ERP = Event-Related Potential; TxC = Treatment Completion; TxR = Treatment Response; LOO = Leave-One-Out Cross-Validation; C = Classification; R = Regression) [73]
| Reference | Substance | Sample Size (N) | Neuroimaging Mode | Input Features | Outcome Type | Cross-Val (K) | Key Finding |
|---|---|---|---|---|---|---|---|
| (20) | Polysubstance | 89 | EEG | ERP PCA | TxC (C) | LOO | Sensory gating (P2) & post-error (Pe) ERPs predicted completion. Neuroimaging model outperformed clinical-only model. |
| (21) | Polysubstance | 139 | fMRI | ICA FC | TxC (C) | 10-fold | Corticolimbic connectivity during a task predicted completion. Neuroimaging model outperformed clinical-only model. |
| (9) | Cocaine | 118 | fMRI | Whole-Brain FC | TxR (R) | LOO | Abstinence predicted by increased FC between frontoparietal and medial frontal networks. Model replicated in an external sample. |
| (25) | Cocaine | 24 | PET | ROI Binding Potential | TxR (C) | 10-fold | Change in dopamine receptor binding in ventral striatum predicted treatment response with accuracy comparable to clinical data. |
Table 2: Performance of Clinical vs. Neuroimaging Models in Predicting Remission. (AUC = Area Under the Curve; OCD = Obsessive-Compulsive Disorder; CBT = Cognitive Behavioral Therapy; rs-fMRI = resting-state fMRI; ReHo = Regional Homogeneity) [74]
| Model Type | Predictive Features | Clinical Outcome | Performance (AUC) | Conclusion |
|---|---|---|---|---|
| Clinical Data Only | Lower symptom severity, younger age, no medication, higher education. | Remission after CBT for OCD | 0.69 | Clinical data provided moderate predictive accuracy. |
| rs-fMRI Data Only | Regional Homogeneity (ReHo) | Remission after CBT for OCD | 0.59 | Neuroimaging data alone did not perform above chance level. |
| Combined Data | Clinical and rs-fMRI features | Remission after CBT for OCD | Not specified | Multicenter neuroimaging data offered no advantage over clinical factors. |
Workflow and Conceptual Diagrams
Model Validation Workflow
Addiction Cycle & Modeling Targets
Technical Support Center
Troubleshooting Guides & FAQs
This section addresses common technical challenges in neurocircuitry mapping experiments, providing targeted solutions for researchers and drug development professionals working in addiction neurocircuitry analysis.
FAQ 1: How do I choose the right functional connectivity (FC) method for my resting-state fMRI study on addiction circuits?
The Challenge: With over 239 pairwise interaction statistics available for mapping FC, researchers face significant confusion in selecting optimal methods for investigating addiction-related circuits, particularly when studying reward (ventromedial prefrontal cortex, vmPFC) and control (dorsolateral prefrontal cortex, dlPFC) pathways [75].
Solution: Tailor your FC method to the specific research question and target neurocircuitry:
- For structure-function coupling: Precision matrices and stochastic interaction metrics demonstrate superior correspondence with anatomical connectivity (R² up to 0.25), making them ideal for investigating structural deficits in addiction [75].
- For individual fingerprinting: Covariance-based measures effectively differentiate individuals, enabling personalized therapeutic targeting [75].
- For addiction-specific applications: When targeting the vmPFC-amygdala circuit in substance use disorders, precision matrices may better capture the inhibitory control deficits characteristic of addiction [76].
Experimental Protocol: Implement the pyspi package to compute multiple FC matrices from resting-state fMRI data. Benchmark against key addiction neurocircuitry features: hub identification in prefrontal-striatal pathways, structure-function coupling in corticostriatal loops, and individual differences in circuit organization [75].
FAQ 2: What strategies can improve spatial specificity when mapping human addiction circuits with fMRI?
The Challenge: Standard gradient-echo BOLD fMRI signals are contaminated by draining veins, blurring activation maps and reducing accuracy for small nuclei critical in addiction circuits (e.g., amygdala, ventral striatum) [77].
Solution: Implement microvessel-specific fMRI approaches:
- Spin-echo BOLD: Reduces large vessel contributions but has lower sensitivity [77].
- CBV-weighted VASO: Provides improved spatial specificity to microvasculature [77].
- High-field systems: Utilize ultrahigh-field (≥7T) scanners for enhanced resolution and specificity [77].
Experimental Protocol: For layer-specific fMRI targeting input layers of prefrontal regions:
- Use CBV-weighted fMRI at high field (≥7T)
- Apply deconvolution methods to account for draining vein effects
- Combine with neuromodulation (TMS) during scanning to establish causal interactions within addiction circuits [77]
FAQ 3: How can I achieve monosynaptic input mapping to specific prefrontal cortex subregions relevant to addiction?
The Challenge: Traditional tracing methods lack monosynaptic specificity and cellular resolution needed to delineate input networks to addiction-relevant orbitofrontal cortex (ORB) subregions [78].
Solution: Implement modified rabies virus systems for retrograde trans-monosynaptic tracing:
- Viral Cocktail: Co-inject rAAV-hSyn-RG + rAAV-hSyn-His-EGFP-2a-TVA (1:1 ratio) followed by RV-ΔG-tdTomato 2 weeks later [78].
- Stereotaxic Targeting: Use precise coordinates for ORB subregions (e.g., ORBm: A/P +2.40mm, M/L -0.20mm, D/V -2.50mm from bregma) [78].
- Quantitative Analysis: Employ whole-brain fluorescence imaging and statistical comparison of input neuron distributions [78].
Experimental Protocol:
- Inject helper viruses (rAAV-RG + rAAV-TVA) into target ORB subregion
- After 14 days, inject RV-ΔG-tdTomato at same coordinates
- Perfuse 7 days post-rabies injection
- Section and image entire brain
- Quantify input neurons across 279 brain regions [78]
Troubleshooting Tip: Low labeling efficiency often results from inaccurate stereotaxic placement or viral titer issues. Verify injection sites with post-hoc histology and titrate viral concentrations [78].
FAQ 4: What non-invasive neuromodulation approaches effectively target addiction circuits in human studies?
The Challenge: Standard TMS coils cannot adequately reach critical nodes of addiction circuits like the vmPFC, limiting therapeutic efficacy [4].
Solution: Implement deep TMS (dTMS) with H-coils and protocol optimization:
- Coil Selection: Brainsway H-coils stimulate up to 5cm beneath skull vs. 1.5cm for figure-eight coils [4].
- Protocol Selection: Use intermittent TBS for dlPFC (excitatory) and continuous TBS for vmPFC (inhibitory) to rebalance addiction circuits [4].
- Outcome Measures: Combine with fMRI and spectral Dynamic Causal Modeling (spDCM) to assess effective connectivity changes [4].
Experimental Protocol for AUD:
- Design: Randomized, single-blind, sham-controlled crossover
- Participants: Adults with moderate-severe AUD
- Intervention: dTMS targeting dlPFC (iTBS) or vmPFC (cTBS)
- Measures: Neural connectivity (fMRI/spDCM), cognitive tasks, craving scales, alcohol consumption (90-day follow-up) [4]
Comparative Analysis of Neurocircuitry Mapping Techniques
Table 1: Technical Specifications and Performance Metrics of Major Mapping Approaches
| Technique | Spatial Resolution | Temporal Resolution | Throughput | Invasiveness | Key Strengths | Primary Limitations |
|---|---|---|---|---|---|---|
| fMRI (BOLD) | 100-500 µm (layer-specific); 1-3 mm (human) | Seconds (hemodynamic lag) | High (whole-brain) | Non-invasive | Whole-brain coverage; human applicable; rich functional connectivity data [77] | Indirect neural measure; slow temporal dynamics; vascular confounds [77] |
| Viral Tracing (RV-ΔG) | Single neuron | Days (transsynaptic) | Low (targeted) | Highly invasive (animal) | Monosynaptic specificity; complete input/output mapping; cellular resolution [78] | Invasive (animal only); no temporal dynamics; terminal experiments [78] |
| Neuropixels | Single neuron | Milliseconds (<1 ms) | Medium (279 regions simultaneously) | Invasive (animal) | Unprecedented neuron count; brain-wide single-cell activity; high temporal precision [79] | Limited to accessible regions; surgical expertise; data complexity [79] |
| Optogenetics+fMRI | 100-500 µm | Milliseconds (opsin) + seconds (BOLD) | Medium | Invasive (animal) | Causal circuit manipulation; cell-type specificity; whole-brain readout [76] [77] | Technical complexity; non-physiological activation; vascular confounds remain [77] |
| dTMS/fMRI | ~1 cm (stimulation) | Minutes (after-effects) | Medium | Non-invasive | Human applicable; therapeutic potential; causal interrogation [4] | Poor spatial precision; indirect effects; mechanisms unclear [4] |
Table 2: Method-Specific Applications in Addiction Neurocircuitry Analysis
| Technique | Addiction Circuit Insights | Optimal Use Cases | Technical Requirements |
|---|---|---|---|
| fMRI FC Analysis | Altered vmPFC-dlPFC-striatal connectivity in AUD; hub reorganization [75] [4] | Individual differences; treatment prediction; network-level deficits | High-field MRI; computational resources for 239 FC metrics [75] |
| Viral Tracing | ORB subregion input differences: ORBvl (intra-ORB), ORBm (prelimbic, hippocampal), ORBl (somatosensory) [78] | Circuit mechanism discovery; anatomical foundation for targeting | ABSL-2/3 facilities; stereotaxic expertise; quantitative neuroanatomy [78] |
| Large-Scale Electrophysiology | Brain-wide correlates of decision-making, reward processing in 621,733 neurons across 279 regions [79] | Neural coding of addiction behaviors; distributed circuit dynamics | Neuropixels systems; computational pipelines for >600K neurons [79] |
| Combined Opto-fMRI | Cell-type-specific contributions to BOLD; inhibitory neuron effects on hemodynamics [77] | Validation of fMRI signatures; cell-specific circuit manipulation | Combined opto-fMRI systems; viral vector expertise [77] |
| dTMS+fMRI | Normalization of vmPFC-amygdala connectivity; reduced craving with circuit modulation [4] [76] | Therapeutic development; causal human circuit interrogation | dTMS H-coils; neuronavigation; concurrent TMS-fMRI capability [4] |
Research Reagent Solutions
Table 3: Essential Materials for Advanced Circuit Mapping Experiments
| Reagent/Tool | Function | Example Application | Key Considerations |
|---|---|---|---|
| RV-ΔG (EnvA-pseudotyped) | Retrograde trans-monosynaptic tracing | Mapping inputs to specific ORB subregions [78] | Requires helper viruses (TVA+RG); strict biosafety protocols |
| rAAV Retrograde | Enhanced retrograde access | Labeling projection neurons | Higher efficiency than standard AAVs; broader tropism |
| Neuropixels 2.0 | Large-scale electrophysiology | Recording 621,733 neurons across 279 brain regions during decision-making [79] | Simultaneous multi-region sampling; specialized data processing |
| GLP-1 Receptor Agonists | Metabolic circuit modulation | Reducing alcohol self-administration in AUD models [5] | Emerging addiction therapeutic; central vs. peripheral effects |
| H-coils (dTMS) | Deep brain stimulation | Targeting vmPFC/dlPFC in AUD patients [4] | Reaches 5cm depth vs. 1.5cm for standard coils |
| Tetracysteine Display of Optogenetic Elements | Real-time monitoring & manipulation | Combined optogenetic control and calcium imaging [76] | Multifunctional probing; enhanced temporal precision |
Methodological Workflows
Troubleshooting Guides
Guide 1: Resolving Poor Neuroimaging Signal Quality in Prefrontal Cortex Assessments
Problem: Low signal-to-noise ratio (SNR) in fMRI data acquired from prefrontal cortex (PFC) regions during cognitive control tasks.
Explanation: The PFC is frequently implicated in addiction pathology, showing alterations in cocaine-dependent individuals [80]. Accurate measurement is crucial for predicting treatment outcomes.
Solution:
- Patient Preparation: Standardize pre-scan instructions to minimize motion. Instruct participants to avoid caffeine for 4 hours prior to scanning.
- Sequence Optimization: Utilize a multiband EPI sequence to reduce acquisition time and motion sensitivity. For a 3T scanner, recommended parameters are: TR=800ms, TE=30ms, flip angle=52°, voxel size=2mm isotropic.
- Real-Time Monitoring: Implement real-time motion tracking software (e.g., Framewise Integrated Real-time MRI Monitoring or FIRMM) to provide immediate feedback on head motion.
- Post-Processing: Apply advanced motion correction algorithms (e.g., FSL
MCFLIRTor AFNI3dVolreg) and integrate motion parameters as regressors in the general linear model.
Guide 2: Addressing High Participant Relapse Rates in Longitudinal Studies
Problem: A significant proportion of study participants relapse during follow-up, complicating the analysis of treatment efficacy.
Explanation: Relapse is a common feature of cocaine dependence, with specific neural circuitries acting as predictors [80].
Solution:
- Biomarker Stratification: At baseline, stratify participants into high-risk and low-risk groups using neuroimaging biomarkers. High-risk individuals exhibit lower pretreatment activity in the dorsolateral prefrontal cortex (dlPFC) and anterior cingulate cortex (ACC) during cognitive control tasks [80].
- Enhanced Support for High-Risk Cohort: For the high-risk group, implement intensified contingency management protocols with more frequent incentives for verified abstinence.
- Proactive Outreach: Establish a proactive outreach system with weekly check-ins (phone or virtual) for the first 90 days post-treatment, the period of highest relapse vulnerability.
- Data Analysis Plan: Pre-register a statistical analysis plan that uses survival analysis (e.g., Cox proportional hazards model) to handle censored data from participants lost to follow-up.
Guide 3: Managing Variable Responses to Brain Stimulation Interventions
Problem: Significant inter-individual variability in clinical response to neuromodulation treatments like TMS.
Explanation: The effects of non-invasive brain stimulation are influenced by individual differences in functional neuroanatomy [80].
Solution:
- Connectivity-Guided Targeting: Move beyond scalp-based targeting (e.g., 5-cm rule). Use individual resting-state fMRI data to identify the specific dlPFC subregion with maximal functional connectivity to the subgenual ACC. Neuronavigate the TMS coil to this personalized target.
- Dose Titration: Replace fixed-dose protocols with dose titration based on neurophysiological biomarkers. Use the individual's resting motor threshold (RMT) and concurrent fMRI or EEG to calibrate stimulation intensity to a neurophysiological effect, such as modulation of ACC activity.
- Closed-Loop Stimulation: For research purposes, explore closed-loop TMS systems that deliver stimulation triggered by specific, pre-identified neural states (e.g., high theta power in the ACC).
Frequently Asked Questions (FAQs)
Q1: What are the most robust neuroimaging biomarkers for predicting relapse in cocaine use disorder? The most consistent predictors include reduced baseline activity in the dorsolateral prefrontal cortex (dlPFC) and anterior cingulate cortex (ACC) during cognitive control tasks like the Stroop task, which is associated with a 74% accuracy in predicting relapse. Heightened reactivity of the amygdala and ventral striatum in response to drug cues is also a strong predictor, correlating with shorter time to relapse [80].
Q2: How can functional neuroimaging data be translated into a clinical treatment? Neuroimaging data can guide the development and application of neuromodulation therapies. For example, identifying a hypofrontal circuit in a patient can inform the target for repetitive Transcranial Magnetic Stimulation (rTMS). Functional MRI is used to pinpoint the specific dlPFC node most functionally connected to a pathological limbic node (e.g., the subgenual ACC), allowing for neuronavigated, circuit-based rTMS treatment [80].
Q3: Our team is new to implementing brain stimulation protocols. What is the essential equipment and its function? Below is a table of key research reagent solutions and essential materials:
| Item Name | Function/Brief Explanation |
|---|---|
| 3T MRI Scanner with fMRI capability | Acquires high-resolution structural and functional images to identify and target aberrant neural circuits. Essential for baseline assessment and neuronavigation [80]. |
| Neuronavigated TMS System | Deliates repetitive TMS pulses to specific brain targets. The neuronavigation component uses the individual's MRI data to guide coil placement for precise stimulation [80]. |
| Magstim Rapid(^2) or equivalent rTMS device | A commonly used research device capable of delivering high-frequency (e.g., 10Hz) stimulation to the prefrontal cortex [80]. |
| EEG Cap with 64+ channels | Records electrophysiological activity before, during, and after stimulation. Used to measure target engagement and neurophysiological effects like changes in P300 amplitude [80]. |
| Cocaine Cue Reactivity Task | A standardized task presented during fMRI scanning that displays drug-related images. It is used to assess limbic system reactivity, a key biomarker for relapse risk [80]. |
Q4: What are the standard parameters for a dorsolateral PFC rTMS protocol in addiction research? A common research protocol for cocaine use disorder involves high-frequency (10 Hz) stimulation applied to the left dlPFC. The typical parameters are: 10 Hz frequency, 3000 pulses per session, 100% of the resting motor threshold (RMT) intensity, delivered in 50 trains of 5-second duration with 25-second inter-train intervals. Treatment is often administered daily for 3-4 weeks [80].
Q5: We are designing a clinical trial. What are the most relevant primary and secondary endpoints for measuring treatment success? The most relevant endpoints are:
- Primary Endpoint: Biologically verified continuous abstinence from cocaine (e.g., via urine toxicology) over a defined period, such as the last 2-4 weeks of the treatment phase.
- Key Secondary Endpoints:
- Time to relapse (analyzed using survival models).
- Change in self-reported craving scores (e.g., using the Cocaine Craving Questionnaire).
- Change in neural circuit function from pre- to post-treatment, measured by fMRI during a cognitive control or cue reactivity task [80].
Data Presentation Tables
Table 1: Key Neural Circuit Biomarkers and Their Predictive Value for Relapse
| Neural Circuit / Region | Associated Function | Measurement Paradigm | Predictive Value for Relapse |
|---|---|---|---|
| Dorsolateral Prefrontal Cortex (dlPFC) | Executive Control, Cognitive Flexibility | fMRI during Stroop Task | Reduced baseline activity predicts relapse with ~74% accuracy [80]. |
| Anterior Cingulate Cortex (ACC) | Conflict Monitoring, Error Detection | fMRI during Stroop Task/Go-No-Go | Lower activity pre-treatment is linked to higher relapse rates [80]. |
| Amygdala / Ventral Striatum | Emotional Salience, Reward Processing | fMRI during Cocaine Cue Reactivity Task | Heightened reactivity predicts shorter time to relapse [80]. |
| Hippocampal Formation | Contextual Memory | Resting-State fMRI Functional Connectivity | Altered baseline functional connectivity predicts cocaine relapse [80]. |
Table 2: Comparison of Brain Stimulation Modalities in Cocaine Use Disorder
| Stimulation Modality | Target Circuit | Typical Parameters | Key Findings & Challenges |
|---|---|---|---|
| High-Frequency rTMS | Dorsolateral Prefrontal Cortex (dlPFC) | 10 Hz, 100% RMT, 3000 pulses/session | Shows promise in reducing craving; effects can be transient. Precise targeting is critical [80]. |
| Theta Burst Stimulation (TBS) | Dorsolateral Prefrontal Cortex (dlPFC) | Intermittent TBS (iTBS) to increase cortical excitability | Shorter protocol duration (3 minutes); efficacy in addiction is still under investigation. |
| Transcranial Direct Current Stimulation (tDCS) | Prefrontal Cortex | Anodal stimulation at 2 mA for 20-30 minutes | Less expensive and more portable; generally produces weaker and more variable effects compared to rTMS. |
Experimental Protocols
Protocol 1: fMRI Scan for Assessing Circuit-Level Biomarkers
Objective: To acquire high-quality structural and functional MRI data for evaluating executive control and cue-reactivity circuits in cocaine-dependent individuals.
Materials:
- 3T MRI Scanner with a 32-channel head coil.
- Standard fMRI preprocessing software (e.g., FSL, SPM, or AFNI).
- Cocaine Cue Reactivity Task and Stroop Task programmed in a stimulus presentation software (e.g., E-Prime or PsychoPy).
Procedure:
- Structural Scan: Acquire a high-resolution T1-weighted anatomical scan (e.g., MPRAGE sequence, 1mm isotropic voxels).
- Resting-State fMRI: Acquire a 10-minute resting-state functional scan (e.g., gradient-echo EPI, TR=2000ms, TE=30ms, voxel size=3mm isotropic). Instruct participants to keep their eyes open and fixate on a cross.
- Task-Based fMRI - Stroop Task: Administer the Stroop Task during fMRI acquisition. The task should include congruent and incongruent trials to probe executive control and conflict monitoring. Scan parameters should match the resting-state scan.
- Task-Based fMRI - Cue Reactivity: Administer the Cocaine Cue Reactivity Task. This block-design task should alternate between blocks of cocaine-related images and matched neutral images.
- Data Preprocessing: Process all functional data through a standardized pipeline including slice-time correction, motion correction, spatial smoothing (e.g., 6mm FWHM kernel), high-pass temporal filtering, and registration to standard (MNI) space.
Protocol 2: Neuronavigated rTMS Application to the dlPFC
Objective: To deliver targeted, high-frequency rTMS to the individual's dorsolateral prefrontal cortex based on their functional neuroanatomy.
Materials:
- Neuronavigated TMS System (e.g., Brainsight, Localite, or Visor2).
- Magstim Rapid(^2) or similar rTMS device with a cooled coil.
- Participant's individual T1-weighted anatomical MRI scan.
Procedure:
- Target Identification: Load the participant's MRI into the neuronavigation system. For the left dlPFC target, use the participant's own fMRI data from the Stroop task to identify the most active voxel within the dorsolateral prefrontal cortex. Alternatively, use a connectivity-based target (e.g., the point of peak functional connectivity with the subgenual ACC).
- Motor Threshold Determination: Locate the primary motor cortex (M1) hotspot for the abductor pollicis brevis (APB) muscle. Determine the Resting Motor Threshold (RMT), defined as the minimum stimulus intensity required to elicit a motor evoked potential (MEP) of >50 μV in at least 5 out of 10 trials.
- Coil Registration and Positioning: Register the participant's head to their MRI scan using the neuronavigation system. Position the TMS coil over the pre-defined dlPFC target, ensuring stable contact and maintaining a coil angle of approximately 45° from the mid-sagittal line.
- Stimulation Delivery: Deliver stimulation at 10 Hz frequency, 100% of RMT intensity. Administer 3000 pulses per session, structured as 50 trains of 5-second duration with 25-second inter-train intervals.
- Safety Monitoring: Continuously monitor the participant for adverse effects, such as headache or seizure. Adhere strictly to established TMS safety guidelines.
Signaling Pathways and Experimental Workflows
Neural Circuit Biomarker Analysis Workflow
rTMS Mechanism of Action on PFC Circuits
Frequently Asked Questions (FAQs)
Q1: What are the core neurocircuits involved in addiction, and how are they mapped onto a common framework?
The addiction cycle can be conceptualized as a three-stage, recurring process—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation (craving)—that involves specific, interacting neurocircuits. The table below summarizes the key brain regions and their primary functions in each stage for both substance and behavioral addictions [13] [6].
Table 1: Core Neurocircuits in the Addiction Cycle
| Addiction Stage | Key Brain Regions | Primary Function in Addiction | Manifestation in Substance Addiction | Manifestation in Behavioral Addiction |
|---|---|---|---|---|
| Binge/Intoxication | Ventral Tegmental Area (VTA), Ventral Striatum (Nucleus Accumbens) | Processes reward and reinforcement; driven by dopamine and opioid peptides [13] [6]. | Direct pharmacological enhancement of dopamine signaling [13]. | Indirect activation of dopamine system via behavior-induced reward [81]. |
| Withdrawal/Negative Affect | Extended Amygdala | Processes stress, anxiety, and negative emotions; driven by CRF, dynorphin, and norepinephrine [13] [6]. | Decreased dopamine function and recruitment of brain stress systems [13]. | Emergence of negative emotional states (e.g., irritability, anxiety) when behavior is prevented [81]. |
| Preoccupation/Anticipation | Prefrontal Cortex (PFC), Orbitofrontal Cortex, Dorsal Striatum, Insula, Anterior Cingulate Cortex | Mediates executive function, craving, decision-making, and inhibitory control [13] [6]. | Compromised executive function and glutamatergic dysregulation leading to craving and relapse [13]. | Pathological preoccupation with the behavior, loss of control, and relapse despite consequences [81]. |
Q2: What are the principal neurotransmitter systems implicated in addiction neurocircuitry, and how do they differ between substance and behavioral addictions?
Neurotransmitter dynamics are a key point of comparison. While substance addictions involve direct chemical intervention, behavioral addictions indirectly modulate similar systems. The following table provides a comparative overview of neurotransmitter changes across the addiction cycle [13] [81].
Table 2: Neurotransmitter Dynamics Across the Addiction Cycle
| Neurotransmitter/Neuromodulator | Change in Substance Addiction (by Stage) | Postulated Role in Behavioral Addiction |
|---|---|---|
| Dopamine | Binge/Intoxication [13]; Withdrawal [13]; Preoccupation (craving) [13] | Central role in reward and motivation, though activated indirectly by the behavior rather than by an exogenous substance [81]. |
| Opioid Peptides | Binge/Intoxication [13]; Receptor function in Withdrawal [13] | Likely involved in the pleasurable or pain-relieving effects of certain behaviors (e.g., compulsive eating, exercise) [81]. |
| Glutamate | Preoccupation/Anticipation (key mediator of craving and relapse) [13] | Implicated in cue-induced craving and relapse for behaviors like gambling [13]. |
| Corticotropin-Releasing Factor (CRF) | Withdrawal/Negative Affect [13]; Preoccupation/Anticipation (stress-induced relapse) [13] | A key mediator of the stress and anxiety experienced during withdrawal from the behavior [81]. |
| Dynorphin | Withdrawal/Negative Affect [13] | Contributes to the dysphoric state associated with withdrawal [13]. |
| Serotonin | Variable ( or depending on stage and substance) [13] | Implicated in mood regulation and impulse control; SSRIs can be an effective treatment for some behavioral addictions [81]. |
Q3: What experimental protocols are used to dissect the neurocircuitry of addiction in animal models?
To investigate the neurocircuitry of addiction, researchers employ a range of sophisticated behavioral paradigms and neural manipulation techniques. The workflow below outlines a standard protocol for studying the transition to compulsion, a core feature of addiction.
Protocol 1: Assessing Compulsive-like Seeking in a Self-Administration Model
- Objective: To determine the role of a specific neural circuit in the transition from controlled to compulsive drug or reward seeking.
- Materials:
- Animal Model: Typically, rodents (rats or mice).
- Apparatus: Operant conditioning chambers (Skinner boxes) equipped with an active lever (triggers reward infusion), an inactive lever (control), cue lights, and an infusion pump (for substance delivery) or a feeder (for behavioral reward like sugar).
- Stereotaxic Surgical Equipment: For implanting guide cannulae or optic fibers into target brain regions.
- Reward Substance: Drug of abuse (e.g., cocaine, heroin) dissolved in saline for intravenous self-administration, or a natural reward like a sugar solution.
- Methodology:
- Surgery & Recovery: Under anesthesia, implant an intravenous catheter for substance delivery and/or a guide cannula/optic fiber for circuit manipulation. Allow for post-surgical recovery [13].
- Acquisition Training: Train animals to self-administer the reward (drug or sugar) by pressing the active lever on a fixed-ratio (FR1) schedule. Each press results in reward delivery paired with a conditioned cue (e.g., light+tone) [13].
- Compulsion Probe Tests: After stable seeking is established, introduce aversive consequences to test for compulsivity.
- Progressive Ratio (PR) Schedule: The number of lever presses required for each subsequent reward increases exponentially. The final ratio completed ("breakpoint") measures motivation [13] [6].
- Signaled No-Conflict/Conflict Test: In one session, seeking is unpunished. In another, seeking is punished with a mild footshock (e.g., 0.2-0.3 mA). Compulsive subjects continue to seek the reward despite the punishment [6].
- Circuit Manipulation: During specific phases (e.g., before a seeking test), use optogenetics (light) or chemogenetics (Designer Receptors Exclusively Activated by Designer Drugs, DREADDs) to either inhibit or excite the neural pathway of interest.
- Example: Inhibit the projection from the prefrontal cortex to the nucleus accumbens core during the conflict test to see if it reduces compulsive seeking [6].
- Data Collection & Analysis:
- Primary Metrics: Number of active/inactive lever presses, breakpoint on PR, latency to seek reward.
- Statistical Analysis: Use t-tests or ANOVA to compare behavior between control and manipulation groups, and between no-conflict and conflict sessions.
Q4: How can researchers troubleshoot issues with behavioral specificity when manipulating neural circuits?
A common challenge is that activating or inhibiting a circuit node affects multiple behaviors, making it difficult to attribute the effect to a specific component of addiction. The following decision tree can guide troubleshooting.
Troubleshooting Guide: Achieving Behavioral Specificity
- Problem: The neural manipulation (e.g., inhibition of a VTA→NAc projection) disrupts not only compulsive seeking but also general locomotor activity and natural reward consumption, confounding interpretation.
- Solution Pathway:
- Verify Anatomical Specificity: Always confirm post-experiment that optic fibers or injection needles were accurately placed in the target region using histology. Subjects with off-target placements should be excluded from analysis.
- Refine Behavioral Assays: Ensure your task can dissociate the psychological process of interest (e.g., compulsion). Include control sessions.
- Example: If studying compulsive shock-resistant seeking, also run a session with a natural reward (e.g., sucrose) under the same conflict conditions. A specific effect on the drug-seeking circuit should not equally impair sucrose seeking [6].
- Control for Performance Confounds: Include control tests for general motor function and motivation. If your manipulation causes a general performance deficit, it cannot be uniquely attributed to compulsion. Using more specific genetic promoters (e.g., Cre-driver lines targeting specific cell types) can help isolate function.
- Increase Temporal Precision: Instead of continuous inhibition during a test session, use brief, phasic manipulations timed to specific events (e.g., only during the presentation of a drug-paired cue, or only during the act of lever pressing). This can isolate the circuit's role in a discrete cognitive process [82] [83].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential reagents and tools for modern addiction neurocircuitry research.
Table 3: Key Research Reagents and Materials for Addiction Neurocircuitry
| Item | Function/Application | Example Use Case |
|---|---|---|
| Cre-driver Mouse/Rat Lines | Provides genetic access to specific cell types (e.g., dopamine neurons, GABAergic neurons in the amygdala) for targeted manipulation [82]. | Expressing DREADDs or opsins specifically in VTA dopamine neurons to study their role in reward. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic tool for remote control of neuronal activity using an inert ligand (e.g., CNO) [6]. | Inhibiting prefrontal cortex neurons during a craving test to assess their necessity. |
| Channelrhodopsin (ChR2), Halorhodopsin (NpHR) | Optogenetic tools for millisecond-precision activation (ChR2) or inhibition (NpHR) of neurons with light [82] [83]. | Phasic stimulation of glutamatergic inputs to the NAc to probe their role in cue-induced relapse. |
| AAV (Adeno-Associated Virus) | Viral vector for delivering transgenes (e.g., DREADDs, opsins, sensors) to specific brain regions with high tropism and low toxicity. | Injecting AAV5-DIO-ChR2 into the VTA of a DAT-Cre mouse to enable optical control of dopamine neurons. |
| Fos-based Neuronal Activity Markers (e.g., c-Fos IHC) | Allows mapping of recently activated neurons (e.g., after a relapse event) to identify candidate circuits [13]. | Identifying which amygdala subnuclei are activated during withdrawal-induced negative affect. |
| Fiber Photometry Systems | Records population-level calcium dynamics in vivo, serving as a proxy for neural activity in a specific circuit during behavior [82]. | Recording real-time activity in the VTA-NAc pathway during the different stages of the addiction cycle. |
| Fast-Scan Cyclic Voltammetry (FSCV) | Measures real-time, phasic changes in neurotransmitter levels (primarily dopamine) in the brain [13]. | Detecting dopamine release in the NAc core upon presentation of a drug-paired cue. |
Frequently Asked Questions (FAQs)
Q1: What are the core neurocircuits involved in the addiction cycle, and what are their primary neurotransmitters? The addiction cycle is conceptualized as a three-stage recurring process: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. Each stage is mediated by distinct neurocircuits and neurotransmitter systems [13] [6].
- Binge/Intoxication Stage: This initial stage is centered on the rewarding effects of the drug. Key areas include the ventral tegmental area (VTA) and the ventral striatum (particularly the nucleus accumbens). The primary neurotransmitter for reward is dopamine, with significant contributions from opioid peptides [13].
- Withdrawal/Negative Affect Stage: When drug access is prevented, a negative emotional state emerges. This stage heavily involves the extended amygdala. Key stress neurotransmitters are upregulated, including corticotropin-releasing factor (CRF) and dynorphin, while reward system function (dopamine) is decreased [13].
- Preoccupation/Anticipation Stage: This craving stage involves a distributed network that includes the prefrontal cortex (orbitofrontal cortex, dorsolateral prefrontal cortex), basolateral amygdala, hippocampus, and insula. Key neurotransmitters here are glutamate and dopamine [13] [6].
Q2: My animal models do not show strong relapse behavior. What are key factors for modeling the transition to compulsion? A critical factor is incorporating models of negative reinforcement, not just positive reinforcement. Addiction often shifts from being about chasing a high to escaping the negative state of withdrawal [84]. Ensure your model includes:
- Withdrawal-Related Learning: Expose animals to repeated cycles of withdrawal and relapse. This teaches them that drug use relieves the "agony of withdrawal," creating a powerful, persistent urge to seek the drug even when faced with punishment [84].
- Focus on Specific Circuits: Recent research implicates the paraventricular nucleus of the thalamus (PVT) as hyperactive when animals learn that alcohol (or other drugs) relieves withdrawal discomfort. Measuring activity in this circuit can be a key biomarker [84].
Q3: What are emerging neurobiological targets for treating substance use disorders? Beyond traditional targets, Glucagon-Like Peptide-1 Receptor Agonists (GLP-1RAs) show promise. Preclinical and early clinical studies indicate that GLP-1 therapies can modulate the neurobiological pathways underlying addictive behaviors [5].
- Alcohol Use Disorder: A clinical trial with low-dose semaglutide showed reduced alcohol self-administration and craving [5].
- Opioid Use Disorder: In rodent models, GLP-1RAs reduce self-administration of heroin, fentanyl, and oxycodone, and reduce reinstatement of drug-seeking [5].
- Tobacco Use Disorder: Preclinical data show reduced nicotine self-administration and reinstatement of nicotine seeking [5].
Q4: How do I select an appropriate animal model for a specific stage of addiction? Animal models should be chosen based on the specific psychological construct or stage of the addiction cycle you wish to study [13]. The model should ideally mimic the transition from controlled use to loss of control.
- For Binge/Intoxication: Models of drug self-administration and conditioned place preference are standard.
- For Withdrawal/Negative Affect: Models that measure elevated anxiety-like behaviors and increased brain stress responses (e.g., CRF in the amygdala) during abstinence are key.
- For Preoccupation/Anticipation (Craving): Reinstatement models (drug-, cue-, or stress-induced) are the gold standard for studying relapse. Focus on circuits involving the prefrontal cortex and its glutamatergic projections to the basal ganglia and extended amygdala [13].
Experimental Protocols & Methodologies
Protocol 1: Whole-Brain Mapping of Cue-Induced Relapse Circuits
This protocol is designed to identify brain-wide networks activated during relapse-like behavior, particularly those linked to withdrawal-related learning [84].
- Animal Groups: Divide rats into four groups: (1) Experimental group with withdrawal-related learning; (2) Control group with drug exposure but no withdrawal learning; (3) Control group with saline; (4) Control group with naive handling.
- Behavioral Training:
- Train animals to self-administer alcohol or a drug of choice.
- The experimental group undergoes repeated cycles of withdrawal, where environmental cues are paired with the relief experienced when the drug is available again.
- Cue Exposure Test: Expose all groups to previously drug-paired cues in a controlled environment. Measure active seeking behaviors.
- Brain Tissue Collection: Euthanize animals immediately after the cue test during peak neural activity.
- Whole-Brain Imaging: Process brains for cellular activity markers (e.g., c-Fos). Use advanced imaging (e.g., serial two-photon tomography) to create activity maps across the entire brain.
- Data Analysis: Compare activity maps between the experimental and control groups. Focus on identifying regions with statistically significant elevated activity, such as the paraventricular nucleus of the thalamus (PVT) [84].
Protocol 2: Quantifying Neurotransmitter Dynamics in the Extended Amygdala During Withdrawal
This protocol details how to measure changes in key neurotransmitters during the withdrawal/negative affect stage [13].
- Surgery: Implant a guide cannula targeting the extended amygdala (e.g., central nucleus) in rats or mice.
- Dependence Induction: Use chronic drug administration (e.g., alcohol vapor inhalation for alcohol dependence) to induce a state of dependence.
- Microdialysis: During peak withdrawal (e.g., 6-8 hours after alcohol vapor removal), insert a microdialysis probe through the guide cannula and perfuse with artificial cerebrospinal fluid.
- Sample Collection: Collect dialysate samples at regular intervals (e.g., every 15-30 minutes).
- Biochemical Analysis: Analyze samples for concentrations of neurotransmitters and neuromodulators using techniques like:
- High-Performance Liquid Chromatography (HPLC) for CRF, dynorphin, dopamine, etc.
- Mass Spectrometry for a broader neuropeptide profile.
- Validation: Correlate neurochemical changes with behavioral measures of negative affect (e.g., elevated plus maze, acoustic startle response).
Data Presentation Tables
Table 1: Key Neurotransmitter Changes Across the Addiction Cycle
This table summarizes the primary neurochemical fluctuations during each stage of addiction [13].
| Stage | Neurotransmitter/Neuromodulator | Direction of Change | Primary Brain Region(s) |
|---|---|---|---|
| Binge/Intoxication | Dopamine | Increase | Ventral Tegmental Area, Ventral Striatum |
| Opioid Peptides | Increase | Ventral Striatum | |
| GABA | Increase | Ventral Tegmental Area | |
| Withdrawal/Negative Affect | Corticotropin-Releasing Factor (CRF) | Increase | Extended Amygdala |
| Dynorphin | Increase | Extended Amygdala | |
| Dopamine | Decrease | Ventral Striatum | |
| Neuropeptide Y | Decrease | Extended Amygdala | |
| Preoccupation/Anticipation | Glutamate | Increase | Prefrontal Cortex to Basal Ganglia/Extended Amygdala |
| Dopamine | Increase | Prefrontal Cortex | |
| Corticotropin-Releasing Factor (CRF) | Increase | Extended Amygdala |
Table 2: Research Reagent Solutions for Addiction Neurocircuitry
A list of essential materials and tools for investigating the neurocircuitry of addiction.
| Item | Function/Application |
|---|---|
| c-Fos Antibodies | Immunohistochemical marker for mapping neuronal activity in specific brain circuits following behavior (e.g., cue-induced relapse). |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic tool to selectively activate or inhibit specific neuronal populations in circuits like the PVT or extended amygdala to test causal roles. |
| AAV vectors for Calcium Indicators (e.g., GCaMP) | For in vivo calcium imaging to monitor real-time neural activity in deep brain structures during drug-seeking behavior. |
| CRF Receptor Antagonists | Pharmacological tools to test the role of brain stress systems in the withdrawal/negative affect stage and potential to reduce relapse. |
| GLP-1 Receptor Agonists (e.g., semaglutide) | Emerging therapeutic agents to test for reduction in drug self-administration and craving across multiple substance use disorders [5]. |
| Microdialysis Probes | For in vivo sampling of neurotransmitter dynamics (e.g., glutamate, dopamine, CRF) in specific brain regions during behavior. |
Experimental Workflow and Signaling Pathways
Diagram 1: Three Stage Addiction Neurocircuitry Model
Diagram 2: PVT Circuit in Withdrawal-Related Relapse
Conclusion
The analysis of addiction neurocircuitry faces significant technical challenges but offers promising pathways for advancing treatment development. Key takeaways include the need for more sophisticated computational models that capture the full addiction cycle, improved methodologies for addressing individual variability in circuit dysfunction, and better integration between different analytical approaches. Future directions should focus on developing personalized neuromodulation protocols based on individual neurocircuitry profiles, creating more comprehensive computational models that simulate multiple addiction symptoms, and establishing standardized validation frameworks for cross-study comparisons. The convergence of advanced computational modeling, precision neuromodulation, and multi-modal neuroimaging represents the most promising approach for translating addiction neurocircuitry research into effective clinical interventions for substance use disorders.
References
- 1. Neurocircuitry of Addiction - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2805560/]
- 2. Common neural patterns of substance use disorder: a seed ... [https://www.nature.com/articles/s41398-025-03396-2]
- 3. Human dopamine systems in addiction disorders [https://www.sciencedirect.com/science/article/abs/pii/B9780443298677000293]
- 4. A deep TMS/fMRI trial in people with alcohol use disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273219/]
- 5. GLP-1s show promise in treating alcohol and drug addiction [https://www.endocrine.org/news-and-advocacy/news-room/2025/glp1s-show-promise-in-treating-alcohol-and-drug-addiction]
- 6. Neurocircuitry of Addiction | Neuropsychopharmacology [https://www.nature.com/articles/npp2009110]
- 7. Ventral Tegmental Area Afferents and Drug-Dependent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4780106/]
- 8. Dopamine Circuit Mechanisms of Addiction-Like Behaviors [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2021.752420/full]
- 9. The ins and outs of the striatum: Role in drug addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4523218/]
- 10. Brain stress systems in the amygdala and addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2774745/]
- 11. Dysfunction of the prefrontal cortex in addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC3462342/]
- 12. Alterations in Striatal Circuits Underlying Addiction-Like ... [https://www.sciencedirect.com/science/article/pii/S1016847823006258]
- 13. Neurobiology of addiction: a neurocircuitry analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6135092/]
- 14. Review Neurobiology of addiction: a neurocircuitry analysis [https://www.sciencedirect.com/science/article/abs/pii/S2215036616001048]
- 15. Addiction and the brain: the role of neurotransmitters in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC80880/]
- 16. The Neuroscience of Drug Reward and Addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6890985/]
- 17. Identifying Internet Addiction and Evaluating the Efficacy of ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.665578/full]
- 18. Dorsal and ventral striatal functional connectivity shifts play ... [https://www.nature.com/articles/s42003-021-02395-5]
- 19. Resting-State Functional Connectivity of the Dorsal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10519818/]
- 20. Mechanisms and interventions promoting healthy ... [https://www.nature.com/articles/s41467-025-62190-2]
- 21. Brain lesions disrupting addiction map to a common ... [https://www.nature.com/articles/s41591-022-01834-y]
- 22. Unbalanced neuronal circuits in addiction [https://www.sciencedirect.com/science/article/abs/pii/S0959438813000184]
- 23. The Neurocircuitry of Fear, Stress, and Anxiety Disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3055419/]
- 24. The Reinforcement Learning Handbook: A Guide to ... [https://towardsdatascience.com/the-handbook-of-reinforcement-learning-guide-to-the-foundational-questions/]
- 25. Computational models of behavioral addictions [https://www.sciencedirect.com/science/article/abs/pii/S0306460322003616]
- 26. Bayesian Statistics: A Modern Data Analysis in 2025 [https://clinilaunchresearch.in/guide-to-bayesian-statistics/]
- 27. Computational Models of Drug Use and Addiction: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC7416739/]
- 28. Functional Magnetic Resonance Imaging (fMRI) - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK538909/]
- 29. Spectral dynamic causal modeling: A didactic introduction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10898785/]
- 30. Brain functional and effective connectivity based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8720201/]
- 31. A Practical Guide for Generating Reproducible and ... [https://apertureneuro.org/article/85104-a-practical-guide-for-generating-reproducible-and-programmatic-neuroimaging-visualizations]
- 32. Effective Connectivity [https://medphysics.wisc.edu/research/fmri/functional-magnetic-resonance-imaging-fmri-2/]
- 33. Brain Imaging: SPECT, fMRI, & QEEG and what they ... [https://www.neurocaregroup.com/news-insights/brain-imaging-what-they-uncover]
- 34. A systematic review and meta-analysis of neuromodulation ... [https://www.nature.com/articles/s41386-023-01776-0]
- 35. Deep TMS™ Patient Manual | Info for MDD Treatment [https://www.brainsway.com/brainsway-treatment-for-major-depressive-disorder-patient-manual/]
- 36. Transcranial magnetic stimulation [https://www.mayoclinic.org/tests-procedures/transcranial-magnetic-stimulation/about/pac-20384625]
- 37. Deep Brain Stimulation Troubleshooting and DBS Failures ... [https://movementdisorders.ufhealth.org/surgery/dbs-troubleshooting-and-dbs-failures-clinic/]
- 38. Support & Resources [https://www.brainproducts.com/support-resources/]
- 39. Ventral medial prefrontal cortex (vmPFC) as a target of the ... [https://pubmed.ncbi.nlm.nih.gov/27138429/]
- 40. Differential roles of medial prefrontal subregions in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4472631/]
- 41. The future of brain circuit-targeted therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10700386/]
- 42. Decoding the hidden variabilities in mPFC descending ... [https://elifesciences.org/reviewed-preprints/105528]
- 43. The functional relevance of right DLPFC and VMPFC in ... [https://www.sciencedirect.com/science/article/pii/S0010945222003288]
- 44. Prefrontal cortex plasticity mechanisms in drug seeking ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763409001821]
- 45. Integrating multimodal data through interpretable heterogeneous ensembles - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9347276/]
- 46. What is Multimodal Data? Types, Examples, Applications & More [https://www.tiledb.com/multimodal-data]
- 47. A Unique Color-Coded Visualization System with Multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10204620/]
- 48. Harnessing multimodal data integration to advance precision oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8810682/]
- 49. Data visualization colors [https://cloudscape.design/foundation/visual-foundation/data-vis-colors/]
- 50. Neuroscience: The Brain in Addiction and Recovery [https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/neuroscience-brain-addiction-and-recovery]
- 51. Variability of Neuronal Responses: Types and Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122744/]
- 52. Machine Learning of Functional Connectivity to Biotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10976073/]
- 53. Identifying alcohol misuse biotypes from neural ... [https://www.nature.com/articles/s41398-022-01983-1]
- 54. Harnessing neural variability: Implications for brain ... [https://www.sciencedirect.com/science/article/pii/S0149763425003136]
- 55. The neural correlates of novelty and variability in human ... [https://elifesciences.org/articles/92892]
- 56. Neurocircuitry-Inspired Hierarchical Graph Causal ... [https://arxiv.org/html/2511.17622v1]
- 57. Theory-driven computational models of drug addiction in ... [https://www.sciencedirect.com/science/article/pii/S2772392523000068]
- 58. Ten simple rules for the computational modeling of ... [https://elifesciences.org/articles/49547]
- 59. Gephi - The Open Graph Viz Platform [https://gephi.org/]
- 60. Motion Artefacts in MRI: a Complex Problem with Many Partial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4517972/]
- 61. Reducing motion artefact in high resolution 7T MRI using ... [https://www.medrxiv.org/content/10.1101/2025.10.10.25337727v1]
- 62. How to measure SNR [https://mriquestions.com/signal-to-noise.html]
- 63. Characterizing motion artifacts in functional near-infrared ... [https://www.sciencedirect.com/science/article/pii/S1746809425007670]
- 64. a new dawn for overcoming substance use disorders [https://www.nature.com/articles/s41398-024-03156-8]
- 65. optimizing stimulation parameters with vagus nerve ... [https://www.sciencedirect.com/science/article/pii/S1935861X25002670]
- 66. Modeling and optimizing deep brain stimulation to ... [https://www.nature.com/articles/s41531-025-00990-5]
- 67. kinematic gait parameters inform optimization of stimulation ... [https://pubmed.ncbi.nlm.nih.gov/40926219/]
- 68. Stimulation-Based Control of Dynamic Brain Networks - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5017638/]
- 69. A Review of Parameter Settings for Invasive and Non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8313807/]
- 70. Translational opportunities in animal and human models to ... [https://www.nature.com/articles/s41398-021-01615-0]
- 71. Common neurocircuitry mediating drug and fear relapse in ... [https://link.springer.com/article/10.1007/s00213-018-5024-3]
- 72. Understanding Addiction Using Animal Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6895146/]
- 73. Toward addiction prediction: An overview of cross- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8274215/]
- 74. Development and validation of a machine learning model ... [https://www.sciencedirect.com/science/article/pii/S0165032725011711]
- 75. Benchmarking methods for mapping functional connectivity ... [https://www.nature.com/articles/s41592-025-02704-4]
- 76. Neural Circuit Mapping and Neurotherapy-Based Strategies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297084/]
- 77. The road to mapping neural circuits with fMRI: Challenges ... [https://apertureneuro.org/article/138741-the-road-to-mapping-neural-circuits-with-fmri-challenges-and-advances]
- 78. Anatomical mapping of whole-brain monosynaptic inputs to ... [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2025.1567036/full]
- 79. A brain-wide map of neural activity during complex behaviour [https://www.nature.com/articles/s41586-025-09235-0]
- 80. Using Neuroimaging to Predict Relapse and Develop Brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0074774216301131]
- 81. Behavioral Addiction versus Substance Addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC3354400/]
- 82. Overlap and divergence of neural circuits mediating distinct ... [https://pubmed.ncbi.nlm.nih.gov/39306846/]
- 83. Overlap and divergence of neural circuits mediating distinct ... [https://www.sciencedirect.com/science/article/pii/S2211124724011331]
- 84. Scientists find brain circuit that traps alcohol users in ... [https://www.sciencedaily.com/releases/2025/10/251006051124.htm]