Targeting the Microbiota-Gut-Brain Axis: Mechanisms and Therapeutic Applications in Neurodegenerative Diseases
This article synthesizes current evidence on the critical role of the microbiota-gut-brain axis (MGBA) in the pathogenesis of neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and Amyotrophic Lateral Sclerosis.
Targeting the Microbiota-Gut-Brain Axis: Mechanisms and Therapeutic Applications in Neurodegenerative Diseases
Abstract
This article synthesizes current evidence on the critical role of the microbiota-gut-brain axis (MGBA) in the pathogenesis of neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and Amyotrophic Lateral Sclerosis. It explores the foundational communication pathways—neural, immune, endocrine, and metabolic—through which gut microbiota influence neuroinflammation, blood-brain barrier integrity, and protein aggregation. For researchers and drug development professionals, the review further evaluates therapeutic strategies such as probiotics, prebiotics, fecal microbiota transplantation, and dietary interventions, analyzing their mechanistic basis and clinical potential. The discussion also addresses key challenges, including inter-individual variability and the translation of pre-clinical findings, while proposing future directions for precision medicine and novel biomarker development in neurology.
Decoding the Gut-Brain Network: Core Pathways and Mechanisms in Neurodegeneration
The microbiota-gut-brain axis (MGBA) represents one of the most significant paradigms in modern neuroscience, delineating a complex, bidirectional communication network that integrates the gastrointestinal tract with the central nervous system (CNS) [1] [2]. This axis is gaining ever more traction in fields investigating the biological basis of neurodegenerative, neuropsychiatric, and neurodevelopmental disorders [1]. The MGBA comprises several anatomical structures and utilizes a multitude of parallel and interconnected signaling pathways, including neural, endocrine, immune, and metabolic routes [2] [3]. Within the context of neurodegenerative diseases such as Alzheimer's disease (AD) and Parkinson's disease (PD), disruptions in this axis are implicated in fundamental pathological processes including neuroinflammation, protein misfolding, and neuronal homeostasis [2] [3]. This whitepaper provides an in-depth anatomical and functional dissection of the core MGBA components, framed for researchers and drug development professionals exploring novel therapeutic avenues in neurodegeneration.
Core Anatomical Components of the MGBA
The integrated MGBA system spans multiple organ systems and interfaces. The table below summarizes the key anatomical components and their primary functions within the axis.
Table 1: Core Anatomical Components of the Microbiota-Gut-Brain Axis
| Anatomical Component | Description | Primary Function in MGBA |
|---|---|---|
| Gut Microbiota | Trillions of commensal microorganisms (bacteria, viruses, archaea, fungi) residing primarily in the colon [2]. | Core regulator; produces a vast repertoire of neuroactive metabolites (SCFAs, neurotransmitters) and antigens that initiate host signaling [2] [3]. |
| Intestinal Mucosa & Barrier | Single-cell epithelial layer with tight junctions, overlain by mucus and patrolled by immune cells [2]. | Critical interface; maintains separation between luminal contents and host interior. "Leaky" gut can permit bacterial translocation and systemic inflammation [2]. |
| Enteric Nervous System (ENS) | An extensive network of ~500 million neurons embedded in the gut wall [2]. | The "second brain"; regulates gut motility, secretion, and blood flow; communicates bidirectionally with the CNS [2] [4]. |
| Vagus Nerve | The major neural highway connecting the gut and the brainstem [2]. | Provides a direct, rapid neural pathway; vagal afferents transmit sensory signals from gut to brain, efferents carry brain commands to gut [2] [4]. |
| Neuroendocrine System (HPA Axis) | The hypothalamic-pituitary-adrenal (HPA) axis, a central neuroendocrine system [2]. | Translates stress signals into systemic hormone release (e.g., cortisol); stress can alter gut barrier integrity and microbiota composition [2] [5]. |
| Systemic Circulation & Blood-Brain Barrier (BBB) | The circulatory system and the specialized vascular interface of the CNS [2] [3]. | Transports gut-derived immune and metabolic signals; BBB permeability determines which factors can access the CNS parenchyma [2] [6]. |
| Central Nervous System (CNS) Cells | Includes neurons, microglia (resident immune cells), astrocytes, and oligodendrocytes [3]. | Ultimate target and regulator; microglia are particularly crucial, as their maturation and function are profoundly influenced by microbial signals [3] [6]. |
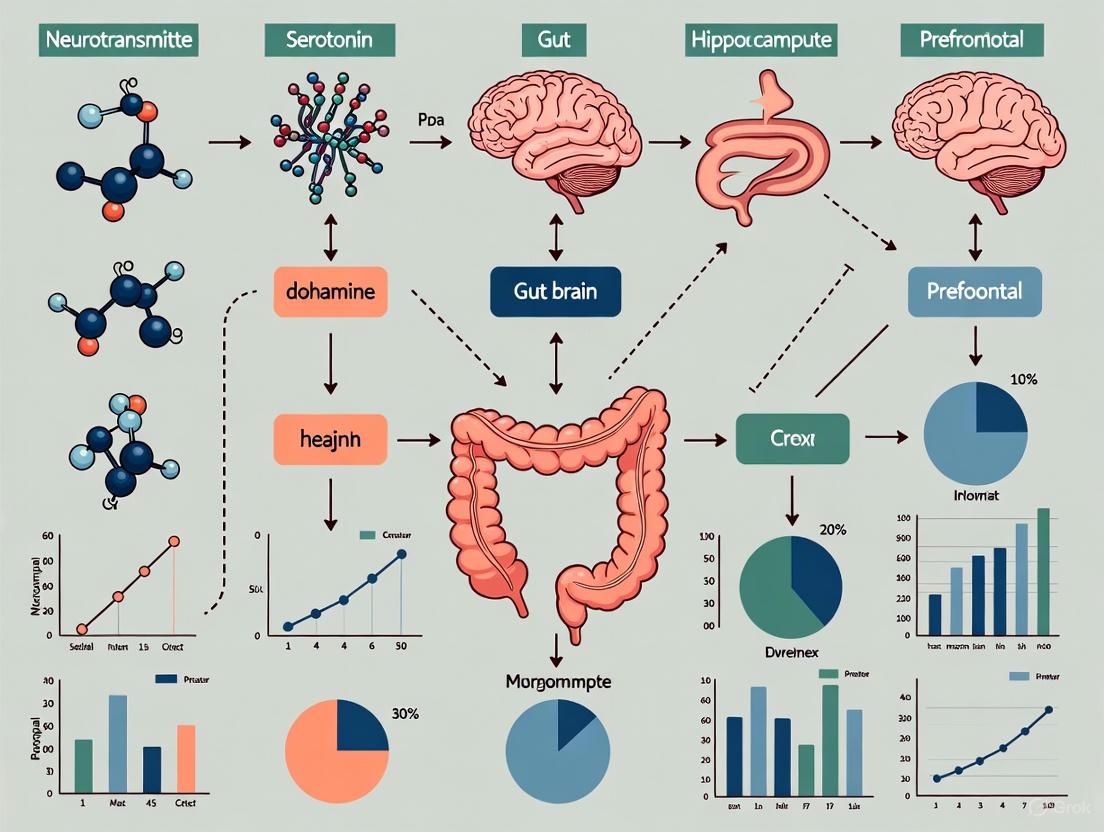
The following diagram illustrates the anatomical structure and primary communication routes of the MGBA:
Diagram 1: Anatomical structure and communication routes of the MGBA.
Key Communication Pathways and Mechanisms
Signaling along the MGBA occurs through several interdependent pathways that can be categorized into four primary types.
Neural Pathways
The vagus nerve is the primary direct neural connection, providing a rapid communication route [2]. Vagal afferents detect nutrients, mechanical stretch, and microbial molecules in the gut, relaying this information to the brainstem [2] [4]. In turn, vagal efferents modulate gastrointestinal secretion, motility, and local immune responses [2]. The enteric nervous system (ENS) acts as a local processor, integrating signals from the gut lumen and communicating with the CNS via the vagus and spinal nerves [2]. Intrinsic Primary Afferent Neurons (IPANs) within the ENS can synapse with the vagus nerve, forming a critical gut-brain neural circuit [4]. This pathway is implicated in the progression of neurodegenerative diseases; for instance, in Parkinson's disease, pathological α-synuclein aggregates are hypothesized to originate in the gut and spread to the brain in a prion-like fashion via the vagus nerve [2].
Immune and Inflammatory Pathways
The gut microbiome fundamentally shapes the host immune system. A compromised intestinal barrier allows microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS), to enter circulation [2]. LPS can then activate Toll-like receptors (e.g., TLR4) on peripheral immune cells and CNS microglia, triggering neuroinflammation via NF-κB signaling [2] [6]. Furthermore, gut-resident immune cells conditioned by the microbiota, such as pro-inflammatory Th17 cells and anti-inflammatory regulatory T cells (Tregs), can traffic to the CNS and influence local inflammation [2] [6]. Microbial metabolites, particularly short-chain fatty acids (SCFAs) like butyrate, promote the differentiation of Tregs and have demonstrated anti-inflammatory effects in experimental models of multiple sclerosis [2].
Endocrine and Metabolic Pathways
The hypothalamic-pituitary-adrenal (HPA) axis is a major neuroendocrine arm of the MGBA. Psychological stress activates the HPA axis, leading to the release of cortisol (corticosterone in rodents), which can increase intestinal permeability and alter microbiota composition, creating a vicious cycle [2] [5]. Conversely, gut microbes and their metabolites can influence HPA axis activity [6]. The gut microbiota also produces or modulates a wide array of neuroactive metabolites. SCFAs (acetate, propionate, butyrate), derived from dietary fiber fermentation, can cross the BBB, influence microglial maturation and function, and modulate systemic inflammation [2] [3]. Other crucial metabolites include tryptophan derivatives and bile acids, which can interact with host receptors to influence CNS function and neuroinflammation [2] [3].
The flow of signals through these primary pathways is summarized below:
Diagram 2: Key signaling pathways from gut to brain in neurodegeneration.
Experimental Approaches for MGBA Investigation
Research into the MGBA relies on a combination of animal models, molecular techniques, and microbial interventions. The following table outlines a detailed experimental protocol from a seminal study investigating the intergenerational effects of an anesthetic on the MGBA [5].
Table 2: Detailed Experimental Protocol for MGBA Research in an Animal Model
| Protocol Aspect | Detailed Methodology |
|---|---|
| Study Objective | To examine whether paternal sevoflurane exposure induces abnormalities in the brain-gut-microbiome (BGM) axis in exposed rats (F0) and their offspring (F1), and whether pretreatment with bumetanide or RU486 mitigates these effects [5]. |
| Animal Model | Male Sprague Dawley rats (F0 generation) and their future offspring (F1 generation) [5]. |
| Treatment Groups | - F0MC: Control males (saline injection, no anesthesia).- F0MS: Sevoflurane-exposed males (2.1% sevoflurane for 3 hours on P56, P58, P60).- F0MBS: Bumetanide (1.84 mg/kg, i.p.) 30 min pre-sevoflurane.- F0MRS: RU486 (10 mg/kg, i.p.) 30 min pre-sevoflurane [5]. |
| Sample Collection | - Gut Microbiota: Fecal samples collected 1 hour and 30 days post-final sevoflurane exposure in F0; from F1 offspring at P95. Profiled via 16S rRNA gene sequencing [5].- Brain Tissue: Hippocampal samples from F0 (P135) and F1 (P95) for RNA sequencing to analyze transcriptomic changes [5].- Blood/Serum: Collected for measuring corticosterone (stress response), IL-6 (inflammation), and LDL-C (metabolism) [5]. |
| Behavioral & Functional Assessments | - Social Hierarchy: Tube test to assess social dominance and forced loss paradigm [7].- Stress Responsiveness: Serum corticosterone measured after a prepulse inhibition (PPI) test [5]. |
| Data Analysis | Variations in biochemical markers analyzed with one-way ANOVA and post-hoc tests. Gut microbiome and RNA sequencing data analyzed and visualized in R [5]. |
The Scientist's Toolkit: Key Research Reagents
The following table catalogues essential reagents and materials used in advanced MGBA research, as derived from the cited experimental protocols.
Table 3: Key Research Reagent Solutions for MGBA Investigation
| Reagent / Material | Function and Application in MGBA Research |
|---|---|
| 16S rRNA Gene Sequencing | A culture-independent method used to profile and characterize the composition of the gut microbiota community from fecal or colonic content samples [5] [7]. |
| Metagenomic Sequencing | Enables comprehensive analysis of the collective genetic material of the gut microbiome, allowing functional inference of microbial pathways (e.g., butanoate metabolism) [7]. |
| Single-Nucleus RNA Sequencing (snRNA-seq) | Allows for the investigation of cell-type-specific transcriptomic changes within complex tissues like the prefrontal cortex (PFC), identifying alterations in specific neuronal and glial populations [7]. |
| Bumetanide | A Na+-K+-Cl- (NKCC1) cotransporter inhibitor. Used in pre-clinical studies to block chloride import into neurons, demonstrating efficacy in mitigating sevoflurane-induced abnormalities in the MGBA [5]. |
| RU486 (Mifepristone) | A glucocorticoid receptor (GR) blocker. Used experimentally to inhibit stress hormone signaling, shown to prevent neurocognitive and MGBA abnormalities induced by paternal sevoflurane exposure [5]. |
| Broad-Spectrum Antibiotic Cocktail | Used to deplete the gut microbiota in animal models (e.g., mice), enabling researchers to study the functional consequences of a absent or disrupted microbiome and establish causal relationships [7]. |
| Probiotics and Prebiotics | Live beneficial bacteria and non-digestible food ingredients that selectively stimulate microbial growth. Used in interventional studies to modulate the gut ecosystem and assess effects on MGBA signaling and brain function [3] [8]. |
| Fecal Microbiota Transplantation (FMT) | The process of transferring fecal material from a donor to a recipient to reconstitute the gut microbiota. A powerful tool to demonstrate causal roles of the microbiome in disease phenotypes [2] [3]. |
Implications for Neurodegenerative Disease Research
Targeting the MGBA presents a transformative perspective for understanding and treating neurodegenerative diseases. Gut dysbiosis has been documented in AD, PD, ALS, and MS, often characterized by reduced microbial diversity, depletion of SCFA-producing bacteria, and enrichment of pro-inflammatory taxa [2] [8]. These alterations are thought to contribute to pathogenesis through the mechanisms detailed above, including driving neuroinflammation, compromising BBB integrity, and promoting the aggregation of pathological proteins like α-synuclein and amyloid-β [2] [3].
Consequently, therapeutic strategies aimed at modulating the MGBA are under intense investigation. These include:
- Probiotics and Prebiotics: Specific bacterial strains and dietary fibers designed to restore a healthy microbial balance and increase the production of beneficial metabolites like SCFAs [8] [9].
- Fecal Microbiota Transplantation (FMT): Shown to modulate disease progression in animal models and is being explored in early human trials [2] [3].
- Dietary Interventions: Diets rich in fiber (e.g., Mediterranean diet) can positively shape the gut microbiome and have been associated with a reduced risk of cognitive decline [8].
- Small-Molecule Modulators: Drugs that target receptors for microbial metabolites (e.g., bile acid receptors, SCFA receptors) or that strengthen barrier integrity are emerging as promising avenues [2] [3].
The anatomy of the microbiota-gut-brain axis is intricate, involving a relay of signals from the gut lumen through epithelial, neural, immune, and endocrine interfaces to the brain. For researchers in neurodegeneration, a deep understanding of these components and their communication pathways is no longer a niche interest but a necessity for pioneering the next generation of therapeutics. The experimental tools and mechanistic insights outlined in this whitepaper provide a foundation for developing targeted interventions that leverage the MGBA to slow disease progression and improve brain health. Future research must focus on establishing causal relationships in humans, accounting for inter-individual variability, and translating these promising pre-clinical findings into robust, effective clinical applications.
The gut-brain axis represents one of the most sophisticated bidirectional communication systems in human physiology, integrating neural, endocrine, and immune signaling pathways between the gastrointestinal tract and the central nervous system (CNS). At the core of this system lie two fundamental neural structures: the vagus nerve (cranial nerve X), which serves as the primary neural superhighway connecting the brain to peripheral organs, and the enteric nervous system (ENS), an extensive intrinsic neural network often described as the "second brain" of the gut [10] [11]. These structures form the foundational neural architecture through which the gut microbiota influences brain function and, consequently, the pathogenesis and progression of neurodegenerative diseases. Understanding their anatomical organization, physiological functions, and communication mechanisms provides critical insights for developing novel therapeutic strategies targeting neurodegenerative conditions through gut-brain pathways.
Anatomical and Functional Organization
The Vagus Nerve: Structural Architecture
The vagus nerve is the longest and most complex cranial nerve, exhibiting extensive anatomical distribution from the brainstem to the abdominal viscera. As a mixed nerve containing approximately 80% afferent and 20% efferent fibers [11], it serves as the primary information conduit between the brain and body. The nerve originates from the medulla oblongata, specifically from three nuclei: the nucleus ambiguus, dorsal motor nucleus, and solitary tract nucleus [12]. It exits the skull through the jugular foramen and descends within the carotid sheath, positioned posterolateral to the internal and common carotid arteries and medial to the internal jugular vein [12] [11].
The vagus nerve demonstrates distinct anatomical trajectories on the left and right sides. The right vagus nerve travels anteriorly to the subclavian artery and posterior to the innominate artery, descending into the thoracic cavity to the right of the trachea and posterior to the right hilum before forming the esophageal plexus with the left vagus nerve [12]. The left vagus nerve passes between the left common carotid and subclavian arteries, descending posteriorly to the left lung before traveling medially to contribute to the esophageal plexus [12]. This extensive anatomical distribution enables the vagus nerve to interface with multiple organ systems, including the heart, lungs, and gastrointestinal tract.
Table: Major Branches of the Vagus Nerve and Their Functions
| Branch | Innervation | Primary Functions |
|---|---|---|
| Pharyngeal branches | Pharyngeal and palate muscles (except tensor veli palatini) | Swallowing, gag reflex, formation of pharyngeal plexus |
| Superior laryngeal nerve | Cricothyroid muscle, mucosa superior to glottis | Voice modulation, laryngeal sensation |
| Recurrent laryngeal nerve | All intrinsic laryngeal muscles except cricothyroid | Vocal cord movement, phonation |
| Superior cardiac nerve | Heart | Parasympathetic control of heart rate (slowing) |
| Anterior and posterior bronchial branches | Lungs | Formation of pulmonary plexuses, bronchoconstriction |
| Gastric and celiac branches | Stomach, pancreas, spleen, kidneys, adrenals, small intestine | Regulation of gastric emptying, acid production, intestinal secretion |
The Enteric Nervous System: Structural Organization
The ENS constitutes an intrinsic nervous system within the gastrointestinal wall, containing approximately 500 million neurons – a number comparable to the spinal cord [2]. This sophisticated network is organized into two major interconnected plexuses: the myenteric plexus (Auerbach's plexus) located between the longitudinal and circular muscle layers, and the submucosal plexus (Meissner's plexus) situated within the submucosa [10]. The myenteric plexus primarily regulates gastrointestinal motility, while the submucosal plexus controls secretory functions and local blood flow [10] [13].
The cellular composition of the ENS includes diverse neuronal subtypes (sensory, motor, and interneurons) and enteric glial cells, which far outnumber neurons and play crucial roles in maintaining intestinal barrier integrity, modulating immune responses, and supporting neuronal function [13]. The ENS operates with significant autonomy but maintains continuous communication with the CNS through parasympathetic (primarily vagal) and sympathetic pathways, positioning it as a critical intermediary in gut-brain communication.
Communication Pathways and Mechanisms
The vagus nerve and ENS participate in sophisticated bidirectional communication through multiple integrated signaling pathways that collectively form the microbiota-gut-brain axis (MGBA). These pathways enable continuous information exchange between the CNS and gastrointestinal system, with profound implications for brain health and neurodegenerative disease progression.
Figure 1: Integrated Communication Pathways of the Microbiota-Gut-Brain Axis. This diagram illustrates the bidirectional communication between the gut and brain through neural, immune, and endocrine/metabolic pathways, with the vagus nerve and enteric nervous system serving as central components.
Neural Signaling Pathways
The vagus nerve provides the most direct neural connection between the gut and brain. Vagal afferent fibers sense mechanical stretch, nutrients, and microbial metabolites in the gut, relaying this information to the brainstem nuclei, particularly the nucleus tractus solitarius [2]. These signals are then integrated within central autonomic networks that influence mood, appetite, and parasympathetic output. Vagal efferent fibers, in contrast, modulate gastrointestinal secretion, motility, and local immune responses [2] [12].
The ENS operates with considerable autonomy but remains under vagal modulation. Gut microbes influence ENS development and function through multiple mechanisms, including the production of neurotransmitters (GABA, serotonin, histamine) that activate enteric neurons [2]. This microbial-ENS communication enables local reflex control of gut functions while simultaneously informing central processes through vagal afferent signaling.
Immune and Inflammatory Pathways
The cholinergic anti-inflammatory pathway, mediated by the vagus nerve, represents a critical mechanism for gut-brain-immune communication. Vagus nerve activation suppresses peripheral inflammation through efferent signaling that inhibits pro-inflammatory cytokine release (e.g., TNF-α, IL-1β, IL-6) from intestinal macrophages and other immune cells [11] [14].
Gut microbes significantly shape host immune responses through direct interaction with pattern recognition receptors. Microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS) from gram-negative bacteria, can breach a compromised intestinal barrier and enter circulation, where they activate Toll-like receptors (TLRs) and other innate immune sensors [2] [6]. This activation triggers neuroinflammatory cascades that contribute to neuronal injury in neurodegenerative diseases [2].
Gut microbiota also influences the differentiation of specialized immune cell populations. Specific commensal bacteria promote regulatory T cell (Treg) development through short-chain fatty acid (SCFA) production, while others, like segmented filamentous bacteria, drive pro-inflammatory Th17 cell expansion [2] [6]. These peripherally activated immune cells can traffic to the CNS, influencing neuroinflammation and neurodegeneration.
Neuroendocrine and Metabolic Signaling
Gut microbiota produce a diverse array of neuroactive metabolites that significantly influence brain function. SCFAs (butyrate, propionate, acetate), derived from microbial fermentation of dietary fiber, modulate brain function through multiple mechanisms: they enhance blood-brain barrier integrity, inhibit histone deacetylases to regulate gene expression, and serve as ligands for G-protein coupled receptors (GPR41, GPR43) on enteroendocrine and immune cells [2] [6].
Microbial neurotransmitters include GABA (major inhibitory neurotransmitter), serotonin (approximately 90% of body's supply), dopamine, and norepinephrine produced by gut bacteria [13]. These microbial neurotransmitters can directly activate enteric neurons and vagal afferents, influencing central neurotransmitter systems involved in mood, cognition, and behavior [13] [11].
The hypothalamic-pituitary-adrenal (HPA) axis serves as a key endocrine pathway in gut-brain communication. Stress activates the HPA axis, leading to cortisol release that increases intestinal permeability and disrupts microbial composition [2]. This creates a vicious cycle wherein stress-induced gut dysfunction promotes inflammation that further exacerbates neuroinflammation.
Relevance to Neurodegenerative Diseases
Dysregulation of vagus nerve and ENS function has been implicated in the pathogenesis of multiple neurodegenerative diseases through mechanisms involving neuroinflammation, protein misfolding, and impaired cellular homeostasis.
Table: Vagus Nerve and ENS Alterations in Major Neurodegenerative Diseases
| Disease | Vagus Nerve Involvement | ENS Pathology | Key Microbial Alterations |
|---|---|---|---|
| Alzheimer's Disease | Reduced vagal tone; VNS being investigated for cognitive benefits | Impaired gut barrier function; Increased permeability | Reduced microbial diversity; Depletion of SCFA-producers; Increased pro-inflammatory taxa |
| Parkinson's Disease | Potential route for α-synuclein propagation from gut to brain; Vagotomy reduces PD risk | Early α-synuclein pathology in ENS; GI symptoms often precede motor symptoms by years | Reduced SCFA production; Increased pro-inflammatory microbes; Altered bile acid metabolism |
| Multiple Sclerosis | VNS modulates neuroinflammation; Cholinergic anti-inflammatory pathway dysfunction | Enteric glial cell activation; Altered gut permeability | Specific bacteria (e.g., Akkermansia) correlate with disease activity; Reduced butyrate producers |
| Amyotrophic Lateral Sclerosis | Autonomic dysfunction including cardiovascular impairment | GI symptoms common; Altered gut motility | Distinct microbial signatures; Reduced butyrate-producing bacteria |
Alzheimer's Disease (AD)
The MGBA contributes to Alzheimer's pathogenesis through multiple interconnected mechanisms. Gut dysbiosis in AD patients is characterized by reduced microbial diversity, depletion of SCFA-producing genera, and enrichment of pro-inflammatory taxa [8]. These alterations promote systemic inflammation that can compromise blood-brain barrier integrity and trigger neuroinflammation [8]. Microbial metabolites, including SCFAs and amyloid proteins produced by certain bacteria, may directly influence amyloid-beta aggregation and tau phosphorylation in the brain [8] [13]. Vagal dysfunction in AD may impair the cholinergic anti-inflammatory pathway, potentially exacerbating neuroinflammation and cognitive decline [8].
Parkinson's Disease (PD)
The dual-hit hypothesis of PD pathogenesis proposes that environmental triggers in the gut initiate α-synuclein misfolding that subsequently spreads to the CNS via the vagus nerve [2]. This is supported by epidemiological studies showing that truncal vagotomy is associated with a reduced risk of developing PD [2]. Pathologically, α-synuclein aggregates appear in the ENS decades before motor symptoms manifest, with gastrointestinal dysfunction (particularly constipation) being a common premotor feature [2] [8]. The gut microbiota in PD patients exhibits reduced SCFA production and increased pro-inflammatory microbes, creating an environment that may promote α-synuclein misfolding and neuroinflammation [8].
Experimental Methodologies and Research Techniques
Vagus Nerve Investigation Methods
Vagus nerve stimulation (VNS) represents both a therapeutic approach and research tool. Invasive VNS involves surgical implantation of a pulse generator in the chest with electrodes attached to the left vagus nerve [15] [12]. Non-invasive VNS devices (e.g., transcutaneous VNS) deliver electrical stimulation through the skin, typically targeting the auricular branch of the vagus nerve in the ear [11] [14]. Research applications include evaluating the effects of VNS on cytokine profiles, neurotransmitter levels, and disease progression in animal models of neurodegeneration.
Vagal tone assessment typically employs heart rate variability (HRV) analysis as a non-invasive measure of parasympathetic activity, with low HRV indicating reduced vagal tone [11] [14]. This method has revealed impaired vagal function in various neurodegenerative conditions and can be used to monitor therapeutic responses.
Vagal afferent recording techniques involve direct electrophysiological measurement of vagal nerve activity in animal models, allowing researchers to characterize neural responses to specific gut-derived signals, including microbial metabolites and nutrients [2].
Enteric Nervous System Research Approaches
ENS imaging and visualization employs techniques including whole-mount immunohistochemistry to visualize enteric neurons and glia within the ganglionic plexuses [10]. Advanced live imaging using calcium indicators permits real-time monitoring of ENS activity in response to various stimuli.
Functional gut assays measure gastrointestinal transit time, mucosal secretion, and gut permeability to assess ENS functional integrity in health and disease states [13]. These assays are particularly valuable in animal models of neurodegeneration that exhibit gastrointestinal dysfunction.
Single-cell RNA sequencing of ENS tissues enables comprehensive characterization of enteric neuron diversity and identification of disease-specific alterations in gene expression profiles [13]. This approach has revealed ENS transcriptional changes in Parkinson's disease and other neurodegenerative conditions.
Figure 2: Experimental Workflow for Microbiota-Gut-Brain Axis Research. This diagram outlines integrated methodological approaches for investigating the role of vagus nerve and ENS in neurodegenerative diseases, spanning preclinical models, interventions, assessment methods, and analytical techniques.
Microbiota-Gut-Brain Axis Integrative Methods
Gnotobiotic models, particularly germ-free animals, permit investigation of microbiota influences on neural development and function by allowing controlled microbial colonization [2] [6]. These models have demonstrated the essential role of gut microbes in blood-brain barrier integrity, microglial maturation, and stress response regulation.
Microbiome profiling utilizes 16S rRNA sequencing and shotgun metagenomics to characterize microbial community structure in health and neurodegenerative diseases [2] [8]. Metabolomic analyses complement these approaches by quantifying microbial-derived metabolites in blood, feces, and brain tissue.
Proteomic analysis of neuronal development, as exemplified by quantitative mass spectrometry studies of rat hippocampal neurons, has identified extensive proteome remodeling during differentiation, with approximately 1,800 of 4,500 quantified proteins showing significant expression changes [14]. This approach can identify protein networks linking gut-derived signals to neuronal function and survival.
Table: Essential Research Reagents for Vagus Nerve and ENS Investigations
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Neural Tracing Agents | Cholera toxin B subunit (CTb), Fluoro-Gold, DiI | Vagal pathway mapping, ENS connectivity studies | Anterograde and retrograde neural tracing |
| Electrophysiology Tools | Multielectrode arrays, Patch clamp systems | Vagus nerve recording, ENS neuronal activity measurement | Direct measurement of neural electrical activity |
| Cell Type-Specific Markers | Anti-HuC/D (neurons), Anti-S100β (glial), Anti-ChAT (cholinergic) | ENS characterization, vagal motor neuron identification | Identification and quantification of specific neural populations |
| Cytokine Analysis Kits | ELISA, Luminex, ELISAspot | Inflammatory mediator quantification | Measurement of immune activation in MGBA |
| SCFA Analysis | GC-MS, LC-MS systems | Microbial metabolite quantification | Analysis of key microbial metabolites |
| Gut Barrier Integrity Assays | FITC-dextran, Ussing chambers | Intestinal permeability assessment | Evaluation of gut barrier function |
| Vagus Nerve Stimulators | Implantable VNS devices, transcutaneous tVNS | Therapeutic efficacy studies, mechanism investigation | Modulation of vagus nerve activity |
| Proteomic Platforms | LC-MS/MS with stable isotope labeling | Protein expression profiling during neuronal differentiation | Quantitative analysis of neural proteome dynamics |
The vagus nerve and enteric nervous system constitute critical neural communication pathways within the microbiota-gut-brain axis, with profound implications for neurodegenerative disease pathogenesis and treatment. Their integrated functions enable bidirectional information flow between the CNS and gastrointestinal tract through neural, immune, and endocrine signaling mechanisms. Dysregulation of these pathways contributes to neuroinflammation, protein misfolding, and neuronal dysfunction in conditions including Alzheimer's disease, Parkinson's disease, and multiple sclerosis.
Future research directions should prioritize the development of advanced neuromodulation approaches targeting vagus nerve pathways, personalized microbiota-based interventions tailored to individual microbial and immune profiles, and multi-omics integration strategies that combine genomic, proteomic, metabolomic, and connectomic data to elucidate complex gut-brain interactions. The progressive characterization of vagus nerve and ENS functions in neurodegenerative diseases promises to reveal novel therapeutic targets and biomarkers, ultimately advancing our ability to diagnose, monitor, and treat these devastating conditions through innovative gut-brain axis interventions.
The immune system plays a central and active role in the central nervous system (CNS), far beyond a mere reactive response to injury or disease. Immune signaling is now recognized as a core pathway in the pathogenesis of neurodegenerative diseases, with microglial activation serving as a critical nexus between peripheral inflammation and central nervous system pathology [16]. This neuroimmune crosstalk is profoundly influenced by the gut-brain axis, a bidirectional communication network in which gut-derived signals, including microbial metabolites and inflammatory mediators, can shape brain immune homeostasis and contribute to neurodegeneration [2] [6]. Key molecular patterns such as lipopolysaccharide (LPS), a component of the outer membrane of Gram-negative bacteria, can traverse physiological barriers, enter systemic circulation, and trigger innate immune responses in the brain, leading to sustained neuroinflammation [2] [17]. This review synthesizes the mechanisms by which cytokines, LPS, and other immune signals drive microglial dysfunction within the framework of the gut-immune-brain axis, providing a technical guide for researchers and drug development professionals.
Core Signaling Pathways in Neuroimmune Communication
The Gut-Immune-Brain Axis: A Bidirectional Highway
The gut–immune–brain axis represents a dynamic, bidirectional communication system involving intricate interactions between the gut microbiota, host immune responses, and the CNS [6]. This axis comprises several integrated components:
- Gut Microbiota: Trillions of commensal microorganisms in the gastrointestinal tract produce a vast array of metabolites and microbial-associated molecular patterns (MAMPs) that continuously shape host immunity [2] [6].
- Mucosal and Systemic Immunity: The gut-associated lymphoid tissue (GALT) serves as a primary interface for microbial-immune interactions. Immune cells activated in the gut can traffic systemically and influence the CNS [2].
- Neural Pathways: The vagus nerve provides a direct neural connection, transmitting signals from the gut lumen to the brainstem [2].
- Circulatory and Neuroendocrine Pathways: Gut-derived molecules, including cytokines, metabolites, and hormones, can reach the brain via the bloodstream and influence the hypothalamic-pituitary-adrenal (HPA) axis, which in turn modulates gut permeability and immune function [2].
The integrity of the intestinal and blood-brain barriers is crucial for regulating this communication; their disruption ("leaky gut") permits the translocation of pro-inflammatory molecules into systemic circulation and, potentially, the CNS [2] [6].
Key Receptors and Signaling Cascades
The innate immune response in neurodegeneration is primarily initiated by pattern recognition receptors (PRRs) that detect damage-associated molecular patterns (DAMPs) released by stressed or dying cells, and pathogen-associated molecular patterns (PAMPs) derived from microbes [17]. Below are the primary signaling cascades involved.
Diagram 1: Innate Immune Signaling Pathways in Microglial Activation. This diagram illustrates how LPS and DAMPs trigger signaling cascades via TLR4 and TREM2, leading to microglial activation and phenotypic transition.
Microglial Phenotypes: From Homeostasis to Neurodegeneration
Microglia, the resident innate immune cells of the CNS, are central players in neuroimmune signaling. They exist in dynamic states [18] [3]:
- Homeostatic Microglia: In a healthy brain, microglia exhibit a "ramified" morphology with extensive processes, continuously surveying the microenvironment. They express signature genes like
P2RY12,SALL1, andTMEM119, and are involved in synaptic pruning, neurotrophic factor release, and clearance of cellular debris [18] [16]. - Activated Microglia (DAM/MGnD): Upon encountering inflammatory signals like LPS or cytokines, microglia undergo a phenotypic transition. They retract processes, adopt an amoeboid morphology, and upregulate genes including
APOE,TREM2, andTYROBP[3]. This "disease-associated microglia" (DAM) or "microglial neurodegenerative phenotype" (MGnD) is characterized by altered phagocytic capacity and sustained release of pro-inflammatory cytokines, which can contribute to neuronal damage in neurodegenerative diseases [3].
Table 1: Key Cytokines in Neuroinflammatory Signaling
| Cytokine | Primary Cellular Source | Major Signaling Pathway | Putative Role in Neurodegeneration |
|---|---|---|---|
| TNF-α | Microglia, Astrocytes, Peripheral Macrophages | NF-κB, MAPK | Synaptic dysfunction, BBB disruption, Direct neurotoxicity at high concentrations [16] [17] |
| IL-1β | Activated Microglia, Infiltrating Myeloid Cells | NF-κB, NLRP3 Inflammasome | Exacerbation of Aβ and tau pathology, Sickness behavior, Pyroptosis [16] [17] |
| IL-6 | Microglia, Astrocytes, T cells | JAK-STAT | Promotion of Th17 cell differentiation, Link to adaptive immune response, Astrogliosis [16] |
| IL-10 | Regulatory T cells (Tregs), Microglial subset | JAK-STAT, Anti-inflammatory | Anti-inflammatory; resolution of inflammation; induced by SCFAs [2] [6] |
| IL-12/IL-23 | Antigen-Presenting Cells | JAK-STAT, T-bet/RORγt | Promotion of pro-inflammatory Th1/Th17 responses; implicated in MS and other neuroinflammatory conditions [2] |
Methodologies for Investigating Neuroimmune Signaling
In Vivo Modeling of Gut-Brain-Immune Interactions
Animal models, particularly mice, are indispensable for dissecting the causal mechanisms of the gut–immune–brain axis.
- Germ-Free (GF) Mice: Raised in sterile isolators without any microorganisms, these models allow researchers to study the fundamental role of microbiota in immune and brain development. GF mice exhibit significant immune deficits and altered microglial maturation and function, which can be reversed by microbial colonization or specific bacterial supplementation [18] [6].
- Gnotobiotic Mice: These are GF mice colonized with a defined set of known microorganisms. This allows for reductionist studies to determine the specific effects of a single bacterial species or consortium on immune and neurological outcomes [6].
- Transgenic Neurodegeneration Models: Mice genetically engineered to develop aspects of AD (e.g., 5xFAD), PD (e.g., α-synuclein overexpressors), or ALS are used to investigate how gut microbiota and immune activation influence disease progression. Studies often combine these models with antibiotic treatments, probiotic supplementation, or fecal microbiota transplantation (FMT) to modulate the gut microbiome [2] [3].
Experimental Workflow:
- Microbiome Manipulation: Administer antibiotics to deplete microbiota, or supplement with probiotics/prebiotics/FMT to alter microbial composition.
- Immune Challenge: Administer LPS systemically (intraperitoneally) or directly into the brain to model peripheral or central innate immune activation.
- Behavioral Phenotyping: Assess cognitive (e.g., Morris water maze, Y-maze) and motor function (e.g., rotarod, beam walking) to correlate immune changes with functional deficits.
- Tissue Collection and Analysis: Collect brain, gut, and blood samples for immunohistochemistry, flow cytometry, and molecular analysis (e.g., RNA-seq, qPCR) to quantify microglial activation, cytokine levels, and gene expression changes [2] [18] [3].
In Vitro and Ex Vivo Techniques
- Primary Microglial Cultures: Isolated from rodent brains, these cultures are used to study microglial responses to direct stimulation with LPS, cytokines, or Aβ in a controlled environment. They are crucial for delineating cell-autonomous signaling pathways [18] [3].
- BV-2 Cell Line: A commonly used immortalized murine microglial cell line for high-throughput screening of neuroimmune modulators.
- Human Induced Pluripotent Stem Cell (iPSC)-Derived Microglia: iPSCs from healthy donors or patients with neurodegenerative diseases can be differentiated into microglia-like cells. These models provide a human-genetic context to study disease mechanisms and are particularly valuable for translational research [16].
Diagram 2: Experimental Workflow for Neuroimmune Research. This flowchart outlines the key steps for in vivo and in vitro investigation of gut-brain-immune interactions.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Neuroimmune Signaling Studies
| Reagent / Tool | Category | Specific Example (Model Organism) | Key Function in Research |
|---|---|---|---|
| Lipopolysaccharide (LPS) | Immune Activator | E. coli O55:B5 or O111:B4 | A classic TLR4 agonist used to model peripheral and central innate immune activation and induce neuroinflammation in vivo and in vitro [2] [17]. |
| Cytokines (Recombinant) | Signaling Molecules | rmTNF-α, rmIL-1β, rmIL-6 (Mouse); rhTNF-α, rhIL-1β (Human) | Used to directly stimulate microglial or other CNS cells in culture to dissect specific cytokine receptor signaling pathways and functional outcomes [16]. |
| Cytokine Neutralizing Antibodies | Immunomodulators | Anti-mouse TNF-α, Anti-IL-1R | Used to block specific cytokine signaling pathways in vivo or in vitro to establish the causal role of a particular cytokine in a pathological process [16]. |
| TREM2 Modulating Antibodies | Immunomodulators | Anti-TREM2 (agonistic or antagonistic) | Tools to experimentally enhance or inhibit the TREM2 signaling pathway, crucial for studying microglial phagocytosis and the DAM phenotype [3]. |
| TLR4 Inhibitors | Small Molecule Inhibitor | TAK-242 (Resatorvid) | Selective inhibitor of TLR4 signaling; used to confirm the specific role of the TLR4 pathway in observed inflammatory responses [2] [17]. |
| Transgenic Mouse Models | In Vivo Model | 5xFAD (AD), TREM2 KO, TLR4 KO | Genetically engineered models to study the role of specific genes in the context of neurodegeneration and neuroinflammation [16] [3]. |
| Fluorescent Probes / Beads | Functional Assay | pHrodo-labeled Aβ or Zymosan, Latex Beads | Used in phagocytosis assays to quantify the engulfment capacity of microglia in culture or in tissue sections via flow cytometry or microscopy [3]. |
Concluding Perspectives and Therapeutic Implications
Understanding the intricate dynamics of immune and inflammatory signaling is paramount for developing novel therapeutic strategies for neurodegenerative diseases. The gut–immune–brain axis provides a mechanistic framework that links peripheral disturbances, such as gut dysbiosis and barrier breakdown, to central neuroinflammation and neuronal loss via cytokines, LPS, and microglial activation [2] [6] [3]. Future research should focus on leveraging multi-omics approaches to identify robust biomarkers of neuroimmune dysfunction and on developing targeted interventions, such as precision probiotics, small molecule modulators of TREM2 or TLR4, and strategies to fortify the intestinal and blood-brain barriers [2] [3]. By targeting the gut–immune–brain axis, the field holds promise for devising effective, personalized therapies to halt or slow the progression of neurodegenerative diseases.
The microbiota-gut-brain axis (MGBA) represents a revolutionary paradigm in neuroscience, outlining a complex, bidirectional communication network between the gastrointestinal tract and the central nervous system (CNS) [19] [3]. Emerging research underscores that this axis plays a significant role in the pathophysiology of neurodegenerative disorders, with gut microbiota dysbiosis being linked to the etiology and pathology of conditions such as Alzheimer's disease (AD) and Parkinson's disease (PD) [19] [20]. The genetic and metabolic potential of the gut microbiome is vast, estimated to contain nearly 150 times more genes than the human genome, which allows it to exert substantial influence on host physiology [3]. A pivotal mechanism of this communication is through microbial-derived metabolites, which can cross the intestinal barrier and influence the brain either directly or indirectly [19]. This whitepaper delves into the specific roles of three critical classes of these messenger molecules—short-chain fatty acids (SCFAs), bile acids (BAs), and tryptophan (TRP) derivatives—synthesizing current evidence on their mechanisms, quantitative profiles, and therapeutic potential within the context of neurodegenerative disease research.
Short-Chain Fatty Acids (SCFAs): Immunomodulatory Metabolites
Short-chain fatty acids (SCFAs), primarily acetate, propionate, and butyrate, are fatty acids with fewer than six carbon atoms, accounting for more than 95% of the total SCFAs composition in the gut [21]. They are produced predominantly in the cecum and colon through microbial fermentation of indigestible dietary fibers and resistant starch via glycolysis [20] [21]. The molar ratio of acetate, propionate, and butyrate in the gut typically ranges from 75:15:10 to 40:40:20, with an average of approximately 3:1:1 [21]. Their production is species-specific; for instance, acetate production is widespread, whereas key butyrate-producers include Faecalibacterium prausnitzii and Eubacterium rectale, and Akkermansia muciniphila is a major contributor to propionate production [21].
Key Signaling Mechanisms in the Brain
SCFAs mediate their effects through multiple mechanisms, crucially influencing brain function and neuroinflammation.
- Receptor-Dependent Signaling: SCFAs are potent agonists for the G-protein-coupled receptors (GPCRs) FFAR2 (GPR43) and FFAR3 (GPR41) [6] [21]. FFAR3 is highly expressed in the peripheral nervous system and the blood-brain barrier (BBB) [21]. Activation of these receptors on immune cells can suppress NF-κB signaling, thereby modulating inflammatory cytokine production [6].
- Epigenetic Regulation: Butyrate and propionate function as potent histone deacetylase (HDAC) inhibitors [6] [21]. This inhibition regulates gene expression, particularly promoting the differentiation and function of anti-inflammatory regulatory T cells (Tregs), which can have systemic immunomodulatory consequences [6].
- The "SCFAs-Microglia" Pathway: SCFAs can cross the BBB and are critical regulators of microglia, the resident immune cells of the CNS [21] [3]. They are essential for maintaining microglial homeostasis and modulating their response in neurodegenerative diseases. SCFAs help regulate the transition of microglia from a homeostatic state to a disease-associated microglial (DAM) phenotype, which is involved in clearing toxic protein aggregates like amyloid-β [3] [21].
Table 1: Physiological Concentrations of Key SCFAs
| SCFA | Typical Molar Ratio in Gut | Systemic Circulation Concentration | Reported Brain Concentration |
|---|---|---|---|
| Acetate | ~60% | 100 - 200 µM [21] | 17 - 19 pmol/mg (tissue); CSF: 0-171 mM [21] |
| Propionate | ~20% | 1 - 15 µM [21] | CSF: 0-6 mM [21] |
| Butyrate | ~20% | 1 - 15 µM [21] | CSF: 0-2.8 mM [21] |
Experimental Protocol: Measuring SCFAs and Microglial Response
Objective: To quantify SCFA concentrations in biological samples and assess their functional impact on microglial phenotype in vitro.
- Sample Collection and Preparation: Collect gut content (cecum/colon), blood plasma, or brain tissue. Homogenize samples and derivatize SCFAs to enhance volatility for analysis [21].
- SCFA Quantification: Analyze derivatized samples using Gas Chromatography-Mass Spectrometry (GC-MS) or Liquid Chromatography-Mass Spectrometry (LC-MS). Quantify acetate, propionate, and butyrate by comparing peak areas to standard curves [21].
- Microglial Cell Culture: Use immortalized microglial cell lines (e.g., BV-2) or primary microglia isolated from rodent brains. Culture cells in appropriate media.
- SCFA Treatment and Analysis: Treat cells with physiological concentrations of SCFAs (e.g., 100-500 µM acetate, 1-50 µM butyrate/propionate). Assess:
- Gene Expression: Use qPCR to analyze markers of microglial activation (e.g., Trem2, Apoe, Il1b, Tnf) and homeostatic markers (e.g., Tmem119, P2ry12) [3] [21].
- Phagocytosis Assay: Incubate cells with fluorescently-labeled latex beads or amyloid-β fragments. Quantify phagocytic capacity via flow cytometry or fluorescence microscopy [3].
- HDAC Activity Assay: Use a commercial fluorometric HDAC activity kit to confirm the inhibitory function of butyrate and propionate in cell lysates [6].
Diagram 1: SCFAs signaling pathway from gut to microglia.
Tryptophan Derivatives: Bridging Metabolism and Neuroinflammation
Metabolic Pathways
Tryptophan (TRP) is an essential amino acid whose metabolism occurs primarily via two pathways in the gut and brain [22]:
- Kynurenine Pathway (KP): Accounts for the metabolism of over 95% of free TRP. The initial step is catalyzed by enzymes indoleamine 2,3-dioxygenase (IDO1) or tryptophan-2,3-dioxygenase (TDO), producing kynurenine (KYN). IDO1 is highly induced by proinflammatory cytokines (IFN-γ, IL-6, TNF-α) [22]. The pathway subsequently branches to produce either neuroprotective kynurenic acid (KYNA) or neurotoxic quinolinic acid (QUINA) and 3-hydroxykynurenine (3-HK).
- Methoxyindole Pathway: A minor pathway that converts TRP to serotonin (5-HT), a key neurotransmitter, and subsequently to melatonin [22].
Neuroimmune Crosstalk in Neurodegeneration
The balance between neuroprotective and neurotoxic TRP metabolites is crucial in CNS homeostasis and is disrupted in neurodegeneration.
- Neuroprotection vs. Neurotoxicity: KYNA acts as an antagonist of glutamate receptors (NMDA, AMPA), providing neuroprotection [22]. In contrast, QUINA is an NMDA receptor agonist, causing excitotoxicity, and both QUINA and 3-HK promote oxidative stress and lipid peroxidation [22].
- Microglial and Astrocytic Control: The KP is compartmentalized in the brain. Microglia preferentially express the enzyme kynurenine 3-monooxygenase (KMO), shunting metabolism toward the neurotoxic QUINA, whereas astrocytes produce the neuroprotective KYNA [22]. Under chronic neuroinflammation, the microglial pathway dominates, creating a neurotoxic milieu.
- Impact on Blood-Brain Barrier: QUINA has been implicated in disrupting BBB integrity, potentially facilitating the entry of harmful substances into the brain [22].
Table 2: Key Tryptophan Metabolites and Their Neuroactive Properties
| Metabolite | Primary Producing Cell Type | Receptor/Target | Primary Effect in CNS |
|---|---|---|---|
| Kynurenic Acid (KYNA) | Astrocytes | NMDA, AMPA, kainate receptor antagonist [22] | Neuroprotective, anti-inflammatory [22] |
| Quinolinic Acid (QUINA) | Microglia, Macrophages | NMDA receptor agonist [22] | Excitotoxicity, pro-oxidant, pro-inflammatory [22] |
| 3-Hydroxykynurenine (3-HK) | Microglia, Macrophages | Promotes oxidative stress [22] | Neurotoxic, pro-oxidant [22] |
| Serotonin (5-HT) | Enteroendocrine cells, Neurons | Serotonin receptors (5-HTR) | Regulation of mood, appetite, sleep; gut-brain signaling [20] |
Experimental Protocol: Profiling the Kynurenine Pathway
Objective: To quantify TRP and its metabolites in serum and brain tissue and correlate levels with microglial activation markers.
- Sample Collection: Collect serum/plasma and brain tissue homogenates from animal models or post-mortem human samples.
- Metabolite Extraction: Deproteinize samples using methanol or acetonitrile. Centrifuge to collect supernatant.
- LC-MS/MS Analysis:
- Use reverse-phase liquid chromatography coupled with tandem mass spectrometry.
- Quantify levels of TRP, KYN, KYNA, 3-HK, and QUINA using stable isotope-labeled internal standards.
- Calculate the KYN/TRP ratio as a proxy for IDO/TDO enzyme activity, a marker of inflammatory status [22].
- Correlative Immunohistochemistry: On adjacent brain tissue sections, perform immunofluorescence staining for microglial marker IBA1 and the DAM-related protein TREM2. Correlate the spatial distribution and intensity of staining with regional concentrations of KP metabolites.
Diagram 2: Tryptophan metabolism branches.
Bile Acids: Metabolic and Signaling Regulators
Biosynthesis and Microbial Modification
Bile acids (BAs) are synthesized from cholesterol in the liver (primary BAs) and are subsequently metabolized by the gut microbiota into secondary BAs [3] [23]. This transformation involves deconjugation, dehydroxylation, and epimerization, significantly altering their chemical and signaling properties [3].
Signaling Mechanisms in the Gut-Brain Axis
BAs influence the CNS through multiple receptor-dependent and independent pathways:
- Receptor-Dependent Signaling: BAs are natural ligands for the nuclear receptor Farnesoid X Receptor (FXR) and the membrane receptor Takeda G-protein receptor 5 (TGR5) [23]. TGR5 activation on intestinal L-cells stimulates the release of glucagon-like peptide-1 (GLP-1), which can exert neuroprotective effects and reduce appetite via the gut-brain axis [23].
- Immune Modulation: BAs can modulate the function of the immune system, which in turn influences neural activity and neuroinflammation [23].
- Receptor-Independent Mechanisms: BAs can directly affect cell membranes and mitochondrial function, potentially influencing neuronal signaling [23].
While clinical evidence most strongly links plasma BA levels to mood disorders like depression and anxiety [23] [24], the mechanisms of BA signaling are also relevant to broader neuroinflammatory processes in neurodegeneration.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Microbial Metabolites in the Gut-Brain Axis
| Reagent / Assay | Primary Function / Target | Example Application in MGBA Research |
|---|---|---|
| GC-MS / LC-MS Kits | Quantification of metabolite concentrations | Measuring SCFA, tryptophan metabolite, and bile acid levels in serum, feces, and brain tissue [21] [22]. |
| HDAC Activity Assay | Fluorometric measurement of histone deacetylase activity | Confirming the epigenetic inhibitory function of butyrate and propionate in microglial cell cultures [6] [21]. |
| FFAR2/3 (GPR43/41) Agonists/Antagonists | Pharmacological modulation of SCFA receptors | Determining the specific contribution of receptor-mediated vs. intracellular (HDAC) SCFA signaling in microglial activation [21]. |
| IDO1 Inhibitor | Suppression of the kynurenine pathway | Investigating the role of inflammation-induced TRP metabolism in neurotoxicity models (e.g., in EAE or Aβ models) [22]. |
| TGR5 Agonist | Activation of the bile acid receptor TGR5 | Probing the neuroprotective effects of BA signaling via GLP-1 release in models of Parkinson's disease [23]. |
| Plexxikon PLX5622 | CSF1R inhibitor depletes microglia | Studying the necessity of microglia for mediating the effects of gut-derived metabolites in vivo [21]. |
| Anti-IBA1 / Anti-TREM2 Antibodies | Immunohistochemical labeling of microglia | Characterizing microglial morphology and activation state (homeostatic vs. DAM) in brain tissue sections [3]. |
| Fluorescent Aβ1-42 / Latex Beads | Substrates for phagocytosis assays | Quantifying the phagocytic capacity of microglia treated with SCFAs or other microbial metabolites in vitro [3]. |
The pathogenesis of neurodegenerative diseases (NDs) such as Alzheimer's disease (AD) and Parkinson's disease (PD) has traditionally been viewed through a neurocentric lens, focusing on protein misfolding and neuronal loss within the central nervous system (CNS). However, emerging evidence demonstrates that pathological changes frequently begin in the periphery years or even decades before classical neurological symptoms appear [25] [26]. The microbiota-gut-brain axis (MGBA) represents a critical bidirectional communication network that integrates neural, immune, endocrine, and metabolic signaling pathways between the gastrointestinal tract and the brain [2] [3].
Compelling clinical observations reveal that gastrointestinal symptoms often precede motor and cognitive manifestations in neurodegenerative diseases. For instance, chronic constipation can present in PD patients up to 20 years before diagnosis [2] [26]. Furthermore, early pathological hallmarks of NDs, including α-synuclein aggregates in PD and amyloid pathology in AD, have been identified in enteric nerves and enteroendocrine cells long before their detection in the CNS [25] [26]. These findings position gut dysbiosis—an imbalance in the gut microbial community—as a potential early contributor to neurodegenerative processes, offering promising avenues for pre-symptomatic diagnosis and intervention.
This technical review synthesizes current evidence on gut dysbiosis as an initiating factor in neurodegeneration, with a focus on microbial signatures in preclinical stages, mechanistic pathways along the MGBA, and translational applications for researchers and drug development professionals.
Microbial Signatures Across Neurodegenerative Diseases
Advancements in microbiome and metabolome profiling have enabled precise identification of microbial taxa and metabolic pathways consistently altered across neurodegenerative diseases. These microbial signatures demonstrate disease-specific patterns while sharing common features of disrupted gut homeostasis [27].
Table 1: Microbial Populations Altered in Preclinical Neurodegeneration
| Neurodegenerative Disease | Increased Taxa | Decreased Taxa | Key Metabolite Alterations |
|---|---|---|---|
| Parkinson's Disease (PD) | Enterobacteriaceae, Akkermansia, Catabacter, Oscillospira, Lactobacillus, Bifidobacterium, Christensenella spp., Methanobrevibacter [25] [27] | Prevotellaceae [25] | ↑ LPS, ↑ SCFAs (inconsistent), ↑ methane [25] |
| Alzheimer's Disease (AD) | Akkermansia [27] | Microbial diversity [2] | ↓ SCFAs, ↑ inflammatory mediators [2] [28] |
| Multiple Sclerosis (MS) | Akkermansia [27] | - | ↓ SCFAs [2] [27] |
| Amyotrophic Lateral Sclerosis (ALS) | - | - | Specific alterations identified but limited characterization [27] |
The table above summarizes consistent observations across multiple studies. In PD, the increase in Enterobacteriaceae—Gram-negative bacteria known to secrete pro-inflammatory lipopolysaccharides (LPS)—correlates positively with the severity of postural instability and gait difficulties [25]. Additionally, the rise in methane-producing bacteria such as Christensenella spp. and Methanobrevibacter may contribute to the constipation prevalent in prodromal PD by increasing intraluminal pressure and reducing peristaltic movements [25].
The reduction of Prevotellaceae in PD is particularly significant as this commensal family produces mucin and secretes neuroprotective short-chain fatty acids (SCFAs) through the fermentation of dietary fibers [25]. The consistent increase of Akkermansia across multiple NDs (PD, AD, and MS) suggests a potential role in disrupting intestinal barrier integrity, potentially facilitating the systemic translocation of microbial products [27].
From a metabolic perspective, the depletion of SCFAs—particularly butyrate, acetate, and propionate—represents a common feature across several NDs [27]. These microbial metabolites are essential for maintaining blood-brain barrier integrity, regulating microglial maturation and function, and exerting anti-inflammatory effects through the induction of regulatory T cells [2] [3].
Mechanisms of Gut-Brain Communication in Neurodegeneration
The MGBA comprises multiple integrated communication pathways that transmit signals from the gut to the brain. Under conditions of dysbiosis, these same pathways can propagate inflammation and pathology to the CNS through well-characterized mechanisms.
Neural Pathways
The vagus nerve serves as a direct neural conduit between the enteric nervous system and the CNS. Vagal afferents detect mechanical stretch, nutrients, and microbial molecules in the gut lumen, while efferent fibers modulate gastrointestinal function [2]. Microbial metabolites, including γ-aminobutyric acid (GABA), serotonin (5-HT), and histamine, can directly activate these vagal pathways [2].
Significantly, misfolded protein aggregates characteristic of NDs may exploit this neural connectivity. In PD, pathological α-synuclein aggregates are hypothesized to originate in the gut and propagate to the CNS in a prion-like fashion through vagal nerve fibers [25] [2]. Supporting this hypothesis, epidemiological studies demonstrate that truncal vagotomy is associated with a reduced risk of developing PD [2].
Immune and Inflammatory Pathways
The intestinal mucosal immune system constantly interacts with the gut microbiota, maintaining a delicate balance between tolerance and defense. Under conditions of dysbiosis and increased intestinal permeability ("leaky gut"), microbial-associated molecular patterns (MAMPs)—such as lipopolysaccharide (LPS) from Gram-negative bacteria—can translocate into systemic circulation [25] [2].
These microbial products activate pattern recognition receptors (e.g., Toll-like receptors) on innate immune cells, triggering NF-κB signaling and the production of pro-inflammatory cytokines including TNF-α, IL-1α, and IL-6 [25]. These inflammatory mediators can then cross the compromised blood-brain barrier or activate its endothelial cells, leading to microglial activation and subsequent neuroinflammation [25] [28].
Once activated, microglia transition from a homeostatic state to a disease-associated microglia (DAM) phenotype, characterized by downregulation of homeostatic markers (e.g., P2RY12, TMEM119) and upregulation of genes associated with neurodegeneration (e.g., APOE, TREM2) [3] [28]. This chronic neuroinflammatory environment promotes neuronal excitotoxicity, oxidative stress, and ultimately cell death [25].
Metabolic and Neuroendocrine Pathways
Gut microbes significantly influence host physiology through the production of bioactive metabolites that can enter systemic circulation and reach the CNS. Short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—are produced by bacterial fermentation of dietary fiber and play crucial roles in maintaining CNS homeostasis [29] [2]. SCFAs promote microglial maturation, strengthen the blood-brain barrier, and support the expansion of anti-inflammatory regulatory T cells [2] [3].
In neurodegenerative conditions, SCFA depletion is a consistent observation, potentially contributing to disease progression through impaired microglial function and increased neuroinflammation [27]. Additionally, gut microbes directly produce or influence the production of various neuroactive molecules, including serotonin (5-HT), dopamine, GABA, and bile acid metabolites, which can systemically influence brain function [2] [3].
The hypothalamic-pituitary-adrenal (HPA) axis further integrates metabolic and endocrine signaling along the MGBA. Psychological and metabolic stress activates the HPA axis, leading to cortisol release that can increase intestinal permeability, alter gut microbiota composition, and create a vicious cycle of gut-brain dysfunction [2].
Methodologies for Investigating the MGBA in Preclinical Models
Research into the MGBA employs specialized experimental models and methodologies designed to elucidate causal relationships and mechanistic pathways.
Key Experimental Models
Germ-Free (GF) Mice: These animals are born and maintained in sterile isolators, completely lacking any microorganisms. GF models enable researchers to study the fundamental role of microbiota in neurodevelopment and neuroinflammation without microbial influence [29]. Studies using GF mice have demonstrated the essential role of microbial signals in microglial maturation and function [29] [3].
Fecal Microbiota Transplantation (FMT): This approach involves transferring fecal material from human donors or diseased model organisms into recipient animals (typically germ-free or antibiotic-treated). FMT from PD patients to mice has been shown to transmit disease phenotypes, including motor deficits and increased neuroinflammation, providing direct evidence for the causal role of gut microbes in neurodegeneration [25].
Antibiotic-Induced Dysbiosis: Administration of non-absorbable antibiotics or broad-spectrum antibiotic cocktails allows researchers to create transient, controlled alterations in the gut microbiota. This method is particularly useful for studying the temporal aspects of microbiome influence on neurodegenerative processes [29].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for MGBA Investigations
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Gnotobiotic Models | Germ-free mice, Humanized microbiota mice | Establish causal relationships between specific microbes and phenotypes [29] |
| Fecal Transplant Materials | Donor fecal samples, Filter systems, Anaerobic chambers | Transfer microbial communities between donors and recipients [25] |
| Antibiotic Cocktails | Ampicillin, Neomycin, Metronidazole, Vancomycin | Deplete gut microbiota to study its functions [29] |
| Bacterial Culturomics | Anaerobic culture systems, Specific growth media | Isolate and expand individual bacterial strains [3] |
| Molecular Probes | FITC-dextran, LPS detectors, Cytokine assays | Measure gut permeability, microbial translocation, inflammation [25] [2] |
| Microglial Markers | IBA1, P2RY12, TMEM119, TREM2 antibodies | Identify and characterize microglial states [3] [28] |
Analytical Approaches
Multi-omics Integration: Combining metagenomics (microbial community analysis), metatranscriptomics (microbial gene expression), metabolomics (metabolite profiling), and proteomics provides a comprehensive view of MGBA interactions in neurodegeneration [2] [27].
Artificial Intelligence and Machine Learning: These computational approaches analyze complex, high-dimensional omics data to identify microbial signatures predictive of disease onset, progression, or treatment response, enabling personalized therapeutic approaches [27].
Diagnostic and Therapeutic Implications
The recognition of gut dysbiosis as an early event in neurodegeneration opens promising avenues for biomarker development and microbiota-targeted interventions.
Biomarker Potential
Microbial signatures identified through metagenomic sequencing of fecal samples offer non-invasive methods for early detection and risk stratification. Specific microbial ratios, such as the Enterobacteriaceae-to-Prevotellaceae ratio in PD, may serve as quantitative biomarkers for disease risk and progression [25] [27]. Additionally, circulating levels of microbial metabolites (SCFAs, LPS, and bile acid derivatives) in blood or CSF could provide accessible biomarkers for monitoring MGBA function in neurodegenerative processes [2] [27].
Microbiota-Targeted Interventions
Dietary Interventions: Restrictive diets and specific nutritional components represent powerful modulators of gut microbiota composition and function. The Mediterranean diet, ketogenic diets, and intermittent fasting regimens have shown promise in preclinical models for restoring microbial balance and reducing neurodegeneration [25] [30]. These dietary approaches primarily function by increasing SCFA-producing bacteria and reducing pro-inflammatory species [25].
Probiotics and Prebiotics: Targeted microbial supplementation with specific strains (e.g., Lactobacillus and Bifidobacterium) or administration of non-digestible fibers that selectively stimulate beneficial bacteria represent promising therapeutic avenues [2] [3]. Clinical trials have demonstrated that certain probiotic formulations can improve cognitive function in mild cognitive impairment and early AD [2].
Fecal Microbiota Transplantation: While still primarily experimental for neurodegenerative indications, FMT offers the potential to rapidly and comprehensively restore a healthy microbial ecosystem. Preclinical studies in PD models have shown that FMT from healthy donors can ameliorate motor deficits and reduce neuroinflammation [25] [2].
The accumulating evidence firmly establishes gut dysbiosis as an early event in the neurodegenerative cascade, preceding characteristic CNS pathology and clinical symptoms by years or even decades. The microbial signatures and MGBA communication pathways detailed in this review provide a mechanistic framework for understanding how peripheral disturbances can ultimately drive CNS degeneration.
For researchers and drug development professionals, these insights open transformative possibilities for early diagnostic biomarkers and novel therapeutic strategies that target the MGBA. The ongoing development of sophisticated experimental models, multi-omics integration, and artificial intelligence approaches will further elucidate the complex causal relationships between specific microbial constituents and neurodegenerative processes.
While challenges remain—particularly in establishing causality in human populations and accounting for significant inter-individual variability—targeting the MGBA represents a promising frontier for developing effective interventions that could prevent or slow the progression of currently incurable neurodegenerative disorders.
From Mechanism to Therapy: Microbiome-Targeting Interventions and Development
The microbiota-gut-brain axis (MGBA) represents a complex, bidirectional communication network that integrates gastrointestinal function with central nervous system homeostasis. Emerging research firmly implicates dysregulation of this axis in the pathogenesis of neurodegenerative diseases, including Alzheimer's disease (AD) and Parkinson's disease (PD) [2] [8]. Patients with these conditions frequently exhibit gut dysbiosis and gastrointestinal symptoms years before classic neurological symptoms appear, suggesting the gut may be a site of early pathology [2] [31]. This paradigm shift has positioned the gut as a promising therapeutic target for intervening in neurodegenerative processes.
Pharmacological strategies targeting the MGBA offer a novel approach to treating neurodegenerative diseases by modulating peripheral pathways that influence brain health. Two key approaches have emerged: gut-restricted small molecules that act locally within the gastrointestinal tract, and bile acid modulators that leverage systemic signaling pathways. This review provides an in-depth technical examination of these strategies, their mechanisms, and their application within neurodegeneration research.
Gut-Restricted Small Molecules
Design Principles and Strategies
Gut-restricted small-molecule drugs are designed to remain confined to the gastrointestinal tract upon oral dosing, thereby maximizing local concentration at the site of action while minimizing systemic exposure and potential off-target effects [32]. The primary design strategy involves engineering physicochemical properties that limit passive permeability across the intestinal epithelium, moving deliberately away from Lipinski's Rule of 5 guidelines that typically predict good oral bioavailability [32].
Table 1: Key Properties for Gut-Restricted Drug Design
| Property | Typical Oral Drug (Rule of 5) | Gut-Restricted Design | Rationale |
|---|---|---|---|
| Molecular Weight (MW) | ≤ 500 Da | Often higher | Reduces passive diffusion |
| Topological Polar Surface Area (TPSA) | < 140 Ų | Often > 140 Ų | Increases hydrophilicity, reduces membrane permeability |
| Hydrogen Bond Donors (HBD) | ≤ 5 | Often ≥ 8 | Increases hydrophilicity |
| Hydrogen Bond Acceptors (HBA) | ≤ 10 | Often ≥ 12 | Increases hydrophilicity |
| Calculated logP (clogP) | < 5 | Often low or negative | Increases hydrophilicity |
Key design strategies include:
- Highly Polar/Charged Compounds: Incorporation of carbohydrate motifs, peptides, or charged groups to increase hydrophilicity and reduce membrane permeability [32].
- Kinetophores: Structural units (e.g., short peptides, polyols, quaternary ammonium salts) tethered to pharmacologically active scaffolds to modulate pharmacokinetics without affecting target engagement [32].
An important design consideration is the location of the target. Drugs targeting apical surface proteins require minimal permeability, while those targeting intracellular gut proteins require a careful balance of sufficient permeability for cellular entry but limited absorption into systemic circulation [32].
Clinical and Preclinical Examples
Several gut-restricted compounds have advanced to clinical development, demonstrating the therapeutic potential of this approach:
- Acarbose (1): An oligosaccharide approved for type 2 diabetes that inhibits α-glucosidase and pancreatic α-amylase in the small intestine. Its high hydrophilicity (clogP = -9, HBD = 14, HBA = 19, TPSA = 321 Ų) results in very low bioavailability (<2%) [32].
- Sibofimloc (2): A carbohydrate-containing compound developed for Crohn's disease that targets FimH-expressing bacteria. Its two mannose units confer high polarity (clogP = 0.3, HBD = 8, HBA = 12, TPSA = 200 Ų), leading to limited systemic exposure [32].
- ZED1227 (3, TAK-227): A covalent tissue transglutaminase 2 (TG2) inhibitor for celiac disease with high TPSA (150 Ų) and low Caco-2 permeability (<10 nm/s) [32].
- Larazotide acetate (4, AT-1001): A tight junction regulator acting as a zonulin antagonist, with elevated hydrophilicity (clogP = -2.2, HBD = 11, HBA = 19, TPSA = 301 Ų) resulting in negligible systemic exposure [32].
- Ileal Bile Acid Transporter (IBAT/ASBT) Inhibitors: Including approved drugs like maralixibat (5), which incorporate charged kinetophores to achieve gut restriction [32].
Table 2: Clinical-Stage Gut-Restricted Small Molecules
| Compound | Target | Indication | Key Properties for Gut Restriction | Development Status |
|---|---|---|---|---|
| Acarbose | α-glucosidase, α-amylase | Type 2 Diabetes | High hydrophilicity (clogP=-9, TPSA=321Ų) | Approved (1995) |
| Sibofimloc | FimH | Crohn's Disease | Polar mannose units (TPSA=200Ų) | Clinical trials |
| ZED1227 | Tissue Transglutaminase 2 | Celiac Disease | High TPSA (150Ų), low permeability | Clinical trials |
| Larazotide acetate | Zonulin | Celiac Disease | High HBD/HBA count (11/19) | Phase III (discontinued) |
| Maralixibat | IBAT/ASBT | Alagille Syndrome | Charged kinetophore | Approved (2021) |
Experimental Protocols for Gut-Restricted Drug Development
In Vitro Permeability Assessment (Caco-2 Assay)
Purpose: To predict intestinal absorption and confirm gut-restricted properties. Protocol:
- Culture Caco-2 cells on semi-permeable membranes for 21-28 days to form differentiated monolayers.
- Validate monolayer integrity by measuring transepithelial electrical resistance (TEER) ≥ 300 Ω·cm².
- Add test compound to the apical compartment (representing intestinal lumen).
- Sample from the basolateral compartment at regular intervals (e.g., 30, 60, 120 minutes).
- Analyze samples using LC-MS/MS to determine compound concentration.
- Calculate apparent permeability (Papp): Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane area, and C₀ is the initial concentration. Interpretation: Compounds with Papp < 10 × 10⁻⁶ cm/s typically have low absorption and are suitable for gut-restricted approaches [32].
In Vivo Pharmacokinetic Validation
Purpose: To confirm limited systemic exposure and gut restriction in live animal models. Protocol:
- Administer test compound to rodents (rats or mice) via oral gavage.
- Collect blood samples at predetermined time points (e.g., 0.5, 1, 2, 4, 8, 24 hours post-dose).
- Euthanize animals at specified time points and collect gastrointestinal tissues (stomach, small intestine segments, colon) and contents.
- Homogenize tissues and extract compounds along with biological matrices.
- Analyze plasma and tissue samples using validated LC-MS/MS methods.
- Calculate pharmacokinetic parameters: Cmax, Tmax, AUC, and tissue-to-plasma ratios. Interpretation: Successful gut-restricted compounds show high concentrations in GI tissues but negligible plasma AUC, confirming minimal systemic exposure [32].
Bile Acid Modulators
Bile Acid Biochemistry and Signaling
Bile acids are hepatically synthesized cholesterol derivatives that function as both digestive surfactants and endocrine signaling molecules [33]. The primary bile acids synthesized in humans are cholic acid (CA) and chenodeoxycholic acid (CDCA), which undergo conjugation with glycine or taurine before biliary secretion [33].
Table 3: Major Bile Acids and Their Signaling Properties
| Bile Acid | Type | Receptor Affinities | Key Physiological Roles |
|---|---|---|---|
| Cholic Acid (CA) | Primary | FXR (weak), TGR5 (weak) | Emulsification, hydrophobicity regulator |
| Chenodeoxycholic Acid (CDCA) | Primary | FXR (potent) | Endogenous FXR agonist, regulates metabolism |
| Deoxycholic Acid (DCA) | Secondary | FXR, TGR5 (moderate) | Pro-apoptotic, promotes hepatic bile acid synthesis |
| Lithocholic Acid (LCA) | Secondary | PXR, VDR, TGR5 (potent) | Toxic at high concentrations, TGR5 activation |
| Ursodeoxycholic Acid (UDCA) | Secondary | FXR (antagonist), glucocorticoid receptor | Choleretic, hepatoprotective |
| Obeticholic Acid (OCA) | Synthetic | FXR (potent) | Therapeutic FXR agonist |
The gut microbiome plays a crucial role in transforming primary bile acids into secondary bile acids through deconjugation, dehydroxylation, and epimerization reactions [33]. These modified bile acids have different signaling properties and contribute to the complexity of bile acid-mediated physiology.
Bile acids signal through multiple receptors:
- Farnesoid X Receptor (FXR): A nuclear receptor that regulates bile acid synthesis, lipid metabolism, and inflammation [33] [34].
- Takeda G Protein-Coupled Receptor 5 (TGR5): A membrane receptor that stimulates energy expenditure and glucagon-like peptide-1 (GLP-1) secretion [33] [34].
- Other Receptors: Including pregnane X receptor (PXR), vitamin D receptor (VDR), and sphingosine-1-phosphate receptor 2 (S1PR2) [35] [33].
Bile Acids in the Gut-Brain Axis and Neurodegeneration
Bile acids function as critical signaling molecules in the gut-liver-brain axis, with demonstrated effects on brain function in both physiological and pathological conditions [35] [36]. Although most brain bile acids are taken up from the systemic circulation, the composition of the brain bile acid pool appears to be regulated by intestinal bacteria, suggesting bile acids may bridge communication between the gut microbiome and the brain [35].
Key mechanisms linking bile acid signaling to neurodegeneration include:
- Blood-Brain Barrier (BBB) Integrity: Bile acids can influence BBB function through receptor-mediated pathways, potentially affecting neuroinflammation [36].
- Neuroinflammation Modulation: TGR5 activation on immune cells can suppress neuroinflammatory responses, which are central to neurodegenerative processes [34].
- Ceramide Metabolism: Aberrant bile acid physiology may drive neurodegeneration through ceramide synthesis, a unifying pathogenic feature in cardiometabolic diseases that also has implications for brain health [33].
- Protein Misfolding: Certain bile acids, particularly tauroursodeoxycholic acid (TUDCA), have shown protective effects against protein misfolding and aggregation in cellular and animal models of neurodegeneration [35].
The therapeutic potential of bile acid modulators is exemplified by obeticholic acid (OCA), an FXR agonist that was developed for liver diseases but has implications for neurodegenerative conditions linked to metabolic dysfunction [33].
Experimental Protocols for Bile Acid Research
Bile Acid Profiling (LC-MS/MS)
Purpose: To comprehensively characterize bile acid composition in biological samples (serum, feces, brain tissue). Protocol:
- Extract bile acids from samples using methanol precipitation or solid-phase extraction.
- Derivatize samples to enhance ionization efficiency (optional for modern LC-MS systems).
- Separate bile acids using reverse-phase UHPLC with a C18 column (e.g., 2.1 × 100 mm, 1.7 μm).
- Perform mass spectrometric detection using multiple reaction monitoring (MRM) on a triple quadrupole instrument.
- Quantify individual bile acids using stable isotope-labeled internal standards (e.g., d₄-CA, d₄-CDCA).
- Analyze data to determine concentrations of individual bile acids and calculate total bile acid pool composition. Applications: Assessing gut microbiome function, monitoring therapy response, and correlating bile acid profiles with disease states [33] [34].
Receptor Activation Assays
Purpose: To characterize compound activity at bile acid receptors (FXR, TGR5). FXR Activation Assay:
- Transfert cells (e.g., HEK293) with an FXR-responsive luciferase reporter construct.
- Treat cells with test compounds for 24 hours.
- Measure luciferase activity as a surrogate for FXR activation.
- Calculate EC₅₀ values relative to reference agonist CDCA. TGR5 cAMP Assay:
- Use cells expressing human TGR5 (e.g., CHO-K1).
- Treat cells with test compounds in the presence of phosphodiesterase inhibitor.
- Measure intracellular cAMP accumulation using ELISA or HTRF.
- Calculate EC₅₀ values relative to reference agonist TLCA. Interpretation: These assays determine compound potency and efficacy for targeted bile acid receptor modulation [34].
Integrated Signaling Pathways
The gut-liver-brain axis represents a sophisticated communication network where signals from the gastrointestinal tract, including gut-restricted compounds and bile acid modulators, can influence brain function and potentially modify neurodegenerative processes [37]. The diagram below illustrates the key communication pathways in this system.
Gut-Liver-Brain Axis Signaling
This integrated view highlights how gut-restricted molecules and bile acid modulators can influence neurodegenerative processes through multiple parallel pathways, offering several potential intervention points for therapeutic development.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Gut-Brain Axis Pharmacology
| Category | Specific Reagents/Assays | Research Application | Key Providers |
|---|---|---|---|
| In Vitro Permeability | Caco-2 cell lines, MDCK cells, TEER measurement systems | Predicting intestinal absorption | ATCC, MilliporeSigma, Corning |
| Bile Acid Analysis | LC-MS/MS systems, bile acid standards, isotope-labeled internal standards | Quantifying bile acid profiles | Waters, Sciex, Agilent, Cambridge Isotopes |
| Receptor Assays | FXR reporter assays, TGR5 cAMP assays, recombinant receptors | Characterizing compound activity at targets | Indigo Biosciences, Cisbio, BPS Bioscience |
| Gut-Barrier Models | Transwell systems, intestinal organoids, gut-on-a-chip platforms | Modeling intestinal barrier function | Emulate, Stemcell Technologies, InSphero |
| Microbiome Tools | Bacterial culture collections, BSH activity assays, anaerobic chambers | Studying microbial metabolism of compounds | ATCC, DSMZ, Anaerobe Systems |
The strategic targeting of gut-restricted small molecules and bile acid modulators represents a promising frontier in the therapeutic landscape for neurodegenerative diseases. By focusing on the gut-brain axis, these approaches offer several advantages: reduced systemic exposure and side effects, access to a rich signaling network with broad influence on brain function, and the potential to intervene early in disease processes.
Future directions in this field should include:
- Development of more sophisticated gut-restricted compounds with enhanced tissue targeting and controlled release properties.
- Exploration of combination therapies that simultaneously modulate multiple pathways in the gut-brain axis.
- Advancement of personalized approaches based on individual microbiome and bile acid profiles.
- Improved preclinical models that better recapitulate human gut-brain communication, including humanized microbiome models and advanced gut-organoid systems.
As our understanding of the intricate relationships between gut physiology, bile acid signaling, and brain health continues to evolve, so too will opportunities for innovative pharmacological interventions that leverage these connections to combat neurodegenerative diseases.
The microbiota-gut-brain axis (MGBA) represents a transformative frontier in neurodegenerative disease research, offering novel therapeutic targets for intervention. This technical guide examines the strategic formulation of probiotic living biotherapeutics and the critical role of mechanism-driven strain selection. We synthesize current evidence on microbial metabolites, neuroimmune pathways, and emerging next-generation probiotics (NGPs) to provide a structured framework for researchers and drug development professionals. By integrating multi-omics approaches with rigorous experimental protocols, we outline a pathway for developing targeted microbial therapeutics that effectively modulate central nervous system function through gut-brain communication networks.
The microbiota-gut-brain axis (MGBA) constitutes a complex, bidirectional communication network linking gastrointestinal microbiota with the central nervous system (CNS) through neural, immune, endocrine, and metabolic pathways [2]. This axis has emerged as a critical regulator of brain health and a potential therapeutic target for neurodegenerative diseases including Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) [3].
Neurodegenerative pathologies are frequently preceded by gastrointestinal disturbances and microbiome alterations years before neurological symptoms manifest. For instance, chronic constipation can precede PD motor symptoms by up to 20 years, while distinct gut microbiota profiles have been identified in AD patients compared to healthy controls [2]. These observations suggest that MGBA perturbations may contribute to disease initiation and progression, positioning gut-targeted therapeutics as a promising intervention strategy.
Living biotherapeutic products (LBPs) represent an advanced category of pharmaceutical preparations containing live microorganisms developed for disease prevention or treatment [38]. Unlike traditional probiotics, LBPs are subject to rigorous regulatory frameworks requiring demonstration of safety, efficacy, and quality through controlled clinical trials. This review examines the scientific foundation for probiotic strain selection, formulation considerations, and mechanistic pathways relevant to neurodegenerative disease applications.
Mechanism-Driven Strain Selection for Neurodegenerative Diseases
Effective living biotherapeutic development requires careful strain selection based on demonstrated mechanisms of action relevant to neurodegenerative pathology. The following table summarizes key candidate organisms and their associated neuroprotective mechanisms.
Table 1: Mechanism-Based Selection of Probiotic Strains for Neurodegenerative Diseases
| Strain Category | Representative Strains | Proposed Mechanisms of Action | Relevance to Neurodegeneration |
|---|---|---|---|
| Traditional Probiotics | Lactobacillus spp., Bifidobacterium spp. | Gut barrier reinforcement, reduced intestinal inflammation, pathogen inhibition [39] | Improved gut integrity reduces systemic inflammation and neuroinflammation [40] |
| Next-Generation Probiotics | Faecalibacterium prausnitzii, Akkermansia muciniphila | Enhanced SCFA production (butyrate), anti-inflammatory effects, mucin restoration [41] | Butyrate enhances blood-brain barrier integrity, reduces neuroinflammation [2] |
| Immunomodulatory Strains | Bacteroides fragilis, Eubacterium hallii | Regulatory T-cell induction, cytokine modulation [41] | Mitigates chronic neuroinflammation, microglial activation [3] |
| Neurotransmitter-Modulating Strains | Lactobacillus spp., Bifidobacterium spp. | GABA, serotonin, dopamine production [3] | Influences neurochemical balance, neuronal signaling [2] |
Next-Generation Probiotics for Neurodegenerative Diseases
Next-generation probiotics (NGPs) represent a promising class of therapeutic microorganisms derived from human gut microbiota with specific health-promoting properties [41]. Unlike traditional probiotics primarily belonging to Lactobacillus and Bifidobacterium genera, NGPs include species such as Faecalibacterium prausnitzii, Akkermansia muciniphila, Eubacterium hallii, and selected Bacteroides species that exhibit enhanced physiological relevance to the human gut environment.
These NGPs demonstrate particular promise for neurodegenerative disease applications through multiple mechanisms:
- SCFA Production: Faecalibacterium prausnitzii and Eubacterium hallii are potent producers of short-chain fatty acids (SCFAs), particularly butyrate, which enhances blood-brain barrier integrity, suppresses neuroinflammation, and promotes regulatory T-cell differentiation [41].
- Mucin Reinforcement: Akkermansia muciniphila strengthens intestinal barrier function by promoting mucin production, reducing microbial translocation and systemic inflammation [41].
- Immunomodulation: Specific Bacteroides strains induce anti-inflammatory cytokine production and regulatory T-cell expansion, potentially dampening neuroinflammatory processes in conditions like AD and PD [41].
The development of NGPs as LBPs faces technical challenges including complex nutritional requirements, oxygen sensitivity, and sophisticated manufacturing processes. However, their physiological advantages position them as promising candidates for future neurodegenerative disease therapeutics.
Key Signaling Pathways in the Microbiota-Gut-Brain Axis
The MGBA comprises multiple integrated communication pathways that enable gut microbes to influence brain function. Understanding these mechanisms is essential for targeted therapeutic development.
Neural Pathways
The vagus nerve serves as a direct neural connection between the gut and brain, transmitting sensory information from the gastrointestinal tract to the brainstem and beyond [2]. Specific gut microbes can activate vagal afferents through neurotransmitter production or metabolite signaling. In PD pathology, misfolded α-synuclein aggregates may originate in the gut and propagate to the CNS via vagal transport, supported by evidence that truncal vagotomy reduces PD risk [2].
Immune and Inflammatory Pathways
Gut microbes profoundly shape systemic and central immune responses. Microbial-associated molecular patterns (MAMPs), including lipopolysaccharide (LPS), can translocate across compromised intestinal barriers into circulation, activating pattern recognition receptors such as Toll-like receptors (TLRs) on peripheral and central immune cells [2]. This triggering of innate immune signaling can lead to microglial activation and neuroinflammation. Additionally, gut microbiota influences the differentiation and trafficking of T-cell populations, with specific bacteria promoting either pro-inflammatory Th17 cells or anti-inflammatory regulatory T-cells that can subsequently infiltrate the CNS and modulate neuroinflammation [2].
Metabolic and Endocrine Pathways
Gut microbes produce numerous metabolites that systemically influence host physiology. Short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—produced through microbial fermentation of dietary fiber, exert profound anti-inflammatory effects, enhance blood-brain barrier integrity, and influence microglial maturation and function [2]. Additionally, gut bacteria produce or precursor numerous neurotransmitters and neuromodulators, including GABA, serotonin, dopamine, and histamine, which can influence central nervous system activity [3]. The gut microbiome also modulates the hypothalamic-pituitary-adrenal (HPA) axis, influencing stress response and cortisol release, which in turn affects gut permeability and microbial composition [2].
The following diagram illustrates the primary communication pathways comprising the microbiota-gut-brain axis:
Diagram 1: Key MGBA communication pathways in neurodegeneration.
Experimental Protocols for Mechanistic Validation
Rigorous experimental validation is essential for establishing causal relationships between probiotic interventions and neurological outcomes. The following section outlines key methodological approaches for investigating probiotic mechanisms in neurodegenerative disease models.
In Vitro Screening Protocols
Blood-Brain Barrier Integrity Assays:
- Objective: Evaluate the effect of microbial metabolites on BBB integrity.
- Methodology: Utilize transwell culture systems with human brain microvascular endothelial cells (HBMECs). Measure transendothelial electrical resistance (TEER) and paracellular permeability using fluorescent tracers (e.g., FITC-dextran) following treatment with probiotic-conditioned media or specific microbial metabolites (e.g., SCFAs) [2] [3].
- Endpoint Measurements: TEER values, permeability coefficients, and immunostaining of tight junction proteins (claudin-5, occludin, ZO-1).
Microglial Activation Assays:
- Objective: Assess the immunomodulatory potential of probiotic strains on microglial cells.
- Methodology: Culture murine BV-2 microglial cells or primary microglia and stimulate with LPS to induce inflammation. Co-treat with probiotic supernatants, SCFAs, or other microbial metabolites. Analyze pro-inflammatory (TNF-α, IL-1β, IL-6) and anti-inflammatory (IL-10, TGF-β) cytokine production via ELISA or multiplex immunoassays [3].
- Endpoint Measurements: Cytokine concentrations, morphological changes, and phagocytic activity.
In Vivo Validation in Animal Models
Germ-Free (GF) and Gnotobiotic Mouse Models:
- Objective: Establish causal relationships between specific microbial strains and neurological phenotypes.
- Methodology: Colonize GF mice with specific probiotic strains or defined microbial communities. Evaluate behavioral outcomes (cognitive function, motor performance), neuropathology (protein aggregation, neuroinflammation), and biochemical changes (neurotransmitter levels, metabolite profiles) [3].
- Endpoint Measurements: Behavioral test batteries (e.g., Morris water maze, open field), immunohistochemical analysis of brain sections, LC-MS/MS for metabolite quantification.
Fecal Microbiota Transplantation (FMT) Studies:
- Objective: Investigate the transferability of microbial-mediated neuroprotection.
- Methodology: Transplant fecal microbiota from human donors (healthy controls or patients) or probiotic-treated animals into recipient mice (often germ-free or antibiotic-treated). Assess transmission of phenotypic traits and correlate with microbial community analysis [2] [3].
- Endpoint Measurements: 16S rRNA sequencing of gut microbiota, behavioral assessments, inflammatory markers in brain and periphery.
The following workflow outlines a comprehensive approach for screening and validating probiotic strains for neurodegenerative disease applications:
Diagram 2: Probiotic strain screening and validation workflow.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Advancing living biotherapeutic development for neurodegenerative diseases requires specialized research tools and platforms. The following table summarizes key reagents and methodologies essential for investigating microbiome-brain interactions.
Table 2: Essential Research Reagents and Platforms for MGBA Investigations
| Category | Specific Reagents/Platforms | Research Application | Key Considerations |
|---|---|---|---|
| Cell Culture Models | Human brain microvascular endothelial cells (HBMECs), BV-2 microglial cells, primary microglia, Caco-2 intestinal epithelial cells | Barrier integrity assessment, immune cell activation studies, transport mechanisms | Primary cells offer physiological relevance; immortalized lines provide reproducibility [3] |
| Animal Models | Germ-free mice, gnotobiotic models, transgenic neurodegenerative models (APP/PS1, SNCA, SOD1) | Causal relationship establishment, pathway mechanistic studies, therapeutic efficacy evaluation | Germ-free models essential for establishing causality; transgenic models recapitulate disease pathology [2] [3] |
| Analytical Platforms | 16S rRNA sequencing, shotgun metagenomics, LC-MS/MS metabolomics, multiplex immunoassays | Microbial community analysis, functional potential assessment, metabolite quantification, inflammatory profiling | Multi-omics integration provides comprehensive mechanistic insights [2] [41] |
| Specialized Reagents | TEER measurement systems, FITC-dextran permeability tracers, tight junction antibodies, cytokine ELISA kits | Barrier function quantification, junctional protein expression, inflammatory mediator measurement | Standardized protocols essential for cross-study comparisons [3] |
Regulatory Considerations for Live Biotherapeutic Products
The regulatory landscape for LBPs differs significantly from that of traditional probiotics. According to the FDA and European Medicines Agency (EMA), LBPs are classified as biological medicinal products when intended for disease treatment or prevention [38]. This classification necessitates compliance with stringent regulatory requirements:
- Quality Requirements: The European Pharmacopoeia monograph on LBPs specifies quality control measures including strain identification, purity testing, viability quantification, and stability assessment [38].
- Safety Assessment: Comprehensive evaluation including toxicological studies, antibiotic resistance profiling, and assessment of potential off-target effects [40] [38].
- Efficacy Demonstration: Well-controlled clinical trials with clinically relevant endpoints specific to the target neurodegenerative indication [38].
The regulatory pathway requires demonstration of a positive benefit-risk ratio through rigorous nonclinical and clinical development programs following ICH guidelines [38]. For neurodegenerative diseases, this typically necessitates large-scale, multicenter trials with validated biomarkers and clinical outcome assessments.
The development of mechanism-driven living biotherapeutics for neurodegenerative diseases represents a promising frontier at the intersection of microbiology and neuroscience. Strategic strain selection based on understanding MGBA signaling pathways enables targeted intervention in disease-relevant mechanisms. The transition from traditional probiotics to defined NGPs and LBPs offers enhanced therapeutic precision but necessitates sophisticated manufacturing approaches and rigorous regulatory evaluation.
Future progress will depend on overcoming key challenges, including the standardization of microbial cultivation methods for oxygen-sensitive commensals, establishment of predictive biomarkers for patient stratification, and implementation of robust clinical trial designs with meaningful neurodegenerative-specific endpoints. As our understanding of gut-brain communication deepens, living biotherapeutics offer transformative potential for modulating neurodegenerative processes through novel mechanism-based approaches.
The microbiota-gut-brain axis (MGBA) represents a complex, bidirectional communication network linking the gastrointestinal tract with the central nervous system [2]. Growing evidence indicates that dietary patterns significantly modulate this axis, influencing neuroinflammation, protein aggregation, and neuronal homeostasis in neurodegenerative diseases [42] [2]. This technical review examines the mechanisms by which fiber-rich, Mediterranean, and high-fat diets impact MGBA function, with implications for Alzheimer's disease (AD), Parkinson's disease (PD), and related disorders. We synthesize current evidence from mechanistic studies and clinical interventions to provide researchers and drug development professionals with a foundation for designing microbiome-targeted therapeutic strategies.
Core Mechanisms of Diet-MGBA Interactions
Dietary components influence MGBA signaling through multiple interconnected pathways, including microbial metabolite production, immune modulation, and barrier integrity maintenance.
Key Signaling Pathways and Microbial Metabolites
Table 1: Primary Microbial Metabolites and Their Neuroactive Effects
| Metabolite | Primary Producing Genera | Receptor Targets | Neurobiological Effects |
|---|---|---|---|
| Butyrate (SCFA) | Faecalibacterium, Roseburia, Lachnospira, Anaerostipes [43] | FFAR2/3, HDAC inhibitor [43] | Enhances BBB integrity [42], inhibits neuroinflammation [43], colonocyte energy source [43] |
| Propionate (SCFA) | Akkermansia, Bacteroides, Dialister [43] | FFAR2/3, HDAC inhibitor [43] | Reduces CD4+ T cell responses [43], anti-inflammatory [43], gluconeogenesis substrate [43] |
| Acetate (SCFA) | Widespread production [43] | FFAR2/3 [43] | Energy metabolism [43], substrate for butyrate production [43], stimulates mucin production [43] |
| LPS (Endotoxin) | Gram-negative bacteria [44] | TLR4/NF-κB [2] [44] | Activates microglia [2], induces neuroinflammation [44], promotes Aβ aggregation [44] |
The gut microbiome ferments dietary components, producing metabolites that systematically influence brain function. Short-chain fatty acids (SCFAs), including butyrate, propionate, and acetate, are key signaling molecules derived from fermentable fibers [43]. These metabolites enhance barrier function by stimulating tight junction assembly and mucus production, while simultaneously exerting anti-inflammatory effects through histone deacetylase (HDAC) inhibition and regulatory T-cell differentiation [43]. Butyrate specifically provides energy for colonocytes and strengthens the blood-brain barrier (BBB) [42] [43].
Conversely, high-fat diets promote the growth of pro-inflammatory taxa that produce endotoxins like lipopolysaccharide (LPS) [45] [44]. LPS translocation across compromised gut and BBB interfaces activates TLR4/NF-κB signaling in microglia, triggering chronic neuroinflammation [2] [44]. This inflammatory environment promotes amyloid-beta (Aβ) deposition and contributes to neurodegenerative pathology [44].
Figure 1: Dietary Modulation of the Microbiota-Gut-Brain Axis. Fiber-rich and Mediterranean diets promote SCFA-producing bacteria that enhance barrier function and neuroprotection. High-fat diets promote LPS-producing bacteria and dysbiosis, leading to barrier disruption and neurodegeneration.
Barrier Integrity and Immune Signaling
Dietary patterns significantly influence intestinal barrier integrity and systemic immune responses. The vitamin A/fiber synergy demonstrates this relationship: all-trans retinoic acid (ATRA), the bioactive form of vitamin A, upregulates tight junction proteins (ZO-1, claudin-1, occludin) that maintain gut barrier function [44]. Simultaneously, SCFAs from fiber fermentation enhance ATRA bioavailability by upregulating aldehyde dehydrogenase gene expression [44]. This synergistic interaction prevents translocation of bacterial endotoxins like LPS into systemic circulation.
Once LPS enters circulation, it can cross the BBB via lipoprotein-mediated transport, triggering microglial activation and neuroinflammation [44]. LPS-activated microglia upregulate CYP26A1, an enzyme that degrades ATRA, creating a vicious cycle of increased neuroinflammation and reduced neuroprotection [44]. This pathway establishes a direct mechanistic link between gut barrier function and neurodegenerative processes.
Dietary Intervention Profiles
Fiber-Rich and Mediterranean Diets
Table 2: Neuroprotective Dietary Interventions and Evidence
| Intervention | Key Components | Microbial Shifts | Biomarker & Cognitive Outcomes |
|---|---|---|---|
| High-Fiber Diet | Fermentable polysaccharides (FOS, GOS, inulin, resistant starch) [43] | ↑ Faecalibacterium, Roseburia, Eubacterium [43]; ↑ SCFA production [43] | Reduced neuroinflammation [43]; Improved cognitive flexibility [46] |
| Mediterranean Diet | Olive oil, fish, vegetables, fruits, whole grains, limited red meat [46] | ↑ Candidatus Saccharimonas; ↓ Bifidobacterium (associated with poor memory) [46] | Better memory and learning [46]; Lower LDL cholesterol [46]; ↓ Aβ deposition [47] |
| MIND Diet | Green leafy vegetables, berries, nuts, whole grains [47] | Enriches SCFA producers [43] | Lower amyloid-beta & tau [47]; Reduced neuroinflammation (CRP, IL-6, TNF-α) [47] |
| Green-Mediterranean Diet | High-polyphenol foods with caloric restriction [43] | ↑ Faecalibacterium, Eubacterium, Roseburia, Blautia [43] | Increased propionic acid; Enhanced anti-inflammatory effects [43] |
Fiber-rich diets provide fermentable substrates for SCFA-producing bacteria, with specific structural differences influencing microbial community composition. Butyrate-producing genera from the Lachnospiraceae and Ruminococcaceae families, including Faecalibacterium, Roseburia, and Lachnospira, are particularly enriched by diverse fiber intake [43]. These bacteria demonstrate functional redundancy in SCFA production, with cross-feeding relationships where acetate produced by some bacteria enhances butyrate production by others [43].
The Mediterranean diet pattern demonstrates significant neuroprotective effects in both animal models and human studies. A Tulane University study found rats fed a Mediterranean-style diet for 14 weeks developed distinct gut microbiota patterns correlated with improved performance in maze tests of memory and learning [46]. These animals showed increased levels of beneficial bacteria like Candidatus Saccharimonas and decreased levels of bacteria associated with poorer memory function [46].
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) specifically targets brain health, with a 5-year prospective cohort study demonstrating significantly better cognitive scores (p < 0.0001), lower amyloid-beta and tau levels, and reduced inflammatory markers (CRP, IL-6, TNF-α) in high adherers [47]. The MIND diet showed marginally superior cognitive protection compared to the traditional Mediterranean diet, potentially due to its specific emphasis on berry fruits and leafy greens rich in polyphenols [47].
High-Fat Diets
High-fat diets (HFD) consistently induce gut dysbiosis characterized by reduced microbial diversity, increased Firmicutes to Bacteroidetes ratio, and depletion of beneficial SCFA-producing bacteria including Akkermansia, Faecalibacterium, and Oscillibacter [45]. These microbial shifts contribute to impaired gut barrier function, allowing translocation of bacterial endotoxins like LPS into circulation [45] [44].
HFD consumption activates neuroinflammatory pathways through multiple mechanisms. Circulating LPS triggers TLR4/NF-κB signaling in microglia, promoting chronic neuroinflammation [48]. Additionally, HFD-induced oxidative stress and impaired synaptic plasticity particularly affect hippocampal and hypothalamic function, potentially accelerating neurodegenerative processes [48]. The type of dietary fat modulates these effects, with saturated fats demonstrating more detrimental impacts than unsaturated varieties [48].
In Parkinson's disease models, the combination of HFD with low-dose rotenone (a pesticide) exacerbated gut-brain axis disruption, including increased intestinal inflammation, gut dysbiosis, and enhanced α-synuclein pathology [49]. This synergy between environmental toxins and diet-induced dysbiosis highlights the multifactorial nature of neurodegenerative pathogenesis.
Disease-Specific Mechanisms and Applications
Table 3: Diet-MGBA Interactions in Neurodegenerative Diseases
| Disease | MGBA Alterations | Key Dietary Influences | Potential Intervention Approaches |
|---|---|---|---|
| Alzheimer's Disease | LPS in hippocampus [44]; Reduced SCFA producers [42] | Vitamin A/fiber synergy enhances barrier function [44]; HFD increases neuroinflammation [48] | MIND/Mediterranean diets lower Aβ/tau [47]; SCFA supplementation [42] |
| Parkinson's Disease | α-synuclein gut-origin hypothesis [2]; Gut dysbiosis precedes motor symptoms [2] | HFD + rotenone exacerbates pathology [49]; Fiber modulates neuroinflammation [43] | High-fiber diets reduce neuroinflammation [43]; Vagal nerve activation [2] |
| Multiple Sclerosis | Pro-inflammatory Th17 cells induced by specific gut microbes [2] | High-fiber diet expands Tregs via SCFAs [2] | SCFA supplementation reduces CNS inflammation in EAE models [2] |
| Amyotrophic Lateral Sclerosis | Shared microbial/immunological mechanisms across spectrum [42] | Reduced microbial diversity [42] | Probiotics, FMT [42] |
Alzheimer's Disease
The endotoxin hypothesis of AD proposes that gut-derived LPS translocates to the brain, promoting neuroinflammation and Aβ aggregation [44]. Post-mortem analyses have detected bacterial LPS in the hippocampus and Aβ plaques of AD patients [44]. The vitamin A and fiber synergy represents a promising dietary approach to counter this process, as ATRA enhances intestinal barrier integrity while SCFAs from fiber fermentation support ATRA bioavailability, reducing systemic LPS exposure [44].
Long-term adherence to Mediterranean and MIND diets correlates with favorable AD biomarker profiles, including reduced amyloid-beta and tau pathology [47]. A 5-year prospective cohort study demonstrated that higher dietary adherence was associated with significantly lower levels of neurofilament light chain (NfL), a marker of neuronal injury, and reduced inflammatory markers including CRP, IL-6, and TNF-α [47].
Parkinson's Disease
The gut-first hypothesis of PD suggests that α-synuclein pathology may originate in the enteric nervous system before spreading to the brain via the vagus nerve [2]. This is supported by epidemiological evidence showing that truncal vagotomy is associated with reduced PD risk [2]. Dietary interventions significantly influence this gut-brain connection, with high-fiber diets enriching SCFA producers that reduce neuroinflammation in PD models [43].
The combination of HFD with rotenone exposure exacerbates PD-like pathology through gut-brain axis disruption, demonstrating synergistic effects on intestinal inflammation, gut dysbiosis, and motor deficits [49]. This highlights how dietary patterns may modulate susceptibility to environmental toxins in neurodegenerative pathogenesis.
Experimental Approaches and Methodologies
Animal Models and Dietary Interventions
Rodent studies employing controlled dietary regimens provide fundamental insights into MGBA mechanisms. Typical protocols involve:
- Diet Formulation: High-fat diets (HFD) typically contain 60% kcal from fat, while normal diets (ND) contain 10% kcal from fat [45]. Mediterranean diets for rodents incorporate olive oil, fish oils, and fiber-rich components mirroring human consumption patterns [46].
- Intervention Duration: Studies typically range from 8-16 weeks, with longer interventions assessing chronic effects [45] [49].
- Microbiome Analysis: Fecal sample collection followed by 16S rRNA gene amplicon sequencing (V4-V5 regions) using Illumina MiSeq platforms [45]. Data processed through QIIME and Calypso software for operational taxonomic unit (OTU) analysis [45].
- Cognitive Assessment: Morris water maze for spatial memory [46], Y-maze for spontaneous alternation [49], and rotarod tests for motor function [49].
Human Clinical Trials
Human studies employ distinct methodological approaches:
- Dietary Assessment: Validated tools including Mediterranean Diet Adherence Screener (MEDAS), MIND Diet Score, food frequency questionnaires (FFQ), and 24-hour dietary recalls [47].
- Cognitive Testing: Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) for comprehensive cognitive evaluation [47].
- Biomarker Analysis: Blood and CSF measurements of amyloid-beta (Aβ42/40), tau, neurofilament light chain (NfL), and inflammatory markers (CRP, IL-6, TNF-α) using ELISA kits [47].
- Microbiome Metrics: 16S rRNA sequencing and metabolomic analyses of fecal SCFAs (butyrate, propionate, acetate) and branched-chain fatty acids (BCFAs) [43] [45].
Figure 2: Experimental Workflow for Diet-MGBA Research. Comprehensive approach integrating controlled dietary interventions with multi-omics data collection and computational modeling to elucidate mechanisms linking nutrition to brain health.
The Scientist's Toolkit
Table 4: Essential Research Reagents and Platforms
| Category | Specific Tools | Application Notes | Key Functions |
|---|---|---|---|
| DNA Isolation & Sequencing | Qiagen QIAamp DNA Stool Mini Kit [45]; Illumina MiSeq [45]; 16S rRNA V4-V5 primers [45] | 200mg fecal samples; minimum 5000 sequences/sample [45] | Microbial community profiling; α-diversity (Chao, Shannon) [45] |
| Bioinformatic Analysis | QIIME [45]; Calypso v8.84 [45]; GreenGenes database (v13.8) [45] | Open-reference OTU picking at 96% similarity [45] | Taxonomic classification; Differential abundance testing |
| Cognitive Testing | Morris Water Maze [46]; Y-Maze [49]; Rotarod [49] | Pre- and post-intervention assessment; Video tracking | Spatial memory; Working memory; Motor coordination |
| Biomarker Assays | ELISA Kits: Aβ42/40 (Thermo Fisher KHB3481) [47]; Tau (R&D Systems DTA00) [47]; NfL (Peninsula 42-1001) [47] | Blood and CSF samples; Sensitivity: <10pg/mL for Aβ [47] | Quantification of neurodegenerative pathology |
| Diet Formulation | Research Diets: D12492 (HFD) [45]; D12450J (ND) [45]; Custom Mediterranean Diet [46] | 60% kcal fat (HFD) vs 10% kcal fat (ND) [45] | Controlled dietary interventions |
Dietary interventions represent promising non-pharmacological approaches for modulating the microbiota-gut-brain axis in neurodegenerative diseases. The evidence reviewed demonstrates that fiber-rich and Mediterranean-style diets consistently promote beneficial microbial taxa, enhance barrier integrity, and reduce neuroinflammation through SCFA-mediated mechanisms. Conversely, high-fat diets induce dysbiosis, compromise barrier function, and promote neuroinflammatory pathways that may accelerate neurodegenerative processes.
Future research should focus on personalized nutrition approaches accounting for genetic factors like APOE-ε4 status, which may influence individual responses to dietary interventions [47]. Additionally, multi-omics integration combining metagenomics, metabolomics, and proteomics will help elucidate precise mechanisms linking specific dietary components to brain health outcomes [2]. The development of robust biomarkers for monitoring MGBA function in response to dietary modulation will be crucial for translating these findings into targeted therapeutic strategies for neurodegenerative disease prevention and management.
The human gastrointestinal tract is populated by a complex community of trillions of microorganisms, collectively known as the gut microbiome, which encodes approximately 150 times more genes than the human genome [3]. This microbiome is not a passive resident; it actively influences host physiology through immune, metabolic, and neural pathways. The microbiota-gut-brain axis (MGBA) represents the bidirectional communication network that links the gut's resident microbiota with the central nervous system (CNS) [2] [3]. Perturbations to the gut microbial ecosystem (dysbiosis) have been implicated in the pathogenesis of a range of neurodegenerative diseases (NDDs), including Alzheimer's disease (AD), Parkinson's disease (PD), multiple sclerosis (MS), and amyotrophic lateral sclerosis (ALS) [2] [9]. Patients with NDDs frequently exhibit gastrointestinal disturbances and distinct gut microbiota profiles years before classic neurological symptoms emerge [2].
Fecal Microbiota Transplantation (FMT) is a therapeutic intervention designed to correct dysbiosis by transferring fecal matter from a healthy, pre-screened donor into the gastrointestinal tract of a recipient [50]. While its most established application is for recurrent Clostridioides difficile infection (rCDI), its potential to modulate the MGBA has spurred investigative interest in neurology [51] [50]. This technical guide details the protocols, outcomes, and mechanistic insights of FMT as a tool for microbial ecosystem engineering, framed within the context of neurodegenerative disease research.
FMT Mechanisms of Action: Implications for Neurodegeneration
The therapeutic effect of FMT in rCDI is primarily attributed to the restoration of a healthy, diverse gut microbiota, which re-establishes colonization resistance against pathogens [51] [50]. This restoration corrects metabolic dysregulations, such as imbalances in bile acid metabolism and the production of short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate [50] [21]. In the context of the MGBA and NDDs, these and other mechanisms are of paramount importance for modulating brain health.
The diagram below illustrates the core pathways through which the gut microbiota, and by extension FMT, communicates with the brain.
The primary mechanistic pathways connecting the gut ecosystem to brain pathology include:
Immunomodulation: Gut microbes profoundly shape the host immune system. A disrupted microbiome can lead to systemic inflammation. Microbial-associated molecular patterns (e.g., LPS) can breach a compromised intestinal barrier, enter circulation, and activate microglia—the brain's resident immune cells—via Toll-like receptors (e.g., TLR4), triggering chronic neuroinflammation [2] [3]. FMT can restore a healthy microbiome, which promotes anti-inflammatory regulatory T-cells (Tregs) via SCFAs, thereby suppressing CNS inflammation [2].
Microbial Metabolites: SCFAs are a critical link in the MGBA. Butyrate, propionate, and acetate, produced by bacterial fermentation of dietary fiber, have systemic anti-inflammatory effects, maintain the integrity of the blood-brain barrier (BBB), and directly influence microglial homeostasis and function [21]. FMT from healthy donors introduces SCFA-producing bacteria, thereby increasing the production of these beneficial metabolites [21].
Neural Pathway: The vagus nerve is a direct neural highway connecting the gut and the brainstem. Gut microbes can produce neurotransmitters (e.g., GABA, serotonin) or stimulate their production, which can activate vagal afferents [2] [3]. Notably, in PD, misfolded α-synuclein is hypothesized to originate in the gut and spread to the brain in a prion-like fashion via the vagus nerve [2].
Technical Protocols for FMT Workflow
The execution of FMT involves a multi-stage process, from stringent donor screening to the selection of an appropriate administration route. Standardization is critical for both safety and efficacy, particularly in a research context.
Donor Screening and Material Preparation
Donor selection is the first and most critical safety step. Potential donors are excluded based on a comprehensive set of criteria, and their stool and blood are rigorously tested for pathogens [50].
Table 1: Standard Donor Screening Criteria for FMT
| Category | Exclusion Criteria |
|---|---|
| Medical History | Recent antibiotics (typically within 3 months), GI disorders (IBD, IBS, cancer), Metabolic syndrome, Neurological or psychiatric disorders, Autoimmune diseases, Atopic conditions, Malignancy [50] [52] |
| Lifestyle & Travel | High-risk sexual behavior, Recent incarceration, Tattoos/piercings within 6 months, Travel to regions with endemic diarrheal pathogens [50] |
| Physical Examination | Signs of infection or metabolic disorder [50] |
| Serological & Stool Tests | HIV, Hepatitis A/B/C, H. pylori, C. difficile, Other enteric pathogens (Salmonella, Shigella, Campylobacter), Multi-drug resistant organisms, Extended-spectrum beta-lactamase producers [50] |
Following donor qualification, fecal material is processed. The stool is mixed with a preservative-free saline or cryoprotectant solution, homogenized, and filtered to remove particulate matter. The final product can be used fresh or frozen at -80°C. Meta-analyses have shown no clinically significant difference in efficacy between fresh and frozen products for rCDI [50].
Administration Routes and Protocols
The choice of administration route depends on clinical context, product formulation, and patient factors. The following workflow outlines the standard procedural steps for the most common routes.
Table 2: Comparison of FMT Administration Routes
| Route | Procedure Details | Advantages | Disadvantages | Common Use |
|---|---|---|---|---|
| Colonoscopy | Infusion of product into the colon/cecum under direct visualization. Requires full bowel cleansing. | High efficacy; allows for diagnostic evaluation of the colon [50] | Invasive, requires sedation, highest cost, risk of perforation [50] | Conventional FMT, Research settings |
| Enema | Retention enema administered rectally. May require limited or no bowel preparation. | Less invasive, low cost, can be self-administered [51] [50] | Possible leakage, lower retention, potentially lower efficacy for proximal colonization [50] | Rebyota [51], Outpatient/clinical |
| Oral Capsules | Ingestion of frozen or lyophilized product in acid-resistant capsules. No bowel prep. | Non-invasive, convenient, high patient acceptability [52] | Requires specialized encapsulation, potential for early gastric release | Vowst [53], Large-scale trials |
| Nasoenteric Tube | Tube passed via nose into duodenum/jejunum. No bowel prep. | Avoids colonoscopy/sedation | Patient discomfort, risk of aspiration, tube-related complications [50] | Patients with contraindications for other routes |
For all lower GI routes, administration of an anti-motility agent like loperamide one hour pre-procedure is often recommended to enhance product retention [50]. Patients should ideally abstain from antibiotics for 12-48 hours prior to FMT.
Quantitative Outcomes and Efficacy Data
Efficacy in RecurrentC. difficileInfection
FMT has achieved its highest success in preventing rCDI, leading to FDA approval of two microbiota-based products. The table below summarizes key efficacy data from pivotal trials.
Table 3: Efficacy of Microbiota-Based Therapeutics for rCDI
| Product / Trial | Modality | Administration | Primary Efficacy Endpoint | Result | Key Findings |
|---|---|---|---|---|---|
| Rebyota (fecal microbiota, live-jslm) [51] | Donor-derived microbiota | Single rectal enema | Prevention of rCDI recurrence at 8 weeks | ~70% success rate | Sustained clinical response of ~90% at 6 months in initial responders; Increased microbial diversity |
| Vowst (fecal microbiota spores, live-brpk) [53] | Purified Firmicutes spores | Oral capsules | Prevention of rCDI recurrence at 8 weeks | High efficacy (specific rates not detailed in sources) | Approved based on pivotal trials; Donor-independent spore formulation |
| Conventional FMT (Meta-analyses) [50] | Donor-derived microbiota | Colonoscopy, enema, etc. | Cure of rCDI | >80% cure rate | Superior to vancomycin alone (81% vs. 31%) [50]; Considered gold standard |
Outcomes in Other Indications and Long-Term Engraftment
Beyond rCDI, FMT is being investigated for a wide range of gastrointestinal and extraintestinal conditions. A 4-year follow-up study of FMT in adolescents with obesity provides compelling evidence of long-term engraftment and metabolic changes, which is highly relevant for chronic NDDs [54].
- Metabolic Health: While there was no significant difference in BMI after 4 years, FMT recipients showed significant improvements in waist circumference (-10.0 cm), total body fat (-4.8%), metabolic syndrome severity score (-0.58), systemic inflammation (-68% hs-CRP), and HDL cholesterol (+0.16 mmol/L) compared to the placebo group [54].
- Microbiome Engraftment: Shotgun metagenomic sequencing revealed the sustained long-term alteration of the gut microbiome in FMT recipients. Donor-derived bacterial and bacteriophage strains were stably retained for years, and FMT gut microbiomes had significantly more species and different functional pathway profiles compared to placebo microbiomes at the 4-year follow-up [54]. This demonstrates that a single FMT intervention can induce durable changes in the gut ecosystem.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing pre-clinical or clinical studies on FMT and the MGBA, the following tools and reagents are essential.
Table 4: Essential Research Tools for FMT and Gut-Brain Axis Studies
| Reagent / Tool | Function & Application | Examples & Notes |
|---|---|---|
| Shotgun Metagenomic Sequencing | Comprehensive analysis of microbial community composition, functional potential, and strain-level tracking [54] | Tracks donor strain engraftment and persistence (e.g., Desulfovibrio piger, Megasphaera sp.) [54] |
| Germ-Free (Gnotobiotic) Mice | In vivo models to establish causality and study mechanisms of gut-brain pathways [3] | Allows for colonization with specific human-derived microbiota; Essential for proving microbial influence on neuroinflammation |
| GC-MS / LC-MS | Quantification of microbial metabolites (e.g., SCFAs, bile acids, tryptophan derivatives) in feces, blood, and cerebrospinal fluid [21] | Acetate, propionate, and butyrate concentrations in human CSF range from 0-171 mM, 0-6 mM, and 0-2.8 mM, respectively [21] |
| GPR43/FFAR2 & GPR41/FFAR3 Agonists/Antagonists | Pharmacological tools to dissect the role of SCFA receptors in microglial activation and neuroinflammation [21] | Receptor expression on microglia is context-dependent and can be induced by sustained SCFA exposure [21] |
| PBS or Saline with Glycerol | Standard cryoprotectant solution for long-term storage of fecal microbiota samples and FMT product [50] | 10-20% glycerol is commonly used; allows for creation of frozen "stool banks" |
| Anti-Motility Agent (e.g., Loperamide) | Pre-treatment to reduce gut motility and improve retention of administered FMT product [50] | Typically administered 1 hour prior to FMT infusion |
FMT has evolved from a niche therapy to a standardized, evidence-based intervention for rCDI, with a growing regulatory framework supporting its use [51] [50]. Its application as a tool for microbial ecosystem engineering within the gut-brain axis represents a frontier in neurodegenerative disease research. The ability of FMT to induce sustained changes in the gut microbiome and improve metabolic parameters, as demonstrated in long-term studies, provides a strong rationale for its investigation in chronic neurological conditions [54].
Future work must focus on elucidating the specific mechanisms by which FMT-derived microbes and their metabolites influence microglial function, neuroinflammation, and protein aggregation [2] [21]. Furthermore, the field is moving towards more refined Live Biotherapeutic Products (LBPs)—defined consortia of bacterial strains that offer greater consistency, safety, and mechanistic clarity than conventional FMT [55] [52]. As our understanding of the MGBA deepens, targeting the gut microbiome through interventions like FMT and LBPs offers a promising, multi-targeted strategy to modify the progression of neurodegenerative diseases.
The integration of metagenomics and metabolomics represents a transformative approach in modern drug development, particularly within the framework of the gut-brain axis and its implications for neurodegenerative diseases. This technical guide explores how multi-omics technologies are revolutionizing target discovery by providing unprecedented insights into the complex interactions between gut microbiota, their metabolic products, and neurological pathophysiology. We present comprehensive methodological frameworks, analytical workflows, and experimental protocols that leverage integrated meta-omics sciences to identify novel therapeutic targets and biomarkers. Through systematic analysis of microbial communities and their functional metabolic outputs, researchers can now decipher the molecular mechanisms underlying neurodegenerative processes and develop targeted interventions that address the root causes rather than merely managing symptoms.
The gut-brain axis represents a complex, bidirectional communication network between the gastrointestinal tract and the central nervous system that is fundamentally mediated by the gut microbiota. Recent advances in meta-omics sciences have revealed that this axis plays a pivotal role in the pathogenesis of various neurodegenerative diseases, including Alzheimer's disease (AD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and Huntington's disease (HD) [3] [56]. The vast genetic and metabolic potential of the gut microbiome—containing nearly 150 times more genes than the human genome—underpins its ubiquity in nearly every aspect of human biology, including health maintenance, development, aging, and disease [3].
The biological importance of the gut microbiome is evident from the earliest stages of life, with microbial colonization contributing to immune system development and remaining stable throughout adulthood until potentially undergoing alterations during neurodegenerative processes [3]. Through the production of neuroactive substances, metabolites, and hormones, gut microbiota can directly and indirectly influence brain function via multiple pathways including modulation of the immune system, vagus nerve, enteric nervous system, neuroendocrine system, and circulatory system [3]. Evidence has unveiled that the gut microbiome provides essential cues to microglia, astrocytes, and oligodendrocytes, making the microbiota-gut-brain axis an actionable target to ameliorate the development and progression of neurodegenerative diseases [3].
Table 1: Key Evidence Linking Gut-Brain Axis to Neurodegenerative Diseases
| Disease | Microbial Alterations | Metabolic Perturbations | Proposed Mechanisms |
|---|---|---|---|
| Alzheimer's Disease (AD) | Gut dysbiosis in preclinical AD patients [3] | Altered short-chain fatty acid profiles [56] | Microglial dysfunction, increased neuroinflammation [3] |
| Parkinson's Disease (PD) | Changes in prodromal PD patients [3] | Modified bile acid metabolism [56] | α-synuclein pathology, immune system activation [56] |
| Huntington's Disease (HD) | Heightened volatility in pre-motor stage [57] | Perturbed butanoate metabolism [58] | Altered Bacteroides species correlated with plasma metabolites [57] |
| Amyotrophic Lateral Sclerosis (ALS) | Reduced microbial diversity [56] | Impaired nicotinamide metabolism [56] | Compromised blood-brain barrier, peripheral immune activation [3] |
Methodological Foundations
Metagenomics in Microbiome Analysis
Metagenomics involves the comprehensive analysis of genomic material recovered directly from environmental samples—in this context, human gut samples—without the need for cultivation. This approach allows researchers to characterize taxonomic composition and functional potential of microbial communities [56].
Shotgun metagenomics represents the gold standard, providing information on the functional potential of the microbiota through high-throughput sequencing of all microbial genomic DNA in a sample. This method enables:
- Taxonomic profiling at species and strain levels
- Functional annotation of microbial genes
- Pathway reconstruction of metabolic capabilities
- Identification of microbial genes encoding enzymes for neuroactive metabolite production
The marker gene approach (e.g., 16S/18S rRNA gene sequencing) offers a cost-effective alternative for taxonomic profiling through PCR-based amplification of hypervariable regions, though with limited functional insights [56].
Metabolomics in Host-Microbe Interactions
Metabolomics provides a comprehensive study of the metabolite array resulting from microbiota-host interactions, capturing phenotypic changes induced by exogenous compounds or disease processes [59]. This systems biology tool is particularly valuable for understanding the functional output of microbial communities and their influence on host physiology [56].
Metabolomics approaches can be divided into:
- Untargeted metabolomics: Broad screening of thousands of metabolites simultaneously to discover novel dysregulations
- Targeted metabolomics: Focused analysis of specific molecules or pathways offering detailed quantitative insights
- Pseudotargeted metabolomics: Integration of both approaches enabling high coverage and accurate quantification [59]
Table 2: Analytical Platforms for Metabolomics in Gut-Brain Axis Research
| Technology | Applications | Advantages | Limitations |
|---|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Broad metabolite coverage, lipidomics, bile acids | High sensitivity, wide dynamic range, handles nonvolatile compounds | Matrix effects, requires expert optimization [59] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Volatile compounds, short-chain fatty acids, organic acids | High selectivity, repeatability, structured databases | Requires derivatization, limited to volatile compounds [59] |
| Capillary Electrophoresis-Mass Spectrometry (CE-MS) | Polar/ionic metabolites, neurotransmitters | Excellent for polar compounds, high resolution | Technical challenges, lower reproducibility [59] |
| Nuclear Magnetic Resonance (NMR) | Absolute quantification, structural elucidation | Non-destructive, quantitative, reproducible | Lower sensitivity compared to MS [59] |
| Mass Spectrometry Imaging (MSI) | Spatial distribution of metabolites in tissues | Spatial information, untargeted discovery | Semi-quantitative, complex sample preparation [59] |
Integrated Multi-Omics Workflow
The combination of metagenomics and metabolomics creates a powerful framework for elucidating the functional relationships between microbial communities and their host effects. This integrated approach follows a systematic workflow:
Experimental Protocols and Methodologies
Sample Collection and Preparation
Protocol 3.1.1: Fecal Sample Collection for Integrated Metagenomics and Metabolomics
Participant Preparation: Subjects should avoid antibiotics, probiotics, and fermented foods for at least 4 weeks prior to sampling. Document dietary intake, medication use, and clinical parameters [60].
Sample Collection: Collect fresh fecal samples in sterile containers with anaerobic environment preservation. Immediately aliquot samples for:
- DNA stabilization (e.g., DNA/RNA Shield or similar preservation buffers)
- Metabolite stabilization (e.g., flash freezing in liquid nitrogen)
- Long-term storage at -80°C [60]
Blood Collection: Draw peripheral blood samples using EDTA tubes. Process within 30 minutes of collection through centrifugation (4°C, 3000 rpm, 10 minutes) to obtain plasma. Store aliquots at -80°C [60].
Metadata Documentation: Record comprehensive clinical phenotypes, including cognitive assessments, motor function, dietary patterns, and medication history [60].
Protocol 3.1.2: DNA Extraction for Shotgun Metagenomics
Cell Lysis: Use mechanical disruption (bead beating) combined with chemical lysis to ensure comprehensive breakdown of diverse bacterial cell walls.
DNA Purification: Employ commercial kits (e.g., QIAamp PowerFecal Pro DNA Kit) with silica membrane-based purification to remove inhibitors.
Quality Assessment: Verify DNA integrity through agarose gel electrophoresis and quantify using fluorometric methods (e.g., Qubit dsDNA HS Assay). Ensure minimum concentration of 10 ng/μL and A260/280 ratio of 1.8-2.0 [60].
Library Preparation: Utilize TruSeq DNA PCR-Free Library Preparation Kit (Illumina) or equivalent. Assess library quality using Bioanalyzer/TapeStation and quantify by qPCR [60].
Metagenomic Sequencing and Analysis
Protocol 3.2.1: Shotgun Metagenomic Sequencing
Sequencing Platform: Perform sequencing using Illumina NovaSeq, BGI-Seq500, or similar platforms with 150 bp paired-end sequencing of ~350 bp inserts [60].
Sequencing Depth: Target minimum 10-20 million reads per sample to ensure adequate coverage for taxonomic and functional analysis.
Quality Control: Process raw reads using FASTP to remove reads containing >50% low-quality bases (quality ≤20) or exceeding five ambiguous bases [60].
Host DNA Depletion: Align reads to human genome (Hg19) using bowtie2 to eliminate host DNA contamination [60].
Protocol 3.2.2: Bioinformatic Analysis
Taxonomic Profiling: Use MetaPhlAn 3.0 with default parameters for species-level profiling from high-quality metagenomic sequencing data [60].
Functional Profiling: Employ HUMAnN 3.0 for analysis of metabolic pathways and gene families. Map reads to reference databases (UniRef90, KEGG, MetaCyc) [60].
Statistical Analysis: Perform alpha-diversity (Shannon, Chao1 indices) and beta-diversity (Bray-Curtis dissimilarity, PCoA) analyses using appropriate tools (QIIME 2, Phyloseq).
Differential Abundance: Identify significantly altered taxa and pathways using statistical models (DESeq2, LEfSe, MaAsLin2) with appropriate covariates.
Metabolomic Profiling and Integration
Protocol 3.3.1: Untargeted Metabolomics of Fecal and Plasma Samples
Metabolite Extraction:
- Fecal Samples: Weigh 50 mg of frozen feces, add 500 μL of cold methanol:water (80:20) with internal standards. Homogenize using bead beating, centrifuge at 14,000×g for 15 minutes at 4°C. Collect supernatant for analysis [60].
- Plasma Samples: Mix 50 μL plasma with 200 μL cold acetonitrile:methanol (50:50) with internal standards. Vortex vigorously, incubate at -20°C for 60 minutes, centrifuge at 14,000×g for 15 minutes at 4°C. Collect supernatant for analysis [59].
LC-MS Analysis:
- Chromatography: Utilize reversed-phase (C18) and HILIC columns for comprehensive metabolite separation. Employ gradient elution with water/acetonitrile containing 0.1% formic acid.
- Mass Spectrometry: Operate in both positive and negative ionization modes with data-dependent acquisition (DDA) or data-independent acquisition (DIA). Use high-resolution mass analyzers (Q-TOF, Orbitrap) with resolution >35,000 [59].
Data Processing:
- Perform peak picking, alignment, and integration using XCMS, Progenesis QI, or MS-DIAL.
- Annotate metabolites using accurate mass, MS/MS fragmentation, and retention time matching against databases (HMDB, METLIN, MassBank).
- Apply rigorous quality control including pooled quality control samples and internal standards [59].
Protocol 3.3.2: Multi-Omics Data Integration
Correlation Analysis: Calculate Spearman correlations between microbial taxa and metabolite levels. Apply false discovery rate (FDR) correction for multiple testing.
Multivariate Statistics: Employ sparse Partial Least Squares Discriminant Analysis (sPLS-DA) to identify multi-omics signatures discriminating disease states.
Pathway Integration: Map significantly altered metabolites and microbial functions to integrated metabolic pathways using KEGG, MetaCyc, and Reactome databases.
Network Analysis: Construct integrated association networks using Cytoscape or similar platforms to visualize relationships between microbial taxa, metabolic pathways, and clinical phenotypes [60].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Multi-Omics Studies
| Category | Specific Products/Platforms | Key Applications | Technical Considerations |
|---|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro DNA Kit, DNeasy PowerSoil Kit | High-quality microbial DNA extraction from fecal samples | Mechanical lysis essential for Gram-positive bacteria |
| Library Preparation | TruSeq DNA PCR-Free Kit (Illumina), Nextera XT DNA Library Prep Kit | Metagenomic library construction for shotgun sequencing | PCR-free preferred to reduce bias |
| Sequencing Platforms | Illumina NovaSeq, BGI-Seq500, PacBio Sequel, Oxford Nanopore | High-throughput sequencing for metagenomic analysis | Short-read for abundance, long-read for assembly |
| Chromatography Systems | Vanquish UHPLC (Thermo), Agilent 1290 Infinity II, Waters ACQUITY | Metabolite separation prior to mass spectrometry | HILIC and reversed-phase for comprehensive coverage |
| Mass Spectrometers | Q-Exactive HF (Orbitrap), TripleTOF, timsTOF | High-resolution metabolomic profiling | High mass accuracy and resolution critical for annotation |
| Statistical Software | R packages: mixOmics, vegan, MaAsLin2, MetaboAnalyst | Multi-omics data integration and statistical analysis | Specialized packages for longitudinal and multivariate data |
| Bioinformatics Tools | MetaPhlAn 3.0, HUMAnN 3.0, XCMS, GNPS, QIIME 2 | Taxonomic profiling, functional analysis, metabolomics | Containerized deployments (Docker) enhance reproducibility |
Biological Pathways and Mechanisms
The integration of metagenomics and metabolomics has elucidated several key pathways through which gut microbiota influence neurodegenerative processes via the gut-brain axis:
Key Pathway Mechanisms in Neurodegeneration
Short-Chain Fatty Acid (SCFA) Signaling: Butyrate, propionate, and acetate produced by microbial fermentation of dietary fiber influence neuroinflammation through:
Tryptophan-Kynurenine Metabolism: Gut microbiota directly metabolize tryptophan, competing with the host kynurenine pathway and influencing:
Bile Acid Transformations: Microbial modifications of primary bile acids generate secondary bile acids with distinct signaling properties:
- FXR and TGR5 receptor activation influencing neuroinflammation
- Mitochondrial function and oxidative stress regulation
- Ceramide metabolism impacting neuronal survival [3]
Applications in Neurodegenerative Disease Research
Huntington's Disease Mechanisms
Integrated metagenomics and metabolomics in R6/1 transgenic mouse models of HD revealed significant gut microbiome alterations during pre-motor symptomatic stages, highlighting the potential role of the gut in modulating disease pathogenesis [57] [58]. Key findings included:
- Heightened volatility in the HD gut microbiome at pre-symptomatic stages, indicating early effects of the HD mutation in the gut
- Perturbed HD gut microbiome function prior to significant cognitive and motor dysfunction
- Elevated butanoate metabolism pathway, suggesting increased production of the protective SCFA butyrate in the gut
- Negative correlations between several Bacteroides species and plasma ATP and pipecolic acid levels [57] [58]
These findings suggest that gut microbiome instability during pre-motor symptomatic stages may have significant consequences on host health and potentially contribute to disease pathogenesis through altered gut-brain signaling.
Pediatric Neurodevelopmental Disorders
A comprehensive study combining shotgun metagenomics and untargeted metabolomics in children with neurodevelopmental disorders (NDD) revealed:
- Reduced gut diversity and significant dysregulation of beneficial taxa including Akkermansia muciniphila and Lactococcus lactis
- Enrichment of GABA/lactate-producing bacteria and disrupted metabolic pathways including polysaccharides, fatty acids, and amino acid metabolism
- Fecal metabolomic alterations with 100 enriched metabolites (including polyamines and GABA) and 254 depleted metabolites (including bile acids and butyrate)
- Plasma metabolomic disturbances with 321 enriched metabolites (like free fatty acids) and 270 depleted metabolites (including glycerophospholipids) [60]
Multi-omics integration identified key microbial-metabolite correlations linking NDD-depleted species to specific metabolic disturbances, providing potential targets for therapeutic intervention.
Target Discovery for Cardiac Diseases
While focusing on cardiac diseases rather than neurodegenerative disorders, a Mendelian randomization approach integrating metabolomics and proteomics demonstrated the power of multi-omics integration for identifying novel drug targets [61]. This study:
- Identified 35 plasma metabolites associated with cardiac disease through genome-wide Mendelian randomization
- Linked these metabolites to 38 druggable proteins expressed in cardiac tissue through cis-Mendelian randomization
- Recapitulated known associations (e.g., digoxin target AT1B2 with taurine and NICM risk)
- Identified novel findings (e.g., RET association with phosphatidylcholines and decreased AF/HF risk) [61]
This approach provides a methodological framework that can be adapted to neurodegenerative disease research for identifying actionable therapeutic targets through multi-omics integration.
The integration of metagenomics and metabolomics represents a paradigm shift in our approach to understanding and treating neurodegenerative diseases through the gut-brain axis. By moving beyond correlative observations to mechanistic explorations, researchers can now identify novel therapeutic targets and develop targeted interventions that address the root causes of neurodegeneration rather than merely managing symptoms. The methodologies and frameworks presented in this technical guide provide a comprehensive roadmap for implementing integrated multi-omics approaches in drug discovery pipelines.
As technologies continue to advance, emerging approaches including single-cell metabolomics, artificial intelligence, and mass spectrometry imaging will further enhance our ability to decipher the complex interactions between gut microbiota and neurological health [59]. The future of neurodegenerative disease therapeutics will likely include microbiota-targeted interventions such as precision probiotics, prebiotics, and fecal microbiota transplantation, all informed by deep multi-omics characterization of individual patients. Through continued refinement of these integrative approaches, we move closer to personalized medicine strategies that can effectively halt or reverse the progression of devastating neurodegenerative disorders.
Navigating Translational Challenges: Variability, Biomarkers, and Personalized Approaches
Addressing Inter-Individual Variability in Microbial Composition and Treatment Response
The gut-brain axis represents one of the most dynamic interfaces in neurogastroenterology, constituting a complex, bidirectional communication network that integrates neural, endocrine, and immune signaling pathways between the gastrointestinal tract and the central nervous system (CNS) [62] [3]. Within this framework, the gut microbiome—the diverse community of microorganisms inhabiting the human gastrointestinal tract—has emerged as a critical regulator of brain development, function, and behavior [62] [6]. However, a fundamental challenge complicating both research and therapeutic development is the profound inter-individual variability in microbial composition [63] and the consequent divergent responses to microbiome-targeted interventions.
Understanding this variability is particularly crucial within the context of neurodegenerative disease research, where the gut microbiome is increasingly implicated in disease pathogenesis and progression [3] [64] [65]. The composition of an individual's gut microbiota is shaped by a multitude of intrinsic and extrinsic factors throughout the lifespan, resulting in a unique microbial fingerprint that influences disease risk, progression, and treatment response [62] [63]. This review provides a technical guide for researchers and drug development professionals seeking to address this variability in their experimental designs and therapeutic strategies.
Quantifying Inter-Individual Variability in Microbial Composition
Inter-individual variability in gut microbiome composition is not random noise but rather a structured phenomenon influenced by identifiable factors. A comprehensive understanding requires quantifying how these factors contribute to microbial diversity.
Table 1: Key Factors Contributing to Inter-Individual Variability in Gut Microbiome Composition
| Factor Category | Specific Factors | Impact on Microbial Diversity | References |
|---|---|---|---|
| Host-Intrinsic Factors | Genetics, Age, Sex | Influences microbial community structure and stability; age-related shifts linked to immunosenescence. | [62] [6] |
| Early-Life Exposures | Mode of delivery (vaginal vs. C-section), Breastfeeding vs. formula, Antibiotic exposure | Foundational for microbiome assembly; has long-lasting effects on immune and neural development. | [62] [6] |
| Lifestyle & Dietary Factors | Long-term dietary patterns (Western, Mediterranean, etc.), Fiber intake, Protein/Fat intake | Diet has the greatest lifelong influence on microbiota composition; rapidly alters metabolite production. | [62] [3] |
| Geographical & Cultural Factors | Geography, Ethnicity, Socioeconomic status | Contributes to large-scale population-level differences in microbiome composition. | [65] |
| Medical Interventions | Antibiotic usage, Other medications (e.g., psychotropics), Fecal Microbiota Transplantation | Antibiotics are a key disruptor; medications have off-target effects on microbiota; FMT can introduce new donor variability. | [62] [65] |
Table 2: Microbiome Alterations in Representative Neurodegenerative Diseases
| Neurodegenerative Disease | Reported Microbial Alterations | Potential Functional Consequences | References |
|---|---|---|---|
| Alzheimer's Disease (AD) | ↑ Proteobacteria, Bifidobacterium; ↓ Firmicutes, Clostridiaceae, Lachnospiraceae | Loss of butyrate-producing bacteria; increased pro-inflammatory potential. | [65] [3] |
| Parkinson's Disease (PD) | ↑ Akkermansia, Lactobacillus; ↓ Roseburia, Faecalibacterium, Lachnospiraceae | Depletion of butyrate-producers; correlates with motor/non-motor deficits and disease duration. | [65] [3] |
| Amyotrophic Lateral Sclerosis (ALS) | ↑ Bacteroidetes, Enterobacteriaceae; ↓ Lachnospiraceae; Lower Firmicutes/Bacteroidetes ratio in cognitively impaired | Altered microbial profile associated with microglial dysregulation and disease progression. | [65] |
| Huntington's Disease (HD) | ↓ Firmicutes, Lachnospiraceae, Akkermansiaceae (in males) | Altered microbiota interacts with peripheral immune responses (e.g., IL-4, IL-6). | [65] |
Diagram 1: Factors driving inter-individual variability and impacting treatment response.
Mechanisms Linking Microbial Variability to Neurodegenerative Diseases
The communication between a variable gut microbiome and the brain occurs through multiple, interconnected pathways. The specific composition of an individual's microbiota directly influences the signaling molecules and inflammatory mediators that travel along these pathways, thereby modulating neurodegenerative processes.
Immunological Signaling Pathway
The immune system acts as a primary conduit for gut-brain communication. Gut microbes and their metabolites, such as short-chain fatty acids (SCFAs) and lipopolysaccharide (LPS), regulate systemic and neuroinflammation [3] [6]. SCFAs (e.g., butyrate, propionate) typically exert anti-inflammatory effects by promoting regulatory T-cell differentiation and inhibiting HDAC, whereas LPS can promote pro-inflammatory responses [6]. The baseline state of an individual's immune system and their specific microbial community determine the tone of this signaling, influencing microglial activation states (e.g., homeostatic vs. disease-associated microglia) in the brain, a key feature in Alzheimer's and Parkinson's pathology [3].
Neuroendocrine and Vagus Nerve Pathways
The gut microbiome influences the hypothalamic-pituitary-adrenal (HPA) axis, modulating the body's neuroendocrine response to stress [62] [66]. A dysregulated HPA axis and elevated glucocorticoids can increase intestinal permeability, potentially exacerbating inflammation [66]. Furthermore, microbial metabolites and neurotransmitters can signal directly to the CNS via the vagus nerve, which serves as a direct neural connection between the enteric nervous system and the brainstem [62] [65]. The production of neuroactive substances like serotonin (5-HT), dopamine, and GABA by gut bacteria provides a direct mechanism for microbiome-to-brain signaling [62] [3]. Inter-individual differences in microbial neuroactive metabolite production or vagal tone could significantly alter the strength of this communication.
Diagram 2: Key communication pathways of the microbiota-gut-brain axis.
Methodological Approaches for Addressing Variability in Research
Robust experimental design and advanced analytical techniques are paramount for dissecting the impact of inter-individual variability in gut-brain axis research.
Animal Models and Experimental Protocols
Animal models, particularly germ-free (GF) and gnotobiotic mice, are indispensable for establishing causality. The protocol below outlines a common approach to investigate the role of specific microbiota in neurodegenerative disease models.
Protocol 1: Fecal Microbiota Transplantation (FMT) in Rodent Neurodegeneration Models
- Objective: To determine the causal role of a human or animal donor's microbiota on disease phenotypes in a recipient rodent model of neurodegeneration.
- Materials:
- Donor subjects (e.g., human patients with neurodegenerative disease, age-matched healthy controls, or transgenic animal models).
- Recipient animals (e.g., germ-free wild-type or transgenic mice, or antibiotic-treated specific pathogen-free mice).
- Anaerobic workstation for sample processing.
- Homogenization equipment (e.g., bead beater).
- Gavage needles for oral administration.
- DNA/RNA extraction and sequencing kits for downstream verification.
- Methods:
- Donor Material Preparation: Collect fresh fecal samples from donors. Under anaerobic conditions, homogenize the sample in sterile phosphate-buffered saline (PBS) or glycerol-based cryopreservative. Filter the homogenate through a mesh to remove large particulate matter. Aliquot and either use immediately or store at -80°C.
- Recipient Preparation: Use adult recipient mice (e.g., 8-12 weeks old). For antibiotic depletion, treat mice with a broad-spectrum antibiotic cocktail (e.g., ampicillin, vancomycin, neomycin, metronidazole) in their drinking water for 2-3 weeks. For germ-free models, maintain them in sterile isolators.
- Transplantation: By oral gavage, administer a single dose (e.g., 200 µL) of the fecal slurry to each recipient mouse. Control groups should receive slurry from control donors (e.g., healthy vs. diseased).
- Phenotypic Assessment: Monitor the animals for several weeks post-FMT. Assess:
- GI Function: Gut permeability, transit time.
- Microbiome Engraftment: Collect fecal samples at regular intervals for 16S rRNA or shotgun metagenomic sequencing to verify colonization.
- Behavior: Cognitive and motor tests relevant to the disease (e.g., Morris water maze for AD, beam walking for PD).
- Neuropathology: Post-mortem analysis of brain pathology (e.g., Aβ plaques, α-synuclein aggregates, microglial activation, astrogliosis).
- Considerations for Variability: Donor-recipient pairing should account for recipient genotype, age, and sex. Using multiple recipient animals from a single donor helps control for donor-specific effects while still capturing inter-donor variability.
Analytical and Statistical Frameworks
Moving beyond simple correlative studies requires sophisticated analytical methods. Systems Biology approaches, including the use of Genome-scale Metabolic Models (GEMs), can infer microbe-microbe and host-microbe interactions to predict how an individual's microbiome might contribute to disease development or prevention [64]. These computational models integrate multi-omics data (metagenomics, metabolomics) to simulate community metabolism and identify key species or metabolites that drive phenotypic differences between individuals.
Table 3: The Scientist's Toolkit: Key Reagents and Models for Gut-Brain Axis Research
| Tool Category | Specific Tool/Reagent | Function/Application | Considerations for Variability |
|---|---|---|---|
| Animal Models | Germ-Free (GF) Mice | Allows colonization with defined microbiota; essential for establishing causality. | Lacks a developed immune system; requires strict isolator housing. |
| Gnotobiotic Mice | Colonized with a known, simplified microbial community. | Reduces complexity but may not fully recapitulate human community interactions. | |
| Humanized Microbiome Mice (via FMT) | Models the human gut ecosystem in a mouse host. | Retains donor variability; host genetics and environment (e.g., diet) still influence outcomes. | |
| Molecular & Cellular Tools | Antibiotic Cocktails | Depletes the endogenous microbiota to create a "clean slate" for intervention. | Effects can be transient and incomplete; can have off-target effects on host physiology. |
| Toll-like Receptor (TLR) Agonists/Antagonists | Probes specific immune signaling pathways (e.g., TLR4 for LPS signaling). | Individual immune cell responses may vary. | |
| SCFAs (Butyrate, Propionate, Acetate) | Used to supplement diet or treat cells to study metabolite-specific effects. | Dose and route of administration critically impact results and interpretation. | |
| Analytical Techniques | 16S rRNA & Shotgun Metagenomic Sequencing | Profiles microbial community composition and functional potential. | Bioinformatic analysis is complex; results can be influenced by sequencing depth and platform. |
| Metabolomics (LC-MS, GC-MS) | Identifies and quantifies microbial and host metabolites in feces, serum, and brain. | Provides a functional readout but requires sophisticated instrumentation and analysis. | |
| Genome-scale Metabolic Models (GEMs) | Computational models to predict metabolic interactions within microbial communities and with the host. | Model predictions require experimental validation. |
Translational Applications and Personalized Therapeutic Strategies
The ultimate goal of understanding inter-individual variability is to develop more effective, personalized therapeutic interventions for neurodegenerative diseases.
Protocol 2: Designing a Personalized, Microbiome-Targeted Dietary Intervention
- Objective: To use individual microbiome profiling to guide a nutritional intervention aimed at improving microbial metabolites and reducing inflammation in a prodromal neurodegenerative disease cohort.
- Materials:
- Prebiotic fibers (e.g., inulin, fructooligosaccharides), Polyphenol-rich foods.
- Food diaries and dietary assessment tools.
- Fecal and blood collection kits.
- Sequencing and metabolomics platforms.
- Methods:
- Baseline Profiling: Recruit participants (e.g., individuals with REM sleep behavior disorder as prodromal PD). Collect detailed metadata (diet, medical history). Perform baseline stool collection for metagenomic sequencing and serum for metabolomics (e.g., SCFAs, inflammatory cytokines).
- Intervention Design: Based on baseline profiles, stratify participants. For example, individuals with low microbial gene count and low SCFA producers might receive a specific, high-fiber, prebiotic-rich dietary plan. A different intervention (e.g., omega-3 supplementation to address inflammation) might be designed for another profile.
- Intervention and Monitoring: Implement the dietary intervention for a set period (e.g., 3-6 months). Use food diaries and biomarker tracking (e.g., fecal SCFAs) for adherence.
- Outcome Assessment: Measure primary outcomes (cognitive/motor scores) and secondary outcomes (microbiome shift, inflammatory markers, SCFA levels). Use machine learning to identify baseline features (microbial signatures) that predict a positive response to the intervention.
- Considerations for Variability: This is a hypothesis-testing framework for personalization. The core idea is to move from a one-size-fits-all intervention to a stratified medicine approach, acknowledging that different individuals will require different interventions based on their unique microbial and metabolic baseline.
Therapeutic strategies such as probiotics, prebiotics, and Fecal Microbiota Transplantation (FMT) have shown promise but are characterized by variable efficacy [65]. A one-size-fits-all approach is unlikely to succeed. For instance, FMT from healthy wild-type mice into a Huntington's disease model improved cognitive functions only in female mice, highlighting how sex and baseline microbial/immune state can dictate treatment outcome [65]. Future clinical trials must integrate deep phenotyping—including metagenomics, metabolomics, and immune profiling—to identify biomarkers that predict which patients are most likely to respond to a given microbiome-targeted therapy. This will pave the way for truly personalized neuro-gastroenterological treatments.
Overcoming Blood-Brain Barrier Hurdles with Gut-Restricted Therapeutic Strategies
The blood-brain barrier (BBB) represents a formidable challenge in treating neurodegenerative diseases, excluding over 98% of small-molecule drugs and all large-molecule therapeutics from the central nervous system (CNS). This whitepaper explores the revolutionary paradigm of targeting the gut-brain axis using gut-restricted therapeutics as a viable strategy to circumvent the BBB. Through elaborate bidirectional communication pathways, the gut microbiome influences central nervous system function, neuroinflammation, and glial cell activity. Gut-restricted drugs, designed to act locally within the gastrointestinal tract without significant systemic absorption, offer a promising approach to modulate this axis, minimizing off-target effects while potentially ameliorating neurodegenerative pathology. This technical guide provides a comprehensive overview of the underlying mechanisms, design strategies, experimental methodologies, and future directions for leveraging gut-restricted therapeutic strategies in neurodegenerative disease research.
The blood-brain barrier is a highly selective semipermeable border of endothelial cells that regulates the transfer of solutes and chemicals between the circulatory system and the central nervous system, thus protecting the brain from harmful or unwanted substances in the blood [67]. This barrier arises from the selectivity of tight junctions between endothelial cells of brain capillaries, effectively restricting the passage of pathogens, large molecules, and most small-molecule drugs [67] [68]. While this protective function is crucial for maintaining CNS homeostasis, it presents a major impediment to pharmacotherapy for neurological disorders, as the BBB excludes 100% of large-molecule neurotherapeutics and more than 98% of all small-molecule drugs [67] [68].
In neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS), the BBB may become compromised, yet drug delivery remains challenging [69] [70]. BBB disruption is increasingly recognized as a feature of neurodegenerative conditions, with alterations in transport systems, enhanced immune cell entry, and dysfunctional signaling contributing to disease progression [69]. Neuroinflammation, a hallmark of neurodegeneration, can further compromise BBB integrity, creating a vicious cycle of neuronal damage [69] [70].
The gut-brain axis represents a multifaceted bidirectional communication network between the gastrointestinal tract and the CNS, involving neural, endocrine, immune, and metabolic pathways [29] [3]. The vast genetic and metabolic potential of the gut microbiome—comprising nearly 150 times more genes than the human genome—underpins its influence on nearly every aspect of human biology, including brain health and disease [3]. Targeting this axis through gut-restricted therapeutics that modulate microbial composition and function offers a novel, indirect approach to influence brain pathophysiology while circumventing the BBB entirely.
The Gut-Brain Axis: Communication Pathways
The microbiota-gut-brain axis encompasses elaborate bidirectional communication channels that enable continuous crosstalk between the gut and the brain. Understanding these pathways is essential for developing effective gut-restricted therapeutic strategies.
Neural Pathways
The vagus nerve serves as a direct neural connection between the gut and the brain, transmitting signals from the intestinal lumen to the CNS [3]. This pathway allows gut-derived signals to influence brain function rapidly. Preclinical studies demonstrate that vagotomy abolishes the effects of certain probiotic interventions, highlighting its critical role in gut-brain communication [29]. The enteric nervous system (ENS), sometimes called the "second brain," also plays a integral role, containing more neurons than the spinal cord and capable of autonomous function while maintaining extensive connections with the CNS [3].
Endocrine and Immune Signaling
Enteroendocrine cells scattered throughout the intestinal epithelium detect gut luminal contents and release hormones such as cholecystokinin (CCK), peptide YY (PYY), and glucagon-like peptide-1 (GLP-1) in response to nutritional and microbial signals [29]. These hormones can enter systemic circulation to reach the brain or act locally on afferent nerve fibers. The immune system provides another crucial communication route, with gut microbiota influencing systemic and CNS immunity through modulation of cytokine production and immune cell function [3]. Microglia, the resident immune cells of the CNS, are particularly responsive to gut-derived immune signals [29] [3].
Microbial Metabolites
Gut microbiota produce or contribute to the production of numerous neuroactive metabolites that can influence brain function. Short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—are produced by bacterial fermentation of dietary fiber and can cross the BBB, directly affecting microglial function and neuroinflammation [29] [3]. Bile acid metabolites transformed by gut bacteria act on various receptors, including the farnesoid X receptor (FXR) and Takeda G-protein-coupled receptor 5 (TGR5), to influence glucose metabolism, immune function, and neurotransmitter release [29]. Tryptophan metabolites, including kynurenine and indole derivatives, serve as crucial intermediaries in gut-brain communication, with kynurenine able to cross the BBB and influence CNS function [29] [3].
Table 1: Key Microbial-Derived Metabolites in Gut-Brain Communication
| Metabolite | Primary Producers | Receptors/Targets | CNS Effects |
|---|---|---|---|
| Short-chain fatty acids (SCFAs) | Bacteroides, Firmicutes | GPR41, GPR43, GPR109A, HDAC inhibition | Microglial maturation, BBB integrity, neuroinflammation modulation |
| Secondary bile acids | Multiple bacterial species | FXR, TGR5 | GLP-1 release, HPA axis modulation, neuroprotection |
| Tryptophan metabolites (indole, kynurenine) | E. coli, Bacteroides | Aryl hydrocarbon receptor (AhR), NMDA receptor | Astrocyte inflammation modulation, neurotoxicity/neuroprotection |
| Neurotransmitters (GABA, serotonin, dopamine) | Lactobacillus, Bifidobacterium, Escherichia | GABA receptors, 5-HT receptors, dopamine receptors | Neuronal excitability, mood, motor control |
The following diagram illustrates the primary communication pathways of the microbiota-gut-brain axis:
Gut-Restricted Therapeutics: Design Strategies and Mechanisms
Gut-restricted drugs are orally administered compounds designed to exert their therapeutic effects specifically within the intestinal lumen while minimizing systemic exposure [32] [71]. This approach offers several advantages for modulating the gut-brain axis: reduced risk of systemic side effects, high local drug concentrations at the site of action, and avoidance of first-pass metabolism [32].
Physicochemical Design Strategies
The design of gut-restricted drugs involves strategic manipulation of physicochemical properties to limit intestinal absorption:
Highly polar and/or charged compounds represent a primary strategy for achieving gut restriction. Passive diffusion, the primary mechanism for small-molecule absorption, favors neutral, lipophilic compounds [32]. Incorporating highly polar functional groups, carbohydrates, or peptide motifs increases hydrophilicity and reduces membrane permeability. For example, acarbose, an α-glucosidase inhibitor for type 2 diabetes, exhibits less than 2% bioavailability due to its high hydrophilicity (clogP = -9, 14 hydrogen-bond donors, 19 hydrogen-bond acceptors) [32]. Similarly, Sibofimloc, a FimH blocker developed for Crohn's disease, incorporates two mannose units that confer high polarity (clogP = 0.3, TPSA = 200 Ų), resulting in limited systemic exposure [32].
High molecular weight compounds including polymers, proteins, and oligonucleotides naturally exhibit restricted absorption across the intestinal epithelium [71]. Larazotide acetate (AT-1001), a zonulin antagonist developed for celiac disease, is an acyclic oligopeptide with high molecular weight and hydrophilicity (clogP = -2.2, TPSA = 301 Ų) that results in negligible systemic exposure [32].
Kinetophore approach involves tethering a pharmacologically active scaffold to a polar or charged structural unit that is non-essential for activity but drastically reduces absorption [32]. This approach has been successfully employed in the development of ileal bile acid transporter (IBAT/asodium-dependent bile acid transporter [ASBT]) inhibitors such as maralixibat, which received FDA approval for cholestatic pruritus in Alagille syndrome [32].
Table 2: Design Strategies and Properties of Gut-Restricted Drugs
| Strategy | Representative Drug | Molecular Weight (Da) | clogP | TPSA (Ų) | Bioavailability | Primary Target |
|---|---|---|---|---|---|---|
| High polarity | Acarbose | 645.6 | -9.0 | 321 | <2% | α-glucosidase |
| Peptidomimetic | ZED1227 | ~500* | N/A | 150 | Low (Caco-2 Papp <10 nm/s) | Tissue transglutaminase |
| Oligopeptide | Larazotide acetate | 851.9 | -2.2 | 301 | Negligible | Zonulin receptor |
| Kinetophore approach | Maralixibat | ~600* | N/A | N/A | Minimal | IBAT/ASBT |
| *Estimated based on structure |
Biological Targets for Gut-Restricted Therapeutics in Neurodegeneration
Gut-restricted drugs can modulate the gut-brain axis by targeting specific processes within the gastrointestinal tract:
Microbiome composition and function can be modulated using non-absorbable prebiotics, antibiotics, or enzyme inhibitors that selectively target specific bacterial taxa or functions [3]. For instance, non-absorbable antibiotics could reduce populations of bacteria producing neurotoxic metabolites, while selectively absorbed prebiotics could promote bacteria producing neuroprotective metabolites [29] [3].
Enteroendocrine cell signaling represents another promising target. Gut-restricted TGR5 agonists or dipeptidyl peptidase-4 (DPP-4) inhibitors can enhance the release of gut hormones such as GLP-1, PYY, and others that indirectly influence brain function through both neural and humoral pathways [29] [32].
Intestinal barrier function is compromised in various neurodegenerative diseases, potentially allowing increased translocation of bacterial products that can trigger systemic and neuroinflammation [29] [3]. Gut-restricted tight junction regulators like larazotide acetate may help restore intestinal barrier integrity, reducing systemic inflammation and its impact on the CNS [32].
Bile acid metabolism is extensively modified by gut bacteria, and bile acid derivatives serve important signaling functions [29]. IBAT inhibitors such as maralixibat block the reabsorption of bile acids in the distal ileum, increasing their delivery to the colon where they can influence the release of gut hormones and potentially modulate the gut-brain axis [32].
Experimental Methodologies for Gut-Brain Axis Research
Investigating the efficacy and mechanisms of gut-restricted therapeutics requires specialized experimental approaches that can elucidate their effects on the gut-brain axis.
In Vitro Permeability and Efficacy Assessment
Caco-2 cell monolayer assays are widely used to predict intestinal absorption. This human colorectal adenocarcinoma cell line spontaneously differentiates into enterocyte-like cells when confluent, forming tight junctions and expressing relevant transporters [32]. The protocol involves:
- Culturing Caco-2 cells on permeable filters until differentiation (typically 21 days)
- Measuring transepithelial electrical resistance (TEER) to confirm barrier integrity
- Applying test compound to the apical (luminal) compartment
- Sampling from the basolateral compartment at timed intervals
- Analyzing drug concentration via LC-MS/MS to calculate apparent permeability (Papp)
Compounds with Papp < 10 × 10⁻⁶ cm/s are generally considered to have low permeability [32].
Enteroendocrine cell models, such as STC-1 and NCI-H716 cell lines, enable investigation of drug effects on gut hormone secretion. These cells respond to nutritional and pharmacological stimuli by secreting GLP-1, PYY, CCK, and other hormones, quantifiable by ELISA [29].
Animal Models and Dosing Strategies
Germ-free (GF) animals raised in completely sterile conditions lack any microorganisms and are indispensable for establishing causal relationships between microbiota and physiological outcomes [29] [3]. These models allow for:
- Investigation of neurodevelopmental and behavioral consequences of complete microbial absence
- Controlled colonization with specific bacterial species or defined communities
- Assessment of microbial transfer from diseased to healthy hosts
Gut-restricted drug administration in animal models requires special consideration to confirm local action. Key methodological aspects include:
- Oral gavage or administration in drinking water/food for gut delivery
- Measurement of plasma and brain drug concentrations to confirm restricted absorption
- Assessment of target engagement in the gut (e.g., hormone secretion, gene expression changes)
- Evaluation of downstream effects on neural function, behavior, and neuropathology
The following diagram illustrates a comprehensive experimental workflow for evaluating gut-restricted therapeutics:
Analysis of Gut-Brain Axis Outcomes
Microbiome analysis using 16S rRNA gene sequencing or shotgun metagenomics provides comprehensive characterization of microbial community structure and functional potential [29] [3]. Fecal samples are collected before, during, and after intervention, with DNA extraction followed by amplification of target regions and high-throughput sequencing.
Metabolomic profiling of feces, serum, and brain tissue using LC-MS or GC-MS enables detection of microbial-derived metabolites (SCFAs, bile acids, tryptophan metabolites) that may mediate gut-brain communication [29] [3].
Neuropathological assessment includes evaluation of microglial activation (Iba1 immunohistochemistry), astrocyte reactivity (GFAP staining), protein aggregation (Aβ, tau, or α-synuclein immunohistochemistry), and neuronal integrity [69] [3]. Behavioral tests relevant to specific neurodegenerative models (e.g., motor function in PD models, memory in AD models) provide functional readouts [3].
BBB integrity assessment involves measuring extravasation of endogenous proteins like albumin or administered tracers (e.g., Evans blue, sodium fluorescein) into the brain parenchyma [69] [70]. Analysis of tight junction protein expression (claudin-5, occludin, ZO-1) via immunohistochemistry or Western blot provides complementary structural information [70].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Gut-Brain Axis Studies
| Category | Reagent/Model | Key Applications | Considerations |
|---|---|---|---|
| Cell Models | Caco-2 cells | Intestinal permeability assessment | Requires 21-day differentiation for full polarization |
| STC-1 enteroendocrine cells | Gut hormone secretion studies | Respond to various secretagogues with hormone release | |
| Primary microglia | Direct effects of microbial metabolites on CNS immune cells | Highly responsive to SCFAs and other bacterial metabolites | |
| Animal Models | Germ-free mice | Establishing causal role of microbiota | Require specialized facilities and procedures |
| Antibiotic-treated mice | Acute microbiota depletion | Confounding effects of antibiotics must be controlled | |
| Transgenic neurodegenerative models (e.g., 5xFAD, APP/PS1) | Disease-specific mechanisms | Variable gut microbiome requires careful monitoring | |
| Analysis Tools | 16S rRNA sequencing | Microbiome community profiling | Limited to taxonomic classification; shotgun metagenomics for functional potential |
| LC-MS/MS platforms | Targeted metabolomics (SCFAs, bile acids, neurotransmitters) | High sensitivity and specificity required for complex biological matrices | |
| ELISA kits (GLP-1, PYY, CCK, cytokines) | Quantification of protein biomarkers | Plasma collection requires protease inhibitors for gut hormones | |
| Chemical Reagents | Short-chain fatty acids (acetate, propionate, butyrate) | Microbial metabolite supplementation | Dose-response important; physiological concentrations in mM range |
| Bile acid derivatives (DCA, LCA, TCA) | Bile acid signaling studies | Differential effects depending on receptor affinity and hydrophobicity | |
| Tight junction modulators (AT-1001) | Intestinal barrier function studies | Confirm localization to gut without systemic effects |
Current Clinical Evidence and Future Directions
Several gut-restricted therapeutics have advanced to clinical development, primarily for gastrointestinal disorders, providing proof-of-concept for this approach [32]. Their potential application in neurodegenerative diseases represents an emerging frontier.
Maralixibat, an IBAT inhibitor, received FDA approval for cholestatic pruritus in Alagille syndrome, demonstrating the clinical viability of gut-restricted approaches [32]. While not yet tested in neurodegenerative trials, its mechanism of influencing bile acid signaling and potentially GLP-1 secretion suggests possible relevance to brain disorders [29] [32].
Larazotide acetate reached Phase III trials for celiac disease, demonstrating the ability to modulate intestinal barrier function in humans [32]. As intestinal permeability is implicated in various neurodegenerative conditions, this approach may have broader applications [29] [3].
Sibofimloc, a FimH blocker, has shown promise in Crohn's disease trials by targeting specific bacterial populations [32]. This precision approach to microbiome modulation could be adapted for neurodegenerative diseases associated with specific microbial alterations [3].
Future directions should focus on developing gut-restricted drugs specifically designed to modulate targets within the gut-brain axis for neurodegenerative diseases. This will require:
- Identification of specific microbial strains and metabolites relevant to each neurodegenerative condition
- Development of more sophisticated animal models that recapitulate both gastrointestinal and neurological aspects of disease
- Advanced formulation technologies to ensure consistent gut-restricted delivery
- Validation of gut-based biomarkers for monitoring target engagement and treatment response
- Adaptive clinical trial designs that account for the personalized nature of microbiome-based interventions
Gut-restricted therapeutics represent a promising strategy for overcoming BBB hurdles in treating neurodegenerative diseases. By targeting the elaborate communication networks of the gut-brain axis, these locally acting compounds can indirectly influence CNS pathology while avoiding the challenges of systemic drug delivery and BBB penetration. The continued development of this approach requires interdisciplinary collaboration between gastroenterologists, neuroscientists, microbiologists, and pharmaceutical chemists. As our understanding of the microbiota-gut-brain axis in neurodegeneration deepens, gut-restricted therapeutics may emerge as a viable component of comprehensive treatment strategies for these currently intractable conditions.
Within the broader thesis on the gut-brain axis's role in neurodegenerative disease research, the development of objective biomarkers is a critical frontier. The microbiota-gut-brain axis (MGBA) represents a complex, bidirectional communication network linking the central nervous system with the gastrointestinal tract through neural, immune, endocrine, and metabolic pathways [2]. Disruptions in this axis, manifesting as gut dysbiosis, are increasingly implicated in the pathogenesis of neurodegenerative diseases (NDDs) such as Alzheimer's disease (AD) and Parkinson's disease (PD) [2] [8]. This technical guide outlines the core principles and methodologies for identifying microbial and metabolomic signatures from the gut microbiome, with the ultimate goal of creating a robust framework for patient stratification in clinical practice and therapeutic development. Such stratification is essential for enabling personalized medicine approaches, potentially predicting disease risk, tracking progression, and evaluating responses to microbiome-targeted interventions [72].
The Gut-Brain Axis and Its Role in Neurodegeneration
The MGBA comprises several key components: the gut microbiota, the intestinal barrier, the enteric nervous system (ENS), the vagus nerve, and central nervous system (CNS) structures like the blood-brain barrier (BBB) and microglia [2]. Communication along this axis occurs through several core pathways:
- Neural Pathways: The vagus nerve serves as a direct neural highway, with afferent fibers relaying gut signals to the brainstem and efferent fibers modulating gut function. Gut microbes can influence this pathway by producing neurotransmitters like GABA, serotonin, and histamine [2].
- Immune and Inflammatory Pathways: Gut dysbiosis can compromise the intestinal barrier, allowing microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS), to enter circulation. This can trigger systemic inflammation and activate microglia in the brain, leading to chronic neuroinflammation [2].
- Metabolite-Mediated Pathways: Gut microbes produce a range of metabolites that can enter the bloodstream and influence brain function. Key metabolites include short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate (which have anti-inflammatory effects and support blood-brain barrier integrity), as well as tryptophan derivatives and bile acids [2] [8].
- Neuroendocrine Pathways: The hypothalamic-pituitary-adrenal (HPA) axis, activated by stress, releases hormones like cortisol that can alter gut permeability and microbiota composition, creating a feedback loop [2].
These pathways provide the mechanistic basis for how gut-derived signals can contribute to protein misfolding, neuroinflammation, and neuronal damage—hallmarks of NDDs. The following diagram illustrates these core communication routes.
Diagram 1: Core Signaling Pathways of the Microbiota-Gut-Brain Axis. This diagram visualizes the primary communication routes (Neural, Immune, Metabolic, Neuroendocrine) through which gut microbiota influence brain health and pathology. MAMPs: Microbe-Associated Molecular Patterns; SCFAs: Short-Chain Fatty Acids; HPA: Hypothalamic-Pituitary-Adrenal.
Microbial and Metabolomic Signatures in Neurodegenerative Diseases
Extensive research has identified distinct, and sometimes overlapping, alterations in the gut microbiome and metabolome across different NDDs. The table below summarizes key signatures associated with major neurodegenerative conditions, which serve as the foundation for biomarker development.
Table 1: Key Microbial and Metabolomic Signatures in Major Neurodegenerative Diseases
| Disease | Reported Microbial Shifts (vs. Healthy) | Key Metabolomic Alterations | Potential Functional Impact |
|---|---|---|---|
| Alzheimer's Disease (AD) | Reduced diversity; Depletion of SCFA-producers (e.g., Lachnospiraceae); Enrichment of pro-inflammatory taxa [2] [8] [72]. | Decreased SCFAs (butyrate); Altered bile acids; Changes in tryptophan metabolism [2] [73]. | Increased neuroinflammation; Impaired BBB integrity; Reduced synaptic plasticity [2]. |
| Parkinson's Disease (PD) | Lower abundance of Prevotellaceae and Lachnospiraceae; Higher abundance of Enterobacteriaceae and Akkermansia [72]. | Reduced SCFAs; Increased fecal SCFAs in some studies (constipation-related); Altered bacterial neurotransmitters [2]. | GI dysfunction (constipation); Aggravation of α-synuclein pathology via inflammation; Vagal nerve transmission [2] [72]. |
| Multiple Sclerosis (MS) | Specific alterations include bacteria that drive Th17 cell expansion (e.g., segmented filamentous bacteria) [2]. | Reduced SCFAs [2] [8]. | Loss of immune tolerance; Promotion of pro-inflammatory Th17 cells; Demyelination [2]. |
| Amyotrophic Lateral Sclerosis (ALS) | Patterns of dysbiosis reported, though specific taxa vary; Reduced microbial diversity common [72]. | Information less defined; SCFA alterations suspected based on shared mechanisms [8]. | Systemic & CNS inflammation; Potential impact on glial function and motor neuron survival [8]. |
A 2024 meta-analysis of clinical trials further supports the functional relevance of these signatures, demonstrating that microbiome-modulating interventions (e.g., probiotics, prebiotics, FMT) not only alter GM composition but also lead to a significant improvement in overall disease burden (SMD: -0.57; 95% CI: -0.93 to -0.21) [72].
Methodologies for Signature Identification and Validation
The pipeline for discovering and validating microbial and metabolomic biomarkers requires a multi-omics approach and rigorous experimental design.
Core Analytical Workflows
The journey from sample collection to a validated biomarker signature involves a structured, multi-stage process, as outlined below.
Diagram 2: Biomarker Development Workflow. This diagram outlines the key stages from initial sample collection to the clinical application of a validated microbial or metabolomic signature.
Experimental Protocol 1: Longitudinal Cohort Study for Biomarker Discovery
- Objective: To identify and validate gut microbial and metabolomic signatures that predict disease progression or therapeutic response in a specific NDD (e.g., Alzheimer's disease).
- Patient Cohort:
- Recruit a large, well-characterized cohort including patients with the NDD, individuals with prodromal symptoms, at-risk individuals, and matched healthy controls.
- Collect extensive metadata: diet, medication, comorbidities, lifestyle, and detailed clinical/cognitive scores (e.g., MMSE for AD, UPDRS for PD).
- Sample Collection (Stage 1):
- Primary Sample Type: Fecal samples, collected using standardized home kits, immediately frozen at -20°C or -80°C.
- Additional Biospecimens (for correlation and multi-omics integration): Blood plasma/serum for host metabolomics and inflammatory markers; CSF when ethically and clinically feasible for direct CNS biomarker correlation.
- Multi-Omics Data Generation (Stage 2):
- Microbiome Analysis:
- 16S rRNA Gene Sequencing: For cost-effective profiling of microbial community structure and diversity. Protocol: DNA extraction using dedicated kits (e.g., QIAamp PowerFecal Pro DNA Kit) -> Amplification of the 16S V3-V4 hypervariable region -> Sequencing on Illumina MiSeq/HiSeq platform -> Processing with QIIME 2 or Mothur.
- Shotgun Metagenomic Sequencing: For high-resolution taxonomic profiling and functional potential analysis (identification of microbial genes and pathways). Protocol: Library preparation from total DNA -> High-depth sequencing on Illumina NovaSeq -> Analysis with tools like HUMAnN3 and MetaPhlAn.
- Metabolomic Analysis:
- Liquid Chromatography-Mass Spectrometry (LC-MS): For broad, sensitive detection of a wide range of metabolites (e.g., SCFAs, bile acids, tryptophan metabolites) in fecal and plasma samples. Protocol: Metabolite extraction (e.g., methanol:water) -> Reverse-phase/UHPLC separation -> High-resolution MS detection (e.g., Q-TOF) -> Data processing with XCMS, Progenesis QI.
- Microbiome Analysis:
- Bioinformatics and Integration (Stage 3):
- Microbiome Data: Alpha/Beta-diversity analysis; Differential abundance testing (DESeq2, LEfSe); Phylogenetic investigation.
- Metabolomics Data: Peak alignment, normalization, multivariate statistics (PCA, PLS-DA), and pathway analysis (MetaboAnalyst).
- Integration: Use multi-omics integration tools (e.g., MixOmics, MMINP) to find correlations between microbial features and metabolomic shifts, creating a unified signature.
Experimental Protocol 2: Interventional Trial for Signature Validation
- Objective: To validate if an identified signature can serve as a pharmacodynamic biomarker by tracking response to a microbiome-targeted intervention.
- Design: Randomized, double-blind, placebo-controlled trial (RCT).
- Intervention Arm: Prebiotic (e.g., inulin), probiotic (e.g., specific Lactobacillus/Bifidobacterium strains), synbiotic, or FMT.
- Control Arm: Placebo.
- Sampling Timeline: Collect fecal and blood samples at baseline (pre-intervention), mid-intervention, end-of-treatment, and during a follow-up period.
- Analysis: Apply the previously defined microbial/metabolomic signature model to the samples from the trial. A successful validation is demonstrated by a significant shift in the signature score in the intervention arm towards a "healthier" state, correlated with improvements in clinical outcomes (e.g., cognitive scores, motor function).
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Gut-Brain Axis Biomarker Studies
| Category / Item | Specific Examples | Function & Application |
|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro DNA Kit, DNeasy PowerSoil Kit | Standardized, efficient lysis of microbial cells and purification of high-quality DNA from complex fecal samples for sequencing. |
| 16S rRNA Sequencing | Illumina MiSeq Reagent Kit v3, primers targeting V3-V4 region | Amplicon-based profiling of bacterial community composition and structure. |
| Shotgun Metagenomics | Illumina DNA Prep, NovaSeq 6000 S-Prime Reagent Kit | Comprehensive analysis of all genetic material in a sample, enabling strain-level taxonomy and functional pathway prediction. |
| Metabolomics Platforms | UHPLC coupled to Q-TOF Mass Spectrometer (e.g., Agilent 6546 LC/Q-TOF) | Untargeted profiling of a wide array of small molecule metabolites in fecal, serum, and CSF samples. |
| SCFA Analysis | GC-MS/FID systems, commercial SCFA standard mixtures | Targeted, quantitative measurement of key microbial metabolites (acetate, propionate, butyrate) with high sensitivity. |
| Cell-Based Assays | Caco-2 cell lines, SH-SY5Y cell lines, primary microglia | Modeling the gut barrier (Caco-2), neurons (SH-SY5Y), and neuroinflammation (microglia) to test the functional impact of microbial metabolites. |
| Gnotobiotic Models | Germ-free C57BL/6 mice | Causality testing; colonizing germ-free mice with defined human microbial communities to study their specific effects on neuropathology. |
The development of microbial and metabolomic signatures for patient stratification represents a paradigm shift in neurodegenerative disease research. By leveraging the accessible and information-rich reservoir of the gut microbiome, researchers can move beyond a one-size-fits-all approach. The path forward requires a concerted effort to standardize methodologies, increase the scale and longitudinal design of human studies, and embrace sophisticated data integration tools. Success in this endeavor will not only refine our understanding of the gut-brain axis but also deliver the practical tools needed for precision neurology, ultimately accelerating the development of effective microbiome-targeted therapies for devastating neurodegenerative conditions.
Standardization Hurdles in FMT and Probiotic Manufacturing for Clinical Trials
The microbiota-gut-brain axis represents a paradigm shift in neurodegenerative disease research, unveiling a complex, bidirectional communication network between the gastrointestinal tract and the central nervous system [3]. This axis integrates neural, immune, endocrine, and metabolic pathways, with the gut microbiota playing a pivotal role in regulating glial function, neuroinflammation, and the integrity of the blood-brain barrier [3] [20]. For neurodegenerative conditions such as Alzheimer's disease (AD) and Parkinson's disease (PD), targeting this axis offers a promising therapeutic frontier. Fecal Microbiota Transplantation (FMT) and specific probiotic interventions have demonstrated potential to modify disease course by rectifying microbial dysbiosis [74].
However, the translation of these promising approaches from bench to bedside is severely hampered by a lack of standardization in their manufacture and preparation. For the gut-brain axis research to yield reliable, reproducible clinical interventions, it is imperative that the biological products used—whether complex fecal communities or defined probiotic strains—are consistent, well-characterized, and safe. This technical guide delves into the specific standardization hurdles in FMT and probiotic manufacturing for clinical trials, providing a roadmap for researchers and drug development professionals to navigate these challenges.
Standardization Challenges in Fecal Microbiota Transplantation (FMT)
FMT, the transfer of processed fecal material from a healthy donor to a patient, is one of the most advanced microbiome-based therapies. Its application in gut-brain axis research, however, is fraught with manufacturing and regulatory complexities.
Donor Screening and Biobanking: A Moving Target
The foundation of a safe FMT product is rigorous donor screening. The core challenge is the evolving nature of safety threats, which necessitates continuously updated screening protocols.
- Dynamic Safety Threats: A seminal FDA safety alert in 2019 was issued after two immunocompromised adults acquired extended-spectrum beta-lactamase (ESBL) producing Escherichia coli from FMT, resulting in one fatality [75]. This highlighted the critical need for screening and testing donors for multi-drug resistant organisms (MDROs). Subsequently, the COVID-19 pandemic introduced new risks, as SARS-CoV-2 viral RNA was detected in feces, prompting the FDA to recommend testing donors and donor stool for the virus [75]. This illustrates a fundamental hurdle: screening protocols must be agile enough to respond to emerging pathogens.
- Logistical and Economic Burdens: The additional testing for MDROs and emerging pathogens is often expensive, difficult to access, and may not be certified through Clinical Laboratory Improvement Amendments (CLIA), creating significant barriers for clinical trial operations [75].
Material Processing and Formulation
A critical hurdle is the lack of a standardized, validated process for converting raw fecal material into a defined, consistent therapeutic.
- Preservation of Functionality: A key scientific challenge is identifying the best processing methods (e.g., fresh vs. frozen, lyophilized) to preserve the critical functionalities of the intestinal ecosystem. Different methods may variably affect microbial viability and the integrity of microbial metabolites, which are crucial for efficacy in gut-brain axis modulation [76].
- Formulation and Delivery: The route of administration (e.g., colonoscopy, nasoduodenal tube, oral capsules) can impact engraftment success and patient acceptability. A large multi-center pediatric study found that oral capsules were used in only 3.8% of FMT procedures, and enemas in 1.1%, suggesting that the routes most feasible for widespread use are less common in practice [75]. Developing formulations that are both stable and amenable to preferred delivery routes remains a significant technical challenge.
Regulatory Heterogeneity
The regulatory landscape for FMT is fragmented globally, creating a major hurdle for multi-center clinical trials.
Table 1: Global Regulatory Classification of FMT
| Region/Country | Regulatory Classification | Implications for Clinical Trials |
|---|---|---|
| United States | For recurrent C. difficile infection (rCDI): Informed consent. For other indications (e.g., neurodegenerative diseases): Investigational New Drug (IND) [76]. | Creates a dual pathway; trials for gut-brain axis applications require full IND compliance, increasing complexity and cost. |
| Europe | Varies by member state. Most classify FMT as a drug, but some, like Finland, regulate it as a therapeutic intervention, and Italy as tissue [76]. | Prevents a harmonized trial protocol across the EU, leading to significant underuse (covering only ~10% of rCDI patients) [76]. |
| Australia | Approved as a listed biological drug for gastrointestinal disorders [76]. | Provides a clearer, centralized pathway for development and approval. |
| Canada | Classified as a biological drug [76]. | Subjects FMT to stringent pharmaceutical requirements. |
This lack of harmonization means that a manufacturing process and trial protocol acceptable in one country may not be valid in another, stifling global research efforts on the gut-brain axis.
Standardization Hurdles in Probiotic Manufacturing
While often perceived as simpler than FMT, the manufacturing of probiotics for clinical investigations faces its own set of rigorous standardization challenges, particularly when destined for vulnerable populations such as patients with neurodegenerative diseases.
Strain Characterization and Genetic Stability
The foundation of probiotic safety and efficacy is a thorough understanding of the microbial strain's genetic makeup.
- Essential of Whole Genome Sequencing (WGS): WGS is considered a cornerstone for assessing probiotic safety [77]. It allows for:
- Strain-Level Identification: Crucial for tracking the strain during production and in post-market surveillance.
- Detection of Genes of Concern: The genome can be interrogated for virulence factors, toxin genes, and antibiotic resistance (AR) genes [77].
- Horizontal Gene Transfer (HGT): A significant theoretical risk is the in vivo transfer of AR genes from a probiotic strain to resident gut pathogens via conjugation. While documented in laboratory settings, the clinical and public health implications of such transfer are still being evaluated, necessitating careful genetic screening and phenotypic testing [77].
Product Quality and Contamination Control
Probiotics are live microbial agents, which dictates a unique set of quality control challenges.
- Purity, Potency, and Composition: The final product must be tested to ensure it is free from unwanted microbial contaminants, contains the advertised quantity of live microbes (potency), and its composition matches what was declared [77].
- Tailored Testing for Vulnerable Populations: Testing specifications must be tailored for the intended use. Probiotics destined for clinical trials involving patients with neurodegenerative diseases—who may be older and have compromised barriers—should undergo more stringent testing than those for the general healthy population [77].
The "Biotherapeutics" Transition and the Pediatric Dilemma
A promising development is the shift from loosely regulated probiotics to defined live biotherapeutic products (LBPs), which are subject to full drug approval pathways. SER-109 (an oral capsule of bacterial spores) and RBX2660 (a microbial suspension) are examples that have undergone Phase III trials for rCDI [75].
However, this transition creates a specific access dilemma. While these biotherapeutics may soon be available for adults, their approval for pediatric populations is expected to be significantly delayed due to a lack of pediatric clinical trials [75]. This is particularly relevant for early-onset neurodegenerative conditions, leaving children without access to these more standardized products and forcing providers to rely on less regulated FMT or probiotics.
Experimental Protocols for Standardization
To overcome these hurdles, implementing rigorous, standardized experimental protocols is non-negotiable.
Protocol for FMT Donor Screening and Material Preparation
This protocol outlines a comprehensive workflow for creating standardized FMT material for clinical trials.
FMT Preparation and Screening Workflow
Step 1: Donor Recruitment and Initial Screening
- Questionnaire: Administer a detailed questionnaire covering medical history (e.g., immunosuppression, GI disorders, neurological conditions), travel history to regions with endemic pathogens, antibiotic use within the past 3-6 months, and high-risk behaviors [75] [76].
- Informed Consent: Obtain informed consent detailing the donation process, testing procedures, and potential for disqualification.
Step 2: Comprehensive Blood and Stool Testing
- Blood Tests: Screen for HIV, Hepatitis A, B, and C, Treponema pallidum (syphilis).
- Stool Tests: Multiplex PCR or culture for enteric pathogens (Salmonella, Shigella, Campylobacter, E. coli O157, Yersinia, C. difficile). Microscopy for ova and parasites.
- MDRO Screening: Specific testing for ESBL-producing Enterobacteriaceae, Vancomycin-Resistant Enterococci (VRE), Carbapenem-resistant Enterobacteriaceae (CRE) [75].
- Viral Screening: Test for SARS-CoV-2, and other relevant enteric viruses (e.g., Norovirus) as per current guidelines [75].
Step 3: Stool Processing and Biobanking
- Processing under Anaerobic Conditions: Process fresh stool within a short time window (e.g., 2-6 hours of passage) in an anaerobic chamber or using closed systems to preserve obligate anaerobes.
- Standardized Dilution: Use a consistent weight/volume ratio of stool to cryoprotectant (e.g., sterile saline with 10-15% glycerol).
- Homogenization and Filtration: Homogenize thoroughly and filter through coarse filters to remove particulate matter.
- Aliquoting and Storage: Aliquot into single-use portions and store at -80°C.
Step 4: Pre-Release Quality Control
- Final Safety Test: Perform a final test on a representative aliquot from the processed batch for MDROs and other emergent pathogens immediately before release.
- Viability Testing: Quantify viable bacterial counts via flow cytometry or culture-based methods to ensure potency.
Protocol for Probiotic Safety and Quality Assessment
This protocol provides a framework for the characterization and quality control of probiotic strains intended for clinical trials.
Probiotic Strain Characterization Workflow
Step 1: Genomic Characterization
- Whole Genome Sequencing (WGS): Perform WGS using an Illumina or PacBio platform to achieve high-quality, contiguous genome assembly.
- Bioinformatic Analysis:
- Taxonomic Assignment: Confirm species and strain identity.
- Safety Assessment: Interrogate the genome for:
- Antibiotic Resistance Genes: Using databases like CARD (Comprehensive Antibiotic Resistance Database).
- Virulence Factors: Using databases like VFDB (Virulence Factor Database).
- Toxin Genes: Assess potential for toxin production.
- Strain Tracking: Identify unique genetic markers for tracking the strain in complex environments like the human gut.
Step 2: Phenotypic Confirmation
- Antibiotic Susceptibility Testing (AST): Perform broth microdilution or agar dilution methods following relevant guidelines (e.g., EFSA or CLSI, where applicable) to confirm the phenotypic resistance profile matches genetic predictions [77].
- Metabolite Production: Validate the production of claimed beneficial metabolites (e.g., SCFAs, neurotransmitters like GABA).
Step 3: cGMP Manufacturing and Quality Control
- Manufacturing under cGMP: Produce the clinical trial lot in a facility following current Good Manufacturing Practices (cGMP).
- In-Process and Release Testing:
- Identity: Confirm identity via PCR or other molecular methods.
- Purity: Test for absence of contaminants (other bacteria, fungi, mycoplasma).
- Potency: Quantify the number of live colony-forming units (CFU) per dose.
- Viability Over Shelf-Life: Conduct real-time and accelerated stability studies to define storage conditions and expiration dates.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for implementing the standardized protocols described above.
Table 2: Key Research Reagent Solutions for Microbiome Therapeutic Manufacturing
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Cryoprotectants (e.g., Glycerol) | Preserves microbial viability during freezing and long-term storage of FMT material and probiotic strains. | Typically used at 10-15% (v/v) final concentration in a sterile solution. |
| Anaerobic Chamber/Workstation | Provides an oxygen-free environment for processing FMT material or cultivating anaerobic gut bacteria, critical for preserving obligate anaerobes. | Maintains an atmosphere of ~85% N₂, 10% CO₂, 5% H₂. |
| Whole Genome Sequencing Kits | For library preparation and sequencing of probiotic strains to fulfill genetic characterization requirements. | Kits from providers like Illumina (Nextera) or PacBio are standard. |
| Bioinformatic Databases (CARD, VFDB) | Used in silico to analyze WGS data for the presence of antibiotic resistance and virulence genes. | Critical for the initial safety assessment of a probiotic strain. |
| Selective Culture Media | Used for MDRO screening in FMT donor stool (e.g., CHROMagar ESBL, VRE agar) and for purity testing of probiotic products. | Allows for selective growth and preliminary identification of resistant pathogens. |
| cGMP Production Facility | A dedicated, regulated facility for the manufacture of probiotic clinical trial materials, ensuring product consistency, purity, and potency. | Essential for the production of Live Biotherapeutic Products (LBPs) destined for Phase II/III trials. |
The pursuit of microbiome-based interventions for neurodegenerative diseases via the gut-brain axis stands at a critical juncture. The therapeutic potential of FMT and probiotics is immense, yet its realization is entirely contingent on our ability to overcome the significant standardization hurdles detailed in this guide. The path forward requires a concerted, collaborative effort. Researchers and clinicians must advocate for and adopt the stringent protocols for donor screening, material processing, and strain characterization. Industry partners must invest in the cGMP manufacturing and advanced analytics required to produce reliable, well-defined biotherapeutics. Finally, regulatory agencies must work towards greater global harmonization, creating clear and feasible pathways that encourage innovation while ensuring patient safety. By systematically addressing these challenges in manufacturing and regulation, we can unlock the full potential of the gut-brain axis and deliver on the promise of novel therapeutics for neurodegenerative diseases.
Longitudinal Study Design to Capture Slow Disease Progression and Intervention Effects
In neurodegenerative disease research, the slow, non-linear progression of conditions like Alzheimer's disease (AD) and Parkinson's disease (PD) presents a fundamental methodological challenge. Understanding this progression is critical for timing therapeutic interventions and designing effective clinical trials [78]. Longitudinal study designs, which measure outcomes repeatedly over time, are uniquely positioned to capture these temporal dynamics, offering significant advantages over cross-sectional approaches through reduced variability and increased statistical power [78].
This technical guide frames longitudinal methodology within the emerging context of the gut-brain axis (MGBA)—the bidirectional communication network linking intestinal microbiota with the central nervous system through immune, neural, endocrine, and metabolic pathways [2]. Dysregulation of this axis is increasingly implicated in the onset and progression of neurodegenerative diseases, suggesting that gut-derived biomarkers and interventions may represent promising new targets for therapeutic development [9] [20]. The integration of MGBA hypotheses into longitudinal frameworks creates new opportunities and challenges for study design, requiring sophisticated approaches to model complex, multi-system interactions over time.
Core Statistical Methodologies for Longitudinal Analysis
Analyzing longitudinal data in neurodegenerative studies is complicated by correlated data, irregularly timed visits, missing data, and mixtures of time-varying and static covariate effects [78]. Several statistical approaches have been developed to address these challenges, each with distinct strengths and limitations.
Table 1: Comparison of Statistical Methods for Longitudinal Data Analysis
| Method | Number of Time Points | Handles Irregular Timing | Time-Varying Predictors | Missing Data Mechanism | Correlation Modeling |
|---|---|---|---|---|---|
| Change Score Analysis | Only 2 | No | Not allowed | Requires complete data; yields unbiased estimates only if Missing Completely at Random (MCAR) | Not applicable |
| Repeated Measures ANOVA | Multiple | No | Time treated as classification variable | Complete-case analysis; unbiased only if MCAR | Assumes equal variances and covariances over time (compound symmetry) |
| Generalized Estimating Equations (GEE) | Multiple | Yes | Allowed | MCAR | "Working" correlation models (independent, exchangeable, autocorrelation, unstructured) |
| Mixed Effect Regression (MER) | Multiple | Yes | Allowed | Missing at Random (MAR) | Random effects quantify variation among units and describe cluster-specific trends |
Among these methods, mixed effect models (MER) are the most flexible for neurodegenerative disease studies, as they explicitly model individual trajectories (random effects) while estimating population-level trends (fixed effects) [78]. The FDA prefers MER for observational and clinical studies because they accommodate irregular timing, model complex correlation structures, and provide valid inference under the more realistic MAR assumption (where missingness depends on observed data) rather than the stricter MCAR assumption (where missingness is independent of both observed and unobserved data) [78].
For example, in a Huntington's disease (HD) study measuring Total Motor Scores (TMS) annually over 10 years, an MER model can estimate individual progression curves while accounting for site-specific effects (in multi-site studies), baseline covariates (e.g., CAG-Age Product score), and time-varying predictors (e.g., medication use) [78].
Disease Progression Modeling and Biomarker Integration
Data-driven disease progression models are computational tools that reconstruct long-term disease timelines from short-term observational data [79]. Unlike traditional 'black box' machine learning, these models are inherently interpretable, combining a priori knowledge with large-scale data processing to estimate the temporal sequence of biomarker changes and clinical manifestations.
These models have revealed substantial heterogeneity in progression pathways across neurodegenerative diseases. In multiple sclerosis, for instance, progression models applied to MRI data have identified three distinct subtypes with different disability progression and treatment responses [79]. Such stratification is crucial for precision medicine and enriched clinical trial design.
Table 2: Key Biomarker Categories in Neurodegenerative Disease Progression Modeling
| Biomarker Category | Examples | Role in Disease Progression | Relevance to Gut-Brain Axis |
|---|---|---|---|
| Neuroimaging | MRI (atrophy patterns), Amyloid-PET, Tau-PET | Quantifies regional brain changes, protein deposition | Potential to visualize effects of gut-derived inflammatory mediators on brain structure |
| Fluid Biomarkers | CSF Aβ42, p-tau, NFL; Plasma p-tau217, GFAP | Tracks core pathological processes and neuronal injury | Gut microbiome influences systemic inflammation measurable in peripheral fluids |
| Clinical Assessments | ADAS-Cog, MMSE, UHDRS TMS | Measures cognitive, motor, and functional decline | Gastrointestinal symptoms often precede classical neurological symptoms |
| Microbiome-Derived | Microbial diversity, SCFA levels, bile acid profiles | Emerging markers of gut ecosystem status and functional output | Direct measurement of MGBA components; potential for early warning biomarkers |
Biomarkers play multiple critical roles in longitudinal studies: patient stratification, prognosis, tracking progression, and treatment monitoring [80]. The inclusion of biomarkers has enabled selective participant recruitment, improved treatment monitoring, and supported more rigorous trial designs in Alzheimer's disease, as evidenced by the recent approval of anti-amyloid antibodies [80].
Incorporating the Gut-Brain Axis into Longitudinal Designs
The microbiota-gut-brain axis (MGBA) represents a paradigm shift in neurodegenerative disease research, with gastrointestinal disturbances frequently appearing years before classic neurological symptoms [2]. For example, chronic constipation can precede PD motor symptoms by up to 20 years, and distinct gut microbiota profiles have been identified in AD patients compared to healthy controls [2]. This extended prodromal phase creates both challenges and opportunities for longitudinal study design.
Key Mechanisms and Measurement Approaches
The MGBA communicates through multiple interdependent pathways that should be considered in longitudinal studies:
Neural Pathways: The vagus nerve provides direct neural connectivity between gut and brainstem. Microbial metabolites (GABA, serotonin, histamine) can activate vagal afferents [2]. In PD, misfolded α-synuclein aggregates may originate in the gut and spread to the brain via vagal fibers [2].
Immune and Inflammatory Pathways: Gut dysbiosis can compromise intestinal barrier integrity, allowing microbial-associated molecular patterns (MAMPs) like LPS to enter circulation, triggering systemic inflammation that can activate brain microglia via TLR4/NF-κB signaling [2]. Gut-resident T cells conditioned by microbiota can traffic to the CNS [2].
Metabolic Pathways: Gut microbes ferment dietary fiber into short-chain fatty acids (SCFAs—butyrate, acetate, propionate) that have profound effects on neuroinflammation, blood-brain barrier integrity, and microglial function [2] [20]. Butyrate, for instance, has been shown to support BBB integrity and reduce neuroinflammation [20].
Experimental Protocols for MGBA Assessment in Longitudinal Studies
Comprehensive Microbiome Sampling Protocol:
- Sample Collection: Collect fecal samples at each study visit using standardized kits (e.g., DNA/RNA Shield Fecal Collection tubes). Immediately freeze at -80°C.
- DNA Extraction: Use bead-beating mechanical lysis protocols (e.g., QIAamp PowerFecal Pro DNA Kit) to ensure efficient extraction from Gram-positive bacteria.
- Sequencing: Perform 16S rRNA gene sequencing (V4 region) for community profiling or shotgun metagenomics for strain-level resolution and functional potential.
- Bioinformatic Analysis: Process using QIIME2 or mothur; analyze diversity (alpha/beta), composition, and predicted metagenomic functions (PICRUSt2).
- Metabolite Validation: Correlate microbial findings with SCFA measurements (by GC-MS) in matched fecal and serum samples.
Intestinal Permeability Assessment:
- Dual Sugar Test: Administer lactulose (non-metabolizable) and mannitol (small probe) orally; measure 0-5h urinary excretion by HPLC-MS.
- Biomarker Analysis: Measure plasma zonulin, lipopolysaccharide-binding protein (LBP), and intestinal fatty acid-binding protein (I-FABP) by ELISA.
- Frequency: Baseline and annually, or more frequently if investigating acute intervention effects.
Peripheral Immune Profiling:
- Flow Cytometry: Comprehensive immunophenotyping of peripheral blood mononuclear cells (PBMCs) for activation markers and trafficking receptors.
- Cytokine Analysis: Multiplex assays (Luminex) to quantify pro-inflammatory (IL-6, TNF-α, IL-1β) and anti-inflammatory (IL-10) cytokines in plasma.
- Frequency: Baseline, 3 months (for early intervention effects), and annually.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Gut-Brain Axis Studies
| Reagent/Material | Function | Example Applications |
|---|---|---|
| DNA/RNA Shield Fecal Collection Tubes | Stabilizes microbial nucleic acids at room temperature | Preserves accurate microbiome profiles during sample transport and storage |
| 16S rRNA Gene Primers (e.g., 515F/806R for V4 region) | Amplifies conserved bacterial gene for community profiling | Taxonomic characterization of gut microbiota in response to interventions |
| SCFA Standard Mixtures | Quantification of short-chain fatty acids by GC-MS | Measurement of key microbial metabolites in fecal and serum samples |
| Zonulin ELISA Kits | Measures protein regulating intestinal tight junctions | Assessment of gut barrier integrity in neurodegenerative disease cohorts |
| Lipopolysaccharide (LPS) Assays | Detects bacterial endotoxin in circulation | Quantification of microbial translocation and systemic immune activation |
| Human Cytokine Multiplex Panels | Simultaneous measurement of multiple inflammatory mediators | Comprehensive immune profiling in longitudinal intervention studies |
| Gnotobiotic Mouse Models | Enables studies with defined microbial communities | Causal investigation of specific bacterial strains in disease pathogenesis |
Application to Clinical Trial Design and Drug Development
Disease progression models (DPMs) have become valuable tools in drug development, integrating mathematical functions with pathophysiological principles to quantitatively describe disease time courses [81]. These models normally contain three essential elements for drug development: (1) a model of the natural progression of the disease, (2) a model of the drug's effects on biomarkers or clinical endpoints, and (3) a model linking biomarkers to clinical outcomes [81].
DPMs informed by gut-brain axis research can significantly enhance clinical trial design:
Patient Enrichment Strategies: Identifying specific microbiota signatures or gut permeability markers associated with rapid progression allows for enrichment of trials with patients most likely to show treatment effects within the trial period [2] [81].
Endpoint Selection: MGBA-derived biomarkers (e.g., SCFA levels, inflammatory markers) may serve as sensitive early endpoints for proof-of-concept trials, potentially detecting intervention effects before changes in traditional cognitive or motor scales [9].
Personalized Medicine Approaches: Understanding how interindividual variability in gut microbiome composition affects treatment response enables development of personalized intervention strategies and microbiome-based treatment matching [2] [20].
Longitudinal study design for capturing slow neurodegenerative disease progression requires sophisticated statistical approaches, multidimensional biomarker integration, and consideration of emerging biological frameworks like the gut-brain axis. Mixed effect models provide the most flexible framework for analyzing longitudinal data with its inherent challenges of correlation, irregular timing, and missing data [78]. The integration of MGBA mechanisms into these studies offers promising new avenues for understanding disease heterogeneity, identifying early biomarkers, and developing targeted interventions.
As research progresses, longitudinal designs incorporating multi-omics approaches, frequent sampling protocols, and data-driven progression models will be essential to unravel the complex temporal relationships between gut ecosystem dynamics and central nervous system pathology. This integrated approach holds significant promise for advancing both our fundamental understanding of neurodegenerative diseases and the development of effective, targeted therapeutics.
Evaluating Therapeutic Efficacy: Pre-clinical Models and Clinical Trial Outcomes
The gut-brain axis represents a complex, bidirectional communication network that integrates gastrointestinal tract function with central nervous system (CNS) signaling. This axis involves neural pathways, immune mediators, endocrine signals, and microbial metabolites, creating a vital interface between the gut's microbial community and brain health [82] [3]. Growing evidence implicates dysregulation of this axis in the pathogenesis of various neurodegenerative diseases, making it a critical area for investigative research. Animal models that manipulate this axis—particularly germ-free animals and transgenic models of proteinopathy—have become indispensable tools for deciphering the mechanistic links between gut microbiota and brain pathology.
The study of proteinopathies, neurodegenerative conditions characterized by aberrant protein aggregation in the CNS, has been revolutionized by these models. Alzheimer's disease (tau and Aβ aggregates), Parkinson's disease (α-synuclein aggregates), and amyotrophic lateral sclerosis (TDP-43 aggregates) represent major proteinopathies whose potential gut-initiated pathogenesis can now be systematically investigated [3] [83] [84]. This technical guide provides an in-depth analysis of germ-free and transgenic model systems, detailing their application, methodologies, and quantitative insights into gut-brain axis contributions to neurodegenerative processes.
Germ-Free Animal Models: Fundamentals and Applications
Model Generation and Core Characteristics
Germ-free (GF) animals are defined as organisms completely devoid of all detectable microorganisms, including bacteria, viruses, fungi, and parasites [82]. The generation and maintenance of these models require stringent protocols:
- Aseptic Cesarean Section: GF rodents are typically derived via cesarean section performed under sterile conditions, preventing microbial exposure during birth [82] [85].
- Isolator Rearing: Immediately after delivery, neonates are transferred to sterile isolators equipped with HEPA-filtered air supply, autoclaved food, water, and bedding [82].
- Continuous Monitoring: Regular microbial screening of body sites and housing environments ensures the sustained germ-free status through culture-dependent and molecular methods [85].
Despite their utility, GF models present significant physiological alterations that must be considered in experimental design. These animals exhibit an enlarged cecum, thinner intestinal villi, reduced epithelial cell renewal, and slower intestinal motility compared to conventionally raised counterparts [82]. Furthermore, they require dietary supplementation with vitamins K and B due to impaired synthesis and absorption [82].
Immune and Neurodevelopmental Consequences
The absence of microbiota in GF animals profoundly impacts systemic and neural immune development, creating both limitations and opportunities for investigating gut-brain signaling:
Table 1: Physiological and Immunological Alterations in Germ-Free Models
| System | Observed Alterations | Functional Consequences |
|---|---|---|
| Systemic Immunity | Underdeveloped gut-associated lymphoid tissue (GALT); reduced IgA+ plasma cells; diminished antimicrobial peptide expression [82] | Compromised response to pathogens; increased infection susceptibility |
| Brain Immunity | Increased numbers of immature microglia; altered morphology and transcriptional markers; reduced responsiveness to immune challenge [82] | Blunted neuroinflammatory responses; impaired defense against CNS infections |
| Intestinal Morphology | Reduced intestinal mass; thinner villi and mucus layers; impaired nutrient absorption [82] | Altered digestive efficiency; requirement for vitamin supplementation |
| Neurodevelopment | Altered blood-brain barrier integrity; changed neurotransmitter levels; modified maturation of neural circuits [82] [86] | Impacts on behavior, stress response, and vulnerability to neuropathology |
These developmental abnormalities highlight a crucial consideration: GF animals do not represent a "normal" physiological state but rather a neuroimmunologically altered system. This limitation necessitates careful interpretation of experimental results, as some observed phenotypes may stem from developmental deficits rather than specific experimental manipulations [82].
Applications in Neurodegenerative Disease Research
GF models have been instrumental in establishing causal relationships between gut microbiota and neurodegenerative processes. Key applications include:
- Microbial Necessity Testing: GF animals can be recolonized with specific microbial communities to assess their necessity for disease development [85].
- Barrier Function Studies: The impact of microbiota on intestinal and blood-brain barrier integrity can be quantified in GF systems [86].
- Immunomodulation Research: GF models allow precise dissection of microbiota-immune system interactions relevant to neuroinflammation [82].
Notably, a 2023 study demonstrated that GF conditions or antibiotic treatment in a tauopathy mouse model (P301S tau transgenic mice) resulted in marked reduction of tau pathology and neurodegeneration, with astrocytes and microglia maintaining a more homeostatic state [86]. This finding directly implicates gut microbiota in tau-driven neurodegeneration through neuroinflammatory mechanisms.
Transgenic Models of Proteinopathy
Modeling Human Proteinopathies in Rodents
Transgenic animal models expressing human disease-associated proteins have become cornerstones of neurodegenerative disease research. These models enable precise investigation of protein aggregation mechanisms and their relationship to gut-brain axis signaling:
Table 2: Transgenic Models of Major Neurodegenerative Proteinopathies
| Model Type | Genetic Features | Key Pathological Features | Applications in GBA Research |
|---|---|---|---|
| ALS-TDP Models | Mutations in TARDBP, C9ORF72, FUS, SOD1 [83] | Phosphorylated TDP-43 aggregates in neurons and glia; microglial activation; oligodendroglial pathology [83] | Quantifying cortical vs. spinal cord pathology; assessing selective vulnerability |
| α-Synuclein Propagation Models | Expression of human α-synuclein; injection of preformed fibrils (PFFs) into gut wall [84] | Gut-to-brain spread of α-syn pathology via vagus nerve; dopaminergic neuron loss; motor deficits [84] | Testing Braak hypothesis of PD; vagus nerve role in pathology spread |
| Tauopathy Models | Expression of mutant human tau (e.g., P301S) [86] | Neurofibrillary tangle formation; neuronal loss; glial activation; cognitive decline [86] | Investigating microbiome-tau pathology interactions |
| Alzheimer Models | APP/PS1 mutations; combination with tau transgenes [87] | Aβ plaque deposition; tau pathology; synaptic loss; neuroinflammation | Exploring microbiome influence on Aβ and tau aggregation |
Quantitative Pathological Assessment
Advanced digital analysis methods have revealed genotype-specific vulnerability patterns in transgenic proteinopathy models. A 2020 quantitative study of motor cortex pathology in ALS models demonstrated that:
- Sporadic ALS-TDP cases exhibited more severe cortical phosphorylated TDP-43 burden and microglial activation compared to C9ORF72-associated ALS (C9-ALS) [83].
- Oligodendroglial TDP-43 pathology was a defining feature across all ALS-TDP genotypes (sporadic, C9-ALS, OPTN, HNRNPA1, TARDBP) [83].
- ALS-FUS and ALS-SOD1 models showed less cortical proteinopathy relative to spinal cord pathology compared to ALS-TDP models, indicating genotype-specific gradients of pathology along the neuroaxis [83].
- Neuronal pTDP-43 aggregates were predominantly found in excitatory neurons, while being rare in GAD67+ and Parvalbumin+ inhibitory interneurons, demonstrating cell-type selective vulnerability [83].
These quantitative approaches provide robust, unbiased assessment of proteinopathy burden that complements traditional histopathological evaluation.
Integrated Experimental Approaches
Gut-to-Brain Proteinopathy Propagation Models
A groundbreaking approach in gut-brain axis research involves modeling the potential gut-initiation of neurodegenerative proteinopathies. Kim et al. (2024) established a paradigm for studying α-synuclein propagation from gut to brain [84]:
- Methodology: Preformed α-synuclein fibrils (PFFs) are injected into the duodenal and pyloric muscular layers of mice.
- Pathology Tracking: α-synuclein pathology progression is monitored via phospho-S129 α-synuclein immunohistochemistry, beginning in the dorsal motor nucleus of the vagus.
- Temporal Spread: Pathology ascends through the brainstem (locus coeruleus) to midbrain (substantia nigra) and limbic regions (amygdala, raphe nuclei).
- Functional Validation: Disease progression correlates with dopaminergic neuron loss and motor/non-motor symptom emergence.
- Pathway Interruption: Truncal vagotomy prevents α-synucleinopathy spread, confirming the vagus nerve as a critical transmission route [84].
This model provides direct experimental support for the Braak hypothesis of Parkinson's disease, which proposes that idiopathic PD may initiate in the gut and spread to the brain via the vagus nerve [84] [88].
Gnotobiotic Colonization Strategies
To overcome the developmental limitations of GF models while maintaining experimental control over microbiota composition, researchers employ gnotobiotic colonization approaches:
- Conventionalization: GF animals are colonized with specific microbial communities at defined developmental timepoints.
- Humanized Microbiome: GF mice receive fecal microbiota transplants from human donors, creating human-relevant microbial ecosystems.
- Pathogen Association: GF animals are monocolonized with specific pathogenic or commensal strains to dissect individual microbial contributions.
- Temporal Control: Inducible colonization systems allow researchers to introduce microbiota at specific disease stages.
These approaches enable causal relationships between specific microbial taxa and proteinopathy progression to be established while controlling for developmental confounds.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Gut-Brain Axis Proteinopathy Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Germ-Free Infrastructure | Flexible film isolators; rigid isolators; HEPA filtration systems; autoclaves [85] | Maintaining axenic conditions throughout lifespan | Regular microbial monitoring essential; specialized training required |
| Transgenic Animal Models | TDP-43 models (TARDBP mutants); α-synuclein models (SNCA mutants, PFF-injected); tauopathy models (P301S, rTg4510) [83] [84] [86] | Studying cell-type and regional vulnerability to protein aggregation | Genetic background effects; variable penetrance; species differences in pathology |
| Pathology Detection Reagents | pTDP-43 antibodies; pS129 α-synuclein antibodies; phospho-tau antibodies (AT8, AT100); p62/SQSTM1 antibodies [83] | Visualizing and quantifying protein aggregates across CNS regions | Fixation-dependent antigen preservation; phosphorylation-specific validation required |
| Microbial Manipulation Tools | Antibiotic cocktails (ampicillin, neomycin, metronidazole, vancomycin); prebiotics (inulin, FOS); probiotic formulations [82] | Depleting or modifying gut microbiota composition | Off-target drug effects; incomplete depletion; potential antibiotic resistance |
| Neural Tracers | Cholera toxin B subunit; Fast Blue; Pseudorabies virus; monosynaptic rabies virus systems [89] | Mapping neural connectivity between gut and brain | Specificity of trans-synaptic spread; potential neurotoxicity at high concentrations |
| Vagus Nerve Manipulation | Subdiaphragmatic vagotomy kits; capsaicin for sensory ablation; vagus nerve stimulation electrodes [84] [88] | Determining vagus nerve role in gut-brain communication | Surgical precision critical; compensatory plasticity may develop over time |
Visualization of Gut-Brain Axis Signaling Pathways
Gut-Brain Axis Communication in Proteinopathies
Experimental Workflow for Integrated Gut-Brain Studies
Integrated Gut-Brain Axis Research Workflow
Germ-free and transgenic proteinopathy models have fundamentally advanced our understanding of gut-brain axis contributions to neurodegenerative diseases. The integration of these approaches has revealed that gut microbiota can influence neuroinflammation, protein aggregation, and selective neuronal vulnerability through multiple interconnected pathways. The emerging paradigm suggests that microbial metabolites, immune activation, and direct neural connectivity via the vagus nerve collectively modulate disease progression.
Future research directions will likely focus on:
- Temporal Dynamics: Defining critical windows during development and disease progression when microbiota exert their greatest influence on proteinopathy.
- Microbial Consortia: Moving beyond single organism studies to define how microbial ecosystems collectively influence neurodegenerative processes.
- Multi-omics Integration: Combining genomics, proteomics, metabolomics, and microbiomics to build comprehensive networks of gut-brain communication.
- Therapeutic Translation: Harnessing mechanistic insights to develop microbiota-targeted interventions for neurodegenerative proteinopathies.
These advanced animal models continue to provide unprecedented insights into the complex relationships between gut microbiota and brain health, offering promising avenues for therapeutic development in currently intractable neurodegenerative conditions.
The therapeutic potential of probiotics and prebiotics extends beyond symptomatic relief to encompass potential disease-modifying effects, particularly within the gut-brain axis framework in neurodegenerative and neuropsychiatric conditions. Current clinical evidence reveals a clear dichotomy: probiotics demonstrate significant symptomatic benefits for conditions like depression and anxiety, while emerging research suggests both probiotics and prebiotics may influence the underlying pathophysiology of neurodegenerative diseases through modulation of neuroinflammation, gut barrier integrity, and protein aggregation. This whitepaper synthesizes the most recent clinical evidence, mechanistic insights, and methodological protocols to guide research and development professionals in leveraging microbiota-targeted interventions for neurological disorders.
The microbiota-gut-brain axis (MGBA) represents a complex, bidirectional communication network connecting the gastrointestinal tract with the central nervous system (CNS) through neural, immune, endocrine, and metabolic pathways [2]. The gut microbiota—comprising trillions of microorganisms—produces a vast array of neuroactive metabolites, including short-chain fatty acids (SCFAs), neurotransmitters, and immune modulators that can significantly influence brain function and health [90] [2]. Dysbiosis, or an imbalance in this gut ecosystem, has been implicated in the pathogenesis of various neurodegenerative diseases, including Alzheimer's disease (AD), Parkinson's disease (PD), and multiple sclerosis (MS) [2]. This pathophysiological link establishes the MGBA as a promising therapeutic target, with probiotics and prebiotics serving as primary intervention strategies to modulate this critical axis.
Clinical Evidence: Differentiating Symptomatic from Disease-Modifying Effects
Evidence for Symptomatic Relief
Neuropsychiatric Symptoms
A recent comprehensive meta-analysis of 23 randomized controlled trials (RCTs) involving 1,401 patients provides robust evidence for the symptomatic efficacy of probiotics in neuropsychiatric conditions. The analysis demonstrated that probiotic supplementation significantly reduced symptoms of depression (Standardized Mean Difference, SMD: -0.96; 95% CI: -1.31, -0.61) and anxiety (SMD: -0.59; 95% CI: -0.98, -0.19) in clinically diagnosed populations [91]. The effect on depression was particularly substantial, with the greatest benefits observed after up to 8 weeks of intervention. Subgroup analyses revealed that single-strain probiotics paradoxically showed stronger effects than multi-strain formulations for depressive symptoms, challenging conventional assumptions about synergistic benefits of bacterial cocktails [91].
In contrast, prebiotics alone showed a non-significant trend toward reducing depression (SMD: -0.28; 95% CI: -0.61, 0.04) based on a more limited set of three trials, suggesting their primary symptomatic role may be adjunctive rather than primary [91].
Gastrointestinal and Systemic Symptoms
Beyond mental health, these interventions demonstrate significant symptomatic benefits in gastrointestinal conditions. In inflammatory bowel disease (IBD), specific probiotic formulations, including single-strain Lactobacillus and mixed-strain combinations of Lactobacillus and Bifidobacterium, have proven effective in improving clinical symptoms and quality of life [92]. Similarly, prebiotics such as galactooligosaccharides (GOS) and fructooligosaccharides (FOS) enhance gut barrier function and reduce gastrointestinal discomfort through mechanisms involving increased beneficial Bifidobacterium populations and SCFA production [93].
In oncology care, a scoping review of RCTs found that probiotic supplementation, particularly with Lactobacillus and Bifidobacterium bifidum, significantly improved patient-reported symptom burden, including reduced chemotherapy-related gastrointestinal side effects [94].
Table 1: Clinically Significant Symptomatic Benefits of Probiotics and Prebiotics
| Condition | Intervention | Outcome Measure | Effect Size (SMD/Other) | Evidence Grade |
|---|---|---|---|---|
| Depression | Probiotics | Symptom severity | SMD: -0.96 [-1.31, -0.61] | Level 1 (High) |
| Anxiety | Probiotics | Symptom severity | SMD: -0.59 [-0.98, -0.19] | Level 1 (High) |
| IBD Symptoms | Probiotics (Lactobacillus/Bifidobacterium) | Clinical symptom scores | Significant improvement | Level 2 (Moderate) |
| Chemotherapy Side Effects | Probiotics (Lactobacillus spp.) | Patient-reported symptoms | Significant reduction | Level 2 (Moderate) |
| Immune Function | Prebiotics (GOS/FOS) | IgA, NK cell activity | Significant increase | Level 2 (Moderate) |
Evidence for Disease-Modifying Effects
Neurodegenerative Disease Pathology
Emerging research suggests that probiotics and prebiotics may exert disease-modifying effects by targeting core pathological processes in neurodegenerative diseases. In Alzheimer's disease, gut dysbiosis can promote neuroinflammation via systemic circulation of microbial metabolites, which may contribute to amyloid-beta aggregation and tau pathology [2]. Specific microbial metabolites, including certain SCFAs like butyrate, demonstrate neuroprotective properties, while others, such as trimethylamine N-oxide (TMAO), may exacerbate neurodegenerative processes [2] [93].
A systematic review and meta-analysis of 41 studies revealed that prebiotics and phytochemicals significantly reduced serum TMAO levels—a gut microbiota-derived metabolite linked to cardiovascular and neurological pathology—in both animal models and human trials [93]. This reduction was associated with favorable shifts in gut microbiota composition, particularly increased Akkermansia and Bifidobacterium genera, suggesting a potential mechanism for modifying disease risk [93].
In Parkinson's disease, the proposed prion-like propagation of α-synuclein from gut to brain via the vagus nerve represents another target for disease-modifying interventions [2]. Epidemiological studies showing reduced PD incidence in individuals with historical vagotomy support this gut-first hypothesis of PD pathogenesis [2]. Preclinical evidence suggests that probiotic and prebiotic interventions may strengthen gut barrier integrity, potentially reducing the initial misfolding and subsequent spread of α-synuclein aggregates [2].
Metabolic and Inflammatory Modulation
Beyond neurological conditions, these interventions demonstrate disease-modifying potential in metabolic disorders. A 2025 randomized, double-blind clinical trial with 131 overweight/obese and healthy participants found that inulin supplementation significantly improved glycemic markers in overweight/obese individuals, reducing glucose levels at 1-hour and 2-hour timepoints during oral glucose tolerance tests and increasing fasting insulin [93]. These metabolic improvements were associated with a 72% reduction in Ruminococcus abundance, illustrating how prebiotics can modify disease trajectories through microbial composition changes [93].
In older adults—a population particularly relevant to neurodegenerative disease—a meta-analysis of 29 RCTs showed that probiotic, prebiotic, and synbiotic interventions significantly increased beneficial Bifidobacterium abundance (prebiotics: SMD = 1.09; probiotics: SMD = 0.40) and enhanced SCFA production, particularly valeric acid (SMD = 0.50) and acetic acid (SMD = 0.62) with synbiotics [95]. Critically, these microbial changes were associated with modified inflammatory profiles, including reduced pro-inflammatory IL-1β (SMD = -0.39 with prebiotics) and TNF-α (SMD = -0.36 with synbiotics), and increased anti-inflammatory IL-10 (SMD = 0.61 with prebiotics) [95]. This immunomodulation represents a key mechanism through which microbiota-targeted interventions may exert disease-modifying effects across multiple age-related conditions.
Table 2: Potential Disease-Modifying Effects of Probiotics and Prebiotics
| Pathological Process | Intervention | Mechanism of Action | Evidence Level |
|---|---|---|---|
| Neuroinflammation | Prebiotics (FOS, GOS) | Reduced microglial activation via SCFA production; decreased circulating LPS | Preclinical (Strong) |
| Protein Misfolding (α-synuclein) | Probiotics | Enhanced gut barrier function; reduced initial misfolding | Preclinical (Moderate) |
| Metabolic Dysregulation | Inulin | Modulation of gut microbiota (↓Ruminococcus); improved insulin sensitivity | Level 2 (Human RCT) |
| Systemic Inflammation | Synbiotics | ↓TNF-α (SMD: -0.36); ↑IL-10 (SMD: 0.61) | Level 1 (Meta-analysis) |
| Vascular Pathology | Prebiotics/Phytochemicals | ↓TMAO production; altered microbial diversity | Level 2 (Human/Animal) |
Mechanistic Insights: Signaling Pathways and Molecular Targets
The gut-brain axis employs multiple communication pathways to mediate the effects of probiotics and prebiotics on neurological health:
MGBA Communication Pathways and Effects
Neural Pathways
The vagus nerve serves as a direct neural highway between the gut and brainstem, transmitting sensory information about gut state to the brain [2]. Certain gut bacteria can directly stimulate vagal pathways by producing neurotransmitters or neuromodulators, including GABA, serotonin, and histamine [2]. This pathway is implicated in the rapid effects of probiotics on mood and anxiety symptoms, as evidenced by studies showing that vagotomy abolishes the anxiolytic effects of certain probiotic strains in animal models [2].
Immune and Inflammatory Pathways
Gut microbes profoundly shape host immune system function throughout life. Beneficial commensals promote immune tolerance and reinforce intestinal barrier function, while dysbiosis can provoke systemic inflammation [2]. Microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS) from Gram-negative bacteria, can breach a compromised gut barrier and enter circulation, where they activate Toll-like receptors (e.g., TLR4) and other innate immune sensors in peripheral tissues and the brain [2]. Even low-grade endotoxin leakage can trigger chronic neuroinflammation through microglial activation via TLR4/NF-κB signaling, contributing to neuronal injury in neurodegenerative diseases [2].
Endocrine and Metabolic Pathways
The hypothalamic-pituitary-adrenal (HPA) axis represents a neuroendocrine arm of the MGBA, translating stress signals into systemic hormone release (e.g., cortisol) that can alter gut barrier integrity and immune function [2]. Conversely, gut microbes produce and influence a wide range of metabolites, including SCFAs, bile acids, and tryptophan derivatives, that can systematically influence CNS function [2]. SCFAs—particularly butyrate, propionate, and acetate—demonstrate neuroprotective properties by enhancing blood-brain barrier integrity, reducing neuroinflammation, and supporting neuronal homeostasis [2] [95].
Experimental Design and Methodological Protocols
Standardized Clinical Trial Protocol for Probiotic Interventions
Objective: To evaluate the efficacy of probiotic strain(s) on neurodegenerative disease biomarkers and symptoms.
Population: Adults (50-80 years) with early-stage neurodegenerative disease (e.g., MCI for AD, prodromal PD) confirmed by standardized diagnostic criteria.
Intervention Structure:
- Duration: 12-24 weeks minimum, with longitudinal follow-up for disease-modification studies
- Dosage: Minimum 10^9-10^10 CFU/day, verified by independent assay
- Strain Specification: Genetically sequenced and deposited in public culture collection
- Control: Isocaloric, visually matched placebo with non-viable bacteria
Primary Outcomes:
- Disease Modification: Neuroimaging biomarkers (amyloid-PET, fMRI), CSF biomarkers (Aβ42, p-tau, α-synuclein)
- Symptomatic Effects: Cognitive battery (e.g., ADAS-Cog, MoCA), motor scales (UPDRS for PD), quality of life measures
Secondary Outcomes:
- Microbiome Analysis: 16S rRNA sequencing (V3-V4 region) with shotgun metagenomics in subset
- Inflammatory Markers: Plasma IL-6, TNF-α, CRP, LPS-binding protein
- Microbial Metabolites: Serum/plasma SCFAs, TMAO via LC-MS/MS
Sample Collection & Storage:
- Stool: Aliquot immediately and store at -80°C in DNA/RNA shield buffer
- Blood: Collect in EDTA tubes, process within 2h, store plasma at -80°C
- CSF: Collect in polypropylene tubes, freeze in aliquots at -80°C
Microbiome Analysis Workflow
Microbiome Analysis Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Gut-Brain Axis Studies
| Category | Specific Tools/Reagents | Application/Function | Technical Notes |
|---|---|---|---|
| Probiotic Strains | Lactobacillus (acidophilus, casei, plantarum, rhamnosus), Bifidobacterium (longum, bifidum, breve), S. boulardii | Mechanistic studies; formulation development | Verify absence of transferable antibiotic resistance genes [90] |
| Prebiotic Substrates | GOS, FOS, Inulin, XOS, Beta-glucans | Selective stimulation of beneficial microbes; SCFA production | Dose-dependent effects; purity critical for reproducibility [93] |
| Cell Culture Models | Caco-2 intestinal epithelium, SH-SY5Y neurons, primary microglia | Barrier integrity, neuroinflammation studies | Transwell systems for gut barrier assessment [2] |
| Animal Models | Germ-free mice, Humanized microbiota mice, Transgenic neurodegeneration models (APP/PS1, SNCA) | Causal mechanism studies | Environmental controls critical (food, bedding, coprophagy) [2] |
| Sequencing Platforms | Illumina (16S rRNA), NovaSeq (shotgun metagenomics), Nanopore (epigenetics) | Microbiome composition and function | Standardized DNA extraction protocols essential [95] |
| Metabolomics | LC-MS/MS (SCFAs, TMAO, neurotransmitters), NMR spectroscopy | Microbial metabolite quantification | Stable isotope tracers for pathway elucidation [2] [93] |
The differentiation between symptomatic and disease-modifying effects of probiotics and prebiotics represents a critical frontier in neurodegenerative disease therapeutics. Current evidence strongly supports the symptomatic benefits of specific probiotic strains for neuropsychiatric symptoms, while emerging research suggests potential disease-modifying effects through modulation of neuroinflammation, protein aggregation, and gut barrier integrity.
Several key challenges must be addressed to advance this field:
- Standardization: Lack of consistent strains, dosages, and outcome measures across studies
- Mechanistic Gaps: Incomplete understanding of strain-specific effects and causal pathways
- Personalization: Significant interindividual variability in response to interventions
- Translational Hurdles: Disconnect between robust preclinical findings and mixed clinical results
Future research should prioritize large-scale, well-controlled clinical trials with standardized methodologies, integrated multi-omics approaches, and targeted interventions based on individual microbiome profiles. The strategic application of probiotics and prebiotics as adjunctive therapies alongside conventional treatments holds substantial promise for addressing both the symptoms and progression of neurodegenerative diseases through the gut-brain axis.
Fecal Microbiota Transplantation (FMT) Outcomes Across Neurodegenerative Indications
The microbiota-gut-brain axis (MGBA) represents one of the most significant paradigm shifts in neuroscience, establishing a framework for understanding bidirectional communication between the gastrointestinal tract and the central nervous system [2] [3]. This intricate network integrates neural, immune, endocrine, and metabolic pathways to maintain neurological homeostasis, with gut microbiota playing a pivotal regulatory role [2] [6]. Emerging evidence indicates that disruption of this axis, termed gut dysbiosis, contributes significantly to the pathogenesis of various neurodegenerative diseases [2] [8]. Against this mechanistic backdrop, Faecal Microbiota Transplantation (FMT) has emerged as an investigative therapy aiming to restore microbial equilibrium and modulate neurodegenerative processes [96]. This whitepaper synthesizes current evidence on FMT outcomes across neurodegenerative indications, providing a technical resource for research and drug development professionals.
The Microbiota-Gut-Brain Axis: Foundation for FMT
Core Components and Communication Pathways
The MGBA is a complex, integrated system facilitating continuous communication between the gut and brain. Key components include the gut microbiota itself, the intestinal barrier and mucosal immune system, the enteric nervous system (ENS), the vagus nerve, central autonomic circuits, and CNS interfaces like the blood-brain barrier (BBB) and microglia [2]. Communication occurs through several interdependent pathways:
- Neural Pathways: The vagus nerve serves as a direct neural highway, with afferent fibers detecting luminal contents and efferent fibers modulating gut function. Gut microbes produce neurotransmitters like GABA, serotonin, and histamine that can directly stimulate these neural pathways [2].
- Immune and Inflammatory Pathways: Gut microbes shape host immunity from development through adulthood. Microbial-associated molecular patterns (MAMPs) like lipopolysaccharide (LPS) can breach intestinal barriers, triggering systemic and neuroinflammation through microglial activation [2] [6]. Conversely, short-chain fatty acids (SCFAs) from fiber-fermenting bacteria promote regulatory T cells (Tregs) with anti-inflammatory properties [2].
- Metabolic and Endocrine Pathways: Gut microbiota produce numerous neuroactive metabolites, including SCFAs, tryptophan derivatives, and secondary bile acids, which circulate systemically to influence brain function [2] [3]. Enteroendocrine cells detect luminal contents and release hormones that can signal to the brain [3].
Mechanistic Basis for FMT in Neurodegeneration
The rationale for FMT in neurodegenerative diseases stems from growing understanding of how gut dysbiosis contributes to pathology through the MGBA. Preclinical and human studies have identified several interconnected mechanistic links:
- Neuroinflammation: Dysbiosis can promote peripheral inflammation that activates microglia, the CNS-resident immune cells, leading to chronic neuroinflammation—a hallmark of neurodegeneration [2] [3].
- Protein Misfolding and Aggregation: Evidence suggests gut dysbiosis may influence the aggregation of pathogenic proteins like α-synuclein in Parkinson's disease and amyloid-β in Alzheimer's disease [2]. The prion-like propagation of α-synuclein from gut to brain via the vagus nerve represents a particularly compelling pathway [2].
- Blood-Brain Barrier Disruption: Inflammatory mediators and microbial metabolites can compromise BBB integrity, increasing CNS exposure to peripheral inflammatory signals and potentially harmful substances [2] [8].
- Glial Cell Dysfunction: Microglia, astrocytes, and oligodendrocytes all receive essential cues from the gut microbiome, making them vulnerable to dysbiosis-induced dysfunction [3].
Table 1: Key Microbial Metabolites Influencing Neurodegenerative Pathways
| Metabolite Class | Representative Molecules | Primary Producers | Proposed Mechanisms in Neurodegeneration |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Acetate, Propionate, Butyrate | Faecalibacterium, Lachnospiraceae | HDAC inhibition; Treg induction; BBB integrity; microglial maturation [2] [6] |
| Tryptophan Derivatives | Kynurenine, Indole derivatives | Multiple bacterial species | Aryl hydrocarbon receptor activation; neuroinflammation modulation; serotonin synthesis precursor [2] [3] |
| Secondary Bile Acids | Deoxycholate, Lithocholate | Multiple bacterial species | FXR and TGR5 receptor signaling; neuroinflammation reduction; neuroprotection [2] |
| Neurotransmitters | GABA, Serotonin, Dopamine | Lactobacillus, Bifidobacterium, Escherichia | Direct receptor activation; vagal nerve stimulation; synaptic transmission modulation [2] [3] |
FMT Outcomes by Neurodegenerative Indication
Parkinson's Disease (PD)
Parkinson's disease represents the most advanced application of FMT among neurodegenerative conditions, with several randomized controlled trials completed. The gut-brain connection is particularly strong in PD, with gastrointestinal symptoms like constipation often preceding motor symptoms by decades [2] [96].
Clinical Outcomes: Recent FMT trials in PD patients have demonstrated promising improvements in both motor and non-motor symptoms [96]. These benefits are potentially mediated through microbiota-linked enhanced SCFA production, reduced systemic inflammation, and modulation of neuroactive metabolite pathways [96]. The specific microbial signatures of PD—often characterized by increases in Lactobacillus, Akkermansia, and Bifidobacterium with decreases in Lachnospiraceae and Faecalibacterium—provide a clear therapeutic target for FMT intervention [97].
Methodological Considerations: Current research focuses on critical questions regarding donor selection, delivery routes (colonoscopy vs. oral capsules), and the timing and frequency of transplantation to optimize clinical outcomes [96].
Alzheimer's Disease (AD)
While clinical FMT trials in Alzheimer's patients are less advanced than in PD, compelling preclinical evidence and microbiome association studies support its therapeutic potential.
Microbiome Alterations: AD patients consistently demonstrate altered gut microbiota composition compared to healthy controls, typically featuring reduced microbial diversity and depletion of SCFA-producing genera [8]. These changes correlate with disease severity and contribute to pathogenesis through neuroinflammatory pathways, microbial metabolite imbalances, and modulation of systemic immune responses [8].
Mechanistic Insights: The MGBA influences AD pathology through multiple pathways, including microglial activation, neuroinflammation, and potentially direct effects on amyloid-β aggregation and clearance [3]. Microglia, as the primary innate immune cells of the CNS, accumulate near Aβ plaques and express many AD-risk genes identified in genome-wide association studies [3].
Amyotrophic Lateral Sclerosis (ALS) and Multiple Sclerosis (MS)
Evidence for gut-brain axis involvement in ALS and MS, while less extensive than for PD and AD, is growing and supports potential FMT applications.
ALS Considerations: Postmortem transcriptomic analyses of ALS spinal cord reveal increased inflammatory reactions driven by microglia and astrocytes [3], cell types known to be modulated by gut microbiome signals [3]. While specific FMT trials in ALS are limited, the shared mechanisms of neuroinflammation and glial dysfunction provide rationale for investigation.
MS Applications: Multiple sclerosis, while primarily an autoimmune demyelinating condition, shares chronic CNS injury and immune dysregulation mechanisms influenced by the microbiome [2]. In experimental autoimmune encephalomyelitis (EAE) models, a high-fiber diet that boosts SCFA production expanded regulatory T cells, strengthened the gut barrier, and reduced CNS inflammation and disease severity [2], suggesting FMT could produce similar benefits.
Table 2: Summary of FMT Outcomes Across Neurodegenerative Indications
| Disease | Clinical Evidence Level | Key Microbial Alterations | Reported FMT Outcomes | Primary Proposed Mechanisms |
|---|---|---|---|---|
| Parkinson's Disease | Randomized Controlled Trials [96] | ↑ Lactobacillus, Akkermansia↓ Lachnospiraceae, Faecalibacterium [97] | Motor/non-motor improvement; enhanced SCFA production; reduced inflammation [96] | Vagus nerve signaling; α-synuclein pathology; systemic inflammation [2] [96] |
| Alzheimer's Disease | Preclinical/Association Studies [8] | Reduced diversity; depleted SCFA producers; enriched pro-inflammatory taxa [8] | Cognitive improvement in animal models; reduced inflammatory markers [8] | Neuroinflammation; microglial activation; amyloid-β pathology [3] [8] |
| Multiple Sclerosis | Preclinical Models [2] | Disorder-specific dysbiosis patterns | Reduced CNS inflammation in EAE models [2] | Immune cell trafficking; Th17/Treg balance; BBB integrity [2] |
| Amyotrophic Lateral Sclerosis | Mechanistic/Association [3] | Emerging dysbiosis patterns | Limited direct evidence | Neuroinflammation; microglial activation [3] |
Experimental Protocols and Methodological Considerations
FMT Preparation and Delivery Protocols
Standardized protocols are essential for rigorous FMT research and future therapeutic applications:
Donor Screening and Selection:
- Comprehensive medical history assessment for infectious, metabolic, and neurological diseases
- Stool testing for pathogens including C. difficile, Salmonella, Shigella, Campylobacter, E. coli O157:H7
- Serological testing for HIV, Hepatitis A/B/C, Syphilis
- Exclusion criteria: recent antibiotic use, high-risk behaviors, chronic gastrointestinal disorders
Fecal Material Preparation:
- Fresh or frozen stool processing within 6-8 hours of donation for fresh preparations
- Suspension in sterile saline or water with glycerol cryopreservation
- Filtration to remove particulate matter
- Quality control: aerobicity and anaerobicity culture from filtrate
Administration Routes:
- Colonoscopy: Direct delivery to colon, enabling maximum colonic mucosal engagement
- Nasoenteric Tube: Less invasive but potential for upper GI side effects
- Oral Capsules: Acid-resistant capsules for targeted colonic release, enhancing patient acceptability
Assessment and Monitoring Protocols
Comprehensive longitudinal assessment is critical for evaluating FMT outcomes in neurodegenerative diseases:
Microbiome Analysis:
- Sampling: Pre-FMT baseline, 1-2 weeks post-FMT, 1-3 month intervals thereafter
- Methodology: 16S rRNA sequencing for community structure; shotgun metagenomics for functional potential; metabolomics for metabolite profiling
- Parameters: Alpha-diversity (Shannon, Chao1), beta-diversity (PCoA, UniFrac), differential abundance analysis
Clinical Outcome Measures:
- Disease-Specific Scales: UPDRS for PD, ADAS-Cog for AD, ALSFRS-R for ALS, EDSS for MS
- Non-Motor Symptoms: Gastrointestinal (constipation, diarrhea), neuropsychiatric (depression, anxiety, apathy)
- Functional Assessments: Activities of daily living, quality of life measures
Biomarker Integration:
- Peripheral: Inflammatory markers (CRP, cytokines), gut hormones (GLP-1, PYY), microbial metabolites (SCFAs, bile acids)
- CNS Imaging: Functional MRI, PET imaging for neuroinflammation, dopamine transporter (DaT) imaging in PD
- Other Biomarkers: Blood-brain barrier integrity markers, exosome analysis for neurodegenerative proteins
Signaling Pathways in the Microbiota-Gut-Brain Axis
The therapeutic potential of FMT operates through multiple interconnected signaling pathways along the microbiota-gut-brain axis. The following diagram synthesizes these primary communication routes:
MGBA Signaling Pathways Diagram Title: FMT Modulation of Gut-Brain Signaling
This schematic illustrates how FMT may counteract neurodegeneration through multiple parallel mechanisms: (1) restoring microbial metabolite production (SCFAs, neurotransmitters); (2) reinforcing intestinal barrier integrity to reduce systemic inflammation; (3) modulating peripheral immune responses; and (4) influencing CNS function via neural and humoral pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for FMT and Gut-Brain Axis Investigations
| Category | Specific Reagents/Assays | Research Application | Technical Considerations |
|---|---|---|---|
| Microbiome Analysis | 16S rRNA sequencing kits; Shotgun metagenomics platforms; Anaerobic culture media | Community profiling; functional potential assessment; bacterial isolation | Preserve samples at -80°C; use stabilization buffers for RNA; maintain anaerobic conditions for cultures |
| Metabolite Detection | GC-MS/MS for SCFAs; LC-MS for bile acids/tryptophan metabolites; ELISA for hormones | Quantify microbial-derived metabolites in feces, serum, CSF | Rapid processing to preserve metabolite integrity; appropriate internal standards for quantification |
| Immunological Assays | Multiplex cytokine panels; flow cytometry panels for immune cells; immunofluorescence | Profile inflammatory mediators; characterize peripheral/CNS immune populations | Control for circadian variations; standardize sample collection times |
| Neuropathological Tools | IHC for protein aggregates (α-syn, Aβ); protein aggregation assays; microglial activation markers | Assess CNS pathology; protein misfolding; neuroinflammation | Post-fixation times critical for epitope preservation; validate antibodies for specific species |
| Gut Barrier Integrity | FITC-dextran assay; zonulin/occludin detection; Ussing chambers | Intestinal permeability assessment; tight junction protein expression | Control for dietary influences; standardize fasting periods before permeability assays |
| Neural Pathway Tools | Vagotomy surgical models; neuronal tracing; electrophysiology | Determine vagus nerve involvement; neural circuit mapping | Surgical controls critical; validate neuronal tracers for specific projections |
Knowledge Gaps and Research Priorities
Despite promising preliminary findings, significant challenges remain in translating FMT into validated neurodegenerative disease therapies:
- Causality Establishment: Most human evidence remains correlative; further studies are needed to establish causal relationships between specific microbial changes and disease modification [2].
- Donor Optimization: Critical questions regarding optimal donor selection, screening protocols, and personalized matching require systematic investigation [96].
- Delivery Standardization: The optimal route, frequency, and formulation of FMT administration need comparative effectiveness research [96].
- Biomarker Development: Robust biomarkers predicting treatment response and monitoring target engagement are essential for advancing the field [96].
- Mechanistic Elucidation: A deeper understanding of how FMT-derived microbes influence specific neurodegenerative pathways will inform targeted interventions [2] [3].
Integration with Broader Therapeutic Strategies
FMT should be viewed as one component within a broader therapeutic arsenal targeting the MGBA. Combination approaches with prebiotics, probiotics, dietary interventions, and pharmacological agents may yield synergistic benefits [8]. Future research should explore how FMT can be integrated with these complementary approaches to maximize clinical efficacy.
FMT represents a promising therapeutic approach grounded in the solid scientific foundation of the microbiota-gut-brain axis. Evidence across neurodegenerative indications, particularly Parkinson's disease, suggests potential for modifying both motor and non-motor symptoms by targeting underlying gut dysbiosis and its systemic consequences. However, considerable research is needed to standardize methodologies, identify optimal candidates, and elucidate precise mechanisms of action. As our understanding of the intricate relationships between gut microbes and neurodegeneration deepens, FMT and related microbiome-targeted therapies offer transformative potential for developing innovative treatment paradigms that bridge neurology, microbiology, and precision medicine.
Comparative Analysis of Dietary Interventions on Cognitive and Motor Metrics
The burgeoning field of nutritional neuroscience increasingly highlights the profound impact of diet on brain health, with effects mediated through complex metabolic, inflammatory, and gut-brain axis pathways. This technical review provides a comparative analysis of major dietary interventions—including the MIND diet, intermittent fasting, ketogenic diets, and nutrient supplementation—on specific cognitive domains and motor function metrics. Evidence synthesized from recent randomized controlled trials, meta-analyses, and systematic reviews demonstrates that dietary interventions exert significant, domain-specific effects on cognitive and motor outcomes, with efficacy modulated by individual risk profiles, genetic factors, and gut microbiota composition. The gut-brain axis emerges as a critical mediator, with microbial metabolites such as short-chain fatty acids (SCFAs), trimethylamine N-oxide (TMAO), and bile acids influencing neuroinflammation, blood-brain barrier integrity, and protein aggregation pathologies. Integration of quantitative data reveals that combined nutritional and lifestyle interventions yield superior outcomes for executive function and memory, while specific nutrient formulations show promise for mitigating motor decline. This analysis provides researchers and drug development professionals with a framework for incorporating nutritional strategies into multi-target therapeutic approaches for neurodegenerative disease prevention and management.
The microbiota-gut-brain axis (MGBA) represents a complex, bidirectional communication network that integrates neural, immune, endocrine, and metabolic pathways between the gastrointestinal tract and the central nervous system [2]. Disruption of this axis, manifesting as gut dysbiosis, impaired intestinal barrier function, and aberrant microbial metabolite signaling, has been implicated in the pathogenesis of diverse neurodegenerative conditions including Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) [8] [9]. Dietary interventions modulate the MGBA through multiple mechanisms: influencing microbial community structure, altering production of neuroactive metabolites (e.g., SCFAs, neurotransmitters), regulating intestinal permeability, and modulating systemic inflammation [2] [98]. These interventions offer promising, accessible approaches for preserving cognitive and motor function across the neurodegenerative disease spectrum.
Understanding the anatomical and physiological foundations of the MGBA is essential for contextualizing dietary interventions. Key components include: (1) the gut microbiota and their metabolic output; (2) the intestinal mucosal barrier and enteric nervous system; (3) vagal and spinal afferent nerves; (4) neuroendocrine pathways including the hypothalamic-pituitary-adrenal (HPA) axis; and (5) central nervous system interfaces including the blood-brain barrier and microglia [2]. Dietary components directly influence each element, creating opportunities for targeted interventions. For instance, specific dietary patterns can enhance populations of SCFA-producing bacteria, which in turn strengthen the intestinal barrier, reduce systemic inflammation, and promote neurotrophic factor expression [8]. This review systematically evaluates the evidence for dietary modulation of the MGBA to improve cognitive and motor outcomes, with particular emphasis on quantitative metrics, experimental methodologies, and translational applications.
Comparative Efficacy of Dietary Interventions on Cognitive Metrics
Domain-Specific Cognitive Responses to Nutritional Approaches
Cognitive function encompasses multiple domains—including memory, executive function, global cognition, and attention—that demonstrate differential sensitivity to dietary interventions. The table below synthesizes evidence from controlled trials and meta-analyses regarding the efficacy of major dietary approaches on specific cognitive metrics.
Table 1: Effects of Dietary Interventions on Cognitive Domains
| Intervention Type | Memory Outcomes | Executive Function | Global Cognition | Key Supporting Evidence |
|---|---|---|---|---|
| MIND/Mediterranean Diets | Consistent improvement in episodic memory [99] | Moderate benefits, particularly in switching ability [100] | Significant positive association [99] [101] | Observational studies & RCTs |
| Intermittent Fasting | Improved memory with combined exercise [100] | Limited standalone benefit | Heterogeneous effects | 3-month RCT in postmenopausal women with obesity [100] |
| Ketogenic Diet | Potential benefit through reduced neuroinflammation | Limited human evidence | Limited human evidence | Preclinical models show reduced amyloid toxicity [99] |
| B Vitamin Supplementation | Enhanced episodic memory, especially with metabolic risk [99] | Minimal standalone effect | Reduced brain atrophy rates in MCI [98] | COSMOS-Web trial; homocysteine reduction mechanisms [99] |
| Omega-3 PUFA Supplementation | Beneficial in combination with B vitamins [99] | Heterogeneous effects | Moderate association | Synergistic effects with B vitamins for memory [99] |
| Polyphenol-Rich Foods | Modest improvement in contextual memory | Enhanced cognitive flexibility | Mild to moderate benefits | Anthocyanin trials with MRI-confirmed perfusion improvements [98] |
Mechanistic Pathways Linking Nutrition to Cognitive Function
The efficacy of dietary interventions on cognitive metrics is mediated through multiple overlapping biological pathways. The following diagram illustrates key gut-brain signaling mechanisms through which nutritional components influence brain health and cognitive function.
Figure 1: Gut-Brain Signaling Pathways in Cognitive Function. This diagram illustrates the key mechanisms through which dietary components influence brain health, including modulation of gut microbiota, production of microbial metabolites, intestinal barrier integrity, systemic circulation, blood-brain barrier function, and ultimately neuroinflammation and neurogenesis. SCFAs = short-chain fatty acids; BDNF = brain-derived neurotrophic factor; BBB = blood-brain barrier.
The molecular mechanisms connecting dietary interventions to cognitive outcomes involve complex interactions between nutritional components, gut microbiota, and brain physiology. B vitamins (folate, B12, B6) participate in one-carbon metabolism and homocysteine re-methylation, with disruption leading to impaired neurotransmitter production and altered gene expression in the amyloid-beta pathway [98]. Omega-3 polyunsaturated fatty acids (PUFAs) mitigate neuroinflammation by serving as precursors to pro-resolving mediators, reducing reactive oxygen species, improving endothelial dysfunction, and maintaining blood-brain barrier integrity [98]. Polyphenols exert antioxidant and anti-inflammatory effects while potentially influencing brain plasticity and amyloid-beta aggregation, though their benefits may be indirectly mediated through gut microbiota modulation [98]. The APOE4 genotype modifies individual responses to dietary fats, suggesting personalized nutritional approaches based on genetic profiles [98].
Effects of Dietary Interventions on Motor Metrics
Quantitative Assessment of Motor Function
While cognitive outcomes are frequently assessed in nutritional studies, motor function represents a crucial domain increasingly recognized as influenced by dietary patterns and nutritional status. Objective measures of motor function provide sensitive metrics for detecting subtle neurological changes in response to interventions. The following table summarizes quantitative motor metrics and their response to nutritional interventions.
Table 2: Effects of Dietary Interventions and Associated Metrics on Motor Function
| Motor Metric | Assessment Method | Intervention Effects | Clinical Significance |
|---|---|---|---|
| Step Velocity | Inertial measurement units (IMUs), motion sensors, 3D motion capture | Significant improvement with combined interventions [102] | Predicts fall risk and functional mobility |
| Step Length | Observational gait analysis, motion sensors | Heterogeneous responses across interventions [102] | Correlates with disease progression in PD |
| Muscle Strength | Resistance testing, physical function batteries | Improved with exercise and combined interventions [100] | Associated with independence in activities of daily living |
| Movement Smoothness | 3D motion capture systems | Limited nutritional studies | Marker of motor control integrity |
Methodologically, objective assessment tools have demonstrated superior sensitivity compared to traditional clinical scales for detecting motor changes in response to interventions. A meta-analysis of 19 randomized controlled trials (n=2,626 participants) found that inertial measurement units (IMUs), motion sensors, and 3D motion capture systems provided statistically significant quantification of changes in step velocity and step length in elderly individuals [102]. These technologies enable precise measurement of gait parameters that may respond to nutritional interventions, particularly in populations with early neurodegenerative conditions.
Protocol for Motor Metric Assessment in Nutritional Studies
Standardized assessment protocols are essential for generating comparable data across nutritional intervention studies. The following workflow details a comprehensive approach to motor function evaluation in clinical trials investigating dietary interventions.
Figure 2: Motor Function Assessment Workflow. This experimental protocol outlines standardized procedures for evaluating motor metrics in dietary intervention studies, incorporating objective measurement technologies and controlled assessment conditions.
Detailed Methodology:
Participant Screening: Recruit adults aged 60-80 years with appropriate exclusion criteria for neurological conditions that might confound motor assessment [102]. Conduct cognitive screening using the Mental State Examination T10 (MSET10) to establish baseline function [100].
Sensor Configuration: Apply inertial measurement units (IMUs) to bilateral lower extremities (thigh, shank, foot) according to manufacturer specifications. For 3D motion capture systems, place reflective markers on anatomical landmarks using a validated marker set (e.g., Plug-in-Gait model) [102].
Testing Protocol: Conduct gait assessment along a 10-meter walkway under three conditions: (1) comfortable pace, (2) dual-task walking (e.g., while performing verbal fluency task), and (3) fast pace. Collect three trials per condition with adequate rest periods to minimize fatigue effects.
Data Processing: Extract spatiotemporal gait parameters including step velocity, step length, step time, and double support time using manufacturer software. Calculate variability measures (coefficient of variation) for each parameter across trials.
Statistical Analysis: Compare pre-post intervention changes using appropriate statistical methods (e.g., mixed-model ANOVA accounting for multiple comparisons). For meta-analytic approaches, calculate standardized mean differences with 95% confidence intervals using random-effects models to account for heterogeneity across studies [102].
Experimental Protocols for Dietary Intervention Studies
Protocol 1: Combined Dietary and Physical-Cognitive Intervention
This protocol is adapted from a randomized controlled trial demonstrating significant improvements in both cognitive and motor metrics in postmenopausal women with obesity [100].
Study Design:
- Type: 3-month, assessor-blinded, four-arm randomized controlled trial
- Participants: 92 postmenopausal women with obesity (BMI ≥25 kg/m², WHR ≥0.80)
- Groups: Dietary intervention alone, physical-cognitive exercise alone, combined intervention, control group
- Primary Outcomes: Executive functions, memory, plasma BDNF levels
- Secondary Outcomes: Global cognition, attention, metabolic parameters, physical function
Dietary Intervention Protocol:
- Regimen: Modified intermittent fasting (2 days/week)
- Weeks 1-4: 75% of estimated energy requirements on fasting days
- Weeks 5-8: 50% of estimated energy requirements on fasting days
- Weeks 9-12: 25% of estimated energy requirements on fasting days
- Ad Libitum Days: 5 days per week with no restrictions
- Compliance Monitoring: Self-recorded dietary intake via mobile application with calculation based on nutritive values of foods
Physical-Cognitive Exercise Protocol:
- Frequency: 3 days/week for 3 months
- Session Structure: 10 min warm-up, 40 min physical-cognitive exercise, 10 min cool-down
- Training Components:
- Physical session: Moderate intensity resistance and aerobic exercise
- Simultaneous physical-cognitive session: Challenging cognitive tasks during movement
- Cognitive session: Domain-specific cognitive training (attention, executive function, memory)
- Progression: Increased physical demand (speed, repetitions, complexity) and cognitive demand (memory load, attentional requirements)
Assessment Timepoints: Baseline and post-intervention (3 months) with identical testing protocols.
Protocol 2: Multinutrient Supplementation Trial
This protocol synthesizes methodologies from multiple studies investigating B vitamin and omega-3 supplementation effects on cognitive outcomes [99] [98].
Supplementation Protocol:
- Duration: 12-24 months (depending on study outcomes)
- Intervention Groups:
- Group 1: B-vitamin complex (folate 0.8mg, vitamin B12 0.5mg, vitamin B6 20mg)
- Group 2: Omega-3 PUFA (EPA 1.1g + DHA 0.9g daily)
- Group 3: Combined B-vitamins and omega-3 PUFAs
- Group 4: Placebo
- Stratification: Based on baseline omega-3 status and homocysteine levels
Cognitive Assessment Battery:
- Memory: CERAD word list memory test, Rey Auditory Verbal Learning Test
- Executive Function: Trail Making Test (TMT Parts A & B), Stroop Color-Word Test
- Global Cognition: Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA)
- Processing Speed: Digit Symbol Substitution Test
Biological Sampling and Analysis:
- Plasma Biomarkers: BDNF, adiponectin, IL-6, insulin
- Nutritional Status: Omega-3 index, vitamin B12, folate, homocysteine
- Microbiota Metrics: Fecal samples for 16S rRNA sequencing, SCFA measurements
Neuroimaging (substudy): Structural MRI for brain volume assessment, particularly hippocampal volume and rate of brain atrophy.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Assessment Tools for Dietary Intervention Studies
| Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Cognitive Assessment | Trail Making Test (TMT), Stroop Color-Word Test, CERAD Memory Battery | Domain-specific cognitive evaluation | Requires trained administrators; consider practice effects in repeated measures |
| Motor Function Sensors | Inertial Measurement Units (IMUs), 3D Motion Capture Systems, Surface EMG | Objective quantification of gait parameters | Standardized placement protocols essential; sampling rates affect data quality |
| Biological Assays | ELISA for BDNF, adiponectin, IL-6; LC-MS for metabolic panels | Biomarker quantification for mechanistic insights | Standardize sampling time relative to interventions; consider diurnal variations |
| Microbiome Analysis | 16S rRNA sequencing kits, Shotgun metagenomics, SCFA analysis | Gut microbiota composition and function | Strict standardization of sample collection, storage, and processing protocols |
| Dietary Compliance Tools | Food frequency questionnaires, 24-hour dietary recalls, Mobile app tracking | Intervention adherence monitoring | Validation against biomarkers recommended (e.g., plasma fatty acids for fish intake) |
| Genetic Analysis | APOE genotyping, DNA methylation assays | Effect modification analysis | Power considerations for subgroup analyses by genotype |
This comparative analysis demonstrates that dietary interventions exert measurable, domain-specific effects on cognitive and motor metrics, with efficacy modulated through gut-brain axis pathways. The evidence supports several key conclusions: (1) Combined interventions targeting multiple lifestyle factors (diet, exercise, cognitive training) generally produce superior outcomes compared to single-component approaches; (2) Individual characteristics including genetic profile, metabolic status, and baseline microbiome composition significantly influence intervention efficacy; (3) Objective metrics for both cognitive and motor function provide sensitive endpoints for detecting intervention effects; (4) Mechanistic insights reveal that nutritional components influence brain health through modulation of inflammation, neurotrophic factors, endothelial function, and microbial metabolite signaling.
Future research priorities include developing standardized assessment methodologies for cross-study comparisons, validating microbiome-derived biomarkers for personalized nutrition approaches, and elucidating temporal dynamics of intervention effects through longitudinal study designs. Integration of multi-omics technologies (genomics, metabolomics, proteomics) with clinical outcomes will advance our understanding of individual variability in response to dietary interventions. For drug development professionals, these findings highlight opportunities for combining nutritional approaches with pharmacological interventions to create multi-target therapeutic strategies for neurodegenerative diseases. The gut-brain axis represents a promising target for developing novel interventions that leverage dietary components to modify disease progression and maintain cognitive and motor function across the lifespan.
The burgeoning field of gut-brain axis research is fundamentally reshaping the therapeutic landscape for neurodegenerative diseases (NDs). Traditionally, drug development has focused on direct interventions within the central nervous system (CNS), often targeting specific proteinopathies like amyloid-beta (Aβ) plaques in Alzheimer's disease (AD) or alpha-synuclein (α-synuclein) aggregates in Parkinson's disease (PD). However, the limited success of these approaches has prompted a paradigm shift. Growing evidence underscores the microbiota-gut-brain axis (MGBA) as a critical regulator of brain health and a novel therapeutic frontier [2] [3]. This in-depth technical guide provides a comparative analysis of the safety and efficacy profiles of conventional pharmacological agents versus emerging microbiome-targeting therapies, framing this discussion within the context of neurodegenerative disease research. It aims to equip researchers and drug development professionals with a mechanistic understanding, current evidence, and practical methodologies for advancing therapeutics in this rapidly evolving space.
The Microbiota-Gut-Brain Axis: A Primer for Neurodegeneration
The MGBA is a complex, bidirectional communication network linking the gastrointestinal tract, its resident microbiota, and the CNS through integrated neural, immune, endocrine, and metabolic pathways [2] [3]. Key communication routes include:
- Neural Pathways: The vagus nerve serves as a direct neural highway, transmitting signals from the gut lumen to the brainstem. Gut microbes can produce neurotransmitters (e.g., GABA, serotonin) or stimulate enteroendocrine cells to release neuroactive substances that influence vagal afferents [2] [3].
- Immune and Inflammatory Pathways: Gut dysbiosis can compromise intestinal barrier integrity, leading to increased circulation of microbial-associated molecular patterns (MAMPs) like lipopolysaccharide (LPS). These molecules can trigger systemic and neuroinflammation by activating microglia, the CNS's resident immune cells, via pattern recognition receptors such as Toll-like receptors (TLRs) [2] [3].
- Metabolic and Endocrine Pathways: Gut microbiota ferment dietary fiber to produce short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—which possess potent immunomodulatory and neuroactive properties. Microbes also bile acid metabolism and produce or influence a range of other bioactive metabolites and gut hormones (e.g., GLP-1) that can cross the blood-brain barrier or signal via the vagus nerve [103] [3].
In neurodegenerative diseases, a common finding is gut dysbiosis, characterized by reduced microbial diversity, depletion of beneficial SCFA-producing bacteria (e.g., Lachnospiraceae, Faecalibacterium), and enrichment of pro-inflammatory taxa [104] [8] [30]. This dysbiosis is thought to contribute to pathogenesis by driving chronic neuroinflammation, aggravating protein misfolding, impairing blood-brain barrier function, and disrupting peripheral immunity [2] [3].
Table 1: Key Microbial Alterations in Neurodegenerative Diseases
| Disease | Reported Microbial Shifts (vs. Healthy Controls) | Key Functional Implications |
|---|---|---|
| Alzheimer's Disease (AD) | ↑ Proteobacteria, Bifidobacterium; ↓ Firmicutes, Clostridiaceae, Lachnospiraceae [104] | Reduced SCFA production; increased inflammation |
| Parkinson's Disease (PD) | ↑ Akkermansia, Lactobacillus; ↓ Roseburia, Faecalibacterium, Blautia [104] | Altered mucin degradation; reduced anti-inflammatory SCFAs |
| Amyotrophic Lateral Sclerosis (ALS) | ↑ Bacteroidetes, Enterobacteriaceae; ↓ Lachnospiraceae [104] | Lower Firmicutes/Bacteroidetes ratio linked to cognitive impairment |
| Huntington's Disease (HD) | ↓ Firmicutes, Lachnospiraceae, Akkermansiaceae (in males) [104] | Loss of beneficial taxa; interaction with immune responses |
Conventional Drugs: Mechanisms, Efficacy, and Microbiome Interactions
Conventional CNS drugs primarily target neurotransmission or specific pathological protein aggregates. Meanwhile, many widely used non-CNS medications, taken chronically by patients, exert significant and often unintended effects on the gut microbiome, which may in turn influence neurological health [103] [105].
CNS-Targeting Drugs
Drugs like acetylcholinesterase inhibitors (e.g., donepezil) for AD or levodopa for PD represent the cornerstone of current neurological treatment. Their primary mechanisms are well-defined, but their efficacy is often symptomatic and does not halt disease progression.
- Efficacy: Typically, these drugs offer modest symptomatic benefits. For instance, acetylcholinesterase inhibitors may temporarily improve cognitive scores in AD, while levodopa effectively manages motor symptoms in PD but loses efficacy over time and causes dyskinesias.
- Safety: Their safety profiles are dominated by on-target CNS and peripheral side effects, such as gastrointestinal disturbances (nausea, diarrhea), dizziness, and sleep issues [103].
- Microbiome Interactions: Emerging evidence suggests these drugs may have bidirectional relationships with the gut microbiome. The microbiome can express enzymes that metabolize these drugs, potentially influencing their pharmacokinetics and efficacy (pharmacomicrobiomics) [105]. Conversely, the drugs may alter microbial composition, though this area requires further mechanistic investigation.
Non-CNS Drugs with Microbiome Impact
Several commonly prescribed systemic medications have been shown to significantly impact the gut microbiota, creating a potential indirect link to brain health [103] [105].
Table 2: Impact of Selected Non-CNS Conventional Drugs on the Gut Microbiome
| Drug Class | Example(s) | Reported Effects on Gut Microbiota | Potential Clinical Consequences |
|---|---|---|---|
| Metformin (Anti-diabetic) | Metformin | ↑ Akkermansia muciniphila, SCFA-producers (Bifidobacterium, Butyrivibrio); ↑ bile acid transformations [103] | Contributes to efficacy; GI side effects (diarrhea, bloating) may be linked to microbiota changes [103]. |
| Proton Pump Inhibitors (PPIs) | Omeprazole, Esomeprazole | ↑ Upper GI tract colonization; often ↓ microbial diversity [103] | May increase risk of infections and potentially influence nutrient absorption with long-term use. |
| Statins (Lipid-lowering) | Atorvastatin, Rosuvastatin | Modest modulation of composition; some studies report ↑ Akkermansia & Lactobacillus [103] | Pleiotropic effects may be partially mediated via microbiome. |
| Non-Steroidal Anti-inflammatory Drugs (NSAIDs) | Ibuprofen, Aspirin | Can inhibit growth of some Gram-positive and Gram-negative bacteria; may contribute to dysbiosis [103] | Microbiome disruption may be linked to GI mucosal injury. |
The field of pharmacomicrobiomics explores these interactions, positing that the gut microbiome acts as a "second genome" that contributes to individual variation in drug response (IVDR) by directly modifying drugs, altering host metabolism, or modulating the immune system [105].
Microbiome-Targeted Therapies: Mechanisms and Applications
Microbiome-targeted therapies offer a fundamentally different approach by aiming to restore a healthy, symbiotic gut ecosystem to exert beneficial effects on the host, including the brain.
Probiotics and Prebiotics
- Probiotics are live microorganisms that confer a health benefit to the host. Specific strains, often called psychobiotics, are selected for their neuroactive potential.
- Prebiotics are non-digestible food ingredients (e.g., specific fibers like FOS, GOS) that selectively stimulate the growth and/or activity of beneficial gut bacteria [8] [106].
Mechanism of Action: They work by:
- Strengthening the intestinal barrier, reducing microbial translocation and systemic inflammation.
- Producing neuroactive metabolites (SCFAs, neurotransmitters).
- Modulating the immune system (e.g., promoting regulatory T-cells) [8] [3].
Efficacy and Safety: Preclinical models show promise in reducing neuroinflammation, improving glymphatic clearance, and ameliorating cognitive and motor deficits [8]. Human trials are preliminary but show potential for alleviating cognitive and emotional symptoms. Safety is generally high in immunocompetent individuals, though effects can be transient and strain-specific [106].
Fecal Microbiota Transplantation (FMT)
FMT involves transferring processed fecal material from a healthy, screened donor into a patient's gastrointestinal tract to restore a healthy microbial community.
Mechanism of Action: It aims for a more comprehensive and durable restoration of gut microbial ecology and function compared to probiotics [104] [3].
Efficacy and Safety:
- Efficacy: In PD mouse models, FMT from healthy donors improved motor and GI function and reduced α-synuclein pathology [104]. In a study on HD mice, FMT improved cognitive function, albeit in a sex-specific manner [104]. Human trials are ongoing.
- Safety: Primary risks include transmission of pathogens, transient GI discomfort, and potential for long-term unknown consequences. It is a highly invasive procedure requiring rigorous donor screening [106].
Dietary Interventions
Diet is one of the most powerful modulators of gut microbiota composition and function.
- Mediterranean and Ketogenic Diets: These diets, rich in fiber, polyphenols, and healthy fats, promote microbial diversity and SCFA production [8] [30].
- Intermittent Fasting/Time-Restricted Feeding: These regimens can alter microbial communities and improve metabolic health, potentially benefiting the MGBA [30].
Mechanism of Action: Diets shape the microbial ecosystem, influencing the production of microbial metabolites that directly or indirectly influence brain function.
Efficacy and Safety: Epidemiological studies link healthy dietary patterns to reduced risk of NDs. Dietary interventions are generally safe but require adherence and can be challenging to implement.
Table 3: Comparative Analysis: Conventional vs. Microbiome-Targeted Therapies
| Feature | Conventional CNS Drugs | Non-CNS Drugs (e.g., Metformin) | Microbiome-Targeted Therapies |
|---|---|---|---|
| Primary Target | CNS receptors, enzymes, protein aggregates | Systemic targets (e.g., liver, pancreas) | Gut microbiota ecosystem & its metabolome |
| Typical Efficacy | Symptomatic, modest, often wanes over time | Effective for primary indication; microbiome effects can be secondary | Disease-modifying potential; effects can be broad & systemic |
| Major Safety Concerns | CNS side effects, peripheral off-target effects | Varies by class; can include GI effects (e.g., metformin) | Generally safe; FMT has risks of infection, unknown long-term effects |
| Onset of Action | Relatively rapid (hours-days) | Rapid for primary indication | Slower, may require weeks to months |
| Treatment Durability | Requires continuous dosing | Requires continuous dosing | Effects may persist post-treatment (especially FMT) |
| Personalization Potential | Pharmacogenomics | Pharmacogenomics & pharmacomicrobiomics | High—based on individual microbiome baseline |
Experimental Protocols for MGBA Research
Robust methodologies are essential for elucidating MGBA mechanisms and evaluating therapies.
In Vivo Modeling of the MGBA in Neurodegeneration
Protocol: Evaluating Microbiome-Targeted Therapies in a Murine Model of AD
- Animal Model Selection: Utilize transgenic models (e.g., APP/PS1, 5xFAD) or induce pathology via methods like intracerebroventricular Aβ injection [104].
- Treatment Groups:
- Healthy control + vehicle
- AD model + vehicle
- AD model + probiotic (e.g., specific Lactobacillus or Bifidobacterium strain)
- AD model + prebiotic (e.g., GOS/FOS mix)
- AD model + FMT from healthy wild-type donor
- (Optional) AD model + conventional drug (e.g., donepezil) for comparison.
- Intervention Duration: Administer treatment for 8-16 weeks via oral gavage (probiotics/prebiotics) or rectal/oral administration (FMT).
- Outcome Measures:
- Behavioral Cognition: Morris water maze, Y-maze, novel object recognition test.
- Neuropathology: Post-mortem brain analysis for Aβ plaque load, tau phosphorylation, glial activation (Iba1 for microglia, GFAP for astrocytes).
- Microbiome Analysis: Collect fecal samples pre-, mid-, and post-treatment for 16S rRNA gene sequencing or shotgun metagenomics.
- Metabolomics: LC-MS/MS on plasma and cecal content to quantify SCFAs, bile acids, and neurotransmitters.
- Gut & BBB Integrity: Measure inflammatory markers (IL-6, TNF-α) in plasma and colon; assess tight junction proteins (occludin, ZO-1) in colon and brain tissue [104] [3].
Human Clinical Trial Design
Protocol: A Phase II Randomized Controlled Trial of a Probiotic in PD
- Design: Double-blind, placebo-controlled, parallel-group trial.
- Participants: 100 patients with early-stage PD, stratified by age, sex, and baseline constipation status.
- Intervention: Daily multi-strain probiotic supplement vs. matched placebo for 6 months.
- Primary Endpoint: Change from baseline in MDS-UPDRS Part III (motor examination) score.
- Secondary Endpoints:
- Non-motor symptoms (e.g., constipation severity, quality of life scales).
- Gut microbiota composition (shotgun metagenomics on serial stool samples).
- Plasma levels of inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) and SCFAs.
- Fecal levels of calprotectin (gut inflammation).
- Statistical Analysis: ITT analysis with longitudinal models to compare the rate of change in endpoints between groups, adjusting for covariates. Correlation analysis between microbial shifts and clinical outcomes [8] [3].
Signaling Pathways and Workflow Visualization
The following diagrams illustrate key mechanistic pathways and experimental workflows in MGBA research.
Gut Microbiota to Brain Signaling Pathways
Gut-Brain Communication Pathways
Therapeutic Development Workflow
MGBA Therapeutic Development Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Models for MGBA Research in Neurodegeneration
| Item Category | Specific Examples | Function/Application |
|---|---|---|
| Animal Models | Transgenic mice (e.g., 5xFAD for AD, α-synuclein-overexpressing for PD), Germ-free (GF) mice, Antibiotic-treated mice [104] [3] | Modeling disease pathology; establishing causality in microbiome studies (GF mice). |
| Molecular Biology Kits | 16S rRNA gene sequencing kits, Shotgun metagenomics kits, RNA/DNA extraction kits (fecal, tissue), ELISA kits for cytokines (IL-6, TNF-α, IL-10) [104] | Profiling microbiome composition/function; measuring host inflammatory response. |
| Cell Culture Models | Primary microglia cultures, Immortalized cell lines (e.g., BV-2, Caco-2), Gut organoids [3] | Mechanistic studies on microglial activation, gut barrier function, and host-microbe interactions. |
| Analytical Standards | Short-Chain Fatty Acids (SCFAs: acetate, propionate, butyrate), Lipopolysaccharide (LPS), Neurotransmitters (GABA, serotonin), Bile acids [2] [3] | Quantification of key microbial and neuroactive metabolites via LC-MS/MS or GC-MS. |
| Intervention Reagents | Single-strain probiotics (e.g., Lactobacillus spp., Bifidobacterium spp.), Prebiotics (FOS, GOS, Inulin), Fecal Microbiota Transplantation (FMT) protocols [104] [8] [106] | Modulating the gut microbiome to assess therapeutic effects in models. |
The comparative analysis reveals a fundamental dichotomy: conventional drugs often offer targeted, rapid, but frequently symptomatic relief, while microbiome-targeted therapies present a more holistic, system-level approach with disease-modifying potential, albeit with a slower onset and a more complex mechanistic landscape. The future of neurodegenerative disease therapeutics lies not in choosing one over the other, but in developing an integrated approach. This includes:
- Personalized Medicine: Leveraging multi-omics data (metagenomics, metabolomics, host genomics) to stratify patients based on their "microbiomeotype" and predict responses to both conventional and microbiome-targeted interventions [105].
- Drug-Microbiome Combination Therapies: Designing trials that combine CNS drugs with specific microbiome modulators to enhance efficacy or mitigate side effects. For instance, co-administering a probiotic with metformin to reduce its GI intolerance [103] [105].
- Mechanism-Driven Discovery: Moving beyond correlations to establish causality using gnotobiotic models, precise bacterial consortia, and postbiotic (purified metabolite) administration [3] [106].
Understanding the intricate dialogue between conventional pharmacology and the gut microbiome will be paramount for developing the next generation of effective, safe, and personalized therapeutics for neurodegenerative diseases.
Conclusion
The microbiota-gut-brain axis represents a transformative paradigm in understanding and treating neurodegenerative diseases, moving beyond a neurocentric view to a systemic one. Key takeaways confirm that gut dysbiosis is a potent modulator of neuroinflammation, protein aggregation, and neuronal homeostasis through well-defined neural, immune, and metabolic pathways. While microbiome-targeted therapies show promising disease-modifying potential in pre-clinical models, their clinical translation requires overcoming significant hurdles, including patient stratification, biomarker validation, and intervention standardization. Future research must prioritize longitudinal human studies, the development of personalized microbial profiles, and the integration of multi-omics data to establish causal relationships. For the drug development community, targeting the MGBA offers a viable path to novel, potentially safer therapeutics that circumvent the blood-brain barrier, heralding a new era in precision neurology.
References
- 1. The Microbiota-Gut-Brain Axis [https://pubmed.ncbi.nlm.nih.gov/31460832/]
- 2. Microbiota–gut–brain axis in neurodegenerative diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436269/]
- 3. Microbiota–gut–brain axis and its therapeutic applications ... [https://www.nature.com/articles/s41392-024-01743-1]
- 4. what do we know about the microbiota-gut-brain axis? [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-016-0604-8]
- 5. The contribution of the brain-gut-microbiome axis to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12431638/]
- 6. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 7. Perturbations in the microbiota-gut-brain axis shaped by ... [https://www.nature.com/articles/s42003-025-07850-1]
- 8. The microbiota–gut–brain axis in mental and ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1667448/full]
- 9. Role of gut-microbiome-brain axis in neurodegenerative ... [https://www.sciencedirect.com/science/article/pii/S295058872500076X]
- 10. The enteric nervous system [https://www.sciencedirect.com/science/article/abs/pii/S0960982225010863]
- 11. Vagus Nerve [https://www.physio-pedia.com/Vagus_Nerve]
- 12. Neuroanatomy, Cranial Nerve 10 (Vagus Nerve) - StatPearls [https://www.ncbi.nlm.nih.gov/books/NBK537171/]
- 13. The microbiota-gut-brain axis and central nervous system ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1583562/full]
- 14. Quantitative Map of Proteome Dynamics during Neuronal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5316641/]
- 15. Vagus Nerve: What It Is, Function, Location & Conditions [https://my.clevelandclinic.org/health/body/22279-vagus-nerve]
- 16. Immune Signaling in Neurodegeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6822103/]
- 17. Innate immune activation in neurodegenerative diseases [https://www.sciencedirect.com/science/article/pii/S1074761324001316]
- 18. Microbiome–microglia connections via the gut–brain axis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6314531/]
- 19. The emerging role of microbiota derived SCFAs in ... [https://pubmed.ncbi.nlm.nih.gov/40502529/]
- 20. Gut-brain axis and neurodegeneration: mechanisms ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1481390/full]
- 21. Elucidating the specific mechanisms of the gut-brain axis [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03454-y]
- 22. Tryptophan Metabolism in Central Nervous System Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10187711/]
- 23. Evidence and Mechanism of Bile Acid-Mediated Gut-Brain ... [https://pubmed.ncbi.nlm.nih.gov/39566821/]
- 24. Evidence and Mechanism of Bile Acid–Mediated Gut-Brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0002944024004127]
- 25. Association of Gut Microbiome Dysbiosis with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8305650/]
- 26. Towards early detection of neurodegenerative diseases [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1087091/full]
- 27. Microbial signatures and therapeutic strategies in ... [https://pubmed.ncbi.nlm.nih.gov/39933444/]
- 28. How the gut microbiota impacts neurodegenerative diseases ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03371-0]
- 29. The Gut–Brain Axis and the Microbiome - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6999848/]
- 30. Microbial signatures and therapeutic strategies in ... [https://www.sciencedirect.com/science/article/pii/S075333222500099X]
- 31. The gut-brain connection: What the science says [https://med.stanford.edu/news/insights/2025/03/gut-brain-connection-long-covid-anxiety-parkinsons.html]
- 32. Trust Your Gut: Strategies and Tactics for Intestinally ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10009798/]
- 33. Bile acid metabolism and signaling in health and disease [https://www.nature.com/articles/s41392-024-01811-6]
- 34. Biological functions and pharmacological behaviors of bile ... [https://www.sciencedirect.com/science/article/pii/S2090123224004958]
- 35. Bile Acids: A Communication Channel in the Gut-Brain Axis [https://pubmed.ncbi.nlm.nih.gov/33085065/]
- 36. Bile acid receptors and signaling crosstalk in the liver, gut ... [https://www.sciencedirect.com/science/article/pii/S2542568421000453]
- 37. Unlocking gut-liver-brain axis communication metabolites [https://pmc.ncbi.nlm.nih.gov/articles/PMC11589602/]
- 38. Live biotherapeutic products: the importance of a defined ... [https://www.nature.com/articles/s12276-020-0437-6]
- 39. Probiotics as modulators of gut-brain axis for cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10912297/]
- 40. A comprehensive overview of the effects of probiotics ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1651965/full]
- 41. Next-generation probiotics: the upcoming biotherapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11018693/]
- 42. The microbiota-gut-brain axis in mental and ... [https://pubmed.ncbi.nlm.nih.gov/41104042/]
- 43. Gut microbiome-mediated health effects of fiber and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425962/]
- 44. The Synergistic Interplay between Vitamin A, Dietary Fiber ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622890/]
- 45. Impact of a High-Fat Diet on the Gut Microbiome [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940932/]
- 46. Study: Mediterranean diet changes gut bacteria, boosting ... [https://news.tulane.edu/pr/study-mediterranean-diet-changes-gut-bacteria-boosting-memory-and-cognition]
- 47. The long-term neuroprotective effect of MIND and ... [https://www.nature.com/articles/s41598-025-17055-5]
- 48. Neurobiochemical Effects of a High-Fat Diet [https://pubmed.ncbi.nlm.nih.gov/41154720/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=01YU7fcJp_MIS_6VsnGTBXsJMAUCpsaNdMo844gxrqi&fc=None&ff=20251029211758&v=2.18.0.post22+67771e2]
- 49. High fat diet and low dose-rotenone exposure exacerbate ... [https://www.sciencedirect.com/science/article/pii/S0014488625002481]
- 50. Fecal microbiota transplantation: Current evidence and ... [https://www.ccjm.org/content/92/7/421]
- 51. What's New and What's Next in Fecal Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377394/]
- 52. Live Biotherapeutic Products: Development, Investment, and ... [https://www.alacrita.com/whitepapers/live-biotherapeutic-products-development-challenges]
- 53. Human Microbiome Market & Therapeutic Pipeline 2025 [https://www.strategicmarketresearch.com/blogs/human-microbiome-market-clinical-trials-pipeline]
- 54. Long-term health outcomes in adolescents with obesity ... [https://www.nature.com/articles/s41467-025-62752-4]
- 55. Shaping the future of probiotics, live biotherapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527994/]
- 56. Gut–Brain Axis and Neurodegeneration: State-of-the-Art of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7312636/]
- 57. An integrated metagenomics and metabolomics approach ... [https://pubmed.ncbi.nlm.nih.gov/33249136/]
- 58. An integrated metagenomics and metabolomics approach ... [https://www.sciencedirect.com/science/article/pii/S0969996120304745]
- 59. ‐driven approaches for Metabolomics therapeutic identifying ... targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC11555024/]
- 60. Combined metagenomic and metabolomic analyses reveal ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1645137/full]
- 61. Integrating metabolomics and proteomics to identify novel drug ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-024-01395-4]
- 62. The Microbiota-Gut-Brain Axis: From Motility to Mood - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634751/]
- 63. Inter-individual variation shapes the human microbiome [https://www.cambridge.org/core/journals/behavioral-and-brain-sciences/article/interindividual-variation-shapes-the-human-microbiome/3612EF7918C1CAC6D17FA2A0DAF70B05]
- 64. Systems Biology Approaches to Understand the Host ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00716/full]
- 65. Therapeutics for neurodegenerative diseases by targeting the ... [https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-024-00404-1]
- 66. From gut to brain: understanding the role of microbiota in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1384270/full]
- 67. Blood–brain barrier - Wikipedia [https://en.wikipedia.org/wiki/Blood%E2%80%93brain_barrier]
- 68. The blood–brain barrier: Structure, regulation and drug delivery | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-023-01481-w]
- 69. The Blood Brain Barrier in Neurodegenerative Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC2761151/]
- 70. The blood-brain barrier in aging and neurodegeneration [https://www.nature.com/articles/s41380-022-01511-z]
- 71. Advancements in intestinally restricted drugs [https://accscience.com/journal/GPD/0/0/10.36922/gpd.5058]
- 72. Effects of microbiome-based interventions on ... [https://www.nature.com/articles/s41598-024-59250-w]
- 73. Tailoring the biomarkers of Alzheimer's disease using a gut ... [https://www.sciencedirect.com/science/article/abs/pii/S156816372500234X]
- 74. The Role of Gut Microbiota in Neurodegenerative Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10680305/]
- 75. Updates and Challenges in Fecal Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8455422/]
- 76. FMT: From clinical trials to market, where are we now? [https://www.gutmicrobiotaforhealth.com/fecal-microbiota-transplantation-from-clinical-trials-to-market-where-are-we-now/]
- 77. Emerging issues in probiotic safety: 2023 perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10026873/]
- 78. Statistical Approaches to Longitudinal Data Analysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5633048/]
- 79. Data-driven modelling of neurodegenerative disease ... [https://www.nature.com/articles/s41583-023-00779-6]
- 80. The Critical Role of Biomarkers for Drug Development ... [https://www.sciencedirect.com/science/article/pii/S2274580724001614]
- 81. Role of Disease Progression Models in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC9000925/]
- 82. From microbes to mind: germ-free models in neuropsychiatric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11481874/]
- 83. Quantitative patterns of motor cortex proteinopathy across ALS ... [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-020-00961-2]
- 84. Gut-induced alpha-Synuclein and Tau propagation initiate ... [https://www.sciencedirect.com/science/article/abs/pii/S0896627324005762]
- 85. Germ-free animal experiments in the gut microbiota studies [https://www.sciencedirect.com/science/article/abs/pii/S1471489219300219]
- 86. Getting closer to modeling the gut-brain axis using induced ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1146062/full]
- 87. Global quantitative analysis of the human brain proteome ... [https://www.nature.com/articles/s41597-020-00650-8]
- 88. Reverse engineering the Gut-Brain Axis and microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11556280/]
- 89. Molecular anatomy of the gut-brain axis revealed with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3728986/]
- 90. A comprehensive overview of the effects of probiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575349/]
- 91. Effects of Prebiotics and Probiotics on Symptoms ... [https://pubmed.ncbi.nlm.nih.gov/39731509/]
- 92. The role of probiotics, prebiotics, and synbiotics in ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1561047/full]
- 93. What's the Latest in Prebiotic Research? – August 2025 ... [https://prebioticassociation.org/whats-the-latest-in-prebiotic-research-august-2025-edition/]
- 94. Symptomatologic outcomes of gut microbiota modifiers ... [https://www.sciencedirect.com/science/article/pii/S1040842825001672]
- 95. Effects of probiotics, prebiotics, and synbiotics on gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482033/]
- 96. Faecal microbiota transplant for Parkinson's disease [https://pubmed.ncbi.nlm.nih.gov/41206012/]
- 97. Recent drug delivery systems targeting the gut-brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325006131]
- 98. Consensus statement on exploring the Nexus between nutrition, brain health and dementia prevention | Nutrition & Metabolism | Full Text [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-025-00981-6]
- 99. Effects of Dietary Interventions on Cognitive Outcomes [https://www.mdpi.com/2072-6643/17/12/1964]
- 100. Effects of combined dietary intervention and physical-cognitive exercise on cognitive function and cardiometabolic health of postmenopausal women with obesity: a randomized controlled trial | International Journal of Behavioral Nutrition and Physical Activity | Full Text [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-024-01580-z]
- 101. Plant-based diets and cognitive outcomes: a systematic ... [https://www.sciencedirect.com/science/article/pii/S2161831325001759]
- 102. Meta-analysis of the quantitative assessment of lower ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-024-01409-7]
- 103. Drugs Versus Microbiota: How Pharmacotherapy Affects Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472414/]
- 104. Therapeutics for neurodegenerative diseases by targeting the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10898075/]
- 105. Drug-microbiota interactions: an emerging priority for ... [https://www.nature.com/articles/s41392-023-01619-w]
- 106. Present and future of microbiome-targeting therapeutics [https://www.jci.org/articles/view/184323]