Neurobiological Mechanisms of Addiction Relapse Vulnerability: From Neural Circuits to Clinical Biomarkers
This article synthesizes current research on the neurobiological underpinnings of addiction relapse vulnerability, addressing the needs of researchers and drug development professionals.
Neurobiological Mechanisms of Addiction Relapse Vulnerability: From Neural Circuits to Clinical Biomarkers
Abstract
This article synthesizes current research on the neurobiological underpinnings of addiction relapse vulnerability, addressing the needs of researchers and drug development professionals. It explores the foundational neural circuits and neuroadaptations in the binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation stages of addiction. The content details methodological approaches for identifying biomarkers, including neuroimaging and stress response measures, and investigates troubleshooting strategies for high-relapse-risk populations by targeting immune and stress systems. Finally, it validates and compares predictive models and emerging pharmacological targets, providing a comprehensive resource for developing novel, mechanism-based relapse prevention therapies.
Core Neurocircuitry and Lasting Neuroadaptations in Relapse Vulnerability
Addiction is a chronically relapsing disorder characterized by a compulsive cycle of drug seeking and taking, loss of control over intake, and emergence of a negative emotional state during withdrawal [1] [2]. The contemporary understanding of addiction has evolved from historical conceptualizations of moral failure to a medical model based on well-defined neurobiological mechanisms [3] [4]. This transition in understanding is supported by extensive evidence showing that addiction produces dramatic, long-lasting changes in brain function that reduce an individual's ability to control substance use [4]. The three-stage cycle of addiction—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—provides a heuristic framework for investigating the neurobiological underpinnings of relapse vulnerability [3] [1] [5]. This cycle worsens over time, involves neuroplastic changes in brain reward, stress, and executive function systems, and creates a self-perpetuating mechanism that drives relapse even after prolonged abstinence [5] [2]. The delineation of this cycle has transformed research approaches, shifting focus from acute drug effects to the chronic neuroadaptations that underlie the transition from controlled use to addiction and persistent relapse vulnerability [1] [4].
The Binge/Intoxication Stage: Neural Substrates of Reward and Habit Formation
The binge/intoxication stage is primarily mediated by the basal ganglia, with key roles for the nucleus accumbens (ventral striatum) and dorsal striatum [3] [5] [6]. During this stage, all addictive substances directly or indirectly increase dopamine transmission in the nucleus accumbens, producing the rewarding effects that positively reinforce drug use [3] [7]. The mesolimbic dopamine pathway, originating in the ventral tegmental area (VTA) and projecting to the nucleus accumbens, serves as a common neural substrate for the acute rewarding effects of all major classes of addictive drugs [1] [5]. Stimulant drugs such as amphetamines and cocaine directly increase dopaminergic transmission, whereas opioids, alcohol, and nicotine indirectly facilitate dopamine release by inhibiting GABAergic interneurons in the VTA, thereby disinhibiting dopamine neurons [7].
As addiction progresses, a fundamental neurobiological shift occurs from voluntary drug use to habitual and ultimately compulsive drug seeking [1] [5]. This transition involves a transfer of behavioral control from the ventral to the dorsal striatum, particularly strengthening the nigrostriatal pathway that controls habitual motor function and behavior [3]. This neural reorganization underlies the development of incentive salience, whereby drug-associated cues (people, places, paraphernalia) themselves begin to elicit dopamine release and motivate drug-seeking behavior, even before the drug is consumed [3] [1]. This phenomenon helps explain the powerful role of conditioned cues in triggering relapse [3].
Table 1: Key Neurotransmitter Systems in the Binge/Intoxication Stage
| Neurotransmitter/Neuromodulator | Direction of Change | Primary Brain Regions | Functional Consequences |
|---|---|---|---|
| Dopamine | Increase [5] | Ventral striatum, dorsal striatum [3] | Reward, reinforcement, habit formation [3] |
| Opioid peptides | Increase [5] | Nucleus accumbens, VTA [6] | Pleasure, reward enhancement [6] |
| GABA | Increase [5] | VTA, nucleus accumbens [7] | Modulation of dopamine neuron activity [7] |
| Endocannabinoids | Increase [7] | VTA, nucleus accumbens [7] | Modulation of reward signaling [7] |
The Withdrawal/Negative Affect Stage: Recruitment of Brain Stress Systems
The withdrawal/negative affect stage is characterized by the emergence of a negative emotional state—including dysphoria, anxiety, irritability, and physical discomfort—when drug use is discontinued [3] [1]. This stage primarily involves the extended amygdala, a macrostructure comprising the bed nucleus of the stria terminalis (BNST), central nucleus of the amygdala (CeA), and a transition zone in the medial portion of the nucleus accumbens (shell) [3] [5]. This stage represents a critical shift in the motivation for drug use from positive reinforcement (seeking pleasure) to negative reinforcement (seeking relief from discomfort) [1] [2].
Two major neuroadaptations characterize this stage: within-system changes in reward circuitry and between-system recruitment of brain stress systems [3]. Chronic drug exposure leads to a decrease in dopaminergic tone in the nucleus accumbens and a shift in the glutamatergic-GABAergic balance toward increased glutamatergic tone, resulting in diminished euphoria from the drug, reduced tolerance for stress, and decreased responsiveness to natural rewards [3]. Simultaneously, the brain's "anti-reward" system becomes upregulated, leading to increased release of stress mediators including corticotropin-releasing factor (CRF), dynorphin, norepinephrine, and orexin (hypocretin), with concomitant positive modulation of the hypothalamic-pituitary-adrenal (HPA) axis [3] [5].
The brain possesses inherent buffer systems to counterbalance this anti-reward system, including cannabinoid (CB1), nociceptin, and neuropeptide Y neurotransmission [3]. alterations in these buffering systems may further increase addiction vulnerability, as evidenced by findings of decreased CB1 receptor density in individuals with alcohol use disorder [3]. The clinical manifestation of these neuroadaptations includes irritability, anxiety, dysphoria, and a general state of psychological and physical distress that powerfully motivates renewed drug use through negative reinforcement mechanisms [3] [1].
Table 2: Key Neurotransmitter Systems in the Withdrawal/Negative Affect Stage
| Neurotransmitter/Neuromodulator | Direction of Change | Primary Brain Regions | Functional Consequences |
|---|---|---|---|
| Corticotropin-releasing factor (CRF) | Increase [5] | Extended amygdala [5] | Stress response, anxiety [3] |
| Dynorphin | Increase [5] | Extended amygdala [5] | Dysphoria, aversive state [5] |
| Norepinephrine | Increase [5] | Extended amygdala [5] | Arousal, stress response [3] |
| Dopamine | Decrease [5] | Nucleus accumbens [3] | Anhedonia, reduced reward [3] |
| Endocannabinoids | Decrease [5] | Extended amygdala [3] | Reduced buffering of stress [3] |
| Neuropeptide Y | Decrease [5] | Extended amygdala [3] | Reduced buffering of stress [3] |
The Preoccupation/Anticipation Stage: Neural Circuits of Craving and Executive Dysfunction
The preoccupation/anticipation stage, characterized by intense craving and loss of cognitive control over drug seeking, primarily involves the prefrontal cortex (PFC) and its connections with the basal ganglia and extended amygdala [3] [5] [2]. This stage represents a critical domain of executive function that includes the ability to organize thoughts and activities, prioritize tasks, manage time, make decisions, and regulate emotions and impulses [4]. In addiction, these regulatory capacities become compromised, leading to the intense preoccupation with drug seeking and diminished ability to resist urges that characterize craving [3] [2].
Researchers have conceptualized two systems within the PFC that contribute to this stage: a "Go system" and a "Stop system" [3]. The Go system, involving the dorsolateral prefrontal cortex and anterior cingulate, is responsible for attention and planning of goal-directed behaviors, including drug seeking [3]. The Stop system is critical for inhibitory control and the ability to suppress maladaptive behaviors such as drug use [3]. In addiction, the balance between these systems becomes disrupted, with hyperactivity in the Go system combined with hypoactivity in the Stop system, resulting in compulsivity and impaired impulse control [3] [5].
The neurochemistry of this stage involves increased glutamatergic transmission from the prefrontal cortex to the nucleus accumbens and other reward-related regions, which drives drug-seeking behavior [5]. Additionally, dopamine, CRF, and orexin systems contribute to the craving state [5]. The persistent vulnerability to relapse characteristic of addiction is thought to stem from long-lasting neuroadaptations in these prefrontal circuits that endure long after acute withdrawal has subsided [4]. Human imaging studies have consistently shown that individuals with substance use disorders exhibit reduced activity in the prefrontal regions responsible for executive control, combined with heightened responsivity of reward and emotional circuits to drug-related cues [2] [4].
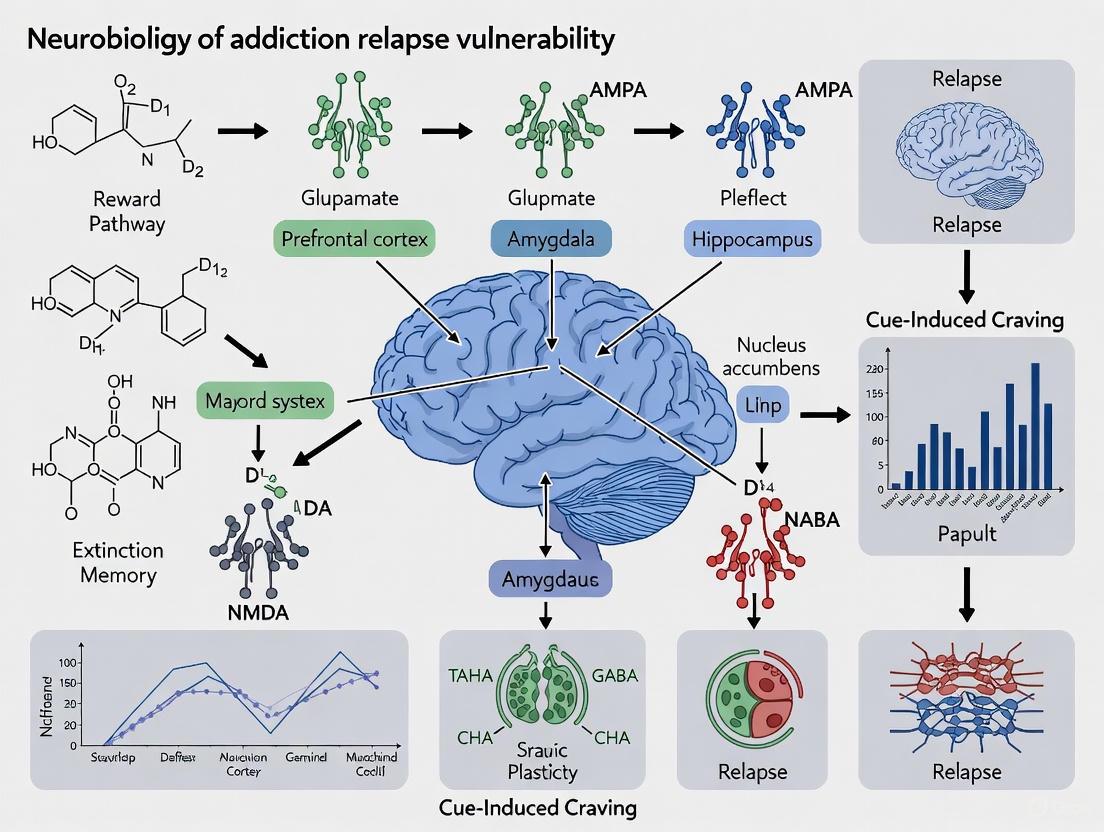
Figure 1: Neural circuitry of the preoccupation/anticipation stage of addiction
Molecular and Cellular Mechanisms of Relapse Vulnerability
The transition through the addiction cycle produces enduring molecular and cellular adaptations that create persistent relapse vulnerability. Key among these adaptations are changes in transcription factors, signaling molecules, and synaptic plasticity mechanisms that alter neural circuit function [5] [7]. Chronic exposure to drugs of abuse induces ΔFosB accumulation in the nucleus accumbens, a transcription factor that promotes increased behavioral responses to drugs and enhances dendritic arborization, potentially strengthening drug-related memories and cues [7]. Conversely, reductions in CREB (cAMP response element-binding protein) in the nucleus accumbens similarly increase behavioral responses to drugs [7].
The brain-derived neurotrophic factor (BDNF) system plays a complex role in relapse vulnerability. As BDNF accumulates, it appears to increase the incubation period of relapse [7]. Additionally, chronic drug exposure produces hyperresponsiveness of the CRF system through increased CREB-mediated gene function, leading to heightened stress reactivity [7]. The hypofrontality observed in addiction involves molecular changes including increased CREB and a shift from dopamine D2 to D1 receptor prevalence mediated by increased expression of ASG3 and cystine-glutamate transporters, contributing to impulsivity and compulsivity [7].
At the synaptic level, drugs of abuse induce long-term potentiation (LTP) in the VTA-nucleus accumbens system, creating persistent hypersensitization to drugs and drug-associated cues [7]. This includes increased expression of glutamate receptor subunit GluR1 in the VTA, increased tyrosine hydroxylase (the rate-limiting enzyme in dopamine synthesis), and alterations in intracellular signaling cascades [7]. These molecular and cellular adaptations collectively create a brain state characterized by heightened sensitivity to drugs and cues, reduced sensitivity to natural rewards, compromised stress regulation, and impaired executive control—establishing a biological basis for persistent relapse vulnerability that can endure for years after drug cessation [5] [4].
Experimental Approaches and Methodologies
Animal Models of the Addiction Cycle
Animal models have been indispensable for elucidating the neurobiological mechanisms underlying the three-stage addiction cycle [1] [5]. These models permit investigations of specific behavioral and neurobiological phenomena under highly controlled conditions that would be impossible or unethical to replicate in humans [4]. Modern animal models take advantage of individual and strain diversity in drug responses, incorporate complex environments with access to alternative reinforcers, and test effects of stressful stimuli, allowing investigation of neurobiological processes underlying addiction risk and environmental resilience factors [5]. These models have been developed to specifically capture features of the binge/intoxication stage (e.g., drug self-administration), withdrawal/negative affect stage (e.g., intracranial self-stimulation thresholds), and preoccupation/anticipation stage (e.g., cue-induced reinstatement of drug seeking) [1].
Human Neuroimaging Studies
Human neuroimaging studies, particularly using functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), have provided critical insights into the human brain alterations associated with addiction and relapse [8] [4]. Resting-state fMRI (rs-fMRI) measures such as regional homogeneity (ReHo) and fractional amplitude of low-frequency fluctuation (fALFF) have proven effective in characterizing localized neural activity alterations associated with addiction [8]. These approaches allow researchers to identify functional abnormalities in specific brain regions and circuits that correlate with relapse vulnerability.
A recent longitudinal study investigating methamphetamine relapse utilized rs-fMRI to compare brain activity in abstinent methamphetamine-dependent individuals (MADIs) who subsequently relapsed, the same individuals after relapse, and healthy controls [8]. The study collected MRI data using a 3.0 Tesla Siemens scanner with T1-weighted structural parameters (repetition time TR = 1900ms; echo time TE = 2.48ms; flip angle FA = 9°; field of view FOV = 250×250mm; slice thickness = 1mm) and rs-fMRI parameters (TR/TE = 3000/40ms; FA = 90°; FOV = 240×240mm; slice thickness = 4mm; volumes = 133) [8]. Data preprocessing was conducted using Data Processing and Analysis for Brain Imaging (DPABI) software in MATLAB, including format conversion, removal of initial time points, slice timing, realignment, T1 reorientation, brain extraction, segmentation, and normalization [8]. Participants with head motion exceeding 2.0mm or rotation greater than 2.0° were excluded to minimize motion artifacts [8].
This study found that MADIs at Stage I (abstinence) demonstrated decreased brain activity in cortical regions and increased activity in subcortical regions, particularly the bilateral putamen [8]. After relapse (Stage II), individuals exhibited more widespread abnormalities, with decreased activity in the middle cingulate gyrus, parietal and occipital regions, and increased activity in subcortical regions (striatum, thalamus, hippocampal structure) and several prefrontal regions [8]. Importantly, fALFF values in the left and right caudate nucleus were negatively associated with duration of relapse, suggesting that increased activity in these regions might be associated with early relapse in abstinent individuals [8].
Figure 2: Experimental workflow for neuroimaging study of relapse prediction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Investigating the Addiction Cycle
| Research Tool Category | Specific Examples | Research Applications |
|---|---|---|
| Animal Models | Rat/mouse self-administration [1] [5], Conditioned place preference [1], Behavioral sensitization [1] | Modeling specific stages of addiction cycle, Investigating neuroadaptations, Testing pharmacological treatments |
| Genetic Manipulation Tools | Knockout/knockin models [5] [7], CRISPR-Cas9 systems [5], RNA interference techniques [5] | Identifying gene functions in addiction vulnerability, Studying molecular mechanisms, Validating drug targets |
| Neuroimaging Approaches | Functional MRI (fMRI) [8] [4], Positron emission tomography (PET) [4], Regional homogeneity (ReHo) [8], fractional ALFF (fALFF) [8] | Mapping brain activity changes in humans, Identifying relapse predictors, Tracking treatment effects |
| Neurochemical Assays | Microdialysis [1], Fast-scan cyclic voltammetry [1], Receptor autoradiography [1] | Measuring neurotransmitter dynamics, Assessing receptor changes, Characterizing drug effects |
| Molecular Biology Reagents | Antibodies for ΔFosB, CREB, BDNF [7], PCR assays for gene expression [7], Protein quantification kits [7] | Quantifying molecular adaptations, Measuring signaling pathway changes, Assessing neuroplasticity |
Implications for Therapeutic Development and Future Research
The three-stage model provides a comprehensive neurobiological framework for developing targeted interventions for substance use disorders [3] [5]. By identifying specific neural circuits, neurotransmitters, and molecular mechanisms involved in each stage, this model enables a more precise approach to medication development [5] [4]. For example, medications targeting the binge/intoxication stage might focus on blocking the rewarding effects of drugs or mitigating the development of incentive salience, while interventions for the withdrawal/negative affect stage could aim to normalize stress system dysregulation and restore hedonic balance [3] [5]. Treatments addressing the preoccupation/anticipation stage might focus on enhancing prefrontal cortical function to improve executive control and reduce craving [3] [2].
Future research directions should include further delineation of the molecular and cellular adaptations that persist during extended abstinence, investigation of individual differences in vulnerability to addiction, exploration of developmental influences (particularly adolescence as a critical risk period), and examination of gender differences in addiction neurobiology [5] [4]. Additionally, research is needed to understand the neurobiological mechanisms underlying the high comorbidity between substance use disorders and other psychiatric conditions [4]. The continued integration of animal and human studies, leveraging increasingly sophisticated technologies and methodologies, will be essential for translating this knowledge into more effective prevention and treatment strategies for substance use disorders [4].
Addiction is a chronic relapsing disorder characterized by compulsive drug seeking despite adverse consequences, rooted in specific neurobiological adaptations. The brain's dopamine systems, particularly those governing incentive salience, undergo profound changes during the transition from casual drug use to addiction. The mesolimbic dopamine pathway, originating in the ventral tegmental area (VTA) and projecting to the nucleus accumbens (NAc), is fundamentally implicated in reward processing, motivation, and reinforcement learning [9]. Drugs of abuse commandeer this evolutionary conserved system, artificially stimulating dopamine release at magnitudes far exceeding those produced by natural rewards [9]. This surfeit triggers a cascade of neuroadaptations that ultimately result in a hypodopaminergic state, characterized by blunted reward circuit responsiveness and a heightened vulnerability to relapse [10].
The concept of incentive salience explains how drugs transform neutral environmental stimuli into potent cues that trigger overwhelming craving. Dopamine does not merely encode pleasure ("liking") but assigns motivational significance ("wanting") to reward-predictive cues [10]. In addiction, this process becomes pathologically skewed, whereby drug-associated cues garner excessive incentive salience, dominating attentional resources and motivating drug-seeking behavior, even when the drug itself is no longer pleasurable [9]. This review examines the neurobiological mechanisms through which dopamine systems and incentive salience processes are hijacked, creating a persistent state of relapse vulnerability.
Neurobiological Mechanisms of Hijacked Incentive Salience
Dopamine Signaling Alterations in Addiction
Chronic drug use induces significant and persistent alterations in dopamine neurotransmission, which underlie the core symptoms of addiction.
- Acute Drug Effects: Different classes of drugs converge on the common pathway of increasing dopamine concentrations in the NAc, though through distinct mechanisms [9]. Psychostimulants like cocaine and amphetamine directly target dopamine transmission: cocaine blocks the dopamine reuptake transporter (DAT), prolonging dopamine presence in the synaptic cleft, while amphetamine increases dopamine release and blocks reuptake [9]. Opioids, conversely, indirectly increase dopamine release by inhibiting GABAergic interneurons in the VTA, thus disinhibiting dopamine neurons [9].
- Chronic Adaptations: With repeated drug exposure, the dopamine system undergoes compensatory changes. These include decreased baseline dopamine levels, reduced dopamine receptor density (particularly D2 receptors), and diminished dopamine receptor sensitivity [9] [10]. This leads to a functional dopamine deficit in the reward circuit, manifesting clinically as anhedonia (inability to feel pleasure from natural rewards) and increased drug-seeking to restore dopamine levels [10].
- Incentive Salience and Prediction Error: Dopamine neurons code for reward prediction error (RPE)—the difference between expected and actual reward [9]. An unexpected reward triggers a phasic dopamine burst, promoting learning. Drugs of abuse cause a massive, unexpected dopamine release, creating a powerful learning signal that solidifies drug-taking behavior. Over time, as drug use becomes predictable, dopamine responses shift to the drug-predictive cues themselves [9]. This is the neural basis of cue-triggered craving; the cues themselves acquire excessive incentive salience, driving compulsive drug-seeking.
Table 1: Dopamine System Alterations in Addiction
| Phase | Dopamine Signaling | Receptor Changes | Behavioral Manifestation |
|---|---|---|---|
| Acute Use | Strong increase in NAc dopamine; magnitude exceeds natural rewards [9] | Transient activation of D1 and D2 receptors [9] | Intense euphoria ("high"); reinforcement of drug-taking action |
| Chronic Use | Decreased baseline dopamine levels; blunted phasic responses [9] [10] | Downregulation and reduced sensitivity of D2 receptors in the striatum [9] [10] | Anhedonia; tolerance; escalation of drug intake |
| Cue Exposure | Dopamine response shifts from drug to drug-predictive cues [9] | Altered signaling in cue-processing pathways [9] | Intense craving; compulsive drug-seeking triggered by cues |
Neuroadaptations, Allostasis, and Relapse Vulnerability
The chronic dysregulation of the dopamine system is part of a broader pattern of allostatic neuroadaptations—persistent changes in brain reward and stress systems that maintain stability at a pathological set-point [9] [11].
- Molecular and Structural Plasticity: Long-term drug use induces neuroplastic changes in the dopamine system and associated circuits. This includes altered gene expression, such as the accumulation of the transcription factor ΔFosB, and synaptic remodeling, like changes in dendritic spine density in the NAc and prefrontal cortex [9]. These changes underlie the long-lasting nature of addiction and the persistence of relapse vulnerability.
- Beyond Dopamine: The Anti-Reward System: The allostatic model of addiction posits that chronic drug use not only dysregates reward circuits (dopamine) but also engages a coordinated "anti-reward" system involving the extended amygdala [11]. This system, which includes the central amygdala (CeA) and bed nucleus of the stria terminalis (BNST), is rich in stress neurotransmitters like corticotropin-releasing factor (CRF) and dynorphin. Its activation produces negative emotional states (dysphoria, anxiety, irritability), especially during withdrawal. The HPA axis and glucocorticoids are also dysregulated, further fueling the stress and negative affect that drives relapse via negative reinforcement [11].
- Emotional Dysregulation as a Relapse Driver: A critical driver of relapse is emotional dysregulation during the withdrawal/negative affect stage [12]. Neuroimaging studies reveal that individuals with substance dependence show altered brain responses to negative emotional stimuli in regions like the amygdala, insula, anterior cingulate cortex (ACC), and medial prefrontal cortex (mPFC) [12]. For example, alcohol dependence is often associated with blunted activation to negative affective stimuli, while cocaine dependence shows heightened activation. This dysregulation in negative emotional processing is a key contributor to the chronic relapsing nature of addiction [12].
Table 2: Key Neuroadaptations Contributing to Relapse Vulnerability
| Adaptation Type | Key Brain Regions/Systems | Neurochemical/Neural Changes | Contribution to Relapse |
|---|---|---|---|
| Allostatic Reward | Mesolimbic Dopamine Pathway, NAc | Reduced baseline dopamine, D2 receptor downregulation [9] [10] | Anhedonia; drug seeking to relieve dopamine deficit |
| Stress System Engagement | Extended Amygdala, HPA Axis | Increased CRF, Dynorphin; Glucocorticoid dysregulation [11] | Negative emotional state (hyperkatifeia); anxiety and dysphoria [12] |
| Executive Function Deficit | Prefrontal Cortex (PFC) | Hypoactivity in dorsolateral PFC, anterior cingulate [9] [11] | Loss of impulse control; impaired decision-making; craving |
| Synaptic Remodeling | NAc, PFC | Altered gene expression (e.g., ΔFosB), changes in dendritic spines [9] | Long-term persistence of addictive behaviors and cue-reactivity |
Experimental Approaches and Methodologies
Probing Dopamine and Policy Learning in Behavioral Models
Recent research utilizing precise behavioral tracking in mice has provided evidence that mesolimbic dopamine regulates the rate of learning from action—a process central to how drug-seeking habits are formed.
Experimental Protocol:
- Subject & Preparation: Naive, head-restrained mice are acclimated to head fixation without prior behavioral shaping [13].
- Behavioral Paradigm: Mice are trained in a classical trace conditioning paradigm. An auditory cue (0.5-s tone) is presented, followed by a 1-s delay, after which a sweetened water reward is delivered irrespective of the animal's behavior [13].
- Data Acquisition: A comprehensive dataset of orofacial and body movements is collected using an accelerometer and high-resolution video to infer lick rate, whisking, pupil diameter, and nose motion [13].
- Analysis of Learning: Behavioral policies are analyzed by measuring two dissociable components: preparatory behavior (activity during the delay period) and reactive behavior (latency to initiate movement following reward delivery). The evolution of these policies is tracked as mice learn to minimize reward collection latency [13].
- Dopamine Manipulation & Measurement: Fiber photometry is used to record dopamine neuron activity in the VTA continuously throughout learning. In separate experiments, closed-loop optogenetic manipulations of VTA dopamine neurons are performed, calibrated to physiological signals, to test causal roles [13].
Key Findings: This approach demonstrated that individual differences in initial phasic dopamine responses correlated with the emergence of a learned behavioral policy, but not with value encoding for a predictive cue. Manipulations of mesolimbic dopamine produced effects consistent with it setting an adaptive learning rate for direct policy learning, rather than solely providing a reward prediction error signal [13]. This expands dopamine's role beyond value learning to directly shaping how actions are optimized, a critical mechanism in the development of compulsive drug-seeking policies.
Investigating Emotional Dysregulation in Human Addiction
Functional magnetic resonance imaging (fMRI) is used to characterize emotional dysregulation, a critical driver of relapse, in individuals with substance dependence.
Experimental Protocol:
- Participant Groups: Individuals with alcohol, cocaine, opioid, or cannabis dependence (typically during early abstinence or treatment) are compared with matched healthy controls [12].
- fMRI Tasks:
- Facial Emotion Processing: Participants view images of emotional faces (e.g., fearful, angry, sad) and neutral faces while undergoing fMRI. They may be asked to identify the emotion or passively view the images [12].
- Aversive Stimuli Exposure: Participants are exposed to generally aversive images (e.g., from the International Affective Picture System) or to individualized stressful experience cues (script-guided imagery of personal stressful events) [12].
- Emotion Regulation: Active tasks where participants are instructed to employ conscious strategies, such as reappraisal, to regulate their emotional response to negative images [12].
- Data Analysis: Blood-oxygen-level-dependent (BOLD) responses are compared between groups and task conditions. Key regions of interest include the amygdala, insula, ACC, and mPFC. Functional connectivity between these regions may also be analyzed [12].
Key Findings: This methodology has revealed substance-specific patterns of emotional dysregulation. For instance, individuals with alcohol dependence often show blunted activation in the ACC, insula, and amygdala in response to negative emotional stimuli. Conversely, those with cocaine dependence may show heightened activation in these regions [12]. These neural response patterns are associated with clinical outcomes, such as treatment success and relapse vulnerability.
Diagram 1: Hijacked dopamine pathway in addiction.
Diagram 2: Relapse vulnerability pathways.
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Reagents and Methodologies
| Reagent / Model / Method | Function / Purpose in Addiction Research |
|---|---|
| Fibre Photometry | A technique for recording neural activity in real-time, used to measure calcium or neurotransmitter dynamics (e.g., dopamine) in specific brain circuits like the VTA-NAc pathway during behavior [13]. |
| Optogenetics | Allows for precise, millisecond-timescale control of specific neuronal populations (e.g., VTA dopamine neurons) using light, enabling causal tests of their role in drug-related behaviors and learning [13]. |
| fMRI with Emotional Tasks | Used in human subjects to map brain reactivity and functional connectivity during emotional processing, revealing dysregulation in amygdala, insula, and PFC circuits associated with relapse risk [12]. |
| Trace Conditioning Paradigm | A behavioral task used in rodents to dissociate the learning of preparatory and reactive behavioral policies, allowing investigation of how dopamine regulates the rate of learning from action [13]. |
| White Matter Neurotransmitter Atlas | A novel MRI-based atlas mapping neurotransmitter circuits (dopamine, acetylcholine, etc.) in white matter, enabling investigation of how lesions or diseases disrupt neurochemical balance and cognitive function [14]. |
| Self-Administration Model | The gold-standard rodent model of addiction, where animals perform an operant response (e.g., pressing a lever) to receive an intravenous drug infusion, modeling human drug-taking and relapse [9]. |
| Mathematical Models of Relapse | Computational models (e.g., using Ornstein-Uhlenbeck and Poisson processes) that incorporate psychological concepts to predict how life events and cues influence relapse probability [15]. |
The hijacking of dopamine systems and the consequent pathological attribution of incentive salience to drug cues create a powerful engine for addiction maintenance and relapse. The transition from controlled use to compulsive drug-seeking is mediated by a cascade of allostatic neuroadaptations that produce a chronic dopamine deficit, engange stress systems, and impair prefrontal control. The interplay between this hijacked reward pathway and emotional dysregulation forms a core mechanism of relapse vulnerability.
Future research must continue to integrate findings across scales, from molecular and cellular adaptations to circuit-level dysfunction and individual behavioral phenotypes. Promising avenues include:
- Further elucidating the role of dopamine in direct policy learning and how this process becomes rigid and habit-like in addiction [13].
- Developing a more precise characterization of emotional dysregulation subtypes across different substance use disorders to inform targeted neuromodulation therapies [12].
- Leveraging computational psychiatry approaches and human neurotransmitter atlases to create personalized models of relapse risk and novel treatment interventions [15] [14].
Addressing the multifaceted neurobiology of addiction, with the hijacked dopamine system at its core, is paramount for developing effective therapeutic strategies that can prevent relapse and promote long-term recovery.
Drug addiction is conceptualized as a chronic, relapsing disorder characterized by a compulsion to seek and take drugs, loss of control over intake, and emergence of a negative emotional state (e.g., dysphoria, anxiety, irritability) when access to the drug is prevented. This negative emotional state reflects what has been termed motivational withdrawal and forms a core component of addiction [16]. The disorder progresses through a three-stage cycle (binging/intoxication, withdrawal/negative affect, and preoccupation/anticipation) that intensifies over time and shifts from positive reinforcement to negative reinforcement mechanisms [3].
The anti-reward system represents a conceptual framework for understanding the neurobiological basis of the negative emotional state in addiction. This system is based on the hypothesis that the brain contains counter-adaptive mechanisms that oppose reward signaling, termed "anti-reward" systems [16] [17]. While reward systems are activated by acute drug administration, chronic drug use leads to recruitment of anti-reward systems that drive aversive states. The neuroanatomical substrate for this anti-reward system is primarily located within the extended amygdala, which plays a key role in the negative reinforcement that perpetuates addictive behavior [16] [3].
Table 1: Key Characteristics of Reward vs. Anti-Reward Systems in Addiction
| Feature | Reward System | Anti-Reward System |
|---|---|---|
| Primary Function | Mediates positive reinforcement | Mediates negative reinforcement |
| Dominant Neurotransmitters | Dopamine, opioid peptides, GABA | CRF, norepinephrine, dynorphin |
| Key Brain Regions | Ventral striatum, nucleus accumbens, ventral tegmental area | Extended amygdala (BNST, CeA, NAcc shell) |
| Temporal Activation | Early stage addiction | Late stage addiction |
| Behavioral Manifestation | Drug seeking for positive effects | Drug seeking to relieve negative affect |
Neuroanatomy of the Extended Amygdala
Structural Components
The extended amygdala is composed of several interconnected structures that share certain cytoarchitectural and circuitry similarities [16]. The primary components include:
- Bed nucleus of the stria terminalis (BNST): Serves as a crucial interface between the amygdala and hypothalamic-pituitary-adrenal axis, playing a key role in stress and anxiety responses [3].
- Central nucleus of the amygdala (CeA): Functions as a principal output nucleus of the amygdala complex and is critically involved in physiological responses to stressors and drug-related stimuli [18].
- Transition zone in the medial subregion of the nucleus accumbens (shell of the NAcc): Represents a bridge between reward and stress systems, integrating motivational information [16].
This macrostructure receives abundant afferents from limbic structures such as the basolateral amygdala and hippocampus, and sends efferents to the medial part of the ventral pallidum and lateral hypothalamus, thereby interfacing classical limbic (emotional) structures with the extrapyramidal motor system [16].
Functional Neurocircuitry
The extended amygdala operates as an integrated functional unit despite its spatially separate components. It represents a critical point of convergence for sensory information from cortical and subcortical regions, enabling it to assess the emotional and motivational significance of stimuli [18]. The basolateral amygdala has a particularly important role in mediating the motivational effects of stimuli previously paired with drug seeking and drug motivational withdrawal, serving as a key node for emotional memories in general [16].
The functional connectivity of the extended amygdala is illustrated in the following diagram, which shows the primary input and output pathways:
Figure 1: Extended Amygdala Neural Circuitry
Neurochemical Substrates of the Anti-Reward System
Primary Neurotransmitter Systems
The neurochemical basis of anti-reward function within the extended amygdala involves several key neurotransmitter systems that are recruited during chronic drug exposure, producing aversive or stress-like states during withdrawal [16]:
- Corticotropin-releasing factor (CRF): Serves as a primary mediator of stress responses, with increased signaling in the extended amygdala during drug withdrawal [16] [3].
- Norepinephrine (NE): Contributes to arousal, anxiety, and stress responses, with enhanced release during withdrawal states [16].
- Dynorphin: An endogenous opioid that acts on kappa-opioid receptors to produce dysphoric effects, opposing the rewarding effects of mu-opioid receptor activation [3] [19].
These neurochemical systems form a complex, buffered system for maintaining hedonic homeostasis. Their activation creates a powerful negative emotional state that drives negative reinforcement – drug seeking to alleviate the aversive state [16].
Signaling Pathways and Neuroadaptations
Chronic drug use induces significant neuroadaptations in extended amygdala circuitry through both "within-system" and "between-system" adaptations. Within-system adaptations involve disruption of the same neurochemical systems implicated in the positive reinforcing effects of drugs, while between-system adaptations engage different neurochemical systems in an attempt to overcome the chronic presence of the drug and restore normal function [16].
The following diagram illustrates the key neurochemical signaling pathways in the anti-reward system:
Figure 2: Anti-Reward System Neurochemical Pathways
Table 2: Neurochemical Systems in the Extended Amygdala Anti-Reward System
| Neurotransmitter | Receptor Targets | Functional Role in Addiction | Direction of Change in Withdrawal |
|---|---|---|---|
| Corticotropin-releasing factor (CRF) | CRF₁, CRF₂ | Mediates stress-like responses | Increased |
| Norepinephrine | α₁, α₂, β adrenoceptors | Contributes to anxiety and arousal | Increased |
| Dynorphin | κ-opioid receptor | Produces dysphoria and aversion | Increased |
| Dopamine | D₁, D₂ receptors | Reward processing | Decreased in NAcc |
| GABA | GABAₐ, GABAᴃ | Inhibitory control | Dysregulated |
| Serotonin | 5-HT₁ʙ, 5-HT₂ᴀ | Mood regulation | Dysregulated |
Methodological Approaches for Studying Extended Amygdala Function
Experimental Models and Behavioral Paradigms
Research on the extended amygdala and anti-reward systems employs several well-validated experimental approaches:
- Intracranial self-stimulation (ICSS) threshold measurement: Used to assess brain reward function, with increased thresholds (decreased reward) observed during drug withdrawal [16]. This provides a direct operational measure of the reward deficit state associated with drug withdrawal.
- Social defeat stress models: Employed to study the contribution of stress on drug-taking and reinforcement, serving as a method of "behavioral sensitization" to drugs of abuse [20]. This model has been particularly valuable for understanding how non-pharmacological stressors exacerbate negative affective states.
- Self-administration with extended access: Animal models that use intermittent extended access to drug self-administration lead to increased motivation for drug-taking and more accurately model the transition to addiction [20].
Neurobiological Assessment Techniques
Modern neuroscience employs multiple approaches to investigate extended amygdala function in addiction:
- Circuit-mapping approaches: Rabies virus-mediated circuit mapping reveals drug-induced changes in functional connectivity, such as the persistent elevation in spontaneous and task-related activity of inhibitory GABAergic cells from the BNST to downstream targets after cocaine exposure [21].
- Chemogenetics and optogenetics: Allow precise control of specific neural populations to establish causal relationships between circuit activity and behavior [21].
- Fiber photometry: Enables real-time monitoring of neural activity in specific pathways during behavior [21].
- Neuroimaging: Human imaging studies of addicts during withdrawal or protracted abstinence have shown decreased dopamine D2 receptors and hypoactivity of the orbitofrontal-infralimbic cortex system [16].
Table 3: Key Experimental Approaches in Extended Amygdala Research
| Methodology | Application | Key Measured Parameters |
|---|---|---|
| Fiber Photometry | Real-time neural activity monitoring | Calcium signals as proxy for neuronal activity |
| Rabies Virus Circuit Mapping | Neural connectivity mapping | Monosynaptic inputs to specific cell populations |
| Chemogenetics (DREADDs) | Targeted neuronal manipulation | Behavioral changes following receptor activation |
| Microdialysis | Neurochemical measurement | Extracellular neurotransmitter levels |
| Operant Self-Administration | Addiction-like behavior measurement | Drug intake, motivation, relapse susceptibility |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Extended Amygdala Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Viral Vector Tools | AAV-DREADDs, RV-ΔG-tdTomato | Circuit manipulation and mapping |
| Cell-Type Specific Markers | GABA antibodies, c-Fos antibodies | Identification of activated neuronal populations |
| Neurochemical Assays | CRF ELISA, CORT RIA | Quantification of stress mediators |
| Receptor Ligands | CRF antagonists, κ-opioid agonists | Pharmacological dissection of systems |
| Genetic Models | CRF receptor knockout mice | Determination of molecular mechanisms |
Experimental Protocols for Key Findings
Protocol 1: Assessing CRF Dependency in Withdrawal-Induced Anxiety
This protocol is adapted from studies establishing the role of CRF in the extended amygdala in negative affect during drug withdrawal [16]:
- Subjects: Laboratory rats (n=10-12/group) with chronic catheter implantation for drug self-administration
- Drug self-administration phase:
- 2-hour daily sessions for 5-7 days to establish stable baseline
- Transition to 6-12 hour extended access sessions for 10-14 days
- Withdrawal phase:
- 24-72 hours after last drug session
- Behavioral testing in elevated plus maze or light-dark box
- Pharmacological manipulation:
- Bilateral microinjection of CRF receptor antagonists (e.g., antalarmin) into BNST or CeA
- Control groups receive vehicle injections
- Outcome measures:
- Time spent in open arms of elevated plus maze
- Plasma corticosterone levels via radioimmunoassay
- c-Fos immunohistochemistry in extended amygdala subregions
Protocol 2: Circuit-Specific Manipulation of BNST→VTA Pathway
This protocol is based on recent work defining the role of specific extended amygdala projections in addiction-related behaviors [21]:
- Viral vector delivery:
- Inject AAV-Cre into VTA of DAT-Cre mice
- Inject CAV-FLEX-TVA-mCherry into amygdala
- Inject RV-ΔG-GFP into VTA 3 weeks later
- Cell-type specific manipulation:
- Express DREADDs (hM4Di) in BNSTGABA→VTA projection neurons
- Administer CNO (clozapine-N-oxide) prior to behavioral testing
- Behavioral assessment:
- Cocaine-induced place preference conditioning
- Anxiety measures during protracted withdrawal (14-28 days)
- Reinstatement testing following extinction
- Neural activity recording:
- Fiber photometry in VTADA→amygdala cells during behavioral tests
- Measure calcium transients as indicator of neuronal activity
Clinical Implications and Translation
The extended amygdala and anti-reward system framework has significant implications for understanding and treating addiction. Human imaging studies have consistently shown abnormalities in extended amygdala regions in individuals with substance use disorders [16] [3]. The Addictions Neuroclinical Assessment (ANA) developed by the National Institute on Alcohol Abuse and Alcoholism translates the three neurobiological stages of addiction into three neurofunctional domains: incentive salience, negative emotionality, and executive dysfunction [3]. This instrument allows clinicians to employ targeted treatments for specific clinical presentations.
The recognition that negative emotional states drive relapse through negative reinforcement mechanisms has shifted therapeutic approaches toward addressing the emotional components of addiction rather than solely focusing on reward. Pharmacotherapeutic strategies that target components of the anti-reward system, particularly CRF and kappa-opioid receptors, show promise for preventing relapse [16] [19].
The extended amygdala serves as a critical neural substrate for negative affect in addiction, functioning as the anatomical basis for the anti-reward system. Through complex neuroadaptations involving CRF, norepinephrine, and dynorphin systems, this region mediates the negative emotional state that defines motivational withdrawal and drives negative reinforcement. Understanding these mechanisms provides a neurobiological framework for developing targeted interventions for addiction that address not only the initial rewarding effects of drugs but also the negative emotional state that perpetuates the addiction cycle. Future research focusing on specific circuit elements within the extended amygdala and their interactions with other reward and stress systems holds promise for advancing addiction treatment strategies.
The preoccupation/anticipation stage of addiction, commonly known as the craving stage, is a critical phase of the addiction cycle that plays a fundamental role in relapse vulnerability [5] [2]. Unlike earlier stages dominated by acute intoxication and withdrawal, this stage is characterized by a persistent desire for the drug and a profound deficit in executive control over drug-seeking behaviors, despite periods of abstinence [5]. Research over the past two decades has established that these clinical phenomena are underpinned by significant dysfunction within the prefrontal cortex (PFC) and its distributed networks [22] [23] [24]. The Impaired Response Inhibition and Salience Attribution (iRISA) model provides a key framework for understanding this dysfunction, positing that addiction is characterized by the assignment of excessive salience to drug-related cues at the expense of non-drug rewards, coupled with a chronic inability to inhibit maladaptive behaviors [22] [24]. This whitepaper synthesizes current neurobiological evidence, detailing the specific PFC subregions involved, their functional roles, and the resulting cognitive deficits that create a perfect storm of relapse vulnerability during the preoccupation stage. Furthermore, it outlines critical experimental methodologies and reagents driving this field of research, providing a comprehensive resource for scientists and drug development professionals.
Neurobiological Basis of PFC Dysfunction
Key Prefrontal Cortex Subregions and Their Roles
The PFC is not a monolithic entity; distinct subregions contribute uniquely to the symptomatology of the preoccupation stage through their specialized roles in cognition, emotion, and motivation [22] [25]. Chronic drug use disrupts the delicate functional balance across these regions.
Table 1: PFC Subregions and Their Dysfunction in Addiction's Preoccupation Stage
| PFC Subregion | Primary Functions | Manifestation of Dysfunction in Addiction |
|---|---|---|
| Dorsolateral PFC (DLPFC) | Working memory, attention regulation, cognitive flexibility [22] [24] | Impaired working memory biased towards drug cues; inflexible attention and difficulty shifting goals away from drug procurement [22] |
| Anterior Cingulate Cortex (ACC) | Error detection, conflict monitoring, emotional regulation [22] [24] [25] | Compromised self-monitoring, failure to detect conflict between drug-seeking and other goals, and heightened stress reactivity [22] |
| Orbitofrontal Cortex (OFC) | Value representation, outcome expectation, reversal learning [22] [24] | Inability to update the value of non-drug reinforcers; choice of immediate drug reward over delayed gratification [22] |
| Ventromedial PFC (vmPFC) | Emotional regulation, decision-making, value coding [22] [24] | Enhanced motivation for drugs with decreased motivation for other goals; poor decision-making despite adverse consequences [22] |
| Ventrolateral PFC (vlPFC)/ Inferior Frontal Gyrus (IFG) | Response inhibition, impulse control [22] [24] | Core impulsivity and inability to suppress prepotent drug-seeking responses [22] |
Structural and Functional Neuroimaging Evidence
Converging evidence from human neuroimaging studies robustly demonstrates that addiction is associated with significant structural and functional alterations within the PFC.
Structural Findings: A consistent pattern of lower gray matter volume is observed across multiple substance use disorders (including tobacco, alcohol, stimulants, and opioids) compared to non-addicted controls [24]. This atrophy is particularly prominent in the OFC and vmPFC, but also extends to the DLPFC, ACC, and IFG/vlPFC [24]. Crucially, these structural deficits often have a dose-response relationship, where a longer duration of drug use correlates with lower PFC gray matter volume [24]. Evidence also suggests that these changes are not entirely permanent. Longitudinal studies indicate that abstinence can lead to a partial recovery of PFC gray matter volume, which parallels improvements in cognitive function [24].
Functional Findings: Functional MRI (fMRI) and PET studies reveal a characteristic pattern of neurofunctional dysregulation. During cue-induced craving tasks, there is a hyperactivation of the OFC and ACC in response to drug-related cues, signaling the excessive salience attributed to these stimuli [22] [2]. Concurrently, there is a hypoactivation of the DLPFC and vlPFC/IFG during tasks requiring inhibitory control or decision-making, reflecting the compromised executive control that defines the iRISA syndrome [22] [23]. This imbalance between a hyperactive "go" system (OFC/ACC) and a hypoactive "stop" system (DLPFC/vlPFC) creates a neural environment highly permissive to relapse [22].
The following diagram illustrates the key neurocircuitry involved in the preoccupation stage, highlighting the imbalance between salience attribution and inhibitory control networks:
Core Deficits: Executive Dysfunction and Craving
The neurobiological alterations described above manifest behaviorally as two core, interlinked deficits: impaired executive control and intrusive craving.
Erosion of Executive Control
Executive functions mediated by the PFC are essential for maintaining abstinence. In the preoccupation stage, a generalized deficit in inhibitory control is evident. The vlPFC/IFG, critical for suppressing prepotent responses, is hypoactive, rendering individuals unable to resist drug-seeking impulses even when they are consciously trying to abstain [22] [24]. This is compounded by deficits in decision-making, largely governed by the OFC and vmPFC. Individuals with addiction display a pronounced bias toward immediate rewards (drug use) despite delayed severe negative consequences, a pattern known as delay discounting [22] [25]. Furthermore, impaired flexibility from DLPFC and ACC dysfunction makes it difficult to shift behavioral strategies away from drug-seeking habits and toward alternative, healthy rewards [22].
Neurocognitive Drivers of Craving
Craving is more than a simple feeling; it is a complex cognitive and emotional state driven by dysregulated neural circuits. The attentional bias toward drug-related cues is a key component. Drug cues automatically capture attention, a process linked to hyperactivation of the ACC and OFC, which assign them excessive incentive salience [22] [2]. This creates a feedback loop where cues trigger craving, and craving further enhances attention to cues. The dysfunctional reward valuation by the OFC and vmPFC means that the expected value of the drug is inflated, while the value of natural reinforcers (e.g., food, social interaction) is diminished [22] [24]. This skewed value system ensures that drug-seeking remains the dominant motivational priority during the preoccupation stage.
Experimental Approaches and Methodologies
Research into PFC dysfunction in addiction relies on a multidisciplinary approach, integrating neuroimaging, neuropsychological testing, and experimental paradigms.
Key Behavioral and Cognitive Paradigms
Well-validated experimental tasks are used to probe specific cognitive functions linked to PFC subregions.
- Cue-Reactivity Paradigms: Participants are exposed to drug-related cues (e.g., pictures, paraphernalia) versus neutral cues while undergoing fMRI. Primary Outcome: Heightened BOLD response in the OFC, ACC, and striatum, correlated with self-reported craving [22] [2]. This measures the "salience attribution" component of iRISA.
- Go/No-Go and Stop-Signal Tasks: These tasks measure response inhibition. In a Go/No-Go task, participants must suppress a preponent response to a "No-Go" stimulus. The Stop-Signal Task involves stopping an already-initiated motor response. Primary Outcome: Increased error rates on inhibition trials and associated hypoactivation in the vlPFC and DLPFC in addicted individuals [22] [24]. This directly assesses the "response inhibition" deficit.
- Delay Discounting Tasks: Participants make choices between a small immediate monetary reward and a larger delayed reward. Primary Outcome: Steeper discounting of delayed rewards (i.e., greater impulsivity) is a robust marker of addiction and is associated with reduced activation in the OFC and vmPFC during choice deliberation [25].
- Iowa Gambling Task and Other Decision-Making Tasks: These tasks simulate real-world decision-making under uncertainty, requiring participants to learn from rewards and punishments. Primary Outcome: Addicted individuals consistently make disadvantageous choices, linked to OFC/vmPFC dysfunction [24].
Neuroimaging and Neurophysiological Protocols
- Structural MRI (sMRI):
- Protocol: High-resolution T1-weighted imaging.
- Analysis: Voxel-Based Morphometry (VBM) or cortical thickness analysis to quantify gray matter volume/density.
- Outcome: Identification of regional atrophy (e.g., in OFC, ACC) in addiction [24].
- Functional MRI (fMRI):
- Protocol: BOLD imaging during performance of cognitive tasks (e.g., those listed above) or at rest (resting-state fMRI).
- Analysis: General Linear Model (GLM) for task-based activation; seed-based correlation or Independent Component Analysis (ICA) for resting-state functional connectivity.
- Outcome: Maps of task-related hyper-/hypoactivation and altered functional connectivity within PFC networks (e.g., between PFC and striatum) [22] [23].
- Positron Emission Tomography (PET):
- Protocol: Administration of radioligands for specific neuroreceptors (e.g., [¹¹C]raclopride for dopamine D2/D3 receptors) or for glucose metabolism ([¹⁸F]FDG).
- Analysis: Binding potential or metabolic rate quantification.
- Outcome: Measurement of neurotransmitter system dysfunction (e.g., reduced D2 receptor availability in PFC) in addiction [5] [2].
The following diagram outlines a typical integrated experimental workflow for investigating PFC function in addiction:
Advancing research in this field requires a suite of specialized reagents, tools, and technologies.
Table 2: Essential Research Reagents and Resources for Investigating PFC in Addiction
| Category / Item | Specific Examples | Research Function and Application |
|---|---|---|
| Neuroimaging Ligands | [¹¹C]raclopride, [¹¹C]FLB-457 | PET radioligands for quantifying dopamine D2/D3 receptor availability in the striatum and extrastriatal regions like PFC [5]. |
| Task-Based fMRI Paradigms | Stop-Signal Task, Monetary Incentive Delay Task, Cue-Reactivity Task | Standardized experimental protocols to reliably evoke and measure specific cognitive processes (inhibition, reward anticipation, craving) and their neural correlates [22] [24]. |
| Structural Analysis Pipelines | Freesurfer, CAT12 (for SPM) | Software tools for automated, precise quantification of cortical thickness and subcortical volume from T1-weighted MRI scans [24]. |
| Genetic & Molecular Kits | DNA microarrays, RNA-seq kits, PCR kits | For identifying genetic polymorphisms (e.g., in dopamine receptor genes) or transcriptional changes associated with addiction vulnerability and PFC function [5] [26]. |
| Neuromodulation Tools | Transcranial Magnetic Stimulation (TMS), tDCS kits | Non-invasive brain stimulation devices to experimentally modulate (inhibit or excite) PFC activity, testing causal roles in craving and cognitive control [23]. |
Implications for Research and Therapeutic Development
The delineation of PFC dysfunction as a core mechanism in the preoccupation stage provides a heuristic framework for developing novel treatment strategies. The evidence of neuroplasticity and partial recovery with abstinence offers a positive outlook and a target for interventions [24]. Treatments aimed at strengthening PFC-mediated inhibitory control are of paramount interest. This includes cognitive remediation therapies designed to train specific executive functions, as well as neuromodulation techniques like Transcranial Magnetic Stimulation (TMS) targeting the DLPFC or IFG to enhance their activity and restore top-down control [23] [24]. Furthermore, the neurocircuitry understanding emphasizes the need for pharmacotherapies that can rebalance the dopamine and glutamate signaling between the PFC, striatum, and extended amygdala to dampen craving and facilitate cognitive control [5] [2]. Future research must continue to leverage cross-species models [23] [24] and longitudinal designs to disentangle pre-existing vulnerabilities from drug-induced effects, ultimately paving the way for personalized and more effective interventions for addiction.
The neurobiological framework for understanding addiction relapse has traditionally centered on neuronal dysfunction. However, emerging research reveals that the brain's immune cells, particularly microglia and astrocytes, drive relapse vulnerability through previously unrecognized mechanisms. This whitepaper synthesizes recent advances demonstrating how neuroimmune interactions after drug exposure create lasting neural circuit alterations that promote drug-seeking behavior. We detail specific signaling pathways, experimental methodologies, and quantitative findings that establish neuroimmune processes as fundamental components of addiction pathology. The evidence compellingly indicates that targeting neuroimmune signaling represents a novel therapeutic frontier for developing innovative treatments for substance use disorders, moving beyond conventional neurotransmitter-focused approaches to address the persistent relapse risk that characterizes addiction.
Addiction is a chronic, relapsing brain disorder characterized by compulsive drug-seeking despite negative consequences. Traditional research has focused on neuronal adaptations within reward circuits, including the basal ganglia, extended amygdala, and prefrontal cortex [4]. The dominant model posits that addiction progresses through a three-stage cycle—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—each involving specific neuronal networks [27]. While this framework has proven valuable, it fails to fully explain the persistent vulnerability to relapse that characterizes substance use disorders (SUDs), with over 60% of individuals treated for SUD experiencing relapse within the first year after treatment [4].
A transformative perspective has emerged with the recognition that neuroimmune mechanisms represent a critical, underappreciated component of addiction neurobiology. Drugs of abuse activate the brain's resident immune cells, initiating cascades of inflammatory signaling that directly modulate synaptic function and neural plasticity [28] [29]. This whitepaper examines how microglia, the CNS's primary immune cells, and their interactions with other glial cells and neurons, create lasting changes that drive relapse vulnerability. We synthesize evidence from recent preclinical studies that identify specific neuroimmune pathways as promising targets for innovative pharmacotherapies aimed at sustaining recovery.
Core Neuroimmune Mechanisms in Addiction Pathology
Microglial Activation and Synaptic Remodeling
Microglia, the resident immune cells of the central nervous system, continuously survey the brain microenvironment and actively participate in synaptic refinement. During abstinence from drugs of abuse, microglia undergo functional changes that significantly impact neural circuits:
- Synaptic Pruning: A groundbreaking study at UNC Chapel Hill demonstrated that during abstinence from cocaine, microglia actively prune parts of astrocytes, critical support cells that help maintain neural circuit balance. This pruning event increases drug-seeking behavior, and when blocked, reduces relapse behaviors [30].
- Regional Specificity: Microglia-induced TNFα release depresses excitatory synaptic activity within the ventral striatum through internalization of AMPARs, a process associated with cocaine-induced locomotor sensitization [28] [31].
- Complement-Mediated Phagocytosis: Microglia can eliminate synapses through complement system signaling, particularly in the developing brain, and evidence suggests similar mechanisms may contribute to drug-induced circuit reorganization [32].
Astrocyte-Microglia Crosstalk in Relapse Vulnerability
Astrocytes and microglia engage in bidirectional communication that profoundly influences neuronal function and addiction-related behaviors:
- Glutamate Dysregulation: Chronic drug use disrupts glutamate homeostasis, particularly in the nucleus accumbens. Astrocytes normally regulate extracellular glutamate levels via glutamate transporters (GLT-1 and system xc-). Drug-induced neuroimmune activation impairs this function, leading to glutamate overflow that promotes compulsive drug-seeking [29].
- Inflammatory Feedforward Loops: Activated microglia release pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNFα) that trigger reactive astrogliosis. These reactive astrocytes further amplify neuroimmune signaling, creating a persistent inflammatory state that maintains addiction-related neural adaptations [29] [33].
Cytokine Modulation of Synaptic Plasticity
Cytokines, traditionally associated with peripheral immune function, are critically involved in regulating synaptic strength and plasticity in reward circuits:
Table 1: Cytokine Effects on Synaptic Plasticity in Addiction-Relevant Brain Regions
| Cytokine | Brain Region | Effect on Plasticity | Behavioral Correlation |
|---|---|---|---|
| TNFα | Hippocampus | Facilitates membrane insertion of CP-AMPARs; enhances excitatory transmission | Contextual associations in drug-seeking |
| TNFα | Striatum | Internalizes CP-AMPARs; reduces corticostriatal synaptic strength | Cocaine-induced locomotor sensitization |
| IL-6 | Hippocampus | Inhibits long-term potentiation (LTP) through MAPK/ERK signaling | Impairs hippocampus-dependent memory tasks |
| IL-1β | Hippocampus | Low concentrations enhance learning; chronic overexpression impairs LTP | Modulates fear conditioning and spatial learning |
The effects of cytokines on synaptic function are concentration-dependent and brain region-specific, creating a complex regulatory landscape that varies across different stages of addiction [28] [31].
Signaling Pathways and Molecular Mechanisms
NF-κB Pathway in Drug-Seeking Behavior
The nuclear factor-kappa B (NF-κB) pathway has emerged as a critical signaling cascade linking drug exposure to persistent neural adaptations:
The NF-κB pathway represents a promising target for pharmacotherapeutic intervention, as its inhibition may disrupt the cycle of drug-induced neuroimmune activation that maintains relapse vulnerability [29].
Neuron-Glia Communication in Reward Circuits
The interactions between neurons and glial cells within reward pathways create a complex signaling network that undergoes specific adaptations following chronic drug use:
This neuron-glia communication network demonstrates how drug-induced neuroimmune activation creates a self-reinforcing cycle that maintains elevated extracellular glutamate and promotes drug-seeking behavior [29] [31].
Quantitative Evidence from Preclinical Studies
Key Experimental Findings
Recent preclinical investigations have yielded quantitative data establishing causal relationships between neuroimmune activation and relapse behaviors:
Table 2: Quantitative Evidence of Neuroimmune Mechanisms in Addiction Models
| Experimental Manipulation | Drug Model | Key Finding | Effect Size/Quantitative Measure |
|---|---|---|---|
| Microglial inhibition (minocycline) | Cocaine | Reduced drug-seeking behavior | ~40-60% decrease in reinstatement |
| Astrocyte pruning blockade | Cocaine | Attenuated relapse behaviors | Significant reduction in cocaine-seeking |
| TNFα neutralization | Psychostimulants | Decreased locomotor sensitization | Altered AMPAR trafficking in striatum |
| TLR4 antagonist administration | Alcohol, Opioids | Reduced self-administration | Decreased motivation in operant tasks |
| NF-κB pathway inhibition | Multiple drugs | Attenuated conditioned place preference | Disrupted drug-context associations |
These quantitative findings from rigorous preclinical studies provide compelling evidence that targeting specific neuroimmune pathways can produce measurable reductions in addiction-related behaviors [30] [28] [29].
Methodological Approaches and Experimental Protocols
Assessing Microglial Function in Addiction Models
To investigate microglial contributions to relapse vulnerability, researchers employ specialized methodologies:
Microglial Depletion and Monitoring Protocol:
- CSF1R Inhibition: Administer PLX5622 (1200 ppm in diet) for 7-21 days to deplete ~80-90% of brain microglia
- Depletion Verification: Confirm microglial reduction via Iba1 immunohistochemistry or TMEM119 staining
- Behavioral Testing: Assess drug-seeking in self-administration or conditioned place preference paradigms
- Synaptic Analysis: Examine dendritic spine density and morphology using Golgi-Cox staining or two-photon imaging
- Cytokine Profiling: Measure TNFα, IL-1β, and IL-6 levels via ELISA or multiplex immunoassays
This approach enables researchers to establish causal relationships between microglial presence/function and drug-seeking behaviors [30] [32].
Astrocyte-Microglia Interaction Studies
To examine bidirectional communication between astrocytes and microglia in addiction models:
Conditioned Media Transfer Protocol:
- Primary Cell Cultures: Establish separate microglial and astrocytic cultures from rodent brains
- Drug Exposure: Treat microglia with drug of interest (e.g., 10μM cocaine) for 24 hours
- Conditioned Media Collection: Harvest media from drug-exposed microglia
- Astrocyte Exposure: Apply microglia-conditioned media to astrocyte cultures
- Functional Assessment: Measure (a) astrocytic glutamate transporter expression (Western blot), (b) inflammatory mediator release (multiplex cytokine array), and (c) morphological changes (GFAP immunostaining)
This methodology reveals how microglial activation directly influences astrocytic function, potentially contributing to glutamate dysregulation in addiction [30] [29].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Neuroimmune Mechanisms in Addiction
| Reagent/Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| Microglial Inhibitors | Minocycline, PLX3397, PLX5622 | Deplete or inhibit microglial function | Determine microglial necessity in drug-seeking behaviors |
| Cytokine Modulators | Etanercept (TNFα inhibitor), IL-1RA (IL-1 receptor antagonist) | Neutralize specific cytokine signaling | Identify cytokine-specific contributions to relapse vulnerability |
| TLR4 Pathway Antagonists | (+)-Naltrexone, Ibudilast (AV411) | Block innate immune receptor activation | Test role of pattern recognition receptors in drug reward |
| Transgenic Mouse Models | CX3CR1-GFP, Iba1-GFP, GFAP-GFP reporters | Visualize and isolate specific glial populations | Enable cell-type-specific manipulation and monitoring |
| GFAP Astrocyte Markers | Anti-GFAP antibodies, ALDH1L1 reporters | Identify and quantify astrocyte reactivity | Correlate astrogliosis with behavioral measures |
| Iba1 Microglia Markers | Anti-Iba1 antibodies, TMEM119 antibodies | Distinguish microglia from peripheral macrophages | Determine microglial activation state and morphology |
This toolkit enables researchers to systematically dissect the contributions of specific neuroimmune components to addiction pathophysiology [30] [29] [33].
Future Directions and Therapeutic Implications
The accumulating evidence for neuroimmune mechanisms in addiction relapse vulnerability suggests several promising research directions and clinical applications:
- Cell-Type-Specific Transcriptomics: Single-cell RNA sequencing of microglia and astrocytes from addiction models will reveal drug-induced molecular changes in specific glial subpopulations across brain regions and addiction stages.
- Temporal Dynamics: Investigating how neuroimmune responses evolve throughout the addiction cycle—from initial drug exposure to protracted abstinence—will identify critical windows for therapeutic intervention.
- Sex-Specific Mechanisms: Preliminary evidence suggests ovarian hormones influence neuroimmune signaling, necessitating dedicated studies of sex differences in glial contributions to addiction.
- Translational Biomarkers: Developing PET ligands for glial activation (e.g., TSPO radiotracers) could provide non-invasive biomarkers to monitor neuroimmune activation in patients and guide targeted therapies.
- Combination Therapies: Integrating neuroimmune-targeting agents with existing behavioral and pharmacological interventions may produce synergistic effects in reducing relapse risk.
The recognition that addiction produces lasting changes in brain immune function represents a fundamental shift in understanding this disorder. By expanding research beyond neuronal-centric models to include the active contributions of microglia and neuroimmune signaling, the field opens new avenues for developing mechanistically innovative treatments for substance use disorders.
Drug addiction is a chronic, relapsing disorder characterized by a profound loss of control over drug use, high rates of relapse, and a shift from voluntary, recreational drug use to compulsive drug-seeking and-taking habits [34] [3]. This transition represents a fundamental reorganization of behavioral control processes within the brain's striatal circuits. Research over the past two decades has established that this progression corresponds to a hierarchical shift in the neural control of behavior from the ventral striatum (involved in reward processing and goal-directed actions) to the dorsal striatum (critical for habit formation and automatic behaviors) [34] [35] [36]. This ventral-to-dorsal progression provides a neurobiological framework for understanding why addiction persists despite adverse consequences and why relapse remains a major challenge even after prolonged abstinence. The shift involves enduring neuroadaptations in cortico-basal ganglia-thalamic circuits that underlie the core features of addiction: compulsion to seek drugs, loss of control in limiting intake, and emergence of a negative emotional state during withdrawal [2]. This whitepaper examines the molecular, cellular, and circuit-level mechanisms underlying this transition and its implications for relapse vulnerability and therapeutic development.
Neuroanatomical Framework of Striatal Circuits
Functional Organization of the Striatum
The striatum serves as the primary input structure of the basal ganglia and is functionally heterogeneous. It can be broadly divided into ventral and dorsal subregions, each with distinct roles in motivation, learning, and behavior:
Ventral Striatum: Centered on the nucleus accumbens (NAc), this region integrates information from limbic structures and is crucial for processing reward, incentive salience ("wanting"), and the initial reinforcing effects of drugs of abuse [37] [38]. The NAc is further subdivided into core and shell subregions, with the shell responding to primary unconditioned stimuli and the core involved in conditioned responses [38].
Dorsal Striatum: Comprising dorsomedial (DMS) and dorsolateral (DLS) subregions, this area is essential for instrumental learning and habit formation [37] [36]. The DMS supports goal-directed actions sensitive to outcome value, while the DLS mediates stimulus-response habits that become automatic and resistant to devaluation [36].
These striatal regions are not independent but are interconnected through a spiral loop system via midbrain dopamine neurons, allowing information to flow from ventromedial to dorsolateral striatum [37] [36].
Microcircuitry of Medium Spiny Neurons
Approximately 95% of striatal neurons are GABAergic medium spiny neurons (MSNs) that form two major output pathways [37]:
Direct pathway MSNs (dMSNs): Express dopamine D1 receptors, project directly to output nuclei (substantia nigra pars reticulata and globus pallidus interna), and facilitate behavior initiation ("go" signal) [37].
Indirect pathway MSNs (iMSNs): Express dopamine D2 receptors, project indirectly to output nuclei via the globus pallidus externa and subthalamic nucleus, and suppress behavior ("brake" signal) [37].
These pathways are dynamically modulated by dopaminergic inputs from the ventral tegmental area (VTA) and substantia nigra pars compacta (SNc), and glutamatergic inputs from prefrontal cortex, hippocampus, amygdala, and thalamus [37].
Table 1: Key Striatal Subregions and Their Functional Roles in Addiction
| Striatal Subregion | Primary Function in Addiction | Key Input Regions | Behavioral Correlate |
|---|---|---|---|
| NAc Shell | Processing unconditioned drug effects; initial reward | Amygdala, Hippocampus, VTA | Drug "liking"; initial reinforcement |
| NAc Core | Processing conditioned cues; incentive salience | Prefrontal Cortex, Amygdala | Cue-induced craving; drug "wanting" |
| Dorsomedial Striatum | Goal-directed drug seeking; action-outcome learning | Prefrontal Cortex, Amygdala | Flexible, value-sensitive drug seeking |
| Dorsolateral Striatum | Habitual drug seeking; stimulus-response learning | Sensorimotor Cortex, Thalamus | Compulsive, inflexible drug seeking |
The Three-Stage Addiction Cycle and Striatal Transitions
Addiction progresses through a recurring three-stage cycle, each involving distinct neuroadaptations in striatal circuits [3] [2] [4]:
Binge/Intoxication Stage
During this initial stage, drugs of abuse powerfully increase dopamine transmission in the ventral striatum, particularly the NAc shell, producing intense euphoria and reinforcing drug use [3] [38]. All addictive substances converge on the mesolimbic dopamine system, albeit through different mechanisms:
- Psychostimulants (cocaine, amphetamine) directly increase synaptic dopamine by targeting dopamine transporters [38]
- Opioids and cannabinoids disinhibit dopamine neurons by reducing GABAergic inhibition of VTA neurons [36]
- Nicotine directly stimulates dopaminergic neurons via nicotinic acetylcholine receptors [4]
This stage primarily involves ventral striatal circuits and establishes strong Pavlovian associations between drug effects and environmental cues [38].
Withdrawal/Negative Affect Stage
With repeated drug use, counter-adaptations occur in the extended amygdala and its connections with striatal circuits, leading to a hypodopaminergic state and increased stress system activation during withdrawal [3] [2]. Key neuroadaptations include:
- Reduced dopamine D2 receptor availability in ventral striatum [3]
- Increased corticotropin-releasing factor (CRF) and dynorphin signaling in extended amygdala [2]
- Altered glutamate homeostasis affecting striatal synaptic plasticity [37]
These changes produce negative emotional states (dysphoria, anxiety, irritability) that drive drug seeking through negative reinforcement [2].
Preoccupation/Anticipation Stage
This stage involves the progressive engagement of dorsal striatal circuits, particularly as drug use transitions from recreational to compulsive [34] [36]. The dorsolateral striatum (DLS) becomes critical for the habitual and compulsive drug-seeking that characterizes addiction [34] [35] [36]. Key features include:
- Shift from action-outcome to stimulus-response learning [36]
- Emergence of task-bracketing neural activity in DLS that chunks drug-seeking sequences into automated routines [36]
- Reduced prefrontal cortical control over habitual behavior [34] [35]
This ventral-to-dorsal progression is facilitated by the spiraling interconnectivity between striatal subregions via midbrain dopamine systems [37] [36].
Table 2: Neuroadaptations Across the Addiction Cycle [3] [2] [4]
| Addiction Stage | Primary Brain Regions | Key Neurotransmitter Changes | Behavioral Manifestation |
|---|---|---|---|
| Binge/Intoxication | Ventral Striatum (NAc), VTA | ↑ Dopamine, ↑ Opioid peptides | Euphoria; positive reinforcement |
| Withdrawal/Negative Affect | Extended Amygdala, Ventral Striatum | ↓ Dopamine, ↑ CRF, ↑ Dynorphin | Dysphoria, anxiety, negative reinforcement |
| Preoccupation/Anticipation | Dorsal Striatum, Prefrontal Cortex | ↑ Glutamate, Altered DA/GLU balance | Craving, compulsivity, impaired control |
Molecular Mechanisms of Striatal Plasticity in Addiction
Dopamine Receptor Signaling and Neuroadaptations
Drug-induced plasticity in striatal circuits involves complex alterations in dopamine receptor signaling [37] [38]:
- D1 receptor activation stimulates adenylyl cyclase, increasing cAMP and protein kinase A (PKA) activity, leading to CREB phosphorylation and gene expression changes [38]
- D2 receptor activation inhibits adenylyl cyclase, reducing cAMP/PKA signaling [38]
- Repeated drug exposure alters the balance between D1 and D2 signaling, promoting long-term potentiation (LTP) in D1-MSNs and long-term depression (LTD) in D2-MSNs [37]
These signaling adaptations strengthen corticostriatal synapses in direct pathway neurons while weakening them in indirect pathway neurons, creating a bias toward continued drug seeking [37].
Glutamatergic Mechanisms and Synaptic Plasticity
Chronic drug exposure produces profound changes in glutamatergic transmission in striatal circuits [37] [38]:
- Altered AMPA receptor trafficking and composition, including increased GluA2-lacking AMPARs in NAc after cocaine withdrawal [37]
- Changes in NMDA receptor function and signaling
- Disrupted glutamate homeostasis via reduced cystine-glutamate exchange, leading to compromised astrocytic regulation of glutamate [2]
These glutamatergic adaptations underlie the enduring synaptic plasticity that maintains addiction and contributes to cue-induced relapse [37].
Experimental Models and Methodologies
Behavioral Paradigms for Studying Compulsive Drug Seeking
Several well-validated behavioral procedures are used to model different aspects of addiction in laboratory animals:
Drug Self-Administration: Animals learn to perform an operant response (e.g., lever press) to receive intravenous drug infusions, modeling the voluntary drug-taking aspect of addiction [39].
Reinstatement Procedures: After extinction of drug-reinforced responding, drug seeking is reinstated by drug priming injections, drug-associated cues, or stressors, modeling relapse triggers in humans [39].
Resistance to Punishment/Devaluation: Measures the persistence of drug seeking despite adverse consequences (e.g., footshock) or reduced drug value, modeling the compulsive aspect of addiction [36].
Habit Assessment: Uses outcome devaluation procedures (e.g., lithium chloride pairing) to determine whether drug seeking is goal-directed or habitual [36].
Neural Manipulation Techniques
Modern neuroscience approaches allow precise manipulation of specific neural circuits:
Optogenetics: Uses light-sensitive opsins to selectively activate or inhibit specific neuronal populations with millisecond precision [37]. For example, channelrhodopsin-2 (ChR2) allows activation of specific MSN pathways, while halorhodopsin (NpHR) enables their inhibition.
Chemogenetics (DREADDs): Engineered G-protein-coupled receptors that are activated by biologically inert compounds like clozapine-N-oxide (CNO), allowing prolonged modulation of neuronal activity [37].
Circuit-Tracing Methods: Anterograde and retrograde tracers (e.g., fluorescent latex microspheres, viral vectors) to map connectivity between striatal subregions and other brain areas [37].
Table 3: Key Experimental Methods for Studying Striatal Transitions in Addiction [37] [39] [36]
| Method Category | Specific Techniques | Application in Addiction Research | Key Insights Generated |
|---|---|---|---|
| Behavioral Models | Drug self-administration, Reinstatement, Devaluation procedures | Modeling different stages of addiction and relapse | Ventral-to-dorsal shift in control of drug seeking; compulsive aspects |
| Neural Monitoring | in vivo electrophysiology, Fiber photometry, fMRI | Recording neural activity during drug-seeking behavior | Emergence of task-bracketing activity in DLS; altered ventral striatal coding |
| Circuit Manipulation | Optogenetics, DREADDs, Lesion studies | Establishing causal role of specific circuits | D1-MSN vs D2-MSN contributions; ventral-dorsal striatal interactions |
| Molecular Analysis | qPCR, Western blot, Immunohistochemistry, Proteomics | Identifying molecular adaptations underlying plasticity | Drug-induced changes in receptor expression, signaling pathways, synaptic proteins |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating Striatal Mechanisms in Addiction
| Reagent/Tool | Specific Examples | Research Application | Key References |
|---|---|---|---|
| Viral Vectors | AAV-DIO-ChR2-eYFP, AAV-DIO-hM4D(Gi)-mCherry | Cell-type specific optogenetic/chemogenetic manipulation of D1- or D2-MSNs | [37] |
| Cre-Driver Lines | D1-Cre, D2-Cre, A2A-Cre transgenic mice | Genetic access to specific MSN populations for selective manipulation | [37] |
| Dopamine Sensors | dLight, GRABDA | Real-time monitoring of dopamine release with high temporal resolution | [38] |
| Calcium Indicators | GCaMP6f, jRGECO1a | Monitoring neuronal activity in specific cell populations during behavior | [36] |
| Receptor Ligands | SCH-23390 (D1 antagonist), Raclopride (D2 antagonist) | Pharmacological dissection of dopamine receptor contributions | [38] |
| Behavioral Apparatus | Operant chambers, Med-Associate systems | Standardized assessment of drug self-administration and seeking | [39] |
Implications for Relapse Vulnerability and Therapeutic Development
The ventral-to-dorsal striatal shift has profound implications for understanding relapse vulnerability and developing novel treatment strategies:
Mechanisms of Relapse Vulnerability
Compulsive drug-seeking habits mediated by the dorsal striatum are notably resistant to extinction and persist despite adverse consequences, contributing to high relapse rates [36]. Several factors maintain this vulnerability:
- Drug-associated cues acquire excessive control over behavior through dorsal striatal mechanisms [39]
- Stress potentiates the motivational salience of drug cues via convergent actions on striatal circuits [39]
- Prefrontal cortical dysfunction impairs top-down control over established habits [34] [35]
Therapeutic Implications
Targeting different components of the striatal circuitry may provide novel approaches for treating addiction:
- Dorsal striatal targets may be particularly relevant for reducing compulsive drug seeking in established addiction [36]
- Restoring prefrontal control over striatal circuits could enhance behavioral flexibility and resistance to relapse [34]
- Normalizing dopamine and glutamate signaling in striatal circuits remains a promising pharmacological approach [37] [38]
The transition from ventral to dorsal striatal control represents a fundamental neurobiological mechanism underlying the development of compulsive drug seeking in addiction. This progression involves complex interactions between dopamine and glutamate systems that drive neuroplasticity across distributed striatal circuits. Understanding these mechanisms at molecular, cellular, and circuit levels provides critical insights into relapse vulnerability and opens new avenues for therapeutic intervention.
Future research should focus on: (1) elucidating the precise molecular mechanisms that initiate and maintain the ventral-to-dorsal transition; (2) developing strategies to reverse established drug-seeking habits without affecting adaptive behaviors; (3) identifying individual differences in vulnerability to striatal transitions; and (4) translating these findings into targeted interventions that restore behavioral flexibility and reduce relapse in addiction.
Biomarker Discovery and Neuroimaging Techniques for Predicting Relapse
Relapse is a hallmark of substance use disorders (SUDs), presenting a major challenge for treatment development. The identification of reliable biomarkers of relapse vulnerability is thus a critical goal in addiction neuroscience. Functional neuroimaging provides a powerful, non-invasive window into the neural circuits underlying addiction, offering objective indices of relapse risk that can inform personalized interventions and improve outcomes. This whitepaper synthesizes current evidence on functional Magnetic Resonance Imaging (fMRI), Positron Emission Tomography (PET), and Electroencephalography (EEG) biomarkers, detailing the specific functional and neurochemical signatures associated with relapse vulnerability. By framing these findings within the neurobiology of addiction, this guide aims to equip researchers and drug development professionals with the experimental protocols and analytical tools necessary to advance this pivotal field.
fMRI Biomarkers of Relapse Risk
Functional MRI (fMRI) studies have identified robust biomarkers of relapse risk by probing brain function during rest, in response to drug cues, and during cognitive tasks. The consistent findings point to dysfunction within and between large-scale brain networks responsible for reward, executive control, and salience detection.
Task-Based fMRI: Drug Cue Reactivity
Exposure to drug-related cues reliably activates craving and engages specific brain regions in individuals with SUDs. This cue-reactivity paradigm has been successfully used to predict treatment outcomes.
A 2025 study on methamphetamine use disorder (MUD) developed a machine learning model using fMRI drug cue reactivity (fDCR) to predict craving intensity. The model, which combined Principal Component Analysis (PCA) with linear regression, achieved a statistically significant predictive performance (out-of-sample RMSE = 0.985, p < 0.026) [40]. The neural signature of craving included increased activity in the parahippocampal gyrus, superior temporal gyrus, medioventral occipital cortex, and amygdala, and decreased activity in the inferior temporal gyrus [40]. This model also successfully classified high versus low craving levels (AUC-ROC = 0.714) and distinguished between drug and neutral cues (AUC-ROC = 0.693) [40].
Table 1: fMRI Cue-Reactivity Biomarkers Linked to Relapse
| Brain Region | Function | Direction of Change in Relapse Risk | Associated Substance |
|---|---|---|---|
| Ventral Striatum / Nucleus Accumbens | Reward processing, craving | Increased activation to drug cues | Alcohol, Cocaine, Nicotine, Methamphetamine [40] [41] |
| Medial Prefrontal Cortex (mPFC) / Orbitofrontal Cortex (OFC) | Valuation, decision-making | Increased activation to drug cues; decreased volume | Alcohol, Nicotine [41] |
| Anterior Cingulate Cortex (ACC) | Conflict monitoring, salience | Altered activation (varies by context) | Alcohol, Nicotine, Heroin [42] [41] |
| Amygdala | Emotional arousal, memory | Increased activation to drug cues | Multiple (Meta-Analysis) [40] [41] |
| Insula | Interoceptive awareness, craving | Increased activation to drug cues; reduced functional connectivity to control networks | Nicotine, Alcohol [41] |
Experimental Protocol: fMRI Drug Cue-Reactivity Task
- Participants: Abstinent individuals with SUD (e.g., ≥1 week abstinence, confirmed by urine toxicology).
- Stimuli: Present block or event-related designs with standardized drug-related images (e.g., drug paraphernalia) matched with neutral images (e.g., household objects) for visual characteristics.
- fMRI Acquisition: Acquire T1-weighted anatomical scan. For functional scans, use T2*-weighted echo-planar imaging (EPI) sequence (e.g., TR/TE = 2000/30 ms, voxel size = 3×3×3 mm³).
- Self-Report: Collect subjective craving ratings (e.g., on a 1-10 scale) after each block or trial.
- Analysis: Preprocess data (realignment, normalization, smoothing). Conduct first-level analysis to model BOLD response to drug vs. neutral cues. Use whole-brain or ROI-based approaches. For prediction, employ machine learning pipelines with cross-validation [40].
Resting-State fMRI (rs-fMRI) and Functional Connectivity (FC)
Resting-state fMRI (rs-fMRI) examines spontaneous, low-frequency fluctuations in the BOLD signal to map intrinsic functional brain architecture and connectivity, revealing trait-like vulnerabilities.
A longitudinal study on methamphetamine dependence found that individuals who relapsed showed increased activity in the bilateral putamen during early abstinence, suggesting this may be a marker for early relapse vulnerability [8]. After relapse, these individuals exhibited more widespread abnormalities, including increased activity in the prefrontal regions, striatum, and thalamus, and decreased activity in the middle cingulate gyrus and parietal-occipital regions [8].
Furthermore, a systematic review of heroin dependence consistently found weaker functional connectivity (FC) between core neurocognitive networks—the Executive Control Network (ECN), Default Mode Network (DMN), and Salience Network (SN) [42]. Interventions like abstinence and Transcranial Magnetic Stimulation (TMS) were shown to strengthen this between-network connectivity, which correlated with reduced craving and relapse risk [42].
Table 2: Resting-State fMRI Biomarkers of Relapse Risk
| Metric/Network | Description | Change Associated with Relapse Risk |
|---|---|---|
| Regional Homogeneity (ReHo) | Local temporal synchronization of BOLD signal | Increased in striatum (putamen) [8] |
| fALFF (fractional Amplitude of Low-Frequency Fluctuations) | Power of spontaneous brain activity within low-frequency range | Increased in subcortical regions; decreased in parietal-occipital areas post-relapse [8] |
| Executive Control Network (ECN) Connectivity | Dorsolateral PFC and posterior parietal circuits for cognitive control | Weaker connectivity to other major networks [42] |
| Default Mode Network (DMN) Connectivity | Medial PFC, PCC, and angular gyrus for self-referential thought | Weaker connectivity to other major networks [42] |
| Salience Network (SN) Connectivity | Anterior insula and ACC for detecting behaviorally relevant stimuli | Weaker connectivity to other major networks [42] |
Electrophysiological (EEG) Biomarkers
EEG, particularly Event-Related Potentials (ERPs), offers high temporal resolution to capture rapid neurocognitive processes that are impaired in addiction, such as inhibitory control and attentional bias.
Key ERP Components as Biomarkers
- N2 (N200): A negative-going wave peaking ~200-350 ms post-stimulus, associated with conflict monitoring and initial response inhibition. Reduced NoGo N2 amplitudes are found in alcohol, tobacco, cannabis, and heroin use disorders, indicating impaired conflict detection [43] [44].
- P3 (P300): A positive component peaking ~300-600 ms post-stimulus, linked to attentional resource allocation and contextual updating. Increased P3 amplitude in response to drug-related cues is a marker of attentional bias and has been linked to relapse vulnerability [43] [44]. Alterations in the P3 during inhibitory control tasks (e.g., NoGo-P3) are also consistently observed.
- N170: A face-specific component that also shows sensitivity to drug cues. In alcohol use disorder, larger NoGo N170 amplitudes to alcohol cues predicted relapse within a 3-month follow-up, suggesting its utility as a visual cue sensitivity marker [44].
Experimental Protocol: Go/No-Go Task with EEG
- Participants: Individuals with SUD and matched healthy controls.
- Task: A modified Go/No-Go task for addiction (MGNT) is recommended. Participants respond frequently to "Go" stimuli (e.g., the letter "X") and withhold responses to infrequent "No-Go" stimuli (e.g., the letter "O"). To probe addiction-specific bias, neutral stimuli (e.g., bottled water) and drug-related stimuli (e.g., a beer bottle) can be used as background images or as the stimuli themselves [43].
- EEG Acquisition: Record continuous EEG from a 64-channel cap according to the 10-20 system. Keep impedance below 5 kΩ. Sampling rate should be at least 500 Hz.
- Analysis: Preprocess data (filtering, artifact removal, epoching). Epochs should be time-locked to stimulus onset (e.g., -200 to 800 ms). Average epochs separately for correct Go and No-Go trials. Measure mean amplitude or peak latency of N2 and P3 components over frontal-central (e.g., FCz) and central-parietal (e.g., Pz) electrode sites, respectively [43] [44].
PET Biomarkers of Neurochemistry
While fewer in number due to cost and complexity, PET studies provide critical insights into the neurochemical dysregulations that underpin relapse vulnerability, with a primary focus on the dopamine system.
A key finding is that lower pretreatment dopamine D2/D3 receptor availability in the limbic striatum is prospectively associated with poorer treatment outcomes and relapse in cocaine and methamphetamine addiction [41]. This dopaminergic deficit is thought to contribute to anhedonia and impulsive drug-taking, thereby increasing relapse risk.
Multi-Modal Integration and The Scientist's Toolkit
The future of relapse prediction lies in integrating multi-modal data (fMRI, EEG, PET, genetics) to create composite biomarkers with higher sensitivity and specificity. Machine learning approaches are particularly promising for this integration, moving from group-level comparisons to individual-level prediction [40] [41].
Table 3: Research Reagent Solutions for Relapse Biomarker Studies
| Reagent/Resource | Function/Description | Example Use in Research |
|---|---|---|
| Battery for Executive Functions in Addiction (BFE-A) | Standardized neuropsychological battery for assessing EFs in addiction (includes MST & MGNT) [43]. | Screening tool for cognitive deficits; can be combined with EEG for neural correlates. |
| Modified Go/No-Go Task for Addiction (MGNT) | Computerized task measuring inhibitory control with addiction-related and neutral stimuli [43]. | Elicits addiction-specific attentional bias and indexes inhibitory control deficits via behavior and ERPs (N2/P3). |
| Activation Likelihood Estimation (ALE) | Coordinate-based meta-analysis algorithm for neuroimaging data [41]. | Identifies consistent brain activation patterns across multiple cue-reactivity studies to establish consensus. |
| [11C]Raclopride | Radioligand for Positron Emission Tomography (PET) imaging of dopamine D2/D3 receptor availability. | Quantifies striatal dopamine receptor function as a predictor of relapse vulnerability [41]. |
| Data Processing & Analysis for (rs-)fMRI (DPABI) | Software toolbox for analyzing resting-state and task-based fMRI data [8]. | Computes metrics like ReHo and fALFF to identify regional brain activity abnormalities. |
Functional neuroimaging has illuminated the core neural circuits and neurocognitive processes that confer vulnerability to relapse in SUD. fMRI biomarkers highlight the critical roles of cue-reactivity in the striatum and vmPFC, as well as disrupted connectivity between the ECN, DMN, and SN. EEG biomarkers capture millisecond-scale deficits in inhibitory control (N2) and attentional bias (P3). PET imaging confirms the fundamental role of depleted striatal dopamine D2/D3 receptors. The path forward requires standardized experimental protocols, the validation of these biomarkers in large, diverse cohorts, and their integration into the development of targeted neuromodulation and pharmacological treatments. By providing objective, brain-based measures of relapse risk, these biomarkers hold the promise of revolutionizing addiction treatment from a one-size-fits-all model to a personalized, preemptive, and more effective approach.
Substance Use Disorders (SUDs) represent a major public health burden, characterized by high relapse rates following treatment. A key driver of this relapsing nature is the dysregulation of the body's central and peripheral stress systems. This whitepaper synthesizes current evidence on three pivotal peripheral biomarkers—cortisol, adrenocorticotropic hormone (ACTH), and brain-derived neurotrophic factor (BDNF)—and their roles in signaling addiction vulnerability and predicting relapse. We outline that chronic drug use induces allostatic changes in the hypothalamic-pituitary-adrenal (HPA) axis and related neurotrophic signaling, creating a measurable biological footprint. The translation of these findings into practical experimental protocols and their implications for future drug development are discussed.
Biomarker Profiles in Addiction and Relapse Vulnerability
The transition from controlled drug use to a chronic, relapsing disorder is marked by specific alterations in peripheral stress biomarkers. These changes reflect underlying neuroadaptations in brain stress and reward circuits. The table below summarizes key biomarker alterations associated with addiction risk and relapse vulnerability.
Table 1: Peripheral Biomarker Alterations in Substance Use Disorders
| Biomarker | Basal/Tonic Levels | Response to Acute Stress/Drug Cue | Association with Relapse & Vulnerability |
|---|---|---|---|
| Cortisol | Elevated in active binge alcohol intake and recent withdrawal [45]. | Blunted response observed in individuals with high addiction risk (e.g., children of parents with SUDs) [46] [47] and chronic users [46]. | Blunted cortisol response to stress or an alcohol challenge predicts future AUD symptoms and heavier use [46]. Hypocortisolism predicts relapse to alcohol and nicotine [45]. |
| ACTH | Lower basal plasma levels in individuals with a high risk for alcoholism [45]. | Altered reactivity, often blunted, in chronic users [45]. | The cortisol:ACTH ratio may be a potent peripheral predictive biomarker of relapse [45]. |
| BDNF | Serum levels change during abstinence; the direction may be substance-dependent. | Involved in neural plasticity during cue exposure and extinction learning [48]. | An increase in serum BDNF during early abstinence is associated with delayed relapse in cocaine-dependent patients [49]. Elevated serum BDNF predicts cocaine relapse outcomes [45]. |
Molecular Mechanisms and Signaling Pathways
The peripheral biomarker changes detailed above are the surface manifestation of profound dysregulation within the brain's stress and reward circuitry.
HPA Axis Dysregulation and the Allostatic Model
The HPA axis is the body's primary neuroendocrine stress system. Its activation follows a specific sequence: a stressful stimulus or drug cue triggers the release of corticotropin-releasing factor (CRF) from the hypothalamus, which stimulates pituitary secretion of ACTH, which in turn drives cortisol release from the adrenal cortex [46] [11]. Cortisol exerts negative feedback on the hypothalamus and pituitary to terminate the stress response.
In addiction, this system is hijacked. Chronic drug use leads to an allostatic state—a chronic deviation from the normal emotional and physiological set-point. This is characterized by within-system neuroadaptations (e.g., decreased reward circuit function) and between-system neuroadaptations (recruitment of brain stress systems) [50]. Initially, most drugs of abuse acutely activate the HPA axis, but with chronic use, the system becomes dysregulated. A crucial shift occurs from positive reinforcement (seeking a "high") to negative reinforcement (relieving the "low"), where the "dark side" of addiction—the anxiety, dysphoria, and irritability of withdrawal—is driven by CRF in brain regions like the central amygdala and BNST, beyond the hypothalamus [51] [50]. This persistent CRF activation contributes to the elevated basal cortisol levels seen in active addiction and the blunted reactivity to new challenges, reflecting a system struggling to maintain stability.
BDNF: A Mediator of Neural Plasticity
BDNF is a key molecular mediator of synaptic plasticity and memory consolidation [48]. In addiction, it plays a dual role, acting in opposing circuits to either promote or suppress drug-seeking behavior.
- Incubation of Craving: In the mesolimbic dopamine pathway, BDNF contributes to the "incubation" of craving, where drug-seeking behavior intensifies over prolonged abstinence [48].
- Extinction of Seeking: Conversely, within the hippocampal-infralimbic prefrontal cortex circuit, BDNF is critical for consolidating extinction memories, which act as a new, inhibitory memory to suppress pathological drug-seeking responses [48]. The increase in serum BDNF during abstinence that is linked to delayed relapse is thought to reflect, at least in part, this beneficial plasticity supporting extinction learning [49].
The following diagram illustrates the core signaling pathways of the HPA axis and BDNF, highlighting their points of interaction with substance use.
Diagram 1: Core Stress and Plasticity Pathways in Addiction. This diagram illustrates the key signaling pathways of the HPA axis (red) and BDNF (blue), and their interactions in the context of substance use. Chronic use leads to HPA axis dysregulation, manifesting as altered peripheral biomarker levels. BDNF acts in competing neural circuits, either promoting craving in the nucleus accumbens (NAc) or promoting the suppression of drug-seeking via the hippocampal-prefrontal cortex pathway.
Experimental Protocols for Biomarker Assessment
To ensure the reliability and reproducibility of biomarker data, standardized experimental protocols are essential.
Trier Social Stress Test (TSST) for HPA Axis Reactivity
The TSST is a widely used and validated protocol to induce a reliable psychosocial stress response in a laboratory setting [46].
- Preparation: Participants are informed they must prepare and deliver a speech and perform mental arithmetic in front of a stern, non-responsive panel.
- Speech Task (5 minutes): The participant delivers their speech. If they stop prematurely, they are prompted to continue.
- Mental Arithmetic (5 minutes): The participant is asked to serially subtract a number from a large sum (e.g., 13 from 1022). If a mistake is made, they must start over.
- Biomarker Sampling:
- Salivary Cortisol: Samples are collected at baseline (pre-test), immediately post-test, and at regular intervals thereafter (e.g., +10, +20, +30, +45, +60 minutes) to capture the stress response curve [46].
- Salivary Alpha-Amylase (sAA): Collected alongside cortisol as a marker of sympathetic nervous system (autonomic) activity [46].
- Plasma ACTH/Cortisol: Blood samples can be drawn via an indwelling catheter at similar time points for a more direct measure [45].
Assessing BDNF in Relapse Prediction
A typical clinical study protocol involves [49]:
- Participant Cohort: Recruit cocaine-dependent patients entering an inpatient detoxification program. Exclude for major psychiatric or organic comorbidities.
- Blood Sampling: Collect serum samples at two time points:
- T1: At admission (baseline, first day of abstinence).
- T2: At discharge (e.g., after 14 days of supervised abstinence).
- Biomarker Analysis: Allow blood samples to clot, centrifuge, and store the serum at -80°C. Serum BDNF levels are quantified using a commercial enzyme-linked immunosorbent assay (ELISA) kit according to the manufacturer's instructions.
- Clinical Follow-up: After discharge, patients undergo a follow-up period (e.g., 22 weeks). They are classified as "Early Relapsers" (relapse within 14 days of discharge) or "Late Relapsers" (relapse after 14 days or remain abstinent).
- Data Analysis: Compare the rate of change in serum BDNF levels (from T1 to T2) between the Early and Late Relapser groups.
The Scientist's Toolkit: Key Research Reagents
The following table lists essential reagents and materials used in the experimental assessment of these biomarkers.
Table 2: Essential Research Reagents and Materials
| Reagent/Material | Specific Function & Application |
|---|---|
| Salivary Cortisol ELISA Kit | Quantifies free, biologically active cortisol levels from saliva samples collected during stress tests like the TSST [46]. |
| High-Sensitivity ACTH ELISA Kit | Measures low-concentration plasma ACTH levels; critical for assessing pituitary response and calculating the cortisol:ACTH ratio [45]. |
| Human BDNF ELISA Kit | Quantifies total BDNF protein levels in human serum or plasma to track changes during abstinence and link to clinical outcomes [49]. |
| Salivary Alpha-Amylase (sAA) Assay Kit | Serves as a surrogate, non-invasive marker of autonomic nervous system (sympathetic) arousal, complementing HPA axis measures [46]. |
| Cortisol:ACTH Ratio | Not a reagent, but a derived measure calculated from assay results. It indicates adrenal gland sensitivity and is a putative biomarker of relapse vulnerability [45]. |
The dysregulation of the stress system, quantified by peripheral biomarkers like cortisol, ACTH, and BDNF, provides a critical window into the neurobiology of addiction relapse. The transition to a chronic, relapsing state is marked by a shift from hyper- to hypo-activation of the HPA axis and dynamic, circuit-specific changes in BDNF that influence the balance between craving and recovery. Translating these findings requires rigorous, standardized experimental protocols. Future research must focus on longitudinal studies to validate the predictive power of biomarker combinations, integrate them with neuroimaging data, and explore their utility in personalizing treatment, such as using HPA axis profiles to identify patients who may best respond to CRF1 receptor antagonists or other stress-targeting therapies.
Cue-reactivity paradigms represent a cornerstone methodology in addiction neuroscience for probing the neurobiological mechanisms underlying relapse vulnerability. These paradigms are founded on the principle that previously neutral stimuli repeatedly paired with drug consumption can, through classical conditioning, acquire potent incentive salience and become conditioned cues capable of eliciting craving and drug-seeking behaviors [52] [53]. In individuals with substance use disorders (SUDs), exposure to these drug-associated cues—whether visual, auditory, or tactile—triggers a measurable cascade of physiological, behavioral, and neural responses, collectively termed "cue-reactivity" [53]. A robust body of evidence demonstrates that this cue-induced neural hyperreactivity, particularly within brain circuits governing reward, motivation, and executive control, is strongly associated with addiction severity, craving intensity, and treatment outcomes [52]. Consequently, mapping this hyperreactivity provides a critical window into the neuroadaptations that perpetuate the cycle of addiction and heighten vulnerability to relapse, even after prolonged periods of abstinence [3] [53]. This whitepaper provides an in-depth technical guide to the design, implementation, and interpretation of cue-reactivity paradigms within the broader context of addiction relapse vulnerability research.
Experimental Paradigms and Methodologies
Core Paradigm Design
The fundamental structure of a cue-reactivity paradigm involves the presentation of drug-related cues contrasted with neutral control cues while measuring dependent variables [52]. The critical within-subject comparison is the neural and physiological response to drug-related cues versus the response to matched, neutral, non-drug-related cues [52].
Key Experimental Controls:
- Neutral Cues: Sensory-matched but emotionally neutral stimuli (e.g., images of pencils instead of cigarettes, water instead of alcohol).
- Between-Group Comparisons: Often include matched non-using control subjects to establish addiction-specific reactivity [52].
- Stimulus Matching: Careful matching of visual complexity, luminance, and presentation timing between drug and neutral cues.
Stimulus Modalities and Presentation Protocols
Cue-reactivity paradigms employ diverse stimulus modalities to engage multiple sensory pathways, enhancing ecological validity and the potency of craving induction [52] [53].
Table 1: Stimulus Modalities in Cue-Reactivity Research
| Modality | Example Stimuli | Presentation Method | Key Considerations |
|---|---|---|---|
| Visual | Pictures of drugs/paraphernalia, silent videos of use scenarios [52] [53] | Computerized presentation, often using E-Prime or Presentation software | Standardize visual angle, complexity, and exposure duration (typically 1-10 seconds) |
| Auditory | Personalized imagery scripts, drug-use sounds [52] [53] | Headphones; scripts may be pre-recorded or read live | Use personalized scripts for higher subjective craving induction |
| Audiovisual | Videos depicting drug preparation or use [52] | Combined video and audio playback | High ecological validity; difficult to perfectly match control stimuli |
| Tactile/Haptic | Handling actual drug paraphernalia (e.g., lighter, pipe) [52] | In-scanner handling of objects | Potently elicits craving; requires specialized MR-compatible materials |
| Olfactory/Gustatory | Smelling alcohol or tasting a preferred beverage [52] | Olfactometer for smell; tasteless solution as control | Technically challenging to implement in scanner environments |
| Multisensory | Combined holding a cigarette while watching smoking videos [52] | Integration of multiple modalities | Most ecologically valid; most complex to implement and control |
Implementation Workflow:
The following diagram outlines a standardized experimental workflow for a multimodal cue-reactivity study, from participant screening to data analysis.
Data Acquisition and Outcome Measures
Cue-reactivity paradigms capture multi-system responses to provide a comprehensive profile of an individual's reactivity.
Table 2: Primary Outcome Measures in Cue-Reactivity Studies
| Domain | Specific Measures | Acquisition Method | Interpretation |
|---|---|---|---|
| Neural | BOLD signal change (fMRI), glucose metabolism (PET), electrophysiology (EEG/ERP) [52] | fMRI, PET, MEG, EEG | Hyperactivation in mesocorticolimbic circuits indicates incentive salience |
| Subjective | Self-reported craving, urge, drug liking, arousal [52] | Visual Analog Scales (VAS), Questionnaires (e.g., AUQ) | Direct measure of conscious experience; subject to bias |
| Autonomic | Skin conductance response (SCR), heart rate (HR), pupillometry [53] | Biopac system, MRI-compatible electrodes | Objective indices of physiological arousal |
| Behavioral | Reaction time, attentional bias (e.g., dot-probe), approach bias [52] | Keyboard/button response, eye-tracking | Implicit measures of cognitive and motivational processes |
Critical Methodology Notes:
- Counterbalancing: The order of drug and neutral cue blocks must be randomized or counterbalanced across participants.
- Baseline Establishment: Adequate washout periods between cue presentations are essential to prevent carryover effects and allow physiological measures to return to baseline [52].
- Subjective Timing: Subjective ratings can be collected trial-by-trial for high temporal resolution or at the end of blocks to minimize task disruption [52].
Neurobiological Substrates of Cue-Reactivity
Core Neural Circuits
Drug cue-reactivity is not localized to a single brain region but emerges from the dynamic interaction of distributed, large-scale brain networks [52] [3]. The following diagram illustrates the primary neural circuits implicated in cue-reactivity and their functional roles.
Neurochemical Mechanisms
The neural circuits depicted above are modulated by complex neurochemical interactions. Chronic drug use induces lasting neuroadaptations in multiple neurotransmitter systems that underlie the heightened cue-reactivity observed in addiction [3] [19].
Table 3: Key Neurotransmitter Systems in Drug Cue-Reactivity
| System | Role in Cue-Reactivity | Key Receptors/ Molecules | Direction of Change in Addiction |
|---|---|---|---|
| Dopamine (DA) | Incentive salience attribution, reward prediction error, motivation [52] [3] | D1, D2 receptors | ↑ Phasic DA release in NAc to cues; ↓ baseline tonic DA levels [3] |
| Opioid Peptides | Regulation of hedonic tone, stress, and reward [19] | μ-opioid, κ-opioid receptors | ↑ μ-receptor stimulation (reinforcement); ↓ κ-receptor activity [19] |
| Glutamate | Synaptic plasticity, learning, memory, executive control [3] | NMDA, AMPA receptors | ↑ Corticostriatal glutamate driving compulsive seeking [3] |
| GABA | Inhibitory control, regulation of DA neurons [3] | GABA-A, GABA-B receptors | ↓ Cortical and subcortical GABA receptor binding [19] |
| CRF / Norepinephrine | Stress and anxiety responses, negative reinforcement [3] [19] | CRF1, α2 receptors | ↑ Amygdalar CRF & NE; dysregulated HPA axis response [3] |
| Serotonin (5-HT) | Mood regulation, impulse control, anti-stress effects [19] | 5-HT1A, 5-HT1B, 5-HT2A | ↓ Activity contributing to negative affect in withdrawal [19] |
| Endocannabinoids | Modulation of DA, GABA, glutamate release; stress buffering [19] | CB1, CB2 receptors | ↓ CB1 receptor density in AUD; altered signaling [19] |
The Three-Stage Addiction Cycle and Cue-Reactivity
Cue-reactivity is most potently expressed within the "preoccupation/anticipation" stage of the addiction cycle, which is characterized by a profound dysregulation of prefrontal executive control systems [3]. The following diagram integrates cue-reactivity into the broader neurobiological framework of addiction, illustrating how it drives relapse vulnerability across the three-stage cycle.
Table 4: Key Research Reagent Solutions for Cue-Reactivity Studies
| Category | Item/Resource | Specific Function/Application | Example Use |
|---|---|---|---|
| Stimulus Sets | Standardized drug/neutral picture sets (e.g., IAPS modified) | Ensure consistency and reliability of visual cue presentation across studies | Visual cue-reactivity fMRI tasks |
| Software Platforms | E-Prime, Presentation, PsychoPy | Precisely control stimulus timing and sequence, collect behavioral responses | Running the cue-exposure protocol and recording reaction times |
| Neuroimaging Analysis | SPM, FSL, AFNI, natverse (for large-scale data) [54] | Process and analyze fMRI/PET data; map neural activation and connectivity | Preprocessing BOLD data, performing group-level analysis of cue > neutral contrast |
| Physiological Recording | MRI-compatible Biopac system, eye-tracker | Acquire SCR, HR, pupillometry data synchronously with neuroimaging | Correlating amygdala BOLD signal with SCR during cue exposure |
| Computational Tools | R, Python, CBMA tools (e.g., GingerALE, Neurosynth) | Perform coordinate-based meta-analysis (CBMA), data-driven ontology mapping [55] | Synthesizing findings across 100+ studies to identify consistent activation foci |
| Databases | BrainMap, Neurosynth, NeuroVault | Access shared data, coordinate results, and decode neural patterns [55] | Reverse inference to determine mental functions associated with a cue-activated region |
Cue-reactivity paradigms provide an indispensable experimental window into the neurobiological mechanisms of relapse vulnerability in substance use disorders. The robust, quantifiable patterns of neural hyperreactivity within mesocorticolimbic circuits—notably the ventral striatum, amygdala, anterior cingulate, and prefrontal cortex—reflect core neuroadaptations that underlie the compulsive drug seeking characterizing addiction. The precise mapping of these circuits, facilitated by the standardized methodologies and analytical frameworks detailed in this whitepaper, is paving the way for a new era of targeted interventions. Future research will increasingly focus on leveraging individual differences in cue-reactivity to develop personalized therapeutic strategies, including neuromodulation, pharmacological agents, and cognitive training protocols aimed at normalizing these dysregulated circuits and enhancing resilience against relapse.
Within the neurobiological framework of addiction, the medial Prefrontal Cortex (mPFC) and Anterior Cingulate Cortex (ACC) are critical hubs of the prefrontal circuitry responsible for executive control, salience attribution, and emotional regulation. The impaired Response Inhibition and Salience Attribution (iRISA) model posits that addiction is characterized by a prefrontal dysfunction wherein drug-related cues acquire excessive salience at the expense of natural rewards, coupled with a diminished capacity for inhibitory control [24]. Atrophy within the mPFC and ACC represents a key structural correlate of this functional breakdown, directly contributing to the compulsive drug-seeking and high relapse vulnerability that define Substance Use Disorders (SUD) [24] [3]. This whitepaper synthesizes current evidence on the structural atrophy of these regions, its quantitative assessment, and its role in addiction relapse mechanisms, providing a technical guide for researchers and drug development professionals.
Quantitative Data on mPFC and ACC Atrophy in Addictive Disorders
Cross-sectional and longitudinal neuroimaging studies consistently demonstrate reduced gray matter volume (GMV) and cortical thickness in the mPFC and ACC across multiple substances of abuse. The following table summarizes key structural findings associated with chronic drug use.
Table 1: Quantitative Structural Alterations in the PFC and ACC in Substance Use Disorders
| Brain Region | Structural Change | Associated Substance | Correlates & Key Findings |
|---|---|---|---|
| Ventromedial PFC/ Orbitofrontal Cortex (vmPFC/OFC) | Lower gray matter volume [24] | Tobacco, Alcohol, Stimulants, Opioids [24] | - Cumulative effect: longer duration of use correlates with lower volume [24].- Predicts relapse; smaller volume associated with earlier relapse [24]. |
| Anterior Cingulate Cortex (ACC) | Lower gray matter volume [24] | Tobacco, Alcohol, Stimulants, Opioids [24] | - Involved in error monitoring and reward-based decisions [24].- Specific reduction in dorsal ACC (dACC) linked to impulsive behavior in SUD [56]. |
| Dorsolateral PFC (dlPFC) | Lower gray matter volume [24] | Alcohol, Stimulants [24] | - Associated with impaired attention allocation and working memory [24].- Negative correlation between years of use and dlPFC volume [24]. |
| Prefront Cortex (Broad) | Gray matter atrophy | Alcohol | Volume recovery observed with abstinence; increases seen at 1 month, nearing healthy control levels by 7.5 months [24]. |
| Inferior Frontal Gyrus (IFG)/ Ventrolateral PFC (vlPFC) | Lower gray matter volume [24] | Tobacco, Stimulants [24] | - Key region for response selection and inhibition [24].- Increased volume following cocaine use reduction correlates with better decision-making [24]. |
The relationship between substance use and prefrontal structure is dynamic. Evidence suggests that at least some of these atrophic changes are reversible with sustained abstinence, indicating a component of neuroplastic recovery. Furthermore, baseline prefrontal volume may serve as a biomarker for treatment outcome, with smaller volumes predicting a higher likelihood of relapse [24].
Experimental Protocols for Investigating Structure-Function Relationships
To establish causal links between mPFC/ACC dysfunction and addictive behaviors, researchers employ sophisticated experimental protocols, often in preclinical models. The following details a key experiment investigating ACC deep brain stimulation (DBS) as a potential intervention for opioid use disorder.
Table 2: Key Experimental Protocol: Deep Brain Stimulation of the ACC in a Rodent Model of Opioid Addiction
| Protocol Component | Detailed Methodology |
|---|---|
| Objective | To investigate the effects of high-frequency DBS of the ACC on the acquisition, extinction, and reinstatement of morphine-induced conditioned place preference (CPP) in rats [56]. |
| Subjects | Male Wistar rats (108 total), housed under standard conditions with a 12-hour light/dark cycle [56]. |
| Surgical Procedure | - Anesthesia: Ketamine (100 mg/kg) and xylazine (10 mg/kg) via intraperitoneal injection.- Stereotaxic Implantation: Bipolar electrodes bilaterally implanted into the ACC (coordinates from Bregma: AP +2 mm, ML ±0.6 mm, DV -3 mm). Electrodes secured to the skull with dental acrylic [56]. |
| Behavioral Paradigm (CPP) | - Preconditioning: Rats freely explore a 3-compartment arena to establish baseline preference.- Conditioning (3 days): Rats receive morphine (3, 5, 7 mg/kg, SC) in their non-preferred compartment and saline in their preferred compartment.- Post-conditioning Test: Measures time spent in the drug-paired compartment, indicating reward learning.- Extinction Phase: Daily drug-free exposure to the arena until preference is extinguished.- Reinstatement Test: A priming dose of morphine is given to provoke relapse of drug-seeking behavior [56]. |
| DBS Intervention | - Applied at 130 Hz with two intensity levels (150 µA and 200 µA).- Tested during the acquisition phase and the extinction phase [56]. |
| Outcome Measures | - Behavioral: Time spent in morphine-paired compartment during CPP tests; performance in novel object recognition (NOR) and open field tests (OFT).- Molecular: post-mortem measurement of c-Fos protein expression (a marker of neuronal activity) in the NAc and PFC [56]. |
Diagram 1: ACC DBS Experiment Workflow. This flowchart outlines the key phases and outcomes of the preclinical protocol investigating ACC DBS effects on opioid addiction behaviors [56].
Molecular and Systems-Level Mechanisms Linking Atrophy to Relapse
The structural atrophy observed in the mPFC and ACC is underpinned by a cascade of neuroadaptations that hijack normal cognitive and emotional processes, creating a brain state vulnerable to relapse.
- Dopaminergic Dysregulation and Incentive Salience: Chronic drug use alters dopaminergic signaling from the midbrain to the PFC and striatum. This process, known as "incentive salience," shifts dopamine release from the drug itself to drug-associated cues (people, places, paraphernalia). This creates powerful motivational urges and cravings, which the atrophied PFC struggles to inhibit [3].
- Recruitment of Brain Stress Systems: The "withdrawal/negative affect" stage of addiction involves the overactivation of brain stress systems in the extended amygdala (e.g., increased corticotropin-releasing factor (CRF) and norepinephrine). This upregulation produces a persistent state of anxiety, irritability, and dysphoria during abstinence. The mPFC and ACC, which normally help regulate these stress responses, are functionally impaired, making the individual more vulnerable to using drugs again for negative reinforcement [3].
- Executive Dysfunction and the Preoccupation/Anticipation Stage: In the third stage of the addiction cycle, atrophy and dysfunction in the PFC circuits manifest as executive failure. This includes diminished impulse control, impaired emotional regulation, and poor decision-making. The "Go" system (involving the dlPFC and ACC), which drives goal-directed behavior, becomes hyper-focused on drug seeking, while the "Stop" system (involving the vlPFC/IFG), which provides inhibitory control, is significantly weakened. This imbalance is a core mechanism underlying the compulsive drug seeking and relapse that characterizes addiction [3].
Diagram 2: Addiction Neuroadaptation Pathways. This diagram illustrates the key neurobiological pathways through which mPFC/ACC dysfunction drives relapse vulnerability [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing research on mPFC and ACC atrophy requires a suite of sophisticated tools and reagents. The following table details essential resources for conducting experiments in this field.
Table 3: Research Reagent Solutions for Investigating PFC/ACC in Addiction
| Tool / Reagent | Function & Application |
|---|---|
| 3 Tesla MRI Scanner | High-field magnetic resonance imaging for acquiring high-resolution T1-weighted structural images to quantify gray matter volume and cortical thickness [57] [58]. |
| Stereotaxic Apparatus | Precision surgical instrument for targeting specific brain regions (e.g., ACC, mPFC) in rodent models for electrode implantation (DBS) or microinjections [56]. |
| Deep Brain Stimulation (DBS) Electrodes | Chronic implanted electrodes for delivering controlled electrical stimulation to modulate neural activity in specific circuits, used to test causal relationships [56]. |
| Conditioned Place Preference (CPP) Apparatus | Behavioral setup consisting of multiple compartments with distinct contextual cues to measure the rewarding or aversive effects of drugs [56]. |
| c-Fos Antibodies | Immunohistochemistry reagents to detect c-Fos protein expression, a marker of recent neuronal activation, allowing mapping of brain activity in response to drugs or stimuli [56]. |
| Structural MRI Analysis Software (e.g., CAT12, FSL, FreeSurfer) | Automated pipelines for processing T1-weighted MRI data to perform voxel-based morphometry (VBM) and calculate regional brain volumes [58]. |
| Diffusion Tensor Imaging (DTI) | An MRI technique that measures the diffusion of water molecules to map white matter tracts and assess the integrity of structural connections to/from the PFC/ACC [59]. |
The evidence is compelling: atrophy of the medial Prefrontal and Anterior Cingulate Cortex is a central pathological feature of addictive disorders, directly contributing to the relapse vulnerability that sustains the addiction cycle. The quantitative structural deficits in these regions correlate with key behavioral manifestations of addiction, including cue-reactivity, craving, and loss of inhibitory control. Preclinical models, utilizing interventions like DBS, are beginning to establish a causal link, suggesting that neuromodulation of these circuits could hold therapeutic promise.
Future research must focus on longitudinal human studies to better distinguish pre-existing vulnerabilities from substance-induced damage. Furthermore, the development of non-invasive neuromodulation techniques (e.g., TMS, tDCS) targeting the mPFC and ACC, informed by the detailed structural and functional maps, represents a critical frontier for developing novel, mechanism-based treatments for addiction.
Assessing Impulsivity and Cognitive Control: Behavioral and Neural Metrics
Impulsivity, a multifaceted construct characterized by actions that are poorly conceived, prematurely expressed, unduly risky, and that often result in undesirable outcomes, represents a significant transdiagnostic endophenotype for numerous psychiatric disorders [60] [61]. Within the context of addiction, impulsivity is not merely a consequence of substance use but is a premorbid vulnerability that predates and perpetuates the cycle of addiction and relapse [61] [62]. Understanding the precise behavioral and neural metrics of impulsivity and cognitive control is therefore paramount for advancing research into the neurobiology of addiction relapse vulnerability. This guide provides a comprehensive technical overview of the dominant experimental paradigms, their underlying neural correlates, and the application of these metrics in predicting relapse, with the aim of equipping researchers and drug development professionals with the tools necessary for mechanistic investigation and therapeutic discovery.
Behavioral Metrics and Experimental Protocols
Behavioral tasks dissect impulsivity into several dissociable neurocognitive dimensions, primarily impulsive action (encompassing motor and attentional disinhibition) and impulsive choice (encompassing delay discounting and decision-making) [60] [61]. The table below summarizes the key behavioral tasks used to quantify these constructs.
Table 1: Key Behavioral Paradigms for Assessing Impulsivity and Cognitive Control
| Construct | Task Name | Primary Metric | Protocol Summary | Neurocognitive Process Measured |
|---|---|---|---|---|
| Motor Disinhibition | Go/No-Go (GNG); Affective GNG | Commission Errors (False Alarms) | Participants respond to frequent "Go" stimuli and must inhibit responses to rare "No-Go" stimuli. The affective variant uses emotional stimuli. | Ability to suppress a prepotent motor response [60]. |
| Attentional Disinhibition | Stroop Color-Word Test | Interference Score (Reaction Time Difference) | Participants name the ink color of color-words that are incongruent (e.g., "RED" printed in blue ink). | Ability to resolve cognitive conflict and inhibit automatic responses (word reading) [63] [60]. |
| Delay Discounting | Monetary Choice Questionnaire (MCQ) | Discounting Parameter (k) | Participants make a series of choices between a smaller, immediate reward and a larger, delayed reward. The parameter k quantifies the devaluation of delayed rewards. | Preference for immediate gratification; impulsive choice [60] [64]. |
| Decision-Making | Iowa Gambling Task (IGT) | Net Score (Advantageous - Disadvantageous Decks) | Participants select cards from four decks that differ in immediate reward magnitude and long-term惩罚. | Ability to forego short-term high rewards to avoid long-term losses; sensitivity to future consequences [60]. |
| Attention & Cognitive Load | Dichotic Listening Task | False Alarms, Intrusion Errors | Participants attend to one ear while ignoring the other. The "mixed" condition involves switching attention between ears, increasing cognitive load [63]. | Auditory selective attention and the effect of attention switching on response inhibition [63]. |
Detailed Experimental Protocols
Protocol for the Affective Go/No-Go Task [60]:
- Stimuli: A series of words with positive, negative, or neutral emotional valence are presented.
- Procedure: The "Go" stimulus (e.g., a specific emotional valence like positive words) is designated for a block of trials. Participants are instructed to press a button as quickly as possible upon seeing a "Go" stimulus and to withhold the response for "No-Go" stimuli (other valences).
- Key Variables:
- Independent Variable: Emotional valence of the "No-Go" stimuli.
- Dependent Variable: Number of commission errors (responses to "No-Go" stimuli), particularly in positive or negative affective contexts.
- Rellevance to Relapse: Commission errors on the affective GNG have been longitudinally associated with relapse at 3 and 12 months in outpatients with substance use disorders (SUD), suggesting affective contexts exacerbate disinhibition in vulnerable individuals [60].
Protocol for Delay Discounting using the Monetary Choice Questionnaire (MCQ) [64]:
- Stimuli: A series of hypothetical choices (e.g., "Would you prefer $27 today or $50 in 21 days?").
- Procedure: Participants make a series of choices. The amounts and delays are systematically varied to estimate an individual's indifference point—the point at which the immediate and delayed rewards are perceived as equally valuable.
- Data Analysis: Indifference points across delays are fit to a hyperbolic discounting function: V = A / (1 + kD), where V is the subjective value, A is the actual reward amount, D is the delay, and k is the subject-specific discounting parameter. A higher k indicates steeper discounting and greater impulsivity.
- Therapeutic Application: Episodic Future Thinking (EFT), which involves vividly imagining positive future events, has been shown to reduce delay discounting and is associated with changes in prefrontal and hippocampal activity, highlighting its potential as a therapeutic intervention [65].
Neural Metrics and Circuitry
The distinct behavioral dimensions of impulsivity are subserved by dissociable, though partially overlapping, large-scale brain networks. A meta-analytic approach confirms that decision-making and response inhibition map onto two distinct functional systems [66].
Neural Circuits of Impulsivity
The following diagram illustrates the primary brain networks implicated in different facets of impulsivity and cognitive control, as identified in functional neuroimaging studies.
Figure 1: Neural Circuits of Impulsivity and Cognitive Control. Diagram depicting the dissociable brain networks underlying impulsive action (red), impulsive choice (green), and the role of large-scale networks like the DMN (blue) and executive dysfunction (gray) in relapse vulnerability. pre-SMA: pre-supplementary motor area; aMCC: anterior midcingulate cortex.
Relapse-Specific Neural Alterations
Longitudinal neuroimaging studies in individuals with substance use disorders have identified specific neural signatures of relapse vulnerability. Research in abstinent methamphetamine-dependent individuals (MADIs) who subsequently relapsed revealed:
- During Abstinence (Stage I): Increased activity in the bilateral putamen compared to healthy controls [8]. This hyperactivation in a key region of the habit and reward system may represent a latent vulnerability to cue-induced craving and automatic drug-seeking behavior.
- After Relapse (Stage II): A more widespread pattern of abnormality emerges, characterized by hypoactivity in parietal and occipital regions (involved in sensory integration and attention) and hyperactivity in subcortical regions (striatum, thalamus, hippocampus) and prefrontal areas [8]. This suggests relapse itself exacerbates neural dysfunction, further entrenching the addiction cycle.
These findings are consistent with the established three-stage addiction cycle (binge/intoxication, withdrawal/negative affect, preoccupation/anticipation), where the prefrontal cortex is "hijacked" during the preoccupation stage, leading to executive dysfunction, diminished impulse control, and heightened craving [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Research on Impulsivity and Relapse
| Tool / Reagent | Function / Application | Example Use-Case |
|---|---|---|
| Barratt Impulsiveness Scale (BIS-11) | Self-report measure of trait impulsivity. | Correlating trait personality measures with behavioral task performance or neural activation [63]. |
| fMRI-Compatible Response Box | Collects behavioral responses (RT, accuracy) inside the MRI scanner. | Simultaneously measuring brain activity and performance on Go/No-Go or Stroop tasks [66] [8]. |
| DPABI / FSL / SPM Software | Preprocessing and statistical analysis of functional and structural MRI data. | Calculating fALFF/ReHo to index regional brain activity, or performing functional connectivity analysis [8]. |
| Activation Likelihood Estimation (ALE) | Coordinate-based meta-analysis technique for neuroimaging data. | Identifying consistent neural activation patterns across multiple studies of response inhibition or delay discounting [66]. |
| GLP-1 Receptor Agonists | Pharmacological probes to investigate reward pathways. | Testing the hypothesis that GLP-1 signaling reduces alcohol cravings by modulating brain reward pathways [65]. |
| International Quit & Recovery Registry | Global cohort for longitudinal study of recovery mechanisms. | Identifying psychosocial and neurocognitive factors that predict long-term success in recovery [65]. |
Impulsivity as a Predictor of Relapse Vulnerability
Converging evidence from behavioral and neuroimaging studies solidifies the role of impulsivity as a critical predictor of relapse. A longitudinal study with SUD outpatients found that performance on behavioral measures of attentional impulsivity (Stroop test) and affective motor disinhibition (Affective Go/No-Go) significantly predicted relapse at 3 and 12 months, while not being associated with treatment dropout [60]. This underscores a specific pathway from disinhibition to resumed drug use, distinct from general treatment adherence.
From a neurobiological perspective, the high relapse rate in addiction is partly mediated by impulsive processes that can be categorized into three neurocognitive models [62]:
- Automaticity: An overlearned, stimulus-bound drug-seeking habit that occurs rapidly and outside conscious awareness, linked to dorsal striatal circuits.
- Deficient Response Inhibition: The inability to suppress these pre-potent drug-seeking behaviors, associated with deficits in the right inferior frontal gyrus and anterior cingulate cortex.
- Impaired Decision-Making: A slower process involving poor assessment of long-term consequences, linked to the ventromedial prefrontal cortex and orbitofrontal cortex.
In conclusion, the precise assessment of behavioral and neural metrics of impulsivity provides a powerful framework for understanding the mechanisms underlying relapse vulnerability. The integration of standardized behavioral protocols, neuroimaging, and emerging pharmacological tools, as outlined in this guide, offers a robust pathway for identifying at-risk individuals, developing targeted neuromodulatory interventions, and evaluating novel therapeutics in the ongoing effort to treat addiction.
Addictive disorders (AD) represent a significant public health crisis, yet their diagnosis remains grounded in clinical presentation rather than etiology or neurobiological process. The current diagnostic approach for Alcohol Use Disorder (AUD) and other substance use disorders, based on DSM-5 symptom counts, creates considerable within-diagnosis heterogeneity. Patients can reach the same diagnostic endpoint through different pathways and from distinctly different starting points of vulnerability [67] [68]. This heterogeneity poses a major barrier to treatment development and application, as individuals with the same diagnosis may respond differently to interventions based on their underlying neurobiological profile.
The Addictions Neuroclinical Assessment (ANA) represents a paradigm shift from purely behavioral diagnosis to a neuroscience-informed framework that captures core functional domains derived from the neurocircuitry of addiction [69]. This approach aligns with precision medicine goals by addressing individual variability in the genetic, environmental, and neurobiological factors that contribute to addictive disorders [70]. By focusing on transdiagnostic functional domains that cut across traditional diagnostic categories, ANA provides a more nuanced understanding of addiction heterogeneity that can inform targeted interventions and improve outcomes.
Theoretical Foundation: The Addiction Cycle and ANA Domains
The ANA framework is conceptually grounded in the addiction cycle model proposed by Koob and Volkow, which describes the progressive dysregulation of brain circuits that leads to compulsive drug use [69] [67]. This cycle comprises three recurring stages that feed into one another: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. Each stage involves distinct neural circuitry and behavioral manifestations that the ANA aims to capture through standardized assessment.
The Three Core Neurofunctional Domains of ANA
The ANA framework operationalizes the addiction cycle through three primary neurofunctional domains, each measured through a combination of behavioral tasks, self-report measures, and neuroimaging paradigms:
Incentive Salience (IS)
The Incentive Salience domain encompasses processes involved in reward, motivational salience, and habit formation, corresponding to the binge/intoxication stage of addiction [71]. This domain reflects the neuroadaptations that cause drugs and drug-associated cues to become increasingly salient, automatically grabbing attention and triggering craving and drug-seeking behavior. Recent research has identified that IS comprises two distinct subfactors: alcohol motivation (reward-driven drinking behavior) and alcohol insensitivity (low response to alcohol effects) [71]. Neuroimaging studies have shown that incentive salience is correlated with alcohol cue-elicited activation in reward-learning and affective regions including the insula and posterior cingulate cortices, though interestingly not with cue-elicited activation in the dorsal or ventral striatum as traditionally hypothesized [72].
Negative Emotionality (NE)
The Negative Emotionality domain captures negative affective states resulting from withdrawal and long-term drug use, corresponding to the withdrawal/negative affect stage of addiction [73] [71]. This domain reflects the dysregulation of brain stress systems that leads to heightened emotional distress, anxiety, irritability, and dysphoria during abstinence, which in turn motivates drinking to obtain relief. Factor analyses have revealed that NE comprises three subfactors: internalizing (depression, anxiety), externalizing (anger, aggression), and psychological strength (resilience factors) [71]. This domain has demonstrated strong measurement invariance across time and gender, and changes in negative emotionality have been shown to correlate with changes in drinking patterns, highlighting its clinical relevance [73] [74].
Executive Function (EF)
The Executive Function domain comprises cognitive functions related to inhibitory control, decision making, and planning of future goals, corresponding to the preoccupation/anticipation stage of addiction [71]. This domain reflects the prefrontal cortex dysfunction that undermines self-regulatory capacity and permits impulses and habits to dominate behavior. EF is the most complex of the three domains, consisting of five identified subfactors: inhibitory control, working memory, rumination, interoception, and impulsivity [71]. Importantly, deficits in this domain contribute to the inability to maintain abstinence despite negative consequences and the heightened vulnerability to relapse triggered by cues, stressors, or drug priming.
Quantitative Assessment of ANA Domains: Standardized Measures and Psychometric Properties
The ANA framework employs a multimodal assessment approach combining neuropsychological tasks, self-report instruments, and neuroimaging paradigms to quantify functioning across the three core domains. Recent research has refined the original assessment battery to improve feasibility while maintaining comprehensive coverage of the target constructs.
Table 1: Standardized Measures for ANA Domain Assessment
| Domain | Subfactors Identified | Primary Assessment Methods | Key Measures | Psychometric Properties |
|---|---|---|---|---|
| Incentive Salience | Alcohol Motivation, Alcohol Insensitivity | Behavioral Tasks, Self-Report | Alcohol Stroop, OCDS, AUQ | Alcohol Motivation shows strongest classification accuracy for AUD [71] |
| Negative Emotionality | Internalizing, Externalizing, Psychological Strength | Self-Report, Clinical Interviews | BDI, BAI, STAXI-T, DrInC | Excellent fit (CFI=0.95-0.98), time and gender invariant [73] [71] |
| Executive Function | Inhibitory Control, Working Memory, Rumination, Interoception, Impulsivity | Neuropsychological Tasks, Self-Report | Stop Signal Task, Digit Span, SSS, SCS | Five-factor structure, impulsivity subfactor shows strong AUD classification [71] |
The ANA battery has undergone significant refinement to address practical implementation concerns. The original assessment was estimated to require approximately 10 hours to complete [70], presenting challenges for widespread adoption in research and clinical settings. Recent studies have developed more streamlined versions that maintain comprehensive coverage while reducing participant burden [73] [71]. This improved feasibility has facilitated the administration of the ANA battery across diverse settings, including both inpatient treatment programs and community samples [71].
Table 2: Classification Accuracy of ANA Domain Factors for Problematic Drinking and AUD
| ANA Factor | AUC for Problematic Drinking | AUC for AUD Diagnosis | Key Correlates |
|---|---|---|---|
| Alcohol Motivation | 0.81 | 0.85 | Strongest correlation with impulsivity (r=0.44) [71] |
| Alcohol Insensitivity | 0.79 | 0.82 | Cross-correlated with internalizing (r=0.24) [71] |
| Impulsivity | 0.77 | 0.80 | Cross-correlated with alcohol motivation (r=0.44) [71] |
| Internalizing | 0.68 | 0.71 | Associated with drinking to cope motives [73] |
Experimental Protocols for ANA Domain Assessment
Standardized ANA Battery Administration Protocol
The implementation of a standardized ANA assessment follows specific methodological procedures to ensure reliability and validity across different populations and settings:
Participant Preparation: Participants should have a negative breath alcohol concentration prior to assessment. For those in treatment programs, testing should occur after completion of detoxification and documentation of no withdrawal symptoms using standardized instruments such as the Clinician Institute Withdrawal Assessment (CIWA-Ar) [71].
Assessment Structure: The full ANA battery is administered in four testing blocks, with the order of blocks randomized across participants. Within each block, behavioral assessments always precede questionnaires to minimize carryover effects. Participants should be offered 15-minute breaks between blocks to reduce fatigue-related response bias [71].
Task Administration: Behavioral tasks are typically administered using standardized software platforms such as Inquisit 5 (Millisecond Software LLC), with specific versions of tasks available through the Millisecond Test Library to ensure consistency across research sites [71].
Data Collection: In addition to primary ANA measures, comprehensive demographic information, detailed alcohol use history, family history of alcohol problems, and comorbid psychiatric conditions should be collected using structured interviews such as the Structured Clinical Interview for DSM-5 (SCID-5) [71].
Neuroimaging Protocols for ANA Validation
Functional magnetic resonance imaging (fMRI) provides critical neural validation for the ANA domains. The following protocol outlines the approach for investigating the neural correlates of the Incentive Salience domain:
Task Design: Participants complete a cue-reactivity task during fMRI scanning. This task presents alcohol-related cues and matched neutral cues in a block or event-related design while measuring blood oxygen level-dependent (BOLD) response.
Image Acquisition: Scanning parameters typically include: whole-brain coverage with TR=2000ms, TE=30ms, flip angle=75°, voxel size=3×3×3mm. High-resolution T1-weighted anatomical images are also acquired for registration.
Analysis Pipeline: Preprocessing includes realignment, normalization to standard stereotactic space, and spatial smoothing. First-level general linear models contrast alcohol cue vs. neutral cue conditions. Second-level analyses examine correlations between cue-elicited activation and incentive salience factor scores, controlling for age, sex, medication status, and smoking status [72].
Region of Interest Analysis: A priori ROIs include the ventral and dorsal striatum. Whole-brain analyses are also conducted to explore involvement of other reward-related regions [72].
Research Reagent Solutions: Essential Materials for ANA Implementation
Table 3: Essential Research Materials and Assessment Tools for ANA Domain Measurement
| Category | Specific Tool/Assessment | Primary Domain | Function/Application | Availability |
|---|---|---|---|---|
| Neuropsychological Tasks | Stop Signal Task | Executive Function | Measures response inhibition capacity | Millisecond Test Library |
| Alcohol Stroop Task | Incentive Salience | Assesses attentional bias to alcohol cues | Millisecond Test Library | |
| Digit Span Task | Executive Function | Measures working memory capacity | Millisecond Test Library | |
| Self-Report Measures | Beck Depression Inventory (BDI) | Negative Emotionality | Quantifies depressive symptom severity | Public Domain |
| Beck Anxiety Inventory (BAI) | Negative Emotionality | Assesses anxiety symptom severity | Public Domain | |
| Obsessive Compulsive Drinking Scale (OCDS) | Incentive Salience | Measures alcohol-related obsessions and compulsions | Public Domain | |
| Sensation Seeking Scale (SSS) | Executive Function | Assesses impulsivity and novelty seeking | Public Domain | |
| Clinical Interviews | Structured Clinical Interview for DSM-5 (SCID-5) | All Domains | Determines AUD and comorbid diagnoses | Licensed |
| Timeline Followback (TLFB) | All Domains | Quantifies alcohol consumption patterns | Public Domain | |
| Neuroimaging Paradigms | Alcohol Cue-Reactivity Task | Incentive Salience | Measures neural response to alcohol cues | Custom Implementation |
Integration with Broader Research Initiatives: Reverse Translation and Precision Medicine
The ANA framework aligns with several major research initiatives aimed at advancing the neuroscience of psychiatric disorders. Most notably, it shares conceptual foundations with the Research Domain Criteria (RDoC) project from the National Institute of Mental Health, which seeks to develop a neuroscience-based classification system for mental disorders [69]. The ANA can be viewed as a substance-specific instantiation of the RDoC framework, adapting its principles specifically for addictive disorders.
A key strength of the ANA is its utility for reverse translational research - the process of translating findings from human studies back to animal models to elucidate underlying mechanisms [67] [68]. The three ANA domains have orthologous counterparts in animal models, enabling researchers to:
- Investigate neurobiological mechanisms underlying domain-specific deficits using controlled animal experiments
- Develop novel pharmacological and behavioral interventions targeting specific domains
- Identify biomarkers that predict treatment response based on domain profiles
The ANA framework also facilitates precision medicine approaches to addiction treatment by enabling the matching of interventions to individual patients based on their specific profile across the three domains [73] [70]. For example:
- Individuals with high Incentive Salience may respond best to interventions that target cue reactivity and reward processing, such as naltrexone or cue exposure therapy.
- Those with high Negative Emotionality may benefit from treatments focusing on emotional regulation and stress management, such as acamprosate or mindfulness-based relapse prevention.
- Patients with significant Executive Function impairments may show improved outcomes with approaches that enhance cognitive control and compensatory strategy use, such as cognitive remediation or cognitive behavioral therapy.
Future Directions and Implementation Challenges
While the ANA framework shows significant promise for advancing addiction research and treatment, several challenges remain for widespread implementation. First, further refinement of the assessment battery is needed to optimize the balance between comprehensive coverage and practical feasibility [70]. This may involve developing abbreviated versions for specific clinical settings or utilizing computerized adaptive testing methods that tailor question selection based on previous responses.
Second, additional research is needed to establish robust neurobiological markers for each domain and to validate their utility in predicting treatment response and long-term outcomes [72]. Large-scale, multisite studies that implement the ANA battery across diverse populations will be essential for establishing normative values and evaluating measurement invariance across different demographic and clinical groups.
Finally, implementation science approaches will be needed to facilitate the integration of ANA-based assessment into real-world clinical practice. This includes developing clinician training protocols, decision support tools for interpreting ANA profiles, and treatment matching algorithms that can guide personalized intervention selection. As these challenges are addressed, the ANA framework holds substantial potential to transform our approach to addiction diagnosis, treatment, and prevention by embedding neuroscience directly into clinical practice.
Addressing Heterogeneity and High-Risk Profiles in Relapse Prevention
This technical guide provides a framework for identifying high-risk phenotypes within substance use disorders (SUDs), integrating clinical, behavioral, and biological stratification. Framed within the neurobiology of addiction relapse vulnerability, this whitepaper details the primary triggers, underlying neural pathways, and advanced methodologies for risk prediction. It presents quantitative data summaries, standardized experimental protocols for relapse research, visualizations of core signaling pathways, and essential research reagent solutions to facilitate translational research aimed at improving treatment retention and reducing relapse.
Relapse, the resumption of drug-taking after periods of abstinence, remains the most significant challenge in treating substance use disorders [39]. Vulnerability to relapse is perpetuated by lasting neural changes resulting from both chronic drug exposure and learning processes associated with drug-related stimuli [39]. Contemporary models define addiction as a chronic, relapsing disorder marked by specific neuroadaptations that predispose an individual to pursue substances despite negative consequences [3]. Identifying high-risk phenotypes—subgroups of individuals sharing distinct clinical, behavioral, and biological characteristics that predict treatment attrition and relapse—is therefore critical for developing targeted interventions. This guide synthesizes current research on stratification methods to advance personalized treatment in addiction medicine.
Quantitative Data Synthesis: Outcome Metrics and Predictors
The evaluation of SUD treatment effectiveness and risk stratification relies on heterogeneous metrics. The following tables standardize key outcome variables and predictive factors identified from recent literature.
Table 1: Core Outcome Variables for SUD Treatment and Relapse Research
| Variable Category | Variable | Operational Definition & Common Metrics |
|---|---|---|
| Substance Use | Abstinence | Self-report of no drug/alcohol use; verified by biological samples (e.g., urine tests); measured over defined periods (e.g., prior 30 days, 3 months) [75]. |
| Relapse | Reinitiation of drug-seeking/taking after abstinence; can be defined by a single use, a return to regular use, or meeting diagnostic criteria for SUD again [75]. | |
| Treatment Process | Dropout / Attrition | Leaving treatment against medical advice (AMA) or before completion; high prevalence (40-70%) and associated with negative sequelae [75] [76]. |
| Retention / Adherence | Duration of stay in a treatment program; attendance at scheduled therapy sessions; associated with long-term positive outcomes [75]. | |
| Readmission | Re-enrollment in a treatment program within a specified period after discharge [75]. | |
| General Wellbeing | Quality of Life (QoL) | Assessment of an individual's overall well-being and functioning across physical, psychological, and social domains [75]. |
Table 2: Robust Predictors of Treatment Attrition and Relapse Vulnerability
| Predictor Category | Specific Factor | Association with Risk |
|---|---|---|
| Clinical & Demographic | Treatment Center & Program Type | Most robust predictor of treatment discontinuation in machine learning models [76]. |
| Age | Younger age is consistently associated with higher risk of treatment dropout [76]. | |
| Employment Status | Unemployment predicts higher risk of treatment attrition [76]. | |
| Substance Use Patterns | Primary Drug at Intake | Certain substances (e.g., heroin, prescription opioids) are linked to higher dropout rates [76]. |
| Frequency of Use at Intake | More frequent use prior to treatment predicts poorer retention [76]. | |
| Neurobiological | Stage of Addiction Cycle | The cyclical stages of binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation involve distinct brain regions and neuroadaptations that perpetuate relapse vulnerability [3]. |
| Incentive Salience | Dopaminergic firing in the basal ganglia shifts from responding to the drug itself to anticipating reward-related cues (people, places, things), driving motivational urges [3]. |
Experimental Protocols: Methodologies for Relapse Research
To ensure reproducibility and cross-study comparisons, researchers should adhere to standardized protocols. Below are detailed methodologies for key experiments.
The Reinstatement Model of Relapse
This animal model is a gold standard for studying relapse triggers [39].
1. Self-Administration Training:
- Subjects: Laboratory rats or mice.
- Apparatus: Operant conditioning chambers equipped with two levers (active and inactive) and a cue light.
- Procedure: Animals are trained to self-administer a drug (e.g., cocaine, heroin) by pressing the active lever. Each active lever press results in an intravenous drug infusion paired with a conditioned stimulus (CS), such as a light or tone. Sessions typically run for 2-6 hours daily until stable responding is achieved.
2. Extinction Training:
- Procedure: The drug is no longer available. Pressing the active lever has no programmed consequence (i.e., no drug infusion and no CS presentation). This phase continues until the animal's lever-pressing behavior is significantly reduced to a pre-determined criterion (e.g., <10-15 responses per session).
3. Reinstatement Test:
- Procedure: While the drug remains unavailable, one of three precipitating factors is introduced:
- Drug-Induced Reinstatement: A non-contingent, priming injection of the previously self-administered drug is given before the session.
- Cue-Induced Reinstatement: Pressing the active lever results in the presentation of the CS previously paired with the drug.
- Stress-Induced Reinstatement: A mild stressor (e.g., intermittent footshock) is administered before the session.
- Outcome Measure: The resumption of active lever pressing during the test session, compared to responding during extinction, indicates reinstatement of drug-seeking behavior.
- Procedure: While the drug remains unavailable, one of three precipitating factors is introduced:
Machine Learning for Predicting Treatment Attrition
Predicting real-world treatment dropout requires handling complex, multi-faceted data [76].
1. Data Collection:
- Cohort: Large datasets from SUD treatment facilities (e.g., N > 29,000).
- Predictors: Collect a wide range of variables at treatment intake, including:
- Demographics: Age, employment status, living situation.
- Substance Use: Primary drug, frequency of use in the month before and at intake.
- Clinical Indices: Co-occurring psychiatric and physical health diagnoses.
- Treatment Characteristics: Treatment center type, program modality.
2. Model Training and Validation:
- Algorithm: Implement a Random Forest classifier, an ensemble machine learning method effective for correlated predictors.
- Process:
- Split data into training and testing sets.
- Grow multiple decision trees on bootstrap samples from the training data.
- The final classification (e.g., "dropout" vs. "completer") is based on a majority vote across all trees.
- Validation: Assess model performance on the held-out test set using Area Under the Curve (AUC), negative predictive value, and positive predictive value.
Visualizing Core Signaling Pathways in Relapse Vulnerability
The neurobiology of addiction relapse involves dysregulation in several key brain systems. The following diagrams, generated with Graphviz, map these critical relationships.
The Three-Stage Addiction Cycle
This diagram illustrates the recurrent cycle of addiction and its primary neural substrates [3].
Neural Circuitry of Relapse Triggers
This diagram outlines the primary neural pathways mediating different triggers of relapse [3] [39].
The Scientist's Toolkit: Essential Research Reagent Solutions
This table catalogs key reagents, databases, and software tools essential for research in this field.
Table 3: Essential Research Reagents and Resources for Stratification Studies
| Category | Item / Resource | Function and Application |
|---|---|---|
| Bioinformatic Databases | Reactome [77] [78] | A curated database of biological pathways for model organisms. Used for pathway enrichment analysis and biological context interpretation of -omics data. |
| WikiPathways [77] | An open-source, user-curated pathway resource. Useful for creating and visualizing custom pathways relevant to addiction neurobiology. | |
| Pathway Commons [77] | A meta-database integrating multiple public pathway and interaction data sources. Provides a more holistic network view. | |
| Data Analysis Tools | R / ggplot2 [79] | A programming language and library for statistical computing and advanced data visualization, essential for creating publication-quality graphs. |
| PathVisio [77] | A stand-alone application for pathway analysis and visualization, allowing customization of pathway maps and overlay of experimental data. | |
| Pathview [77] | An R package for pathway-based data integration and visualization, supporting genomic, proteomic, and metabolomic data. | |
| Experimental Models | Reinstatement Model [39] | A behavioral paradigm in animals to study drug-seeking behavior precipitated by drugs, cues, or stress. Critical for testing relapse vulnerability. |
| Addictions Neuroclinical Assessment (ANA) [3] | A clinical instrument that translates the three neurobiological stages of addiction into measurable neurofunctional domains for human assessment. | |
| Molecular Reagents | Specific Receptor Antagonists | Pharmacological tools (e.g., dopamine, opioid, CRF receptor antagonists) used to dissect the contribution of specific neurotransmitter systems to relapse behavior in animal models [39]. |
Stratifying high-risk phenotypes in addiction requires a multi-dimensional approach that converges clinical predictors, behavioral paradigms, and a deep understanding of the underlying neurobiology. The integration of advanced computational methods like machine learning with robust experimental models of relapse holds significant promise for identifying individuals at greatest risk for treatment failure and relapse. Future research must focus on validating these stratified models in diverse clinical populations and translating these insights into targeted, circuit-based therapeutics that disrupt the addiction cycle and promote sustained recovery.
The neurobiology of addiction has historically focused on neuronal adaptations within the brain's reward circuitry. However, emerging evidence indicates that the brain's resident immune cells, microglia, play a critical role in the development, maintenance, and relapse vulnerability of substance use disorders. This whitepaper synthesizes current research demonstrating that psychostimulants and other drugs of abuse activate microglia, triggering neuroimmune signaling that modulates synaptic plasticity, increases neuroinflammation, and contributes to addictive behaviors. We detail the molecular mechanisms involved, including specific signaling pathways and microglial-neuronal interactions, and evaluate pharmacological strategies for microglial inhibition. Targeting microglial activation represents a paradigm shift in addiction therapeutics, offering novel interventions to reduce relapse vulnerability by addressing non-neuronal mechanisms within the addiction neurocircuitry.
Addiction is a chronic, relapsing disorder characterized by neuroadaptations in reward, stress, and executive control systems of the brain [3]. Traditional research has focused on neuronal pathways, particularly dopaminergic and glutamatergic transmission in the mesocorticolimbic system. However, recent advances have revealed that microglial cells, the primary immune effector cells of the central nervous system (CNS), significantly contribute to addiction pathophysiology [80] [81]. These cells comprise 5-10% of brain cells and exist in dynamic, heterogeneous states that respond to CNS insults, including exposure to drugs of abuse [80] [82].
Microglia undergo functional polarization into various activation states with distinct secretory profiles and physiological effects. While historically simplified as "resting" (ramified) versus "activated" (ameboid) states, contemporary single-cell technologies reveal a spectrum of microglial phenotypes with high spatial and temporal heterogeneity [82]. Upon exposure to psychostimulants, microglia transition toward reactive phenotypes that release pro-inflammatory mediators, engage in synaptic remodeling, and contribute to the neuroplastic adaptations that underlie addiction [80] [83].
Molecular Mechanisms of Microglial Activation in Addiction
Pattern Recognition Receptors and Initial Activation
Microglia detect changes in the brain microenvironment through pattern recognition receptors (PRRs) that recognize damage-associated molecular patterns (DAMPs) released during neuronal stress or injury induced by drugs of abuse [80] [81].
Key Signaling Pathways:
- Toll-like Receptor 4 (TLR4): Multiple psychostimulants, including cocaine, morphine, and methamphetamine, directly bind to TLR4 or its accessory protein MD-2, initiating intracellular signaling cascades that trigger pro-inflammatory cytokine release [80] [83]. This pathway represents a primary mechanism for drug-induced microglial activation independent of traditional neurotransmitter systems.
- NLRP3 Inflammasome: Stress and drugs of abuse activate the NLRP3 inflammasome through TLR signaling, leading to caspase-1 activation and maturation of pro-inflammatory cytokines such as IL-1β and IL-18 [81].
The following diagram illustrates the primary signaling pathways through which drugs of abuse and stress activate microglia, leading to pro-inflammatory responses that influence neuronal function and addiction-related behaviors:
Microglial-Neuronal Communication: The CX3CL1-CX3CR1 Axis
The fractalkine signaling system represents a crucial pathway for microglia-neuron communication in addiction. Neurons constitutively express the chemokine CX3CL1 (fractalkine), which signals through its receptor CX3CR1, predominantly expressed on microglia [80] [84]. This axis regulates microglial activation, migration, and synaptic interactions.
Studies demonstrate that cocaine administration and CSF1R inhibition alter CX3CL1-CX3CR1 signaling. CSF1R inhibition increased CX3CL1 levels in the striatum, prefrontal cortex, and hippocampus while reducing CX3CR1 expression in the hippocampus [84]. These modifications directly influence drug-seeking behavior, as disruption of this pathway prevents microglia from appropriately responding to neuronal activity and engaging in synaptic remodeling.
Microglial Regulation of Synaptic Plasticity
Microglia directly modulate addiction-related neuroplasticity through several mechanisms:
- Synaptic Pruning: During abstinence from cocaine, microglia actively prune parts of astrocytes, specifically their fine processes that envelope synapses. This disruption of astrocytic support increases drug-seeking behavior, demonstrating a direct mechanism by which microglia drive relapse vulnerability [30].
- Structural Plasticity: Microglia regulate dendritic spine density and morphology in reward-related brain regions. They contribute to experience-dependent synaptic modification in the adult brain through direct contacts with synaptic elements, particularly in activity-dependent manners [83].
- Glutamatergic Regulation: Activated microglia release cytokines such as TNF-α and IL-1β that regulate AMPA receptor expression and homeostatic synaptic scaling, boosting glutamatergic neurotransmission [80]. Microglia also produce quinolinic acid, which promotes glutamate release through NMDA receptor activation, potentially contributing to excitotoxicity in addiction [83].
Pharmacological Targeting of Microglia: Experimental Evidence
Established Microglial Inhibitors
Multiple pharmacological agents that inhibit microglial activation have demonstrated efficacy in preclinical addiction models:
Table 1: Pharmacological Agents Targeting Microglia in Addiction Models
| Agent | Molecular Target | Experimental Model | Key Findings | Citation |
|---|---|---|---|---|
| Minocycline | Multiple targets including microglial polarization | Cocaine conditioning; Alcohol addiction | Decreased cocaine preference in CPP; Reduced ethanol drinking | [83] [84] |
| Ibudilast | Phosphodiesterase inhibition | Cocaine behavioral sensitization | Attenuated behavioral sensitization | [84] [83] |
| PLX3397 | CSF1R inhibitor | Cocaine behavioral sensitization and CPP | Reduced behavioral sensitization; No effect on CPP; Reduced microglia number | [84] |
| TLR4 Antagonists | TLR4 signaling | Morphine, cocaine, alcohol models | Reduced pro-inflammatory cytokine release; Attenuated drug reward | [83] |
CSF1R Inhibition: A Selective Approach
PLX3397 (pexidartinib) represents a targeted approach to microglial modulation by inhibiting the colony-stimulating factor 1 receptor (CSF1R), which is essential for microglial viability. Experimental evidence demonstrates that CSF1R inhibition:
- Attenuates the development and expression of cocaine-induced behavioral sensitization [84]
- Reduces the number of Iba-1+ microglia in the nucleus accumbens core and shell [84]
- Increases ramification and branch length of remaining microglia, indicating morphological changes [84]
- Enhances CD68+ stained areas, suggesting increased phagocytic activity in remaining microglia [84]
Notably, CSF1R inhibition did not reverse cocaine-induced conditioned place preference, suggesting distinct mechanisms underlie different addiction behavioral paradigms [84].
Experimental Protocols for Microglial Research in Addiction
Assessing Microglial Activation in Addiction Models
Protocol: Comprehensive Analysis of Microglial Response to Psychostimulants
Animals: Adult male and female C57BL/6 mice (8-10 weeks old) or equivalent transgenic models (e.g., CX3CR1-GFP for in vivo imaging).
Drug Administration:
- Cocaine hydrochloride: 15-20 mg/kg, i.p., once daily for 7-14 days for chronic studies or acute administration for immediate effects [84].
- Control groups receive saline vehicle.
Microglial Analysis:
- Immunohistochemistry and Morphometric Analysis
- Perfuse transcardially with 4% paraformaldehyde (PFA)
- Section brains at 30-40μm thickness using vibratome
- Immunostain with:
- Primary antibodies: Iba-1 (microglia), CD68 (phagocytic activity), GFAP (astrocytes)
- Appropriate fluorescent secondary antibodies
- Image using confocal or epifluorescence microscopy
- Perform Sholl analysis to assess microglial morphology and complexity
- Calculate cell body to total cell size ratio as activation index [84]
Flow Cytometry of Microglial Populations
- Dissociate brain tissue using neural tissue dissociation kit
- Isolate microglia using CD11b+ magnetic bead separation or FACS sorting
- Stain for surface markers: CD45, CD11b, CX3CR1
- Analyze intracellular cytokines: IL-1β, TNF-α, IL-10 using intracellular staining protocols
Molecular Analysis
- Extract RNA from purified microglial populations
- Perform qRT-PCR for pro-inflammatory (TNF-α, IL-1β, IL-6) and anti-inflammatory (Arg-1, IL-10) markers
- Analyze cytokine levels in brain homogenates using multiplex ELISA
Behavioral Correlation:
- Conduct behavioral tests (sensitization, CPP, self-administration) following microglial manipulation
- Administer microglial inhibitors (minocycline: 30-50 mg/kg; PLX3397: 40 mg/kg) prior to behavioral testing [84] [83]
Assessing Microglia-Mediated Synaptic Remodeling
Protocol: Evaluating Microglial Role in Structural Plasticity
- Utilize CX3CR1-GFP mice for in vivo two-photon imaging through cranial windows
- Image dendritic spines and microglial interactions in nucleus accumbens and prefrontal cortex
- Administer fluorescently-labeled cocaine to track drug distribution
- Implement minocycline or PLX3397 during abstinence periods to assess prevention of synaptic pruning [30]
- Perform 3D reconstruction of microglial-astrocyte-synaptic interactions using electron microscopy
- Quantify synaptic density and astrocytic coverage using immunohistochemistry for PSD-95, vGlut1, and GFAP
The following workflow outlines the key methodological approaches for investigating microglial function in preclinical addiction models, integrating behavioral, molecular, and structural analyses:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Microglial Research in Addiction
| Reagent/Category | Specific Examples | Research Application | Key Findings in Addiction | |
|---|---|---|---|---|
| Microglial Inhibitors | Minocycline, Ibudilast, PLX3397 | Behavioral sensitization, CPP, self-administration | Attenuated drug-seeking, reduced sensitization | [84] [83] |
| Transgenic Models | CX3CR1-GFP, CX3CR1-CreER; Iba1-GFP | In vivo imaging, cell-specific manipulation | Visualized microglial dynamics, synaptic interactions | [30] [82] |
| Microglial Markers | Iba1, TMEM119, P2RY12, CD68 | Immunohistochemistry, flow cytometry | Identification, morphological analysis, phagocytic activity | [80] [84] |
| Cytokine Assays | Multiplex ELISA, Luminex, intracellular staining | Protein quantification, cell signaling | Inflammatory profile characterization | [80] [81] |
| TLR4 Pathway Tools | TLR4 antagonists, TLR4 knockout mice | Signaling studies, behavioral correlation | Role in drug-induced neuroinflammation | [80] [83] |
Discussion and Future Directions
The evidence supporting microglial involvement in addiction pathophysiology presents compelling opportunities for novel therapeutic interventions. Several key considerations emerge for translating these findings into clinical applications:
Therapeutic Implications and Challenges
Timing of Intervention: Microglial activation appears to have distinct roles in different addiction phases. While inhibition during initial drug exposure may prevent neuroadaptations, interventions during abstinence may specifically target relapse vulnerability by preventing excessive synaptic pruning [30].
Sex Differences: Emerging evidence indicates sexual dimorphism in microglial responses, with stress decreasing activated microglia in female rats while increasing them in males [81]. These differences necessitate inclusion of both sexes in preclinical studies and potential sex-specific therapeutic approaches.
Specificity of Targeting: Current microglial inhibitors lack complete specificity. PLX3397 depletes microglia but may affect other macrophage lineages [84]. Future therapies should aim for state-specific microglial modulation rather than broad suppression, potentially targeting specific activation phenotypes or regional microglial populations [82] [85].
Integration with Existing Addiction Treatments
Microglial-targeted therapies should be viewed as adjunctive to rather than replacements for established addiction treatments. Combining microglial modulation with medications that address neuronal adaptations (e.g., naltrexone, acamprosate) may provide synergistic benefits by targeting both neuronal and non-neuronal mechanisms of addiction.
Novel Therapeutic Avenues
Several promising directions warrant further investigation:
- Fractalkine Signaling: Modulating the CX3CL1-CX3CR1 axis presents opportunities for fine-tuning microglial-neuronal communication without broad immunosuppression [80] [84].
- Metabolic Modulation: The diabetes and weight loss medication class GLP-1 receptor agonists (e.g., semaglutide) has shown unexpected benefits for addictive behaviors, potentially through indirect effects on neuroinflammation [86].
- State-Specific Targeting: Emerging single-cell technologies enable identification of specific microglial states associated with protective versus detrimental functions in addiction, allowing for precise therapeutic targeting [82] [85].
Microglial inhibition represents a promising therapeutic avenue for reducing relapse vulnerability in substance use disorders. By targeting the neuroimmune components of addiction, this approach addresses mechanisms distinct from traditional neuronal-focused treatments. The evidence summarized in this whitepaper demonstrates that microglia contribute significantly to addiction pathophysiology through multiple mechanisms, including synaptic remodeling, neuroinflammation, and altered neuronal communication. Further research optimizing the timing, specificity, and personalization of microglial-targeted interventions may yield novel strategies to address the persistent challenge of relapse in addiction treatment.
Substance use disorders (SUDs) are chronically relapsing conditions characterized by compulsive drug-seeking, loss of control over intake, and emergence of a negative emotional state during withdrawal [2]. The development of addiction involves dramatic dysregulation of motivational circuits caused by a combination of exaggerated incentive salience, habit formation, reward deficits, and stress surrogates [26]. This condition represents a fundamental shift in brain homeostasis wherein the brain's reward and stress systems become recalibrated to prioritize drug use over natural rewards and essential physiological needs [87] [86]. The very adaptability, or plasticity, of the human brain that contributes to the development of addiction also forms the foundation for recovery, with evidence suggesting that abstinence-mediated neural recovery can reverse at least some drug-induced neuroadaptations [87] [88].
The process of addiction can be understood as a repeating three-stage cycle: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation (craving) [87] [2]. Each stage involves specific neurocircuits and neurotransmitters, creating a self-perpetuating pattern that becomes increasingly difficult to break without intervention. Within this framework, recovery can be conceptualized as consisting of two distinct processes: the restoration of brain function through the cessation of neurotoxic influences, and the active process of abstaining from use through enhanced cognitive control mechanisms [89]. This review synthesizes current evidence on the neurobiological mechanisms underlying abstinence and protracted recovery, with particular focus on their implications for relapse vulnerability and therapeutic development.
Theoretical Framework: Addiction Neurocircuitry and Homeostatic Dysregulation
The Three-Stage Addiction Cycle
The neurobiological framework of addiction centers on three interconnected stages that form a reinforcing cycle:
Binge/Intoxication Stage: This initial stage involves the acute rewarding effects of substances primarily mediated by dopamine release from ventral tegmental area (VTA) projections to the nucleus accumbens (NAc) in the basal ganglia [87] [2] [26]. Addictive substances activate the brain's reward processing system, with dopamine serving as a critical teaching signal that strengthens associations between the drug and environmental cues through incentive salience mechanisms [87]. With repeated exposure, control over drug-seeking behavior shifts from the prefrontal cortex to the basal ganglia, promoting habitual use that is less dependent on conscious control [87].
Withdrawal/Negative Affect Stage: When drug use ceases, reward circuit activity decreases while brain stress systems become hyperactive, leading to a hypersensitive negative emotional state termed hyperkatifeia (hyper-kuh-TEE-fee-uh) [87]. This state encompasses symptoms such as dysphoria, malaise, irritability, emotional pain, and sleep disturbances mediated primarily by the extended amygdala [87]. The neurobiological substrates include a hypodopaminergic state, activation of stress neurotransmitters (corticotropin-releasing factor, dynorphin, norepinephrine), and possibly proinflammatory immune agents, alongside inhibition of anti-stress neurotransmitters (neuropeptide Y, nociceptin, endocannabinoids) [87].
Preoccupation/Anticipation Stage: This stage involves intense craving and impaired executive function, primarily mediated by dysregulated prefrontal cortical circuits [87] [2]. The prefrontal cortex, particularly regions involved in cognitive control and decision-making, becomes compromised, reducing the ability to resist strong urges to use drugs [26]. Neurotransmitters including glutamate and ghrelin are implicated in this stage, which is characterized by strong cue-induced cravings and diminished inhibitory control [87].
Figure 1: The Three-Stage Addiction Cycle. This diagram illustrates the neurocircuitry and primary neurotransmitters involved in the binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation stages that characterize addiction. CRF = Corticotropin-Releasing Factor.
Homeostatic Dysregulation in Addiction
The transition to addiction involves a fundamental dysregulation of brain homeostasis across multiple systems. Repeated drug use disrupts the brain's natural reward balance through several mechanisms:
Dopamine System Dysregulation: Addictive substances cause exaggerated dopamine surges that far exceed those produced by natural rewards [86]. The brain compensates by reducing dopamine receptor availability and sensitivity, creating a hypodopaminergic state that diminishes responsiveness to natural rewards and necessitates continued drug use to maintain normal function [86].
Brain Stress System Activation: Chronic drug use leads to persistent activation of brain stress systems, particularly those involving corticotropin-releasing factor (CRF) and dynorphin in the extended amygdala [87] [2]. This creates a persistent negative emotional state that becomes a major driver of continued drug use to achieve relief.
Executive Function Impairment: The prefrontal cortex, responsible for executive functions including impulse control, decision-making, and emotional regulation, becomes progressively impaired [87]. This damage reduces the ability to resist drug urges despite awareness of negative consequences.
The net effect is a shift from positive reinforcement (seeking pleasure) to negative reinforcement (seeking relief from discomfort) as the primary motivation for drug use [87]. This shift represents a profound change in the brain's homeostatic set point, wherein the drug becomes necessary to maintain equilibrium, albeit at a maladaptive level.
Neurobiological Mechanisms of Abstinence and Recovery
Temporal Dynamics of Neural Recovery During Abstinence
Longitudinal neuroimaging studies provide compelling evidence that abstinence from substances of abuse is associated with at least partial recovery of brain structure and function. A systematic review of 45 longitudinal neuroimaging studies demonstrated that the majority showed evidence of neural recovery with abstinence, though the timing and extent varied by brain region and substance type [88].
Table 1: Temporal Dynamics of Neural Recovery During Abstinence
| Recovery Domain | Brain Regions Involved | Onset of Recovery | Key Changes |
|---|---|---|---|
| Structural Recovery | Frontal cortical regions, insula, hippocampus, cerebellum [88] | Relatively rapid (observable within weeks) [88] | Increased gray matter volume, cortical thickness, and white matter integrity [88] [89] |
| Functional Recovery | Prefrontal cortical regions, midbrain, striatum, thalamus [88] | Requires longer abstinence periods [88] | Normalization of task-related activation, with abstainers sometimes showing hyperactivation possibly reflecting increased cognitive control effort [89] |
| Neurochemical Recovery | Prefrontal cortex, striatum [88] | Varies by substance; may begin soon after cessation (particularly for alcohol) [88] | Restoration of dopamine receptor availability and function, normalization of glutamate/GABA systems [86] [89] |
| Metabolic Recovery | Global cerebral metabolism | Within 16-30 days for alcohol [89] | Recovery of PET measures of brain metabolism after alcohol cessation [89] |
The trajectory of recovery appears to follow a generally consistent pattern across substance types, though with notable variations. Structural recovery often precedes functional and neurochemical recovery, suggesting that anatomical restoration provides the foundation for subsequent normalization of brain activity and neurotransmission [88]. The most rapid volume recovery has been observed in individuals with the greatest baseline brain shrinkage and drinking severity, potentially reflecting a ceiling effect or greater capacity for plasticity in the most impaired brains [89].
Molecular and Cellular Mechanisms of Homeostatic Reset
At the molecular level, recovery of homeostasis during abstinence involves multiple adaptive processes:
Dopamine System Recovery: Protracted abstinence allows for gradual normalization of dopamine signaling, including potential upregulation of dopamine D2 receptors and restoration of basal dopamine levels [86] [89]. This recovery underlies the renewed ability to experience pleasure from natural rewards and reduced anhedonia.
Glutamatergic System Rebalancing: Chronic drug use disrupts the balance between glutamate and GABA, particularly in corticostriatal circuits [2]. Abstinence permits restoration of this balance, though the process may be protracted and contribute to vulnerability to cravings and relapse.
Stress System Normalization: Hyperactive brain stress systems, particularly CRF and norepinephrine signaling in the extended amygdala, gradually normalize during abstinence [87]. This reduction in stress system hyperactivity corresponds with diminished negative emotional states and reduced negative reinforcement motivation for drug use.
The brain's innate neuroplasticity enables these recovery processes, though the extent of restoration varies based on factors including duration and intensity of use, genetic vulnerabilities, age, and environmental factors [88]. Some drug-induced neuroadaptations may persist despite extended abstinence, potentially explaining the phenomenon of "addiction memory" and persistent vulnerability to relapse even after long periods of recovery [86].
Experimental Approaches for Studying Recovery Mechanisms
Neuroimaging Methodologies for Tracking Abstinence-Related Changes
Advanced neuroimaging techniques provide powerful tools for investigating the neurobiological changes associated with abstinence and recovery. The table below outlines key methodologies and their applications in abstinence research.
Table 2: Neuroimaging Methodologies for Studying Neural Recovery in Abstinence
| Methodology | Measured Parameters | Application in Abstinence Research | Key Findings |
|---|---|---|---|
| Structural MRI | Gray matter volume, cortical thickness, white matter integrity [88] | Quantifying brain tissue recovery during abstinence [88] [89] | Abstinence is associated with increased gray matter volumes in frontal regions and reduced ventricle size [89] |
| Functional MRI (fMRI) | Blood oxygen level-dependent (BOLD) signal during tasks or at rest [88] | Assessing functional brain changes and cognitive control during abstinence [89] | Abstinent users often show hyperactivation in prefrontal regions, possibly reflecting increased cognitive control effort [89] |
| Diffusion Tensor Imaging (DTI) | White matter integrity, fractional anisotropy (FA) [89] | Tracking recovery of white matter pathways with abstinence [89] | Mixed findings with some tracts showing improved FA with abstinence while others remain impaired [89] |
| Positron Emission Tomography (PET) | Receptor availability, brain metabolism, neurotransmitter dynamics [88] [89] | Measuring neurochemical recovery during abstinence [89] | Recovery of brain metabolism within 16-30 days of alcohol abstinence; dopamine receptor normalization [89] |
| Magnetic Resonance Spectroscopy (MRS) | Brain metabolite concentrations (e.g., GABA, glutamate) [88] | Assessing neurochemical changes during abstinence [88] | Limited but growing evidence for normalization of metabolite levels with sustained abstinence [88] |
Longitudinal Research Designs for Abstinence Studies
Optimal investigation of abstinence-mediated neural recovery requires longitudinal within-subject designs that control for individual variability and provide greater statistical power than cross-sectional approaches [88]. Key methodological considerations include:
Assessment Timepoints: Multiple assessments spanning early abstinence (first few weeks) through protracted abstinence (months to years) are necessary to map recovery trajectories [88]. Critical timepoints typically include baseline (within first week of abstinence), 1-month, 3-months, 6-months, and 1-year.
Control Groups: Comparisons with healthy controls and current users help distinguish abstinence-specific changes from pre-existing characteristics or general time effects [89].
Multimodal Approach: Combining structural, functional, and neurochemical imaging provides a comprehensive picture of recovery across different neural domains [88].
Behavioral Correlates: Linking neural changes to cognitive performance, clinical symptoms, and functional outcomes strengthens the clinical relevance of findings [88] [89].
Figure 2: Longitudinal Research Design for Abstinence Studies. This diagram outlines the optimal methodology for investigating neural recovery during abstinence, emphasizing multiple assessment timepoints and control groups. SUD = Substance Use Disorder; sMRI = structural MRI; fMRI = functional MRI; DTI = Diffusion Tensor Imaging; PET = Positron Emission Tomography; MRS = Magnetic Resonance Spectroscopy.
Table 3: Research Reagent Solutions for Addiction Recovery Studies
| Research Tool Category | Specific Examples | Research Applications | Key Insights Generated |
|---|---|---|---|
| Neuroimaging Platforms | 3T/7T MRI scanners, PET with specific radioligands (e.g., [^11C]raclopride for D2/D3 receptors), MRS sequences [88] [89] | Quantifying structural, functional and neurochemical recovery during abstinence [88] [89] | Identification of prefrontal cortex as primary site of recovery; hyperactivation in abstainers suggesting increased cognitive control demands [89] |
| Cognitive Task Paradigms | Go-NoGo, Stroop, Delay Discounting, Attentional Bias tasks [89] | Assessing recovery of executive function, inhibitory control, and decision-making in abstinence [89] | Prefrontal functional recovery correlates with improved performance on executive function tasks [89] |
| Genetic and Molecular Tools | Genome-wide association studies, epigenetic analyses, animal models of addiction and recovery [90] | Identifying genetic vulnerabilities and molecular mechanisms of resilience [90] | Genetic factors account for 50-60% of addiction risk; specific markers for vulnerability identified [86] [90] |
| Biomarker Assays | Inflammatory markers, stress hormones, neurotransmitter metabolites [90] | Linking peripheral biomarkers to central recovery processes | Potential connections between immune system activation and addiction vulnerability [90] |
| Behavioral Phenotyping Tools | Impulsivity measures, novelty-seeking assessments, reward dependence scales [90] | Characterizing endophenotypes associated with recovery outcomes | Impulsivity and novelty-seeking traits correlate with increased relapse risk [90] |
Implications for Relapse Vulnerability and Therapeutic Development
The neurobiological findings on abstinence and recovery have profound implications for understanding relapse vulnerability and developing more effective treatments. Research indicates that while abstinence facilitates considerable neural recovery, certain alterations may persist and contribute to long-term relapse risk.
Neurobiological Predictors of Relapse Vulnerability
Several neurobiological factors have been identified as predictors of relapse susceptibility:
Prefrontal Cortex Integrity: The functional integrity of prefrontal regions, particularly the dorsolateral prefrontal cortex (DLPFC) and anterior cingulate cortex (ACC), appears critical for successful abstinence [89]. Individuals with better baseline prefrontal function are more likely to maintain abstinence, likely due to enhanced cognitive control capabilities.
Attentional Biases: Neuroimaging studies have shown that attentional biases to drug-related cues are particularly good indicators of treatment outcome and predict relapse better than standard dependence measures [89].
Stress Reactivity: Persistent hypersensitivity of brain stress systems, particularly in the extended amygdala, during early abstinence may increase vulnerability to stress-induced relapse [87].
Executive Function Deficits: Impairments in response inhibition, decision-making, and emotional regulation that persist despite abstinence contribute to relapse risk [87] [89].
Therapeutic Implications and Future Directions
The evolving understanding of abstinence-related neural recovery informs several promising therapeutic approaches:
Cognitive Training Interventions: Given the importance of prefrontal function in maintaining abstinence, cognitive training approaches designed to enhance executive function and cognitive control show promise [89]. These include working memory training, inhibitory control training, and mindfulness-based practices that collectively strengthen prefrontal regulatory circuits.
Pharmacological Strategies: Medications that support the recovery of homeostasis in dopamine, glutamate, and stress systems may facilitate successful abstinence [91]. Emerging approaches include:
- GLP-1 Receptor Agonists: Originally developed for diabetes and weight loss, these medications have shown unexpected benefits for alcohol, food, and nicotine use disorders [86].
- Neuromodulation: Techniques such as transcranial magnetic stimulation (TMS) targeting prefrontal regions may enhance cognitive control and reduce craving [89].
Personalized Medicine Approaches: Identifying individual neurobiological profiles associated with different recovery trajectories may enable more targeted interventions [90]. This includes matching treatments to specific patterns of neural deficit or genetic profile.
The evidence collectively suggests that successful recovery involves not only the reversal of drug-induced neuroadaptations but also the active engagement of cognitive control mechanisms to maintain abstinence. Future research should focus on elucidating the dynamic interplay between these passive and active recovery processes, with the goal of developing interventions that optimally support both aspects of the recovery journey.
Substance use disorders (SUDs) are chronic, relapsing conditions characterized by compulsion to seek and take drugs despite negative consequences. A critical challenge in treatment is the high rate of relapse, which is often provoked by exposure to stress [92] [93]. The hypothalamic-pituitary-adrenal (HPA) axis, the body's central stress response system, plays a multifaceted role in both the development of addiction and the vulnerability to relapse [94] [95]. This whitepaper examines the neurobiological mechanisms through which stress influences relapse and details the pharmacological strategies targeting the HPA axis to achieve sustained recovery.
The HPA axis is activated in response to stressors, initiating a neuroendocrine cascade. The hypothalamus releases corticotropin-releasing factor (CRF), which stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH). ACTH then prompts the adrenal cortex to release glucocorticoids (cortisol in humans, corticosterone in rodents) into the systemic circulation [95] [11]. In the context of addiction, this stress response interacts with the brain's reward circuitry. Preclinical studies demonstrate that stress-induced glucocorticoids facilitate dopamine release in the nucleus accumbens (NAc), a key region for reward processing, thereby enhancing the rewarding properties of drugs and priming the organism for relapse [94]. Chronic drug use leads to profound dysregulation of the HPA axis, including altered baseline cortisol levels, a blunted or exaggerated response to subsequent stressors, and impaired negative feedback mechanisms [93] [96]. This dysregulation contributes to a persistent state of negative affect and heightened anxiety during withdrawal, which creates a powerful motivational drive to resume drug use to alleviate this aversive state [3].
Neurobiological Mechanisms of Stress-Induced Relapse
The transition from drug use to addiction involves a three-stage cycle—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—each with distinct neurobiological substrates that are significantly influenced by stress and the HPA axis [3].
Cross-Talk Between Stress and Reward Circuits
The neural circuitry of stress and reward are densely interconnected. The mesolimbic dopamine pathway, originating in the ventral tegmental area (VTA) and projecting to the NAc, is central to processing both natural rewards and the reinforcing effects of drugs [94] [3]. Stress and the subsequent release of glucocorticoids potentiate dopamine synthesis in the VTA and reduce its clearance in the NAc [11]. This stress-induced enhancement of dopaminergic transmission is a key mechanism underlying the sensitization to psychomotor stimulants and the reinstatement of drug-seeking behavior [94] [11]. Furthermore, the extended amygdala, comprising the bed nucleus of the stria terminalis (BNST), central amygdala (CeA), and NAc shell, serves as a critical "anti-reward" system [3]. During the withdrawal/negative affect stage, this system becomes hyperactive, releasing stress mediators such as CRF, norepinephrine, and dynorphin, which generates a negative emotional state that fuels relapse through negative reinforcement [92] [3].
Neuropharmacology of Relapse
Over 20 years of research using reinstatement models in rodents has established the critical neuropharmacological systems governing stress-induced relapse. Table 1 summarizes the key neurotransmitter systems involved.
Table 1: Key Neurotransmitter Systems in Stress-Induced Reinstatement
| Neurotransmitter/System | Role in Stress-Induced Reinstatement | Key Brain Regions |
|---|---|---|
| Corticotropin-Releasing Factor (CRF) | Primary driver; CRF receptor antagonism blocks stress-induced reinstatement [92]. | BNST, Central Amygdala [92] |
| Norepinephrine (NE) | Noradrenergic transmission is critical; α2-adrenoceptor agonists (e.g., clonidine) can prevent reinstatement [92]. | BNST, Central Amygdala [92] |
| Dopamine (DA) | Stress and glucocorticoids increase DA synthesis and release, facilitating reward salience [94] [11]. | VTA, NAc [94] |
| Glutamate | Mediates relapse via actions in the NAc; stress alters AMPA/NMDA receptor ratios [94] [92]. | NAc, Prefrontal Cortex [94] |
| Dynorphin/κ-Opioid | Activated during withdrawal/negative affect stage; contributes to dysphoric state [3]. | Extended Amygdala [3] |
| GABA | Stress-induced alterations in GABAergic inhibition disinhibit VTA dopamine neurons [94]. | VTA, NAc [94] |
The following diagram illustrates the core signaling pathways and brain regions implicated in stress-induced relapse.
Figure 1: HPA Axis and Neural Pathways in Stress-Induced Relapse. Abbreviations: VTA, ventral tegmental area; NAc, nucleus accumbens; BNST, bed nucleus of the stria terminalis; CeA, central amygdala; CRF, corticotropin-releasing factor; ACTH, adrenocorticotropic hormone; DA, dopamine; NE, norepinephrine.
Pharmacological Interventions Targeting the HPA Axis
Drug development has focused on multiple nodes within the HPA axis and associated stress systems to mitigate relapse risk. The efficacy of these approaches is supported by both preclinical models and clinical trials. Table 2 provides a comparative overview of major HPA-targeting pharmacotherapies.
Table 2: Pharmacological HPA Axis Modulators in Preclinical and Clinical Development
| Pharmacological Class | Prototype Drug(s) | Mechanism of Action | Stage of Development & Key Findings |
|---|---|---|---|
| CRF Receptor Antagonists | R121919, Pexacerfont, Verucerfont | Antagonism of CRF1 receptors in the extended amygdala, blocking stress-induced CRF signaling [92] [95]. | Preclinical: Robustly blocks stress-induced reinstatement of heroin, cocaine, alcohol, and nicotine seeking [92]. Clinical: Development for SUDs has been challenging due to efficacy or safety concerns, though the approach remains theoretically sound [93]. |
| Glucocorticoid Receptor Antagonists | Mifepristone (RU-486) | Competitive antagonism of glucocorticoid receptors, disrupting GR-mediated negative feedback and stress-enhanced dopamine transmission [97] [11]. | Clinical (Meta-Analysis): Significant effect for MDD (SMD = 0.136, 95%CI = 0.049, 0.223, p = 0.002); shows promise for cocaine and alcohol use disorders [97]. |
| Vasopressin 1B (V1B) Receptor Antagonists | ABT-436 | Blocks arginine-vasopressin potentiation of ACTH release; targets HPA axis hyperactivity, particularly under chronic stress conditions [97]. | Clinical (Meta-Analysis): Significant positive effect on depressive symptoms (SMD = 0.136); early-phase trials for AUD showed reduced alcohol consumption in high-drinking subgroups [97]. |
| α2-Adrenoceptor Agonists | Clonidine, Lofexidine | Activate presynaptic α2-adrenoceptors, inhibiting the release of norepinephrine from neurons in the BNST and amygdala, thereby dampening the stress response [92]. | Clinical: Inspired by preclinical reinstatement studies, a clinical trial demonstrated efficacy in decreasing stress-induced heroin craving and lapse [92]. Lofexidine is FDA-approved for opioid withdrawal. |
| Cortisol Synthesis Inhibitors | Metyrapone, Ketoconazole | Inhibit enzymes (e.g., 11β-hydroxylase) required for cortisol synthesis, thereby reducing circulating glucocorticoid levels [97]. | Clinical: Mixed results in trials for MDD. Metyrapone as an adjunctive treatment showed efficacy in some studies [97] but not others, potentially due to compensatory HPA axis mechanisms. |
Experimental Models and Methodologies
Preclinical Reinstatement Model
The gold standard for studying relapse is the rodent operant self-administration-reinstatement model [92]. The detailed protocol is as follows:
- Self-Administration Training: Rats or mice are trained to perform an operant response (e.g., lever press or nose poke) to receive an intravenous infusion of a drug (e.g., heroin, cocaine, methamphetamine) or oral alcohol. Training typically occurs in daily sessions over several weeks until stable self-administration behavior is established.
- Extinction: The drug is removed, and responses on the previously active lever no longer result in drug delivery. This phase continues until operant behavior is significantly diminished, indicating extinction of the drug-reinforced behavior.
- Reinstatement Test: Following extinction, the ability of a stressor to provoke resumption of drug-seeking behavior (responses on the previously active lever, still without drug available) is measured. The most commonly used stressor is intermittent electric footshock (typically 5-15 minutes of brief, unpredictable footshocks), which robustly reinstates seeking for heroin, cocaine, methamphetamine, nicotine, and alcohol [92]. Other effective stressors include forced swim, social defeat, and pharmacological stressors like exogenous CRF administration.
This model has high translational validity, as the phenomenon generalizes across drug classes and specific stressors, and its neuropharmacology closely mirrors findings in human laboratory studies [92].
Human Laboratory Stress Paradigms
Human studies often employ controlled psychological stress tasks to probe HPA axis function and its relationship to craving and relapse risk. A typical protocol used in residential treatment populations includes [98]:
- Participants: Individuals with SUDs early in treatment (e.g., within the first week).
- Baseline Measures: Collection of baseline salivary cortisol via the "passive drool" technique and assessment of state negative mood (e.g., using the Positive and Negative Affect Schedule, PANAS).
- Stress Induction: Participants complete computerized psychological stress tasks, such as:
- The Maastricht Acute Stress Test (MAST): Combines alternating periods of mental arithmetic with immersion of the hand in cold water.
- Public Speech / Mental Arithmetic Tasks: Participants prepare and deliver a speech or perform difficult arithmetic under time pressure and social evaluation.
- Post-Stress Measures: Salivary cortisol is collected immediately after stressor cessation (0 min) and at multiple time points thereafter (e.g., 10, 20, 30 min) to capture the HPA axis response trajectory. Craving and negative affect are also repeatedly assessed.
- Outcome Correlation: The cortisol stress response is then correlated with clinical outcomes, such as treatment dropout or relapse at follow-up. A higher peak cortisol response to stress has been prospectively associated with a shorter time to treatment dropout [98].
The following diagram outlines this experimental workflow.
Figure 2: Workflow of Key Experimental Models for Stress-Induced Relapse. Abbreviations: MAST, Maastricht Acute Stress Test.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating HPA Axis in Relapse
| Reagent / Resource | Function and Application in Research |
|---|---|
| CRF Receptor Antagonists | Examples: CP-154,526, NBI 27914, Antalarmin. Function: Tool compounds used in preclinical studies to delineate the role of extra-hypothalamic (BNST, CeA) vs. hypothalamic CRF1 receptors in stress-induced reinstatement [92]. |
| GR/MR Modulators | Examples: Mifepristone (GR antagonist), Spironolactone (MR antagonist), CORT113176 (selective GR antagonist). Function: To dissect the specific contributions of glucocorticoid and mineralocorticoid receptor signaling in different stages of addiction and relapse [97] [11]. |
| Salivary Cortisol Kits | Examples: Salivette collection devices with corresponding immunoassays (ELISA, CLIA). Function: Non-invasive measurement of unbound, biologically active cortisol in human studies for assessing HPA axis basal activity and stress reactivity [98]. |
| Validated Stressors | Examples: Intermittent footshock apparatus, Forced swim tanks, Social defeat chambers. Function: Standardized, reproducible methods to induce a reliable stress response and probe stress-induced reinstatement of drug seeking in rodent models [92]. |
| CRF and AVP Immunoassays | Function: To quantify peptide levels in plasma (HPA axis activity) or brain tissue microdialysates (extrahypothalamic circuits) following stress or drug exposure in preclinical models. |
| DREADDs/Chemogenetics | Function: To achieve cell-type-specific (e.g., VTA dopamine neurons, BNST CRF neurons) and circuit-specific control of neuronal activity to establish causal links between specific pathways and stress-induced relapse behavior [11]. |
Targeting the HPA axis represents a promising, mechanism-based strategy for preventing stress-induced relapse in substance use disorders. Substantial evidence from preclinical models confirms that pharmacological disruption of CRF, norepinephrine, and glucocorticoid signaling can effectively block stress-precipitated drug seeking [92]. Translational efforts have yielded encouraging results, with medications like mifepristone, V1B receptor antagonists, and α2-adrenoceptor agonists showing efficacy in modulating the stress response and improving outcomes in early human trials [92] [97]. The integration of sophisticated behavioral models with precise molecular tools will continue to refine our understanding of the stress pathophysiology of addiction. Future research must focus on developing more selective compounds with improved safety profiles, identifying biomarkers that predict treatment response, and designing clinical trials that stratify patients based on their individual stress pathophysiology [93]. Ultimately, combining these targeted pharmacotherapies with established behavioral interventions that foster coping skills and social support offers the most comprehensive path toward breaking the cycle of addiction and relapse.
Executive dysfunction is a transdiagnostic core feature of addictive disorders, fundamentally underpinning the relapse vulnerability that characterizes substance use disorders (SUDs). Executive functions (EFs) are a family of top-down, effortful processes essential for managing cognitive resources and directing goal-oriented behavior when automatic responses are insufficient or inadvisable [99]. In addiction, neurocognitive impairments especially affecting higher cognition have been widely documented, with deficits involving inhibitory control, decision-making, cognitive flexibility, and strategic orientation of cognitive resources [99]. These impairments are linked to alterations in mesocorticolimbic dopaminergic circuits and corticostriatal glutamatergic circuits in prefrontal regions [99].
The neurobiological framework of addiction reveals that executive dysfunction prominently features in the preoccupation/anticipation stage of the addiction cycle, where the prefrontal cortex (PFC)—the brain's primary executive control center—becomes dysregulated [3]. This PFC dysfunction manifests as diminished impulse control, impaired executive planning, and poor emotional regulation, creating clinical vulnerability to cravings and relapse [3]. Within the PFC, researchers have identified two key systems relevant to addiction: a "Go system" for goal-directed behaviors requiring attention and planning, and a "Stop system" for inhibitory control [3]. The hijacking of these executive control systems in addiction predisposes individuals to repeat the cycle of substance use despite adverse consequences.
Neurobiological Foundations of Executive Dysfunction
The executive dysfunction observed in addictive disorders stems from specific neuroadaptations within brain networks responsible for cognitive control, reward processing, and emotional regulation. The PFC, particularly its dorsolateral and anterior cingulate regions, shows significant alterations in both structure and function in individuals with SUDs [3]. These regions are crucial for the "Stop system" that enables individuals to override strong urges to use substances [3].
Neuroimaging studies have identified abnormal regional activity in key brain networks of individuals with addictive disorders. In methamphetamine-dependent individuals, for instance, research has revealed decreased brain activity in cortical regions and increased activity in subcortical regions, especially the bilateral putamen, during abstinence [8]. Following relapse, these individuals exhibit a wider range of abnormal brain activity, with decreased activity primarily in the middle cingulate gyrus, parietal and occipital regions, and increased activity mostly in subcortical regions (striatum, thalamus, and hippocampal structure) and several prefrontal regions [8]. These neural signatures may represent potential biomarkers for relapse vulnerability.
The neurocognitive models of addiction posit that executive deficits create a vicious cycle: they not only result from substance use but also contribute to making it more difficult to decide to stop using substances or enacting dysfunctional behaviors, as well as to persist in this decision [99]. The ability to develop conscious decision-making strategies and the efficiency of self-awareness and metacognition also appear to be partially compromised due to alterations in neural circuits that foster decision-making processes [99].
Table 1: Key Brain Regions Implicated in Executive Dysfunction in Addiction
| Brain Region | Primary Executive Function | Alteration in Addiction | Impact on Behavior |
|---|---|---|---|
| Prefrontal Cortex (PFC) | Executive control, planning, decision-making | Decreased activity, impaired connectivity | Reduced impulse control, poor judgment |
| Anterior Cingulate Cortex | Error monitoring, conflict detection | Hypoactivation | Impaired error processing, reduced cognitive control |
| Dorsolateral PFC | Working memory, cognitive flexibility | Decreased gray matter volume | Rigid thinking, difficulty adapting to change |
| Ventromedial PFC | Value-based decision-making | Altered reward processing | Poor risk assessment, preference for immediate reward |
| Striatum (Caudate/Putamen) | Habit formation, response inhibition | Hyperactivity to drug cues | Enhanced habitual drug-seeking, reduced inhibitory control |
Assessment of Executive Dysfunction
A comprehensive neuropsychological assessment is a prerequisite for effective cognitive remediation, as it establishes the baseline cognitive profile and identifies specific areas of impairment [100]. Unfortunately, assessment practices at psychiatric emergency or addiction services typically rely on basic aspecific screening batteries such as the Mini Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), or Frontal Assessment Battery [99]. While these tools offer advantages in administration time and ease of use, they were originally devised for different clinical populations (e.g., neurology or geriatric patients) and may lack sensitivity for detecting the often subtle impairments characteristic of younger individuals with SUDs [99].
The limitations of existing assessment tools have prompted the development of more specialized instruments. The Battery for Executive Functions in Addiction (BFE-A) represents a novel digitalized assessment tool specifically designed to address this gap [99]. This modular battery consists of seven subtests targeting cognitive domains particularly vulnerable in addiction:
- Verbal Memory Test (VMT) - assessing short/long-term verbal memory
- Working Memory Test (WMT) - evaluating transient storage and active processing of numerical material
- Focused Attention Test (FAT) - measuring detection and selection of target visual-spatial stimuli
- Verbal Fluency Test (VFT) - examining cognitive flexibility with linguistic material
- Non-verbal Fluency Test (NvFT) - assessing cognitive flexibility with visual-spatial patterns
- Modified Stroop Task for Addiction (MST) - evaluating attention regulation and suppression of interference
- Modified Go/No-go Task for Addiction (MGNT) - testing inhibitory control with addiction-related stimuli [99]
The BFE-A enables examiners to run intra-individual comparisons across different cognitive functions and identify both strengths and weaknesses, facilitating the development of personalized rehabilitation interventions [99].
Table 2: Domains of Neuropsychological Assessment in Addictive Disorders
| Cognitive Domain | Specific Functions Assessed | Common Assessment Tools |
|---|---|---|
| Attention | Focused attention, sustained attention, divided attention | Letter cancellation, Continuous Performance Test |
| Mental Speed | Processing speed, reaction time | Trail Making Test Part A, Digit Symbol Coding |
| Working Memory | Transient storage and manipulation of information | Digit Span Backward, N-back task |
| Executive Functions | Planning, cognitive flexibility, response inhibition | Trail Making Test Part B, Stroop Task, Wisconsin Card Sorting Test |
| Learning and Memory | Verbal learning, visual memory, recall and recognition | Verbal Learning and Memory Test, Rey-Osterrieth Complex Figure |
| Visuo-Spatial Functions | Visuo-spatial construction, visual perception | Block Design, Figure Copying |
Cognitive Remediation Approaches
Cognitive remediation for addictive disorders represents a therapeutic approach that uses neuroscience and learning principles to train cognitive strategies in a psychosocial therapeutic context to produce lasting cognitive improvements and functional changes [101]. This approach differs from simple cognitive training, which typically relies on repetitive practice alone, often via computerized software, without the psychosocial component that helps clients link trainings to everyday life [101].
Goal Management Training (GMT)
GMT is a therapist-led cognitive remediation intervention originally designed for people with brain injuries that has been adapted for addictive disorders [101]. GMT trains executive functions through strategy learning, scaffolding of new skills, and experiential learning of common errors. It also teaches clients the application of metacognitive skills to individual goals and real-world situations. The program is delivered in groups and includes both in-session activities and between-session skills practice [101].
In a randomized proof-of-concept trial, a modified version of GMT (GMT+) tailored for people with methamphetamine use disorder demonstrated large effects at improving performance on an information gathering task and an impulsive choice task compared to an active matched psychoeducation control [101]. Additionally, GMT+ led to a significant and large reduction in methamphetamine dependence severity four weeks after treatment [101].
Neuropsychological Educational Approach to Cognitive Remediation (NEAR)
The NEAR model incorporates a selection of personalized computerized cognitive training activities delivered to individuals with SUDs in therapeutic settings [101]. Therapists facilitate discussions about the use of strategies in everyday life, emphasizing the application of cognitive skills to real-world situations. In a pilot trial, this approach demonstrated a moderate effect at improving performance on the Wisconsin Card Sorting Test, a disinhibition task that captures difficulties in cognitive shifting [101].
Integrated Cognitive Remediation Approaches
Some interventions combine multiple evidence-based approaches. Marceau and colleagues administered a combined protocol of cognitive remediation and computerized cognitive training compiled from numerous programs for acquired brain injury (including GMT) [101]. This integrated approach showed significant improvements in performance on an attentional control (Stroop) task as well as quality of life in individuals with SUDs enrolled in residential treatment [101].
EEG Neurofeedback
EEG neurofeedback represents an innovative circuitry-based approach to cognitive rehabilitation that uses operant conditioning to modify brain activity and bring it under voluntary control [100]. In this approach, electrodes are placed according to the International 10-20 system, and individuals receive feedback on their brainwave patterns, learning to self-regulate neural activity [100].
A case study of a patient with alcohol dependence syndrome demonstrated the potential efficacy of EEG neurofeedback [100]. Following neurofeedback training, the patient showed significant improvement on measures of focused attention, verbal working memory, verbal learning and memory, response inhibition, visuo-spatial construction, and visual memory [100]. Importantly, the patient maintained abstinence six months following the intervention, suggesting enduring benefits of this approach [100].
Experimental Evidence and Efficacy
Research on cognitive remediation for addictive disorders, while still developing, provides preliminary evidence supporting its efficacy for addressing executive dysfunction and potentially improving treatment outcomes. A review of cognitive remediation for impulsivity in addictive disorders identified six studies that delivered cognitive remediation and assessed state impulsivity in substance use disorders [101]. Although substantial heterogeneity exists in intervention ingredients and delivery approaches, the findings offer promising directions.
For impulsive choice (the preference for smaller immediate rewards over larger delayed rewards), cognitive remediation has shown positive effects. In one study, GMT+ demonstrated a significant effect on delay discounting tasks, reflecting a shift in preferences from smaller immediate rewards to larger delayed rewards [101]. This is particularly relevant for addiction treatment, as the ability to favor long-term goals over immediately gratifying experiences is crucial for recovery.
For disinhibition mechanisms, the evidence is mixed but encouraging. Two studies delivering GMT-related interventions found positive effects on information gathering task performance, reflecting an increased tendency to collect and consider the accuracy of information prior to responding [101]. Effects on attentional control and feedback monitoring/shifting were less consistent, with some studies reporting benefits [101] while others found no significant improvements [101].
Table 3: Efficacy of Cognitive Remediation Approaches for Executive Dysfunction in Addiction
| Intervention Type | Sample Characteristics | Effects on Cognition | Effects on Clinical Outcomes |
|---|---|---|---|
| Goal Management Training (GMT+) | Methamphetamine use disorder (n=36) | Large effects on information gathering and impulsive choice | Large reduction in dependence severity |
| GMT + Mindfulness | Polysubstance use (n=34) | Improved attentional control and decision-making | Not assessed |
| Paper-and-Pencil Cognitive Remediation | Opioid use disorder (n=120) | No significant effect on attentional control | Lower opiate use at 3-month follow-up |
| NEAR Approach | Mixed SUDs (n=65) | Moderate effect on cognitive shifting | Not assessed |
| Integrated Cognitive Remediation | Mixed SUDs (n=33) | Improved attentional control | Improved quality of life |
| EEG Neurofeedback | Alcohol dependence (case study) | Improved attention, memory, and inhibition | Maintained abstinence at 6-month follow-up |
Implementation Considerations and Research Gaps
Despite promising findings, several methodological challenges and research gaps remain in the field of cognitive remediation for addictive disorders. The empirical evidence presents mixed findings, with some studies demonstrating reductions in substance use and consumption-related problems [102], while others observe no significant differences between treatment and control groups [102].
A primary concern is the transferability of cognitive improvements to everyday functioning. While many cognitive training interventions demonstrate effects on trained tasks, evidence supporting their transfer to functional domains in real life remains limited [102]. Many individuals with SUDs struggle to apply cognitive skills learned in clinical settings to real-world challenges and triggers, highlighting the need for interventions that specifically facilitate this transfer.
Several factors may optimize the effectiveness of cognitive remediation:
- Co-designing interventions with frontline clinicians and clients with lived experience of addictive disorders [101]
- Incorporating specific impulsivity training strategies that target the core mechanisms of disinhibition [101]
- Increasing opportunities to practice skills through sufficiently intensive and prolonged training [101]
- Supporting skill transfer to everyday settings through therapist-led discussions and real-world application [101]
- Demonstrating clinician compassion to enhance engagement and therapeutic alliance [101]
Additionally, individual differences in treatment response require further investigation. Factors such as lifestyle behaviors (nutrition, physical activity, sleep routines), specific substance use patterns, co-occurring psychiatric conditions, and demographic variables may significantly influence cognitive remediation outcomes but have been insufficiently studied [102].
Research Reagent Solutions and Methodological Tools
Table 4: Essential Research Tools for Cognitive Remediation Studies
| Tool Category | Specific Instrument | Primary Research Application |
|---|---|---|
| Neuropsychological Assessment | Battery for Executive Functions in Addiction (BFE-A) | Digital assessment of addiction-specific cognitive profiles |
| Neuropsychological Assessment | NIMHANS Neuropsychology Battery | Comprehensive cognitive assessment across multiple domains |
| Clinical Outcomes | Clinical Institute Withdrawal Assessment for Alcohol scale | Measurement of withdrawal symptom severity |
| Clinical Outcomes | Structured Clinical Interview for DSM Disorders (SCID) | Diagnostic confirmation of substance use disorders |
| Neuroimaging | Resting-state functional MRI (rs-fMRI) | Assessment of regional brain activity and connectivity |
| Neuroimaging | Fractional Amplitude of Low-Frequency Fluctuation (fALFF) | Measurement of spontaneous neural activity |
| Neuroimaging | Regional Homogeneity (ReHo) | Evaluation of local functional connectivity |
| Cognitive Training | Goal Management Training (GMT) Manual | Standardized protocol for executive function training |
| Cognitive Training | Neuropsychological Educational Approach to Cognitive Remediation (NEAR) | Framework for personalized cognitive training |
| Psychophysiological Assessment | EEG Neurofeedback System | Brainwave monitoring and training system |
The field of cognitive remediation for executive dysfunction in addictive disorders is at a promising but preliminary stage. Future research should prioritize rigorous methodological designs with adequate sample sizes, appropriate control conditions, blinded assessments, and comprehensive reporting of dropouts and potential biases [102]. There is a particular need for studies that specifically examine the underlying mechanisms of change in cognitive remediation to determine how and for whom these interventions are most effective.
From a clinical implementation perspective, cognitive remediation should be viewed as an adjunctive treatment rather than a standalone intervention for SUDs [102] [101]. These approaches are designed to complement rather than replace established treatments, addressing the cognitive barriers that may limit engagement and response to primary psychosocial and pharmacological interventions.
The neurobiological framework of addiction provides a strong rationale for targeting executive dysfunction as a pathway to reducing relapse vulnerability. By addressing the cognitive impairments that characterize the preoccupation/anticipation stage of the addiction cycle—particularly those mediated by PFC dysfunction—cognitive remediation strategies offer the potential to strengthen the neural systems necessary for maintaining recovery [3]. As research advances, the integration of cognitive remediation with other treatment modalities, personalized based on individual cognitive profiles and neural characteristics, holds promise for more effectively addressing the complex challenge of addiction relapse.
Relapse to drug use following periods of abstinence remains the most significant challenge in the long-term treatment of substance use disorders. This whitepaper explores the integration of the Theory of Planned Behavior (TPB) as a framework for understanding the cognitive and motivational processes underlying relapse vulnerability. By synthesizing evidence from clinical studies, behavioral neuroscience, and quantitative relapse analysis, we establish how TPB constructs—behavioral intention, attitude, subjective norms, and perceived behavioral control—interact with established neurobiological mechanisms of relapse. The paper provides a comprehensive technical guide for researchers, including standardized experimental protocols, quantitative data synthesis, visualization of neurobehavioral pathways, and essential research reagents for investigating this integrated model.
Addiction is widely recognized as a chronic, relapsing brain disorder characterized by compulsive drug seeking and use despite harmful consequences [103]. The neurobiological perspective reveals that chronic drug exposure produces lasting adaptations in brain circuits involved in reward, stress, executive control, and learning [39]. These changes create a persistent vulnerability to relapse that can persist long after acute withdrawal has subsided. Understanding the interplay between these stable neuroadaptations and the dynamic cognitive processes that guide decision-making is crucial for advancing relapse prevention strategies.
The Theory of Planned Behavior (TPB) provides a validated conceptual framework for understanding how intentions to remain abstinent are formed and translated into behavior [104]. According to this model, behavioral intention—the central predictor of behavior—is influenced by three factors: (1) behavioral attitude (personal evaluation of the behavior and its outcomes), (2) subjective norms (perceived social pressure regarding the behavior), and (3) perceived behavioral control (beliefs about one's capability to perform the behavior) [103] [104]. When applied to addiction relapse, this model helps explain why individuals with strong initial abstinence intentions may nevertheless resume drug use when facing triggers, stressors, or temptations.
Quantitative studies of relapse patterns reveal a remarkably consistent reverse J-shaped curve across different substances of abuse, with the highest risk occurring early in abstinence and decelerating over time [105] [106]. This universal pattern suggests an underlying mechanism that transcends specific drug classes, treatment modalities, or patient populations. The accumulated duration of continuous abstinence itself appears to be a significant variable moderating long-term resistance to relapse, possibly through strengthening self-efficacy and normalizing neuroadaptive processes [105].
Quantitative Foundations of Relapse Behavior
Epidemiological Patterns of Relapse
Recent clinical studies provide substantial quantitative evidence on relapse rates and predictors. A 2022 cross-sectional study of 400 male patients in addiction treatment centers in Shiraz, Iran, found that 85.5% had a history of relapse, with 50.29% experiencing between 1-5 relapse episodes [103]. Demographic risk factors significantly associated with relapse included marital status, occupation, and income level, while behavioral risk factors prominently featured associations with addicted friends and close relatives [103].
The substances used by participants in this study reflected poly-drug use patterns, with methamphetamine (59.5%), heroin (53%), opium (48%), and alcohol (40%) being most prevalent [103]. The early onset of substance use was also notable, with 48% of respondents reporting first use between ages 16-20, and 34.5% indicating their first consumption occurred at friends' houses [103]. These findings highlight the critical roles of both developmental timing and social environment in establishing patterns of use that predict later relapse vulnerability.
Table 1: Demographic and Behavioral Characteristics of Individuals with Substance Use Disorders (N=400) [103]
| Characteristic | Category | Percentage |
|---|---|---|
| Age | 31-40 years | 47.50% |
| Marital Status | Married | 66.25% |
| Living Arrangement | With spouse | 56.00% |
| First Use Age | 16-20 years | 48.00% |
| First Use Location | Friends' houses | 34.50% |
| Relapse History | Any relapse | 85.50% |
| Number of Relapses | 1-5 episodes | 50.29% |
Table 2: Substance Use Patterns Among Study Participants (N=400) [103]
| Substance | Usage Prevalence |
|---|---|
| Methamphetamine | 59.5% |
| Heroin | 53.0% |
| Opium | 48.0% |
| Alcohol | 40.0% |
Quantitative Modeling of Relapse Curves
Statistical analyses of relapse patterns across multiple studies demonstrate that the log-logistic distribution provides the most accurate model for the characteristic relapse curve [105] [106]. This model captures the initially high risk of relapse immediately following treatment, with a subsequent deceleration in risk over time. The survival function for the log-logistic distribution is described by:
[ S(x) = \frac{1}{1 + \lambda x^{\alpha}}, \quad \lambda > 0, \quad \alpha > 0, \quad x > 0 ]
where (S(x)) represents the probability of remaining abstinent at time (x), (\lambda) is the scale parameter, and (\alpha) is the shape parameter [105]. The hazard function (h(x) = \frac{\alpha \lambda x^{\alpha-1}}{1 + \lambda x^{\alpha}}) increases to a maximum at time ([(\alpha-1)\lambda]^{1/\alpha}) and then decreases to zero as time approaches infinity when (\alpha > 1) [105].
This quantitative framework confirms that the probability of maintaining abstinence increases with cumulative abstinence duration, supporting the clinical observation that "abstinence begets abstinence" [105]. From a neurobiological perspective, this decreasing hazard rate may reflect the gradual normalization of neural systems compromised by chronic drug use, including the recovery of prefrontal regulatory control and the weakening of hyperactive stress and cue reactivity systems [39].
Theory of Planned Behavior: Constructs and Measurement
Core TPB Constructs in Relapse Context
The TPB provides a structured framework for investigating the psychological antecedents of relapse behavior. In the context of addiction recovery, the three primary constructs operate as follows:
Behavioral Attitude: The individual's positive or negative evaluation of maintaining abstinence, considering both the expected outcomes (e.g., improved health, social functioning) and the perceived costs (e.g., withdrawal, loss of coping mechanism) [103] [104]. In the Iranian study, positive attitudes toward abstinence significantly predicted reduced relapse risk, accounting for the individual's personal desire to remain drug-free [103].
Subjective Norms: The perceived social pressure from important others (family, friends, treatment providers) to maintain abstinence [103] [104]. The study identified "insistence of friends" and the presence of "addicted friends and close relatives" as significant interpersonal factors influencing relapse, highlighting how social networks can either support or undermine recovery efforts [103].
Perceived Behavioral Control: The extent to which individuals believe they can successfully execute behaviors required to maintain abstinence, including confidence in resisting cravings, avoiding high-risk situations, and implementing coping strategies [103] [104]. Regression analyses demonstrated that perceived behavioral control was a significant predictor of drug relapse among addicts, with greater perceived control associated with reduced relapse risk [103].
The central outcome of these three constructs is behavioral intention—the level of motivation or commitment to maintain abstinence. Research has consistently shown that intention is the most proximal mediator of behavior, explaining more variance in behavioral outcomes than attitudes, norms, self-efficacy, or demographic variables [107].
Measurement Methodologies for TPB Constructs
Valid assessment of TPB constructs requires carefully designed instruments with established psychometric properties. The Iranian study developed a researcher-made questionnaire that demonstrated strong reliability, with Cronbach's alpha values of 0.82 for awareness, 0.89 for attitude, 0.89 for subjective norms, 0.88 for perceived behavioral control, and 0.87 for behavioral intention [103].
The measurement approach included:
- Awareness: 15 items on a 5-point Likert scale (range: 15-75)
- Attitude: 10 items on a 5-point Likert scale (range: 10-50)
- Subjective Norms: 8 items on a 5-point Likert scale (range: 8-40)
- Perceived Behavioral Control: 8 items on a 5-point Likert scale (range: 8-40)
Content validity was established through expert review (10 health education specialists, 1 psychiatrist, 1 psychologist), with an item effect size >0.15 and content validity ratio >0.79 [103]. Face validity was confirmed by 40 patients with demographic characteristics similar to the study population.
Research indicates that intention measures referencing specific behaviors (e.g., "I intend to avoid drug use when with using friends") demonstrate stronger predictive validity than general measures (e.g., "I intend to stay abstinent") [107]. Similarly, the predictive power of intention measures varies based on item wording, with comparative studies showing that an aggregate of multiple items provides the most reliable assessment [107].
Table 3: Psychometric Properties of TPB Questionnaire in Relapse Research [103]
| TPB Construct | Number of Items | Scale Range | Cronbach's Alpha |
|---|---|---|---|
| Awareness | 15 | 15-75 | 0.82 |
| Attitude | 10 | 10-50 | 0.89 |
| Subjective Norms | 8 | 8-40 | 0.89 |
| Perceived Behavioral Control | 8 | 8-40 | 0.88 |
| Behavioral Intention | Not specified | Not specified | 0.87 |
| Overall Questionnaire | 41+ | N/A | 0.89 |
Neurobiological Mechanisms of Relapse Vulnerability
Primary Triggers and Neural Substrates
Preclinical and human laboratory studies have identified three primary categories of relapse triggers, each with partially distinct neural substrates:
Drug-Associated Cues: Environmental stimuli previously paired with drug consumption acquire incentive-motivational properties through associative learning processes, enabling them to evoke conditioned responses that promote drug seeking [39] [108]. Functional neuroimaging studies in humans show that drug cues activate brain regions involved in reward processing (ventral striatum, orbitofrontal cortex) and attention (anterior cingulate, prefrontal regions) [39] [108].
Stressors: Acute exposure to stressors reliably provokes drug craving and seeking in both humans and laboratory animals [39] [108]. The involvement of corticotropin-releasing factor (CRF) and noradrenergic systems in the extended amygdala and bed nucleus of the stria terminalis appears critical for stress-induced relapse [39].
Drug Priming: Small doses of the previously used drug or pharmacologically similar compounds can reinstate drug-seeking behavior [39]. This effect involves rapid neurochemical changes in mesocorticolimbic dopamine systems and glutamate release in the nucleus accumbens [39].
The mesocorticolimbic dopamine system and its glutamatergic connections form the core circuitry mediating these relapse phenomena [39]. Specifically, the ventral tegmental area (VTA), nucleus accumbens (NAc), prefrontal cortex (PFC), amygdala, and hippocampus constitute a integrated network that processes drug-related memories, incentive motivation, and executive control over drug-seeking behaviors [39].
Neuroadaptations in Relapse Vulnerability
Chronic drug exposure produces enduring neuroadaptations that perpetuate vulnerability to relapse through multiple mechanisms:
Synaptic Plasticity: Drugs of abuse induce long-term potentiation (LTP) of excitatory synapses on medium spiny neurons in the NAc and other striatal regions, strengthening associations between drug contexts and reward [39].
Dysregulated Glutamate Transmission: Chronic drug use disrupts basal glutamate levels in the NAc and impairs prefrontal glutamate transmission, compromising cognitive control and enhancing responsiveness to drug cues [39].
CRF and Stress System Sensitization: Beyond their acute effects, stressors produce long-lasting sensitization of CRF and noradrenergic systems, creating a persistent hyperresponsiveness to future stressors [108].
Structural Changes: Repeated drug administration can produce proliferative changes in dendritic spines in the NAc and PFC, with cocaine exposure increasing spine density through mechanisms dependent on cyclin-dependent kinase-5 [39].
These neuroadaptations create a biological foundation for the cognitive and motivational processes described by the TPB. For instance, diminished prefrontal regulation may impair perceived behavioral control, while enhanced cue reactivity may strengthen positive attitudes toward drug use in specific contexts.
Diagram 1: Integration of TPB Constructs with Neurobiological Systems in Relapse Vulnerability
Experimental Protocols for Integrated Relapse Research
Human Laboratory Studies of Relapse Predictors
Protocol: Assessing TPB Constructs and Cue Reactivity in Individuals with Substance Use Disorders
Participant Recruitment: Recruit individuals with substance use disorders currently in early recovery (1-3 months abstinence) from addiction treatment centers. Sample size calculation should target approximately 400 participants for correlational designs, based on previous research detecting significant relationships among TPB constructs [103].
Baseline Assessment:
- Administer TPB questionnaire assessing awareness, attitude, subjective norms, perceived behavioral control, and behavioral intention related to maintaining abstinence [103].
- Collect demographic information (age, marital status, occupation, income), substance use history (age of first use, substances used, previous treatment episodes), and social environment factors (living situation, substance-using associates) [103].
- Validate instruments through expert review and pilot testing to ensure content validity and appropriate psychometric properties [103].
Cue Reactivity Testing:
- Present drug-related cues (drug paraphernalia, imagery) and neutral cues in counterbalanced order while measuring physiological responses (heart rate, skin conductance) and subjective craving ratings [108].
- For a subset of participants, conduct functional neuroimaging (fMRI) during cue exposure to assess activation in reward processing regions (ventral striatum, orbitofrontal cortex) and attention networks (anterior cingulate, prefrontal cortex) [39] [108].
Longitudinal Follow-up:
- Track participants for 6-12 months using structured interviews at regular intervals (e.g., monthly) to assess continuous abstinence, lapse/relapse episodes, and contextual factors surrounding these events [103] [105].
- Collect collateral information from significant others or treatment providers to verify self-reported abstinence when possible.
Data Analysis:
- Use linear and binary logistic regression to examine whether TPB constructs predict relapse outcomes after controlling for demographic and clinical variables [103].
- Apply survival analysis (particularly log-logistic distribution models) to examine the pattern of relapse over time [105] [106].
- Conduct mediation analyses to test whether neurobiological responses to drug cues mediate the relationship between TPB constructs and relapse outcomes.
Preclinical Models of Relapse Mechanisms
Protocol: Reinstatement Model of Drug Seeking in Laboratory Animals
Self-Administration Training:
- Train animals (typically rats or mice) to self-administer drugs of abuse (e.g., cocaine, heroin, alcohol) by pressing an active lever that results in intravenous drug infusion accompanied by a conditioned stimulus (e.g., light, tone) [39].
- Continue training until stable self-administration behavior is established (typically 2-3 weeks).
Extinction Training:
- Place animals in the same self-administration context but eliminate drug delivery and conditioned stimulus presentation when the active lever is pressed [39].
- Continue extinction sessions until responding on the previously active lever decreases to a predetermined criterion (e.g., <15 responses per session for consecutive sessions).
Reinstatement Testing:
- Test for cue-induced reinstatement by presenting the conditioned stimulus non-contingently or contingent on lever pressing [39].
- Test for drug-induced reinstatement by administering a non-contingent priming injection of the training drug prior to the session [39].
- Test for stress-induced reinstatement by exposing animals to an acute stressor (e.g., intermittent footshock) before the session [39].
- Include appropriate control groups that receive neutral stimuli, vehicle injections, or no stress exposure.
Pharmacological and Circuit Manipulations:
- Systemically or locally administer receptor-selective compounds to identify neurochemical systems necessary for reinstatement (e.g., dopamine, glutamate, CRF receptor antagonists) [39] [108].
- Use chemogenetic or optogenetic approaches to selectively activate or inhibit specific neural pathways implicated in relapse (e.g., projections from prefrontal cortex to nucleus accumbens) [39].
Molecular and Structural Analyses:
- Process brain tissue for immunohistochemical or biochemical analyses of protein expression, activation markers, or structural changes following reinstatement tests [39].
- Examine drug-induced neuroadaptations in specific cell populations using techniques such as fluorescence-activated cell sorting followed by RNA sequencing.
Diagram 2: Integrated Experimental Workflow for Human and Preclinical Relapse Research
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Investigating Relapse Mechanisms
| Reagent/Material | Application | Technical Function |
|---|---|---|
| TPB Questionnaire [103] | Human studies | Validated instrument assessing awareness (15 items), attitude (10 items), subjective norms (8 items), and perceived behavioral control (8 items) using 5-point Likert scales |
| Conditioned Stimuli (Drug Cues) [39] [108] | Human and animal studies | Standardized drug-related paraphernalia, images, or sensory stimuli that elicit conditioned responses and reinstate drug-seeking behavior |
| LY379268 (mGlu2/3 agonist) [108] | Preclinical studies | Group II metabotropic glutamate receptor agonist that attenuates context-induced reinstatement of drug seeking by modulating glutamate transmission |
| CRF Receptor Antagonists [39] [108] | Preclinical studies | Compounds that block corticotropin-releasing factor receptors to inhibit stress-induced reinstatement of drug seeking |
| Dopamine Receptor Antagonists [39] | Preclinical studies | Compounds that block D1-like or D2-like dopamine receptors to examine dopaminergic contributions to drug priming-induced reinstatement |
| Chemogenetic Tools (DREADDs) [39] | Preclinical studies | Designer receptors exclusively activated by designer drugs for selective manipulation of specific neural circuits in reinstatement tests |
| Optogenetic Constructs [39] | Preclinical studies | Light-sensitive opsins for millisecond-timescale control of specific neural populations and pathways during reinstatement behavior |
| BDNF Assays [108] | Molecular studies | Antibodies and kits for measuring brain-derived neurotrophic factor, implicated in the "incubation" of craving and reinstatement |
| Dendritic Spine Morphometry Reagents [39] | Structural studies | Fluorescent markers and imaging tools for quantifying drug-induced changes in dendritic spine density and morphology |
The integration of the Theory of Planned Behavior with neurobiological models of relapse provides a powerful framework for understanding the complex interplay between cognitive processes and neural mechanisms in sustained recovery from addiction. The TPB constructs—behavioral attitude, subjective norms, and perceived behavioral control—contribute unique variance in predicting relapse outcomes, while also mapping onto specific neurobiological systems [103] [104]. The quantitative consistency of relapse curves across different substance classes [105] [106] suggests common underlying mechanisms that may be effectively targeted through integrated interventions.
Future research should prioritize longitudinal designs that simultaneously assess TPB constructs, neurobiological markers, and relapse outcomes across the recovery timeline. Experimental studies using pharmacological or neuromodulation approaches to target specific neurobiological systems can test causal hypotheses about their influence on TPB constructs and relapse behavior. Additionally, developing more precise measures of intention that account for contextual factors and fluctuations over time will enhance predictive validity [107]. This integrated approach holds promise for developing personalized relapse prevention strategies that address both the cognitive and neurobiological dimensions of addiction.
Validating Predictive Models and Comparing Emerging Therapeutic Targets
In the field of neurobiology of addiction, the high rate of relapse following treatment remains a significant challenge. Substance use disorders (SUDs) are chronic, relapsing conditions marked by high variability in treatment response [109]. The development of validated biomarkers is crucial for stemming this crisis, offering the potential to define pathophysiological subsets of addiction, evaluate target engagement of new drugs, and predict therapeutic efficacy [110]. Prospective biomarker validation represents the critical process of confirming, in a pre-planned manner, that a biomarker is fit for its intended clinical purpose. This journey from laboratory discovery to clinical application is long and arduous, requiring rigorous statistical design and multidisciplinary collaboration to ensure that biomarkers are reliable, reproducible, and meaningful for patient care [111]. This guide outlines the core principles and methodologies for the prospective validation of biomarkers, with a specific focus on applications within addiction relapse vulnerability research.
Biomarker Definitions and Context in Addiction Research
A biological marker (biomarker) is formally defined as "a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or biological responses to an exposure or intervention" [111]. In the context of addiction and clinical trials, several key categories of biomarkers are recognized by regulatory agencies like the FDA and EMA [110]:
- Susceptibility/Risk Biomarkers: Identify individuals at higher risk of developing a substance use disorder.
- Diagnostic Biomarkers: Confirm the presence or absence of a substance use disorder or its subtypes.
- Prognostic Biomarkers: Provide information about the overall expected clinical outcome, such as the likelihood of relapse, regardless of a specific therapy [111].
- Predictive Biomarkers: Inform the expected clinical outcome based on a specific treatment decision in biomarker-defined patients only [111]. For example, a biomarker might predict which patients will respond to a particular anti-craving medication.
- Pharmacodynamic/Response Biomarkers: Reflect a biological response to a therapeutic intervention, often used to demonstrate target engagement.
- Monitoring Biomarkers: Used to track disease progression (e.g., relapse susceptibility) or therapeutic response over time.
The neurobiology of addiction provides a rich substrate for biomarker discovery. Cocaine use disorder (CUD), for instance, is characterized by a loss of control over consumption and intense craving, which is central to dependence and relapse [112]. Research has shown that alterations in brain homeostasi—particularly within the reward system—can serve as a source for predictive biomarkers. These include changes in brain activity measured by functional MRI (fMRI), such as increased activity in the ventral striatum and nucleus accumbens during reward tasks, which has been associated with lower abstinence rates [112]. The overarching goal of precision medicine in SUDs is to integrate these behavioral, environmental, and biological insights to tailor treatment to patient-specific characteristics [109].
The Biomarker Validation Pipeline
The journey of a biomarker from discovery to clinical use is a systematic, multi-stage process. Failure to adequately address each stage is a primary reason why only about 0.1% of potentially clinically relevant biomarkers progress to routine clinical use [113].
Key Validation Stages
The following diagram illustrates the end-to-end biomarker validation pipeline:
Prospective Validation Study Design
Prospective validation requires careful statistical consideration to avoid bias and ensure robust results.
- Intended Use and Target Population: The specific clinical context and target population for the biomarker must be defined a priori [111]. For addiction relapse, this could be, "To predict relapse susceptibility within 4 months post-treatment in adults with severe Cocaine Use Disorder."
- Avoiding Bias: Bias is one of the greatest causes of failure in biomarker validation studies [111]. Key tools to mitigate bias include:
- Randomization: Specimens from controls and cases should be randomly assigned to testing plates or batches to control for non-biological experimental effects (batch effects) [111].
- Blinding: Individuals who generate the biomarker data should be kept from knowing the clinical outcomes to prevent assessment bias [111].
- Statistical Rigor:
- Pre-specified Analysis Plan: The analytical plan, including primary outcomes, hypotheses, and success criteria, should be finalized before data collection begins [111].
- Power and Sample Size: An a priori power calculation ensures a sufficient number of subjects and events to provide adequate statistical power [111].
- Controlling Multiple Comparisons: When evaluating multiple biomarkers, methods to control the false discovery rate (FDR) are essential [111].
Distinguishing Prognostic and Predictive Biomarkers
The statistical approach to validation differs fundamentally between prognostic and predictive biomarkers, a critical distinction in addiction research where both natural history of relapse and response to intervention are of interest.
- Prognostic Biomarker Identification: A prognostic biomarker is identified through a main effect test of association between the biomarker and the outcome in a statistical model. It can be studied in properly conducted retrospective studies, case-control studies, and single-arm trials [111]. For example, a study might find that decreased gray matter volume in the prefrontal cortex is associated with a higher likelihood of relapse, regardless of the psychosocial therapy received.
- Predictive Biomarker Identification: A predictive biomarker must be identified in secondary analyses of a randomized clinical trial through an interaction test between the treatment and the biomarker in a statistical model [111]. For instance, a specific genetic variant in the opioid receptor gene might predict a significantly better response to naltrexone compared to a placebo, while those without the variant show no difference.
Performance Metrics and Quantitative Data Analysis
Evaluating biomarker performance requires a standard set of statistical metrics. The appropriate metric depends on the study goals and should be determined by a team including clinicians, scientists, and statisticians [111].
Table 1: Key Statistical Metrics for Biomarker Validation
| Metric | Description | Application in Addiction Research |
|---|---|---|
| Sensitivity | The proportion of true positives that are correctly identified (e.g., relapsers with a positive biomarker test). | Measures the test's ability to correctly identify individuals who will relapse. |
| Specificity | The proportion of true negatives that are correctly identified (e.g., abstainers with a negative biomarker test). | Measures the test's ability to correctly identify individuals who will remain abstinent. |
| Positive Predictive Value (PPV) | The proportion of test-positive patients who actually have the event (relapse). | Of all patients with a biomarker-positive test, the proportion that actually relapses. |
| Negative Predictive Value (NPV) | The proportion of test-negative patients who truly do not have the event. | Of all patients with a biomarker-negative test, the proportion that remains abstinent. |
| Area Under the Curve (AUC) | A measure of how well the biomarker distinguishes between two groups (e.g., relapsers vs. abstainers). Ranges from 0.5 (coin flip) to 1.0 (perfect). | A single value summarizing the overall diagnostic performance of the biomarker. |
Table 2: Example Performance Metrics from an Addiction Biomarker Study (Structural MRI)
| Biomarker | Condition / Comparison | Area Under Curve (AUC) | Sensitivity | Specificity | Study Details |
|---|---|---|---|---|---|
| Left Insula GMV | Detecting craving state in MA dependence [114] | 0.82 | 78% | 70% | Cut-off point determined by Youden index. |
| Right Insula GMV | Detecting craving state in MA dependence [114] | 0.80 | 70% | 75% | Validated in a follow-up cohort. |
| Right Insula GMV | Predicting future relapse in MA dependence [114] | N/R | 50-55% | 80-90% | Demonstrated high specificity but low sensitivity for predicting relapse. |
| Ventral Striatum Activity (fMRI) | Predicting lower abstinence in CUD [112] | N/R | N/R | N/R | Associated with decreased abstinence in a prospective study. |
N/R: Not explicitly reported in the cited search results.
Experimental Protocols and Methodologies
This section provides detailed methodologies for key experiments cited in the field of addiction biomarker research.
Protocol: Structural MRI for Craving and Relapse Prediction
This protocol is based on a study investigating insula cortex gray matter volume as a biomarker for craving and relapse in methamphetamine dependence [114].
1. Subject Recruitment and Assessment:
- Participants: Recruit subjects meeting diagnostic criteria for substance dependence (e.g., DSM-5). Include exclusion criteria for neurological illness, other substance dependencies, and psychiatric disorders.
- Clinical Measures: Administer the Visual Analog Scale for Craving (VASc) immediately prior to scanning. Define groups (e.g., "craving" vs. "without craving") based on a pre-specified VASc cut-off score.
- Follow-up: Conduct a follow-up assessment (e.g., at 4 months) via interview and urine toxicology to determine relapse status.
2. MRI Data Acquisition:
- Scanner: 3.0-T MRI scanner.
- Sequence: High-resolution T1-weighted structural scan.
- Parameters (Example): Repetition time (TR) = 2000 ms; Echo time (TE) = 2.26 ms; Field of view (FOV) = 256 × 256 mm²; Matrix size = 256 × 256; Slice thickness = 1 mm; 176 slices [114].
3. Data Analysis Pipeline:
- Preprocessing: Use statistical parametric mapping software (e.g., SPM12).
- Segmentation: Segment T1-weighted images into gray matter (GM), white matter, and cerebrospinal fluid.
- Normalization: Spatially normalize images using a high-dimensional registration algorithm (e.g., DARTEL) to a custom template.
- Smoothing: Smooth the modulated, normalized GM images with an 8 mm Gaussian kernel.
- Statistical Analysis:
- Region of Interest (ROI): Define the insula cortex using an automated anatomical labeling atlas.
- Group Comparison: Use a two-sample t-test within the ROI, covarying for age, gender, education, and whole brain volume. Apply a family-wise error (FWE) correction for multiple comparisons.
- Biomarker Performance Assessment:
- Extract mean GMV from significant ROIs.
- Perform Receiver Operating Characteristic (ROC) analysis to evaluate the sensitivity and specificity of the GMV for distinguishing groups.
- Determine an optimal cut-off value (e.g., using the Youden Index) and apply it to the follow-up cohort for validation.
Protocol: Functional MRI (fMRI) for Predicting Treatment Outcome
This protocol summarizes approaches from studies using fMRI to predict abstinence in Cocaine Use Disorder [112].
1. Task-Based fMRI Paradigms:
- Monetary Incentive Delay Task (MIDT): Assesses anticipation of reward. Abnormal activity in the midbrain, ventral striatum, and nucleus accumbens is linked to abstinence outcomes [112].
- Cue-Reactivity Task: Exposes patients to drug-related cues (e.g., images of cocaine paraphernalia) to probe craving-related neural circuits. Activity in the prefrontal cortex (PFC), posterior cingulate (PCC), and temporal lobes has been associated with relapse [112].
- Cognitive Control Tasks (e.g., Stroop Task, Response Inhibition): Measures conflict monitoring and impulse control. Activity in the dorsolateral prefrontal cortex (dlPFC) and anterior cingulate cortex (ACC) during these tasks can predict treatment retention and abstinence [112].
2. Data Acquisition and Analysis:
- Acquisition: Collect blood-oxygen-level-dependent (BOLD) signals during task performance.
- Analysis: Compare brain activity between groups (e.g., abstainers vs. relapsers) or correlate brain activity with future outcomes (e.g., days to relapse) using general linear models.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Biomarker Research in Addiction
| Tool / Reagent | Function / Application | Specific Examples / Notes |
|---|---|---|
| 3.0-T MRI Scanner | High-resolution structural, functional, and neurochemical imaging of the brain. | Essential for acquiring sMRI, fMRI, and DTI data to identify neural correlates of relapse vulnerability [114]. |
| Meso Scale Discovery (MSD) U-PLEX | Multiplexed immunoassay for simultaneous measurement of multiple protein biomarkers (e.g., cytokines, neurotrophins) from a single sample. | Offers superior sensitivity and a broader dynamic range than ELISA; allows for custom panel design [113]. |
| LC-MS/MS (Liquid Chromatography Tandem Mass Spectrometry) | Highly sensitive and specific detection and quantification of low-abundance molecules, including metabolites, neuropeptides, and lipids. | Surpasses ELISA in sensitivity and is useful for detecting low-abundance species in complex biological mixtures [113]. |
| SPM (Statistical Parametric Mapping) | Software for the analysis of brain imaging data sequences (MRI, fMRI, PET). | Standard platform for voxel-based morphometry (VBM) and statistical analysis of functional imaging data [114]. |
| Next-Generation Sequencing (NGS) | Comprehensive analysis of genetic, genomic, and epigenetic variations associated with addiction vulnerability and treatment response. | Used for genotyping, gene expression analysis, and exploring the dopaminergic and opioidergic systems [109] [115]. |
| Structured Clinical Interviews (e.g., SCID) | Gold-standard diagnostic tool for confirming substance use disorder diagnoses and assessing comorbidities. | Critical for ensuring a phenotypically well-defined subject cohort [114]. |
The prospective validation of biomarkers is a complex but essential endeavor for advancing the treatment of substance use disorders. Moving from promising laboratory findings to clinically useful tools requires a disciplined approach that includes a pre-specified analytical plan, rigorous study design to avoid bias, and a clear understanding of the statistical distinction between prognostic and predictive biomarkers. The integration of advanced neuroimaging, genomic, and proteomic technologies, combined with multifactorial models and machine learning, holds the promise of identifying robust biomarkers that can stratify patients, predict relapse vulnerability, and ultimately guide personalized treatment decisions [109]. While the path is fraught with challenges, a methodical commitment to validation standards is the key to translating our growing understanding of the neurobiology of addiction into improved outcomes for patients.
Comparative Efficacy of Neuromodulation vs. Pharmacotherapy for Craving Reduction
Craving, a core feature of substance use disorders (SUDs), is a significant predictor of substance use and relapse [116]. Within the research on the neurobiology of addiction relapse vulnerability, two primary therapeutic approaches have emerged to combat craving: neuromodulation, which directly targets and alters neural circuit activity, and pharmacotherapy, which uses systemically administered drugs to modify neurochemistry. Neuromodulation techniques, such as repetitive Transcranial Magnetic Stimulation (rTMS), use magnetic fields to non-invasively stimulate brain regions implicated in craving [117]. Pharmacotherapy employs medications that act as agonists, antagonists, or mixed agents on neurotransmitter systems to reduce craving and withdrawal symptoms [118]. This review provides a comparative analysis of the efficacy, mechanisms, and methodological protocols of these two approaches, providing a technical guide for researchers and drug development professionals.
Quantitative Efficacy Comparison
Table 1: Efficacy of Neuromodulation for Craving Reduction by Substance
| Substance | Technique | Key Target(s) | Effect Size/Outcome | Evidence Notes |
|---|---|---|---|---|
| Tobacco | rTMS (SFG) | Superior Frontal Gyrus | Reduced craving & withdrawal vs. control (95% CI: 0.0476-7.9559) [116] | Larger effect in men (D=0.59) than women (D=0.30) [116] |
| Tobacco | rTMS (dlPFC) | Dorsolateral Prefrontal Cortex | Medium to large effect sizes (Hedge's g > 0.5) for use & craving [117] | Most promising with multiple sessions [117] |
| Alcohol | rTMS | dlPFC | Promising results; multi-sessions superior to single-sessions [119] | Mixed results in some studies [119] |
| Stimulants | rTMS | dlPFC | Positive outcomes for craving/use reduction [119] | --- |
| Opioids | rTMS | dlPFC | Positive outcomes for craving/use reduction [119] | --- |
| Various | tDCS | dlPFC (Right Anodal) | Medium effect sizes for drug use & craving [117] | Effects highly variable and less robust than rTMS [117] |
| Opioids | Focused Ultrasound | Anterior Cingulate Cortex/Insula | 91% reduction in cravings at 90 days post-treatment [119] | Pilot study (N=8); 62.5% abstinent at 3 months [119] |
Table 2: Efficacy of Pharmacotherapy for Craving Reduction by Substance
| Substance | Medication | Mechanism | Effect Size/Outcome | Evidence Notes |
|---|---|---|---|---|
| Alcohol | Naltrexone | Opioid Receptor Antagonist | NNT to prevent return to any drinking = 20 [91] | Reduces cravings [91] |
| Alcohol | Acamprosate | Multiple | NNT to prevent return to any drinking = 12 [91] | Helps maintain abstinence [91] |
| Alcohol | Disulfiram | Aldehyde Dehydrogenase Inhibitor | Superior to naltrexone & acamprosate in observed dosing [91] | Acts as a deterrent; adherence is a challenge [91] |
| Opioids | Buprenorphine | Partial μ-opioid Agonist | Increases treatment retention and reduces illicit use [118] | Used for maintenance therapy [118] |
| Opioids | Methadone | Full μ-opioid Agonist | Increases treatment retention and reduces illicit use [118] | Used for maintenance therapy [118] |
| Opioids | Naltrexone | Opioid Receptor Antagonist | Reduces likelihood of use by blocking drug effects [118] | --- |
| Nicotine | Bupropion | Atypical Antidepressant | Effective for relapse prevention (OR=1.49) for up to 12 months [91] | --- |
| Nicotine | Varenicline | Partial Nicotinic Agonist | --- | Insufficient evidence on relapse prevention [91] |
Detailed Experimental Protocols
Protocol for rTMS in Tobacco Use Disorder
A recent randomized clinical trial provides a robust protocol for applying rTMS to reduce cigarette craving [116] [120].
- Participant Selection: Participants (aged 18-45) must meet DSM-5 criteria for Tobacco Use Disorder, have a history of daily smoking for ≥1 year, and smoke >4 cigarettes per day. Smoking status is verified via expired carbon monoxide and urinary cotinine tests. Key exclusion criteria include other recent SUDs (except mild cannabis use), major psychiatric conditions, and standard MRI/TMS contraindications [116].
- Study Design: A repeated-measures, crossover design is employed. Participants receive stimulation to all three experimental targets and one control site in a randomized order. Participants are asked to be abstinent for >12 hours before each session [116] [120].
- Stimulation Parameters:
- Equipment: A Magstim Super Rapid2 Plus1 or Magventure Magpro X100 system with a figure-8 coil, coupled with neuronavigation (e.g., Brainsight) for precise targeting [116].
- Targets: Individualized targets within the left dorsolateral prefrontal cortex (dlPFC, executive control network node), left superior frontal gyrus (SFG, salience network node), and left posterior parietal cortex (PPC, default mode network node). Area V5 of the visual cortex serves as an active control [116].
- Protocol: 3000 pulses of 10 Hz stimulation are delivered in 50 trains of 5-second duration, with a 10-second inter-train interval (total duration: 15 minutes). Stimulation intensity is set at 100% of the resting motor threshold [116].
- Outcome Measures:
- Primary Behavioral: Craving is measured using the Urge to Smoke scale (UTS), and withdrawal is measured with the Shiffman-Jarvik Withdrawal Questionnaire (SJWS). These are administered before and immediately after TMS [116] [120].
- Neuroimaging: Resting-state functional MRI (on a 3-Tesla Siemens Prisma scanner) is acquired before and after TMS. Data is processed for motion correction, normalized, and parcellated to analyze within- and between-network functional connectivity of the targeted networks [116].
Protocol for Pharmacotherapy with Agonist Medication
The following general protocol outlines the use of an agonist medication for Opioid Use Disorder, a common pharmacotherapy strategy [118].
- Participant Selection: Patients diagnosed with Opioid Use Disorder per DSM-5 criteria. Medical and psychiatric history is assessed to determine suitability and rule out contraindications.
- Medication Dosing & Administration:
- Induction: For medications like buprenorphine (a partial agonist), treatment is initiated once the patient exhibits clear signs of withdrawal. The initial dose is administered, with subsequent doses titrated upwards over several hours or days until withdrawal suppression and craving reduction are achieved, without precipitating withdrawal or causing oversedation.
- Maintenance: Once stabilized, the patient is maintained on a steady daily dose (e.g., sublingual buprenorphine or supervised methadone administration). The dose may be adjusted periodically based on clinical response, continued substance use, or side effects.
- Monitoring: Adherence and illicit drug use are monitored through regular urine drug screens. Patients are also monitored for medication diversion and assessed for any side effects.
- Adjunct Therapies: Pharmacotherapy is typically combined with psychosocial support, such as Cognitive-Behavioral Therapy (CBT) or contingency management, to address behavioral aspects of addiction and improve long-term outcomes [118].
- Outcome Measures:
- Primary: Self-reported craving, illicit opioid use (verified by urine toxicology), and retention in treatment.
- Secondary: Overdose events, engagement in employment/social activities, and improvement in co-occurring psychiatric symptoms.
Mechanisms of Action
Neuromodulation Targets Neural Circuits of Craving
Neuromodulation techniques directly alter activity in the dysregulated neural circuits that underlie craving and relapse vulnerability. The mesocorticolimbic pathway, particularly involving projections from the prefrontal cortex (PFC) to the nucleus accumbens (NAc), is a primary target [121] [117].
- rTMS: High-frequency (e.g., 10 Hz) rTMS applied to the dlPFC is thought to have an excitatory effect on the underlying cortex. This stimulation can modulate the mesolimbic dopamine system, increasing dopamine release in deeper structures like the NAc [117]. This helps to counteract the chronic hypodopaminergia (low dopamine state) associated with addiction. Furthermore, by enhancing activity in the dlPFC—a key region for executive control, decision-making, and inhibition—rTMS can strengthen top-down control over the reward system, thereby reducing the impulse to use substances triggered by drug cues [117]. The superior frontal gyrus (SFG), a node of the salience network, is a promising target as it may act as a switch between the default mode network (self-referential thought) and the executive control network, a balance that is disrupted during craving [116].
- tDCS: This technique uses a low-intensity electrical current (e.g., 0.5-2.0 mA) to modulate cortical excitability. Anodal stimulation of the right dlPFC is thought to increase excitability in this region, thereby potentially enhancing inhibitory control, while cathodal stimulation of the left dlPFC may suppress hyperactivity associated with craving [117].
- DBS: An invasive technique where electrodes are surgically implanted in deep brain structures like the NAc. High-frequency electrical stimulation is then used to block the abnormal neural activity that drives addictive behaviors within this core reward region [121] [117].
Figure 1: Neuromodulation Targets Craving Neurocircuitry. DBS = Deep Brain Stimulation; rTMS = repetitive Transcranial Magnetic Stimulation; tDCS = transcranial Direct Current Stimulation.
Pharmacotherapy Modulates Neurochemical Signaling
Pharmacological agents reduce craving by acting on specific neurotransmitter receptors to restore chemical balance in the brain's reward and stress systems [118].
- Agonists & Partial Agonists: These substances bind to and activate neurotransmitter receptors. In addiction treatment, they are used to offset the withdrawal and craving caused by receptor under-stimulation when a person stops using a drug. For example, methadone (a full agonist) and buprenorphine (a partial agonist) activate the mu-opioid receptor, but in a controlled manner, which reduces craving and withdrawal without producing the same intense high or euphoria as illicit opioids [118].
- Antagonists: These medications bind to receptors but do not activate them. Instead, they block the receptor, preventing drugs of abuse from binding and producing their rewarding effects. Naltrexone is an opioid receptor antagonist used for both Alcohol and Opioid Use Disorders; by blocking the rewarding effects of alcohol or opioids, it can help reduce craving and the risk of relapse over time [91] [118].
- Other Mechanisms: Disulfiram for alcohol works as a deterrent by inhibiting aldehyde dehydrogenase, causing an unpleasant physical reaction if alcohol is consumed [91]. Acamprosate is thought to stabilize the glutamatergic system, which becomes hyperactive during alcohol withdrawal, thereby reducing post-acute withdrawal symptoms and craving [91].
Figure 2: Pharmacotherapy Mechanisms of Action.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Craving Reduction Research
| Item | Primary Function in Research |
|---|---|
| Magstim Super Rapid2 Plus1 / Magventure Magpro X100 | Magnetic pulse generators for delivering rTMS in clinical trials [116]. |
| Figure-8 Coil / H-Coil | TMS coils for focal or deeper brain stimulation, respectively [117]. |
| Neuronavigation System (e.g., Brainsight) | Ensures precise and consistent TMS targeting across sessions using individual MRI data [116]. |
| 3-Tesla fMRI Scanner | Acquires high-resolution structural and functional MRI data to measure target engagement and network-level changes (e.g., functional connectivity) [116]. |
| Urge to Smoke Scale (UTS) | Validated self-report questionnaire for primary craving measurement in smoking studies [116] [120]. |
| Shiffman-Jarvik Withdrawal Questionnaire (SJWS) | Validated self-report scale for primary withdrawal measurement [116] [120]. |
| Micro+ Smokerlyzer Breath CO Monitor | Objectively verifies smoking status and abstinence via expired carbon monoxide [116]. |
| Urinary Cotinine Test (e.g., Abbott NicQuick) | Biochemically verifies recent nicotine use and confirms smoking status [116]. |
| Urinalysis Test Cups (e.g., Abbott iCup) | Screens for illicit substance use to maintain abstinence requirements in study protocols [116]. |
| FDA-approved Agonists/Antagonists (e.g., Buprenorphine, Naltrexone) | Active comparators in clinical trials for evaluating the relative efficacy of novel neuromodulation or pharmacological treatments [91] [118]. |
Addiction is a chronic, relapsing neuropsychiatric disorder characterized by compulsive substance use despite adverse consequences, with high rates of relapse presenting a formidable treatment challenge [122] [123]. Conventional pharmacotherapies targeting dopaminergic systems have demonstrated only modest long-term efficacy, highlighting the critical need for novel treatment strategies that address the complex neurobiological mechanisms underlying relapse vulnerability [122]. Recent research has illuminated several promising non-dopaminergic targets, including glucagon-like peptide-1 (GLP-1) receptors, neurokinin systems, and neuroimmune mechanisms. This whitepaper provides a comprehensive technical review of these emerging pharmacological targets, focusing on their mechanistic underpinnings, preclinical validation, and translational potential for preventing addiction relapse. The integration of metabolic signaling, neuropeptide systems, and neuroimmune mechanisms represents a paradigm shift in addiction therapeutics that may ultimately lead to more effective interventions for substance use disorders.
GLP-1 Receptor Agonists
Mechanisms of Action
GLP-1 receptor agonists (GLP-1RAs), originally developed for type 2 diabetes and obesity, have emerged as promising modulators of reward-related brain circuits relevant to addiction [122] [124]. Glucagon-like peptide-1 (GLP-1) is a gut-derived incretin hormone secreted by enteroendocrine L-cells in response to nutrient ingestion, with additional production by preproglucagon neurons in the Nucleus Tractus Solitarius (NTS) [122]. The GLP-1 receptor (GLP-1R) belongs to the class B family of G protein-coupled receptors (GPCRs) and is expressed not only in metabolic centers but also in reward-relevant brain regions including the ventral tegmental area (VTA), nucleus accumbens (NAc), and prefrontal cortex (PFC) [122] [125].
GLP-1R signaling primarily occurs through Gαs-mediated increases in cAMP levels and protein kinase A (PKA) activation, though it also engages β-arrestin-mediated MAPK signaling [122]. Different GLP-1RAs exhibit distinct signaling bias, with semaglutide demonstrating G protein-biased agonism that favors prolonged cAMP signaling while limiting β-arrestin recruitment, potentially enhancing therapeutic efficacy [122]. These receptors are positioned to influence addiction processes through multiple mechanisms: (1) direct modulation of dopaminergic neurotransmission in the mesolimbic pathway; (2) interaction with glutamatergic and GABAergic pathways in mesocorticolimbic circuits; (3) integration of peripheral metabolic signals via gut-brain vagal pathways; and (4) potential modulation of neuroinflammatory processes [122] [125].
Table 1: GLP-1 Receptor Expression in Addiction-Relevant Brain Regions
| Brain Region | Function in Addiction | Mechanism of Action |
|---|---|---|
| Ventral Tegmental Area (VTA) | Inhibits drug reward and motivation | Decreases dopamine neuron firing via increased VTA GABA neuron activity [122] |
| Nucleus Accumbens (NAc) | Reduces drug reward | Inhibits dopamine signaling and alters synaptic plasticity [122] |
| Prefrontal Cortex (PFC) | Modulates cognitive control, craving | Increases GABAergic tone; effects on executive function [122] [126] |
| Area Postrema/NTS | Mediates nausea side effects | Activates GLP-1Rs outside blood-brain barrier; triggers emetic reflex [122] |
Preclinical and Clinical Evidence
Preclinical studies demonstrate that GLP-1R activation reduces the reinforcing properties of addictive substances across multiple drug classes. GLP-1R agonists attenuate intake and relapse-like behavior for alcohol, nicotine, cocaine, and opioids in rodent models [122] [124] [125]. Specifically, these compounds reduce voluntary alcohol consumption, prevent relapse, and blunt stress-induced alcohol seeking [126]. Mechanistically, these behavioral effects correlate with reduced dopamine release and decreased activation in reward centers [126].
Clinical evidence, though more limited, supports the potential efficacy of GLP-1RAs in substance use disorders. Early-phase clinical trials suggest safety and potential efficacy in reducing craving [122]. A randomized controlled trial with low-dose semaglutide reduced laboratory alcohol self-administration, drinks per drinking days, and craving in people with alcohol use disorder (AUD) [124]. Interestingly, effects may be more pronounced in specific subgroups; exenatide reduced alcohol intake in individuals with AUD and comorbid obesity but not in the overall study population [124]. Beyond alcohol, preliminary evidence suggests potential benefits for tobacco use disorder, with GLP-1RAs reducing cigarettes per day and preventing weight gain after smoking cessation [124]. In rodent models, GLP-1RAs reduce self-administration of heroin, fentanyl, and oxycodone, and decrease reinstatement of drug seeking [124].
Diagram 1: GLP-1 receptor signaling in addiction. GLP-1RAs activate GLP-1 receptors, primarily signaling through Gαs to increase cAMP and PKA activation, leading to VTA GABA neuron activation that reduces dopamine release in the NAc and drug reward. Biased agonists like semaglutide limit β-arrestin recruitment.
Experimental Protocols for GLP-1 Research
Operant Self-Administration with Reinstatement:
- Animals: Male and female rodents (typically rats or mice)
- Drug Preparation: GLP-1RAs (e.g., semaglutide, liraglutide, exenatide) dissolved in appropriate vehicle, administered via subcutaneous injection
- Dosing Regimen: Acute or chronic administration (varies by compound; semaglutide typically administered once daily or less frequently due to long half-life)
- Behavioral Procedure:
- Training Phase: Animals trained to self-administer drug (e.g., alcohol, nicotine, cocaine) via lever press or nose poke in operant chambers
- Maintenance: Stable self-administration established (typically 2-3 weeks)
- Extinction: Drug delivery discontinued, responding gradually decreases
- Reinstatement Test: Drug-seeking behavior precipitated by stress (e.g., footshock), drug-paired cues, or drug priming
- Outcome Measures: Number of active vs. inactive responses during self-administration; response rate during extinction; reinstatement of drug-seeking behavior
Alcohol Two-Bottle Choice Protocol:
- Procedure: Continuous or intermittent access to two bottles - one with alcohol solution (typically 10-20% v/v), one with water
- GLP-1RA Administration: Acute or chronic treatment during access period
- Measurements: Daily alcohol and water intake; preference ratio (alcohol/total fluid)
Neurokinin Receptor Antagonists
NK1 Receptor Mechanisms
Neurokinin receptors, particularly neurokinin-1 (NK1R), represent another promising target for addiction treatment. Substance P (SP) is the primary endogenous ligand for NK1R, with both SP and NK1R widely distributed in brain regions mediating affective behaviors, including the amygdala, striatum, hippocampus, and brainstem [127]. NK1Rs are primarily coupled to the Gαq mechanism, stimulating phospholipase C activity to cleave PIP2 into IP3 and diacylglycerol, resulting in calcium mobilization and activation of protein kinases including calcium/calmodulin kinase and protein kinase C [127].
NK1R activation generally exerts a positive, stimulatory effect on dopaminergic signaling in the mesolimbic pathway [127]. Morphine administration induces SP release in the VTA, and NK1R antagonism attenuates dopamine release in the NAc following morphine injection [127]. Genetic deletion or pharmacological antagonism of NK1R reduces morphine self-administration and conditioned place preference [127]. One of the most consistent findings across drug classes is that NK1R antagonism attenuates stress-induced reinstatement of drug seeking, likely mediated through the extended amygdala stress circuitry [127].
Table 2: Neurokinin Receptor Roles in Addiction-Related Behaviors
| Receptor Type | Primary Ligand | Key Functions in Addiction | Drug Classes Affected |
|---|---|---|---|
| NK1 Receptor | Substance P | Stress-induced reinstatement; opiate reward; escalated alcohol seeking | Opiates, alcohol, cocaine, nicotine |
| NK3 Receptor | Neurokinin B | Alcohol consumption; cocaine-induced behaviors | Alcohol, cocaine |
Preclinical and Clinical Evidence
NK1 receptor antagonism demonstrates particularly robust effects on stress-induced relapse across multiple substance classes. The NK1 antagonist L822429 potently and dose-dependently suppresses footshock stress-induced reinstatement of alcohol seeking in rats, with essentially complete suppression at the highest dose, without affecting alcohol self-administration or cue-induced reinstatement [128]. This effect is behaviorally specific, as L822429 did not affect conditioned suppression of operant responding, locomotor activity, or self-administration of sucrose solution [128].
For alcohol, NK1R inhibition attenuates alcohol consumption in C57BL/6J mice, which naturally consume high amounts of alcohol [127]. NK1R antagonism also blocks escalated alcohol consumption induced by chronic social defeat stress, which concomitantly increases NK1R expression [127]. Similar effects extend to opioids and psychostimulants, with NK1R antagonism reducing morphine self-administration and conditioned place preference, while also influencing neurochemical and behavioral responses to cocaine [127].
Clinical studies have yielded mixed but promising results. Genetic association studies link NK1R (TACR1) polymorphisms with risk of alcohol abuse and related comorbid disorders [127]. The FDA-approved NK1R antagonist aprepitant (for chemotherapy-induced nausea) has been investigated for addiction, with some studies showing reduced alcohol craving and consumption, though results have been inconsistent [127]. This variability may reflect methodological differences or genetic heterogeneity in treatment response.
Experimental Protocols for Neurokinin Research
Stress-Induced Reinstatement Protocol:
- Animals: Rats (commused Sprague-Dawley or Wistar)
- NK1 Antagonist: L822429 (specifically engineered for high affinity at rat NK1R) at doses 15 and 30 mg/kg
- Procedure:
- Self-Administration Training: Rats trained to self-administer drug (e.g., alcohol) in daily 30-min sessions
- Extinction: Drug delivery discontinued until operant responding reaches extinction criterion
- Reinstatement Test: Following pretreatment with NK1 antagonist, footshock stress (typically intermittent, 0.5-0.8 mA) administered to precipitate drug-seeking
- Controls: Include vehicle-treated groups; test specificity using cue-induced reinstatement and natural reward self-administration
- Outcome Measures: Number of active responses during reinstatement test; comparison across treatment groups
Conditioned Place Preference (CPP) with NK1 Manipulation:
- Apparatus: Two or three-chamber place conditioning apparatus with distinct contextual cues
- Procedure:
- Pre-test: Baseline preference assessed
- Conditioning: Drug paired with non-preferred chamber, vehicle with preferred chamber
- Test: Preference assessed drug-free
- NK1 Manipulation: NK1 antagonist administered during acquisition, expression, or both
- Measurements: Time spent in drug-paired chamber; locomotor activity
Diagram 2: NK1 receptor signaling in stress-induced reinstatement. Stress exposure triggers substance P release, activating NK1 receptors coupled to Gαq signaling, ultimately enhancing dopamine transmission and promoting drug-seeking. NK1 antagonists block this pathway.
Neuroimmune Mechanisms
Neuroimmune Signaling in Addiction
The hypothesis that neuroimmune mechanisms contribute significantly to drug reward and addiction represents a fundamental shift in understanding substance use disorders [129]. Drugs of abuse interact with the neuroimmune system, altering neuroimmune gene expression and signaling, which in turn modulates various aspects of addiction [130]. The key conceptual advancement is that proinflammatory immune signaling within the central nervous system enhances engagement of classical mesolimbic dopamine reward pathways and withdrawal centers [129].
Microglia and astrocytes perform critical functions in synapse formation and refinement, and disruptions in glial function are implicated in numerous neurological disorders, including addiction [32]. Drugs of abuse can activate microglia and astrocytes through signaling at innate immune receptors, influencing neuronal function through secretion of soluble factors (cytokines, chemokines) and potentially through direct remodeling of synapses [32]. Alcohol and other substances activate Toll-like receptor 4 (TLR4) signaling, triggering downstream neuroimmune cascades that enhance drug reward [129]. This neuroimmune activation occurs in key addiction-relevant regions including the VTA, NAc, and amygdala [130] [32].
Table 3: Neuroimmune Signaling Molecules in Addiction
| Immune Factor | Function in Normal CNS | Role in Addiction |
|---|---|---|
| TLR4 Receptors | Pattern recognition; innate immunity | Primary trigger for drug-induced neuroinflammation; enhances reward [129] |
| Proinflammatory Cytokines (TNFα, IL-1β) | Synaptic scaling; LTP modulation | Enhance drug reward; contribute to dependence [130] [32] |
| Chemokines (CCL2, CXCL12) | Neuronal migration; neurodevelopment | Regulate neurotransmitter release (glutamate, GABA, DA) [130] |
| Microglia | Synaptic pruning; circuit refinement | Mediate drug-induced synaptic alterations [32] |
Mechanisms and Evidence
Neuroimmune mechanisms influence addiction processes through multiple pathways: (1) modulation of synaptic function via cytokine and chemokine regulation of neurotransmitter release; (2) mediation of neuroinflammation through microglial activation; (3) regulation of neurodevelopment and adult neurogenesis; and (4) modulation of neuroendocrine function, particularly HPA axis responses to stress [130].
Specific immune molecules have been implicated in synaptic modulation relevant to addiction. Chemokines CCL2 and CXCL12 regulate the release of several neurotransmitters, including glutamate, GABA, and dopamine [130]. The chemokine receptor CCR2 cross-desensitizes GABAA and mu-opioid receptors [130]. Proinflammatory cytokines such as TNFα differentially modulate trafficking of AMPA-type glutamate receptors and GABA receptors, regulating synaptic strength by facilitating excitatory synaptic transmission while decreasing inhibitory synaptic transmission [130].
Evidence from animal models demonstrates that alcohol exposure significantly impacts the neuroimmune system. Expressions of immune-related genes are altered in human alcoholic brains and differentially correlated with high and low alcohol consuming rodent lines [130]. Opioid activation of central immune signaling, particularly through TLR4, contributes substantially to opioid reward and dependence [129]. Additionally, adolescent binge drinking leads to persistent upregulation of innate immune signaling in the prefrontal cortex that correlates with adult neurocognitive dysfunction [130].
Experimental Protocols for Neuroimmune Research
TLR4 Signaling Assessment in Drug Reward:
- Animals: Wild-type and TLR4 knockout mice
- Drug Treatment: Acute or chronic administration of drug of abuse (e.g., morphine, alcohol)
- Procedures:
- Conditioned Place Preference: Assess reward using standard CPP protocol
- Microglial Activation: Immunohistochemistry for Iba1 (microglial marker) and CD11b (activation marker)
- Cytokine Measurement: ELISA or multiplex assays for TNFα, IL-1β, IL-6 in brain homogenates
- Gene Expression: qPCR for cytokine and chemokine mRNA in reward-relevant brain regions
- Pharmacological Manipulation: TLR4 antagonists (e.g., (+)-naltrexone) administered prior to drug exposure
Glial-Neuronal Coculture Studies:
- Cell Cultures: Primary microglia/astrocytes with neuronal cultures from rodent brain
- Drug Exposure: Add drug of abuse to culture medium
- Measurements:
- Cytokine release into medium (ELISA)
- Neuronal dendritic morphology and spine density
- Synaptic protein expression (Western blot)
- Electrophysiological recordings of synaptic function
The Scientist's Toolkit: Research Reagents & Materials
Table 4: Essential Research Reagents for Addiction Pharmacology Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| GLP-1 Receptor Agonists | Semaglutide, Liraglutide, Exenatide | Reward and relapse studies | Modulate dopamine signaling via GLP-1 receptors in VTA/NAc [122] [124] |
| Neurokinin Antagonists | L822429 (rat-specific), Aprepitant | Stress-induced reinstatement models | Block NK1 receptors to attenuate stress-driven relapse [128] [127] |
| TLR4 Antagonists | (+)-Naltrexone, LPS-RS | Neuroimmune mechanism studies | Inhibit innate immune activation by drugs of abuse [129] |
| Genetic Models | NK1R knockout mice, TLR4 knockout mice | Target validation studies | Determine necessity of specific receptors for drug effects [127] |
| Behavioral Assays | Operant self-administration, Conditioned Place Preference, Elevated Plus Maze | Preclinical efficacy assessment | Measure reward, reinforcement, anxiety-like behavior [128] [127] |
| Neurochemical Analysis | Microdialysis, Fast-Scan Cyclic Voltammetry | Mechanism studies | Measure dopamine release in NAc and other regions [122] |
| Immunohistochemistry | Iba1 (microglia), GFAP (astrocytes), c-Fos (activation) | Neuroimmune activation mapping | Visualize glial activation and neuronal ensemble engagement [32] |
Integrated Signaling Pathways in Relapse Vulnerability
Diagram 3: Integrated pathways in relapse vulnerability. Multiple triggers (stress, drug cues, drug exposure) converge on VTA dopamine activity through distinct but interacting pathways. Novel therapeutics target these pathways at different points to reduce relapse vulnerability.
The emerging targets reviewed herein—GLP-1 receptors, neurokinin systems, and neuroimmune mechanisms—represent significant advances in the neurobiology of addiction relapse vulnerability. These systems interact with traditional reward circuitry while introducing novel signaling pathways that may be leveraged for therapeutic benefit. GLP-1RAs show particular promise due to their pleiotropic actions on reward processing, stress responses, and cognitive function, combined with favorable pharmacokinetic profiles and clinical tolerability [122] [124] [126]. NK1 antagonists offer a targeted approach specifically for stress-induced relapse, a major clinical challenge in addiction maintenance [128] [127]. Neuroimmune modulators address the increasingly recognized role of glial cells and immune signaling in persistent addiction adaptations [129] [130] [32].
Future research directions should include: (1) optimization of biased signaling profiles for GLP-1RAs to maximize therapeutic effects while minimizing side effects; (2) identification of patient subgroups most likely to respond to specific mechanisms; (3) development of compounds with improved blood-brain barrier penetration and central exposure; and (4) exploration of combination therapies targeting multiple systems simultaneously. The continued elucidation of these novel pharmacological targets holds considerable promise for addressing the persistent challenge of relapse in substance use disorders.
Relapse, the resumption of substance use after a period of abstinence, remains the most significant challenge in treating substance use disorders (SUDs). Despite the unique pharmacological profiles of different addictive substances, a conserved neurobiological framework underpins the vulnerability to relapse across substances. This whitepaper delineates the shared and distinct pathways that perpetuate the relapse cycle, synthesizing evidence from behavioral, neurochemical, and circuit-level studies. The core thesis is that while the initial molecular targets of various drugs differ, the ensuing neuroadaptations converge upon a final common pathway involving the basal ganglia, extended amygdala, and prefrontal cortex. Understanding these cross-substance mechanisms is paramount for developing novel, targeted interventions that disrupt the relapse cycle and improve long-term treatment outcomes.
Neurobiological Framework of Relapse: The Three-Stage Cycle
Decades of research have established that addiction is a chronic brain disorder characterized by a recurring cycle of three distinct stages: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation (craving) [4] [3]. This cycle is driven by progressive and enduring neuroadaptations in specific brain circuits, which become more severe with continued substance use and reduce an individual's ability to control their substance use [4].
Binge/Intoxication Stage: This stage is centered on the rewarding and reinforcing effects of the substance. All addictive substances directly or indirectly increase dopamine signaling in the basal ganglia, particularly the nucleus accumbens (NAc), which produces feelings of pleasure and reinforces the substance-taking behavior [4] [3]. With repeated use, the dopamine response shifts from the substance itself to the cues associated with it (people, places, paraphernalia), a process known as incentive salience [3].
Withdrawal/Negative Affect Stage: When substance use ceases, the brain's attempt to counteract the chronic perturbation leads to a withdrawal state. This stage is primarily mediated by the extended amygdala and its stress systems [4] [3]. Key changes include a decrease in baseline dopaminergic activity (leading to anhedonia) and the recruitment of brain stress neurotransmitters, such as corticotropin-releasing factor (CRF) and dynorphin, leading to feelings of unease, anxiety, and irritability [39] [3]. Substance use is then negatively reinforced to alleviate this dysphoric state.
Preoccupation/Anticipation Stage: This stage involves the relapse to drug seeking after abstinence. The prefrontal cortex (PFC), critical for executive functions like impulse control, decision-making, and emotional regulation, is central to this stage [4] [3]. Chronic substance use disrupts the PFC, leading to executive dysfunction, characterized by heightened craving, impaired impulse control, and poor decision-making when confronted with drug-related cues, stress, or the substance itself [131] [3].
Table 1: Primary Brain Regions and Neurotransmitters in the Relapse Cycle
| Stage of Cycle | Core Brain Region | Key Neurotransmitters/Systems Involved | Primary Behavioral Output |
|---|---|---|---|
| Binge/Intoxication | Basal Ganglia (Nucleus Accumbens) | Dopamine, Opioid Peptides | Positive Reinforcement, Habit Formation |
| Withdrawal/Negative Affect | Extended Amygdala | CRF, Dynorphin, Norepinephrine | Negative Reinforcement, Stress, Anxiety |
| Preoccupation/Anticipation | Prefrontal Cortex | Glutamate, Dopamine | Craving, Impaired Executive Control, Relapse |
Primary Triggers of Relapse: Cross-Substance Commonalities
Research in both humans and animal models has consistently identified three primary triggers for relapse: exposure to drug-associated cues, exposure to stress, and re-exposure to a small amount of the drug itself (a "priming" dose) [39]. These triggers can precipitate craving and drug-seeking behavior by acting upon the compromised neural circuits described above.
Drug-Associated Cues: Environmental stimuli previously paired with drug use (e.g., sight of a needle, a specific location) acquire conditioned incentive value through learning processes. Upon re-exposure, these cues can trigger a powerful dopamine release in the mesolimbic pathway, reinstating drug-seeking behavior [39] [44]. Brain imaging studies show that cue exposure activates regions including the dorsolateral prefrontal cortex (DLPFC), ventral striatum, and amygdala [44].
Stress: Acute stressors activate the extended amygdala and its CRF and norepinephrine systems. This stress state enhances the salience of drug-related cues and creates a negative emotional state that motivates drug use to achieve relief, thereby driving relapse [39]. Notably, a history of chronic drug use can lead to a sensitized stress response, making individuals more vulnerable to stress-induced relapse.
Drug Priming: A small dose of the previously used drug can trigger intense craving and relapse by rapidly activating the reward circuitry, thereby "renewing the significance or salience of the learned stimulus–drug associations" [39]. This suggests the priming injection acts to restore the incentive value of drug-related cues.
The neural circuits mediating these triggers are partially dissociable but share common pathways, particularly the mesocorticolimbic dopamine system and its glutamatergic connections [39].
Cross-Substance Comparison of Relapse Mechanisms
While the overarching three-stage cycle and relapse triggers are conserved, the specific neuropharmacological actions of different drug classes can lead to nuanced differences in how relapse manifests.
Table 2: Comparative Analysis of Relapse Mechanisms Across Substance Classes
| Substance Class | Key Molecular Targets | Shared Relapse Pathways | Substance-Specific Nuances in Relapse |
|---|---|---|---|
| Psychostimulants(e.g., Cocaine, Methamphetamine) | Dopamine Transporter (DAT),Monoamine Transporters | Strong cue-induced reinstatement;Major PFC/executive dysfunction | Potent induction of incentive salience;Drug priming is a powerful trigger. |
| Opioids(e.g., Heroin, Fentanyl) | μ-Opioid Receptors | Profound stress-induced reinstatement;Severe withdrawal/negative affect | Dysphoria and physical distress in withdrawal are pronounced drivers; High overdose risk upon relapse due to lost tolerance. |
| Alcohol | GABAA Receptors, NMDA Receptors | Strong cue- and stress-induced reinstatement | Withdrawal involves significant glutamatergic hyperactivity; FDA accepts "reduction in heavy drinking days" as a clinical endpoint [132]. |
| Nicotine | Nicotinic Acetylcholine Receptors (nAChRs) | Powerful cue-reactivity | Smoking cues are pervasive in environment; 50% reduction in cigarettes smoked is a meaningful endpoint for cancer risk reduction [132]. |
| Cannabis | CB1 Cannabinoid Receptors | Cue-induced craving | Reduced use (even non-abstinence) is associated with clinical improvement (e.g., sleep, CUD symptoms) [132]. |
Key Experimental Models and Methodologies
The "reinstatement model" in rodents is the gold standard for studying the neurobiology of relapse [39]. This model allows for the systematic investigation of cue-, drug-, and stress-induced relapse in a controlled laboratory setting.
Reinstatement Model Protocol
Objective: To investigate the neural mechanisms and pharmacological modulation of drug-seeking behavior triggered by cues, stress, or a priming drug dose.
Subjects: Typically, laboratory rats or mice.
Apparatus: Operant conditioning chambers equipped with two levers (an "active" lever that delivers drug/saline and a "inactive" lever) and a cue light/tone.
Procedure:
Self-Administration Training:
- Animals are trained to press the active lever to receive an intravenous infusion of a drug (e.g., cocaine, heroin) or oral alcohol.
- Each drug infusion is paired with a presentation of a conditioned stimulus (CS), such as a light or tone.
- Training continues until stable self-administration behavior is established.
Extinction Training:
- The drug is no longer available. Pressing the active lever results in the delivery of saline (or nothing) and the CS is not presented.
- This phase continues until the animal's lever-pressing behavior declines to a predetermined low level, indicating that the behavior is extinguished.
Reinstatement Test:
- Animals are divided into groups and exposed to one of the following triggers, while drug remains unavailable:
- Cue-Induced Reinstatement: Response-contingent presentation of the previously drug-paired CS.
- Drug-Priming-Induced Reinstatement: A non-contingent, experimenter-administered injection of a low dose of the training drug or a pharmacologically similar drug.
- Stress-Induced Reinstatement: Exposure to an acute stressor, such as intermittent footshock.
- The primary dependent variable is the number of responses on the previously active lever during the test session. A significant increase in lever pressing indicates reinstatement of drug-seeking behavior.
- Animals are divided into groups and exposed to one of the following triggers, while drug remains unavailable:
Electrophysiological Biomarkers in Human Research
Human studies complement animal models by using non-invasive techniques like electroencephalography (EEG) to identify Event-Related Potentials (ERPs) as biomarkers of addiction-related neurocognitive deficits [44].
- Protocol: Participants are typically presented with substance-related and neutral cues in inhibitory control paradigms (e.g., Go/NoGo, Oddball tasks) while EEG is recorded.
- Key ERP Components:
- N2/NoGo-N2: A negative deflection ~200-350ms post-stimulus, reflecting conflict monitoring and response inhibition. Reduced NoGo-N2 amplitudes are observed in alcohol, tobacco, cannabis, and heroin use disorders, indicating impaired cognitive control [44].
- P3/P300: A positive deflection ~300-600ms post-stimulus, associated with attentional allocation and contextual updating. Enhanced P3 amplitudes in response to drug cues reflect attentional bias and are predictive of treatment outcomes [44].
- Error-Related Negativity (ERN): A negative deflection following an error commission, linked to performance monitoring. Blunted ERN is found in individuals with substance use disorders, suggesting reduced error awareness.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Relapse Pathway Research
| Item/Category | Function/Application in Research | Specific Examples |
|---|---|---|
| Operant Conditioning Chambers | Controlled environment for measuring drug self-administration, extinction, and reinstatement of drug-seeking behavior. | Med Associates (Fairfax, VT, USA) operant chambers with levers, cue lights, tone generators, and drug infusion pumps. |
| Drug Solutions for Rodent Models | Used in self-administration and priming studies to model human drug taking and relapse. | Cocaine HCl, Heroin (Diacetylmorphine HCl), Ethanol, Nicotine hydrogen tartrate salt, dissolved in sterile saline or vehicle. |
| Selective Pharmacological Agents | To dissect the neurochemical mechanisms of relapse via targeted receptor agonism/antagonism. | Dopamine D1/D2 receptor antagonists (SCH-23390, Raclopride); CRF receptor antagonists (e.g., R121919); NMDAR antagonists (MK-801). |
| Viral Vector Systems | For cell-type-specific manipulation of neural circuits (optogenetics, chemogenetics) to establish causality. | Adeno-Associated Viruses (AAVs) for Cre-dependent expression of Channelrhodopsin (ChR2) or Designer Receptors Exclusively Activated by Designer Drugs (DREADDs). |
| Positron Emission Tomography (PET) Ligands | Non-invasive imaging of receptor availability and neurotransmitter dynamics in the human and animal brain. | [¹¹C]Raclopride for dopamine D2/D3 receptor binding; [¹¹C]Carfentanil for μ-opioid receptor binding. |
| Electroencephalography (EEG) Systems | Recording high-temporal-resolution brain activity to assess cognitive and cue-reactivity biomarkers (ERPs). | High-density (64-128 channel) EEG systems from vendors like Brain Vision (Morrisville, NC, USA) or BioSemi (Amsterdam, Netherlands). |
Implications for Treatment Development and Future Directions
The recognition of shared relapse pathways provides a robust framework for developing treatments that target core mechanisms rather than specific substances. The Addictions Neuroclinical Assessment (ANA) is a dimensional framework that translates the three-stage cycle into three measurable domains: incentive salience, negative emotionality, and executive function [131] [3]. This allows for a more personalized assessment and treatment approach.
Beyond Abstinence: There is a growing movement to recognize reduced substance use as a valid and clinically meaningful endpoint in treatment trials, similar to how reduced heavy drinking days is accepted for Alcohol Use Disorder [132]. Evidence shows that reduced use of cocaine, methamphetamine, and cannabis is associated with significant improvements in psychosocial functioning and addiction severity [132].
Neuromodulation: Techniques like transcranial Magnetic Stimulation (TMS) and transcranial Direct Current Stimulation (tDCS) are being explored to target dysfunctional circuits, particularly in the PFC, to reduce craving and improve cognitive control [44].
Biomarker-Driven Interventions: Future directions include the development of closed-loop systems that can detect addiction-related neurophysiological signatures (e.g., specific ERPs) and deliver adaptive neuromodulation to preempt relapse [44].
In conclusion, the pathways to relapse demonstrate a remarkable conservation across different substances of abuse, converging on a core network of brain regions and processes. A deep understanding of these commonalities and subtle divergences is critical for forging new paths in the treatment and prevention of substance use disorders.
The neurobiology of addiction relapse vulnerability is fundamentally linked to the brain's capacity for repair following chronic substance use. Longitudinal research designs are critical for disentangling the pre-existing neural vulnerabilities from the consequences of drug exposure and for mapping the dynamic trajectory of recovery. This review synthesizes evidence from neuroimaging, behavioral, and clinical studies to delineate the temporal patterns of neural and functional recovery. Evidence indicates that abstinence-mediated neuroplasticity enables significant, albeit often partial, restoration of brain structure and function. This recovery is not uniform; it proceeds along distinct timelines across different neural circuits and is modulated by a complex interplay of neurobiological, clinical, and social factors. A deeper understanding of these trajectories is paramount for developing targeted, evidence-based interventions that can effectively mitigate relapse risk.
Addiction is a chronically relapsing disorder characterized by a compulsive cycle of binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation (craving) [2]. This cycle is subserved by specific, yet overlapping, neurocircuits. The transition to addiction involves neuroplasticity across these circuits, beginning with changes in the mesolimbic dopamine system and cascading to the dorsal striatum, orbitofrontal cortex, prefrontal cortex, and extended amygdala [2]. These adaptations underpin the core clinical features of addiction: loss of control over intake, compulsive drug-seeking, and the emergence of a negative emotional state during withdrawal.
Relapse vulnerability is a hallmark of Substance Use Disorders (SUD), and its neurobiological basis is rooted in the persistence of these drug-induced neuroadaptations. Cross-sectional studies, while valuable, are often confounded by between-subject variability and cannot establish causality [133]. Longitudinal within-subject designs are therefore essential to directly explore the temporal dynamics of abstinence-mediated neural recovery and its relationship with sustained abstinence or relapse. Elucidating the trajectory of brain recovery—identifying which systems recover, in what sequence, and at what pace—forms a heuristic basis for identifying targets for relapse prevention [133].
Neurobiological Foundations of Recovery
The brain's capacity for change, or neuroplasticity, is the central mechanism enabling recovery from SUD. Neuroplasticity encompasses synaptic remodeling, structural changes in gray and white matter, and functional reorganization of neural networks [134]. In the context of addiction, the reversal of drug-induced maladaptive plasticity is a key process. Recovery is not merely the absence of the drug but an active process of neural repair.
Longitudinal neuroimaging studies provide the most direct evidence for this plasticity. A systematic review of such studies found that the majority demonstrated at least partial neurobiological recovery with abstinence [133]. This recovery manifests in a region-specific and time-dependent manner:
- Structural Recovery: Increases in gray matter volume have been observed predominantly in the frontal cortical regions (including the middle and inferior frontal gyrus, cingulate, and precentral gyrus), insula, hippocampus, and cerebellum [133].
- Functional and Neurochemical Recovery: Restoration of normal brain activity and neurochemistry has been documented in prefrontal cortical regions and several subcortical structures [133].
The timing of these changes is crucial. Structural recovery appears to commence soon after cessation, while full functional recovery may require longer periods of abstinence [133]. This temporal dissociation suggests that the restoration of brain tissue may be a precursor to the normalization of complex neural circuit functions essential for cognitive control and emotional regulation.
Longitudinal Evidence for Neural and Functional Recovery
Longitudinal studies tracking individuals over time are indispensable for characterizing the trajectory of recovery. The evidence reveals a complex picture of interrelated changes across structural, functional, and behavioral domains.
Structural and Functional Neuroimaging Data
A systematic review of 45 longitudinal neuroimaging studies in treatment-seeking individuals with SUD provides robust evidence for brain recovery. The following table synthesizes key findings on regional brain changes observed during abstinence.
Table 1: Longitudinal Brain Changes During Abstinence from Substance Use Disorders
| Brain Region | Type of Change | Substance Studied | Approximate Abstinence Period | Key Findings |
|---|---|---|---|---|
| Frontal Cortex | Structural (GM Volume) | Alcohol | 2 weeks | ↑ volume in middle/inferior frontal gyrus, cingulate gyrus, precentral gyrus [133] |
| Insula | Structural (GM Volume) | Alcohol | 2 weeks | ↑ volume [133] |
| Hippocampus | Structural (GM Volume) | Alcohol | 2 weeks | ↑ volume in hippocampal subfields (CA2+3) [133] |
| Cerebellum | Structural (GM Volume) | Alcohol | 2 weeks | ↑ volume [133] |
| Subcortical Regions | Structural (GM Volume) | Alcohol | 1 day vs. 2 weeks | ↓ volume in amygdala, putamen, nucleus accumbens at 1-day abstinence; some recovery possible [133] |
| Prefrontal Cortex | Functional / Neurochemical | Multiple | Varies (protracted) | Normalization of activity and neurochemistry [133] |
These structural improvements often parallel cognitive and functional gains. For instance, recovery in frontal cortical regions and the hippocampus is likely associated with improvements in executive function, response inhibition, and memory, which are critical for maintaining abstinence [133].
Trajectories of Functional and Behavioral Recovery
Beyond neural changes, the restoration of real-world function is a critical outcome. Longitudinal assessments in other neurological disorders provide models for understanding these trajectories. In patients with first-episode psychosis, data-driven cluster analysis identified four distinct functional recovery trajectories: "Poor," "Intermediate," "High," and "Catch-up" [135]. This heterogeneity highlights that recovery is not a universal experience and is influenced by risk factors such as poor premorbid adjustment, low executive function, and substance use history [135].
Similarly, research on spinal cord injury recovery in animal models, such as zebrafish, emphasizes the value of longitudinal tracking and multi-parameter assessment. These studies can correlate cellular regeneration (e.g., axonal bridging) with the recovery of complex behaviors, establishing a direct link between neural repair and functional restoration [136].
Experimental Protocols for Key Methodologies
To facilitate replication and further research, this section details the core methodologies employed in the cited longitudinal studies.
Longitudinal Neuroimaging Study Protocol
This protocol is adapted from studies investigating brain recovery in alcohol use disorder [133].
- Objective: To quantify within-subject changes in brain structure and function during early and protracted abstinence.
- Participants: Treatment-seeking individuals with SUD (sample size ≥10 at follow-up) and matched healthy controls.
- Design:
- Timepoints: Minimum of two assessment timepoints, with an inter-scan interval greater than 24 hours. A common paradigm involves scans at ~1-3 days of abstinence (T1) and again at ~2 weeks of abstinence (T2), with longer follow-ups for protracted abstinence.
- Abstinence Monitoring: Verified via self-report, biological markers (e.g., breathalyzer, urine toxicology), and clinical observation.
- Imaging Acquisition:
- Modality: 3 Tesla MRI scanner.
- Structural Imaging: T1-weighted MPRAGE sequence for high-resolution anatomical images.
- Analysis: Volumetric analysis of regions of interest (ROIs: e.g., frontal cortex, insula, hippocampus, cerebellum, subcortical nuclei) and whole-brain cortical thickness measurement.
- Statistical Analysis:
- Primary Analysis: Within-subject longitudinal models to test for changes in brain metrics between T1 and T2.
- Statistical Thresholds: ROI-based analyses may use corrections for multiple comparisons (e.g., Bonferroni). Whole-brain analyses use cluster-wise correction with Monte Carlo simulations (vertex-wise threshold p < 0.05) [133].
- Controls: Comparison with healthy control trajectories to account for normal scan-rescan variability.
Longitudinal Behavioral Trajectory Analysis
This protocol is adapted from studies on functional recovery in first-episode psychosis [135] and disorders of consciousness [137].
- Objective: To identify homogeneous subgroups of patients following distinct functional recovery trajectories over time.
- Participants: Patients assessed at multiple timepoints post-diagnosis or post-injury.
- Design:
- Data Analysis:
- Clustering Method: K-means cluster modeling for longitudinal data (kml3d) or similar algorithms to group individuals based on their pattern of scores over time.
- Trajectory Identification: The analysis outputs distinct clusters (e.g., "Poor," "Intermediate," "Catch-up").
- Predictor Analysis: Regression models are then used to explore potential risk or protective factors (e.g., demographics, clinical history, neurocognitive scores) associated with membership in a particular trajectory group.
Visualizing the Neurocircuitry of Addiction and Recovery
The following diagram illustrates the key brain networks involved in the addiction cycle and their role in recovery trajectories, based on established models [2].
Diagram 1: Addiction Neurocircuitry and Recovery Trajectories. The three-stage addiction cycle is mediated by distinct but overlapping brain circuits. Longitudinal recovery involves structural and functional plasticity within these circuits, with regional specificity and different temporal profiles [133] [2].
This table outlines essential tools and methodologies for conducting research on addiction recovery trajectories.
Table 2: Essential Research Tools for Investigating Recovery Trajectories
| Tool / Resource | Category | Primary Function / Application | Example Use in Research |
|---|---|---|---|
| 3T MRI Scanner | Imaging Hardware | Acquires high-resolution structural, functional, and spectroscopic brain data. | Tracking longitudinal changes in gray matter volume in frontal cortex during abstinence [133]. |
| T1-weighted MPRAGE | Imaging Sequence | Provides high-contrast anatomical images for volumetric and cortical thickness analysis. | Quantifying hippocampal volume changes between 1-day and 2-week abstinence timepoints [133]. |
| Coma Recovery Scale-Revised (CRS-R) | Behavioral Assessment | A standardized behavioral scale to assess consciousness levels in patients with severe brain injury. | Mapping long-term behavioral recovery trajectories in patients with disorders of consciousness every 3 months for 2 years [137]. |
| Global Assessment of Functioning (GAF) Scale | Clinical / Functional Assessment | Provides a single score for overall psychological, social, and occupational functioning. | Identifying distinct "Poor," "Intermediate," "High," and "Catch-up" functional recovery trajectories in first-episode psychosis [135]. |
| K-means Longitudinal Clustering (kml3d) | Data Analysis Algorithm | A data-driven method to identify homogeneous subgroups of individuals following similar longitudinal trajectories. | Classifying patients based on their pattern of functional scores over multiple timepoints without a priori assumptions [135]. |
| DeepLabCut / SLEAP | Behavioral Analysis Software | Machine learning-based tools for markerless pose estimation and behavioral annotation from video data. | Quantifying gait quality and swim kinematics in animal models of spinal cord injury to correlate behavior with neural regeneration [136]. |
Discussion and Synthesis
The evidence confirms that the addicted brain retains a significant capacity for plasticity and recovery. The trajectory of this recovery is characterized by several key principles: it is often partial rather than complete, occurs in a region-specific manner, and follows a temporal sequence where structural changes may precede full functional normalization [133]. This has profound implications for the neurobiology of relapse vulnerability. An individual may be behaviorally abstinent but remain at high relapse risk if critical prefrontal control circuits or subcortical emotional circuits have not yet functionally recovered.
This understanding aligns with clinical models of relapse, which describe it as a gradual process beginning with emotional and mental stages long before drug consumption [138]. The neural dysregulation during early abstinence, particularly in prefrontal and salience networks, directly undermines an individual's capacity for self-care, judgment, and coping, thereby fueling the relapse process [138] [2].
Future research must focus on integrating multi-level data—from molecular and circuit-level neuroimaging to behavioral and social functioning—to build predictive models of individual recovery trajectories. Furthermore, harnessing mechanisms of enhanced plasticity, such as those observed in the adolescent brain's social attunement [139], offers promising avenues for novel interventions. The ultimate goal is to translate this knowledge into targeted therapies that can proactively support neural repair, accelerate functional restoration, and decisively reduce relapse vulnerability.
The transition of relapse-prevention therapies from fundamental neurobiological discovery (bench) to clinical application (bedside) represents a formidable challenge in addiction medicine. Despite advanced understanding of the neurocircuitry and molecular mechanisms underpinning addiction relapse, the development of effective pharmacological interventions has been hampered by the heterogeneous nature of substance use disorders, complexity of relapse triggers, and limitations in translational methodologies. This whitepaper examines the core neurobiological systems governing relapse vulnerability, analyzes key translational barriers, and proposes integrated frameworks and methodologies to accelerate the development of targeted relapse-prevention therapeutics. Emphasis is placed on the allostatic model of addiction, the critical roles of stress and cue reactivity systems, and innovative approaches for deconstructing addiction heterogeneity to enable precision medicine applications.
Drug addiction is a chronic, relapsing disease characterized by a loss of control over drug consumption despite negative consequences [140] [141]. The clinical management of addiction is shadowed by high relapse rates, with more than two-thirds of individuals relapsing within weeks to months of initiating treatment [142]. For 1-year outcomes across alcohol, nicotine, and illicit drug abuse, studies indicate that more than 85% of individuals return to drug use within one year of treatment [142]. This persistent relapse vulnerability underscores the critical need for effective relapse-prevention medications targeting the underlying neurobiology of addiction.
The "bench to bedside" pipeline for relapse-prevention therapies has been hindered by several fundamental challenges. The heterogeneous nature of substance use disorders means that diverse clinical presentations are captured under a single diagnostic category, likely encompassing multiple biologically distinct entities [143]. Furthermore, the development of treatments is complicated by the multifaceted nature of relapse triggers, which include stress, drug-associated cues, and internal states such as negative mood [142]. This whitepaper examines these challenges through the lens of contemporary neurobiological frameworks and proposes integrated strategies for advancing relapse-prevention pharmacotherapies.
Neurobiology of Relapse Vulnerability
Core Neurocircuitry of Addiction and Relapse
Addiction can be conceptualized as a disorder involving progressive dysregulation of brain reward and anti-reward systems [144]. The fundamental model has been expanded to include newer concepts such as motivational circuitry and anti-reward pathways [144]. The mesolimbic pathway, particularly dopaminergic neurons in the ventral tegmental area (VTA) and their targets in the nucleus accumbens (NAc), forms the central hub of the brain's reward system [140] [141].
The progression of drug addiction begins with voluntary drug intake for hedonic effects and progressively consolidates during repeated use, transitioning to habitual and compulsive use in vulnerable individuals [140]. This progression represents a shift from ventromedial to more dorsolateral regions of the striatum and from prefrontal cortex (PFC) to orbitofrontal (OFC) and broader cortical regions [140]. The transition is conceptually defined as a three-stage cycle: (1) consumption/binge/intoxication, (2) withdrawal with negative affect, and (3) craving stage [140]. Different brain regions are implicated in each stage, with the VTA-NAc pathway and dorsal striatum important for the consumption stage, the extended amygdala in the withdrawal stage, and cortical areas, dorsal striatum, hippocampus, and basolateral amygdala in the craving stage [140].
Table 1: Key Brain Regions Implicated in Relapse Vulnerability
| Brain Region | Primary Function in Addiction | Role in Relapse Processes |
|---|---|---|
| Ventral Tegmental Area (VTA) | Origin of dopaminergic projections to reward regions | Acute drug reward; synaptic plasticity induced by drugs |
| Nucleus Accumbens (NAc) | Integration of reward and motivation | Gateway for drug reward; mediator of drug-seeking |
| Prefrontal Cortex (PFC) | Executive function, behavioral control | Compromised inhibitory control; heightened drug-seeking |
| Amygdala | Emotional processing, stress response | Stress-induced relapse; emotional dysregulation |
| Hippocampus | Memory formation, context processing | Contextual cues triggering drug-seeking |
| Dorsal Striatum | Habit formation, stimulus-response learning | Compulsive drug-seeking and habitual behaviors |
Molecular Mechanisms and Synaptic Plasticity
Drugs of abuse induce specific synaptic plasticity in the mesolimbic circuitry. A single injection of an addictive drug can modify excitatory synaptic strength in the VTA, increasing the AMPA/NMDA ratio and exchanging GluA2-containing AMPA receptors for GluA2-lacking ones [140]. Concurrently, NMDA receptor function decreases, causing impairment in eliciting long-term potentiation (LTP) [140]. These drug-induced neuronal modifications represent a usurpation of neuronal processes that normally serve reward-related learning and memory [140].
At the molecular level, maladaptive neuroplastic changes involving CREB, ΔFosB, and BDNF are identified as key drivers of sensitization across both pain and addiction domains [145]. These transcription factors mediate long-term adaptations that contribute to the persistence of addiction phenotypes. Chronic drug exposure leads to epigenetic modifications that stably alter gene expression patterns, potentially explaining the enduring nature of relapse vulnerability even after prolonged abstinence [140].
Theoretical Frameworks for Relapse Vulnerability
Several theoretical models provide frameworks for understanding relapse vulnerability. The allostatic model of addiction explains the intricate balance between positive and negative reinforcement in addiction [143]. This model is informed by the Opponent Process Theory, which contends that over time, addiction becomes less about positive reinforcement and more about negative reinforcement [143] [141]. The neurobiological basis involves a shift from dopamine-dominated reward processing to CRF-mediated stress system activation [143].
The Dopaminergic Hypothesis of Addiction posits that drugs act through a common mechanism of increasing dopamine in the brain's reward system, promoting positive reinforcement and motivating drug consumption [141]. However, this theory has been expanded to incorporate the critical role of glutamatergic systems in relapse, particularly the mediation of cue-induced drug-seeking through projections from prefrontal cortex to nucleus accumbens [140].
Diagram 1: Relapse Triggers and Neurocircuitry. This diagram illustrates the primary triggers of relapse and their convergence on key neurobiological systems.
Key Challenges in Translational Research
Heterogeneity of Addiction Phenotypes
The phenomenological heterogeneity that characterizes substance use disorders has significantly impacted treatment development [143]. The DSM-5 diagnosis of substance use disorder requires any combination of at least two of 11 diagnostic criteria, meaning that studies on substance use disorder often involve patients with different clinical presentations [143]. This heterogeneity likely explains why medications for alcohol use disorder (AUD)—disulfiram, acamprosate, oral naltrexone, and injectable naltrexone—have only modest efficacy, as no single medication works for every patient suffering from this disorder [143].
To address this heterogeneity, the Addictions Neuroclinical Assessment (ANA) was proposed as a clinical framework that captures information in three neurofunctional domains: incentive salience, negative emotionality, and executive (dys)function [143]. These domains have been derived across independent laboratories using a combination of clinical, behavioral, and self-report measures [143]. This framework can be applied across substances, as demonstrated by its application in individuals who use methamphetamine [146].
Biomarker Development and Validation Challenges
The identification of biological markers predicting relapse risk has proven challenging despite promising leads. Several prospective studies have examined whether changes in biological stress responses predict future relapse [142]. In alcoholics, blunted stress- and cue-induced cortisol responses have been associated with poor alcohol relapse outcomes [142]. Similarly, nicotine-deprived smokers showed blunted corticotropin (ACTH), cortisol, and blood pressure responses to stress, which predicted poor nicotine relapse outcomes [142].
The field of metabolomics faces specific technical challenges in biomarker development, particularly ion suppression or enhancement in mass spectrometry-based assays, which can lead to false positives and inaccurate biological interpretations [146]. Additionally, the lack of harmonized workflows in metabolomics has resulted in increased risk of incorrect metabolite annotations and biological interpretations [146].
Table 2: Biological Predictors of Relapse Vulnerability
| Biological System | Measurable Marker | Relapse Prediction | Technical Challenges |
|---|---|---|---|
| HPA Axis | Cortisol reactivity | Blunted response predicts poorer outcomes | State-dependent variability; circadian influences |
| HPA Axis | Cortisol/ACTH ratio | Higher ratio indicates adrenal sensitivity | Requires precise timing of measurements |
| Neurotrophic Factors | Serum BDNF | Lower levels associated with vulnerability | Peripheral vs. central correspondence unclear |
| Autonomic Nervous System | Heart rate variability | Reduced HRV predicts relapse | Confounding by medications, comorbidities |
| Inflammatory System | Cytokine levels (e.g., IL-6, TNF-α) | Elevated levels associated with risk | Multiple confounding factors affect levels |
| Neuroimaging | Anterior cingulate activity | Hyperreactivity during withdrawal predicts relapse | Cost and accessibility limitations |
Complexity of Relapse Triggers and Temporal Dynamics
Relapse is a complex phenomenon influenced by multiple triggers including stress, drug-related cues, negative mood, and internal states [142]. Research has demonstrated that acute stress exposure in the laboratory increases drug craving and anxiety in individuals dependent on opiates, alcohol, nicotine, cocaine, and marijuana [142]. The temporal dynamics of relapse follow a characteristic pattern, with survival analyses demonstrating that a log-logistic distribution most accurately reflects the relapse curve, which is uniform across drug classes and populations [106].
The allostatic model provides a framework for understanding how chronic deviation of brain reward set points leads to a state where individuals use drugs primarily to alleviate withdrawal and associated unpleasant affective and physical symptoms [143]. This shift from positive to negative reinforcement explains what patients describe as using drugs to feel "normal" rather than to get high [143].
Experimental Models and Methodologies
Preclinical Models of Relapse Vulnerability
Preclinical research has developed sophisticated models to study relapse mechanisms, primarily using reinstatement procedures in rodents. These models demonstrate that different triggers—drug primes, stress, or drug-associated cues—engage partially distinct neurocircuitry, requiring tailored pharmacological approaches.
Synaptic plasticity measurements in rodent brain slices have revealed how drugs of abuse alter excitatory synaptic strength in the mesolimbic circuitry. Key findings include increased AMPA/NMDA ratio in VTA dopamine neurons after a single dose of cocaine and exchange of GluA2-containing AMPA receptors for GluA2-lacking ones [140]. These measurements typically involve whole-cell patch-clamp recordings from VTA neurons in acute brain slices, comparing AMPA and NMDA receptor-mediated currents.
Optogenetic and chemogenetic approaches now enable precise manipulation of specific neural circuits to establish causal relationships between circuit activity and relapse behaviors. These tools allow researchers to mimic or inhibit activity in projections from specific regions, such as prefrontal cortex to nucleus accumbens, during relapse tests.
Human Laboratory Models of Relapse Risk
Human laboratory studies provide a controlled environment to examine provoked relapse risk using stress, drug cue, or drug priming methodologies. Standardized protocols include:
- Guided Imagery Stress and Cue Exposure: Participants develop personalized scripts for stress and drug cue scenarios, with neutral scenarios as controls [142]. During sessions, subjective craving, anxiety, cardiovascular measures, and HPA axis markers (cortisol, ACTH) are collected.
- Trier Social Stress Test: This standardized psychosocial stressor involves public speaking and mental arithmetic tasks before an audience, reliably activating stress systems and measuring subsequent effects on drug craving [142].
- Pharmacological Challenge Tests: Administration of compounds like corticotropin-releasing factor (CRF) or yohimbine (an alpha-2 adrenergic antagonist) to probe specific stress systems and their effects on craving and physiological responses [142].
These laboratory paradigms demonstrate predictive validity, as stress-induced and cue-induced craving and physiological responses predict subsequent time to relapse and drug use outcomes [142].
Clinical Trial Design for Relapse Prevention
Pharmacotherapy trials for relapse prevention face unique methodological challenges. Traditional abstinence-based endpoints may not capture reductions in drug use that are clinically meaningful. Alternative endpoints include:
- Time to relapse: Analyzing time to first use or time to relapse using survival analyses [106].
- Percentage of abstinent days: Capturing reductions in use frequency rather than complete abstinence.
- Biomarker-informed stratification: Enriching trials with participants showing specific biological characteristics (e.g., HPA axis dysregulation) that might predict responsiveness to the tested medication.
The Addictions Neuroclinical Assessment (ANA) framework can be leveraged to advance precision medicine for alcohol use disorder using pharmacological treatments by stratifying patients based on their dominant neurofunctional domains (incentive salience, negative emotionality, executive function) [143].
Diagram 2: Precision Medicine Framework. The ANA approach to matching biomarkers and targeted therapies.
Research Toolkit: Key Reagents and Methodologies
Table 3: Essential Research Reagents and Platforms for Relapse Mechanism Studies
| Reagent/Platform | Function/Application | Key Considerations |
|---|---|---|
| GABAB receptor agonists (e.g., baclofen) | Reduces cocaine craving and use; acts via VTA dopamine neuron GABAB receptors [140] | Sedation side effects; precise receptor targeting needed |
| Dopamine receptor ligands (D1/D2/D3 selective) | Probing dopamine system involvement in reward and relapse | Receptor subtype specificity; blood-brain barrier penetration |
| CRF receptor antagonists | Targeting stress-induced relapse via CRF systems in extended amygdala | Differential effects in dependent vs. non-dependent states |
| AMPA/NMDA receptor modulators | Investigating synaptic plasticity in addiction models | Region-specific effects; balance between efficacy and toxicity |
| Chemogenetic tools (DREADDs) | Remote control of specific neural circuits in relapse models | Temporal precision; potential compensatory mechanisms |
| Optogenetic constructs | Millisecond-timescale control of specific neural projections | Fiber placement limitations; translation to humans |
| Metabolomics platforms | Identifying metabolic signatures of relapse vulnerability | Standardization challenges; ion suppression effects [146] |
| Synthetic cell mimics | Controls for biomarker assays; improve standardization [147] | Reproducibility across experiments and laboratories |
Integrated Approaches for Relapse Prevention
Advancing relapse-prevention medications requires integrated approaches that address the multifactorial nature of relapse vulnerability. Promising strategies include:
- Dual-target pharmacotherapies that address both reward and stress systems, particularly for comorbidities such as chronic pain and substance use disorders where shared neurobiological mechanisms exist [145].
- Pharmacogenomics to identify genetic predictors of treatment response, moving beyond diagnostic categories to target underlying biological mechanisms [143].
- Neuroimaging-based stratification using techniques that identify individuals with specific neural circuit dysfunctions (e.g., prefrontal hypoactivity) who might benefit from targeted interventions.
The translation of relapse-prevention therapies from bench to bedside remains challenging due to the complex neuroadaptations underlying addiction persistence, the heterogeneous nature of substance use disorders, and limitations in current biomarker development and validation. However, new frameworks such as the Addictions Neuroclinical Assessment [143] and improved translational models offer promising pathways forward. By deconstructing addiction heterogeneity and targeting specific neurofunctional domains, the field can advance toward personalized medicine approaches for relapse prevention. Success will require coordinated efforts across basic and clinical research, innovative clinical trial designs, and the development of validated biomarkers that can guide treatment selection and monitor response.
Conclusion
The neurobiology of addiction relapse vulnerability is characterized by persistent dysregulation across interconnected brain circuits governing reward, stress, and executive control. Foundational research confirms that lasting neuroadaptations—from dopaminergic signaling deficits to microglia-mediated synaptic pruning—create a biological substrate for relapse. Methodological advances have yielded promising biomarkers, including neural cue-reactivity and HPA axis measures, for stratifying relapse risk. Troubleshooting relapse requires personalized approaches that target specific neurobiological dysfunctions, such as neuroimmune activation or stress system hyperactivity. Finally, validating these models and comparing new targets, from GLP-1 agonists to immunotherapies, is the critical next step. Future research must prioritize longitudinal studies and randomized controlled trials to translate these mechanistic insights into clinically effective, biomarker-informed relapse prevention strategies, ultimately transforming the treatment landscape for substance use disorders.
References
- 1. Neurocircuitry of Addiction - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2805560/]
- 2. Neurocircuitry of Addiction | Neuropsychopharmacology [https://www.nature.com/articles/npp2009110]
- 3. Neurobiology of Addiction - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK597351/]
- 4. THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ... [https://www.ncbi.nlm.nih.gov/books/NBK424849/]
- 5. of Neurobiology : a neurocircuitry analysis - PMC addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC6135092/]
- 6. Understanding the 3-Stage Model of Addiction [https://www.wecaremoreohio.com/blog/3-stage-addiction-model]
- 7. of Neurobiology , | PPT addiction [https://www.slideshare.net/slideshow/neurobiology-of-addiction-12196879/12196879?nway-refresh=B]
- 8. Abnormal regional brain activity associated with relapse in ... [https://www.nature.com/articles/s41598-025-11438-4]
- 9. and other neurotransmitters in Dopamine | Fiveable addiction [https://fiveable.me/physiology-motivated-behaviors/unit-9/dopamine-neurotransmitters-addiction/study-guide/Jpg9UIEZtDZLK8y3]
- 10. in the Brain: Hypothesizing Surfeit or Deficit Links to... Dopamine [https://pubmed.ncbi.nlm.nih.gov/27398406/]
- 11. Neurobiological intersections of stress and substance use ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1548372/full]
- 12. emotional dysregulation is a critical driver of relapse to ... [https://www.nature.com/articles/s41398-024-03159-5]
- 13. Mesolimbic dopamine adapts the rate of learning from action [https://www.nature.com/articles/s41586-022-05614-z]
- 14. Neurotransmitters' white matter mapping unveils the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910582/]
- 15. A probabilistic model of relapse in drug addiction [https://www.sciencedirect.com/science/article/pii/S0025556424000440]
- 16. Dynamics of Neuronal Circuits in Addiction - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2739305/]
- 17. Introduction: Addiction and Brain Reward and Anti-Reward ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4549070/]
- 18. Neuroanatomy, Amygdala - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK537102/]
- 19. The neurobiology of addiction. A vulnerability/resilience ... [https://www.elsevier.es/es-revista-european-journal-psychiatry-431-articulo-the-neurobiology-addiction-a-vulnerability-resilience-S0213616317300800]
- 20. The influence of stress and social defeat on ... [https://link.springer.com/article/10.1007/s00213-025-06852-5]
- 21. An extended amygdala-midbrain circuit controlling cocaine ... [https://www.sciencedirect.com/science/article/pii/S2211124722005393]
- 22. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3462342/]
- 23. The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex | Neuropsychopharmacology [https://www.nature.com/articles/s41386-021-01153-9]
- 24. The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8617203/]
- 25. Prefrontal Cortex and Drug Abuse Vulnerability - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3005953/]
- 26. Neurobiology of addiction | Addiction Conferences 2025 [https://addiction-behavioral-conferences.magnusgroup.org/program/scientific-program/2025/neurobiology-of-addiction]
- 27. The neurobiology of substance use and addiction [https://www.cambridge.org/core/journals/bjpsych-advances/article/neurobiology-of-substance-use-and-addiction-evidence-from-neuroimaging-and-relevance-to-treatment/81D3A088F077F86689C03F63A8798AE7]
- 28. Neuroimmune Mechanisms as Novel Treatment Targets for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8082184/]
- 29. Interactions of neuroimmune signaling and glutamate ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-021-02072-8]
- 30. How the brain's immune system drives drug relapse (and a ... [https://college.unc.edu/2025/09/microglia-cocaine-addiction/]
- 31. Neuroimmune Mechanisms as Novel Treatment Targets for ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.650785/full]
- 32. Glial and Neuroimmune Mechanisms as Critical ... [https://www.nature.com/articles/npp2016121]
- 33. Neuroimmune Mechanisms of Alcohol and Drug Addiction [https://www.sciencedirect.com/science/article/abs/pii/B9780128012840000014]
- 34. Devolving views of their roles in drug addiction [https://www.sciencedirect.com/science/article/pii/S0149763413000468]
- 35. devolving views of their roles in drug addiction [https://pubmed.ncbi.nlm.nih.gov/23438892/]
- 36. Dorsal Striatal Circuits for Habits, Compulsions and ... [https://www.frontiersin.org/journals/systems-neuroscience/articles/10.3389/fnsys.2019.00028/full]
- 37. The ins and outs of the striatum: Role in drug addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4523218/]
- 38. Frontiers | Striatal Signal Transduction and Drug Addiction [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2011.00060/full]
- 39. Psychological and neural mechanisms of relapse - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2607321/]
- 40. Craving Prediction From fMRI Drug Cue Reactivity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537833/]
- 41. Neuroimaging and Biomarkers in Addiction Treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4427893/]
- 42. Differences in fMRI-based connectivity during abstinence ... [https://www.sciencedirect.com/science/article/pii/S0149763425001162]
- 43. Integrating EEG biomarkers in the neurocognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11446767/]
- 44. Biomarkers and neuromodulation techniques in substance ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-020-0040-0]
- 45. Central and Peripheral Biomarkers of Stress Response for ... [https://www.sciencedirect.com/science/article/abs/pii/S1471491417302344]
- 46. Central and Peripheral Biomarkers of Stress Response for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6511993/]
- 47. Cortisol secretion patterns in addiction and addiction risk - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2257874/]
- 48. Brain-derived neurotrophic factor and addiction: Pathological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4425618/]
- 49. Changes in brain-derived neurotrophic factor (BDNF) ... [https://www.sciencedirect.com/science/article/abs/pii/S0165178114010129]
- 50. The Brain Stress System in the Neurobiology of the “Dark ... [https://www.intechopen.com/chapters/72714]
- 51. adverse effects of stress on drug addiction [https://www.jci.org/articles/view/33946]
- 52. Factors modulating neural reactivity to drug cues in addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC3913480/]
- 53. Cue Reactivity Paradigm - an overview [https://www.sciencedirect.com/topics/psychology/cue-reactivity-paradigm]
- 54. The natverse, a versatile toolbox for combining and ... [https://elifesciences.org/articles/53350]
- 55. A data-driven framework for mapping domains of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8761068/]
- 56. Deep brain stimulation of the anterior cingulate cortex ... [https://www.nature.com/articles/s41598-025-86279-2]
- 57. Structural MRI correlates of apathy symptoms in older ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4013817/]
- 58. Brain structural correlates of an impending initial major ... [https://www.nature.com/articles/s41386-025-02075-6]
- 59. The Brain in Recovery [https://www.recoveryanswers.org/recovery-101/brain-in-recovery/]
- 60. Impulsivity Predicts Relapse—but Not Dropout—in ... [https://link.springer.com/article/10.1007/s11469-023-01024-y]
- 61. Impulsivity, Compulsivity, and Top-Down Cognitive Control [https://www.sciencedirect.com/science/article/pii/S0896627311000687]
- 62. Impulsivity, Neural Deficits, and the Addictions: The “Oops” ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4321793/]
- 63. Relationships between trait impulsivity and cognitive control [https://pubmed.ncbi.nlm.nih.gov/26245649/]
- 64. toward a comprehensive neural account of future-oriented ... [https://www.sciencedirect.com/science/article/pii/S0149763425001150]
- 65. Experts highlight science-driven approaches to addiction [https://news.vt.edu/articles/2025/09/fralinbiomed-national-recovery-month-addiction-experts.html]
- 66. Charting the brain networks of impulsivity: Meta-analytic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290857/]
- 67. Addictions Neuroclinical Assessment: A reverse ... [https://www.sciencedirect.com/science/article/abs/pii/S0028390817300898]
- 68. Addictions Neuroclinical Assessment: A Reverse Translational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5569299/]
- 69. Addictions Neuroclinical Assessment: A Neuroscience- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4870153/]
- 70. Commentary: Addictions Neuroclinical Assessment [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2017.00002/full]
- 71. Factors underlying the neurofunctional domains of ... [https://www.nature.com/articles/s41398-024-02987-9]
- 72. Neural correlates of the addictions neuroclinical ... [https://www.sciencedirect.com/science/article/pii/S0166432824000822]
- 73. The Addictions Neuroclinical Assessment Negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7069798/]
- 74. "Validation of the Addictions Neuroclinical Assessment ... [https://digitalrepository.unm.edu/psy_etds/406/]
- 75. Substance Use Disorder Treatment Outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180564/]
- 76. Predictors of treatment attrition among individuals in ... [https://www.sciencedirect.com/science/article/abs/pii/S0306460325000206]
- 77. Tools for visualization and analysis of molecular networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4461095/]
- 78. Home - Reactome Pathway Database [https://reactome.org/]
- 79. 1 Data visualization - R for Data Science (2e) - Hadley Wickham [https://r4ds.hadley.nz/data-visualize.html]
- 80. Role of Microglia in Psychostimulant Addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10190137/]
- 81. A potential role for microglia in stress- and drug-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6924541/]
- 82. Microglia in neurodegenerative diseases: mechanism and ... [https://www.nature.com/articles/s41392-023-01588-0]
- 83. Frontiers | Microglia and Drug-Induced Plasticity in ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2012.00074/full]
- 84. Inhibition of CSF1R, a receptor involved in microglia ... [https://www.nature.com/articles/s41598-021-95059-7]
- 85. Microglia as therapeutic targets for central nervous system ... [https://www.sciencedirect.com/science/article/pii/S1471489222000121]
- 86. Why our brains are wired for addiction: What the science says [https://med.stanford.edu/news/insights/2025/08/addiction-science-human-brain-ancient-wiring.html]
- 87. Neuroscience: The Brain in Addiction and Recovery [https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/neuroscience-brain-addiction-and-recovery]
- 88. Structural and functional brain recovery in individuals with ... [https://www.sciencedirect.com/science/article/abs/pii/S0376871622000564]
- 89. The Neurobiology of Successful Abstinence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3706547/]
- 90. Neurobehavioural Mechanisms of Resilience and ... [https://www.frontiersin.org/research-topics/9375/neurobehavioural-mechanisms-of-resilience-and-vulnerability-in-addictive-disorders/magazine]
- 91. Addiction Relapse Prevention - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK551500/]
- 92. Stress-Induced Reinstatement of Drug Seeking: 20 Years of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4677117/]
- 93. Stress and substance use disorders: risk, relapse, and ... [https://www.jci.org/articles/view/172883]
- 94. Cross-talk between the HPA axis and addiction-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10161713/]
- 95. The Role of Stress in Alcohol Use, Alcoholism Treatment, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6760383/]
- 96. Drug-induced stress responses and addiction risk ... [https://www.sciencedirect.com/science/article/pii/S2352289518300754]
- 97. Efficacy of Treatments Targeting Hypothalamic-Pituitary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8461240/]
- 98. HPA axis response to psychological stress and treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3774292/]
- 99. Neurocognitive impairment in addiction: A digital tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9579426/]
- 100. Cognitive rehabilitation in addictive disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5844160/]
- 101. Cognitive Remediation for Impulsivity in Addictive Disorders [https://link.springer.com/article/10.1007/s40429-023-00504-4]
- 102. Cognitive training interventions for substance use disorders [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1388935/full]
- 103. The factors affecting substance abuse relapse based on theory of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11080208/]
- 104. The Theory of Planned - A Level Psychology Revision Behaviour [https://www.savemyexams.com/a-level/psychology/aqa/17/revision-notes/17-addiction-a-level-only/17-6-applying-models-of-behaviour-change/17-6-1-the-theory-of-planned-behaviour/]
- 105. A quantitative review of the ubiquitous relapse curve - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3151675/]
- 106. A quantitative review of the ubiquitous relapse curve [https://www.sciencedirect.com/science/article/abs/pii/S0740547208000573]
- 107. comparing validated measures of intention and assessing the ... [https://implementationsciencecomms.biomedcentral.com/articles/10.1186/s43058-020-00050-4]
- 108. Neurobiology of craving, conditioned reward and relapse [https://www.sciencedirect.com/science/article/abs/pii/S147148920400205X]
- 109. Precision medicine in substance use disorders [https://pubmed.ncbi.nlm.nih.gov/40752782/]
- 110. Discovery and validation of biomarkers to aid the ... [https://www.nature.com/articles/s41582-020-0362-2]
- 111. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 112. Biomarkers of Relapse in Cocaine Use Disorder: A Narrative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405750/]
- 113. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 114. Structural Imaging-Based Biomarkers for Detecting Craving ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2020.599099/full]
- 115. The Value of Biomarkers in Clinical Trials. [https://medicover-mics.com/value-of-biomarkers-in-clinical-trials/]
- 116. Comparing neuromodulation targets to reduce cigarette ... [https://www.nature.com/articles/s41386-025-02106-2]
- 117. A systematic review and meta-analysis of neuromodulation ... [https://www.nature.com/articles/s41386-023-01776-0]
- 118. Pharmacotherapy – Medications [https://www.recoveryanswers.org/resource/pharmacotherapy-medication-assisted-treatments/]
- 119. Neuromodulation for Treating Substance Use Disorders [https://www.addictionpolicy.org/post/neuromodulation-for-treating-substance-use-disorders]
- 120. Comparing neuromodulation targets to reduce cigarette ... [https://www.medrxiv.org/content/10.1101/2024.10.10.24315204v1.full-text]
- 121. Neuromodulation for Substance Addiction in Human Subjects [https://pmc.ncbi.nlm.nih.gov/articles/PMC7405948/]
- 122. Mechanisms of GLP-1 in Modulating Craving and Addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372146/]
- 123. of craving, conditioned reward and Neurobiology relapse [https://pubmed.ncbi.nlm.nih.gov/15661620/]
- 124. GLP-1s show promise in treating alcohol and drug addiction [https://www.endocrine.org/news-and-advocacy/news-room/2025/glp1s-show-promise-in-treating-alcohol-and-drug-addiction]
- 125. Glucagon-like peptide-1 (GLP-1) and substance use ... [https://www.sciencedirect.com/science/article/pii/S1043661824002573]
- 126. A turning point in addiction psychiatry? [https://sph.brown.edu/news/2025-07-24/brain-science-glp-1s-addiction]
- 127. Neurokinin receptors in drug and alcohol addiction [https://www.sciencedirect.com/science/article/abs/pii/S0006899320300858]
- 128. Stress-induced reinstatement of alcohol-seeking in rats is ... [https://pubmed.ncbi.nlm.nih.gov/21340476/]
- 129. Why is Neuroimmunopharmacology crucial for the future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3858520/]
- 130. Neuroimmune Mechanisms of Alcohol and Drug Addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC4804710/]
- 131. Dimensional Approaches to Understanding Addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6233300/]
- 132. Advancing reduction of drug use as an endpoint in addiction ... [https://nida.nih.gov/about-nida/noras-blog/2025/03/advancing-reduction-drug-use-endpoint-in-addiction-treatment-trials]
- 133. Structural and Functional Brain Recovery in Individuals with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8885813/]
- 134. The neuroplastic brain: current breakthroughs and ... [https://www.sciencedirect.com/science/article/pii/S0006899325002021]
- 135. Longitudinal trajectory of early functional recovery in patients ... [https://pubmed.ncbi.nlm.nih.gov/30826261/]
- 136. Functional trajectories during innate spinal cord repair [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2023.1155754/full]
- 137. Longitudinal assessments highlight long-term behavioural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6924536/]
- 138. Relapse Prevention and the Five Rules of Recovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4553654/]
- 139. Adolescent resilience to addiction: a social plasticity hypothesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC6373770/]
- 140. Drug addiction: from bench to bedside [https://www.nature.com/articles/s41398-021-01542-0]
- 141. Neurobiological Theories of Addiction: A Comprehensive ... [https://www.mdpi.com/2813-1851/3/1/3]
- 142. New Findings on Biological Factors Predicting Addiction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3674771/]
- 143. Translational Models of Addiction Phenotypes to Advance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823887/]
- 144. From the Science to the Practice of Addiction Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4781796/]
- 145. Neurobiological convergence of pain and substance use ... [https://www.sciencedirect.com/science/article/pii/S2772392525000264]
- 146. Challenges in Translating Clinical Metabolomics Data Sets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8720260/]
- 147. Biomarkers from Bench to Bedside: Tools, Targets, and ... [https://insidescientific.com/webinar/biomarkers-from-bench-to-bedside-tools-targets-and-translational-insights/]