Precision Gene Delivery for Neural Circuit Manipulation: Strategies, Tools, and Clinical Frontiers
This article provides a comprehensive overview of the cutting-edge gene delivery strategies revolutionizing neural circuit manipulation for researchers and drug development professionals.
Precision Gene Delivery for Neural Circuit Manipulation: Strategies, Tools, and Clinical Frontiers
Abstract
This article provides a comprehensive overview of the cutting-edge gene delivery strategies revolutionizing neural circuit manipulation for researchers and drug development professionals. It covers the foundational principles of viral vectors, notably adeno-associated viruses (AAVs), and their axonal transport properties. The scope extends to methodological applications, including serotype and promoter selection for cell-type-specific targeting, the integration of CRISPR tools for functional genomics, and advanced delivery techniques. It further addresses critical troubleshooting and optimization challenges such as immune responses and off-target effects, and concludes with rigorous validation and comparative analysis of emerging technologies. This resource synthesizes the current state of the field, offering a practical guide for designing precise neural circuit interventions with strong therapeutic potential.
The Blueprint of Brain Access: Viral Vectors and Circuit Tracing Fundamentals
Adeno-associated virus (AAV) has emerged as the predominant viral vector for in vivo gene delivery to the nervous system, revolutionizing approaches for neural circuit manipulation and the treatment of neurological disorders. Its ascendancy stems from a unique combination of favorable biological properties: non-pathogenicity, low immunogenicity, and the ability to mediate long-term transgene expression in post-mitotic neurons [1] [2]. The fundamental structure of AAV is elegantly simple—a protein capsid approximately 25 nm in diameter protecting a single-stranded DNA genome of ~4.7 kilobases—yet its application is powerfully versatile [3] [1]. For neuroscience research, AAV provides a precision toolset for delivering sensors, actuators, and modulators to defined neural populations, enabling unprecedented dissection of circuit function and therapeutic intervention. This article details the anatomical features of AAV that make it indispensable for neural gene delivery, providing application notes and protocols tailored for research and drug development professionals working in neuroscience.
Anatomical Deconstruction of the AAV Vector
The AAV Genome: ITRs and Transgene Cassette
The recombinant AAV (rAAV) genome is a masterwork of minimalistic design, wherein all viral coding sequences are replaced by the therapeutic or experimental transgene expression cassette, flanked by the essential Inverted Terminal Repeat (ITR) sequences [3] [1]. These 145-base-pair ITRs are the only viral cis-elements retained in rAAV vectors and serve as critical functional components [4]. They function as origins of replication, primers for second-strand synthesis, and signals for genome packaging into the capsid [1] [4]. The ITRs form highly stable, GC-rich hairpin structures that are notoriously challenging for standard molecular biology workflows, as they are prone to recombination and mutation during plasmid propagation in bacteria, necessitating specialized sequencing and cloning strategies for validation [4].
The transgene cassette, housed between the ITRs, typically consists of a promoter, the cDNA of interest, and a polyadenylation signal [1]. For neural applications, promoter selection is paramount for targeting specific cell types. Constitutive promoters like CAG (a hybrid of CMV early enhancer and chicken β-actin) provide strong, ubiquitous expression, while cell-type-specific promoters (e.g., Synapsin for neurons, GFAP for astrocytes, CaMKIIa for excitatory neurons) enable precise targeting within heterogeneous brain tissues [1]. The total size of the expression cassette must not exceed ~4.5–4.7 kb, a constraint that requires careful optimization of all regulatory elements [5].
The AAV Capsid: Serotypes and Tropism
The AAV capsid, an icosahedral shell assembled from 60 copies of VP1, VP2, and VP3 proteins in an approximate 1:1:10 ratio, is the primary interface with the host organism and the main determinant of tissue tropism and immunogenicity [3] [1]. The variable regions on the capsid surface mediate interactions with cell-surface receptors, dictating the vector's binding, internalization, and transduction efficiency in different tissues [6] [2].
Diverse naturally occurring AAV serotypes exhibit distinct neural tropisms, enabling researchers to select a vector optimized for their experimental needs. AAV9 and AAVrh.10 are particularly notable for their ability to cross the blood-brain barrier (BBB) following systemic administration, enabling non-invasive brain transduction [6] [2]. AAV2 is a well-characterized serotype with a broad tropism but is often used with other serotypes through "pseudotyping" (packaging an AAV2 genome into a different serotype's capsid) to combine the robust ITR function of AAV2 with the enhanced neural transduction of other capsids [1]. AAV5 exhibits high transduction efficiency for neurons in specific brain regions, such as the cortex and striatum, due to its use of sialic acid as a primary receptor [6] [1].
Table 1: AAV Serotypes and Their Neural Applications
| Serotype | Primary Receptors | Neural Tropism & Key Characteristics | Example Neural Applications |
|---|---|---|---|
| AAV1 | Sialic acid [6] | High transduction in muscle and CNS [2] | Intraparenchymal delivery to specific brain regions |
| AAV2 | HSPG [6] | Broad CNS tropism; well-characterized [1] [2] | Preclinical models of Parkinson's disease [6] |
| AAV5 | Sialic acid, PDGFR [6] | Efficient transduction of cortical and striatal neurons [1] | Neural circuit mapping in cortex and striatum |
| AAV8 | Laminin Receptor [6] | Strong liver and muscle tropism; moderate CNS [6] [2] | Comparative studies with other serotypes |
| AAV9 | Terminal N-linked galactose [6] | Robust BBB penetration; widespread CNS transduction after systemic delivery [6] [2] | Treatment of spinal muscular atrophy (SMA) with Zolgensma [2] |
| AAV-DJ | Hybrid | Engineered for high transduction in multiple cell types [2] | When a single, high-potency vector is needed for screening |
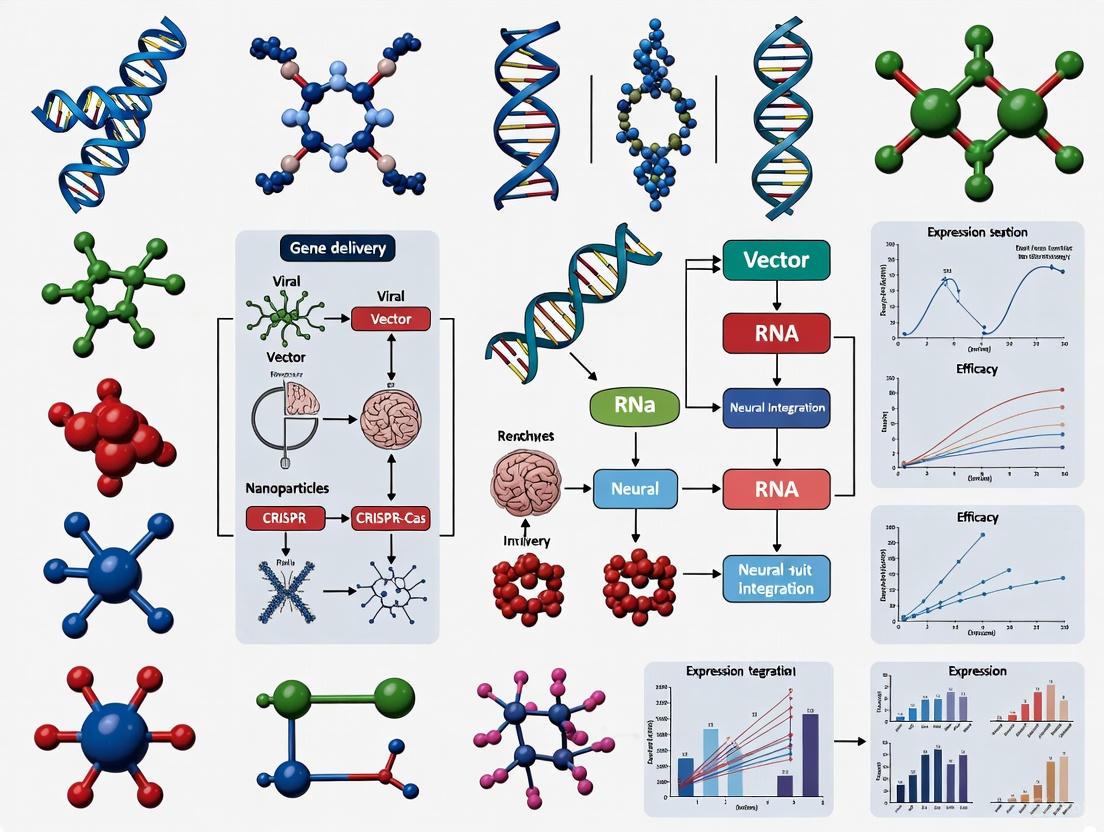
The following diagram illustrates the journey of an AAV vector from cellular entry to transgene expression, a critical process for neuroscientists to understand for optimizing experimental outcomes.
Advanced AAV Engineering for Neuroscience
Overcoming the Packaging Limit: Dual AAV Strategies
The strict ~4.7 kb packaging constraint is a significant limitation for neuroscientists aiming to deliver large transgenes, such as those encoding certain Cas proteins for CRISPR editing, optogenetic tools with complex regulatory elements, or large genomic regulatory sequences. Dual AAV vector systems have been developed to circumvent this limitation, effectively doubling the deliverable payload to ~8-9 kb [5]. These systems rely on co-transduction of the same cell by two separate AAV vectors, each carrying a portion of the full transgene, which is then reconstituted inside the nucleus.
The three primary dual AAV strategies, differentiated by their reconstitution mechanism, are summarized below.
Table 2: Comparison of Dual AAV Vector Strategies
| Strategy | Reconstitution Level | Mechanism | Advantages & Limitations |
|---|---|---|---|
| Hybrid/Overlapping | DNA | Homologous recombination between overlapping regions in the two vector genomes [5] | Higher efficiency in some studies; requires careful design of homologous region [5] |
| Trans-Splicing (REVeRT) | RNA | Splice donor/splice acceptor sites facilitate ligation of two pre-mRNAs into a single mature mRNA [5] | Avoids potential issues with DNA-level recombination; efficiency depends on splicing machinery |
| Split Intein | Protein | Fusion of two protein fragments mediated by autocatalytic intein sequences [5] | Reconstitution at protein level; suitable for specific large proteins; intein activity is context-dependent |
The choice of strategy depends on the experimental goal and the nature of the transgene. For extensive genomic elements, the hybrid or trans-splicing approaches are typically used, while the split intein approach is ideal for large proteins where the split site is known and does not disrupt function.
Capsid Engineering and Promoter Selection for Specificity
Beyond leveraging natural serotypes, the field is rapidly advancing through rational capsid engineering and directed evolution to create vectors with enhanced properties for neuroscience [3]. These next-generation capsids aim to achieve:
- Enhanced CNS specificity and reduced off-target transduction.
- Higher transduction efficiency for specific neuronal subtypes (e.g., dopaminergic, GABAergic).
- Evasion of pre-existing neutralizing antibodies to broaden patient eligibility in clinical trials [7].
- Retrograde transport from projection terminals to cell bodies, enabling access to neurons based on their connectivity.
Parallel to capsid engineering, the selection of cell-specific promoters is a critical and complementary strategy for restricting transgene expression. The use of promoters such as hSyn (human synapsin) for pan-neuronal expression or CaMKIIa for excitatory neurons provides an additional layer of precision, ensuring that the delivered genetic payload is active only in the intended cellular population [1].
Essential Protocols for AAV Application in Neural Research
Protocol: Design and Production of a Dual AAV System
This protocol outlines the key steps for implementing the overlapping dual AAV strategy, which is often the most efficient for delivering large genes to the nervous system [5].
I. Design and Cloning (Duration: 4-6 weeks)
- Identify Split Site: Choose a suitable location within the large transgene to split it into two fragments (5' and 3'). The split site should be in a region tolerant to the addition of a short peptide sequence or intron, if needed.
- Design Vector Components:
- Vector A (5' half): Contains the ITR, a promoter, the 5' fragment of the transgene, and a homologous overlapping region or splice donor site.
- Vector B (3' half): Contains the ITR, a homologous overlapping region or splice acceptor site, the 3' fragment of the transgene, and a polyA signal.
- The homologous overlapping region is typically an artificial, highly recombinogenic sequence of 200-500 bp.
- Molecular Cloning: Clone the designed fragments into AAV transfer plasmids. Use bacterial strains optimized for ITR stability (e.g., Stbl2, SURE, or proprietary strains) and validate all plasmid preps with specialized ITR-sequencing to prevent mutations in these critical regions [4].
II. AAV Production and Purification (Duration: 2-3 weeks)
- Co-transfection: Co-transfect HEK293 cells with the dual AAV transfer plasmids (Vector A and Vector B), a Rep/Cap plasmid (e.g., for AAV9), and an adenoviral helper plasmid using polyethylenimine (PEI) or PEI MAX in suspension culture [3] [2].
- Harvest and Lysis: Harvest cells 48-72 hours post-transfection. Lyse cells via freeze-thaw cycles and/or detergent treatment to release viral particles.
- Purification: Purify the crude lysate using iodixanol gradient centrifugation or affinity chromatography to isolate filled capsids from empty ones and cellular debris [3].
- Quality Control (QC): Determine the genome titer (vg/mL) of each batch by qPCR. Analyze the integrity and purity of the packaged genome using next-generation sequencing (NGS) to detect potential rearrangements or contaminants [4]. Assess the full/empty capsid ratio by ELISA or analytical ultracentrifugation.
III. In Vitro Evaluation (Duration: 3-4 weeks)
- Co-transduction: Transduce relevant neural cell models (e.g., primary neurons, iPSC-derived neurons, neurospheres) with a 1:1 mixture of Vector A and Vector B. Include controls transduced with each vector alone.
- Assess Reconstitution: After 7-14 days, assess functional reconstitution:
- Microscopy: If the transgene is a fluorescent protein, directly visualize reconstituted fluorescence.
- Western Blot: Detect the full-length, reconstituted protein.
- Functional Assay: Measure the activity of the reconstituted protein (e.g., electrophysiology for ion channels, CRISPR editing efficiency for Cas9).
Protocol: Intraparenchymal Delivery of AAV in Mouse Brain
This is a standard surgical protocol for precise, localized AAV delivery, a common requirement for neural circuit manipulation.
I. Pre-Surgical Preparation (Duration: 1-2 hours)
- Vector Preparation: Thaw the AAV stock on ice and dilute to the desired working titer (e.g., 1x10^12 – 1x10^13 vg/mL) in sterile PBS. Centrifuge briefly before loading to remove aggregates. Keep on ice and protected from light.
- Animal Anesthesia: Induce anesthesia in an adult mouse (e.g., C57BL/6) using 4-5% isoflurane in an induction chamber. Maintain anesthesia at 1-2% isoflurane via a nose cone on the stereotaxic frame.
- Stereotaxic Setup: Secure the mouse in the stereotaxic instrument. Apply ophthalmic ointment to prevent corneal drying. Shave the scalp and disinfect the surgical site with alternating scrubs of betadine and 70% ethanol.
II. Surgical Procedure (Duration: 30-60 minutes per animal)
- Incision: Make a midline incision (~1.5 cm) in the scalp to expose the skull.
- Bregma Identification: Identify Bregma and Lambda landmarks. Level the skull to ensure Bregma and Lambda are in the same dorsal-ventral plane.
- Coordinate Calculation: Calculate the target coordinates relative to Bregma for your brain region of interest (e.g., Primary Motor Cortex M1: AP +1.8 mm, ML ±1.5 mm; Dorsal Striatum: AP +0.5 mm, ML ±1.8 mm, DV -2.8 mm).
- Craniotomy: Drill a small burr hole at the calculated anterior-posterior (AP) and medial-lateral (ML) coordinates.
- Viral Injection:
- Load a calibrated glass micropipette or a 33-gauge Hamilton syringe with the AAV solution.
- Lower the needle slowly to the target dorsal-ventral (DV) coordinate.
- Infuse the virus at a slow, controlled rate (e.g., 50-100 nL/minute) using a microinjection pump. A typical injection volume is 500 nL - 1 µL.
- Wait 5-10 minutes after infusion to allow for pressure dissipation before slowly retracting the needle.
III. Post-Surgical Care and Analysis
- Closure: Suture or glue the scalp incision. Administer analgesic (e.g., Carprofen) and place the animal in a clean, warm cage until fully recovered from anesthesia.
- Expression Time: Allow sufficient time for transgene expression. Robust protein expression typically peaks 2-4 weeks post-injection for most AAV serotypes and neural transgenes.
- Validation: Sacrifice the animal and analyze the brain for transgene expression and function using histology, microscopy, electrophysiology, or behavioral assays.
The workflow for this protocol, from design to analysis, is outlined below.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagent Solutions for AAV Neuroscience
| Reagent/Material | Function & Application | Key Considerations |
|---|---|---|
| AAV Transfer Plasmid | Backbone for transgene cassette cloning; contains ITRs [1] [4] | Use plasmids with validated, intact ITRs [4]. Select a backbone with appropriate promoter (e.g., CAG, hSyn, CaMKIIa). |
| Rep/Cap Plasmid | Provides AAV replication (Rep) and capsid (Cap) proteins in trans during production [3] [2] | Defines the serotype (e.g., AAV9, AAV5, AAV-DJ). Pseudotyping (e.g., AAV2/9) is common. |
| Adenoviral Helper Plasmid | Provides essential helper functions from adenovirus (E4, E2a, VA) for AAV replication [3] [2] | Necessary for AAV life cycle in production cells. |
| HEK293 Cells | Production cell line; provides adenovirus E1 gene [2] | Can be used in adherent or suspension culture for scale-up. |
| PEI MAX | Transfection reagent for delivering plasmids to HEK293 cells [3] | Cost-effective and scalable compared to commercial lipid-based reagents. |
| Iodixanol | Density gradient medium for purifying AAV particles post-lysis [3] | Effectively separates full capsids from empty ones and contaminants. |
| DNase I | Enzyme used during qPCR titering to degrade unencapsidated DNA, ensuring accurate genome titer (vg/mL) [3] | Critical for quality control and determining accurate dosing. |
| Stereotaxic Instrument | Precision apparatus for targeting specific brain regions in vivo [citation:Protocol 4.2] | Must be calibrated regularly. Includes micromanipulators and injectors. |
| Glass Micropipettes / Hamilton Syringe | For delivering small volumes of AAV suspension directly into brain parenchyma [citation:Protocol 4.2] | Provides precise control over injection volume and location. |
AAV vectors represent a sophisticated and continually evolving platform for delivering genetic cargo to the nervous system. Their anatomy—from the compact ITR-flanked genome to the versatile and engineerable capsid—is perfectly suited for the demands of modern neuroscience research and therapeutic development. By understanding the principles of AAV biology, including serotype selection, capsid engineering, and strategies to overcome payload limitations, researchers can harness this powerful tool with greater precision and efficacy. The protocols and resources provided here serve as a foundation for the successful design, production, and application of AAV vectors to manipulate neural circuits, model disease, and pioneer the next generation of gene therapies for neurological disorders.
The era of genomic medicine has firmly arrived, with viral vectors standing as indispensable tools for both basic neuroscience research and the development of therapeutic interventions for neurological disorders. While adeno-associated virus (AAV) vectors have emerged as a predominant choice for in vivo neuronal transduction due to their safety profile and neuronal tropism, a comprehensive gene delivery strategy for neural circuit manipulation requires a broader arsenal [8]. AAV's limitations, particularly its constrained packaging capacity of approximately 4.7 kb, can be prohibitive for delivering larger genetic payloads or complex transcriptional regulatory elements [8] [9]. Furthermore, its predominantly episomal persistence may not support long-term transgene expression in scenarios requiring stable genomic integration, such as in tracking cell lineages or permanent genetic modifications.
This application note moves beyond AAV to provide a detailed comparison of three critical viral vector systems—Lentivirus (LV), Retrovirus (RV), and Adenovirus (AdV)—for neuroscience applications. We focus on their unique biological characteristics, which present distinct solutions to the challenges of gene therapy and neural circuit analysis [10]. Key differentiators include their genome integration capabilities, transgene expression duration, payload capacity, and cellular tropism within the complex environment of the central nervous system (CNS) [11]. By framing these vectors within the context of gene delivery strategies for neural circuit manipulation, we aim to equip researchers with the knowledge to select the optimal vector for specific experimental or therapeutic goals, from manipulating specific neuronal populations to achieving long-term genetic modification in the brain and spinal cord.
Comparative Analysis of Viral Vector Systems
Selecting the appropriate viral vector is a critical first step in designing robust and interpretable neuroscience experiments. The table below provides a systematic, quantitative comparison of the key features of Lentivirus, Retrovirus, and Adenovirus vectors, contrasting them with the familiar benchmark of AAV.
Table 1: Comparative Analysis of Viral Vectors for Neuroscience Applications
| Feature | Lentivirus (LV) | Retrovirus (RV) | Adenovirus (AdV) | Adeno-associated Virus (AAV) |
|---|---|---|---|---|
| Genome Type | Single-stranded RNA | Single-stranded RNA | Double-stranded DNA | Single-stranded DNA |
| Packaging Capacity | ~8 kb [9] | ~8 kb [9] | Up to ~35 kb [11] [9] | ~4.7 kb [8] [9] |
| Integration Profile | Integrates into host genome (prefers active genes) [8] | Integrates into host genome (requires cell division) [11] | Non-integrating (episomal) [9] | Predominantly non-integrating (episomal) [10] [11] |
| Expression Duration | Long-term (stable integration) [12] | Long-term (stable integration) | Short- to medium-term (transient, weeks) [9] | Long-term (episomal, can persist for years) [9] |
| Tropism in CNS | Broad (neurons, glia); can be pseudotyped (e.g., VSV-G) [8] [11] | Dividing cells (e.g., progenitors, glioma cells) [11] | Broad (neurons, astrocytes, oligodendroglia, ependymal cells, microglia) [11] | Varies by serotype; neurons preferred for AAV2/5/9 [11] [13] |
| Typical Titer (functional) | ~10^8 - 10^9 IU/mL | ~10^7 - 10^8 IU/mL | ~10^10 - 10^12 VP/mL [9] | ~10^11 - 10^13 VG/mL |
| Immunogenicity | Low to Moderate | Low to Moderate | High (adjuvant properties) [11] | Very Low [8] [14] |
| Key Neuroscience Applications | Stable gene expression in neurons, ex vivo cell engineering, delivery of large or multiple transgenes [8] | Lineage tracing, targeting neural progenitors and brain tumors [11] | High-level transient expression, delivery of very large genetic payloads (e.g., CRISPR-Cas9 systems), cancer gene therapy [15] | Long-term gene expression in post-mitotic neurons, gene therapy for monogenic disorders, optogenetics/chemogenetics [8] [13] |
This comparative analysis reveals clear strategic trade-offs. Lentiviral vectors are distinguished by their ability to mediate stable genomic integration in non-dividing cells, a critical feature for long-term manipulation of mature neuronal circuits [8]. In contrast, Retroviral vectors remain the tool of choice for studies focused on dividing cell populations, such as neural stem cells or gliomas, due to their dependence on cell division for integration [11]. Adenoviral vectors excel where high levels of transient transgene expression are needed or for delivering exceptionally large genetic payloads, such as the ~10 kb CRISPR-Cas9 nuclease, though their pronounced immunogenicity must be carefully considered [11] [15].
Decision Workflow and Experimental Protocols
Vector Selection and Experimental Workflow
The following diagram outlines a systematic decision-making workflow for selecting the most appropriate viral vector based on key experimental parameters. This logical pathway helps researchers align their goals with the inherent strengths of each vector system.
Detailed Protocol: Lentiviral Transduction of Spinal Cord Neurons for Stable Gene Expression
This protocol details the methodology for direct in vivo lentiviral vector delivery to the spinal cord, a common paradigm for manipulating motor and sensory circuits, based on established procedures in rodent models [12].
Title: Lentiviral-Mediated Gene Delivery to Rat Spinal Cord
Objective: To achieve stable, long-term transgene expression in spinal cord neurons via direct parenchymal injection of lentiviral vectors.
Materials & Reagents:
- Viral Vector: Third-generation, self-inactivating (SIN) lentiviral vector, pseudo-typed with VSV-G envelope, titer ≥ 1x10^8 IU/mL [8] [14].
- Animals: Adult Sprague-Dawley rats (200-300 g).
- Anesthesia: Isoflurane vaporizer system (5% for induction, 1.5-2.5% for maintenance in O2).
- Surgical Equipment: Stereotaxic apparatus, fine-glass micropipette (30-50 μm tip) or Hamilton syringe, microinjection pump.
- Analgesia: Carprofen (4 mg/kg, s.c.) [16].
Procedure:
- Anesthesia and Prepping: Induce and maintain anesthesia with isoflurane. Secure the rat in a stereotaxic frame. Maintain body temperature at 37°C using a homeothermic blanket. Administer carprofen pre-emptively for analgesia.
- Surgical Exposure: Perform a dorsal midline incision over the vertebral column. Conduct a hemilaminectomy at the target vertebral level (e.g., L4/L5 for lumbar enlargement) to expose the spinal cord without durotomy.
- Vector Injection: Load the lentiviral preparation into the injection system. Position the glass pipette approximately 100 μm lateral to the central vein and insert it 150 μm into the spinal cord parenchyma [16]. Inject a total volume of 500 nL per site at a slow, controlled rate of 50 nL/min to minimize tissue damage and reflux [16]. Multiple injections along the rostro-caudal axis can be performed to cover a larger area.
- Post-injection Care: Wait 5-10 minutes before slowly retracting the pipette to allow for pressure equilibration. Suture the muscle and skin layers. Administer post-operative carprofen for 48-72 hours and monitor the animal until full recovery.
Validation & Analysis:
- Time Course: Transgene expression is typically assessed 2-4 weeks post-injection to allow for stable integration and protein expression [12].
- Histology: Perfuse animals transcardially with 4% paraformaldehyde (PFA). Process spinal cord tissue for cryosectioning and immunohistochemistry using antibodies against the transgene product (e.g., EGFP) and neuronal markers (e.g., NeuN) to confirm neuronal transduction and quantify efficiency.
The Scientist's Toolkit: Essential Research Reagents
Successful execution of viral vector-based experiments relies on a suite of specialized reagents and tools. The following table catalogues key solutions for working with lentiviral, retroviral, and adenoviral vectors.
Table 2: Essential Research Reagent Solutions for Viral Vector Neuroscience
| Reagent / Solution | Function & Application | Example Use-Case |
|---|---|---|
| VSV-G Pseudotyped LV Particles | Expands tropism to a broad range of dividing and non-dividing cells, including neurons, by utilizing the Vesicular Stomatitis Virus Glycoprotein (VSV-G) envelope [8]. | Enables efficient transduction of primary neuronal cultures or CNS neurons in vivo for stable gene expression [8] [11]. |
| Third-Generation, SIN Lentiviral Packaging Systems | Enhances biosafety by splitting viral genes across multiple plasmids and deleting the viral promoter/enhancer to prevent replication-competent virus generation and reduce genotoxicity [14]. | Standard for clinical-grade ex vivo cell engineering (e.g., CAR-T cells) and preclinical research requiring high safety standards [8]. |
| Polybrene (Hexadimethrine Bromide) | A cationic polymer that reduces electrostatic repulsion between viral particles and the cell membrane, thereby increasing transduction efficiency in vitro. | Added to cell culture media (at 4-8 μg/mL) during viral infection to enhance retroviral or lentiviral transduction of primary glial cells or neural stem cell lines. |
| CellSTACK / HYPERStack Culture Chambers | Scale-up platforms for adherent cell culture, providing high surface area in a small footprint for large-scale viral vector production under controlled, scalable conditions [14]. | Used in upstream bioprocessing to grow the producer cells (e.g., HEK293T) needed for high-yield lentivirus or adenovirus manufacturing. |
| AI-Based Enhancer Prediction Tools | Computational tools that identify short, cell-type-specific genomic "enhancer" sequences to drive selective transgene expression, overcoming the limited packaging capacity of viral vectors [13]. | Designing compact, cell-type-specific AAV or LV expression cassettes (e.g., for targeting spinal inhibitory interneurons) without the need for large genomic promoters [16] [13]. |
The strategic selection of viral vectors is fundamental to advancing neuroscience research and therapeutic development. While AAV remains a powerful tool for many in vivo applications, a sophisticated understanding of lentiviral, retroviral, and adenoviral vector systems dramatically expands the experimental toolbox. Lentiviral vectors are unparalleled for achieving stable genetic manipulation in post-mitotic neurons, retroviral vectors provide exclusive access to dividing cellular compartments, and adenoviral vectors offer a solution for delivering very large or highly immunogenic transgenes on a transient basis.
Future developments in viral vectorology will continue to enhance the precision and safety of neural circuit manipulation. Emerging trends include the engineering of novel synthetic capsids and envelopes to refine cellular tropism, the development of integration-deficient lentiviral vectors for safer transient expression, and the increasing use of computational biology and AI to design compact, highly specific genetic regulatory elements [13]. The ongoing NIH BRAIN Initiative's "Armamentarium for Precision Brain Cell Access" project exemplifies this direction, generating a versatile set of validated gene delivery systems for targeting specific neural cell types with exceptional accuracy [13]. By leveraging the distinct advantages of each viral vector system and integrating these next-generation technologies, researchers are poised to deconstruct the complexities of neural circuits with unprecedented precision, paving the way for transformative therapies for a broad spectrum of neurological and neuropsychiatric disorders.
Recombinant adeno-associated viruses (rAAVs) have emerged as a preeminent tool for delineating the intricate connectivity of neural circuits in the mammalian brain. Their prominence in neuroscience research stems from an ideal safety profile (Biosafety Level-1), low immunogenicity, capacity for high-titer production (10¹¹–10¹⁴ viral genomes/mL), and ability to achieve stable, long-term transgene expression in the nervous system [17]. The fundamental principle underlying their application in circuit mapping is axonal transport—the natural capacity of viruses to be trafficked within neurons, either from the soma toward axon terminals (anterograde) or from axon terminals back to the soma (retrograde) [18] [17]. This application note details the mechanisms, serotype selection, and methodological protocols for employing AAVs in anterograde and retrograde neuronal tracing, framed within the broader context of gene delivery strategies for neural circuit manipulation.
Fundamental Transport Mechanisms and AAV Serotypes
Cellular Mechanisms of Axonal Transport
AAV trafficking within neurons is an active process mediated by cellular motor proteins and specific endosomal compartments. Research on AAV9, which provides insights into the general mechanisms, has demonstrated that after cellular entry, the virus is trafficked into various vesicular compartments [19] [20]. Crucially, Rab7-positive late endosomes or lysosomes containing AAV exhibit high motility [19]. The retrograde transport of these compartments (toward the cell body) is driven primarily by the motor protein cytoplasmic dynein, and this process is dependent on Rab7 function [19] [20]. Conversely, anterograde transport (away from the cell body toward synaptic terminals) is driven by kinesin-2 [19] [20]. This understanding of the underlying cellular machinery is essential for designing effective tracing strategies and interpreting experimental results.
Key AAV Serotypes and Their Transport Properties
The propensity for anterograde or retrograde transport is heavily influenced by the AAV capsid serotype, which determines the virus's tropism and interaction with host cell receptors.
Table 1: Key AAV Serotypes for Neuronal Tracing
| Serotype | Primary Transport Direction | Key Characteristics | Common Applications |
|---|---|---|---|
| AAV1 | Predominantly Anterograde | Can exhibit anterograde transsynaptic transport at high titers (>10¹³ GC/ml); also shows some retrograde transport [21] [17]. | Mapping output pathways; transsynaptic labeling of postsynaptic neurons [22]. |
| AAV2 | Anterograde (Non-transsynaptic) | Wide neuronal tropism; binds heparan sulfate proteoglycan (HSPG); traditionally used for local transduction [17] [23]. | Local gene delivery to neurons within an injection site. |
| AAV9 | Bidirectional | Efficient axonal transport driven by dynein (retrograde) and kinesin-2 (anterograde) [19] [20]. | Widespread transduction in the CNS; global gene delivery. |
| AAV-retro | Efficient Retrograde | Engineered variant for high-efficiency retrograde access to projection neurons [18] [17]. | Mapping input networks; targeting neurons based on their projection targets. |
Protocols for Anterograde and Retrograde Tracing
Protocol 1: Anterograde Transsynaptic Tracing with AAV1
This protocol describes the use of high-titer AAV1 for mapping monosynaptic outputs from a defined brain region, enabling the genetic manipulation of postsynaptic neurons.
1. Viral Vector Preparation:
- Use a self-complementary AAV1 (scAAV1) vector to bypass the rate-limiting step of second-strand DNA synthesis, leading to stronger and faster transgene expression [17] [22].
- Employ a strong ubiquitous promoter, such as CAG or CBA, to drive high-level expression of the transgene, which is critical for detectable transsynaptic transfer [23] [22].
- The viral titer is critical. Ensure a high titer ≥ 1.0 × 10¹³ genome copies (GC)/mL for efficient transneuronal spread [21] [22]. Reducing the titer to 10¹¹ GC/mL can eliminate this property [17].
2. Stereotaxic Intracranial Injection:
- Anesthetize the animal (e.g., mouse) and secure it in a stereotaxic frame. Maintain anesthesia with 1.5-2% isoflurane [21].
- After exposing the skull, use calibrated coordinates to drill a small hole above the target brain region (e.g., prefrontal cortex, medial geniculate nucleus).
- Load the viral preparation into a glass micropipette with a beveled tip (inner diameter ~20 µm).
- Inject the virus via pressure injection at a slow, controlled rate (e.g., 15-30 nL/min) [21]. The total injection volume is typically 40-100 nL for mice.
- Leave the pipette in place for 5-10 minutes post-injection to minimize backflow along the injection tract [21].
3. Post-Injection and Analysis:
- Allow adequate time for viral transport and gene expression. Transsynaptic labeling can be observed within 3-6 weeks post-injection [22].
- Perfuse and fix the brain for histological processing. Analyze the injection site and putative downstream target regions for the presence of the transgene (e.g., GFP) using microscopy.
- Specificity can be confirmed by the known anatomy of the pathway (e.g., robust labeling in the contralateral, but not ipsilateral, superior colliculus after retinal injection) [22].
Protocol 2: Retrograde Tracing with AAV-retro
This protocol utilizes the engineered AAV-retro serotype for efficient retrograde access to neurons that project to the injection site.
1. Viral Vector Preparation:
- Use an AAV-retro vector packaged with a transgene of interest (e.g., Cre recombinase, fluorescent protein) [18] [17].
- While AAV-retro is highly efficient, note that not all neuronal pathways are transduced equally; some, such as certain brainstem and catecholamine pathways, may show poor transduction [18].
2. Stereotaxic Intracranial Injection:
- Follow the same stereotaxic surgery and injection procedures as in Protocol 1.
- Inject the AAV-retro vector into the target region where axon terminals of interest are located (e.g., striatum).
3. Post-Injection and Analysis:
- Allow 2-4 weeks for retrograde transport and sufficient transgene expression in the cell bodies of projecting neurons [18].
- Identify retrogradely labeled neurons in upstream brain regions that are known to project to the injection site.
- For functional manipulation, AAV-retro can deliver optogenetic tools (e.g., Channelrhodopsin), chemogenetic tools (e.g., DREADDs), or recombinases for intersectional strategies [18] [17].
Table 2: Comparison of Key Tracing Methodologies
| Parameter | Anterograde Tracing (AAV1) | Retrograde Tracing (AAV-retro) |
|---|---|---|
| Direction of Spread | Presynaptic → Postsynaptic | Postsynaptic → Presynaptic |
| Primary Application | Mapping output networks | Mapping input networks |
| Key Experimental Consideration | Requires very high titer for transsynaptic spread | Pathway-dependent transduction efficiency |
| Toxicity & Expression | Low cytotoxicity; long-term expression | Low cytotoxicity; long-term expression |
| Complexity | Can be achieved with a single vector in wild-type animals [22] | Can be combined with Cre-dependent systems for cell-type specificity |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of AAV tracing experiments requires a suite of reliable reagents and tools.
Table 3: Essential Research Reagents for AAV Tracing
| Reagent / Tool | Function / Description | Example Use Case |
|---|---|---|
| scAAV1 Vector | Self-complementary AAV1 for efficient anterograde transsynaptic tracing [22]. | Delivering fluorescent proteins or functional effectors to postsynaptic cells. |
| AAV-retro Vector | Engineered capsid for highly efficient retrograde tracing [18]. | Labeling or manipulating neurons based on their projection targets. |
| Cre/loxP System | Enables cell-type-specific transgene expression. | Injecting AAV1-Cre into a region; Cre-dependent reporter vector or AAV-DIO effector in a Cre-driver mouse line [18]. |
| Fluorescent Reporters | (e.g., GFP, tdTomato). Visualize infected neurons and their processes. | Determining injection site spread and locating transduced cells in target regions. |
| Digital PCR (ddPCR) | Method for absolute quantification of viral genome titer without a standard curve; more robust than qPCR for in-process samples [24]. | Accurately determining the viral titer, a critical parameter for transsynaptic tracing. |
| Transmission Electron Microscopy (TEM) | Visualizes AAV capsid integrity, aggregation, and sample impurities [24]. | Quality control of viral vector preparations. |
Workflow and Pathway Visualization
The following diagram illustrates the logical workflow for designing and executing an AAV-based circuit tracing experiment, integrating the key decision points and methodologies discussed.
Figure 1: Experimental Workflow for AAV-Based Circuit Tracing. This flowchart outlines the key steps and strategic decisions involved in designing an experiment to map neural connections using anterograde (red) or retrograde (blue) AAV vectors.
The molecular mechanism of AAV trafficking within the neuron is summarized in the following pathway diagram.
Figure 2: Intracellular Trafficking Pathway of AAV. This diagram visualizes the dual transport mechanisms of AAV within a neuron after endocytosis. The virus in Rab7-positive late endosomes is transported retrogradely by dynein towards the soma or anterogradely by kinesin-2 towards the axon terminal [19] [20].
AAV-based viral vectors provide a powerful and versatile toolkit for dissecting the complex wiring of the brain. Understanding the distinct axonal transport mechanisms—anterograde and retrograde—enables researchers to select the appropriate serotype (e.g., AAV1 or AAV-retro) and design rigorous protocols for mapping neural inputs and outputs. The continued development of engineered capsids with enhanced tropism and the refinement of intersectional genetic strategies promise to further accelerate the precise functional dissection of neural circuits, advancing both fundamental neuroscience and the development of gene therapies for neurological disorders.
The Armamentarium for Precision Brain Cell Access is a transformative project under the NIH BRAIN Initiative, established to develop and disseminate a comprehensive collection of molecular genetic reagents [25]. Its primary goal is to enable neuroscientists to target specific brain cell types with high precision, facilitating the study of neural circuits in both laboratory animals and human tissue specimens [25]. This initiative aims to bring the precision of molecular targeting to specific neural circuits that underlie behavior and network function, potentially revolutionizing our understanding of the brain and informing new approaches for treating neurological disorders [25].
A key driver for the Armamentarium is the need to extend precision targeting to less genetically tractable organisms, such as non-human primates, which are critical for understanding the human brain [25]. While genetically engineered animals like transgenic mice have enabled considerable progress, the Armamentarium focuses on developing non-transgenic tools (e.g., engineered viral vectors) for species where traditional genetic models are not feasible [25]. The project encompasses multiple funded efforts, including the development of molecular genetic access reagents, optimization of functional probes for delivery, widespread dissemination of reagents to the neuroscience community, and building research infrastructure [25].
Viral vectors are the cornerstone of modern neural circuit manipulation, providing the means to deliver genetic instructions for sensors and actuators to specific cell types. The table below summarizes the key viral vectors used in neuroscience research, highlighting their characteristics and primary applications in neural circuit mapping and manipulation [17].
Table 1: Viral Vectors for Neural Circuit Mapping and Manipulation
| Virus Type | Genome Size | Vector Capacity | Cytotoxicity | Transport Characteristics | Primary Applications |
|---|---|---|---|---|---|
| Adeno-associated Virus (AAV) | ~4.7 kb | ~4.7 kb | Low | Anterograde, non-transsynaptic; AAV1 at high titer can be anterograde trans-monosynaptic; AAV-retro enables efficient retrograde access [17]. | Gene delivery for optogenetics, chemogenetics, and sensors; circuit mapping [17]. |
| Rabies Virus (RV), glycoprotein G-deleted (RVdG) | ~12 kb | ~3.7 kb | High | Complete retrograde transport; efficient infection of axon terminals; EnvA-pseudotyped RVdG enables retrograde trans-monosynaptic tracing [17]. | Retrograde trans-monosynaptic tracing to map direct inputs to starter cells [17]. |
| Herpes Simplex Virus Type 1 (HSV1) H129 | ~150 kb | ~50 kb | High | Anterograde trans-multisynaptic trafficking [17]. | Anterograde polysynaptic circuit mapping of output networks [17]. |
| Canine Adenovirus (CAV-2) | ~31 kb | ~30 kb | Moderate | Preferentially transduces neuronal axon terminals with efficient retrograde transport [17]. | Retrograde access to neurons projecting to an injection site [17]. |
The selection of an appropriate viral vector depends on the experimental goal, such as the direction of tracing (anterograde vs. retrograde), the desired synaptic specificity (monosynaptic vs. polysynaptic), and the payload size required.
Table 2: Comparison of Viral Strategies for Circuit Mapping
| Strategy | Tracing Direction | Synaptic Specificity | Key Viral Tools | Ideal Use Cases |
|---|---|---|---|---|
| Anterograde Tracing | Forward (maps outputs) | Non-synaptic, monosynaptic, or polysynaptic | AAV (non-synaptic), AAV1 high-titer (monosynaptic), HSV1-H129 (polysynaptic) [17] | Mapping the projections and synaptic outputs of a specific neuronal population. |
| Retrograde Tracing | Backward (maps inputs) | Non-synaptic, monosynaptic, or polysynaptic | CAV-2, AAV-retro (non-synaptic), EnvA+RVdG (monosynaptic), PRV (polysynaptic) [17] | Identifying the source of inputs to a defined population of "starter" cells. |
| Cell-Type Specific Targeting | N/A | N/A | AAVs with cell-specific promoters or Cre-dependent (DIO) systems [26] [17] | Manipulating or monitoring a genetically defined cell type without regard to its connections. |
| Projection-Specific Targeting | N/A | N/A | AAVs with retrograde functionality (e.g., CAV-Cre) combined with Cre-dependent AAVs [17] | Accessing neurons based on both their cell type and their long-range projection targets. |
Detailed Experimental Protocols
Protocol 1: Retrograde Monosynaptic Tracing with RVdG
This protocol details the use of glycoprotein-deleted Rabies Virus (RVdG) for mapping the direct, monosynaptic inputs to a genetically defined population of "starter" neurons [17].
1. Principle: The method involves a two-step, helper virus system. First, "starter cells" are genetically defined and made to express the missing rabies glycoprotein (RG) and a fluorescent marker (e.g., TVA receptor for EnvA-pseudotyping). In the second step, the RVdG vector, which lacks the gene for glycoprotein (G), is injected. This virus can only infect the starter cells (via TVA) and can only spread retrogradely to their direct presynaptic partners because those partners lack the glycoprotein required to package new, infectious viral particles [17].
2. Materials:
- Plasmid DNA: Plasmids encoding TVA (receptor for EnvA-pseudotyped virus) and Rabies Glycoprotein (RG).
- Helper Viral Vectors: AAV vectors for delivering TVA and RG genes, or a transgenic mouse line expressing TVA and RG in a Cre-dependent manner.
- Tracing Viral Vector: EnvA-pseudotyped, G-deleted Rabies Virus (RVdG) encoding a fluorescent reporter (e.g., mCherry).
- Stereotaxic surgery equipment, including microsyringe pump and fine-glass micropipettes.
3. Step-by-Step Procedure: 1. Stereotaxic Injection of Helper Components: Inject the AAV helper viruses (e.g., AAV-FLEX-TVA and AAV-FLEX-RG) into the target brain region of a Cre-driver mouse. Alternatively, use a transgenic mouse line that already expresses TVA and RG in a Cre-dependent manner. - Parameters: Use a microsyringe pump for controlled injection (e.g., 50-100 nL/min). Allow 2-4 weeks for adequate expression of the helper proteins. 2. Stereotaxic Injection of RVdG: Inject the EnvA-pseudotyped RVdG-mCherry into the same coordinates. - Parameters: The virus titer should be > 1x10^8 infectious units/mL. Allow 5-7 days for retrograde trans-monosynaptic spread. 3. Perfusion and Tissue Processing: Transcardially perfuse the animal with 4% paraformaldehyde (PFA). Extract the brain and post-fix in 4% PFA for 24 hours, then section into 50-100 µm thick slices using a vibratome. 4. Imaging and Analysis: Image the brain sections using a slide scanner or confocal microscope. The starter cells (co-expressing the helper virus fluorophore and mCherry) and the direct presynaptic input neurons (expressing only mCherry) can be identified and quantified.
4. Critical Considerations:
- Specificity: The starter cell population must be precisely defined, as only these cells will initiate the trans-synaptic spread.
- Cytotoxicity: RVdG is cytotoxic; the analysis must be completed within 1-2 weeks post-injection to avoid degradation of the signal and loss of infected neurons [17].
- Controls: Always include controls without the helper viruses to confirm the absence of non-specific RVdG infection.
Protocol 2: Cell-Type Specific Neural Circuit Manipulation
This protocol combines Cre-recombinase driver lines with Cre-dependent AAVs to achieve cell-type specific expression of optogenetic actuators for functional circuit manipulation [26] [17].
1. Principle: A Cre-dependent (DIO or FLEX) AAV vector, which contains an inverted coding sequence for an opsin (e.g., Channelrhodopsin-2), is injected into a specific brain region of a transgenic mouse expressing Cre-recombinase under a cell-type specific promoter. Cre-mediated recombination flips the inverted sequence into the correct orientation, allowing opsin expression exclusively in the targeted cell population. An implanted optical fiber then allows light delivery to manipulate the activity of these neurons [26].
2. Materials:
- Animal Model: Transgenic Cre-driver mouse line.
- Viral Vector: Cre-dependent AAV (e.g., AAV5-EF1α-DIO-ChR2-eYFP).
- Optogenetics System: Laser or LED light source, optical fibers, ferrule, fiber-optic patch cord.
- Stereotaxic surgery equipment, including drill and microsyringe pump.
- Behavioral apparatus and electrophysiology setup for functional validation.
3. Step-by-Step Procedure: 1. Stereotaxic Viral Injection: Inject the Cre-dependent AAV into the target brain region of the anesthetized Cre-driver mouse. - Parameters: Use a titer of > 1x10^12 vg/mL. Inject 200-500 nL at a slow flow rate (50-100 nL/min). Leave the pipette in place for 5-10 minutes post-injection to prevent backflow. 2. Optical Cannula Implantation: Immediately following the viral injection, implant a chronic optical cannula above the injection site and secure it to the skull with dental cement. 3. Recovery and Expression: Allow the animal to recover for at least 3-4 weeks to ensure robust opsin expression. 4. Functional Validation: - Ex vivo: Conduct patch-clamp recordings in brain slices to confirm light-evoked spiking in ChR2-expressing neurons. - In vivo: Connect the implanted cannula to a patch cord and deliver light pulses (e.g., 5-20 ms pulses of 473 nm blue light) during behavioral tasks to assess the causal role of the manipulated circuit.
4. Critical Considerations:
- Opsin Selection: Choose an opsin with kinetics and light sensitivity appropriate for the experiment (e.g., ChR2 for millisecond-scale activation, stabilized step-function opsins for sustained activation) [26].
- Light Power: Titrate light power to achieve effective neural modulation without causing thermal damage.
- Off-Target Effects: Verify opsin expression and function histologically and physiologically post-experiment.
Visualization of Core Workflows and Signaling Pathways
Workflow for Monosynaptic Circuit Tracing
This diagram illustrates the core principle and workflow for retrograde monosynaptic tracing using the helper virus and RVdG system.
Logic of Cell-Type Specific Targeting
This diagram outlines the genetic strategy for achieving cell-type specific transgene expression using the Cre-loxP system and engineered AAVs.
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogs essential reagents and tools provided by the Armamentarium and associated BRAIN Initiative efforts for precision neuroscience.
Table 3: Essential Research Reagents for Precision Neural Circuit Analysis
| Reagent/Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Viral Vector Systems | AAV serotypes (e.g., AAV1, AAV5, AAV9), AAV-retro, DIO/FLEX AAVs, RVdG, CAV-2, HSV1-H129 [25] [17]. | Deliver genetic payloads (sensors, actuators, Cre recombinase) to specific cell types or circuits based on tropism and route of administration. |
| Cell Type Access Reagents | Cre-driver transgenic lines; AAVs with cell-specific promoters; transgenic mice expressing TVA and RG for rabies tracing [25] [17]. | Genetically define and gain experimental access to specific neuronal or glial cell populations for manipulation or monitoring. |
| Genetically Encoded Actuators | Channelrhodopsins (ChR2), Halorhodopsins (NpHR), Chemogenetic Receptors (DREADDs) [26] [17]. | Precisely activate or inhibit targeted neuronal populations with light (optogenetics) or inert ligands (chemogenetics) to test causal roles in circuits and behavior. |
| Genetically Encoded Sensors | Calcium indicators (GCaMP), voltage-sensitive fluorescent proteins (VSFP), iGluSnFR [27]. | Monitor neural activity (calcium influx, membrane potential, neurotransmitter release) in specific cell types during behavior or processing. |
| Molecular Profiling Tools | Single-cell RNA sequencing, spatial transcriptomics, ATAC-seq, antibody panels from BICCN [28]. | Characterize and classify the molecular identity of brain cell types, enabling the definition of target populations for the Armamentarium. |
The BRAIN Initiative Armamentarium represents a paradigm shift in neuroscience methodology, moving the field from observation to causal dissection of neural circuits with cellular and synaptic precision. By providing a centralized, validated, and expanding toolkit of molecular reagents for cell-type-specific access, the Armamentarium empowers researchers to deconstruct the functional architecture of the brain systematically [25]. The integration of these tools with other BRAIN Initiative projects, such as the Brain Initiative Cell Census Network (BICAN) and the BRAIN CONNECTS program, creates a powerful synergistic framework for understanding the brain from molecules to circuits to behavior [25] [28].
Looking forward, the focus will be on refining these tools for enhanced specificity, lower immunogenicity, and greater utility in non-human primates and human-derived tissue models, thereby accelerating the translational path for treating brain disorders [25]. The continued development and dissemination of these precision delivery tools are fundamental to achieving the BRAIN Initiative's ultimate vision: a comprehensive, mechanistic understanding of mental function that paves the way for novel therapeutic interventions [29].
Precisely defining neural cell types is a fundamental prerequisite for modern neuroscience research aimed at understanding brain function and dysfunction. The incredible cellular heterogeneity of the brain means that even microscopically discrete regions contain multiple cell types with distinct functions, connectivity, and molecular signatures. Early lesion and electrical stimulation techniques, while groundbreaking, lacked the specificity to target these distinct cellular populations, often leading to confounding results from affecting multiple circuit elements simultaneously [30] [31]. The advent of genetic tools has revolutionized this landscape, enabling researchers to move beyond crude anatomical targeting to precise manipulation based on a neuron's genetic identity or its connectivity within a circuit [31].
This shift in methodology is particularly critical for gene delivery strategies in neural circuit research. The ability to deliver genes encoding functional actuators (e.g., for optogenetics or chemogenetics) or reporters (e.g., for activity monitoring or tracing) to specific cell types relies entirely on our capacity to define and target those populations using unique molecular markers [30] [17]. This protocol outlines the conceptual frameworks and practical methodologies for defining neural cell types and leveraging these definitions for targeted manipulation, providing a foundation for probing circuit function in health and disease.
Core Principles: Genetic and Connectivity-Based Targeting Strategies
Two complementary paradigms form the cornerstone of contemporary neural circuit dissection: targeting by genetic identity and targeting by spatial connectivity. Each approach offers distinct advantages and is suited to different experimental questions.
Genetic Identity
This approach exploits the unique gene expression profiles of neuronal subtypes to achieve specificity. Defined by transcription factors, neurotransmitter systems, calcium-binding proteins, or other molecular markers, this genetic identity often reflects a neuron's developmental history and functional role [31]. In practice, this is achieved by placing transgenes under the control of cell-type-specific promoter regions. For example, promoters for vesicular glutamate transporter 2 (Vglut2) target glutamatergic neurons, while promoters for calcium/calmodulin kinase II alpha (CaMKIIα) target forebrain neurons [31]. Transgenic mouse lines expressing Cre recombinase under the control of such promoters (e.g., the Crym promoter for corticospinal neurons) allow for flexible genetic access to these defined populations [31]. The primary advantages of this method are its non-invasiveness when using germline transgenics and its comprehensive coverage of the targeted cell type throughout the brain [31].
Spatial Control (Connectivity-Based Targeting)
This strategy uses the physical connectivity of a circuit—its origin and termination points—to achieve specificity. It involves introducing one genetic element at the cell bodies of origin (e.g., via an anterograde virus) and another at the axonal terminals (e.g., via a retrograde virus) [31]. Only neurons that are co-infected with both viruses—and thus form that specific connection—will express the transgene required for manipulation. This approach is powerful for dissecting circuits defined by their wiring rather than their molecular signature and allows for targeting specific projections from a heterogeneous region [31]. These two general approaches can be combined for even greater precision, such as by introducing a regulatory gene into the origin or termination of a circuit to manipulate neurons with a specific genetic identity within that pathway [31].
Table 1: Core Strategies for Defining and Targeting Neural Cell Types
| Strategy | Basis for Specificity | Key Tools | Primary Advantage | Common Application |
|---|---|---|---|---|
| Genetic Identity | Unique gene expression profile (e.g., transcription factors, neurotransmitters) | Cell-type-specific promoters (e.g., Vglut2, CaMKIIα); Cre/Lox and Flp/FRT recombinase systems [31] | Non-invasive; comprehensive coverage of a defined cell type across the brain [31] | Manipulating all neurons of a specific molecular class (e.g., all GABAergic neurons) |
| Spatial Control (Connectivity) | Physical wiring from point A to point B | Combinatorial viral delivery (anterograde + retrograde) [31]; Retrogradely transported viruses (e.g., CAV-2, AAV-retro) [17] | Targets circuits based on function rather than molecular identity; projects specificity from heterogeneous regions [31] | Isolating a specific pathway (e.g., prefrontal-to-amygdala projection) |
Essential Genetic Tools for Cell-Type Specificity
The implementation of the above strategies relies on a sophisticated genetic toolbox, with site-specific recombination systems serving as the core engine for precise targeting.
Site-Specific Recombination and Intersectional Genetics
Site-specific recombination (SSR) systems, most commonly Cre/loxP and Flp/FRT, allow for conditional expression of transgenes in genetically defined cells [30]. In these systems, a recombinase (Cre or Flp) is expressed under the control of a cell-type-specific promoter. This recombinase then acts on its target sites (loxP or FRT) that have been engineered to flank a "stop" cassette in a separate reporter or effector construct. The removal of the stop cassette activates expression of the downstream gene, ensuring it is only turned on in the desired cell type [30]. This is often achieved using the "Lox-Stop-Lox" (LSL) or "double-inverted orientation" (DIO, also known as FLEX) methods, the latter being particularly useful in viral vectors [30].
Intersectional genetics takes this specificity a step further by requiring the coincidence of two genetic features. For example, a neuron might only express a transgene if it expresses both Cre and Flp recombinases [30]. This allows for targeting of highly specific neuronal subpopulations that are defined by the overlap of two genetic markers, dramatically increasing precision beyond what is possible with a single promoter.
Activity-Dependent Targeting
Beyond static genetic identity, neurons can also be defined by their activity patterns during specific behaviors or states. Technologies such as TRAP (Targeted Recombination in Active Populations) and FLiCRE (Fast Light and Calcium-Regulated Expression) allow for permanent genetic labeling of neurons that are active during a defined time window [30]. In TRAP, administration of tamoxifen triggers Cre recombinase activity only in neurons that are simultaneously expressing the activity-dependent immediate early gene cfos [30]. FLiCRE uses a light- and calcium-dependent enzyme to label active neurons with high temporal precision [30]. These approaches enable researchers to tag and later manipulate functional ensembles, rather than just molecularly defined populations.
Diagram Title: Logic Flow for Targeted Neural Circuit Manipulation
Viral Vectors for Delivery of Genetic Tools
Viral vectors are the workhorses for delivering genetic tools to specific neural populations, with adeno-associated viruses (AAVs) being the most widely used due to their safety, low immunogenicity, and ability to achieve stable long-term expression [17].
Key Viral Vector Characteristics
- Adeno-Associated Virus (AAV): A replication-defective virus with a ~4.7 kb single-stranded DNA genome. Different serotypes exhibit tropism for different cell types. It is primarily anterograde and non-transsynaptic, ideal for labeling axonal projections, though AAV1 at high titers can show anterograde trans-monosynaptic transmission [17].
- Rabies Virus (RV): A retrograde, transsynaptic virus. The glycoprotein-deleted variant (RVdG) is used for retrograde tracing from a defined starter population in a monosynaptic manner, allowing for mapping of direct inputs [17].
- Herpes Simplex Virus (HSV1-H129): An anterograde, transsynaptic tracer with a large DNA genome, allowing for a big insert capacity. Used for mapping output circuits [17].
- Canine Adenovirus (CAV-2): A retrograde vector that preferentially transduces neuronal axon terminals, useful for retrograde access to projection neurons [17].
Table 2: Viral Vectors for Neural Circuit Mapping and Manipulation
| Virus | Genome Size / Capacity | Transport Direction | Transsynaptic Capability | Primary Use Case |
|---|---|---|---|---|
| AAV | ~4.7 kb / ~4.7 kb [17] | Predominantly anterograde [17] | Low (AAV1 can be anterograde monosynaptic at high titer) [17] | General gene delivery; anterograde tracing; expression of actuators/sensors |
| AAV-retro | ~4.7 kb / ~4.7 kb [17] | Efficient retrograde [17] | No | Retrograde access to projection neurons from a terminal field |
| RVdG | ~12 kb / ~3.7 kb [17] | Complete retrograde [17] | Monosynaptic (when complemented) | Monosynaptic input mapping to a defined starter cell population |
| HSV1-H129 | ~150 kb / ~50 kb [17] | Anterograde [17] | Polysynaptic (monosynaptic variants exist) | Anterograde output mapping across multiple synapses |
| CAV-2 | ~31 kb / ~30 kb [17] | Retrograde [17] | No | Efficient retrograde labeling from axon terminals |
Detailed Protocols for Targeted Manipulation
The following protocols integrate the principles and tools described above to outline specific methodologies for defining and manipulating neural circuits.
Protocol 1: Intersectional Targeting of a Specific Projection Pathway
Aim: To selectively express an optogenetic actuator in a genetically defined population that projects from Brain Region A to Brain Region B.
Workflow:
- Starter Cell Definition: Inject an AAV expressing Cre recombinase in a retrograde manner (e.g., AAV-retro or CAV-2-Cre) into the terminal field (Region B). This will deliver Cre retrogradely to neurons in Region A that project to Region B.
- Effector Delivery: In the same animal, inject a Cre-dependent AAV (e.g., DIO-ChR2) into the region of the cell bodies (Region A).
- Intersectional Expression: Only neurons in Region A that project to Region B (and thus received the retrograde Cre) will express the Cre-dependent ChR2. Neighboring neurons in Region A that project elsewhere will not be transfected.
Diagram Title: Intersectional Targeting of a Specific Projection
Protocol 2: Monosynaptic Input Mapping with Rabies Virus
Aim: To identify all direct presynaptic partners (inputs) of a genetically defined population of "starter" neurons.
Workflow:
- Label Starter Cells: Inject a Cre-dependent AAV expressing (a) a fluorescent protein (e.g., EGFP) and (b) the essential rabies glycoprotein (oG) into the target brain region of a Cre-driver mouse.
- Complement RVdG: After 3-4 weeks, inject the modified rabies virus (RVdG) that is EnvA-pseudotyped (to limit infection to cells expressing the TVA receptor) and encodes a different fluorescent protein (e.g., mCherry). The starter cells, which express oG, will package and release infectious RVdG particles.
- Transsynaptic Spread: The newly packaged RVdG spreads retrogradely, across one synapse, to infect the direct presynaptic neurons. These input neurons will express mCherry but cannot produce infectious particles because they lack oG, limiting the spread to one step.
Protocol 3: Functional Manipulation Using DREADDs
Aim: To chronically inhibit or excite a defined neural population during a behavioral task.
Workflow:
- Target and Deliver: Inject a Cre-dependent AAV encoding either the inhibitory (hM4Di) or excitatory (hM3Dq) DREADD into the target brain region of a Cre-driver mouse.
- Express and Recover: Allow 3-4 weeks for adequate expression of the DREADD receptor in the target cells.
- Administer Ligand: Systemically administer the inert designer drug Clozapine-N-Oxide (CNO) (typically 1-5 mg/kg, i.p.) 30-60 minutes before behavioral testing. CNO binding to hM4Di silences neuronal activity, while binding to hM3Dq increases it.
- Assess Behavior: Compare task performance (e.g., memory retrieval, fear expression, feeding) between CNO and vehicle sessions to infer the circuit's function.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Targeted Neural Circuit Research
| Reagent / Tool | Category | Function in Experiment |
|---|---|---|
| Cre/loxP & Flp/FRT Systems | Genetic Engine | Enables conditional, cell-type-specific expression of transgenes via site-specific recombination [30]. |
| AAV (Various Serotypes) | Viral Delivery Vehicle | Safely and efficiently delivers genetic cargo (opsins, DREADDs, sensors) to specific brain regions with cell-type specificity using Cre-dependent constructs [17]. |
| Rabies Virus (RVdG) | Viral Tracer | Maps monosynaptic inputs to a defined "starter" cell population when complemented with helper proteins (TVA and oG) [17]. |
| Channelrhodopsin-2 (ChR2) | Optogenetic Actuator | A light-sensitive cation channel that depolarizes and excites neurons upon blue light exposure, allowing for millisecond-timescale control [32]. |
| Halorhodopsin (NpHR)/Archaerhodopsin (Arch) | Optogenetic Actuator | Light-sensitive chloride or proton pumps that hyperpolarize and silence neurons upon yellow/green light exposure [32]. |
| DREADDs (hM3Dq, hM4Di) | Chemogenetic Actuator | Engineered GPCRs that modulate neuronal activity (excite or inhibit, respectively) for tens of minutes to hours upon administration of the inert ligand CNO [32]. |
| GCaMP | Neural Activity Sensor | A genetically encoded calcium indicator whose fluorescence increases with neuronal spiking, allowing for optical monitoring of population activity [32]. |
Engineering Precision: AAV Serotypes, Promoters, and CRISPR Integration
The precise manipulation of neural circuits for research and therapeutic purposes is critically dependent on the selective targeting afforded by specific adeno-associated virus (AAV) serotypes. This application note details the specialized use of three powerful capsids: PHP.eB for widespread central nervous system (CNS) transduction following intravenous administration, PHP.S for peripheral nervous system (PNS) targeting, and AAV2-retro for efficient high-resolution retrograde tracing of neural projections. We provide a structured comparison of their properties, summarized in the table below, alongside detailed protocols and essential reagent solutions to facilitate their effective implementation in gene delivery strategies for neural circuit dissection.
Table 1: Key Characteristics of Specialized AAV Serotypes
| Feature | PHP.eB | PHP.S | AAV2-Retro |
|---|---|---|---|
| Primary Application | Widespread CNS transduction from bloodstream [33] | Peripheral Nervous System (PNS) targeting [33] | Efficient retrograde access to projection neurons [34] [35] |
| Key Advantage | Efficiently crosses the blood-brain barrier (BBB) [33] | Enhanced tropism for peripheral tissues [33] | Retrograde transport efficiency comparable to classical tracers [35] |
| Injection Route | Intravenous (IV) [36] | Intravenous (IV) / Intraperitoneal (IP) | Focal injection into axon terminal fields [34] [18] |
| Tropism | Broad CNS cell types (neurons, astrocytes, oligodendrocytes) | DRG neurons, motor neurons, other PNS tissues | Projection neurons defined by injection site [34] [35] |
| Reported Transduction Efficiency | High throughout CNS after IV delivery [34] [33] | High in PNS tissues (e.g., dorsal root ganglia) [33] | Robust labeling in afferent brain regions (e.g., cortex, striatum) [34] [35] |
Serotype Profiles and Experimental Applications
PHP.eB for Central Nervous System (CNS) Transduction
PHP.eB is an engineered capsid derived from AAV9, selected for its superior ability to cross the blood-brain barrier (BBB) after systemic administration [33]. This property enables robust, non-invasive gene delivery to the brain and spinal cord without the need for direct intracranial injection, making it a transformative tool for modeling and treating global CNS diseases [34] [33].
Key Workflow: The standard protocol involves intravenous injection (e.g., via jugular or tail vein) of high-titer PHP.eB vectors ( [36], see Section 3.1 for detailed protocol). The virus circulates, binds to receptors on CNS vasculature, and is transcytosed into the brain parenchyma. For example, injection into deep cerebellar nuclei results in transduction of Purkinje cells, demonstrating its widespread reach [34].
AAV2-Retro for Efficient Retrograde Tracing
AAV2-retro is a specially engineered variant designed for highly efficient retrograde transport [35]. When injected into a brain region containing axonal terminals, the virus is internalized and transported backward along the axon to the connected neuronal cell bodies, enabling researchers to map and manipulate the inputs to a specific site [18] [35].
Key Workflow: AAV2-retro is delivered via precise, low-volume focal injection into the brain region of interest (e.g., basal pontine nuclei or striatum) [34] [35]. The virus is then taken up by axon terminals present in that region and retrogradely transported. This leads to transgene expression in the somata of projecting neurons, which can be located in remote regions such as the cortex or substantia nigra [34]. This process is summarized in the diagram below.
PHP.S for Peripheral Nervous System (PNS) Targeting
PHP.S is part of the same engineered family as PHP.eB but has been optimized for enhanced transduction of the PNS, including dorsal root ganglia (DRG) and motor neurons, after systemic delivery [33]. This serotype is invaluable for studying sensory perception, pain, and peripheral neuropathies. A related capsid, AAV-ROOT, was specifically developed for retrograde tracing from peripheral organs like adipose tissue to DRG neurons, demonstrating the power of specialized serotypes for PNS circuit mapping [37].
Quantitative Serotype Comparison
Selecting the optimal AAV serotype requires a comparative understanding of their performance across multiple metrics. The table below synthesizes data from key studies to guide this decision.
Table 2: Comparative Performance of AAV Serotypes in Neural Targeting
| Serotype | Injection Site | Target Region/Cell Type | Key Quantitative Finding/Note | Source |
|---|---|---|---|---|
| PHP.eB | Deep Cerebellar Nuclei | Purkinje Cells | Efficient transduction from a distal injection site. | [34] |
| AAV2-retro | Basal Pontine Nuclei (BPN) | Layer V Cortical Neurons | Dense labeling of afferent neurons in a highly convergent pathway. | [35] |
| AAV2-retro | Striatum | Substantia Nigra Neurons | Labels neurons projecting to the injection site. | [34] |
| AAV9 | Striatum | Substantia Nigra | Demonstrates natural, though less efficient, retrograde transport. | [34] |
| AAV5 | Hippocampus (Dentate Gyrus) | Entorhinal Cortex | Labeled cells co-localized with the retrograde tracer CTB. | [34] [38] |
| AAV-DJ | CNS (ICV/IT administration) | Widespread Brain & Spinal Cord | Significantly increased vector genome uptake in CNS vs. AAV9. | [36] |
Detailed Experimental Protocols
Protocol: Intravenous (IV) Delivery of PHP.eB for CNS Transduction
This protocol is adapted from methods used to compare AAV9 and AAV-DJ, applicable for PHP.eB [36].
Materials:
- Purified PHP.eB vector (e.g., ~1x10^13 vg/kg in 150 µL for mice [36])
- Anesthetic (e.g., 1-3% isoflurane)
- Sterile surgical tools (scissors, forceps)
- 28-30 gauge insulin syringe or catheter
- Analgesic (e.g., Meloxicam, 0.5 mg/kg)
Procedure:
- Anesthetize the mouse and secure it in a supine position.
- Perform a small incision (~0.5 cm) in the neck parallel to the midline to expose the external jugular vein.
- Slowly inject the viral preparation (e.g., 150 µL) into the vein using a bent 28-gauge needle.
- Apply gentle pressure for hemostasis upon needle withdrawal and close the incision with tissue adhesive.
- Administer analgesic subcutaneously and monitor the animal post-operatively according to IACUC guidelines.
- Allow 2-4 weeks for robust transgene expression before analysis.
Protocol: Focal Stereotaxic Injection of AAV2-retro for Circuit Mapping
This standard protocol for intracranial injection is used for AAV2-retro [34] [35].
Materials:
- AAV2-retro vector (high titer, ≥10^12 vg/mL)
- Stereotaxic apparatus
- Microsyringe (e.g., Hamilton, 26-gauge) or glass micropipette
- Anesthetic (e.g., ketamine/xylazine or isoflurane)
Procedure:
- Anesthetize the mouse and fix its head securely in the stereotaxic frame.
- Expose the skull through a midline scalp incision and identify Bregma and Lambda.
- Calculate target coordinates for the brain region of interest (e.g., striatum, basal pontine nuclei).
- Drill a small craniotomy at the calculated coordinates.
- Lower the needle slowly to the target depth.
- Infuse the virus (e.g., 50-500 nL at a rate of 50-100 nL/min) to minimize tissue damage and backflow.
- Leave the needle in place for 5-10 minutes post-injection before slow withdrawal.
- Suture the wound and provide post-operative care.
- Allow 2-4 weeks for retrograde transport and transgene expression.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for AAV-Based Neural Circuit Research
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| AAV2-retro Capsid Plasmid | Packaging plasmid for producing AAV2-retro viral particles. | Enables high-titer production of AAV2-retro for retrograde tracing experiments [39]. |
| AAV Helper Plasmid | Provides adenoviral helper functions (e.g., E4, VA, E2A) essential for AAV production. | Co-transfected with Rep/Cap and ITR-containing vector during AAV packaging [39]. |
| Cre-Dependent AAV Vectors | AAVs with a flipped transgene that is only expressed in the presence of Cre recombinase. | Restricts transgene expression to Cre-positive, retrogradely labeled cells for cell-type-specific manipulation [18]. |
| Cholera Toxin Subunit B (CTB) | A classical, non-viral retrograde tracer. | Used to validate the retrograde transport efficiency of AAV vectors via co-injection and co-localization [34] [38]. |
| Transgenic Cre Mouse Lines | Mice expressing Cre recombinase under a cell-type-specific promoter. | Provides genetic access to specific neuronal populations for intersectional targeting with retrograde AAVs [18]. |
Integrated Workflow for Intersectional Neural Circuit Manipulation
Combining AAV2-retro with Cre-lox technology represents a powerful strategy for achieving input-specific manipulation of defined neuronal populations. The following diagram and protocol outline this advanced workflow.
Procedure:
- Select an appropriate transgenic mouse expressing Cre recombinase in a neuronal population of interest (e.g., hippocampal neurons).
- Inject an AAV2-retro vector expressing Cre (not a Cre-dependent vector) into a target region receiving projections from these neurons (e.g., Broca's area analog). The virus will be retrogradely transported to the cell bodies in the Cre-positive population [18].
- In a second surgery, inject a Cre-dependent AAV (e.g., expressing a DREADD or channelrhodopsin) directly into the brain region containing the Cre-positive cell bodies (e.g., the hippocampus). This ensures the effector is only present where Cre is expressed.
- The effector transgene is activated only in the specific projection neurons (e.g., hippocampus → Broca's area) that were retrogradely accessed, allowing for precise functional manipulation [18]. This two-step method avoids spurious expression at the injection site of the retrograde vector.
Precise genetic manipulation of specific neural cell types is fundamental to advancing our understanding of brain function and developing targeted therapies for neurological disorders. The choice of promoter represents a critical determinant of specificity in gene delivery systems, controlling both the level and cellular localization of transgene expression. Within the context of neural circuit manipulation, three promoters have emerged as essential tools for targeting major neural cell populations: the human synapsin 1 (hSyn) promoter for neurons, the glial fibrillary acidic protein (GFAP) promoter for astrocytes, and the CD68 promoter for microglia.
Each of these promoters exhibits distinct specificity profiles and expression characteristics that make them uniquely suited for particular research applications. The development of these promoter systems represents a significant advancement over conventional ubiquitous promoters, which lack the cellular precision required for sophisticated neural circuit analysis. This application note provides a comprehensive technical resource for researchers utilizing these promoter systems, including quantitative performance comparisons, detailed protocols, and practical implementation guidelines for gene delivery strategies in neural circuit research.
Promoter Performance Characteristics and Quantitative Comparisons
Performance Metrics of Neural Cell-Type-Specific Promoters
Table 1: Performance characteristics of cell-type-specific promoters in the central nervous system
| Promoter | Target Cell Type | Specificity | Expression Strength | Key Advantages | Limitations |
|---|---|---|---|---|---|
| hSyn | Neurons | High (neuron-specific) [40] [41] | Strong [40] | Minimal off-target glial expression; activity-dependent regulation [42] | Variable expression across neuronal subtypes [42] |
| CD68 | Microglia | Moderate to High (when combined with specific AAV serotypes) [43] | Moderate [43] | Functional modulation of microglia possible [43] | May require specialized AAV capsids (e.g., AAV6 variants) [43] |
| mPGK | Broad (neurons + oligodendrocytes) [40] | Low specificity | Strong [40] | Compact size; strong overall expression | Lacks cellular specificity |
| hCMV | Broad (neurons + glia) [40] | Low specificity | Strong [40] | Very strong expression; widely available | Pronounced off-target glial expression [40] |
Performance Metrics of AAV Serotypes for Microglia Targeting
Table 2: Microglia transduction efficiency and specificity of scAAV serotypes with the hIBA1 promoter (1-week post-injection) [44]
| AAV Serotype | Microglia Specificity (%) | Transduction Efficiency (%) | Key Characteristics |
|---|---|---|---|
| AAV5 | 93.68 ± 1.14 | 69.7 ± 7.23 | Highest specificity |
| AAV8 | 77.42 ± 4.97 | 82.11 ± 0.8 | Highest efficiency |
| AAV1 | 46.55 ± 7.39 | 61.71 ± 7.52 | Moderate performance |
| AAV9 | 35.12 ± 7.82 | 70.27 ± 6.77 | Moderate efficiency, lower specificity |
| AAV6 | 29.69 ± 9.45 | 48.13 ± 8.83 | Lower performance |
| PHP.eB | 26.33 ± 4.0 | 37.84 ± 2.19 | Lower performance |
Molecular Mechanisms and Regulatory Features
hSyn Promoter Architecture and Neuronal Specificity
The human synapsin 1 (hSyn) promoter exhibits exceptional neuronal specificity through a sophisticated molecular architecture that integrates multiple regulatory mechanisms. Its specificity derives from cis-regulatory elements that interact with neuron-specific transcription factors, including binding sites for neuron-restrictive silencer factor (NRSF) which suppresses non-neuronal expression, and cyclic AMP response elements (CREs) that enable activity-dependent transcription [42]. This combination ensures that gene expression remains confined to neurons while allowing dynamic modulation in response to cellular signals.
The promoter also exhibits epigenetic regulation that reinforces its cell-type specificity. In neuronal cells, the hSyn promoter maintains a hypomethylated state with enriched histone H3 acetylation at lysines 9 and 27 (H3K9ac and H3K27ac), creating an open chromatin configuration permissive for transcription [42]. Conversely, in non-neuronal cells, the promoter is typically densely methylated and carries repressive histone marks that prevent activation. This epigenetic regulation creates a binary switch that restricts expression to neuronal contexts, making it particularly valuable for neuroscience applications requiring high specificity.
CD68 Promoter and Microglia Targeting Strategies
Microglia have proven particularly challenging to transduce with conventional AAV systems, necessitating specialized approaches. The CD68 promoter (a macrophage/microglia-specific marker) has shown utility when combined with specific viral vector configurations. Unlike neuronal targeting, effective microglia transduction requires optimization of both promoter selection and viral capsid engineering [45] [43].
The most successful microglia-targeting approaches have utilized modified AAV6 capsids, particularly the triple mutant T492V/Y705F/Y731F (TM6) combined with microglia-specific promoters like CD68 or F4/80 [43]. This capsid modification enhances intracellular trafficking in myeloid-lineage cells, overcoming natural barriers that limit microglial transduction. Additionally, recent work has identified the human IBA1 (hIBA1) promoter as a highly effective alternative, with a truncated 466-bp fragment (hIBA1a) maintaining strong microglia specificity while allowing packaging of larger transgenes [44]. Further specificity improvements can be achieved by incorporating target sequences for miR-9 and miR-129-2-3p, which exploit microglia-specific miRNA profiles to suppress off-target expression in other neural cells [45].
Experimental Protocols and Workflows
Intracranial AAV Delivery for Neuron-Specific Expression
Principle: This protocol enables targeted delivery of AAV vectors to specific brain regions for neuron-specific transgene expression using the hSyn promoter, allowing functional analysis of defined neural circuits [46].
Materials and Reagents:
- AAV vectors (serotypes 8 or 9) with hSyn promoter driving transgene of interest [46]
- C57BL/6 mice (or other appropriate model system)
- Digital stereotaxic instrument [46]
- Micropipette puller (e.g., Sutter P-97) [46]
- Microsyringe pump system (e.g., World Precision Instruments UMP3) [46]
- Glass capillary tubes for micropipettes [46]
- Sterile saline (0.9% NaCl) for viral dilution [46]
- Anesthesia equipment and reagents
Procedure:
- Micropipette Preparation: Pull glass capillary tubes using a micropipette puller to create injection micropipettes with a tip diameter of 10-25 μm. Carefully break the tip to achieve appropriate diameter using fine forceps [46].
Viral Solution Preparation: Thaw AAV aliquots on ice. For co-expression experiments, mix different AAV preparations at appropriate ratios (typically 1:1 for similar titer viruses). Dilute with sterile saline if necessary to achieve desired concentration and volume [46].
Stereotaxic Surgery: Anesthetize the animal and secure in stereotaxic apparatus. Identify coordinates for target region (e.g., hippocampus: AP -2.0 mm, ML ±1.5 mm, DV -1.8 mm from bregma for juvenile mice). Adjust coordinates based on age and brain region of interest.
Viral Injection: Load viral solution into micropipette. Lower micropipette slowly to target coordinate at approximately 1 mm/min. Inject virus at rate of 50-100 nL/min using microsyringe pump. Typical volumes range from 200-500 nL depending on target region. Allow 5-10 minutes post-injection before slowly retracting micropipette to minimize backflow [46].
Post-operative Care: Monitor animals until fully recovered from anesthesia. Allow adequate time for transgene expression (typically 2-6 weeks depending on AAV serotype and promoter).
Technical Notes:
- AAV serotypes 8 and 9 have demonstrated high efficiency for hippocampal dentate granule cell transduction when paired with the hSyn promoter [46].
- Optimal expression timing should be determined empirically for each construct and application.
- For specific neuronal pathway targeting, retrograde AAV vectors (HiRet/NeuRet) can be employed [47].
Microglia-Targeted Transduction Using Engineered AAV Vectors
Principle: This protocol describes a method for achieving microglia-specific transgene expression through combined use of the CD68 or hIBA1 promoter with engineered AAV capsids, enabling genetic manipulation of this typically refractory cell population [44] [43].
Materials and Reagents:
- scAAV vectors with CD68 or hIBA1 promoter packaged in AAV5 or AAV8 serotype [44]
- AAV6 TM6 variant (T492V/Y705F/Y731F) for enhanced microglia transduction [43]
- Appropriate animal model (consider disease models for enhanced transduction)
- Stereotaxic injection equipment
- L-NIO or other reagents for stroke induction (if using disease models) [44]
Procedure:
- Vector Selection: Select appropriate promoter-capsid combination based on specificity/efficiency requirements. scAAV5-hIBA1-GFP demonstrates >90% specificity for microglia, while AAV6 TM6 with CD68 promoter provides an alternative approach [44] [43].
Disease Model Induction (Optional): For enhanced microglia transduction, induce ischemic stroke via L-NIO administration or MCAO procedure one week prior to virus injection. This increases microglia receptivity to transduction [44].
Stereotaxic Injection: Perform standard stereotaxic procedure as described in Protocol 4.1, targeting striatum or other region of interest. Inject 1-2 μL of viral preparation (titer ≥ 10¹² gc/mL) at appropriate coordinates.
Expression Analysis: Allow 1-4 weeks for transgene expression. scAAV vectors typically show strong expression by 1 week that persists for at least 4 weeks [44].
Validation: Process tissue for immunohistochemical analysis using microglia-specific markers (IBA1, TMEM119) to confirm specificity and quantify transduction efficiency.
Technical Notes:
- Self-complementary AAV (scAAV) vectors provide stronger and more rapid expression than single-stranded AAV in microglia [44].
- The minimal 466-bp hIBA1a promoter maintains high specificity while allowing larger transgene packaging [44].
- Specificity can be further enhanced by incorporating miR-124 target sequences to suppress off-target expression in neurons [44].
Research Reagent Solutions and Toolkit
Table 3: Essential research reagents for neural cell-type-specific targeting
| Reagent Type | Specific Examples | Applications/Function | Source/Reference |
|---|---|---|---|
| AAV Serotypes | AAV1, AAV5, AAV8, AAV9 | Differential tropism for neural cell types | [40] [44] |
| Engineered Capsids | AAV6 TM6 (T492V/Y705F/Y731F) | Enhanced microglia transduction | [43] |
| Neuronal Promoters | hSyn (human synapsin 1) | Neuron-specific expression | [40] [41] [42] |
| Microglia Promoters | CD68, hIBA1 (466-bp fragment) | Microglia-specific expression | [44] [43] |
| Specificity Enhancers | miR-9, miR-124, miR-129-2-3p target sequences | Suppress off-target expression via miRNA regulation | [44] [45] |
| Vector Systems | scAAV (self-complementary AAV) | Faster, stronger expression compared to ssAAV | [44] |
| Retrograde Vectors | HiRet, NeuRet lentiviral vectors | Anterograde/retrograde neural circuit mapping | [47] |
Applications in Neural Circuit Research and Therapeutic Development
The targeted promoter systems described herein enable sophisticated approaches for dissecting neural circuit function and developing precision therapeutics. The hSyn promoter has been successfully employed to map functional connectivity and manipulate specific neuronal populations, with particular utility in cortical pyramidal neurons, hippocampal granule cells, and striatal medium spiny neurons [42]. When combined with activity-dependent regulatory elements, this promoter can report on and manipulate neurons based on their functional activation state, providing powerful insights into neural coding principles.
For microglia research, the CD68 and hIBA1 promoters have enabled critical advances in understanding neuroimmune interactions in health and disease. These tools have revealed microglial signaling pathways involved in purinergic signaling, neuroinflammation, and synaptic pruning [45]. The ability to selectively modulate microglial function through targeted gene delivery has particular therapeutic relevance for conditions including Alzheimer's disease, Parkinson's disease, and neuropathic pain [45]. Recent NIH BRAIN Initiative resources have significantly expanded the available toolkit, providing validated delivery systems for specific brain cell types across multiple species [13] [48].
The continuing refinement of these promoter systems—through truncation to minimize size while maintaining specificity, incorporation of regulatory elements for inducible control, and optimization for use with advanced serotypes—promises to further enhance their utility for basic research and therapeutic applications in the nervous system.
The CRISPR-Cas system has evolved from a bacterial adaptive immune system into a revolutionary toolkit for precision genome manipulation in eukaryotic cells, including post-mitotic neurons [49] [50]. This technology provides neuroscientists with unprecedented capabilities to dissect neural circuit function, model neurological disorders, and develop novel therapeutic strategies. The fundamental CRISPR-Cas system consists of two key components: a Cas nuclease and a guide RNA that directs the nuclease to specific genomic or transcriptomic targets [49]. While the original CRISPR-Cas9 system targets DNA, recent advancements have expanded the toolkit to include RNA-targeting Cas13 variants and precise single-base editors, each offering distinct advantages for neural circuit manipulation research [51] [52] [53].
The application of these technologies in neuroscience requires special consideration of neuronal biology. Unlike dividing cells, neurons pose unique challenges for gene editing due to their post-mitotic nature, low efficiency of homology-directed repair, and critical need for precision to avoid altering circuit function [54]. This application note details practical methodologies for implementing three major CRISPR-Cas platforms—Cas9, Cas13, and base editing—in neuronal systems, providing quantitative comparisons, optimized protocols, and resource guides for researchers.
CRISPR-Cas9 for Targeted Genome Editing in Neurons
Mechanism and Applications
The type II CRISPR-Cas9 system from Streptococcus pyogenes remains the most widely used platform for generating targeted double-strand breaks (DSBs) in genomic DNA [49] [50]. The system comprises the Cas9 endonuclease and a single-guide RNA (sgRNA) that directs Cas9 to complementary DNA sequences adjacent to a protospacer adjacent motif (PAM, typically 5'-NGG-3') [50]. Cas9 contains two nuclease domains: RuvC cleaves the non-target DNA strand, while HNH cleaves the target strand, resulting in a DSB [49]. Cellular repair of these breaks occurs primarily through non-homologous end joining (NHEJ), often introducing insertions or deletions (indels) that disrupt gene function, or through homology-directed repair (HDR) for precise gene insertion when a donor template is provided [49] [50].
In neurons, CRISPR-Cas9 has been successfully applied to study gene function in neural development, synaptic plasticity, and disease mechanisms. A key advancement for neuronal applications is the Targeted Knock-In with Two (TKIT) guides approach, which enables precise genomic knock-in in post-mitotic neurons by targeting non-coding regions rather than the coding sequence itself [54]. This method protects against INDEL mutations within the coding region and provides greater flexibility in guide RNA selection.
Quantitative Performance Metrics
Table 1: Editing Efficiencies of CRISPR-Cas9 Systems in Neuronal Applications
| Application | System | Model | Efficiency | Key Outcomes |
|---|---|---|---|---|
| Endogenous protein tagging | TKIT-Cas9 | Mouse primary cortical neurons | Up to 42% | Precise knock-in of SEP tag to GluA2 subunit [54] |
| In vivo neuronal tagging | TKIT-Cas9 | Mouse brain (in utero electroporation) | Not specified | Successful labeling of endogenous AMPARs [54] |
| Gene disruption | Plasmid-based Cas9 | Human iPSC-derived neurons | Variable (cell-dependent) | Dependent on delivery method and cell type [55] |
| Therapeutic editing | AAV-Cas9 | Mouse HD models | Significant reduction in mHTT | Improved motor function [56] |
Detailed Protocol: TKIT-Cas9 for Endogenous Protein Tagging in Neurons
Principle: The TKIT (Targeted Knock-In with Two guides) method enables precise labeling of endogenous proteins in neurons by using two guides that target non-coding regions flanking the insertion site, minimizing potential damage to the coding sequence [54].
Materials:
- Plasmid encoding SpCas9 and two guide RNAs targeting non-coding regions
- Donor DNA fragment containing tag (e.g., SEP) with flipped PAM sequences
- Primary neuronal cultures (DIV7-9)
- Transfection reagents (e.g., Lipofectamine)
- mCherry plasmid for morphology visualization
Procedure:
- Guide Design: Select two guide RNAs targeting non-coding regions (e.g., 5'-UTR and intron) approximately 100 bp from splice junctions.
- Donor Construct Design: Create a donor DNA fragment containing: the endogenous sequence with inserted tag, and the same two guides with opposite locations and flipped PAM sequences relative to the genomic DNA.
- Neuronal Transfection: Co-transfect primary cortical neurons (DIV7-9) with:
- Cas9 and dual-guide plasmid (1 µg)
- Donor DNA fragment (1 µg)
- mCherry morphology marker (0.5 µg)
- Incubation: Maintain transfected neurons for 7-10 days before analysis.
- Validation: Confirm successful knock-in via:
- Live imaging for punctate tag signal in dendritic spines
- Immunostaining with antibodies against the tag and endogenous protein
- RT-PCR and sequencing to verify intact splice junctions
Technical Notes:
- The flip-and-switch donor design promotes forward insertion through repeated Cas9 cutting of reverse insertions
- Efficiency can be enhanced by using high-fidelity Cas9 variants
- Include controls without Cas9/guides to confirm knock-in specificity
Visual Workflow: TKIT-Cas9 Mechanism
CRISPR-Cas13 for RNA Targeting in Neurological Disorders
Mechanism and Applications
CRISPR-Cas13 systems represent a breakthrough in RNA-targeting capabilities for neurological research and therapy. Unlike DNA-targeting Cas9, Cas13 proteins (type VI CRISPR effectors) are RNA-guided RNases that specifically bind and cleave single-stranded RNA targets [57] [56]. The Cas13d variant from Ruminococcus flavefaciens (RfxCas13d or CasRx) is particularly valuable for neuroscience applications due to its compact size (~930 amino acids), allowing packaging into a single AAV vector with its guide RNAs [57] [56].
A key advantage of Cas13 is its reversible action—by targeting RNA rather than DNA, it transiently reduces gene expression without permanently altering the genome [56]. This is particularly beneficial for therapeutic applications where temporary modulation of disease-related genes is desired. Cas13 has demonstrated exceptional utility in targeting repeat expansion disorders such as Huntington's disease (HD) and C9ORF72-linked ALS/FTD by selectively degrading mutant transcripts while sparing wild-type alleles [57] [56].
Quantitative Performance Metrics
Table 2: Therapeutic Efficacy of CRISPR-Cas13 in Neurological Disease Models
| Disease Model | Target | Delivery Method | Efficiency | Phenotypic Outcomes |
|---|---|---|---|---|
| Huntington's (zQ175 mice) | CAG repeat RNA | AAV9-Cas13d-CAGEX | Selective mHTT reduction | Improved motor coordination, reduced striatal atrophy, decreased protein aggregates [56] |
| C9-ALS/FTD (C9-BACexp mice) | G4C2 repeat RNA | AAV-Cas13d | Reduced repeat RNA without affecting normal C9ORF72 | Decreased RNA foci, reduced DPR proteins, reversed transcriptional deficits [57] |
| HD patient iPSC-neurons | CAG repeat RNA | Lentiviral-Cas13d | Allele-selective mHTT reduction | Sustained mutant HTT lowering without off-target effects [56] |
Detailed Protocol: Cas13d for Allele-Selective Targeting in HD Models
Principle: Cas13d can be programmed to selectively target and degrade expanded CAG repeat RNA in Huntington's disease while preserving normal HTT alleles, leveraging the longer repeat length in mutant transcripts for selective recognition [56].
Materials:
- AAV or lentiviral vector encoding nuclear-localized RfxCas13d
- U6-driven guide RNA expression cassette (CAGEX gRNA-2: 5'-TCG-3')
- HD patient fibroblasts or iPSC-derived neurons
- zQ175 knock-in HD mouse model
- Western blot reagents (polyQ antibody MAB1574)
- RNA isolation and blotting materials
Procedure:
- Guide RNA Selection: Design guides complementary to the CAG repeat RNA, testing different codons within the repeat (CAGEX gRNA-1: GTC; gRNA-2: TCG; gRNA-3: CGT). Empirical testing shows gRNA-2 provides optimal efficiency and specificity [56].
- Vector Packaging: Package Cas13d and guide RNA into a single AAV vector (serotype 9 for CNS delivery) or lentiviral vector for in vitro studies.
- In Vitro Validation: Transduce HD patient-derived fibroblasts or iPSC neurons with Cas13d-CAGEX.
- Assess polyQ protein reduction via western blot (MAB1574 antibody) at 7-14 days post-transduction
- Quantify mutant HTT mRNA reduction via RNA blotting
- Confirm specificity using CUG expansion controls
- In Vivo Delivery: For zQ175 mice, administer AAV-Cas13d-CAGEX via intrastriatal injection (2-3 µL per site, multiple sites).
- Functional Assessment: Monitor animals for 1-8 months post-injection:
- Motor coordination (rotarod, beam walk)
- Striatal volume (histology or MRI)
- HTT aggregate load (immunohistochemistry)
- Transcriptomic off-target effects (RNA-seq)
Technical Notes:
- Nuclear localization signals enhance Cas13d efficacy against nuclear RNA foci
- Include nontargeting gRNA controls (e.g., λ bacteriophage sequence)
- Optimal guide: CAGEX gRNA-2 shows highest efficiency with minimal collateral effects
- AAV9 provides broad CNS transduction; consider tissue-specific promoters
Visual Workflow: Cas13d Therapeutic Application
Base Editing for Precision Genome Modification in Neurons
Mechanism and Applications
Base editors represent a revolutionary advancement that combines the targeting capability of CRISPR systems with the precision of single-nucleotide changes without creating double-strand DNA breaks [52] [53]. These systems utilize catalytically impaired Cas proteins (nickase or dead Cas) fused to nucleobase deaminase enzymes that chemically convert one DNA base to another [52] [58]. Cytosine base editors (CBEs) convert C•G to T•A base pairs, while adenine base editors (ABEs) convert A•T to G•C base pairs [52] [53].
The key advantage of base editors for neurological applications is their ability to install precise point mutations without relying on HDR, which is inefficient in post-mitotic neurons [53]. Additionally, by avoiding DSBs, base editors minimize the introduction of indels and chromosomal abnormalities that can occur with Cas9 nuclease [52] [53]. This precision makes base editors particularly valuable for correcting point mutations associated with neurological disorders, introducing protective mutations, or creating precise disease models in neurons.
Quantitative Performance Metrics
Table 3: Base Editing Applications in Neurological Disease Models
| Application | Editor Type | Model System | Efficiency | Functional Outcomes |
|---|---|---|---|---|
| Spinal Muscular Atrophy | ABE | SMA mouse model | 87% conversion in motor neurons | Restored motor function, 6.5x lifespan extension, 40-fold SMN protein increase [58] |
| Therapeutic correction | CBE/ABE | Patient-derived neurons | Variable (target-dependent) | Correction of pathogenic point mutations [53] |
| Disease modeling | CBE | iPSC-derived neurons | Up to 60% editing | Introduction of specific pathogenic variants [53] |
Detailed Protocol: ABE-Mediated Correction for Spinal Muscular Atrophy
Principle: Adenine base editors can convert a single T•A base pair in the SMN2 gene to C•G, effectively transforming it into a functional SMN1 gene, thereby increasing survival motor neuron (SMN) protein levels in SMA [58].
Materials:
- ABE8e expression plasmid or mRNA
- sgRNA targeting SMN2 (5'-CTTCTCTACAGACTTACACA-3')
- SMA patient fibroblasts or iPSC-derived motor neurons
- SMA mouse model
- AAV delivery vectors (dual AAV system for in vivo)
- Nusinersen (commercial SMA drug) for combination therapy
- Western blot reagents for SMN protein detection
Procedure:
- Target Selection: Identify the target adenine (position 6 of SMN2 exon 7) within the base editing window (approximately positions 4-8).
- Editor Design: Select ABE8e variant with optimized editing efficiency and specificity.
- In Vitro Testing: Transfect SMA patient fibroblasts with ABE8e and sgRNA.
- Quantify base conversion efficiency via Sanger or next-generation sequencing (3-7 days post-transfection)
- Measure SMN protein levels via western blot (7-14 days)
- Assess cell viability and off-target editing
- In Vivo Delivery: For SMA mice, administer ABE via dual-AAV system (intracerebroventricular or systemic injection in neonates).
- AAV1: ABE8e expression cassette
- AAV2: U6-driven sgRNA expression
- Combination Therapy: Co-administer nusinersen (intrathecal injection, 12 mg/kg) to extend therapeutic window.
- Functional Assessment: Monitor mice for:
- Motor function (righting reflex, grip strength)
- Survival curve analysis
- SMN protein levels in spinal cord (western blot)
- Motor neuron counts (histology)
Technical Notes:
- Dual-AAV system required due to ABE size constraints; consider single-AAV with smaller Cas variants
- Combination with nusinersen shows synergistic effects
- Optimal editing window: positions 4-8 for ABE8e
- Include untreated SMA and wild-type controls
- Assess potential off-target RNA editing
Visual Workflow: Base Editing Mechanism
Research Reagent Solutions
Table 4: Essential Reagents for CRISPR-Cas Neural Applications
| Reagent Category | Specific Examples | Function | Applications |
|---|---|---|---|
| CRISPR Effectors | SpCas9, SaCas9, RfxCas13d, ABE8e, CBE4 | Core editing machinery | DNA cleavage, RNA targeting, base conversion |
| Delivery Vectors | AAV9, AAV-PHP.eB, Lentivirus, LNPs | Transport editors into neurons | In vivo and in vitro delivery |
| Guide RNA Systems | U6-driven sgRNA, tRNA-gRNA arrays | Target specificity | All CRISPR applications |
| Model Systems | Primary neurons, iPSC-derived neurons, zQ175 mice, SMA mice | Experimental context | Disease modeling, therapeutic testing |
| Validation Tools | NGS platforms, Western blot, Immunostaining | Confirmation of editing | Quality control, efficacy assessment |
| Specialized Components | Nuclear localization signals, Tissue-specific promoters | Enhancing efficiency and specificity | Cell-type targeting, subcellular localization |
Concluding Remarks
The CRISPR-Cas toolkit has dramatically expanded the capabilities of neuroscientists to manipulate neural circuits and model neurological disorders. Each platform—Cas9 for gene disruption, Cas13 for RNA targeting, and base editors for single-nucleotide precision—offers complementary strengths that can be matched to specific research goals. The protocols and data presented here provide a foundation for implementing these technologies in neuronal systems, with particular attention to the unique challenges of working with post-mitotic cells.
Future directions will likely focus on enhancing the precision and safety of these systems through improved editors with reduced off-target effects, advanced delivery methods for cell-type-specific targeting, and combination approaches that leverage the strengths of multiple platforms. As these technologies continue to evolve, they will undoubtedly yield deeper insights into neural circuit function and accelerate the development of novel therapies for neurological disorders.
The mammalian nervous system comprises a complex network of interconnected cells, requiring sophisticated tools for precise dissection of specific neural pathways. Intersectional approaches represent a paradigm shift in neural circuit manipulation, enabling researchers to target discrete neuron populations based on their combined genetic identity and connectivity profiles. These systems utilize recombinase technologies—primarily Cre and Flp—to achieve unprecedented specificity in labeling and manipulating neural circuits. By requiring multiple genetic elements for transgene activation, intersectional methods overcome the limitations of single-recombinase systems, allowing access to previously intractable neural populations. This precision is critical for understanding how specific circuits mediate brain function and behavior, particularly in densely packed brain regions where distinct cell types intermingle.
The fundamental principle underlying intersectional approaches is combinatorial genetic control, where transgene expression occurs only in cells meeting two or more predefined conditions. This strategy leverages the growing arsenal of Cre and Flp driver mouse lines while incorporating spatial and connectivity information through viral delivery methods. The development of these tools has accelerated research in systems neuroscience, providing means to dissect circuits with cellular precision in intact mammalian brains. As these technologies mature, they continue to reveal the organizational principles of neural systems and their roles in behavior and disease.
Conceptual Foundation of Intersectional Strategies
Core Principles of Genetic Intersectionality
Intersectional targeting strategies rely on two fundamental approaches for achieving circuit specificity: genetic identity and spatial connectivity. The genetic identity method targets neurons based on their molecular profile, such as expression of specific transcription factors, neurotransmitters, or calcium-binding proteins. This approach exploits the fact that certain genes are expressed uniquely in particular circuit components [31]. For example, corticospinal neurons can be distinguished from other corticofugal pathways by specific genes including Fezf2, Diap3, and Crym [31]. When a transgene is placed under control of the promoter region of these cell type-specific genes, only neurons with that genetic identity express the manipulative tool.
In contrast, the spatial connectivity approach uses knowledge of neural wiring to achieve specificity. This method introduces one genetic element at the origin of a circuit and another at its termination point. Only neurons that contain both elements—those connecting the two defined locations—express the functional transgene [31]. For instance, projection neurons in cortex sending axons to spinal cord can be targeted by injecting an anterograde virus into motor cortex and a retrograde virus into spinal cord, with only double-infected neurons undergoing genetic manipulation [31]. This approach excludes neurons near the origin that terminate elsewhere and neurons that terminate in the same location but originate elsewhere.
Advantages Over Traditional Methods
Traditional lesion and electrical stimulation techniques have provided foundational knowledge in systems neuroscience but lack the specificity required to dissect complex neural circuits. These methods affect all cell types within a region regardless of their connectivity or molecular identity [31]. Similarly, single-recombinase systems (Cre-only) can target broad cell classes but cannot access subsets defined by multiple criteria [59].
Intersectional approaches provide several distinct advantages:
- Subpopulation Access: Enable targeting subsets of cells within a Cre-positive population based on additional criteria such as projection target or Flp expression [59]
- Spatial Precision: Allow manipulation of Cre-expressing cells within a defined CNS site while excluding Cre-expressing cells in closely apposed brain regions [59]
- Circuit-Based Targeting: Permit genetic access based on connectivity rather than molecular identity alone [60] [31]
- Enhanced Specificity: Reduce off-target effects by requiring multiple conditions for transgene activation
The combination of these approaches provides neuroscientists with a powerful toolkit for addressing questions about neural circuit structure and function with unprecedented precision.
Recombinase Systems: Cre and Flp Tools
Core Recombinase Technologies
The Cre/loxP and Flp/FRT systems form the foundation of intersectional approaches in neuroscience. Cre recombinase from bacteriophage P1 recognizes loxP sites, while Flp recombinase from Saccharomyces cerevisiae recognizes FRT sites. When these recombinases act on their respective target sites flanking a DNA sequence, they can cause excision, inversion, or translocation depending on the orientation and position of the sites.
Cre-dependent systems have become the gold standard for cell-type-specific manipulation in neuroscience. Hundreds of Cre mouse lines generated through individual labs and large-scale efforts direct specific gene expression in wide-ranging cell types throughout the nervous system [61]. These tools are often combined with Cre-dependent AAV vectors that utilize loxP-flanked ("floxed")-stop or floxed-inverse (FLEX) cassettes, where only Cre-positive cells activate expression of the transgene [61].
Flp-dependent systems have advanced significantly with the development of thermostable, codon-optimized versions (Flpo) that function efficiently in mammals [62]. The combinatorial use of Cre and Flp in double-transgenic mice, where each recombinase is driven by tissue- or cell-type-specific promoters, enables more detailed investigations of neural populations through conditional genetic manipulation [62].
Advanced Recombinase Applications
Recent developments have further expanded the recombinase toolkit for intersectional approaches:
Photoactivatable Flp recombinase (PA-Flp) represents a breakthrough in spatiotemporal control of genetic manipulation. This highly light-sensitive tool enables noninvasive activation of Flp in deep mouse brain regions using external LED illumination [63] [62]. PA-Flp is constructed by splitting Flpo into two fragments fused to light-inducible heterodimerization domains from the Magnet system. Blue light illumination induces recombination, allowing precise temporal and spatial control of genetic manipulation [62]. This system can be extended to the Cre-lox system through a viral vector as a Flp-dependent Cre expression platform, thereby activating both Flp and Cre [62].
Enhanced recombinase efficiency has been addressed through molecular engineering. For Cre-dependent systems, the development of robust transgenic mouse lines with high-level, Cre-dependent expression of optogenetic molecules from a modified Rosa26 locus represents a significant advance over previous lines [61]. These systems incorporate a CAG promoter and the woodchuck hepatitis virus post-transcriptional regulatory element (WPRE) to drive strong, ubiquitous, Cre-dependent expression [61].
Table: Key Recombinase-Dependent AAV Plasmids for Intersectional Approaches
| Catalog Number | Name | Recombinase Dependence | Function |
|---|---|---|---|
| 105555 | pENN.AAV.hSyn.Cre.hGH | None | Expresses Cre using hSyn1 promoter |
| 51669 | AAV phSyn1(S)-FlpO-bGHpA | None | Expresses FlpO using hSyn1 promoter |
| 28306 | pAAV-FLEX-tdTomato | Cre | Cre-dependent fluorescent reporter |
| 114471 | pAAV-Ef1a-fDIO mCherry | Flp | Flp-dependent fluorescent reporter |
| 55650 | pAAV-hSyn Con/Fon EYFP | Cre + Flp | Requires both Cre and Flp activity |
| 149296 | pAAV-nef-CIAO2-Flp | Cre | For Cre-dependent expression of FlpO |
Intersectional Methodologies and Implementation
Dual-Recombinase Systems
Dual-recombinase systems represent the cornerstone of intersectional neural circuit manipulation, with several implementations offering different advantages:
The INTRSECT system utilizes a single AAV vector that flanks the transgene coding sequence with lox and FRT sites in a specific configuration where combinatorial expression of Cre and Flp permits expression of a functional pre-mRNA that is spliced to produce mature coding sequence [59]. While this system works well in contexts with robust Flp and Cre activities, its multiple inversion and splicing steps can limit transgene expression, particularly with poor recombinase activity [59].
The tTARGIT system addresses limitations in recombinase activity and represents a more sensitive dual-recombinase approach. This system employs two separate AAVs: a Flp-dependent "Driver" AAV expressing the tetracycline transactivator (tTA) and a Cre-dependent "Payload" AAV containing the transgene under control of a tetracycline response element (TRE) [59]. Only cells expressing both Cre and Flp activate transgene expression. The system incorporates two tetracycline operators to drive a positive feedback loop that enhances tTA expression, increasing sensitivity [59].
Dre recombinase represents an orthogonal system that can be combined with Cre and Flp for even higher-order intersectional control, although it was not specifically covered in the search results.
Diagram: tTARGIT Dual-Recombinase System Logic. This diagram illustrates how the tTARGIT system requires both Cre and Flp activity for transgene expression. The Flp-dependent Driver AAV produces tTA, which then activates the Cre-dependent Payload AAV. Only intersectional neurons containing both recombinases express the final transgene.
Connectivity-Based Intersectional Targeting
Beyond genetic intersectionality, neural circuits can be targeted based on their input-output connectivity patterns. These approaches use the axonal transport properties of AAV vectors to deliver genetic elements to specific neuronal populations based on their connections [60].
Input-based targeting focuses on neurons receiving specific inputs by injecting a retrograde AAV expressing one recombinase at the projection site and an AAV expressing a recombinase-dependent transgene at the cell body location. Only neurons that both contain the transgene and project to the specific site will express the manipulative molecule.
Output-based targeting identifies neurons based on their axonal projections by injecting an anterograde AAV expressing one recombinase at the cell body location and a retrograde AAV expressing the other recombinase at the projection site. Again, only double-infected neurons express the transgene.
Input-output convergence targets neurons that receive specific inputs and send specific outputs by combining these approaches, requiring evidence of both input and output connectivity for transgene expression.
Table: Intersectional Connectivity Targeting Strategies
| Targeting Strategy | Injection 1 Site | Injection 1 Vector | Injection 2 Site | Injection 2 Vector | Targeted Population |
|---|---|---|---|---|---|
| Input-Based | Projection site | Retrograde AAV-Flp | Cell body region | Cre-dependent transgene | Neurons projecting to site 1 |
| Output-Based | Cell body region | Anterograde AAV-Cre | Projection site | Flp-dependent transgene | Neurons receiving from site 1 |
| Input-Output | Input source | Retrograde AAV-Flp | Output target | Retrograde AAV-Cre | Neurons connecting site 1 to site 2 |
| Divergence-Based | Cell body region | Cre-dependent + Flp-dependent | Multiple sites | Different retrograde AAVs | Neurons with divergent projections |
Research Reagent Solutions and Protocols
Essential Research Toolkit
Implementation of intersectional approaches requires specific genetic tools, viral vectors, and animal models. The following table summarizes key reagents for establishing these systems in the laboratory:
Table: Research Reagent Solutions for Intersectional Neural Circuit Manipulation
| Reagent Category | Specific Tools | Function | Source/Reference |
|---|---|---|---|
| Cre Driver Mouse Lines | Emx1-Cre, Pvalb-IRES-Cre, Camk2a-CreERT2 | Provide cell-type-specific Cre expression | [61] |
| Flp Driver Mouse Lines | Slc17a6FlpO, Various Flp driver lines | Provide cell-type-specific Flp expression | [59] |
| Cre-Dependent AAV Reporters | AAV-FLEX-tdTomato, AAV-FLEX-EGFP | Cre-dependent fluorescent labeling | [60] |
| Flp-Dependent AAV Reporters | AAV-fDIO-mCherry, AAV-fDIO-EGFP | Flp-dependent fluorescent labeling | [60] |
| Dual-Recombinase AAV Systems | INTRSECT AAVs, tTARGIT AAVs | Require both Cre and Flp for transgene expression | [59] |
| Optogenetic Actuators | ChR2(H134R)-tdTomato, ChR2(H134R)-EYFP | Light-activated neural excitation | [61] |
| Optogenetic Silencers | Arch-ER2, eNpHR3.0-EYFP | Light-activated neural inhibition | [61] |
| Chemogenetic Tools | hM3D(Gq)-mCherry, hM4D(Gi)-mCherry | Drug-activated neural modulation | [60] |
Detailed Protocol: tTARGIT System Implementation
Objective: Target leptin receptor-expressing neurons in the ventromedial hypothalamus (LepRbVMH) while excluding neighboring LepRb populations using Slc17a6FlpO;LeprCre mice and tTARGIT AAVs.
Materials:
- Slc17a6FlpO;LeprCre double-transgenic mice
- AAV-hSYN1-fDIO-tTA (tTARGIT Driver AAV)
- AAV-TRE-DIO-ChR2-TdTomato (tTARGIT Payload AAV)
- Stereotaxic apparatus
- Microinjection system
- Anaesthesia equipment
- Standard surgical supplies
Procedure:
Stereotaxic Surgery
- Anesthetize adult Slc17a6FlpO;LeprCre mice using appropriate anesthetic (e.g., ketamine/xylazine or isoflurane)
- Secure mouse in stereotaxic apparatus with head level
- Make midline scalp incision and clean skull surface
- Identify bregma and lambda coordinates, adjust until level
- Calculate target coordinates for ventromedial hypothalamus (VMH): -1.5 mm AP, ±0.5 mm ML, -5.8 mm DV from bregma
- Drill craniotomy at target coordinates
Viral Injection
- Prepare viral mixture combining AAV-hSYN1-fDIO-tTA (Driver) and AAV-TRE-DIO-ChR2-TdTomato (Payload) in 1:1 ratio
- Load viral mixture into glass micropipette or Hamilton syringe
- Lower injection needle slowly to target coordinates
- Inject 300-500 nL of viral mixture at rate of 50 nL/min
- Wait 10 minutes after injection to allow diffusion
- Slowly retract injection needle
- Close surgical site with sutures or wound clips
- Provide postoperative care and monitoring
Incubation and Expression
- Allow 3-4 weeks for viral expression and transgene activation
- Verify expression pattern histologically before experimentation
Validation and Experimental Application
- Prepare brain sections containing VMH
- Confirm TdTomato fluorescence specifically in VMH LepRb neurons
- Verify absence of labeling in adjacent hypothalamic regions
- Proceed with functional studies using optical stimulation
Troubleshooting:
- Low expression: Ensure viral titer > 10^12 genome copies/mL
- Off-target expression: Verify specificity of Flp and Cre driver lines
- Incomplete coverage: Optimize injection coordinates and volume
Applications in Neural Circuit Analysis
Functional Circuit Mapping
Intersectional approaches enable precise functional mapping of neural circuits by allowing selective manipulation of defined cell populations while monitoring downstream effects. The tTARGIT system demonstrated this capability in studying LepRbVMH neurons, revealing their specific role in suppressing food intake and increasing energy expenditure [59]. By selectively expressing channelrhodopsin in these neurons, researchers could optically stimulate this population while measuring metabolic parameters and feeding behavior, establishing a causal relationship between circuit activity and physiological function.
Similar approaches can be applied to numerous neural systems:
Corticospinal circuit manipulation uses intersectional approaches to target layer 5 pyramidal neurons projecting to specific spinal cord segments while excluding other corticofugal projections [31]. This precision is crucial for understanding the differential control of motor functions by distinct cortical outputs.
Striatal circuit dissection employs intersectional tools to distinguish direct and indirect pathway neurons based on their differential expression of dopamine receptors and neuropeptides, while further segregating subpopulations based on their input from specific cortical areas or output to particular basal ganglia targets.
Behavioral Circuit Analysis
The precise cell-type targeting afforded by intersectional approaches enables researchers to establish causal links between specific neural populations and complex behaviors:
Emotional behavior circuits can be dissected by targeting amygdala neurons defined by both genetic markers and their connectivity to specific prefrontal or hypothalamic regions. This allows researchers to determine how distinct amygdala subcircuits contribute to fear, anxiety, and reward-related behaviors.
Sensorimotor integration studies benefit from intersectional approaches that selectively manipulate neurons processing specific sensory modalities while controlling particular motor outputs, revealing how sensory information is transformed into appropriate behavioral responses.
Cognitive circuit analysis uses these tools to target prefrontal and hippocampal neurons involved in working memory, decision making, and spatial navigation, with the ability to distinguish contributor populations based on both molecular identity and long-range connectivity.
Diagram: Intersectional Approaches Application Workflow. This diagram illustrates how different intersectional targeting approaches combine with manipulation tools to enable various research applications in neural circuit analysis, from basic mapping to disease modeling.
Technical Considerations and Optimization
Implementation Challenges
Successful implementation of intersectional approaches requires careful consideration of several technical factors:
Recombinase efficiency varies significantly between systems and cell types. Flp recombinase generally exhibits lower efficiency than Cre, potentially limiting transgene expression in dual-recombinase systems [59]. The tTARGIT system addresses this limitation through signal amplification using the tTA-TRE system, which can enhance expression even with moderate recombinase activity [59].
Viral tropism and spread influence which cells are infected and how much transgene they express. Different AAV serotypes exhibit varying preferences for different cell types and varying spread characteristics from injection sites [60]. Serotype selection should be optimized for each experimental context.
Temporal control of recombinase activity is crucial for developmental studies and for avoiding compensatory mechanisms. Inducible systems including photoactivatable Flp [62] and chemically inducible Cre (Cre-ERT2) provide temporal control over recombination events.
Specificity validation is essential for interpreting results from intersectional experiments. Controls should include verification of driver line specificity, viral targeting accuracy, and absence of leaky expression in single-recombinase conditions.
Optimization Strategies
Several strategies can enhance the performance of intersectional approaches:
Promoter selection influences the strength and specificity of transgene expression. Synapsin promoters (hSYN1) generally drive strong expression in neurons, while CaMKIIα promoters provide specificity for excitatory neurons [61]. The CAG promoter offers strong, ubiquitous expression but may lack cell-type specificity.
Vector design improvements include the incorporation of woodchuck hepatitis virus post-transcriptional regulatory element (WPRE) to enhance mRNA stability and nuclear export, leading to increased transgene expression [61]. Self-complementary AAV genomes can achieve more rapid and robust expression than single-stranded genomes.
Expression amplification systems like the tTA-TRE feedback loop in the tTARGIT system can dramatically increase transgene expression levels, compensating for moderate recombinase activity or low viral titer [59].
Serotype mixing using different AAV serotypes for Driver and Payload vectors can reduce competition for cellular entry and enhance the proportion of double-infected cells.
Emerging Technologies
Intersectional approaches continue to evolve with several promising developments on the horizon:
Higher-order intersectionality using additional recombinase systems (Dre) or split-intein approaches will enable targeting of increasingly specific cell populations defined by three or more genetic or connectivity features.
Temporal precision improvements through engineered photoactivatable recombinases with different activation spectra will enable sequential manipulation of different neural populations within the same experiment.
Noninvasive manipulation advances using engineered AAV capsids that cross the blood-brain barrier or respond to systemically administered ligands will reduce the need for invasive surgical procedures.
Multiplexed recording and manipulation tools will allow simultaneous monitoring and control of multiple distinct neural populations within the same brain, revealing how different circuit elements interact during behavior.
Intersectional approaches using Cre-dependent and Flp-dependent systems have revolutionized neural circuit research by enabling unprecedented precision in targeting defined cell populations. These methodologies overcome fundamental limitations of traditional techniques by combining genetic identity with connectivity information to access specific neural subpopulations. The continued development of increasingly sensitive and specific tools—including the tTARGIT system for challenging targets and photoactivatable Flp for spatiotemporal control—promises to further accelerate discovery in systems neuroscience.
As these technologies become more widely adopted and integrated with other advanced methods for monitoring and manipulating neural activity, they will continue to illuminate the organizational principles of neural circuits and their contributions to behavior, cognition, and disease. The flexibility and precision of intersectional approaches make them indispensable tools in the modern neuroscience toolkit, with applications ranging from basic circuit mapping to therapeutic development.
Gene delivery to the central nervous system (CNS) represents a transformative approach for both basic research in neural circuit manipulation and the treatment of neurological disorders. The unique protective barriers of the CNS, particularly the blood-brain barrier (BBB), pose significant challenges for delivering genetic material to specific neural cell types. Researchers have developed three primary administration routes to overcome these obstacles: direct intracranial injection, intravenous delivery, and cerebrospinal fluid (CSF) conduit routes. Each method offers distinct advantages and limitations in terms of invasiveness, transduction efficiency, biodistribution, and specificity. This article provides a comprehensive technical overview of these delivery modalities within the context of neural circuit manipulation research, offering structured experimental protocols and practical guidance for implementation. The selection of an appropriate gene delivery strategy is critical for achieving targeted expression while minimizing off-target effects, ultimately enabling precise interrogation of neural circuit function.
Comparative Analysis of Delivery Modalities
Table 1: Comparison of CNS Gene Delivery Modalities
| Delivery Method | Key Advantages | Key Limitations | Transduction Efficiency | Primary Applications |
|---|---|---|---|---|
| Intracranial Injection | High local concentration; Bypasses BBB; Precise targeting of specific regions | Invasive; Limited distribution volume; Tissue damage risk | Very high in immediate injection area | Focal neural circuit modulation; Localized gene expression |
| Intravenous Delivery | Minimal invasiveness; Whole-body distribution; Clinically translatable | Limited BBB penetration requires high doses; Significant off-target exposure | Low in CNS without enhanced vectors | Global CNS transduction with engineered AAVs; Systemic applications |
| CSF Routes | Widespread CNS distribution; Less invasive than intraparenchymal; Reduced systemic exposure | Requires specialized surgical skills; Variable distribution patterns | Moderate to high depending on serotype and injection site | Broad CNS targeting; Spinal cord interventions |
Table 2: Quantitative Parameters for CNS Gene Delivery in Animal Models
| Parameter | Intracranial Injection | Intravenous Delivery | Intrathecal (CSF) Delivery | Intracisternal (CSF) Delivery |
|---|---|---|---|---|
| Typical Volume (Mouse) | 0.5-2 µL | 100-200 µL | 5-10 µL | 5-10 µL |
| Viral Titer Range | 10¹¹-10¹³ vg/mL | 10¹²-10¹⁴ vg/kg | 10¹¹-10¹³ vg | 10¹¹-10¹³ vg |
| Distribution Pattern | Focal, ~1-3 mm from injection site | Widespread but limited CNS penetration without enhanced vectors | Rostral flow along neuraxis; Strong spinal and brainstem transduction | Widespread brain and spinal cord distribution |
| Expression Onset | 3-7 days | 7-14 days | 7-14 days | 7-14 days |
| Peak Expression | 2-4 weeks | 3-6 weeks | 3-6 weeks | 3-6 weeks |
The biodistribution patterns vary significantly across delivery methods. Direct intracranial injection provides highly localized transduction ideal for targeting specific nuclei within neural circuits [64]. Intravenous delivery leads to widespread distribution throughout the body, with CNS transduction dependent on the AAV serotype's ability to cross the BBB [65]. CSF routes via intrathecal or intracisternal delivery enable broad distribution along the entire neuraxis, making them suitable for conditions requiring widespread CNS gene expression [66] [67]. Recent advances in AAV engineering have produced capsid variants with enhanced CNS tropism and reduced liver targeting, improving the specificity of both intravenous and CSF-delivered vectors [68] [69].
Intracranial Injection Protocols
Stereotaxic Intraparenchymal Delivery
Direct intracranial injection remains the gold standard for precise, localized gene delivery to specific brain regions. This method involves stereotaxically guided injection of viral vectors directly into the brain parenchyma, enabling highly targeted transduction of discrete neural populations within a circuit.
Table 3: Materials for Stereotaxic Intracranial Injection
| Category | Specific Items | Purpose/Function |
|---|---|---|
| Surgical Equipment | Stereotaxic frame with manipulator arm; UltraMicroPump with controller (e.g., UMP3 with SYS-Micro4); Microtorque drill with 1.4mm burr | Precise positioning and controlled delivery; Automated infusion control; Creating cranial access |
| Injection Components | Glass micropipettes or Hamilton syringes; Wiretrol capillary micropipettes (1-5 µL); Mineral oil | Viral vector containment and delivery; Precise fluid handling; Preventing capillary clogging |
| Viral Vector Prep | AAV aliquots (avoid freeze-thaw cycles); Dry ice or freezer at -80°C; Biohazard waste container with 10% bleach | Maintaining vector viability; Viral storage; Safe disposal of contaminated materials |
| Animal Prep | Anesthetic (Avertin 200mg/kg or isofluorane); Analgesic (Buprenorphine 0.05-0.1mg/kg); Ophthalmic ointment; Heating pad | Surgical anesthesia; Post-operative pain management; Eye protection; Maintaining body temperature |
Step-by-Step Protocol:
Viral Vector Preparation: Thaw viral aliquots on ice and briefly vortex. For AAV vectors, typical titers range from 10¹²-10¹³ vg/mL. Draw up the viral solution into a glass micropipette or Hamilton syringe using a microinjection pump. For precise labeling of neural circuits, volumes of 0.5-2 µL are typically infused over 10-20 minutes [64].
Animal Preparation: Anesthetize the animal using appropriate anesthesia (e.g., 200 mg/kg Avertin intraperitoneally or isofluorane inhalation). Secure the animal in the stereotaxic frame using ear bars and a nose cone. Maintain body temperature at 37°C using a heating pad throughout the procedure. Apply ophthalmic ointment to prevent corneal drying. Administer preoperative analgesics (e.g., buprenorphine at 0.05-0.1 mg/kg) [64].
Surgical Exposure: Shave the scalp and disinfect the skin with alternating scrubs of ethanol and betadine. Make a midline incision on the scalp and retract the skin to expose the skull. Gently remove the fascia using fine-tipped forceps to visualize cranial landmarks (bregma and lambda). Level the skull to ensure accurate stereotaxic coordinates [64].
Coordinate Identification and Craniotomy: Identify the target coordinates relative to bregma. Mark the injection site on the skull. Using a microdrill with a 0.5-1.0 mm burr, perform a craniotomy at the marked location, taking care not to damage the underlying dura. Keep the skull moist with sterile saline throughout the procedure [64].
Viral Injection: Slowly lower the loaded micropipette to the target depth at a rate of approximately 1 mm/minute. Initiate infusion at a controlled rate (typically 0.1-0.2 µL/min for most applications). After completing the injection, leave the pipette in place for an additional 5-10 minutes to prevent reflux along the injection tract. Slowly retract the pipette (1 mm/minute) [64].
Post-operative Care: Suture the scalp and apply tissue adhesive to seal the wound. Administer postoperative analgesics every 8-12 hours for 48-72 hours. Monitor animals until they fully recover from anesthesia and resume normal behavior. Allow 1-4 weeks for transgene expression before conducting functional experiments [64].
Technical Considerations for Intracranial Delivery
The efficiency of intracranial gene delivery depends on several critical parameters. Injection volume and rate must be optimized based on the target region to minimize tissue damage and reflux. AAV serotype selection significantly influences tropism; AAV1, AAV2, AAV5, and AAV9 effectively transduce neurons, while AAV4 shows preference for ependymal cells [64]. Promoter selection (e.g., synapsin for neurons, GFAP for astrocytes) enables cell-type specific expression within targeted circuits. For neural circuit mapping, modified vectors capable of anterograde (AAV1) or retrograde (AAV6, AAVretro) transport can be employed to label projection-specific populations [66].
Intravenous Delivery Protocols
Systemic Vector Administration
Intravenous delivery offers a less invasive approach for widespread CNS transduction, particularly with engineered AAV capsids that efficiently cross the blood-brain barrier.
Step-by-Step Protocol:
Vector Preparation: Thaw and prepare AAV vectors on ice. For systemic delivery, higher doses (10¹²-10¹⁴ vg/kg) are typically required compared to direct CNS injection methods. Dilute the vector in sterile saline to achieve the desired concentration in an injectable volume (100-200 µL for mice) [65].
Animal Preparation: Warm the animal under a heat lamp to facilitate vasodilation. Place the animal in a restraining device that allows access to the tail. Clean the tail with alcohol to improve visibility of lateral tail veins.
Injection Procedure: Using a 27-30 gauge insulin syringe, insert the needle bevel-up into the lateral tail vein at a shallow angle. Confirm proper placement by observing a slight flashback of blood. Slowly inject the vector solution over 30-60 seconds. Apply gentle pressure to the injection site for hemostasis after needle withdrawal [65].
Post-injection Monitoring: Return the animal to its home cage and monitor until fully recovered. Transgene expression in the CNS typically peaks at 3-6 weeks post-injection.
Enhancing CNS Transduction
Several strategies can enhance CNS transduction following intravenous delivery. Selection of AAV serotypes with innate neurotropism is crucial; AAV9 and AAV-PHP.B variants show significantly improved CNS penetration compared to other serotypes [69] [65]. Mannitol pretreatment (25% solution, 200 µL via tail vein 20 minutes before vector injection) can temporarily disrupt the BBB and enhance CNS vector entry [65]. Recent capsid engineering approaches have identified variants with improved BBB crossing and cell-type specificity, such as AAVs targeting human carbonic anhydrase IV for enhanced brain delivery [69].
Cerebrospinal Fluid Route Protocols
Intrathecal and Intracisternal Delivery
CSF-based delivery methods provide excellent distribution throughout the CNS while being less invasive than direct intraparenchymal injection. These approaches are particularly valuable for conditions requiring widespread CNS gene expression.
Table 4: CSF Delivery Methods and Applications
| Method | Injection Site | Technical Considerations | Best For |
|---|---|---|---|
| Intrathecal Lumbar Puncture | Lumbar subarachnoid space (L4-L5) | Simple procedure in awake animals; Rostral CSF flow | Spinal cord and brainstem targeting; Sensory ganglia |
| Intracisternal Magna Injection | Cisterna magna (cerebellomedullary cistern) | Requires anesthesia and precise needle placement; Risk of brainstem injury | Widespread brain and spinal cord distribution |
| Intracerebroventricular Injection | Lateral cerebral ventricle | Stereotaxic surgery required; Ependymal barrier limits parenchymal penetration | Periventricular structures; Global CNS delivery |
Intrathecal Lumbar Puncture Protocol (Mouse):
Vector Preparation: Prepare AAV vector at appropriate titer (typically 10¹¹-10¹³ vg in 10 µL for mice). Keep on ice until injection.
Animal Restraint: Manually restrain the awake mouse in a flexed position to separate the lumbar vertebrae. Alternatively, use a specialized restraint device.
Injection Procedure: Identify the L4-L5 intervertebral space. Using a 30-gauge needle attached to a Hamilton syringe, perform a direct lumbar puncture. Correct placement is confirmed by a tail flick reflex. Slowly inject the vector over 30-60 seconds. Leave the needle in place for an additional 30 seconds before withdrawal [65].
Intracisternal Magna Injection Protocol (Mouse):
Animal Preparation: Anesthetize the animal and secure in a stereotaxic frame or position in ventral recumbency with the neck flexed.
Landmark Identification: Palpate the occipital crest and the atlas to identify the cisterna magna.
Injection Procedure: Using a 30-gauge needle attached to a Hamilton syringe, carefully puncture the cisterna magna at the midline. Slowly inject the vector solution (5-10 µL for mice) over 60 seconds. Withdraw the needle slowly and monitor the animal until recovery [67].
Technical Considerations for CSF Delivery
The distribution of AAV vectors within the CSF is influenced by several factors. Convection-enhanced delivery or infusion pumps can improve distribution compared to bolus injection. Different AAV serotypes exhibit varying transduction patterns after CSF delivery; AAV9 transduces both neurons and glia throughout the CNS, while AAVrh.10 shows strong neuronal tropism [66]. The injection site significantly influences biodistribution; intracisternal delivery generally provides more widespread brain transduction, while intrathecal lumbar delivery preferentially targets spinal cord and sensory ganglia [67]. Patient positioning after injection can influence vector distribution through the CSF pathways, making this an important consideration for translational applications [66].
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for CNS Gene Delivery
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| AAV Serotypes | AAV1, AAV2, AAV5, AAV6, AAV8, AAV9, AAVrh.10 | Cell-type and route-specific transduction; AAV9 for widespread CNS delivery after IV or CSF administration; AAV6 for retrograde transport in neural circuits |
| Engineered Capsids | AAV-PHP.B, AAV-PHP.eB, AAVretro, AAV-F | Enhanced BBB penetration; Anterograde/retrograde neural circuit tracing; Cell-type specific targeting |
| Promoters | CAG (broad expression), Synapsin (neuronal), GFAP (astrocytic), MBP (oligodendrocytic) | Cell-type specific transgene expression within neural circuits |
| Reporters | GFP, mCherry, Luciferase, D2R80A (dopamine receptor mutant) | Visualization of transduction patterns; Quantification of expression levels; PET imaging (D2R80A) |
| Delivery Equipment | UltraMicroPump systems, Glass micropipettes, Hamilton syringes, Stereotaxic frames | Precise vector administration; Reproducible targeting of specific CNS regions |
Visualization of Experimental Workflows
Diagram 1: CNS Gene Delivery Route Selection Workflow
Diagram 2: CSF Delivery Route Comparison
The selection of an appropriate gene delivery modality is fundamental to the success of neural circuit manipulation experiments. Intracranial injection provides unparalleled precision for focal circuit interventions, intravenous delivery offers a less invasive approach for global CNS transduction with engineered vectors, and CSF routes balance invasiveness with broad distribution. Recent advances in AAV capsid engineering, promoter design, and delivery techniques continue to enhance the specificity and efficiency of CNS gene delivery. Researchers should carefully consider their experimental goals, target neural circuits, and required specificity when selecting a delivery approach. As the field progresses, continued refinement of these modalities will further enable precise manipulation of neural circuits for both basic research and therapeutic applications.
Navigating the Challenges: Immune Responses, Specificity, and Delivery Hurdles
Mitigating Immune Responses and Inflammation to AAV Vectors
Within the field of gene delivery strategies for neural circuit manipulation, adeno-associated virus (AAV) vectors have emerged as a cornerstone technology due to their ability to mediate stable, long-term transgene expression in the nervous system [17] [70]. A key advantage for neuroscience research is the availability of multiple AAV serotypes and engineered variants with distinct neural cell tropisms, enabling targeted manipulation of specific cell types and circuits [17] [70]. However, the efficacy and safety of AAV-based approaches are significantly challenged by host immune responses, which can lead to vector neutralization, loss of transgene expression, and neuroinflammatory toxicity [70] [71]. These immune reactions present substantial barriers to experimental reproducibility and the therapeutic translation of neural circuit findings. This Application Note provides a detailed framework for understanding and mitigating AAV immunogenicity, with specific protocols and tools tailored for researchers developing gene delivery strategies for neural circuit interrogation.
Immunogenicity of AAV Vectors: Mechanisms and Challenges
AAV vectors trigger a biphasic immune response involving both innate and adaptive immunity. The innate immune system is the first responder, recognizing AAV components as foreign through pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) and cytosolic DNA sensors [71]. TLR9, which detects unmethylated CpG dinucleotides in the AAV genome, is particularly implicated in initiating pro-inflammatory cytokine and type I interferon responses [71]. This innate activation subsequently primes the adaptive immune system, leading to the generation of cytotoxic T lymphocytes that can eliminate transduced cells, and B cells that produce neutralizing antibodies (NAbs) against the AAV capsid [71].
A critical consideration for experimental design is pre-existing immunity, as 30-60% of the human population possesses circulating anti-AAV antibodies from natural exposures [72]. These antibodies can neutralize systemically administered vectors, potentially confounding preclinical studies and clinical translation. Furthermore, the transgene product itself can be recognized as foreign, particularly in loss-of-function models where the protein is not expressed during immune development, leading to its immune-mediated clearance [71].
The route of administration significantly influences immunogenicity. Direct intracranial or intrathecal delivery partially restricts vector exposure to the systemic immune system compared to intravenous administration, which results in widespread biodistribution and greater immune recognition [71]. Understanding these mechanisms is fundamental to developing effective mitigation strategies.
Visualizing AAV-Induced Immune Pathways and Mitigation Strategies
The following diagram illustrates the key immune recognition pathways for AAV vectors and the strategic points for intervention, as discussed in the sections below.
Quantitative Data on AAV Seroprevalence and Immune Suppression
The tables below consolidate key quantitative data essential for planning in vivo studies, including the prevalence of pre-existing immunity and the efficacy of different immune suppression regimens.
Table 1: Pre-existing Neutralizing Antibody (NAb) Seroprevalence in Humans by Serotype and Region [72]
| AAV Serotype | Geographic Region | NAb Positivity (%) | Implication for Neural Targeting |
|---|---|---|---|
| AAV1 | United States (Wisconsin) | 32% | Consider for intramuscular or CNS delivery circuits. |
| AAV1 | United States (South Carolina) | 67% | High regional variability affects cohort selection. |
| AAV1 | Europe (Sweden) | 48% | Moderate prevalence. |
| AAV1 | Europe (Poland/Hungary) | 79% | Very high prevalence; pre-screening is critical. |
| AAV2/8 | Asia | Up to 72% | High prevalence may limit systemic use for CNS targeting. |
Table 2: Efficacy of B-Cell Focused Immune Suppression on AAV Re-administration [73]
| Immune Suppression (IS) Regimen | Initiation Timing | Key Findings | Impact on Transgene-Specific T Cells |
|---|---|---|---|
| None (Control) | N/A | Failed re-administration due to high NAb titers. | Baseline levels. |
| α-CD20, α-BAFF, or Rapa alone | Concurrent with AAV | Failed re-administration; exacerbated anti-capsid IgM. | Increased incidence in some groups (e.g., 75% with α-BAFF vs. 12% control). |
| α-CD20 + α-BAFF (Extended) | Before AAV & prolonged | Successful re-administration; abrogated prolonged anti-capsid IgM. | Prevented; enabled effective re-dosing and higher expression. |
Experimental Protocols
Protocol: B-Cell Targeted Transient Immune Suppression for AAV Re-dosing
This protocol describes a method for enabling effective AAV re-administration in a murine model by depleting B cells and suppressing their repopulation, based on the work of Rana et al. [73].
Application: This is particularly useful for longitudinal neural circuit studies requiring multiple AAV deliveries, such as sequential labeling of different neural populations.
Materials:
- Animals: C57BL/6 mice (or other relevant disease model).
- Immune Suppressants:
- Monoclonal antibody against CD20 (e.g., anti-mouse CD20).
- Monoclonal antibody against BAFF (e.g., anti-mouse BAFF).
- Control Groups: Isotype control antibodies.
- AAV Vectors: e.g., AAV8-OVA (2x10^9 vg/mouse) for initial dose and AAV8-hFIX (1x10^11 vg/mouse) for re-administration.
- Equipment: Flow cytometer, ELISA plates, reagents for immunohistochemistry.
Procedure:
- Pre-treatment: Initiate immune suppression 1-3 days before the first AAV administration.
- Administer a single dose of α-CD20 antibody (e.g., 250 µg per mouse, i.p.) to deplete circulating B cells.
- Administer the first dose of α-BAFF antibody (e.g., 500 µg per mouse, i.p.).
- Primary AAV Dosing: On day 0, administer the first AAV vector (e.g., AAV8-OVA via systemic or intracerebral route, depending on the experimental target).
- Prolonged BAFF Suppression: Continue α-BAFF antibody administration according to a defined schedule (e.g., twice weekly for 6-8 weeks) to slow B cell repopulation.
- Monitoring:
- B Cell Depletion: Verify >99% depletion of circulating B cells via flow cytometry (e.g., using B220 or CD19 markers) 2 days after α-CD20 injection.
- Immune Responses: At 4 weeks post-AAV, collect plasma to measure capsid-specific IgM and IgG by ELISA. Use tetramer staining to assess transgene-specific CD8+ T cell responses.
- Re-administration: At 8 weeks, administer the second AAV vector (AAV8-hFIX).
- Efficacy Assessment:
- Measure circulating levels of the transgene product (e.g., hFIX) 2-4 weeks after re-administration to assess success.
- Compare expression levels to naive animals that received only a single dose.
Troubleshooting:
- Failed Re-administration: Ensure IS is initiated before the first AAV dose and that BAFF suppression is maintained for a sufficient duration.
- High Transgene-Specific T Cells: Optimize the AAV dose to a level that favors tolerance over immunogenicity.
Protocol: Pre-Screening for Anti-AAV Antibodies Using High-Throughput Immunoassays
Robust pre-screening is essential for selecting appropriate animal models and for translational research. This protocol outlines steps for serum screening using ELISA or advanced automated platforms [74] [72].
Application: Ensuring baseline seronegativity in animal cohorts for CNS studies or screening human serum samples for clinical trial enrollment.
Materials:
- Samples: Animal or human serum/plasma samples.
- Kit: Anti-AAV Antibody ELISA Kit (serotype-specific) or Gyrolab Anti-AAVX Kit.
- Equipment: Microplate reader and washer (for ELISA) or Gyrolab automated system.
Procedure:
- Sample Preparation: Centrifuge samples to remove debris and lipids. Prepare recommended dilutions in the assay buffer.
- Assay Setup:
- ELISA: Load samples, controls, and standards onto the pre-coated plate. Follow kit instructions for incubation, washing, and detection steps.
- Gyrolab: Transfer samples to a microplate compatible with the automated system. The system handles subsequent steps.
- Cut-point Calculation: Establish a cut-point for determining sample positivity using a statistically relevant number of naive samples (e.g., 30-50). The cut-point is typically set as the mean signal of naive samples + 2 or 3 standard deviations.
- Validation (Confirmatory Assay): For samples near or above the cut-point, perform a confirmatory assay by pre-incubating the sample with an excess of free AAV capsid. A significant reduction in signal (% inhibition) confirms specificity.
- Data Analysis: Classify samples as positive or negative based on the validated cut-point.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Mitigating AAV Immunogenicity
| Reagent / Solution | Function / Application | Key Considerations |
|---|---|---|
| Anti-CD20 mAb | Depletes circulating B cells to prevent antibody production. | Timing is critical; administer before AAV. Efficacy of depletion should be verified by flow cytometry. |
| Anti-BAFF mAb | Blocks B cell activating factor, slowing B cell repopulation and maturation. | Essential for sustained effect; requires prolonged administration post-AAV dosing. |
| AAV Titration ELISA Kit | Precisely quantifies physical capsid titer (vg/mL) for consistent dosing. | Critical for quality control. Accurate dosing is key to balancing efficacy and immunogenicity [74]. |
| Anti-AAV Antibody ELISA Kit | Detects and quantifies total binding antibodies against specific AAV serotypes. | Useful for initial screening. Correlates with but does not exclusively measure neutralizing capacity [74]. |
| Gyrolab Anti-AAVX Kit | Automated, high-throughput immunoassay for anti-AAV antibody detection. | Requires lower sample volumes, offers increased efficiency and reproducibility for large-scale studies [72]. |
| mTOR Inhibitors (e.g., Rapamycin) | Broad immunosuppressant that can modulate T and B cell responses. | Can be combined with B-cell depletion; efficacy varies between species (e.g., mice vs. NHPs) [73]. |
Visualization of Pre-Screening and Immune Suppression Workflow
The following diagram outlines the core decision-making workflow for mitigating pre-existing and de novo immune responses in a preclinical AAV study.
Strategies for Enhancing Blood-Brain Barrier Penetration
The blood-brain barrier (BBB) represents a significant challenge for the development of therapeutics and gene delivery systems targeting the central nervous system (CNS). This highly selective membrane between the bloodstream and the nervous system restricts and regulates the entry of small molecules, with only an estimated 2% of biologically active small molecules able to cross the intact BBB to reach the brain at varying degrees [75]. For neurological diseases requiring gene therapy approaches, such as neurodegenerative diseases, the BBB presents a formidable obstacle that must be overcome to deliver therapeutic genetic material to specific neural circuits [17] [76]. This application note details current strategies and experimental protocols for enhancing BBB penetration, with particular emphasis on their application in neural circuit manipulation research.
Computational Prediction of BBB Permeability
In Silico Screening Approaches
Computational-aided drug development (CADD) has emerged as a powerful technique in early-stage drug discovery, offering the potential to screen active molecules and predict BBB permeability based on physicochemical and pharmacokinetic properties with higher predictability and clinical applicability [75]. These in silico approaches utilize machine learning models ranging from physicochemical properties to structure-activity relationships in CNS drug discovery pipelines to identify BBB-permeable molecules [75].
Table 1: Key Properties for BBB Permeability Prediction
| Property Category | Specific Parameters | Ideal Range for BBB Permeation |
|---|---|---|
| Lipophilicity | Partition coefficient (aLogP) | ~3.4 [77] |
| Molecular Size | Molecular weight | <400-600 Da [77] |
| Polarity | Polar surface area (tPSA) | <70 Ų [77] |
| Structural Features | Hydrogen bond donors/acceptors, rotatable bonds | H-bond donors ≤5, acceptors ≤10 [78] |
Advanced Machine Learning Models
Recent advances in artificial intelligence have significantly improved the accuracy of BBB permeability prediction. Transformer-based models like MegaMolBART, leveraging the SMILES representations of molecules, show great promise for applications in new drug discovery [79]. These models have demonstrated area under the receiver operating characteristic curve values of up to 0.88 on held-out test datasets, providing reliable predictions for BBB permeability [79].
The DeePred-BBB model, which applies deep neural networks to a dataset of 3,605 diverse compounds, has achieved prediction accuracies of 98.07% by encoding each compound with 1,917 features containing 1,444 physicochemical properties, 166 molecular access system fingerprints, and 307 substructure fingerprints [78].
Chemical and Biological Enhancement Strategies
Permeation Enhancers: Borneol as a Case Study
Borneol, a naturally occurring bicyclic monoterpene, has demonstrated significant potential as a BBB permeation enhancer. This traditional Chinese medicine compound has an 'orifice-opening' effect principally derived from opening the BBB through multiple mechanisms [80]:
- Modulation of ATP-binding cassette transporters including P-glycoprotein
- Regulation of tight junction proteins
- Enhancement of vasodilatory neurotransmitters
The BBB-opening effect of borneol is characterized as a reversible physiological process with rapid and transient penetration of the BBB and highly specific brain regional distribution [80]. The kinetics of borneol demonstrate its rapid absorption, with maximum concentration (Cmax) in the brain reached within 1 hour after dosing [80].
Table 2: Pharmacokinetic Parameters of Borneol Administration Routes
| Parameter | Intravenous | Intranasal | Oral |
|---|---|---|---|
| Plasma Cmax (μg/mL) | 68.0 ± 8.4 | 25.9 ± 5.0 | 15.6 ± 2.3 |
| Tmax (min) | 1.0 | 3.0 | 10.0 |
| AUC0–120 min (μg·mL⁻¹·min) | 632.3 ± 50.8 | 573.4 ± 77.7 | 271.8 ± 37.4 |
Experimental Protocol: Assessing BBB Permeability Enhancement with Borneol
Objective: To evaluate the BBB permeability enhancement effect of borneol on co-administered therapeutic compounds.
Materials:
- Test compound(s) of interest
- Borneol (natural or synthetic, purity ≥96%)
- Animal model (rat or mouse)
- LC-MS/MS system for quantification
- Surgical equipment for administration
Procedure:
- Prepare borneol solution in appropriate vehicle (e.g., saline with minimal DMSO)
- Administer borneol (dose range: 17-34 mg/kg for rodents) via selected route (oral, intranasal, or intravenous)
- Administer test compound at predetermined time points post-borneol administration
- Sacrifice animals at specified time intervals (e.g., 5, 15, 30, 60, 120 minutes)
- Collect blood samples via cardiac puncture and brain regions of interest
- Homogenize brain tissues and extract compounds using appropriate methods
- Quantify compound concentrations in plasma and brain homogenates using LC-MS/MS
- Calculate key pharmacokinetic parameters: Cmax, Tmax, AUC, brain-to-plasma ratio
Data Analysis: Compare pharmacokinetic parameters of test compounds with and without borneol co-administration. Statistical significance can be determined using Student's t-test or ANOVA with post-hoc analysis.
Mechanism of Borneol in Enhancing BBB Permeability
Advanced BBB Models for Permeability Assessment
Engineered Human BBB Microfluidic Model
Traditional in vitro BBB models have limitations in replicating the complex cellular architecture and functionality of the human BBB. Recent advances in microfluidic technology have enabled the development of more physiologically relevant models that incorporate human brain microvascular endothelial cells, pericytes, and astrocytes in a three-dimensional configuration [81].
Protocol: Engineered Human BBB Microfluidic Model
Device Fabrication (1.5 days):
- Generate microfluidic device molds using 3D printing or soft lithography
- Prepare polydimethylsiloxane (PDMS) mixture and pour onto molds
- Cure PDMS at 65°C for 4 hours, then peel off from molds
- Bond PDMS devices to glass coverslips using oxygen plasma treatment
- Sterilize devices using UV irradiation or autoclaving
Cell Culture and Device Seeding (7 days):
- Culture human brain microvascular endothelial cells (HBMECs), primary brain pericytes, and primary brain astrocytes separately
- Prepare cell suspension mixture at optimized ratios (e.g., 2:1:1 HBMECs:pericytes:astrocytes)
- Inject cell suspension into device central channel
- Allow cells to self-assemble into microvascular networks for 7 days with regular medium changes
- Confirm formation of intact vessels with tight junctions using immunofluorescence
Permeability Measurements (30 minutes per device):
- Prepare fluorescently tagged molecules of interest at physiological concentrations
- Perfuse molecules through the vascular channels using controlled flow rates
- Capture time-lapse images of fluorescence distribution
- Quantify fluorescence intensity in vascular and parenchymal regions
- Calculate permeability coefficients using established mathematical models
This BBB model features relevant cellular organization and morphological characteristics, with values of molecular permeability within the range expected in vivo (e.g., 1.7 × 10⁻⁷ cm/s for 10 kDa dextran) [81].
Viral Vector Strategies for Neural Circuit Manipulation
Double Viral Vector Technology for Selective Neural Targeting
For gene delivery strategies targeting specific neural circuits, double viral vector technology has emerged as a powerful approach for selective manipulation of neural pathways with higher levels of efficiency and safety [76]. This technique enables pathway-selective gene delivery by combining an injection of a retrograde transport viral vector into the projection area of the target neurons and an anterograde viral vector into their somas [76].
Table 3: Viral Vectors for Neural Circuit Manipulation
| Vector Type | Examples | Transport Characteristics | Applications |
|---|---|---|---|
| Anterograde | AAV1, AAV5, AAVDJ | Anterograde non-transsynaptic or transsynaptic | Mapping output networks |
| Retrograde | rAAV2retro, CAV-2, Lenti-FuG/E | Efficient axon terminal absorption | Mapping input networks |
| Transsynaptic | HSV1-H129, RVdG, PRV | Anterograde or retrograde transsynaptic spread | Complete circuit mapping |
Experimental Protocol: Double Viral Vector Transfection
Objective: To achieve selective gene delivery to specific neural circuits using double viral vector technology.
Materials:
- Retrograde viral vector (e.g., rAAV2retro-CAGGS-Cre)
- Anterograde viral vector (e.g., AAV5-EF1α-DIO-ChR2-EYFP)
- Stereotaxic apparatus
- Microinjection system (glass micropipettes, syringe pump)
- Animal model (rat or mouse)
Procedure:
- Anesthetize animal and secure in stereotaxic apparatus
- Inject retrograde viral vector (0.5 μL) into the projection area of target neurons at a flow rate of 100 nL/min
- Wait 2-3 days for retrograde transport to occur
- Inject anterograde viral vector (0.3 μL) into the soma location of target neurons
- Allow 3-6 weeks for gene expression and protein production
- Perfuse and fix brain tissue for analysis
- Verify specific gene expression in target circuits using immunohistochemistry
Key Considerations:
- Vector combinations must be optimized for specific pathways (e.g., rAAV2retro with AAV5 shows moderate transduction efficiency with low toxicity)
- Expression specificity is achieved through genetic elements (e.g., Cre-loxP system)
- Appropriate controls must be included to verify circuit specificity
Double Viral Vector Workflow for Selective Neural Circuit Targeting
Research Reagent Solutions
Table 4: Essential Materials for BBB Penetration and Neural Circuit Research
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| BBB Permeation Enhancers | Borneol, synthetic permeation enhancers | Temporary, reversible BBB opening for improved drug delivery |
| Viral Vectors | AAV serotypes (1, 5, DJ), rAAV2retro, HSV1-H129 | Gene delivery to specific neural cell types and circuits |
| Computational Tools | DeePred-BBB, MegaMolBART, molecular fingerprinting algorithms | In silico prediction of BBB permeability for compound screening |
| BBB Model Components | HBMECs, brain pericytes, astrocytes, microfluidic devices | In vitro assessment of BBB permeability in human-relevant systems |
| Genetic Tools | Cre-loxP system, DIO vectors, optogenetic/chemogenetic actuators | Precise manipulation and monitoring of neural circuit activity |
The strategies outlined in this application note provide researchers with multiple approaches to overcome the significant challenge of BBB penetration for neural circuit manipulation. Computational prediction methods enable rapid screening of candidate compounds, while chemical enhancers like borneol offer reversible modulation of BBB permeability. Advanced in vitro models bridge the gap between traditional cell culture and in vivo studies, and viral vector technologies enable unprecedented precision in targeting specific neural circuits. The integration of these approaches will accelerate the development of novel therapeutics and research tools for understanding and treating neurological disorders.
Minimizing Off-Target Effects in CRISPR-Based Neural Gene Editing
The precision manipulation of neural circuits using CRISPR-based gene editing holds transformative potential for neuroscience research and the treatment of neurological disorders. A central challenge in this endeavor is the mitigation of off-target effects—unintended modifications at genomic sites with sequence similarity to the target locus. These effects pose significant risks, including disruption of essential genes, genomic instability, and potential oncogenesis [82] [83]. This application note provides a structured framework of strategies and validation protocols to minimize off-target effects specifically within the context of neural circuit manipulation, enabling more reliable and interpretable experimental outcomes.
Mechanisms and Risks of Off-Target Activity
In CRISPR-Cas9 systems, off-target cleavage occurs when the Cas9 nuclease cuts DNA at sites other than the intended target. This primarily happens due to toleration of mismatches between the guide RNA (gRNA) and the target DNA, particularly in the seed region (the 8-12 nucleotides closest to the Protospacer Adjacent Motif or PAM) [82]. Other contributing factors include sequence homology in the genome, high GC content leading to Cas9 misfolding, and PAM-independent binding events [82]. In the context of neural circuits, where specific cell subtypes govern precise functions, off-target effects can confound experimental results by altering the function of non-targeted neurons or glia, potentially leading to misinterpretation of circuit mechanisms [47].
Strategic Framework for Minimizing Off-Target Effects
A multi-layered approach is essential to ensure high editing specificity in neural tissue. The following strategies can be systematically employed.
Selection of High-Fidelity Editing Tools
Moving beyond standard SpCas9 to engineered enzymes with enhanced specificity is a critical first step.
Table 1: High-Fidelity CRISPR Systems for Neural Gene Editing
| Editing System | Key Mechanism | Specificity Advantage | Best Use Cases in Neural Research |
|---|---|---|---|
| High-Fidelity Cas9 Variants (e.g., SpCas9-HF1, eSpCas9) | Engineered to reduce non-specific interactions with the DNA backbone [82]. | Up to 10-fold reduction in off-target events [83]. | General gene knockout in specific neural populations. |
| SuperFi-Cas9 | Redesigned protein with 4,000 times lower off-target activity [83]. | Dramatically reduced cleavage at mismatched sites. | Critical for targets with high genomic homology. |
| Cas9 Nickase | Cuts only one DNA strand; requires paired gRNAs for double-strand break [83]. | Significantly reduces unwanted mutations [83]. | When two highly specific target sites are proximate. |
| Altered PAM Specificity Cas9 (e.g., SaCas9) | Requires a more complex PAM sequence (NNGRRT) [83]. | Lower probability of random PAM occurrence, reducing off-target sites. | Accessing genomic regions with limited SpCas9 PAM sites. |
| Base Editors | Chemically converts one base to another without double-strand breaks [84] [85]. | Avoids DSB repair pathways, minimizing indels [85]. | Precision single-nucleotide conversion (e.g., disease modeling). |
| Prime Editors | Uses reverse transcriptase to write edited sequence from a pegRNA template [84] [85]. | Highest precision for small edits; no DSBs [85]. | Installing or correcting point mutations in neuronal genes. |
Optimization of Guide RNA (gRNA) Design
gRNA design is paramount for specificity. Key principles include:
- Specificity Screening: Use bioinformatics tools (e.g., CRISPOR, CHOPCHOP) to scan the reference genome and select gRNA sequences with minimal off-target sites, especially avoiding those with 3-5 base pair mismatches in the PAM-distal region [86] [83].
- Sequence Optimization: Maintain a gRNA length of 18-23 nucleotides. Truncated gRNAs ("tru-gRNAs") can increase specificity [84] [82]. Optimize GC content to 40-60% to balance stability and specificity [86].
- Chemical Modifications: Incorporate chemical modifications like 2'-O-methyl-3'-phosphonoacetate into the gRNA backbone to improve stability and reduce off-target cleavage [83].
Advanced Delivery Methods for Neural Circuits
The method and duration of editor delivery directly impact off-target rates.
- Ribonucleoprotein (RNP) Complex Delivery: Direct delivery of pre-assembled Cas9-gRNA complexes via electroporation leads to rapid editing and rapid degradation of the system in the cell, minimizing the window for off-target activity [83]. This method has shown higher on-target efficiency and lower off-target mutations compared to plasmid-based delivery [83].
- Novel Viral Vector Systems: Recent breakthroughs from the NIH BRAIN Initiative have produced a versatile set of adeno-associated virus (AAV) vectors capable of reaching specific neural cell types in the brain and spinal cord with exceptional accuracy [13] [48] [68]. These systems use cell-type-specific enhancers to restrict Cas9/gRNA expression to targeted neural subpopulations, thereby limiting off-target potential in non-target cells [13]. This is a significant advancement for precise neural circuit manipulation without requiring transgenic animals.
Diagram 1: Off-target mitigation workflow. This workflow integrates computational design and experimental profiling to minimize risks in neural gene editing.
Experimental Protocol for Off-Target Assessment and Validation
This protocol outlines a step-by-step process for designing, executing, and validating a CRISPR-based neural gene editing experiment with stringent off-target control.
Pre-Experimental Design and In Silico Analysis
- Target Identification: Define the genomic target based on prior QTL/GWAS data or functional hypotheses to narrow candidate sites [86].
- Editor Selection: Refer to Table 1 to select the most appropriate high-fidelity editor for your application (e.g., Base Editor for point mutations, SuperFi-Cas9 for knockouts).
- gRNA Design:
- Input the target sequence into bioinformatics tools like CRISPOR or GuideScan2 [86].
- Select 3-5 candidate gRNAs based on high on-target scores and low off-target potential.
- The tool will generate a list of potential off-target sites for each candidate gRNA across the genome for subsequent empirical validation.
Empirical Off-Target Profiling
Before proceeding to in vivo models, perform genome-wide off-target screening.
- Method Selection: Choose a sensitive, cell-based or cell-free method.
- GUIDE-seq: Genome-wide Unbiased Identification of DSBs Enabled by Sequencing. Detects double-strand breaks in cells by capturing integrated oligonucleotides [82].
- CIRCLE-seq: Circularization for In Vitro Reporting of Cleavage Effects by Sequencing. A highly sensitive in vitro method using purified genomic DNA [82] [83].
- Procedure for CIRCLE-seq: a. Genomic DNA Isolation: Purify high-molecular-weight genomic DNA from the target cell type or tissue (e.g., neuronal progenitor cells). b. DNA Shearing and Circularization: Fragment the DNA and ligate it into circular molecules. c. In Vitro Cleavage: Incubate the circularized DNA library with the pre-assembled RNP complex (your selected Cas9 variant and gRNA). d. Sequencing and Analysis: Break the DNA at cleavage sites, prepare a sequencing library, and sequence. Bioinformatically map the breaks to the reference genome to identify all potential off-target sites [82].
In Vivo Delivery and Validation in Neural Tissue
- Delivery:
- For RNP Delivery: Use electroporation for ex vivo editing of neural stem cells or primary neurons [83].
- For In Vivo Delivery: Utilize the latest AAV toolkits from the Armamentarium for Precision Brain Cell Access (e.g., Addgene). These AAVs are engineered with specific enhancers to target cortical subtypes, interneurons, or spinal cord neurons [13] [48].
- Validation:
- On-Target Efficiency: Amplify the target region via PCR from harvested neural tissue genomic DNA and analyze by Sanger sequencing or next-generation sequencing (NGS) to quantify editing efficiency [86].
- Off-Target Analysis: Use targeted amplicon sequencing to screen the top potential off-target sites identified in Section 4.2. For a broader assessment, methods like DISCOVER-Seq can be applied to identify off-targets directly in tissues [83].
Table 2: Key Reagents for Off-Target Minimization in Neural Editing
| Reagent Category | Specific Example | Function/Application |
|---|---|---|
| High-Fidelity Nucleases | SpCas9-HF1, SuperFi-Cas9, SaCas9 [83] | Engineered protein variants for reduced off-target cleavage. |
| Precision Editors | ABE8e (Adenine Base Editor), PE2 (Prime Editor) [87] [85] | Enable single-base changes or small insertions/deletions without double-strand breaks. |
| Targeted AAV Serotypes | BRAIN Initiative AAV Toolkit (e.g., for prefrontal cortex, striatum, spinal cord) [13] [68] | Deliver genetic payloads to specific neural cell types with high precision. |
| Bioinformatics Tools | CRISPOR, GuideScan2, DeepMEns [87] [86] | Predict gRNA efficiency and potential off-target sites during design. |
| Off-Target Detection Kits | GUIDE-seq, CIRCLE-seq, SITE-Seq [82] [83] | Empirically identify off-target cleavage sites genome-wide. |
Diagram 2: Strategic pillars for off-target minimization. The four core strategies contribute through distinct mechanisms to achieve the final goal of specific neural circuit manipulation.
The successful application of CRISPR-based gene editing in neural circuit research is critically dependent on the rigorous control of off-target effects. By integrating the strategic selection of high-fidelity editors, computationally optimized gRNAs, advanced delivery systems like the latest AAV toolkits, and thorough empirical validation, researchers can significantly enhance the specificity and reliability of their experiments. This multi-faceted approach, as outlined in this application note, provides a robust pathway toward precise genetic manipulation of neural circuits, thereby enabling more accurate functional studies and accelerating the development of safer genetic therapies for neurological disorders.
Overcoming Transduction Barriers for Challenging Cells like Microglia
Microglia, the resident immune cells of the central nervous system (CNS), play crucial roles in brain development, homeostasis, and neurodegenerative diseases [88] [89]. Their ability to dynamically sculpt neural circuits and orchestrate immune responses makes them prime targets for genetic manipulation in neural circuit research [90]. However, achieving efficient gene delivery in microglia has remained a significant challenge due to their unique resistance to conventional transduction methods and their highly dynamic activation states [91] [88].
The refractory nature of microglia to genetic manipulation stems from several biological barriers. As professional phagocytes, microglia efficiently recognize and clear foreign particles, including viral vectors [88]. Additionally, their heterogeneous functional states—ranging from homeostatic to disease-associated phenotypes—further complicate the development of universal transduction strategies [92] [89]. The blood-brain barrier presents an additional obstacle for in vivo applications, limiting vector access to CNS targets [88]. This application note details recent breakthroughs in overcoming these barriers, with a focus on practical implementation for neural circuit manipulation studies.
Advanced AAV Capsid Engineering for Microglia Targeting
Directed Evolution of Microglia-Tropic AAV Variants
Directed evolution of AAV capsids has emerged as a powerful strategy for generating microglia-tropic vectors. A landmark study employed this approach to develop AAV-cMG and AAV-MG variants capable of mediating efficient in vitro and in vivo microglial transduction [90]. These engineered variants demonstrate remarkable efficiency in delivering genetic payloads to microglia, enabling sufficient transgene expression to support advanced applications including fluorescent labeling, Ca2+ and neurotransmitter imaging, and in vivo genome editing [90].
A critical advantage of these evolved capsids is their ability to transduce microglia without inducing immune activation. Single-cell RNA sequencing analysis confirmed that AAV-MG variants mediate in vivo transgene delivery while maintaining microglial homeostasis, a crucial consideration for neural circuit studies where inflammatory responses could confound experimental results [90]. This preservation of native microglial state distinguishes these vectors from previous attempts that often triggered unwanted immune activation.
Environmentally Optimized AAV2/6 Capsids
The retinal model system has provided valuable insights into environmental influences on microglial transduction. Research demonstrates that AAV2/6 can transduce microglia in retinal synaptic layers, with layer preference corresponding to the delivery method (intravitreal or subretinal) [91]. Surprisingly, microglial transduction efficiency significantly enhanced during photoreceptor degeneration, suggesting that disease states can improve vector uptake [91].
To capitalize on this finding, researchers developed an optimized AAV6 capsid containing four point mutations (K531E, R576Q, K493S, and K459S) that reduce heparin binding [91]. This modification resulted in increased microglial transduction in the outer plexiform layer, demonstrating how strategic capsid engineering can overcome biological barriers. The enhanced performance in degenerative environments suggests these vectors may be particularly useful for studying microglial responses in injury or disease models relevant to neural circuit dysfunction.
Table 1: Engineered AAV Capsids for Microglia Transduction
| Capsid Variant | Development Method | Key Features | Validated Applications | Reference |
|---|---|---|---|---|
| AAV-cMG/AAV-MG | Directed evolution | High efficiency, no immune activation | Fluorescent labeling, Ca2+ imaging, genome editing | [90] |
| AAV2/6 (4x mutant) | Rational design (point mutations) | Reduced heparin binding, enhanced OPL transduction | Retinal studies, degeneration models | [91] |
| rAAV2 | Natural serotype | Efficient cultured microglia transduction | IL-15 expression for glioma therapy | [88] |
| TM6 (modified rAAV6) | Capsid modification + promoter | Microglia-specific expression, crosses BBB | Pro-inflammatory cytokine expression | [88] |
Critical Validation Considerations for Novel Capsids
Recent findings highlight the importance of rigorous validation for newly proposed microglia-targeting capsids. The AAV-MG1.2 capsid, initially reported as microglia-specific, was subsequently shown to primarily target forebrain excitatory neurons in hippocampal formation and visual cortex, with no detectable microglial expression [93]. This discrepancy underscores the necessity of thorough cross-laboratory validation for any proposed microglia-targeting vector, particularly when applying them to neural circuit manipulation studies where cell-type specificity is paramount.
Experimental Protocols for Microglia Transduction
In Vivo Microglia Transduction Using Engineered AAVs
Materials Required:
- Engineered AAV capsid (AAV-cMG, AAV-MG, or optimized AAV2/6)
- Appropriate microglia-specific promoter (e.g., F4/80, CD68, or Cx3cr1)
- Sterile surgical instruments
- Stereotactic apparatus
- Anesthesia equipment
- Microinjection pump and calibrated glass capillaries
Procedure:
- Vector Preparation: Purify AAV vectors using affinity chromatography and dialyze against sterile PBS. Determine viral titer (typically ≥ 1×10¹³ vg/mL) using qPCR.
- Surgical Setup: Anesthetize the animal and secure in stereotactic frame. Maintain body temperature at 37°C throughout procedure.
- Brain Injection: Identify target coordinates (e.g., hippocampus: AP -2.0 mm, ML ±1.7 mm, DV -1.9 mm from bregma). Load viral suspension (1-2 μL per site) into injection capillary.
- Vector Delivery: Lower capillary to target depth and infuse at 100 nL/min using microinjection pump. Allow 5-10 minutes for diffusion before slowly retracting capillary.
- Post-operative Care: Monitor animals until recovery from anesthesia. Allow 2-4 weeks for transgene expression before analysis.
Critical Parameters:
- Optimal microglial transduction requires specific promoters such as F4/80 or CD68 in combination with engineered capsids [88].
- For retinal transduction, subretinal injection targets outer plexiform layer microglia, while intravitreal delivery targets inner retinal microglia [91].
- A titer-dependent response has been observed with some capsids, requiring optimization for each experimental system [93].
In Vitro Microglia Transduction and Engineering
Materials Required:
- Primary microglia cultures or iPSC-derived microglia-like cells
- Recombinant AAV vectors (rAAV2, rAAV6, or engineered variants)
- Polycistronic TF expression cassettes (for reprogramming)
- Appropriate culture media and transfection reagents
Procedure for Microglia Generation (TFiMGL Protocol):
- iPSC Preparation: Culture human iPSCs in essential 8 medium on vitronectin-coated plates until 70-80% confluent.
- TF Transfection: Transfect with polycistronic vector expressing SPI1, CEBPA, FLI1, MEF2C, CEBPB, and IRF8 using appropriate transfection method.
- Differentiation Induction: Add doxycycline (1 μg/mL) to induce TF expression for 4 days.
- Validation: Assess microglial markers (CX3CR1, P2RY12, CD11b) via flow cytometry at day 4.
- Transduction: Apply engineered AAV vectors to differentiated microglia at MOI 10⁴-10⁵ for 24-48 hours.
Functional Validation:
- Confirm phagocytic capability using pHrodo-labeled beads or synaptosomes
- Assess inflammatory responses to LPS stimulation (TNF-α, IL-6 secretion)
- Validate electrophysiological properties where relevant
Figure 1: Rapid Generation of Engineered Microglia from iPSCs. This workflow enables production of microglia-like cells within 4 days using a six transcription factor combination, followed by AAV transduction for genetic manipulation.
Research Reagent Solutions for Microglia Studies
Table 2: Essential Research Reagents for Microglia Transduction Studies
| Reagent Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Engineered AAV Capsids | AAV-cMG, AAV-MG, TM6 (modified AAV6) | Efficient microglia transduction in vivo and in vitro | [90] [88] |
| Microglia-Specific Promoters | F4/80, CD68, Cx3cr1, TMEM119 | Drive transgene expression specifically in microglia | [88] |
| Reprogramming Transcription Factors | SPI1, CEBPA, FLI1, MEF2C, CEBPB, IRF8 | Rapid generation of microglia from iPSCs (TFiMGL protocol) | [94] |
| Microglial Markers | Iba1, P2RY12, CX3CR1, TREM2 | Identification and validation of microglial identity | [95] [89] |
| Detection Tools | YOLOv3 deep learning algorithm | Automated microglia detection and quantification in tissue sections | [95] |
Microglia-Targeting Strategies for Neural Circuit Research
Cell-Type Specific Targeting Approaches
Achieving microglia-specific transgene expression requires combinatorial strategies involving engineered capsids and cell-specific regulatory elements. The most successful approaches combine:
- Modified Capsids: Engineered AAV variants with enhanced tropism for microglial surface receptors [90] [91].
- Microglial Promoters: Specific promoters such as F4/80, CD68, or Cx3cr1 that restrict expression to microglial lineages [88].
- Cre-Dependent Systems: Using Cx3cr1-CreERT2 mouse lines with Cre-dependent AAV vectors for enhanced specificity [91].
The Cx3cr1 promoter has been particularly valuable for targeting microglia in neural circuit studies, though recent evidence suggests it may also label peripheral macrophages in certain contexts [96]. Newer markers like TMEM119 and Sall1-based genetic lines offer improved specificity for CNS-resident microglia [96].
Signaling Pathways in Microglial Manipulation
Key molecular pathways regulate microglial functions that are relevant to neural circuit manipulation. Understanding these pathways enables more precise experimental design:
- TREM2 Signaling: Regulates microglial phagocytosis, survival, and lipid metabolism; enhanced TREM2 signaling improves clearance of protein aggregates in neurodegenerative models [92].
- CX3CR1/Fractalkine: Critical for microglia-neuron communication and synaptic pruning; disruption affects circuit refinement and plasticity [96].
- P2Y12 Receptors: Mediate microglial process extension toward injury sites; important for rapid response to neural damage [89].
Figure 2: Key Signaling Pathways for Microglial Manipulation. Targeting TREM2, P2Y12, and CX3CR1 pathways allows precise control of microglial functions relevant to neural circuit studies.
The field of microglial transduction has advanced significantly through directed evolution of AAV capsids and optimization of delivery parameters. The development of vectors like AAV-cMG/MG and modified AAV2/6 variants now enables efficient gene delivery to these challenging cells, opening new possibilities for studying microglial functions in neural circuit formation, maintenance, and dysfunction.
Future directions will likely focus on enhancing the specificity of these tools through more refined promoter systems and additional capsid engineering. The integration of single-cell omics technologies with high-throughput screening approaches will further accelerate the development of next-generation microglia-targeting vectors [92] [94]. As these tools become more sophisticated, they will undoubtedly provide unprecedented insights into how microglia shape neural circuits in health and disease.
For researchers implementing these protocols, careful attention to capsid selection, promoter design, and delivery method is essential. The rapid progress in this field promises to dissolve longstanding barriers to microglial manipulation, finally enabling comprehensive genetic access to these crucial CNS immune cells.
Optimizing Titer and Injection Parameters for Robust In Vivo Expression
Within gene delivery strategies for neural circuit manipulation, achieving robust and specific in vivo expression is a cornerstone for both investigative and therapeutic applications. This goal hinges on the precise optimization of two critical, interdependent factors: the viral titer and the physical injection parameters. The selection of a delivery vehicle, such as an adeno-associated virus (AAV) serotype with a specific cellular tropism, must be strategically paired with a promoter that ensures expression is restricted to the target cell population (e.g., neurons). Furthermore, the practical execution of the injection—encompassing speed, volume, and surgical technique—directly governs the distribution and transduction efficiency within the desired brain region. This protocol details a systematic approach to optimizing these parameters to ensure high penetrance and specificity of transgene expression for manipulating neural circuits.
Optimizing the Viral Vector and Promoter
The foundational step for successful gene delivery is selecting the appropriate combination of viral serotype and promoter. This combination determines which cells are infected and which cells express the transgene.
Key Experimental Protocols
Serotype and Promoter Comparison Protocol: To empirically determine the optimal vector for a specific neural target, a comparative study should be conducted as follows [97]:
- Vector Preparation: Package a reporter gene (e.g., GFP) into a panel of AAV serotypes (e.g., AAV1, AAV2, AAV6, AAV8, AAV9) using both a ubiquitous promoter (e.g., CMV) and a cell-specific promoter (e.g., synapsin for neurons, GFAP for astrocytes, or TH for dopaminergic neurons).
- In Vivo Injection: Stereotactically inject each vector into the target brain region of animal models (e.g., mouse or non-human primate). Standardize the injection volume and speed across all test conditions.
- Tissue Processing and Analysis: After a suitable expression period (e.g., 3-6 weeks), perfuse and section the brain.
- Immunohistochemistry: Stain brain sections for cell-specific markers (e.g., NeuN for neurons, GFAP for glia) and the reporter transgene.
- Quantification: Use fluorescence microscopy to count the number of cells double-labeled for the reporter and the cell marker to calculate penetrance (percentage of target cells expressing the transgene) and specificity (percentage of reporter-positive cells that are of the target type).
Quantitative Data and Recommendations
Table 1: Comparison of AAV Serotypes and Promoters for Neural Targeting
| AAV Serotype | Promoter | Reported Penetrance in Neurons | Specificity | Key Characteristics and Recommendations |
|---|---|---|---|---|
| AAV2 | Synapsin | ~41% (in monkey cortex) [97] | High (Neuronal) [97] | Well-defined expression spread (2-4 mm from injection site); suitable for confined cortical targeting [97]. |
| AAV6 | Synapsin | ~36% (in monkey cortex) [97] | High (Neuronal) [97] | Similar neuronal specificity and penetrance to AAV2 [97]. |
| AAV9 | cTnT (Cardiac) | >85% (in mouse cardiomyocytes) [98] | >640-fold heart vs. liver [98] | Highly efficient crossing of endothelial barriers; broad tissue tropism requires cell-specific promoters for neural applications. |
| Lentivirus | CMV | Low in neurons, high in glia [97] | Low (Primarily Glial) [97] | The CMV promoter in lentivirus context preferentially transduces glial cells in the primate brain. |
| Lentivirus | Synapsin | High (in monkey cortex) [97] | High (Neuronal) [97] | Suitable for high, neuron-specific expression across all cortical layers with a single injection [97]. |
Optimizing Injection Parameters and Titer
The physical delivery of the viral vector is as critical as its genetic design. Injection parameters directly control the spatial extent and cellular density of transduction.
Key Experimental Protocols
Injection Parameter Optimization Protocol: To define the parameters that yield the desired coverage and expression strength, a systematic approach is recommended [97]:
- Parameter Survey: Inject a standardized AAV vector (e.g., AAV2-synapsin-GFP) into the target region while varying:
- Volume: Test a range (e.g., 1 µL to 5 µL).
- Speed: Test a range (e.g., 100 nL/min to 2000 nL/min).
- Titer: Use the same viral prep at a standardized titer (e.g., 10¹³ particles/mL).
- Spread Analysis: After expression, analyze the volume of tissue expressing GFP. Measure the radial spread from the injection site.
- Quantitative Relationship: Establish the inverse relationship between injection speed and tissue spread: slower injections yield larger distribution volumes per unit volume injected [97].
Poisson-Based Titer Estimation Protocol: The required viral load can be modeled to achieve a specific transduction goal [98]:
- Dose-Response: Inject a series of viral particle doses into the target region (e.g., (3.15 \times 10^9), (1 \times 10^{10}), (3.15 \times 10^{10}) vp/mouse).
- Single-Cell Analysis: Quantify transgene expression (e.g., eGFP fluorescence intensity) on a cell-by-cell basis.
- Model Fitting: Fit the distribution of expression levels to a Poisson distribution. The study on cardiomyocytes revealed that an average of nearly two vector genomes per cell are required to achieve 85% transduction efficiency [98].
Quantitative Data and Recommendations
Table 2: Optimization of Injection Parameters and Titer
| Parameter | Tested Range | Optimal Value / Finding | Impact on Expression |
|---|---|---|---|
| Injection Speed | 100 - 2000 nL/min [97] | 500 nL/min (recommended) [97] | Inverse relationship with spread. Slower speeds yield larger, more uniform coverage relative to volume injected [97]. |
| Injection Volume | 1 - 5 µL [97] | 2 µL (good compromise) [97] | Larger volumes cover larger areas; optimal volume depends on target size and number of injection sites. |
| AAV Titer (Particles/mL) | (10^{12} - 10^{13}) | (3.15 \times 10^{10}) vp/mouse achieved 96% transduction [98] | Higher titer increases probability of cell infection. Model load using Poisson distribution (target ~2 genomes/cell for >85% efficiency) [98]. |
| Number of Injection Sites | N/A | Multiple sites for large/irregular areas [97] | Required to achieve uniform coverage in large or anatomically complex structures like the cortical sheet. |
Integrated Workflow for Robust In Vivo Expression
The following workflow synthesizes the optimization of viral vectors, promoters, and injection parameters into a single, coherent experimental pathway.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for In Vivo Gene Delivery
| Item / Reagent | Function / Description | Example Application |
|---|---|---|
| AAV Serotypes (1, 2, 6, 8, 9) | Viral vectors with differing cellular tropism and spread characteristics. | AAV2 for confined cortical expression; AAV9 for highly efficient transduction across barriers [98] [97]. |
| Cell-Specific Promoters | DNA sequences that restrict transgene expression to specific cell types. | Synapsin for pan-neuronal expression; Tyrosine Hydroxylase (TH) for dopaminergic neurons [97]. |
| Lipid Nanoparticles (LNPs) | Non-viral delivery vehicle for encapsulating and delivering nucleic acids (DNA, mRNA, RNP). | Emerging alternative to viral vectors, offering reduced immunogenicity concerns [99]. |
| Stereotactic Frame & Pump | Precision apparatus for targeting specific brain coordinates and controlling injection flow rate. | Essential for reproducible intracranial delivery of viral vectors at recommended speeds (e.g., 500 nL/min) [97]. |
| Immunohistochemistry Antibodies | Labels for identifying specific cell types and quantifying transgene co-expression. | Anti-NeuN to label neurons; anti-GFAP to label astrocytes; anti-GFP to detect reporter [97]. |
Bench to Bedside: Validating Tools and Comparing Therapeutic Platforms
In modern neuroscience research, the manipulation of neural circuits via gene delivery strategies requires robust functional validation to confirm intended molecular, cellular, and behavioral outcomes. The integration of electrophysiological recordings, calcium imaging, and behavioral phenotyping forms a critical triad for comprehensively assessing the functional consequences of genetic interventions. These methodologies enable researchers to bridge the gap between genetic manipulation and its impact on ion channel function, cellular excitability, network dynamics, and ultimately, organism-level behavior. The development of sophisticated gene delivery systems, such as the novel adeno-associated virus (AAV) vectors from the NIH BRAIN Initiative, allows for unprecedented cell-type-specific targeting [13] [48]. This technological advancement makes rigorous functional validation not merely advantageous but essential for accurately interpreting the outcomes of neural circuit manipulation experiments. This document provides detailed application notes and standardized protocols for implementing these key validation methodologies within the context of gene delivery research.
Electrophysiology for Validating Neural Circuit Manipulation
Electrophysiology serves as a direct method for quantifying changes in neuronal excitability and synaptic function following genetic manipulation. The selection of an appropriate technique depends on the specific research question, ranging from single-channel analysis to network-level activity assessment.
High-Throughput Automated Patch-Clamp Electrophysiology
For high-throughput functional analysis of ion channels—a critical consideration when validating effects of gene delivery on neuronal excitability—automated patch-clamp (APC) systems have transformed the field.
- Primary Role: APC enables rapid, quantitative measurement of ion channel function (kinetics, voltage dependence) in high-volume settings [100]. This is particularly valuable for characterizing functional defects caused by ion channel mutations or for screening compounds in neuronal cells derived from iPSCs following genetic modification.
- Workflow: The process involves automated cell dispensing, Gigaohm seal formation, and rapid solution exchange, facilitating robust concentration-response curve generation and voltage-dependent inactivation studies [100].
- Quality Control: Implementing strict quality control metrics, such as monitoring seal resistance and series resistance drift, is essential to ensure the electrophysiological integrity of recorded currents and the reliability of data used to predict functional outcomes of genetic manipulation [100].
Optical Mapping for Network-Level Electrophysiological Assessment
While patch-clamp focuses on single-cell properties, optical mapping provides a holistic view of electrical propagation across neural networks or intact brain circuits.
- Technique Principle: This method employs voltage-sensitive dyes (VSDs) combined with high-speed, high-resolution cameras to capture spatiotemporal dynamics of electrical activity [100]. It is indispensable for visualizing complex network dynamics following circuit-specific manipulations.
- Key Protocol Considerations:
- Motion Artifacts: Use mechanical uncouplers, such as blebbistatin, which inhibit myosin II activity without significantly altering the VSD signal [100].
- Dye Selection: Voltage dyes (e.g., Di-4-ANEPPS) must be photo-stable and efficiently incorporated into the membrane [100].
- Signal Processing: Raw optical signals require filtering to remove noise and normalization to account for non-uniform dye loading [100].
Table 1: Key Analysis Metrics in Optical Mapping for Neural Circuit Studies
| Parameter Analyzed | Importance in Neural Circuit Research |
|---|---|
| Conduction Velocity | Quantifies tissue excitability and the speed of signal propagation within a circuit. |
| Action Potential Duration (APD) | Measures neuronal repolarization dynamics; altered in various channelopathies. |
| Activation Maps | Visualizes the temporal sequence and spatial pattern of impulse conduction across a neural network. |
Stimulation Protocol Design
Choosing the correct stimulation protocol is fundamental to probing specific electrical properties.
- Voltage Clamp: Holds the membrane potential at a specific voltage and measures the resulting current. Ideal for studying the properties of expressed ion channels and their modulation [101].
- Current Clamp: Injects a specific current into a cell and measures the resulting change in membrane potential. Used for studying intrinsic excitability and synaptic integration [101].
The decision-making process for selecting an appropriate electrophysiology method can be visualized as follows:
Calcium Imaging for Functional Circuit Interrogation
Calcium imaging serves as a powerful proxy for neuronal activity, allowing researchers to monitor the dynamics of large populations of neurons simultaneously, which is highly valuable for assessing the efficacy and functional outcomes of gene delivery in neural circuits.
Intracellular Calcium Imaging Protocol for Agonist Screening
This protocol is adapted for validating chemogenetic (e.g., DREADD) or optogenetic actuator function in transfected neurons by measuring calcium flux in response to ligand application [102] [103].
Required Materials
- Cells: Cultured neuronal cells (e.g., primary neurons, iPSC-derived neurons), transiently transfected with your gene of interest and/or calcium indicator [102].
- Reagents:
- Hanks’ Balanced Salt Solution (HBSS)
- Fluo-4, AM (a calcium-sensitive dye)
- Pluronic F-127 (a dispersing agent)
- DMSO
- Agonists/Ligands relevant to your gene delivery strategy (e.g., acetylcholine, glutamate, or specific ligands for engineered receptors) [103].
- Tools and Equipment:
- Inverted microscope (e.g., Nikon T2000)
- High-speed illumination system (e.g., Sutter Instruments Lambda DG-4)
- Digital camera (e.g., Hamamatsu ORCA-ER)
- Software for data acquisition and analysis (e.g., MetaFluor) [103].
Step-by-Step Methodology
- Preparation of Fluo-4 AM Loading Solution:
- Reconstitute fluo-4 AM by adding 44 µL of DMSO to one vial (50 µg) and vortex thoroughly.
- Add 9 µL of Pluronic F-127 to the reconstituted fluo-4 AM and vortex. This agent is critical for dispersing the AM ester in aqueous solution.
- Add 50 µL of this ~860 µM fluo-4 AM/Pluronic F-127 solution to 14.3 mL of HBSS to create the working loading solution. Use this solution immediately [103].
Loading Cells with Fluo-4 AM:
- Wash the neuronal cells once with 100 µL of HBSS.
- Incubate the cells with 100 µL of the fluo-4 AM loading solution per well of a 96-well plate in the dark at room temperature for approximately 60 minutes.
- After incubation, wash the cells with 100 µL of HBSS to remove excess dye and maintain in the dark until data acquisition [103].
Data Acquisition:
- Place the plate on an inverted microscope. Define regions of interest (ROIs) around 50-100 transfected neurons for analysis.
- Excite the fluo-4 dye with 488-nm light and collect emitted light at 520 nm.
- Challenge the cells by adding the ligand or agonist. For example, add 20 µL of 3 mM acetylcholine to achieve a final concentration of 500 µM in the well [103]. The concentration will depend on the receptor being targeted.
- Collect time-lapse image data using appropriate software before, during, and after ligand application.
Data Analysis:
- Integrate the fluorescence intensity for each ROI over time.
- Normalize the signal (F/F₀), where F is the fluorescence at time t and F₀ is the baseline fluorescence (average of the first ten data points) [103].
- Plot the normalized fluorescence against time. A neuron is typically considered responsive if the normalized signal increases by more than 10% within 60 seconds of agonist addition compared to baseline [103].
The workflow for this calcium imaging assay is outlined below:
Behavioral Assays for Phenotypic Validation
Behavioral assays provide the ultimate functional readout of neural circuit manipulation, linking molecular and cellular changes to alterations in organism-level function. Rigorous experimental design is paramount for generating reliable and reproducible data.
Foundational Principles for Behavioral Testing
The following pillars of reproducibility must be integrated into the experimental design of any behavioral validation study [104].
- Blinding: The technician conducting behavioral evaluations and analyzing data must be unaware of the treatment groups (e.g., control vector vs. experimental gene delivery vector) to eliminate unconscious bias. If complete blinding is impossible, an independent researcher should perform the final interpretation [104].
- Randomization and Counterbalancing: Animals must be randomly assigned to treatment groups. Furthermore, testing should be counterbalanced across time of day, testing apparatus, and experimenter to distribute unknown confounding variables evenly [104].
- Controls: For gene delivery studies, control groups are critical. These should include animals treated with a control vector (e.g., empty vector or vector expressing a fluorescent protein only) and should be handled identically to the experimental group. This controls for the effects of the surgical procedure and viral injection itself [104].
- Sample Size: Group sizes of 10-20 animals per sex per genotype/treatment are typically the minimum required to achieve statistical significance in behavioral assays, based on power analyses. Pilot studies can be used to determine the appropriate sample size for a given effect [104].
- Technical Proficiency: Technicians must be trained to a level of proficiency where they can reliably reproduce established behavioral phenotypes or pharmacological effects (e.g., the effect of a known anxiolytic like diazepam in an anxiety assay) before testing experimental animals [104].
The Gold Standard: Functional Analysis in Behavioral Assessment
When validating behaviors relevant to neurological or neuropsychiatric disorders, the most rigorous approach involves determining the function of the behavior.
- Functional Behavioral Assessment (FBA): This is a suite of methods used to identify the environmental factors that maintain a challenging or atypical behavior.
- Functional Analysis (FA): This is the gold-standard component of FBA, as it is the only method that can demonstrate a causal relationship between a specific environmental consequence and the behavior [105]. It involves systematically manipulating antecedents and consequences in a controlled setting.
- Comparative Effectiveness: While functional analyses are the benchmark, other FBA methods (indirect assessments and descriptive assessments) are more commonly used in practice due to feasibility, though they show only modest correspondence with FA results. Treatment based on FA results, however, is highly effective, with studies showing that functional communication training (FCT) based on FA results successfully reduces challenging behavior [105].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful functional validation relies on a core set of reliable reagents and tools. The table below details key solutions for the experiments described in this document.
Table 2: Key Research Reagent Solutions for Functional Validation
| Reagent / Tool | Function / Application | Example & Notes |
|---|---|---|
| AAV Vector Toolkit [13] [48] | Cell-type-specific gene delivery in brain and spinal cord. | NIH BRAIN Initiative collection; targets excitatory neurons, interneurons, cortical subtypes, etc. |
| HiRet/NeuRet Vectors [47] | Retrograde gene transfer for specific neural pathway manipulation. | Lentiviral vectors for labeling or manipulating projection-specific neurons. |
| Voltage-Sensitive Dyes (VSDs) [100] | Optical mapping of electrical activity propagation in neural tissue. | e.g., Di-4-ANEPPS; requires matching excitation light source and motion suppression. |
| Calcium Indicator Dyes [103] | Real-time monitoring of neuronal activity via calcium flux. | e.g., Fluo-4 AM; requires Pluronic F-127 for loading and proper imaging setup. |
| Genetically Encoded Calcium Indicators (GECIs) [102] | Long-term, cell-specific calcium imaging in transfected cells. | e.g., GCaMP series; allows for activity monitoring in defined neuronal populations. |
| Mechanical Uncouplers [100] | Suppress tissue movement artifact in optical mapping. | e.g., Blebbistatin; inhibits myosin II without significantly altering electrical signals. |
Integrated Data Analysis and Computational Modeling
The complex, high-dimensional data generated by these functional validation techniques require sophisticated analytical approaches.
- Activation Mapping: Specialized software can reconstruct the temporal sequence of electrical activation across a neural network, producing isochronal maps that are critical for pinpointing the origin of ectopic activity or defining propagation patterns following circuit manipulation [100].
- Power Spectrum Analysis (PSA): For studying oscillatory network activity or seizure-like events, PSA involves applying a Fast Fourier Transform (FFT) to electrograms. The dominant frequency provides a quantitative measure of the rate and organization of network activity [100].
- Computational Modeling: Biophysically detailed computer models of neurons and neural circuits integrate data on ion channel kinetics, synaptic properties, and network structure. These models can be used to test hypotheses about the mechanisms by which a genetic manipulation alters circuit function in silico, providing a powerful complement to empirical data [100].
- Action Potential Duration (APD) Restitution Analysis: This is a crucial metric for assessing neuronal stability, plotting APD as a function of the preceding diastolic interval. A steep restitution slope (>1) indicates increased instability and a higher risk of aberrant activity, which could be relevant in studies of hyperexcitability disorders [100].
Comparative Analysis of AAV-CRISPR vs. RNAi for Gene Regulation in the Brain
The advent of sophisticated gene regulation technologies has revolutionized the study and therapeutic targeting of neurological disorders. Adeno-associated virus (AAV) vectors have emerged as the premier delivery platform for genetic cargo to the nervous system due to their low immunogenicity, stable episomal persistence, and ability to transduce non-dividing neurons [106] [107] [17]. Within this framework, two powerful strategies for gene silencing—AAV-delivered CRISPR-based systems and RNA interference (RNAi)—offer distinct mechanisms, advantages, and challenges for modulating gene expression in the brain. This analysis provides a comparative evaluation of these platforms, focusing on their application in neural circuit manipulation research.
The fundamental distinction lies in their target and mechanism: CRISPR systems, particularly those utilizing nuclease-null Cas9 (dCas9) repressors or RNA-targeting Cas13, can achieve DNA-level epigenetic silencing or RNA degradation, respectively [108] [109] [110]. In contrast, RNAi, including shRNA and antisense oligonucleotides (ASOs), functions primarily through post-transcriptional mRNA degradation or blockade [106]. The choice between these modalities impacts the permanence, specificity, and potential off-target effects of the genetic intervention, critical considerations for both basic research and therapeutic development.
Comparative Mechanisms of Action
AAV-CRISPR Platforms
CRISPR systems for gene regulation can be engineered to target either DNA or RNA, offering versatile research applications.
DNA-Targeting CRISPR (dCas9-Repressors): This system employs a catalytically "dead" Cas9 (dCas9) fused to transcriptional repressor domains like the Krüppel-associated box (KRAB). Upon guided binding to genomic DNA, it induces epigenetic silencing without altering the DNA sequence itself. A key advantage is the potential for sustained, long-term gene repression from a single treatment, as the effect persists via stable epigenetic marks [110]. For instance, a Staphylococcus aureus dCas9-KRAB (dSaCas9KRAB) system, packaged into AAV, successfully silenced Pcsk9 in mouse liver for 24 weeks [110].
RNA-Targeting CRISPR (Cas13): Systems like CRISPR/CasRx utilize the Cas13 nuclease to directly cleave target messenger RNA (mRNA) in the cytoplasm. Because it leaves the genome untouched, it presents a favorable safety profile by eliminating risks associated with DNA double-strand breaks or inadvertent genomic editing [109]. Its smaller size (∼930 amino acids for CasRx) allows for easier packaging into AAV vectors alongside additional regulatory elements [109].
RNA Interference (RNAi) Platforms
RNAi platforms achieve gene knockdown through complementary base-pairing with mRNA.
Antisense Oligonucleotides (ASOs): These are single-stranded synthetic oligonucleotides that, upon binding their target mRNA, trigger degradation by cellular enzymes like RNase H [106]. A significant delivery advantage for neurological applications is their widespread CNS distribution following intrathecal injection, as demonstrated by the approved drug Nusinersen for Spinal Muscular Atrophy [106].
Short Hairpin RNA (shRNA) delivered by AAV: shRNA is transcribed from an AAV vector within the host cell nucleus and then processed into siRNA by the cellular machinery to guide mRNA cleavage. This allows for long-lasting, endogenous production of the silencing trigger from a single AAV administration [106].
The following diagram illustrates the core mechanistic pathways for these different gene regulation technologies operating within a neuronal cell.
Quantitative Comparison of System Characteristics
The selection between AAV-CRISPR and AAV-RNAi is guided by specific experimental requirements. The table below summarizes key performance and safety characteristics to inform this decision.
Table 1: Quantitative and Qualitative Comparison of AAV-CRISPR and RNAi Platforms
| Characteristic | AAV-CRISPR/dCas9 (DNA) | AAV-CRISPR/Cas13 (RNA) | AAV-RNAi (shRNA) | RNAi (ASO) |
|---|---|---|---|---|
| Molecular Target | Genomic DNA | mRNA | mRNA | mRNA |
| Mechanism of Action | Epigenetic repression | RNA cleavage | RISC-mediated cleavage | RNase H degradation |
| Theoretical Permanence | Long-term (epigenetic memory) | Transient (requires target mRNA turnover) | Long-term (stable shRNA expression) | Transient (requires repeated dosing) |
| Onset of Action | Slower (chromatin remodeling) | Rapid | Rapid | Rapid |
| Packaging Size Constraint | Significant (dSaCas9~3.2kb) [110] | Moderate (CasRx~2.7kb) [109] | Minimal (shRNA) | Not Applicable |
| Reported In Vivo Knockdown Efficiency | >90% (Pcsk9 mRNA) [110] | Significant reduction (HD model mRNA) [109] | High (model-dependent) | High (clinically validated) [106] |
| Primary Safety Concern | Potential off-target DNA binding | Off-target RNA cleavage | Seed-based off-targets [106] | Immune stimulation, off-targets |
| Delivery Route (to CNS) | Direct intracranial or systemic (with BBB-crossing capsid) [13] | Direct intracranial injection [109] | Direct intracranial or systemic | Intrathecal or intracerebroventricular [106] |
Detailed Experimental Protocol for AAV-CRISPR/dCas9-Mediated Gene Silencing
This protocol details the implementation of AAV-delivered dSaCas9-KRAB for transcriptional silencing in the mouse brain, based on established methodologies [110].
Reagent Preparation
- AAV Vectors: Utilize a dual-vector system to circumvent AAV packaging constraints.
- Vector 1: AAV8-CMV-dSaCas9-KRAB (titer: ≥ 1x10¹³ vg/mL)
- Vector 2: AAV8-U6-gRNA (containing target-specific guide sequence, titer: ≥ 1x10¹³ vg/mL)
- Target Sequence Design: Design gRNAs to bind within a 500 bp window upstream or downstream of the transcription start site of the target gene, leveraging DNase I hypersensitivity data if available [110].
- Control AAVs: Include control groups injected with AAV expressing a non-targeting gRNA and dSaCas9-KRAB.
Intracranial Stereotaxic Injection
- Anesthesia and Fixation: Anesthetize a 6-8 week old C57BL/6 mouse and securely place it in a stereotaxic frame.
- Surgical Procedure: Perform a midline scalp incision and identify Bregma. Calculate the coordinates for the target brain region (e.g., Striatum: AP +1.0 mm, ML ±2.0 mm from Bregma; DV -3.0 mm from the brain surface).
- Virus Mixture Preparation: Combine AAV8-CMV-dSaCas9-KRAB and AAV8-U6-gRNA in a 1:1 ratio (v/v) for a total final injection volume of 2 µL per site.
- Virus Delivery: Using a Hamilton syringe with a 33-gauge needle, infuse the virus mixture at a slow, controlled rate of 0.2 µL/min to minimize tissue damage and backflow.
- Post-operative Care: After injection, suture the incision and monitor the animal until it fully recovers from anesthesia.
Validation and Functional Analysis (4-6 Weeks Post-Injection)
- Molecular Validation:
- qRT-PCR: Extract total RNA from the injected brain region. Quantify the reduction in target mRNA levels relative to control-injected tissue.
- Western Blot: Analyze protein lysates to confirm the knockdown of the target protein.
- Phenotypic Assessment:
- Conduct region-specific behavioral assays relevant to the target gene's function.
- Perform immunohistochemistry to assess changes in neuronal morphology, markers, or downstream pathway activation.
The workflow for this protocol, from preparation to analysis, is summarized below.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these gene regulation technologies relies on a curated set of high-quality reagents and resources.
Table 2: Essential Research Reagents for AAV-Mediated Gene Regulation
| Reagent/Tool | Function/Description | Example Sources/References |
|---|---|---|
| AAV Serotypes (e.g., AAV9, AAVrh10, AAV-retro) | Determines cellular tropism and transduction efficiency in different brain regions and cell types [108] [13] [17]. | Academic vector cores; Addgene [13]. |
| dSaCas9-KRAB Plasmid | Source for engineering the compact transcriptional repressor. | Addgene (e.g., plasmid #109049) [110]. |
| CasRx (RfxCas13d) Plasmid | Source for the RNA-targeting Cas13 nuclease. | Addgene (e.g., plasmid #109049) [109]. |
| gRNA Expression Backbone | Plasmid for cloning and expressing target-specific guide RNAs. | Addgene (e.g., plasmid #109053 for CasRx gRNAs) [109]. |
| Pre-validated gRNA Sequences | Optimized sequences for targeting specific genes, reducing experimental optimization time. | Published screens (e.g., [110]); design tools (e.g., CHOPCHOP). |
| Neural Cell-Type Specific Promoters | Restricts transgene expression to specific neuronal populations (e.g., CaMKIIa for excitatory neurons, hSyn for pan-neuronal expression). | Literature-derived constructs [17]. |
| NIH Armamentarium Project Tools | A publicly available collection of validated AAVs and computational tools for precise brain cell access [13]. | BRAIN Initiative Cell Access |
The strategic choice between AAV-CRISPR and RNAi for neuronal gene regulation is not a matter of superiority but of context. AAV-CRISPR/dCas9 platforms are ideal for experimental questions demanding durable, long-term transcriptional silencing, making them suitable for modeling chronic neurodegenerative diseases or studying stable epigenetic modifications. Conversely, AAV-RNAi (shRNA) offers a well-established, compact, and effective tool for robust mRNA knockdown where permanent genomic manipulation is undesirable. The emerging CRISPR/Cas13 technology presents a compelling middle ground, offering DNA-free, specific RNA targeting with a potentially superior safety profile, though it is a newer platform requiring further validation.
Future directions will focus on mitigating immunogenicity, enhancing delivery specificity through novel capsid engineering [13] [107], and developing more precise CRISPR effectors like base editors. The continued development and rigorous comparative application of these powerful tools will undoubtedly accelerate both the deconvolution of neural circuit function and the development of next-generation gene therapies for neurological diseases.
The advent of precise genome editing tools has revolutionized biomedical research, offering unprecedented opportunities for investigating and treating human diseases. For research focused on gene delivery strategies for neural circuit manipulation, two innovative platforms have recently emerged with significant potential: retron editing for multi-gene correction and CRISPR-Cas13 for RNA modulation. These technologies address complementary challenges in genetic manipulation—retron editing enables simultaneous correction of multiple genomic loci, while CRISPR-Cas13 provides precise control over RNA expression without altering the genome. This application note provides a comprehensive technical evaluation of both platforms, including quantitative performance data, detailed experimental protocols, and specific considerations for their application in neural circuit research.
Retron Editing Systems
Retrons are bacterial genetic elements that produce multicopy single-stranded DNA (ssDNA) through self-primed reverse transcription [111]. When engineered for genome editing, retron systems consist of a reverse transcriptase (RT) and a noncoding RNA (ncRNA) that serves as a template for producing editing donor DNA. The ncRNA contains two key regions: the msr (multicopy single-stranded RNA) recognized by the RT, and the msd (multicopy single-stranded DNA) that encodes the desired donor sequence [111]. Recent engineering efforts have dramatically improved retron editing efficiency from approximately 1.5% to 30% in mammalian cells, making them viable for therapeutic applications [112].
Table 1: Performance Metrics of Advanced Retron Editing Systems
| Retron System | Source Organism | Editing Efficiency | Key Applications | Notable Features |
|---|---|---|---|---|
| Mva1-RT | Myxococcus vastator | ~30% (6x improvement over Eco1) [111] | Multi-gene correction, large deletions | High activity in mammalian cells |
| Efe1-RT | Escherichia fergusonii | ~10x improvement over Eco1 in genomic assays [111] | Genomic integration | Excellent performance in integrated reporters |
| Multitron | Engineered arrays | Simultaneous editing at 2-3 loci [113] | Metabolic engineering, molecular recording | Enables combinatorial editing in single step |
| All-RNA Retron | Delivery-optimized | Comparable to ssODN donors [111] | Vertebrate embryo editing | RNA-based delivery via lipid nanoparticles |
CRISPR-Cas13 Systems for RNA Modulation
CRISPR-Cas13 is a Class 2 Type VI RNA-guided RNA-targeting system that has been adapted for precise RNA modulation without permanent genomic changes [114]. Unlike DNA-editing CRISPR systems, Cas13 enzymes target and cleave single-stranded RNA molecules after recognition by a CRISPR RNA (crRNA) guide. The most widely used variant, RfxCas13d, is particularly valuable for research applications due to its compact size, high specificity, and lack of protospacer flanking sequence (PFS) requirements [114].
Table 2: CRISPR-Cas13 Variants and Their Research Applications
| Cas13 Variant | Size (aa) | PFS Requirement | Primary Applications | Efficiency in Neural Models |
|---|---|---|---|---|
| Cas13a (LshCas13a) | ~1,250 | Yes | RNA knockdown, nucleic acid detection | Limited data |
| Cas13b (PspCas13b) | ~1,150 | Yes | RNA base editing (REPAIR, RESCUE) | Limited data |
| RfxCas13d | ~900-1,000 | No | Transcript knockdown, splicing modulation | Effective in chick embryos [115] |
| Cas13X/Y (Cas13bt) | ~775-800 | No | Compact RNA editing, AAV delivery | Limited data |
Retron Editing: Applications and Protocols for Multi-Gene Correction
Key Applications in Neural Circuit Research
Retron editing offers several unique capabilities that are particularly valuable for neural circuit manipulation research:
Simultaneous Multi-Gene Correction: Multitron systems can edit multiple non-adjacent genomic locations in a single experiment, enabling complex genetic engineering of neuronal populations [113]. This is invaluable for studying polygenic traits or correcting multiple disease-associated mutations in neural circuit models.
Large Genomic Deletions: Sequential deletion strategies using multitrons enable researchers to remove large genomic regions by "collapsing" distant segments, facilitating the study of regulatory elements that control neural gene expression [116].
Molecular Recording: Retrons can record transient molecular events in cells, potentially enabling tracking of neuronal activity or signaling pathway activation over time [113]. This capability could be harnessed to map functional neural connections.
Metabolic Engineering: Multi-site editing allows optimization of metabolic pathways in engineered neural cells, potentially enhancing the production of neurotransmitters or neuroprotective compounds [117].
Detailed Protocol: Multi-Site Genome Editing with Multitrons
Principle: Engineered retron arrays produce multiple donor DNA sequences from a single transcript, enabling simultaneous editing at distinct genomic loci when combined with CRISPR nucleases [113].
Workflow:
Multitron Construct Design
- For arrayed msd design: Clone 2-3 donor sequences (70-90 bp each) in tandem within a single msd region, separated by appropriate linker sequences
- For arrayed ncRNA design: Clone complete msr-msd units (∼229 bp each) in tandem, with each unit encoding a distinct donor
- Include appropriate homology arms (∼29-40 bp) flanking each edit in the donor sequences
- For neural cell applications: Incorporate neuronal-specific promoters (e.g., Syn1, CaMKIIa) for controlled expression
Delivery System Assembly
- Clone the multitron construct into an appropriate expression vector
- Co-express with CRISPR nuclease (Cas9 nickase or Cas12a) and guide RNAs targeting each locus
- For all-RNA delivery: Incorporate multitron RNA, Cas nuclease mRNA, and guide RNAs into lipid nanoparticles (LNPs) [112]
Cell Transfection and Analysis
- Transfert primary neuronal cultures or neural stem cells using optimized LNP formulations
- Include control singleplex retron editors for efficiency comparison
- After 72-96 hours, harvest cells for genomic DNA extraction
- Analyze editing efficiency using next-generation sequencing of all target loci
- Validate functional effects using cell-type-specific phenotypic assays
Troubleshooting Notes:
- Position-dependent efficiency variations may occur; prioritize critical edits at the 5' end of tandem arrays
- For difficult-to-edit neuronal populations, consider Cas9 nickase rather than wild-type Cas9 to reduce indels
- Optimize LNP formulations for blood-brain barrier penetration for in vivo applications
Multitron Experimental Workflow for Neural Cell Editing
CRISPR-Cas13: Applications and Protocols for RNA Modulation
Key Applications in Neural Circuit Research
CRISPR-Cas13 systems provide powerful capabilities for transient RNA manipulation in neural cells:
Targeted Transcript Knockdown: RfxCas13d enables efficient and specific degradation of target mRNAs without permanent genomic alterations, ideal for studying essential genes in neuronal function and development [115].
RNA Base Editing: Catalytically dead Cas13 (dCas13) fused to deaminase domains enables precise single-nucleotide RNA editing through REPAIR (A-to-I) and RESCUE (C-to-U) systems, offering potential for correcting point mutations associated with neurological disorders [114].
Splicing Modulation: dCas13 can be targeted to splice junctions to influence alternative splicing patterns, relevant for studying neurological disorders with splicing defects [114].
Live Cell RNA Imaging: dCas13 fused with fluorescent proteins enables tracking of specific RNA molecules in live neurons, facilitating studies of RNA transport and localization in neural processes.
Detailed Protocol: Targeted Gene Knockdown in Neural Cells with RfxCas13d
Principle: RfxCas13d, guided by specific crRNAs, binds and cleaves target mRNA molecules, leading to their degradation and subsequent reduction in protein expression [115].
Workflow:
crRNA Design and Validation
- Design 3-5 crRNAs (∼30 nt) targeting different regions of the transcript of interest
- Avoid secondary structures and ensure specificity through BLAST analysis
- For neural applications: Consider targeting splice variants specific to neuronal cell types
- Validate crRNA efficiency using a dual-luciferase reporter system before proceeding to endogenous targets
Delivery Construct Preparation
- Clone RfxCas13d codon-optimized for mammalian expression under control of appropriate promoter
- Express crRNAs from U6 polymerase III promoter
- For in vivo applications: Package into AAV vectors (serotypes 1, 2, 5, 8, 9, or PHP.eB for enhanced CNS tropism)
- Include fluorescent markers (e.g., EGFP) for tracking transduction efficiency
Cell Transduction and Analysis
- Transduce primary neuronal cultures or brain slices using optimized AAV protocols
- For in vivo applications: Administer via stereotactic injection to target brain regions
- Harvest cells/tissue 5-7 days post-transduction
- Analyze knockdown efficiency using:
- qRT-PCR to measure transcript levels
- Western blot or immunostaining to assess protein reduction
- Functional assays relevant to the target gene (electrophysiology, calcium imaging, behavioral tests)
Troubleshooting Notes:
- Include mismatch controls and non-targeting crRNAs to control for off-target effects
- Titrate AAV doses to achieve optimal transduction without cellular toxicity
- For difficult-to-target transcripts, test multiple crRNAs and consider combinatorial approaches
- Account for protein half-life when interpreting early knockdown results
CRISPR-Cas13d Workflow for Neural Gene Knockdown
Research Reagent Solutions
Table 3: Essential Research Reagents for Retron and Cas13 Applications
| Reagent Category | Specific Examples | Function/Application | Key Considerations for Neural Research |
|---|---|---|---|
| Retron Systems | Mva1-RT, Efe1-RT, Eco1-RT [111] | Reverse transcription of donor DNA | Mva1-RT shows highest activity in mammalian cells |
| Multitron Architectures | Arrayed msd, Arrayed ncRNA, Trans msr [113] | Simultaneous multi-site editing | Arrayed ncRNA minimizes positional efficiency bias |
| CRISPR Nucleases | Cas9 nickase (D10A), Cas12a [111] | DNA cleavage for HDR initiation | Cas9 nickase reduces indels; Cas12a expands target range |
| Cas13 Variants | RfxCas13d, PspCas13b, Cas13X [114] | RNA targeting and cleavage | RfxCas13d: no PFS requirement, compact size |
| Delivery Vectors | AAV (serotypes 1,2,5,8,9, PHP.eB), Lentivirus, LNPs [112] | In vivo and in vitro delivery | AAV-PHP.eB shows enhanced blood-brain barrier penetration |
| Promoters | Synapsin-1, CaMKIIa, hU6, CAG | Cell-type-specific expression | Synapsin-1 for pan-neuronal expression |
| Reporting Systems | EGFP, mCherry, BFP | Tracking transduction/transfection | Multiple colors for multiplexed experiments |
Retron editing and CRISPR-Cas13 technologies represent significant advancements in genetic manipulation tools for neural circuit research. Retron systems address the critical challenge of multi-locus genome editing, enabling complex genetic engineering previously achievable only through laborious sequential approaches. The development of multitron architectures with improved efficiency (up to 30% in mammalian cells) makes simultaneous correction of multiple neural disease-associated mutations a tangible goal [111] [112]. Meanwhile, CRISPR-Cas13 platforms offer precise RNA-level modulation ideal for studying essential genes where permanent genomic alteration would be detrimental. The successful application of RfxCas13d in model organisms, including chick embryos [115], demonstrates its potential for neural development studies.
For neural circuit manipulation research, these technologies can be complementary: retron editing enables stable genomic modifications of circuit components, while Cas13 allows transient manipulation of neuronal activity regulators. The ongoing development of delivery strategies, particularly lipid nanoparticles for retron RNA [112] and enhanced AAV capsids for Cas13, will further enhance their utility for challenging neural applications. As these platforms continue to mature, they promise to accelerate our understanding of neural circuit function and dysfunction, potentially enabling new therapeutic strategies for neurological and psychiatric disorders.
Adeno-associated virus (AAV)-mediated gene therapy has revolutionized the treatment of monogenic neurological diseases, demonstrating a clear pathway from preclinical model systems to clinical application. Two particularly instructive examples are spinal muscular atrophy (SMA) and aromatic L-amino acid decarboxylase (AADC) deficiency, which together illustrate the critical importance of matching vector design, delivery route, and target neural circuits to achieve therapeutic efficacy. SMA, a severe neuromuscular disorder caused by mutations in the survival motor neuron 1 (SMN1) gene, results in the degeneration of motor neurons in the spinal cord and brainstem [118]. AADC deficiency is a rare neurodevelopmental disorder characterized by mutations in the dopa decarboxylase (DDC) gene, leading to severe deficits in the synthesis of dopamine and serotonin [119]. This application note examines the translational journey of AAV-based therapies for these distinct disorders, providing key insights and protocols for researchers developing gene delivery strategies for neural circuit manipulation.
Table 1: Clinical and Preclinical Profile of AAV Therapies for SMA and AADC Deficiency
| Parameter | AAV Therapy for SMA (GC101) | AAV Therapy for AADC Deficiency (Kebilidi/Upstaza) |
|---|---|---|
| Target Disease | Spinal Muscular Atrophy (Types 1, 2, 3) | Aromatic L-Amino Acid Decarboxylase (AADC) Deficiency |
| Therapeutic Transgene | Codon-optimized human SMN1 (coSMN1) | Human dopa decarboxylase (DDC) |
| AAV Serotype | AAV9 | AAV2 |
| Primary Route of Administration | Intrathecal (IT) or Intracerebroventricular (ICV) | Intraputaminal (direct brain injection) |
| Key Preclinical Models | Taiwanese SMA-like mouse model (Smn1-/-, SMN2+/+), Cynomolgus Monkeys [118] | Non-human primates, Murine models |
| Clinical Efficacy Endpoints | Motor neuron rescue, tail length preservation, muscle histopathology [118] | Complete resolution of oculogyric crises, head control, independent sitting [119] [120] |
| Notable Clinical Outcomes | Widespread CNS distribution, no toxic inflammatory responses in DRG [118] | 6/7 subjects gained normal head control; 4/7 could sit independently at 12 months [119] |
| FDA Approval Status | In clinical trials (NCT05824169, NCT05901987, NCT06421831) [118] | Approved (Nov 2024 - Kebilidi) [120] |
Therapeutic Mechanisms and Signaling Pathways
The therapeutic strategies for SMA and AADC deficiency address fundamentally different pathophysiological processes within the nervous system, necessitating distinct AAV vector designs and delivery approaches.
Diagram 1: Therapeutic Mechanisms for SMA and AADC Deficiency
For SMA, the therapeutic goal is to restore survival motor neuron (SMN) protein expression in motor neurons and associated tissues. Codon-optimization of the SMN1 transgene has been shown to enhance protein expression levels, which is critical for rescuing motor neuron function [118]. The AAV9 vector is selected for its ability to cross the blood-brain barrier and achieve widespread transduction throughout the central nervous system (CNS) when delivered via intrathecal or intracerebroventricular routes [118] [121].
In contrast, AADC deficiency requires restoration of dopamine and serotonin synthesis in specific nigrostriatal and mesolimbic pathways. The therapeutic strategy involves direct intraputaminal delivery of the AADC enzyme via AAV2 vectors to the substantia nigra and ventral tegmental area [119] [120]. This approach takes advantage of anterograde axonal transport to deliver the AADC enzyme to neuroanatomically appropriate brain regions, effectively bypassing the blood-brain barrier and minimizing systemic exposure [119].
Quantitative Data Comparison
The transition from model systems to clinical application requires careful dose optimization and efficacy assessment across species. The following tables summarize key quantitative data from preclinical and clinical studies for both therapeutic approaches.
Table 2: Efficacy Metrics from Preclinical and Clinical Studies
| Study Metric | SMA (AAV9-coSMN1) Preclinical | AADC Deficiency (AAV2-hAADC) Clinical |
|---|---|---|
| Vector Doses | 5 μL/pup (PND1 mice); 800 μL/animal (NHP) [118] | 1.3 × 10^11 vg (n=3); 4.2 × 10^11 vg (n=4) [119] |
| Target Coverage | Widespread CNS distribution post-IT/ICV [118] | 98% SN and 70% VTA coverage [119] |
| Functional Improvement | Tail length preservation, improved muscle histopathology [118] | Oculogyric crises resolved in 6/7 subjects by Month 3 [119] |
| Motor Milestones | Rescue of motor neuron pathology [118] | 6/7 subjects gained head control; 4/7 could sit independently at 12 months [119] |
| Biomarker Changes | Increased SMN protein in CNS and peripheral tissues [118] | Increased dopamine metabolism and FDOPA uptake in striatum [119] |
| Long-term Outcomes | No toxic inflammatory responses in dorsal root ganglia [118] | 2 subjects could walk with 2-hand support at 18 months [119] |
Table 3: Vector and Transgene Configuration
| Vector Characteristic | AAV9-coSMN1 for SMA | AAV2-hAADC for AADC Deficiency |
|---|---|---|
| Promoter | Undisclosed (likely CAG or CB) [118] | Likely CMV or similar constitutive promoter |
| Transgene Optimization | Codon-optimized hSMN1 (coSMN1) [118] | Wild-type human DDC sequence |
| Capsid Engineering | Wild-type AAV9 | Wild-type AAV2 |
| Regulatory Elements | Undisclosed (standard ITR configuration) [118] | Standard ITR configuration |
| Packaging Capacity | ~4.7 kb (full-length SMN1 + regulatory elements) [122] | ~4.7 kb (DDC gene + regulatory elements) |
| Production System | Baculovirus/Sf9 system [118] | Plasmid transfection/HEK293 system |
Experimental Protocols
Preclinical Efficacy Testing in SMA Mouse Models
Purpose: To evaluate the therapeutic efficacy of AAV9-coSMN1 in rescuing motor neuron survival and function in SMA model mice.
Materials:
- Taiwanese SMA-like mouse model (Smn1-/-, SMN2+/+) [118]
- AAV9-coSMN1 vector (titer: ≥1×10^13 vg/mL)
- Control: AAV9-empty vector or saline
- Ice anesthesia apparatus
- Hamilton syringe (33G) for ICV injection
- Western blot equipment and SMN antibodies (BD Biosciences, #610646) [118]
- Histopathology supplies (H&E staining, immunofluorescence)
Procedure:
- Neonatal Injections: On postnatal day 1 (PND1), anesthetize neonatal mice on ice.
- ICV Injection: Using a 33G Hamilton syringe, unilaterally inject 5 μL of AAV9-coSMN1 or control into the lateral ventricle using stereotaxic coordinates: X = 1.0 mm lateral to bregma, Y = 0.3 mm posterior, Z = 2.0 mm depth (adjusted for neonatal skull thickness) [118].
- Post-injection Care: Rewarm pups until normal temperature and limb movement returns, then return to dam.
- Functional Assessment: Monitor tail length weekly as a biomarker of SMA progression.
- Tissue Collection: At study endpoint (typically 8-12 weeks), collect spinal cord, muscle, and peripheral tissues.
- Histopathological Analysis: Process tissues for H&E staining and immunofluorescence to quantify motor neuron survival and muscle pathology.
- Biochemical Analysis: Perform Western blot on spinal cord and muscle tissues to confirm SMN protein expression using anti-SMN antibodies.
Troubleshooting: Ensure precise injection coordinates for consistent ventricular delivery. Maintain strict temperature control during neonatal anesthesia to maximize survival.
Intraputaminal Delivery in Non-Human Primates
Purpose: To establish the safety, biodistribution, and transduction efficiency of AAV2-hAADC following direct convection-enhanced delivery to the putamen.
Materials:
- Cynomolgus monkeys (2.5 years old) with AAV2 neutralizing antibody titer ≤1:50 [118]
- AAV2-hAADC vector (dose: 1.3×10^11 - 4.2×10^11 vg total)
- MR-guided stereotactic surgery system
- Convection-enhanced delivery (CED) catheters and pump
- Ketamine anesthesia (7.5 mg/kg intramuscular)
- 1 mL disposable sterile syringes and matching needles
- PET imaging for FDOPA uptake assessment [119]
Procedure:
- Preoperative Planning: Conduct MR imaging to identify target coordinates for bilateral putamen.
- Anesthesia: Administer ketamine (7.5 mg/kg IM) after at least 6 hours of fasting.
- Sterotactic Setup: Secure head in stereotactic frame and register with preoperative MR images.
- Catheter Placement: Under real-time MR guidance, position CED catheters to target bilateral substantia nigra and ventral tegmental area.
- Vector Infusion: Slowly infuse total volume of 80 μL per hemisphere (160 μL total) using convection-enhanced delivery over several hours to maximize distribution [119].
- Real-time Monitoring: Use MR imaging to monitor infusate distribution and ensure target coverage of SN and VTA.
- Post-operative Care: Monitor vital signs until full recovery from anesthesia.
- Efficacy Assessment: At 3, 6, and 12 months post-infusion, perform FDOPA-PET imaging to quantify restoration of dopamine synthesis and monitor behavioral improvements.
Troubleshooting: Optimize infusion rate to prevent reflux along the catheter track. Use real-time MR monitoring to confirm target coverage and adjust catheter position if needed.
Delivery Strategies and Surgical Workflows
The route of administration is a critical determinant of therapeutic efficacy for CNS-directed AAV therapies, with each approach offering distinct advantages for targeting specific neural circuits.
Diagram 2: Administration Routes for Neural Circuit Targeting
For SMA, the intrathecal delivery approach targets the broad network of spinal motor neurons responsible for neuromuscular function. This method involves injecting the AAV9 vector into the cerebrospinal fluid (CSF), allowing for widespread distribution throughout the spinal cord and brain [118] [123]. The AAV9 serotype is particularly suited for this application due to its ability to efficiently transduce neurons across the CNS when delivered via CSF routes [121].
For AADC deficiency, the intraputaminal approach provides precise targeting of the nigrostriatal pathway, which is specifically impaired in this disorder. This method employs convection-enhanced delivery (CED) with real-time MR guidance to ensure accurate coverage of the substantia nigra and ventral tegmental area [119] [120]. The focal delivery minimizes systemic exposure and potential immune responses while maximizing therapeutic transgene expression in the critical dopamine-producing circuits.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for AAV Neuroscience Applications
| Reagent / Material | Function & Application | Examples & Specifications |
|---|---|---|
| AAV Serotype Panels | Screening for optimal neural circuit transduction | AAV1, AAV2, AAV5, AAV8, AAV9, AAV-PHP.eB, AAV-retro [121] [124] |
| Cell-Type Specific Promoters | Targeting transgene expression to specific neuronal populations | Synapsin (Syn1) - neurons; GFAP - astrocytes; NSE - neurons [23] |
| Neural Activity Reporters | Monitoring neuronal function and circuit dynamics | GCaMP6 (calcium imaging), GRAB sensors (neurotransmission), ASAP (voltage) [124] |
| Circuit Tracing AAVs | Mapping neural connectivity | AAV-retro (retrograde tracing), Anterograde tracers [124] |
| Optogenetic/ Chemogenetic Actuators | Precise manipulation of neural activity | Channelrhodopsins (ChR2), DREADDs, Halorhodopsins [124] |
| CNS Delivery Equipment | Precise administration to neural targets | Stereotactic frames, Hamilton syringes (33G), CED catheters [118] [119] |
| Immunodetection Reagents | Validating transgene expression and cellular responses | Anti-SMN (BD Biosciences #610646), Anti-AADC, Anti-dopamine antibodies [118] |
Discussion and Future Perspectives
The comparative analysis of AAV therapies for SMA and AADC deficiency reveals several overarching principles for successful neural circuit targeting. First, the route of administration must align with the neuroanatomical distribution of the pathological circuit—widespread intrathecal delivery for diffusely affected motor systems in SMA versus precise intraputaminal infusion for focal nigrostriatal pathology in AADC deficiency. Second, capsid selection should optimize for the required transduction profile, with AAV9 providing broad CNS access for SMA and AAV2 offering efficient neuronal transduction for AADC deficiency. Third, therapeutic success depends on matching the transgene design to the molecular pathology, whether through codon-optimization for enhanced SMN expression in SMA or precise restoration of AADC enzyme activity in AADC deficiency.
Future developments in AAV-mediated neural circuit manipulation will likely focus on several key areas: capsid engineering to enhance blood-brain barrier penetration and cell-type specificity [121] [23]; regulatory element optimization to fine-tune transgene expression levels and persistence [23]; and novel delivery approaches that maximize target engagement while minimizing immune responses [123]. The recent FDA approval of Kebilidi for AADC deficiency validates the direct brain delivery approach and paves the way for similar strategies targeting other complex neural circuits [120]. As these technologies mature, researchers will increasingly be able to design AAV-based interventions with the precision necessary to correct specific circuit dysfunctions while preserving overall neural network integrity.
AI-Powered Enhancer Discovery for Next-Generation Specificity
The precise manipulation of specific neural circuits is a fundamental goal in modern neuroscience, critical for advancing our understanding of brain function and developing novel therapies for neurological disorders. Current therapies for brain disorders predominantly address symptoms rather than underlying causes, highlighting a significant unmet need for targeted interventions [13] [48]. The advent of sophisticated gene delivery systems now enables researchers to access and manipulate specific cell types within the complex environment of the brain and spinal cord with unprecedented accuracy [13]. This capability represents a paradigm shift from broadly acting interventions to precisely targeted molecular therapies.
A central challenge in achieving this specificity has been the identification of genetic regulatory elements, known as enhancers, that can drive gene expression in particular neural cell types without affecting others. Traditional methods for enhancer discovery have been limited by their reliance on manual curation and their inability to efficiently analyze the vast genomic datasets required for precise targeting. The integration of artificial intelligence (AI) into this discovery process has emerged as a transformative solution, enabling the rapid identification of functional enhancer sequences from complex multi-species genomic data [13] [48]. This AI-powered approach, developed through the NIH's Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative, has yielded a versatile toolkit that significantly accelerates our understanding of neural circuitry [68].
This application note details the methodologies and protocols for implementing AI-powered enhancer discovery to achieve next-generation specificity in neural circuit manipulation. The described workflows integrate computational AI tools with experimental viral vector systems to enable targeted gene delivery for both basic research and therapeutic development.
Key Technological Components
AI-Powered Computational Tools
The core innovation enabling next-generation specificity lies in AI-powered computer programs specifically designed to identify genetic enhancers. These tools analyze extensive genomic datasets across multiple species to pinpoint sequences that function as cell-type-specific "light switches" for gene expression [13] [48]. The AI algorithms cut considerable time and effort for scientists who previously relied on manual approaches to identify these critical regulatory elements. This computational capability forms the foundation for designing targeted gene delivery systems that can access specific neural populations based on their intrinsic genetic signatures rather than their anatomical location alone.
Viral Vector Delivery Systems
The computational identification of enhancers is functionally implemented through advanced viral vector systems. The recently developed toolkit utilizes a stripped-down adeno-associated virus (AAV) to deliver genetic material to target cells in the brain and spinal cord [13] [48]. These delivery systems have been validated in intact living systems and can be broadly applied across many species and experimental models, including human brain tissue samples obtained during surgical procedures. The vectors are engineered to incorporate AI-identified enhancers, enabling them to target dozens of specific brain cell types with exceptional accuracy, including excitatory neurons, inhibitory interneurons, striatal and cortical subtypes, and hard-to-reach neurons in the spinal cord that are affected in conditions such as amyotrophic lateral sclerosis (ALS) and spinal muscular atrophy [13].
Table 1: Quantitative Performance of AI-Enhanced Gene Delivery Systems
| Target Cell Type | Specificity Level | Applications | Therapeutic Relevance |
|---|---|---|---|
| Excitatory Neurons | Exceptional accuracy [13] | Circuit mapping, activity modulation | Epilepsy, Alzheimer's disease [48] |
| Inhibitory Interneurons | Exceptional accuracy [13] | Network regulation, silencing | Epilepsy, neuropsychiatric disorders [48] |
| Spinal Cord Neurons | Exceptional accuracy [13] | Motor circuit analysis | ALS, spinal muscular atrophy [13] [48] |
| Prefrontal Cortex Cells | Critical area access [13] | Decision-making studies | Cognitive disorders, uniquely human traits [13] |
| Brain Blood Vessel Cells | Selective targeting [13] | Blood-brain barrier research | Drug delivery, vascular disorders [13] |
Experimental Protocols
Protocol 1: AI-Driven Enhancer Discovery Workflow
This protocol details the computational pipeline for identifying cell-type-specific enhancers using AI tools.
Materials Required:
- High-performance computing cluster with GPU acceleration
- Multi-species genomic databases (human, mouse, non-human primate)
- Single-cell RNA sequencing datasets from target neural tissues
- AI enhancer discovery software (available through BRAIN Initiative resources)
Procedure:
- Data Curation and Preprocessing (Timeline: 2-3 days)
- Collect and align epigenetic data (ATAC-seq, Hi-C, ChIP-seq) from target cell types across multiple species
- Annotate open chromatin regions and histone modification marks indicative of regulatory elements
- Normalize datasets to account for technical variations and batch effects
Model Training and Validation (Timeline: 3-5 days)
- Implement neural network architectures trained to recognize enhancer signatures
- Cross-validate predictions using orthogonal datasets from published literature
- Establish specificity metrics to minimize false positive identifications
Enhancer Selection and Prioritization (Timeline: 1-2 days)
- Filter candidates based on evolutionary conservation and cell-type specificity scores
- Rank enhancers by predicted strength and specificity for target cell population
- Select top candidates for experimental validation in vector constructs
The entire computational workflow typically requires 5-10 days to complete, substantially faster than traditional manual approaches [13].
Protocol 2: Viral Vector Construction and Validation
This protocol describes the implementation of AI-identified enhancers into viral vector systems for neural targeting.
Materials Required:
- Plasmid backbone with AAV inverted terminal repeats (ITRs)
- Synthetic enhancer sequences (100-500 bp) based on AI predictions
- Minimal promoter elements for transcriptional initiation
- Reporter genes (e.g., GFP, mCherry) or effector genes (DREADDs, opsins, etc.)
- Cell lines for packaging (HEK293T) and primary neuronal cultures
Procedure:
- Vector Assembly (Timeline: 7-10 days)
- Clone synthetic enhancer sequences upstream of minimal promoters
- Incorporate reporter/effector cassettes downstream of promoter
- Verify construct sequence fidelity through Sanger sequencing
Virus Production and Purification (Timeline: 14 days)
- Transfect packaging cells with vector plasmid and helper plasmids
- Harvest viral particles 72 hours post-transfection
- Purify using iodixanol gradient ultracentrifugation
- Concentrate and titer using qPCR methods
Specificity Validation (Timeline: 21-28 days)
- Apply vectors to primary neuronal cultures or brain slice preparations
- Assess cell-type-specific expression using immunohistochemistry
- Quantify targeting specificity using automated cell counting algorithms
- Compare with positive and negative control vectors
Table 2: Experimental Parameters for Vector Validation
| Parameter | Measurement Method | Acceptance Criteria | Quality Control |
|---|---|---|---|
| Viral Titer | Quantitative PCR | >1×10¹² vg/mL | Endotoxin <5EU/mL |
| Infection Efficiency | Flow cytometry | >70% in permissive cells | Sterility testing |
| Target Specificity | Immunofluorescence | >80% target cell expression | <5% off-target expression |
| Expression Level | Western blot/fluorescence | Consistent batch-to-batch | Reference standard comparison |
| In Vivo Performance | Animal model testing | Cell-type-specific expression | Histological validation |
AI Enhancer Discovery Workflow: This diagram illustrates the complete pipeline from data collection to precise neural circuit manipulation.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of AI-powered enhancer discovery for neural circuit manipulation requires access to specialized research reagents and tools. The following table details essential materials and their functions within the experimental workflow.
Table 3: Essential Research Reagents for AI-Enhanced Neural Targeting
| Reagent/Tool | Function | Source/Availability |
|---|---|---|
| AAV Vector Toolkit | Delivery of genetic material to specific neural cell types [13] | Addgene (global supplier) [13] |
| Cell-Type-Specific Enhancers | AI-identified genetic switches for targeted expression [13] [48] | BRAIN Initiative resources [13] |
| AI Prediction Algorithms | Computer programs identifying enhancers across species [13] | BRAIN Initiative supported tools [13] |
| Standard Operating Procedures | Protocols for tool use and validation [13] | Published in Neuron, Cell, Cell Reports [13] |
| Multi-species Genomic Data | Training and validation datasets for AI models [48] | Public and proprietary databases |
| Neural Cell Markers | Validation of targeting specificity (e.g., NeuN, GFAP, etc.) | Commercial antibody suppliers |
| Primary Neuronal Cultures | In vitro testing of vector specificity | Tissue dissection or commercial sources |
Applications in Neural Circuit Research
The integration of AI-powered enhancer discovery with viral vector technology enables sophisticated approaches to neural circuit manipulation with broad research applications. These tools allow investigators to illuminate fine structures of brain cells with fluorescent proteins and activate or silence circuits that control behavior and cognition [13] [48]. This capability is particularly valuable for studying neural pathways affected in neurological and neuropsychiatric conditions, including seizure disorders, ALS, Parkinson's disease, Alzheimer's disease, and Huntington's disease [48].
A significant advantage of this platform is its ability to provide researchers with gene delivery systems for various species used in research without requiring genetically modified animals [13]. This feature substantially reduces the time and cost associated with establishing new animal models for circuit analysis. Furthermore, the toolkit enables access to specific brain cell types in the prefrontal cortex, an area critical for decision-making and uniquely human traits that has been challenging to target with previous technologies [13].
Vector Targeting Mechanism: This diagram shows how AI-identified enhancers enable cell-type-specific gene expression in neural targets.
The fusion of AI-powered enhancer discovery with advanced viral vector systems represents a transformative advancement in neural circuit research. This methodology provides unprecedented specificity and accuracy in accessing distinct neural cell populations, enabling more precise investigation of neural circuit function and dysfunction [13]. The availability of these tools through centralized repositories like Addgene ensures broad accessibility to the research community, accelerating the pace of discovery across multiple neuroscience domains [13].
Looking forward, these technologies establish a foundation for next-generation gene therapies that can target only affected cells in the brain, spinal cord, or brain blood vessels, potentially revolutionizing treatment approaches for neurological disorders [13] [48]. As AI algorithms continue to evolve and incorporate larger datasets, their predictive accuracy for cell-type-specific enhancers will further improve, enabling even more refined manipulation of neural circuits. This progression toward increasingly precise interventions promises to unlock new therapeutic possibilities while minimizing off-target effects, ultimately advancing both basic neuroscience and clinical applications.
Conclusion
The field of gene delivery for neural circuit manipulation is advancing at an unprecedented pace, moving from broad interventions to exquisitely precise cell-type and circuit-specific control. The synergy between refined AAV toolkits—featuring novel capsids and promoters—and versatile CRISPR technologies is creating a powerful platform for both foundational neuroscience and therapeutic development. Success hinges on systematically addressing persistent challenges in delivery efficiency, immune evasion, and target specificity. Future directions will be shaped by the clinical translation of these technologies, the development of non-viral delivery methods, and the creation of even more sophisticated systems capable of manipulating multiple neural populations simultaneously. The ongoing work, exemplified by the NIH BRAIN Initiative's latest toolkits, promises to unlock new treatments for a wide spectrum of neurological and psychiatric disorders by finally enabling precise, causal interrogation and correction of faulty neural circuits.
References
- 1. Adeno-Associated Virus ( AAV ) as a Vector for Gene Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5548848/]
- 2. What are AAV : A Powerful Tool for Gene Therapy Vectors [https://www.atlantisbioscience.com/blog/what-is-aav-vector-how-does-it-work-and-why-is-it-used-for-gene-therapy/]
- 3. A clinician’s guide to AAV production – How manufacturing platforms shape vector properties - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268253/]
- 4. AAV Vectors in Gene Therapy: Measuring & Optimizing Quality [https://blog.genewiz.com/aav-vectors-in-gene-therapy-measuring-optimizing-quality]
- 5. Dual AAV vectors for efficient delivery of large transgenes | Nature Protocols [https://www.nature.com/articles/s41596-025-01243-8]
- 6. Frontiers | AAV viral vectors as therapeutic interventions for inherited... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1678325/full]
- 7. Unlocking the Future of Gene Therapy: AAV Pipeline Insight... Vectors [https://www.linkedin.com/pulse/unlocking-future-gene-therapy-aav-vectors-pipeline-insight-bora-bvglc]
- 8. Vs. AAV - Life in the Lab Lentiviral Vectors [https://www.thermofisher.com/blog/life-in-the-lab/aav-vs-lv/]
- 9. Viral Vectors 101: Types of viruses [https://blog.addgene.org/viral-vectors-101-types-of-viruses]
- 10. Viral Vectors for Gene Delivery to the Central Nervous System - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3293995/]
- 11. Viral vectors for gene delivery to the nervous system | Nature Reviews Neuroscience [https://www.nature.com/articles/nrn1104]
- 12. Gene delivery to the spinal cord: comparison between lentiviral ... [https://pubmed.ncbi.nlm.nih.gov/16786574/]
- 13. Scientists design gene delivery systems for cells in the brain and spinal cord | National Institutes of Health (NIH) [https://www.nih.gov/news-events/news-releases/scientists-design-gene-delivery-systems-cells-brain-spinal-cord]
- 14. vs. AAV | Gene Transfer Tools Lentiviral Vectors Comparison [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/comparing-gene-transfer-tools-adeno-associated-virus-and-lentiviral-vectors.html]
- 15. system: construction, history and therapeutic... Adenovirus vector [https://pubmed.ncbi.nlm.nih.gov/36475496/]
- 16. Frontiers | An evaluation of distinct adeno-associated virus vector ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1558581/full]
- 17. for Targeting Neural Circuits: How to Manipulate Neurons... Strategies [https://pmc.ncbi.nlm.nih.gov/articles/PMC9099413/]
- 18. Learn how you can use retrograde for neuronal AAV . tracing [https://blog.addgene.org/retrograde-aav-making-the-journey-from-axon-to-nucleus]
- 19. Long-distance axonal transport of AAV9 is driven by dynein and kinesin-2 and is trafficked in a highly motile Rab7-positive compartment - PubMed [https://pubmed.ncbi.nlm.nih.gov/24100640/]
- 20. Long-distance Axonal Transport of AAV9 Is Driven by Dynein and Kinesin-2 and Is Trafficked in a Highly Motile Rab7-positive Compartment - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1525001616311807]
- 21. Synaptic Specificity and Application of Anterograde Transsynaptic... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7159884/]
- 22. Recombinase-independent AAV for anterograde transsynaptic tracing [https://molecularbrain.biomedcentral.com/articles/10.1186/s13041-023-01053-7]
- 23. Designing and optimizing AAV-mediated gene therapy for neurodegenerative diseases: from bench to bedside | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05661-2]
- 24. Frontiers | Accurate Quantification and Characterization of ... [https://www.frontiersin.org/articles/10.3389/fmicb.2019.01570/full]
- 25. for Precision Armamentarium Cell Access | Brain BRAIN Initiative [https://braininitiative.nih.gov/research/tools-and-technologies-brain-cells-and-circuits/armamentarium-precision-brain-cell-access]
- 26. Optogenetics: Illuminating Neural with Circuits Control... Precision [https://vprc.in/genetics/optogenetics-illuminating-neural-circuits-with-precision-control/]
- 27. Frontiers | Precision neurocircuitry: emerging tools to map, modulate... [https://www.frontiersin.org/research-topics/73257/precision-neurocircuitry-emerging-tools-to-map-modulate-and-model-behavior]
- 28. Cell Census Network Brain Initiative [https://www.nature.com/collections/cicghheddj?error=cookies_not_supported&code=1023710b-0fd2-437e-b009-4d9e34efb5a8]
- 29. BRAIN 2025: A Scientific Vision | BRAIN Initiative [https://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 30. Frontiers | Advancements in the Quest to Map, Monitor, and... [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2022.886302/full]
- 31. Selective Manipulation of Neural Circuits - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4824027/]
- 32. Contemporary approaches to neural circuit manipulation and mapping: focus on reward and addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4528822/]
- 33. AAV serotypes and AAV Tissue-specific Tropism | GeneMedi [https://www.genemedi.net/i/aav-serotypes-tissue-specific-tropism]
- 34. capabilities of adeno-associated virus vectors in the... Retrograde [https://pmc.ncbi.nlm.nih.gov/articles/PMC9642939/]
- 35. A designer AAV variant permits efficient retrograde access to projection neurons - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872824/]
- 36. AAV-DJ is superior to AAV9 for targeting brain and spinal cord, and de-targeting liver across multiple delivery routes in mice | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05599-5]
- 37. Nature Breakthrough: AAV -ROOT Serotype Enables Precise Tracing ... [https://www.ebraincase.com/support/literature-interpretation/2547.html]
- 38. Analysis of Transduction Efficiency, Tropism and Axonal Transport of AAV Serotypes 1, 2, 5, 6, 8 and 9 in the Mouse Brain | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0076310]
- 39. AAV2-Retro (Retrograde) vector system (AAV2-Retro expression and packaging plasmid system) | GeneMedi [https://www.genemedi.net/i/aav-retro-packaging-system]
- 40. Optimization of adeno-associated viral vector-mediated transduction of... [https://www.nature.com/articles/s41434-020-0169-1?error=cookies_not_supported&code=521ed056-2a81-4981-8668-fc67d5460580]
- 41. Human synapsin 1 gene promoter confers highly neuron -specific... [https://pubmed.ncbi.nlm.nih.gov/12595892/]
- 42. Insights Into the hsyn for Promoter -Specific... - Biology Insights Neuron [https://biologyinsights.com/insights-into-the-hsyn-promoter-for-neuron-specific-expression/]
- 43. Microglia-specific targeting by novel capsid-modified AAV6 vectors - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2329050116301681]
- 44. Simple and Highly Specific Targeting of Resident Microglia with Adeno-Associated Virus - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10760038/]
- 45. Microglia targeting by adeno-associated viral vectors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11257843/]
- 46. of AAV for Expression of Fluorescent Biosensors in Juvenile... Delivery [https://bio-protocol.org/en/bpdetail?id=4259&type=0]
- 47. Genetic manipulation of specific neural circuits by use of a viral vector system - PubMed [https://pubmed.ncbi.nlm.nih.gov/28058503/]
- 48. Scientists design gene delivery systems for cells in the brain and spinal cord | ScienceDaily [https://www.sciencedaily.com/releases/2025/05/250521124115.htm]
- 49. of the Delivery - Strategies Gene- CRISPR System for... Cas 9 Editing [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723556/]
- 50. Application of the CRISPR / Cas -based gene editing technique in basic... 9 [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-021-01431-6]
- 51. / CRISPR genome editing for neurodegenerative diseases - PMC Cas 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10450213/]
- 52. News: Explainer: What Are Base Editors and How Do They Work? - CRISPR Medicine [https://crisprmedicinenews.com/news/explainer-what-are-base-editors-and-how-do-they-work/]
- 53. From bench to bedside: cutting-edge applications of base editing and prime editing in precision medicine | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05957-3]
- 54. An optimized CRISPR / Cas approach for precise genome editing in... 9 [https://elifesciences.org/articles/65202]
- 55. / CRISPR Systems to Enhance Gene Cas Efficiency 9 Delivery Editing [https://www.preprints.org/manuscript/202503.2038]
- 56. An RNA-targeting CRISPR–Cas13d system alleviates disease-related phenotypes in Huntington’s disease models | Nature Neuroscience [https://www.nature.com/articles/s41593-022-01207-1]
- 57. A high-fidelity CRISPR-Cas13 system improves abnormalities associated with C9ORF72-linked ALS/FTD | Nature Communications [https://www.nature.com/articles/s41467-024-55548-5]
- 58. Base editing treats spinal muscular atrophy in mice | Broad Institute [https://www.broadinstitute.org/news/base-editing-treats-spinal-muscular-atrophy-mice]
- 59. tTARGIT AAVs mediate the sensitive and flexible manipulation of intersectional neuronal populations in mice | eLife [https://elifesciences.org/articles/66835]
- 60. Intersectional Targeting of Defined Neural Circuits by AAV Vectors - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8786212/]
- 61. A toolbox of Cre - dependent optogenetic... | Nature Neuroscience [https://www.nature.com/articles/nn.3078?error=cookies_not_supported&code=7963976a-1eb8-4710-b3c2-97667bb7b291]
- 62. Noninvasive optical activation of Flp recombinase for genetic ... [https://www.nature.com/articles/s41467-018-08282-8?error=cookies_not_supported&code=88a9cff0-7514-4e4b-b7ae-0844bcd3180b]
- 63. Noninvasive optical activation of Flp recombinase for genetic ... [https://pubmed.ncbi.nlm.nih.gov/30659191/]
- 64. of Adeno-associated Viral... | JoVE | Intracranial Injection Protocol [https://www.jove.com/cn/t/2140/intracranial-injection-of-adeno-associated-viral-vectors-video-jove]
- 65. Frontiers | Biodistribution of adeno-associated virus serotype... [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2014.00042/full]
- 66. Frontiers | Pre-clinical delivery of gene therapy products to the cerebrospinal fluid: challenges and considerations for clinical translation [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2023.1248271/full]
- 67. Intracisternal vs intraventricular injection of AAV1 result in comparable, widespread transduction of the dog brain | Gene Therapy [https://www.nature.com/articles/s41434-024-00510-9]
- 68. Scientists Design Gene Systems for Delivery Cells | NIH Record Neural [https://nihrecord.nih.gov/2025/07/04/scientists-design-gene-delivery-systems-neural-cells]
- 69. Gene Delivery [https://glab.caltech.edu/gene-delivery/]
- 70. Frontiers | Viral vectors in neurodegenerative diseases: immune ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1603125/full]
- 71. Immunogenicity of Recombinant Adeno-Associated Virus (AAV) Vectors for Gene Transfer | BioDrugs [https://link.springer.com/article/10.1007/s40259-023-00585-7]
- 72. Enhancing AAV gene therapy: Insights from Bayer’s immunogenicity... [https://www.gyrosproteintechnologies.com/spinblog/enhancing-aav-gene-therapy-insights-from-bayers-immunogenicity-testing-study]
- 73. B cell focused transient immune suppression protocol for efficient... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10911854/]
- 74. Exploring solutions for AAV R&D | News-Medical [https://www.news-medical.net/whitepaper/20240903/Exploring-solutions-for-AAV-RD.aspx]
- 75. Frontiers | Neurotherapeutics across blood–brain barrier: screening of... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1616144/full]
- 76. Double viral vector technology for selective manipulation of neural ... [https://www.nature.com/articles/s41434-020-00212-y?error=cookies_not_supported]
- 77. Computational Prediction of Blood-Brain Barrier Permeability Using Decision Tree Induction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6269008/]
- 78. Frontiers | DeePred-BBB: A Blood Brain Barrier Permeability Prediction Model With Improved Accuracy [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.858126/full]
- 79. Predicting blood–brain barrier permeability of molecules with a large language model and machine learning | Scientific Reports [https://www.nature.com/articles/s41598-024-66897-y]
- 80. Borneol, a novel agent that improves central nervous system drug... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8241164/]
- 81. Engineered human blood–brain barrier microfluidic model for vascular permeability analyses | Nature Protocols [https://www.nature.com/articles/s41596-021-00635-w]
- 82. - CRISPR : Mechanisms and Solutions | Danaher Life... Off Target Effects [https://lifesciences.danaher.com/us/en/library/crispr-off-target-effects.html]
- 83. -Cas9 CRISPR - Off : Challenges and Solutions Target Effects [https://www.azolifesciences.com/article/CRISPR-Cas9-Off-Target-Effects-Challenges-and-Solutions.aspx]
- 84. Latest Developed Strategies to Minimize the Off - Target in... Effects [https://pubmed.ncbi.nlm.nih.gov/32630835/]
- 85. ( Gene ) Editing : Rewriting... - GOWTHAM TECH CRISPR Guide 2025 [https://gowthamtech.com/gene-editing-crispr-guide/]
- 86. Screening CRISPR : A Step-by-Step Protocol - CD Genomics Guide [https://www.cd-genomics.com/biomedical-ngs/resource/crispr-screening-protocol-genetyping.html]
- 87. - Minimizing and Enhancing Off Precision... Target Effects Editing [https://www.linkedin.com/pulse/minimizing-off-target-effects-enhancing-editing-huang-md-phd-a8fje]
- 88. Taming microglia: the promise of engineered microglia in treating neurological diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785527/]
- 89. in neurodegenerative diseases: mechanism and potential... Microglia [https://www.nature.com/articles/s41392-023-01588-0?error=cookies_not_supported]
- 90. Directed evolution of adeno-associated virus for efficient gene delivery to microglia - PubMed [https://pubmed.ncbi.nlm.nih.gov/35879607/]
- 91. Optimizing AAV2/6 microglial targeting identified enhanced efficiency in the photoreceptor degenerative environment - PubMed [https://pubmed.ncbi.nlm.nih.gov/34703843/]
- 92. Biomarkers and therapeutic strategies targeting microglia in... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00867-4]
- 93. An AAV capsid proposed as microglia-targeting directs genetic expression in forebrain excitatory neurons - PubMed [https://pubmed.ncbi.nlm.nih.gov/40403726/]
- 94. Iterative transcription factor screening enables rapid generation of microglia-like cells from human iPSC | Nature Communications [https://www.nature.com/articles/s41467-025-59596-3]
- 95. A deep convolutional neural network for efficient microglia detection | Scientific Reports [https://www.nature.com/articles/s41598-023-37963-8]
- 96. A Role for Microglia in Retinal Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6705986/]
- 97. and virus dependent choice of promoters to... Injection parameters [https://www.nature.com/articles/gt201375?error=cookies_not_supported]
- 98. Cardiomyocyte-Specific Robust Following Systemic... Gene Expression [https://pmc.ncbi.nlm.nih.gov/articles/PMC2988989/]
- 99. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 100. Using Electrophysiology to Study Cardiac Arrhythmias: Tools and... [https://www.labx.com/resources/using-electrophysiology-to-study-cardiac-arrhythmias-tools-and-protocols/5625]
- 101. Stimulation Electrophysiology Protocols [https://www.numberanalytics.com/blog/electrophysiology-stimulation-protocols-guide]
- 102. Intracellular calcium for agonist screening imaging [https://www.biophysics-reports.org/article/doi/10.52601/bpr.2024.240026]
- 103. | Thermo Fisher Scientific - US Electrophysiology [https://www.thermofisher.com/us/en/home/references/protocols/neurobiology/neurobiology-protocols/electrophysiology.html]
- 104. Methodological Considerations for Optimizing and Validating Behavioral Assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054129/]
- 105. A comparative effectiveness trial of functional behavioral assessment methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843530/]
- 106. therapy for ALS: A review - PMC Gene [https://pmc.ncbi.nlm.nih.gov/articles/PMC8636154/]
- 107. Evolving AAV-delivered therapeutics towards ultimate cures | Journal of Molecular Medicine [https://link.springer.com/article/10.1007/s00109-020-02034-2]
- 108. Adeno-associated virus-mediated delivery of CRISPR-Cas9 for genome editing in the central nervous system - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8153090/]
- 109. -Targeting RNA /CasRx system relieves disease symptoms in... CRISPR [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-024-00794-w]
- 110. -guided transcriptional silencing in vivo... | Nature Communications RNA [https://www.nature.com/articles/s41467-018-04048-4?error=cookies_not_supported&code=0719ca49-2481-4219-8ee0-fdd160e86291]
- 111. Discovery and engineering of retrons for precise genome editing [https://www.nature.com/articles/s41587-025-02879-3?error=cookies_not_supported&code=d22dd084-3170-47f3-a8da-cceeccb3732d]
- 112. Scientists just made gene editing far more powerful | ScienceDaily [https://www.sciencedaily.com/releases/2025/10/251025084545.htm]
- 113. Simultaneous multi -site editing of individual genomes using retron ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11512673/]
- 114. – CRISPR : Pioneering Cas for Nucleic Acid... 13 RNA Editing [https://pmc.ncbi.nlm.nih.gov/articles/PMC11371277/]
- 115. CRISPR-Cas13d as a molecular tool to achieve targeted gene expression knockdown in chick embryos - PubMed [https://pubmed.ncbi.nlm.nih.gov/39622311/]
- 116. New one-step method to make multiple to a cell's edits genome [https://www.sciencedaily.com/releases/2024/07/240709184155.htm]
- 117. Efficient multi -site genome with editing -derived multitrons retron [https://www.news-medical.net/news/20240710/Efficient-multi-site-genome-editing-with-retron-derived-multitrons.aspx]
- 118. Preclinical evaluation of AAV 9-coSMN1 gene for therapy ... spinal [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01207-4]
- 119. for aromatic L-amino acid decarboxylase Gene by... therapy deficiency [https://pmc.ncbi.nlm.nih.gov/articles/PMC8275582/]
- 120. First brain-delivered AAV approved by... | Drug Discovery News therapy [https://www.drugdiscoverynews.com/first-brain-delivered-aav-therapy-approved-by-fda-16214]
- 121. Progress in AAV-Mediated In Vivo Gene Therapy and Its Applications in Central Nervous System Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899905/]
- 122. Optimization strategies and advances in the research and development of AAV‐based gene therapy to deliver large transgenes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10941601/]
- 123. In vivo applications and toxicities of AAV -based gene in rare... therapies [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03893-z]
- 124. AAV Tools for Neuroscience_AAVnerGene [https://aavnergene.com/2025/08/01/aav-as-a-tool-for-neuroscience-unlocking-the-brains-secrets/]