Modeling Compulsive Drug Seeking: Advanced Animal Models for Addiction Research and Therapeutic Development
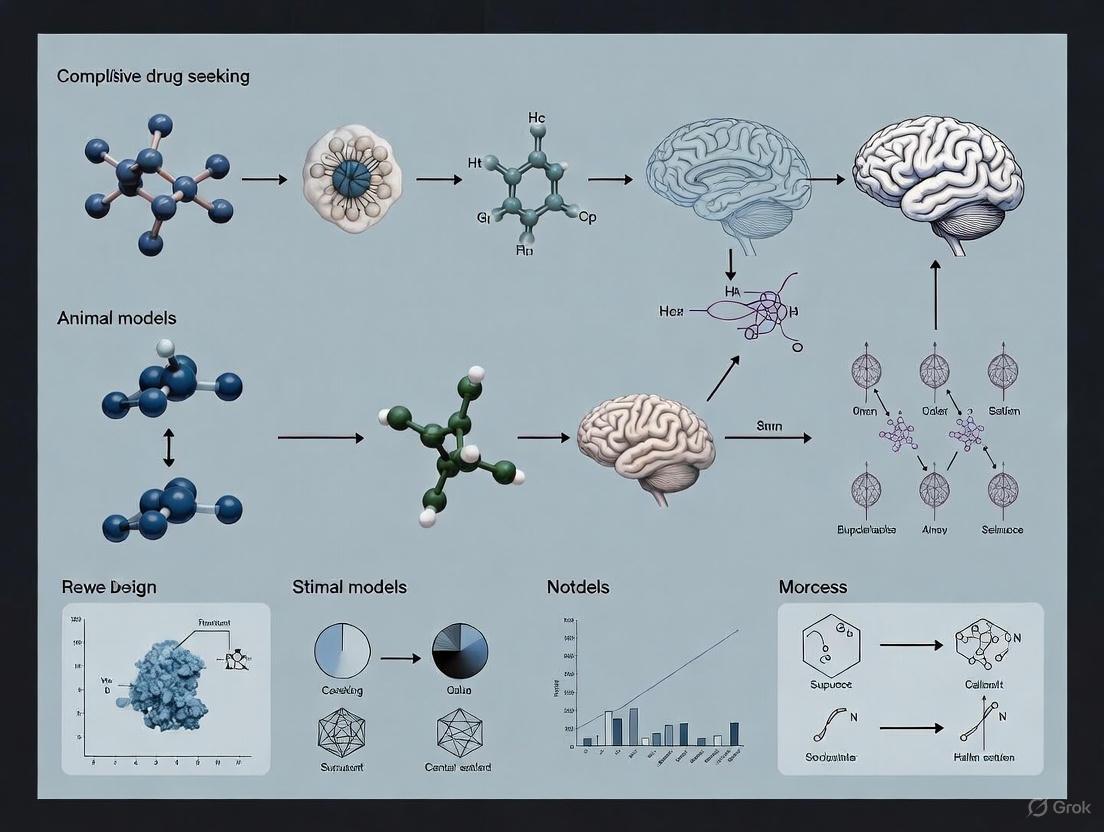
This comprehensive review explores the evolution, application, and validation of animal models for studying compulsive drug-seeking behavior—a core feature of substance use disorders.
Modeling Compulsive Drug Seeking: Advanced Animal Models for Addiction Research and Therapeutic Development
Abstract
This comprehensive review explores the evolution, application, and validation of animal models for studying compulsive drug-seeking behavior—a core feature of substance use disorders. We examine foundational theories and neurocircuitry, detail established and emerging methodological approaches including self-administration paradigms with adverse consequences, and critically address conceptual challenges and optimization strategies. By integrating multidimensional validation frameworks and discussing translational gaps, this article provides researchers and drug development professionals with a sophisticated understanding of how preclinical models are advancing to better capture the complexity of human addiction, thereby enhancing the discovery of novel therapeutic interventions.
The Theoretical Basis of Compulsivity: From Brain Circuits to Behavioral Constructs
Frequently Asked Questions (FAQs)
Q1: How does the DSM-5 define a Substance Use Disorder, and what is the role of "compulsivity"? The DSM-5 defines a Substance Use Disorder (SUD) as a problematic pattern of use leading to clinically significant impairment, as manifested by at least 2 out of 11 criteria within a 12-month period [1]. The criteria cover four main areas: impaired control, social impairment, risky use, and pharmacological criteria (tolerance and withdrawal) [2] [1].
While the term "compulsive" is commonly used in definitions of addiction (e.g., by NIDA), it is not explicitly listed as a standalone criterion in the DSM-5 [3]. Instead, the concept is operationally captured by criteria such as:
- "There is a persistent desire or unsuccessful efforts to cut down or control substance use."
- "The substance is often taken in larger amounts or over a longer period than was intended."
- "Important social, occupational, or recreational activities are given up or reduced because of substance use."
- "Continued substance use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance." [1]
Q2: What are the key differences between DSM-IV and DSM-5 criteria for Substance Use Disorders? The DSM-5 introduced major revisions to overcome limitations identified in the DSM-IV. The key changes are summarized below [2] [1]:
Table: Key Differences Between DSM-IV and DSM-5 Substance Use Disorder Criteria
| Feature | DSM-IV | DSM-5 |
|---|---|---|
| Diagnostic Categories | Two distinct disorders: Abuse and Dependence | A single, unified Substance Use Disorder |
| Diagnostic Threshold | Abuse: 1+ of 4 criteria. Dependence: 3+ of 7 criteria. | Mild: 2-3 criteria, Moderate: 4-5 criteria, Severe: 6+ criteria |
| Specific Criteria | Included "recurrent substance-related legal problems" | Removed "legal problems" and added "craving, or a strong desire or urge to use the substance" |
| Remission Specifiers | Early remission: 1-12 months without criteria (except tolerance/withdrawal) | Early remission: 3-12 months without criteria (craving may be present). Sustained remission: 12+ months without criteria (craving may be present). |
Q3: How is compulsive drug seeking operationalized in preclinical animal models? In preclinical research, "compulsivity" is primarily inferred from behaviors that persist despite adverse consequences, as animals cannot self-report feelings of compulsion. The main operationalizations are [4] [3]:
- Punishment-Based Models: Measuring the persistence of drug self-administration or seeking when the action is paired with an aversive outcome, such as a mild footshock or a bitter-tasting quinine adulterant [4] [3].
- Conflict-Based Models: Assessing the propensity to resume drug seeking after a period of abstinence enforced by the introduction of an adverse consequence (e.g., an electrified barrier near the drug lever) [4].
It is critical to note that these models are a subject of debate. A behavior observed under these conditions should be precisely described as "persistent responding despite adverse consequences," as multiple alternative explanations (e.g., reduced pain sensitivity, learning deficits) can account for the results without implying a human-like experience of "compulsion" [3].
Q4: What are common pitfalls when interpreting "compulsive-like" behavior in animals, and how can I avoid them? A primary pitfall is equating persistent drug use despite punishment directly with the clinical concept of compulsivity. Several factors must be controlled for to strengthen your conclusions [3]:
- Altered Sensitivity: Animals may be less sensitive to the punishing stimulus (e.g., footshock) at baseline or due to drug effects.
- Learned Resistance: Animals may acquire a learned resistance to the behavior-suppressing effects of punishment over time.
- Contingency Learning Deficits: The behavior may persist because the animal has not properly learned the association between its action and the punishment.
Troubleshooting Guide: How to control for alternative explanations in punishment models Table: Controls for Punishment-Based Models of Compulsive-like Behavior
| Problem Symptom | Possible Root Cause | Resolution Steps & Controls |
|---|---|---|
| High resistance to punishment in a subset of animals. | Innately reduced sensitivity to the aversive stimulus (e.g., footshock, quinine). | 1. Test baseline sensitivity: Conduct separate experiments to assess innate nociceptive thresholds or taste aversion in all animals before or after the main experiment.2. Use an alternative aversive stimulus: If an effect is found with one punisher (e.g., shock), confirm it with another type (e.g., quinine adulteration of an oral drug). |
| All animals show a gradual increase in punished responding over sessions. | Learned resistance to the punishing stimulus. | Include a control group: Test a separate group of animals that receive the same punishment contingency but for a non-drug reinforcer (e.g., sucrose). This determines if the resistance is specific to the drug reward. |
| An animal does not suppress responding even when punishment intensity is high. | Failure to learn the instrumental punishment contingency. | Verify contingency learning: Implement probe sessions where the punishment contingency is briefly omitted or signaled differently to test if the animal's behavior flexibly changes, indicating intact learning. |
| A treatment reduces punished drug-seeking. | The treatment generally reduces motivation or motor activity, rather than specifically affecting compulsion. | Test for specificity: Run a parallel experiment to confirm the treatment does not affect responding for a natural reward (e.g., food) under the same punishment schedule. |
Experimental Protocols for Modeling Compulsivity
Protocol 1: Punishment-Induced Suppression of Drug Seeking
Objective: To assess the persistence of drug-seeking behavior in the face of explicit adverse consequences [4] [3].
Methodology:
- Train Stable Self-Administration: Rats are trained to self-administer a drug (e.g., cocaine, alcohol) on a fixed-ratio schedule until stable baseline intake is established.
- Introduce Punishment Contingency: In subsequent sessions, a portion (e.g., 30-50%) of the drug-reinforced responses are concurrently paired with a mild, unpredictable footshock (e.g., 0.2-0.5 mA, 0.5 sec duration) through the grid floor.
- Measure and Classify: Animals are classified based on their response suppression. "Compulsive-like" or "Punishment-Resistant" animals are typically defined as those maintaining a high rate of drug intake (e.g., >80% of baseline) despite the punishment, compared to "Punishment-Sensitive" animals that significantly suppress their intake [4].
Protocol 2: Conflict-Based Relapse After Self-Abstinence
Objective: To model relapse to drug seeking after a period of voluntary abstinence driven by adverse consequences [4].
Methodology:
- Self-Administration Training: As in Protocol 1.
- Induce Self-Abstinence: Introduce an "electric barrier" or consistent punishment that makes the cost of drug-seeking prohibitively high. The animal is allowed to choose not to respond.
- Define Abstinence Criterion: Animals that cease lever-pressing for the drug for a set number of consecutive days (e.g., 3 days) are considered to have achieved self-abstinence.
- Probe for Relapse: In a subsequent session where the punishment is temporarily removed, the animal is exposed to drug-paired cues, a drug prime (small non-contingent infusion), or stress. The resumption of drug-seeking behavior is measured as "relapse." [4]
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents for Preclinical Models of Compulsive Drug Seeking
| Item | Function & Application |
|---|---|
| Operant Conditioning Chamber | Sound-attenuated box with levers, cue lights, and a drug infusion system. The core apparatus for drug self-administration studies. |
| Programmable Footshock Generator | Delivers precise, scrambled mild electric shocks to the chamber grid floor to serve as the adverse consequence in punishment models. |
| Intravenous Catheter & Swivel System | Allows for chronic, intravenous drug self-administration in freely moving rodents. |
| Quinine Hydrochloride | A bitter tastant used to adulterate oral drug solutions (e.g., alcohol) to create an aversive consequence. |
| Microdialysis/Licrodialysis System | For in vivo sampling of neurotransmitters (e.g., glutamate, dopamine) from specific brain regions during compulsive-like behavior. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) or Chemogenetics Kit | Tools for selectively activating or inhibiting specific neural circuits to establish causal links with behavior. |
| c-Fos or pERK Antibodies | Immunohistochemical markers for mapping neuronal activation in brain tissue following behavioral tests. |
| Schedule-Controlled Contingency Software | Software (e.g., Med-PC) to program complex reinforcement schedules and precisely control experimental sessions. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the functional organization of the corticostriatal pathway in the context of goal-directed behaviors? The corticostriatal pathway is the primary input channel to the basal ganglia and is topographically organized. It integrates information across reward, cognitive, and motor functions to orchestrate goal-directed behaviors [5]. The striatum is divided into functional territories: the ventral striatum (reward), the caudate nucleus (cognition), and the putamen (motor control). These regions are part of a larger cortico-basal ganglia-thalamo-cortical loop, where the cortex projects to the striatum, which then projects through the pallidal complex and substantia nigra to the thalamus, and back to the cortex [5].
FAQ 2: How do dopamine and glutamate interact synaptically in the striatum to influence behavior? Dopamine and glutamate interact at the level of the striatal medium spiny neurons (MSNs) to modulate synaptic plasticity, including the induction of long-term depression (LTD) and long-term potentiation (LTP) [6]. This interaction is critical for reward-related learning and the fine-tuning of behavioral repertoire. Dopaminergic input from the substantia nigra pars compacta (SNc) and ventral tegmental area (VTA) terminals converges with glutamatergic inputs from the cortex and thalamus onto the spines and dendritic shafts of MSNs, allowing dopamine to regulate the strength of cortical signals [5] [6].
FAQ 3: What neurochemical imbalances are observed in the frontal cortex in compulsive disorders? In individuals with Obsessive-Compulsive Disorder (OCD), a disorder characterized by compulsive behavior, elevated glutamate levels and a disrupted balance between glutamate and GABA (gamma-aminobutyric acid) are observed in the anterior cingulate cortex (ACC). Specifically, studies using 7-Tesla magnetic resonance spectroscopy (MRS) show that OCD participants have significantly higher Glu:GABA ratios in the ACC compared to healthy volunteers. Furthermore, in the supplementary motor area (SMA), glutamate levels positively correlate with clinical measures of compulsive behavior [7].
FAQ 4: How do drugs of abuse alter the dopamine system to contribute to addiction? Drugs of abuse induce large and fast increases in extracellular dopamine in the striatum, particularly in the ventral striatum/nucleus accumbens, which is associated with their reinforcing effects (the "high") [8] [9]. In individuals with addiction, chronic drug use leads to decreases in dopamine D2 receptors and reduced dopamine release in the striatum. This hypodopaminergic state is linked to reduced activity in prefrontal regions (orbitofrontal cortex, cingulate gyrus, dorsolateral prefrontal cortex), underlying symptoms like loss of inhibitory control and compulsive drug intake [8].
Troubleshooting Guide: Common Experimental Challenges
Behavioral Modeling
Table: Addressing Challenges in Modeling Compulsive Drug Seeking
| Challenge | Potential Cause | Solution |
|---|---|---|
| High behavioral variability in animal models | Individual differences in transition from controlled to compulsive use. | Use progressive ratio schedules or long-access self-administration protocols to model escalation. Select subjects based on behavioral cut-offs (e.g., high vs. low compulsive responders) [9] [10]. |
| Difficulty distinguishing goal-directed from habitual actions | Over-reliance on a single behavioral test; lack of specific molecular markers. | Implement outcome devaluation and contingency degradation protocols [10]. Use circuit-specific monitoring (e.g., fiber photometry in DMS vs DLS) to confirm a shift from mesostriatal to nigrostriatal dopamine dependency [10]. |
Neurochemical and Circuit Interrogation
Table: Addressing Challenges in Neurochemical and Circuit Analysis
| Challenge | Potential Cause | Solution |
|---|---|---|
| Measuring subtle neurotransmitter changes in vivo | Low sensitivity of techniques; confounding signals from metabolites. | Use high-field MRS (7-Tesla) with optimized sequences (e.g., semi-LASER) to reliably separate glutamate, glutamine, and GABA [7]. Control for neuronal integrity by co-measuring N-acetylaspartate (NAA) [7]. |
| Achieving pathway-specific manipulation | Off-target effects from traditional pharmacological or lesion approaches. | Employ cell-type-specific cre-lox systems and projection-targeted optogenetics/chemogenetics (DREADDs) to selectively manipulate dSPNs vs iSPNs, or VTA vs SNc dopamine neurons [11] [10]. |
Detailed Experimental Protocols
Protocol 1: Measuring Drug-Induced Dopamine Release Using PET Imaging
This protocol is used to investigate the role of fast dopamine increases in the reinforcing effects of drugs of abuse in human participants [8].
- Radiotracer Administration: Inject a specific D2 dopamine receptor radioligand (e.g., [¹¹C]raclopride or [¹⁸F]N-methylspiroperidol) intravenously.
- PET Data Acquisition: Use Positron Emission Tomography (PET) to monitor the binding of the radioligand in the striatum over time. Baseline binding potential is an index of D2 receptor availability.
- Drug Challenge: Administer the drug of interest (e.g., intravenous methylphenidate or amphetamine) during the scan.
- Data Analysis: Calculate the displacement of the radioligand by the drug-induced increase in endogenous dopamine. A greater displacement indicates a larger dopamine release.
- Behavioral Correlation: Correlate the magnitude of dopamine release (percent change in binding potential) with subjective self-reports of "high" or "euphoria" using standardized rating scales.
Protocol 2: Assessing Glutamate and GABA in Cortical Regions Using 7-Tesla MRS
This protocol details the use of high-field MRS to quantify regional levels of glutamate and GABA, providing an index of excitatory/inhibitory balance in disorders like OCD [7].
- Subject Preparation: Recruit participant groups (e.g., individuals with OCD and healthy controls). Acquire high-resolution anatomical scans (e.g., T1-weighted MRI).
- Voxel Placement: Precisely place spectroscopic voxels in regions of interest based on anatomical landmarks. Key regions include the Anterior Cingulate Cortex (ACC), Supplementary Motor Area (SMA), and a control region like the Occipital Cortex (OCC).
- Spectral Acquisition: Use a semi-LASER sequence or equivalent optimized for 7-Tesla to acquire spectra. This ensures reliable and separate quantification of Glu and GABA.
- Spectral Processing and Quantification: Process the raw data to remove artifacts and fit the spectra using specialized software (e.g., LCModel) to estimate absolute concentrations of Glu, GABA, and other metabolites (e.g., Gln, NAA).
- Statistical Analysis: Compare metabolite levels between groups within each voxel. Perform correlation analyses between metabolite levels (e.g., Glu in SMA) and behavioral scores (e.g., Yale-Brown Obsessive Compulsive Scale (YBOCS) or Obsessive-Compulsive Inventory (OCI)).
Signaling Pathways and Circuit Diagrams
Direct and Indirect Pathway Circuit Logic
Addiction Cycle Neurocircuitry
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Reagents and Materials
| Item | Function/Application |
|---|---|
| [¹¹C]raclopride | A radioligand for Positron Emission Tomography (PET) imaging used to quantify dopamine D2/D3 receptor availability and measure drug-induced changes in synaptic dopamine levels in the striatum [8]. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic tools (e.g., hM3Dq, hM4Di) used for remote, reversible, and cell-type-specific manipulation of neuronal activity in defined circuits (e.g., selective targeting of D1 vs D2 MSNs) [10]. |
| Sapap3 Knockout Mice | A genetic mouse model lacking the SAPAP3 protein, which is a postsynaptic scaffolding protein at corticostriatal synapses. These mice exhibit excessive self-grooming and anxiety-like behaviors, providing a model for compulsive behaviors relevant to OCD [12]. |
| 7-Tesla MRI/MRS Scanner | High-field magnetic resonance imaging and spectroscopy hardware that allows for the reliable and separate quantification of neurometabolites, particularly glutamate and GABA, in specific brain regions like the ACC and SMA [7]. |
| AAV-hSyn-FLEX-ChR2 | A Cre-dependent adeno-associated virus (AAV) carrying Channelrhodopsin-2 (ChR2) under a human synapsin promoter. Used for projection-specific optogenetic stimulation of defined neural pathways (e.g., corticostriatal projections) [10]. |
Frameworks in Focus: FAQ
Q1: What is the core distinction between the "wanting" and "liking" processes in the Incentive-Sensitization Theory?
The Incentive-Sensitization Theory posits that "liking" (the pleasure derived from a reward) and "wanting" (the motivation to obtain it) are distinct processes [13] [14]. Repeated drug use can sensitize the mesocorticolimbic dopamine system, particularly the neural pathways that attribute incentive salience to rewards and their cues [15] [13]. This leads to a core pathology: a dramatic increase in pathological "wanting" for the drug, while "liking" for the drug may remain unchanged or even decrease [13] [14]. This sensitized "wanting" is persistent and can trigger compulsive seeking and relapse, often in response of drug-associated cues, long after withdrawal has ended [13].
Q2: How does the habit formation theory explain the transition from voluntary drug use to compulsive behavior?
The habit theory suggests a shift from action-outcome to stimulus-response control [16] [17]. Early drug use is goal-directed, driven by the desirable outcome (e.g., euphoria). With repetition, the behavior becomes habitual [16]. In this stage, drug-seeking is automatically triggered by contextual cues (e.g., a specific location) with minimal influence from the current value of the outcome, making the behavior inflexible and persistent even when the outcome is devalued (e.g., when the negative consequences outweigh the high) [16] [17]. Some research further proposes distinguishing between motor habits (simple S-R contingencies) and motivational habits (S-R connections modulated by an urge, such as craving) [16].
Q3: What is the role of impaired executive control in addiction?
Executive control, governed primarily by the prefrontal cortex, encompasses higher-order cognitive functions like inhibitory control, working memory, and cognitive flexibility [18]. Impaired executive control, particularly deficient response inhibition, is theorized to contribute to addiction by reducing the ability to suppress strong urges to take drugs, despite negative consequences [18] [19]. This deficit can create a vicious cycle where impaired inhibitory control allows for uninhibited obsessions and compulsions, which in turn further reinforces the behavior [18]. This dysfunction may represent a pre-existing vulnerability factor for developing addiction [18].
Q4: Can these frameworks be applied to behavioral addictions like Gambling Disorder?
Yes. The Incentive-Sensitization Theory is considered a promising model for understanding Gambling Disorder [15] [14]. The uncertainty of reward in gambling is thought to enhance dopaminergic activity in the mesolimbic pathway, potentially sensitizing the "wanting" system and increasing the incentive value of gambling-related cues [15]. This suggests transdiagnostic neurobiological mechanisms underlying both substance and behavioral addictions [15] [14].
Q5: How do stress and anxiety interact with these frameworks in addiction?
Significant evidence points to a phenomenon known as cross-sensitization [15]. This means that sensitization to one stimulus (e.g., a drug) can enhance the sensitivity and dopaminergic response to another (e.g., stress) [15]. Since stress is a major trigger for relapse, this interaction creates a powerful mechanism through which sensitized neural 'wanting' pathways, anxiety, and substance use can coalesce and exacerbate comorbid pathology [15].
The Scientist's Toolkit: Experimental Protocols & Reagents
Key Behavioral Paradigms for Modeling Addiction in Animals
The table below summarizes core behavioral assays used to investigate different aspects of addiction pathology [20].
Table 1: Key Animal Models in Addiction Research
| Behavioral Paradigm | Core Construct Measured | Methodology Summary | Key Interpretive Consideration |
|---|---|---|---|
| Behavioral Sensitization [20] [13] | Incentive Sensitization / Neural Hypersensitivity | Repeated, experimenter-administered non-contingent drug exposure (e.g., daily i.p. injections), followed by a drug challenge after a withdrawal period. Locomotor activity is measured. | Sensitization (enhanced locomotor response) is indirect evidence of drug-induced neuroadaptations in motivation circuitry. Sensitization can be context-specific [13]. |
| Drug Self-Administration (SA) [20] | Drug-Taking & Motivation | An animal performs an operant response (e.g., lever press, nose poke) to receive an intravenous drug infusion. | Allows for contingent drug delivery. Key variations include progressive ratio (to measure motivation) and SA with punishment (to measure compulsivity). |
| Reinstatement Model [20] | Relapse | After SA and subsequent extinction of drug-seeking, the behavior is reinstated by a drug prime, a stressor, or presentation of drug-paired cues. | Models triggers of relapse in humans (drug exposure, stress, cues). Considered the gold standard for studying relapse. |
| Conditioned Place Preference (CPP) [20] | Reward Learning / Pavlovian Conditioning | An animal learns to associate one distinct chamber with a drug and another with saline. Preference for the drug-paired chamber is tested in a drug-free state. | Measures the conditioned rewarding effects of drugs and cues. It involves non-contingent drug administration. |
Research Reagent Solutions
Table 2: Essential Research Reagents and Their Functions
| Reagent / Tool Category | Example(s) | Primary Function in Research |
|---|---|---|
| Dopamine Receptor Agonists/Antagonists | SCH-23390 (D1 antagonist), Raclopride (D2 antagonist) | To pharmacologically dissect the role of specific dopamine receptor subtypes in sensitization, SA, and reinstatement [20] [13]. |
| c-Fos Immunohistochemistry | c-Fos antibodies | To map and quantify neural activity in specific brain regions (e.g., NAc, VTA, PFC) following behavioral tests like a sensitization challenge or cue-induced reinstatement [21]. |
| Viral Vector Technology | DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | For cell-type-specific neuromodulation (inhibition or excitation) to establish causal roles of specific neural circuits in addiction behaviors with temporal precision. |
| Radioligands for PET Imaging | [11C]Raclopride | Used in tandem with microdialysis or Positron Emission Tomography (PET) in animals and humans to measure drug-induced dopamine release, providing evidence for sensitization [14]. |
Troubleshooting Common Experimental Challenges
Challenge 1: Failure to observe behavioral sensitization.
- Potential Cause: The expression of sensitization is often context-dependent. If the drug challenge is given in an environment that is different from the environment where the drug was experienced during the induction phase, sensitization may not be expressed [13].
- Solution: Ensure consistency between the training and testing environments (same context, handling procedures, etc.). Control for the potential role of context by including separate groups of animals tested in paired vs. unpaired environments.
Challenge 2: High variability in self-administration acquisition.
- Potential Cause: Individual genetic and behavioral traits significantly influence vulnerability to drug use. Using outbred rodent strains without pre-screening can lead to high variability, masking strong effects in a subset of animals [20].
- Solution: Implement pre-screening to isolate subpopulations with specific traits. Common models include:
- High-Responder (HR) vs. Low-Responder (LR): Based on initial locomotor response to a novel environment, predicting acquisition of drug SA [20].
- Sign-Tracker (ST) vs. Goal-Tracker (GT): Based on individual variation in Pavlovian conditioned approach, with STs showing greater cue-triggered "wanting" and being more vulnerable to relapse [20].
Challenge 3: Distinguishing goal-directed from habitual actions in animals.
- Potential Cause: The standard outcome devaluation test (e.g., using LiCl to induce taste aversion) can be confounded by general motivational or sensorimotor effects [17].
- Solution: Use a two-action, outcome devaluation task. Train animals to perform two different actions (e.g., press left lever, press right lever) for two distinct outcomes. Then, devalue one outcome (e.g., specific food) by specific satiety or LiCl pairing. In a subsequent extinction test, a goal-directed animal will reduce performance of the action associated with the devalued outcome, while a habitual animal will not [17].
Conceptual Workflow and Signaling Pathways
Incentive Sensitization in the Mesolimbic Pathway
Experimental Workflow for Modeling Compulsive Seeking
FAQs and Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: What are the core factors that determine individual vulnerability in animal models? Individual vulnerability to compulsive drug seeking is not determined by a single factor but by the interaction of three core domains:
- Genetic & Biological Factors: The genetic makeup of an animal accounts for a significant portion of its risk. This includes innate predispositions in brain reward circuitry and epigenetic modifications that can be inherited transgenerationally [22].
- Environmental Factors: The animal's living conditions, such as an Enriched Environment (EE) that provides sensory, cognitive, and social stimulation, can serve as a protective factor, reducing drug consumption and relapse [23]. Conversely, stressful environments increase vulnerability.
- Behavioral Traits: Innate behavioral characteristics, such as high impulsivity, sensation-seeking, or a sign-tracking (vs. goal-tracking) phenotype, are strong predictors of increased drug self-administration and relapse [20].
FAQ 2: How can I reliably segregate populations into "addiction-like" and "resilient" groups in my experiments? The most valid method is to use a multi-criteria approach based on key symptoms of addiction, rather than relying on a single measure like total drug intake. A standard protocol involves [22] [20]:
- Drug Self-Administration: Allow animals to self-administer a drug.
- Progressive Ratio (PR) Testing: Assess the motivation to seek the drug by measuring the "break point" (the maximum number of lever presses an animal will perform for a single drug infusion).
- Persistence of Use despite Negative Consequences: Challenge drug-taking by pairing it with an aversive stimulus (e.g., a mild footshock). Animals are then classified based on their combined scores across these measures, typically identifying the top 20-25% as the "addiction-like" group [22].
FAQ 3: My animal model shows high drug intake but does not persist when challenged. Is this still a valid model of addiction? High drug intake alone is not synonymous with the clinical diagnosis of addiction, which is characterized by a loss of control. The DSM-5 criteria for Substance Use Disorder include compulsive use despite harmful consequences [24]. An animal that ceases use when faced with a negative consequence (like footshock) is demonstrating intact control and is often classified as a "Non-addict" or "Resilient" phenotype in research settings [22] [20]. Your model is valid for studying drug use, but to model the core pathology of addiction, incorporating a measure of persistence despite punishment is crucial.
FAQ 4: Can the vulnerability acquired by a parent generation be passed to offspring? Yes, research demonstrates transgenerational transmission of addiction vulnerability. Crucially, this transmission is linked to the motivational state of the parent, not merely drug exposure. Offspring (F1 and F2 generations) of male rats classified as "Addict" based on high incentive motivation for cocaine themselves show higher motivation to seek cocaine. This effect is not seen in the offspring of rats that passively received the same amount of cocaine (yoked controls), highlighting the role of experience-driven epigenetic mechanisms [22].
Troubleshooting Common Experimental Issues
Issue 1: Low differentiation between "Addiction-like" and "Non-addict" phenotypes.
- Potential Cause: Inadequate stringency in the classification criteria.
- Solution:
- Ensure you are using a multi-symptomatic approach (e.g., combining motivation (PR) and persistence despite punishment).
- Consider adjusting the aversive stimulus in the punishment test to a level that is sufficient to deter most "Non-addict" animals but is overcome by the "Addiction-like" group.
- Verify that your statistical method for classification (e.g., selecting the top and bottom percentiles of a combined z-score) is correctly implemented.
Issue 2: High variability in self-administration data within treatment groups.
- Potential Cause: Unaccounted for innate behavioral traits influencing the behavior.
- Solution:
- Pre-screen animals: Before beginning drug studies, screen for known predictive traits like impulsivity (using the 5-choice serial reaction time task) or sign-tracking vs. goal-tracking behavior. You can then balance these traits across experimental groups or use them as co-variates in your analysis [20].
- Control environmental factors: Standardize housing conditions (e.g., all isolated or all enriched) to minimize this source of variability. Note that standard laboratory housing is a form of environmental impoverishment that can heighten vulnerability [23].
Issue 3: Difficulty in translating "Environmental Enrichment" (EE) from rodent to human studies.
- Potential Cause: EE is a multi-faceted construct that is complex to define and measure in humans.
- Solution: A recently developed self-report EE scale for humans can be a valuable translational tool. This scale measures components such as [23]:
- Physical activity and exercise.
- Social interaction and support.
- Cognitive stimulation (e.g., reading, playing music).
- Sensory richness and novelty. Validated in smokers and patients with alcohol use disorder, this scale confirms that higher EE scores are associated with lower consumption, dependence, and craving [23].
Data Presentation
Quantitative Data on Individual Vulnerability Factors
Table 1: Key Factors Predicting Individual Vulnerability in Animal Models
| Factor Domain | Specific Factor / Paradigm | Key Quantitative Finding | Associated Behavioral Phenotype |
|---|---|---|---|
| Genetic/Epigenetic | Transgenerational Inheritance (Motivation-driven) [22] | F1 & F2 offspring of "Addict" F0 rats showed ~30-50% higher lever presses (FR5) and break points (PR) for cocaine. | Increased motivation and vulnerability to cocaine-seeking. |
| Environmental | Environmental Enrichment (EE) in Smokers [23] | Higher EE scores were significantly correlated with lower nicotine consumption, dependence, and craving. | Protective effect, reduced consumption and relapse risk. |
| Behavioral Trait | Sign-Tracking (ST) vs. Goal-Tracking (GT) [20] | ST animals show significantly higher rates of drug-seeking and relapse after extinction compared to GT animals. | Increased propensity for cue-induced craving and relapse. |
| Behavioral Trait | Impulsivity (5-CSRTT) [20] | High impulsivity scores predict faster acquisition of drug self-administration and increased drug intake. | Predisposition to initiate and maintain drug use. |
| Behavioral Trait | High Responder (HR) vs. Low Responder (LR) [20] | HR animals (high novelty-induced locomotion) acquire amphetamine self-administration at a lower dose than LR animals. | Increased vulnerability to the initial acquisition of drug use. |
Experimental Protocols for Key Methodologies
Protocol 1: Classifying "Addiction-like" vs. "Non-addict" Phenotypes using a Multi-Criteria Approach [22]
- Subjects: Male Sprague-Dawley rats.
- Drug Self-Administration (SA) Training:
- Implant intravenous catheters.
- Place animals in operant chambers equipped with two levers (active and inactive).
- Train animals on a Fixed-Ratio 1 (FR1) schedule, where each press on the active lever delivers a cocaine infusion (e.g., 0.75 mg/kg/infusion). Gradually increase the schedule to FR5.
- Conduct daily 4-hour sessions for approximately 10-12 days.
- Progressive Ratio (PR) Testing:
- To assess motivation, switch the reinforcement schedule to a PR, where the response requirement for each subsequent infusion increases exponentially.
- The session ends when the animal fails to meet the response requirement within a set time (e.g., 1 hour).
- The primary outcome is the break point (the last ratio completed).
- Persistence despite Punishment:
- During SA sessions, introduce a contingent punisher (e.g., a mild footshock) upon active lever presses.
- The intensity is set to deter most animals but is overcome by the most compulsive ones.
- Measure the percentage of suppression of drug intake compared to baseline.
- Classification:
- For each animal, calculate normalized Z-scores for (a) drug intake under FR5, (b) break point under PR, and (c) resistance to punishment.
- Sum the Z-scores to create a combined "addiction score."
- Classify the top 25% of the population as "Addiction-like" and the bottom 40% as "Non-addict" for further study.
Protocol 2: Assessing the Protective Role of Environmental Enrichment (EE) [23]
- EE Construction for Rodents:
- Control Group: Standard laboratory housing (2-3 animals per standard cage).
- EE Group: Larger cages (e.g., 100 x 50 x 50 cm) housing 8-12 animals.
- Enrichment Items: Provide a variety of stimulating objects such as running wheels, plastic tubes, wooden blocks, nesting materials, and Lego structures. Re-arrange and replace a portion of the objects 2-3 times per week to maintain novelty.
- Experimental Timeline:
- Pre-Exposure: House animals in their respective (EE or control) conditions for 2-4 weeks prior to any drug exposure.
- Drug SA or Relapse: Proceed with standard drug self-administration protocols. To test the therapeutic effect of EE, it can also be introduced during abstinence after SA training.
- Key Outcome Measures:
- Compare the two groups on measures of:
- Acquisition: Rate and level of drug SA.
- Motivation: Break point on a PR schedule.
- Relapse: Drug-seeking behavior after extinction, triggered by cues, stress, or a prime dose of the drug.
- Compare the two groups on measures of:
Signaling Pathways and Experimental Workflows
Vulnerability Factor Integration
Multi-Criteria Phenotype Classification
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Modeling Individual Vulnerability
| Item / Reagent | Function / Application | Specific Examples / Notes |
|---|---|---|
| Intravenous Catheters | Chronic, reliable delivery of drugs during self-administration sessions. | Typically made of Silastic tubing; surgically implanted into the jugular vein. Requires regular flushing with heparinized saline to maintain patency. |
| Operant Conditioning Chambers | The controlled environment for measuring drug-seeking and taking behaviors. | Equipped with levers, cue lights, speakers (for tones), and an infusion pump. Often housed within sound-attenuating cubicles. |
| Controlled Substances | The primary reinforcer in the study. | Cocaine HCl, heroin, methamphetamine, etc. Doses are typically reported in mg/kg/infusion. Must be handled and stored according to strict DEA and institutional schedules [25]. |
| Footshock Generator | To provide a quantifiable negative consequence for assessing compulsive use. | Used in "persistence despite punishment" tests. Intensity is critical (e.g., 0.1-0.5 mA); must be calibrated to deter most but not all animals. |
| Environmental Enrichment Caging | To model the protective effects of a stimulating environment. | Large cages containing running wheels, plastic toys, wooden blocks, and shelters. Objects are rotated regularly to maintain novelty [23]. |
| Epigenetic Analysis Kits | To investigate transgenerational and experience-driven mechanisms. | Kits for Bisulfite Sequencing (to analyze DNA methylation) and ChIP (Chromatin Immunoprecipitation) are used on tissue samples (e.g., sperm, brain regions like NAc) [22]. |
Operationalizing Compulsion: Key Behavioral Paradigms and Protocols
Frequently Asked Questions (FAQs)
Q1: Why is drug self-administration considered the "gold standard" in preclinical addiction research?
Drug self-administration is regarded as the gold standard because it has high predictive validity and face validity for modeling human substance use disorders [26] [27]. It is an operant conditioning paradigm where animals voluntarily perform a behavior (e.g., lever press) to receive a drug infusion, directly measuring the drug's reinforcing properties [28] [20]. Virtually all drugs abused by humans are self-administered by animals, and the patterns of drug intake resemble those observed in humans [28] [27]. This model is critical for assessing the abuse liability of novel compounds and the efficacy of potential pharmacotherapies [28] [29].
Q2: What are the key differences between Short Access (ShA) and Long Access (LgA) protocols, and why are they important?
The key difference lies in session duration and the resulting drug intake pattern, which models different stages of addiction.
- Short Access (ShA): Typically involves limited daily sessions (e.g., 1-2 hours). This protocol produces stable, controlled drug intake and is often used to study the initial acquisition and maintenance of drug-taking behavior [28].
- Long Access (LgA): Involves extended daily sessions (e.g., >4-6 hours). This protocol leads to an escalation of drug intake over time, modeling the transition from controlled use to the compulsive, addiction-like drug seeking seen in humans [28] [20]. Escalation is a hallmark of addiction and reflects a loss of control over intake [28].
Q3: What common technical challenge is associated with intravenous catheters in rodent studies, and how can it be managed?
The primary challenge is maintaining catheter patency (preventing blockages and failures) over the course of a long-term study [30]. This can be managed through:
- Aseptic Surgical Technique: Ensuring sterile implantation of the jugular or femoral vein catheter.
- Post-operative Care: Allowing sufficient recovery time (e.g., 5-7 days) before starting experiments [30].
- Catheter Maintenance: Implementing a strict daily flushing regimen with heparinized saline and an antibiotic solution to prevent clotting and infection [30].
- Patency Testing: Regularly verifying catheter functionality, for example, by administering a short-acting anesthetic (e.g., propofol) through the catheter and observing for a rapid effect [30].
Q4: How can I troubleshoot a situation where my animals are not acquiring stable self-administration (e.g., poor lever discrimination)?
Poor acquisition can stem from several factors. The troubleshooting guide below outlines common issues and solutions.
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Failure to acquire self-administration | Incorrect drug dose, surgical complications, poor health | Validate catheter patency, adjust drug dose, ensure full post-surgical recovery [30] |
| Poor active/inactive lever discrimination | Inadequate training, weak reinforcement | Implement contingent advancement training protocols, use a distinct cue light for active lever, consider mild food restriction to enhance initial learning [30] |
| High variability in drug intake | Genetic heterogeneity, differences in catheter function | Use genetically defined rodent strains, standardize handling procedures, routinely check catheter patency [30] [31] |
Q5: What neurobiological adaptations are associated with the transition to compulsive drug seeking?
Chronic drug self-administration induces persistent neuroadaptations, particularly within the mesolimbic dopamine system and associated circuits [28]. Key adaptations include:
- Synaptic Plasticity: Long-term potentiation (LTP) and depression (LTD) in the Ventral Tegmental Area (VTA) and Nucleus Accumbens (NAc) [28].
- Molecular Changes: Increased expression of transcription factors like ΔFosB and CREB in the NAc, which regulate gene expression related to addiction [28].
- Glutamatergic System Dysregulation: Functional upregulation of AMPA receptors and decreased expression of the glutamate transporter GLT1 in the NAc, contributing to heightened relapse vulnerability [28].
- Circuit-Level Shifts: A progression from ventral striatal (reward-driven) to dorsal striatal (habit-driven) control over drug-seeking behavior [28].
Experimental Protocols & Methodologies
Core Self-Administration Paradigms
Intravenous Self-Administration (IVSA) Protocol This is the most direct method to model human drug taking [28] [27] [30].
- Animal Preparation: Surgically implant an indwelling intravenous catheter into the jugular or femoral vein of a rodent (rat or mouse). Allow 5-7 days for recovery [30].
- Acquisition Training: Place the animal in an operant chamber. A response on the "active" lever results in:
- Schedule of Reinforcement:
- Start with a Fixed-Ratio 1 (FR1) schedule, where each active lever press delivers one drug infusion.
- Gradually increase the response requirement (e.g., to FR2, FR4) to strengthen the operant behavior [30].
- Session Type:
- Short Access (ShA): Conduct 1-2 hour daily sessions to establish stable baseline intake.
- Long Access (LgA): Conduct 6+ hour daily sessions to induce escalation of drug intake [28].
Oral Self-Administration Protocol Primarily used for alcohol research, this model has high face validity for human drinking [26] [27].
- Two-Bottle Choice Paradigm: In the home cage, provide two bottles: one with an alcohol solution (e.g., 10-12% v/v) and one with water. Measure fluid consumption over 24 hours to assess preference [26] [27].
- Operant Oral Self-Administration: Animals perform a lever press or nose poke to gain access to a sipper tube containing an alcohol solution. This allows for the measurement of motivated responding for the drug [27].
- Intermittent-Access Model: To model binge-like drinking, offer the alcohol solution for 24 hours, followed by 24 hours of abstinence. This cycle leads to higher and more pharmacologically relevant levels of alcohol intake [27].
Advanced Behavioral Schedules
To probe different facets of addiction, more complex schedules are used after stable self-administration is acquired.
- Progressive Ratio (PR): The response requirement for each subsequent drug infusion increases exponentially (e.g., 1, 2, 4, 6, 9...). The final ratio completed before the animal ceases to respond is the "breakpoint," which quantifies the motivation to work for the drug [28] [32].
- Extinction & Reinstatement: Drug-seeking behavior is "extinguished" by withholding the drug and its associated cues. Subsequently, "reinstatement" of drug-seeking is triggered by a priming injection of the drug, exposure to drug-associated cues, or a stressor. This models relapse in humans [28] [20] [30].
- Choice Procedures: Animals are given a choice between a drug infusion and an alternative reinforcer (e.g., sweet food or a social interaction). This paradigm is highly predictive of human outcomes and measures the relative value of the drug [32] [20].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials required for establishing a self-administration study.
| Item | Function & Application | Key Considerations |
|---|---|---|
| Intravenous Catheters | Chronic, direct delivery of drugs into the bloodstream [30]. | Material (e.g., silicone), size, and vessel (jugular vs. femoral) are critical for long-term patency [30]. |
| Operant Chambers | Controlled environment where animals learn the lever-press/nose-poke response for drug [28]. | Must include active/inactive manipulanda, cue lights, tone generator, and an infusion pump. |
| Infusion Pumps | Precisely deliver a set volume of drug solution contingent on a correct response [28]. | Must be calibrated for the specific drug dose (mg/kg/infusion) and animal species. |
| Drugs of Abuse | The primary reinforcer (e.g., Cocaine HCl, Heroin, Morphine, Nicotine, Alcohol) [28]. | Purity, solubility, and stability in solution are paramount. Dose must be optimized for the species and route. |
| Conditioned Stimuli | Cue lights and tones paired with drug delivery, which acquire motivational properties [28]. | Critical for second-order schedules and cue-induced reinstatement of drug-seeking. |
Signaling Pathways & Neuroadaptations in Compulsive Seeking
Chronic drug self-administration leads to profound changes in brain circuitry. The diagram below illustrates the key neural pathways and adaptations.
Key Neurocircuitry of Addiction
The tables below consolidate key quantitative findings from the literature to aid in experimental design and data interpretation.
Table 1: Neurobiological Markers of Chronic Drug SA
| Adaptation | Drug Class | Brain Region | Measurable Change | Functional Consequence |
|---|---|---|---|---|
| ΔFosB Accumulation | Psychostimulants | NAc | ↑ Protein Expression [28] | Persistent transcription, increased relapse vulnerability |
| CREB Activation | Various | NAc | ↑ Phosphorylation [28] | Mediates tolerance & dysphoria during withdrawal |
| GluA2 Upregulation | Psychostimulants | NAc | ↑ AMPA subunit transcription [28] | Enhanced glutamatergic transmission |
| GLT-1 Downregulation | Cocaine | NAc | ↓ Astrocyte transporter [28] | Impaired glutamate clearance, hyperexcitability |
| Dendritic Spine Changes | Psychostimulants | NAc, PFC | ↑ Density & length [28] | Structural plasticity, habit formation |
| Depressants (e.g., Morphine) | NAc, Hippocampus | ↓ Density [28] | Altered structural connectivity |
Table 2: Behavioral Escalation & Model Criteria
| Behavioral Measure | Limited Access (ShA) | Extended Access (LgA) | Relevance to DSM-5 [28] |
|---|---|---|---|
| Drug Intake | Stable over time | Escalates progressively [28] | Loss of control over use |
| Motivation (Breakpoint) | Moderate | Significantly increased [28] | Great deal of time spent to obtain drug |
| Resistance to Punishment | Low | High (persistent use despite adverse consequences) [28] | Use despite physical/psychological problems |
| Cue-Induced Reinstatement | Moderate | Augmented [28] | Craving triggered by cues |
Punishment-based models are critical tools in preclinical research for studying the compulsive dimension of substance use disorders. These paradigms model a core clinical feature of addiction: the persistence of drug-seeking and drug-taking behaviors despite the occurrence of negative consequences. A quintessential method involves challenging an animal's operant responding for a drug, such as cocaine, with the presentation of an adverse stimulus like an electric footshock. This guide details the protocols, troubleshooting, and resources for implementing these models to investigate the neurobiological underpinnings of compulsion-like behavior.
Detailed Experimental Protocol
The following section provides a step-by-step methodology for a punishment-based self-administration experiment, adapted from established models in the field [33].
Animal Subjects
- Species/Strain: Male Wistar rats are commonly used.
- Surgery: Implant with a chronic intravenous jugular catheter to permit intravenous drug delivery.
Cocaine Self-Administration Training
- Apparatus: Standard operant conditioning chambers equipped with at least two nose-poke ports or levers, a house light, and a cue light/tone generator.
- Session Parameters:
- Duration: 1-hour daily sessions.
- Reinforcement Schedule: Fixed-Ratio 3 (FR3). The animal must make three responses on the "active" port to receive a single drug infusion.
- Drug Infusion: A dose of 0.5 mg/kg/infusion of cocaine is standard [34].
- Conditioned Stimulus (CS): Each cocaine infusion is paired with a compound audiovisual stimulus (e.g., activation of a nose-poke light and a tone) for 2-5 seconds.
- Acquisition Criterion: Animals typically must achieve a stable baseline of responding (e.g., >10 infusions per session for 3 consecutive days) before progressing to the punishment phase [34].
Punishment Phase
- Objective: To assess the resilience of drug-seeking behavior when it is paired with a negative outcome.
- Punishment Contingency: A portion (e.g., 30-50%) or all of the drug-paired responses now also result in the delivery of a mild electric footshock to the grid floor of the chamber.
- Footshock Parameters:
- Intensity: Typically escalated across sessions (e.g., from 0.1 mA to 0.9 mA) [33].
- Duration: A brief shock, usually 0.5 seconds.
- Control: It is critical to include a control group that continues to self-administer cocaine without any punishment contingency to control for non-specific changes in behavior over time [35].
Key Behavioral Measures
- Primary Measure: The number of punished responses on the active port compared to baseline and control group levels.
- Suppression Ratio: (Baseline Responses - Punished Responses) / (Baseline Responses + Punished Responses). A higher ratio indicates greater behavioral suppression.
- Inactive Port Responses: Responses in the non-drug-associated port are measured to assess general locomotor activity and non-specific behavioral suppression.
The table below summarizes the quantitative outcomes from a key study investigating how prior experience with intense punishment alters future behavior [33].
| Experimental Phase | Punishment Intensity | Behavioral Outcome | Interpretation |
|---|---|---|---|
| Initial Punishment | 0.1 mA | Minimal suppression | This intensity is initially ineffective at suppressing well-established drug-taking. |
| Initial Punishment | 0.3 - 0.9 mA | Progressive suppression | Drug-taking decreases as the cost (shock intensity) increases. |
| Post-High-Intensity Experience | 0.1 mA (Retest) | Significant suppression | A previously ineffective shock intensity now potently suppresses drug-taking. |
| Control (Passive Shock) | 0.1 mA (Retest) | Minimal suppression | Mere exposure to shock is insufficient; the contingent experience is critical. |
Frequently Asked Questions (FAQs)
Q1: What is the critical distinction between "punishment" and other aversive learning paradigms like "fear conditioning"? Punishment is a form of instrumental aversive learning where a specific behavior (e.g., a lever press) causes an aversive event (e.g., footshock). This leads to the formation of a response-outcome (R-O) association that suppresses that specific behavior. In contrast, fear conditioning is a Pavlovian process where a neutral stimulus (a tone) predicts an aversive event, regardless of the animal's behavior, forming a stimulus-outcome (S-O) association that can cause a general, non-specific suppression of behavior like freezing [35]. Conflating these contingencies will confound data interpretation.
Q2: My animals show complete suppression of drug-taking during punishment. Is this a failed experiment? Not necessarily. Complete suppression indicates that the chosen punisher (e.g., footshock intensity) is too high for the reinforcing strength of the drug dose/schedule in your specific setup. To model compulsion, the goal is often to identify the subset of animals that continue to respond. Troubleshooting: Titrate down the shock intensity or increase the drug dose (e.g., by using a progressive ratio schedule prior to punishment) to find a parameter where a bimodal distribution of "suppressors" and "non-suppressors" emerges [35] [33].
Q3: Why is it important to use a "contingent" punishment design rather than just giving animals non-contingent footshocks? The contingency is fundamental. A key study demonstrated that rats that experienced response-contingent high-intensity punishment subsequently became more sensitive to lower punishment intensities. Animals that received the same shocks non-contingently did not show this increased sensitivity [33]. This shows that the learning of the action-consequence relationship is essential for the behavioral adaptation, directly modeling the conflict faced by humans with addiction.
Q4: What neurobiological mechanisms are implicated in punishment resistance? Research points to specific alterations in the mesolimbic dopamine system and associated circuits [34] [36].
- Dopamine: Signaling in the nucleus accumbens core evolves differently based on context. Dopamine to non-contingent drug cues increases, promoting cue reactivity, while dopamine to contingent cues (following a drug-seeking action) decreases, which may disinhibit and promote escalated consumption [34].
- Serotonin: This neurotransmitter is more strongly associated with processing punishments and promoting behavioral inhibition. Pharmacological manipulations of serotonin in humans affect punishment learning and aversive Pavlovian biases [36]. An imbalance between dopamine-driven reward seeking and serotonin-driven punishment avoidance may underlie compulsion.
The Scientist's Toolkit: Essential Research Reagents & Materials
The table below catalogues the key resources required to establish a punishment-based self-administration model.
| Item | Function/Description |
|---|---|
| Operant Conditioning Chambers | Sound-attenuating boxes equipped with nose-poke ports/levers, cue lights, tone generators, and a grid floor for delivering scrambled footshock. |
| Footshock Generator | A precision current shock generator capable of delivering a range of mild, scrambled shocks (e.g., 0.1 - 0.9 mA) to prevent animals from avoiding the current. |
| Intravenous Catheter & Infusion Pump | A chronic jugular vein catheter connected to a syringe pump for the precise, automated delivery of intravenous cocaine. |
| Cocaine HCl | The primary reinforcer. Typically dissolved in sterile saline (e.g., 0.9% NaCl) and filtered for self-administration. |
| Fast-Scan Cyclic Voltammetry (FSCV) | An electrochemical technique used in conjunction with carbon-fiber microelectrodes to measure real-time, phasic dopamine release in brain regions like the nucleus accumbens during behavior [34]. |
| Carbon-Fiber Microelectrodes | Implanted bilaterally in the brain (e.g., NAcc core) for FSCV recordings to detect neurotransmitter dynamics [34]. |
Experimental Workflow and Behavioral Outcomes
The following diagram illustrates the key stages and decision points in a typical punishment experiment, culminating in the separation of punishment-sensitive and punishment-resistant individuals.
Diagram 1: Workflow for isolating punishment-resistant individuals.
Signaling Pathways in Compulsive Drug Seeking
This diagram summarizes the opposing roles of mesolimbic dopamine signaling, which vary dramatically depending on whether a drug cue is presented contingent on an action or non-contingently.
Diagram 2: Opposing dopamine pathways in addiction behaviors.
A core challenge in treating drug addiction is the high rate of relapse to drug use after periods of abstinence [37]. In humans, relapse is often triggered by exposure to three primary categories of stimuli: stress, drug-associated cues, and the drug itself (drug priming) [38] [39]. For several decades, preclinical research has sought to understand and mitigate this problem using animal models, predominantly the reinstatement model [40] [39]. This model allows researchers to study the resumption of drug-seeking behavior in laboratory animals following extinction of drug-reinforced responding. The fundamental principle is that after a period of extinction, non-contingent exposure to a stressor, a drug-associated cue, or a small priming dose of the drug can robustly reinstate lever-pressing behavior that was previously associated with drug delivery [39]. This technical support document outlines the core methodologies, neurobiological mechanisms, and common troubleshooting points for these foundational models of relapse, framed within the context of a broader thesis on modeling compulsive drug seeking.
Core Reinstatement Models: Protocols and Mechanisms
The reinstatement model is the most established paradigm for studying relapse-like behavior. The general procedure involves three sequential phases: self-administration training, extinction, and reinstatement testing [39]. The table below summarizes the key characteristics of the primary reinstatement models.
Table 1: Summary of Primary Reinstatement Models
| Model Type | Key Triggering Stimulus | Typical Protocol for Induction | Key Neurobiological Substrates |
|---|---|---|---|
| Drug-Priming-Induced [39] | Non-contingent injection of the previously self-administered drug. | After extinction, a priming injection of the drug (e.g., heroin, cocaine) is administered prior to the test session. | Dopamine receptors (D1, D2) in NAc; Opioid receptors; Glutamate receptors in NAc core [39]. |
| Cue-Induced [39] [41] | Discrete cue (e.g., tone, light) previously paired with drug infusion. | After extinction in the absence of the cue, lever presses during testing once again result in the presentation of the discrete cue. | Basolateral amygdala; Nucleus accumbens core; Ventral tegmental area (VTA) [39] [41]. |
| Stress-Induced [42] | Physical or psychological stressor. | After extinction, a stressor (e.g., intermittent footshock, injection of yohimbine) is administered prior to the test session. | CRF and norepinephrine in BNST and CeA; Dopamine and glutamate in VTA, mPFC, and NAc [42]. |
| Context-Induced [39] | Background environment previously associated with drug availability. | Self-administration in Context A, extinction in Context B, then testing back in Context A. | Ventral hippocampus; Basolateral amygdala; Medial prefrontal cortex [39]. |
Drug-Priming-Induced Reinstatement
Experimental Protocol:
- Training: Animals are trained to self-administer a drug (e.g., cocaine, heroin) by pressing a lever. Each infusion is paired with a discrete cue (e.g., light+tone).
- Extinction: The drug and the associated discrete cue are withheld. Lever presses have no programmed consequence. This phase continues until responding reaches a predetermined low level.
- Reinstatement Test: Under extinction conditions, animals receive a non-contingent, priming injection of the drug or a pharmacologically related compound before the session. Reinstatement is quantified as a significant increase in lever-pressing behavior compared to extinction levels [39].
Troubleshooting FAQ:
- Q: What is an appropriate priming dose for cocaine reinstatement?
- A: Doses are typically in the low-to-moderate range (e.g., 0.5-2.0 mg/kg, i.p. or s.c.) that are sufficient to trigger seeking without producing profound locomotor or sedative effects. A dose-response curve should be established for a new lab setup [39].
Cue-Induced Reinstatement
Experimental Protocol:
- Training: Identical to drug-priming protocols. The discrete cue is critically paired with each drug infusion.
- Extinction: Lever presses are extinguished in the absence of the discrete cue.
- Reinstatement Test: Under extinction conditions (no drug available), lever presses now result in the presentation of the discrete cue alone. The ability of this contingent cue to reinstate lever-pressing is measured [39] [41].
Troubleshooting FAQ:
- Q: How can I ensure my discrete cue acquires robust conditioned reinforcing properties?
- A: Ensure a tight temporal contiguity between cue onset and drug delivery. Use a cue duration that overlaps with the drug infusion. A sufficient number of training sessions (often 10+ days) is required for strong conditioning [41].
Stress-Induced Reinstatement
Experimental Protocol:
- Training & Extinction: Conducted as in the other models.
- Reinstatement Test: Prior to the test session, animals are exposed to a stressor. The most common are:
- Intermittent Footshock: Typically, a series of brief, unpredictable footshocks (e.g., 0.5-1.0 mA, 0.5-1.0 sec duration) delivered over a period (e.g., 15 minutes) [42].
- Pharmacological Stressors: Systemic administration of the α2-adrenergic receptor antagonist yohimbine (e.g., 1.25-2.5 mg/kg, i.p.), which induces a stress-like state by increasing noradrenaline release [42]. Reinstatement is then measured under extinction conditions.
Troubleshooting FAQ:
- Q: My stress-induced reinstatement is inconsistent. What could be wrong?
- A: Stress-induced reinstatement is highly dependent on the specific stressor and drug class. Not all stressors are effective. Footshock and yohimbine are the most reliable. Ensure stressor parameters are calibrated correctly and that animals are not habituated to the stress context [42].
Beyond Extinction: Emerging Models of Voluntary Abstinence
A significant development in the field is the creation of models where abstinence is voluntary rather than experimenter-imposed via extinction. This is considered to have greater translational relevance to human addiction, where abstinence is often self-initiated [43] [44].
Table 2: Models of Relapse after Voluntary Abstinence
| Model | Method to Induce Voluntary Abstinence | Relapse Test | Key Advantage |
|---|---|---|---|
| Adverse Consequences [44] | Introducing a negative consequence to drug taking (e.g., footshock punishment) or seeking (e.g., an electric barrier). | Exposure to drug cues, priming, or stress. | Models the clinical scenario where users quit due to negative repercussions. |
| Discrete Choice [43] [44] | Providing mutually exclusive choices between a drug and a palatable food reward. Rats consistently choose food, leading to voluntary abstinence. | Exposure to drug cues or stress after a period of choice-induced abstinence. | Incorporates the role of alternative, non-drug rewards in maintaining abstinence, akin to contingency management in humans. |
Neurobiological Pathways of Relapse
Understanding the neural circuitry of relapse is essential for target identification. The following diagrams summarize the key brain regions and neurochemical systems implicated in different forms of reinstatement.
Core Reinstatement Circuitry
Diagram 1: Neural circuitry of different relapse triggers. Key: BLA (Basolateral Amygdala); NAc (Nucleus Accumbens); VTA (Ventral Tegmental Area); BNST (Bed Nucleus of Stria Terminalis); CeA (Central Amygdala); vmPFC (ventromedial Prefrontal Cortex); DA (Dopamine); CRF (Corticotropin-Releasing Factor).
The Orexin System in Stress and Cue-Induced Relapse
Recent research has highlighted the role of the orexin (hypocretin) system, originating in the lateral hypothalamus (LH), in regulating relapse behaviors, particularly in response to stress and drug cues [45].
Diagram 2: The orexin pathway in relapse. Orexin neurons in the LH project to key regions like the posterior paraventricular nucleus of the thalamus (pPVT), VTA, and BNST. Blocking orexin receptors (OXR) in the pPVT with an antagonist like suvorexant can selectively prevent stress-induced reinstatement of drug seeking [45].
Table 3: Key Research Reagents for Relapse Studies
| Reagent / Resource | Function / Target | Example Use in Relapse Models |
|---|---|---|
| Yohimbine | α2-adrenergic receptor antagonist | Induces a stress-like state to provoke stress-induced reinstatement of drug seeking [42]. |
| Suvorexant (SUV) | Dual Orexin Receptor (OXR) Antagonist | Used to probe the role of the orexin system; e.g., intra-pPVT infusion blocks stress-induced reinstatement of oxycodone seeking [45]. |
| Naltrexone | Opioid receptor antagonist | Reduces drug-priming-induced and cue-induced reinstatement for heroin and alcohol [39]. |
| Daun02 Chemogenetic Procedure | Inactivation of behaviorally activated neuronal ensembles | Used in Fos-lacZ transgenic rats to ablate specific neuronal ensembles encoding drug-cue memories, preventing context-induced relapse [44]. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic excitation or inhibition of specific neural pathways | The retro-DREADD approach allows selective manipulation of defined neuronal projections to dissect their role in relapse circuits [44]. |
The reinstatement model has been an invaluable tool for unraveling the neuropharmacological basis of relapse [38]. However, the field is evolving. Future research must continue to bridge the gap between traditional extinction-based models and newer paradigms that incorporate voluntary abstinence driven by adverse consequences or the availability of alternative rewards [43] [44]. Furthermore, while the orexin system represents a promising target, particularly for stress-induced relapse [45], a critical challenge remains: the neuropharmacological mechanisms controlling relapse after voluntary abstinence can differ from those controlling reinstatement after extinction [44]. This underscores the necessity of using multiple, complementary models to fully understand the complex phenomenon of relapse and to develop effective, translationally relevant pharmacotherapies for its prevention.
Troubleshooting Guides & FAQs
FAQ: Behavioral Modeling & Experimental Design
Q: What are the core behavioral criteria for modeling compulsive drug seeking in animals? A: Compulsive drug seeking, a hallmark of addiction, is operationally defined in animal models through specific behavioral manifestations. Key criteria include escalation of drug intake with extended access, increased motivation for the drug as measured by progressive ratio schedules, persistence of drug seeking despite adverse consequences (e.g., punishment), and preference for drug over natural rewards like food or social interaction [46] [47]. These criteria translate DSM-IV diagnostic criteria for substance use disorder into quantifiable experimental measures [46].
Q: How can I determine if drug-seeking behavior has become a "habit" in my experiments? A: The gold-standard test for habitual (stimulus-response) behavior is outcome devaluation [48] [49]. In a goal-directed state, animals will reduce drug-seeking efforts if the drug outcome is devalued (e.g., by pairing it with an aversive stimulus like lithium chloride-induced malaise). If drug seeking persists despite devaluation, the behavior is classified as a habit. Neurobiologically, this transition from goal-directed to habitual drug seeking is associated with a shift in neural control from the ventral striatum (e.g., nucleus accumbens) to the dorsal striatum [48] [49].
Q: Why do only a subset of animals typically develop compulsive phenotypes in my studies? A: Individual vulnerability is a key feature of addiction. Pre-existing behavioral traits, such as high impulsivity, predict a greater propensity to escalate drug intake and develop compulsive drug seeking [48] [49]. These traits are linked to individual differences in neurobiology, such as low dopamine D2/3 receptor levels in the nucleus accumbens [49]. Using outbred rodent populations and including measures of impulsivity or other traits as co-variables in your experimental design can help account for this heterogeneity.
Q: My drug and natural reward seeking data are highly variable. Which brain circuits are selectively involved in drug seeking? A: While drug and natural rewards activate overlapping brain circuits, causal studies reveal a drug-selective circuit [50]. The table below summarizes key regions and their necessity for drug versus natural reward seeking.
Table: Necessity of Brain Regions for Drug vs. Natural Reward Seeking
| Brain Region | Necessity for Drug Reward Seeking | Necessity for Natural Reward Seeking |
|---|---|---|
| Nucleus Accumbens Core (NAcore) | Drug-Selective [50] | Not Necessary [50] |
| Prelimbic Cortex (PL) | Drug-Selective [50] [47] | Not Necessary [50] |
| Ventral Tegmental Area (VTA) | Drug-Selective [50] | Not Necessary [50] |
| Central Amygdala (CeA) | Drug-Selective [50] | Not Necessary [50] |
| Basolateral Amygdala (BLA) | Shared [50] | Necessary [50] |
| Hippocampus (HIPP) | Shared [50] | Necessary [50] |
FAQ: Technical & Measurement Challenges
Q: How does cue contingency affect the dopamine signals I'm measuring in the NAcc? A: The context of cue presentation critically determines the direction of phasic dopamine signaling in the Nucleus Accumbens Core (NAcc) [34]. Non-contingent cue presentation (outside the drug-taking context) elicits a craving-like state and dopamine signals increase with extended drug use. Conversely, contingent cue presentation (as a feedback signal for a drug-taking action) is linked to drug "satiety" and its evoked dopamine signal decreases in animals that escalate consumption [34]. These diametrically opposed dopamine trajectories can occur concurrently in the same animal.
Q: What are the best practices for modeling the choice between drug and natural rewards? Q: What are the best practices for modeling the choice between drug and natural rewards? A: Modern paradigms move beyond simple self-administration to incorporate conflict and choice. Effective methods include:
- Concurrent Choice Schedules: Animals choose between a drug-associated lever and a natural reward (e.g., food or sucrose)-associated lever. Compulsion is indicated by a persistent preference for the drug despite the availability of a palatable alternative [46] [50].
- Punishment-Based Conflict: Animals must overcome an aversive consequence (e.g., footshock) to obtain the drug. Resistance to punishment is a direct model of compulsive use despite negative consequences [46] [47].
- Behavioral Economic Procedures: These models assess the relative value of a drug by evaluating consumption as a function of price (response requirement), revealing demand elasticity and its differences from natural rewards.
Experimental Protocols & Methodologies
Protocol: Second-Order Schedule of Reinforcement for Studying Drug Seeking
Purpose: To dissociate the neural mechanisms of drug seeking (appetitive behavior) from drug taking (consummatory behavior) and to study the powerful influence of drug-associated cues [48] [49].
Workflow:
Procedure:
- Acquisition: Animals are first trained to self-administer a drug (e.g., intravenous cocaine) on a simple continuous reinforcement schedule (Fixed Ratio 1, or FR1), where each active lever press results in a drug infusion paired with a conditioned stimulus (CS) [48].
- Second-Order Schedule: Once behavior is stable, a second-order schedule is introduced (e.g., FR10 (FI 15min:S)). In this schedule:
- The animal must complete 10 responses on the active lever (FR10) to produce the drug-associated CS.
- The first response after a 15-minute fixed interval (FI 15min) has elapsed results in both the CS and the drug infusion.
- This means the animal works for an extended period (e.g., 15 minutes) where the only "reward" is the presentation of the drug-paired CS, which acts as a conditioned reinforcer to maintain seeking behavior [48] [49].
- Measurement: The primary dependent variable is the number of responses during the seeking (FI) interval. This paradigm allows for the separate analysis of cue-maintained seeking behavior and the final consummatory act of drug taking.
Protocol: Punishment-Resistance Model of Compulsive Seeking
Purpose: To model the core clinical feature of addiction—continued drug use despite negative consequences [46] [47].
Workflow:
Procedure:
- Extended Access: Animals are given prolonged access to the self-administered drug (e.g., 6 hours or more daily for cocaine). This extended history is critical for inducing the neuroadaptations necessary for a compulsive phenotype to emerge in a subset of animals [46] [47].
- Punishment Contingency: In probe sessions, a punishment is introduced. For example, a percentage (e.g., 30-50%) of drug infusions are paired with a mild footshock. Alternatively, seeking responses can be punished.
- Phenotype Classification: Animals are classified based on their behavior:
- Punishment-Sensitive: Animals that significantly suppress their drug seeking.
- Punishment-Resistant (Compulsive): Animals that continue to seek and take the drug despite the adverse consequence. This resistance is linked to prelimbic cortex (PL) hypofunction [47].
Protocol: Choice-Based Paradigm for Drug vs. Natural Reward
Purpose: To quantify the relative value of a drug reward compared to a natural reward and model the clinical symptom where drug use supersedes important social and occupational activities [46] [50].
Procedure:
- Training: Animals are trained to self-administer a drug (e.g., heroin, cocaine) and separately to self-administer a natural reward (e.g., a palatable sucrose solution).
- Choice Testing: Animals are presented with a choice between two levers or nose-poke ports: one leading to the drug and the other to the natural reward. This can be done after a period of forced abstinence to measure "incubation of craving" for each reward type [50].
- Measurement: The primary measure is the percentage of choices for the drug over the natural reward. Escalated and compulsive drug use is associated with a persistent preference for the drug even when a high-value natural reward is available. Studies using this paradigm have helped identify the circuitry selectively necessary for drug seeking but not natural reward seeking [50].
Quantitative Data Synthesis
Table: Key Behavioral Metrics in Animal Models of Addiction
| Behavioral Metric | Experimental Measure | Interpretation & Significance |
|---|---|---|
| Escalation of Intake | Increased daily drug consumption over time with long-access (LgA, 6+ hrs) but not short-access (ShA, 1 hr) self-administration [46]. | Models transition from controlled use to loss of control over intake. |
| Increased Motivation | Elevated breakpoint under a progressive ratio (PR) schedule, where the response requirement for each subsequent infusion increases [46]. | Reflects increased effort an animal is willing to expend to obtain the drug. |
| Punishment Resistance | Persistence of drug seeking when a probability (e.g., 30-50%) of footshock punishment is delivered contingent on drug infusion [46] [47]. | Core model of compulsive drug use despite negative consequences. |
| Preference over Natural Reward | Choice of a drug-associated lever over a lever associated with a high-value natural reward (e.g., sucrose) in a concurrent choice paradigm [46] [50]. | Models the clinical diagnostic criterion where drug use supplants previously important activities. |
Signaling Pathways & Neural Circuitry
Dopamine Prediction Error Signaling in Addiction
The role of midbrain dopamine neurons in signaling reward prediction errors (RPEs) is a fundamental mechanism subverted in addiction [51]. These neurons signal the difference between received and predicted reward, driving learning.
Mechanism in Addiction: Addictive drugs directly cause massive dopamine release, creating a persistent, pharmacological positive prediction error that powerfully reinforces drug-taking actions and associated cues, independent of the animal's expectations [51]. Over time, this corrupts the learning process, leading to the development of maladaptive habits.
Ventral to Dorsal Striatal Shift in Drug Seeking
A key neurobiological transition in the progression to addiction is the shift in control over drug-seeking behavior from ventral to dorsal striatal circuits [48] [49].
This shift underlies the change from flexible, goal-directed actions to inflexible, automatic habits triggered by drug-associated stimuli [48] [49] [47].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Modeling Reward Conflict
| Reagent / Resource | Function & Application in Research |
|---|---|
| Outbred Rat Strains | Modeling individual vulnerability; only a subset develops compulsive phenotypes, mimicking the human population [49]. |
| Intravenous Catheters | Allows for chronic self-administration of drugs like cocaine, heroin, and methamphetamine [48] [46]. |
| Operant Conditioning Chambers | Standardized environments for measuring lever press or nose-poke operant responses for drug or natural rewards [48]. |
| Fast-Scan Cyclic Voltammetry (FSCV) | A technique for measuring real-time, phasic dopamine release (on a sub-second timescale) in structures like the NAcc during behavior [34]. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) & Optogenetics | Chemogenetic and optical tools for the reversible, cell-type-specific inhibition or stimulation of defined neural populations (e.g., PL cortex neurons) to establish causal roles in behavior [47]. |
| Second-Order Schedules | Complex reinforcement schedules used to study the conditioned reinforcing properties of drug-associated cues and dissociate seeking from taking [48]. |
| Progressive Ratio (PR) Schedules | Schedules used to measure the motivation or "craving" for a drug by determining the maximum effort (breakpoint) an animal will expend for a single infusion [46]. |
| Punishment Apparatus | Devices (e.g., grid floors for footshock delivery) for introducing adverse consequences to model compulsive use despite negative outcomes [46] [47]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Conditioned Place Preference (CPP)
Q1: Our CPP results are inconsistent between experiments. What are the key factors we should control for?
A: Inconsistent CPP can stem from several methodological variables. Key factors to control include [52] [53]:
- Apparatus Bias: Determine if you are using a biased (drug paired with initially least-preferred side) or unbiased (random compartment assignment) design. An unbiased design may fail to reveal a preference if animals have a strong innate bias, whereas a biased design can confound anxiolytic effects with genuine reward [52] [53].
- Species and Strain: Albino rats, for example, do not rely on visual cues as much as other strains. Ensure your contextual cues (tactile, olfactory) are appropriate for your species [52].
- Dose and Timing: The rewarding vs. aversive effects of a drug are often dose-dependent. Higher doses of a drug like nicotine can produce conditioned place aversion (CPA) instead of CPP. Furthermore, the drug must be administered so its peak effect coincides with exposure to the context [52] [53].
- Handling and Stress: Inconsistent or stressful handling of animals can weaken conditioning and introduce variability [53].
Q2: How can we determine if a lack of CPP indicates the drug is non-rewarding?
A: A lack of CPP does not automatically mean the drug is non-rewarding. Consider these troubleshooting points [52]:
- Insufficient Conditioning: Drugs with weaker rewarding properties may require more conditioning sessions to establish a CPP.
- Pharmacokinetics: Drugs with a slow onset or long duration of action are poor candidates for establishing CPP, as the temporal association between the drug's effects and the context is weak.
- Dose Selection: Test a range of doses. A drug may produce CPP at intermediate doses but not at low or high doses.
Q3: What is the relevance of CPP to human addiction, given the animal is passively receiving the drug?
A: While the passive administration is a limitation, CPP models the powerful role of Pavlovian conditioning in addiction. In humans, the specific environments where drugs are taken can themselves trigger craving and relapse. CPP directly models this phenomenon, where a previously neutral context becomes a conditioned stimulus that can elicit a conditioned response (e.g., approach, dopamine release in the nucleus accumbens) [52] [54]. Furthermore, humans have been shown to develop CPP for environments paired with therapeutic amphetamine use [53].
Behavioral Sensitization
Q4: We are unable to reliably induce locomotor sensitization. What could be going wrong?
A: The induction of behavioral sensitization is highly sensitive to the administration protocol [55] [56]:
- Intermittent Dosing: Sensitization requires repeated, intermittent administration of the drug. Continuous infusion or too-frequent administration often fails to produce sensitization and can lead to tolerance.
- Test Environment: Sensitization can be context-dependent. If animals are tested in an environment different from where they received the drug, the expression of sensitization may be attenuated.
- Drug Course: Ensure the drug challenge dose for testing expression is given after a sufficient withdrawal period (abstinence) and that the drug has rapid pharmacokinetics.
Q5: How is behavioral sensitization, which measures locomotion, relevant to compulsive drug seeking in humans?
A: Behavioral sensitization is at the core of the incentive-sensitization theory of addiction. It is not the locomotor activation itself that is directly translated, but the underlying neuroadaptations. The theory posits that repeated drug use sensitizes the mesolimbic dopamine system and its connected circuitry, leading to a hyper-reactivity to the drug and drug-associated cues. This neural hypersensitivity manifests in humans as heightened "drug wanting" or craving, making stimuli associated with the drug more salient and compelling, thereby contributing to compulsive seeking and relapse [20] [57].
Q6: Is behavioral sensitization reliably observed in humans?
A: The study of behavioral sensitization in humans is limited, but existing evidence suggests similar phenomena occur. Studies with oral d-amphetamine have shown that repeated, intermittent exposure can lead to progressive increases in subjective effects like euphoria and energy, as well as in drug-induced brain activation patterns [58] [55]. However, more research is needed to fully characterize this phenomenon in humans under ecological conditions [55].
Experimental Protocols
Detailed CPP Protocol
The CPP paradigm is a three-phase process designed to measure the rewarding or aversive properties of a stimulus by associating it with a distinct environment [52] [53] [54].
Table 1: Key Phases of the Conditioned Place Preference Protocol
| Phase | Purpose | Procedure | Key Considerations |
|---|---|---|---|
| 1. Habituation/Pre-Test | To establish a baseline preference and habituate the animal to the apparatus. | The animal is given free access to all compartments of the multi-chamber apparatus (typically for 5-15 minutes). The time spent in each compartment is recorded. | This data determines whether a biased or unbiased experimental design will be used [53]. |
| 2. Conditioning | To form an association between the drug (UCS) and a specific context (CS). | This phase consists of multiple sessions (often 8, each 5-60 min). On alternating days, the animal is:• Injected with the drug and confined to one compartment.• Injected with the vehicle and confined to the other compartment. | The compartments are often distinguished by visual, tactile, and olfactory cues. The order of drug/vehicle administration should be counterbalanced [52]. |
| 3. Post-Conditioning Test | To measure the strength of the learned association. | The animal is placed in the neutral/central area (if using a 3-compartment box) and given free access to all compartments in a drug-free state. The time spent in each compartment is recorded and compared to baseline. | A significant increase in time spent in the drug-paired compartment indicates CPP. A decrease indicates CPA [52]. |
The following workflow diagram illustrates the procedural sequence and key decision points in a CPP experiment:
Detailed Behavioral Sensitization Protocol
Behavioral sensitization refers to the progressive and persistent enhancement of certain behavioral responses (e.g., locomotion) following repeated, intermittent administration of a drug [55] [56].
Table 2: Key Phases of the Behavioral Sensitization Protocol
| Phase | Purpose | Procedure | Key Considerations |
|---|---|---|---|
| 1. Acquisition (Initiation) | To induce neuroadaptive changes through repeated drug exposure. | Animals receive daily, intermittent injections of the drug or vehicle for 5-10 days. Locomotor activity is measured immediately after each injection. | Intermittency is critical. Continuous administration may cause tolerance. The environment (same vs. different from test) can influence the strength of sensitization [55] [56]. |
| 2. Abstinence (Withdrawal) | To allow for the consolidation of neuroadaptations. | A drug-free period, which can last from a few days to several months. | This phase demonstrates the long-lasting nature of the changes induced during acquisition [55]. |
| 3. Expression (Challenge) | To reveal the sensitized response. | After the abstinence period, all animals receive a challenge injection of the drug (often at the same dose used in acquisition). Locomotor activity is measured and compared to the initial response. | Sensitized animals will show a significantly greater locomotor response to the challenge injection compared to controls and their own initial response [56]. |
The following diagram illustrates the multi-phase structure of a behavioral sensitization experiment and the underlying neural adaptations:
Signaling Pathways & Neurocircuitry
The development and expression of CPP and behavioral sensitization involve complex, overlapping neural circuits, primarily the mesocorticolimbic system.
Core Neurocircuitry of Reward and Sensitization
This diagram outlines the primary brain regions and connections implicated in these models, highlighting the distinct roles of the Ventral Tegmental Area (VTA) and Nucleus Accumbens (NAc) in the initiation and expression of plasticity.
Molecular Signaling in the Nucleus Accumbens
Upon dopamine and glutamate release in the NAc, intricate intracellular signaling cascades are activated, leading to long-term synaptic plasticity that underlies the persistent behavioral changes observed in both models.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for CPP and Behavioral Sensitization Research
| Item/Category | Function/Application | Specific Examples & Notes |
|---|---|---|
| Apparatus | Provides the distinct environments for conditioning and testing. | CPP: 2- or 3-compartment boxes with different walls, floors, and textures [52] [53]. Sensitization: Open fields, activity chambers, or photocell cages to quantify locomotion [55]. |
| Drug Agonists | To establish reward/sensitization and study receptor mechanisms. | Psychostimulants: Cocaine, Amphetamine, Nicotine [52] [55]. Opioids: Morphine, Heroin, Oxycodone [52] [31]. Others: Ethanol, Diazepam [52]. |
| Receptor Antagonists | To block specific receptors and probe their necessity in acquisition or expression. | Dopamine: SCH-23390 (D1), Haloperidol (D2) [52] [55]. Glutamate: MK-801 (NMDA), CNQX (AMPA) [55]. Opioid: Naloxone, Naltrexone (μ-opioid) [26] [31]. |
| Signal Transduction Modulators | To investigate intracellular pathways involved in neuroplasticity. | PKA inhibitors (e.g., Rp-cAMPS), PKC inhibitors, CREB antisense oligonucleotides. |
| Animal Models | Genetically defined subjects to study vulnerability and mechanisms. | Inbred Strains: C57BL/6J (high opioid preference), DBA/2J (low preference) [31]. Outbred Stocks: Sprague-Dawley, Wistar rats (model population variance) [31]. Transgenic/Knockout Mice: To study specific gene function [20]. |
Refining Compulsivity Assessment: Addressing Pitfalls and Enhancing Model Validity
Frequently Asked Questions (FAQs) for Troubleshooting Punishment Models
FAQ 1: Our conditioned suppression experiments are yielding inconsistent results. What are the most critical parameters to control for?
Answer: Inconsistent conditioned suppression often stems from inadequate optimization of the aversive stimulus. Key parameters to control and validate include [59]:
- Shock Intensity: Suppression of seeking behavior is proportional to footshock intensity. A higher intensity is typically required to suppress drug (e.g., cocaine) seeking compared to natural reward (e.g., sucrose) seeking.
- CS Presentation Sequence: The most pronounced conditioned suppression is observed when the test session begins with the presentation of the aversive conditioned stimulus (CS), rather than presenting it after a period of unreinforced seeking.
- Self-Administration History: The longevity of drug experience is a critical factor. Animals with an extended self-administration history show significantly reduced conditioned suppression, mirroring the compulsive drug use seen in human addiction.
FAQ 2: How can we distinguish between a habit and a goal-directed compulsion in punished drug-seeking?
Answer: This is a central challenge in the field. The behavior can be dissected by examining its sensitivity to outcome devaluation and the role of craving [60].
- Outcome Devaluation Tests: If drug seeking persists despite a devalued outcome (e.g., adulterating alcohol with quinine), it suggests habitual control. However, if seeking is sensitive to devaluation, it may remain goal-directed but be driven by an excessively high valuation of the drug.
- Integrating Craving Measures: Compulsivity in humans is characterized by both automaticity (habit) and conscious craving. A comprehensive model should therefore incorporate measures of craving (e.g., relapse tests, Pavlovian-instrumental transfer) alongside punishment resistance to capture the full spectrum of compulsive pathology [60].
FAQ 3: What are the limitations of using quinine adulteration to model insensitivity to negative consequences?
Answer: Quinine adulteration is a valid model, but it has specific limitations [59]:
- Taste-Specific: It primarily models consequences related to the drug's palatability, which may not generalize to other types of negative consequences like social or physical harm.
- Development of Resistance: Studies have shown that motivation for alcohol can become resistant to quinine adulteration after several months of intermittent self-administration. This highlights that the emergence of compulsivity is a time-dependent process, and short-term experiments may not capture it fully.
Troubleshooting Guide: Common Experimental Pitfalls and Solutions
| Problem | Possible Cause | Solution |
|---|---|---|
| No observed suppression of drug-seeking | Aversive stimulus (e.g., footshock) intensity is too low. | Systematically increase footshock intensity in different cohorts of animals to establish the minimum effective level for suppression [59]. |
| High variability in compulsive behavior between subjects | This is an expected and valid finding, reflecting individual vulnerability. | Pre-screen animals for traits like impulsivity or sign-tracking behavior, which are known to predict greater addiction liability, and stratify subjects into groups accordingly [61]. |
| Punished behavior extinguishes too quickly | The aversive contingency may be too effective, or the motivation for the drug is too low. | Use a longer-access self-administration protocol (Long Access, LgA) to escalate drug intake and motivation before introducing punishment [61]. |
| Difficulty interpreting if behavior is habitual or goal-directed | Lack of tests for outcome devaluation. | Incorporate a separate devaluation test (e.g., using quinine or lithium chloride pairing) to determine the underlying behavioral control mechanism [60]. |
Detailed Experimental Protocols
Protocol 1: Conditioned Suppression of Drug Seeking
This protocol uses a conditioned stimulus (CS) previously paired with footshock to suppress drug-seeking behavior [59].
Methodology:
- Training: Rats are trained to self-administer a drug (e.g., cocaine) or a natural reward (e.g., sucrose) in an operant chamber.
- Conditioning (Separate Sessions): In a distinct context, a neutral CS (e.g., a light+tone) is repeatedly paired with a mild footshock (e.g., 0.5 mA for 2-3 seconds). The intensity of the shock is critical and must be calibrated.
- Testing: Animals are returned to the operant chamber and allowed to seek the drug. During the seeking period, the aversive CS is presented. The degree of suppression in the rate of seeking responses during the CS is the primary measure.
- Key Parameters:
- Footshock Intensity: A higher intensity (e.g., 0.5 mA) is often needed for cocaine compared to sucrose (e.g., 0.25-0.35 mA).
- CS Sequence: Start the test session with the aversive CS to achieve the most robust suppression effect.
Protocol 2: Resistance to Aversion via Quinine Adulteration
This model tests the persistence of consumption when the drug itself is made aversive [59].
Methodology:
- Stable Baseline: Establish stable oral self-administration of a drug like alcohol.
- Adulteration: Adulterate the drug solution with a bitter tastant, quinine hydrochloride, at a concentration that would normally suppress consumption (e.g., 0.1-0.3 g/L).
- Measurement: Compare the volume of adulterated drug consumed to baseline levels. Resistance to devaluation is indicated by a smaller reduction in intake than observed in control animals.
- Critical Factor: The emergence of resistance is dependent on a long and intermittent history of drug use.
Table 1: Key Parameters for Conditioned Suppression Experiments [59]
| Parameter | Sucrose Seeking | Cocaine Seeking | Notes |
|---|---|---|---|
| Effective Footshock Intensity | 0.25 - 0.35 mA | 0.5 mA or higher | Intensity is more critical than the number of shocks. |
| Suppression Ratio (Limited History) | ~0.4 | ~0.4 | Lower ratio indicates greater suppression (0 = complete suppression). |
| Suppression Ratio (Extended History) | ~0.4 | ~0.6 | Extended cocaine history significantly reduces suppression, indicating compulsive-like behavior. |
| Seeking Latency (Extended History) | Unchanged | Increased | Animals with extended cocaine history initiate seeking faster despite the aversive CS. |
Table 2: Comparing Punishment Modalities
| Punishment Model | Type of Consequence | Face Validity | Key Limitation |
|---|---|---|---|
| Conditioned Suppression (Footshock CS) | Threat of Physical Harm | High for fear of consequences | Requires careful conditioning; measures seeking, not taking. |
| Quinine Adulteration | Directly Aversive Drug Effect | High for ignoring drug quality | Limited to orally consumed substances; models a specific type of consequence. |
| Contingent Footshock (Response-Cost) | Direct Physical Harm | High for physical risk | Can be overly effective, suppressing all behavior. |
Experimental Workflow and Logic Diagrams
Diagram 1: Core logic of punishment-based models of compulsion.
Diagram 2: Troubleshooting guide for weak punishment effects.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Punishment Experiments
| Item | Function in Experiment | Key Consideration |
|---|---|---|
| Operant Conditioning Chamber | The controlled environment for self-administration and punishment testing. | Must be equipped with cue lights, speakers, a drug infusion system, and a grid floor for footshock delivery. |
| Programmable Footshock Generator | Provides a precise and controllable aversive stimulus (unconditioned stimulus). | Calibration is critical; intensity (mA) and duration (ms) must be accurate and consistent. |
| Quinine Hydrochloride | Used to adulterate oral drugs like alcohol to create an directly aversive consequence. | Concentration must be titrated to be aversive but not completely suppress all fluid consumption. |
| Data Analysis Software | For calculating key metrics like suppression ratio and seeking latency. | The suppression ratio formula is: CS responding / (CS responding + pre-CS responding). A ratio of 0.5 indicates no suppression. |
Fundamental Concepts: Understanding the Core Confounds
Why is it essential to control for these specific confounds in studies of compulsive drug seeking? In animal models of substance use disorder, behaviors like drug self-administration and reinstatement are the primary outcome measures. However, these behaviors can be significantly influenced by underlying biological variables. Failure to control for them can lead to misinterpretation of a drug's motivational properties. The core confounds are:
- Pain Sensitivity: Changes in pain threshold can alter the perceived rewarding or aversive properties of a drug, directly impacting volitional drug intake [62].
- Learning Deficits: Compromised associative learning can impede the formation of context-drug or cue-drug memories, which are central to the development and expression of compulsive seeking [63].
- Altered Tastant Perception: Since tastants are often used as palatable rewards or in conditioned taste aversion paradigms, underlying differences in taste perception can confound the interpretation of reward valuation and learning [64] [65].
What are the key neural circuits where these confounds converge with reward pathways? The neural circuits governing reward, pain, learning, and taste processing share significant overlap. The table below summarizes the key brain regions involved.
Table 1: Key Brain Regions in Core Confounds and Reward Processing
| Brain Region | Role in Reward & Addiction | Role in Pain Modulation | Role in Learning & Memory | Role in Taste Processing |
|---|---|---|---|---|
| Ventral Tegmental Area (VTA) | Dopamine source for reward signaling [66] | Projects to pain modulatory regions [62] | - | - |
| Nucleus Accumbens (NAc) | Integration of reward and motivation [62] | Altered in chronic pain states [62] | - | - |
| Amygdala | Processes emotional salience of drug cues [62] | Modulates pain affect [62] | Critical for emotional memory (e.g., CTA) [64] | - |
| Prefrontal Cortex (PFC) | Executive control, regulates drug seeking [62] | Top-down pain modulation [62] | Decision-making, behavioral flexibility [63] | - |
| Insular Cortex | Interoception, drug craving [62] | Pain perception [62] | - | Primary gustatory cortex [64] |
| Parabrachial Nucleus | - | Relay for nociceptive information | - | Relay for gustatory and visceral information [64] |
Neural Circuit Convergence of Key Confounds
Troubleshooting Guides & FAQs
Section 1: Pain Sensitivity
FAQ: My animal model shows a high variance in drug self-administration. Could undetected differences in pain sensitivity be a factor? Yes. The neurobiological pathways of pain and reward are deeply intertwined, particularly within the mesolimbic dopamine system [62]. For instance, chronic pain states can alter dopamine release in the Nucleus Accumbens, potentially changing the perceived reward value of a drug and leading to increased or decreased self-administration that is not purely due to the drug's addictive properties [62].
Troubleshooting Guide: How to control for and assess pain sensitivity.
- Problem: Uncontrolled variability in pain thresholds confounds drug reward measurements.
- Solution: Implement standardized baseline pain sensitivity assays.
- Recommended Assay: Hargreaves Test (for cutaneous sensitivity) or Von Frey Filaments (for mechanical sensitivity).
- Protocol Outline:
- Acclimatize animals to the testing apparatus.
- Apply a standardized noxious stimulus (e.g., a radiant heat source for Hargreaves).
- Measure the latency to withdraw from the stimulus.
- Stratify experimental subjects into groups based on their baseline pain sensitivity to ensure balanced distribution across drug and control conditions. Do not exclude outliers without justification, as they may represent a valid biological phenotype.
Section 2: Learning Deficits
FAQ: After a chronic stress paradigm, my animals fail to reinstate drug-seeking behavior. Is this a protective effect or a learning impairment? This is a classic interpretation challenge. A failure to reinstate could indicate resilience, but it could also stem from stress-induced learning deficits or an inability to form or recall the associative memories between environmental cues and the drug [63]. You must disentangle motivation from capability.
Troubleshooting Guide: How to determine if learning deficits are confounding reinstatement behavior.
- Problem: Inability to distinguish impaired associative learning from reduced drug motivation.
- Solution: Implement a separate, drug-free learning assay.
- Recommended Assay: Fear Conditioning or Novel Object Recognition.
- Protocol Outline for Fear Conditioning:
- Training: Place animals in a novel chamber and present a neutral tone (Conditioned Stimulus, CS) followed by a mild foot shock (Unconditioned Stimulus, US).
- Testing (Context): 24 hours later, return animals to the same chamber and measure freezing behavior (a memory-dependent fear response) in the absence of the shock.
- Testing (Cue): Place animals in a novel context, present the tone (CS), and measure freezing.
- Interpretation: Animals that show deficits in freezing in both tests likely have generalized learning or memory impairments that could confound reinstatement tests. Intact learning in this paradigm strengthens the conclusion that changes in drug-seeking are motivation-specific.
Section 3: Altered Tastant Perception
FAQ: I use sucrose preference as a measure of anhedonia. What if my genetic animal model has an inherent, yet unknown, difference in taste perception? This is a critical consideration. A reduced sucrose preference is typically interpreted as anhedonia, or a reduced ability to feel pleasure. However, it could also be caused by a fundamental inability to perceive the sweet taste, which is a sensory deficit, not a motivational one [65]. This confound can lead to a false positive diagnosis of anhedonia.
Troubleshooting Guide: How to control for underlying differences in tastant perception.
- Problem: Inability to distinguish between a lack of pleasure (anhedonia) and a lack of perception (sensory deficit).
- Solution: Implement a taste discrimination or detection task.
- Recommended Assay: Two-bottle brief-access test (Davis Rig).
- Protocol Outline:
- Train water-deprived animals to drink from two spouts in a test chamber.
- Present a series of trials where one spout contains water and the other contains a sucrose solution of varying concentrations.
- Measure the animal's licking behavior and preference at each concentration.
- Interpretation: Animals with intact taste perception will show a concentration-dependent increase in sucrose licking. A flat response curve suggests an underlying sensory deficit. Animals that can discriminate the sucrose but do not increase consumption may truly be anhedonic.
Detailed Experimental Protocols
Protocol 1: Conditioned Taste Aversion (CTA) to Assess Drug Aversive Effects
Objective: To evaluate the aversive properties of a drug of abuse by pairing its administration with a novel taste and measuring subsequent taste avoidance [64]. This is crucial for interpreting the dual rewarding/aversive properties of drugs.
Workflow Diagram:
Conditioned Taste Aversion Workflow
Materials:
- Standard rodent housing cages
- Drinking bottles (1 or 2 per cage)
- 0.1% - 0.5% Sodium Saccharin solution
- Lithium Chloride (LiCl, 0.15M)
- Saline (for control injections)
Procedure [64]:
- Baseline (5-7 days): House animals with ad libitum food. Implement a water restriction schedule to create a stable daily water intake (e.g., 20-30 min access per day).
- Conditioning (1 day): On the conditioning day, replace the water bottle with a novel saccharin solution (CS). Allow access for 20 minutes. Record the amount consumed. Approximately 15-20 minutes after the end of access, administer an intraperitoneal injection of LiCl (0.15 M, at 2% of body weight) to induce gastrointestinal malaise (US). A control group should receive a saline injection.
- Recovery (1-2 days): Return to the baseline water restriction schedule.
- Testing (1 day): Present the saccharin solution again (in a one-bottle test or in a two-bottle choice with water). Measure the intake of both fluids. A significant reduction in saccharin intake in the LiCl group compared to the saline control group indicates a successful CTA.
Protocol 2: Chronic Unpredictable Mild Stress (CUMS) to Model Stress-Induced Learning Deficits
Objective: To induce a depression-like state in animals, which is often associated with learning impairments, in order to study its interaction with drug-seeking behavior [63].
Materials:
- Animal housing rooms
- Various stressors (e.g., damp bedding, tilted cages, stroboscopic light, white noise, period of food/water restriction)
Procedure [63]:
- Baseline Testing: Before starting CUMS, conduct baseline behavioral tests (e.g., sucrose preference, open field).
- Stress Regimen (3-8 weeks): Daily, expose the experimental group to 2-3 different mild stressors in an unpredictable sequence. The order should be randomized and not follow a pattern. Examples of stressors include:
- 45° cage tilt for 12 hours
- Damp bedding for 12 hours
- Intermittent white noise for 1 hour
- Stroboscopic lighting for 1 hour
- Periods of food or water deprivation (e.g., 12 hours)
- Control Group: The control group should be handled regularly but not subjected to the stressors.
- Post-Stress Testing: After the stress regimen, repeat the behavioral tests (sucrose preference, learning assays like fear conditioning) to confirm the induction of anhedonia and learning deficits.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Controlling Key Confounds
| Reagent | Function & Application | Key Consideration |
|---|---|---|
| Lithium Chloride (LiCl) | Unconditioned Stimulus (US) in Conditioned Taste Aversion (CTA) to create a visceral malaise association [64]. | Standard dose is 0.15M at 2% of body weight (i.p.); saline-injected controls are mandatory. |
| Saccharin / Sucrose | Conditioned Stimulus (CS) in CTA or for measuring reward/anhedonia via Sucrose Preference Test [64]. | Use a novel taste for CTA. For preference tests, control for tastant perception deficits as described in troubleshooting guides. |
| Von Frey Filaments | To assess mechanical pain sensitivity by applying calibrated forces to the paw and measuring withdrawal threshold. | Requires proper animal acclimation. Stratify groups based on baseline scores. |
| Carnosic Acid | A compound from rosemary extract that activates KCNQ3/5 proteins, dampening neuronal activity in addiction-related circuits [66]. | Emerging therapeutic; shown to reduce volitional cocaine intake in mice by modulating a specific dopamine subcircuit [66]. |
| Methadone / Buprenorphine | FDA-approved medications for Opioid Use Disorder (OUD); used as reference controls in relapse studies [67]. | In animal studies, they are used to validate models of opioid seeking and relapse. Their efficacy sets a benchmark for novel interventions. |
Frequently Asked Questions: Troubleshooting Animal Models of Compulsion
Q: My rodent subjects are not exhibiting compulsive drug-seeking despite long-access sessions. What could be the issue? A: Compulsion is not a guaranteed outcome of long-access self-administration. A majority of rodents may suppress drug intake when adverse consequences like footshocks are introduced (punishment-sensitive phenotype) [68]. To model the clinical reality of Substance Use Disorders (SUDs), your experimental design must be able to distinguish this group from the smaller, punishment-resistant subgroup that continues drug-seeking despite negative outcomes [68]. Ensure your protocol includes a phase where adverse consequences are contingently applied to identify this clinically relevant phenotype.
Q: What are the primary neurobiological correlates of the compulsive phenotype? A: Research indicates that punishment-resistant, compulsive drug-seeking is associated with substantial decreases in the intrinsic excitability of neurons in the prelimbic cortex, an area critical for cognitive control [68]. This prefrontal cortex hypoactivity is a key pathological feature observed in addicted populations and can be a target for intervention, as optogenetic stimulation of this region has been shown to decrease compulsive seeking [68].
Q: How can cognitive deficits be incorporated into my addiction model? A: Cognitive deficits are a recognized component of SUDs and vary according to the abused substance [68]. You can incorporate cognitive testing, such as assessments of executive function and decision-making, into your longitudinal study design. An important, yet often overlooked, research approach is to investigate whether these cognitive deficits precede the diagnosis of a SUD, which would help elucidate their role as either a cause or a consequence of addiction [68].
Q: Are there ways to improve the translational value of my preclinical model? A: Yes. Consider moving beyond models based solely on escalation of drug intake. The field is advancing towards dimensional approaches that represent specific symptom clusters observed in humans [68]. Furthermore, incorporating therapeutic interventions such as environmental enrichment (EE) or cognitive therapies in your animal models can provide valuable preclinical data on their efficacy for treating the cognitive aspects of SUDs [68].
Key Experimental Protocols
Protocol 1: Identifying Punishment-Resistant (Compulsive) Phenotypes
This protocol is designed to isolate the subset of subjects that best model the clinical diagnostic criterion of continued use despite adverse consequences [68].
- Objective: To differentiate punishment-sensitive from punishment-resistant animals following escalation of drug intake.
- Procedure:
- Self-Administration Training: Subjects are trained to self-administer a drug (e.g., cocaine or methamphetamine) [68].
- Long-Access Escalation: Subjects are given long-access (6-12 hours) to the drug to promote escalation of intake [68].
- Adverse Consequence Introduction: A contingent footshock is applied during self-administration sessions.
- Phenotype Classification:
- Punishment-Sensitive: Subjects that significantly suppress their drug intake.
- Punishment-Resistant: Subjects that continue to compulsively self-administer the drug [68].
- Key Measurements: Infusions per session, latency to resume drug-taking post-shock.
Protocol 2: Assessing Cognitive Deficits in Addiction Models
This protocol outlines a framework for evaluating cognitive function, a key domain impaired in SUDs [68].
- Objective: To characterize cognitive deficits in subjects with a history of drug exposure.
- Procedure:
- Baseline Cognitive Assessment: Perform pre-drug cognitive testing (e.g., attentional set-shifting, working memory tasks) to establish a baseline [68].
- Drug Exposure Phase: Proceed with the self-administration protocol (as in Protocol 1).
- Post-Drug Cognitive Assessment: Re-administer cognitive tests after the development of escalated or compulsive drug use.
- Correlation with Neural Markers: Ex vivo analysis of brain tissue (e.g., prelimbic cortex) can be conducted to correlate cognitive performance with neuropathological changes [68].
- Key Measurements: Performance accuracy in cognitive tasks, neural excitability in relevant brain regions.
Experimental Workflow and Signaling Pathway
The following diagram illustrates the logical workflow for modeling and interrogating compulsive drug-seeking behavior, integrating the key protocols above.
The Scientist's Toolkit: Key Research Reagent Solutions
The table below details essential materials and their functions for conducting research in this field.
| Item/Reagent | Function in Research |
|---|---|
| Punishment-Resistant Phenotype | The crucial subject group that continues drug-seeking despite adverse consequences (e.g., footshock), directly modeling the clinical DSM criterion for SUDs [68]. |
| Optogenetic Stimulation Apparatus | Used to experimentally increase activity in specific brain regions (e.g., the prelimbic cortex) to test causality and potential therapeutic reversal of compulsive drug-seeking [68]. |
| Cognitive Behavioral Tasks | A suite of tests (e.g., for executive function, decision-making) used to quantify the cognitive deficits that accompany SUDs and can be investigated in animal models [68]. |
| Environmental Enrichment (EE) | A therapeutic intervention used in animal models to investigate the potential beneficial effects of enhanced sensory, motor, and social stimulation on drug-seeking behaviors and cognitive function [68]. |
| Intracranial Self-Stimulation (ICSS) | A behavioral procedure used to assess brain reward function and the interplay between the rewarding effects of drugs and natural rewards, which is often dysregulated in addiction. |
In the study of substance use disorders (SUDs), preclinical research has traditionally relied on measures of persistent drug use despite adverse consequences, such as punishment, to model compulsive drug seeking [3]. While valuable, this approach provides an incomplete picture of the motivational conflict that is a core feature of addiction—the simultaneous experience of powerful urges to use a substance and equally powerful desires to abstain [69] [70].
This technical resource provides support for researchers aiming to incorporate sophisticated measurements of motivational conflict and response latency into their experimental designs. By moving beyond simple punishment-based models, these methods capture the internal struggle characterized by hesitation and vacillation, offering a more translationally valid approach to studying addiction [3] [71].
Troubleshooting Guides
Guide 1: Implementing the Runway Conflict Model
Problem: Researchers observe no significant latency differences between experimental and control groups in the runway conflict model, suggesting failure to induce measurable motivational conflict.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Insufficient motivation | Measure baseline running speeds for reward alone (no conflict). | Ensure appropriate food/water deprivation schedules; use higher-value rewards (e.g., higher sucrose concentration) [71]. |
| Aversive stimulus too intense or mild | Conduct separate tests of shock reactivity or taste aversion. | Calibrate shock intensity (e.g., 0.27-0.5 mA) or quinine concentration (e.g., 0.01%-0.05%) to create conflict, not complete suppression [3] [71]. |
| Poorly discriminated cues | Verify distinct cue conditions (light, sound) for reward vs. punishment. | Use highly distinct sensory cues (e.g., pure tone vs. white noise) and ensure reliable cue delivery before behavior measurement. |
| History of extended drug access | Review animal drug exposure history. | Utilize animals with chronic drug exposure that achieves clinically relevant intoxication levels, as this alters motivational processing [3]. |
Guide 2: Troubleshooting the Active Avoidance Runway Task
Problem: Inconsistent results in the Active Avoidance (AA) runway task, where cocaine-pre-exposed animals do not show the expected longer latencies to avoid shock.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Inadequate AA training | Check if >80% of trials show successful avoidance before runway test. | Extend training until stable avoidance is achieved; ensure shock intensity is sufficient to motivate avoidance (e.g., 0.27 mA) [71]. |
| Altered shock sensitivity | Test pain threshold responses in experimental vs. control animals. | Include control tests for baseline nociception; match shock levels to ensure equal perceived intensity across groups [3]. |
| General motor impairment | Measure run times in non-conflict reward-seeking scenarios. | Confirm that latency differences are conflict-specific and not due to drug-induced motor deficits. |
| Task disengagement | Monitor additional behaviors (aborted runs, freezing). | Use shorter session durations; ensure appropriate motivational state (e.g., not satiated) [71]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental advantage of measuring response latency over simple punishment resistance?
A: Response latency directly captures the hesitation and vacillation characteristic of motivational conflict, providing a dynamic measure of the decision-making process itself. Whereas simple punishment resistance only tells you that an animal continued drug seeking, latency measures can reveal how the animal deliberated between competing goals—approach versus avoidance—which more closely mirrors the human experience of addiction [69] [3] [71].
Q2: How can I determine if latency changes are due to motivational conflict versus general motor or cognitive impairment?
A: Implement a tiered testing protocol:
- First, establish baseline running speeds in a reward-only condition with no conflict
- Test motor coordination in a separate apparatus (e.g., rotarod)
- Compare latency increases specifically in the conflict condition versus neutral conditions Significant latency increases that are specific to the conflict condition suggest authentic motivational conflict rather than general impairment [71].
Q3: What neural circuits are most relevant to motivational conflict paradigms?
A: The critical circuitry involves:
- Orbitofrontal Cortex (OFC): Encodes expected value of rewards and is active during goal-directed decision making [70]
- Amygdala: Processes aversive stimuli and threat anticipation [72]
- Ventral Striatum: Integrates motivational signals during approach-avoidance conflicts
- Anterior Insular Cortex: Implicated in awareness of motivational conflict and negative states [73]
Q4: How do I design an experiment that distinguishes between goal-directed and compulsive drug seeking?
A: Utilize a multidimensional assessment approach that combines several measures:
- Drug vs. Non-Drug Choice: Animals choosing drugs over palatable food or social interaction demonstrates excessive drug value [73] [70]
- Response Latency in Conflict: Increased hesitation indicates active deliberation between competing goals
- Punishment Resistance: Continued use despite adverse consequences
- Economic Demand: Measuring willingness to "pay" for drugs under increasing costs
Animals showing both high drug choice and increased response latency demonstrate the conflict characteristic of goal-directed but problematic decision-making, rather than automatic habit-driven behavior [70].
The Scientist's Toolkit: Research Reagent Solutions
Key Materials for Motivational Conflict Research
| Item | Function/Application | Example Use |
|---|---|---|
| Modular Runway Apparatus | Straight alley maze with start box and goal compartment; allows measurement of traversal time | Active Avoidance Runway Task [71] |
| Programmable Shock Generator | Delivers calibrated footshock as aversive stimulus | Punishment contingency in conflict paradigms [73] [71] |
| Stimulus-Response Compatibility (SRC) Software | Measures automatic approach/avoidance tendencies using manikin figure | Assessing implicit cognitive biases in humans [69] |
| Quinine Hydrochloride | Aversive tastant added to drug solution in oral consumption models | Measuring persistence of consumption despite unpleasant taste [3] |
| Operant Conditioning Chambers | Standard self-administration setup with levers, cues, and drug delivery | Drug self-administration training prior to conflict testing [74] [73] |
| Approach-Avoidance Conflict (AAC) Task | Virtual human paradigm adapted from animal runway models | Translational studies of decision-making under conflict [72] |
Integrating measurements of motivational conflict and response latency represents a significant advancement in modeling the complexity of addictive behavior. These approaches capture the internal struggle that characterizes substance use disorders more effectively than punishment-based models alone. The methodologies outlined in this technical guide provide researchers with practical tools to implement these sophisticated paradigms, ultimately contributing to more translationally relevant models of addiction and potentially more effective treatment strategies that address the core conflict driving compulsive drug use.
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: Why is multidimensional phenotyping necessary when a single measure like "drug intake despite punishment" seems sufficient? A single measure, such as punished drug seeking, is insufficient to capture the full heterogeneity of addiction-like behaviors [3]. Relying on one metric can be confounded by other factors, such as reduced pain sensitivity or learning deficits, and fails to represent the complex clinical reality of substance use disorders [3]. Multidimensional profiling allows for the identification of distinct behavioral endophenotypes, which may respond differently to treatments, enabling a more precise and personalized research approach [75].
FAQ 2: What are the key principles for designing an effective multidimensional phenotyping study? A robust design requires [76] [77]:
- Defined Variables: Clearly identify independent (e.g., drug exposure history, genetic manipulation) and dependent variables (e.g., compulsive-like behavior, affective states, motivation).
- Testable Hypothesis: Formulate specific, testable hypotheses, such as "a history of chronic drug intoxication will increase compulsive-like behavior on three distinct operational measures."
- Controlled Experimental Treatments: Systematically manipulate your independent variable(s) while controlling for confounders like baseline nociceptive sensitivity [3].
- Proper Group Assignment: Use random assignment to treatment groups to minimize bias. Consider between-subjects designs for irreversible manipulations or within-subjects designs to reduce animal numbers.
- Validated Measurements: Ensure your methods for measuring dependent variables are reliable and valid. For example, use multiple tests to confirm an anxiety-like phenotype.
FAQ 3: My animal model shows high variability in compulsive-like behavior. Is this a problem? No, this heterogeneity is a feature, not a bug [78] [79]. Isogenic populations, even under controlled conditions, exhibit significant phenotypic variability [78]. Rather than averaging this out, your analysis should characterize this variation. Computational approaches like logistic regression or principal component analysis (PCA) can model how an ensemble of features differentiates subtle mutants from wild types, turning population variance into a source of discovery [78] [79].
FAQ 4: How can I troubleshoot an experiment where my positive control fails to show the expected phenotype? Follow a structured troubleshooting protocol [80] [81]:
- Repeat the experiment to rule out simple human error.
- Verify your controls to ensure the experimental setup is valid.
- Check equipment and reagents for proper function, calibration, and storage conditions. Reagents may have degraded or been from a bad batch.
- Change variables one at a time, starting with the simplest or most likely culprit (e.g., light settings on a microscope), and document every change meticulously [81].
Troubleshooting Guides
Problem: High variability in compulsive responding measures, making it difficult to classify individuals.
| Possible Cause | How to Diagnose | Solution |
|---|---|---|
| Insufficient sample size | Perform a power analysis on pilot data. | Increase the number of subjects to better capture population heterogeneity [78]. |
| Inadequate operational definition of "compulsion" | Review literature; ensure the measure (e.g., resistance to punishment) aligns with the theoretical construct [3]. | Implement multiple, concurrent behavioral measures (see Table 1) to create a composite phenotype profile [78] [3]. |
| Uncontrolled confounding variable | Review protocol for variables like time of day, handler, or room humidity. | Standardize all environmental and procedural factors. Use randomization and blocking in experimental design [76]. |
| Learned resistance to punishment | Test baseline sensitivity to the aversive stimulus (e.g., footshock) in a separate cohort [3]. | Ensure the aversive stimulus retains its salience throughout the experiment; consider varying its intensity. |
Problem: A new therapeutic shows efficacy in one phenotypic subgroup but not the overall population.
| Possible Cause | How to Diagnose | Solution |
|---|---|---|
| Underlying neurobiological heterogeneity | Use computational models (e.g., reinforcement learning) to simulate different endophenotypes and their response to treatment [75]. | Re-analyze data by clustering subjects based on pre-treatment multidimensional profiling. Treatment effects may be specific to a distinct endophenotype [75] [79]. |
| Treatment only targets one neural circuit | Review neuroanatomical and pharmacological data on the therapeutic's mechanism of action. | The balance between ventral (goal-directed) and dorsal (habitual) cortico-striatal circuits dictates treatment response [75]. Develop a combination therapy that targets multiple circuits. |
Quantitative Data and Experimental Protocols
Table 1: Core Behavioral Dimensions for Multidimensional Phenotyping in Rodent Models
This table outlines key domains and specific measures for characterizing individual differences in addiction models [75] [3].
| Phenotypic Domain | Specific Behavioral Measure | Operational Definition | Key Consideration |
|---|---|---|---|
| Compulsive-Like Behavior | Punishment Resistance | Continued drug self-administration despite contingent footshock or bitter tastant (quinine) adulteration. | Must rule out alternative explanations like decreased shock sensitivity or taste perception [3]. |
| Effort Expenditure | Maximal price (e.g., lever presses) an animal will pay to obtain a drug infusion on a progressive ratio schedule. | Distinguishes high motivation from compulsive habit. | |
| Motivational Drive | Escalation of Intake | Increased drug consumption over time in long-access (LgA) self-administration sessions. | Models the transition from controlled to dysregulated use. |
| Negative Affect | Withdrawal Signs | Somatic signs (e.g., tremors) and affective signs (e.g., elevated intracranial self-stimulation thresholds) following drug abstinence. | Measures the negative reinforcement drive. |
| Cognitive Function | Impulsivity | Performance on the 5-choice serial reaction time task (5-CSRTT) or delay discounting task. | A known vulnerability trait for addiction. |
| Habit Formation | Outcome Devaluation | Assessing whether drug-seeking behavior is insensitive to devaluation of the drug outcome (e.g., by satiation or pairing with lithium chloride). | Indicates a shift from goal-directed to habitual behavior. |
Table 2: Contrasting Simulated Endophenotypes Based on Cortico-Striatal Balance
This table summarizes data from a computational study showing how different neural starting states (endophenotypes) lead to distinct phenotypic outcomes and treatment responses [75].
| Endophenotype | Neural / Algorithmic Bias | Predicted Phenotype (Addiction Severity) | Response to Simulated Treatment A (e.g., Goal-Directed System Enhancer) |
|---|---|---|---|
| Ventral-Dominant | Over-reliance on ventral, model-based, goal-directed system. | High likelihood of developing addiction, severe drug-taking. | Poor response. May even exacerbate behavior due to increased planning for drug reward. |
| Dorsal-Dominant | Over-reliance on dorsal, model-free, habitual system. | High likelihood of developing addiction, severe drug-taking. | Good response. Reduces automaticity of drug-seeking habits. |
| Balanced | Equal contribution of ventral/model-based and dorsal/model-free systems. | Lower likelihood and severity of addiction. | Not applicable (less vulnerable). |
Experimental Protocol: Multidimensional Screening for Compulsive-Like Phenotypes
Objective: To identify and characterize distinct subpopulations of animals exhibiting addiction-like behaviors across multiple operational dimensions.
Materials:
- Standard rodent operant chambers for self-administration.
- Equipment for delivering aversive stimuli (e.g., footshock generators).
- Solutions: Drug of interest (e.g., cocaine), saline, quinine solution.
Methodology:
- Chronic Drug Exposure: Subject animals to extended access (e.g., 6-12 hours daily) to intravenous drug self-administration for several weeks to establish dependence and intoxication history [3].
- Behavioral Battery: After stabilization, sequentially or concurrently assess animals on the following:
- Punishment Resistance Test: Introduce a mild footshock contingent upon drug-seeking. The intensity is titrated to suppress behavior in a subset, but not all, animals. Record the number of infusions earned despite punishment [3].
- Progressive Ratio Test: Replace the fixed-ratio schedule with a progressive ratio schedule where the response requirement for each subsequent infusion increases. The final ratio completed (break point) is recorded as a measure of motivation [75].
- Affective State Assessment: Following 24-48 hours of abstinence, measure anxiety-like behavior on an elevated plus maze or measure anhedonia via sucrose preference test.
- Data Integration: Use multivariate statistics (e.g., PCA, cluster analysis) on the data from all measures to identify clusters of animals with similar phenotypic profiles [78] [79].
Signaling Pathways and Workflows
Computational Framework for Phenotype Variation
Multidimensional Phenotyping Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material / Resource | Function in Multidimensional Phenotyping |
|---|---|
| Operant Conditioning Chambers | The core apparatus for administering self-administration protocols, delivering aversive stimuli (footshock), and measuring precise behavioral outputs (lever presses, nose pokes). |
| Positive Control Compounds | Pharmacological agents with known efficacy (e.g., Naltrexone for alcohol) used to validate the sensitivity of your behavioral assays and as a benchmark for testing new therapeutics. |
| Aversive Stimuli (Footshock, Quinine) | Critical for operationalizing the "continued use despite adverse consequences" dimension of compulsive-like behavior [3]. |
| Data Analysis Software (R, Python) | Essential for performing advanced multivariate statistics like Principal Component Analysis (PCA) and cluster analysis to define phenotypic groups from high-dimensional data [78] [79]. |
| Computational Models (RL Models) | Used to simulate neural dynamics and algorithmic choice selection, helping to formalize hypotheses about how different endophenotypes (e.g., model-based vs. model-free dominance) lead to observed behaviors [75]. |
Measuring Success: Biomarker Discovery, Predictive Validity, and Translational Gaps
Substance use disorder (SUD) is a heterogeneous medical condition characterized by impaired control over substance use despite adverse consequences [82]. A core challenge in addiction research is the phenomenological heterogeneity that defines diagnostic categories; a single SUD diagnosis likely encompasses numerous biologically distinct entities, as it requires any combination of at least two of 11 diagnostic criteria [82]. This heterogeneity has significantly impeded treatment development, as pharmaceutical compounds with specific mechanisms of action may only be relevant to a subset of patients within a diagnostic category [82].
To address this complexity, the field has increasingly turned to neuroscience-based frameworks like the National Institute of Mental Health's Research Domain Criteria (RDoC) and the Alcohol Addiction RDoC (AARDoC) [82]. These approaches aim to parse heterogeneity by focusing on transdiagnostic behavioral assays that are translatable and biologically informative. Similarly, the Addictions Neuroclinical Assessment (ANA) captures information across three core neurofunctional domains—incentive salience, negative emotionality, and executive (dys)function—to better understand addiction heterogeneity [82]. This technical support center provides troubleshooting guidance for researchers working with animal models designed to capture these complex human addiction phenotypes, with a specific focus on face validity assessment.
Troubleshooting Guides: Addressing Common Experimental Challenges
Guide: Low Face Validity in Compulsive Seeking Measures
Problem: Animals show limited compulsive drug-seeking despite adverse consequences, failing to mimic a core human addiction phenotype.
Affected Environments: Rat and mouse self-administration paradigms using footshock punishment, quinine adulteration, or progressive ratio schedules.
| Possible Cause | Diagnostic Questions | Solution Path |
|---|---|---|
| Insufficient drug exposure | - How many sessions has the animal completed?- Is intake stable or escalating? | Implement Long Access (LgA) or Intermittent Access (IntA) protocols to promote escalation [61]. |
| Inadequate negative consequence | - Is the punishment sufficient to suppress natural behaviors?- Are consequences predictable? | Calibrate footshock to a level that suppresses natural reward seeking but does not cause freezing. Use unpredictable punishment schedules [61]. |
| Wrong animal population | - Are you using outbred strains without screening?- Is individual variability being analyzed? | Use high-responder models or screen for innate traits like high impulsivity or sign-tracking that predict vulnerability [61]. |
Guide: Poor Translation to Human Relapse Behavior
Problem: Reinstatement models fail to produce robust and reliable drug-seeking behavior, limiting predictive validity for human relapse.
Affected Environments: Rodent reinstatement paradigms testing cue-induced, stress-induced, or drug-primed relapse.
| Possible Cause | Diagnostic Questions | Solution Path |
|---|---|---|
| Weak cue association | - Were cues consistently paired with every drug infusion?- Was the conditioning period long enough? | Ensure consistent cue-drug pairing across all training sessions. Extend training to strengthen associations [61]. |
| Insufficient extinction | - Has responding stabilized at a low level?- Is there high day-to-day variability in responding? | Continue extinction sessions until responding is stable and low. Do not proceed based on a fixed session number alone. |
| Stress paradigm mismatch | - Does the stressor induce a robust physiological response? | For stress-induced reinstatement, validate that the chosen stressor (e.g., forced swim, footshock) reliably increases corticosterone levels in your lab [61]. |
Experimental Protocols: Core Methodologies for Addiction Modeling
Long Access (LgA) Self-Administration Protocol
Purpose: To model the escalation of drug intake and transition to compulsive use observed in human addiction [61].
- Animals: Typically adult male rats (e.g., Sprague-Dawley).
- Apparatus: Standard operant conditioning chambers equipped with two levers (active and inactive), a cue light, and an intravenous drug delivery system.
- Training:
- Acquisition (1-2 weeks): Train animals on a Fixed-Ratio 1 (FR1) schedule of reinforcement during short (1-3 hour) sessions. Each press on the active lever results in a drug infusion (e.g., 0.1 mg/kg/infusion cocaine) paired with a discrete cue light.
- Stable Baseline: Continue until the number of infusions per session stabilizes (less than 20% variation over 3 consecutive days).
- Escalation Phase (LgA; ≥2 weeks):
- Divide animals into two groups: Short Access (ShA, 1-hour sessions) and Long Access (LgA, 6-hour sessions).
- Conduct sessions daily. The LgA group will typically show a progressive increase in drug intake, especially during the first hour of the session, indicating escalation.
- Key Outcome Measures:
- Number of infusions per session (escalation curve).
- Drug intake during the first hour vs. subsequent hours.
- Motivation for drug (assessed via progressive ratio breakpoint).
Conditioned Place Preference (CPP) Protocol
Purpose: To assess the rewarding or aversive properties of a drug by measuring an animal's preference for an environment previously paired with drug exposure [61].
- Animals: Mice or rats.
- Apparatus: A box with two or more distinct compartments differing in visual, tactile, and sometimes olfactory cues.
- Procedure:
- Pre-Test (Day 1): Place the drug-naïve animal in the neutral central area and allow it to freely explore all compartments for 15-20 minutes. Time spent in each compartment is recorded. Animals with a strong innate preference (>80% time in one side) are excluded.
- Conditioning (Days 2-9): This phase consists of 8 sessions (4 drug-paired, 4 vehicle-paired).
- On drug-pairing days, administer the drug (e.g., morphine) and confine the animal to one compartment for 30-40 minutes.
- On alternate days, administer vehicle and confine the animal to the other compartment.
- Post-Test (Day 10): Conducted exactly like the pre-test, with the animal drug-free. The time spent in the drug-paired compartment is compared to the pre-test.
- Key Outcome Measure:
- CPP Score: The difference in time spent in the drug-paired compartment during the post-test versus the pre-test. A significant increase indicates a rewarding effect.
Research Framework and Experimental Workflow
The following diagram illustrates the conceptual relationship between major research frameworks and the progression of a typical animal experiment designed to model human addiction.
The Scientist's Toolkit: Key Reagents and Materials
Table: Essential Research Reagents for Addiction Phenotyping
| Item | Function/Application | Key Considerations |
|---|---|---|
| Cocaine HCl | Prototypical psychostimulant for self-administration studies. | Dose range: 0.1-1.0 mg/kg/infusion (rat IV). Maintain stable pH in solution [61]. |
| Morphine Sulfate | Prototypical opioid for CPP and self-administration. | Conditioning dose: 5-10 mg/kg (mouse/sc). Watch for strain-dependent sensitivity. |
| Operant Chambers | Controlled environment for behavioral testing (SA, reinstatement). | Ensure reliable cue lights, sound generators, and fluid/swivel systems to prevent data loss. |
| Osmotic Minipumps | For chronic, non-contingent drug delivery or antagonist testing. | Match pump flow rate and drug concentration to desired daily dose and animal size. |
| Video Tracking System | Automated analysis of locomotor activity (sensitization) and place preference. | Essential for objective, high-throughput behavioral scoring. Validate against manual scoring. |
Frequently Asked Questions (FAQs)
Q1: What is the single most important factor for improving face validity in my addiction model? A1: There is no single factor, but a combination is crucial. The most impactful approach is using contingent drug administration (self-administration) over non-contingent models, coupled with extended access (LgA) to promote escalation and the use of vulnerable animal populations (e.g., high-impulsive subgroups) to model individual differences seen in humans [61].
Q2: My CPP experiment failed; animals showed no preference. What went wrong? A2: Common reasons for failed CPP include:
- Dosing: The drug dose may be too low (no reward) or too high (aversive). Run a full dose-response curve.
- Conditioning Parameters: The number or duration of conditioning sessions may be insufficient.
- Apparatus Bias: A strong, un-counterbalanced innate bias in the pre-test can mask a CPP effect. Use an unbiased or fully counterbalanced design.
- Strain/Species: Check literature for your specific animal strain's response to the drug [61].
Q3: How do I best model the transition from recreational use to addiction in a rodent? A3: The transition is best modeled by moving beyond simple drug intake to measure symptoms of addiction. This includes assessing: 1) Escalation of intake (LgA vs. ShA), 2) Motivation (progressive ratio breakpoint), 3) Persistence despite negative consequences (punished seeking), and 4) Relapse vulnerability (reinstatement) [61]. No single test captures the transition; a battery is required.
Q4: Can animal models truly capture the complexity of human addiction, which involves social and environmental factors? A4: While no model is perfect, newer paradigms are incorporating these factors. For example, social defeat stress is used to model environmental adversity, and choice paradigms between drugs and alternative rewards like social interaction or saccharin are being developed to model competing motivations, greatly improving face validity [61].
Q5: How are the ANA domains (Incentive Salience, Negative Emotionality, Executive Function) operationalized in animal tests? A5:
- Incentive Salience: Measured by sign-tracking behavior, cue-induced reinstatement of drug-seeking, and drug-primed reinstatement [82] [61].
- Negative Emotionality: Assessed by measures of anxiety-like behaviors (elevated plus maze), response to stress, and stress-induced reinstatement of drug-seeking [82].
- Executive Function: Evaluated using tests of impulsivity (5-choice serial reaction time task) and cognitive flexibility (attentional set-shifting) [82].
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the advantage of using hair follicles over brain tissue for transcriptomic analysis in addiction models? A1: Hair follicles provide a minimally invasive source for comprehensive transcriptomic biomarker discovery. They reflect systemic physiological adaptations and contain biomarkers for processes like energy metabolism, cell proliferation, and cytokine interactions, which are also relevant to brain function. This allows for repeated sampling in longitudinal studies without terminal procedures, facilitating the monitoring of molecular responses over time [83].
Q2: My RNA sequencing data from rodent hair follicles shows high variability after drug exposure. What could be the cause? A2: High variability can stem from several factors:
- Hair Cycle Asynchronization: Hair follicles undergo dynamic growth (anagen), regression (catagen), and resting (telogen) phases, each with distinct transcriptional programs [84]. Ensure you note the specific stage or use methods like single-cell RNA sequencing to deconvolute these cellular states.
- Sample Collection Timing: Molecular responses are dynamic. Inconsistent timing between drug administration and sample collection can capture different phases of the transcriptional response.
- Drug Administration Paradigm: The method of drug exposure (e.g., contingent vs. non-contingent) can produce different transcriptional outcomes. Self-administration models often have higher face validity for addiction behaviors [26] [20].
Q3: How can I validate that molecular changes in peripheral tissues like hair follicles are relevant to brain pathology in addiction? A3: Employ an integrated multi-omics approach. Correlate transcriptomic or proteomic findings from hair follicles with data from brain tissue in the same animal model. For instance, identify differentially expressed genes (DEGs) or proteins (DEPs) that are consistently altered in both tissues. Pathway enrichment analysis (e.g., KEGG, GO) can then reveal if these shared molecules converge on common pathways, such as inflammation or synaptic plasticity, validating their systemic and brain relevance [85] [86].
Q4: What are the key signaling pathways identified by transcriptomics in addiction-related studies? A4: Omics studies frequently implicate several key pathways. In hair follicle transcriptome analysis upon high-intensity interval training, pathways like phosphatidylinositide 3-kinases (PI3K) – protein kinase B (PKB) and Janus kinase (JAK) – Signal Transducer and Activator of Transcription (STAT) were over-represented [83]. In brain tissue studies of addiction and related disorders, pathways involving inflammation, cytokine-cytokine interaction, and G-protein-mediated signal transduction are commonly identified [83] [86] [87].
Q5: We are considering single-cell RNA sequencing. What insights can it provide for hair follicle analysis in our research? A5: Single-cell RNA sequencing (scRNA-seq) is transformative for heterogeneous tissues. It can:
- Identify Specific Cellular Contributors: Resolve different cell populations (e.g., follicular keratinocytes, dermal sheath fibroblasts, stem cells) and pinpoint which ones drive the observed transcriptomic changes during the hair cycle or in response to drug exposure [84].
- Reconstruct Cellular Interactions: Reveal cell-cell communication networks that are crucial for tissue remodeling and function, which may be dysregulated in disease states [84].
Troubleshooting Common Experimental Issues
Issue: Low RNA Yield or Quality from Hair Follicles
- Cause: Improper dissection or preservation. The hair follicle bulb, which is rich in RNA, must be intact.
- Solution: Pluck follicles carefully to include the root sheath. Immediately place samples in RNA stabilization solution (e.g., RNAlater) and store at -80°C. Use a dedicated micro-scale RNA extraction kit [83].
Issue: Poor Correlation Between Transcriptomic and Proteomic Data
- Cause: Biological discordance due to post-transcriptional regulation, or technical differences in platform sensitivity.
- Solution: This is a common challenge. Focus on integrated analysis rather than expecting a 1:1 match. Use robust statistical thresholds for both datasets and prioritize overlapping DEGs/DEPs for functional validation. Techniques like data-independent acquisition (DIA) mass spectrometry can improve proteomic depth [86].
Issue: High Background in Animal Models Due to Stress from Drug Administration
- Cause: Experimenter-administered (non-contingent) drug injection can induce stress, confounding transcriptomic profiles.
- Solution: Where possible, use contingent models like drug self-administration. These models have excellent face and predictive validity, as the animal controls drug intake, more closely mimicking human drug-taking behavior and yielding cleaner molecular data [26] [20].
Summarized Quantitative Data
Table 1: Key Transcriptomic and Proteomic Findings from Select Studies
| Study Focus / Model | Tissue Analyzed | Omics Method | Key Quantitative Finding (DEGs/DEPs) | Enriched Pathways / Key Biomarkers |
|---|---|---|---|---|
| High-Intensity Interval Training [83] | Human Hair Follicle | RNA-Seq | Identification of differentially expressed protein-coding genes and miRNAs | Energy metabolism, PI3K-PKB signaling, JAK-STAT signaling, miR-99a |
| Ischemic Stroke [85] | Mouse Heart, Spleen, Intestine | Proteomics | Heart: Highest number of DEPs; 10 DEPs shared across 3 organs | Complement/coagulation cascades, metabolic processes, accelerated biological aging |
| Alzheimer's Disease (APP/PS1 mouse) [86] | Mouse Hippocampus | Transcriptomics & DIA Proteomics | 263 DEGs, 448 DEPs; 5 co-upregulated and 1 co-downregulated DEG/DEP | Complement/coagulation cascade, neurodegeneration; APP, LY86, CD180, C1QB as potential targets |
| Androgenetic Alopecia [88] | Human Hair Follicle | Genomics, Transcriptomics | 107 DEGs via microarray; 32 DEGs via RNA-Seq | Wnt signaling, TGF signaling, Notch signaling, IL-17 pathways, cell cycle proteins |
| Sepsis Subtyping [87] | Human Blood | Transcriptomics (Microarray/RNA-Seq) | 18-gene classifier panel for consensus transcriptomic subtypes (CTS) | CTS1: Inflammatory/neutrophil; CTS2: Heme metabolism/platelet; CTS3: Interferon/lymphocyte |
Experimental Protocols
Protocol 1: Hair Follicle Collection and RNA-Seq for Longitudinal Studies
Application: Tracking molecular adaptations to chronic drug exposure in rodent models. Materials: Fine forceps, RNAlater, RNeasy Micro Kit, sonicator, NanoDrop spectrophotometer [83].
- Sample Collection: At each time point (e.g., pre-exposure, during maintenance, post-withdrawal), gently pluck approximately 10 hair follicles from the vertex scalp region of the rodent using fine forceps. Ensure the follicular bulb is intact.
- Sample Preservation: Immediately place follicles in RNAlater solution and store at -80°C until batch processing.
- RNA Extraction:
- Homogenize samples in a buffer using a sonicator.
- Extract and purify total RNA using a silica-membrane spin column kit (e.g., RNeasy Micro Kit).
- Determine RNA concentration and purity (A260/A280 ratio >1.8) using a spectrophotometer. Assess RNA integrity (RIN > 8) with a bioanalyzer if possible.
- Library Preparation and Sequencing:
- Use 1 µg of total RNA for library preparation. Enrich for polyadenylated mRNA using oligo(dT)-coupled magnetic beads.
- Fragment RNA, synthesize cDNA, and ligate with adapters.
- Perform size selection and amplify the library.
- Sequence on a platform such as Illumina NovaSeq (e.g., PE150).
- Bioinformatic Analysis:
- Quality control of raw reads (e.g., with fastp).
- Align clean reads to a reference genome (e.g., HISAT2).
- Assemble transcripts and estimate abundance (e.g., StringTie).
- Identify differentially expressed genes (DEGs) using software that applies thresholds like \|log2FC\| > 1.0 and adjusted p-value < 0.05 [83] [86].
Protocol 2: Integrated Transcriptomic and Proteomic Analysis of Brain Tissue
Application: Deep phenotyping of neuropathology in addiction or related brain disease models. Materials: TRIzol, Agilent Bioanalyzer, BCA assay kit, trypsin, triethylammonium bicarbonate (TEAB), mass spectrometer [86].
Part A: Transcriptomic Analysis
- Tissue Homogenization: Homogenize snap-frozen brain tissue (e.g., hippocampus/prefrontal cortex) in TRIzol reagent to isolate total RNA.
- RNA QC and Library Prep: Evaluate RNA integrity. Construct sequencing libraries from high-quality RNA using a stranded mRNA prep kit.
- Sequencing and DEG Calling: Perform high-throughput sequencing and bioinformatic analysis as described in Protocol 1 to identify DEGs.
Part B: DIA Proteomic Analysis
- Protein Extraction and Digestion: Lyse tissue in protein lysis buffer. Determine protein concentration with a BCA assay. Reduce, alkylate, and digest proteins (e.g., with trypsin) into peptides.
- Peptide Clean-up: Desalt digested peptides using a solid-phase extraction column.
- Liquid Chromatography and Mass Spectrometry:
- Separate peptides using liquid chromatography (e.g., nano-LC).
- Analyze eluted peptides using a mass spectrometer in Data-Independent Acquisition (DIA) mode.
- Proteomic Data Analysis: Process DIA data with specialized software (e.g., Spectronaut) to identify and quantify proteins. Define DEPs using criteria such as fold change ≥ 1.2 and p-value < 0.05 [86].
Part C: Integrative Analysis
- Correlate lists of DEGs and DEPs to find overlapping molecules.
- Perform pathway enrichment analysis (KEGG, GO) on the combined dataset to identify key dysregulated biological processes.
Signaling Pathways and Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Transcriptomic and Omics Biomarker Discovery
| Item | Function / Application | Example Products / Kits |
|---|---|---|
| RNA Stabilization Solution | Preserves RNA integrity in freshly collected tissues (hair follicles, brain) during storage and transport. | RNAlater [83] |
| Micro-Scale RNA Extraction Kit | Isolves high-quality total RNA from small, precious samples like a few hair follicles or brain micropunches. | RNeasy Micro Kit [83] |
| RNA Quality Assessment Tools | Accurately determines RNA concentration and assesses integrity (RIN) prior to sequencing. | NanoDrop Spectrophotometer, Agilent Bioanalyzer [83] [86] |
| Stranded mRNA Library Prep Kit | Prepares sequencing libraries from total RNA, enriching for polyadenylated mRNA transcripts. | Illumina Stranded mRNA Prep [86] |
| Mass Spectrometry-Grade Trypsin | Digests proteins into peptides for subsequent liquid chromatography-mass spectrometry (LC-MS/MS) analysis. | Sequencing-grade trypsin [86] |
| Triethylammonium Bicarbonate (TEAB) | Buffer used in proteomic sample preparation for digesting and solubilizing peptides. | TEAB Buffer [86] |
| Data-Independent Acquisition (DIA) Software | Analyzes complex DIA mass spectrometry data for comprehensive protein identification and quantification. | Spectronaut [86] |
Troubleshooting Guides and FAQs
Q1: Our experiments with the delta opioid agonist SNC80 show diminishing analgesic effects over time. What are the potential mechanisms and how can we address this?
A1: Diminishing effects are likely due to tolerance. The mechanism depends on the specific agonist used:
- For internalizing agonists like SNC80: Chronic administration induces robust receptor internalization and degradation via lysosomal pathways, leading to widespread behavioral tolerance [89].
- For non-internalizing agonists like ARM390: Tolerance can still occur through receptor internalization-independent mechanisms, potentially specific to pain pathways, without widespread receptor loss [89].
- Troubleshooting Steps:
- Characterize the Agonist: Determine if your therapeutic candidate induces receptor internalization using live-cell imaging or similar techniques.
- Explore Alternative Agonists: Consider switching to a non-internalizing agonist (e.g., ARM390) or novel compounds reported to have a lower tolerance liability (e.g., JNJ-20788560, SB-235863) [89].
- Adjust Dosing Schedule: Investigate intermittent dosing regimens to allow for receptor recovery if internalization is observed.
Q2: How can we behaviorally distinguish between goal-directed drug seeking and compulsive drug seeking in our animal models?
A2: The transition from goal-directed to compulsive seeking is a core feature of addiction modeling. You can distinguish them using behavioral paradigms:
- Devaluation Procedures: Test if the seeking behavior is sensitive to outcome devaluation. In a goal-directed state, animals will reduce drug-seeking when the value of the drug outcome is decreased (e.g., by pairing it with a malaise-inducing agent). In a habitual/compulsive state, seeking persists despite devaluation [48] [49].
- Second-Order Schedules of Reinforcement: These schedules are used to maintain seeking behavior over prolonged periods and are highly dependent on drug-associated conditioned stimuli. Well-established performance on these schedules is indicative of habitual behavior [48] [49].
- Compulsion-Assessed Tests: Measure the persistence of drug seeking despite the presentation of an aversive consequence, such as a footshock. Resistance to punishment is a key indicator of compulsion [49].
Q3: What neural circuits should we target to validate the efficacy of a therapeutic aimed at reducing compulsive seeking?
A3: The transition to compulsion involves a shift in neural circuit control:
- Ventral to Dorsal Striatum Shift: Early, goal-directed drug seeking depends on the ventral striatum (nucleus accumbens core) and its afferents from the basolateral amygdala. Compulsive habits are mediated by the dorsolateral striatum [49] [90].
- Loss of Prefrontal Control: The emergence of compulsivity also reflects a loss of inhibitory control from the prefrontal cortex over established drug-seeking habits [48] [90].
- Validation Strategy: A therapeutic effective against compulsion should normalize activity or neurotransmission within the dorsolateral striatum and/or enhance prefrontal cortical inhibitory function.
Q4: We are observing convulsant effects with some delta opioid agonists. Is this a class-wide effect and how can it be managed?
A4: Convulsions are a known effect of some delta opioid agonists, but not all.
- Agonist-Specific Effect: The agonist SNC80 is associated with mild, absence-like seizures. This effect is not necessarily representative of the entire class [89].
- Management Strategies:
- Select Alternative Agonists: Consider agonists that may have a better safety profile.
- Dose Titration: Carefully determine the therapeutic window where beneficial effects are observed without proconvulsant side effects.
- Pharmacological Control: SNC80-induced seizures can be prevented by drugs used to treat absence seizures in humans [89].
Experimental Protocols for Key Assays
Protocol 1: Assessing Compulsive Drug Seeking Using Punishment Resistance
Objective: To determine the effectiveness of a delta opioid receptor therapeutic in reducing compulsive cocaine seeking.
Materials:
- Animal model: Rats trained to self-administer cocaine.
- Test compound: Delta opioid receptor agonist/antagonist.
- Apparatus: Operant conditioning chambers.
Methodology:
- Training: Train rats to self-administer cocaine on a second-order schedule of reinforcement (e.g., FR15 (S:HR10)) to establish robust drug-seeking habits [48].
- Baseline Compulsion Test: Introduce a mild footshock (0.2-0.3 mA) upon active lever pressing. Rats that continue to seek drug despite punishment are classified as "compulsive" [49].
- Drug Treatment: Administer the test compound or vehicle to the compulsive cohort.
- Post-Treatment Test: Re-run the punishment resistance test and compare the rate of drug seeking to the baseline.
Outcome Measures:
- Number of active lever presses during punished sessions.
- Percentage of animals classified as "compulsive" pre- and post-treatment.
Protocol 2: Evaluating Analgesic Tolerance to Delta Opioid Agonists
Objective: To characterize the development of tolerance to the analgesic effects of a novel delta opioid agonist.
Materials:
- Animal model: Mice (e.g., DOR-eGFP knock-in mice).
- Test compound: Novel delta opioid agonist.
- Nociceptive assay: Inflammatory pain model (e.g., Complete Freund's Adjuvant-induced hypersensitivity).
Methodology:
- Acute Response: Measure the baseline pain response (e.g., mechanical allodynia) and administer a single dose of the agonist. Record the analgesic effect.
- Chronic Dosing: Administer the agonist chronically over 5-7 days.
- Tolerance Assessment: On the final day, re-administer the agonist and measure the analgesic response. Compare to the acute effect.
- Cellular Analysis (if using DOR-eGFP mice): Image the brains to assess agonist-induced receptor internalization and trafficking following acute and chronic treatment [89].
Outcome Measures:
- Withdrawal threshold (grams) pre- and post-drug administration.
- Degree of receptor internalization visualized via fluorescence.
Signaling Pathways and Experimental Workflows
Delta Opioid Receptor Signaling and Trafficking
Transition to Compulsive Drug Seeking
Research Reagent Solutions
Table 1: Key Pharmacological and Genetic Tools for Delta Opioid Receptor Research
| Reagent Name | Type | Primary Function/Application | Key Characteristic(s) |
|---|---|---|---|
| SNC80 [89] | Small Molecule Agonist | Prototypic, non-peptide DOR agonist for pain, depression, and anxiety studies. | Induces receptor internalization and subsequent tolerance. |
| ARM390 [89] | Small Molecule Agonist | Analgesic studies where receptor internalization is not desired. | Does not induce receptor internalization in vivo. |
| JNJ-20788560 [89] | Small Molecule Agonist | Analgesic studies with a focus on minimizing tolerance. | Reported to not produce analgesic tolerance in animal models. |
| ADL5859 [89] | Small Molecule Agonist | Clinical candidate for analgesia and depression. | Phase II clinical trials completed. |
| Naltrindole [89] | Antagonist | Prototypic DOR antagonist to block receptor function. | Increases anxiety and depressive-like behaviors. |
| DOR-eGFP Mice [89] | Genetic Model | Visualizing receptor localization and trafficking in vivo. | Expresses a functional, fluorescently tagged delta opioid receptor. |
| Delta Receptor KO Mice [89] | Genetic Model | Studying the physiological role of DOR by its absence. | Display increased anxiety, depression, and enhanced pain sensitivity. |
Frequently Asked Questions (FAQs)
Q1: What are the primary limitations of current rodent models in studying human addiction?
Current rodent models face several key limitations in bridging the gap to human clinical experience. They often fail to fully capture the cognitive-linguistic dimensions of human addiction, particularly aspects requiring self-reflection such as using more than intended or desire but failure to quit, which are fundamental to human addiction diagnosis [91]. Rodent models also typically lack the complex social and environmental contexts that significantly influence human addiction, including social opposition or support systems [91]. Additionally, these models struggle to incorporate the emergence of psychopathology - while humans with addiction experience compulsive dysregulated use as a major cognitively and emotionally involved dysfunction, animal substance use behavior remains normal rodent behavior in specifically designed non-native environments [91].
Q2: How can researchers determine if drug-seeking behavior in rodents is goal-directed or habitual?
Researchers can employ specific behavioral tests to distinguish between goal-directed and habitual drug-seeking. The outcome devaluation procedure assesses whether animals reduce responding when the drug outcome is devalued (e.g., through satiation or pairing with malaise) - persistent responding despite devaluation indicates habitual control [92] [70]. The contingency degradation test evaluates whether animals suppress responding when the causal relationship between action and outcome is weakened - continued responding suggests habitual behavior [92]. For drug seeking, second-order schedules of reinforcement can help dissociate these processes by examining the persistence of seeking responses when drug delivery is delayed or omitted [48].
Q3: What factors should be considered when modeling compulsive drug use in rodents?
Modeling compulsion requires careful consideration of several factors. Drug exposure history is critical - compulsive-like behavior should be studied after chronic drug exposure that repeatedly achieves clinically relevant intoxication levels, as limited intoxication history does not equivalently model human addiction [3]. Alternative explanations for persistent use despite adverse consequences must be ruled out, including reduced sensitivity to punishment, learned resistance to aversive stimuli, or impaired contingency learning [3]. Multidimensional assessment is recommended rather than relying solely on punishment resistance, including measures of motivation, withdrawal, and choice between drug and alternative rewards [93] [3].
Q4: How do sex differences impact translation from rodent models to human addiction?
Substantial sex differences exist in both rodent models and human addiction, impacting translational validity. Female rodents generally develop addiction-like characteristics faster and/or following less drug exposure than males [93]. Human studies show a "telescoping effect" where women progress from initial drug use to substance abuse disorders more rapidly than men [93]. Ovarian hormones, particularly estradiol, appear to modulate vulnerability in females for psychostimulant addiction [93]. These findings highlight the importance of including both sexes in preclinical studies and considering hormonal status when translating results to human populations.
Q5: What strategies can enhance the translational validity of rodent addiction models?
Several strategies can improve translational validity. Incorporating extended access models (Long Access) that produce escalation of intake better captures the transition from controlled use to addiction [61] [93]. Modeling individual vulnerability through procedures that identify subpopulations with different addiction-like behaviors enhances face validity [61]. Including negative consequences such as punished responding or quinine-adulterated solutions helps assess compulsive aspects [93] [3]. Providing alternative rewards (e.g., sweet solutions, social interaction) allows assessment of drug preference over natural rewards [93]. Ensuring clinically relevant drug exposure patterns and blood levels improves predictive validity [3].
Troubleshooting Common Experimental Challenges
Table 1: Addressing Limitations in Rodent Models of Addiction
| Challenge | Potential Solutions | Considerations for Translation |
|---|---|---|
| Modeling Cognitive Aspects | Incorporate behavioral paradigms assessing decision-making (e.g., cost-benefit analysis, delay discounting) [70] | Focus on cognitive processes with conserved neural substrates across species [91] |
| Assessing Compulsivity | Use multidimensional approach: punished responding, progressive ratio, resistance to extinction, choice paradigms [3] | Avoid over-reliance on single measure; rule out alternative explanations (e.g., reduced pain sensitivity) [3] |
| Incorporating Social Factors | Study drug self-administration in social housing conditions; implement social choice paradigms [91] [93] | Recognize inherent limitations in modeling complex human social dynamics [91] |
| Individual Differences | Employ population-based approaches identifying vulnerable vs. resistant subpopulations [61] [93] | Align inclusion criteria with human vulnerability factors (e.g., impulsivity, stress reactivity) [61] |
| Drug Access Patterns | Implement extended access (6h+), intermittent access, or escalating dose regimens [61] [93] | Pattern of access critically influences development of addiction-like features [93] |
Table 2: Optimization of Self-Administration Paradigms
| Parameter | Standard Approach | Enhanced Approach | Translational Rationale |
|---|---|---|---|
| Session Duration | Short Access (ShA: 1-2h) [93] | Long Access (LgA: 6h+) or Intermittent Access (IntA) [61] | Extended access promotes escalation and addiction-like features [93] |
| Reinforcement Schedule | Fixed Ratio 1 (FR1) [94] | Progressive Ratio (PR) or Second-Order Schedules [48] [94] | PR measures motivation; second-order schedules model complex drug-seeking [48] |
| Drug History | Limited drug exposure [3] | Chronic exposure achieving intoxication-level blood concentrations [3] | Addiction develops after chronic use; blood levels should match human recreational use [3] |
| Consequence Sensitivity | Standard operant chambers [94] | Incorporation of adverse consequences (footshock, bitter tastants) [93] [3] | Persistence despite negative consequences is clinical hallmark of addiction [3] |
| Behavioral Economic Measures | Simple intake measurements [70] | Demand curve analysis, drug vs. alternative reward choice [70] | Economic demand better correlates with dependence severity than simple intake [70] |
Experimental Protocols for Enhanced Cross-Species Validity
Protocol 1: Punished Drug Self-Administration to Assess Compulsive-Like Behavior
Purpose: To evaluate the persistence of drug seeking and taking despite negative consequences, modeling a core feature of human addiction [3].
Materials:
- Standard rodent self-administration apparatus
- Programmable footshock generator or quinine supply system
- Computer interface for behavioral control and data collection
Procedure:
- Establish stable drug self-administration (minimum 10-14 days) using standard training procedures.
- Gradually introduce adverse consequences contingent upon drug seeking/taking:
- Include appropriate control groups:
- Unpunished drug self-administration group
- Shock/quinine sensitivity controls (test response to aversive stimulus alone)
- Yoked controls receiving non-contingent punishment
- Classify animals as "compulsive-like" or "non-compulsive" based on persistence of responding despite punishment (typically using median split or resistance ratio) [3].
Troubleshooting:
- If animals show complete suppression of responding, reduce punishment intensity or probability
- Test innate sensitivity to punishment in separate cohort to ensure group differences aren't due to differential sensitivity
- Include multiple measures of compulsive-like behavior (latency to respond, aborted responses) to capture motivational conflict [3]
Protocol 2: Drug vs. Alternative Reward Choice Paradigm
Purpose: To assess the relative value of drug reward compared to natural rewards, modeling the clinical phenomenon of drug use superseding other rewarding activities [70].
Materials:
- Operant chambers with two response options (levers or nose-pokes)
- Separate delivery systems for drug and natural reward (e.g., sucrose solution)
- Programming capability for concurrent schedules of reinforcement
Procedure:
- Train animals to self-administer drug on one response option and a natural reward (e.g., sucrose) on the other option in separate sessions.
- Implement choice sessions where both options are available simultaneously under equivalent reinforcement schedules.
- Systematically manipulate decision parameters:
- Effort requirements (ratio schedules)
- Reward magnitude
- Delay to reward delivery
- Introduce environmental manipulations:
- Stress exposure prior to choice sessions
- Alternative reward enrichment
- Quantify preference as percentage of choices directed toward drug option [70].
Troubleshooting:
- If position bias develops, counterbalance response-reward assignments across subjects
- If animals fail to acquire both responses, ensure sufficient training on each option separately
- If choice behavior is unstable, use longer session durations or block designs
Experimental Workflow for Enhanced Rodent Models
Enhanced Rodent Model Development Workflow
This workflow outlines a systematic approach to developing rodent models with improved translational validity. The process begins with model selection and optimization, incorporating extended access protocols, adverse consequences, and alternative rewards to better capture clinical features of addiction [61] [93] [3]. The behavioral assessment phase emphasizes multidimensional phenotyping to capture the heterogeneity of addiction-like behaviors, including analysis of individual differences and cognitive-motivational aspects often overlooked in traditional models [3]. Finally, the translational validation stage explicitly compares model outcomes with human clinical features and assesses predictive validity for treatments, creating a feedback loop for continuous model refinement [91] [70].
Research Reagent Solutions
Table 3: Essential Materials for Addiction Modeling
| Category | Specific Items | Function & Application | Considerations |
|---|---|---|---|
| Behavioral Assessment | Operant chambers with dual response capability [94] | Drug vs. alternative reward choice paradigms; concurrent schedule assessment | Ensure programming flexibility for complex reinforcement schedules |
| Programmable aversive stimulus delivery (footshock, bitter tastant) [3] | Modeling persistence despite adverse consequences | Include sensitivity controls to rule out alternative explanations | |
| Pharmacological Tools | Selective dopamine receptor agonists/antagonists [48] | Probing mesolimbic system involvement in drug seeking | Consider receptor subtype specificity and injection timing |
| CRF receptor antagonists [70] | Testing stress-induced drug seeking mechanisms | Administer systemically or into specific stress-related brain regions | |
| Genetic Modulators | CRISPR/Cas9 systems for targeted gene editing [95] | Modeling polygenic risk factors identified in human studies | Use cell-type specific approaches for precision; control for off-target effects |
| Cre-loxP systems for cell-type specific manipulation [95] | Circuit-specific interrogation of addiction mechanisms | Verify specificity and efficiency of recombination | |
| Monitoring & Analysis | in vivo microdialysis or fiber photometry systems [48] | Real-time neurochemical monitoring during drug seeking | Consider temporal resolution and neurotransmitter specificity |
| scRNA-seq platforms for cell-type specific transcriptomics [95] | Identifying molecular adaptations in specific neuronal populations | Account for cellular heterogeneity and validation requirements |
The diagnosis and treatment of complex neuropsychiatric disorders, such as substance use disorders (SUDs), are undergoing a profound transformation. Moving beyond traditional, subjective diagnostic methods, the field is advancing towards a future powered by the integration of multi-scale biological data. This approach combines insights from transcriptomics (gene expression), proteomics (protein expression), and neuroimaging (brain structure and function) to create a holistic and mechanistic understanding of disease. For researchers modeling compulsive drug seeking in animals, this integrated framework is not just a distant goal but an emerging reality that promises to bridge the gap between preclinical models and human clinical applications. This technical support center is designed to guide you through the methodologies, troubleshooting, and practical implementation of these cutting-edge techniques within your research.
Technical Support & Troubleshooting Guides
This section addresses common experimental challenges when integrating multi-omics and neuroimaging data in the context of addiction research.
FAQ: Data Integration & Analysis
Q1: Our transcriptomic data from animal brain tissue and neuroimaging data exist on different spatial scales. How can we meaningfully correlate them?
A: This is a fundamental challenge in multiscale integration. The most robust approach is to use a standardized brain atlas as a computational bridge.
- Recommended Workflow:
- Regional Mapping: Map your transcriptomic data (e.g., from striatum or prefrontal cortex) to specific regions in a standardized rodent brain atlas.
- Image Parcellation: Parcellate your neuroimaging data (e.g., fMRI, PET) using the same atlas to extract region-specific signals.
- Spatial Correlation: Perform spatial correlation analyses, such as Partial Least Squares (PLS) regression, to identify relationships between the gene expression patterns in a region and the corresponding neuroimaging phenotype [96] [97]. This tests whether brain regions with a specific gene expression profile also show changes in a neuroimaging metric (e.g., functional connectivity or gray matter volume).
Q2: We have identified promising candidate biomarkers in our animal model. How can we validate their relevance for human substance use disorder (SUD)?
A: Translational validation is a multi-step process that leverages public databases and targeted experiments.
- Step 1: In-Silico Cross-Reference: Use human brain transcriptomic databases like the Allen Human Brain Atlas (AHBA) to check if your candidate genes are expressed in brain circuits relevant to addiction in humans (e.g., prefrontal cortex, anterior cingulate cortex, striatum) [96] [97].
- Step 2: Literature and Genetic Mining: Interrogate genome-wide association study (GWAS) summaries for SUDs to see if your candidate genes or their regulatory regions contain genetic variants linked to the disorder [98] [99].
- Step 3: Human Peripheral Validation: In collaboration with clinical researchers, analyze the expression of these candidates in accessible human tissues. Promising sources include:
Q3: What is the most effective way to analyze high-dimensional omics data to find robust, rather than coincidental, biomarkers?
A: The key is to use multivariate analysis methods that reduce dimensionality and identify underlying patterns.
- Essential Techniques:
- Principal Component Analysis (PCA): An unsupervised method to visualize the overall structure of your data and identify outliers or natural groupings [101].
- Partial Least Squares-Discriminant Analysis (PLS-DA): A supervised method that maximizes the separation between predefined groups (e.g., saline vs. drug-exposed animals) and identifies the variables (genes/proteins) most responsible for that separation [101].
- Multivariate ROC Analysis: Allows you to build a diagnostic model based on a panel of multiple biomarkers, which is almost always more accurate and robust than relying on a single biomarker [101].
Troubleshooting Common Experimental Issues
Problem: Low concordance between transcriptomic and proteomic findings from the same animal tissue samples.
| Potential Cause | Solution |
|---|---|
| Post-transcriptional Regulation | This is a common biological phenomenon. Integrate miRNA sequencing data to identify regulators that degrade mRNA or inhibit its translation [100]. |
| Protein Turnover Rates | Proteins often have longer half-lives than mRNAs. Consider the timing of your sample collection after a behavioral test or drug exposure to account for this delay. |
| Assay Sensitivity | Ensure your proteomics platform (e.g., mass spectrometry) is sensitive enough to detect low-abundance proteins that may be critical in addiction pathways. |
Problem: High variability in compulsive-like behavior (e.g., aversion resistance) in an animal cohort, complicating omics comparisons.
| Potential Cause | Solution |
|---|---|
| Underlying Genetic Heterogeneity | Use genetically diverse outbred strains to model human variation, or leverage selectively bred lines (e.g., bred High-Responders vs. Low-Responders) to amplify specific traits [100]. |
| Insufficient Behavioral Stratification | Do not group animals simply as "drug-exposed." Use a median split on the behavioral metric (e.g., quinine consumption) to create distinct "High-Compulsivity" and "Low-Compulsivity" groups for downstream omics analysis [100]. |
| Sex Differences | Sex is a critical biological variable. Female rodents often show higher levels of compulsive-like drinking [100]. Always analyze data by sex initially, as the molecular mechanisms underlying the same behavior may differ significantly between males and females [100]. |
Core Experimental Protocols
Below are detailed methodologies for key experiments in an integrated biomarker pipeline for compulsive drug use research.
Protocol: Modeling Compulsive-like Drug Taking in Rodents
Objective: To establish a reliable model of aversion-resistant alcohol drinking (a core feature of compulsion) in mice/rats [100].
- Train Stable Self-Administration: Train animals to operantly self-administer alcohol (e.g., 2-hour daily sessions) or provide continuous access in a two-bottle choice paradigm until stable baseline intake is achieved.
- Introduce Aversive Component:
- Quinine-Adulteration: Add increasing concentrations of the bitter tastant quinine (e.g., 0.03 mM to 0.1 mM) to the alcohol solution [100].
- Footshock Punishment: Deliver a mild footshock contingent on alcohol-reinforced lever presses.
- Define Compulsive-like Phenotype: Animals that maintain ≥80% of their baseline alcohol consumption despite the aversive contingency are classified as "compulsive-like" (or non-recovered, NR). Those that significantly reduce intake are classified as "non-compulsive" (or almost-recovered, AR) [100] [101].
- Tissue Collection: Euthanize animals and rapidly dissect brain regions of interest (e.g., anterior insular cortex, prefrontal cortex, striatum) [100]. Snap-freeze in liquid nitrogen for subsequent omics analysis.
Protocol: Integrated Transcriptomic and Proteomic Analysis from a Single Tissue Sample
Objective: To extract both RNA and protein from the same brain tissue sample to enable multi-omics correlation.
- Homogenization: Homogenize ~30 mg of frozen tissue in 1 mL of TRIzol reagent.
- Phase Separation: Add 0.2 mL of chloroform, shake vigorously, and centrifuge. The mixture separates into three phases:
- Lower, red phenol-chloroform phase: Contains DNA.
- Interphase: Contains denatured proteins.
- Upper, colorless aqueous phase: Contains RNA.
- RNA Precipitation: Transfer the aqueous phase to a new tube. Precipitate RNA with isopropanol, wash with ethanol, and resuspend in RNase-free water. Proceed to RNA-seq library preparation.
- Protein Precipitation: Remove the interphase and organic phase. Precipitate proteins with isopropanol, wash with guanidine hydrochloride, and resuspend in SDS buffer.
- Protein Digestion and Proteomics: Quantify protein. Digest proteins with trypsin and analyze the resulting peptides by Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS) for label-free or TMT-based quantification.
Protocol: Imaging-Transcriptomic Integration Analysis
Objective: To identify genes whose spatial expression patterns in the brain are associated with neuroimaging-derived phenotypes [96] [97].
- Acquire Reference Transcriptomic Data: Obtain a standardized brain-wide gene expression atlas. For mice, the Allen Mouse Brain Atlas is the equivalent resource.
- Generate Study-Specific Neuroimaging Phenotype Map: From your animal study, create a statistical map (e.g., t-statistic or effect size map) showing regional differences in a neuroimaging metric (e.g., functional connectivity strength, cerebral blood flow, gray matter density) between compulsive-like and control groups.
- Spatial Correlation using PLS Regression: Map both the gene expression data and the neuroimaging phenotype map onto a common brain atlas with multiple regions. Use PLS regression to identify the latent components that best explain the covariance between the two datasets [96] [97].
- Identify Significant Genes: Extract genes with high weights (e.g., |Z| > 3) on the first PLS component (PLS1), as these contribute most to the spatial correlation with the neuroimaging phenotype [97].
Diagram 1: Workflow for integrating transcriptomic and neuroimaging data in rodent models.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and tools for implementing the described integrated biomarker approaches.
| Item | Function/Application in SUD Research |
|---|---|
| Quinine Hydrochloride | Used to adulterate alcohol or drug solutions in rodent models to test for compulsion-like, aversion-resistant intake [100]. |
| TRIzol Reagent | Enables simultaneous extraction of RNA, DNA, and protein from a single, small tissue sample (e.g., from a specific brain nucleus), maximizing multi-omics data from one animal [101]. |
| Allen Brain Atlases | Publicly available brain-wide transcriptomic datasets (human and mouse) essential for spatial integration of gene expression with neuroimaging data and for translational validation [96] [97]. |
| LC-MS/MS System | The core platform for high-throughput proteomic analysis, allowing identification and quantification of thousands of proteins from brain tissue or biofluids [98] [99]. |
| miRNA Assays (e.g., miR-320, miR-222) | Tools to investigate epigenetic regulators. Altered levels in plasma or exosomes show promise as translational biomarkers for diagnosing and assessing states like methamphetamine use disorder [100] [101]. |
| PLS-DA Software (e.g., MetaboAnalyst) | A vital multivariate statistical tool for analyzing high-dimensional omics data, identifying biomarker panels that best discriminate between experimental groups (e.g., compulsive vs. non-compulsive) [101]. |
Data Presentation & Visualization
Quantitative Data from Key Studies
Table 1. Performance Metrics of a Transcriptomic Diagnostic Model for Methamphetamine Use Disorder (MUD) [101]
| Diagnostic Model Step | Objective | Prediction Accuracy | Key Biomarker Count |
|---|---|---|---|
| Step 1 | Distinguish non-recovered patients (NR) from all others | 98.7% | 10-Gene Panel |
| Step 2 | Distinguish almost-recovered patients (AR) from healthy controls (HC) | 81.3% | 10-Gene Panel |
Table 2. Key Neurobiological Domains for Addiction Biomarker Assessment [102]
| Domain | Measurable Construct | Example Assay/Modality |
|---|---|---|
| Incentive Salience | Drug craving, cue reactivity | fMRI cue-reactivity task |
| Negative Emotionality | Stress reactivity, anxiety, withdrawal | Serum cortisol, amygdala fMRI |
| Executive Function | Impulsivity, cognitive control | Go/No-Go task, prefrontal cortex fMRI |
Visualizing the Integrated Diagnostic Framework
Diagram 2: The integrated biomarker discovery pipeline, from animal models to clinical validation.
Conclusion
The field of preclinical addiction research has made significant strides in developing sophisticated animal models that capture core features of compulsive drug seeking, particularly through advanced self-administration protocols that measure persistence despite adverse consequences. However, a critical synthesis reveals that over-reliance on single behavioral measures like punishment resistance risks oversimplifying the complex, multifaceted nature of addiction. Future directions must prioritize models that incorporate chronic drug exposure histories, control for alternative explanations of behavioral persistence, and employ multidimensional assessment strategies that reflect the clinical heterogeneity of substance use disorders. The integration of cutting-edge transcriptomic and omics technologies with these refined behavioral paradigms offers a promising path toward identifying novel biomarkers and therapeutic targets, ultimately enhancing the translational value of preclinical research for developing effective treatments for addiction.
References
- 1. Appendix A: DSM-IV-TR and DSM-5 Diagnostic Criteria [https://www.publicsafetymedicine.org/leo/substance-use-disorders/appendix-a-dsm-iv-tr-and-dsm-5-diagnostic-criteria]
- 2. DSM-5 Criteria for Substance Use Disorders - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3767415/]
- 3. Are we compulsively chasing rainbows? [https://www.nature.com/articles/s41386-022-01419-w]
- 4. How preclinical models evolved to resemble the diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4702261/]
- 5. Corticostriatal circuitry - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4826773/]
- 6. Synaptic plasticity and physiological interactions between ... [https://pubmed.ncbi.nlm.nih.gov/9195611/]
- 7. Cortical glutamate and GABA are related to compulsive ... [https://www.nature.com/articles/s41467-023-38695-z]
- 8. Imaging dopamine's role in drug abuse and addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2696819/]
- 9. Neurobiology of addiction: a neurocircuitry analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6135092/]
- 10. Dopamine Circuit Mechanisms of Addiction-Like Behaviors [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2021.752420/full]
- 11. The functional logic of corticostriatal connections - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5334428/]
- 12. Investigating the Role of Glutamate in Obsessive-Compulsive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7173854/]
- 13. The incentive theory of addiction: some current issues... sensitization [https://pmc.ncbi.nlm.nih.gov/articles/PMC2607325/]
- 14. Applying incentive sensitization models to behavioral ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763414001730]
- 15. Cued for risk: Evidence for an incentive sensitization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6482104/]
- 16. The Role of Habits and Motivation in Human Drug Addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC3905212/]
- 17. Critical Review of the Habit Theory in Substance Use ... [https://link.springer.com/article/10.1007/s40429-025-00651-w]
- 18. An Integrative Model for Understanding Obsessive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9784452/]
- 19. Impaired Executive Functioning in Subclinical Compulsive ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2011.00078/full]
- 20. Understanding Addiction Using Animal Models [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2019.00262/full]
- 21. Animal Models of Addiction [https://www.sciencedirect.com/science/chapter/edited-volume/abs/pii/B9780128122020000026]
- 22. Drug-seeking motivation level in male rats determines ... [https://www.nature.com/articles/ncomms15527]
- 23. Moving beyond animal models: enriched environments ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2025.1629918/full]
- 24. Computational Models of Drug Use and Addiction: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC7416739/]
- 25. Part II. Identification and Management of the Drug-Seeking ... [https://www.aafp.org/pubs/afp/issues/2000/0415/p2401.html]
- 26. Animal models of addiction - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741108/]
- 27. Self-Administration - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/self-administration]
- 28. Drug Self-Administration - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/drug-self-administration]
- 29. Drug Self-administration [https://www.transpharmation.com/research/self-administration]
- 30. Establishment of multi-stage intravenous self ... [https://www.nature.com/articles/s41598-022-24740-2]
- 31. Animal Models of Addiction and the Opioid Crisis [https://www.taconic.com/resources/animal-models-addiction-opioid-crisis]
- 32. Unpredictability as a Modulator of Drug Self-Administration [https://pmc.ncbi.nlm.nih.gov/articles/PMC7396285/]
- 33. Increased responsiveness to punishment of cocaine... [https://www.nature.com/articles/s41386-021-01159-3?error=cookies_not_supported]
- 34. Cocaine seeking and consumption are oppositely ... [https://www.nature.com/articles/s41467-025-64885-y]
- 35. Behavioral and neurobiological mechanisms of punishment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6006171/]
- 36. Dopamine and serotonin differentially associated with reward ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159863/]
- 37. of Animal and models : From drug ... relapse craving drug [https://pubmed.ncbi.nlm.nih.gov/26822352/]
- 38. Recent developments in animal models of drug relapse [https://www.sciencedirect.com/science/article/abs/pii/S0959438813000196]
- 39. The reinstatement model of drug relapse - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3770775/]
- 40. The reinstatement model and relapse prevention: a clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1242108/]
- 41. The Winding Road to Relapse: Forging a New ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2018.00017/full]
- 42. -Induced Stress of Reinstatement Seeking: 20 Years of Progress Drug [https://www.nature.com/articles/npp2015142?error=cookies_not_supported&code=8c502269-7430-4cc0-8c91-754dbd1c95ec]
- 43. Novel models of drug relapse and craving after voluntary ... [https://www.nature.com/articles/s41386-018-0196-4]
- 44. Animal Models of Drug Relapse and Craving after Voluntary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11060480/]
- 45. Rat Race to Recovery: Uncovering the Secrets of Relapse [https://sqonline.ucsd.edu/2024/10/rat-race-to-recovery-uncovering-the-secrets-of-relapse/]
- 46. Animal Studies of Addictive Behavior - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3683998/]
- 47. Behavioral and neural mechanisms underlying habitual ... [https://www.sciencedirect.com/science/article/abs/pii/S0278584617303548]
- 48. Neural and psychological mechanisms underlying compulsive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4145664/]
- 49. Neural mechanisms underlying the vulnerability to develop ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2607322/]
- 50. Circuit Selectivity in Drug Versus Natural Reward Seeking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8178159/]
- 51. Dopamine prediction errors in reward learning and addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC4760620/]
- 52. Conditioned Place Preference - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK5229/]
- 53. Conditioned place preference [https://en.wikipedia.org/wiki/Conditioned_place_preference]
- 54. Drug-Induced Conditioned Place Preference and Its ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2020.582147/full]
- 55. Behavioral sensitization to psychostimulants and opioids [https://www.sciencedirect.com/science/article/abs/pii/S0278584623001100]
- 56. Drug Wanting: Behavioral Sensitization and Relapse to Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3082449/]
- 57. Behavioral Sensitization and Relapse to Drug-Seeking ... [https://www.sciencedirect.com/science/article/abs/pii/S0031699724009116]
- 58. Behavioral sensitization in humans - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/11681593/]
- 59. Using conditioned suppression to investigate compulsive ... [https://www.sciencedirect.com/science/article/abs/pii/S0376871614009648]
- 60. Development and Validation of the Compulsive Substance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341498/]
- 61. Understanding Addiction Using Animal Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6895146/]
- 62. Neurobiological convergence of pain and substance use ... [https://www.sciencedirect.com/science/article/pii/S2772392525000264]
- 63. Behavioral Animal Models and Neural-Circuit Framework ... [https://link.springer.com/article/10.1007/s12264-024-01270-7]
- 64. Taste Processing: Insights from Animal Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7397205/]
- 65. Sensory Abnormalities in Autism Spectrum Disorders [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2019.01016/full]
- 66. A Possible Biomarker for Cocaine Misuse and a Novel ... [https://bbrfoundation.org/content/possible-biomarker-cocaine-misuse-and-novel-treatment-cocaine-addiction-based-compound]
- 67. Emerging neuromodulation treatments for opioid and ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1570555/full]
- 68. of addiction: Animal taking and cognition... models Compulsive drug [https://pmc.ncbi.nlm.nih.gov/articles/PMC7458131/]
- 69. To Approach or Avoid Alcohol? Automatic and Self-Reported ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3417376/]
- 70. Addiction is driven by excessive goal-directed drug choice ... [https://www.nature.com/articles/s41386-020-0600-8]
- 71. Repeated Cocaine Exposure Attenuates the Desire to ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2018.00108/full]
- 72. Approach–Avoidance Conflict Paradigms in Animal and ... [https://www.mdpi.com/2076-328X/15/11/1528]
- 73. Animal Models of Drug Relapse and Craving after ... [https://www.sciencedirect.com/science/article/abs/pii/S0031699724006793]
- 74. Animal Models of the Behavioral Symptoms of Substance Use ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8327824/]
- 75. A Multilevel Computational Characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6071202/]
- 76. Guide to Experimental Design | Overview, Steps, & Examples [https://www.scribbr.com/methodology/experimental-design/]
- 77. Use of Experimental Designs in Research [https://sawtoothsoftware.com/resources/blog/posts/experimental-designs-in-research]
- 78. Deep phenotyping unveils hidden traits and genetic relations in subtle mutants | Nature Communications [https://www.nature.com/articles/ncomms12990]
- 79. The graded multidimensional geometry of phenotypic variation and progression in neurodegenerative syndromes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788217/]
- 80. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 81. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 82. Translational Models of Addiction Phenotypes to Advance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823887/]
- 83. Human hair follicle transcriptome profiling - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5727284/]
- 84. Single-cell transcriptomic reconstruction of the human hair ... [https://www.sciencedirect.com/science/article/pii/S2211124725009672]
- 85. Integrated omics identifies molecular networks of brain-body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12320092/]
- 86. Combined multi-omics and brain pathology reveal novel ... [https://www.nature.com/articles/s41598-025-21983-7]
- 87. A consensus blood transcriptomic framework for sepsis [https://www.nature.com/articles/s41591-025-03964-5]
- 88. Application of multi-omics techniques to androgenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11253216/]
- 89. The delta opioid receptor: an evolving target for the treatment of brain disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3197801/]
- 90. Devolving views of their roles in drug addiction [https://www.sciencedirect.com/science/article/pii/S0149763413000468]
- 91. Addiction Models and the Challenge of Having Impact - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6722013/]
- 92. On habits and addiction: An associative analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2891067/]
- 93. Modeling the Development of Drug Addiction in Male and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5732087/]
- 94. Rodent models of drug addiction - Maze Engineers [https://maze.conductscience.com/rodent-models-of-addiction/]
- 95. for psychiatric disorders: problems and promises Rodent models [https://labanimres.biomedcentral.com/articles/10.1186/s42826-020-00039-z]
- 96. Integrated transcriptomic and neuroimaging brain model ... [https://elifesciences.org/articles/62589]
- 97. Integrative omics analysis reveals epigenomic and ... [https://www.nature.com/articles/s41398-023-02724-8]
- 98. Integrated Genomic, Transcriptomic and Proteomic Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8700271/]
- 99. Application of omics-based biomarkers in substance use ... [https://www.sciencedirect.com/science/article/pii/S2950162823000085]
- 100. Editorial: Molecular aspects of compulsive drug use [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2023.1252507/full]
- 101. Identification of Potential Biomarkers for Diagnosis ... [https://www.mdpi.com/1422-0067/24/10/8672]
- 102. Dimensional Approaches to Understanding Addiction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6233300/]