Strategies for Optimizing Dopamine Antagonist Dosing: Minimizing EPS, Akathisia, and Tardive Dyskinesia in Clinical Practice and Drug Development
This article provides a comprehensive analysis of contemporary strategies for optimizing doses of dopamine receptor antagonists (DRAs) to minimize motor side effects, including extrapyramidal symptoms (EPS), akathisia, and tardive dyskinesia.
Strategies for Optimizing Dopamine Antagonist Dosing: Minimizing EPS, Akathisia, and Tardive Dyskinesia in Clinical Practice and Drug Development
Abstract
This article provides a comprehensive analysis of contemporary strategies for optimizing doses of dopamine receptor antagonists (DRAs) to minimize motor side effects, including extrapyramidal symptoms (EPS), akathisia, and tardive dyskinesia. Targeted at researchers, scientists, and drug development professionals, it explores the neurobiological foundations of DRA-induced motor dysfunction, reviews current and emerging methodological approaches for dose titration and prediction, examines troubleshooting protocols for managing side effects, and validates optimization strategies through comparative analysis of novel compounds and delivery systems. The synthesis offers a roadmap for improving therapeutic windows in both existing treatments and future drug development.
Understanding the Neurobiology: Dopamine Receptor Antagonism and Motor Circuit Dysfunction
Technical Support Center
Troubleshooting Guide & FAQs
Q1: In our in vivo electrophysiology recordings, we observe inconsistent firing patterns in substantia nigra pars compacta (SNc) neurons following systemic antagonist administration. What could be the cause?
A: Inconsistent firing often stems from off-target effects or dose miscalibration. D1- and D2-receptor antagonists have distinct, sometimes opposing, effects on direct (D1-expressing) and indirect (D2-expressing) pathway medium spiny neurons (MSNs). Ensure precise targeting:
- Verify Specificity: Use highly selective antagonists (see Reagent Table). At low doses, off-target binding to other receptor types (e.g., 5-HT2, adrenergic) can confound results.
- Check Administration Route: Intraperitoneal (IP) injection can lead to variable bioavailability. Consider intracerebroventricular (ICV) or direct intrastriatal infusion for localized action. Always include vehicle controls.
- Monitor Vital Signs: Systemically administered antagonists can affect blood pressure and temperature, indirectly altering neuronal activity. Monitor and report these parameters.
Q2: Our behavioral assays (e.g., rotarod, open field) show high variability in motor impairment scores after antagonist dosing. How can we improve reproducibility?
A: High variability is common when optimizing doses to minimize side effects. Key factors are:
- Animal Factors: Standardize animal age, weight, and housing conditions. Diurnal cycles significantly influence basal dopamine tone; conduct experiments at the same time daily.
- Habitution: Animals must be thoroughly habituated to the testing apparatus (≥30 min/day for 3 days) to reduce anxiety-driven locomotion.
- Dose-Response Curve: Do not rely on a single dose. Use a minimum of 5 doses, spaced logarithmically, to establish a full curve. Include both a positive control (a known impairing dose) and a vehicle control.
- Temporal Window: Map the onset and duration of effect for your chosen antagonist. Perform behavioral tests within the drug's peak activity window.
Q3: When using immunohistochemistry to assess c-Fos expression as a marker of neuronal activity post-antagonist treatment, we see unexpected staining patterns in the striatum. How should we interpret this?
A: c-Fos expression in striatal MSNs is differentially regulated by D1 and D2 receptor signaling.
- D1 Antagonist Effect: Reduces activity in the direct pathway, leading to decreased c-Fos in D1-MSNs.
- D2 Antagonist Effect: Disinhibits the indirect pathway, leading to increased c-Fos in D2-MSNs.
Unexpected patterns may indicate:
- Insufficient Antagonist Selectivity: Your D1 antagonist may have partial D2-blocking activity, or vice versa, at the dose used.
- Compensatory Mechanisms: Chronic or high-dose treatment can trigger long-term adaptations (e.g., receptor upregulation).
- Fixation Issues: Ensure consistent perfusion and fixation times across all subjects.
Q4: What are the critical control experiments when testing a new dopamine receptor antagonist to isolate its motor side effect profile?
A: A robust control panel is essential for thesis-level research.
- Pharmacological Controls:
- Selective Agonist Rescue: Co-administer a selective D1 (e.g., SKF 81297) or D2 (e.g., Quinpirole) agonist to reverse deficits and confirm receptor mediation.
- Negative Control: Test an inactive enantiomer of the antagonist, if available.
- Behavioral Controls:
- Catalepsy Test: The gold standard for assessing drug-induced motor rigidity (a primary side effect).
- Spontaneous Locomotion vs. Skilled Motor Task: Use both (e.g., open field and beam walking) to distinguish general sedation from specific motor coordination deficits.
- Molecular Controls:
- Receptor Occupancy Assay: Use quantitative autoradiography or PET imaging to confirm target engagement at your tested doses.
Key Experimental Protocols
Protocol 1: Establishing a Dose-Response Curve for Akinesia Using the Rotarod Test Objective: To determine the ED₅₀ for motor coordination impairment induced by a novel D2 antagonist. Materials: Rotarod apparatus, test compounds, vehicle, stopwatch, rodent subjects. Procedure:
- Train animals on the rotarod at a constant speed (e.g., 16 rpm) until a stable baseline latency to fall is achieved (3-5 training sessions).
- Randomly assign animals to treatment groups (vehicle + 4-5 logarithmically spaced antagonist doses, n≥8/group).
- Administer compound via IP injection at a standardized volume (e.g., 5 mL/kg).
- Place animals on the rotarod 30 minutes post-injection (adjust based on drug pharmacokinetics).
- Record latency to fall over a maximum 300-second trial. Perform three trials with 15-minute rest intervals.
- Calculate mean latency for each animal. Express group data as percentage of vehicle control performance.
- Fit data using a four-parameter logistic (4PL) nonlinear regression model to determine ED₅₀ and confidence intervals.
Protocol 2: Assessing Striatal Pathway-Specific Activity via c-Fos Immunohistochemistry Objective: To visualize and quantify neuronal activity in direct vs. indirect pathways after acute antagonist treatment. Materials: Perfusion pump, fixative (4% PFA), cryostat, primary antibodies (anti-c-Fos, anti-DARP-32 or anti-ENK/SP for pathway identification), fluorescent secondary antibodies, confocal microscope. Procedure:
- Treat animals with antagonist or vehicle (n=4-6/group) and perfuse transcardially 90-120 minutes post-injection.
- Extract brains, post-fix for 24h, and cryoprotect in 30% sucrose.
- Section striatum (coronal, 40µm thickness) using a cryostat.
- Perform dual-label immunofluorescence: incubate sections in primary antibody cocktail (e.g., mouse anti-c-Fos + rabbit anti-Substance P for direct pathway; or rabbit anti-c-Fos + mouse anti-Enkephalin for indirect pathway) for 48h at 4°C.
- Incubate with appropriate fluorescent secondary antibodies (e.g., Alexa Fluor 488 and 594).
- Image using a confocal microscope. Quantify the number of c-Fos+ nuclei that are co-localized with each pathway-specific marker in standardized regions of interest (e.g., dorsomedial vs. dorsolateral striatum) using image analysis software (e.g., ImageJ/Fiji).
Table 1: Common Dopamine Receptor Antagonists & Typical Experimental Doses for Motor Studies
| Antagonist | Primary Target | Common In Vivo Dose Range (IP, mg/kg) | Key Behavioral Effect | Notes for Dose Optimization |
|---|---|---|---|---|
| SCH 23390 | D1-like | 0.01 - 0.1 | Mild hypolocomotion | High doses induce catalepsy via 5-HT2C binding. |
| SKF 83566 | D1 | 0.03 - 0.3 | Reduced grooming | More selective than SCH 23390. |
| Raclopride | D2-like | 0.1 - 3.0 | Catalepsy, akinesia | Gold standard for inducing parkinsonian side effects. ED₅₀ for catalepsy ~1.5 mg/kg. |
| Eticlopride | D2-like | 0.01 - 0.3 | Profound catalepsy | 10x more potent than raclopride. Use lower dose range. |
| L-741,626 | D2 | 1.0 - 10.0 | Moderate catalepsy | Selective for D2 over D3 receptors. |
| GR 103691 | D3 | 1.0 - 10.0 | Minimal acute motor effect | Used to isolate D3 contribution. |
Table 2: Expected Molecular & Behavioral Outcomes of Selective Antagonism
| Pathway / Receptor Blocked | Expected Change in Neuronal Activity | Behavioral Motor Readout (Acute) | c-Fos Expression Change |
|---|---|---|---|
| Direct Pathway (D1) | ↓ | Slight bradykinesia, reduced initiation | ↓ in striatonigral neurons |
| Indirect Pathway (D2) | ↑ | Akinesia, rigidity, catalepsy | ↑ in striatopallidal neurons |
| D1 + D2 (Combined) | ↓ Direct, ↑ Indirect | Severe, synergistic motor deficit | ↓ in D1-MSNs, ↑ in D2-MSNs |
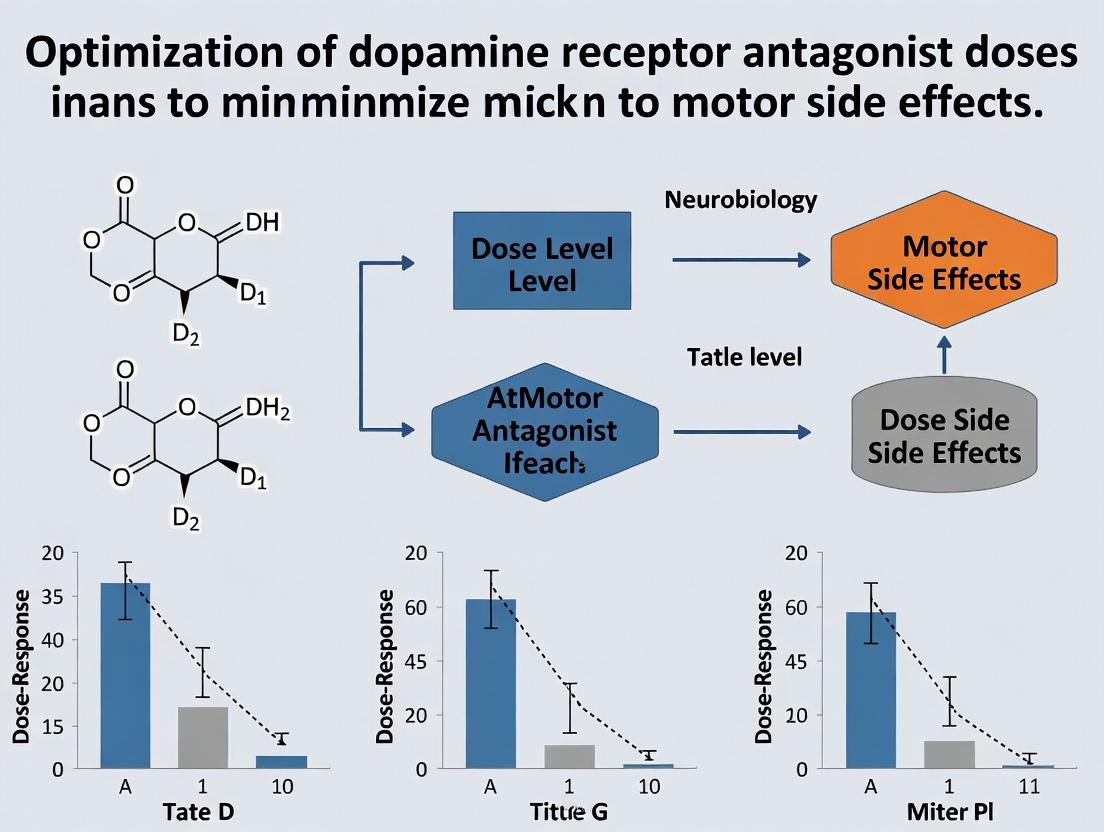
Diagrams
Diagram Title: Nigrostriatal Pathways & Dopamine Receptor Roles
Diagram Title: Experimental Workflow for Dose Optimization
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Role in Research | Example Product/Catalog # |
|---|---|---|
| Selective D1 Antagonist | To pharmacologically dissect the role of the direct pathway in motor control. Critical for establishing a baseline of D1-mediated effects. | SCH 39166 (aka Ecopipam), Tocris (Cat# 2281) |
| Selective D2 Antagonist | To induce and study parkinsonian side effects (catalepsy, akinesia). The primary tool for modeling motor side effects in rodents. | Raclopride tartrate, Sigma-Aldrich (Cat# R121) |
| Phospho-ERK1/2 Antibody | To assess downstream signaling activity in MSNs post-receptor blockade. pERK is a rapid, pathway-specific readout of neuronal activity. | Cell Signaling Technology, Phospho-p44/42 MAPK (Thr202/Tyr204) Antibody (Cat# 9101) |
| Fluorescent RNAscope Probe | For in situ hybridization of Drd1 and Drd2 mRNAs. Allows precise anatomical identification of direct vs. indirect pathway neurons without relying on protein markers. | ACD Bio, Mm-Drd1 (Cat# 461901) & Mm-Drd2 (Cat# 406501) |
| Microdialysis Kit | To measure extracellular dopamine and metabolite (DOPAC, HVA) levels in striatum in vivo following antagonist administration, linking receptor blockade to neurotransmitter dynamics. | CMA Microdialysis, 830 Series (e.g., 831 guide) |
| Catalepsy Test Apparatus | Standardized equipment (typically a horizontal bar or vertical grid) to quantitatively measure drug-induced muscular rigidity, a key extrapyramidal side effect. | San Diego Instruments, Catalepsy Test Kit (Bar Test) |
Technical Support Center: Troubleshooting & FAQs
FAQ: Dosing & Side Effect Onset
Q: In our rodent catalepsy assay (a proxy for acute EPS), we observe a steep dose-response curve. What is the recommended approach to establish a therapeutic window? A: This is a common challenge. The key is to perform parallel dose-response studies for both the desired central activity (e.g., apomorphine-induced climbing antagonism for antipsychotic effect) and the motor side effect (e.g., bar catalepsy). The latest meta-analyses suggest that for typical antipsychotics, the ED50 for catalepsy often lies within 0.5-2.5x the ED50 for antipsychotic-like efficacy, leaving a narrow window. Quantitative data from recent studies (2023-2024) on representative antagonists are summarized below.
Table 1: Comparative ED50 Values for Efficacy vs. Acute EPS (Catalepsy) in Rodent Models
| Dopamine D2 Antagonist | ED50 for APO-Climb Antag. (mg/kg, sc) | ED50 for Bar Catalepsy (mg/kg, sc) | Catalepsy Ratio (ED50 Cat/ED50 APO) |
|---|---|---|---|
| Haloperidol | 0.08 - 0.12 | 0.3 - 0.5 | ~3.5 |
| Risperidone | 0.15 - 0.25 | 2.5 - 4.0 | ~16.0 |
| Aripiprazole | 1.0 - 3.0 | >10 (atypical) | >10 |
Protocol: Parallel Dose-Response Assay
- Animals: Randomize rats or mice into groups (n=8-10).
- Dosing: Administer test compound subcutaneously at logarithmic doses (e.g., 0.1, 0.3, 1, 3 mg/kg) and vehicle.
- Catalepsy Testing (60 min post-dose): Place animal's forepaws on a horizontal bar (4 cm high). Record the time immobile (descent latency) with a 30s cutoff. Perform triplicate trials.
- APO-Climb Test (30 min post-dose): Inject apomorphine (1 mg/kg, sc). Place animal in a cylindrical wire-mesh cage. Score climbing behavior (all four paws on cage) every 5 min for 30 min.
- Analysis: Calculate % maximal catalepsy and % inhibition of climbing. Determine ED50 values using nonlinear regression (four-parameter logistic model).
Q: Our cell-based assay shows high D2R occupancy, but in vivo, we see no acute EPS. What other receptor profiles should we investigate to explain this dissociation? A: This likely indicates engagement of mitigating receptor systems. Prioritize profiling against serotonin 5-HT1A and 5-HT2A receptors. Agonism at 5-HT1A and antagonism at 5-HT2A are strongly associated with reduced EPS liability. A high 5-HT2A/D2 binding ratio is a historical predictor of low acute EPS. Include muscarinic M1 affinity as well, as anticholinergic activity can mask EPS.
FAQ: Tardive Dyskinesia (TD) Models & Mechanisms
Q: What is the most validated preclinical model for investigating tardive dyskinesia pathogenesis, and what is the critical dosing regimen? A: The VMAT2 inhibitor (tetrabenazine) model is preferred for its reversibility and face validity. Chronic dopamine depletion followed by D2 antagonist treatment is also used. The key is prolonged exposure, not single high doses.
Protocol: Chronic TD Model in Rodents
- Animals: Rats (preferred for orofacial movements).
- Dosing Regimen: Administer the D2 antagonist (e.g., Haloperidol) via subcutaneous osmotic minipump or daily intraperitoneal injection for 3-6 weeks. A common dose is 1.0 mg/kg/day of haloperidol decanoate.
- Vacuous Chewing Movements (VCMs) Assessment: In week 4, begin weekly assessments. Place rat in a clear plexiglass chamber for a 10-minute habituation, followed by a 2-minute video recording period under blind conditions. Count spontaneous VCMs (mouth openings in the vertical plane not directed at physical material).
- Validation: A significant increase in VCMs in the treatment group vs. vehicle control by week 6 indicates dyskinetic behavior.
Q: Our transcriptomic analysis of striatal tissue from a chronic model shows dysregulation. Which signaling pathways should we prioritize for diagramming? A: Focus on the dysregulated D1R (direct) and D2R (indirect) pathway crosstalk, and the downstream mTOR/ΔFosB axis, which is central to current TD pathophysiology theories.
Pathway to Tardive Dyskinesia in Chronic Model
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for DRA Motor Side Effect Research
| Item & Supplier Example | Function in Research |
|---|---|
| Selective D2 Ligand (e.g., Raclopride, Sigma-Aldrich) | Radioligand for receptor occupancy studies in vivo (PET) and in vitro. |
| VMAT2 Inhibitor (e.g., Tetrabenazine, Tocris) | Induces reversible dopamine depletion to model TD-predisposing state. |
| Apomorphine Hydrochloride (Cayman Chemical) | Dopamine agonist used to elicit stereotypy (climbing) for efficacy assays. |
| Osmotic Minipumps (Alzet) | Enables continuous, chronic subcutaneous drug delivery for TD models. |
| Phospho-specific Antibodies (p70S6K, p-rpS6) (Cell Signaling Tech.) | Detect activation of the mTOR pathway in striatal immunohistochemistry/Western blot. |
| ΔFosB Antibody (Santa Cruz Biotechnology) | Marker for chronic neuronal adaptation in striatum. |
| Automated Video Tracking System (Noldus EthoVision) | Quantifies locomotor activity and catalepsy descent latency with high objectivity. |
Q: When measuring receptor occupancy ex vivo, what is the critical time point for sacrifice relative to dosing to accurately correlate with behavioral EPS? A: Sacrifice time is paramount. For correlating with peak catalepsy (acute EPS), sacrifice animals at the Tmax of the compound (typically 30-60 min post-sc injection for many DRAs). For occupancy related to TD mechanisms, measure at trough levels during chronic dosing to understand baseline striatal adaptation.
Occupancy-Behavior Correlation Workflow
Technical Support & Troubleshooting Hub
Context: This resource is part of a broader research thesis on Optimizing dopamine receptor antagonist doses to minimize motor side effects. The following guides address common experimental challenges in quantifying and interpreting D2 receptor occupancy (D2RO).
FAQs & Troubleshooting Guides
Q1: Our PET imaging data shows high inter-subject variability in D2RO despite controlled dosing. What are the primary sources of this variability? A: High variability often stems from:
- Radioligand Selection: Using a non-selective radioligand (e.g., [¹¹C]raclopride for D2/D3) in brain regions with high D3 density. Solution: Validate with a more selective D2 ligand (e.g., [¹¹C]FLB 457 for extrastriatal regions) or perform blocking studies.
- Reference Region Integrity: The cerebellum, often used as a reference region, may exhibit off-target binding or pathology in your cohort. Solution: Confirm the absence of significant D2/D3 receptors in the reference region via post-mortem data or use a simplified reference tissue model with careful validation.
- Pharmacokinetic Factors: Differences in metabolism, plasma protein binding, or blood-brain barrier permeability affecting drug availability. Solution: Correlate D2RO with free plasma drug concentration, not just administered dose.
Q2: When establishing an occupancy-efficacy curve, our clinical correlation is weak. How can we improve the predictive power of our imaging data? A: This indicates a potential disconnect between central occupancy and clinical measure.
- Troubleshooting Step: Ensure temporal alignment. Peak receptor occupancy may not coincide with the timing of your clinical assessment. Protocol: Perform serial PET scans at Tmax (peak plasma concentration) and at trough (just before next dose) to model the occupancy-time relationship.
- Key Experiment Protocol - Occupancy-Response Lag Analysis:
- Administer a stable, fixed dose of the antagonist to patient cohort (n>20).
- Conduct [¹¹C]raclopride PET scans at: (i) 2-4 hours post-dose (peak), (ii) 12 hours post-dose, and (iii) 24 hours post-dose (trough).
- Measure clinical efficacy (e.g., PANSS score) simultaneously with each scan.
- Plot occupancy vs. clinical score for each time point. The strongest correlation indicates the pharmacologically relevant timepoint for assessment.
Q3: How do we reliably differentiate the occupancy threshold for efficacy from the threshold for inducing motor side effects like akathisia? A: This requires parallel measurement in distinct brain regions.
- Core Principle: Therapeutic efficacy is primarily linked to D2 blockade in mesolimbic pathways (e.g., ventral striatum), while motor side effects (EPS) are linked to blockade in the nigrostriatal pathway (dorsal striatum).
- Experimental Protocol - Differential Occupancy Mapping:
- Subject Grouping: Include a patient group on stable therapy with good efficacy/no EPS, and a group experiencing EPS.
- Imaging: Perform high-resolution PET with [¹¹C]raclopride.
- ROI Analysis: Quantify D2RO separately in the ventral striatum (limbic) and dorsal putamen (motor).
- Analysis: Calculate the Occupancy Differential (Dorsal RO - Ventral RO). A high positive differential (>15%) is strongly predictive of EPS risk.
Table 1: Empirical D2 Receptor Occupancy Thresholds for Antipsychotics
| Outcome | Brain Region | Typical Threshold Range | Notes & Variability Sources |
|---|---|---|---|
| Clinical Efficacy | Ventral Striatum / Limbic Cortex | 65% - 80% | Lower for partial agonists (e.g., Aripiprazole: ~50-70%). Threshold lower in first-episode psychosis. |
| Prolactin Elevation | Pituitary (Tuberoinfundibular) | 70% - 75% | Early marker of D2 blockade. Highly drug-dependent due to BBB penetration differences. |
| Extrapyramidal Symptoms (EPS) | Dorsal Striatum (Putamen) | >78% - 82% | Risk increases steeply above 80%. Inter-patient sensitivity varies based on neuronal adaptation. |
| Hyperprolactinemia | Pituitary | >72% - 78% | Sustained occupancy above threshold leads to clinical symptomology. |
Table 2: Common Radioligands for D2RO Studies
| Radioligand | Primary Target | Optimal Use Case | Key Limitation |
|---|---|---|---|
| [¹¹C]Raclopride | D2/D3 (antagonist) | Striatal occupancy, dose-finding studies. | Low signal-to-noise in extrastriatal regions; binds D3. |
| [¹¹C]FLB 457 | D2/D3 (antagonist) | High-affinity for extrastriatal/low-density regions (cortex, thalamus). | Vulnerable to changes in cerebral blood flow; requires long scan time. |
| [¹⁸F]Fallypride | D2/D3 (antagonist) | High-resolution whole-brain D2 mapping (striatal & extrastriatal). | Long half-life allows longer scans but increases subject burden. |
| [¹¹C]PHNO | D2/D3 (agonist) | Measuring "high-affinity state" D2 receptors; believed to be more functionally relevant. | Binding is highly sensitive to endogenous dopamine tone. |
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in D2RO Research |
|---|---|
| Selective D2/D3 Radioligands ([¹¹C]Raclopride) | Enables quantitative in vivo imaging of receptor availability before and after drug administration. |
| High-Affinity Antagonist (e.g., Haloperidol) | Used in pre-blocking studies to determine non-specific binding for PET modeling. |
| Reference Tissue (e.g., Cerebellum) | Serves as a region devoid of specific D2/D3 receptors, simplifying kinetic modeling without arterial blood sampling. |
| PET Image Analysis Software (PMOD, SPM) | For coregistration, atlas-based region-of-interest (ROI) definition, and kinetic modeling (e.g., SRTM) to calculate Binding Potential (BP) and D2RO. |
| Validated Clinical Scales (SAS, PANSS) | Standardized tools to quantify motor side effects (Simpson-Angus Scale) and psychiatric efficacy, enabling correlation with occupancy data. |
Experimental Workflow & Pathway Diagrams
Title: D2 Antagonist Action Path from Dose to Clinical Outcomes
Title: D2 Receptor Antagonism Signaling Pathway
Title: D2RO and Motor Side Effect Assessment Protocol
Troubleshooting Guide & FAQs
Q1: During dose-response experiments for D2 antagonists, we observe high variability in motor side effect onset (e.g., catalepsy) between young and aged rodent models, complicating dose optimization. What are the primary experimental factors to check? A1: First, verify pharmacokinetic parameters. Age-related changes in liver metabolism and blood-brain barrier permeability can alter drug bioavailability. Implement the following protocol:
- Plasma & Brain Concentration Assay: Euthanize cohorts (n=8 per age group) at T=30, 60, 120, 240 minutes post-injection. Collect plasma and homogenize brain tissue in acidified methanol. Quantify antagonist concentration via LC-MS/MS using an internal standard.
- Data Normalization: Express motor scores (e.g., bar test duration) as a function of striatal drug concentration, not just administered dose.
- Check Comorbid Pathology: Screen aged subjects for spontaneous neurodegeneration. Perform a quick post-mortem immunohistochemistry for α-synuclein (for Lewy body pathology) and Iba1 (for microgliosis) on a subset of high-variability subjects.
Q2: Our genotyping for DRD2 Taq1A (rs1800497) and GRIN2B (rs7301328) polymorphisms shows inconsistent correlation with extrapyramidal symptom (EPS) severity in our cohort. How should we adjust our protocol? A2: This suggests polygenic risk. Move beyond single SNPs.
- Shift to Polygenic Risk Score (PRS): Use microarray or NGS data to calculate a PRS incorporating variants in DRD2, ANKK1, GRIN2A, GRIN2B, COMT, and CYP2D6. Standardize the PRS for your population.
- Functional Assay Correlation: For subjects with high PRS but low EPS (or vice-versa), run an ex vivo receptor binding assay on fibroblast-derived neurons or post-mortem tissue to measure actual D2 receptor density (Bmax) and affinity (Kd).
- Protocol - Saturation Binding Assay: Homogenize striatal tissue. Incubate with increasing concentrations of [3H]raclopride (0.1-10 nM) with/without 10 µM sulpiride (to define non-specific binding). Filter and count radioactivity. Analyze data with Scatchard plot to derive Bmax and Kd.
Q3: When modeling comorbid Parkinson's Disease (PD) in animals receiving antagonists, we face confounding severe motor worsening. How can we design a dose-finding study that is still informative? A3: Employ a stepped, biomarker-driven approach.
- Pre-Dose Baseline Characterization: Quantify baseline dopaminergic deficit via [18F]DOPA PET imaging or CSF homovanillic acid levels. Stratify subjects into severity tiers.
- Microdosing Start: Begin antagonist administration at 1/50 of the standard effective dose. Use intracerebral microdialysis to monitor real-time changes in striatal glutamate, not just dopamine.
- Titrate Against Electrophysiology: Titrate doses weekly, using beta-band (13-30 Hz) oscillatory power in the subthalamic nucleus (measured via implanted electrodes or acute recordings) as a proxy for network dysfunction. Aim to avoid exceeding 130% of baseline beta power.
Summarized Quantitative Data
Table 1: Impact of Age on Pharmacokinetics of Haloperidol in Rodent Models
| Parameter | Young Adult (3 months) | Aged (22 months) | Change | Measurement Method |
|---|---|---|---|---|
| Plasma Half-life (t½) | 1.8 ± 0.3 hrs | 3.5 ± 0.6 hrs | +94% | LC-MS/MS |
| Brain-to-Plasma Ratio | 12.5 ± 1.8 | 18.2 ± 2.7 | +46% | LC-MS/MS of homogenates |
| Striatal D2 Occupancy (at 0.1 mg/kg) | 68 ± 5% | 85 ± 7% | +25% | Ex vivo autoradiography |
| ED50 for Catalepsy | 0.25 mg/kg | 0.12 mg/kg | -52% | Bar test, 30min post-inj. |
Table 2: Genetic Polymorphism Association with EPS Incidence in Clinical Cohort (Hypothetical Meta-Analysis Data)
| Gene | SNP | Risk Allele | Odds Ratio for EPS (95% CI) | P-value | Notes |
|---|---|---|---|---|---|
| DRD2 | rs1800497 (Taq1A) | A1 | 1.45 (1.20-1.75) | 3.2e-05 | Affects D2 density in striatum |
| ANKK1 | rs2734849 | C | 1.30 (1.08-1.56) | 0.006 | In linkage disequilibrium with Taq1A |
| GRIN2B | rs7301328 | G | 1.60 (1.32-1.94) | 1.1e-06 | Encodes NMDA receptor GluN2B subunit |
| CYP2D6 | rs3892097 | T (PM) | 2.10 (1.70-2.59) | 4.5e-10 | Poor metabolizer phenotype |
| COMT | rs4680 (Val158Met) | Val | 1.15 (0.98-1.35) | 0.089 | Moderate effect on prefrontal dopamine |
Experimental Protocols
Protocol 1: Integrated In Vivo Protocol for Dose Optimization Against Risk Factors Title: Simultaneous EEG-EMG and Microdialysis in an Aged Rodent Model. Objective: To correlate local neurochemistry with network and motor output following antagonist challenge. Steps:
- Surgery: Implant a guide cannula targeting the striatum and EEG electrodes over sensorimotor cortex. Insert EMG wires into biceps femoris.
- Recovery & Habituation: Allow 7 days recovery, then habituate to recording chamber for 3 days.
- Baseline Recording: Insert microdialysis probe, perfuse with aCSF (1 µL/min). Collect 20-min fractions. Simultaneously record baseline EEG/EMG for 1 hour.
- Drug Challenge: Administer candidate antagonist dose (i.p.). Continue neurochemical and electrophysiological recording for 3 hours.
- Analysis: Quantify glutamate/dopamine via HPLC in dialysates. Compute EEG power spectra (focus 4-30 Hz) and EMG root mean square for corresponding epochs. Derive cross-correlation metrics.
Protocol 2: Ex Vivo D2 Receptor Autoradiography on Post-Mortem Human Brain Tissue Objective: To quantify D2 receptor availability in subjects with known genotype and medication history. Steps:
- Tissue Preparation: Obtain fresh-frozen striatal sections (20 µm thickness) from a brain bank. Store at -80°C.
- Pre-incubation: Thaw and air-dry sections. Pre-incubate in Tris-HCl buffer (50 mM, pH 7.4) for 30 min at room temperature to remove endogenous ligands.
- Incubation: Incubate sections with 2 nM [3H]raclopride in buffer for 60 min at RT. Include adjacent sections with 10 µM (+)-butaclamol to define non-specific binding.
- Washing & Exposure: Rinse twice in cold buffer (2 min each), dip in cold distilled water, and air-dry. Expose to tritium-sensitive film alongside radioactive standards for 4-6 weeks.
- Quantification: Digitize films. Convert optical density to receptor density (fmol/mg tissue equivalent) using standard curve from co-exposed radioactivity standards.
Visualizations
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application | Example Product/Catalog |
|---|---|---|
| Selective D2 Antagonist (Radiolabeled) | High-affinity ligand for ex vivo/in vitro receptor binding and autoradiography to quantify D2 occupancy. | [3H]Raclopride, [11C]Raclopride (for PET) |
| CYP2D6 Activity Assay Kit | Phenotype subject metabolic capacity from liver microsomes or recombinant enzymes to account for PK variability. | Vivid CYP2D6 Fluorometric Screening Kit |
| Multiplex SNP Genotyping Panel | Simultaneously genotype key polymorphisms (DRD2, ANKK1, GRIN2B, COMT, CYP2D6) for polygenic risk scoring. | TaqMan SNP Genotyping Assays |
| In Vivo Microdialysis Kit | Monitor real-time changes in striatal neurotransmitters (DA, Glu, GABA) in response to drug challenge. | CMA 7 or 12 Guide Cannula & Probes |
| Wireless EEG/EMG Telemetry System | Record neural oscillatory activity and muscle tone in freely moving animals post-drug administration. | DSI or Neurologger systems |
| α-Synuclein & Iba1 Antibodies | Immunohistochemical detection of comorbid Lewy pathology and neuroinflammation in aged models. | Phospho-Synuclein (pS129) Antibody, Anti-Iba1 (ab178846) |
| LC-MS/MS Internal Standard | Stable isotope-labeled drug analog for precise, matrix-corrected quantification of drug levels in plasma/brain. | Haloperidol-d4, Risperidone-d4 |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: In our catalepsy test, we observe high variability in response to a fixed dose of haloperidol across different mouse strains. What could be the cause and how can we optimize our model? A1: Genetic variability in serotonin (5-HT2A) and muscarinic (M4) receptor expression significantly impacts DRA-induced motor side effects. To optimize:
- Pre-screen Strains: Use Western blot or qPCR to baseline expression levels of 5-HT2A and M4 receptors in the striatum of your candidate strains.
- Utilize Pharmacological Probes: Administer a subthreshold dose of a 5-HT2A antagonist (e.g., M100907, 0.1 mg/kg) or a positive allosteric modulator of the M4 receptor prior to DRA administration. A reduced catalepsy response in one strain confirms a stronger modulatory tone in that pathway.
- Recommended Adjustment: Select the strain showing intermediate sensitivity for dose-response studies to avoid floor or ceiling effects.
Q2: When co-administering glutamate NMDA receptor modulators with our DRA to mitigate side effects, we see paradoxical worsening of akinesia in some subjects. How should we troubleshoot this? A2: This likely indicates an imbalance in NMDA receptor modulation. Excessive blockade or dysregulated enhancement can disrupt corticostriatal feedback loops.
- Check Your Compound: Verify the specificity and dose of your NMDA modulator. Use low, sub-anesthetic doses of an NMDA channel blocker (e.g., memantine, 1-5 mg/kg) or a glycine-site partial agonist.
- Timing is Critical: Administer the modulator 30 minutes post-DRA, not concurrently. Concurrent administration can acutely exacerbate dysfunction.
- Assess Locomotion in Phases: Use an open field test to distinguish between reduced locomotion (akinesia) and increased muscular rigidity. This data will clarify if the issue is primarily motor or involves increased rigidity.
Q3: Our in vivo microdialysis shows inconsistent changes in striatal glutamate following DRA administration. What are the key protocol points to ensure reliable data? A3: Consistency in probe placement and post-surgical recovery is paramount.
- Protocol Verification:
- Coordinates: Double-check stereotaxic coordinates for the anterior striatum (e.g., Bregma: +1.0 mm AP, ±2.2 mm ML, -3.5 mm DV in rats). Use a fresh brain slice after sacrifice to confirm placement.
- Recovery: Allow a minimum of 24-48 hours post-probe implantation before starting experiments to normalize glial reactivity and baseline neurotransmitter levels.
- Perfusate: Use an artificial cerebrospinal fluid (aCSF) containing 3 mM glucose, pH 7.4, perfused at a constant 1.0 µL/min. Equilibrate the system for 60-90 minutes before sample collection.
- Positive Control: Include a group receiving a high-dose NMDA antagonist to confirm the system can detect a large glutamate increase.
Table 1: Efficacy of Adjunctive Agents in Reducing DRA-Induced Catalepsy in Rodents
| Adjunctive Agent (Class) | Example Compound | Effective Dose Range | % Reduction in Catalepsy vs. DRA alone | Key Receptor Target |
|---|---|---|---|---|
| 5-HT2A Antagonist | M100907 | 0.1 - 0.5 mg/kg | 40-60% | 5-HT2A Receptor |
| mGluR2/3 Agonist | LY354740 | 1 - 3 mg/kg | 30-50% | Metabotropic Glutamate Receptor 2/3 |
| M4 PAM | VU0467154 | 3 - 10 mg/kg | 50-70% | Muscarinic M4 Receptor |
| NMDA Receptor Glycine-Site Agonist | D-cycloserine | 10 mg/kg | 20-30% | NMDA Receptor Glycine Site |
Table 2: Recommended DRA Dose Optimization Protocol (Rodent)
| Step | Assay | Primary Readout | Goal |
|---|---|---|---|
| 1. Baseline DRA Response | Catalepsy Bar Test | Time immobile (sec) | Establish ED50 for motor side effect. |
| 2. Adjunctive Modulator Titration | Open Field + Catalepsy | Locomotor counts & immobility time | Find dose of modulator that reverses DRA effect without inducing hyperlocomotion. |
| 3. Validation of Specificity | Radioligand Binding / Western Blot | Receptor occupancy or expression | Confirm target engagement of adjunctive modulator. |
| 4. Functional Rescue | Electrophysiology (ex vivo) | Striatal MSN firing rate | Demonstrate normalization of neuronal activity. |
Experimental Protocol: Assessing Synergistic Modulation
Title: Integrated Protocol for Evaluating 5-HT2A/M4 Synergy on DRA-Induced Akathisia. Objective: To determine if combined subthreshold modulation of 5-HT2A and M4 receptors synergistically reduces DRA-induced motor agitation. Materials: Animals, DRA (e.g., Haloperidol), 5-HT2A antagonist (M100907), M4 PAM (VU0467154), open field apparatus, video tracking software. Method:
- Randomize subjects into 6 groups (n=8-10): Vehicle, DRA only, DRA + low M100907, DRA + low VU0467154, DRA + combination (low M100907 + low VU0467154), combination only.
- Administer DRA (dose at ED50 for inducing increased locomotion) intraperitoneally (i.p.).
- At T+20 minutes, administer vehicle, M100907 (0.05 mg/kg, i.p.), VU0467154 (1 mg/kg, i.p.), or the combination.
- At T+40 minutes, place each subject in the open field for a 30-minute session.
- Primary Analysis: Quantify total distance traveled and repetitive ambulatory patterns (corner-to-corner transitions).
- Statistical Analysis: Use two-way ANOVA followed by post-hoc tests to compare the combination group against all others.
Research Reagent Solutions
Table 3: Essential Reagents for Mechanistic Studies
| Item | Function | Example Product/Catalog # |
|---|---|---|
| Selective 5-HT2A Antagonist | To probe serotonin system's mitigating role in EPS. | M100907 (Tocris, cat. # 1009) |
| M4 Positive Allosteric Modulator (PAM) | To enhance muscarinic M4 receptor signaling without peripheral side effects. | VU0467154 (Hello Bio, cat. # HB6124) |
| mGluR2/3 Agonist | To modulate presynaptic glutamate release. | LY354740 (Abcam, cat. # ab120241) |
| Phospho-Specific Antibody (pERK1/2) | To map downstream signaling changes in striatal pathways post-DRA & modulation. | Anti-Phospho-p44/42 MAPK (Cell Signaling, cat. # 4370) |
| FosB/ΔFosB Antibody | To label chronically activated striatal neurons. | Anti-FosB (Santa Cruz, cat. # sc-48) |
| In vivo Microdialysis Kit | For measuring real-time glutamate, dopamine, and serotonin in striatum. | CMA 7 Guide Cannula & Probe (Harvard Apparatus) |
Signaling Pathways and Workflows
Precision Dosing in Practice: From Therapeutic Drug Monitoring to Predictive Models
Troubleshooting Guides & FAQs
Q1: Our HPLC-MS/MS assay for haloperidol shows inconsistent recovery rates and high background noise. What could be the cause and solution? A: Inconsistent recovery often stems from improper sample preparation. Ensure protein precipitation is complete using a 3:1 ratio of cold acetonitrile to plasma. Vortex for 2 minutes, then centrifuge at 15,000 x g for 10 minutes at 4°C. High background noise in MS/MS is frequently due to ion suppression or mobile phase contaminants. Use a stable isotope-labeled internal standard (e.g., Haloperidol-d4). Purify all solvents (water, methanol) through 0.22 µm filters. Perform a post-column infusion experiment to identify the exact retention time of ion suppression and adjust the gradient elution to shift the analyte away from that region.
Q2: When establishing a population pharmacokinetic (PopPK) model for risperidone and its active metabolite, 9-hydroxyrisperidone, our model fails to converge. How should we proceed? A: Non-convergence often indicates over-parameterization or issues with initial estimates. First, ensure your structural model is sound. A one-compartment model for both parent and metabolite with first-order metabolism and elimination is typical. Use a stepwise approach:
- Fit the parent drug data alone.
- Fix those parameters, then fit the metabolite data.
- Perform a full model fit using the previous estimates. For initial estimates, consult literature: Risperidone typical clearance (CL) is ~5-8 L/h, volume of distribution (Vd) is ~1-2 L/kg. For inter-individual variability, start with a diagonal matrix (OMEGA) with values of 0.1-0.3 (CV ~30-50%). Use software diagnostic plots (e.g., conditional weighted residuals vs. time/predictions) to identify structural model misspecification.
Q3: We observe poor correlation between plasma levels of amisulpride and its clinical effect (PANSS score reduction) in our cohort. Is TDM still valid for this drug? A: Yes, but consider these factors. Amisulpride has a relatively flat dose-response curve for psychosis in its therapeutic range (200-800 mg/day). The poor correlation may be due to:
- Delayed Clinical Response: PANSS improvements lag behind steady-state plasma concentrations by several weeks. Align your pharmacokinetic sampling with appropriate clinical assessment timelines (e.g., 4-6 weeks after dose stabilization).
- High Inter-patient Variability in Pharmacodynamics: Genetic polymorphisms in dopamine D2/D3 receptors (e.g., DRD2 Taq1A) can affect drug response. Consider genotyping your cohort as a covariate in your exposure-response model.
- Narrow Therapeutic Window for Side Effects: The correlation with motor side effects (e.g., serum prolactin elevation, akathisia) is often stronger. TDM is crucial to maintain levels below the extrapyramidal symptom (EPS) threshold while ensuring efficacy.
Q4: What is the optimal sampling strategy for a limited sampling model (LSM) to estimate the AUC of olanzapine in patients?
A: For olanzapine, which has a long half-life (~30 hours) and achieves stable levels, trough sampling (just before the next dose) is often sufficient for routine TDM. However, for precise AUC estimation in research, a two-point LSM is validated. Collect samples at 2-4 hours post-dose (approximating Cmax) and at trough (24h post-dose). The following equation is commonly used:
AUC0-24 ≈ (Cmax + Ctrough)/2 * 24
Ensure patients are at steady-state (after 5-7 days of consistent dosing).
Data Presentation: Key TDM Parameters for Selected Dopamine Antagonists
Table 1: Pharmacokinetic and Therapeutic Reference Ranges for Common Antipsychotics
| Drug (Active Metabolite) | Primary Elimination Route | Average Half-life (hours) | Time to Steady-State | Therapeutic Reference Range (ng/mL) | Level Suggestive of EPS Risk (ng/mL) |
|---|---|---|---|---|---|
| Haloperidol | Hepatic (CYP3A4, 2D6) | 18-24 | 4-5 days | 1-10 | >5-10 |
| Risperidone (+ 9-OH-Risperidone) | Hepatic (CYP2D6) | 3 (20) for poor metabolizers | 1-2 days (parent) | 20-60 (active moiety) | >60-120 (active moiety) |
| Olanzapine | Hepatic (CYP1A2, UGT) | 30 | 5-7 days | 20-80 | >80-100 |
| Amisulpride | Renal (unchanged) | 12 | 2-3 days | 100-400 | >400-500 |
| Aripiprazole (+ Dehydro-Aripiprazole) | Hepatic (CYP3A4, 2D6) | 75 (94) | 14 days | 150-500 (parent + metabolite) | >500-700 |
Table 2: Common Drug-Drug Interactions Affecting Antipsychotic Plasma Levels
| Object Drug (Antipsychotic) | Precipitant Drug | Effect on Plasma Level | Clinical Recommendation |
|---|---|---|---|
| Haloperidol | Carbamazepine (CYP3A4 inducer) | Decreased by 50-70% | Increase haloperidol dose; monitor TDM closely. |
| Risperidone | Fluoxetine/Paroxetine (CYP2D6 inhibitors) | Increased by 2-5 fold | Start with 50% risperidone dose; TDM essential. |
| Olanzapine | Smoking (CYP1A2 inducer) | Decreased by 30-50% | Smokers may require higher dose; monitor TDM. |
| Aripiprazole | Itraconazole (CYP3A4 inhibitor) | Increased by 2-3 fold | Reduce aripiprazole dose by 50%. |
Experimental Protocols
Protocol 1: Determination of Haloperidol in Human Plasma by LC-MS/MS 1. Sample Preparation (Protein Precipitation):
- Pipette 100 µL of patient plasma into a microcentrifuge tube.
- Add 10 µL of internal standard working solution (Haloperidol-d4, 100 ng/mL in methanol).
- Add 300 µL of ice-cold acetonitrile.
- Vortex vigorously for 2 minutes.
- Centrifuge at 15,000 x g for 10 minutes at 4°C.
- Transfer 200 µL of the clear supernatant to an autosampler vial with insert.
- Evaporate to dryness under a gentle stream of nitrogen at 40°C.
- Reconstitute the dry residue with 100 µL of mobile phase A (0.1% formic acid in water).
2. LC-MS/MS Conditions:
- Column: C18, 2.1 x 50 mm, 1.7 µm particle size.
- Mobile Phase: A) 0.1% Formic Acid in Water, B) 0.1% Formic Acid in Acetonitrile.
- Gradient: 0-1 min: 10% B, 1-3 min: 10%→90% B, 3-4.5 min: 90% B, 4.6-6 min: 10% B.
- Flow Rate: 0.3 mL/min.
- Injection Volume: 5 µL.
- MS Detection: ESI positive mode. MRM transitions: Haloperidol 376.1→165.1 (collision energy 25 eV); Haloperidol-d4 380.1→169.1 (collision energy 25 eV).
Protocol 2: Population PK Model Building (NONMEM) for Dose Optimization 1. Data Structure (Dataset.csv):
- Columns: ID, TIME, AMT (dose in mg), DV (plasma conc. in ng/mL), EVID (0=observation, 1=dose), MDV, CMT (compartment), WT (weight), AGE, CYP2D6_GENO (0=poor, 1=extensive metabolizer).
2. Control Stream (simplified for risperidone):
Visualizations
TDM-Informed Dose Optimization Workflow
Pathway from D2 Blockade to Motor Side Effects
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for TDM & PK/PD Studies
| Item | Function in Experiment | Example/Specification |
|---|---|---|
| Stable Isotope-Labeled Internal Standards (IS) | Corrects for variability in sample prep, injection, and ion suppression in MS. | Haloperidol-d4, Risperidone-d4, Olanzapine-d3. Purity >98%. |
| Human Blank Plasma (Matrix) | Used to prepare calibration standards and quality controls (QCs). Ensures matrix-matched quantification. | K2EDTA or lithium heparin anti-coagulant. Screen for absence of analytes. |
| Solid Phase Extraction (SPE) Cartridges | Optional for cleaner extracts than protein precipitation. Improves sensitivity and reduces matrix effects. | Mixed-mode cation exchange (MCX) for basic drugs like antipsychotics. |
| Mobile Phase Additives (LC-MS Grade) | Essential for chromatographic separation and ionization efficiency. | 0.1% Formic Acid or 5-10 mM Ammonium Acetate. LC-MS grade purity. |
| Pharmacogenomic (PGx) Panel | To genotype covariates (e.g., CYP2D6, CYP3A5, DRD2) influencing PK and PD. | TaqMan SNP Genotyping Assays or next-generation sequencing panel. |
| Population PK/PD Modeling Software | For building mathematical models to describe drug disposition and effect. | NONMEM, Monolix, R (with packages like nlmixr2, rxode2). |
| Certified Reference Material (CRM) | Primary standard for preparing stock solutions of the analyte. | USP Reference Standards or Cerilliant Certified Solutions. |
Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling for Dose Optimization
Troubleshooting Guides & FAQs
Q1: During PK modeling of a D2 antagonist in rats, I observe bi-exponential plasma concentration decay, but the model fails to converge. What could be wrong? A1: This is often due to poor initial parameter estimates or an incorrectly specified model structure.
- Check: Ensure your structural model (e.g., 2-compartment vs. 3-compartment) is justified by the data. Use visual inspection of the log-concentration vs. time plot.
- Solution: Derive initial estimates using the method of residuals ("curve stripping"). Simplify the model first, then add complexity. Verify dosing records and assay sensitivity at late time points.
Q2: When linking plasma concentration (PK) to receptor occupancy (RO) PD, the estimated EC50 is physiologically implausible (e.g., far above known in vitro Ki). Why? A2: This indicates a potential "effect compartment" or transduction delay (hysteresis) not accounted for.
- Check: Plot effect (RO) vs. concentration. A counterclockwise hysteresis loop confirms a delay.
- Solution: Implement an effect-compartment (link) model or an indirect response model to account for the temporal dissociation between plasma PK and brain PD.
Q3: My PK/PD model predicts >80% D2 occupancy for minimizing motor side effects, but in vivo catalepsy assays show significant side effects at this level. What factors might explain the discrepancy? A3: This highlights the complexity of translating receptor occupancy to functional outcomes.
- Check: Are you modeling occupancy in the correct brain region (e.g., striatum vs. cortex)? Different dopamine circuits have different thresholds.
- Solution: Consider a multi-receptor model (e.g., including 5-HT2A occupancy) or a downstream signal transduction model. Validate with region-specific ex vivo autoradiography or PET data.
Q4: How do I handle high inter-subject variability in drug clearance when optimizing a dose for a patient population? A4: This is addressed through Population PK/PD (PopPKPD) modeling and covariate analysis.
- Protocol: Use non-linear mixed-effects modeling (NONMEM, Monolix, Phoenix NLME). Collect covariate data (weight, age, renal/hepatic function, CYP450 genotype).
- Solution: Identify significant covariates on PK parameters (e.g., creatinine clearance on drug clearance). Simulate dosing regimens for various subpopulations to find one that maximizes target occupancy while minimizing side effects across most individuals.
Q5: What is the best way to model the development of tolerance to motor side effects over repeated dosing? A5: Incorporate a tolerance model component, such as an indirect response model with a feedback inhibitor.
- Protocol: Collect serial data on both PK and a quantitative PD motor side effect biomarker (e.g., locomotor activity, catalepsy score) over multiple dosing cycles.
- Model Structure: An example: Drug stimulates the production of a counter-regulatory factor (RC) which inhibits the side effect response.
Experimental Protocols
Protocol 1: In Vivo PK/PD Study for D2 Antagonist Dose Optimization (Rat)
Objective: To establish the relationship between plasma concentration, striatal D2 receptor occupancy, and catalepsy score.
- Animal Dosing & Sampling: Administer a range of single subcutaneous/oral doses of the antagonist (n=6-8 per dose). Collect serial blood samples (e.g., 5, 15, 30, 60, 120, 240, 480 min) via a catheter for LC-MS/MS plasma drug concentration analysis.
- Behavioral PD Endpoint: At matched time points, assess catalepsy using the bar test (duration of immobility on a horizontal bar, max 300 sec).
- Receptor Occupancy PD Endpoint: Terminate subsets of animals at key time points (e.g., Tmax, 1h, 4h). Rapidly extract brains, dissect striata. Conduct ex vivo radioligand binding assay using [³H]-raclopride to determine percent D2 receptor occupancy.
- Modeling: Develop a PK model from plasma data. Link PK to both RO and catalepsy using separate PD models (Emax model for RO, logistic model for catalepsy probability).
Protocol 2: Population PK/PD Analysis for Covariate Identification
Objective: To identify sources of variability in drug exposure and response from clinical phase Ib/IIa data.
- Data Assembly: Compile a dataset of sparse plasma concentrations, PANSS (efficacy) and SAS (motor side effect) scores, and patient covariates (weight, age, sex, creatinine clearance, CYP2D6 phenotype).
- Base Model Development: Using non-linear mixed-effects software, develop a population PK model and a linked PD model (e.g., an indirect response model for SAS scores).
- Covariate Model Building: Systematically test covariates using stepwise forward inclusion/backward elimination based on statistical criteria (ΔOFV > 3.84, p<0.05).
- Model Validation: Perform visual predictive checks (VPC) and bootstrap analysis.
- Dose Simulation: Simulate 1000 virtual patients under various dosing regimens to predict the probability of therapeutic efficacy (PANSS reduction >30%) vs. side effect (SAS score >3) across different covariate subgroups.
Data Presentation
Table 1: Simulated Dose Optimization for a Novel D2 Antagonist (Hypothetical Data)
Dosing Regimen (mg/day)
Avg. Cmin (ng/mL)
Avg. Striatal D2 RO at Trough (%)
Predicted % Pts with Efficacy (PANSS↓≥30%)
Predicted % Pts with Significant EPS (SAS≥4)
Therapeutic Index (Efficacy/EPS)
2.5
0.8
45
18
<1
18.0
5.0
2.1
65
52
5
10.4
7.5
3.5
75
78
12
6.5
10.0
5.2
82
85
28
3.0
15.0
8.9
88
88
55
1.6
Table 2: Key Research Reagent Solutions
Item
Function/Explanation
Example/Source
Selective D2 Antagonist (Test Compound)
Reference compound for in vitro and in vivo studies to validate assays and models.
Haloperidol, Raclopride
Radioactive D2 Ligand
For quantifying receptor occupancy in tissue (ex vivo) or in vitro binding assays.
[³H]-Raclopride, [¹¹C]-Raclopride (for PET)
LC-MS/MS System
Gold standard for quantifying drug and potential metabolite concentrations in biological matrices (plasma, brain homogenate).
Triple quadrupole systems
Catalepsy Bar Test Apparatus
Standardized equipment for quantifying motor side effects (akinesia) in rodent models.
Horizontal bar, 9-10 cm height
Non-linear Mixed-Effects Modeling Software
Essential for population PK/PD analysis and simulation-based dose optimization.
NONMEM, Monolix, R (nlmixr2)
Physiological-Based PK (PBPK) Software
To predict human PK and brain penetration from in vitro and preclinical data.
GastroPlus, Simcyp
Workflow & Pathway Diagrams
Diagram Title: Integrated PK/PD Modeling Workflow for Dose Optimization
Diagram Title: D2 Receptor Signaling & Antagonist Action in Striatum
Technical Support Center: Troubleshooting & FAQs for DRA Dose Optimization Research
Q1: Our preclinical rodent model is showing severe akathisia-like behavior at low doses of a D2 antagonist, derailing our titration schedule. What are the primary troubleshooting steps?
A: This indicates a potential hypersensitivity or an unexpectedly high D2 receptor occupancy at the "low" starting dose. Follow this protocol:
- Verify Receptor Occupancy: Perform an ex vivo receptor occupancy assay. Sacrifice animals 30 minutes post-administration, extract striatal tissue, and use a radioligand (e.g., [³H]raclopride) binding assay with Scatchard analysis. Target starting occupancy should be 40-50%.
- Re-calibrate Dose: If occupancy >60%, re-calculate your "low" dose using the ED₅₀ for occupancy from your PK/PD model.
- Check for Metabolites: Analyze plasma for active metabolites via LC-MS/MS that may have longer half-lives.
- Alternative Model: Consider using a strain with different D2 receptor expression levels (e.g., D2 knockdown mice) to validate dose-response relationship.
Experimental Protocol: Ex Vivo D2 Receptor Occupancy Assay
- Materials: Test DRA, [³H]raclopride, unlabeled raclopride, scintillation fluid, tissue homogenizer.
- Method: Administer DRA. At Tmax, sacrifice and dissect striatum. Homogenize tissue. Incubate homogenate with 5 nM [³H]raclopride ± 10 µM unlabeled raclopride (for non-specific binding) for 60 min at room temp. Filter and wash. Measure bound radioactivity via scintillation counting. Calculate specific binding and percent occupancy relative to vehicle control.
Q2: When titrating upwards per the "go slow" schedule, we are not observing the expected linear reduction in positive symptoms (in our validated behavioral assay) but see a sharp increase in catalepsy at a specific dose step. How should we adjust the protocol?
A: This suggests a narrow therapeutic window and a potential threshold effect for motor side effects. The titration schedule may need to be non-linear.
- Implement Micro-Dosing Steps: Instead of doubling the dose, increase by 25-30% increments at the critical range.
- Prolong Inter-Dose Interval: Extend the observation period between titrations to ensure steady-state plasma and brain concentrations are reached.
- Concurrent Biomarker Monitoring: At each dose step, measure serum prolactin (a D2 antagonism biomarker) and perform a validated motor function test (e.g, rotarod, bar test). Correlate these with symptom reduction scores.
Table 1: Proposed Modified Titration Schedule for Narrow Therapeutic Window DRA
| Phase | Dose Step (mg/kg) | Duration (Days) | Primary Monitoring Assay | Target Biomarker Range |
|---|---|---|---|---|
| Initiation | 0.1 | 5 | Open Field (Locomotion) | D2 RO < 50% |
| Slow Upshift 1 | 0.15 | 7 | Bar Test (Catalepsy) | Prolactin increase ≤ 200% |
| Slow Upshift 2 | 0.2 | 7 | Rotarod / Social Interaction | Symptom Score reduction ≥ 20% |
| Therapeutic Window Probe | 0.25 | 5 | All assays | Optimization Point |
Q3: Our cell-based signaling assay shows inconsistent ERK phosphorylation responses to gradual DRA exposure, making "start low" mechanistic studies unreliable. What are the key controls?
A: Inconsistent pERK signaling is common due to D2 receptor desensitization and feedback loops.
- Standardize Serum Starvation: Ensure consistent pre-assay serum starvation (e.g., 0.5% FBS for 16 hours).
- Include Pathway Modulators: Run parallel controls with a cAMP agonist (e.g., forskolin) to confirm Gi/o coupling integrity, and a GRK inhibitor to assess desensitization effects.
- Time-Course is Critical: Perform a detailed time-course (5, 15, 30, 60, 120 min) at each concentration. Use a longer pre-incubation period (e.g., 30 min) for the DRA before stimulating with an agonist if studying pre-blockade.
Experimental Protocol: pERK Response Time-Course for DRA Titration
- Materials: HEK-293/D2L cells, phospho-ERK1/2 antibody, total ERK antibody, DRA compound, quinpirole (agonist), HTRF or Western blot detection.
- Method: Plate cells in 96-well. Serum starve. Pre-incubate with increasing DRA doses (0.1 nM - 100 nM) for 30 min. Stimulate with 100 nM quinpirole for varying times (5-120 min). Lyse and measure pERK/tERK via HTRF immunoassay. Plot signal vs. time for each DRA concentration.
Q4: What are the essential reagents and solutions for establishing a robust "start low, go slow" preclinical research pipeline?
A: The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Radioiodinated IBZM ([¹²³I]IBZM) | SPECT radioligand for in vivo D2 receptor occupancy imaging in non-human primates, critical for translational dose-setting. |
| β-Arrestin-2 Recruitment Assay (e.g., BRET) | To quantify biased signaling of DRA; compounds favoring β-arrestin over Gαi may have distinct motor side effect profiles. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) System | For precise quantification of DRA and its metabolites in plasma and brain homogenate to confirm PK linearity during titration. |
| Validated Catalepsy Bar Test Setup | Standardized apparatus (horizontal bar at 4-5 cm height) to objectively measure motor side effect threshold. |
| D2 Receptor Knockdown (KD) or Knock-in (KI) Rodent Models | Genetically modified models to isolate the role of D2 receptor density or genetic variants in titration sensitivity. |
Visualization 1: D2 Receptor Signaling & Titration Impact Pathway
Diagram Title: D2 Receptor Signaling Pathways & Titration Effects
Visualization 2: Preclinical Dose Titration Optimization Workflow
Diagram Title: Preclinical DRA Dose Optimization Workflow
Troubleshooting Guides & FAQs
1. Genotyping Data Inconsistency Q: After genotyping patient samples for CYP2D6, my TaqMan assay results are inconsistent with Sanger sequencing. What could be the cause? A: This is often due to the presence of rare or novel alleles not covered by standard TaqMan probe sets. A known issue is the difficulty in detecting hybrid or structural variants (e.g., CYP2D6*36, gene conversions). Verify by performing long-range PCR followed by nested sequencing to confirm the full gene structure. Always include positive controls for common alleles and a negative control in each run.
2. Poor Correlation between Predicted and Observed Plasma Levels Q: My dose prediction model, based on CYP2D6 phenotype, shows poor correlation with observed risperidone active moiety plasma levels. How can I improve accuracy? A: This typically indicates unaccounted-for covariates. First, ensure patient adherence is confirmed. Then, systematically check for:
- Inhibitors/Inducers: Concurrent medication review (e.g., fluoxetine, paroxetine are strong CYP2D6 inhibitors).
- Other Pharmacogenes: Incorporate CYP3A4 status (metabolizes risperidone to 9-hydroxyrisperidone) and ABCB1 polymorphisms affecting transport.
- Liver Function: Incorporate ALT/AST and albumin levels into your model. Recalibrate your model using multiple linear regression with these factors.
3. Cell Viability Assay Interference with Metabolite Testing Q: When testing haloperidol metabolites from recombinant enzyme systems in cell-based assays, I see unexpected cytotoxicity that interferes with endpoint readings. A: This is likely due to solvent (DMSO) concentration or metabolite solubility. Haloperidol metabolites can precipitate at high concentrations. Troubleshoot by:
- Ensuring final DMSO concentration is ≤0.1%.
- Running a metabolite solubility test in your assay buffer prior to cell exposure.
- Including a vehicle control with the exact same processing steps as your metabolite generation step.
4. Inconclusive Phenotype from Activity Score Q: For a patient with a CYP2D6 genotype of 4/41, the activity score is ambiguous, falling between the standard Poor Metabolizer (PM) and Intermediate Metabolizer (IM) ranges. How should I proceed for dose prediction? A: This is a common clinical dilemma. The recommended protocol is:
- Perform a controlled probe drug administration (e.g., dextromethorphan) to empirically determine the metabolic ratio.
- If a probe study is not possible, default to the more cautious phenotype (PM) in your initial model to minimize overdose risk.
- Use a Bayesian forecasting approach, starting with the PM-predicted dose, then tightly monitoring plasma levels after the first dose to individualize further.
Experimental Protocols
Protocol 1: CYP2D6 Diplotyping and Phenotype Assignment Objective: To determine CYP2D6 diplotype from genomic DNA and assign a predicted phenotype. Method:
- DNA Extraction: Use a validated column-based method from whole blood (≥50 ng/µL, A260/A280 = 1.8-2.0).
- Genotyping: Use a multiplexed, FDA-cleared array (e.g., Luminex xTAG CYP2D6) covering core alleles (*2, *3, *4, *5, *6, *9, *10, *17, *29, *41, gene duplication). Include *5 (gene deletion) detection by separate long PCR.
- Copy Number Variation (CNV) Analysis: For samples with ambiguous results, perform quantitative PCR or MLPA to confirm gene duplications/multiplications.
- Activity Score (AS) Calculation: Assign values per allele: 0 for non-functional (e.g., *3, *4, *5), 0.5 for decreased function (e.g., *10, *41), 1.0 for functional (e.g., *1, *2). For duplications, multiply the value of that allele by the copy number.
- Phenotype Assignment:
- PM: AS = 0
- IM: AS = 0.5 - 1.0
- Normal Metabolizer (NM): AS = 1.5 - 2.0
- Ultrarapid Metabolizer (UM): AS > 2.0
Protocol 2: In Vitro Metabolite Formation using Human Liver Microsomes (HLMs) Objective: To compare the formation rate of 9-hydroxyrisperidone from risperidone across CYP2D6 genotypes. Method:
- HLM Incubation: Use genotyped HLMs (CYP2D6 PM, IM, NM, UM pools). Set up 100 µL reactions: 0.1 mg/mL HLM protein, 1-100 µM risperidone, 1 mM NADPH in phosphate buffer (pH 7.4). Pre-incubate 3 min at 37°C, initiate reaction with NADPH.
- Time Course: Terminate aliquots at 0, 5, 10, 20, 30, 45, 60 min with 100 µL ice-cold acetonitrile.
- Sample Analysis: Centrifuge (13,000g, 10 min). Analyze supernatant via LC-MS/MS for risperidone and 9-hydroxyrisperidone.
- Kinetic Analysis: Plot metabolite formation vs. time. Calculate reaction velocity (V). Use nonlinear regression to determine Km and Vmax.
Data Tables
Table 1: CYP2D6 Phenotype Frequency & Recommended Dose Adjustment for Risperidone
| Predicted Phenotype | Activity Score | Approx. Population Frequency* | Recommended Starting Dose Adjustment vs. Standard |
|---|---|---|---|
| Ultrarapid Metabolizer (UM) | > 2.0 | 1-10% (varies by ancestry) | Increase by 50-100% or use alternative drug not metabolized by CYP2D6. |
| Normal Metabolizer (NM) | 1.5 - 2.0 | ~70-80% | Standard dose. |
| Intermediate Metabolizer (IM) | 0.5 - 1.0 | 10-15% | Reduce by 25-50%. |
| Poor Metabolizer (PM) | 0 | 5-10% | Reduce by 50-75%. Monitor closely for EPS. |
*Frequencies are global estimates; significant population stratification exists.
Table 2: Key CYP450 Enzymes in Dopamine Antagonist Metabolism
| Drug | Primary Metabolizing Enzyme(s) | Key Polymorphic Enzyme Impacting Exposure | Notable Inhibitors (↑ Drug Levels) |
|---|---|---|---|
| Risperidone | CYP2D6, CYP3A4 | CYP2D6 | Fluoxetine, Paroxetine |
| Haloperidol | CYP3A4, CYP2D6 | CYP2D6 (reduced clearance to reduced haloperidol) | Ketoconazole |
| Aripiprazole | CYP2D6, CYP3A4 | CYP2D6 | Quinidine, Grapefruit Juice |
| Olanzapine | CYP1A2, UGT1A4 | CYP1A2*1F (inducible) | Fluvoxamine |
Diagrams
CYP2D6 Genotype to Dose Prediction Workflow
Drug Metabolism & Receptor Interaction Pathway
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research | Example/Catalog Consideration |
|---|---|---|
| Genotyped Human Liver Microsomes (HLMs) | Pooled or individual microsome lots with defined CYP450 genotypes for in vitro metabolism studies. Essential for determining genotype-specific kinetic parameters (Km, Vmax). | Corning Gentest, Xenotech. Select pools characterized for CYP2D6 (PM, IM, NM, UM). |
| Recombinant CYP450 Enzymes (Supersomes) | Individual human cDNA-expressed enzymes. Used to confirm the specific enzyme responsible for a metabolic pathway and to obtain clean kinetic data without interference from other enzymes. | Corning Supersomes (rCYP2D6, rCYP3A4). |
| TaqMan Genotyping Assays | Validated, allele-specific PCR probes for high-throughput, accurate genotyping of known single nucleotide variants (SNVs) and small indels. | Thermo Fisher Scientific's validated CYP2D6 assays for *3, *4, *10, etc. |
| Long-Range PCR Kit | For amplifying large DNA fragments to detect structural variants like CYP2D6 gene deletions (*5) and duplications/multiplications. | Takara LA Taq, Qiagen LongRange PCR Kit. |
| LC-MS/MS System | Gold standard for quantifying drugs and their metabolites in biological matrices (plasma, microsomal incubations) with high sensitivity and specificity. | Sciex Triple Quad, Agilent 6470. |
| Pharmacokinetic Modeling Software | To build and simulate population PK/PD models that incorporate genetic polymorphisms as covariates for dose prediction. | NONMEM, Phoenix NLME, Monolix. |
| Probe Drug Substrate | Used for in vivo phenotyping to confirm metabolic activity. Dextromethorphan (CYP2D6) is a common probe. | Pharmaceutical grade dextromethorphan HBr for clinical studies. |
Technical Support Center
FAQs & Troubleshooting
Q1: During in vitro release testing of our novel risperidone-loaded PLGA microspheres, we observe an unexpected "burst release" exceeding 40% in the first 24 hours, compromising the target release profile. What are the primary causes and mitigation strategies?
A: A high initial burst release is a common formulation challenge. It typically indicates drug crystals or adsorbed drug on the microsphere surface, inadequate polymer encapsulation, or high porosity.
- Primary Causes:
- Inadequate Drug Encapsulation: Drug partitioning to the aqueous phase during emulsion/solvent evaporation.
- Fast Solvent Removal: Rapid solvent diffusion creates porous surfaces, allowing easy drug diffusion.
- Poor Drug-Polymer Affinity: Hydrophilic drugs (like many antagonists) in hydrophobic polymers (PLGA).
- Troubleshooting Steps:
- Optimize Emulsion Stability: Increase homogenization speed/time, adjust surfactant (e.g., PVA) concentration (e.g., from 1% to 2-3% w/v) to stabilize the primary emulsion.
- Modify Solvent Removal Rate: Add a co-solvent (e.g., acetone) to the organic phase or adjust the stirring rate in the hardening bath to slow down diffusion.
- Implement a Coating Step: Apply a thin, dense PLGA layer via a secondary emulsion or use a surface washing step with a non-solvent for the drug.
- Alter Drug Loading: Reduce the theoretical drug load from, e.g., 30% to 15-20% to improve encapsulation efficiency.
Q2: Our in vivo pharmacokinetic study in a rat model for a new haloperidol decanoate LAI shows high inter-subject variability (CV > 35%) in AUC and Cmax. What experimental factors should we investigate?
A: High variability in LAI PK often stems from administration technique or formulation inconsistency.
- Investigation Protocol:
- Administration Technique Verification:
- Site: Ensure consistent intramuscular (e.g., gluteal) or subcutaneous injection site across all subjects.
- Needle Gauge/Length: Use the same specification (e.g., 22G, 1-inch) for all injections. A too-narrow gauge can shear microparticles.
- Injection Depth & Angle: Standardize using a restrainer/guide.
- Formulation Homogeneity: Re-check the suspension protocol. Gently vortex or roll the vial for a standardized time (e.g., 5 minutes) immediately before drawing each dose to ensure uniform particle resuspension.
- Animal Model Consideration: Account for potential differences in muscle vascularization or metabolism. Randomize animals strictly across groups.
- Administration Technique Verification:
Q3: When developing an in vitro-in vivo correlation (IVIVC) for an aripiprazole LAI, the in vitro release profile (USP Apparatus 4) does not align with the in vivo absorption profile. What are critical points of failure?
A: IVIVC failure indicates the in vitro method does not adequately simulate in vivo conditions.
- Critical Checkpoints:
- Release Medium: Physiological pH (7.4) may not be sufficient. Consider incorporating esterases (for PLGA hydrolysis) or a low concentration of a surfactant (e.g., 0.1% w/v SDS) to better simulate interstitial fluid and sink conditions.
- Hydrodynamics: The flow rate in Apparatus 4 must mimic tissue fluid turnover. A too-high rate (e.g., 16 mL/min) can over-erode the matrix. Test a lower, pulsatile flow (e.g., 4-8 mL/min).
- In Vivo Data Accuracy: Ensure the in vivo absorption rate is calculated using a validated deconvolution method, not just plasma concentration, to account for distribution and elimination.
Key Experimental Protocols
Protocol 1: Preparation of PLGA Microspheres via Double Emulsion (W/O/W) Solvent Evaporation Objective: To encapsulate a hydrophilic dopamine receptor antagonist (e.g., sulphide) into PLGA microspheres for sustained release.
- Primary Emulsion: Dissolve 100 mg drug in 1 mL of 0.1% acetic acid aqueous solution (W1). Dissolve 500 mg PLGA (50:50, 0.55 dL/g) in 5 mL dichloromethane (DCM, organic phase). Emulsify W1 in the organic phase using a probe sonicator (40% amplitude, 60 sec) on ice to form W1/O.
- Secondary Emulsion: Pour the primary emulsion into 100 mL of 2% w/v polyvinyl alcohol (PVA) solution (W2) with continuous high-speed stirring (1000 rpm). Stir for 1 hour to form the (W1/O)/W2 emulsion.
- Solvent Evaporation: Transfer the entire beaker to a magnetic stirrer and stir at 500 rpm for 4 hours at room temperature to allow complete DCM evaporation and particle hardening.
- Collection & Washing: Collect microspheres by centrifugation (10,000 rpm, 10 min, 4°C). Wash thrice with deionized water to remove PVA and surface drug. Lyophilize for 48 hours.
- Characterization: Determine particle size (laser diffraction), drug loading (HPLC after dissolution in DMSO), and surface morphology (SEM).
Protocol 2: In Vitro Release Study for LAI Formulations (USP Apparatus 2 with Modification) Objective: To simulate the sustained release profile of an olanzapine pamoate suspension.
- Media Preparation: Prepare 500 mL of phosphate buffer (pH 7.4) with 0.02% w/v sodium azide (preservative) and 0.1% w/v Tween 80 (to maintain sink condition).
- Apparatus Setup: Use a standard paddle apparatus (Apparatus 2). Place 5 mg equivalent of microspheres/suspension in a small dialysis bag (MWCO 100 kDa) to prevent particle loss, and immerse in 250 mL of release medium. Set paddle speed to 50 rpm. Maintain temperature at 37.0 ± 0.5°C.
- Sampling: Withdraw 2 mL samples at predetermined intervals (1, 4, 8, 24 hours, then every 3-7 days). Replace with an equal volume of fresh, pre-warmed medium.
- Analysis: Filter samples (0.22 µm), dilute as necessary, and quantify drug content via HPLC-UV. Calculate cumulative release percentage.
Quantitative Data Summary
Table 1: Comparison of Commercial Dopamine Antagonist LAIs: Key Formulation & PK Parameters
| API (Brand) | Polymer/Vehicle | Nominal Dose Strengths | Tmax | Terminal t1/2 | Dosing Interval |
|---|---|---|---|---|---|
| Risperidone (Risperdal Consta) | PLGA microspheres | 12.5, 25, 37.5, 50 mg | 4-5 weeks | 3-6 days* | 2 weeks |
| Paliperidone palmitate (Invega Sustenna) | Aqueous nanosuspension | 39, 78, 117, 156, 234 mg eq. | 13 days | 25-49 days | 4 weeks (init. 1 wk) |
| Aripiprazole lauroxil (Aristada Initio) | Aqueous nanosuspension | 441, 662, 882 mg | 5-7 days | 23-47 days | 4-8 weeks |
| Haloperidol decanoate (Haldol Decanoate) | Sesame oil solution | 50, 100 mg/mL | 3-9 days | 3 weeks | 4 weeks |
* Refers to the released drug (risperidone), not the microsphere elimination.
Table 2: Common PLGA Grades & Properties for LAIs
| PLGA Lactide:Glycolide Ratio | Inherent Viscosity (dL/g) | Degradation Time (Approx.) | Key Release Characteristic |
|---|---|---|---|
| 50:50 | 0.15-0.25 | 1-2 months | Fastest erosion, suitable for 1-month release. |
| 50:50 | 0.40-0.60 | 2-4 months | Moderate erosion, standard for 1-3 month release. |
| 75:25 | 0.60-0.80 | 4-6 months | Slower, more lactide provides longer release (>3 months). |
| 85:15 | >0.70 | 5-6+ months | Slowest erosion, for extended release (>6 months). |
The Scientist's Toolkit
Table 3: Essential Research Reagents & Materials
| Item | Function in LAI Research |
|---|---|
| PLGA (various LA:GA ratios & IV) | Biodegradable polymer matrix forming the depot, controlling release rate via hydrolysis. |
| Polyvinyl Alcohol (PVA) | Common surfactant/stabilizer in emulsion methods to control microsphere size and prevent aggregation. |
| Dichloromethane (DCM) / Ethyl Acetate | Volatile organic solvents to dissolve polymer, subsequently evaporated to form solid particles. |
| In Vitro Release Media (PBS with SDS/Tween) | Simulates physiological conditions; surfactants maintain "sink conditions" for hydrophobic drugs. |
| USP Apparatus 2 (Paddle) & 4 (Flow-Through Cell) | Standardized equipment for in vitro release testing under controlled hydrodynamics. |
| Sonication Probe/Homogenizer | Critical for creating stable primary emulsions with controlled droplet (and hence particle) size. |
| Lyophilizer (Freeze Dryer) | Gently removes water from washed microspheres without compromising morphology or stability. |
| HPLC-UV/MS System | For quantifying drug loading, encapsulation efficiency, and in vitro release kinetics. |
| Laser Diffraction Particle Size Analyzer | Characterizes particle size distribution of microspheres/nanosuspensions, crucial for release and injectability. |
| Scanning Electron Microscope (SEM) | Visualizes surface morphology (porosity, smoothness) and internal structure of microspheres. |
Pathway & Workflow Visualizations
Title: Mechanism of LAI Action for Side Effect Mitigation
Title: LAI Formulation Development & Optimization Workflow
Managing Side Effects: Protocols for Mitigation, Reversal, and Dose Adjustment
Technical Support Center
Troubleshooting Guide: Acute EPS Management in Preclinical & Clinical Research
Issue 1: Subject exhibits acute dystonia during dose-escalation phase of a D2 antagonist trial.
- Diagnosis: Likely acute dystonic reaction, a common early-onset EPS. Characterized by involuntary muscle contractions, often in neck, jaw, or eyes.
- Immediate Action (Clinical): Administer a rapid-acting anticholinergic (e.g., benztropine 1-2 mg IM/IV) or antihistamine (e.g., diphenhydramine 25-50 mg IV). Relief is typically diagnostic.
- Protocol Adjustment: For the affected subject, consider temporary dose hold. For the study protocol, review the dose-escalation schedule. The starting dose may be too high or the titration too rapid.
- Preventive Analysis: Correlate plasma levels of the antagonist with EPS onset. Determine the therapeutic window for D2 occupancy vs. EPS threshold.
Issue 2: Akathisia reported, but researchers are unsure if it's drug-induced or anxiety.
- Diagnosis: Akathisia is a subjective feeling of inner restlessness and an objective observation of fidgeting, pacing, or inability to remain still.
- Differential Test: Utilize validated scales (Barnes Akathisia Rating Scale). A trial dose reduction may clarify: if symptoms diminish, it is likely drug-induced akathisia. Note: Anticholinergics are less effective for akathisia; consider dose reduction as primary strategy.
- Experimental Control: Ensure baseline restlessness is quantified pre-trial. Monitor for correlation with peak serum drug levels.
Issue 3: Parkinsonian symptoms (tremor, bradykinesia) emerge after weeks of stable dosing.
- Diagnosis: Drug-induced parkinsonism, a later-onset EPS.
- Management Algorithm:
- Step 1: Confirm diagnosis using UPDRS or similar scale.
- Step 2: For mild symptoms, initiate add-on anticholinergic (e.g., benztropine 0.5-2 mg BID) or amantadine (100 mg BID).
- Step 3: For moderate-severe symptoms, dose reduction of the primary D2 antagonist is the preferred evidence-based strategy to preserve long-term tolerability and minimize anticholinergic side effects.
- Step 4: Re-assess efficacy of the primary drug at lower dose. The research goal is to find the minimal effective dose that maintains therapeutic efficacy without EPS.
Issue 4: Determining whether to use anticholinergic prophylaxis in a study design.
- Recommendation: Prophylaxis is generally not recommended in research settings as it can confound the natural incidence and severity of EPS, which is a key safety endpoint. It may be ethically considered in high-risk trials (e.g., high-potency D2 antagonists, first-in-human). If used, it must be standardized across arms and its impact on data interpretation explicitly stated.
Frequently Asked Questions (FAQs)
Q1: What is the pharmacologic rationale for using anticholinergics to treat EPS from dopamine antagonists? A: Dopamine receptor antagonists (DRAs) in the striatum create a functional imbalance, reducing inhibitory dopaminergic signaling and allowing relative excess of cholinergic activity from interneurons. Anticholinergic agents (muscarinic receptor antagonists) restore this balance by blocking the excessive excitatory cholinergic output, thereby mitigating motor side effects.
Q2: When should dose reduction be prioritized over anticholinergic add-on therapy? A: Dose reduction should be the first consideration in a managed research protocol when: 1) EPS symptoms are moderate to severe; 2) The subject is at high risk for anticholinergic side effects (cognitive impairment, constipation, urinary retention); 3) The research question involves finding the minimal effective dose. Add-on therapy is useful for mild symptoms or when the current dose is critically efficacious and cannot be reduced without loss of primary effect.
Q3: What are the key pharmacokinetic/dynamic parameters to monitor when optimizing doses to minimize EPS? A: Key parameters include:
- D2 Receptor Occupancy: Target 65-78% for antipsychotic efficacy; >80% occupancy strongly correlates with EPS risk.
- Plasma Half-life & Cmax: A high Cmax may trigger EPS even with acceptable average occupancy. Consider divided dosing or extended-release formulations.
- Muscarinic Receptor Affinity: Drugs with inherent anticholinergic activity (e.g., clozapine) have lower EPS risk at equipotent D2 blockade doses.
Q4: What experimental models are used to predict EPS liability in drug development? A: Standard preclinical models include:
- Catalepsy Test in Rodents: A primary screen for drug-induced motor immobility (akin to parkinsonism).
- Conditioned Avoidance Response: Assesses disruption of motivated motor behavior without sedation.
- In vivo Receptor Occupancy Imaging (PET): Correlates plasma levels with striatal D2 occupancy in primates or humans.
Table 1: Common Anticholinergic Agents for EPS Management
| Agent | Typical Acute Dose (IM/IV) | Typical Oral Maintenance Dose | Time to Onset (Acute) | Key Considerations for Research |
|---|---|---|---|---|
| Benztropine | 1-2 mg | 1-2 mg BID | 5-30 min | Longer half-life; also has antihistaminic properties. |
| Diphenhydramine | 25-50 mg | 25-50 mg QID | 5-30 min | Useful for acute dystonia; sedating. |
| Trihexyphenidyl | - | 2-5 mg BID/TID | 60 min (oral) | Pure anticholinergic; can be titrated. |
Table 2: Correlation between Striatal D2 Occupancy & EPS Risk
| D2 Occupancy Level (PET Scan) | Clinical Outcome | Implication for Dose Optimization |
|---|---|---|
| <65% | Inadequate therapeutic response | Below effective dose threshold. |
| 65-78% | Therapeutic window; low EPS risk | Target range for minimal effective dose. |
| >80% | High probability of EPS | Indicates need for dose reduction. |
Experimental Protocols
Protocol 1: Assessing Catalepsy in Rodents (Bar Test) Objective: To quantify the EPS liability of a novel dopamine receptor antagonist. Materials: Test compound, vehicle control, positive control (e.g., haloperidol), horizontal bar (1 cm diameter, elevated 5-8 cm), stopwatch. Procedure:
- Animals are acclimatized to the testing room for 1 hour.
- Administer test compound/vehicle at designated doses (n=6-10 per group).
- At Tpeak plasma time (e.g., 30-60 min post-injection), gently place the animal's forepaws on the horizontal bar.
- Start the stopwatch. Measure the time until the animal removes both forepaws from the bar.
- Set a cut-off time (e.g., 60 seconds). An animal remaining on the bar for this duration is considered cataleptic.
- Record descent latency for each animal. Calculate mean catalepsy time per dose group.
- Analysis: Compare mean catalepsy scores vs. vehicle control. Establish an ED50 for catalepsy and compare to the ED50 for the primary therapeutic effect (e.g., in a conditioned avoidance test) to calculate a therapeutic index.
Protocol 2: Clinical Assessment of EPS using the Simpson-Angus Scale (SAS) Objective: To objectively measure drug-induced parkinsonism in a clinical trial setting. Materials: Simpson-Angus Scale form, quiet examination room. Procedure:
- The subject is assessed at baseline (pre-dose) and at regular intervals post-dose initiation.
- The rater evaluates and scores 10 items (e.g., gait, arm dropping, shoulder shaking, elbow rigidity, wrist rigidity, leg pendulousness, head dropping, glabellar tap, tremor, salivation) on a 0-4 or 0-5 scale.
- Scores are summed. A total score >3 suggests clinically significant parkinsonism.
- Dose Optimization Link: If SAS score >3, the algorithm triggers: a) review of DRA dose for reduction, or b) initiation/add-on of anticholinergic medication, per protocol. Serial SAS scores track intervention efficacy.
Visualizations
Diagram 1: Striatal Neurotransmitter Imbalance in EPS
Diagram 2: EPS Management Decision Algorithm
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EPS-Related Research
| Item | Function in Research | Example/Supplier Note |
|---|---|---|
| Selective D2 Antagonist | Positive control for inducing EPS in preclinical models. | Haloperidol, raclopride. |
| Muscarinic Antagonist | Tool compound to reverse/rescue EPS in models. | Scopolamine, benztropine. |
| Catalepsy Test Apparatus | Standardized equipment for measuring rodent immobility. | Horizontal bar or vertical grid. Automated systems available (e.g., Bioseb). |
| Barnes Akathisia Scale (BAS) | Validated clinical tool to quantify akathisia objectively. | Must be used by trained raters. |
| Simpson-Angus Scale (SAS) | Validated clinical tool to quantify drug-induced parkinsonism. | Gold standard for EPS measurement in trials. |
| Radioligand for D2 Receptor | For in vitro binding assays to determine compound affinity (Ki). | [³H]Spiperone, [³H]Raclopride. |
| PET Radioligand ([¹¹C]Raclopride) | For in vivo imaging of striatal D2 receptor occupancy in humans/animals. | Critical for establishing dose-occupancy-EPS relationships. |
Troubleshooting Guides & FAQs
FAQ 1: In our rodent model, propranolol pretreatment fails to prevent D2 antagonist-induced akathisia. What are potential causes and solutions?
- A: Failure can stem from dose timing, receptor subtype selectivity, or model-specific pathophysiology.
- Check Timing: Beta-blockers may mitigate the expression of akathisia more effectively than preventing its initiation. Administer propranolol (5-10 mg/kg i.p. in rats) concurrently or 30-minutes post D2 antagonist injection, not just as a long-term pretreatment.
- Verify Selectivity: Propranolol is non-selective (β1/β2). If the mechanism is central β1 antagonism, confirm CNS penetration. Consider testing more CNS-penetrant beta-blockers like pindolol.
- Review Model: Validate your akathisia metrics (e.g., open field activity monitoring, paw treading counts). Ensure observed behaviors are not confounded by sedation or other motor effects.
FAQ 2: When co-administering a benzodiazepine (e.g., lorazepam) with our D2 antagonist, we observe excessive sedation that confounds akathisia measurements. How can we adjust the protocol?
- A: This indicates an excessive GABAergic potentiation masking the target behavior.
- Titrate Dose: Implement a rigorous dose-response curve for lorazepam. Start at a very low dose (e.g., 0.1 mg/kg i.p. in mice) and incrementally increase to find the threshold where akathistic behaviors are reduced without significant locomotor impairment.
- Switch Agent: Consider a benzodiazepine with a shorter half-life (e.g., midazolam) to provide a narrower window of observation.
- Timing Adjustment: Stagger administration. Administer the D2 antagonist, allow akathisia to establish (e.g., 60 minutes), then administer the low-dose benzodiazepine to assess reversal rather than prevention.
FAQ 3: Our serotonergic approach (5-HT2A antagonism) shows efficacy but complicates the receptor profile of our lead D2 antagonist compound. How do we isolate the mechanism for our thesis?
- A: You need to dissect the contribution of 5-HT2A blockade vs. D2 blockade.
- Control Experiment: Use a selective 5-HT2A antagonist (e.g., M100907, volinanserin) as an adjunctive therapy. Administer a fixed, suboptimal dose of your D2 antagonist to induce mild akathisia, then co-administer the 5-HT2A antagonist to demonstrate synergistic reduction.
- Binding Assay: Run a comparative receptor binding profile (Ki table) for your lead compound versus a pure D2 antagonist (like haloperidol) to quantify its 5-HT2A affinity.
- Genetic Model: If resources allow, utilize 5-HT2A knockout mice treated with a pure D2 antagonist to confirm the role of this serotonergic pathway in your model.
FAQ 4: We are measuring plasma levels, but how do we correlate them with central (CNS) exposure for these adjunctive treatments?
- A: Plasma levels often poorly correlate with CNS efficacy for akathisia treatments.
- Conduct a PK/PD Study: Measure drug concentrations in both plasma and brain homogenate (or CSF) at serial time points post-administration. Correlate these levels with a key behavioral endpoint (e.g., activity count).
- Use a Biomarker: For beta-blockers, monitor heart rate reduction as a peripheral pharmacodynamic marker to confirm bioactivity concurrent with behavioral scoring.
- Microdialysis: For direct evidence, employ in vivo microdialysis in relevant brain regions (e.g., striatum, prefrontal cortex) to measure extracellular neurotransmitter changes (DA, NE, 5-HT) induced by the D2 antagonist and its modulation by the adjunctive agent.
Experimental Protocols
Protocol 1: Assessing Adjunctive Drug Efficacy in a Rodent Acute Akathisia Model
Objective: To evaluate the efficacy of beta-blockers or benzodiazepines in reducing acute akathisia induced by a high-potency D2 antagonist.
- Animals: Male C57BL/6J mice (n=10-12/group).
- Drug Preparation:
- D2 Antagonist: Haloperidol (1 mg/kg) in 0.3% lactic acid/saline.
- Adjunctive: Propranolol HCl (10 mg/kg) or Lorazepam (0.25 mg/kg) in saline (with <1% DMSO if needed).
- Procedure:
- Group animals into: Vehicle+Vehicle, Haloperidol+Vehicle, Haloperidol+Propranolol, Haloperidol+Lorazepam.
- Administer Haloperidol or its vehicle intraperitoneally (i.p.).
- After 30 minutes, administer the adjunctive treatment or its vehicle i.p.
- Place animals in individual open-field arenas.
- Data Acquisition: Record for 60 minutes, starting 10 minutes post-second injection.
- Primary Outcome: Total distance traveled (cm). Akathisia is indicated by a significant increase in Haloperidol+Vehicle group vs. Vehicle control. Efficacy is shown by a reduction in this hyperactivity in adjunctive groups.
- Secondary Outcomes: Rearing frequency, focused grooming bouts.
Protocol 2: Receptor Binding Affinity Assay (Competition Binding)
Objective: To determine the Ki of a novel D2 antagonist compound for D2 and 5-HT2A receptors.
- Membrane Preparation: Harvest transfected HEK-293 cells expressing human D2 or 5-HT2A receptors. Homogenize and centrifuge to prepare membrane fractions.
- Radioligand Selection: Use [³H]Spiperone for D2, [³H]Ketanserin for 5-HT2A.
- Assay Setup: In a 96-well plate, add:
- Buffer (50 mM Tris-HCl, pH 7.4)
- Membrane protein (5-10 µg)
- Increasing concentrations of your test compound (e.g., 10^-12 to 10^-5 M, in triplicate).
- A fixed concentration of the radioligand (~ at its Kd).
- Include wells for total binding (no competitor) and nonspecific binding (with 10 µM haloperidol/ketanserin).
- Incubation: Incubate for 60-90 mins at room temperature.
- Filtration & Measurement: Terminate reaction by rapid vacuum filtration through GF/B filters. Wash filters, add scintillation fluid, and count radioactivity.
- Data Analysis: Use nonlinear regression (e.g., GraphPad Prism) to fit competition curves and calculate IC50, then derive Ki using the Cheng-Prusoff equation.
Table 1: Comparative Efficacy of Adjunctive Agents in Preclinical Models of D2 Antagonist-Induced Akathisia
| Adjunctive Class | Example Agent | Typical Rodent Dose (i.p.) | Proposed Primary Mechanism | % Reduction in Hyperactivity* (Mean ± SEM) | Key Limitation in Model |
|---|---|---|---|---|---|
| Beta-Blocker | Propranolol | 10 mg/kg | Peripheral & Central β1/2 antagonism | 65% ± 8% | Sedation at higher doses |
| Benzodiazepine | Lorazepam | 0.25 mg/kg | Positive allosteric modulation of GABA-A | 80% ± 6% | Confounding sedation, tolerance |
| 5-HT2A Antagonist | M100907 | 0.5 mg/kg | Central 5-HT2A receptor blockade | 55% ± 10% | Limited effect on somatic restlessness |
*Hypothetical data based on composite literature values for illustration. Reduction compared to D2 antagonist + vehicle control group.
Table 2: Receptor Binding Profile of Select Agents Relevant to Akathisia Management
| Compound Name | Primary Target (Ki, nM) | D2 (Ki, nM) | 5-HT2A (Ki, nM) | α1 Adrenergic (Ki, nM) | Clinical Use for Akathisia |
|---|---|---|---|---|---|
| Propranolol | β1/2 Adrenoceptor (2.0) | >10,000 | >10,000 | 20 | First-line |
| Clonazepam | GABA-A PAM (N/A) | >10,000 | >10,000 | >10,000 | Second-line |
| Mirtazapine | 5-HT2A/2C Antag. (0.1) | >1,000 | 0.1 | 500 | Emerging evidence |
| Haloperidol | D2 Antagonist (1.0) | 1.0 | 50 | 10 | Causative agent |
| Brexpiprazole | D2 Partial Agonist (0.3) | 0.3 | 0.47 | 0.17 | Lower intrinsic risk |
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Relevance to Akathisia Research |
|---|---|
| High-Potency D2 Antagonist (e.g., Haloperidol, Raclopride) | Function: Standardized pharmacologic tool to reliably induce acute akathisia-like hyperkinesis in rodent models. Note: Use lactate vehicle for solubility. |
| Selective 5-HT2A Antagonist (e.g., M100907, Volinanserin) | Function: To isolate the role of 5-HT2A receptor blockade in modulating D2 antagonist side effects without significant off-target activity. |
| β1-Selective (Metoprolol) & β1/2 Non-Selective (Propranolol) Antagonists | Function: Comparator agents to determine the relative contribution of central vs. peripheral beta-adrenergic receptors in akathisia pathophysiology. |
| Radioactive Ligands: [³H]Spiperone, [³H]Ketanserin | Function: Essential for conducting competition binding assays to determine the receptor affinity (Ki) of novel compounds for D2 and 5-HT2A receptors. |
| Automated Behavioral Tracking Software (e.g., EthoVision, ANY-maze) | Function: Provides objective, high-throughput quantification of locomotor activity, distance traveled, and specific movement patterns crucial for assessing akathisia and drug efficacy. |
| LC-MS/MS System | Function: Gold standard for quantifying drug and metabolite concentrations in biological matrices (plasma, brain homogenate) to establish PK/PD relationships. |
| Telemetry System (ECG/EMG) | Function: Allows simultaneous monitoring of peripheral physiological markers (heart rate for beta-blocker PD) and movement in freely moving animals, reducing stress artifacts. |
Technical Support Center: Troubleshooting Guides & FAQs
Q1: In our rodent model of haloperidol-induced VMAT2 upregulation, Western blot results show inconsistent VMAT2 protein levels across treatment groups. What are potential causes and solutions?
A: Inconsistent VMAT2 protein quantification is a common issue. Primary troubleshooting steps:
- Sample Preparation: Ensure striatal tissue is homogenized in fresh, ice-cold RIPA buffer with protease inhibitors (e.g., 1X Halt Protease Inhibitor Cocktail). Degradation can cause variability.
- Membrane Fraction Enrichment: VMAT2 is a vesicular membrane protein. Use a subcellular fractionation protocol to enrich for synaptic vesicles before lysis. This increases signal-to-noise ratio.
- Antibody Validation: Confirm antibody specificity (e.g., Anti-VMAT2 antibody [EPR11021], Abcam) using VMAT2 knockout tissue as a negative control. High background can obscure results.
- Loading Control: Use a membrane-specific loading control (e.g., Na+/K+ ATPase) instead of total protein or cytosolic controls.
Q2: When administering valbenazine in a long-term DRA prophylaxis study, we observe significant weight loss in the rodent cohort. Is this a drug effect or a dosing error?
A: Weight loss is a documented, dose-dependent side effect of VMAT2 inhibitors in preclinical models. Follow this checklist:
- Verify Dose Calculation: Re-calculate dose based on most recent animal body weight. Standard dosing range is 3-12 mg/kg/day for valbenazine (free-base equivalent) in rodent studies.
- Administration Route: Ensure correct oral gavage technique to avoid esophageal injury or pulmonary aspiration, which can cause rapid weight loss.
- Control Groups: Confirm weight loss is specific to the DRA+Valbenazine group and not seen in DRA-only or vehicle-only groups, which would indicate other husbandry issues.
- Mitigation Strategy: If the effect is confirmed as drug-related, consider dose reduction within the therapeutic window or implement a paired-feeding protocol for control animals to isolate the metabolic effect.
Q3: Our AIMS (Abnormal Involuntary Movement Scale) scoring for a clinical trial shows high inter-rater variability. How can we improve consistency?
A: Standardize the assessment protocol:
- Centralized Rater Training: Use the School of Medicine at Yale's training website and certification program for the AIMS exam.
- Video Recording: Record patient assessments. Have all raters score the same videos, then discuss discrepancies with a lead neurologist to calibrate.
- Clear Operational Definitions: Create a lab-specific SOP that defines anchor points for each score (0-4) for classic TD manifestations (oro-buccal-lingual, choreoathetoid movements).
- Environmental Control: Conduct assessments in a quiet, well-lit room with the patient seated in a hard, armless chair, per the standard AIMS protocol.
Q4: In cell-based assays screening for DRA-induced synaptic changes, what is the optimal method to quantify dendritic spine density following antipsychotic exposure?
A: A standardized protocol for primary striatal neuron cultures is recommended:
- Culture & Transfection: Plate primary striatal neurons (E18 rat) at low density (50-100 cells/mm²). Transfect at DIV 7-10 with a plasmid expressing fluorescent protein (e.g., GFP, mCherry) under a neuronal promoter (e.g., hSyn1) to fill dendrites.
- Treatment: Apply DRA (e.g., 10-100 nM haloperidol) and/or VMAT2 inhibitor (e.g., 10 nM tetrabenazine) at DIV 14-21. Include vehicle controls.
- Imaging & Analysis: At DIV 21-28, fix cells and image using high-resolution confocal microscopy (63x/100x oil objective). Acquire z-stacks (0.3 µm steps) of secondary/tertiary dendrites.
- Quantification: Use automated software (e.g., NeuronStudio, FiloTracer) for unbiased spine counting. Analyze ≥30 dendrites per condition from 3 independent cultures. Express as spines per µm.
Experimental Protocols
Protocol 1: In Vivo Prophylaxis Model for Tardive Dyskinesia in Rats Objective: To assess if co-administration of a VMAT2 inhibitor with a DRA prevents the emergence of VACNTs (Vacuous Chewing Movements, a TD surrogate).
- Animals: Male Sprague-Dawley rats (n=10-12/group).
- Dosing: Administer daily intraperitoneal injections for 12 weeks.
- Group 1: Vehicle control (1% acetic acid/saline).
- Group 2: Haloperidol decanoate (28.5 mg/kg/month, IM) + Vehicle oral.
- Group 3: Haloperidol decanoate + Valbenazine (12 mg/kg/day, oral gavage).
- Group 4: Valbenazine only.
- Behavioral Scoring: In weeks 4, 8, and 12, place rats in transparent observation cages. After 5 min acclimation, score VACNTs (rapid, purposeless jaw movements) in a 2-min period by a blinded observer. Counts are summed over five sessions.
- Terminal Analysis: Euthanize, dissect striatum. Process for HPLC (dopamine/metabolite levels) or Western blot (VMAT2, D2R).
Protocol 2: D2 Receptor Internalization Assay in HEK293 Cells Objective: To measure if VMAT2 inhibition modulates D2 dopamine receptor trafficking upon antagonist binding.
- Cell Prep: Culture HEK293 cells stably expressing human D2 receptor tagged with pH-sensitive GFP (pHluorin-D2R).
- Treatment: Pre-treat cells with 100 nM tetrabenazine or vehicle for 1 hour. Then, stimulate with 10 µM haloperidol or vehicle for 30 min.
- Imaging: Use live-cell confocal microscopy. pHluorin fluorescence is quenched in acidic endosomes upon receptor internalization.
- Quantification: Calculate the change in cell surface fluorescence intensity (regions of interest on the plasma membrane) over time. Internalization rate is expressed as % loss of surface fluorescence/min.
Data Presentation
Table 1: Efficacy of VMAT2 Inhibitors in TD Clinical Trials (Key Outcomes)
| Drug (Brand) | Trial Phase | Primary Endpoint | Mean AIMS Score Change (Drug vs. Placebo) | NNT for Response* | Common AEs (>10%) |
|---|---|---|---|---|---|
| Valbenazine (Ingrezza) | 3 (KINECT 3) | AIMS Change (wk 48) | -3.2 vs -0.1 (p<0.001) | 4 | Somnolence, Headache |
| Deutetrabenazine (Austedo) | 3 (ARM-TD, AIM-TD) | AIMS Change (wk 12) | -3.3 vs -1.4 (p<0.001) | 5 | Headache, Diarrhea |
| Tetrabenazine (Xenazine) | Open-label | AIMS Change (wk 12) | -4.5 (baseline) | N/A | Depression, Sedation |
NNT (Number Needed to Treat) for ≥50% reduction in AIMS score. *Used off-label for TD; not FDA-approved for this indication.
Table 2: Key Experimental Parameters for Preclinical TD/VMAT2 Studies
| Model Type | Species/ Cell Line | Common DRA Challenge | VMAT2 Inhibitor Dose Range (Prophylaxis) | Primary Readout | Duration |
|---|---|---|---|---|---|
| Chronic DRA | Rat (SD) | Haloperidol decanoate (21-28 mg/kg/4wks, IM) | Valbenazine: 3-12 mg/kg/day (oral) | VACNTs Counts | 12+ weeks |
| Acute DRA | Mouse (C57BL/6) | Haloperidol acute (1 mg/kg, IP) | Tetrabenazine: 1-3 mg/kg (IP) | Catalepsy Time | 30-120 min |
| In Vitro | Primary Striatal Neurons | Haloperidol (10-100 nM) | Tetrabenazine (10-100 nM) | Spine Density, VMAT2 WB | 24-72 hrs |
| In Vitro | SH-SY5Y Cells | Risperidone (50 nM) | Valbenazine metabolite ([+]-α-HTBZ) (nM range) | DA Release (HPLC) | 1-6 hrs |
Diagrams
Title: TD Prophylaxis Experimental Workflow
Title: VMAT2 Inhibitor Mechanism of Action
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in TD/VMAT2 Research |
|---|---|
| Haloperidol Decanoate | Long-acting DRA for establishing chronic rodent models of TD. Ensures stable receptor blockade. |
| Valbenazine (Free Base) | Selective VMAT2 inhibitor for preclinical prophylaxis and reversal studies. More stable in vivo than tetrabenazine. |
| Anti-VMAT2 Antibody (EPR11021) | For Western blot or IHC to quantify VMAT2 protein expression changes in striatal tissue. |
| pHluorin-D2R Plasmid | Enables live-cell imaging of D2 receptor trafficking dynamics in response to DRAs. |
| Synaptosomal Preparation Kit | Isolates nerve terminals for functional assays of vesicular dopamine uptake (H3-DA uptake). |
| Crawley's Jaw Movement Software | Automated video tracking software for objective, high-throughput scoring of rodent VACNTs. |
| Dopamine ELISA Kit | Measures extracellular or tissue levels of dopamine with high sensitivity in microdialysates or homogenates. |
| Striatal Primary Neuron Kit | Ready-to-use cells and media for establishing in vitro models of dopamine neurotransmission. |
Technical Support Center: Troubleshooting & FAQs for Dopamine Receptor Antagonist (DRA) Switching Experiments
This support center provides guidance for common experimental and clinical translation challenges encountered when investigating antipsychotic switching strategies to minimize motor side effects (e.g., akathisia, dystonia, parkinsonism, tardive dyskinesia) within dose optimization research.
FAQ Section
Q1: During a cross-titration switch in an animal model, we observe a paradoxical spike in catalepsy scores. What could be the cause?
- A: This is often due to simultaneous partial occupancy at D2 receptors by both the outgoing and incoming antipsychotic, leading to a transient cumulative over-antagonism. Ensure the dose reduction curve of the first agent is steeper. Re-evaluate the receptor binding kinetics (Koff rates) of both drugs; a slow-dissociating outgoing drug may require a longer washout period before the new drug is introduced.
Q2: Our plasma level monitoring during a switch shows expected concentrations, but receptor occupancy modeling (using PET data or surrogate markers) is inconsistent. How should we troubleshoot?
- A: First, verify the pharmacokinetic (PK) model used. Antipsychotics often have active metabolites (e.g., norclozapine) that contribute to total receptor occupancy but may not be measured by your assay. Check for drug-drug interactions affecting protein binding or liver metabolism (CYP450 enzymes), which alter free, pharmacologically active drug levels despite normal total plasma concentrations.
Q3: When implementing a "stop-and-go" protocol to switch to aripiprazole, some subjects exhibit acute akathisia. What is the recommended mitigation strategy for the protocol?
- A: Acute akathisia upon initiating aripiprazole is linked to its partial agonist activity at D2 receptors. The protocol should include a lower starting dose (e.g., 2-5 mg in humans; proportionally scaled for preclinical models) than the target therapeutic dose. A slower up-titration schedule over 10-14 days is mandatory. Consider transient use of a beta-blocker (e.g., propranolol) or benzodiazepine in the experimental design as a rescue metric, but account for their confounding effects on locomotor assays.
Q4: How do we objectively differentiate between emergent tardive dyskinesia (TD) and withdrawal dyskinesias during an antipsychotic switch?
- A: This requires temporally dense assessment. Use standardized rating scales (e.g., AIMS) weekly. Withdrawal dyskinesias typically appear within 1-4 weeks of dose reduction/discontinuation and are often reversible. Emergent TD appears after initiating the new drug or during stable therapy. Polymyography or accelerometer-based motion capture can quantify dyskinetic movements' frequency and amplitude for clearer differentiation. Key differential data is summarized in Table 2.
Experimental Protocols
Protocol 1: Cross-Titration Switch with Behavioral & Molecular Correlates in a Rodent Model
- Objective: To seamlessly transition from haloperidol to lurasidone while minimizing catalepsy and monitoring striatal molecular adaptations.
- Animals: DBA/2J mice or Sprague-Dawley rats.
- Dosing:
- Days 1-7: Stabilize on haloperidol (1 mg/kg/day, i.p.).
- Days 8-14: Cross-titration. Reduce haloperidol by 0.2 mg/kg every other day while simultaneously initiating lurasidone at 1 mg/kg/day and increasing by 1 mg/kg every other day.
- Day 15 onward: Maintain on lurasidone (5 mg/kg/day).
- Assessment:
- Catalepsy Test: Daily, 2 hours post-dose, using the bar test. Record descent latency (max 30s).
- Tissue Collection: Subgroups euthanized at baseline, Day 7 (haloperidol stable), Day 10 (mid-switch), and Day 18 (lurasidone stable). Extract striatal protein.
- Western Blot: Analyze ∆FosB and phosphorylated ERK levels as markers of chronic neuronal adaptation and signaling pathway engagement.
- Troubleshooting: If severe catalepsy persists on Day 10, adjust the titration schedule to a 20% slower rate.
Protocol 2: In Vitro D2 Receptor Occupancy Kinetics Assay for Switching Predictions
- Objective: To measure the dissociation constant (Koff) of various DRAs to inform switching schedules.
- Cell Line: CHO or HEK293 cells stably expressing human D2L receptors.
- Method:
- Incubate cells with 5 nM [³H]-raclopride (a radiolabeled antagonist) for 60 mins at 37°C to achieve binding equilibrium.
- Initiate dissociation by adding 1000x excess of unlabeled competitor (e.g., haloperidol, olanzapine, aripiprazole).
- Rapidly wash and harvest replicate samples at time points: 0, 2, 5, 10, 20, 40, 60 minutes post-competition.
- Quantify remaining bound radioactivity via liquid scintillation counting.
- Plot natural log of % bound vs. time. The slope of the linear fit = -Koff.
- Application: Drugs with a slow Koff (e.g., olanzapine) will require a longer overlap or more gradual withdrawal when switching from them.
Data Presentation
Table 1: Receptor Binding Profiles of Common Antipsychotics in Switching Paradigms
| Antipsychotic | D2 Ki (nM) | D2 Koff Rate | 5-HT2A Affinity | Muscarinic M1 Affinity | Common Switch Rationale |
|---|---|---|---|---|---|
| Haloperidol | 1.1 | Moderate | Low | Very Low | High motor SE → Switch to newer agent |
| Olanzapine | 11 | Slow | High | High | Metabolic SE → Switch to neutral agent |
| Risperidone | 3.0 | Fast | High | Low | Prolactin elevation → Switch |
| Aripiprazole | 0.8 | Fast | High (Partial) | Low | For residual negative/cognitive symptoms |
| Lurasidone | 1.1 | Moderate | High | Very Low | From sedating/ metabolic risk agents |
Table 2: Differentiating Dyskinesias During Switching
| Feature | Withdrawal Dyskinesias | Emergent Tardive Dyskinesia |
|---|---|---|
| Typical Onset | 1-4 weeks after dose reduction | 3+ months after drug initiation (can be earlier in vulnerable) |
| Course | Usually transient (weeks-months) | Persistent and potentially irreversible |
| Topography | Often similar to prior TD, if present | Can be oro-buccal-lingual or limb-truncal |
| Response to Re-challenge | Suppresses with DRA re-introduction | May worsen or be unaffected |
Mandatory Visualizations
Title: Decision Flowchart for Antipsychotic Switching Strategy Selection
Title: Key Striatal Signaling Pathway Modulated by DRA Binding
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in Switching Studies |
|---|---|
| [[³H]-Raclopride | Radioligand for competitive binding assays to determine D2 receptor occupancy and dissociation constants (Koff) in vitro. |
| cAMP ELISA Kit | Quantifies intracellular cAMP levels downstream of D2 receptor antagonism in cell cultures or tissue homogenates. |
| Phospho-ERK (Thr202/Tyr204) Antibody | Detects activation of the MAPK/ERK pathway, a key signaling change associated with chronic antipsychotic treatment and motor side effects. |
| ΔFosB Antibody | Marker of chronic neuronal adaptation in the striatum; elevated levels correlate with long-term DRA exposure and dyskinesia risk. |
| Catalepsy Bar Test Apparatus | Standardized equipment (typically a horizontal bar) to objectively measure motor rigidity and bradykinesia in rodent models. |
| Accelerometer/Telemetry Implants | For continuous, objective monitoring of locomotor activity and dyskinetic movements in freely moving animals during switch protocols. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold standard for quantifying plasma and tissue levels of antipsychotics and their active metabolites during PK/PD studies. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: In our rodent model, amantadine pre-treatment fails to significantly reduce catalepsy induced by a high-potency D2 antagonist. What are potential experimental issues?
- A: This could be due to pharmacokinetic mismatching or receptor saturation.
- Check Timing: Amantadine's peak NMDA antagonism occurs 1-3 hours post-administration in rodents. Ensure your D2 antagonist is administered during this window. Consider a time-course experiment.
- Verify Dose: Standard rodent doses range from 10-40 mg/kg IP. Use the lower range for pre-treatment. See Table 1 for reference.
- Assess D2 Antagonist Dose: Your DRA dose may be too high, fully saturating D2 receptors and overriding modulatory effects. Titrate the DRA dose downward to find a window where modulation is detectable.
- Control for Core Temperature: Amantadine can cause mild hyperthermia, which may independently affect motor activity. Monitor and control for body temperature.
Q2: When testing Vitamin E (alpha-tocopherol) for preventing tardive dyskinesia (TD) in a long-term model, what formulation and route are optimal, and how do we assess bioavailability?
- A: Vitamin E's efficacy is highly dependent on formulation.
- Route & Formulation: For chronic studies in rodents, use dietary supplementation (500-2000 IU/kg of diet) for stable plasma levels. For acute/intervention studies, use water-miscible forms of d-alpha-tocopherol (not acetate) administered orally or via injection (e.g., 100-300 mg/kg). Oil-based oral gavage has poor and variable absorption.
- Assess Bioavailability: Do not rely solely on administered dose. At sacrifice, collect plasma and brain striatal tissue. Measure alpha-tocopherol levels via HPLC with electrochemical detection. A significant increase in brain tocopherol confirms CNS penetration.
Q3: Our cell-based assay shows inconsistent results when co-administering a sigma-1 receptor agonist with a D2 antagonist to measure cAMP shifts. What are key protocol controls?
- A: Inconsistency often stems from variable receptor expression levels or off-target effects.
- Characterize Receptor Density: Validate your cell line's D2 and sigma-1 receptor expression via radioligand binding or qPCR at the start of each experimental batch.
- Include Precise Controls: For each experiment, include: 1) Vehicle control, 2) D2 antagonist alone (e.g., 100 nM haloperidol), 3) Sigma-1 agonist alone (e.g., 10 nM PRE-084), 4) Co-administration group. Run all conditions in the same passage of cells.
- Use a Validated cAMP Assay: Use a HTRF or ELISA-based cAMP kit with a phosphodiesterase inhibitor (e.g., IBMX) in the assay buffer to prevent cAMP degradation. Pre-incubate sigma-1 ligand for 15 minutes before adding D2 antagonist.
Q4: How do we design a protocol to test the synergy between an anticholinergic (e.g., benztropine) and amantadine for reducing acute dystonia?
- A: A rigorous isobolographic analysis is required to prove synergy, not just additive effects.
- Experimental Design: Establish dose-response curves for each drug alone in reducing dystonia scores. From these, calculate the ED50 for each.
- Combination Ratios: Administer fixed-ratio combinations of the two drugs (e.g., 1:1, 1:3, 3:1 of their respective ED50s).
- Analysis: Plot the combined ED50 values on an isobologram. If the data points fall below the line of additivity, synergy is indicated. Statistical analysis requires testing the difference between the observed combined ED50 and the theoretical additive ED50.
Table 1: Adjunctive Therapy Dosing & Efficacy in Preclinical Models
| Modulator | Primary Mechanism | Typical Preclinical Dose (Rodent) | Model & Outcome Measure | Reported Efficacy (% Reduction vs. DRA alone) |
|---|---|---|---|---|
| Amantadine | NMDA receptor antagonism | 10-40 mg/kg (IP or SC) | Haloperidol-induced catalepsy (bar test) | 40-60% reduction in catalepsy time |
| Vitamin E (α-Tocopherol) | Lipid peroxidation inhibition | 100-300 mg/kg/day (PO, chronic) | Reserpine- or VMAT2 inhibitor-induced orofacial dyskinesia | 30-50% reduction in vacuous chewing movements |
| Benztropine | Muscarinic M1 antagonism | 0.1-1 mg/kg (IP) | Acute dystonia induced by high-dose DRA | 60-80% reduction in dystonia severity score |
| Pramipexole | D2/D3 autoreceptor agonist | 0.1-0.3 mg/kg (SC) | L-DOPA-induced dyskinesia (6-OHDA model) | 45-65% reduction in abnormal involuntary movements (AIMs) |
| Deuterated Tetrabenazine | VMAT2 inhibitor (with reduced metabolism) | 0.5-1.5 mg/kg (PO) | Tardive Dyskinesia (chronic haloperidol model) | 50-70% reduction in AIMs with improved pharmacokinetic profile |
Table 2: Key Human Clinical Trial Outcomes for Adjunctive Therapies
| Modulator | Patient Population | Trial Design & Duration | Primary Endpoint | Result (vs. Placebo + DRA) |
|---|---|---|---|---|
| Amantadine | Schizophrenia with TD | RCT, 4 weeks | AIMS (Abnormal Involuntary Movement Scale) | Significant reduction (Δ -3.5 points) |
| Vitamin E | Tardive Dyskinesia | Meta-analysis of RCTs, 4-52 weeks | AIMS or TD severity scale | Modest, short-term benefit; no disease-modifying evidence |
| Ginkgo Biloba Extract | Schizophrenia with TD | RCT, 12 weeks | AIMS total score | Significant reduction (Δ -2.7 points) |
Experimental Protocols
Protocol 1: Assessing Amantadine on DRA-Induced Catalepsy in Mice Objective: To quantify the reduction in catalepsy duration via amantadine pre-treatment.
- Animals: C57BL/6J mice (n=10-12/group).
- Drug Prep: Prepare amantadine HCl (10 mg/kg) in saline. Prepare haloperidol (1 mg/kg) in a weak acetic acid/saline solution.
- Pre-treatment: Administer amantadine or vehicle (IP) at time T=0.
- DRA Challenge: At T=60 min, administer haloperidol (IP).
- Catalepsy Test: At T=90, 120, 150, 180 min, place mouse's forepaws on a horizontal bar (0.5 cm diameter, 4.5 cm high). Measure time until mouse removes one paw (cut-off: 120 sec).
- Analysis: Calculate total catalepsy time (sum of durations across time points). Compare groups using one-way ANOVA.
Protocol 2: Evaluating Vitamin E in a Rat Model of Tardive Dyskinesia Objective: To determine if chronic Vitamin E diet prevents VCMs induced by a typical antipsychotic.
- Animals & Diet: Sprague-Dawley rats. Randomize to: Control diet, Vitamin E-enriched diet (2000 IU/kg), Haloperidol-decanoate (28.5 mg/kg IM every 3 weeks) + Control diet, Haloperidol + Vitamin E diet.
- Chronic Dosing: Continue for 12 weeks.
- Behavioral Scoring: In the final week, record 10-minute video sessions in a clear observation chamber. A blinded rater scores Vacuous Chewing Movements (VCMs) defined as vertical jaw movements without substrate.
- Biochemical Verification: Euthanize, dissect striatum. Homogenize and extract lipids. Analyze alpha-tocopherol content via HPLC-ECD.
- Analysis: Compare mean VCMs/hour between haloperidol groups using t-test, correlating with brain tocopherol levels.
Visualizations
Title: Amantadine Modulation of DRA-Induced Motor Pathway
Title: Integrated Workflow for Testing Adjunctive Therapies
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Relevance to Research |
|---|---|
| Haloperidol Decanoate (oil-based) | Long-acting D2 antagonist for creating chronic, stable antagonism in rodent TD models, mimicking clinical depot injections. |
| d-alpha-Tocopherol (water-miscible) | The bioactive, antioxidant form of Vitamin E required for intervention studies; ensures consistent bioavailability. |
| IBMX (3-Isobutyl-1-methylxanthine) | A phosphodiesterase inhibitor used in cell-based cAMP accumulation assays to prevent degradation of the second messenger. |
| Crawley's Behavioral Rig | Standardized apparatus for catalepsy testing (bar, corks) ensuring reproducible measurements of motor rigidity. |
| HTRF cAMP Gs Dynamic Kit | Homogeneous, non-radioactive assay for quantifying intracellular cAMP levels in real-time in D2-expressing cell lines. |
| AIMS (Abnormal Involuntary Movement Scale) | The gold-standard clinical assessment tool; must be adapted and rigorously blinded for scoring rodent dyskinesias (VCMs, AIMs). |
| Isobologram Analysis Software | Essential for determining drug interactions (additive, synergistic, antagonistic) between DRAs and adjunctive agents. |
| HPLC with Electrochemical Detection | Required for sensitive quantification of antioxidants (e.g., alpha-tocopherol) and monoamines in brain tissue. |
Evaluating Efficacy: Comparative Analysis of Novel Agents and Optimization Strategies
Technical Support Center: Troubleshooting & FAQs
FAQ 1: What are the primary methodological controls required when assessing catalepsy in rodent models to ensure data accurately reflects D2 receptor antagonism in the nigrostriatal pathway?
Answer: Ensure the following controls are in place:
- Positive Control: Administer a known typical antipsychotic (e.g., haloperidol, 1 mg/kg i.p.) to establish a baseline catalepsy response.
- Negative Control: Use vehicle-only administration (e.g., saline, 1% Tween-80) to account for handling and injection stress.
- Strain/Sex Matching: Use age- and weight-matched animals from the same inbred strain and sex to reduce biological variability.
- Blinded Scoring: The experimenter scoring the catalepsy duration (e.g., time the animal remains on a horizontal bar) must be blinded to the treatment groups.
- Environment: Conduct tests in a quiet, low-light, consistent environment at the same time of day to minimize circadian and stress-induced fluctuations.
FAQ 2: In PET imaging studies quantifying striatal D2 receptor occupancy, how do we troubleshoot high inter-subject variability in occupancy measurements for a given dose?
Answer: High variability often stems from pharmacokinetic differences. Follow this checklist:
- Verify Radiotracer Kinetics: Ensure the scanning protocol (e.g., for [¹¹C]raclopride) uses an equilibrium method or a validated kinetic model (like Simplified Reference Tissue Model, SRTM). Re-analyze raw time-activity curves for outliers.
- Control Plasma Protein Binding: Measure free fraction (fP) of the radiotracer in plasma. High variability in fP directly causes variability in occupancy estimates. Correct Binding Potential (BP) values using the individual's fP.
- Confirm Dose Administration & Compliance: For human studies, use directly observed therapy or plasma level monitoring of the antipsychotic to confirm the administered dose.
- Account for Endogenous Dopamine: Subject arousal/stress can alter synaptic dopamine, competing with the radiotracer. Standardize pre-scan conditions (resting state, minimal stimuli).
FAQ 3: When performing immunohistochemistry for c-Fos expression in the striatum to map neuronal activity, how can non-specific staining in the dorsolateral striatum (DLS) be minimized?
Answer: Non-specific staining in the DLS is common. Optimize your protocol:
- Fixative Perfusion: Ensure rapid and consistent perfusion with 4% paraformaldehyde (PFA). Incomplete fixation increases background.
- Antibody Titration: Perform a serial dilution series for your primary anti-c-Fos antibody (e.g., 1:500, 1:1000, 1:2000) to find the optimal signal-to-noise ratio. A too-concentrated antibody causes background.
- Blocking Step: Extend the blocking time to 2 hours at room temperature using a blocking solution containing 5% normal serum from the secondary antibody host species and 0.3% Triton X-100.
- Stringent Washes: Increase the number and duration of washes with PBS-T (0.1% Tween-20) after primary and secondary antibody incubations (e.g., 5 x 5 minutes).
- Secondary Control: Always include a "no-primary" antibody control section to identify non-specific binding from the secondary antibody or detection system.
Data Presentation: Quantitative Side Effect Profiles
Table 1: Comparative Incidence of Motor Side Effects in Clinical Populations
| Antipsychotic Class & Example | Approximate D2 Occupancy at Therapeutic Dose | Incidence of Parkinsonism | Incidence of Akathisia | Incidence of Tardive Dyskinesia (Annualized) |
|---|---|---|---|---|
| Typical (High-Potency) Haloperidol | 70-80% | High (25-35%) | High (20-30%) | ~5% |
| Typical (Low-Potency) Chlorpromazine | 60-75% | Moderate (15-25%) | Moderate (10-20%) | ~4% |
| Atypical (SDA) Risperidone | 70-80% | Moderate-Dose Dependent (15-30%) | Moderate-Dose Dependent (15-25%) | ~1-2% |
| Atypical (MARTA) Olanzapine | 60-70% | Low (5-10%) | Low (5-10%) | ~0.5-1% |
| Atypical (Partial Agonist) Aripiprazole | 70-90% (partial) | Low-Moderate (10-15%) | Moderate-High (20-25%) | ~0.5% |
Table 2: Key Metrics from Preclinical Catalepsy Models
| Antipsychotic | ED₅₀ for Catalepsy (mg/kg, rodent) | Threshold D2 Occupancy for Catalepsy Onset | Serotonin 5-HT₂A/D2 Binding Affinity Ratio (Ki ratio) |
|---|---|---|---|
| Haloperidol (Typical) | ~0.5 - 1.0 | ~75-80% | Low (~0.1 - 1) |
| Risperidone (Atypical) | ~1.0 - 2.5 | ~80-85% | High (~10 - 20) |
| Olanzapine (Atypical) | ~2.5 - 5.0 | ~75-80% | Very High (~20 - 40) |
| Clozapine (Atypical) | >20 (often absent) | No clear threshold | Extremely High (>100) |
Experimental Protocols
Protocol 1: In Vivo D2 Receptor Occupancy Assessment using [³H]Raclopride Ex Vivo Autoradiography
Objective: Quantify striatal D2 receptor occupancy by an antipsychotic in a rodent brain. Materials: See "Scientist's Toolkit" below. Procedure:
- Dosing: Administer test antipsychotic or vehicle to rats (n=6-8/group) via appropriate route (e.g., i.p., s.c.).
- Radiotracer Injection: At expected Tmax of drug (e.g., 60 min post-injection), administer [³H]Raclopride (300 μCi/kg, i.v.) via tail vein.
- Sacrifice & Dissection: Euthanize animal 30 minutes after radiotracer injection by rapid decapitation. Immediately extract brain, freeze in isopentane (-40°C), and store at -80°C.
- Sectioning: Cut 20 μm coronal sections at the striatal level using a cryostat. Thaw-mount onto charged glass slides.
- Autoradiography: Expose slides, along with radioactive standards, to a tritium-sensitive phosphor imaging plate for 3-4 weeks.
- Analysis: Quantify optical density in dorsolateral striatum using imaging software. Convert to radioactivity (nCi/mg) using the standard curve. Calculate receptor occupancy: Occupancy (%) = [1 - (BoundDrug / BoundVehicle)] * 100.
Protocol 2: Bar Test for Catalepsy Measurement
Objective: Quantify drug-induced catalepsy as a proxy for extrapyramidal side effects. Procedure:
- Habituation: Habituate rodents to the testing room and apparatus (a horizontal wooden bar of 1 cm diameter, elevated 10 cm) for 30 minutes prior to testing.
- Dosing & Timing: Administer drug or vehicle. Begin testing at pharmacokinetic Tmax.
- Testing: Gently place the animal's front paws over the bar. Start a stopwatch.
- Scoring: Stop the timer when the animal removes one front paw from the bar or makes a coordinated movement to climb onto the bar. The maximum cutoff time is typically 60 seconds.
- Replication: Perform the test 3-4 times per animal at each time point (e.g., every 30 min for 3 hours), with at least 5 minutes between trials. Use the average score for analysis.
- Data Normalization: Express data as mean catalepsy duration (sec) ± SEM per group. Compare to positive (haloperidol) and negative (vehicle) controls.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Research |
|---|---|
| [³H]Raclopride or [¹¹C]Raclopride | Radioligand for quantifying D2/D3 receptor density and occupancy in vitro (autoradiography) or in vivo (PET). |
| Haloperidol (High-Potency D2 Antagonist) | Gold-standard positive control for inducing catalepsy and high striatal D2 occupancy in preclinical models. |
| Clozapine (Atypical Antagonist) | Gold-standard negative control for minimal catalepsy despite D2 binding; used to study "atypical" mechanisms. |
| Selective 5-HT₂A Antagonist (e.g., M100907) | Pharmacological tool to dissect the contribution of serotonin receptor blockade to mitigating motor side effects. |
| Phospho-Specific Antibodies (e.g., pERK, pAKT, pGSK3β) | Detect activation states of intracellular signaling pathways downstream of D2 and 5-HT₂A receptors in striatal tissue. |
| c-Fos & ΔFosB Antibodies | Markers for neuronal activity and long-term neuroadaptations in striatal subregions (matrix vs. striosome). |
| AIMS (Abnormal Involuntary Movement Scale) | Standardized clinical assessment tool for rating severity of tardive dyskinesia in human subjects. |
| Simulated PET Data Analysis Software (e.g., PMOD) | Used for kinetic modeling of dynamic PET data to calculate Binding Potential and receptor occupancy. |
Mandatory Visualizations
Title: Mechanism of Atypical APs Reducing Motor Side Effects
Title: Ex Vivo D2 Occupancy Assay Workflow
Troubleshooting Guides & FAQs
FAQ 1: In our rodent catalepsy assay, cariprazine shows negligible effect at low doses but induces significant motor impairment at higher doses, contradicting its reported favorable motor profile. What could be the cause?
- Answer: This is likely due to the dose-dependent receptor occupancy profile. Cariprazine is a D3-preferring partial agonist. At low doses, it predominantly occupies D3 receptors. At higher doses, it occupies a significant proportion of D2 receptors. The motor side effects (catalepsy) are directly linked to high striatal D2 receptor occupancy (>80%). Troubleshooting Steps:
- Validate your dose range using receptor occupancy modeling. Perform an ex vivo receptor occupancy assay parallel to your behavioral study.
- Ensure you are using a clinically relevant dose translation from animal to human equivalents; the therapeutic window may be narrower in your model.
- Check the pharmacokinetics; cariprazine has active metabolites (DCAR and DDCAR) with long half-lives. Your observed effect may be due to metabolite accumulation.
FAQ 2: When testing a multi-targeting agent (e.g., acting on 5-HT2A, D2, and α2A), how do we isolate which receptor action is responsible for reducing D2 antagonist-induced EPS in our model?
- Answer: Employ a selective antagonist co-administration (pharmacological subtraction) protocol.
- Experimental Protocol:
- Group 1: Vehicle + Standard D2 antagonist (e.g., haloperidol).
- Group 2: New multi-target agent + haloperidol.
- Group 3: New multi-target agent + haloperidol + Selective 5-HT2A antagonist (e.g., M100907).
- Group 4: New multi-target agent + haloperidol + Selective α2A antagonist (e.g., BRL-44408).
- Measure EPS (e.g., step-down test, bar test). If EPS returns in Group 3, the 5-HT2A action of the new agent is likely critical for EPS mitigation.
- Experimental Protocol:
FAQ 3: Our cell-based β-arrestin recruitment assay shows weak signal for a new partial agonist, making efficacy (%Emax) calculations unreliable.
- Answer: This is a common issue with low-intrinsic-activity compounds. Troubleshooting Steps:
- Signal Amplification: Switch to a more sensitive reporter system (e.g., NanoBiT β-arrestin).
- Positive Control: Use a full agonist (e.g., quinpirole for D2) and a full antagonist to define your window. Ensure your reference partial agonist (e.g., aripiprazole) performs as expected in your system.
- Cell Line Verification: Confirm high receptor expression levels via qPCR or flow cytometry. Low receptor density can compress the signal window.
Table 1: Receptor Binding Profiles (Ki, nM) of Selected Agents
| Agent | D2 | D3 | 5-HT1A (Agonism) | 5-HT2A (Antag.) | α2A (Antag.) | Reference |
|---|---|---|---|---|---|---|
| Cariprazine | 0.49 | 0.085 | NA | 18.8 (Weak) | 155 (Weak) | Kiss et al., 2010 |
| Aripiprazole | 1.64 | 4.57 | Partial Agonist | 8.7 | 28 | Shapiro et al., 2003 |
| Haloperidol | 1.1 | 2.9 | NA | 45 | 410 | Seeman, 2002 |
| Brexpiprazole | 0.3 | 1.1 | Partial Agonist | 0.47 | 0.17 | Maeda et al., 2014 |
Table 2: In Vivo EPS Threshold (Estimated D2 Occupancy)
| Agent / Class | Catalepsy Threshold (% Striatal D2 Occupancy) | Key Differentiating Property |
|---|---|---|
| Typical Antipsychotic | ~70-80% | High D2 affinity, full antagonism |
| Aripiprazole | >90% | D2 partial agonism, high 5-HT1A activity |
| Cariprazine | ~80-85% | D3-preference, functional selectivity |
| Multi-target Agent (e.g., Brexpiprazole) | ~85-90% | Combined 5-HT1A/5-HT2A/α2A modulation |
Experimental Protocols
Protocol 1: Ex Vivo Dopamine D2/D3 Receptor Occupancy Assay in Rodent Striatum
- Objective: Quantify the percentage of D2/D3 receptors occupied by a test agent at a given time post-administration.
- Materials: Radioligand [³H]-raclopride (D2/D3 antagonist), [³H]-PD-128907 (D3-preferring agonist), test compound, vehicle, tissue homogenizer, scintillation counter.
- Method:
- Administer test compound or vehicle to rats (n=6/group) and sacrifice at Tmax (e.g., 30-60 min for many APs).
- Rapidly dissect striatum, homogenize in ice-cold buffer.
- Incubate homogenate with a saturating concentration of [³H]-raclopride (for total D2/D3) or [³H]-PD-128907 (for D3) with/without excess unlabeled competitor (e.g., haloperidol) to define total and non-specific binding.
- Filter and wash to separate bound from free radioligand.
- Measure radioactivity via scintillation counting.
- Calculation: % Occupancy = [1 - (Specific bound drug-treated / Specific bound vehicle-treated)] x 100.
Protocol 2: Functional Selectivity Assay – G protein vs. β-arrestin Pathway
- Objective: Determine if a novel agent exhibits bias toward G protein (cAMP inhibition) or β-arrestin recruitment at the D2 receptor.
- Materials: HEK-293 cells stably expressing human D2L receptor, cAMP-Glo Assay (Promega), PathHunter β-Arrestin Assay (Eurofins), test agonists (full, partial, antagonist), forskolin.
- Method (Parallel Assays):
- G Protein (cAMP Inhibition): Stimulate cells with forskolin (to elevate cAMP) + varying doses of test agent. Use cAMP-Glo to quantify luminescence (inversely proportional to cAMP). Fit data to calculate EC50 and Emax.
- β-Arrestin Recruitment: Use engineered PathHunter cells. Add varying doses of test agent to induce β-arrestin recruitment, which complements an enzyme fragment, generating chemiluminescence. Measure signal and calculate EC50 and Emax.
- Bias Calculation: Normalize data to a reference full agonist (e.g., dopamine). Calculate ΔΔLog(τ/KA) using the Black-Leff operational model to quantify bias factor (β-arrestin vs. G protein).
Diagrams
Title: Signaling Bias of D2 Partial Agonists
Title: EPS Mitigation via Multi-Receptor Targeting
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research | Example Product / Cat. Number |
|---|---|---|
| Cell Line: hD2L-HEK293 | Stable expression of human dopamine D2 Long receptor for consistent in vitro signaling assays. | ATCC CRL-1573 (modified) |
| Radioligand: [³H]-Raclopride | Antagonist radioligand for measuring total D2/D3 receptor density and occupancy in binding studies. | PerkinElmer NET-975 |
| cAMP Detection Kit | Homogeneous, luminescent assay to quantify intracellular cAMP levels for G protein activity profiling. | Promega cAMP-Glo Assay V1502 |
| β-Arrestin Recruitment Assay | Enzyme fragment complementation assay for measuring ligand-induced β-arrestin recruitment. | Eurofins DiscoverX PathHunter 93-0001 |
| Selective Pharmacological Tool: M100907 | Highly selective 5-HT2A receptor antagonist for pathway isolation experiments. | Tocris 2582 |
| In Vivo EPS Model: Bar Test Apparatus | Standardized equipment for quantifying catalepsy (immobility time) in rodents. | Ugo Basile 78250 |
Meta-Analyses of Dose-Response Relationships and Side Effect Incidence
Troubleshooting Guides & FAQs
Q1: Our systematic search for DRA studies yields heterogeneous motor side effect scales (e.g., SAS, AIMS, BAS). How do we standardize data for the meta-analysis? A: Heterogeneity is common. Perform a data transformation to a common metric.
- For continuous data (e.g., total score change), calculate the Standardized Mean Difference (SMD), typically Hedges' g, which corrects for small sample bias. Use the pre- and post-treatment means, standard deviations, and sample sizes from each arm. Software like RevMan or R (
metaforpackage) automates this. - For dichotomous data (e.g., incidence of akathisia), use the Risk Ratio (RR) or Odds Ratio (OR) with their 95% confidence intervals. Ensure you extract the number of events and total patients per dose group.
- Protocol: Always pre-specify your chosen method and all secondary/sensitivity analyses in your PROSPERO protocol.
Q2: When modeling dose-response, how do we handle studies that report only categorical dose levels (e.g., low, medium, high) instead of exact mg/day doses? A: Assign a numerical value based on established dose equivalency tables and conduct sensitivity analyses.
- Use consensus tables (e.g., Andreasen et al., Leucht et al.) to convert doses to chlorpromazine or haloperidol equivalents for the specific DRA.
- Assign the mid-point of the reported dose range. For an open-ended "high dose" category, use 1.5 times the lower limit (e.g., ">20mg" becomes 30mg).
- Critical Step: Perform a sensitivity analysis by excluding these studies or using different assignment rules to test the robustness of your dose-response curve.
Q3: Our dose-response meta-regression shows high statistical heterogeneity (I² > 75%). What are the main sources and how can we address them? A: High I² is expected. Investigate and model the heterogeneity, do not just note it.
- Common Sources:
- Patient population (treatment-naïve vs. chronic, diagnosis specificity).
- DRA generation (typical vs. atypical).
- Study duration (acute vs. maintenance).
- Definition and measurement tool for the side effect.
- Solutions:
- Subgroup Analysis: Stratify by the above factors. See Table 1.
- Meta-Regression: Model heterogeneity by including covariates (e.g., mean patient age, baseline severity) in your regression model to explain variance.
- Use a Random-Effects Model: Always assume a distribution of true effects.
- Report and discuss residual heterogeneity.
Q4: How should we graphically present the incidence of different motor side effects (EPS, akathisia, TD) across multiple DRA agents? A: Use a structured, comparative table for clarity. Supplement with a forest plot for key comparisons. See Table 2 for an example structure.
Q5: What is the best method to model a non-linear (e.g., U-shaped or sigmoidal) dose-response relationship for efficacy vs. side effects? A: Use restricted cubic splines or fractional polynomial models in a one-stage or two-stage meta-analysis.
- Protocol (Two-Stage):
- Fit a flexible non-linear model (e.g., cubic spline with 3 knots) within each study that reports multiple dose arms.
- Extract the dose-specific effect estimates (e.g., log OR for side effect) at a set of pre-defined dose values (e.g., 0, 5, 10, 20mg haloperidol eq.).
- Pool these dose-specific estimates across studies in the second stage using multivariate meta-analysis, accounting for within-study correlation.
Data Presentation
Table 1: Subgroup Analysis to Investigate Heterogeneity in DRA-Induced Akathisia Incidence
| Subgroup | Studies (n) | Pooled RR vs. Placebo | 95% CI | I² | P for Subgroup Difference |
|---|---|---|---|---|---|
| DRA Type | |||||
| Typical Antagonists | 12 | 3.45 | [2.80, 4.25] | 78% | <0.01 |
| Atypical Antagonists | 18 | 1.82 | [1.50, 2.21] | 65% | |
| Treatment Duration | |||||
| ≤ 6 weeks | 20 | 2.95 | [2.40, 3.62] | 81% | 0.04 |
| > 6 weeks | 10 | 2.20 | [1.85, 2.62] | 45% | |
| Baseline Risk | |||||
| High (>10% in placebo) | 8 | 2.10 | [1.70, 2.59] | 30% | 0.02 |
| Low (≤10% in placebo) | 22 | 3.10 | [2.55, 3.77] | 82% |
Table 2: Comparative Incidence of Motor Side Effects for Selected DRAs (from Meta-Analysis)
| Drug (Haloperidol Eq. Dose) | Acute EPS Pooled Incidence (%) | Akathisia Pooled RR | Tardive Dyskinesia (Annualized Risk %) | Key Dose-Dependent Threshold |
|---|---|---|---|---|
| Haloperidol (5mg/day) | 22.5 | 4.2 | ~5.0% | EPS risk increases sharply >3mg/day |
| Risperidone (4mg/day) | 15.1 | 2.5 | ~2.5% | EPS > 6mg/day approaches typicals |
| Olanzapine (10mg/day) | 8.4 | 1.8 | ~1.8% | Low EPS across therapeutic range |
| Aripiprazole (10mg/day) | 7.9 | 2.1 | ~1.2% | Akathisia peak at initiation/low dose |
Experimental Protocols
Protocol: Two-Stage Dose-Response Meta-Analysis for DRA Motor Side Effects Objective: Quantify the relationship between DRA dose (in haloperidol equivalents) and probability of acute parkinsonism.
- Systematic Search & Inclusion:
- Databases: PubMed, Embase, Cochrane Central, clinicaltrials.gov.
- Inclusion: RCTs comparing ≥2 fixed doses of the same oral DRA or a fixed dose to placebo, reporting parkinsonism (SAS or specific item) as dichotomous outcome or continuous score.
- Data Extraction:
- For each study arm: sample size, number of events (for dichotomous) OR mean score change and SD (for continuous), exact dose (converted to haloperidol equivalents using defined table).
- Covariates: mean age, diagnosis, study duration, DRA agent.
- Statistical Analysis (Two-Stage):
- Stage 1: Within each multi-arm study, fit a logistic regression (for dichotomous outcome) or linear regression (for continuous outcome) with dose as the independent variable. From each model, predict the log(Odds Ratio) or mean difference at reference doses (e.g., 0, 2, 5, 10, 15, 20mg) relative to 0mg.
- Stage 2: Perform a multivariate random-effects meta-analysis to pool the dose-specific estimates from all studies, using the mvmeta package in R. This accounts for within-study correlation.
- Output: A pooled dose-response curve with 95% confidence band. Estimate the Effective Dose 50 (ED50) for a clinically significant increase in side effect risk.
Mandatory Visualization
Diagram 1: Two-Stage Dose-Response Meta-Analysis Workflow
Diagram 2: DRA Signaling Pathways Influencing Motor Side Effects
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in DRA Dose-Optimization Research |
|---|---|
| Haloperidol Equivalency Conversion Table | Standardizes dose comparisons across heterogeneous DRA agents for meta-analysis. |
| Simpson-Angus Scale (SAS) Tool | Validated 10-item instrument for quantifying drug-induced parkinsonism in clinical trials. |
| Barnes Akathisia Rating Scale (BARS) | Standard for assessing subjective and objective components of drug-induced akathisia. |
Multivariate Meta-Analysis Software (R mvmeta) |
Performs the crucial second-stage pooling in dose-response meta-analysis, modeling within-study correlation. |
Restricted Cubic Spline Functions (R rms package) |
Enables flexible modeling of non-linear dose-response relationships within studies. |
| Striatal D2 Receptor Occupancy PET Ligands (e.g., [11C]Raclopride) | Correlates administered dose with target engagement, establishing therapeutic vs. side-effect occupancy windows. |
Technical Support & Troubleshooting Center
FAQ & Troubleshooting Guide
Q1: During our longitudinal [¹¹C]Raclopride PET study to track D2 receptor occupancy, we observe high inter-scan variability in Binding Potential (BPND) in the striatum for the same subject under the same nominal dose. What are the primary technical sources of this variability and how can we mitigate them?
A: High variability in BPND can compromise dose-occupancy curve modeling. Key sources and solutions include:
- Motion Artifact: Head movement during the 60-90min scan significantly impacts quantification.
- Solution: Use a custom thermoplastic mask for immobilization. Implement real-time motion tracking with correction (e.g., frame-by-frame realignment) during reconstruction.
- Incorrect Arterial Input Function (AIF): Plasma metabolite analysis errors or delay/dispersion in the arterial line directly affect modeling.
- Solution: Regularly calibrate HPLC for metabolite analysis. Use a consistent, warmed saline flush for the arterial line. Validate AIF with a population-based approach if direct sampling is unreliable.
- Reference Region Selection: Use of the cerebellum as a reference assumes negligible D2 density. This can be invalidated by off-target binding or cerebellar pathology.
- Solution: Confirm participant screening excludes neurological cerebellar conditions. For novel drugs, validate reference region validity with a blocking study or consider using a supervised cluster-based reference region method.
Q2: When performing local field potential (LFP) recordings in the substantia nigra pars reticulata (SNr) to gauge indirect pathway activity post-antagonist administration, we encounter persistent 60 Hz line noise. Standard filtering removes the noise but also distorts our beta/gamma power signal of interest.
A: This common issue requires a hardware and processing approach:
- Grounding & Shielding: Ensure the recording rig, headstage, and animal ground are connected to a single, common earth ground point. Place the animal Faraday cage on a grounded copper plate. Use shielded cables for all inputs.
- Differential Recording: Confirm your system is using a true differential amplifier, recording the signal between an active and a reference electrode placed in quiet tissue (e.g., corpus callosum).
- Digital Notch Filtering: Apply a narrow-band notch filter (e.g., 58-62 Hz) only after extracting all segments of raw data for time-domain analysis. For spectral analysis (e.g., PSD), use a method robust to line noise, such as multitaper spectral estimation, which minimizes spectral leakage.
Q3: Our attempt to correlate striatal PET occupancy with cortical EEG beta power (13-30 Hz) yields inconsistent relationships across subjects. What are the key methodological pitfalls in this multimodal correlation?
A: This is a complex correlation. Ensure alignment in these three domains:
- Temporal Alignment: PET gives a time-averaged occupancy (~30-60 min window). EEG power must be averaged over the exact same temporal window post-drug administration, accounting for the drug's pharmacokinetic profile. Do not use a single 5-minute EEG epoch.
- Spatial Misalignment: PET occupancy is measured in the dorsal striatum (motor circuit). Your cortical EEG electrodes (e.g., C3, C4) must be validated to reflect activity from the cortico-striatal motor loop. Consider using source-localized EEG or concurrent MEG to improve spatial specificity.
- State Dependency: EEG beta power is highly state-dependent (alert vs. drowsy).
- Solution: Maintain vigilance monitoring (e.g., simultaneous EMG, video tracking) during the recording window and analyze only epochs of consistent, alert wakefulness.
Experimental Protocol: Integrated PET-EEG for D2 Antagonist Dose Validation
Objective: To establish a quantitative relationship between striatal D2 receptor occupancy (via PET) and electrophysiological biomarker change (cortical beta power) following administration of a dopamine receptor antagonist.
Detailed Methodology:
- Participant Preparation: Screen healthy volunteers for MRI/PET/EEG contraindications. Obtain informed consent.
- Baseline Scans:
- MRI: Acquire a high-resolution T1-weighted structural MRI for anatomical co-registration and ROI definition.
- PET Baseline: Perform a 60-minute dynamic [¹¹C]Raclopride PET scan with concurrent arterial blood sampling for AIF generation. BPND is calculated using the Simplified Reference Tissue Model (SRTM) with cerebellum as reference.
- EEG Baseline: Immediately following PET, conduct a 15-minute resting-state, eyes-open EEG recording with 64+ channels, impedance <5 kΩ. Maintain vigilance.
- Drug Administration & Post-Dose Session: After a washout period (>2 weeks), administer a pre-determined, single oral dose of the D2 antagonist.
- Post-Dose Scans (Time-Matched):
- At Tmax (time of peak plasma concentration) for the drug, repeat the dynamic PET scan (identical protocol).
- Simultaneously, conduct continuous EEG recording from pre-injection to 90 minutes post-injection.
- Data Analysis:
- PET: Calculate receptor occupancy (%) in the putamen ROI using the Lassen plot approach or the formula:
Occupancy (%) = (1 - (BP<sub>ND-post</sub> / BP<sub>ND-baseline</sub>)) * 100. - EEG: For the 30-60 minute window post-injection (matching the PET integration window), preprocess EEG (filter 1-100 Hz, notch 60 Hz, artifact rejection). Compute relative power spectral density (PSD) in the beta band (13-30 Hz) at central electrodes. Express as % change from baseline.
- Correlation: Perform linear/monotonic regression for occupancy (%) vs. beta power change (%) across subjects for each tested dose.
- PET: Calculate receptor occupancy (%) in the putamen ROI using the Lassen plot approach or the formula:
Data Presentation
Table 1: Common PET Radiotracers for D2/D3 Receptor Quantification
| Tracer | Primary Target | Key Advantage | Limitation for Dose Optimization |
|---|---|---|---|
| [¹¹C]Raclopride | D2/D3 (antagonist) | Well-validated, gold standard for occupancy studies. | Short half-life (20 min) limits scanning to ~90 min. |
| [¹⁸F]Fallypride | D2/D3 (antagonist) | High affinity, allows imaging of extrastriatal regions. | Long scanning requirement (~4 hours), slow kinetics. |
| [¹¹C]PHNO | D2/D3 (agonist) | Bias towards high-affinity state; differentiates agonist effects. | Binding is sensitive to endogenous dopamine swings. |
Table 2: Expected Direction of Key Biomarkers with D2 Antagonist Dose Escalation
| Biomarker Modality | Specific Measure | Expected Change with Increasing Dose | Rationale |
|---|---|---|---|
| PET Imaging | Striatal D2 Receptor Occupancy (BPND) | Decrease (Log-linear with dose) | Direct competition between drug and radiotracer. |
| Electrophysiology (LFP in rodents) | SNr Gamma Power (60-90 Hz) | Increase | Disinhibition of the indirect pathway leading to increased SNr activity. |
| Electrophysiology (EEG in humans) | Cortico-Muscular Coherence (Beta) | Increase | Reflects enhanced oscillatory coupling in the motor loop due to reduced dopaminergic inhibition. |
| Clinical Assessment | SAS (Simpson-Angus Scale) Score | Increase (after threshold) | Direct measure of emerging motor side effects (e.g., rigidity). |
The Scientist's Toolkit
Key Research Reagent Solutions for D2 Antagonist Biomarker Studies
| Item | Function & Rationale |
|---|---|
| Selective D2/D3 Antagonist (e.g., Raclopride, Haloperidol) | Function: Reference compound for establishing occupancy-side effect curves. Rationale: Well-characterized binding profile allows calibration of novel drug effects. |
| [¹¹C]Raclopride Radiotracer | Function: PET ligand for quantifying striatal D2/D3 receptor availability. Rationale: Reversible binding kinetics suitable for dynamic scanning and occupancy calculation. |
| Arterial Line Kit w/ Heparinized Saline | Function: Enables continuous arterial blood sampling during PET for metabolite-corrected input function. Rationale: Essential for accurate kinetic modeling of BPND. |
| High-Density EEG System (64+ channels) | Function: Records cortical electrophysiological activity with sufficient spatial detail. Rationale: Allows for source localization and identification of motor-cortex-specific oscillatory changes. |
| Stereotaxic Frame & Tungsten Microelectrodes (Rodent) | Function: Precise targeting of deep brain structures (e.g., Striatum, SNr) for in vivo electrophysiology. Rationale: Enables direct recording of pathway-specific neural ensemble activity. |
| Vigilance Monitoring System (EMG, EOG, Video) | Function: Tracks subject arousal state during EEG recordings. Rationale: Critical for controlling the confound of drowsiness on oscillatory power spectra. |
| Kinetic Modeling Software (e.g., PMOD, SPM) | Function: Processes dynamic PET data to generate parametric maps of BPND. Rationale: Provides the quantitative endpoint (receptor occupancy) for correlation with dose and side effects. |
Visualizations
Title: Multimodal Biomarker Correlation for Dose Optimization
Title: D2 Antagonist Effect on Indirect Pathway & Biomarkers
Cost-Effectiveness and Long-Term Outcomes of Optimized Dosing Regimens
Troubleshooting Guide & FAQs for Dopamine Receptor Antagonist Dosing Research
This technical support center is designed for researchers investigating optimized dosing regimens of dopamine receptor antagonists (DRAs) to minimize extrapyramidal motor side effects (EPS). The FAQs address common experimental challenges within the context of long-term efficacy and cost-effectiveness analysis.
FAQ 1: In our rodent catalepsy assay, we observe high variability in response to a fixed DRA dose. What are the primary factors to check?
Answer: High variability often stems from animal model or pharmacokinetic factors. Follow this troubleshooting protocol:
- Verify Animal Homogeneity: Ensure consistent species, strain, age, and weight across groups. Randomize housing and treatment assignment.
- Check Drug Preparation & Administration:
- Confirm solvent compatibility and stability of your DRA.
- Standardize injection technique (route, time of day, volume).
- Use freshly prepared solutions or validated frozen aliquots.
- Review Experimental Conditions: Maintain consistent environmental conditions (light/dark cycle, noise, handling) during the behavioral test.
- Protocol Suggestion: Implement a pilot dose-response curve (see Table 1) to establish the effective range for your specific model before optimization studies.
FAQ 2: When calculating the "cost-effectiveness" of a novel dosing regimen in a preclinical model, what parameters should be quantified?
Answer: For preclinical cost-effectiveness modeling, integrate both efficacy and resource data. Key parameters are summarized in Table 2.
Table 1: Example Dose-Response Data for DRA "X" in Rat Catalepsy Model
| DRA Dose (mg/kg) | Catalepsy Score (Mean ± SEM) | % Animals with EPS | Plasma Concentration (ng/mL) at Tmax |
|---|---|---|---|
| Vehicle | 0.5 ± 0.2 | 0% | 0 |
| 0.5 | 1.8 ± 0.3 | 10% | 15 ± 2 |
| 1.0 | 3.5 ± 0.4 | 45% | 32 ± 5 |
| 2.0 | 4.2 ± 0.5 | 85% | 68 ± 9 |
| 4.0 | 4.3 ± 0.6 | 90% | 135 ± 20 |
Table 2: Parameters for Preclinical Cost-Effectiveness Analysis
| Parameter Category | Specific Metrics | Measurement Method |
|---|---|---|
| Efficacy/Outcome | Reduction in PANSS score (simulated); EPS score; QoL behavioral metrics | Behavioral batteries, scoring scales. |
| Direct Costs | Drug quantity per dose; Dosing frequency; Duration of treatment. | Experimental design logs. |
| Resource Utilization | Staff time for administration; Monitoring equipment hours; Cost of managing side effects (e.g., additional meds for akathisia). | Lab time-tracking logs. |
| Composite Metric | Cost per unit of efficacy gain (e.g., cost per 1-point reduction in EPS score). | (Total Cost Regimen A - Cost Regimen B) / (Efficacy Outcome A - Efficacy Outcome B) |
FAQ 3: Our cell-based D2 receptor binding assay shows inconsistent results when testing sustained-release formulations. How should we adapt the protocol?
Answer: Traditional binding assays are designed for acute drug exposure. For sustained-release (SR) formulations, you must modify the protocol to mimic prolonged exposure.
- Revised Protocol:
- Pre-incubation: Incubate cells or membrane preparations with the SR DRA formulation for an extended period (e.g., 4-24 hours) under physiological conditions (37°C, 5% CO₂).
- Wash Steps: Carefully wash cells to remove unbound drug, simulating clearance while retaining receptor-bound drug.
- Radioligand Challenge: Perform the standard radioligand (e.g., [³H]-spiperone) binding assay. Reduced radioligand binding indicates occupancy by the pre-bound DRA.
- Control: Include a group pre-incubated with an equivalent dose of immediate-release DRA for comparison.
- Key Consideration: Validate that your wash procedure effectively removes free drug but does not strip receptor-bound drug by using a known high-affinity ligand control.
FAQ 4: What are the key steps to model long-term (6-month) outcomes for a novel intermittent DRA dosing regimen versus standard daily dosing?
Answer: Implement a longitudinal preclinical study with multiple outcome checkpoints.
- Experimental Workflow: See the diagram "Long-Term Preclinical Study Design" below.
- Core Assessments:
- Primary Efficacy: Behavioral tests relevant to the disease model (e.g., prepulse inhibition) at baseline, 1, 3, and 6 months.
- Motor Side Effects: Regular EPS scoring (catalepsy, tardive dyskinesia assessments).
- Pharmacokinetic (PK) Trough Levels: Measure plasma DRA concentration before the next dose to ensure consistent exposure.
- Post-Mortem Analysis: At endpoint, analyze striatal tissue for biomarkers like ΔFosB (long-term neural adaptation) and D2 receptor supersensitivity.
Long-Term Preclinical Study Design
FAQ 5: How do we establish a causal link between optimized dosing, reduced EPS, and long-term changes in striatal signaling pathways?
Answer: Integrate behavioral data with molecular endpoint analysis. The key signaling pathway involved in DRA-induced EPS is the D2 receptor-mediated indirect pathway in the striatum. Optimized dosing aims to modulate this pathway with less disruption.
D2 Antagonism Alters Striatal Motor Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for DRA Dosing Optimization Research
| Item | Function & Rationale |
|---|---|
| Selective D2/D3 Receptor Antagonist (e.g., Raclopride, Haloperidol) | Gold-standard tool for establishing baseline EPS response and validating animal models. |
| Atypical DRA with Lower EPS Risk (e.g., Clozapine, Aripiprazole) | Comparator for testing if optimized dosing of typical DRAs can achieve a similar side effect profile. |
| C-Fos & ΔFosB Antibodies | Immunohistochemistry markers for acute and chronic neuronal activation in striatal regions. |
| [³H]-Spiperone / [³H]-Raclopride | Radioligands for in vitro receptor binding assays and ex vivo receptor occupancy studies. |
| Catalepsy Bar Test Apparatus | Standardized equipment for quantifying the primary rodent model of drug-induced Parkinsonism. |
| Validated Tardive Dyskinesia Model (e.g., VCM in rats) | Essential for assessing long-term risk of irreversible motor side effects. |
| LC-MS/MS Assay Kit | For precise quantification of DRA and metabolite concentrations in plasma and brain tissue (PK/PD analysis). |
| Activity Monitoring Cages | To measure general locomotor activity and detect signs of akathisia (restlessness) in rodents. |
Conclusion
Optimizing dopamine receptor antagonist dosing to minimize motor side effects requires a multi-faceted approach grounded in a deep understanding of neurobiology, guided by precision medicine methodologies, and responsive to individual patient presentations. Key takeaways include the critical importance of staying within therapeutic receptor occupancy windows, the utility of TDM and pharmacogenomics for personalization, and the necessity of proactive monitoring and management protocols. The comparative success of newer agents with unique receptor profiles highlights a future direction focused on developing compounds with inherently higher therapeutic indices. For biomedical and clinical research, the implications point toward increased integration of real-world data with PK/PD models, the pursuit of validated predictive biomarkers, and the design of clinical trials that prioritize dose-finding for tolerability alongside efficacy, ultimately aiming to redefine the risk-benefit paradigm in DRA therapy.