Neuroplasticity in Addiction: From Maladaptive Rewiring to Therapeutic Recovery
This article provides a comprehensive analysis of the dual role of neuroplasticity in substance use disorders, exploring both its contribution to addiction development and its potential as a mechanism for...
Neuroplasticity in Addiction: From Maladaptive Rewiring to Therapeutic Recovery
Abstract
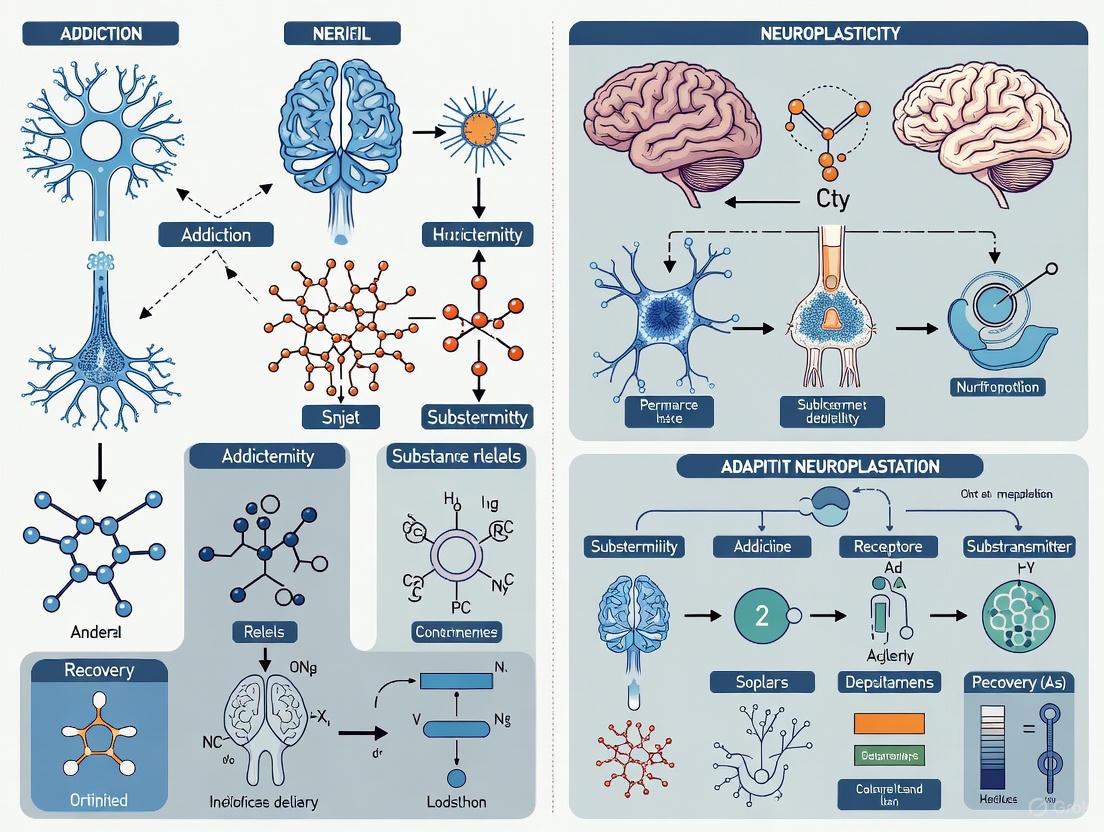
This article provides a comprehensive analysis of the dual role of neuroplasticity in substance use disorders, exploring both its contribution to addiction development and its potential as a mechanism for recovery. Aimed at researchers, scientists, and drug development professionals, it synthesizes foundational neuroscience with emerging methodological approaches. The content covers the brain's reward system hijacking, the addiction cycle, novel therapeutic targets like neuroinflammation and gasotransmitters, and advanced assessment tools such as high-content imaging and VEP-based biomarkers. It further evaluates comparative intervention strategies, discusses troubleshooting for translational challenges, and outlines future directions for biomarker development and non-canonical organ system research to guide next-generation therapeutics.
The Hijacked Brain: Foundational Mechanisms of Neuroplasticity in Addiction Pathology
Substance use disorders (SUDs) represent a critical challenge to global health, affecting millions of individuals worldwide and exerting a tremendous economic and social cost [1]. Traditional approaches to understanding addiction have often focused on its characterization as a personality disorder or moral failing. However, a more profound explanatory framework emerges when examining addiction through the lens of human evolution. This whitepaper posits that addiction arises from a fundamental mismatch between our ancient neurobiological wiring and our modern environment of abundant, potent rewards [2]. The very neural pathways and reward systems that evolved to ensure survival in environments of scarcity have been hijacked by contemporary substances and behaviors, creating a pervasive biological vulnerability.
This document will explore the evolutionary origins of this vulnerability, detailing the conserved brain systems involved. It will then delineate how modern research methodologies are uncovering the precise molecular and circuit-level mechanisms of addiction. Finally, within the context of a broader thesis on neuroplasticity, this review will chart a course for therapeutic development, arguing that the brain's inherent plasticity—the very substrate upon which addiction writes its damaging script—also provides the most promising avenue for recovery and lasting change.
Evolutionary Origins of a Vulnerable Brain
The Ancient Reward System
The human brain's reward circuitry is not a recent evolutionary development but a deeply conserved system shared across mammalian species and beyond. This system is primed to reinforce behaviors essential for survival and procreation, such as eating, drinking, and social bonding [2]. The mesolimbic dopamine pathway serves as the cornerstone of this system. Dopamine, originating in the ventral tegmental area (VTA) and projecting to the nucleus accumbens (NAc), mediates excitatory processes that promote focus, motivation, and the reinforcement of adaptive behaviors [3]. From an evolutionary standpoint, pursuing activities that release dopamine was, until recently, synonymous with pursuing behaviors critical for fitness.
The Co-Evolutionary Hypothesis: Archaeological evidence suggests a long and intertwined history between mammals and psychotropic plants. Receptor systems in the mammalian brain, such as the opioid receptor system, exist for plant substances not endogenously produced by the body [1]. This suggests a history of ecological interaction and co-evolution, where plants evolved psychoactive allelochemicals to deter herbivores, and mammalian brains, in turn, evolved receptor systems and metabolic pathways to interact with these compounds. In ancient environments, these substances were often mild and their availability limited, posing little risk of widespread addiction. They were sometimes viewed as food sources, providing nutritional value and conferring perceived advantages like increased energy and thermal tolerance [1].
The Modern World: An Environment of Abundance
The advent of global commerce and industrial chemistry has created an environment radically different from that in which our brains evolved. We are now inundated with highly refined substances and behaviors engineered to deliver a faster, more intense dopamine surge than anything encountered in nature [2]. This novel environment transforms a once-minor vulnerability into a significant liability.
As Dr. Keith Humphreys of Stanford Medicine notes, "We’ve got an old brain in a new environment... That vulnerability didn’t matter much for 99.9% of human evolution, until global commerce and industrial chemistry made highly addictive substances easy to access" [2]. The brain's ancient wiring, lacking a built-in regulatory system for such potent and readily available stimuli, is easily overwhelmed. The result is a cascade of maladaptive learning, where the brain begins to treat the substance as more important than basic needs like food, safety, or social connection [2].
Modern Experimental Approaches to an Ancient Problem
Contemporary research is dissecting the neurobiological consequences of this evolutionary mismatch using sophisticated tools. The following section details key experimental paradigms and findings.
Key Experimental Models and Findings
Recent studies have employed a multi-level approach to unravel the epigenetic and circuit-level mechanisms that underpin addiction vulnerability and relapse.
Table 1: Key Quantitative Findings from Recent Addiction Studies
| Study Focus | Experimental Model | Key Metric | Result | Implication |
|---|---|---|---|---|
| Epigenetic Regulation of Relapse [4] | Rat cocaine self-administration | Relapse-like cocaine seeking | HDAC5 limits Scn4b expression, reducing relapse. | Identified HDAC5/SCN4B as a selective target for cocaine relapse. |
| Structural Brain Recovery [5] | Human PET neuroimaging (Methamphetamine) | Dopamine transporter (DAT) density in striatum | Protracted abstinence recovered lost DATs. | Demonstrated the brain's capacity for neurochemical healing. |
| Lifestyle Intervention Efficacy [3] | Meta-analysis (22 studies, 1,487 participants) | Abstinence Rate (Odds Ratio) | OR = 1.69 (95% CI: 1.44, 1.99), p < .001. | Physical exercise significantly increases abstinence rates. |
Detailed Experimental Protocol: Epigenetic Mechanisms in Relapse
A seminal 2025 study by Wood et al. provides a robust model for investigating relapse mechanisms [4]. The methodology below outlines their comprehensive approach.
Objective: To determine the role of the epigenetic enzyme HDAC5 and the sodium channel auxiliary subunit gene Scn4b in regulating relapse-like drug seeking.
Materials and Methods:
- Animal Model: Adult rats are trained to self-administer intravenous cocaine or a natural reward (sucrose) by pressing a lever, modeling substance use and natural reward-seeking behaviors.
- Extinction Training: The lever press no longer delivers the reward, leading to a gradual reduction in the behavior.
- Relapse Test (Reinstatement): Following extinction, animals are exposed to drug-associated cues or contexts, and lever pressing is measured as a proxy for relapse.
- Multilevel Analysis:
- Molecular: Tandem mass spectrometry and enzymatic activity assays to measure HDAC5 function. Quantitative mRNA analysis to measure gene expression changes in the nucleus accumbens.
- Electrophysiological: Patch-clamp electrophysiology on neurons from the nucleus accumbens to measure changes in neuronal excitability following manipulation of HDAC5 or SCN4B.
- Computational: Modeling of sodium channel properties with and without the SCN4B subunit.
- Behavioral: Comparison of cocaine-seeking vs. sucrose-seeking behaviors following genetic or pharmacological manipulation of the HDAC5-SCN4B pathway.
Key Finding: The study revealed that HDAC5 exerts a protective effect by limiting the expression of Scn4b. The SCN4B protein, in turn, functions to limit the excitability of key neurons in the nucleus accumbens. This pathway selectively limits the formation of powerful, long-lasting drug-cue associations that trigger relapse, without affecting natural reward seeking [4]. This specificity makes the HDAC5-SCN4B axis a novel and promising therapeutic target.
The following diagram illustrates the experimental workflow and the core signaling pathway discovered in this study.
Neuroplasticity: The Double-Edged Sword
The brain's remarkable ability to change its structure and function in response to experience—neuroplasticity—is the central mechanism in both the development of and recovery from addiction [6].
Maladaptive Plasticity in Addiction Development
Repeated dopamine surges from drug use strengthen the connections between the drug-taking behavior, associated environmental cues, and the powerful dopamine response [3]. This process, known as synaptic plasticity, underlies the formation of strong, habit-like drug memories. Concurrently, the brain attempts to maintain homeostasis by downregulating dopamine receptors and their sensitivity, leading to a blunted response to natural rewards and a need for more of the drug to achieve the same effect (tolerance) [2]. This represents a maladaptive form of learning, where "someone might begin using a substance or behavior to have fun or solve a problem, but our brains adapt and we stop getting the same effect" [2]. These changes are further reinforced by neuroinflammation and alterations in other neurotransmitter systems, such as serotonin [3].
Harnessing Adaptive Plasticity for Recovery
The same neuroplasticity that enables addiction also facilitates recovery. The brain retains a lifelong capacity to rewire itself. The core of recovery involves fostering adaptive neuroplasticity to outcompete drug-related patterns [5].
Key Mechanisms of Recovery-Focused Plasticity:
- Structural and Functional Recovery: Longitudinal neuroimaging studies in humans show that with sustained abstinence, recovery occurs in key regions. This includes structural recovery in the prefrontal cortex, hippocampus, and cerebellum, and functional recovery of dopamine systems and other neurochemical pathways [5].
- Cognitive Restructuring: Therapies like Cognitive Behavioral Therapy (CBT) help individuals identify and reframe maladaptive thought patterns, effectively creating new, healthier neural pathways that reduce cravings and promote positive behaviors [6].
- Lifestyle Interventions: Specific, non-pharmacological interventions can directly promote healthy neuroplasticity.
- Physical Exercise: A meta-analysis of 22 studies showed exercise increases abstinence rates, reduces withdrawal symptoms, and alleviates co-occurring anxiety and depression [3]. Exercise stimulates neurotrophic factors and improves overall brain function.
- Social Connection: Positive social interactions and support groups stimulate oxytocin release, which reduces stress and promotes feelings of safety and trust, counteracting the isolation of addiction [6].
Table 2: Research Reagents for Studying Neuroplasticity in Addiction
| Reagent / Tool | Category | Primary Function in Research |
|---|---|---|
| Viral Vectors (e.g., AAV) | Molecular Biology | Used to overexpress or knock down genes (e.g., HDAC5, Scn4b) in specific brain regions to study their function. |
| Patch-Clamp Electrophysiology | Electrophysiology | Measures changes in neuronal excitability and synaptic strength in brain slices following drug exposure or manipulation. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetics | Allows precise remote control of specific neuronal populations to establish causal links between circuit activity and behavior. |
| PET/CT Radioligands (e.g., for DAT) | Neuroimaging | Enables quantification of protein targets like dopamine transporters in the living human brain to track disease progression and recovery. |
| Cocaine HCL | Pharmacological | The primary reinforcer in self-administration models to study addiction-like behavior and test potential therapies. |
The evolutionary perspective provides a powerful explanatory model for the pervasive vulnerability to addiction. Our brains, optimized for an ancient world, are biologically unprepared for the potent rewards of the modern era. This "old brain in a new environment" is susceptible to hijacking by substances that mimic, with unparalleled intensity, the neurochemical signals of fitness and survival.
The path forward, however, is not one of biological determinism. Research unequivocally demonstrates that the neuroplasticity which underwrites addiction also provides the substrate for healing. The focus of modern drug development must therefore shift towards leveraging this inherent plasticity. This involves a multi-pronged strategy: targeting specific molecular pathways like the HDAC5-SCN4B axis to selectively weaken drug memories [4]; developing pharmacological aids such as GLP-1 receptor agonists that may reduce the desire for substances [2]; and formally integrating evidence-based lifestyle interventions like exercise and social support into treatment paradigms to actively promote healthy neural rewiring [3] [5].
Viewing addiction through this dual lens of evolutionary mismatch and neuroplastic potential reframes the disorder. It is not a moral failure but a predictable, albeit tragic, consequence of our biology. By developing therapies that work in concert with the brain's innate capacity for change, we can create more effective, compassionate, and enduring solutions for recovery.
The transition from voluntary drug use to compulsive addiction represents a profound dysregulation of the brain's innate reward circuitry, driven by maladaptive neuroplasticity. This whitepaper examines the exploitation of the mesolimbic pathway through dopamine-mediated reinforcement and subsequent glutamatergic restructuring that establishes persistent addiction cycles. Beyond initial dopamine surges, the addiction process involves coordinated dysregulation of stress systems, executive control networks, and synaptic remodeling processes that vary by substance class. Current research reveals that these same neuroplastic mechanisms can be harnessed for recovery through targeted behavioral and pharmacological interventions. Understanding the hierarchical recruitment of neurotransmitter systems—from initial dopamine signals to enduring glutamate-mediated structural changes—provides critical insights for developing novel treatment strategies that address the full neurobiological scope of substance use disorders.
The brain's reward system evolved as a conserved neurobiological network to reinforce behaviors essential for survival, such as eating and social bonding. Central to this system is the mesolimbic dopamine pathway, comprising dopaminergic neurons originating in the ventral tegmental area (VTA) that project to the nucleus accumbens (NAc) in the basal ganglia [7] [8]. Under natural conditions, rewarding stimuli trigger moderate dopamine release in the NAc, creating pleasure sensations and reinforcing the associated behaviors through positive reinforcement mechanisms [7].
This reward processing system operates in concert with other brain regions, including:
- Prefrontal cortex (PFC): Mediates executive control, decision-making, and impulse regulation
- Amygdala: Processes emotional salience and associates cues with rewarding experiences
- Hippocampus: Encodes contextual information related to reward experiences [7] [9]
Drugs of abuse exploit this conserved reinforcement system by triggering disproportionate dopamine signaling—up to 10 times greater than natural rewards—which establishes powerful, maladaptive learning pathways [10]. The initial neurochemical effects vary by substance class, but all converge on the final common pathway of increased dopamine in the NAc, initiating a cascade of neuroadaptations that progressively shift control from voluntary to habitual and ultimately compulsive drug use [7].
Molecular Mechanisms of Reward Exploitation
Dopamine: The Primary Reward Signal
Dopamine serves as the principal neurotransmitter in reward processing, with its release in the nucleus accumbens constituting a conserved neural signal for reinforcement across species [7]. While early models emphasized dopamine's role in mediating pleasure ("liking"), contemporary research indicates its more crucial function involves incentive salience ("wanting")—the attribution of motivational importance to reward-predicting cues [7] [9]. This distinction explains why addicted individuals compulsously seek drugs despite reporting diminished pleasure from their use.
Drugs of abuse increase dopamine through diverse initial molecular targets, as detailed in Table 1, but ultimately converge on enhanced dopamine signaling in the mesolimbic pathway [7]. With repeated drug exposure, the brain adapts through downregulation of dopamine receptors and reduced basal dopamine activity, creating a hypodopaminergic state that diminishes sensitivity to natural rewards and creates negative emotional states during withdrawal [7] [9].
Table 1: Neuropharmacological Mechanisms of Major Drug Classes
| Drug Class | Primary Molecular Targets | Effect on Dopamine Transmission | Additional Neurotransmitters Involved |
|---|---|---|---|
| Opioids | Mu opioid receptors (MOR) | ↑ DA via disinhibition of VTA GABAergic neurons | Endogenous opioids, GABA |
| Stimulants | Dopamine transporter (DAT), VMAT2 | ↑ DA via reuptake blockade or reversal of DAT | Norepinephrine, serotonin |
| Alcohol | Multiple: GABAₐ, NMDA, MOR | ↑ DA via indirect VTA activation | GABA, glutamate, endogenous opioids |
| Nicotine | Nicotinic ACh receptors (α4β2) | ↑ DA via direct activation of VTA neurons | Acetylcholine, GABA |
| Cannabis | CB1 cannabinoid receptors | ↑ or ↓ DA via GABA/glutamate modulation | Endocannabinoids, GABA, glutamate |
Beyond Dopamine: Recruitment of Additional Neurotransmitter Systems
While dopamine initiates reward reinforcement, the transition to addiction involves progressively broader neurotransmitter system recruitment:
Glutamate mediates the learned associations between drug effects and environmental contexts through synaptic plasticity in corticostriatal circuits [7]. Chronic drug use triggers homeostatic synaptic scaling that strengthens glutamatergic signaling from prefrontal regions to the NAc, establishing automatic habitual responses to drug-associated cues [7] [11].
Stress neurotransmitters, including corticotropin-releasing factor (CRF), dynorphin, and norepinephrine, become hyperactive in the extended amygdala during withdrawal, creating a persistent negative emotional state termed hyperkatifeia (heightened negative emotional state) [9]. This hypersensitivity to stress and diminished reward function drives drug seeking through negative reinforcement—using drugs to relieve distressing states rather than to experience pleasure [9].
Endogenous opioid and cannabinoid systems contribute to both the hedonic effects of drugs and the regulation of stress responses [7]. The mu opioid receptor (MOR), for instance, is essential for the rewarding properties of not just opioids but also alcohol, cocaine, and nicotine [7].
Neuroplastic Adaptations in Addiction
The Three-Stage Addiction Cycle
Addiction progresses through a recurrent cycle with distinct neurobiological substrates, as conceptualized by Koob and Volkow [9]. Each stage involves specific brain regions, neurocircuits, and neurotransmitters that become progressively dysregulated:
Binge/Intoxication Stage: Substance use activates reward circuits in the basal ganglia, with dopamine, opioid peptides, GABA, and glutamate reinforcing the drug-taking behavior and establishing incentive salience [9]. With repetition, control shifts from voluntary action to habit formation in the dorsal striatum [7] [9].
Withdrawal/Negative Affect Stage: Cessation of drug use triggers hyperactivity in brain stress systems (CRF, dynorphin) within the extended amygdala, coupled with reduced reward function (dopamine depletion) [9]. The resulting hyperkatifeia—characterized by dysphoria, anxiety, irritability, and emotional pain—drives further drug use through negative reinforcement [9].
Preoccupation/Anticipation Stage: In this stage, executive function becomes dysregulated due to disrupted prefrontal cortex activity [9]. Glutamate-mediated cravings and impaired impulse control lead to compulsive drug seeking, particularly when triggered by stress, drug-associated cues, or negative emotional states [7] [9].
Molecular Signaling Pathways in Neuroplasticity
Chronic drug exposure induces synaptic remodeling through conserved molecular pathways. The diagram below illustrates key signaling cascades involved in addiction-related neuroplasticity:
The progression from initial drug use to addiction involves hierarchical recruitment of molecular pathways:
Drug-Receptor Interactions: Specific pharmacological targets vary by substance class (Table 1), but all ultimately increase VTA dopamine neuron activity [7].
Dopamine-Glutamate Interactions: Repeated dopamine surges potentiate glutamatergic transmission from prefrontal regions to the striatum, strengthening drug-associated cue responses [7].
Neurotrophic Signaling: Chronic administration induces brain-derived neurotrophic factor (BDNF) release, activating mTOR pathway signaling that promotes synaptogenesis and structural plasticity [12] [11].
Epigenetic Modifications: Persistent changes in gene expression through chromatin remodeling and DNA methylation create stable molecular memories of addiction [7].
These coordinated molecular adaptations result in the structural and functional brain changes that characterize addiction, including prefrontal hypofunction (impaired executive control), striatal hyperfunction (enhanced habit formation), and amygdala hyperreactivity (negative emotionality) [7] [9].
Experimental Methodologies in Addiction Neuroscience
Key Research Approaches
Addiction neuroscience employs diverse methodological approaches, each with specific applications and reporting standards [13]:
Quantitative Methods:
- Experimental designs: Randomized controlled trials testing pharmacological or behavioral interventions
- Observational studies: Cohort and cross-sectional studies examining addiction prevalence, risk factors, and natural history
- Neuroimaging: fMRI, PET, and structural MRI to identify brain changes associated with addiction
- Genetic studies: Genome-wide association studies (GWAS) and gene expression analyses to identify hereditary factors
Qualitative Methods:
- In-depth interviews: Exploring subjective experiences of addiction and recovery
- Focus groups: Examining social and contextual factors influencing drug use
- Phenomenological analysis: Understanding the lived experience of addiction
Mixed-Methods Approaches: Integrating quantitative and qualitative data to provide comprehensive insights into addiction phenomena [13].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Materials in Addiction Neuroscience
| Reagent/Material | Function/Application | Example Use Cases |
|---|---|---|
| Transgenic animal models | Genetic manipulation of specific neural pathways | Studying role of dopamine receptors, opioid receptors in reward processing |
| Radioligands for PET imaging | Quantifying receptor availability and occupancy | Measuring dopamine receptor density in human addicts |
| Receptor-specific agonists/antagonists | Pharmacological dissection of neurotransmitter systems | Testing candidate medications for addiction treatment |
| Viral vector systems (AAV, lentivirus) | Targeted gene delivery to specific cell populations | Circuit-specific manipulation of gene expression |
| Electrophysiology setups | Measuring neuronal activity and synaptic plasticity | Assessing LTP/LTD in reward circuits after drug exposure |
| Behavioral testing apparatus | Modeling addiction-like behaviors in animals | Self-administration, conditioned place preference paradigms |
| CRISPR-Cas9 systems | Precise genome editing | Validating candidate addiction-related genes |
Standardized Experimental Protocols
Self-Administration Paradigm:
- Purpose: Model compulsive drug seeking and taking in animals
- Procedure: Animals are surgically implanted with intravenous catheters and trained to perform an operant response (e.g., lever press) to receive drug infusions
- Key measures: Acquisition rate, breaking point under progressive ratio schedules, resistance to punishment, relapse during extinction
- Variations: Context-induced reinstatement, cue-induced reinstatement, stress-induced reinstatement
Conditioned Place Preference (CPP):
- Purpose: Measure drug reward and associative learning
- Procedure: Animals receive drug in one distinct context and vehicle in another; preference for drug-paired context is quantified
- Key measures: Time spent in drug-paired context, extinction rate, reinstatement
Quantitative Neuroimaging Protocol:
- Purpose: Identify structural and functional brain changes in human addicts
- Procedure: Acquisition of high-resolution structural MRI, resting-state fMRI, and task-based fMRI during cue exposure or decision-making tasks
- Key measures: Gray matter volume, functional connectivity, BOLD response to drug cues, diffusion tensor imaging of white matter integrity
Electrophysiological Recording in Brain Slices:
- Purpose: Measure synaptic plasticity in reward circuits
- Procedure: Prepare acute brain slices containing VTA, NAc, or PFC; record field EPSPs or whole-cell currents before and after drug application
- Key measures: Long-term potentiation (LTP), long-term depression (LTD), miniature excitatory/inhibitory postsynaptic current frequency and amplitude
Harnessing Neuroplasticity for Recovery and Treatment
The same neuroplastic mechanisms that underlie addiction present opportunities for intervention through targeted behavioral and pharmacological approaches:
Medication-Assisted Treatment (MAT) utilizes the neuroplastic capacity of the brain to normalize function [10] [14]. Opioid agonist therapies (e.g., methadone, buprenorphine) stabilize opioid systems, while antagonist therapies (e.g., naltrexone) block the rewarding effects of drugs, allowing extinction learning to occur [10].
Behavioral Therapies leverage experience-dependent neuroplasticity to establish alternative cognitive and behavioral patterns [14]. Cognitive Behavioral Therapy (CBT) teaches recognition and avoidance of drug-use triggers, while contingency management provides alternative reinforcement to strengthen abstinence-related behaviors [14].
Emerging Neuroplasticity-Based Interventions show promise for enhancing recovery outcomes. Psychedelic-assisted therapy using psilocybin or ketamine may promote rapid neuroplastic changes that disrupt maladaptive patterns [12]. These substances appear to stimulate BDNF-trKB signaling and mTOR-mediated synaptogenesis, potentially "resetting" addictive circuitry [12]. Neuromodulation approaches including transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS) directly target dysregulated circuits to restore functional balance [11].
Table 3: Neuroplasticity-Focused Treatment Approaches
| Treatment Approach | Proposed Mechanism of Action | Targeted Circuitry | Evidence Status |
|---|---|---|---|
| Cognitive Behavioral Therapy | Strengthens prefrontal top-down control; creates new learning to override drug associations | Prefrontal-striatal pathways | Strong efficacy evidence for multiple SUDs |
| Medication-Assisted Treatment | Stabilizes neurotransmitter systems; reduces reward from drug use and withdrawal severity | Dopamine, opioid, or stress systems | Gold standard for OUD and AUD |
| Contingency Management | Provides alternative reinforcement to compete with drug rewards; leverages dopamine prediction error signaling | Mesolimbic reward system | Highly effective for stimulant use disorders |
| Psychedelic-Assisted Therapy | Promotes rapid synaptogenesis; disrupts rigid patterns through altered belief systems | Cortico-striatal-thalamic circuits | Promising early results for AUD, tobacco |
| Transcranial Magnetic Stimulation | Modulates cortical excitability; enhances cognitive control and reduces craving | Prefrontal cortex projections to striatum | FDA-cleared for depression; investigational for SUD |
The exploitation of the brain's reward system in addiction represents a hierarchical recruitment of neurotransmitter pathways, beginning with dopamine-mediated reinforcement and progressing to glutamate-driven structural plasticity that establishes persistent addiction cycles. This understanding reframes addiction as a disorder of maladaptive learning and neuroplasticity, rather than simply a dopamine dysregulation syndrome.
Future research directions should focus on:
- Circuit-specific interventions that target defined neural populations rather than broad brain regions
- Personalized medicine approaches based on genetic, developmental, and environmental vulnerability factors
- Chronotherapeutic strategies that account for circadian influences on reward system function
- Combination therapies that simultaneously target multiple nodes of the addiction cycle
The expanding toolkit for investigating and manipulating neuroplastic mechanisms—from optogenetics and chemogenetics to circuit-specific neuromodulation—promises to revolutionize addiction treatment by targeting the specific neural adaptations that maintain substance use disorders. By understanding how the brain's reward system is exploited, we can develop more effective strategies to harness neuroplasticity for recovery.
Addiction is a chronic relapsing disorder characterized by a compulsion to seek and take a substance, loss of control over intake, and emergence of a negative emotional state during withdrawal [15]. Contemporary neurobiological research frames addiction as a disorder arising from pathological neuroadaptations within specific brain circuits, driven by the brain's inherent plasticity [9] [16]. The three-stage cycle—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—provides a heuristic model for understanding how these neuroadaptations escalate and perpetuate the disorder [17] [18]. This cycle worsens over time, involving a shift from positive to negative reinforcement and from impulsive to compulsive drug use [15]. The very plasticity that allows for the development of addiction also underpins the potential for recovery, as evidenced by the brain's ability to partially reverse these changes during sustained abstinence and through targeted interventions [9] [14].
Stage 1: Binge/Intoxication
The binge/intoxication stage is defined by the pleasurable or rewarding effects of a substance, which positively reinforce its use and initiate the addiction cycle [17] [18]. This stage is primarily associated with neuroplasticity within the basal ganglia, a key node of the brain's reward circuit [16].
Core Neurocircuitry and Neurotransmitters
The rewarding effects are largely mediated by the mesolimbic dopamine pathway, which projects from the ventral tegmental area (VTA) to the nucleus accumbens (NAcc) [8]. Drugs of abuse cause a rapid and steep increase in dopamine release in the NAcc, which is critical for the subjective "high" and for triggering conditioned responses [15]. This surge preferentially stimulates low-affinity dopamine D1 receptors, which are necessary for drug reward [15]. Concurrently, other neurotransmitters contribute to the hedonic experience; for instance, alcohol activates opioid receptors in the NAcc, contributing to its pleasurable effects [9].
Key Neuroadaptive Changes
With repeated cycling, the brain undergoes significant plasticity in the basal ganglia:
- Incentive Salience: Dopamine firing patterns shift from responding to the drug itself to anticipating drug-related cues (e.g., people, places, paraphernalia) [17]. This process, known as incentive salience, attaches powerful motivational value to these cues, transforming them into potent triggers for drug seeking [9].
- Habit Formation: Control over drug-seeking behavior progressively shifts from the ventral striatum (reward) to the dorsal striatum [17] [16]. This transition from goal-directed action to habitual responding is a core component of compulsion, making the behavior automatic and difficult to suppress [9].
Table 1: Key Neurotransmitter Systems in the Binge/Intoxication Stage
| Neurotransmitter/System | Change | Primary Brain Region | Functional Role |
|---|---|---|---|
| Dopamine | Increase [15] | VTA, NAcc [8] | Reward, reinforcement, incentive salience [9] |
| Opioid Peptides | Increase [15] | NAcc [9] | Pleasure, euphoria [9] |
| GABA | Increase [15] | VTA, Basal Ganglia | Modulation of dopamine neuron activity |
| Glutamate | Increase [15] | Dorsal Striatum [15] | Habit formation and synaptic plasticity [16] |
Figure 1: Neurocircuitry of the Binge/Intoxication Stage. Substance use activates the VTA, leading to dopamine release in the NAcc and opioid peptide release within the NAcc itself. Repeated exposure drives plasticity that establishes incentive salience and shifts behavioral control to the dorsal striatum, promoting habit formation.
Stage 2: Withdrawal/Negative Affect
The withdrawal/negative affect stage emerges when drug use ceases or is reduced, leading to a pronounced negative emotional state termed hyperkatifeia (a hypersensitivity to negative emotional states) [9]. This stage is driven by a combination of reward deficits and the recruitment of brain stress systems, primarily within the extended amygdala [17] [16].
Core Neurocircuitry and Neurotransmitters
This stage is defined by two major neuroadaptations:
- Within-System Neuroadaptation: Chronic drug use leads to a hypofunctioning of the brain's reward systems. There is a decrease in dopaminergic tone in the NAcc and a shift in the glutamate-GABA balance towards increased excitatory tone, leading to diminished pleasure from the drug and from natural rewards (anhedonia) [17].
- Between-Systems Neuroadaptation: The extended amygdala, comprising the bed nucleus of the stria terminalis (BNST), central amygdala (CeA), and a part of the NAcc shell, becomes hyperactive [17] [16]. This "anti-reward" system is upregulated, leading to increased release of stress neurotransmitters [17].
Table 2: Key Neurotransmitter Systems in the Withdrawal/Negative Affect Stage
| Neurotransmitter/System | Change | Primary Brain Region | Functional Role |
|---|---|---|---|
| Dopamine | Decrease [15] | NAcc [17] | Anhedonia, low reward |
| CRF | Increase [15] | Extended Amygdala [17] | Anxiety, stress response |
| Dynorphin | Increase [15] | Extended Amygdala [17] | Dysphoria, stress |
| Norepinephrine | Increase [15] | Extended Amygdala | Anxiety, arousal |
| Neuropeptide Y | Decrease [15] | Extended Amygdala | Reduced anti-stress buffer |
| Endocannabinoids | Decrease [15] | Extended Amygdala | Reduced anti-stress buffer |
Key Neuroadaptive Changes
The plasticity in this stage manifests as a persistent change in emotional set point:
- Allostatic Load: The chronic overactivation of stress systems and underactivation of reward systems creates an allostatic state—a dysregulated emotional baseline that is lower than pre-addiction levels [16]. This state of persistent distress is a major driver of relapse via negative reinforcement, where the individual seeks the drug not for pleasure but to alleviate the misery of withdrawal [9] [17].
- Loss of Anti-Stress Buffers: Systems that normally buffer stress, such as neuropeptide Y, nociceptin, and endocannabinoids, are downregulated, further tilting the balance towards a negative emotional state [17] [15].
Figure 2: Neurocircuitry of the Withdrawal/Negative Affect Stage. Abstinence triggers a reward deficit and activates the extended amygdala, leading to a surplus of stress. The convergence of these processes produces hyperkatifeia, which motivates further drug use through negative reinforcement.
Stage 3: Preoccupation/Anticipation
The preoccupation/anticipation (or "craving") stage involves the persistent desire for the drug and a high risk of relapse, even after prolonged abstinence [15] [18]. This stage is characterized by deficits in executive function and is primarily associated with dysregulation of the prefrontal cortex (PFC) and its connections to the basal ganglia and extended amygdala [9] [16].
Core Neurocircuitry and Neurotransmitters
The PFC, responsible for executive functions like impulse control, decision-making, and emotional regulation, becomes compromised in addiction [9] [18]. Two key systems within the PFC are implicated:
- "Go" System: Involves the dorsolateral PFC and anterior cingulate, driving goal-directed behaviors. In addiction, this system may become hyperactive towards drug-seeking goals [17].
- "Stop" System: Exerts inhibitory control over impulses. This system is hypoactive in addiction, reducing the ability to resist cravings [17]. The primary neurotransmitter implicated in cravings is glutamate. Projections from the PFC to the NAcc and extended amygdala, using glutamate, can trigger intense urges to use drugs in response to cues, stress, or the drug itself [15].
Key Neuroadaptive Changes
- Executive Dysfunction: The PFC shows reduced activation, leading to poor judgment, impaired impulse control, and an inability to regulate the powerful motivational drives generated in the earlier stages of the cycle [9] [18].
- Cue-Reactivity: Environmental cues previously associated with drug use can activate a distributed network including the orbitofrontal cortex, basolateral amygdala, hippocampus, and insula, triggering intense cravings and preoccupation with drug seeking [16]. The insula, in particular, is involved in interoceptive awareness of these craving states [15].
Table 3: Key Neurotransmitter Systems in the Preoccupation/Anticipation Stage
| Neurotransmitter/System | Change | Primary Brain Region | Functional Role |
|---|---|---|---|
| Glutamate | Increase [15] | PFC to NAcc/Amygdala [15] | Craving, relapse |
| Dopamine | Increase [15] | PFC, Striatum | Motivation for drug seeking |
| Corticotropin-Releasing Factor | Increase [15] | PFC, Extended Amygdala | Stress-induced craving |
Experimental Models and Methodologies
To study the neuroplasticity underlying the addiction cycle, researchers employ a range of sophisticated animal models and experimental protocols that mirror the human condition.
Key Behavioral Paradigms
- Drug Self-Administration (Binge/Intoxication): Animals are trained to perform an operant response (e.g., pressing a lever) to receive an intravenous infusion of a drug [15] [19]. This model directly assesses the reinforcing properties of drugs. "Escalation of intake" models, where animals have extended access to the drug, are used to model the transition from controlled use to binge-like and compulsive use [16].
- Conditioned Place Preference (Binge/Intoxication): A non-operant model where one environment is paired with the drug and another with saline. The animal's subsequent preference for the drug-paired environment is used to measure the rewarding effects of the drug [19].
- Reinstatement Models (Preoccupation/Anticipation): After self-administration training and subsequent extinction of the drug-seeking behavior, the reemergence of drug seeking is triggered by: 1) a priming injection of the drug (drug-induced reinstatement), 2) exposure to drug-associated cues (cue-induced reinstatement), or 3) exposure to a stressor (stress-induced reinstatement) [15] [19]. This is a primary model for studying relapse.
- Motivational Measures of Withdrawal (Withdrawal/Negative Affect): The elevated plus maze, light-dark box, and measures of intracranial self-stimulation thresholds are used to quantify anxiety-like behavior and anhedonia during acute and protracted withdrawal [16] [19].
Neurobiological Assessment Techniques
- Chemogenetics (DREADDs) & Optogenetics: These techniques allow for the precise, reversible control of specific neuronal populations or pathways. For example, researchers can inhibit or activate glutamatergic projections from the PFC to the NAcc during a reinstatement test to determine their causal role in relapse [16].
- In Vivo Electrophysiology: This involves recording the electrical activity of neurons (e.g., in the VTA or NAcc) in behaving animals during different stages of the addiction cycle to understand how firing patterns change with addiction development [15].
- Microdialysis and Electrochemistry: These techniques are used to measure transient changes in neurotransmitter levels (e.g., dopamine, glutamate) in specific brain regions in real-time during drug intake, withdrawal, or cue exposure [15].
Table 4: Research Reagent Solutions for Studying Addiction Neurocircuitry
| Reagent / Tool | Category | Primary Function in Research |
|---|---|---|
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetics | Allows remote, reversible control of specific neuronal circuits; e.g., to inhibit a stress circuit during withdrawal. |
| Channelrhodopsin (ChR2) | Optogenetics | Allows millisecond-timescale activation of specific neurons or pathways with light; e.g., to stimulate dopamine neurons. |
| CREB Transgenic Mice | Genetic Models | Used to study the role of the transcription factor CREB in the extended amygdala in regulating negative affect. |
| Fast-Scan Cyclic Voltammetry (FSCV) | Neurochemistry | Provides real-time, second-by-second measurement of dopamine release in awake, behaving animals. |
| CX546 (AMPA Receptor Potentiator) | Pharmacological Probe | Used to test the hypothesis that potentiating glutamate signaling in the accumbens can reduce relapse. |
| CRF Receptor Antagonists | Pharmacological Probe | Used to test the role of CRF in stress-induced reinstatement and withdrawal-induced negative affect. |
Figure 3: Generalized Experimental Workflow. A typical protocol for establishing a causal link between a neural circuit and a behavior. After training an animal in a relevant paradigm, a specific circuit is manipulated during a behavioral test, and subsequent tissue analysis can reveal molecular correlates.
Implications for Therapeutic Development
The three-stage model and its underlying neuroplasticity mechanisms provide a robust framework for developing novel treatment strategies. The goal is to reverse or compensate for the specific neuroadaptations in each stage [18].
- Targeting the Binge/Intoxication Stage: Medications that block the rewarding effects of drugs (e.g., opioid receptor antagonists like naltrexone) can be effective by reducing the positive reinforcement that initiates the cycle [9]. Vaccines that generate antibodies to sequester the drug in the bloodstream, preventing it from reaching the brain, are also under investigation.
- Targeting the Withdrawal/Negative Affect Stage: A major therapeutic focus is on dampening the overactive brain stress systems. CRF receptor antagonists, nociceptin agonists, and neuropeptide Y enhancers are being explored to alleviate the negative emotional state that drives negative reinforcement [17] [15].
- Targeting the Preoccupation/Anticipation Stage: Strategies here aim to restore executive control and reduce cravings. N-acetylcysteine, which normalizes glutamatergic transmission at the cystine-glutamate exchanger, has shown promise in reducing craving and relapse in clinical trials [15]. Non-invasive brain stimulation (e.g., TMS) of the PFC is being tested to enhance cognitive control. Furthermore, behavioral therapies like Cognitive Behavioral Therapy (CBT) and contingency management leverage neuroplasticity to help patients form new, healthier neural pathways and coping strategies [14].
The brain's inherent neuroplasticity means that these interventions, combined with sustained abstinence, can promote recovery. The reversal of drug-induced changes, such as the potential normalization of neurogenesis in the hippocampus and prefrontal cortex through exercise and environmental enrichment, represents a promising avenue for promoting long-term resilience against relapse [19] [14].
Addiction is understood as a chronic brain disorder characterized by specific neuroadaptations that fundamentally alter motivational processes and behavioral control [17] [20]. The transition from voluntary substance use to compulsive addiction represents a cascade of neuroplastic changes that reorganize brain circuits responsible for reward, motivation, and executive function [16]. This progression follows a recognizable three-stage cycle—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—each mediated by distinct but interacting neural circuits [17] [16]. Central to this transition is the shift from incentive salience attribution, which generates pathological "wanting," to habit formation, which establishes compulsive drug-seeking behaviors that persist despite adverse consequences [21] [22]. Understanding these mechanisms provides critical insights for developing targeted interventions that address the specific neurobiological processes underlying addiction.
Neurobiological Mechanisms of Incentive Salience
Theoretical Foundations and Neural Substrates
Incentive salience is defined as a form of motivationally-charged "wanting" that is distinct from both hedonic "liking" and cognitive forms of desire [21] [23]. According to the incentive-sensitization theory, repeated drug use sensitizes mesocorticolimbic dopamine systems, resulting in pathological levels of incentive salience attribution to drugs and drug-associated stimuli [21] [22]. This neural sensitization produces compulsive drug "wanting" that can occur independently of conscious desire or even in opposition to cognitive goals [21].
The primary neural circuit for incentive salience involves mesocorticolimbic dopamine pathways originating in the ventral tegmental area (VTA) and projecting to the nucleus accumbens (NAc), with additional contributions from the amygdala, ventral pallidum, and prefrontal cortex [23] [24]. Dopamine release in this circuit, particularly phasic dopamine signaling, attributes motivational value to reward-predictive cues, making them attention-grabbing and attractive [21] [23]. Importantly, this "wanting" system is neurobiologically distinct from "liking" systems, which involve smaller hedonic hotspots in the NAc and ventral pallidum that utilize opioid and endocannabinoid signaling [21].
Molecular Mechanisms and Sensitization
At the molecular level, repeated drug exposure induces neuroadaptations that enhance dopamine reactivity to drug-associated stimuli. These include:
- Increased sensitivity of D1 receptors and reduced availability of D2 receptors in the striatum [23]
- Synaptic plasticity in medium spiny neurons of the NAc, including increased dendritic length and spine density [23]
- Enhanced glutamatergic signaling from prefrontal cortex and amygdala to the VTA and NAc, regulating dopamine neuron burst firing [23]
These changes create a hypersensitive dopamine system that responds excessively to drug cues, generating powerful motivation to seek and consume drugs [22]. Sensitization can persist long after drug cessation, contributing to the chronic relapse risk characteristic of addiction [22].
The Transition to Habitual Compulsive Use
Neurocircuitry of Habit Formation
As addiction progresses, behavioral control shifts from goal-directed actions to habitual responses mediated by different neural circuits. This transition involves a progression from ventral to dorsal striatal control [16] [24]. Early drug use primarily engages the mesolimbic pathway (VTA to NAc), which mediates the rewarding effects of substances and initial incentive salience attribution [24]. With repeated use, control shifts to the nigrostriatal pathway (substantia nigra to dorsolateral striatum), which mediates habit formation and automatic behaviors [24].
This neural reorganization is reflected in two distinct corticostriatal loops [25]:
- The associative loop (prefrontal cortex and orbitofrontal cortex to dorsomedial striatum) supports goal-directed behavior
- The sensorimotor loop (sensorimotor cortex to dorsolateral striatum) supports habitual behavior
As drug use escalates, the sensorimotor loop dominates behavioral control, leading to compulsive drug-seeking that is triggered automatically by environmental cues without regard to consequences [25].
Behavioral Manifestations of the Transition
The shift from incentive salience to habit is marked by specific behavioral changes:
- Progression from impulsive to compulsive use despite negative consequences [17]
- Reduced behavioral flexibility and persistence of drug-seeking even when rewards are devalued [25] [22]
- Context-dependent automaticity where drug-associated cues trigger drug-seeking behaviors without conscious intent [25]
This transition explains key clinical features of addiction, including the resourcefulness of addicts in obtaining drugs (incentive salience) and the ritualized patterns of drug consumption once obtained (habits) [22].
Experimental Approaches and Methodologies
Behavioral Paradigms for Measuring Incentive Salience and Habits
Table 1: Behavioral Paradigms for Studying Addiction Transitions
| Paradigm | Purpose | Key Measures | Neural Correlates |
|---|---|---|---|
| Sign-tracking vs Goal-tracking | Measures incentive salience attribution | Approach to cue (sign-tracking) vs reward location (goal-tracking) | Dopamine release in NAc; individual variation in vulnerability [23] |
| Reward Devaluation | Assesses habitual vs goal-directed behavior | Persistence of responding after reward devaluation | Dorsolateral striatum activity (habits) vs medial prefrontal cortex (goal-directed) [25] |
| Contingency Degradation | Determines action-outcome vs stimulus-response learning | Response rate when action-outcome contingency is disrupted | Shift from ventral to dorsal striatal control [25] |
| Conditioned Place Preference | Measures drug-context associations | Time spent in drug-paired context | Mesolimbic dopamine system activation [16] |
| Self-administration with Reinstatement | Models relapse behavior | Drug-seeking after extinction in response to cues, stress, or primes | Prefrontal cortex, amygdala, and dopamine system engagement [16] |
Neurobiological Assessment Techniques
Table 2: Neurobiological Methods for Studying Addiction Transitions
| Method | Application | Key Findings in Addiction |
|---|---|---|
| Fast-Scan Cyclic Voltammetry | Measures real-time dopamine dynamics | Phasic dopamine signals to drug cues; sensitized responses after repeated drug exposure [24] |
| Chemogenetics (DREADDs) | Circuit-specific manipulation | Causal roles for specific pathways; VTA-NAc circuit in incentive salience; nigrostriatal circuit in habits [24] |
| Optogenetics | Precise temporal control of neural activity | Direct activation of dopamine neurons reinforces behavior; mimics drug effects [24] |
| fMRI/PET Imaging | Human brain activity and receptor quantification | Reduced D2 receptors in striatum; enhanced reactivity to drug cues in striatum and PFC [20] [23] |
| Electrophysiology | Neuronal firing patterns | Altered firing rates and patterns in VTA and striatum after chronic drug exposure [16] |
Research Reagent Solutions
Table 3: Essential Research Reagents for Addiction Neuroscience
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Dopaminergic Compounds | SCH23390 (D1 antagonist), Eticlopride (D2 antagonist) | Receptor-specific manipulation of dopamine signaling; dissecting roles in "wanting" vs "liking" [23] |
| Optogenetic Tools | Channelrhodopsin (ChR2), Halorhodopsin (NpHR) | Precise temporal control of specific neuronal populations in addiction circuits [24] |
| Chemogenetic Receptors | DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Remote control of neuronal activity in specific circuits over longer time scales [24] |
| Genetic Models | Cre-Lox system, DAT-Cre, D1-Cre, D2-Cre mice | Cell-type specific manipulation of medium spiny neurons in striatal pathways [24] |
| Sensitization Protocols | Repeated amphetamine or cocaine administration | Induction of behavioral and neural sensitization; modeling transition to addiction [22] |
| Viral Vectors | AAVs for gene delivery, Ca²⁺ indicators (GCaMP) | Circuit mapping and monitoring neuronal activity during behavior [24] |
Visualization of Neurocircuitry Transitions
Three-Stage Addiction Cycle Neurocircuitry
Transition from Goal-Directed to Habitual Behavior
Incentive Sensitization Mechanism
Implications for Therapeutic Development
Understanding the transition from incentive salience to habit formation provides critical insights for developing targeted addiction treatments. Effective interventions must address both the sensitized "wanting" driven by dopamine systems and the compulsive habits mediated by dorsal striatal circuits [23] [22]. Potential approaches include:
- Pharmacological interventions that target specific dopamine receptor subtypes to reduce cue-triggered craving without affecting natural reward processing [23]
- Cognitive training to enhance prefrontal cortical control over sensitized incentive salience and habitual responses [25]
- Cue exposure therapy to extinguish the learned associations between drug cues and motivational states [23]
- Mindfulness-based interventions that reduce activity in the subgenual anterior cingulate cortex and ventral striatum during cue exposure [23]
Future research should focus on developing circuit-specific interventions that can reverse the neuroadaptations underlying incentive sensitization and habit formation while preserving adaptive learning and motivation [24].
The transition from incentive salience to habit represents a fundamental reorganization of brain circuits that drives the development of compulsive drug use. This progression involves neuroplastic changes across multiple brain regions, beginning with sensitization of mesolimbic dopamine systems that generate pathological "wanting" for drugs and culminating in a shift to dorsal striatal control that establishes automatic, habitual drug-seeking behaviors [16] [22]. Understanding these mechanisms provides a framework for developing targeted interventions that address the specific neurobiological processes underlying different stages of addiction. Future research using increasingly precise circuit-manipulation tools will continue to elucidate these transitions, potentially identifying new opportunities for therapeutic intervention that can restore behavioral control and reduce relapse in addiction.
Addiction is a complex, chronic relapsing disorder conceptualized as a neuroplasticity-driven process involving maladaptive learning within the brain's reward circuitry [26] [14]. Vulnerability to developing a substance use disorder is not predetermined but arises from the dynamic interplay of an individual's genetic makeup and their lifetime exposure to environmental factors [27]. This interaction governs the transition from voluntary, recreational drug use to compulsive, habitual drug-seeking and taking, which is the hallmark of addiction [16]. Understanding these risk factors is paramount for researchers and drug development professionals aiming to develop targeted interventions that can bolster resilience and mitigate vulnerability. This technical guide provides an in-depth analysis of the genetic and environmental determinants of addiction, framed within the context of neuroplasticity, and details the experimental methodologies used to investigate them.
Genetic Risk Factors
Genetic predispositions account for a substantial portion of the risk for addiction, with heritability estimates explaining 40–70% of the population's variability in developing a substance use disorder [27] [8]. These genetic influences are highly polygenic, involving variations in numerous genes that affect the brain's reward, stress, and self-control systems.
Key Genetic Associations and Polymorphisms
Table 1: Key Genetic Variations Associated with Addiction Vulnerability
| Gene/Polymorphism | Function/Pathway | Associated Phenotype | Effect Size/OR (if provided) |
|---|---|---|---|
| DRD2 Taq1A (rs1800497) | Dopamine D2 Receptor Density [27] | General Addiction Vulnerability [27] | A1 allele associated with lower D2 receptor density [27] |
| Alcohol-Metabolizing Genes (e.g., ADH, ALDH) | Ethanol Metabolism [27] | Alcohol Use Disorder [27] | Not Specified |
| Serotonin Transporter Genes | Serotonergic Signaling [27] | Response to Stress, Impulsivity [27] | Not Specified |
| Dopaminergic & Opioid System Genes | Reward Processing [27] | Specific Substance Addictions [27] | Not Specified |
Genome-wide association studies (GWAS) have identified specific single nucleotide polymorphisms (SNPs) linked to addiction. The most well-replicated finding is the A1 allele of the Taq1A polymorphism near the DRD2 gene, which codes for the dopamine D2 receptor. Individuals carrying this allele exhibit a lower density of D2 receptors in the striatum, a condition associated with a higher risk for various addictions and reduced sensitivity to natural rewards [27]. Beyond dopaminergic pathways, genes influencing the serotonergic system (e.g., serotonin transporters) are linked to impulse control, a key risk factor, while genes for alcohol-metabolizing enzymes (e.g., ADH, ALDH) significantly influence the risk for alcohol use disorder [27].
The Role of Epigenetics
Gene expression is dynamically regulated by epigenetic mechanisms, which are themselves influenced by environmental exposures. DNA methylation and histone modification are the most studied epigenetic alterations in addiction research [27]. Repeated stressful life events or drug exposure can cause stable epigenetic changes, altering the expression of genes critical for neuroplasticity and stress response without changing the underlying DNA sequence [27]. For instance, downregulation of the G9a histone methyltransferase in the nucleus accumbens has been linked to resilient phenotypes in animal models of chronic stress [27]. Furthermore, paternal and maternal experiences, such as stress, can induce epigenetic changes that are heritable and alter the offspring's hypothalamic-pituitary-adrenal (HPA) axis response to stress, thereby influencing vulnerability across generations [27].
Environmental Risk Factors
Environmental factors modulate genetic risk and can directly instigate neuroplastic changes that predispose an individual to addiction. These factors operate across the lifespan, from early childhood to adulthood.
Table 2: Environmental Risk and Resilience Factors
| Category | Risk Factors | Resilience/Protective Factors |
|---|---|---|
| Social & Early Life | Childhood Adversity [27]; Low Socioeconomic Status [27]; Parental Neglect [8] | High Parental Monitoring [27]; Higher Level of Education [27]; Strong Social Support [27] [8] |
| Psychological & Behavioral | Preexisting Mental Illness [27] [8]; High Stress [8]; Trauma/PTSD [8] | Effective Coping Styles [27]; Impulse Control [27] |
| Substance-Specific | Early Drug Exposure [27]; High Drug Availability [27] | Not Specified |
Key environmental risk factors include:
- Childhood Adversity and Stress: Exposure to trauma, neglect, or chronic stress during development is a powerful risk factor. These experiences can cause epigenetic changes and dysregulate the brain's stress and reward pathways, increasing vulnerability to drugs as a coping mechanism [27] [8].
- Social and Economic Factors: Lower levels of education, socioeconomic status, and a lack of social support are correlated with increased risk. Conversely, parental monitoring during adolescence has been shown to attenuate genetic risk, as demonstrated in twin studies on smoking [27].
- Preexisting Mental Health Conditions: Comorbid conditions such as depression, anxiety, and PTSD significantly increase vulnerability, often leading to self-medication with substances [8].
- Drug Availability and Exposure: The nature of the addictive agent itself, including its pharmacokinetics and psychoactive potency, influences its addictive potential [27].
Neurobiological Pathways and Neuroplasticity
The convergence of genetic and environmental risk factors leads to enduring neuroplastic changes in specific brain circuits, driving the transition to addiction. The disorder is characterized by a three-stage cycle—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—each mediated by distinct but overlapping neurocircuitry [8] [16].
The Reward System and Dopaminergic Pathway
The mesolimbic dopamine pathway, originating in the ventral tegmental area (VTA) and projecting to the nucleus accumbens (NAc), is the cornerstone of the brain's reward system [27] [8]. All addictive substances directly or indirectly increase dopamine in the NAc, producing pleasure and reinforcing drug-taking behavior. With repeated use, neuroplasticity occurs: the brain adapts by reducing natural dopamine production and D2 receptor sensitivity, leading to tolerance [8] [26]. This creates a hypo-dopaminergic state where the individual no longer experiences pleasure from the drug or natural rewards, requiring more substance just to feel normal [27].
The Glutamatergic Pathway and Synaptic Plasticity
Chronic drug use profoundly disrupts glutamate homeostasis, which is critical for learning and memory. The transition from goal-directed to habitual drug-seeking involves a shift in control from the ventral to the dorsal striatum, mediated by glutamatergic projections [26] [16]. Key neuroadaptations include:
- Reduced basal glutamate levels in the NAc.
- Potentiated synaptic glutamate release during drug cue exposure.
- An increased ratio of AMPA to NMDA receptors at synapses in the NAc, stabilizing strong cue-drug associations [26]. These changes disrupt normal synaptic plasticity, such as long-term potentiation (LTP) and long-term depression (LTD), underlying the persistence of addictive memories [26].
The Stress and Executive Control Systems
The withdrawal/negative affect stage is primarily mediated by the extended amygdala and its stress neurotransmitters, such as corticotropin-releasing factor (CRF) [16]. This generates the anxiety, dysphoria, and irritability that drive negative reinforcement (using the drug to avoid withdrawal). The preoccupation/anticipation stage involves a widely distributed network including the prefrontal cortex (PFC), orbitofrontal cortex (OFC), anterior cingulate, and hippocampus [8] [16]. Addiction is associated with prefrontal hypofunction, which impairs executive functions, decision-making, and impulse control, making it difficult to resist cravings and drug-related cues [8].
Experimental Protocols and Methodologies
Research into the genetic and neurobiological basis of addiction relies on a combination of human studies and controlled animal models.
Key Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application in Research |
|---|---|
| N-acetylcysteine | A cystine prodrug used to restore glutamate homeostasis via cystine-glutamate exchange in the NAc; tested to reduce drug-seeking in animals and humans [26]. |
| Ceftriaxone | An antibiotic that upregulates glutamate transporter 1 (GLT-1), increasing glutamate uptake and shown to prevent reinstatement of drug-seeking in rodents [26]. |
| Raclopride (³H-labeled) | A radioactive dopamine D2/D3 receptor antagonist used in positron emission tomography (PET) and in vitro binding assays to quantify receptor availability and dopamine release [26]. |
| Brain-Derived Neurotrophic Factor (BDNF) Assays | ELISA and other immunoassays to measure levels of this key growth factor, which increases during incubation of craving in reward areas [26]. |
| Delta FosB Antibodies | Immunohistochemistry and Western Blotting to detect and quantify this stable transcription factor, which accumulates in the NAc and striatum after chronic drug exposure and regulates plasticity genes [26]. |
Protocol: Conditioned Place Preference (CPP)
Objective: To measure the rewarding effects of a substance by assessing the development of an association between the drug effects and a specific environment.
- Apparatus: A rectangular box divided into two or more distinct compartments with unique visual and tactile cues.
- Pre-Test: Mice/rats are allowed to freely explore the entire apparatus. The time spent in each compartment is recorded to establish a baseline preference.
- Conditioning: Over several days, animals are injected with the drug of abuse and confined to one compartment. On alternate days, they are injected with saline and confined to the other compartment.
- Post-Test: Animals are again allowed free access to all compartments while in a drug-free state. A significant increase in time spent in the drug-paired compartment compared to pre-test indicates a conditioned preference for the drug's effects.
- Reinstatement/Relapse: After extinction of the CPP, drug-seeking can be reinstated by a priming drug dose, stress, or exposure to drug-paired cues, modeling relapse.
Protocol: Operant Self-Administration and Reinstatement
Objective: To model active drug-taking and relapse in animals.
- Surgery: Rats or mice are surgically implanted with an intravenous catheter allowing for drug delivery.
- Training: In an operant chamber, animals learn to perform a response (e.g., pressing a lever) to receive an intravenous infusion of a drug (e.g., cocaine). A cue light is often paired with each infusion.
- Extinction: The drug is disconnected. Lever presses no longer result in drug or cue presentation, leading to a gradual reduction in lever-pressing behavior.
- Reinstatement Test: Following extinction, drug-seeking behavior is reinstated by one of three triggers:
- Drug-induced: A non-contingent, low-dose priming injection of the drug.
- Cue-induced: Re-presentation of the drug-paired cue light.
- Stress-induced: Exposure to a mild stressor (e.g., foot shock).
- Measurement: The number of active lever presses during the test session, in the absence of drug reward, quantifies the motivation to relapse.
Human Brain Imaging Protocols
Objective: To identify structural and functional brain changes in individuals with addiction.
- fMRI Cue-Reactivity Task:
- Stimuli: Participants are shown drug-related cues (e.g., pictures of drug paraphernalia) and neutral cues in a block design.
- Data Acquisition: Blood-oxygen-level-dependent (BOLD) signals are measured using fMRI.
- Analysis: Contrasting brain activity during drug-cue blocks vs. neutral-cue blocks identifies regions activated by craving (e.g., amygdala, dorsal striatum, OFC). Connectivity analyses can reveal circuit-level dysfunctions [26].
- PET with [¹¹C]Raclopride:
- Tracer Injection: The radioligand [¹¹C]Raclopride, which binds to D2/D3 receptors, is administered intravenously.
- Baseline Scan: A PET scan is performed to measure baseline D2/D3 receptor availability.
- Challenge Scan: After administration of a stimulant drug (e.g., methylphenidate) or exposure to drug cues, a second scan is performed. The stimulant-induced dopamine release competes with raclopride for receptors, leading to a reduction in binding potential. This displacement quantifies the magnitude of dopamine release in the striatum [26].
Implications for Intervention and Future Research
The neuroplasticity framework of addiction suggests that recovery is possible by harnessing the brain's inherent capacity for change. Evidence-based behavioral therapies like Cognitive Behavioral Therapy (CBT) and contingency management work by promoting new learning and strengthening prefrontal inhibitory control, thereby creating new, resilient neural pathways to compete with drug-seeking ones [8] [14]. Pharmacological approaches aim to correct underlying neurobiological deficits, such as using N-acetylcysteine to restore glutamate homeostasis or medications to manage withdrawal and craving [26].
Future research should focus on:
- Developing personalized medicine approaches based on an individual's unique genetic and epigenetic profile.
- Novel therapeutics that directly target the stable neuroplastic changes underlying addictive memories (e.g., by erasing or reconsolidating them).
- Leveraging advanced technologies like real-time fMRI neurofeedback and non-invasive brain stimulation (TMS, tDCS) to directly modulate dysfunctional circuits and enhance resilience [26] [28].
Harnessing Plasticity: Methodological Advances and Therapeutic Applications
Neuroplasticity, the brain's fundamental capacity to reorganize its structure and function in response to experience, represents a critical biological process in both the development of and recovery from substance use disorders (SUDs). The same neural adaptability that makes the brain susceptible to addiction also enables it to heal, particularly when internal and external conditions support recovery [5]. Research from the National Institute on Drug Abuse (NIDA) has demonstrated that prolonged abstinence from drugs like methamphetamine allows for the recovery of lost dopamine transporters in the striatum, while longitudinal neuroimaging studies show structural and functional recovery in frontal cortical regions, hippocampus, and cerebellum during sustained remission [5]. As individuals learn new behaviors, goals, and rewards, this learning process reshapes synaptic connectivity across neural circuits, ultimately outcompeting drug-related memories and automatic behavioral patterns that weaken over time [5]. High-content imaging platforms provide the technological bridge to quantitatively measure these neuroplastic changes at the cellular level, offering unprecedented insights into the mechanisms of addiction and recovery for researchers and drug development professionals.
High-Content Imaging Technology Platforms
Core Principles and Terminology
High-content screening (HCS) integrates automated multicolor fluorescence imaging with quantitative data analysis to simultaneously evaluate multiple molecular features in individual cells [29]. This approach differs from traditional microscopy by capturing hundreds to millions of cellular images, thereby generating robust datasets with statistical power far exceeding conventional methods [29]. The terminology in this field includes:
- High-Content Imaging (HCI): Refers to the underlying automated image-based high-throughput technology used to measure and monitor phenotypic changes [29].
- High-Content Screening (HCS): Applies HCI to screen hundreds to millions of compounds to identify new drug targets and hits in complex cellular systems, including 3D cultures [29].
- High-Content Analysis (HCA): Utilizes multiparameter algorithms to extract detailed cellular physiology profiles from HCS data, enabling complex analyses of cell populations [29].
Leading Platform Specifications
Thermo Fisher Scientific offers some of the most widely cited HCA instruments in scientific literature, including the ArrayScan High-Content Platforms, CellInsight CX5 High-Content Screening Platform, and the recently introduced CellInsight CX7 High-Content Analysis Platform [30]. These platforms provide the resolution of microscopy combined with statistical power inherent in quantitative analysis of large cell numbers. The CellInsight CX7 HCA Platform represents an integrated benchtop instrument that interrogates multiple sample types with a wide range of techniques, leveraging advanced image acquisition and analysis software [30]. These systems build on a 20-year legacy of HCA instrument development and over 40 years of fluorescence imaging and probe development, making them particularly suitable for neuroplasticity research requiring precise quantification of subtle morphological changes [30].
Table 1: Comparison of High-Content Analysis Platforms
| Platform | Key Features | Applications in Neuroplasticity Research | Analysis Software |
|---|---|---|---|
| CellInsight CX7 HCA Platform | Integrated benchtop design, confocal acquisition, multiple sample type interrogation | Neurite outgrowth, synaptic connectivity, neural cell differentiation | HCS Studio with specialized bioapplications |
| CellInsight CX5 HCS Platform | High-content screening capabilities, temperature and CO₂ control | Cell health parameters, oxidative stress, protein synthesis/degradation | HCS Studio Cell Analysis Software |
| ArrayScan Platforms | High-resolution imaging, live-cell capabilities, temperature control | Mitochondrial function, lysosomal activity, neural progenitor proliferation | HCS Studio with customizable algorithms |
| CellInsight NXT Platform | Advanced automation compatibility, high-speed imaging | Neural progenitor proliferation, synaptic puncta counting | HCS Studio with machine learning options |
Quantitative Phenotypic Screening for Neuroplasticity
Neurite Outgrowth as a Key Metric
Sygnature Discovery has developed a semi-automated high-content imaging platform that specifically quantifies neurite outgrowth across PC12, SH-SY5Y, and primary neuron models [31]. This robust, scalable tool enables phenotypic screening of neuroplasticity modulators, accelerating the identification of new therapies for neuropsychiatric and neurodegenerative disorders [31]. The platform measures multiple parameters of neurite development, including total outgrowth length, branching complexity, and process diameter, which serve as quantitative indicators of structural neuroplasticity. These measurements provide crucial data on a compound's ability to promote neural connectivity, a fundamental process compromised in addiction and essential for recovery.
Recent research has leveraged these approaches to investigate specific molecular pathways. For instance, studies using the ArrayScan XTI High-Content Platform have demonstrated that Nrf2 nuclear translocation in response to rotenone treatment correlates with neurite retraction in neural stem cells derived from human induced pluripotent stem cells (iPSCs) [30]. Similarly, Hill et al. utilized the CellInsight NXT High-Content Screening Platform to study how mutations in the transcription factor gene TCF4 affect human cortical cell progenitor proliferation, with implications for cognitive deficits found in Pitt-Hopkins syndrome [30].
Synaptogenesis Screening Applications
A groundbreaking application of high-content imaging in neuroplasticity research involves optical pooled screening to investigate synapse formation. A recent study published in Cell Reports employed high-throughput single-cell optical pooled screening to analyze over two million single-cell phenotypic profiles, identifying 102 candidate regulators of neuroligin-1 linked to cell adhesion, cytoskeletal dynamics, and signaling [32]. Among these, researchers demonstrated that the phosphatase PTEN and the dystrophin-associated glycoprotein DAG1 promote neuroligin's roles in inducing presynaptic assembly, with DAG1 selectively regulating inhibitory synapses [32]. This work establishes a scalable high-content screening approach for cell-cell interactions that enables systematic studies of the molecular interactions guiding synaptogenesis, a crucial process underlying the neural rewiring that occurs during recovery from addiction.
Table 2: Key Quantitative Parameters in Neuroplasticity Screening
| Parameter Category | Specific Measurements | Biological Significance | Research Applications |
|---|---|---|---|
| Neurite Morphology | Total outgrowth length, number of branches, branch points, average process diameter | Indicators of structural connectivity and neural network formation | Screening neurotrophic compounds, assessing developmental neurotoxicity |
| Synaptic Density | Puncta count per neurite, synaptic protein clustering, colocalization of pre- and postsynaptic markers | Functional connectivity and information processing capacity | Studying synaptogenesis mechanisms, evaluating cognitive enhancers |
| Cell Body Morphology | Nuclear size, cytoplasmic volume, organelle distribution | Cellular health and metabolic activity | Neuroprotection studies, cytotoxicity assessment |
| Mitochondrial Function | Membrane potential, ROS production, distribution along neurites | Energy supply for plasticity processes and oxidative stress status | Investigating metabolic aspects of addiction and recovery |
Experimental Protocols for Neuroplasticity Assessment
Neurite Outgrowth Protocol
A standardized protocol for assessing neurite outgrowth using high-content imaging platforms involves several critical steps:
Cell Model Selection: Choose appropriate cellular models based on research objectives. Common models include:
- PC12 cells (rat pheochromocytoma) - Responsive to NGF-induced differentiation
- SH-SY5Y cells (human neuroblastoma) - Relevant for human-specific mechanisms
- Primary neurons from relevant brain regions - Highest physiological relevance
- Neural progenitor cells derived from human iPSCs - Enables patient-specific studies [31] [30]
Fluorescent Staining: Implement multiplexed staining protocols to visualize key cellular structures:
- Neurites: β-III-tubulin antibody staining (green fluorescence)
- Nuclei: DAPI or Hoechst staining (blue fluorescence)
- Synaptic markers: PSD-95, synapsin-1, or other specific proteins (red fluorescence)
- Cell viability markers: Propidium iodide or calcein AM for live/dead assessment
Image Acquisition: Utilize automated microscopy with the following parameters:
- 20x magnification for overall neurite network assessment
- 40x or 60x magnification for detailed synaptic analysis
- Multiple non-overlapping fields per well (minimum 9 fields for statistical robustness)
- Z-stack acquisition (5-7 slices with 1μm interval) for 3D reconstruction
Image Analysis: Apply specialized bioapplications in HCS Studio software:
- Nuclear identification algorithm for cell counting
- Neurite tracing algorithm for outgrowth quantification
- Puncta detection for synaptic marker analysis
- Colocalization analysis for functional synapse identification [30]
3D Model Development for Enhanced Physiological Relevance
While 2D cultures provide valuable data, 3D cell culture models of neural tissues offer more physiologically relevant systems for neuroplasticity research. Advanced protocols involve:
Matrix Selection: Combining Matrigel with type I collagen (1:1 ratio) provides a suitable compromise that supports the growth of both neuronal cells and supporting glial elements [33].
Cell Seeding Density Optimization: Restricting density (300-700 cells/well) ensures clonal origin of organoids and prevents early fusion of emerging structures [33].
Image Analysis Adaptation: Implement local entropy filters and global thresholding methods to separate 3D microtissues from background, followed by automated classification into neuronal and non-neuronal cells based on texture features [33].
Signaling Pathways in Neuroplasticity and Addiction
Research using high-content imaging has revealed critical signaling pathways involved in neuroplasticity that are hijacked in addiction states. Studies at The Rockefeller University and Mount Sinai have identified that drugs like cocaine and morphine activate specific subsets of neurons in the nucleus accumbens (NAc) that also respond to natural reward consumption [34]. Specifically, both cocaine and morphine activate D1 medium spiny neurons (involved in positive reinforcement and motivation), while morphine additionally activates D2 medium spiny neurons (involved in dampening responses to rewarding stimuli) [34].
Through sophisticated molecular and genomic techniques, including FOS-Seq, CRISPR-perturbation, and snRNAseq, researchers identified that drug addiction skews natural urges by hijacking the Rheb-mTOR pathway, which plays a crucial role in neural plasticity [34]. When drugs activate neurons expressing Rheb, it stimulates the mTOR pathway, likely altering how neurons communicate, learn, and remember stimuli from food and water, explaining why addicted individuals may neglect basic needs [34].
Diagram 1: Neural pathway hijacking in addiction. Addictive drugs activate specific neuron populations in the reward circuit, triggering molecular pathways that alter neural plasticity and shift behavioral priorities.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Neuroplasticity Screening
| Reagent Category | Specific Products | Function in Neuroplasticity Research | Application Notes |
|---|---|---|---|
| Cell Models | PC12 cells, SH-SY5Y cells, primary neurons, iPSC-derived neural progenitors | Provide biologically relevant systems for screening | Selection depends on throughput needs and physiological relevance requirements [31] |
| Fluorescent Probes | Alexa Fluor conjugates, MitoSOX Red, CellEvent Caspase-3/7, CellROX Green | Enable visualization of specific cellular structures and functions | Multiplexing requires careful spectral separation [30] |
| Antibodies | β-III-tubulin, MAP2, PSD-95, synapsin-1, NeuN | Specific labeling of neuronal structures and synaptic components | Validation for specific model systems is essential |
| Functional Dyes | DAPI, Hoechst (nuclei), Phalloidin (F-actin), JC-1 (mitochondrial potential) | Fundamental cellular staining and organelle-specific assessment | Concentration optimization required for each cell type |
| Assay Kits | Click-iT Plus OPP Protein Synthesis, Live/Dead viability, apoptosis detection | Quantitative assessment of cell health and functional states | Compatibility with imaging platforms must be verified [30] |
Workflow Integration for Addiction Research
Implementing high-content imaging for neuroplasticity studies in addiction research requires careful workflow design. The following diagram illustrates an integrated approach from experimental setup to data analysis:
Diagram 2: High-content screening workflow for neuroplasticity. The integrated process from model selection to pathway validation enables comprehensive assessment of compounds affecting neural structure and function.
High-content imaging platforms have revolutionized phenotypic screening for neuroplasticity modulators by providing robust, quantitative data on neurite outgrowth, synaptogenesis, and related neural processes at scale. These technologies offer researchers and drug development professionals unprecedented ability to investigate the neural rewiring that occurs both in addiction development and recovery processes. The integration of advanced cellular models, including 3D systems and patient-derived cells, with sophisticated image analysis algorithms positions high-content imaging as an indispensable tool in the quest to develop novel therapies for substance use disorders. As NIDA continues to invest in research on recovery support services [5], and basic science reveals the intricate molecular pathways hijacked by addictive drugs [34], high-content screening platforms will play an increasingly vital role in translating these discoveries into effective interventions that support long-term neural recovery and behavioral change.
Addiction is now understood as a chronic disorder of maladaptive neuroplasticity, characterized by intense and compulsive drug-seeking behavior and a high risk of relapse [35]. The brain's remarkable capacity to change its structure and function in response to experience—neuroplasticity—underlies both the development of and recovery from substance use disorders (SUDs) [14] [36]. While all drugs of abuse initially activate the brain's reward pathways, primarily through dopamine release in the nucleus accumbens (NAcc), the progression to chronic addiction involves more fundamental restructuring of neural circuits [2] [26]. This whitepaper examines three interconnected mechanistic pillars driving this maladaptive plasticity: neuroinflammation, oxidative stress, and dysregulated gasotransmitter systems. These pathways represent promising therapeutic targets for disrupting the cycle of addiction by addressing its underlying neurobiology beyond conventional dopamine-centric approaches [35] [37].
The transition from voluntary drug use to compulsive addiction mirrors a transition in the brain's operational state. As noted by Stanford Medicine researchers, "We've got an old brain in a new environment," highlighting the mismatch between evolutionarily conserved reward systems and modern access to highly reinforcing substances [2]. This transition is mediated through neuroplastic changes that become increasingly entrenched with repeated drug exposure. Addiction, once established, becomes a chronic illness with relapses and remissions, requiring chronic treatment strategies based on understanding these fundamental brain changes [26].
Core Pathophysiological Mechanisms
Neuroinflammation in Substance Use Disorders
Chronic drug consumption activates the brain's innate immune response, initiating a cascade of neuroinflammatory processes that drive addiction pathology. Microglia and astrocytes, the central nervous system's primary immune cells, undergo phenotypic changes characterized by increased production of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 [37]. This neuroinflammatory response has been demonstrated across multiple drug classes including amphetamines, cocaine, ethanol, opioids, cannabinoids, and nicotine [37].
The triggering mechanisms vary by substance class but converge on common inflammatory pathways. Toll-like receptors (TLRs), particularly TLR4, recognize drugs of abuse as pathogen-like molecules, activating NF-κB signaling and subsequent cytokine production [37]. This drug-induced neuroinflammation disrupts critical neural functions, particularly glutamate homeostasis, by reducing the expression and activity of astrocytic glutamate transporters (GLT-1) and the cystine-glutamate antiporter (system Xc-) [37]. The resultant glutamate dysregulation strengthens drug-associated synaptic connections and weakens prefrontal cortical control, creating conditions primed for relapse [26] [37].
Table 1: Neuroinflammatory Targets in Substance Use Disorders
| Therapeutic Target | Mechanism of Action | Experimental Compounds/Approaches | Stage of Development |
|---|---|---|---|
| TLR4 Signaling | Inhibits drug-induced microglial activation | (+)-Naltrexone, Ibudilast | Preclinical to Phase II trials |
| Cytokine Signaling | Reduces pro-inflammatory mediators | Infliximab (anti-TNF-α), IL-1 receptor antagonists | Preclinical evidence |
| Microglial Activation | Modulates microglial phenotype | Minocycline, N-acetylcysteine | Mixed results in clinical trials |
| Astrocytic Function | Restores glutamate homeostasis | N-acetylcysteine, Ceftriaxone | Preclinical to Phase II trials |
Oxidative Stress and Its Consequences
The brain's high metabolic rate and relative scarcity of antioxidant defenses render it particularly vulnerable to oxidative stress [37]. Drug abuse exacerbates this vulnerability through multiple mechanisms that generate reactive oxygen species (ROS) and reactive nitrogen species (RNS). The oxidative stress-neuroinflammation vicious cycle represents a self-perpetuating cascade that persists long after drug clearance [37].
Dopamine metabolism itself contributes significantly to oxidative load. Once released from synaptic vesicles into the neutral pH of the synaptic cleft, dopamine undergoes spontaneous oxidation forming dopamine quinones and superoxide radicals [37]. Enzymatic metabolism by monoamine oxidase-B (MAO-B) and cyclooxygenases (COX-1/2) further generates H₂O₂ and other oxidative species [37]. Mitochondrial dysfunction amplifies this process, as most drugs of abuse impair mitochondrial electron transport chain function, increasing electron leakage and superoxide production [37].
The consequences of drug-induced oxidative stress extend beyond neuronal damage to include altered synaptic plasticity, impaired decision-making, and enhanced drug-seeking behavior. Oxidative modifications of proteins critical for glutamate transport and synaptic plasticity consolidate addiction-related learning, while lipid peroxidation compromises neuronal membrane integrity and signaling capacity [37].
Table 2: Antioxidant Therapeutic Approaches for Substance Use Disorders
| Approach Category | Specific Interventions | Proposed Mechanisms | Evidence Base |
|---|---|---|---|
| Direct Antioxidants | N-acetylcysteine, Vitamin E, Melatonin | Scavenges ROS/RNS, replenishes glutathione | Preclinical to clinical trials |
| Indirect Antioxidants | Sulforaphane, Dimethyl fumarate | Activates Nrf2/ARE pathway | Preclinical models |
| Mitochondrial Support | MitoQ, Coenzyme Q10 | Targets mitochondrial ROS | Early preclinical |
| Anti-inflammatory Antioxidants | Astaxanthin, Curcumin | Dual antioxidant and anti-inflammatory effects | Preclinical models |
Gasotransmitter Systems in Addiction Neurobiology
Gasotransmitters—including nitric oxide (NO), carbon monoxide (CO), and hydrogen sulfide (H₂S)—represent a novel class of neuromodulators with emerging roles in addiction processes. These small, gaseous molecules freely diffuse across membranes, modulating synaptic transmission, neuronal excitability, and neuroplasticity [35]. Their dysregulation contributes significantly to addiction pathophysiology, offering promising new therapeutic targets.
Nitric oxide, synthesized by nitric oxide synthase (NOS) isoforms, interacts extensively with dopamine and glutamate systems central to addiction. NO modulates presynaptic neurotransmitter release, influences dopamine transporter function, and regulates neuronal excitability in reward-related regions [35]. Upregulation of the inducible NOS (iNOS) in glial cells during neuroinflammation creates sustained NO production that contributes to nitrosative stress and synaptic dysfunction [37].
Hydrogen sulfide, produced primarily by cystathionine-β-synthase (CBS) and cystathionine-γ-lyase (CSE), exerts complex effects on neuronal function through protein sulfhydration, ion channel modulation, and antioxidant effects. Emerging evidence suggests H₂S signaling intersects with drug-induced plasticity in the nucleus accumbens and prefrontal cortex [35]. Similarly, carbon monoxide, generated by heme oxygenase, influences stress responses and drug reward, though its specific addiction-related roles remain less characterized [35].
Experimental Methodologies and Assessment Techniques
Assessing Neuroinflammatory States
Microglial Activation Imaging: Utilize transgenic CX3CR1-GFP mice or immunostaining with Iba-1 antibodies to quantify microglial morphology changes following drug exposure. Administer drugs of abuse via established paradigms (e.g., chronic intermittent ethanol vapor for alcohol, daily injections for psychostimulants). Process brains for immunohistochemistry and analyze microglial branching complexity, soma size, and density using automated software such as Imaris or FIJI ImageJ. Confirm findings with PET imaging using [¹¹C]PBR28 or [¹⁸F]DPA-714 for TSPO expression in human subjects [37].
Cytokine Profiling Protocol: Extract brain regions of interest (NAcc, PFC, VTA, hippocampus) following drug administration and abstinence periods. Homogenize tissue in RIPA buffer with protease and phosphatase inhibitors. Quantify cytokine levels (TNF-α, IL-1β, IL-6, IL-10) using multiplex ELISA arrays (e.g., Luminex technology). Normalize protein concentrations and compare to saline-treated controls. For human translation, measure cytokine levels in CSF or plasma using the same methodology, correlating with clinical measures of craving and relapse [37].
Quantifying Oxidative Stress Parameters
Lipid Peroxidation Assessment: Apply the thiobarbituric acid reactive substances (TBARS) assay to brain tissue homogenates. Briefly, incubate samples with thiobarbituric acid at 95°C for 60 minutes, measure fluorescence at 532nm excitation/553nm emission. Quantify using malondialdehyde (MDA) standards. Alternatively, employ immunohistochemistry for 4-hydroxynonenal (4-HNE) protein adducts in fixed brain sections [37].
Antioxidant Capacity Measurement: Assess glutathione levels using the DTNB-GSSG reductase recycling assay. Homogenize brain tissue in sulfosalicylic acid, centrifuge, and separate supernatant for total glutathione and pellet for protein quantification. For the assay, mix sample with DTNB, NADPH, and glutathione reductase, monitoring absorbance at 412nm. Calculate reduced (GSH) and oxidized (GSSG) glutathione ratios, a sensitive indicator of oxidative stress [37].
Behavioral Paradigms for Therapeutic Validation
Drug Self-Administration and Reinstatement: Train rats or mice to self-administer drugs of abuse (e.g., cocaine, heroin, alcohol) via lever pressing or nose-poking. Establish stable baseline responding (typically 2-3 weeks). Implement extinction training where drug responses are no longer reinforced. Assess drug-seeking behavior through reinstatement models: cue-induced (presentation of drug-paired cues), drug-primed (low-dose drug administration), or stress-induced (intermittent footshock). Test experimental compounds during extinction or before reinstatement sessions [26].
Conditioned Place Preference (CPP): Utilize apparatus with distinct contextual chambers. During conditioning, pair one chamber with drug administration and the other with saline. After multiple pairings, test for preference by allowing free access to both chambers. For extinction, repeatedly expose animals to both chambers without drug. Test for reinstatement following stress or drug priming. This model assesses drug reward and relapse-like behavior [26].
Signaling Pathways in Addiction Pathology
The following diagram illustrates the key signaling pathways connecting neuroinflammation and oxidative stress in substance use disorders:
Figure 1: Neuroinflammation-Oxidative Stress Cycle in Addiction. This self-perpetuating cascade drives maladaptive plasticity and increases relapse vulnerability.
Emerging Therapeutic Interventions
Pharmacological Approaches
N-acetylcysteine (NAC) represents one of the most promising anti-inflammatory/antioxidant interventions for SUDs. NAC restores glutamate homeostasis through multiple mechanisms: as a cysteine prodrug it stimulates the cystine-glutamate antiporter (system Xc-), while as a glutathione precursor it enhances antioxidant capacity [26] [37]. In human trials, NAC reduces cocaine craving and cigarette smoking, with ongoing investigations for other substance dependencies [26].
GLP-1 receptor agonists, including exenatide and liraglutide, have demonstrated unexpected efficacy in reducing drug and alcohol consumption [2]. Initially developed for diabetes and obesity, these agents modulate mesolimbic dopamine signaling and exhibit anti-inflammatory properties. Ongoing clinical trials are evaluating their potential as novel SUD treatments.
Drugs targeting neuroimmune signaling include ibudilast, a phosphodiesterase inhibitor that suppresses pro-inflammatory cytokine production, and minocycline, a tetracycline antibiotic with potent microglial inhibition properties. Both have shown promise in early-phase human studies for alcohol and opioid use disorders [37].
Neuromodulation Techniques
Non-invasive brain stimulation approaches represent a paradigm shift in addiction treatment by directly modulating neural circuits implicated in addiction pathology. Repetitive transcranial magnetic stimulation (rTMS) can induce long-lasting changes in cortical excitability and connectivity, particularly when targeted to the dorsolateral prefrontal cortex (dlPFC) [38]. Current clinical trials combine rTMS with cognitive behavioral therapy to enhance smoking cessation outcomes, especially in challenging populations such as veterans with PTSD [38].
The mechanism by which rTMS exerts therapeutic effects likely involves normalization of addiction-related circuitry, including reduction of drug cue reactivity, enhancement of cognitive control, and potentially modulation of neuroinflammatory processes. The following diagram illustrates a representative experimental workflow for evaluating neuromodulation therapies:
Figure 2: Neuromodulation Clinical Trial Workflow. Representative study design for evaluating rTMS efficacy in substance use disorders.
Biomolecule-Based Strategies
Emerging approaches utilize endogenous biomolecules with potent anti-inflammatory and antioxidant properties. Mesenchymal stem cell-derived secretions contain a cocktail of trophic factors, microvesicles, and mitochondria that can be delivered via intranasal administration to target neuroinflammation and oxidative stress without cell transplantation [37].
MicroRNA-based therapies represent another innovative approach, targeting the epigenetic regulation of neuroinflammatory pathways. For example, anti-miRNAs that suppress pro-inflammatory microglial activation show promise in reducing drug craving in preclinical models [37]. Similarly, natural products with dual antioxidant and anti-inflammatory properties, such as curcumin, resveratrol, and sulforaphane, are being investigated for their potential to normalize addiction-related plasticity [39] [37].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Novel Neurotherapeutic Targets
| Reagent/Category | Specific Examples | Research Application | Key Mechanisms |
|---|---|---|---|
| Cytokine Modulators | Ibudilast, Infliximab, IL-1ra | Targeting neuroimmune activation | Phosphodiesterase inhibition, TNF-α neutralization, IL-1 receptor blockade |
| ROS Scavengers | N-acetylcysteine, MitoTEMPO, Tempol | Reducing oxidative stress | Glutathione precursor, mitochondrial ROS targeting, superoxide dismutase mimetic |
| Nrf2 Activators | Sulforaphane, Dimethyl fumarate, Bardoxolone | Enhancing antioxidant defense | KEAP1 inhibition, ARE pathway activation |
| Gasotransmitter Modulators | L-NAME, Aminooxyacetic acid, ZnPP | Manipulating NO, H₂S, CO signaling | NOS inhibition, CBS/CSE inhibition, HO blockade |
| Glutamate Modulators | Ceftriaxone, N-acetylcysteine, Riluzole | Restoring glutamate homeostasis | GLT-1 upregulation, system Xc- activation, glutamate release inhibition |
| Microglial Modulators | Minocycline, PLX5622, Fingolimod | Targeting microglial function | Anti-inflammatory, CSF1R inhibition, sphingosine-1-phosphate modulation |
| Epigenetic Regulators | BET inhibitors, HDAC inhibitors, miRNA mimics | Modifying addiction-related gene expression | Bromodomain inhibition, histone acetylation, post-transcriptional regulation |
The reconceptualization of addiction as a disorder of maladaptive neuroplasticity driven by neuroinflammation, oxidative stress, and dysregulated gasotransmitter systems opens promising new avenues for therapeutic intervention. Targeting these fundamental mechanisms offers the potential to disrupt the self-perpetuating cycles that maintain addiction long after drug cessation. The most promising approaches include combination therapies that simultaneously address multiple pathological processes, such as pairing anti-inflammatory agents with neuromodulation or behavioral interventions.
Future research should prioritize the development of biomarkers to identify patient subgroups most likely to respond to specific mechanism-based treatments, the optimization of delivery methods to enhance blood-brain barrier penetration, and the exploration of sequential treatment algorithms that address different phases of the addiction cycle. As our understanding of these novel neurotherapeutic targets deepens, we move closer to effective treatments that address the root causes rather than merely the symptoms of substance use disorders.
Substance Use Disorders (SUDs) are chronic, relapsing conditions traditionally conceptualized through the lens of brain-centric models, focusing on dysregulation of the reward circuitry, executive control systems, and neuroplastic adaptations that drive compulsive drug-seeking behavior [35] [40]. However, a growing body of evidence indicates that this brain-centered perspective is incomplete. The progression of SUDs involves complex, bidirectional communication between the central nervous system and peripheral organ systems, both as consequences of chronic substance exposure and as active drivers of the addiction cycle [35] [41]. This whitepaper explores the critical roles of non-canonical organ systems—specifically the cardiac system, liver, and immune system—in SUD progression, framing this discussion within the broader context of neuroplasticity in addiction development and recovery.
The transition from controlled use to addiction is marked by intense and compulsive drug-seeking behavior and a high risk of relapse, characteristics that cannot be fully explained by the "euphoria reward" model alone [35] [41]. Recent research emphasizes that neuroinflammation and oxidative stress in the brain, often originating from or amplified by peripheral inflammation, play a critical role in altering neural circuitry involved in reward, motivation, and decision-making [35]. This paper proposes that a comprehensive understanding of SUDs requires an integrated approach that examines toxicity and adaptive changes across the brain, heart, and liver, focusing on mechanisms of neuroinflammation, neuroplasticity, and gasotransmitter systems that facilitate organ crosstalk [35] [41]. By developing pharmacotherapies that target these peripheral mechanisms and their interactions with the brain, researchers may discover new successes in SUD therapeutic development.
Neuroplastic Foundations of SUD: A Primer
Neuroplasticity, defined as the nervous system's ability to change its activity in response to intrinsic or extrinsic stimuli by reorganizing its structure, functions, or connections, serves as the fundamental mechanism underlying both the development of and recovery from SUDs [3] [14]. In the context of addiction, neuroplasticity manifests as experience-dependent learning where repeated drug exposure strengthens the association between drug consumption, drug-associated cues, and the predictable neurochemical response, particularly in the mesolimbic dopamine pathway [3] [40].
The dopamine reward pathway, originating in the ventral tegmental area (VTA) and projecting to the nucleus accumbens (NA) and prefrontal cortex (PFC), undergoes significant neuroadaptive changes with repeated drug use [3]. Chronically elevated dopamine levels lead to downregulation of dopamine receptor density, a protective mechanism that paradoxically increases dopamine-seeking behaviors as individuals attempt to compensate for the reduced receptor availability [3]. These neuroplastic changes are not limited to synaptic alterations but extend to structural modifications, including the sprouting of new axonal dendritic spines and the formation of new synaptic connections that cement drug-related memories and behaviors [3].
Recent research has revealed that adaptive myelination represents another crucial mechanism of neuroplasticity in addiction. A groundbreaking study demonstrated that a single dose of morphine was sufficient to trigger the proliferation of oligodendrocyte precursor cells in the VTA within just three hours of administration [42]. With repeated drug exposure, this process leads to increased oligodendrocyte numbers and thicker myelin around dopamine-producing neurons, specifically in the VTA, which enhances the efficiency and synchrony of reward circuit signaling and promotes drug-seeking behavior [42]. This myelination process is dependent on BDNF-TrkB signaling; when this pathway is blocked, mice failed to generate new oligodendrocytes and did not acquire a preference for the chamber where they received morphine [42].
These neuroplastic changes in the brain do not occur in isolation. They are profoundly influenced by, and in turn influence, peripheral organ systems through inflammatory mediators, stress hormones, and other signaling molecules, creating a self-reinforcing cycle that drives the progression of SUDs [35].
Non-Canonical Organ Systems in SUD Pathophysiology
Cardiac System and Brain Reward Circuitry
The heart-brain axis represents a critical bidirectional pathway in SUD progression, with the cardiac system both affected by substance use and actively influencing neurological function. Chronic substance abuse places considerable strain on the cardiovascular system, leading to conditions such as hypertension, cardiomyopathy, and arrhythmia [43]. These cardiac abnormalities can indirectly affect brain function by altering cerebral blood flow, promoting neuroinflammation, and activating stress pathways that subsequently reinforce addictive behaviors.
Quantitative proteomic analyses have revealed significant molecular-level disruptions in cardiac tissue associated with substance use. The table below summarizes key protein alterations observed in cardiac tissue that may influence SUD progression:
Table 1: Cardiac Protein Alterations Relevant to SUD Pathology
| Protein Category | Specific Proteins | Functional Consequences | Impact on SUD Progression |
|---|---|---|---|
| Myofilament Proteins | MYL7, MYL4, MYH11 | Altered contractility, heart rate variability | Modified interoceptive feedback to brain |
| Ion Channels & Transporters | SLC8A1, ATP2B1 | Calcium signaling disruption, arrhythmogenesis | Affects stress response, drug cue reactivity |
| Natriuretic Peptides | NPPA | Volume dysregulation, hemodynamic stress | Activates hypothalamic-pituitary-adrenal axis |
| Extracellular Matrix Proteins | Multiple collagens | Tissue remodeling, reduced compliance | Promotes systemic inflammation |
These cardiac protein disturbances create a pathological feedback loop to the brain through multiple mechanisms. Altered cardiac function affects cerebral blood flow and oxygenation, potentially impairing prefrontal cortical function and reducing inhibitory control over drug-seeking behaviors [44]. Additionally, cardiac stress activates the hypothalamic-pituitary-adrenal axis, increasing cortisol release that can sensitize the reward system to drugs of abuse [35]. The resulting systemic inflammation from cardiac dysfunction promotes neuroinflammation, which alters neural circuitry involved in reward, motivation, and decision-making [35].
Hepatic Dysfunction and Neurological Consequences
The liver plays a crucial role in SUD progression beyond its traditional function in drug metabolism. Hepatic dysfunction resulting from chronic substance abuse—particularly alcohol-induced cirrhosis and drug-related hepatotoxicity—has significant neurological implications through multiple pathways [43]. The liver serves as the primary source of inflammatory cytokines and acute-phase proteins during systemic inflammation, and liver damage results in elevated circulating levels of pro-inflammatory mediators that can cross the blood-brain barrier or activate endothelial signaling.
Liver-derived inflammatory molecules, including TNF-α, IL-1β, and IL-6, promote microglial activation in brain regions critical for reward processing and executive control [35]. This neuroinflammatory state heightens the reward value of drugs while simultaneously blunting the response to natural rewards, creating a neurobiological environment conducive to relapse. Additionally, hepatic dysfunction disrupts ammonia clearance and tryptophan metabolism, leading to alterations in serotonin and dopamine synthesis that further dysregulate reward circuitry [35].
The liver is also responsible for producing brain-derived neurotrophic factor (BDNF), a key mediator of neuroplasticity, and liver-induced reductions in BDNF availability may impair adaptive plasticity in recovery [3]. Furthermore, the liver plays a central role in gasotransmitter signaling, particularly in the metabolism of hydrogen sulfide, which has been implicated in both neuroprotection and neurotoxicity in SUD contexts [35] [41].
Peripheral Immune Activation and Neuroinflammation
The peripheral immune system serves as a critical intermediary between peripheral organ damage and central nervous system dysfunction in SUDs. Substance abuse compromises the lymphatic and immune systems, increasing susceptibility to infections and viruses while simultaneously establishing a state of chronic low-grade inflammation [43]. This persistent immune activation has profound implications for brain function and addiction processes.
Alcohol and drugs of abuse compromise the immune system by altering lymphocyte function, cytokine production, and cell-mediated immunity [43]. The resulting systemic inflammation allows peripheral immune cells, particularly monocytes, to infiltrate the brain parenchyma, where they differentiate into macrophages and augment the neuroinflammatory response initiated by microglia [35]. These infiltrating cells release additional pro-inflammatory cytokines and reactive oxygen species that directly alter synaptic plasticity and dopamine neurotransmission [35] [3].
Peripheral inflammation induces changes in the blood-brain barrier permeability, facilitating the entry of inflammatory mediators into the brain and potentially altering drug access to central targets [35]. This inflammatory signaling also activates the brain's stress circuitry, particularly the extended amygdala, contributing to the negative emotional state that develops during withdrawal and drives compulsive drug-taking to alleviate this aversive state [35] [41].
Table 2: Key Inflammatory Mediators in SUD Progression
| Inflammatory Mediator | Primary Source | Effect on Brain Function | Role in Addiction Cycle |
|---|---|---|---|
| TNF-α | Macrophages, Kupffer cells | Enhances glutamate excitotoxicity, reduces synaptic strength | Increases reward sensitivity, impairs decision-making |
| IL-1β | Monocytes, microglia | Modulates dopamine release in NAc, affects synaptic plasticity | Promotes negative affect in withdrawal |
| IL-6 | T-cells, hepatocytes | Alters BDNF signaling, affects neurogenesis | Contributes to cognitive inflexibility |
| MCP-1/CCL2 | Endothelial cells, astrocytes | Recruits monocytes to brain, enhances neuroinflammation | Strengthens drug-associated memories |
Quantitative Proteomics in Multi-Organ SUD Research
Advanced proteomic technologies have revolutionized our ability to quantify protein expression changes across multiple organ systems in SUDs, providing unprecedented insights into the molecular networks connecting peripheral organ pathology to brain function in addiction. Mass spectrometry-based proteomics enables the simultaneous measurement and evaluation of thousands of proteins across cardiac chambers, liver tissue, and brain regions, creating comprehensive protein signatures of SUD progression [45] [44].
The experimental workflow for comparative quantitative proteomics in SUD research typically follows these essential steps:
Sample Conditioning: Fresh tissue collection from cardiac chambers, liver, and brain regions relevant to reward processing (e.g., VTA, NAc, PFC), followed by immediate snap-freezing in liquid nitrogen and storage at -80°C [44].
Protein Extraction and Preparation: Tissue homogenization using a ceramic bead mill, followed by protein extraction with detergent-based buffers that solubilize cellular membranes and compartments. Elimination of contaminants (lipids, nucleic acids) while maintaining protein integrity [45] [44].
Protein Digestion and Fractionation: Enzymatic digestion of proteins into peptides using trypsin, followed by pre-fractionation at high pH by reverse-phase high-pressure liquid chromatography (RP-HPLC) to reduce sample complexity [45] [44].
LC-MS/MS Analysis: Separation of peptides using liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS) on high-resolution instruments such as Q-Exactive HF quadrupole Orbitrap systems, with measurement of approximately 7,000 proteins per sample [44].
Data Processing and Normalization: Identification and quantification of proteins using search engines like Andromeda, followed by normalization of raw data to a common scale to enable cross-tissue and cross-species comparisons [44].
Bioinformatic Integration: Orthology/paralogy mapping based on fine-grained orthology groups (e.g., EggNOG) to enable comparison of protein expression profiles across model organisms and humans, followed by pathway and network analysis [44].
This proteomic approach has revealed that up to a quarter of proteins with differential abundances between cardiac chambers show opposite chamber-specific enrichment between species, including numerous proteins implicated in cardiac disease that may influence SUD progression [44]. These findings highlight the importance of considering organ-specific protein expression patterns when modeling SUD pathophysiology and developing therapeutic interventions.
Methodologies for Investigating Organ-Brain Axis in SUD
Experimental Models and Translational Considerations
Choosing appropriate model systems is paramount for investigating the role of non-canonical organ systems in SUD progression. Quantitative proteomic comparisons across species have revealed significant differences in cardiac protein profiles that must be considered when translating findings from preclinical models to humans [44]. Unsupervised hierarchical clustering of cardiac proteomes shows that species branches cluster according to evolutionary distance, with horse and pig forming one cluster, mouse and rat forming another, and zebrafish as the most evolutionarily distant [44].
Notably, protein-level differences between organisms often explain why pharmacological interventions fail to translate from animals to humans, as illustrated by statins [44]. For structural studies of cardiac manifestations of SUD, the pig represents a particularly valuable model due to its anatomical and pathophysiological similarity to human hearts, successfully serving as a model for cardiac arrhythmias [44]. In contrast, zebrafish may be less suitable for certain aspects of SUD research due to fundamental differences in protein enrichment across cardiac chambers [44].
To facilitate appropriate model selection, researchers have developed open-access databases (e.g., atlas.cardiacproteomics.com) that allow straightforward comparison of protein expression levels of orthologs across chambers for multiple species, enabling informed decisions on target proteins and model organisms for SUD research [44].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Non-Canonical Organs in SUD
| Reagent/Category | Specific Examples | Application in SUD Research | Technical Considerations |
|---|---|---|---|
| Mass Spectrometry Reagents | Trypsin, DTT, IAA, TMT/Isobaric tags | Protein quantification across organs | Compatibility with multi-organ protein extraction buffers |
| Antibodies for Inflammation Markers | Anti-TNF-α, Anti-IL-1β, Anti-GFAP | Assessing neuroinflammation and peripheral inflammation | Validate cross-reactivity for species-specific applications |
| Myelin Staining Agents | Anti-MBP, Luxol Fast Blue, Electron Microscopy reagents | Evaluating adaptive myelination in reward pathways | Combine with neuronal activity markers (c-Fos) |
| Signaling Pathway Modulators | BDNF, TrkB inhibitors, Morphine, Cocaine | Manipulating reward circuitry and plasticity | Dose-response critical for distinguishing acute vs. chronic effects |
| Proteomics Sample Prep Kits | Detergent-based extraction buffers, Protein assay kits | Tissue protein extraction for LC-MS/MS | Optimize for membrane-bound proteins from cardiac tissue |
Visualization of Key Pathways and Experimental Workflows
Organ-Brain Signaling in SUD Progression
Diagram 1: Organ-Brain Axis in SUD
Myelination in Reward Circuitry
Diagram 2: Myelination in Reward Circuitry
Proteomic Workflow for Multi-Organ SUD Research
Diagram 3: Proteomic Workflow for SUD Research
The investigation of non-canonical organ systems in SUD progression represents a paradigm shift in addiction research, moving beyond brain-centric models to embrace a holistic, whole-organism perspective. The evidence presented in this whitepaper demonstrates that peripheral organs—particularly the cardiac system, liver, and immune system—actively contribute to the development and maintenance of addiction through complex bidirectional communication with the brain [35] [41]. These organ systems are not merely passive targets of drug-induced damage but dynamic participants in the addiction process, driving neuroinflammation, altering neuroplasticity, and reinforcing maladaptive learning through multiple signaling pathways.
Future research directions should prioritize the development of multi-organ proteomic databases that systematically map protein networks across species and organ systems in the context of substance exposure [44]. Additionally, greater emphasis on gasotransmitter systems as mediators of organ-brain crosstalk may reveal novel therapeutic targets for disrupting the feedback loops that perpetuate addiction [35] [41]. The recent discovery that adaptive myelination can be harnessed to promote addiction-like behaviors also opens exciting possibilities for reversing this process to facilitate recovery [42].
From a therapeutic perspective, this integrated understanding of SUD pathophysiology suggests that interventions targeting peripheral inflammation or organ-specific dysfunction may yield unexpected benefits in treating addiction. Similarly, lifestyle interventions that improve overall organ health may strengthen recovery by promoting healthier neuroplastic changes and reducing the systemic inflammation that drives relapse [3]. As our knowledge of these complex organ-brain interactions deepens, we move closer to comprehensive treatment approaches that address the full biological context of Substance Use Disorders.
Substance use disorders (SUDs) are chronic, relapsing brain conditions characterized by profound dysregulation of cortical and subcortical circuits governing reward, motivation, and executive control. While pharmacological and behavioral treatments have demonstrated utility, relapse rates remain as high as 60%, underscoring the critical need for neuroscience-informed therapeutics [46] [47]. Neuromodulation techniques, particularly repetitive Transcranial Magnetic Stimulation (rTMS) and Transcranial Direct Current Stimulation (tDCS), represent promising interventions that directly target the neuroplastic alterations underlying addiction. This technical review synthesizes current evidence on the application of TMS and tDCS to restore cortical balance in SUDs. We provide a comprehensive analysis of stimulation parameters, molecular mechanisms, efficacy data, and detailed methodological protocols to guide researchers and clinicians in leveraging these tools to counteract addiction-related neurocircuitry dysfunction and promote sustained recovery.
Neurobiological Foundation of Addiction and Cortical Imbalance
Addiction is conceptualized as a cycle involving three stages—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—each mediated by discrete, reproducible neural circuits [48] [49]. Prolonged substance exposure induces maladaptive neuroplasticity across key brain networks:
- Reward System Dysregulation: All addictive substances, directly or indirectly, enhance dopamine release in the nucleus accumbens (NAc), overstimulating the mesolimbic pathway. Over time, this leads to hypodopaminergic functioning, reducing sensitivity to natural rewards [50] [47].
- Prefrontal Cortex Impairment: The dorsolateral prefrontal cortex (DLPFC), orbitofrontal cortex (OFC), and anterior cingulate cortex (ACC exhibit reduced activity, compromising executive functions such as impulse control, decision-making, and behavioral regulation [50] [47]. This creates an imbalance between hyperactive "go" signals from limbic regions and weakened "stop" signals from prefrontal regions.
- Cortico-Striatal Circuit Alterations: A shift occurs from goal-directed (ventral striatum-mediated) to habitual (dorsal striatum-mediated) drug-seeking behavior, reflecting a transition toward compulsive use patterns [50].
This cortical-subcortical imbalance establishes a biological basis for therapeutic neuromodulation, wherein targeted stimulation can potentially restore homeostasis by enhancing prefrontal control and modulating reward sensitivity [51] [47].
Repetitive Transcranial Magnetic Stimulation (rTMS)
Mechanism of Action: rTMS is a non-invasive technique that uses alternating magnetic fields generated by a copper coil placed on the scalp to induce localized electrical currents in cortical tissue [46] [47]. These currents modulate neuronal membrane potentials, leading to changes in cortical excitability and the induction of neuroplasticity. The effects extend beyond the stimulation site via connectivity to distributed networks, including deep structures like the NAc [47].
Key Stimulation Parameters:
- Frequency: Low-frequency rTMS (≤1 Hz) generally induces long-term depression (LTD)-like effects, reducing cortical excitability. High-frequency rTMS (≥5 Hz, typically 10-20 Hz) induces long-term potentiation (LTP)-like effects, increasing cortical excitability [46] [47].
- Coil Design: Standard figure-8 coils stimulate superficial cortical areas to a depth of 1.5-2 cm. H-coils used in deep TMS (dTMS) can reach deeper and broader areas (up to 3.2-4 cm), potentially targeting the medial prefrontal cortex (mPFC) and insula [48] [52].
- Patterned Protocols: Theta Burst Stimulation (TBS) delivers bursts of 50 Hz pulses. Intermittent TBS (iTBS) facilitates cortical excitability, while Continuous TBS (cTBS) inhibits it [46] [47].
Transcranial Direct Current Stimulation (tDCS)
Mechanism of Action: tDCS applies a low-intensity, constant current (0.5-2.0 mA) via scalp electrodes to modulate neuronal resting membrane potentials. Anodal stimulation typically depolarizes neurons, increasing cortical excitability, while cathodal stimulation hyperpolarizes neurons, decreasing excitability [50] [47]. Unlike rTMS, tDCS does not directly elicit action potentials but rather modulates neuronal responsiveness to other inputs [51].
Key Stimulation Parameters:
- Electrode Configuration: Unilateral: One electrode over the target area (e.g., DLPFC), the other over the contralateral supraorbital region or extracephalically. Bilateral: Electrodes over homologous regions of both hemispheres [53].
- Current Intensity and Duration: Typically 1-2 mA for 10-30 minutes. Longer sessions (>10-15 minutes) over multiple days appear more effective [51] [47].
Molecular Mechanisms and Signaling Pathways
Both rTMS and tDCS induce neuroplastic changes that share common molecular pathways with canonical learning and memory processes. The following diagram illustrates the key signaling pathways implicated in this plasticity.
Pathway Explanation: The therapeutic effects of TMS and tDCS are mediated through the induction of long-term potentiation (LTP)-like plasticity [54]. Stimulation triggers calcium influx through voltage-gated channels, activating NMDA receptors and initiating a molecular cascade. This leads to CREB phosphorylation and binding to the BDNF promoter, enhancing BDNF expression [53]. BDNF, via its TrkB receptor, facilitates AMPA receptor trafficking (including phosphorylation at Ser831) and dendritic spine remodeling, ultimately strengthening synaptic connections and promoting network-level reset of dysregulated circuits in addiction [53]. These structural and functional changes underpin observed clinical benefits, such as reduced craving and improved cognitive control [51] [53].
Efficacy Data and Outcome Analysis
Quantitative Synthesis of Clinical Outcomes
Table 1: Meta-Analysis Findings for rTMS and tDCS on SUD Outcomes
| Modality | Substance | Primary Outcome | Effect Size (Hedge's g) | Key Parameters | Citation |
|---|---|---|---|---|---|
| rTMS | Tobacco, Stimulants, Opioids | Craving/Use Reduction | Medium to Large (> 0.5) | HF to left DLPFC; Multiple sessions | [47] |
| rTMS (dTMS) | Various SUDs & Gambling | Craving Reduction | SMCC = -1.26 | H-coil targeting deep PFC | [52] |
| tDCS | Tobacco, Stimulants, Opioids | Craving/Use Reduction | Medium (highly variable) | Right anodal DLPFC; Longer sessions | [51] [47] |
| tDCS | Alcohol | Craving/Use Reduction | Less Consistent | Right anodal DLPFC | [51] [47] |
Table 2: Protocol Efficacy Based on Stimulation Parameters
| Parameter | More Effective Protocol | Less Effective Protocol | Clinical Rationale |
|---|---|---|---|
| Session Number | Multiple sessions (e.g., 10-15) [51] [47] | Single session [51] | Induces sustained neuroplasticity |
| Stimulation Frequency | High-frequency (10-20 Hz) rTMS [51] [47] | Low-frequency (≤1 Hz) rTMS [46] | Increases excitability of hypoactive DLPFC |
| Stimulation Target | Left DLPFC (rTMS) [47]; Right Anodal DLPFC (tDCS) [47] | Variable or mPFC targets [48] | DLPFC is a key node in executive control network |
| Stimulation Duration | tDCS > 10-15 min/session [51] | tDCS single short session | Longer duration required for subthreshold tDCS |
Key Efficacy Insights
- rTMS Superiority: rTMS generally demonstrates more robust and consistent effects on craving and consumption reduction compared to tDCS, attributed to its greater depth of penetration and stronger ability to directly depolarize neurons [51] [47].
- Target Specificity: The dorsolateral prefrontal cortex (DLPFC) is the most validated and effective target. For rTMS, the left DLPFC is most commonly stimulated with high frequencies to enhance cortical control. For tDCS, a right anodal/left cathodal montage may help rebalance hemispheric asymmetry in addiction [47].
- Treatment Durability: Multiple stimulation sessions are critical. Single sessions show little to no lasting benefit, whereas repeated sessions over days or weeks produce significant reductions in craving and substance use that are more likely to persist [51] [46].
Experimental Protocols and Methodologies
Standardized rTMS Protocol for Substance Craving
Objective: To reduce cue-induced craving and consumption in patients with cocaine use disorder [48] [47].
Equipment:
- rTMS machine with a figure-8 coil for focused stimulation or an H-coil for deep TMS.
- Neuronavigation system based on individual MRI for precise targeting.
- EMG system for monitoring motor-evoked potentials if targeting motor cortex for parameter setup.
Procedure:
- Subject Screening & Preparation: Confirm diagnosis using DSM-5 criteria. Exclude contraindications (e.g., metallic implants, seizure history). Obtain informed consent.
- Target Localization: Use neuronavigation to localize the left DLPFC. A common method is to identify the site 5-6 cm anterior to the motor hotspot along a parasagittal line [55] [47].
- Motor Threshold (MT) Determination: Determine resting MT over the primary motor cortex. This is defined as the minimum intensity required to elicit a motor-evoked potential of 50 μV in the contralateral hand muscle in 5 out of 10 trials.
- Stimulation Parameters:
- Frequency: 10 Hz
- Intensity: 100-120% of resting MT
- Train Duration: 4 seconds
- Inter-train Interval: 26 seconds
- Pulses per Session: 3000 pulses
- Total Session Duration: ~20 minutes
- Treatment Course: Administer sessions daily, 5 days per week, for 3-4 weeks (total 15-20 sessions).
- Outcome Assessment: Measure craving using validated scales (e.g., Visual Analog Scale for craving, Obsessive Compulsive Drinking Scale) pre- and post-session, and track substance use with self-report and biochemical verification (e.g., urine drug screens) [47].
Standardized tDCS Protocol for Executive Function Enhancement
Objective: To improve inhibitory control and reduce craving in alcohol use disorder [51] [47].
Equipment:
- tDCS stimulator with battery-driven constant current source.
- Saline-soaked surface sponge electrodes (typically 25-35 cm²).
Procedure:
- Subject Screening & Preparation: As above. Clean scalp area to ensure good electrode contact.
- Electrode Montage:
- Anodal Electrode: Place over the right DLPFC (located similarly to rTMS protocol, F4 according to the 10-20 EEG system).
- Cathodal Electrode: Place over the left DLPFC (F3) for a bilateral montage, or over the contralateral supraorbital area.
- Stimulation Parameters:
- Current Intensity: 2 mA
- Stimulation Duration: 20-30 minutes
- Ramp-Up/Ramp-Down: 30-60 seconds at beginning and end to minimize discomfort.
- Treatment Course: Daily sessions, 5 days per week, for 2-3 weeks (total 10-15 sessions).
- Outcome Assessment: Assess craving, administer cognitive tasks of inhibitory control (e.g., Go/No-Go, Stop-Signal Task), and monitor alcohol consumption (e.g., timeline followback method) [51] [47].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Materials and Equipment for Neuromodulation Research
| Item | Function/Application | Technical Notes |
|---|---|---|
| MRI-guided Neuronavigation System | Precisely targets cortical regions (e.g., DLPFC) based on individual anatomy. | Crucial for reproducibility; minimizes variability in coil/electrode placement [55]. |
| Figure-8 Coil | Standard TMS coil for focused stimulation of superficial cortical areas. | Induces a focal electric field; ideal for targeting specific prefrontal regions [46] [47]. |
| H-Coil | Deep TMS coil for modulating deeper brain structures (e.g., mPFC, insula). | Allows stimulation at depths up to 3.2-4 cm; broader field of stimulation [48] [52]. |
| tDCS Stimulator & Electrodes | Delivers low-intensity direct current via scalp electrodes. | Electrode size (25-35 cm²) and configuration (unilateral/bilateral) are key parameters [50] [47]. |
| Sham Stimulation Setup | Placebo control for blinding in clinical trials. | For TMS: coil tilting or magnetic shielding. For tDCS: brief current fade-in/fade-out [47]. |
| Electromyography (EMG) | Measures motor-evoked potentials (MEPs) for determining motor threshold. | Fundamental for calibrating TMS intensity and probing cortical excitability [55]. |
| Validated Craving Scales | Quantifies subjective craving (primary outcome). | e.g., Visual Analog Scale (VAS), Obsessive Compulsive Drinking Scale (OCDS) [47]. |
The targeted application of TMS and tDCS to restore cortical balance represents a paradigm shift in the therapeutic approach to SUDs. Evidence confirms that these modalities, particularly multi-session, high-frequency rTMS targeted at the left DLPFC, can significantly reduce craving and consumption across multiple substances by inducing beneficial neuroplasticity [51] [47] [52]. However, the field must overcome significant challenges, including high heterogeneity in stimulation protocols, small sample sizes in existing studies, and a lack of long-term follow-up data [48] [47]. Future research must prioritize large-scale, randomized controlled trials with standardized protocols, extended follow-up periods, and multimodal assessment that integrates neuroimaging and electrophysiology to elucidate the precise neural mechanisms of action. Furthermore, exploring accelerated stimulation protocols, personalized targets based on connectivity biomarkers, and combination therapies with behavioral interventions will be critical to fully realizing the potential of neuromodulation as a cornerstone in the treatment of addictive disorders.
Addiction is increasingly recognized as a chronic, relapsing brain disorder characterized by profound and lasting neuroplastic changes within key neural circuits governing reward, motivation, stress, and executive control [26] [40]. These drug-induced adaptations create a pathological learning state, where maladaptive drug-seeking behaviors become compulsive and entrenched [14]. The transition from voluntary drug use to compulsive addiction involves a cascade of neuroplastic events, including synaptic remodeling in the nucleus accumbens (NAc), altered glutamate homeostasis, and strengthened cue-reward associations that persist long after detoxification [26] [40]. This understanding of addiction as a pathology of staged neuroplasticity provides a critical framework for evaluating novel pharmacotherapies. Among the most promising emerging agents are Glucagon-like Peptide-1 Receptor Agonists (GLP-1 RAs), traditionally used for type 2 diabetes and obesity, and the serotonergic psychedelic psilocybin. This review provides an in-depth technical analysis of the preclinical and clinical evidence for these compounds, their proposed mechanisms targeting addiction-related neuroplasticity, detailed experimental methodologies, and the challenges and opportunities in their development as addiction therapeutics.
GLP-1 Receptor Agonists: From Metabolic to Addiction Therapeutics
Neurobiology and Mechanism of Action
Glucagon-like peptide-1 (GLP-1) is an incretin hormone secreted by intestinal L-cells and neurons in the nucleus tractus solitarius (NTS) [56]. Its receptor (GLP-1R), a class B G-protein coupled receptor, is expressed in peripheral tissues and widely throughout the central nervous system (CNS), including key regions involved in reward processing such as the ventral tegmental area (VTA), nucleus accumbens (NAc), amygdala, and hippocampus [56] [57]. Upon GLP-1 binding, GLP-1R primarily couples with the stimulatory G protein (Gs), activating adenylate cyclase to increase cyclic adenosine monophosphate (cAMP) production, which in turn activates Protein Kinase A (PKA) and Exchange Protein directly activated by cAMP 2 (Epac2) [56]. This signaling cascade modulates neuronal excitability, neurotransmitter release, and gene expression.
In the context of addiction, GLP-1R activation in the VTA is critical. The VTA contains dopamine neurons that project to the NAc and other limbic regions, forming the mesolimbic dopamine pathway—the primary neural substrate for reward and reinforcement. Preclinical evidence indicates that GLP-1R agonists reduce drug-induced dopamine release in the NAc [56]. By modulating the activity of VTA dopamine neurons, GLP-1 RAs attenuate the perceived rewarding value of addictive substances, thereby reducing drug intake and relapse-like behaviors in animal models [56] [58]. Beyond direct reward modulation, GLP-1 RAs also influence addiction through effects on stress systems and cognitive function [58].
Figure 1: GLP-1 Receptor Agonist Signaling Pathway. GLP-1RAs activate GLP-1 receptors, leading to reduced dopamine release in the nucleus accumbens (NAc) and attenuated drug reward.
Quantitative Evidence from Preclinical and Clinical Studies
Table 1: Summary of Preclinical Evidence for GLP-1 RAs in Substance Use Disorders
| Substance | Animal Model | GLP-1 RA Tested | Key Findings | Proposed Mechanism |
|---|---|---|---|---|
| Alcohol | Rodent self-administration | Exendin-4, Liraglutide | Reduced alcohol intake, seeking, and relapse [58] | Attenuated alcohol-induced dopamine release in NAc [58] |
| Psychostimulants (Cocaine, Amphetamine) | Rodent self-administration, Conditioned Place Preference | Exendin-4, Liraglutide | Decreased drug intake, lowered reinstatement of drug-seeking [56] | Modulation of dopamine release in reward circuit; reduced cue reactivity [56] |
| Opioids | Rodent self-administration | Semaglutide | Reduced cravings for opioids by ~40% in one study [59] | Not fully elucidated; may involve direct VTA action or stress pathway modulation [59] |
| Nicotine | Rodent self-administration | Liraglutide | Reduced nicotine self-administration [58] | Reduced rewarding effects of nicotine [58] |
Emerging, though still limited, clinical evidence largely supports the promising preclinical data. Observational studies and small clinical trials have reported potential benefits:
- Opioid Use Disorder (OUD): In a small study, a GLP-1 medication reduced cravings for opioids by 40% over three weeks [59]. Another observational study found that individuals with OUD or Alcohol Use Disorder (AUD) who took GLP-1s had a 40% lower rate of opioid overdose and a 50% lower rate of alcohol intoxication compared to those not on the medications [59].
- Alcohol Use Disorder (AUD): Preliminary phase 2 evidence suggests that semaglutide can improve measures of craving, heavy drinking, and hospitalizations in individuals with AUD [57].
- General Findings: A 2024 review concluded that while clinical studies have been limited, most support the safety and potential efficacy of GLP-1 RAs in treating Substance Use Disorders (SUDs), noting effects related to reward processing, stress, and cognitive function [58].
Detailed Experimental Protocol: Preclinical Reinstatement Model
The reinstatement model in rodents is a gold-standard procedure for evaluating the efficacy of GLP-1 RAs in preventing relapse. The following protocol details a typical experiment.
Objective: To determine the effect of a GLP-1 RA (e.g., Exendin-4) on cue-induced reinstatement of cocaine-seeking behavior.
Animals: Male and female Sprague-Dawley or Wistar rats (~300g), individually housed with ad libitum access to food and water, maintained on a reverse 12-hour light/dark cycle. All procedures require IACUC approval.
Materials and Reagents:
- Cocaine HCl: dissolved in sterile 0.9% saline.
- GLP-1 RA (e.g., Exendin-4): dissolved in sterile saline or vehicle.
- Operant Conditioning Chambers (Skinner boxes): equipped with two levers (active and inactive), a cue light above the active lever, a syringe pump for intravenous drug delivery, and a sound-attenuating cubicle.
- Intravenous Catheters: implanted into the right jugular vein.
Procedure:
- Surgery: Implant rats with intravenous catheters under aseptic conditions and ketamine/xylazine anesthesia. Allow 5-7 days for recovery with daily catheter flushing using heparinized saline and an antibiotic.
- Self-Administration Training (14 days, 3h sessions): Train rats to self-administer cocaine (e.g., 0.5 mg/kg/infusion) on a Fixed-Ratio 1 (FR1) schedule of reinforcement. Each activation of the active lever results in a cocaine infusion paired with a 5-second cue light presentation, followed by a 20-second timeout period. Responses on the inactive lever are recorded but have no consequence.
- Extinction (10-14 days, 3h sessions): Replace the cocaine solution with sterile saline in the syringe. The previously active lever presses now result only in a saline infusion with no cue presentation. Continue sessions until the number of active lever presses is ≤25% of the mean during the last 3 days of self-administration.
- Reinstatement Test (1 day, 2h session): Randomly assign rats to pretreatment groups (e.g., Vehicle vs. Exendin-4 at 1.0 µg/kg, administered subcutaneously 30 minutes prior to session). During the test session, responses on the previously active lever are reinforced by the conditioned cue light but not by cocaine (saline continues to be infused). The primary dependent variable is the number of active lever presses.
Data Analysis: Compare active lever presses during the reinstatement test between vehicle and GLP-1 RA treated groups using a t-test or one-way ANOVA. A significant reduction in active lever presses in the drug-treated group indicates an anti-relapse effect.
Psilocybin: A Psychedelic Approach to Rewiring Addiction
Neurobiology and Proposed Therapeutic Mechanisms
Psilocybin is a classic serotonergic psychedelic that acts as a partial agonist at several serotonin receptor subtypes, most notably the 5-HT2A receptor [60]. Its acute psychedelic effects are primarily mediated by 5-HT2A receptor activation in cortical regions, particularly layer V pyramidal neurons in the prefrontal cortex (PFC) [60]. In the context of addiction, its therapeutic mechanism is thought to be multifaceted, involving both acute neurobiological changes and sustained psychological effects.
The proposed mechanisms include:
- Disruption of Maladaptive Networks: Psilocybin-induced activation of 5-HT2A receptors leads to a temporary increase in neural entropy and global brain connectivity, which may disrupt rigid, maladaptive thought and behavior patterns associated with addiction [60].
- Promotion of Neuroplasticity: Like other psychedelics, psilocybin may promote neuroplasticity, including increases in dendritic spine growth and synaptogenesis, potentially facilitating the learning of new, non-addictive behaviors [60].
- Psychological and Contextual Insights: In the context of Psilocybin-Assisted Psychotherapy (PAP), the subjective mystical or insightful experience can lead to altered perspectives on one's life and relationship with substances, which is correlated with positive therapeutic outcomes [61] [60]. This is often supported by neuroimaging findings indicating normalization of brain activity in regions dysregulated in addiction [60].
Figure 2: Proposed Therapeutic Mechanisms of Psilocybin in Addiction. Psilocybin's active metabolite, psilocin, acts on the 5-HT2A receptor to produce neuroplastic, network-disrupting, and psychological effects that contribute to therapeutic outcomes.
Quantitative Evidence from Clinical Studies
Clinical research on psilocybin for SUDs, while still in early stages, has shown notable promise for certain disorders. A 2024 systematic review of 16 published studies provides a key summary of the evidence [60].
Table 2: Summary of Clinical Evidence for Psilocybin in Substance Use Disorders
| Substance | Study Design (Number of Studies) | Dosing Protocol (Psilocybin) | Key Efficacy Findings | Safety and Tolerability |
|---|---|---|---|---|
| Alcohol (AUD) | Open-label trials, cross-sectional (7) | 20-40 mg/70 kg (psychedelic doses) in PAP | Significant reductions in alcohol consumption, fewer heavy drinking days, increased abstinence rates [60]. | Generally safe in controlled settings. Adverse effects typical of psychedelics (anxiety, transient BP/heart rate increase) [60]. |
| Tobacco (TUD) | Open-label trials (5) | 20-30 mg/70 kg (psychedelic doses) in PAP | High smoking cessation rates; mystical experiences predicted long-term success [60]. | Generally safe in controlled settings. |
| Opioid (OUD) | Open-label trial (1) | Psychedelic doses in PAP | Showed potential in reducing opioid dependence [60]. | Generally safe in controlled settings. |
| Cocaine (CUD) | Open-label trial (1) | Psychedelic doses in PAP | Mixed findings; limited conclusive evidence [60]. | Generally safe in controlled settings. |
Recent research from the Yale Program for Psychedelic Science also reports "quite encouraging" results in a pilot study of over 30 participants with severe, treatment-resistant OCD, a disorder sharing compulsivity features with addiction, noting greater effectiveness than established standard of care [61].
Detailed Experimental Protocol: Clinical Psilocybin-Assisted Psychotherapy
The following outlines a standardized protocol for a clinical trial investigating psilocybin for Alcohol Use Disorder (AUD), based on established methodologies [61] [60].
Objective: To evaluate the efficacy and safety of psilocybin-assisted psychotherapy (PAP) in reducing alcohol consumption in participants with moderate to severe AUD.
Participants: Adults (age 25-65) meeting DSM-5 criteria for moderate to severe AUD, medically and psychiatrically stable (excluding other active SUDs or psychotic disorders). Participants must agree to abstain from alcohol before and after dosing sessions.
Materials and Reagents:
- Psilocybin: Synthesized, pharmaceutical-grade psilocybin in capsules (doses: 25 mg/70 kg and 40 mg/70 kg for active dose; 1-5 mg/70 kg for active placebo control).
- Therapy Manual: A standardized psychotherapy guide focusing on preparation, support during the session, and integration afterward.
- Setting: A comfortable, living-room-like environment with a couch, audio system for music, and medical monitoring equipment (e.g., blood pressure cuff, pulse oximeter).
- Ratings Scales: Primary: Percentage of heavy drinking days (PHDD), Alcohol Use Disorders Identification Test (AUDIT). Secondary: Mystical Experience Questionnaire (MEQ), Ego-Dissolution Inventory (EDI).
Procedure:
- Screening & Informed Consent (1-3 visits): Comprehensive medical/psychiatric screening to ensure safety and eligibility. Obtain full informed consent, emphasizing the experimental nature and potential risks of the psychedelic experience.
- Preparation Sessions (2-3 sessions, 4-8 hours total): Participants meet with two trained therapists to build rapport, establish intention, discuss the effects of psilocybin, and develop strategies for navigating the acute experience. Safety procedures are reviewed.
- Dosing Session 1 (8-10 hours): Participants are randomized to receive either a low (placebo control) or moderate/high dose (25 mg/70 kg) of psilocybin. They arrive fasting, take the capsule, and recline on a couch. Therapists provide non-directive support throughout the session, which lasts 6-8 hours. Standardized music playlists are used. Vital signs are monitored. Participants remain at the facility until the next morning.
- Integration Session 1 (1-2 sessions, week following dosing): Participants meet with therapists to process and make meaning of their experience, discussing insights and how they relate to their AUD and life context.
- Dosing Session 2 & Integration (4-8 weeks after first dose): The procedure is repeated, with the active dose group often receiving a higher dose (e.g., 40 mg/70 kg) to deepen the experience. Followed by further integration.
- Follow-up Assessments: Conducted at 1, 3, 6, and 12 months post-treatment to assess long-term outcomes on drinking measures and psychological well-being.
Data Analysis: Primary analysis compares change in PHDD from baseline to the end of the trial (e.g., 4 weeks after the last dosing session) between the high-dose and control groups using a mixed-model repeated measures ANOVA.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Addiction Pharmacology Research
| Item / Reagent | Function / Application in Research | Example Use Case |
|---|---|---|
| GLP-1 Receptor Agonists (e.g., Exendin-4, Liraglutide, Semaglutide) | Selective activation of central and peripheral GLP-1 receptors to probe their role in addiction behaviors. | Subcutaneous or intraperitoneal injection in rodent reinstatement models to assess anti-relapse efficacy [56] [58]. |
| Pharmaceutical-Grade Psilocybin | The primary investigational compound for clinical trials in PAP; must be synthesized to GMP standards for regulatory approval. | Administered orally in capsules within clinical trials for AUD and TUD [60]. |
| Operant Conditioning Chambers | Controlled environments for measuring drug self-administration, extinction, and cue-induced reinstatement in animal models. | Training rats to press a lever for intravenous cocaine infusions paired with a cue light [26]. |
| In Vivo Microdialysis | Technique for measuring extracellular levels of neurotransmitters (e.g., dopamine, glutamate) in specific brain regions of behaving animals. | Quantifying the reduction in cocaine-induced NAc dopamine release following GLP-1 RA administration [56]. |
| fMRI / PET Imaging | Non-invasive methods for assessing brain activity, connectivity, and receptor occupancy in human participants. | Measuring normalization of brain activity in the prefrontal cortex and limbic regions following PAP in individuals with AUD [60]. |
| Validated Clinical Scales (e.g., AUDIT, MEQ) | Standardized tools for quantifying clinical symptoms, craving, and subjective experiences in trials. | Using the Mystical Experience Questionnaire (MEQ) to correlate the quality of the psychedelic experience with long-term smoking abstinence [60]. |
The repurposing of GLP-1 RAs and the investigation of psilocybin represent a paradigm shift in addiction therapeutics, moving toward agents that directly target the core neuroplasticity underlying this disorder. However, significant translational challenges remain.
For GLP-1 RAs, a primary hurdle is the limited blood-brain barrier (BBB) penetration of current compounds, driving research into novel, CNS-penetrant analogues [56]. Furthermore, there is considerable interindividual variability in treatment response, likely influenced by genetic, metabolic, and environmental factors, necessitating a personalized medicine approach [56] [59]. From a development perspective, high costs, regulatory complexity, and intellectual property hurdles surrounding drug repurposing are slowing venture investment and clinical progress [62].
For psilocybin, the major challenge lies in standardizing the therapeutic protocol and dissociating the pharmacological effects from the extensive psychological support. Larger, more rigorous double-blind, placebo-controlled trials are needed to definitively establish efficacy across different SUDs [60]. The Schedule I status of psilocybin creates significant regulatory and logistical barriers to research, despite policy shifts in some states [61] [62].
Future research must focus on elucidating the precise molecular and circuit-level mechanisms through which these compounds facilitate therapeutic neuroplasticity, identifying patient biomarkers predictive of response, and optimizing treatment protocols to maximize efficacy, accessibility, and safety. The convergence of metabolic psychiatry (via GLP-1 RAs) and psychedelic science marks an extraordinarily promising frontier in the quest to develop transformative treatments for addiction.
Troubleshooting Recovery: Overcoming Relapse and Optimizing Interventions
The Challenge of Persisting Craving and Addiction Memory
Addiction is fundamentally a disorder of neuroplasticity, characterized by the formation of robust and persistent memories that associate drug-related cues with intense craving and compulsive drug-seeking behavior. Unlike normal memory processes, addiction memory represents a pathological learning process where drugs of abuse hijack the brain's natural reward and memory systems [26] [40]. This phenomenon explains why individuals recovering from addiction continue to experience powerful cravings even after prolonged abstinence, often triggered by environmental cues, stress, or drug-associated contexts. The persistence of craving and addiction memory poses one of the most significant challenges in addiction treatment, as these deeply encoded memories can trigger relapse months or years after the last drug use [26].
Research over the past decade has established that addiction, once established, becomes a chronic illness with relapses and remissions, requiring chronic treatment approaches based on understanding the fundamental nature of these changes in the brain [26]. The central nervous system changes underlying conditioned drug-seeking behavior involve stable and potentially permanent alterations in neural circuitry [26]. This whitepaper examines the neurobiological mechanisms underlying addiction memory persistence, explores experimental approaches for its investigation, and discusses emerging therapeutic strategies that target the neuroplastic underpinnings of this devastating phenomenon.
Neurobiological Mechanisms of Addiction Memory
Structural and Functional Neural Plasticity in Addiction
Addictive drugs induce profound structural and functional changes in brain regions critical for reward, motivation, and memory. These drug-induced neuroadaptations occur at multiple levels, from molecular and cellular alterations to circuit-level reorganization.
Table 1: Neural Plasticity Changes in Addiction Memory Formation
| Brain Region | Plasticity Change | Functional Consequence |
|---|---|---|
| Nucleus Accumbens | Increased dendritic spine density in medium spiny neurons [26] | Enhanced drug-seeking behavior |
| Prefrontal Cortex | Reduced glutamate levels; disrupted glutamate homeostasis [26] | Impaired inhibitory control; heightened craving |
| Hippocampus | Reduced neurogenesis with chronic opioid exposure [26] | Strengthened drug-context associations |
| Ventral Tegmental Area | Reduced dendritic spines with chronic morphine [26] | Altered dopamine signaling |
| Amygdala | Increased extracellular signal-related kinase (ERK) [26] | Enhanced cue-induced drug seeking |
The dopamine system plays a pivotal role in the initial stages of addiction memory formation. All drugs of abuse activate dopamine circuits in brain reward systems through various mechanisms, creating a powerful reinforcement signal that stamps in drug-associated memories [26]. However, the transition to addiction involves more widespread neuroadaptations in glutamatergic systems that mediate learning and memory processes [40]. With repeated drug exposure, the reward system becomes reflexively activated by drug-associated cues alone, leading to a powerful drive toward drug-taking behavior [26].
Molecular Mechanisms of Addiction Memory Persistence
At the molecular level, addiction memory formation involves a cascade of intracellular signaling events that ultimately remodel neural circuits. Key molecular players include:
- Brain-Derived Neurotrophic Factor (BDNF): Levels increase in the ventral tegmental area and nucleus accumbens during abstinence, contributing to the "incubation" of craving over time [26].
- DeltaFosB: This transcription factor accumulates in dopamine terminals in the cortex and striatum with repeated drug exposure and appears to be involved in the development of motivated behaviors [26].
- Glutamate Homeostasis Disruption: Chronic drug use leads to reduced basal extracellular glutamate levels and potentiated release of synaptic glutamate during drug-seeking [26].
- Immediate Early Genes: Drugs of abuse rapidly induce expression of genes like c-fos and Arc, which are involved in synaptic plasticity and memory formation [63].
The stabilization of addiction memories involves protein synthesis-dependent consolidation processes similar to those underlying normal memory formation, but with distinct mechanistic features that may contribute to their exceptional persistence and resistance to extinction [40].
Experimental Models and Assessment Methodologies
Animal Models of Addiction Memory
Several well-established animal models permit the investigation of addiction memory and persistence of drug-seeking behavior:
Self-Administration and Reinstatement Models: Rats are trained to self-administer drugs intravenously. After extinction of the drug-seeking behavior, various triggers (cues, stress, or a single drug prime) are tested for their ability to reinstate drug-seeking [26].
Conditioned Place Preference: Animals develop a preference for environments paired with drug effects, providing a measure of the rewarding properties of drugs and their ability to form context-drug associations [40].
Incubation of Craving Model: Animals are trained to self-administer drugs, followed by forced abstinence. The strength of drug-seeking behavior in response to drug-associated cues is then tested at different time points during abstinence. This model demonstrates that craving intensifies ("incubates") during the first weeks of abstinence [26].
Table 2: Quantitative Measures in Addiction Memory Research
| Measurement Approach | Experimental Readout | Significance in Addiction Memory |
|---|---|---|
| Urine Drug Screens | Percentage of negative screens over time [64] | Objective measure of reduced use; 75% negative screens associated with improved functioning in cocaine trials |
| Brain Imaging (fMRI/PET) | Limbic activation during cue-induced craving [26] | Neural correlate of craving; rapid activation even with subliminal cues |
| Dendritic Spine Analysis | Spine density and morphology changes [26] | Structural basis of persistent addiction memories |
| Extracellular Glutamate | Microdialysis measures in nucleus accumbens [26] | Indicator of glutamate homeostasis disruption |
| Real-time fMRI Biofeedback | Frontal lobe activation during craving suppression [26] | Measure of inhibitory control capacity |
Human Experimental Approaches
Human research on addiction memory utilizes multiple complementary approaches:
Brain Imaging Studies: Functional MRI and PET imaging reveal that drug-associated cues activate limbic regions (including the amygdala and nucleus accumbens) in addicted individuals, even after prolonged abstinence [26]. These cue-induced activations correlate strongly with self-reported craving.
Psychophysiological Measures: Craving responses can be measured through physiological indicators such as galvanic skin response, heart rate, and salivary responses to drug-related cues.
Cognitive Tasks: Measures of attentional bias toward drug-related stimuli and impaired response inhibition provide behavioral indices of addiction memory strength.
Real-time fMRI Biofeedback: This emerging approach allows researchers to provide patients with feedback about their frontal lobe activation, helping them learn to activate inhibitory structures to suppress drug craving [26].
Emerging Therapeutic Approaches Targeting Addiction Memory
Pharmacological Interventions
Novel pharmacological approaches aim to reverse or disrupt the neuroplastic changes underlying persistent addiction memories:
N-acetylcysteine: This compound helps restore glutamate homeostasis in the nucleus accumbens by promoting cystine-glutamate exchange. Clinical studies show it reduces desire for cocaine and decreases cigarette smoking and pathological gambling [26].
GLP-1 Receptor Agonists: Originally developed for diabetes and obesity, drugs like semaglutide and liraglutide have shown unexpected benefits for addiction. They modulate dopamine and glutamate transmission in reward circuits and have demonstrated efficacy in reducing alcohol, nicotine, and cocaine intake in preclinical models [65].
Psychedelics: Compounds like psilocybin and LSD promote neuroplasticity, potentially "resetting" maladaptive neural circuits. They rapidly stimulate dendritogenesis, synaptogenesis, and expression of plasticity-related genes, with clinical improvements lasting months or years after treatment [63].
Medications Targeting Intracellular Signaling: Drugs that modulate mTOR, ERK, and other intracellular signaling pathways involved in memory consolidation and reconsolidation offer promise for disrupting addiction memory persistence.
Behavioral and Neuromodulatory Approaches
Non-pharmacological interventions also show promise for modifying addiction memories:
Extinction-Based Therapies: Repeated exposure to drug-associated cues in the absence of drug consumption can weaken cue-drug associations, though the persistence of these effects is often limited.
Memory Reconsolidation Interference: Timing behavioral interventions during the brief window when memories are destabilized after retrieval may allow for permanent modification of addiction memories.
Cognitive Behavioral Therapy (CBT): CBT teaches individuals to recognize, avoid, and cope with situations where they are likely to experience craving and drug use [14].
Non-Invasive Brain Stimulation: Techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) can modulate cortical excitability and disrupt addiction-related neural circuits [66].
Research Reagents and Methodological Tools
Table 3: Essential Research Reagents for Investigating Addiction Memory
| Research Reagent | Application/Function | Experimental Use |
|---|---|---|
| N-acetylcysteine | Restores glutamate homeostasis via cystine-glutamate exchange [26] | Reduces reinstatement of drug-seeking in animal models; human clinical trials for addiction |
| Varenicline | Nicotine receptor partial agonist; reduces withdrawal and smoking satisfaction [2] | Smoking cessation clinical trials; model for nicotine addiction mechanisms |
| BDNF Assays | Quantifies brain-derived neurotrophic factor levels [26] [63] | Measures neuroplasticity changes in response to drugs or treatments |
| Positron Emission Tomography (PET) Radioligands | Labels synaptic density proteins (e.g., SV2A) [63] | Quantifies synaptic changes in human addiction |
| Dopamine Receptor Ligands | Labels dopamine receptors (e.g., raclopride for D2 receptors) [26] | Measures dopamine release during craving using displacement assays |
| Ketanserin | Selective 5-HT2A receptor antagonist [63] | Blocks psychedelic effects and neuroplasticity to study mechanism |
| Semaglutide | GLP-1 receptor agonist with central nervous system penetration [65] | Investigates metabolic-reward system interactions in addiction models |
Signaling Pathways in Addiction Memory
The following diagram illustrates key signaling pathways involved in addiction memory persistence, highlighting potential therapeutic targets:
Signaling Pathways in Addiction Memory Persistence
This diagram illustrates how drug cue exposure triggers neurotransmitter release and subsequent intracellular signaling cascades that ultimately lead to structural and functional neural changes supporting addiction memory persistence.
The persistence of craving and addiction memory represents a formidable challenge in addiction treatment, rooted in stable neuroplastic adaptations that hijack normal learning and memory systems. Research over the past decade has illuminated the molecular mechanisms, circuit-level changes, and structural adaptations that underlie this phenomenon. Importantly, this understanding is now driving the development of novel therapeutic approaches that specifically target the neuroplastic underpinnings of addiction memory.
Future research directions should focus on: (1) Developing more precise biomarkers of neuroplasticity to track addiction memory strength and treatment response; (2) Optimizing timing interventions to capitalize on windows of enhanced plasticity; (3) Exploring combination therapies that simultaneously target multiple mechanisms underlying addiction memory; (4) Investigating individual differences in vulnerability to addiction memory formation and persistence; and (5) Developing non-invasive neuromodulation approaches that can directly reverse the circuit abnormalities associated with addiction memory.
As our understanding of the neurobiology of addiction memory deepens, we move closer to effective strategies that can permanently disrupt the cycle of craving and relapse, offering hope for lasting recovery from substance use disorders.
Addressing Co-occurring Mental Health Disorders and Self-Medication
The intricate relationship between co-occurring mental health disorders and substance use disorders (SUDs), often initiated through self-medication, represents a significant challenge and opportunity in addiction neuroscience. This whitepaper examines this complex interplay through the lens of neuroplasticity, detailing the shared neural pathways that underlie both conditions and the mechanisms through which persistent substance use creates lasting maladaptive changes in brain circuitry. We synthesize current neurobiological evidence, present standardized methodological approaches for investigating these mechanisms, and outline emerging therapeutic strategies that leverage neuroplasticity for recovery. The findings underscore the necessity of integrated treatment approaches that simultaneously address both psychiatric symptoms and substance use through targeted neurobiological interventions.
The self-medication hypothesis proposes that individuals with untreated mental health disorders frequently initiate substance use as a means to alleviate distressing psychiatric symptoms [67]. Epidemiological studies demonstrate that approximately 50% of individuals with SUDs have co-occurring mental health conditions that require integrated treatment approaches [68]. This comorbidity creates a complex clinical presentation that significantly impacts treatment outcomes, with dual diagnosis often leading to more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization compared to either disorder alone [69].
From a neuroplasticity perspective, both mental health disorders and substance use involve maladaptive changes in brain structure and function that follow similar neural pathways. Neuroplasticity, defined as the nervous system's ability to change its activity in response to intrinsic or extrinsic stimuli by reorganizing its structure, functions, or connections, provides a unifying framework for understanding the development and maintenance of co-occurring disorders [3] [70]. The chronicity of mental health illness and the underlying brain dysregulation associated with co-occurring disorders tend to follow a trajectory that is chronic, recurring, and episodic, with slow recovery and high rates of relapse [70]. This pattern reflects the durable nature of maladaptive neuroplastic changes that occur in these conditions.
Research landscape analyses indicate that investigations into dual diagnosis have been steadily increasing since the mid-1990s, with emerging research topics focusing on neurobiological aspects, innovative interventions, and special populations [69]. This whitepaper synthesizes current understanding of these mechanisms, methodological approaches for investigation, and targeted interventions that leverage neuroplasticity principles to disrupt the cycle of self-medication and promote recovery.
Neurobiological Mechanisms of Co-occurring Disorders
Shared Neural Pathways and Neurotransmitter Systems
The neurobiological interface between mental health disorders and substance use disorders centers on overlapping neural circuits, particularly those regulating reward processing, stress response, and emotional control:
Dopaminergic Pathways: Central to both disorders is the mesolimbic dopamine pathway, comprising the ventral tegmental area (VTA) and nucleus accumbens (NA) [3] [8]. This pathway mediates reward processing, motivation, and reinforcement learning. Substances of abuse cause dopamine release from the VTA to the prefrontal cortex, amygdala, and striatum, producing long-term plastic changes that increase motivation for the substance while driving tolerance and dependence [70]. In mental health disorders such as depression and schizophrenia, dysregulation of this same pathway contributes to anhedonia and disrupted reward processing.
Glutamatergic Signaling: The glutamate system, particularly NMDA and AMPA receptors, serves as a primary mechanism for synaptic plasticity through long-term potentiation (LTP) and long-term depression (LTD) [70]. These receptors function as "coincidence detectors" that strengthen synaptic connections in response to correlated pre- and postsynaptic activity. Substance use and stress associated with mental health disorders disrupt the delicate balance of glutamatergic signaling, leading to maladaptive synaptic changes in prefrontal and limbic regions.
Other Neurotransmitter Systems: Serotonergic, GABAergic, opioidergic, and endocannabinoid systems also demonstrate overlapping dysregulation in co-occurring disorders [3]. For instance, chronic dopamine elevation can decrease serotonin function by up to 75% in the PFC, dorsal striatum, nucleus accumbens, hippocampus, and hypothalamus, contributing to both depressive symptoms and substance dependence [3].
Neuroplastic Adaptations in Specific Comorbidities
Different psychiatric comorbidities demonstrate distinct neurobiological interactions with substance use, suggesting unique neuroplastic adaptation patterns:
Table 1: Neurobiological Interactions in Specific Co-occurring Disorders
| Co-occurring Disorder | Effect on SUD Neurobiology | Key Brain Regions Affected |
|---|---|---|
| Schizophrenia | Amplifying effects on SUD-related changes | Prefrontal cortex, hippocampus, striatum |
| Cluster B/C Personality Disorders | Amplifying and unique effects | Prefrontal cortex, amygdala |
| ADHD | Unique neurobiological changes | Prefrontal cortex, basal ganglia |
| Depression | Attenuating or no additional effects | Prefrontal cortex, anterior cingulate |
| PTSD | Contradictory and inconsistent effects | Amygdala, hippocampus, medial PFC |
Research indicates that co-occurring schizophrenia and personality disorders appear to amplify SUD-related neurobiological changes, while ADHD, schizophrenia, and personality disorders demonstrate unique neurobiological effects not observed in SUD alone [71]. Conversely, depression appears to have attenuating or no additional effects on SUD-related neurobiology, while findings on PTSD remain contradictory and inconsistent across studies [71].
These differential effects highlight the importance of precise diagnostic characterization in both research and clinical practice, as neuroplastic mechanisms vary substantially across different forms of comorbidity.
Methodological Approaches for Investigating Neuroplasticity Mechanisms
Neuroimaging Protocols for Assessing Neuroplastic Changes
Modern neuroscience employs multiple imaging modalities to investigate neuroplastic changes in co-occurring disorders:
Structural MRI Protocols: Voxel-based morphometry (VBM) techniques allow measurement of volume and thickness changes in brain structures. Standardized protocols include T1-weighted magnetization-prepared rapid acquisition gradient echo (MPRAGE) sequences with 1mm³ isotropic resolution. Processing pipelines (e.g., FSL, FreeSurfer) enable quantification of gray matter changes reflective of neuroplasticity in adults after interventions [70]. Analysis focuses on regions of interest including dorsolateral PFC, anterior cingulate, hippocampus, and amygdala, which demonstrate volumetric changes in both mental health disorders and SUDs.
Functional MRI (fMRI) Protocols: Task-based and resting-state fMRI protocols assess functional connectivity changes. Echo planar imaging (EPI) sequences with TR=2000ms, TE=30ms, and 3-4mm isotropic voxels are standard. For task-based fMRI, reward processing paradigms (e.g., monetary incentive delay task) and emotional face matching tasks probe dysfunction in reward and emotional regulation networks. Resting-state protocols examine intrinsic functional connectivity within and between networks including the default mode, salience, and executive control networks [70].
Diffusion Tensor Imaging (DTI) Protocols: DTI sequences with 30+ diffusion directions, b-values of 1000 s/mm², and 2-2.5mm isotropic resolution assess white matter integrity through fractional anisotropy and mean diffusivity metrics. Tract-based spatial statistics (TBSS) or tractography approaches evaluate structural connectivity in pathways connecting prefrontal, striatal, and limbic regions [70].
Positron Emission Tomography (PET) Protocols: Radioligands targeting dopamine (e.g., [¹¹C]raclopride), serotonin (e.g., [¹¹C]DASB), and glutamate (e.g., [¹¹C]ABP688) systems quantify neurotransmitter system dysfunction. Standardized uptake values and binding potential calculations assess receptor availability and density in states of intoxication, withdrawal, and recovery [70].
Experimental Models for Investigating Self-Medication Behaviors
Animal models and human laboratory paradigms provide controlled methods for investigating self-medication mechanisms:
Animal Model Protocols: Rodent models of comorbid disorders involve genetic manipulations (e.g., DAT knockdown mice for ADHD models), environmental manipulations (e.g., chronic mild stress for depression models), or early life stress (e.g., maternal separation for anxiety models). Subsequent drug self-administration paradigms (operant conditioning with fixed-ratio or progressive-ratio schedules) quantify substance use behaviors. Optogenetics or chemogenetics (DREADDs) allow circuit-specific manipulation to establish causal relationships [8].
Human Laboratory Protocols: Controlled laboratory studies administer substances (alcohol, stimulants) to individuals with specific mental health disorders (e.g., social anxiety disorder, PTSD) using placebo-controlled, double-blind designs. Subjective effects (Visual Analog Scales for anxiety, craving), physiological measures (heart rate, cortisol), and neuroimaging assessments evaluate acute responses that may underlie self-medication tendencies [67].
Longitudinal Cohort Studies: Prospective designs follow individuals with mental health disorders who do not initially have SUDs, assessing substance use initiation patterns, contextual factors, and neurobiological changes over time (e.g., Adolescent Brain Cognitive Development Study). Multilevel modeling approaches account for nested data structures and missing data in longitudinal designs [67].
The following diagram illustrates the integrated experimental workflow for investigating self-medication neurobiology:
Experimental Workflow for Self-Medication Research
Neuroplasticity-Targeted Interventions for Co-occurring Disorders
Pharmacological Approaches
Medication-assisted treatment (MAT) forms a cornerstone of intervention for co-occurring disorders, with several evidence-based approaches:
Table 2: Pharmacological Interventions Targeting Neuroplasticity in Co-occurring Disorders
| Medication Class | Neuroplasticity Mechanism | Evidence in Co-occurring Disorders |
|---|---|---|
| Buprenorphine/ Methadone | μ-opioid receptor agonism; normalizes dopamine dysregulation | Opioid use disorder with PTSD, depression; reduces craving and withdrawal |
| Naltrexone | Opioid receptor antagonism; modulates dopamine reward pathway | Alcohol use disorder with PTSD; reduces rewarding effects of alcohol |
| Acamprosate | GABA stabilization; glutamate modulation | Alcohol use disorder with anxiety disorders; reduces hyperglutamatergic state |
| Atypical Antipsychotics | D2/5-HT2A receptor modulation; promotes cortical synaptogenesis | Schizophrenia with SUD; reduces psychosis and substance craving |
| Antidepressants (SSRIs/SNRIs) | Enhanced monoamine transmission; increases BDNF expression | Depression/anxiety with SUD; improves mood and reduces self-medication |
FDA-approved medications like buprenorphine, methadone, naltrexone, disulfiram, and acamprosate work to restore normal brain chemistry while reducing cravings and withdrawal symptoms in individuals with alcohol or opioid addictions, and have shown utility in co-occurring disorders [68]. These medications essentially create a neurochemical environment conducive to adaptive neuroplasticity by stabilizing neurotransmitter systems disrupted in both mental health and substance use disorders.
Lifestyle Medicine and Behavioral Interventions
Lifestyle interventions promote healthy neuroplasticity through multiple mechanisms including increased synaptogenesis, enhanced neurotrophic factors, improved mitochondrial function, and reduced neuroinflammation [3]:
Physical Exercise Protocols: Aerobic exercise regimens (30+ minutes, 3-5×/week at 60-80% maximum heart rate) demonstrate significant benefits for co-occurring disorders. A 2014 meta-analysis of 22 studies with 1,487 participants with SUDs found that physical exercise increased abstinence rates (OR=1.69), moderated withdrawal symptoms (SMD=-1.24), and reduced anxiety (SMD=-0.31) and depressive symptoms (SMD=-0.47) [3]. Mechanisms include increased release of neurotrophic factors (BDNF), enhanced serotonin function, and reduced neuroinflammation.
Mindfulness-Based Interventions: Standardized protocols include Mindfulness-Based Stress Reduction (8-week program with weekly 2.5-hour sessions and daily home practice) and Mindfulness-Based Relapse Prevention. These approaches promote neuroplastic changes in prefrontal regulatory regions while reducing amygdala reactivity, with studies showing measurable improvements in stress reduction and relapse prevention [68] [6].
Cognitive-Behavioral Therapies: Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) directly target maladaptive neural pathways through cognitive restructuring and emotional regulation training. These approaches help rewire thought patterns to reduce cravings and promote more positive behaviors, essentially leveraging the brain's neuroplastic capacity to create more adaptive cognitive-emotional-behavioral patterns [68] [6].
The following diagram illustrates how various interventions target different components of the shared neurobiology of co-occurring disorders:
Intervention Targets in Shared Neurobiology
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Investigating Co-occurring Disorders
| Reagent/Material | Application | Specific Function |
|---|---|---|
| CRISPR/Cas9 Systems | Genetic modeling | Targeted gene editing for disease-relevant polymorphisms (e.g., BDNF, COMT, OPRM1) |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Circuit manipulation | Chemogenetic control of specific neural pathways in rodent models |
| Calcium Indicators (GCaMP系列) | Neural activity imaging | Real-time monitoring of neuronal ensemble activity in vivo |
| Radioligands ([¹¹C]raclopride, [¹¹C]DASB) | PET imaging | Quantification of dopamine D2/D3 and serotonin transporter availability |
| BDNF ELISA Kits | Protein quantification | Measurement of brain-derived neurotrophic factor in serum or tissue |
| RNAseq Libraries | Transcriptomic profiling | Genome-wide expression analysis of postmortem brain tissue |
| fMRI Task Paradigms | Functional imaging | Standardized probes of reward processing (monetary incentive delay) and emotional regulation (face matching) |
These research tools enable multidimensional investigation of neuroplasticity mechanisms across molecular, cellular, circuit, and behavioral levels. Combined with the methodological approaches outlined in Section 3, they provide a comprehensive toolkit for elucidating the complex neurobiology of co-occurring disorders and developing more targeted interventions.
The investigation of co-occurring mental health disorders and self-medication through a neuroplasticity framework provides powerful insights for both understanding mechanisms and developing interventions. Research indicates that integrated treatment approaches that simultaneously address both conditions are essential for successful recovery and improved patient outcomes [69]. The emerging understanding of how different co-occurring psychiatric disorders have distinct effects on the neurobiology of SUD provides a roadmap for more personalized and targeted interventions [71].
Future research directions should include: (1) longitudinal studies examining neuroplastic changes across the developmental trajectory of co-occurring disorders; (2) increased focus on the role of glial cells (astrocytes, microglia) in mediating neuroplastic changes in co-occurring disorders; (3) development of novel therapeutic agents that specifically target neuroplasticity mechanisms; and (4) optimization of non-invasive neuromodulation approaches (TMS, tDCS) for circuit-specific restoration of adaptive plasticity. Additionally, research on how environmental and sociocultural factors influence neuroplasticity in these conditions represents an important emerging frontier [69].
As research methodologies continue to advance, particularly in areas of multi-omics integration, circuit neuroscience, and computational modeling, our ability to precisely characterize and therapeutically modulate neuroplasticity in co-occurring disorders will continue to improve. This progress holds significant promise for developing more effective, neurobiologically-informed interventions that can disrupt the cycle of self-medication and promote sustainable recovery.
Optimizing Stimulation Parameters for Neuromodulation Therapies
The efficacy of neuromodulation therapies is critically dependent on the precise selection of stimulation parameters, a challenge particularly relevant in the context of addiction treatment. Substance use disorders (SUDs) involve profound alterations in the brain's reward circuitry, including the mesolimbic dopamine pathway connecting the ventral tegmental area (VTA) to the nucleus accumbens [8] [72]. These neuroadaptations, driven by the brain's inherent neuroplasticity, create a cycle of addiction characterized by binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation stages [8]. Neuromodulation aims to reverse these maladaptive plastic changes by delivering targeted electrical, magnetic, or ultrasound energy to specific neural circuits. However, given the dynamic nature of both addiction and neuroplasticity, a one-size-fits-all approach to parameter setting is insufficient. This guide synthesizes current evidence and methodologies for optimizing stimulation parameters across various neuromodulation modalities, providing researchers and clinicians with a structured framework for maximizing therapeutic outcomes in addiction and related neurological disorders.
Core Stimulation Parameters and Their Physiological Effects
Fundamental Parameters and Their Roles
Stimulation parameters define the physical characteristics of the energy delivered to neural tissue. Each parameter interacts with biological tissue differently, influencing both efficacy and safety.
- Pulse Width (μs): The duration of each individual electrical pulse. Wider pulse widths generally recruit a larger volume of neural tissue and can activate axons farther from the electrode but consume more power and may increase the risk of side effects [73] [74].
- Frequency (Hz): The number of pulses delivered per second. Frequency is a primary determinant of the neural response, with low frequencies (e.g., < 30 Hz) often yielding inhibitory effects and high frequencies (e.g., > 100 Hz) producing excitatory effects on the target neural population [73] [75].
- Amplitude/Current (mA or V): The intensity of the stimulation. Amplitude directly influences the spatial extent of neural activation. Sub-therapeutic amplitudes fail to modulate the target circuit, while excessive amplitudes can lead to side effects from stimulation of adjacent structures [75].
- Duty Cycle (%): The temporal pattern of stimulation, defined by the ratio of "on" time to the total cycle time. Continuous stimulation delivers constant input, while intermittent cycling (e.g., 1 minute on/5 minutes off) can conserve battery life and potentially reduce tolerance [73] [75].
- Waveform: The shape of the electrical pulse (e.g., monophasic, biphasic). Biphasic pulses are commonly used as they help balance charge delivery, minimizing the risk of tissue damage.
Parameter Interactions and the Therapeutic Window
These parameters do not operate in isolation; they interact to define the therapeutic window—the range of settings that provide maximal symptom control without adverse effects. The total charge delivered per unit time is a key composite metric, often calculated as the product of amplitude, pulse width, and frequency. A recent large-scale VNS study highlighted that seizure-free patients had a significantly lower total charge (122.4 mC) compared to those with persistent seizures (250.1 mC), underscoring the importance of optimizing this overall dosage [75].
Evidence-Based Parameter Optimization Across Modalities
Deep Brain Stimulation (DBS)
DBS involves the surgical implantation of electrodes to deliver electrical stimulation to deep brain structures. Optimization is complex due to the anatomical precision required.
Table 1: Optimized DBS Parameters from Clinical Studies
| Target / Condition | Amplitude | Frequency | Pulse Width | Duty Cycle | Key Outcome | Source |
|---|---|---|---|---|---|---|
| Anterior Thalamic Nuclei (Epilepsy) | - | 145 Hz (iHFS) vs 7 Hz (cLFS) | 90 μs (iHFS) vs 200 μs (cLFS) | 1 min on/5 min off (iHFS) vs Continuous (cLFS) | cLFS showed superior seizure reduction (73%) vs iHFS (33%) | [73] |
| Femoral Nerve (SCI) | - | - | - | - | Selective stimulation achieved knee moments of 11.6-43.2 Nm with <10% overlap between contacts | [74] |
| Addiction (OUD/StUD) | Target-dependent | Target-dependent | Target-dependent | Typically continuous | 27% abstinence rate across studies; nearly 50% showed significant use reduction | [72] |
Experimental Protocol for Multi-Contact DBS Optimization: A method for optimizing selective stimulation with multi-contact electrodes involves a systematic characterization of recruitment and overlap [74].
- Recruitment Characterization: For each contact, the twitch response to single stimulus pulses is measured across a range of amplitudes.
- Overlap Quantification: For pairs of contacts, the combined response is measured and compared to the linear addition of their individual responses. The deviation indicates functional overlap.
- Model Fitting: Mathematical models are fit to the recruitment and overlap data.
- Cost Function Optimization: A cost function is defined to maximize recruitment and minimize overlap across all contacts. Automated algorithms can then determine the stimulus parameters that minimize this cost function, enabling strong, selective muscle contractions or neural activation.
Vagus Nerve Stimulation (VNS)
The NOR-Current study, a large registry-based analysis, provides high-level evidence for VNS parameter optimization in epilepsy, with findings likely generalizable to other indications [75].
Table 2: Optimal VNS Parameters from the NOR-Current Study (n=415)
| Parameter | Recommended Setting | Clinical Effect | Notes |
|---|---|---|---|
| Output Current | 1.5 - 2.25 mA | Strongest predictor of seizure reduction; probability of ≥75% reduction more than doubled with 1 mA increase, peaking at 2.70 mA. | Primary focus of titration; should be increased as tolerated. |
| Frequency | 20 Hz | Standard frequency associated with the best effect. | - |
| Pulse Width | 250 μs | Standard pulse width associated with the best effect. | - |
| Duty Cycle | Standard cycle | Changes were not significantly associated with outcome. | May benefit patients unresponsive to current adjustment. |
| Therapy Duration | Long-term (Median 79 mos) | Effectiveness improved over time (p < 0.001). | Highlights role of long-term neuroplasticity. |
Non-Invasive Techniques (rTMS & tDCS)
Non-invasive neuromodulation is increasingly investigated for addiction, targeting circuits like the dorsolateral prefrontal cortex (DLPFC).
Table 3: Parameters for Non-Invasive Neuromodulation in Addiction
| Technique | Key Parameters | Evidence in Addiction | Considerations | |
|---|---|---|---|---|
| rTMS | Frequency: High-frequency (e.g., 10 Hz) to left DLPFC.Pattern: Theta-burst stimulation (intermittent).Dosage: Repeated, multi-session protocols. | Positive outcomes for tobacco, stimulant, and opioid use disorders in reducing craving. Multi-session protocols are significantly more effective than single-sessions. | FDA-cleared for smoking cessation. Accelerated paradigms (full course in 5 days) are under investigation to improve retention. | [51] [72] |
| tDCS | Electrode Placement: Anode/cathode over prefrontal regions.Session Duration: >10-15 minutes.Treatment Course: Multiple days. | Modest but meaningful improvements in craving for tobacco, alcohol, stimulant, and opioid use disorders. Evidence is less consistent than for rTMS. | Effects are less focal than rTMS. Optimal parameters and standardization of protocols are still needed. | [51] |
Experimental Protocol for rTMS in Addiction:
- Screening: Participants are typically veterans or adults with a specific SUD (e.g., tobacco, stimulant), often with comorbid PTSD [38].
- Baseline Assessment: Includes MRI scan for neuronavigation, clinical assessment of craving, and quantification of substance use.
- Randomization & Blinding: Two-arm, parallel design comparing active versus "sham" rTMS.
- Stimulation Protocol: Active rTMS involves applying high-frequency (e.g., 10 Hz) or theta-burst stimuli to the left DLPFC using a figure-of-eight or H-coil. The sham procedure mimics the sensation without delivering effective stimulation.
- Adjunctive Therapy: Participants concurrently undergo Cognitive Behavioral Therapy (CBT) for smoking cessation and may receive nicotine replacement therapy.
- Outcome Measures: Primary outcomes include feasibility, acceptability, reduction in cue-induced craving, and biological measures of substance use (e.g., urine toxicology). Post-treatment MRI assesses neural target engagement.
Advanced Computational and Workflow Approaches
Time-Adaptive Bayesian Optimization
A significant limitation of static parameter sets is their inability to account for physiological fluctuations (e.g., circadian rhythms, medication cycles, disease progression). Time-Varying Bayesian Optimization (TV-BayesOpt) is a novel computational framework designed to address this [76].
- Concept: TV-BayesOpt treats the relationship between stimulation parameters and clinical outcome as a time-varying function. It incorporates "forgetting" mechanisms (for gradual drift) and periodic covariance functions (for rhythmic variations) to continuously adapt parameters.
- Application: In silico models of movement disorders have demonstrated TV-BayesOpt's superiority over time-invariant methods for tracking gradual and periodic changes in optimal settings. This approach can be leveraged to adjust amplitude, pulse width, frequency, and phase for both invasive and non-invasive neuromodulation.
The following diagram illustrates the core workflow of this adaptive optimization process.
Data Management for FAIR Parameter Optimization
Robust optimization relies on high-quality, well-annotated data. The FAIR Data Principles (Findable, Accessible, Interoperable, Reusable) provide a framework for managing experimental data tables generated during parameter optimization [77].
- The ODAM Approach: This approach involves structuring data in spreadsheets from the point of acquisition, using a data dictionary-like format with clear column definitions and links to community ontologies.
- Benefits: This upstream structuring facilitates easy data merging and analysis, saves time, and ensures that data is FAIR-compliant by design, ready for deposition in public repositories to support meta-analyses and machine learning.
Table 4: Key Resources for Neuromodulation Research
| Category | Item / Resource | Function / Application | |
|---|---|---|---|
| Computational Tools | Time-Varying Bayesian Optimization (TV-BayesOpt) Algorithm | Tracks optimal stimulation parameters across gradual and periodic physiological changes. | [76] |
| ODAM (Open Data for Access and Mining) | Software and protocol for preparing FAIR-compliant experimental data tables to improve data management and analysis. | [77] | |
| Experimental Materials | Multi-Contact Cuff/Depth Electrodes | Enables selective stimulation of different neural populations within a nerve or brain region. | [73] [74] |
| Sham/Placebo Coils & Electrodes | Critical for conducting double-blinded, controlled trials of neuromodulation therapies. | [38] [72] | |
| Data Resources | WIKISTIM.org | A searchable database of clinical studies that employ neuromodulation methodologies. | [38] |
| FDA-approved rTMS Systems (e.g., BrainsWay) | Platform for conducting clinical trials of rTMS for addiction (e.g., smoking cessation). | [72] |
Optimizing stimulation parameters is a dynamic and multifaceted process central to the success of neuromodulation therapies. As evidenced by clinical and computational studies, moving beyond fixed, empirical settings toward personalized, adaptive, and data-driven approaches is critical. This is particularly true in addiction, where the underlying neuroplasticity necessitates interventions that can guide and reinforce recovery-oriented circuit changes. Future directions will involve:
- Larger-Scale Trials: Conducting larger, randomized controlled trials for conditions like OUD and StUD to establish definitive efficacy and optimal parameters [51] [72].
- Closed-Loop Systems: Integrating biomarkers of craving or relapse risk with adaptive algorithms like TV-BayesOpt to create "closed-loop" neuromodulation systems that respond in real-time to a patient's state [76].
- Standardization and FAIR Data: Widespread adoption of standardized protocols and FAIR data principles to accelerate collective knowledge and the development of predictive models for parameter selection [77].
The following diagram summarizes the integrated view of how neuromodulation interacts with the addiction cycle and neuroplasticity to promote recovery, highlighting the critical role of parameter optimization.
The Role of Abstinence and 30-Day Resets in Re-establishing Homeostasis
The brain's reward system, a conserved evolutionary survival mechanism, becomes profoundly dysregulated in substance use disorders. This whitepaper examines the therapeutic potential of targeted abstinence periods, specifically the 30-day reset, as an intervention to counteract addiction-driven neuroplasticity and re-establish homeostasis in the mesolimbic dopamine pathway. We synthesize clinical observations and preclinical data to present a mechanistic model explaining how sustained abstinence facilitates the normalization of dopamine signaling, rectifies glutamatergic imbalances, and initiates structural neural reorganization. The protocol is framed within the broader context of addiction as a learned behavior stemming from maladaptive neuroplasticity, offering a non-pharmacological strategy to recalibrate core reward circuitry for researchers and drug development professionals.
Addiction is fundamentally a disease of neuroplasticity, characterized by experience-dependent learning that results in compulsive drug use despite negative consequences [26]. The central nervous system changes underlying this conditioned behavior are stable and potentially permanent, establishing a chronic illness with a high propensity for relapse [26]. The brain disease model of addiction posits that repeated drug exposure triggers structural and functional adaptations within key neural circuits governing reward, motivation, and executive control [14].
Neuroplasticity, the brain's ability to change its functional and structural organization in response to experience, is the fundamental process underpinning both the development of and recovery from addiction [78]. While this plasticity enables learning and adaptation, it becomes maladaptive in the context of addiction. Drugs of abuse co-opt evolutionary conserved reward pathways, inducing neuroplastic changes that strengthen synaptic connections reinforcing drug-seeking behavior while weakening those for natural rewards [79] [8]. This whitepaper examines the hypothesis that a defined period of complete abstinence—a "30-day reset"—can leverage the brain's inherent plasticity to reverse these maladaptive changes and restore homeostatic function to the reward system.
Neurobiological Mechanisms of Addiction
Dopaminergic Dysregulation in the Reward Pathway
All drugs of abuse directly or indirectly activate the mesolimbic dopamine pathway, which projects from the ventral tegmental area (VTA) to the nucleus accumbens (NAc) [8]. This pathway, central to processing natural rewards like food and social interaction, responds to addictive substances with a dopamine surge that is faster, more intense, and longer-lasting than that produced by natural stimuli [79] [8].
Repeated drug exposure induces compensatory neuroadaptation. The brain downregulates its own dopamine production and reduces dopamine receptor density (particularly D2 receptors) in the striatum to counter the chronic overstimulation [79] [80]. This leads to a dopamine deficit state, where the individual experiences diminished pleasure from natural rewards (anhedonia) and requires the drug merely to feel normal [81] [8]. These changes are quantified in neuroimaging studies, which show that individuals with cocaine use disorder exhibit dopamine increases in response to stimulants that are approximately 50% lower than those without addiction [80].
The Three-Stage Cycle and Glutamatergic Dysregulation
Addiction perpetuates through a recurrent three-stage cycle, each with distinct neurobiological underpinnings [80] [8]:
- Binge/Intoxication: Characterized by supraphysiological dopamine release in the NAc, reinforcing drug-taking behavior.
- Withdrawal/Negative Affect: Driven by recruitment of the brain's stress systems (e.g., corticotropin-releasing factor in the extended amygdala) and compromised reward system function, leading to negative emotional states.
- Preoccupation/Anticipation: Involves dysregulation of the prefrontal cortex (PFC) and glutamatergic pathways, resulting in craving and impaired impulse control.
The preoccupation/anticipation stage is critical for relapse. Chronic drug use disrupts glutamate homeostasis in the NAc, reducing basal extracellular glutamate levels through impaired cystine-glutamate exchange and glutamate uptake [26]. This creates a state where drug-associated cues can trigger a potentiated release of synaptic glutamate, driving compulsive drug-seeking [26]. Concurrently, PFC dysfunction—including reduced activity in the orbitofrontal cortex (OFC), anterior cingulate cortex (ACC), and dorsolateral prefrontal cortex (DLPFC)—impairs executive control, decision-making, and inhibitory regulation [80].
Table 1: Key Neuroadaptations in Addiction
| Neural System | Acute Drug Effect | Chronic Adaptation |
|---|---|---|
| Dopamine (VTA-NAc) | Supraphysiological release; intense pleasure/reward | Blunted response; reduced D2 receptors; dopamine deficit state |
| Glutamate (PFC-NAc) | Contributes to synaptic plasticity and learning | Disrupted homeostasis; potentiated cue-induced release |
| Prefrontal Cortex | Acute modulation of activity | Generalized hypoactivity; impaired executive function and impulse control |
The 30-Day Reset: Mechanism and Protocol
Theoretical Foundation and Definition
The 30-day reset is a clinical protocol grounded in the principle of leveraging neuroplasticity to reverse addiction-related neuroadaptations. Proposed by addiction expert Dr. Anna Lembke, it involves a period of complete abstinence from the addictive substance or behavior [81] [79]. The underlying hypothesis is that this sustained period without dopamine hyperstimulation allows the brain's reward system to gradually restore its homeostatic balance, including natural dopamine production and receptor sensitivity [81] [8].
The 30-day timeframe is based on clinical observation that this duration is typically sufficient for individuals to pass through the acute withdrawal phase and begin experiencing early signs of neurological recalibration, though the complete restoration of glutamate homeostasis and reversal of structural plasticity may require longer periods [26] [79].
Mechanistic Basis for Homeostatic Restoration
The reset protocol facilitates recovery through several interconnected mechanisms:
- Dopamine System Recovery: Abstinence removes the artificial dopamine surges, allowing the brain to gradually upregulate natural dopamine synthesis and restore the density and sensitivity of dopamine receptors [79] [8]. This process reverses the dopamine deficit state, enabling natural rewards to regain their salience.
- Restoration of Glutamate Homeostasis: Preclinical models suggest that prolonged abstinence is necessary for restoring cystine-glutamate exchange and glutamate transporter function in the NAc [26]. Interventions like N-acetylcysteine (which promotes cystine-glutamate exchange) have shown promise in reducing craving and drug-seeking in human trials, supporting the role of glutamate homeostasis in recovery [26].
- Structural Neuroplasticity: Chronic drug use alters dendritic spine density and morphology on neurons in the NAc and PFC. Persisting synaptic changes underscore the necessity of a sustained intervention like the 30-day reset to initiate and support the structural rewiring necessary for stable recovery [26].
Diagram 1: The 30-Day Reset Re-establishes Homeostasis
Experimental Evidence and Research Methodologies
Preclinical Models of Abstinence
Animal models, particularly rodent self-administration studies, provide direct evidence for abstinence-induced neuroplasticity. In a classic reinstatement model, animals are trained to self-administer a drug (e.g., intravenous cocaine) paired with a conditioned stimulus (CS), such as a light. After the behavior is extinguished, the ability of the CS to reinstate drug-seeking (a model of "relapse") is tested after varying periods of forced abstinence [26].
Key Finding: The propensity to relapse intensifies over the first month of abstinence, a phenomenon termed "incubation." Reinstatement is significantly greater at 4 weeks compared to 1 week, associated with increased levels of brain-derived neurotrophic factor (BDNF) in the VTA and NAc [26]. This suggests that early abstinence is a dynamic period of active neural restructuring.
Table 2: Quantifiable Outcomes in Preclinical Abstinence Studies
| Measurement | Technique | Finding During Abstinence | Functional Implication |
|---|---|---|---|
| Relapse Susceptibility | Reinstatement Test (e.g., lever presses) | Increases up to 6 months ("incubation") [26] | Measures strength of cue-induced craving |
| BDNF Expression | Immunohistochemistry, ELISA | Increases in VTA & NAc over first month [26] | Promotes synaptic plasticity & remodeling |
| Dendritic Spine Density | Golgi Staining, 2-Photon Microscopy | Increased in NAc after cocaine; decreased in VTA after morphine [26] | Correlates with persistent behavioral sensitization |
| Extracellular Signal-Related Kinase (ERK) | Western Blot | Increased in central amygdala after 30 days [26] | Involved in cue-induced memory reconsolidation |
Human Studies and Clinical Protocols
Human research, while more complex, corroborates preclinical findings. Brain imaging studies show that individuals with addiction who have been abstinent for at least a month still exhibit rapid limbic activation upon exposure to drug-related cues, correlating with self-reported craving [26]. This highlights the persistence of conditioned neural responses and the challenge of recovery.
The 30-day reset protocol in a clinical setting involves:
- Initiation: Complete cessation of the substance/behavior. Medical supervision is critical for substances where withdrawal can be life-threatening (e.g., alcohol, benzodiazepines) [68].
- Withdrawal Management (Days 1-7): Peak physical withdrawal symptoms occur, often requiring pharmacological support (e.g., MAT for opioids) to ensure safety and retention [68].
- Protracted Abstinence (Weeks 2-4): Acute physical symptoms subside, but cravings, anhedonia, and emotional dysregulation may persist as the brain adjusts to the absence of the drug. Behavioral strategies like CBT are crucial [81] [8].
- Assessment and Transition: At day 30, patients can make an informed decision about future engagement with the substance, based on their experience of the reset [81].
Diagram 2: Experimental vs. Clinical Abstinence Models
The Scientist's Toolkit: Key Reagents and Modalities
Table 3: Essential Research Reagents and Modalities for Abstinence Research
| Reagent / Modality | Category | Primary Function in Research |
|---|---|---|
| N-acetylcysteine (NAC) | Pharmacological Probe | Restores cystine-glutamate exchange in NAc; reduces drug-seeking in reinstatement models [26]. |
| BDNF Assays | Biochemical Assay | Quantifies levels of this key growth factor to correlate with incubation of craving and synaptic plasticity [26]. |
| Raclopride ([¹¹C]-labeled) | Radioligand for PET | Binds to D2/D3 dopamine receptors; used in human PET studies to measure dopamine release and receptor availability [26]. |
| Deep Brain Stimulation (DBS) | Neuromodulation | Applies high-frequency stimulation to targets like NAc; probes circuit function and may restore glutamate homeostasis [80]. |
| Cognitive Behavioral Therapy (CBT) | Behavioral Intervention | A learning-based therapy that utilizes neuroplasticity to modify maladaptive habits and thought patterns [14] [78]. |
The 30-day reset represents a strategic application of neuroplasticity principles to counteract the profound dysregulation of the brain's reward system in addiction. The protocol targets core mechanisms—dopaminergic dysregulation, glutamatergic imbalance, and PFC dysfunction—initiating a process of homeostatic restoration that is both measurable and behaviorally relevant.
Future research should focus on personalizing abstinence-based interventions. Key areas include identifying genetic (e.g., polymorphisms in dopamine receptor genes) and neuroimaging biomarkers that predict individual variability in response to abstinence. Furthermore, exploring synergies between enforced abstinence and emerging neuromodulation techniques like Deep Brain Stimulation (DBS) or pharmacological adjuncts like N-acetylcysteine holds promise for enhancing and accelerating the recovery of homeostatic function in treatment-resistant cases [26] [80]. For the drug development community, the 30-day reset provides a clean experimental model and a clinically relevant timeframe for testing novel therapeutic agents aimed at facilitating neurobiological recovery.
Addiction is increasingly recognized as a chronic brain disorder characterized by profound changes in neural circuitry, yet also defined by a remarkable capacity for recovery driven by neuroplasticity. The integrated treatment of substance use disorders (SUDs) represents a paradigm shift from isolated interventions to a comprehensive, whole-person approach that synergistically combines pharmacotherapy, behavioral interventions, and psychosocial support systems. This approach is fundamentally grounded in the understanding of neuroplasticity—the brain's ability to reorganize itself by forming new neural connections throughout life. The development of addiction hijacks the brain's natural reward and learning systems, creating maladaptive pathways that strengthen compulsive drug-seeking behaviors [5]. Conversely, recovery harnesses this very same neuroplastic potential to weaken these associations and build healthier cognitive and behavioral patterns. As described by the National Institute on Drug Abuse (NIDA), "the very same adaptability and neuroplasticity of the brain that makes it susceptible to developing addiction in the first place also enables it to heal, especially when internal and external conditions are supportive of recovery" [5]. Integrated treatment creates these supportive conditions by addressing the biological, psychological, and social dimensions of addiction simultaneously, thereby facilitating the neural rewiring essential for sustained recovery.
Core Components of Integrated Treatment
Pharmacological Interventions
Medications for addiction treatment work by normalizing brain chemistry, blocking the euphoric effects of drugs, and relieving intense cravings, thereby creating a stable neurobiological foundation upon which behavioral and social interventions can build. Medications are a cornerstone of treatment for opioid use disorder (OUD), including methadone, buprenorphine, and naltrexone [82]. These medications help stabilize individuals by acting on the same opioid receptors in the brain targeted by illicit drugs, but in a controlled and safe manner. For alcohol and other substance use disorders, various medications can help reduce symptoms of withdrawal and prevent relapse. The integration of medication with psychosocial supports is a defining characteristic of Medication-Assisted Treatment (MAT), which recognizes that "pharmacological treatments for OUD are most effective when combined with psychosocial supports" [82]. These medications essentially dampen the "fire" of active addiction, allowing the brain's neuroplasticity mechanisms to begin the process of recovery and rewiring.
Behavioral and Psychotherapeutic Interventions
Behavioral therapies directly target the maladaptive learning patterns and cognitive distortions that underlie addiction, leveraging principles of learning and neuroplasticity to establish new, healthier neural pathways. These evidence-based interventions are essential for helping individuals modify their attitudes and behaviors related to substance use, develop healthier life skills, and persist with other forms of treatment.
Core Psychotherapy Approaches in Integrated Treatment:
- Cognitive-Behavioral Therapy (CBT): Helps patients recognize, avoid, and cope with situations in which they are most likely to use substances by restructuring dysfunctional thought patterns and reinforcing positive behaviors [83] [82].
- Motivational Enhancement Therapy (MET): A patient-centered counseling approach that harnesses internal motivation for change rather than imposing it externally, effectively preparing individuals for more intensive treatment [83] [82].
- Contingency Management: Uses positive reinforcement to provide tangible rewards for maintaining sobriety, leveraging the brain's reward system to strengthen abstinent behaviors [82].
- Relapse Prevention: A specific form of CBT that teaches individuals to identify and navigate high-risk situations for use, developing proactive coping strategies to maintain long-term recovery [83].
These behavioral interventions work by actively engaging the brain's prefrontal cortical regions—responsible for executive function, decision-making, and impulse control—which are often compromised in addiction. Through repeated practice and skill-building, these therapies promote neural rewiring that strengthens top-down cognitive control over the reward system [5].
Psychosocial Supports and Recovery Services
Psychosocial supports encompass the formal and informal counseling, peer support, and community-based services that address the social and environmental determinants of recovery. These services are critical for creating the "external conditions" that support neural rewiring by fostering meaningful connections and building recovery capital. As one neuroscientist in recovery powerfully stated, "The opposite of addiction is connection" [84]. This connection becomes "literally chemical" as "positive social interaction floods the brain with chemicals like oxytocin and dopamine, which aren't just feel-good modulators in the brain; they're molecular glue that helps form new neural links" [84].
Key psychosocial supports include:
- Peer Recovery Support: Services provided by individuals with lived experience of addiction who offer guidance, mentorship, and practical support based on their own recovery journeys [5] [82].
- Mutual Help Groups: Traditional 12-step programs (e.g., AA, NA) and alternative models (e.g., SMART Recovery, Recovery Elevator Café RE) that provide community and structured support [5] [84].
- Recovery Housing and Community Centers: Sober living environments that remove triggers and provide stability while reinforcing recovery-oriented behaviors [5].
- Case Management and Wrap-around Services: Assistance with practical needs such as housing, employment, childcare, and transportation that remove barriers to treatment engagement and promote life stabilization [82].
These psychosocial elements create an environment where the brain can heal by reducing stress, providing alternative rewards, and fostering the social bonds that are fundamental to human well-being. NIDA has made significant research investments in understanding these recovery support services, recognizing their potential impact in helping people maintain remission from SUDs [5].
Quantitative Evidence and Outcomes
The efficacy of integrated treatment approaches is supported by a growing body of clinical evidence and neurobiological research. The tables below summarize key quantitative findings from treatment studies and neuroimaging research that demonstrate the effectiveness of combined interventions and their neural correlates.
Table 1: Clinical Outcomes Associated with Integrated Treatment Components
| Treatment Component | Measured Outcome | Impact/Effect Size | Assessment Method |
|---|---|---|---|
| Pharmacotherapy (MAT) | Treatment retention | Significantly higher retention rates compared to placebo or no medication | Randomized controlled trials [82] |
| Cognitive-Behavioral Therapy | Reduced drug use days | Moderate to large effects in reducing frequency of use | Self-report, urine toxicology [83] [85] |
| Contingency Management | Continuous abstinence | Doubles rates of sustained abstinence compared to treatment as usual | Objective verification (e.g., urine tests) [82] |
| Peer Recovery Support | Engagement in care | Increased connection to clinical services and social supports | Service utilization records [5] [82] |
| Integrated Treatment (Overall) | Psychiatric hospitalization | Reduced rates of psychiatric relapses and ER utilization | Health services research [83] |
Table 2: Neurobiological Recovery Trajectories Documented via Neuroimaging
| Neural System | Observed Change with Sustained Recovery | Timeframe for Significant Recovery | Imaging Modality |
|---|---|---|---|
| Prefrontal Cortex | Structural and functional recovery in regulatory regions | Observable changes within months of treatment; continues to improve | MRI, fMRI [5] |
| Striatal Dopamine System | Recovery of dopamine transporters (e.g., in methamphetamine use disorder) | Documented with protracted abstinence | PET imaging [5] |
| Hippocampus | Structural recovery potentially linked to improved memory function | Longitudinal studies show improvement over years | Structural MRI [5] |
| Global White Matter | Improved integrity of connective pathways | Can track with behavioral improvements over 12+ months | Diffusion Tensor Imaging [5] |
| Functional Connectivity | Restored communication between cognitive control and reward networks | Dynamic changes observable early in treatment | Resting-state fMRI [5] |
Assessment methodologies in treatment research have evolved to include both objective and self-report measures. While self-reported drug use provides valuable context, quantitative and qualitative urinalysis often reveals higher rates of drug use, highlighting the importance of multimodal assessment in treatment studies [85]. Longitudinal neuroimaging studies show that "structural and functional brain recovery" occurs across multiple regions including the "frontal cortical regions, insula, hippocampus, and cerebellum" [5]. This neural recovery parallels clinical improvements, with research indicating it can take "as much as 8 years and 4-5 engagements in treatment or mutual support groups to achieve sustained remission" [5], underscoring the chronic nature of addiction and the need for prolonged support.
Experimental Protocols and Methodologies
Protocol for Assessing Integrated Treatment Efficacy
Objective: To evaluate the synergistic effects of combined pharmacotherapy, behavioral intervention, and peer support on clinical outcomes and neural recovery markers in participants with opioid use disorder.
Population: Adults (n=120) meeting DSM-5 criteria for moderate-to-severe OUD, stratified by duration of illness and presence of co-occurring mental health conditions.
Study Design: Randomized, controlled trial with 2x2 factorial design comparing: (1) Medication only (buprenorphine/naloxone), (2) Medication + CBT, (3) Medication + peer recovery support, (4) Full integrated treatment (all components).
Intervention Specifications:
- Pharmacotherapy: Buprenorphine/naloxone initiated following FDA guidelines, with flexible dosing based on clinical response [82].
- Cognitive-Behavioral Therapy: 16-week manualized protocol delivered in individual sessions twice weekly, focusing on coping skills, craving management, and cognitive restructuring [83] [82].
- Peer Recovery Support: Weekly sessions with certified peer specialists focusing on recovery goals, community integration, and mentorship [5] [82].
Assessment Schedule:
- Baseline: Comprehensive clinical interview, urine toxicology, self-report measures (Addiction Severity Index, Brief Symptom Inventory), neurocognitive testing, structural and functional MRI.
- Monthly: Urine drug screens, self-reported substance use, treatment retention, medication adherence.
- Quarterly: Comprehensive clinical and functional assessment, neurocognitive testing.
- Endpoint (12 months): Repeat of all baseline assessments plus recovery capital measure.
Primary Outcomes: Percentage of opioid-negative urine tests over 12-month period; retention in treatment at 3, 6, and 12 months; changes in brain structure/function in prefrontal-striatal circuitry.
Data Integration: Mixed-effects models will test main effects and interactions of treatment components, with mediation analyses examining whether neural changes explain clinical improvements.
Neuroimaging Protocol for Tracking Neuroplastic Change
Objective: To quantify neuroplastic changes associated with recovery using longitudinal multimodal neuroimaging.
Imaging Modalities:
- Structural MRI: T1-weighted scans for cortical thickness and volume analysis.
- Diffusion Tensor Imaging (DTI): For white matter integrity assessment (fractional anisotropy).
- Functional MRI (fMRI): Task-based (monetary incentive delay, emotional regulation) and resting-state for functional connectivity.
Scanning Schedule: Baseline (pre-treatment), 3 months, 12 months.
Preprocessing Pipeline:
- Structural: Cortical reconstruction and volumetric segmentation using Freesurfer; voxel-based morphometry.
- DTI: Eddy current correction, tensor fitting, tract-based spatial statistics.
- fMRI: Slice-time correction, motion correction, spatial normalization, smoothing.
Analysis Plan:
- Structural: Longitudinal analysis of cortical thickness changes using mixed-effects models.
- DTI: Within-subject change in fractional anisotropy along major white matter tracts.
- fMRI: Seed-based connectivity analysis focusing on prefrontal-striatal circuits; activation during reward processing tasks.
This protocol allows researchers to track how "the learning process reshapes synaptic connectivity across a range of circuits, ultimately outcompeting drug-related memories and automatic behavioral patterns, which weaken over time" [5].
Research Reagent Solutions and Methodological Tools
Table 3: Essential Research Materials and Analytical Tools for Addiction Recovery Research
| Reagent/Tool | Specifications | Research Application | Key Function |
|---|---|---|---|
| Urinalysis (Quantitative) | Mass spectrometry detection of drug metabolites (e.g., benzoylecgonine for cocaine) | Objective verification of self-reported abstinence; pattern analysis [85] | Provides quantitative data on recent substance use with high specificity and sensitivity |
| Structural MRI Atlas | Standardized brain templates (e.g., MNI space) for volumetric analysis | Tracking gray matter changes in prefrontal cortex, hippocampus, and striatum during recovery [5] | Enables voxel-based morphometry to detect subtle structural plasticity over time |
| Resting-state fMRI Preprocessing Suite | Software packages (e.g., FSL, AFNI, CONN) for motion correction and denoising | Mapping functional connectivity changes in default mode and executive control networks [5] | Quantifies reorganization of large-scale brain networks with recovery |
| Cognitive Battery | Standardized tests (e.g., Trail Making, Stroop, N-back) | Assessing recovery of executive function, working memory, and cognitive control [5] | Links behavioral improvements in cognitive function to neural recovery |
| Plasticity Rule Modeling | Meta-learning algorithms (e.g., genetic programming/CGP) | Discovering how neural circuits self-organize and maintain function despite perturbation [86] [87] | Models how learning rules shape circuit dynamics relevant to recovery processes |
Visualizing the Integrated Treatment Model and Neural Pathways
The following diagrams illustrate the conceptual framework of integrated treatment and its proposed effects on neural systems, created using DOT language and compliant with the specified color and contrast requirements.
Integrated Treatment Conceptual Model
Neuroplasticity in Addiction Recovery
Integrated treatment represents a transformative approach to addiction that aligns with our current understanding of addiction as a chronic brain disorder with profound neuroplastic underpinnings. By simultaneously addressing the biological, psychological, and social dimensions of the illness, this approach creates the necessary conditions for neural rewiring and sustainable recovery. The evidence strongly supports the efficacy of combining medications that normalize brain function, behavioral therapies that reshape maladaptive thought and behavior patterns, and psychosocial supports that provide the connection and community essential for long-term healing.
Future research should focus on several critical areas: optimizing the timing and sequencing of treatment components across different stages of recovery; developing personalized approaches based on individual neurobiological and psychosocial profiles; understanding the optimal duration of various recovery supports; and exploring how to effectively integrate emerging technologies like digital peer-support platforms [5]. Additionally, more research is needed to elucidate the specific neural mechanisms through which psychosocial supports influence brain recovery, potentially through oxytocin-mediated social reward pathways or stress-regulation mechanisms [84]. As the field advances, the integration of meta-learning approaches to understand neural plasticity rules [86] [87] with clinical intervention research promises to yield more targeted and effective strategies for harnessing the brain's innate capacity for change in the service of recovery.
Validation and Comparison: Biomarkers, Models, and Intervention Efficacy
Visually Evoked Potentials (VEPs) recorded via electroencephalography (EEG) represent a promising non-invasive method for assessing neuroplasticity in the human visual cortex. These potentials are electrical responses generated in the visual cortex in response to visual stimuli and have been demonstrated to exhibit stimulus-selective response plasticity (SRP) that shares key properties with canonical long-term potentiation (LTP) mechanisms [88]. The VEP paradigm displays several Hebbian properties including N-methyl-D-aspartate receptor (NMDAR) dependency, input specificity, and persistence, providing compelling evidence that SRP-induced VEP changes can serve as indices of LTP-like plasticity in the human primary visual cortex [88]. As disturbances in neuroplasticity are associated with numerous psychiatric and neurological disorders, including addiction, the development of optimized VEP paradigms offers strong translational potential for assessing neuroplasticity deficits and developing new biomarkers and therapeutic strategies [88].
The application of VEP-based biomarkers extends particularly to addiction research, where substance use disorders are characterized by profound alterations in brain reward circuits and plasticity mechanisms. The brain's reward pathways, conserved over millions of years of evolution, can be hijacked by addictive substances and behaviors that produce exaggerated dopamine surges, leading to subsequent compensatory reductions in dopamine receptors and diminished sensitivity to natural rewards [2]. Understanding these plasticity changes through non-invasive assays like VEPs provides crucial insights into the mechanisms underlying addiction and recovery processes.
Methodological Foundations of VEP-Based Plasticity Assessment
Core Experimental Protocol
The standard protocol for assessing plasticity through VEPs involves a sequential design consisting of baseline measurements, a modulation phase, and post-modulation assessments [88]. In a typical experimental setup, participants are seated at a controlled distance from a visual display system. A checkerboard reversal stimulus with individual checkers subtending a visual angle of 0.5° is commonly used to evoke VEPs, with the pattern inverting at a temporal frequency of two reversals per second (rps) [88]. The baseline VEP recording involves presenting this checkerboard reversal stimulus for 20 seconds, generating approximately 40 sweeps per block.
Following baseline recording, participants undergo a modulation phase involving intense sensory stimulation designed to induce plastic changes. This phase varies significantly depending on the specific protocol employed, with different stimulation patterns producing distinct plasticity outcomes. The duration and frequency of this modulation phase serve as critical determinants of the resulting plastic effects [88].
Post-modulation assessment involves recording VEPs at multiple time points following the modulation phase to track the persistence of plastic changes. Typical experimental designs include measurements at 2, 8, 12, 18, 22, and 28 minutes after modulation [88]. Throughout the recording session, participants are instructed to maintain fixation on a central cross and perform an attention-monitoring task, such as reading numbers that appear randomly within the cross, to ensure consistent attention levels [88].
Research Reagent and Equipment Solutions
Table 1: Essential Research Materials and Equipment for VEP Plasticity Studies
| Item Category | Specific Examples | Function/Application |
|---|---|---|
| Visual Stimulation System | 55" OLED screen (120 Hz refresh rate) [88] | Presents precise visual stimuli (checkerboard reversals) |
| Stimulus Generation Software | Expyriment (Python) [88] | Programs and controls visual stimulus parameters and timing |
| EEG Recording System | High-density EEG systems [89] | Records electrical activity from the visual cortex |
| Recording Electrodes | 1 cm steel needle electrodes [90] | Captures cortical potentials at specific scalp locations |
| Experimental Control | Central fixation cross with number reading task [88] | Maintains participant attention and alertness during recordings |
VEP Plasticity Modulation Protocols and Outcomes
Comparative Analysis of Stimulation Protocols
Research has systematically compared multiple VEP modulation protocols to identify optimal parameters for inducing short- and long-term synaptic plasticity. Each protocol produces distinct temporal patterns of plasticity induction and maintenance [88]:
Low-frequency stimulation (2 Hz): This protocol involves a single 10-minute block at a reversal frequency of 2 rps, producing 1200 stimuli. It generates transient changes in plasticity that peak at 2 minutes post-modulation but dissipate within 12 minutes [88].
Repeated low-frequency stimulation: This enhanced protocol consists of three 10-minute blocks at a reversal frequency of 2 rps. It induces more sustained plastic changes that persist for up to 22 minutes, potentially by overcoming ceiling effects through repeated stimulation [88].
High-frequency stimulation (~9 Hz): Utilizing short (2-minute), high-frequency tetanic modulation, this protocol induces sharp but brief increases in plasticity indices. The effects are pronounced but short-lived compared to other protocols [88].
Theta-pulse stimulation: This approach uses pulsed application of synaptic stimulation at theta frequency, resulting in moderate but prolonged changes in plasticity that can last up to 28 minutes post-modulation. Theta bursts mimic naturally occurring firing patterns in the brain and provide optimal calcium dynamics and synaptic recovery during intervals [88].
Table 2: Quantitative Comparison of VEP Plasticity Modulation Protocols
| Protocol Type | Stimulation Parameters | Plasticity Peak | Duration of Effects | Key Characteristics |
|---|---|---|---|---|
| Low-Frequency | 10 min at 2 rps (1200 stimuli) [88] | 2 min post-modulation [88] | <12 min [88] | Transient changes, simple protocol |
| Repeated Low-Frequency | 3×10 min at 2 rps (3600 stimuli) [88] | Sustained elevation [88] | Up to 22 min [88] | Overcomes ceiling effect, sustained |
| High-Frequency | 2 min at ~9 Hz [88] | Sharp initial peak [88] | Brief [88] | Tetanic stimulation, brief potentiation |
| Theta-Pulse | Theta-frequency pattern [88] | Moderate elevation [88] | Up to 28 min [88] | Prolonged effects, natural patterning |
Signaling Pathways in Visual Cortical Plasticity
The plasticity measured through VEP modulation protocols involves complex signaling pathways that bridge sensory processing and addiction mechanisms. The following diagram illustrates key pathway interactions:
Pathway Diagram Title: VEP Plasticity to Reward Pathway Signaling
This diagram illustrates how visual stimulation initiates a cascade of neurochemical events leading to synaptic plasticity, which intersects with reward pathways relevant to addiction. The process begins with visual stimuli generating VEP responses, followed by NMDA receptor activation and glutamatergic signaling [88]. This triggers BDNF-trKB signaling and subsequent mTOR pathway activation, ultimately promoting synaptogenesis and cortical LTP-like plasticity [12]. These plasticity changes in the visual cortex can influence and be influenced by reward pathway modulation and dopamine release, creating a bridge between sensory plasticity and addiction mechanisms [2].
VEP Biomarkers in Disease States and Therapeutic Development
Plasticity Deficits in Neuropsychiatric Disorders
VEP-based biomarkers have revealed significant impairments in neuroplasticity across various psychiatric conditions. Research has consistently demonstrated altered VEP plasticity in individuals with major depressive disorder, bipolar disorder, and schizophrenia [88]. These findings provide translational validation of results from animal models and support the crucial role of neuroplasticity deficits in psychiatric pathophysiology. Importantly, these impairments are not merely epiphenomena but appear to correlate with clinical features and treatment responses.
The relationship between VEP plasticity and addiction is particularly relevant given the shared neural substrates. Addiction involves maladaptive learning processes where the brain begins to treat substances as more important than basic needs like food, safety, or connection [2]. This learning depends on plasticity mechanisms that can be probed through VEP paradigms. The dopamine surges caused by addictive substances lead to compensatory reductions in dopamine receptors and diminished sensitivity to natural rewards, creating a cycle of compulsive use despite reduced pleasure [2].
Monitoring Therapeutic Interventions
VEP biomarkers show significant promise for tracking treatment responses in addiction and related disorders. Pharmacological interventions including selective serotonin reuptake inhibitors, ketamine, and other novel compounds have been shown to modulate VEP-based plasticity measures [88]. Additionally, non-invasive brain stimulation approaches such as transcranial direct current stimulation can enhance plasticity indices measured through VEP protocols [88].
Emerging research indicates that psychedelic-assisted therapies may exert their therapeutic effects through neuroplasticity mechanisms measurable via VEP paradigms. Serotonergic psychedelics and ketamine appear to share common cellular mechanisms, recruiting glutamatergic neurons to stimulate BDNF-trKB signaling, which promotes synaptogenesis via the mTOR pathway [12]. These plasticity-enhancing effects may underlie their therapeutic potential for conditions including depression, PTSD, and addiction [12].
Novel therapeutic targets for substance use disorders increasingly focus on neuroplasticity, neuroinflammation, and interactions between brain and peripheral systems [41]. The development of pharmacotherapies targeting these mechanisms represents a promising frontier in addiction treatment, with VEP biomarkers providing crucial objective measures of target engagement and treatment efficacy.
Experimental Design and Technical Considerations
Standardized Experimental Workflow
Implementing robust VEP plasticity assessment requires careful attention to experimental design and technical parameters. The following workflow outlines a comprehensive approach:
Workflow Diagram Title: VEP Plasticity Assessment Protocol
This workflow begins with careful participant screening and consent procedures, ensuring participants have no history of neurological, psychiatric, or ocular disorders and are not taking psychoactive medications [88]. Baseline VEP recording establishes pre-modulation values using a standardized checkerboard reversal stimulus. The critical modulation phase follows, with protocol selection based on research objectives—low-frequency for transient effects, repeated low-frequency for sustained plasticity, high-frequency for brief potentiation, or theta-pulse stimulation for prolonged effects [88]. Post-modulation assessments at specified intervals track the time course of plastic changes, with data processing focusing on predefined VEP components (C1, P1, N1) and their amplitude changes from baseline [88] [91].
Methodological Optimization and Validation
Several technical considerations are essential for obtaining reliable VEP plasticity measures:
Stimulus Parameters: Checkerboard stimuli typically use individual checkers subtending 0.5° visual angle, with reversal rates of 2 rps for baseline and post-modulation recordings [88]. Stimulus presentation software such as Expyriment in Python provides precise temporal control [88].
EEG Recording Parameters: High-density EEG systems capture optimal spatial resolution, with active electrodes placed medially along the sagittal suture to optimize proximity to the visual cortex [90]. Reference and ground electrodes are typically positioned at the nose and tail, respectively [90].
Attention Control: Participants perform a central fixation task with randomly appearing numbers to maintain consistent attention levels throughout recordings, preventing vigilance fluctuations from confounding plasticity measures [88].
Component Analysis: Early VEP components (C1, P1, N1) reflect primary visual processing and show robust LTP-like modulation independent of sex, while later components (350-426 ms) may reflect attention-related processing with subtle sex differences [91].
Validation studies have established the biological specificity of VEP measures, demonstrating that latency improvements following remyelinating treatments like clemastine correspond to quantitative histological and ultrastructural measures of myelination [90]. This biological certification strengthens the utility of VEP biomarkers for preclinical verification of therapeutic efficacy.
Applications in Addiction Research and Future Directions
The application of VEP-based biomarkers to addiction research offers unique insights into the plasticity mechanisms underlying substance use disorders. Addiction involves profound alterations in brain reward circuits that can be conceptualized as maladaptive learning processes [2]. The neural plasticity that enables learning and adaptation becomes co-opted by addictive substances, leading to compulsive drug-seeking despite negative consequences.
VEP paradigms can probe the integrity of plasticity mechanisms across different stages of addiction and recovery. The reward prediction error signaling central to addiction involves dopamine-mediated plasticity that shares mechanisms with the LTP-like plasticity measured through VEP protocols [2]. As addiction progresses, there is a shift from pleasure-seeking to compulsive use marked by reduced hedonic effects but intensified craving—a transition that may reflect alterations in plasticity mechanisms measurable through VEP biomarkers [41].
Future research directions should focus on:
Linking VEP plasticity measures with specific addiction phenotypes: Different substance use disorders may manifest distinct patterns of plasticity impairment.
Tracking plasticity changes during recovery: VEP biomarkers could objectively measure the restoration of normative plasticity during abstinence and treatment.
Evaluating plasticity-enhancing interventions: Non-invasive neuromodulation approaches such as rTMS are being investigated for addiction treatment [38], with VEP biomarkers providing measures of target engagement.
Integrating multi-modal assessments: Combining VEP with other physiological, behavioral, and self-report measures creates comprehensive plasticity profiles.
As research continues to elucidate the complex relationships between synaptic plasticity, reward processing, and addiction, VEP-based biomarkers offer a versatile toolset for advancing both theoretical understanding and clinical applications. The non-invasive nature, relatively low cost, and translational potential of VEP paradigms position them as valuable components of the addiction research arsenal, capable of bridging mechanistic insights from animal models to human clinical applications.
Comparative Analysis of Land-based vs. Water-based Exercise on Neuroplasticity
This technical review examines the differential impacts of land-based and water-based aerobic exercise on neuroplasticity, framed within the context of addiction development and recovery research. While both exercise modalities demonstrate significant neuroplastic benefits, emerging evidence suggests they may engage distinct molecular pathways and neural mechanisms. Land-based exercise typically produces more robust functional performance improvements, whereas water-based exercise appears to offer unique advantages for specific populations and may engage different neuroplasticity-related biomarkers. This analysis synthesizes current findings from randomized controlled trials, biomarker studies, and mechanistic investigations to provide researchers and drug development professionals with a comprehensive framework for integrating exercise modalities into targeted neuroplasticity interventions for addiction treatment.
Neuroplasticity, the nervous system's capacity to adapt structurally and functionally to experiential demands, serves as a fundamental biological substrate for both addiction development and recovery [26]. In addiction, maladaptive neuroplasticity occurs through repeated drug exposure that hijacks reward circuitry, strengthens conditioned associations to drug cues, and creates stable memory traces that drive compulsive drug-seeking behavior [26] [14]. This pathologically strengthened circuitry involves increased dendritic spine density in the nucleus accumbens, disrupted glutamate homeostasis, and transcription factor alterations such as delta FosB accumulation [26].
Conversely, exercise-induced neuroplasticity represents a powerful counter-mechanism that can potentially remodel neural circuits compromised by addiction. Physical activity promotes adaptive changes through multiple mechanisms including increased neurotrophic factor expression (particularly BDNF), enhanced synaptic plasticity, improved functional connectivity in fronto-hippocampal circuits, and elevated neurogenesis [92] [93]. The comparative efficacy of different exercise modalities—specifically land-based versus water-based—in stimulating these beneficial plastic changes remains an area of active investigation with significant implications for designing targeted interventions for substance use disorders.
Comparative Effects on Neuroplasticity Outcomes
Cognitive and Functional Outcomes
Table 1: Comparative Effects on Cognitive and Functional Measures
| Outcome Measure | Land-based Exercise | Water-based Exercise | Population | Citation |
|---|---|---|---|---|
| Functional Performance | Significant improvements in figure-8 hop and single-limb side-hop tests | Less improvement in functional tasks | Athletes with Chronic Ankle Instability | [94] |
| Quality of Life (Physical) | Moderate improvements | Superior improvements in physical and overall quality of life | Athletes with Chronic Ankle Instability | [94] |
| Processing Speed | Limited biomarker mediation | KIF3C and TBX3 proteins mediated improvements in Stroop Color test | Older Adults with MCI | [95] |
| Memory Functions | Improved encoding and recall performance | Comparable improvements in verbal and visual memory | Older Mexican Adults | [96] |
| Executive Functions | Variable effects on cognitive flexibility and inhibitory control | No significant changes observed in 4-week program | Older Mexican Adults | [96] |
Research indicates that both land-based and water-based exercise enhance cognitive function, albeit through potentially different mechanisms. A study on older adults with mild cognitive impairment found that water-based exercise uniquely engaged specific neuroplasticity-related biomarkers (KIF3C and TBX3) that mediated improvements in processing speed, particularly on the Stroop Color test—a measure of executive function that assesses response inhibition and cognitive flexibility [95]. In contrast, land-based exercise did not demonstrate similar biomarker mediation despite comparable clinical improvements, suggesting divergent mechanistic pathways for similar functional outcomes.
For memory domains, both modalities show comparable efficacy. A 4-week intervention with older Mexican adults demonstrated that both aquatic and land-based exercise significantly improved encoding and recall performance on the Rey Auditory Verbal Learning Test, along with enhanced visual memory on the Rey Osterrieth Complex Figure test [96]. This suggests that the mnemonic benefits of exercise may be modality-independent, potentially engaging shared hippocampal and medial temporal lobe circuits.
Neurobiological Mechanisms and Biomarkers
Table 2: Neurobiological Mechanisms and Biomarkers
| Mechanism/Biomarker | Land-based Exercise | Water-based Exercise | Research Context |
|---|---|---|---|
| BDNF Expression | Robust increases demonstrated | Presumed similar effects, limited direct evidence | Animal models and human studies |
| Fronto-Hippocampal Connectivity | Enhanced functional connectivity | Comparable benefits suggested, less researched | Human neuroimaging studies |
| KIF3C Protein | No significant mediation effects | Mediates processing speed improvements | Older adults with MCI |
| TBX3 Protein | No significant mediation effects | Mediates processing speed improvements | Older adults with MCI |
| Dopamine Signaling | Normalizes reward processing | Potential similar effects, unexplored in addiction | Addiction recovery models |
| Glutamate Homeostasis | Restores balance in preclinical models | Unknown effects on glutamate systems | Cocaine addiction models |
The neurobiological mechanisms underlying exercise-induced neuroplasticity differ between modalities in potentially significant ways. Land-based exercise has been more extensively studied and demonstrates robust effects on BDNF expression, a critical neurotrophin that promotes synaptic plasticity, neurogenesis, and neuronal survival [93]. Animal models reveal that land-based aerobic exercise (typically modeled using running wheels or treadmills) enhances hippocampal neurogenesis and strengthens functional connectivity along the fronto-hippocampal axis—circuitry critically implicated in both cognitive function and addiction pathology [93].
Water-based exercise may engage complementary mechanisms that are just beginning to be understood. The identification of KIF3C and TBX3 as specific mediators of cognitive improvement following aquatic exercise points to potentially unique molecular pathways [95]. KIF3C is a kinesin motor protein involved in intracellular transport, while TBX3 is a transcription factor implicated in development—neither has been prominently associated with land-exercise-induced neuroplasticity. This suggests that the unique physical properties of water-based exercise (buoyancy, hydrostatic pressure, viscosity) may engage distinct molecular cascades to promote cognitive benefit.
Experimental Protocols and Methodologies
Land-based Exercise Protocols
Chronic Ankle Instability Study Protocol [94]:
- Duration: 8 weeks, 24 sessions of 30-45 minutes each
- Frequency: 3 sessions per week
- Exercises: Balance training exercises performed on land
- Assessments: Functional ankle instability (CAIT), kinesiophobia (TSK-17), quality of life (SF-36), dynamic postural control (Y Balance Test), functional performance (Figure-8 hop and single-limb side-hop tests)
- Population: Athletes with chronic ankle instability (n=20)
Land-based Protocol for Older Adults with MCI [95] [96]:
- Duration: 4-12 weeks
- Frequency: 3 sessions per week, 60 minutes each
- Intensity: Moderate aerobic exercise (50-70% heart rate reserve)
- Exercises: Walking, cycling, or similar aerobic activities
- Cognitive Assessments: Trail Making Test, Stroop Test, Symbol Digit Modalities Test, Rey Auditory Verbal Learning Test
Water-based Exercise Protocols
Aquatic Exercise for Older Adults [96]:
- Duration: 4 weeks, 12 sessions
- Frequency: 3 sessions per week, 60 minutes each
- Water Temperature: Maintained at 30°C
- Water Depth: Shoulder to waist level
- Exercises: Aerobic and resistance exercises performed in a structured pool environment including:
- Warm-up: 5 minutes of walking and joint mobility exercises
- Aerobic component: 30 minutes of continuous movement (e.g., walking, cross-country skiing motion, jumping jacks)
- Resistance component: 15 minutes using water resistance (e.g., upper and lower limb movements against water viscosity)
- Cool-down: 10 minutes of stretching and relaxation
- Population: Older Mexican adults (n=9)
Water-based Balance Training [94]:
- Duration: 8 weeks, 24 sessions of 30-45 minutes each
- Frequency: 3 sessions per week
- Exercises: Balance training exercises performed in water
- Assessments: Identical to land-based protocol for direct comparison
- Population: Athletes with chronic ankle instability (n=21)
Figure 1: Experimental Workflow for Comparative Exercise Studies
Implications for Addiction Research and Treatment
The differential neuroplastic effects of land-based versus water-based exercise have significant implications for addiction treatment and recovery. Addiction fundamentally represents a disorder of maladaptive learning and compromised neural circuitry in prefrontal regulatory regions and the striatal reward system [26] [14]. Exercise represents a promising non-pharmacological intervention that can potentially reverse these pathological plastic changes through multiple mechanisms:
Dopamine System Normalization: Both exercise modalities likely modulate the mesolimbic dopamine system, which is critically implicated in addiction. By providing alternative sources of reward and stimulation, exercise may help normalize dopamine signaling that becomes dysregulated in substance use disorders [14].
Prefrontal Cortex Strengthening: Executive function deficits stemming from prefrontal dysfunction are common in addiction. The demonstrated benefits of both exercise modalities—particularly land-based exercise—on executive functions suggest potential for strengthening cognitive control mechanisms that are essential for maintaining abstinence [96] [93].
Stress Response Modulation: Both land and water-based exercise modulate the hypothalamic-pituitary-adrenal axis and reduce physiological stress responses. Since stress is a potent trigger for relapse, this effect may be particularly valuable in addiction recovery [78].
Cognitive Bias Restructuring: The differential effects on specific cognitive domains (e.g., the unique benefits of water-based exercise on processing speed mediated by specific biomarkers) suggest that modality selection could be tailored to individual cognitive deficits commonly observed in addiction [95].
Figure 2: Neuroplasticity Pathways in Addiction and Exercise Modulation
Research Reagents and Methodological Tools
Table 3: Essential Research Reagents and Methodological Tools
| Tool/Reagent | Application | Function in Neuroplasticity Research |
|---|---|---|
| SomaScan Neuroscience Panel | Biomarker discovery | Multiplexed proteomic analysis of 1,316 neurology-related analytes in plasma samples [95] |
| BDNF Assays (ELISA, Western Blot) | Neurotrophin measurement | Quantifies brain-derived neurotrophic factor, a key mediator of exercise-induced neuroplasticity [93] |
| fMRI/BOLD Imaging | Functional brain assessment | Measures changes in blood oxygenation related to neural activity following exercise interventions [93] |
| Rey Auditory Verbal Learning Test (RAVLT) | Cognitive assessment | Evaluates verbal memory and learning functions sensitive to exercise interventions [96] |
| Stroop Color and Word Test | Executive function assessment | Measures processing speed, cognitive flexibility, and response inhibition [95] |
| Trail Making Test (TMT-A/B) | Processing speed assessment | Evaluates visual attention and task switching abilities [95] |
| Y Balance Test | Functional performance | Assesses dynamic balance and neuromuscular control [94] |
| Gene Expression Arrays | Molecular mechanisms | Profiles transcription changes in neuroplasticity-related genes (e.g., TBX3, KIF3C) [95] |
The comparative analysis of land-based versus water-based exercise reveals a complex landscape of neuroplastic effects with significant implications for addiction research. While both modalities promote beneficial neural adaptations, they appear to engage partially distinct mechanisms and produce differential cognitive and functional outcomes. Land-based exercise demonstrates particular efficacy for enhancing functional performance and executive functions, while water-based exercise offers unique advantages for quality of life and engages specific biomarker pathways that may be particularly relevant for individuals with comorbidities that limit land-based activity.
Future research should prioritize several key directions: (1) direct comparison of these modalities in addiction populations, (2) investigation of combined/interleaved training approaches to maximize therapeutic benefits, (3) longer-term studies to determine the sustainability of observed effects, and (4) mechanistic studies to elucidate the molecular pathways uniquely engaged by each modality. Such research will enable more precise exercise prescriptions tailored to individual patient characteristics and addiction profiles, ultimately enhancing recovery outcomes through targeted neuroplastic modulation.
The study of neuroplasticity—the brain's ability to reorganize its structure, function, and connections in response to experience—provides a critical framework for understanding both the development of and recovery from addiction [97] [14]. In the context of addiction, repeated drug exposure triggers maladaptive plasticity in brain reward circuits, strengthening neural pathways associated with drug-seeking behavior while weakening those responsible for natural rewards and cognitive control [14]. This mechanistic understanding positions neuroplasticity as a central therapeutic target, where interventions aim to reverse detrimental changes or harness the brain's innate adaptive capacity to support recovery.
Validated preclinical models that accurately measure neuroplasticity are therefore indispensable for translational research. This technical guide examines the validation pathway from foundational rodent brain slice studies to sophisticated human sensory plasticity protocols, with particular emphasis on their application in addiction research. We detail experimental methodologies, quantitative benchmarks, and analytical approaches that establish construct validity for measuring plasticity mechanisms relevant to addiction pathology and treatment.
Rodent Brain Slice Models: Foundational Plasticity Assays
Ex Vivo Long-Term Potentiation (LTP) Protocols
The hippocampal brain slice preparation remains the gold standard for investigating synaptic plasticity mechanisms at the cellular level. This system allows precise control of the extracellular environment while permitting pharmacological and electrophysiological interrogation of synaptic function.
Slice Preparation and Viability: Transverse hippocampal slices (400 μm thick) are prepared from juvenile rodents (typically 4-6 weeks old) using a tissue chopper or vibratome. Slices are maintained in oxygenated (95% O₂/5% CO₂) artificial cerebrospinal fluid (aCSF) containing (in mM): 124 NaCl, 3 KCl, 26 NaHCO₃, 1.25 NaH₂PO₄, 2 MgSO₄, 2 CaCl₂, and 10 glucose. Viability is confirmed by stable field excitatory postsynaptic potential (fEPSP) responses for at least 30 minutes prior to experimentation [98].
LTP Induction Paradigms: Two principal stimulation patterns are employed to induce LTP:
- High-Frequency Stimulation (HFS): Delivering 1-2 trains of 100 Hz stimulation for 1 second each, separated by 20-second intervals. This protocol induces robust, protein synthesis-independent LTP that typically persists for 2-3 hours [98].
- Theta-Burst Stimulation (TBS): Applying 5-10 bursts of 4 pulses at 100 Hz, with 200 ms inter-burst intervals, which mimics endogenous hippocampal theta rhythms. TBS generally produces longer-lasting, protein synthesis-dependent LTP more relevant to learning and memory processes [98] [99].
Data Acquisition and Analysis: fEPSPs are recorded in the stratum radiatum of CA1 following stimulation of Schaffer collateral axons. The initial slope of the fEPSP is measured and normalized to baseline. LTP is quantified as the percentage increase in fEPSP slope 50-60 minutes post-induction compared to baseline [98].
Visual Evoked Potentials in Rodents
In vivo visual evoked potentials (VEPs) in rodents bridge reduced slice preparations and complex human behavior. The protocol involves surgically implanting electrodes in the primary visual cortex (V1) of anesthetized or awake, head-fixed mice [99].
- Stimulation Paradigms: Awake, head-fixed mice are presented with repetitive visual stimuli, such as:
- Plasticity Measurement: VEP amplitude is measured before and after stimulus exposure. Plasticity is expressed as the normalized change in VEP amplitude, which develops over hours to days for SRP but can occur within seconds for FVP [99].
- Genetic Models: The use of transgenic animals, such as Grin2a (NR2A) knockout mice, models plasticity deficits observed in neuropsychiatric disorders, including addiction, providing a platform for therapeutic validation [99].
Human Sensory Plasticity Protocols: Translational Biomarkers
Visual Evoked Potential (VEP) Modulation Protocols
Noninvasive EEG recordings of VEPs have emerged as promising biomarkers for assessing LTP-like plasticity in the human visual cortex [98]. The standard protocol involves recording baseline VEPs, applying a plasticity-inducing modulation block, and tracking post-modulation VEP changes.
Experimental Workflow for Human VEP Protocols:
Table 1: Comparison of VEP Modulation Protocols for Assessing Human Visual Cortical Plasticity
| Protocol | Stimulation Parameters | Plasticity Onset | Plasticity Duration | Plasticity Profile | Best Applications |
|---|---|---|---|---|---|
| Low-Frequency (LF) [98] | 2 Hz for 10 min (1200 stimuli) | Rapid (peak at 2 min) | Short (<12 min) | Transient enhancement | Acute drug effects, baseline plasticity |
| Repeated Low-Frequency (RLF) [98] | Repeated 2 Hz cycles | Sustained | Long (up to 22 min) | Progressive, sustained | Longer-term modulation studies |
| High-Frequency (HF) [98] | ~9 Hz for 2 min | Immediate | Brief (sharp decay) | Sharp, high-magnitude increase | Sensitivity testing, STP assessment |
| Theta-Pulse Stimulation (TPS) [98] | Theta-frequency pulses | Gradual | Extended (up to 28 min) | Moderate, prolonged | Therapeutic development, chronic studies |
Key Methodological Considerations for Human VEP
- Participant Selection: Studies typically enroll healthy adults (age 20-40) with no history of neurological, psychiatric, or ocular disorders, not taking psychoactive medications, and with normal or corrected-to-normal vision [98].
- Stimulus and Task: Checkerboard reversal stimuli (0.5° visual angle) are presented at 1-2 reversals per second. Participants maintain fixation on a central cross and verbally identify randomly presented numbers to ensure attention [98].
- Data Quantification: VEP amplitude is measured from the N1 to P1 components. The plasticity index is calculated as the percentage change from baseline at each post-modulation time point [98].
Bridging Preclinical and Clinical Research in Addiction
Maladaptive Plasticity in Addiction
Addiction fundamentally involves experience-dependent learning driven by maladaptive neuroplasticity [14]. Repeated drug use increases dopamine release, strengthening connections in reward pathways (e.g., ventral tegmental area to nucleus accumbens) and creating powerful drug-cue associations. Simultaneously, plasticity in prefrontal circuits governing executive control is impaired, reducing capacity for self-regulation [14]. These opposing plasticity processes—hyper-sensitization of reward signals and hypo-function of control systems—underpin the compulsive nature of addiction. VEP and other sensory plasticity protocols can detect these circuit-level alterations, serving as biomarkers for disease severity and treatment response.
Harnessing Plasticity for Recovery
Therapeutic interventions for addiction aim to reverse maladaptive plasticity or harness the brain's innate plastic capacity for recovery. Cognitive Behavioral Therapy (CBT) utilizes neuroplasticity to create new, healthier cognitive patterns and behaviors [14]. Contingency Management, based on operant conditioning, reinforces abstinence through positive rewards, actively reshaping behavioral outputs via plastic mechanisms [14]. Pharmacotherapies may facilitate this process by creating a neurochemical environment conducive to adaptive plasticity.
Signaling Pathways in Neuroplasticity and Addiction:
Validation and Translation
Effective translation requires demonstrating that preclinical models accurately predict human therapeutic outcomes. Key validation steps include:
- Face Validity: The model should exhibit plasticity impairments analogous to those seen in human addiction. For example, mouse models of schizophrenia (Grin2a knockout) show VEP plasticity deficits mirroring those in patients [99].
- Predictive Validity: The model's response to pharmacological or behavioral interventions should correlate with clinical outcomes. For instance, if a compound restores impaired VEP plasticity in a rodent model of addiction, it should similarly improve plasticity and clinical symptoms in patients.
- Construct Validity: The neurobiological mechanisms underlying plasticity in the model (e.g., NMDAR dependence, LTP-like changes) should align with those operating in humans [98] [99].
Table 2: Key Research Reagent Solutions for Plasticity Studies
| Item | Function/Application | Example Use |
|---|---|---|
| NMDAR Antagonists (e.g., AP5, MK-801) | Block NMDA receptors to test necessity for LTP induction | Establishing NMDAR-dependence of VEP plasticity [98] [99] |
| BDNF (Brain-Derived Neurotrophic Factor) | Key regulator of synaptic plasticity and neuronal survival | Investigating trophic factor effects on plasticity maintenance |
| Bromodeoxyuridine (BrdU) | Thymidine analog labeling newly generated cells | Assessing adult neurogenesis in plasticity studies [97] |
| Electrophysiology Setup (microelectrodes, amplifiers, acquisition software) | Recording field potentials (fEPSPs, VEPs, LFP) | Measuring synaptic responses in slice preparations and in vivo [98] [99] |
| EEG Systems (high-density, 64+ channels) | Noninvasive recording of human brain activity | Acquiring VEPs in human sensory plasticity protocols [98] |
| Stimulation Software (e.g., Expyriment, PsychoPy) | Precisely controlling visual stimulus parameters | Presenting checkerboard reversals or grating stimuli [98] |
| hPSC-Derived Neural Cells | Human-relevant platform for mechanistic studies | Modeling human cortical circuitry and testing therapeutics [100] |
The validation continuum from rodent brain slices to human VEP protocols provides a robust framework for investigating neuroplasticity mechanisms relevant to addiction. Rodent models offer unparalleled mechanistic insight through precise electrophysiological and genetic manipulation, while human SRP/VEP protocols provide noninvasive, translational biomarkers for clinical studies. As research continues to elucidate how addictive drugs hijack brain plasticity and how recovery-oriented interventions can restore it, these validated preclinical models will remain essential for developing effective treatments for substance use disorders. The future of addiction therapeutics lies in strategically targeting the brain's innate plastic capacity to reverse maladaptive changes and promote sustainable recovery.
The treatment of substance use disorders (SUDs) requires interventions that are not only behaviorally effective but also capable of countering the neurobiological changes sustained by chronic drug use. Within the context of addiction, neuroplasticity—the nervous system's ability to change its activity in response to stimuli—is a double-edged sword [3]. Chronic substance use induces maladaptive neuroplasticity, strengthening neural pathways associated with drug-seeking while weakening circuits governing executive control and self-regulation [14]. This paper evaluates three prominent behavioral interventions—Cognitive-Behavioral Therapy (CBT), Mindfulness-based Interventions (MBIs), and Contingency Management (CM)—through the lens of their comparative efficacy and their capacity to harness neuroplasticity for therapeutic benefit. A growing body of evidence suggests these therapies promote healthy neuroplastic changes, potentially reversing the neural pathophysiology of addiction [3] [101]. The following sections provide a detailed analysis of each modality's clinical outcomes, methodological protocols, and underlying neurobiological mechanisms, offering a scientific resource for researchers and drug development professionals.
Comparative Efficacy and Outcomes
Clinical research demonstrates that CBT, CM, and MBIs each produce distinct effect profiles across substance use outcomes, with efficacy often varying across the temporal course of recovery.
Table 1: Comparative Clinical Outcomes of Behavioral Interventions for Stimulant Dependence
| Intervention | Short-Term Abstinence (End of Treatment) | Long-Term Abstinence (Follow-Up) | Effect on Craving | Key Strengths |
|---|---|---|---|---|
| Contingency Management (CM) | High efficacy. Participants 2.4x more likely to submit stimulant-negative urine tests during treatment [102]. | Moderate. Self-reported use reductions at follow-up; urinalysis advantages may not persist [103]. | Indirect reduction via reinforcement of abstinence. | Produces robust retention and abstinence during active intervention [103] [104]. |
| Cognitive-Behavioral Therapy (CBT) | Moderate efficacy. Lower rates of stimulant use during study period compared to CM [103]. | High efficacy. Produces comparable long-term outcomes to CM at 52-week follow-up [103]. | Targets craving via cognitive restructuring and skill-building. | Produces durable, long-term outcomes; teaches coping skills for relapse prevention [103]. |
| Mindfulness-Based Interventions (MBIs) | Moderate efficacy. May slightly reduce percentage of days with substance use post-treatment vs. other treatments [105]. | Moderate efficacy. May sustain slight reduction in days of substance use at 4-10 month follow-up [105]. | Mixed evidence. Theoretical basis for reducing craving via decentering and non-reactivity [101]. | Effective in reducing comorbid anxiety/depression; may target automaticity [105] [101]. |
Table 2: Secondary and Mechanistic Outcomes Across Interventions
| Intervention | Retention & Adherence | Impact on Co-occurring Conditions | Postulated Core Mechanism of Action |
|---|---|---|---|
| Contingency Management (CM) | High study attrition in some SMI populations [102], but effective retention in others [104]. | Reduces alcohol use, injection drug use, psychiatric symptoms, and psychiatric hospitalizations [102]. | Operant Conditioning: Positive reinforcement (vouchers, prizes) for verified abstinence strengthens alternative behaviors [104] [14]. |
| Cognitive-Behavioral Therapy (CBT) | Good retention in structured group settings [103]. | Targets underlying cognitions and moods that drive substance use. | Cognitive Restructuring & Skill Acquisition: Identifies and modifies drug-related thoughts; teaches coping skills to handle high-risk situations [103] [14]. |
| Mindfulness-Based Interventions (MBIs) | Little to no difference in attrition compared to no treatment or other treatments [105]. | Shows benefit for emotional distress, depression, anxiety, and stress, which are common triggers for use [101]. | Metacognitive Awareness & De-automatization: Cultivates non-judgmental, present-moment awareness to disrupt automatic habitual responses [101]. |
Detailed Experimental Protocols
A clear understanding of the methodological details of key clinical trials is essential for evaluating the evidence base and designing future research.
Protocol for Contingency Management Trials
The protocol from a randomized controlled trial for individuals with serious mental illness and stimulant dependence illustrates a rigorous CM methodology [102].
- Design: Three-month randomized controlled trial with a three-month post-treatment follow-up period.
- Participants: 176 outpatients with co-occurring serious mental illness (e.g., schizophrenia, bipolar disorder, recurrent major depressive disorder) and stimulant dependence.
- Randomization: Urn-randomization procedure to balance groups on gender, substance use severity, mood vs. psychotic disorder, and recent psychiatric hospitalization.
- Intervention (Contingent Group):
- Participants provided urine samples three times per week (Monday, Wednesday, Friday).
- Each stimulant-negative urine sample was reinforced using a variable magnitude of reinforcement procedure, often known as the "fishbowl" prize draw system.
- Participants drew slips of paper from a bowl; slips indicated a prize of varying value (e.g., small, large, jumbo) or "good job!" with no prize. This probabilistic system maintains engagement at a lower cost than fixed-value vouchers.
- Control Condition (Non-Contingent Group):
- Participants provided samples on the same schedule but received rewards of comparable value regardless of urine test results, controlling for the non-specific effects of material reward and staff interaction.
- Measures:
- Primary Outcome: Urinalysis for amphetamine, methamphetamine, and cocaine (onsite immunoassays).
- Secondary Outcomes: Self-reported days of substance use (Addiction Severity Index-lite), psychiatric symptom severity (Brief Symptom Inventory; Positive and Negative Symptom Scale), HIV-risk behavior, and administrative data on service utilization (hospitalizations, incarcerations).
Protocol for Cognitive-Behavioral Therapy Trials
A direct comparison study of CM and CBT for stimulant-dependent individuals provides a standard protocol for group-based CBT [103].
- Design: 16-week randomized clinical trial with assessments at baseline, week 17, 26, and 52.
- Participants: 171 stimulant-dependent individuals.
- Intervention (CBT Condition):
- Participants attended three 90-minute group therapy sessions each week for 16 weeks.
- The therapy was based on a structured, manualized protocol focusing on key skills:
- Understanding the relationship between thoughts, feelings, and behaviors related to drug use.
- Coping with cravings and urges.
- Refusing offers of drugs and alcohol.
- Managing time and increasing non-drug-related rewarding activities.
- Problem-solving skills for intrapersonal and interpersonal challenges.
- Measures:
- Primary Outcomes: Urinalysis for stimulant drugs and self-reported stimulant use.
- Secondary Outcomes: Psychiatric disorders, alcohol use, and concomitant social problems.
Neuroplastic Mechanisms of Action
The therapeutic effects of behavioral interventions are increasingly understood through their ability to induce beneficial neuroplastic changes, countering the maladaptive plasticity of addiction.
Figure 1: Neuroplastic Pathways of Behavioral Therapies. This diagram illustrates how CBT, CM, and Mindfulness target dysregulated brain circuits in addiction to promote healthy neuroplasticity.
Cognitive-Behavioral Therapy
CBT functions as a form of cognitive training that strengthens top-down executive control networks. Addiction is characterized by a hijacking of the brain's reward system and a weakening of prefrontal cortical regions responsible for inhibitory control, decision-making, and self-regulation [14]. CBT directly targets these deficits by engaging patients in exercises that require cognitive effort to identify automatic thoughts, challenge drug-related beliefs, and practice alternative coping strategies. This repeated mental exercise is hypothesized to promote neuroplasticity within the prefrontal cortex (PFC), enhancing its functional capacity and strengthening its inhibitory control over the limbic-striatal reward system [14]. This restored balance between top-down control and bottom-up drives is a key mechanism underlying the durable, long-term benefits of CBT.
Contingency Management
CM operates on principles of operant conditioning to systematically reshape reward learning. Chronic drug use leads to a downregulation of dopamine D2 receptors and a blunted response to natural, non-drug rewards, making drug use the most salient reinforcer [3]. CM directly counteracts this by providing alternative, immediate, and tangible rewards for verified abstinence. This process leverages the brain's inherent neuroplasticity to strengthen new, adaptive neural pathways associated with non-drug-related behaviors. By making abstinence more rewarding, CM can help recalibrate the dysregulated dopamine reward pathway, increasing the salience of natural rewards and facilitating a "re-learning" process that is fundamental to recovery [3] [104].
Mindfulness-Based Interventions
MBIs target the core addictive process of automaticity—the habitual, cue-driven drug-seeking that occurs with minimal conscious volition [101]. Through practices like focused attention and open monitoring, MBIs train individuals to cultivate metacognitive awareness, allowing them to observe cravings and negative emotions without automatically reacting to them. This "decentering" is thought to promote neuroplasticity by increasing functional connectivity between prefrontal cognitive control networks and limbic-striatal circuits [101]. Neuroimaging studies suggest that mindfulness practice can strengthen the anterior cingulate cortex (ACC) and ventromedial PFC, regions critical for self-monitoring and regulation, thereby providing a "wedge" in the cycle of automatic reactivity and helping to de-automatize addictive behaviors [101].
The Scientist's Toolkit: Research Reagents & Materials
Table 3: Essential Materials and Assessments for Behavioral Therapy Research
| Item/Tool | Primary Function in Research | Exemplar Use in Context |
|---|---|---|
| Urinary Immunoassay Cups (e.g., Integrated E-Z Split Key Cup) | Rapid, on-site screening for recent drug use (amphetamines, cocaine, marijuana, opiates) [102]. | Primary objective outcome measure in CM trials to determine reinforcement eligibility [102]. |
| Structured Clinical Interviews (e.g., MINI - Mini International Neuropsychiatric Interview) | Standardized diagnostic tool to confirm participant eligibility based on DSM/ICD criteria for SUD and co-occurring disorders [102]. | Used at screening to establish diagnoses of stimulant dependence and serious mental illness [102]. |
| Manualized Therapy Protocols | Ensure treatment fidelity, standardization, and replicability across therapists and study sites [103] [104]. | CBT condition delivered via a fixed protocol with three 90-minute group sessions per week [103]. |
| Addiction Severity Index (ASI) | A semi-structured interview assessing multiple domains of life functioning impacted by substance use (medical, employment, drug, alcohol, legal, family/social, psychiatric) [102]. | Used as a secondary outcome measure to track changes in self-reported days of substance use and broader life function [102]. |
| Voucher/Prize Reinforcement System | The tangible reinforcer in CM; vouchers are redeemable for goods/services, or a prize draw system is used [104]. | Variable magnitude "fishbowl" method used to reinforce stimulant-negative urine samples in CM trials [102] [104]. |
Figure 2: Experimental Workflow for a Comparative Trial. This flowchart visualizes the sequence of a typical RCT comparing CBT, CM, and a control condition.
The comparative efficacy of CBT, CM, and MBIs cannot be reduced to a single hierarchy; rather, each demonstrates a unique profile of strengths. CM produces the most robust, short-term abstinence, making it ideal for initiating recovery and engaging patients in treatment. CBT produces durable, long-term outcomes, likely due to its focus on teaching enduring cognitive and behavioral coping skills. MBIs show promise in addressing the automaticity of addiction and comorbid emotional distress. The emerging paradigm in addiction treatment research views these therapies not merely as behavioral modifiers but as potent neuromodulators. Their ability to harness experience-dependent neuroplasticity to reverse the maladaptive neural changes wrought by addiction represents a fundamental shift in understanding their mechanisms. Future research should prioritize multimodal studies that integrate detailed clinical assessment with neuroimaging and biomarker analysis to further elucidate the plastic changes induced by these therapies, paving the way for more personalized and neurobiologically-informed treatment strategies.
Neuroplasticity, the brain's capacity to adapt its structure and function in response to experience, represents a fundamental process disrupted across major psychiatric disorders. This whitepaper examines deficits in neuroplasticity as a transdiagnostic mechanism underlying substance use disorders (SUDs), depression, and schizophrenia. While each disorder manifests distinct clinical phenotypes, emerging evidence reveals striking convergences in their underlying neurobiological substrates, particularly regarding impairments in synaptic strengthening, neuronal connectivity, and cellular resilience. Understanding these shared pathways provides unprecedented opportunities for developing novel therapeutic interventions that target core plasticity mechanisms rather than disorder-specific symptoms. The examination of these cross-disorder insights is framed within a broader research context on neuroplasticity in addiction development and recovery, highlighting how maladaptive plasticity perpetuates illness and how adaptive plasticity can be harnessed for therapeutic benefit.
Research conducted over the past decade has demonstrated that SUDs, depression, and schizophrenia each involve substantial alterations in brain regions critical for learning, reward processing, and executive function [26] [106] [107]. The prefrontal cortex, hippocampus, amygdala, and striatum show pronounced structural and functional changes across these disorders, suggesting common vulnerabilities in the brain's circuit architecture. Furthermore, neurotransmitter systems implicated in plasticity—particularly glutamate, dopamine, and GABA—show dysregulation across all three conditions, though through distinct molecular mechanisms. This whitepaper synthesizes evidence from neuroimaging, neurophysiological, and molecular studies to provide researchers and drug development professionals with an integrated perspective on plasticity deficits across these disorders, with particular emphasis on experimental methodologies, signaling pathways, and promising therapeutic targets.
Comparative Pathology of Neuroplasticity Across Disorders
Structural and Functional Brain Alterations
Table 1: Neuroplasticity-Related Brain Alterations in SUDs, Depression, and Schizophrenia
| Brain Region | Substance Use Disorders | Major Depression | Schizophrenia |
|---|---|---|---|
| Prefrontal Cortex | Reduced gray matter volume; impaired glutamate homeostasis [26] [5] | Decreased gray matter volume and cortical thinning [106] | Altered dopamine neurotransmission; dendritic spine deficits [107] [108] |
| Hippocampus | Structural recovery during abstinence [5] | Reduced volume; suppressed neurogenesis [106] | Functional deficits in memory encoding and retrieval |
| Striatum | Dopamine transporter loss recovering with abstinence [5] | Decreased grey matter intensity [106] | Altered reward processing and motor control |
| Amygdala | Hyper-reactivity to drug cues [26] | Increased volume and hyperactivity [106] | Emotion processing disturbances |
| Cortical Inhibition | Reduced frontal activity during impulse control [26] | Default mode network overactivation [106] | Reduced GABAergic neurotransmission [107] |
Molecular Mechanisms of Plasticity Impairment
Table 2: Molecular Mechanisms Underlying Plasticity Deficits
| Molecular Target | SUDs | Depression | Schizophrenia |
|---|---|---|---|
| Dopamine Signaling | Increased release with drugs vs. natural rewards [26] | Altered dopaminergic pathways in anhedonia [106] | Prefrontal D1 receptor dysfunction [108] |
| Glutamate System | Reduced basal extracellular glutamate; potentiated synaptic release [26] | Glutamate accumulation due to impaired astrocyte function [106] | NMDA receptor hypofunction [107] |
| GABA System | Secondary dysregulation following glutamate/dopamine changes | Impaired GABAergic interneurons in cortical regions | Decreased GABAergic interneurons; altered GAD67 [107] [108] |
| BDNF | Increased in ventral tegmental area during incubation [26] | Reduced neurotrophic support [106] | Altered expression impacting neuronal development |
| Transcription Factors | Delta FosB accumulation [26] | Changes in stress-responsive transcription factors | Altered expression of immediate early genes |
Disorder-Specific Plasticity Deficits: Mechanisms and Methodologies
Substance Use Disorders: Maladaptive Learning and Memory
In substance use disorders, drugs of abuse co-opt natural reward learning mechanisms through intense activation of the brain's dopamine systems, producing powerful learned associations between drug-predictive cues and reward [26]. With repeated exposure, the reward system becomes reflexively activated by cues alone, triggering compulsive drug-seeking behavior. This process involves lasting neuroadaptations in corticostriatal-limbic circuits that normally subserve learning and goal-directed behaviors [109].
The neuroplastic changes in addiction are characterized by a cascade of molecular events. Animal models demonstrate that repeated drug exposure increases levels of brain-derived neurotrophic factor (BDNF) in the ventral tegmental area and nucleus accumbens during abstinence, a process correlated with the "incubation" of craving [26]. Additionally, transcription factors such as Delta FosB accumulate in dopamine terminals, potentially promoting motivated drug-taking behaviors. At the structural level, increased dendritic spine density in nucleus accumbens medium spiny neurons persists during abstinence, potentially underpinning long-term vulnerability to relapse [26].
A critical mechanistic insight involves dysregulation of glutamate homeostasis. Following chronic cocaine exposure, research has demonstrated reduced basal extracellular glutamate levels in the nucleus accumbens alongside potentiated release of synaptic glutamate during drug-seeking [26]. This imbalance is associated with increased AMPA to NMDA current ratios and loss of both long-term potentiation (LTP) and long-term depression (LTD)—the fundamental mechanisms underlying learning and memory [26].
Experimental Protocol: Reinstatement Model of Relapse
- Objective: To study neural mechanisms underlying drug-seeking behavior and relapse in rodents.
- Subjects: Rats trained to self-administer intravenous cocaine.
- Apparatus: Operant conditioning chambers with levers and cue lights.
- Procedure:
- Training Phase: Rats learn to press a lever for cocaine infusion paired with light cue.
- Extinction Phase: Cocaine is withheld; lever pressing no longer delivers drug or cue.
- Reinstatement Test: After extinction, return to chamber and presentation of light cue alone.
- Measurement: Number of lever presses (drug-seeking) without cocaine reward.
- Outcome Measures:
- Behavioral: Lever presses during reinstatement.
- Molecular: BDNF levels, ERK activation, glutamate dynamics.
- Structural: Dendritic spine density via immunohistochemistry.
- Key Finding: Reinstatement strength increases with longer abstinence periods ("incubation effect") [26].
Major Depressive Disorder: Stress-Induced Atrophy and Impaired Rewiring
Depression manifests as a disorder of impaired neuroplasticity characterized by neuronal atrophy in specific cortical and limbic regions that control mood and emotion [106]. Chronic stress and elevated cortisol levels play a central role in suppressing plasticity processes in the hippocampus and prefrontal cortex while simultaneously promoting maladaptive plasticity in the amygdala.
The hypothalamic-pituitary-adrenal (HPA) axis dysregulation in depression leads to excessive glucocorticoid exposure, which exerts neurotoxic effects particularly in the hippocampus [106]. Preclinical studies demonstrate that glucocorticoids decrease apical dendritic branching of pyramidal cells and inhibit adult neurogenesis in the hippocampal dentate gyrus. Similar atrophic effects occur in the medial prefrontal cortex, where chronic stress induces debranching of dendritic arbors and loss of spine density [106]. These structural changes correlate with the cognitive deficits and emotional dysregulation characteristic of depression.
Conversely, depression is associated with evidence of maladaptive plasticity in the amygdala, where prolonged stress can induce development of dendritic spines and enhanced synaptic connectivity [106]. This negative neuroplasticity effect potentially underlies the persistent negative emotional rumination and enhanced fear learning observed in depressed patients. Additionally, default mode network (DMN) overactivation contributes to excessive self-referential thinking and negative rumination [106].
Experimental Protocol: Chronic Stress Model of Depression
- Objective: To investigate structural and functional plasticity changes following chronic stress.
- Subjects: Rodents (rats or mice).
- Stress Paradigms: Chronic restraint stress, chronic mild stress, or social defeat stress.
- Procedure:
- Stress Induction: Daily application of stressor for 2-6 weeks.
- Behavioral Testing: Sucrose preference (anhedonia), forced swim test (behavioral despair), elevated plus maze (anxiety).
- Tissue Collection: Perfusion fixation for morphological analysis.
- Histological Analysis: Golgi staining for dendritic arborization and spine density; immunohistochemistry for neurogenesis (BrdU/NeuN).
- Outcome Measures:
- Behavioral: Sucrose preference, immobility time, anxiety indices.
- Morphological: Dendritic length, branch points, spine density/density.
- Neurogenesis: Number of new neurons in dentate gyrus.
- Key Finding: Stress-induced dendritic atrophy in PFC and hippocampus; decreased neurogenesis; spine changes in amygdala [106].
Schizophrenia: Dysregulated Cortical Circuits and Synaptic Signaling
Schizophrenia involves profound disturbances in neuroplasticity that affect cortical microcircuits, particularly in the dorsolateral prefrontal cortex (DLPFC) [107] [108]. The core cognitive deficits of schizophrenia are associated with a range of molecular and morphological alterations that reflect impaired neuroplasticity in response to the underlying disease process.
A central theory posits NMDA receptor hypofunction as a key mechanism underlying aberrant LTP and LTD in schizophrenia [107]. Administration of NMDA receptor antagonists such as ketamine reproduces certain aspects of schizophrenia, including cognitive deficits and thought disorder. This NMDA receptor hypofunction disrupts the delicate balance between excitation and inhibition in cortical circuits, leading to both hypoglutamatergic and periodic hyperglutamatergic states [107].
GABAergic dysfunction represents another crucial component of plasticity deficits in schizophrenia. Postmortem studies reveal decreased density of GABAergic interneurons, particularly those containing parvalbumin, in multiple cortical regions along with alterations in glutamic acid decarboxylase (GAD67), the enzyme responsible for GABA synthesis [107] [108]. These GABAergic alterations likely contribute to abnormal gamma oscillations and impaired cognitive function.
Non-invasive brain stimulation (NIBS) techniques have provided direct evidence for impaired cortical plasticity in schizophrenia. Studies using repetitive transcranial magnetic stimulation (rTMS), paired-associative stimulation (PAS), and transcranial direct current stimulation (tDCS) consistently demonstrate deficits in both LTP-like and LTD-like plasticity in the motor cortex of schizophrenia patients [107]. These plasticity impairments are frequently associated with altered cortical inhibition and dysfunctional intracortical connectivity.
Experimental Protocol: Non-Invasive Brain Stimulation to Assess Cortical Plasticity
- Objective: To measure LTP-like and LTD-like plasticity in human motor cortex.
- Subjects: Schizophrenia patients and matched healthy controls.
- Stimulation Techniques:
- PAS: Paired associative stimulation (median nerve stimulation + TMS) to induce LTP-like plasticity.
- rTMS: Low-frequency (1 Hz) for LTD-like; high-frequency (≥5 Hz) for LTP-like.
- tDCS: Cathodal for LTD-like; anodal for LTP-like plasticity.
- Procedure:
- Baseline Measurement: Motor evoked potential (MEP) amplitude, resting motor threshold.
- Plasticity Induction: Application of specific NIBS protocol.
- Post-Stimulation: MEP measurements at 0, 15, 30, 60 minutes after intervention.
- Control Conditions: Sham stimulation sessions.
- Outcome Measures:
- MEP amplitude changes (% baseline).
- Resting motor threshold changes.
- Cortical silent period (GABAergic inhibition).
- Key Finding: Schizophrenia patients show deficient LTP-like and LTD-like plasticity [107].
Signaling Pathways in Neuroplasticity Deficits
Glutamatergic Signaling Pathway in Addiction
Figure 1: Glutamatergic Signaling Pathway in Addiction. This diagram illustrates how chronic drug exposure disrupts glutamate homeostasis in the nucleus accumbens, leading to synaptic and structural changes that promote drug-seeking behavior, and how N-acetylcysteine treatment can restore balance.
HPA Axis and Neuroplasticity in Depression
Figure 2: HPA Axis and Neuroplasticity in Depression. This diagram shows how chronic stress activates the HPA axis, leading to elevated cortisol that causes contrasting structural changes in hippocampus/PFC (atrophy) versus amygdala (hypertrophy), and how antidepressants promote recovery.
GABA-Glutamate Interaction in Schizophrenia
Figure 3: GABA-Glutamate Interaction in Schizophrenia. This diagram illustrates how NMDA receptor hypofunction leads to GABAergic interneuron dysfunction, creating excitation/inhibition imbalance that disrupts neural synchrony and contributes to cognitive deficits in schizophrenia.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Neuroplasticity Studies
| Reagent/Resource | Function/Application | Disorder Context |
|---|---|---|
| N-acetylcysteine | Precorder for cystine; restores glutamate homeostasis via cystine-glutamate exchange [26] | SUDs: Reduces cocaine seeking in reinstatement models |
| Ketamine | NMDA receptor antagonist; rapidly reverses behavioral deficits in depression models [106] | Depression: Study of fast-acting antidepressant mechanisms |
| D-amphetamine | Dopamine releaser; induces behavioral sensitization with repeated administration | SUDs: Models of stimulant addiction and cross-sensitization |
| Recombinant BDNF | Neurotrophic factor; promotes neuronal survival, differentiation, and synaptic plasticity | All disorders: Study of trophic factor effects on plasticity |
| Radiolabeled raclopride | D2/D3 receptor antagonist; measures dopamine release via PET displacement [26] | SUDs: Correlates craving with dopamine release in humans |
| Ceftriaxone | Antibiotic; increases glutamate transporter GLT-1 expression and glutamate uptake [26] | SUDs: Restores glutamate homeostasis and reduces reinstatement |
| Golgi-Cox stain | Histological method; visualizes complete neuronal morphology including dendritic spines | All disorders: Quantitative analysis of dendritic architecture |
| BrdU/NeuN labeling | Cell proliferation marker combined with neuronal marker; identifies newborn neurons | Depression: Measures adult hippocampal neurogenesis |
| Parvalbumin antibodies | Immunohistochemical marker for specific subclass of GABAergic interneurons | Schizophrenia: Quantification of cortical interneuron deficits |
| AAV vectors | Gene delivery; targeted manipulation of gene expression in specific brain regions | All disorders: Circuit-specific manipulation of plasticity genes |
Therapeutic Implications and Future Directions
The convergence of plasticity deficits across SUDs, depression, and schizophrenia suggests promising transdiagnostic therapeutic approaches. Interventions that target shared mechanisms of impaired neuroplasticity rather than disorder-specific symptoms may yield broader clinical efficacy. Several promising directions emerge from current research.
Pharmacological approaches that restore glutamate homeostasis show particular promise, especially for SUDs. The finding that N-acetylcysteine can reduce cocaine craving in human addicts represents a direct translation from animal models of glutamate dysregulation [26]. Similarly, the rapid antidepressant effects of ketamine, though acting initially through NMDA receptor blockade, appear to work through subsequent enhancement of synaptic plasticity and increased spine formation [106]. For schizophrenia, drugs that enhance NMDA receptor function or modulate glutamatergic signaling without causing excitotoxicity represent an active area of investigation.
Non-pharmacological approaches also leverage neuroplasticity mechanisms. Real-time functional magnetic resonance imaging (fMRI) biofeedback allows patients to learn voluntary regulation of brain circuits implicated in their disorders [26]. For depression, non-invasive brain stimulation techniques like repetitive transcranial magnetic stimulation (rTMS) and electroconvulsive therapy (ECT) demonstrate robust effects on neuroplasticity that correlate with clinical improvement [110]. Cognitive training interventions harness experience-dependent plasticity to strengthen alternative neural pathways that may compete with those engaged by pathology [109].
Recovery-oriented interventions emphasize that the same neuroplasticity that makes the brain vulnerable to addiction also enables healing, especially when internal and external conditions are supportive [5]. Longitudinal neuroimaging studies show structural recovery in frontal cortical regions, hippocampus, and cerebellum during sustained remission from SUDs, along with functional and neurochemical recovery in prefrontal cortical and subcortical regions [5]. This suggests that promoting new learning experiences and non-drug rewards can gradually reshape synaptic connectivity across affected circuits.
Future research should focus on developing biomarkers that can precisely quantify neuroplasticity deficits in individual patients, enabling personalized interventions targeting specific plasticity mechanisms. Additionally, optimizing the timing, duration, and combination of plasticity-enhancing interventions will be crucial for maximizing therapeutic outcomes. The integration of pharmacological and non-pharmacological approaches represents a particularly promising avenue, potentially creating synergistic effects on neuroplasticity that exceed the benefits of either approach alone.
SUDs, depression, and schizophrenia share fundamental disturbances in neuroplasticity mechanisms despite their distinct clinical presentations. Cross-disorder examination reveals common vulnerabilities in brain circuits governing reward, executive function, and emotional regulation, with overlapping alterations in glutamate, dopamine, and GABA systems. The detailed experimental methodologies and signaling pathways outlined in this whitepaper provide researchers with tools to investigate these shared mechanisms further. As our understanding of these transdiagnostic plasticity deficits deepens, we can develop more targeted interventions that address the root causes of these disorders rather than their surface manifestations. The ultimate goal is to harness the brain's inherent plastic capacity to restore function and promote recovery across the spectrum of psychiatric illness.
Conclusion
The intricate interplay between neuroplasticity and addiction reveals a dynamic brain system that can be steered toward both disease and recovery. The maladaptive plasticity underlying addiction is not a life sentence; the brain's inherent capacity for change provides a powerful foundation for healing. Future research must prioritize the development of objective, non-invasive biomarkers to precisely quantify plasticity states in patients. Furthermore, exploring the complex roles of neuroinflammation, gasotransmitters, and brain-body interactions opens exciting avenues for novel pharmacotherapies. A truly transformative path forward lies in developing integrated, personalized treatment regimens that combine targeted neuromodulation, pharmacotherapy, and behavioral interventions, all informed by a deep understanding of the individual's unique neuroplasticity profile. This synthesis of foundational knowledge and innovative application will ultimately empower the development of more effective and enduring solutions for substance use disorders.
References
- 1. The evolutionary origins and significance of drug addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1174878/]
- 2. Why our brains are wired for addiction : What the science says [https://med.stanford.edu/news/insights/2025/08/addiction-science-human-brain-ancient-wiring.html]
- 3. Strengthening Neuroplasticity in Substance Use Recovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11412380/]
- 4. Brain study increases understanding of what triggers drug ... [https://www.sciencedaily.com/releases/2025/04/250410160955.htm]
- 5. Advancing Recovery Research | National Institute on ... - NIDA [https://nida.nih.gov/about-nida/noras-blog/2025/06/advancing-recovery-research]
- 6. Exploring the Science of Neuroplasticity in Addiction Recovery [https://firstcitymentalhealthcenter.com/uncategorized/exploring-the-science-of-neuroplasticity-in-addiction-recovery/]
- 7. The Neuroscience of Drug Reward and Addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6890985/]
- 8. Neuroscience and addiction: Unraveling the brain's reward ... [https://lpsonline.sas.upenn.edu/features/neuroscience-and-addiction-unraveling-brains-reward-system]
- 9. Neuroscience: The Brain in Addiction and Recovery [https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/neuroscience-brain-addiction-and-recovery]
- 10. How an Addicted Brain Works | News [https://www.yalemedicine.org/news/how-an-addicted-brain-works]
- 11. Neuroplasticity: Brain Changes in Addiction [https://www.frontiersin.org/research-topics/68592/neuroplasticity-brain-changes-in-addictionundefined]
- 12. neuroplastic mechanisms underlying the therapeutic effect ... [https://pubmed.ncbi.nlm.nih.gov/41130352/]
- 13. How to Peer Review Quantitative Studies, Qualitative Studies, and... [https://link.springer.com/article/10.1007/s40429-024-00594-8]
- 14. Brain plasticity in drug addiction: Burden and benefit [https://www.health.harvard.edu/blog/brain-plasticity-in-drug-addiction-burden-and-benefit-2020062620479]
- 15. Neurobiology of addiction: a neurocircuitry analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6135092/]
- 16. Neurocircuitry of Addiction | Neuropsychopharmacology [https://www.nature.com/articles/npp2009110]
- 17. Neurobiology of Addiction - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK597351/]
- 18. The Brain Disease Model of Addiction [https://www.hazeldenbettyford.org/research-studies/addiction-research/brain-disease-model]
- 19. putative role for adult-born progenitors in promoting recovery [https://www.sciencedirect.com/science/article/abs/pii/S0166223611002025]
- 20. THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ... [https://www.ncbi.nlm.nih.gov/books/NBK424849/]
- 21. Liking, Wanting and the Incentive-Sensitization Theory of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5171207/]
- 22. The incentive sensitization theory of addiction: some current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2607325/]
- 23. Incentive Salience - an overview [https://www.sciencedirect.com/topics/neuroscience/incentive-salience]
- 24. Dopamine Circuit Mechanisms of Addiction-Like Behaviors [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2021.752420/full]
- 25. The Neuroscience of Habit and Purposeful Behavior [https://pmc.ncbi.nlm.nih.gov/articles/PMC6701929/]
- 26. Neuroplasticity in addictive disorders - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181920/]
- 27. Understanding the genetics and neurobiological pathways ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8014976/]
- 28. The Neuroscience of Change: Neuroplasticity [https://www.numberanalytics.com/blog/neuroplasticity-mechanisms-addiction-recovery]
- 29. High Content What? Deciphering between ... [https://blog.crownbio.com/differences-between-hci-hcs-hca]
- 30. HCA Platforms for Automated, Quantitative Analyses [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-76/hca-platforms-automated-quantitative-analyses.html]
- 31. SfN 2025 - High-Content Imaging Platforms for Assessing ... [https://www.sygnaturediscovery.com/publications/posters/high-content-imaging-platforms-for-assessing-neuroplasticity-in-early-stage-drug-discovery/]
- 32. Article High-content image-based pooled screens reveal ... [https://www.sciencedirect.com/science/article/pii/S2211124725006606]
- 33. A high-content image analysis approach for quantitative ... [https://www.nature.com/articles/s41598-017-06544-x]
- 34. Newly discovered brain pathway sheds light on addiction [https://www.rockefeller.edu/news/35742-newly-discovered-brain-pathway-sheds-light-on-addiction/]
- 35. Novel neurotherapeutic targets for substance use disorders [https://www.sciencedirect.com/science/article/pii/S187874792500248X]
- 36. The neuroplastic brain: current breakthroughs and ... [https://www.sciencedirect.com/science/article/pii/S0006899325002021]
- 37. Oxidative Stress and Neuroinflammation as a Pivot in Drug ... [https://www.mdpi.com/2076-3921/9/9/830]
- 38. Noninvasive Neuromodulation for Addiction (2025-2026) [https://bassconnections.duke.edu/project/noninvasive-neuromodulation-addiction-2025-2026/]
- 39. Novel therapeutic target and drug discovery for neurological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11903713/]
- 40. Drug Addiction as a Pathology of Staged Neuroplasticity [https://www.nature.com/articles/1301564]
- 41. Novel neurotherapeutic targets for substance use disorders [https://pubmed.ncbi.nlm.nih.gov/41193380/]
- 42. Myelination in the brain may be key to 'learning' opioid addiction [https://med.stanford.edu/news/all-news/2024/06/myelin-addiction.html]
- 43. Damaged Organs in Drug and Alcohol Abuse [https://bradfordhealth.com/damaged-organs-i-drug-alcohol/]
- 44. Quantitative proteome comparison of human hearts with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8084454/]
- 45. Comparative and Quantitative Global Proteomics Approaches [https://pmc.ncbi.nlm.nih.gov/articles/PMC5302699/]
- 46. A Review of Brain Stimulation Methods to Treat Substance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6034717/]
- 47. A systematic review and meta-analysis of neuromodulation ... [https://www.nature.com/articles/s41386-023-01776-0]
- 48. Invasive and Non-Invasive Neuromodulation for the Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294003/]
- 49. Emerging Interventions in Behavioral Addictions [https://www.mdpi.com/2076-3425/15/9/980]
- 50. Neuromodulation interventions for addictive disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC6059187/]
- 51. Neuromodulation for Treating Substance Use Disorders [https://www.addictionpolicy.org/post/neuromodulation-for-treating-substance-use-disorders]
- 52. Deep Transcranial Magnetic Stimulation Efficacy in ... [https://www.sciencedirect.com/science/article/pii/S2451902225001259]
- 53. Tuning brain networks: The emerging role of transcranial ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2022.945777/full]
- 54. Transcranial direct current stimulation induces long-term ... [https://www.nature.com/articles/s41398-020-01134-4]
- 55. Evidence of Neuroplastic Changes after Transcranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313265/]
- 56. GLP-1 Analogues in the Neurobiology of Addiction - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155186/]
- 57. Transformation 2.0: The GLP-1 RAs as Psychiatric ... [https://www.psychiatrictimes.com/view/transformation-2-0-the-glp-1-ras-as-psychiatric-medications]
- 58. Glucagon-like peptide-1 (GLP-1) and substance use ... [https://www.sciencedirect.com/science/article/pii/S1043661824002573]
- 59. Five things to know about GLP-1s and addiction [https://med.stanford.edu/news/insights/2025/04/ozempic-addiction-glp-1s-mounjaro-lembke.html]
- 60. Efficacy and safety of psilocybin for the treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763425001630]
- 61. Psilocybin: A breakthrough in mental health treatment or mere ... [https://news.yale.edu/2025/09/23/psilocybin-breakthrough-mental-health-treatment-or-mere-magical-thinking]
- 62. GLP-1 Drug Repurposing for Addiction Disorders ... [https://www.pharmexec.com/view/glp-1-drug-repurposing-addiction-disorders-hampered-high-costs-legal-hurdles]
- 63. Towards an understanding of psychedelic-induced ... [https://www.nature.com/articles/s41386-022-01389-z]
- 64. Advancing reduction of drug use as an endpoint in addiction ... [https://nida.nih.gov/about-nida/noras-blog/2025/03/advancing-reduction-drug-use-endpoint-in-addiction-treatment-trials]
- 65. Mechanisms of GLP-1 in Modulating Craving and Addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372146/]
- 66. The pharmacology of neuroplasticity induced by non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3487028/]
- 67. Self-Medication of Mental Health Problems - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC1361129/]
- 68. What Sobriety Means in 2025: Evidence-Based Recovery [https://recoverycentersofamerica.com/blogs/sobriety-in-2025-evidence-based-recovery/]
- 69. Research landscape analysis on dual diagnosis of substance ... [https://annals-general-psychiatry.biomedcentral.com/articles/10.1186/s12991-024-00517-x]
- 70. Synaptic plasticity and mental health: methods, challenges ... [https://www.nature.com/articles/s41386-022-01370-w]
- 71. Psychiatric comorbidity in substance use disorders, a ... [https://www.sciencedirect.com/science/article/pii/S0149763425003264]
- 72. Emerging neuromodulation treatments for opioid and ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1570555/full]
- 73. Optimizing stimulation parameters for anterior thalamic nuclei ... [https://pubmed.ncbi.nlm.nih.gov/40423665/]
- 74. Optimization of selective stimulation parameters for multi ... [https://pubmed.ncbi.nlm.nih.gov/23442372/]
- 75. optimizing stimulation parameters with vagus nerve ... [https://www.sciencedirect.com/science/article/pii/S1935861X25002670]
- 76. Time-adaptive bayesian optimization for neurostimulation [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1011674]
- 77. Making experimental data tables in the life sciences more FAIR [https://pmc.ncbi.nlm.nih.gov/articles/PMC7736789/]
- 78. The Role of Neuroplasticity in Overcoming Addiction [https://englishmountain.com/blog/neuroplasticity-addiction-recovery/]
- 79. The ancient origins of the addiction-prone mind [https://news.stanford.edu/stories/2025/08/addiction-brains-science-treatment-prevention-research]
- 80. How Deep Brain Stimulation Repairs Neural Pathways To ... [https://globalrph.com/2025/06/how-deep-brain-stimulation-repairs-neural-pathways-to-end-the-addiction-cycle/]
- 81. The future of addiction - Stanford Engineering [https://engineering.stanford.edu/news/future-addiction]
- 82. Psychosocial Supports in Medication -Assisted Treatment ... | ASPE [https://aspe.hhs.gov/reports/psychosocial-supports-medication-assisted-treatment-recent-evidence-current-practice-0]
- 83. of co-occurring mental illness and Integrated ... treatment addiction [https://pubmed.ncbi.nlm.nih.gov/15618940/]
- 84. How a neuroscientist rewired his brain to recover from addiction [https://www.statnews.com/2025/11/04/addiction-brain-healing-choice-neuroscience/]
- 85. Comparison of self-reported drug use with quantitative and ... [https://pubmed.ncbi.nlm.nih.gov/9243560/]
- 86. Discovering plasticity rules that organize and maintain neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11601609/]
- 87. Evolving interpretable plasticity for spiking networks [https://elifesciences.org/articles/66273]
- 88. Development of VEP-based biomarkers to assess plasticity ... [https://www.nature.com/articles/s41398-025-03676-x]
- 89. Noninvasive Biomarkers for Assessing the Excitatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590124/]
- 90. visual evoked potentials as a preclinical, quantitative... Validating [https://pmc.ncbi.nlm.nih.gov/articles/PMC10200282/]
- 91. Sex differences in attentional visual processing but not in ... [https://www.sciencedirect.com/science/article/pii/S030105112500153X]
- 92. Exploring the landscape of physical activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510986/]
- 93. Walking, Running, Swimming: An Analysis of the Effects ... [https://www.mdpi.com/1660-4601/19/23/16310]
- 94. Comparative analysis of land-based vs. water ... [https://pubmed.ncbi.nlm.nih.gov/39828772]
- 95. Identifying Neuroplasticity-related Biomarkers Linked With ... [https://pubmed.ncbi.nlm.nih.gov/40963395/]
- 96. Effect of a short-term water-based exercise program on ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1593969/full]
- 97. Exploring the Role of Neuroplasticity in Development, ... [https://www.mdpi.com/2076-3425/13/12/1610]
- 98. Development of VEP-based biomarkers to assess plasticity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537939/]
- 99. Rapid and cumulative adult plasticity in the mouse visual ... [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2025.1537305/full]
- 100. Forebrain neural progenitors effectively integrate into host ... [https://www.nature.com/articles/s41467-025-60187-5]
- 101. Mindfulness-based treatment of addiction: current state of the ... [https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-018-0115-3]
- 102. A randomized controlled trial of contingency management ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4242089/]
- 103. A comparison of contingency and... management [https://pubmed.ncbi.nlm.nih.gov/16445555/]
- 104. Behavioral Therapies for Drug Abuse - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3633201/]
- 105. Mindfulness‐based interventions for substance use disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC8527365/]
- 106. Neuroplasticity and depression: Rewiring the brain's networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8383338/]
- 107. A Review of Impaired Neuroplasticity in Schizophrenia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4810231/]
- 108. Neuroplasticity of Neocortical Circuits in Schizophrenia [https://www.nature.com/articles/1301563]
- 109. Neuroplastic and cognitive impairment in substance use ... [https://www.sciencedirect.com/science/article/abs/pii/S014976341830294X]
- 110. Changes in Neural Activities and Neuroplasticity Related to ... [https://www.sciencedirect.com/science/article/pii/S2667174325001260]