Mapping the Mind: Neural Circuitry in Depression and the Mechanisms of Antidepressant Response
This article synthesizes contemporary research on the neural circuit dysfunctions underlying Major Depressive Disorder (MDD) and the mechanisms through which treatments confer their effects.
Mapping the Mind: Neural Circuitry in Depression and the Mechanisms of Antidepressant Response
Abstract
This article synthesizes contemporary research on the neural circuit dysfunctions underlying Major Depressive Disorder (MDD) and the mechanisms through which treatments confer their effects. Aimed at researchers and drug development professionals, it explores the transition from a monoamine-centric view to a circuit-based taxonomy of depression. The content details the application of advanced techniques like optogenetics and chemogenetics for dissecting circuit-specific pathologies, analyzes the limitations of current monoaminergic treatments, and evaluates novel, rapid-acting glutamatergic agents and neuromodulation therapies. By integrating foundational exploration with methodological applications, troubleshooting, and comparative validation, this review provides a comprehensive framework for developing next-generation, circuit-targeted antidepressant strategies.
The Stressed Brain: Defining the Neural Circuit Pathology of Major Depressive Disorder
The pathophysiological understanding of major depressive disorder (MDD) has evolved substantially from initial monoamine-based hypotheses toward sophisticated circuit-level models that integrate neuroimaging, molecular biology, and computational approaches. This whitepaper examines this evolution, highlighting how deficiencies in monoamine neurotransmitters—serotonin (5-HT), norepinephrine (NE), and dopamine (DA)—map onto distinct neural circuits and clinical manifestations of MDD. We synthesize current evidence linking monoaminergic systems to large-scale brain networks involved in reward processing, emotion regulation, and executive function. Advanced neuroimaging techniques and personalized computational modeling now enable researchers to predict treatment response and identify novel therapeutic targets within defined neural circuits. This paradigm shift from chemical imbalance to circuit dysfunction provides a more comprehensive framework for developing targeted, effective interventions for this heterogeneous disorder.
Major depressive disorder (MDD) represents a significant global health challenge, affecting over 350 million people worldwide and ranking as a leading cause of disability [1]. The economic burden is substantial, with depression-associated costs estimated at $83 billion annually in the United States alone [1]. Traditionally, depression has been characterized by persistent sad mood, anhedonia (loss of pleasure), changes in appetite and sleep, fatigue, and cognitive impairments [2]. The heterogeneity of these clinical manifestations suggests diverse underlying pathophysiological mechanisms that have been the focus of intensive research.
The evolution of depression models has followed a trajectory from neurotransmitter-based theories to circuit-level explanations:
- 1960s-1990s: Dominance of monoamine hypothesis focusing on synaptic neurotransmitter deficiencies
- 2000-2010s: Integration of neuroendocrine, neuroplasticity, and inflammation hypotheses
- 2010-present: Emergence of circuit-based models integrating neuroimaging, genetics, and computational approaches
This whitepaper examines this evolutionary trajectory, emphasizing how modern research frameworks reconcile monoaminergic mechanisms with circuit-level dysfunction to advance both understanding and treatment of MDD.
Historical Foundation: The Monoamine Hypothesis
Core Monoamine Deficits in MDD
The monoamine hypothesis, originating in the 1960s, proposed that MDD results from deficiencies in key neurotransmitters: serotonin (5-HT), norepinephrine (NE), and dopamine (DA) [3] [2]. This hypothesis gained support from the observed therapeutic effects of early antidepressants that increased synaptic concentrations of these monoamines. While this model has been refined over decades, it continues to inform treatment development and understanding of depression pathophysiology.
Table 1: Monoamine Systems and Their Roles in Depression Pathophysiology
| Monoamine | Primary Brain Regions | Proposed Role in MDD | Therapeutic Target |
|---|---|---|---|
| Serotonin (5-HT) | Raphe nuclei, widespread cortical projections | Mood regulation, sleep, appetite, cognitive functions [3] | SSRIs, SNRIs, atypical antidepressants |
| Norepinephrine (NE) | Locus coeruleus, limbic system, prefrontal cortex | Arousal, attention, stress response, emotional memory [3] | SNRIs, TCAs, NDRIs |
| Dopamine (DA) | Ventral tegmental area, nucleus accumbens, prefrontal cortex | Reward, motivation, pleasure, executive function [3] | Bupropion, atypical antipsychotics |
The Three Primary Color Model of Basic Emotions
Recent refinements to the monoamine hypothesis propose distinct emotional domains for each neurotransmitter system. The "Three Primary Color Model" suggests that DA mediates joy/reward, NE mediates fear/anger, and 5-HT mediates disgust/sadness [3]. This model provides a framework for understanding how monoamine systems work in concert to generate diverse emotional states, with imbalances leading to specific depressive symptomatology.
Limitations and Evolution of Monoamine Theories
Clinical Challenges to the Monoamine Hypothesis
Despite its historical influence, several clinical observations challenge the simplicity of the monoamine hypothesis:
- Treatment Resistance: Approximately 30% of MDD patients do not respond adequately to conventional monoamine-targeting antidepressants [2].
- Delayed Onset: While pharmacological effects on monoamines occur within hours, clinical improvement typically requires weeks of treatment [3].
- Incomplete Efficacy: Even among responders, many patients experience residual symptoms despite adequate monoaminergic modulation [1].
These limitations prompted investigation into additional pathophysiological mechanisms, including hypothalamic-pituitary-adrenal (HPA) axis dysregulation, neuroinflammation, and impaired neuroplasticity [2].
Expanding Pathophysiological Models
Modern understanding recognizes multiple interacting systems in MDD pathogenesis:
Table 2: Evolving Pathophysiological Models of Depression
| Model | Key Mechanisms | Supporting Evidence | Limitations |
|---|---|---|---|
| Monoamine Hypothesis | Deficiencies in 5-HT, NE, and DA signaling [3] | Antidepressant efficacy; neurochemical studies | Incomplete explanation of treatment resistance |
| HPA Axis Dysregulation | Chronic stress, cortisol excess, glucocorticoid receptor resistance [2] | Hypercortisolemia in MDD; CRF abnormalities | Not specific to MDD; inconsistent across patients |
| Neuroinflammation | Elevated pro-inflammatory cytokines; microglial activation [2] | Increased CRP, IL-6 in MDD; sickness behavior | Causal relationships not fully established |
| Neuroplasticity Model | Reduced BDNF, impaired neurogenesis, synaptic dysfunction [2] | Post-mortem brain studies; animal models | Temporal relationship with depression onset unclear |
| Circuit Dysfunction | Large-scale network disruption; functional connectivity changes [4] | fMRI studies; network-based computational models | Heterogeneity in circuit abnormalities |
The Circuit-Level Paradigm: Integrating Monoamines with Neural Networks
Key Circuits in Depression Pathophysiology
Modern neuroimaging research has identified several large-scale brain networks consistently implicated in MDD:
- Reward Circuit: Includes ventral striatum, ventral pallidum, orbitofrontal cortex (OFC), anterior cingulate cortex (ACC), and thalamus [4]. Dysfunction in this circuit underlies anhedonia and amotivation, core features of MDD.
- Emotion Regulation Circuit: Involves prefrontal cortex, hippocampus, amygdala, OFC, and ACC [4]. This circuit modulates emotional responses, with dysfunction leading to persistent negative affect.
- Cognitive Control Network: Encompasses dorsolateral prefrontal cortex (DLPFC) and associated regions. Impairment contributes to executive dysfunction in MDD.
Monoamine-Circuit Interactions
The circuit-level paradigm does not discard monoamine theories but rather incorporates them into a more comprehensive model. Monoaminergic systems modulate information processing within these circuits:
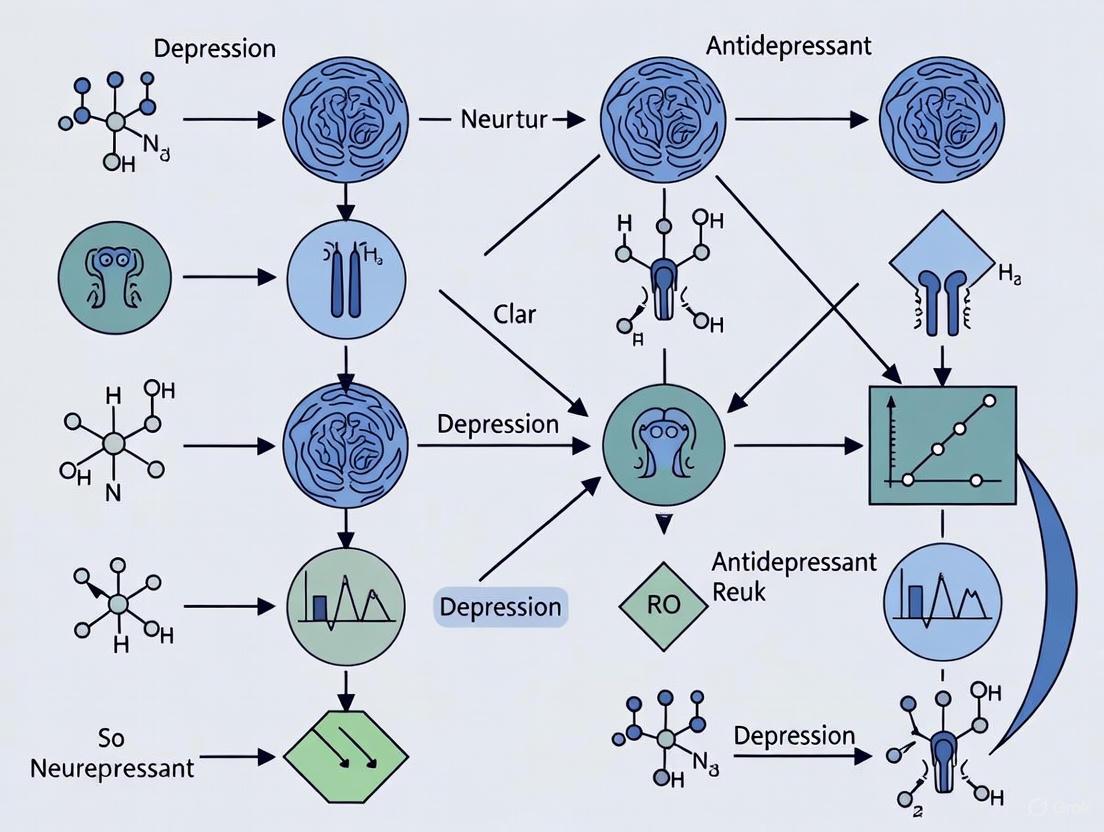
Monoamine-Circuit Interactions in MDD Pathophysiology
This diagram illustrates how primary monoamine systems modulate specific neural circuits that give rise to core clinical manifestations of MDD, while also demonstrating the cross-system interactions that contribute to the disorder's complexity.
Glial Cell Contributions to Circuit Dysfunction
Recent research has highlighted the crucial role of glial cells, particularly astrocytes, in modulating circuit function in MDD. Postmortem studies of MDD patients show reduced densities of glial cells in prefrontal cortex, hippocampus, and amygdala [2]. Astrocytic dysfunction affects multiple pathways relevant to depression:
- Glutamate Homeostasis: Reduced expression of glutamate transporter-1 (GLT-1) and glutamine synthase in astrocytes impairs glutamate clearance, potentially contributing to excitotoxicity [2].
- Purinergic Signaling: Activation of purinergic ligand-gated ion channel 7 receptors (P2X7R) in astrocytes under chronic stress contributes to depressive-like behaviors in animal models [2].
- Blood-Brain Barrier Function: Altered aquaporin-4 (AQP4) expression in astrocytic endfeet may affect neurovascular coupling in MDD [2].
Methodological Approaches for Circuit-Level Analysis
Neuroimaging Biomarkers and Predictive Modeling
Advanced neuroimaging techniques enable researchers to identify circuit-based biomarkers of treatment response. Recent studies using hierarchical local-global imaging and clinical feature fusion graph neural network models have achieved 76.21% accuracy in predicting remission following SSRI treatment [4]. Key contributing brain regions include:
- Right globus pallidus and bilateral putamen (reward processing)
- Left hippocampus (memory and contextual processing)
- Bilateral thalamus (sensory integration)
- Bilateral anterior cingulate gyrus (emotion regulation)
Table 3: Experimental Protocols for Circuit-Level Depression Research
| Methodology | Key Applications in Depression Research | Technical Considerations | References |
|---|---|---|---|
| Resting-state fMRI | Functional connectivity mapping; network identification | Sensitivity to motion artifacts; analytical pipeline variability | [4] |
| Graph Neural Networks (GNNs) | Predictive modeling of treatment response; network analysis | Requires large datasets; computational intensity | [4] |
| Personalized Brain Modeling | Individualized treatment prediction; circuit targeting | Integration of multiple data types; validation challenges | [5] |
| Electroencephalography (EEG) | Measuring slow-wave activity; treatment response biomarkers | Limited spatial resolution; signal processing complexity | [5] |
Protocol: Local-Global Graph Neural Network for Predicting Antidepressant Response
This protocol outlines the methodology for implementing a hierarchical local-global imaging and clinical feature fusion graph neural network (LGCIF-GNN) to predict antidepressant treatment outcomes [4]:
Participant Selection and Clinical Assessment
- Recruit medication-free MDD patients (sample size: ~279)
- Collect demographic data (age, sex, education)
- Administer clinical assessments: Hamilton Depression Rating Scale (HAMD), Quality of Life Enjoyness and Satisfaction Questionnaire (QLES)
Neuroimaging Data Acquisition
- Acquire resting-state fMRI using standard parameters (TR/TE: 2000/30ms, voxel size: 3×3×3mm)
- Collect high-resolution structural images (MPRAGE sequence)
Data Preprocessing
- Implement standard fMRI preprocessing pipeline: slice timing correction, motion realignment, normalization to MNI space, smoothing
- Extract time series from predefined regions of interest (ROIs)
Feature Extraction and Graph Construction
- Compute dynamic functional connectivity using sliding window approach
- Construct subject-level graphs with ROIs as nodes and functional connectivity as edges
- Create population-level graph based on functional and clinical similarity between subjects
Model Architecture and Training
- Implement local GNN to capture intra-subject ROI-level dynamics using bidirectional GRU encoder
- Implement global GNN to model inter-subject relationships
- Fuse imaging and clinical features in final layers
- Train model using cross-validation with remission status as outcome
Model Validation
- Evaluate performance on internal validation dataset
- Test generalizability on external independent dataset
- Assess key predictive brain regions through feature importance analysis
Computational Workflow for Predicting Antidepressant Response
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Circuit-Level Depression Investigations
| Category | Specific Reagents/Tools | Research Applications | Key Functions |
|---|---|---|---|
| Neuroimaging Biomarkers | Resting-state fMRI; Structural MRI; DTI | Circuit identification; connectivity analysis | Maps structural and functional neural networks [4] |
| Computational Modeling | Graph Neural Networks (GNNs); Personalized brain modeling | Treatment prediction; dose optimization | Integrates multimodal data for individual predictions [4] [5] |
| Molecular Assays | PCR; Western Blot; Immunohistochemistry | Gene expression; protein quantification | Measures molecular correlates of circuit dysfunction [2] |
| Electrophysiology Tools | EEG; Slow-wave measurement | Brain dynamics; treatment response biomarkers | Quantifies brain activity patterns relevant to depression [5] |
| Genetic Analysis | GWAS; Transcriptomic profiling | Risk variant identification; pathway analysis | Identifies genetic factors in circuit vulnerability [2] |
Therapeutic Implications and Future Directions
Circuit-Targeted Interventions
The circuit-based model of depression has stimulated development of novel therapeutic approaches:
- Neuromodulation Techniques: Transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS) target specific nodes within dysfunctional circuits.
- Anesthetic Manipulation: Propofol and ketamine are investigated for their ability to modulate slow-wave activity and produce rapid antidepressant effects [5].
- Personalized Dosing: Computational models optimize drug dosing based on individual brain dynamics to achieve therapeutic "sweet spots" [5].
Integrated Pathophysiological Model
The evolving understanding of MDD pathophysiology integrates multiple levels of analysis:
Integrated Pathophysiological Model of MDD
The pathophysiological understanding of depression has evolved substantially from simplistic monoamine theories toward integrated circuit-based models. This paradigm shift acknowledges the complex interactions between genetic vulnerability, environmental stressors, molecular mechanisms, and large-scale neural network dysfunction. Modern research approaches that combine advanced neuroimaging, computational modeling, and molecular biology provide unprecedented opportunities to decode depression heterogeneity and develop targeted, effective interventions.
The future of depression research lies in personalized medicine approaches that account for individual variability in circuit organization and function. By identifying specific circuit-based biomarkers and developing interventions that normalize dysfunctional network activity, researchers can move beyond the limitations of conventional monoamine-targeting treatments. This evolving framework not only enhances our understanding of depression pathophysiology but also promises more effective, precisely targeted therapeutic strategies for this debilitating disorder.
Chronic Stress as a Key Instigator of Maladaptive Neural Circuit Rewiring
Chronic stress is a significant precipitant of maladaptive neural plasticity, disrupting the intricate balance of limbic and cortical circuits to foster vulnerability to psychiatric disorders such as major depressive disorder (MDD). This whitepaper delineates the mechanisms through which repeated stress exposure instigates pathophysiological rewiring within key brain networks, including the amygdala, prefrontal cortex (PFC), hippocampus, and reward circuits. We synthesize evidence of stress-induced alterations at molecular, cellular, and systems levels, highlighting the opposing patterns of plasticity in nodes of the limbic system. Furthermore, we explore the implications of these neural circuit changes for the heterogeneity of antidepressant treatment response. The insights provided herein aim to inform the development of targeted, circuit-based therapeutics for stress-related psychopathologies.
The physiological response to stress, encompassing neuroendocrine, autonomic, and behavioral changes, is fundamentally adaptive, promoting survival in the face of acute threats [6]. However, chronic activation of stress response systems leads to a cumulative burden, or "allostatic load," which has deleterious effects on health, including increased risk for hypertension, metabolic syndrome, and neuropsychiatric illnesses [6]. The brain is a primary target of stress mediators, and persistent exposure to glucocorticoids (cortisol in primates, corticosterone in rodents) and other stress-signaling molecules can trigger maladaptive plasticity within emotionally salient neural circuits [6] [7].
A critical insight from recent research is that chronic stress does not uniformly weaken the brain; rather, it pathologically rewires specific circuits, leading to contrasting patterns of plasticity in different regions. Convergent evidence indicates that prolonged stress leads to overall neuronal atrophy and synaptic depression in the PFC and hippocampus, while regions such as the amygdala and nucleus accumbens (NAc) exhibit changes consistent with neuronal hypertrophy and synaptic potentiation [7]. This maladaptive reorganization underlies core symptoms of depression, including negative affect, anhedonia, and cognitive deficits. This whitepaper examines the mechanisms of this stress-induced circuit rewiring within the context of depression research and its implications for predicting and improving antidepressant response.
Maladaptive Rewiring of Key Neural Circuits by Chronic Stress
Chronic stress disrupts the delicate equilibrium between key brain regions responsible for emotional regulation, reward processing, and cognition. The following sections detail the pathophysiological changes in specific circuits.
Limbic Forebrain Networks: A Central Hub for Stress Integration
Emotional stressors are distinguished by their capacity to induce long-term alterations in limbic forebrain networks, which are associated with the cognitive and affective symptoms in stress-related disorders [6]. The hypothalamic-pituitary-adrenal (HPA) axis, the canonical stress response system, is heavily regulated by these forebrain regions. Chronic stress and conditions like MDD are linked to diminished sensitivity to glucocorticoids in the limbic forebrain, which impairs negative feedback regulation of the HPA axis and disrupts the capacity for adaptive cognitive and affective adjustments [6].
Table 1: Contrasting Effects of Chronic Stress on Key Brain Regions
| Brain Region | Effect of Chronic Stress | Functional Consequence | Molecular Correlates |
|---|---|---|---|
| Prefrontal Cortex (PFC) | Neuronal atrophy, dendritic spine loss, synaptic depression [7] | Impaired executive function, cognitive inflexibility | Deficits in BDNF, disrupted mTOR signaling [7] |
| Hippocampus | Neuronal atrophy, suppressed neurogenesis, synaptic deficits [7] | Impaired context memory, dysregulated HPA feedback | Reduced BDNF, increased glucocorticoid signaling [6] [7] |
| Amygdala (Basolateral & Central) | Neuronal hypertrophy, dendritic arborization, synaptic potentiation [7] | Hyper-anxiety, heightened fear response | Increased BDNF and CRF signaling [7] |
| Nucleus Accumbens (NAc) | Synaptic potentiation [7] | Anhedonia, reduced motivation | Increased BDNF and CRF signaling [7] |
Molecular Signaling Pathways in Stress-Induced Plasticity
The structural and functional rewiring of neural circuits is driven by alterations in key molecular signaling pathways.
- Brain-Derived Neurotrophic Factor (BDNF): BDNF plays a region-specific role in stress pathology. Chronic stress decreases BDNF levels in the hippocampus and PFC, contributing to neuronal atrophy. In contrast, stress increases BDNF in the NAc and amygdala, promoting maladaptive synaptic strengthening. This opposing regulation is a core mechanism for the divergent plasticity observed across circuits [7].
- Glutamatergic Signaling & mTOR Pathway: The rapid-acting antidepressant ketamine, an NMDA receptor antagonist, has illuminated the role of glutamate and downstream signaling. Ketamine blockade of NMDA receptors leads to a burst of glutamate release and subsequent activation of AMPA receptors. This triggers signaling cascades that activate the mTOR pathway, a critical regulator of protein synthesis, leading to rapid synaptogenesis in stress-atrophied regions like the PFC and hippocampus [7]. Chronic stress is believed to suppress this pathway, and its restoration is a promising therapeutic avenue.
- Calcium/Calmodulin-Dependent Protein Kinase II (CaMKII): In the lateral habenula (LHb), a nucleus hyperactive in depression, stress upregulates βCaMKII. This increases membrane insertion of GluR1-containing AMPA receptors, enhancing excitatory drive and contributing to depressive phenotypes [7].
The diagram below illustrates the core signaling pathway implicated in stress-induced synaptic deficits and the proposed mechanism of rapid-acting antidepressants like ketamine.
Experimental Protocols for Investigating Circuit Rewiring
To establish causal and mechanistic evidence for stress-induced rewiring, researchers employ a suite of sophisticated techniques. The following protocol exemplifies a comprehensive approach.
Integrated Protocol: Assessing Social Defeat Stress-Induced Rewiring of Reward Circuits
This protocol is widely used to study anhedonia and depression-like behaviors in rodents [7].
1. Stress Induction (Chronic Social Defeat Stress):
- Animals: Adult male C57BL/6J mice are used as intruders; larger, aggressive CD-1 mice are used as residents.
- Procedure: Each C57BL/6J mouse is placed in the home cage of a novel, aggressive CD-1 mouse for 5-10 minutes, resulting in physical confrontation. After the confrontation, the animals are housed in divided cages with sensory contact for the remainder of the 24-hour period. This cycle is repeated for 10 consecutive days with a novel CD-1 mouse each day.
- Control: Control mice are housed in pairs but are not exposed to aggressive conspecifics.
2. Behavioral Phenotyping (Post-Stress):
- Sucrose Preference Test: Measures anhedonia. Mice are presented with two bottles, one with sucrose solution and one with water. A significant reduction in sucrose preference compared to controls indicates anhedonia.
- Social Interaction Test: Measures social avoidance. The mouse is placed in an arena with a novel CD-1 mouse enclosed in a wire cage. Time spent in the "interaction zone" around the cage is measured. Defeated mice typically show reduced interaction.
- Forced Swim Test: Measures behavioral despair. The mouse is placed in a inescapable cylinder of water for 6 minutes. Increased immobility time is interpreted as a depressive-like phenotype.
3. Neural Circuit Analysis:
- Viral Vector-Mediated Circuit Mapping: Inject a Cre-dependent AAV encoding a fluorescent reporter (e.g., GFP) into the VTA of dopamine transporter (DAT)-Cre mice. This labels VTA dopamine neurons and their projections to the NAc.
- Ex Vivo Electrophysiology: Prepare brain slices containing the NAc. Record excitatory postsynaptic currents (EPSCs) from medium spiny neurons (MSNs) while optically stimulating VTA dopamine terminals. This assesses the strength of VTA-NAc synapses.
- In Vivo Fiber Photometry: Inject an AAV encoding a genetically encoded calcium indicator (e.g., GCaMP) into the VTA of DAT-Cre mice. Implant an optical fiber above the VTA to record population-level calcium dynamics in VTA neurons during behavioral tasks, providing a readout of neural activity.
Table 2: Key Reagents for Investigating Stress-Induced Circuit Rewiring
| Research Reagent / Tool | Function & Application in Stress Research |
|---|---|
| AAV Vectors (e.g., AAV5-syn-GCaMP8m) | Deliver genes for sensors (GCaMP, jRGECO1a) or actuators (Channelrhodopsin, Halorhodopsin) to specific cell types for monitoring or manipulating neural activity [4]. |
| Cre-Driver Mouse Lines (e.g., DAT-Cre) | Enable genetic access to specific neuronal populations (e.g., dopamine neurons) for targeted expression of transgenes [7]. |
| c-Fos Immunohistochemistry | Maps neural activity patterns in response to stress or other stimuli by labeling the protein product of the immediate-early gene c-fos [6]. |
| Fiber Photometry Systems | Allow real-time, in vivo recording of population-level neural activity (via calcium or neurotransmitter sensors) in freely behaving animals [4]. |
| Optogenetics Hardware | Used to precisely stimulate or inhibit specific neural pathways with light to establish causal roles in behavior [8]. |
| scRNA-seq | Resolves cell-type-specific transcriptional changes in response to stress, identifying novel molecular targets [9]. |
The workflow for a comprehensive circuit analysis experiment, from stress induction to data collection, is summarized below.
Implications for Antidepressant Research and Development
Understanding maladaptive circuit rewiring provides a roadmap for developing novel antidepressants and personalizing treatment.
- Predicting Treatment Response: Neuroimaging biomarkers derived from dysfunctional reward and emotion regulation circuits can predict response to antidepressants like SSRIs. A recent hierarchical graph neural network model that integrated pre-treatment neurocircuitry and clinical features achieved 76.21% accuracy in predicting remission following SSRI treatment [4]. Key predictive brain regions included the globus pallidus, putamen, hippocampus, thalamus, and anterior cingulate gyrus [4].
- Targeting Circuit Dysfunction: Treatments are increasingly evaluated based on their ability to reverse specific maladaptive changes. For instance, the efficacy of ketamine is attributed to its rapid restoration of synaptic connectivity in the PFC and hippocampus, countering the synaptic deficits induced by stress [7]. This highlights a shift from monoamine-based targeting to circuit-specific remediation.
- Guideline Adherence and Treatment Gaps: Despite the availability of evidence-based guidelines, adherence in clinical practice is often suboptimal [10]. Improving the implementation of guideline-concordant care, which may include psychotherapy, pharmacotherapy, and integrative practices, is crucial for achieving better patient outcomes [11] [10].
Chronic stress instigates maladaptive neural circuit rewiring through a complex interplay of molecular signaling pathways, leading to a functional imbalance between nodes of the limbic system. The patterns of synaptic weakening in the PFC and hippocampus, coupled with synaptic strengthening in the amygdala and NAc, create a neural substrate prone to depressive symptomatology. Modern research approaches that combine circuit manipulation, in vivo monitoring, and computational modeling are essential for deciphering this complexity. The future of antidepressant development lies in leveraging this knowledge to create interventions that directly target and rectify these pathological circuit changes, moving toward a future of personalized, circuit-informed psychiatry.
Major depressive disorder (MDD) represents one of the most substantial burdens on global public health, ranking among the leading causes of disability worldwide [12]. Despite its prevalence, the treatment of depression remains hindered by profound etiological and phenotypic heterogeneity, with current psychiatric diagnostics assigning a single label to syndromes that likely involve multiple distinct neurobiological processes [13]. This heterogeneity is reflected in strikingly low treatment success rates; the landmark STAR*D trial revealed that only approximately one-third of patients achieve remission with first-line selective serotonin reuptake inhibitor (SSRI) treatment, and approximately 20% remain symptomatic despite multiple, often aggressive, interventions [14]. The prevailing "one-size-fits-all" approach to depression treatment has therefore yielded limited success, creating an urgent need for quantitative measures based on coherent neurobiological dysfunctions, or 'biotypes', to enable improved patient stratification [13].
This whitepaper proposes a circuit-based taxonomy for depression that links specific neural circuit dysfunctions to distinct symptom profiles and treatment outcomes. The approach is grounded in accumulating evidence that depression involves disruptions across multiple large-scale brain networks, including the default mode, salience, and frontoparietal attention circuits [13]. By moving beyond syndromic classification toward a neurobiologically-grounded taxonomy, we aim to provide researchers and drug development professionals with a framework for developing targeted interventions matched to specific patterns of circuit dysfunction. Such advances are crucial for advancing precision medicine in psychiatry and improving the abysmally low remission rates that have plagued conventional antidepressant development.
A Taxonomy of Depression Biotypes: Linking Circuits to Clinical Profiles
Recent research utilizing standardized functional magnetic resonance imaging (fMRI) protocols has enabled the identification of distinct biotypes of depression and anxiety based on personalized, interpretable scores of brain circuit dysfunction [13]. In a comprehensive analysis of 801 participants with depression and anxiety when treatment-free, researchers derived six clinically distinct biotypes defined by unique profiles of intrinsic task-free functional connectivity within core brain networks, along with distinct patterns of activation and connectivity during emotional and cognitive tasks [13].
Table 1: Depression Biotypes: Circuit Dysfunctions, Symptom Profiles, and Treatment Response
| Biotype | Core Circuit Dysfunctions | Clinical Symptom Profile | Treatment Response Patterns |
|---|---|---|---|
| Biotype 1 | Hyperconnectivity in default mode network; reduced cognitive control circuit activation | Prominent anhedonia, rumination, and negative self-focus | Better response to behavioral therapy targeting rumination than standard pharmacotherapy |
| Biotype 2 | Salience network hyperconnectivity; heightened threat circuit reactivity | Severe anxiety, vigilance, threat sensitivity | Moderate response to SSRIs; potentially better response to anxiety-targeted interventions |
| Biotype 3 | Attention control network hypoconnectivity; reduced cognitive control activation | Cognitive dysfunction, impaired concentration, executive deficits | Poor response to conventional antidepressants; may benefit from cognitive-enhancing adjuncts |
| Biotype 4 | Default mode and salience network co-dysregulation; emotional task hyperreactivity | Mixed depressive-anxious symptoms with emotional lability | Moderate response to both pharmacotherapy and behavioral interventions |
| Biotype 5 | Default mode hypoconnectivity; blunted positive affect circuit activity | Apathy, anergia, blunted affect | Better response to antidepressants with activating properties |
| Biotype 6 | Mild circuit deviations across multiple networks | Milder, more heterogeneous symptoms | Good response to first-line treatments (both therapy and medication) |
These biotypes demonstrate remarkable consistency with theoretical frameworks of circuit dysfunction in depression and are distinguished by specific symptom profiles, behavioral performance on cognitive tests, and differential responses to various treatment modalities [13]. The identification of such biotypes provides a neurobiological foundation for parsing the heterogeneity of depression and represents a promising approach for advancing precision clinical care in psychiatry.
Molecular Pathways Converging on Synaptic Dysfunction in Depression
The neural circuit dysfunctions observed in depression biotypes arise from disturbances at the molecular level that ultimately converge on synaptic dysfunction. Major depressive disorder involves a complex interplay of numerous interrelated pathways, including monoamine systems, neurotrophin signaling, glutamatergic neurotransmission, inflammatory processes, and (epi)genetic regulation [12].
The monoamine theory of depression, which posited deficiencies in serotonin, norepinephrine, and dopamine signaling, has evolved to acknowledge that these neurotransmitters represent only one component of a far more complex picture [12]. While monoamine-based antidepressants remain first-line treatments, their limitations – including delayed onset of action and limited efficacy in a substantial proportion of patients – have prompted investigation into alternative mechanisms. Notably, the rapid antidepressant effects of ketamine have highlighted the crucial role of glutamate signaling and synaptic plasticity in depression pathophysiology [15].
Genetic studies have provided compelling evidence for the synaptic basis of depression. The largest genome-wide association study of depression to date, involving over 1.2 million participants, identified 178 genetic risk loci, with top biological processes including synapse assembly and function [12]. Key MDD-associated genes such as NEGR1, DRD2, and CELF4 are all implicated in the control of synaptic number, maturation, and plasticity [12]. These genetic variants likely serve as "first hits" in a multifactorial disease model, increasing vulnerability to environmental stressors that subsequently induce epigenetic modifications affecting synaptic function.
The neurotrophic hypothesis of depression, focusing particularly on brain-derived neurotrophic factor (BDNF), provides a crucial link between molecular pathways and circuit-level dysfunction. Reduced BDNF levels in acute MDD impair synaptic support and plasticity, while effective antidepressant treatments – including both conventional medications and ketamine – increase BDNF signaling and promote synaptogenesis [12]. Recent research has demonstrated that antidepressants bind directly to the transmembrane domain of TrkB receptors, enhancing BDNF signaling and promoting synaptic connectivity [12].
Table 2: Key Molecular Pathways in Depression and Their Synaptic Targets
| Molecular Pathway | Key Components | Synaptic Actions | Experimental Modulators |
|---|---|---|---|
| Monoamine Signaling | Serotonin, norepinephrine, dopamine receptors; monoamine transporters | Modulate neurotransmitter release; regulate synaptic plasticity through G-protein coupled receptors | SSRIs, SNRIs, TCAs, MAOIs |
| Glutamatergic System | NMDA, AMPA, metabotropic glutamate receptors | Regulate excitatory neurotransmission; control synaptic plasticity and strength | Ketamine, psilocybin, AMPA potentiators |
| Neurotrophic Signaling | BDNF, TrkB, mTOR | Promote synaptogenesis; enhance synaptic plasticity and stability | TrkB agonists, mTOR modulators |
| Opioid System | μ, δ, κ opioid receptors | Modulate neurotransmitter release through potassium channel activation; influence neuronal excitability | KOR antagonists, MOR modulators |
| Inflammatory Pathways | Cytokines, CRP, microglial activation | Alter synaptic pruning; reduce synaptic plasticity | Anti-cytokine therapies, minocycline |
The convergence of these diverse molecular pathways on synaptic function provides a framework for understanding how genetic vulnerability, environmental stressors, and biological systems interact to produce the circuit-level dysfunctions observed in depression biotypes. This multi-level perspective enables researchers to connect molecular targets with systems-level approaches for drug development.
Experimental Methodologies for Circuit-Based Taxonomy Development
Neuroimaging Protocols for Biotype Identification
The identification of depression biotypes requires standardized functional magnetic resonance imaging protocols that assess both task-free and task-evoked brain circuit function. The Stanford Et Cere Image Processing System represents one such approach, quantifying circuit dysfunction at the individual participant level through 41 distinct measures of activation and connectivity across six brain circuits of interest [13]. These measures are expressed in standard deviation units from the mean of a healthy reference sample, creating interpretable personalized circuit scores that enable patient stratification.
The imaging protocol should include both task-free (resting-state) and task-evoked conditions. Task-free functional connectivity assesses intrinsic relationships between brain regions, while task-evoked fMRI probes circuit function during specific cognitive and emotional challenges. Emotional tasks typically involve viewing faces with emotional expressions or processing emotionally valenced stimuli, whereas cognitive tasks often assess attention, cognitive control, or working memory [13]. This multi-modal approach captures both the brain's intrinsic organization and its dynamic engagement during psychologically relevant processes.
For data analysis, hierarchical clustering algorithms applied to regional circuit scores can identify coherent biotypes. Validation should include multiple procedures: the elbow method for determining optimal cluster number; simulation-based significance testing of the silhouette index; stability assessment through leave-one-out and leave-20%-out cross-validation; split-half reliability of cluster profiles; and theoretical consistency with established frameworks of circuit dysfunction in depression [13]. This comprehensive validation ensures that identified biotypes reflect meaningful neurobiological distinctions rather than algorithmic artifacts.
Dynamic Functional Connectivity for Enhanced Classification
Traditional static functional connectivity (SFC) analyses, which assume temporal stationarity in correlations between regional BOLD time courses, have limitations in capturing the dynamic nature of brain function in depression. Dynamic functional connectivity (DFC) analyses using sliding-window algorithms reveal time-varying co-activation patterns that provide a more detailed description of interactions in the brain [16].
The DFC analysis protocol involves acquiring resting-state fMRI data with standard parameters (e.g., TR=2000ms, TE=30ms, flip angle=90°, FOV=240mm). Following preprocessing, a sliding-window algorithm calculates functional connectivity in successive time windows throughout the scan duration [16]. A non-linear support vector machine (SVM) classifier with recursive feature elimination (SVM-RFE) can then select optimal feature subsets for classification model development.
This approach has demonstrated remarkable efficacy in distinguishing MDD patients from healthy controls, achieving an area under the curve (AUC) of 0.9913 compared to 0.8685 for SFC-based approaches [16]. The most discriminative connections typically distribute across visual, somatomotor, dorsal and ventral attention, limbic, frontoparietal, and default mode networks, with particular importance of frontoparietal, default mode, and visual network connections [16].
Machine Learning Approaches for Multi-Modal Data Integration
Advanced artificial intelligence systems using local-global multimodal fusion graph neural networks (LGMF-GNN) can integrate functional MRI, structural MRI, and electronic health records to provide objective diagnostic methods [17]. These systems analyze both individual brain regions and population-level data, achieving classification accuracy of 78.75% and AUROC of 80.64% across multi-center cohorts [17].
Such approaches can identify distinct brain connectivity patterns in MDD, including reduced functional connectivity between the left gyrus rectus and right cerebellar lobule VIIB, and increased connectivity between the left Rolandic operculum and right hippocampus [17]. Structural analyses reveal MDD-associated thickness changes at the gray-white matter interface, indicating potential neuropathological conditions or brain injuries [17].
Diagram 1: Circuit Biotype Identification Workflow. This workflow illustrates the standardized protocol for identifying depression biotypes from neuroimaging data, culminating in clinically validated circuit-based classifications.
Visualization of Molecular Pathways and Experimental Workflows
Molecular Pathways Converging on the Synapse
The molecular etiology of depression involves numerous pathways that ultimately converge on synaptic function, representing the closest physical representation of mood, emotion, and consciousness that can be currently conceptualized [12]. The following diagram illustrates how diverse molecular systems interact to influence synaptic neurotransmission in depression.
Diagram 2: Molecular Pathways Converging on Synaptic Dysfunction. This diagram illustrates how diverse molecular systems, influenced by genetic and environmental factors, ultimately converge on synaptic function to produce circuit-level dysregulation and depression symptoms.
Dynamic Functional Connectivity Analysis Pipeline
The analysis of dynamic functional connectivity provides superior classification of MDD patients compared to traditional static approaches. The following workflow outlines the key steps in DFC analysis for depression biotyping.
Diagram 3: Dynamic Functional Connectivity Analysis Pipeline. This workflow outlines the process for analyzing dynamic functional connectivity in depression, resulting in superior classification accuracy compared to static approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Resources for Circuit-Based Depression Studies
| Resource Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Animal Models | Chronic mild stress (CMS), Social defeat, Chronic corticosterone | Study antidepressant response mechanisms; model treatment resistance | BALB/c mice most sensitive to UCMS; C57BL/6 slightly susceptible [14] |
| Genetic Tools | NEGR1, DRD2, CELF4 variants; CRISPR/Cas9 systems | Investigate genetic vulnerability; model specific molecular pathways | SNP-based heritability of MDD ~11.3%; highly polygenic [12] |
| Neuroimaging Protocols | Stanford Et Cere System; sliding-window DFC analysis | Quantify circuit dysfunction; identify biotypes; track treatment response | Combine task-free and task-evoked fMRI; standardized processing essential [13] [16] |
| Rapid-Acting Antidepressants | Ketamine, Psilocybin, NMDA receptor antagonists | Investigate synaptic plasticity mechanisms; fast-acting treatment models | Ketamine affects AMPA receptors, adenosine A1 receptors, L-type calcium channels [15] |
| Molecular Assays | BDNF/TrkB signaling panels; synaptic protein markers | Quantify synaptic plasticity; assess treatment effects | BDNF levels reduced in acute MDD; increase after antidepressant treatment [12] |
| Behavioral Assessments | Forced swim test, Sucrose preference, Social interaction | Model depression-like behaviors; assess treatment efficacy | Correlate with neurobiological measures; multiple tests recommended [14] |
The resources outlined in Table 3 represent essential tools for investigating the circuit basis of depression and developing the proposed taxonomy. Animal models, particularly chronic stress paradigms, enable the study of antidepressant response mechanisms and treatment resistance [14]. Genetic tools allow researchers to investigate the polygenic architecture of depression, with particular focus on genes implicated in synaptic function such as NEGR1, DRD2, and CELF4 [12].
Neuroimaging protocols form the cornerstone of circuit-based taxonomy development, with standardized systems like the Stanford Et Cere enabling quantification of circuit dysfunction at the individual participant level [13]. Complementary DFC analyses provide superior classification accuracy compared to traditional static approaches [16]. Pharmacological tools, particularly rapid-acting antidepressants like ketamine and psilocybin, facilitate investigation of synaptic plasticity mechanisms and fast-acting treatment models [15]. These resources collectively enable a multi-level approach to depression research, linking molecular mechanisms to circuit dysfunction and ultimately to clinical symptom profiles.
The proposed circuit taxonomy for depression represents a paradigm shift from symptom-based classification to neurobiologically-grounded stratification. By linking specific circuit dysfunctions to distinct symptom profiles and treatment outcomes, this approach addresses the profound heterogeneity that has long hampered depression research and treatment development. The identification of six clinically distinct biotypes, defined by unique patterns of task-free and task-evoked circuit dysfunction, provides a validated foundation for precision medicine in psychiatry [13].
Future research must further refine this taxonomy through multi-modal data integration, including genetic, molecular, and circuit-level information. The convergence of diverse molecular pathways on synaptic function [12] suggests that ultimately, effective depression treatments must target these final common pathways to restore circuit homeostasis. Rapid-acting antidepressants like ketamine have demonstrated the therapeutic potential of directly targeting synaptic plasticity mechanisms [15], offering promising directions for future drug development.
For researchers and drug development professionals, this circuit taxonomy provides a framework for designing targeted interventions matched to specific patterns of neurobiological dysfunction. Rather than continuing the "one-size-fits-all" approach that has yielded limited success, the future of depression treatment lies in matching specific circuit dysfunctions with mechanistically-targeted interventions. This approach promises to improve the tragically low remission rates that have characterized conventional antidepressant development, ultimately offering hope for the substantial proportion of patients currently failed by existing treatments.
The prefrontal-amygdala circuit is a fundamental neural system for processing threat, regulating emotional responses, and evaluating ambiguity. In major depressive disorder (MDD) and anxiety disorders, dysregulation of this circuit—particularly a state of functional hyperactivity—is a core neurobiological feature underlying symptoms of negative affect and anxious apprehension. This whitepaper synthesizes current research on the circuit's functional anatomy, quantitative signatures of its dysregulation, and detailed experimental methodologies for its investigation, framed within the context of identifying biomarkers for antidepressant response. Understanding these circuit-level changes is critical for developing targeted, mechanistically-informed treatments for mood and anxiety disorders.
Functional Neuroanatomy of the Prefrontal-Amygdala Circuit
The prefrontal-amygdala circuit integrates subcortical regions for rapid emotional processing with prefrontal areas for higher-order cognitive control. The amygdala, an almond-shaped structure in the medial temporal lobe, is comprised of subnuclei including the basolateral nucleus (BLA) and central nucleus (Ce), which have distinct functions and connectivity [18]. The amygdala detects biologically salient stimuli, orchestrates fear responses, and encodes ambiguity in the environment [19].
The medial prefrontal cortex (mPFC) is roughly divided into dorsal (dmPFC) and ventral (vmPFC) subregions relative to the corpus callosum's genu. The dmPFC (including supragenual anterior cingulate) mediates cognitive control, conflict monitoring, and emotion regulation. The vmPFC (including subgenual anterior cingulate and medial orbitofrontal cortex) facilitates fear extinction, value comparison, and social cognition [19] [18].
Anatomically, the mPFC and amygdala share reciprocal connections. The amygdala sends robust efferent projections to the mPFC, which are heavier than the reciprocal cortical afferents. The mPFC provides top-down regulation of amygdala output, primarily through inputs to the BLA and intercalated cells that inhibit BLA projections to the Ce, thereby dampening fear expression [18]. In humans, the structural integrity of this white matter pathway can be quantified using Diffusion Tensor Imaging (DTI) to measure fractional anisotropy [18].
Figure 1: Prefrontal-Amygdala Circuit Pathways. The dmPFC and vmPFC provide top-down regulation of amygdala output, particularly through inhibition of the basolateral amygdala (BLA) to central nucleus (Ce) pathway, which governs fear expression and autonomic responses.
Quantitative Signatures of Circuit Hyperactivity
Aberrant Functional Connectivity Patterns
Hyperactivity in the prefrontal-amygdala circuit manifests as altered directionality and strength of functional coupling, measurable with fMRI. In healthy individuals, stronger negative coupling between the amygdala and vmPFC typically correlates with better emotional regulation and lower anxiety. In pathological states, this coupling becomes dysregulated, showing either exaggerated negative connectivity or a reversal to positive coupling, indicating failed inhibitory control [20] [19] [18].
Table 1: Functional Connectivity Patterns in Prefrontal-Amygdala Circuitry
| Population / Condition | Amygdala-dmPFC Connectivity | Amygdala-vmPFC Connectivity | Behavioral Correlation |
|---|---|---|---|
| Healthy Adults | Moderate negative coupling during emotional tasks [19] | Strong negative coupling during threat safety discrimination [20] | Lower anxiety; better emotion regulation [18] |
| Anxious Adults | Increased positive coupling during threat appraisal [20] | Reduced negative/positive coupling during extinction recall [20] | Impaired threat-safety discrimination; higher anxiety [20] |
| Anxious Youth | Exaggerated negative coupling during threat appraisal [20] | More negative coupling during extinction recall [20] | Developmental disruption of emotion regulation [20] |
| MDD Patients | Altered effective connectivity with frontolimbic network [21] | Reduced inhibitory control [19] | Severity of anhedonia and depressed mood [4] |
| Early Life Stress (Mouse Model) | Hyperconnectivity [22] | Hyperconnectivity [22] | Increased anxiety-like behavior in open-field test [22] |
Neural Signatures of Emotion Ambiguity Processing
Processing ambiguous emotional stimuli particularly engages the prefrontal-amygdala circuit. Single-neuron recordings in neurosurgical patients show that amygdala neurons respond earlier than dmPFC neurons to emotion ambiguity, reflecting a bottom-up affective process for ambiguity representation. This is followed by dmPFC engagement, reflecting top-down cognitive processes for ambiguity resolution. In MDD and anxiety disorders, this temporal dynamics are disrupted, leading to biased interpretation of ambiguous stimuli as threatening [19].
Table 2: Quantitative fMRI and Metabolic Findings in Circuit Hyperactivity
| Brain Region | Metric | Healthy Controls | MDD/Anxiety Patients | Experimental Paradigm |
|---|---|---|---|---|
| Right Amygdala | Task-based activation (post-treatment change) | N/A | Consistent decrease with successful treatment (peak MNI: 30, 2, -22) [23] | Emotion face processing tasks |
| Amygdala-vmPFC Circuit | Effective connectivity (DCM) | Balanced bottom-up/top-down | Aberrant connections to VMPFC, sgACC, NAC [21] | Resting-state fMRI |
| Amygdala-Hippocampus | Resting-state functional connectivity (rs-fMRI) | Normal range correlation | Hyperconnectivity in early stress models [22] | Rodent rsfMRI |
| dlPFC-sgACC | Theta burst stimulation response | N/A | Normalized connectivity with treatment response [21] | SAINT rTMS protocol |
Experimental Protocols for Circuit Investigation
Human Neuroimaging Protocols
Task-Based fMRI for Threat-Safety Discrimination
- Purpose: To assess amygdala-prefrontal dynamics during extinction recall and threat appraisal [20]
- Participants: Anxious vs. healthy cohorts across developmental stages (youth vs. adults)
- Task Design: Extinction recall paradigm with three attention conditions:
- Threat Appraisal: Evaluate how threatening a stimulus is
- Explicit Threat Memory: Recall previously learned threat associations
- Physical Discrimination: Perceptual judgment of stimulus characteristics (control condition)
- fMRI Acquisition: 3T scanner, T2*-weighted echo planar imaging, standardized parameters (e.g., TR=2000ms, TE=30ms, voxel size=3×3×3mm)
- Analysis: Generalized psychophysiological interaction (gPPI) to test task-dependent functional connectivity with anatomically-defined amygdala seeds
- Statistical Modeling: Whole-brain analyses with ANOVA examining interactions between anxiety diagnosis, age group, and attention task
Dynamic Causal Modeling (DCM) for Effective Connectivity
- Purpose: Estimate causal relationships among depression-related regions [21]
- Participants: Large sample sizes (e.g., 270 healthy controls, 175 MDD patients) for adequate power
- Data Acquisition: Multi-site resting-state fMRI with standardized protocols
- ROI Selection: Focus on regions functionally connected to left DLPFC: amygdala, nucleus accumbens, anterior insula, sgACC, and VMPFC
- Model Specification: Define a priori model of network architecture based on depression circuitry literature
- Parameter Estimation: Bayesian inversion to estimate directed connectivity between regions
- Statistical Analysis: Parametric empirical Bayes for between-group comparisons (MDD vs. controls)
Animal Model Protocols
Unpredictable Postnatal Stress (UPS) Model
- Purpose: Investigate effects of early-life stress on amygdala-prefrontal connectivity and anxiety-like behavior [22]
- Subjects: C57BL/6 mice, with precise genetic background control
- Stress Paradigm: From postnatal days 1-14, expose pups to unpredictable stressors in a variable sequence:
- Cage tilting
- Wet bedding
- Social isolation
- Predator odor
- Light cycle alterations
- Behavioral Testing: In juvenile and adult stages, using:
- Open-field test (anxiety-like behavior)
- Elevated plus maze (anxiety-like behavior)
- rsfMRI Acquisition: In adult males, under isoflurane anesthesia
- Connectivity Analysis: Seed-based correlation focusing on amygdala-prefrontal and amygdala-hippocampus pathways
- Correlation Analysis: Relationship between connectivity strength and anxiety-like behavior metrics
Figure 2: Unpredictable Postnatal Stress Experimental Workflow. This protocol induces frontolimbic hyperconnectivity and anxiety-like behavior in mouse models, mimicking features of human anxiety and depression.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources
| Resource Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Animal Models | Unpredictable Postnatal Stress (UPS) mice [22] | Early life stress research | Induces amygdala-prefrontal hyperconnectivity |
| Chronic Mild Stress (CMS) models [14] | Depression pathophysiology & treatment response | Models anhedonia & antidepressant response | |
| Genetic Tools | BALB/c vs C57BL/6 mouse strains [14] | Stress susceptibility studies | Differential sensitivity to UCMS procedures |
| Neuroimaging Databases | DecNef Project Brain Data Repository [21] | Multi-site fMRI studies | Large-sample, standardized neuroimaging data |
| SRPBS dataset (AMED) [21] | MDD biomarker discovery | Japanese population neuroimaging data | |
| Behavioral Paradigms | Fear extinction recall with attention modulation [20] | Threat processing in anxiety | Tests anxiety & age effects on amygdala-PFC coupling |
| Fear-happy morph emotion judgment [19] | Emotion ambiguity processing | Assesses amygdala-dmPFC-vmPFC network dynamics | |
| Analysis Tools | Generalized Psychophysiological Interaction (gPPI) [20] | Task-based functional connectivity | Measures context-dependent connectivity changes |
| Dynamic Causal Modeling (DCM) [21] [19] | Effective connectivity estimation | Models directional influences between brain regions | |
| Graph Neural Networks (GNNs) [4] | Treatment response prediction | Integrates multimodal data for outcome prediction |
Implications for Antidepressant Response Research
Circuit-level dysfunction in the prefrontal-amygdala pathway represents a promising biomarker for predicting and monitoring treatment response in depression and anxiety disorders. A 2025 meta-analysis of task-based fMRI studies across 302 depressed patients revealed that successful treatment with various modalities (pharmacotherapy, psychotherapy, ECT, psilocybin, ketamine) consistently normalizes hyperactivity in the right amygdala (peak coordinates: 30, 2, -22) [23]. This convergence suggests that despite different mechanisms of action, effective treatments share a common neural pathway of dampening amygdala hyperreactivity.
Advanced computational approaches are now leveraging these circuit biomarkers to predict individual treatment outcomes. Hierarchical graph neural network (GNN) models integrating baseline neuroimaging and clinical features can predict SSRI remission with 76.21% accuracy by analyzing dysfunction in reward and emotion regulation circuits [4]. Key contributing regions include the amygdala, hippocampus, thalamus, and anterior cingulate gyrus, highlighting the importance of distributed circuit-level assessment rather than single-region biomarkers.
Neuromodulation treatments specifically target this dysregulated circuitry. Repetitive TMS applied to the left DLPFC exerts its antidepressant effects by remotely modulating the broader depression network, including amygdala, sgACC, VMPFC, and nucleus accumbens [21]. The recently developed SAINT protocol uses accelerated intermittent theta burst stimulation to normalize causal connections between the sgACC, anterior insula, and amygdala, demonstrating how precise circuit targeting can enhance treatment efficacy [21].
The directionality of amygdala-prefrontal connectivity may also serve as a treatment selection biomarker. Patients with predominantly bottom-up amygdala-driven pathology may respond better to treatments that directly target amygdala hyperactivity (e.g., ketamine), while those with top-down regulatory deficits may benefit more from prefrontal-focused interventions (e.g., rTMS, cognitive remediation therapy) [19] [24]. This circuitry-based stratification approach represents a promising path toward personalized neurotherapeutics for depression and anxiety disorders.
The hippocampus and nucleus accumbens (NAc) form a critical neural circuit within the brain's limbic system, integrating cognitive processes with motivational and reward pathways. In major depressive disorder (MDD), and particularly in its melancholic and anhedonic subtypes, dysfunction of this circuit is increasingly recognized as a core neurobiological feature. This whitepaper synthesizes current research demonstrating how hypoactivity within the hippocampus-NAc pathway contributes to the pathophysiology of anhedonia—the diminished capacity to experience pleasure—and explores the implications of these findings for antidepressant development and circuit-based therapeutics.
Converging evidence from preclinical models and human neuroimaging reveals that chronic stress induces maladaptive plasticity and functional deficits in this circuit, disrupting reward processing and approach behavior. The ventral hippocampus (vHPC), through its glutamatergic projections to the NAc shell, plays a particularly crucial role in resolving approach-avoidance conflicts and guiding reward-seeking behaviors. When this circuit becomes hypoactive, it produces a behavioral bias toward avoidance and diminished motivation for rewards, clinically manifesting as anhedonia. Understanding these mechanisms provides a foundation for developing targeted interventions that normalize circuit function for patients with treatment-resistant depression.
Anatomical and Functional Basis of the Hippocampus-NAc Circuit
Circuit Architecture and Connectivity
The hippocampus-NAc circuit originates primarily from the ventral region of the hippocampus (anterior in humans), which projects strongly to the shell subregion of the NAc via glutamatergic pathways [25] [26]. This pathway represents a key anatomical substrate through which cognitive and contextual information from the hippocampus modulates motivated behavior through the striatal reward system. The vHPC-NAc shell projection predominantly targets GABAergic medium spiny neurons in the NAc, which integrate these hippocampal inputs with signals from prefrontal cortex, amygdala, and ventral tegmental area to regulate behavioral output [27].
The circuit exhibits functional topography, with the vHPC-NAc pathway specifically implicated in approach behaviors during motivational conflict. Chemogenetic inhibition of this pathway increases decision-making time and promotes avoidance bias when animals face stimuli with competing positive and negative valences [25] [26]. This demonstrates its critical role in arbitrating approach-avoidance conflicts—a process fundamentally disrupted in anhedonia.
Functional Role in Reward Processing and Motivation
The vHPC-NAc circuit functions as a contextual reward integrator, translating learned environmental associations into motivated action selection. During reward-seeking behavior, neuronal populations in the vHPC and NAc exhibit coordinated activation patterns that predict and guide reward choices [28]. In stress-resilient animals, these circuits show robust discrimination between different reward options, whereas susceptible animals display altered dynamics characterized by impaired reward discrimination and enhanced "switch-stay" intention states [28].
Table 1: Key Functional Attributes of the Hippocampus-NAc Circuit
| Functional Attribute | Biological Substrate | Behavioral Manifestation |
|---|---|---|
| Approach-avoidance arbitration | vCA1 to NAc shell projections | Resolution of motivational conflict |
| Reward valuation | Integrated hippocampal-accumbens activity | Preference for high-value rewards |
| Contextual reward learning | Hippocampal contextual input to NAc | Environment-appropriate reward seeking |
| Motivational drive | Glutamatergic excitation of NAc neurons | Sustained goal-directed behavior |
Mechanisms of Circuit Dysfunction in Anhedonia
Stress-Induced Hypoactivity and Synaptic Deficits
Chronic stress exposure, a key predisposing factor for depression, induces structural and functional maladaptations in the hippocampus-NAc circuit. In animal models of depression, chronic unpredictable mild stress (CUMS) significantly reduces hippocampal high gamma oscillation power and synaptic spine density in both hippocampus and NAc-projecting regions [27]. These morphological changes correlate with behavioral manifestations of anhedonia, including reduced sucrose preference and social interaction.
At the molecular level, stress-induced circuit hypoactivity involves impaired neurotrophic signaling and synaptic protein synthesis. CUMS reduces expression of brain-derived neurotrophic factor (BDNF), postsynaptic density protein-95 (PSD-95), and phosphorylation of key signaling molecules in the AKT/mTOR pathway [27]. This pathway is essential for protein synthesis-dependent synaptic plasticity, and its disruption provides a mechanistic link between stress exposure and circuit hypoactivity.
Altered Neural Dynamics in Reward Processing
Recent high-density electrophysiology studies reveal distinctive population-level neural signatures in the hippocampus-NAc circuit that differentiate stress-resilient from susceptible animals. When actively seeking rewards, resilient animals exhibit robust discrimination between reward choices in ventral hippocampal and basolateral amygdala activity patterns [28]. In contrast, susceptible animals show a rumination-like signature characterized by enhanced encoding of intention to switch or stay on a previously chosen reward, reflecting maladaptive decision-making processes underlying anhedonic behavior [28].
During rest periods, susceptible animals display a greater number of distinct neural population states in spontaneous activity, allowing researchers to decode stress history and susceptibility status with greater accuracy than from behavioral measures alone [28]. This suggests that circuit-level biomarkers may provide more sensitive indicators of anhedonic vulnerability than traditional behavioral assessments.
Quantitative Evidence from Preclinical and Clinical Studies
Preclinical Findings on Circuit Manipulations
Table 2: Experimental Evidence from Preclinical Studies of the Hippocampus-NAc Circuit
| Experimental Manipulation | Model System | Key Quantitative Findings | Behavioral Outcome |
|---|---|---|---|
| Chemogenetic inhibition of vCA1-NAc shell pathway | Long Evans rats [25] [26] | ↓ c-Fos+ cells in NAc shell (p<0.001); No change in core (p=0.54) | ↑ decision time; ↑ avoidance bias; ↓ social interaction |
| Deep brain stimulation of NAc (NAc-DBS) | CUMS mouse model [27] | Restores high gamma power; ↑ synaptic spine density; ↑ PSD-95, BDNF, p-AKT, p-mTOR | Attenuates depressive-like behaviors |
| vCA1-BLA circuit manipulation | Stress-susceptible mice [28] | Alters population dynamics; enhances reward discrimination | Reverses anhedonic behavior |
| mTOR inhibition with Rapamycin | CUMS mice with NAc-DBS [27] | Blocks NAc-DBS-induced increases in synaptic proteins | Moderates antidepressant effects of DBS |
Human Neuroimaging Evidence
Human neuroimaging studies provide translational validation of preclinical findings, demonstrating functional alterations in the hippocampus-NAc circuit across depressive subtypes. Resting-state functional connectivity (FC) studies reveal that melancholic depression, characterized by profound anhedonia, is associated with increased FC between the NAc and middle frontal gyrus compared to non-melancholic depression [29]. This hyperconnectivity may represent a compensatory mechanism or maladaptive reorganization in response to circuit hypoactivity elsewhere.
Large-scale analyses have identified that altered reward circuit connectivity patterns can stratify patients into distinct biotypes with differential treatment responses. One study classified six biologically distinct subtypes of depression and anxiety based on circuit dysfunction profiles, including patterns of intrinsic connectivity within the default mode, salience, and frontoparietal attention circuits [13]. These biotypes showed distinct symptom profiles and responded differently to pharmacotherapy and behavioral interventions, highlighting the translational potential of circuit-based stratification.
A coordinate-based meta-analysis of treatment studies found that successful intervention across multiple treatment modalities was associated with normalization of right amygdala activity [23], a region interconnected with both hippocampus and NAc, suggesting that downstream effects on extended circuit dynamics may be crucial for therapeutic efficacy.
Methodological Approaches for Circuit Investigation
Experimental Protocols and Workflows
Chronic Unpredictable Mild Stress (CUMS) Protocol: The CUMS paradigm involves exposing animals to a variety of stressors over 14 days, including both short-term stimuli (1-hour restraint, 1-hour cold exposure, 5-minute heat exposure, 4-hour pepper smell exposure, 20-minute cage shaking, 2-minute tail pinch) and long-term stimuli (24-hour food/water deprivation, cage tilting, bedding removal) [27]. Animals are exposed to randomly selected stimulus combinations daily, preventing habituation. Behavioral assessments (sucrose preference, social interaction, forced swim) are conducted pre- and post-stress, with neurobiological measures taken post-mortem.
Circuit-Specific Neuronal Inhibition: Pathway-specific chemogenetic inhibition involves transducing vCA1 neurons with inhibitory DREADDs (hM4Di-mCherry) via AAV delivery, combined with cannula implantation in NAc shell for later microinfusion of CNO or saline [25] [26]. After recovery, animals undergo behavioral testing during which CNO administration selectively inhibits the vCA1-NAc pathway. Control groups receive empty vector (GFP) with similar CNO administration. Efficacy of manipulation is verified through c-Fos immunohistochemistry and histological confirmation of electrode placements.
Deep Brain Stimulation Parameters: For NAc-DBS, electrodes are implanted bilaterally in the Nac core using stereotaxic surgery [27]. After recovery from CUMS exposure, animals receive high-frequency stimulation (typically 100-200 Hz, 100-200 μA, 60-100 μs pulse width) for specified periods. Control groups undergo sham stimulation with implanted electrodes but no current delivery. Behavioral tests are conducted during and after stimulation periods, followed by electrophysiological recordings and molecular analyses.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents for Investigating the Hippocampus-NAc Circuit
| Reagent/Solution | Primary Function | Application Examples |
|---|---|---|
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic control of neuronal activity | Pathway-specific inhibition of vCA1-NAc projections [25] [26] |
| AAV Vectors (Serotypes 1, 5, 8) | Targeted gene delivery to specific cell populations | Expression of fluorescent reporters, optogenetic tools, DREADDs in circuit neurons |
| Clozapine N-Oxide (CNO) | Pharmacological activation of DREADDs | Selective inhibition of hM4Di-expressing neurons during behavioral tasks |
| Neuropixels Probes | High-density electrophysiology recording | Simultaneous monitoring of hundreds of neurons in BLA and vCA1 [28] |
| Rapamycin | Specific mTOR pathway inhibition | Blocking protein synthesis-dependent synaptic plasticity [27] |
| Golgi-Cox Staining Solution | Neuronal morphology visualization | Quantifying dendritic spine density and complexity [27] |
| c-Fos Antibodies | Neural activity mapping | Identifying recently activated neurons following behavioral tasks |
Signaling Pathways Mediating Circuit Plasticity
The AKT/mTOR/BDNF signaling pathway has been identified as a crucial molecular mechanism underlying synaptic plasticity in the hippocampus-NAc circuit and its response to neuromodulation [27]. Under normal conditions, activity-dependent BDNF release activates AKT, which in turn stimulates mTOR-mediated protein synthesis, leading to enhanced synaptic spine formation and strengthened circuit connectivity.
In depression models, chronic stress reduces BDNF expression and decreases phosphorylation of AKT and mTOR, resulting in synaptic spine loss and circuit hypoactivity. Deep brain stimulation of the NAc reverses these effects, potentially through increased BDNF protein expression and activation of the AKT/mTOR signaling pathway [27]. The specific mTOR inhibitor rapamycin blocks these synaptic and behavioral effects, confirming the pathway's essential role.
Implications for Therapeutic Development
Circuit-Targeted Interventions
The delineation of hippocampus-NAc circuit dysfunction in anhedonia opens promising avenues for targeted therapeutic development. Deep brain stimulation of the NAc has demonstrated efficacy in reversing both behavioral and neurobiological correlates of anhedonia in preclinical models [27]. Clinical studies of NAc-DBS for treatment-resistant depression have reported symptom improvement, particularly for anhedonic features [29].
Emerging brain-circuit-based biotyping approaches offer a framework for personalizing these interventions. By stratifying patients according to distinct patterns of circuit dysfunction, including hippocampus-NAc connectivity profiles, clinicians may better match individuals to optimal treatments [13]. For example, patients with prominent hypoactivity in reward circuits might preferentially benefit for interventions that directly target these pathways.
Biomarker Development and Personalized Approaches
Quantitative electroencephalography (QEEG) and functional connectivity measures show promise as translational biomarkers for circuit dysfunction. QEEG patterns such as frontal alpha asymmetry and altered gamma band power may provide accessible proxies for hippocampus-NAc circuit function [30]. Similarly, resting-state fMRI measures of NAc connectivity with hippocampal and frontal regions can identify patient subtypes most likely to respond to targeted treatments [31] [29].
Advanced computational approaches, including graph neural networks applied to neuroimaging data, are improving prediction of treatment response based on circuit dysfunction patterns [4]. These methods can integrate multiple data modalities to identify complex, multivariate signatures of circuit dysfunction that transcend traditional diagnostic boundaries.
The hippocampus-NAc circuit represents a critical nexus where cognitive, contextual, and emotional information converges to guide motivated behavior. Hypoactivity within this circuit, induced by chronic stress and mediated through impaired neurotrophic signaling and synaptic plasticity, underlies the profound reward processing deficits characteristic of anhedonia in depression.
Recent methodological advances in circuit-specific manipulation and population-level neural dynamics analysis have provided unprecedented insight into the mechanisms of circuit dysfunction and recovery. The development of circuit-based biotypes and targeted neuromodulation approaches holds promise for more effective, personalized interventions for treatment-resistant depression. Future research should focus on translating these preclinical findings into clinical applications, particularly for patients whose anhedonic symptoms remain refractory to conventional treatments.
The Default Mode Network (DMN), a large-scale brain network active during rest and self-referential thought, has emerged as a critical neural substrate in the pathophysiology of major depressive disorder (MDD). Its intuitive link to depressive rumination—a recurrent, self-reflective, and often uncontrollable focus on one's depressed mood and its causes—has positioned it as a primary focus in the search for neural circuitry changes underlying depression [32]. A core and replicated finding in this domain is DMN hyperconnectivity, an aberrant increase in functional connectivity between its constituent regions and with other neural structures, which often predicts levels of depressive rumination [32]. This whitepaper synthesizes current evidence on DMN hyperconnectivity, detailing its quantitative characterization, its specific association with ruminative processes, and its implications for antidepressant response research, thereby framing it within the broader context of neural circuitry changes in depression.
Quantitative Characterization of DMN Hyperconnectivity in MDD
Meta-analyses of resting-state functional magnetic resonance imaging (rs-fMRI) studies provide robust evidence for specific patterns of aberrant DMN connectivity in MDD. The hyperconnectivity is not global but involves distinct pathways, particularly those integrating the DMN with limbic regions.
Table 1: Reliably Increased Functional Connectivity in MDD from Meta-Analysis
| Connected Regions | Nature of Connectivity Change | Association with Symptomatology |
|---|---|---|
| DMN Subgenual Prefrontal Cortex (sgPFC) | Reliably increased functional connectivity | Often predicts higher levels of depressive rumination [32] |
| DMN Medial-Dorsal Thalamus (MDT) | Reliably increased functional connectivity | Implicated in information integration [32] |
| DMN Dorsal Anterior Cingulate Cortex (dACC) | Reliably increased functional connectivity | Part of the salience network [32] |
| Posterior Cingulate Cortex (PCC) sgACC | Higher ROI-to-ROI FC in antidepressant responders | Suggests role in treatment response [33] |
Furthermore, the dynamics of DMN connectivity are also impaired in MDD. A two-sample confirmation study demonstrated greater connectivity variability between the medial prefrontal cortex (mPFC) and the posterior cingulate cortex (PCC) in MDD patients compared to healthy controls. This finding, replicated across two independent samples, indicates that alterations within the DMN in MDD extend beyond static connectivity strength to include reduced temporal stability [34].
Table 2: Dynamic Functional Connectivity Changes in the DMN in MDD
| Connectivity Measure | Finding in MDD | Interpretation |
|---|---|---|
| mPFC-PCC Connectivity Stability | Reduced stability (increased variability) over time [34] | Reflects a fluctuating, unstable DMN subsystem critical for self-referential thought |
| Global DMN Connectivity | Increased spatial promiscuity (hypoalignment) with underlying structure [35] | Suggests a less specialized and more disorganized network |
The Functional Neural Ensemble: Integrating the DMN and Subgenual PFC
The persistent observation of DMN-sgPFC hyperconnectivity has led to an integrated neural model of rumination. This model posits that increased functional connectivity between these regions represents the formation of a pathological functional neural ensemble [32].
In this model:
- The DMN supports self-referential processes and the internal generation of thoughts.
- The sgPFC is associated with affectively laden, behavioral withdrawal, and negative affect.
Their hyperconnectivity in MDD integrates these functions, creating a circuit uniquely suited to support depressive rumination: a persistent, negative, and self-focused pattern of thinking. This integrated ensemble is thought to abnormally tax the sgPFC, explaining the regional cerebral blood flow abnormalities observed there, while the core DMN nodes may not exhibit similar metabolic abnormalities [32]. The model is illustrated in the following functional pathways diagram.
Methodological Approaches for Investigating DMN-Rumination Pathways
Research into DMN hyperconnectivity relies on a suite of advanced neuroimaging and analysis protocols. The following workflow outlines a standard experimental pipeline for acquiring and analyzing resting-state fMRI data to investigate these pathways, from participant recruitment to statistical modeling.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for DMN Rumination Studies
| Tool Category | Specific Examples & Functions | Application in DMN Research |
|---|---|---|
| Clinical Characterization | Structured Clinical Interview for DSM-5 (SCID-5): Gold-standard diagnostic tool. | Ensures cohort purity for MDD patients and healthy controls (HCs) [36]. |
| Symptom Quantification | Rumination Response Scale (RRS): 22-item self-report measure of trait rumination. Perseverative Thinking Questionnaire (PTQ): 15-item measure of repetitive negative thought. | Provides quantitative behavioral correlate for connectivity analysis [34] [36]. |
| fMRI Acquisition & Denoising | Multi-Echo ICA (ME-ICA): Advanced denoising for removing non-BOLD artifacts. RETROICOR: Physiological noise correction for cardiac/respiratory signals. | Improves data quality and specificity of functional connectivity measures [34]. |
| Connectivity Analysis Software | FSL (FEAT, MELODIC), AFNI, SPM, CONN: Software packages for preprocessing and analyzing fMRI data. | Enables seed-based correlation, ICA, and network-level statistics [34]. |
| Advanced Analysis Algorithms | Nadam-Accelerated SCAlable and Robust (NASCAR) tensor decomposition: Identifies group-level networks. BrainSync: Temporally synchronizes rs-fMRI data across subjects. | Used for high-resolution mapping of DMN subcortical connectivity [37]. |
DMN Connectivity as a Biomarker for Predicting Antidepressant Response
The role of DMN hyperconnectivity extends beyond a mere correlate of symptoms to a potential biomarker for predicting treatment outcomes. A recent meta-analysis of 16 studies and 892 MDD patients investigated the predictive power of baseline rsFC on intervention outcomes [38].
Key findings include:
- Within-DMN rsFC: Demonstrated a significant pooled predictability for antidepressant outcomes (pooled r = 0.207, p < 0.001), suggesting that higher baseline connectivity within the DMN is associated with better response to pharmacotherapy [38].
- DMN-Frontoparietal Network (FPN) rsFC: Showed a differential predictive effect, with a stronger negative correlation (pooled r = -0.215, p < 0.001) for outcomes following non-invasive brain stimulation (e.g., TMS) [38]. This implies that weaker anti-correlation between the DMN and FPN at baseline predicts better response to these interventions.
Furthermore, a 2025 rs-fMRI study found that antidepressant responders exhibited significantly higher functional connectivity between the posterior cingulate cortex (PCC) and the subgenual anterior cingulate cortex (sgACC) at baseline compared to non-responders [33]. This underscores the importance of specific DMN-limbic pathways in mediating treatment effects.
Evidence consistently implicates DMN hyperconnectivity, particularly with limbic regions like the sgPFC, as a core neural substrate of rumination in MDD. This dysfunction manifests as both increased static connectivity and abnormal temporal dynamics, contributing to the persistent, negative self-referential thought that characterizes the disorder. The reconceptualization of this abnormality as a maladaptive functional ensemble provides a powerful framework for understanding the neurobiology of depression.
The translation of this knowledge into clinical applications is progressing. The predictive relationship between baseline DMN connectivity and treatment outcome heralds a future of precision psychiatry, where neuroimaging biomarkers guide intervention selection [38]. Simultaneously, the DMN itself is becoming a direct target for novel neuromodulation therapies. Promisingly, a 2025 clinical trial demonstrated that transcranial Focused Ultrasound (tFUS) targeting the anterior medial prefrontal cortex (aDMN hub) significantly reduced depression symptoms and repetitive negative thought [36]. This approach leverages the funnel effect of subcortical structures, where targeted neuromodulation of a small nucleus can widely influence cortical networks [37]. Future research, incorporating control arms and mechanistic neuroimaging, will be crucial to fully ascertain the causal role of DMN modulation in treating depression and disrupting the cycle of rumination.
Dysregulation within the salience network (SN) and negative affect circuits constitutes a core transdiagnostic feature of mood and anxiety disorders, fundamentally driving maladaptive behaviors such as anxious avoidance [39]. The SN, primarily comprising the anterior insula (aINS), dorsal anterior cingulate cortex (dACC), and ventrolateral prefrontal cortex (vlPFC), is responsible for detecting salient stimuli and coordinating autonomic, cognitive, and attentional responses [39]. Its function is dynamically modulated by subcortical regions, including the amygdala and the periaqueductal gray (PAG), which are central to processing threat and negative emotions. In healthy states, these circuits work in concert to facilitate adaptive behavior. However, in conditions like major depressive disorder (MDD) and anxiety disorders, aberrant effective connectivity among these regions leads to a biased processing of negative emotional events, heightened salience attribution to potential threats, and a behavioral tendency towards avoidance, which is a hallmark of pathological anxiety [39] [40]. This whitepaper synthesizes recent neuroimaging and computational evidence to delineate the mechanisms of this dysregulation and places these findings within the broader context of neural circuitry changes in depression and antidepressant response research.
Mechanistic Framework of Circuit Dysregulation
Recent ultra-high field neuroimaging studies provide compelling evidence for a mechanistic model in which inhibitory control over the salience network is disrupted. A 2025 study using dynamic causal modeling (DCM) on 7-Tesla fMRI data revealed a critical breakdown in the PAG-to-aINS inhibitory pathway in individuals with mood and anxiety disorders [39]. In healthy controls, the PAG exerts a tonic inhibitory influence on the aINS, which is essential for modulating interoceptive inference and preventing the oversalience of negative emotional stimuli. This effect was absent in the clinical group, with a posterior probability of 1.00 [39].
Concurrently, there is a strengthening of bottom-up excitatory drives. The same study found group differences in modulatory amygdala-to-PAG connections and intrinsic PAG self-inhibition [39]. This suggests a model where heightened amygdala activity, a consistent finding in depression meta-analyses [23], combines with disinhibited SN activity, leading to the characteristic cognitive and affective symptoms of these disorders. This circuit-based dysfunction aligns with the predictive processing framework, wherein psychopathology arises from a failure to down-weight the precision of interoceptive signals, resulting in false inferences about bodily states and their emotional causes [39].
Table 1: Key Neural Circuits in Salience and Negative Affect Dysregulation
| Brain Region/Circuit | Primary Function | Dysregulation in Mood/Anxiety Disorders |
|---|---|---|
| Salience Network (SN) | Detects salient stimuli; coordinates cognitive & autonomic response | Hyperactivity & maladaptive salience attribution to negative stimuli [39] |
| Anterior Insula (aINS) | Interoceptive awareness, subjective emotional experience | Loss of inhibitory control from subcortical regions [39] |
| Dorsal Anterior Cingulate (dACC) | Conflict monitoring, autonomic regulation | Altered engagement during negative emotional processing [39] |
| Amygdala | Threat detection, negative emotion generation | Increased activity & altered functional connectivity with SN [39] [23] |
| Periaqueductal Gray (PAG) | Coordinating autonomic arousal & defensive behaviors | Disrupted inhibitory projections to aINS; intrinsic self-inhibitory connections [39] |
| Amygdala-PAG-aINS Pathway | Bottom-up influence on salience processing & autonomic gain | Bi-directional interactions are disrupted, contributing to maladaptive affective response [39] |
Quantitative Synthesis of Neuroimaging Findings
Meta-analytic evidence consolidates findings across multiple treatment modalities, highlighting the right amygdala as a critical convergence point for depression treatment effects. A 2025 coordinate-based meta-analysis of 18 task-based fMRI studies encompassing 302 depressed patients revealed the right amygdala as a consistent region of change following various treatments, including pharmacology, psychotherapy, electroconvulsive therapy, psilocybin, and ketamine [23]. Follow-up analyses indicated that this change was primarily characterized by a decrease in amygdala activity post-treatment [23].
Furthermore, quantitative syntheses directly contrasting treatment modalities reveal distinct neural change patterns. A 2021 meta-analysis contrasting the neural effects of antidepressant medication and psychotherapy found that these treatments evoke changes in anatomically distinct regions. Antidepressants primarily modulated activity in the amygdala, whereas psychotherapy evoked changes in the medial prefrontal cortex [41]. Despite their different points of action, both treatment-related changes converged on the brain's affect network [41]. These findings underscore that the amygdala is not only a key node in the pathophysiology of negative affect but also a primary substrate for treatment-induced normalization.
Table 2: Neural Changes Associated with Treatment Response
| Treatment Modality | Key Brain Regions/Networks Affected | Nature of Change | Source |
|---|---|---|---|
| Various (Pharmacology, Psychotherapy, ECT, etc.) | Right Amygdala | Consistent decrease in activity post-treatment across modalities | [23] |
| Antidepressant Medication | Amygdala | Evokes neural changes in this subcortical structure | [41] |
| Psychotherapy | Medial Prefrontal Cortex | Evokes anatomically distinct changes in this cortical region | [41] |
| SSRIs (Predictive Biomarker) | Right Globus Pallidus, Bilateral Putamen, Left Hippocampus, Bilateral Thalamus, Bilateral Anterior Cingulate | Pre-treatment activity predicts remission with 76.21% accuracy | [4] |
Experimental Protocols & Methodologies
Functional Magnetic Resonance Imaging (fMRI) Paradigms
To probe salience network dysfunction, researchers employ specialized tasks during fMRI scanning. The emotional oddball paradigm is one such robust protocol. In this task, participants view a rapid stream of images consisting of a frequently presented standard image (80% of trials) and infrequent oddball images, which include a target, neutral distractors, and negative emotional distractors [39]. Participants are instructed to identify the target, while the presentation of negative emotional distractors creates a salience processing event. The key measures are neural activation and effective connectivity in response to these negative emotional oddballs. Data are typically acquired using ultra-high field 7-Tesla fMRI to enhance signal resolution in small subcortical structures like the PAG. Pre-processing pipelines must account for physiological noise and head motion, with subsequent analysis using Dynamic Causal Modeling (DCM) to infer the directionality of influence between the amygdala, PAG, and nodes of the SN [39].
Computational Modeling of Avoidance Behavior
The Approach-Avoidance Reinforcement Learning (AARL) task is a translational paradigm designed to quantify the cognitive mechanisms of anxious avoidance [40]. In this computer-based task, participants choose between options that are probabilistically associated with rewards (points or money) and punishments (mild electric shocks or loss of points). Critically, the more rewarding options are also associated with a higher probability of punishment, creating a approach-avoidance conflict. Participants must learn these contingencies through trial-and-error experience, not from explicit instruction.
The behavioral data from the AARL task is analyzed using computational modeling based on reinforcement learning algorithms. A standard model involves estimating individual parameters such as:
- Learning rates (α): How quickly a participant updates the value of a stimulus based on new outcomes.
- Sensitivity to punishment (β~avoid~) vs. reward (β~approach~): The relative weight given to punishing versus rewarding outcomes when making a decision.
Studies using this protocol have shown that individuals with greater task-induced anxiety display higher punishment sensitivity, leading them to avoid potentially rewarding choices that carry a risk of punishment, thereby modeling real-world anxious avoidance [40]. The test-retest reliability of this task has been demonstrated as fair-to-excellent [40].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for Investigating Salience and Avoidance Circuits
| Research Tool | Primary Application/Function | |
|---|---|---|
| 7-Tesla Functional MRI | High-resolution imaging of small subcortical structures (e.g., PAG, amygdala) and functional connectivity. | [39] |
| Dynamic Causal Modeling (DCM) | A Bayesian framework for inferring effective (directed) connectivity between brain regions from fMRI data. | [39] |
| Emotional Oddball Paradigm | An fMRI task protocol to probe neural responses to salient, negative emotional stimuli versus a neutral baseline. | [39] |
| Approach-Avoidance Reinforcement Learning Task | A translational behavioral task to quantify learning and decision-making in the context of reward-punishment conflict. | [40] |
| Computational Models (Reinforcement Learning) | Mathematically formalizes learning and decision processes to estimate latent cognitive parameters (e.g., learning rates, punishment sensitivity). | [40] |
| Activation Likelihood Estimation (ALE) | A coordinate-based meta-analysis algorithm to identify significant convergence of brain activation across multiple neuroimaging studies. | [41] [23] |
Visualizing the Circuitry and Workflows
Effective Connectivity in the Salience Network
Figure 1: A directed graph illustrating the effective connectivity between subcortical nodes and the Salience Network, highlighting the key inhibitory pathway from the PAG to the anterior insula that is disrupted in mood and anxiety disorders.
Predictive Modeling of Antidepressant Response
Figure 2: Workflow of a hierarchical local-global Graph Neural Network (GNN) model that integrates neuroimaging and clinical data to predict individual patient response to SSRI treatment.
The lateral habenula (LHb) is an epithalamic structure that serves as a critical hub, connecting forebrain regions to midbrain monoaminergic centers [42] [43]. Often termed the brain's "anti-reward" or "disappointment" center, the LHb plays a pivotal role in encoding negative motivational values, processing aversive stimuli, and regulating motivational states [44] [43]. Its unique anatomical position enables it to integrate value-based, sensory, and experience-dependent information to fine-tune various motivational, cognitive, and motor processes [43]. In major depressive disorder (MDD), dysregulation of this structure—particularly a state of hyperactivity—has been strongly implicated in the pathophysiology of depressive symptoms, including anhedonia, helplessness, and excessive focus on negative experiences [45]. This whitepaper provides an in-depth examination of the LHb's role in depressive illness, detailing the underlying molecular mechanisms, summarizing key experimental evidence, and presenting essential research methodologies for investigating this promising therapeutic target.
Neuroanatomical Connectivity
The LHb is a small, bilaterally paired neuronal structure located in the posterior-medial aspect of the dorsal thalamus, forming part of the epithalamus alongside the pineal gland [42] [46]. It is phylogenetically highly conserved across vertebrates, underscoring its fundamental role in brain function [42] [46]. The habenula complex is subdivided into medial (MHb) and lateral (LHb) components, each with distinct neuronal populations, input and output pathways, and functional specializations [42].
The LHb receives afferent inputs from several limbic forebrain and basal ganglia structures, establishing it as a convergence point for emotional and motivational information [43]. Key input regions include:
- Lateral preoptic area (bringing input from the hippocampus and lateral septum) [42]
- Ventral pallidum (bringing input from the nucleus accumbens and mediodorsal nucleus of the thalamus) [42]
- Lateral hypothalamus [42]
- Internal segment of the globus pallidus (bringing input from other basal ganglia structures) [42]
The efferent projections of the LHb primarily target midbrain monoaminergic centers, through which it exerts its "anti-reward" functions [42] [43]:
- Dopaminergic regions: Substantia nigra pars compacta and ventral tegmental area (VTA) [42]
- Serotonergic regions: Median raphe and dorsal raphe nuclei [42]
- Cholinergic region: Laterodorsal tegmental nucleus [42]
This complex connectivity pattern positions the LHb as a central regulator of monoaminergic transmission, enabling it to modulate dopamine, serotonin, and norepinephrine systems in response to negative experiences and stimuli [45] [43].
The LHb as an "Anti-Reward" Center
The LHb functions as an "anti-reward" center by encoding negative motivational values and suppressing dopamine and serotonin release when an organism encounters unpleasant events, the absence of expected rewards, or punishment [42] [45]. Neurons in the LHb are 'reward-negative' as they are activated by stimuli associated with unpleasant events, particularly when these are unpredictable [42].
The mechanism involves LHb projections to the rostromedial tegmental nucleus (RMTg), a GABAergic region that inhibits dopaminergic neurons in the VTA [45] [43]. When a reward is smaller than expected or an aversive event occurs, increased LHb firing activates the RMTg, leading to inhibition of dopamine neurons and reduced dopamine release in target regions like the nucleus accumbens [45]. This signaling pathway allows the LHb to encode negative reward prediction errors—discrepancies between expected and actual outcomes [43].
Table 1: Functional Roles of the Lateral Habenula in Reward Processing
| Function | Mechanism | Behavioral Outcome |
|---|---|---|
| Negative Reward Encoding | Increased firing in response to negative outcomes or reward omission | Learning from aversive experiences; avoidance behavior |
| Dopamine Regulation | Inhibition of VTA dopamine neurons via RMTg GABAergic transmission | Reduced motivation and reward-seeking |
| Serotonin Regulation | Inhibition of dorsal raphe serotonergic neurons | Altered mood state and stress responsiveness |
| Decision Making | Integration of negative valence information | Value-based decision making under uncertainty |
LHb Hyperactivity in Depression: Pathophysiological Mechanisms
Neurophysiological Changes in Depressive States
In major depression, the LHb undergoes significant pathophysiological changes characterized primarily by hyperactivity. Preclinical and clinical studies consistently demonstrate increased neuronal firing, particularly burst firing, in the LHb in depressive states [44] [45]. This hyperactivity leads to excessive inhibition of dopaminergic and serotonergic systems, resulting in core depressive symptoms such as anhedonia, helplessness, and low mood [45].
Postmortem studies reveal morphological alterations in the LHb of depressed patients, including reduced volume and decreased total neuron numbers on the right side [42] [44]. Such changes are specific to depression and not observed in other psychiatric conditions like schizophrenia [42]. Neuroimaging studies further support these findings, showing altered activation and connectivity patterns in the habenula complex in depressed individuals [44].
Several molecular mechanisms contribute to LHb hyperactivity in depression:
1. Enhanced Glutamatergic Transmission: Increased excitatory synaptic input to LHb neurons, particularly those projecting to the VTA, has been observed in animal models of depression. This enhanced glutamatergic drive potentiates LHb output and subsequent inhibition of monoaminergic systems [43].
2. Potassium Channel Dysregulation: Downregulation of astrocyte-specific potassium channels (Kir4.1) in the LHb leads to neuronal hyperexcitability. Recent research has implicated Kir4.1 upregulation in postpartum depression models, suggesting a role in hormone-sensitive depressive states [47].
3. Calcium/Calmodulin-Dependent Protein Kinase II (βCaMKII) Upregulation: This key molecular pathway underlies synaptic hyperactivity in the LHb. Upregulated βCaMKII enhances synaptic strength and promotes burst firing in LHb neurons [43].
4. CRH Receptor Activation: The LHb expresses corticotropin-releasing hormone receptor 1 (CRHR1), which is activated by stress. CRH signaling decreases potassium channel abundance, increasing LHb firing rate and contributing to stress-related depressive states [45].
Signaling Pathways in LHb Hyperactivity
The following diagram illustrates key molecular pathways contributing to LHb hyperactivity in depression:
Figure 1: Molecular Pathways Driving LHb Hyperactivity in Depression. This diagram illustrates how stress, βCaMKII upregulation, and enhanced glutamatergic signaling converge to increase LHb burst firing, leading to inhibition of ventral tegmental area (VTA) dopamine (DA) neurons and depressive symptoms. CRH: corticotropin-releasing hormone; Kir4.1: potassium channel.
Quantitative Evidence of LHb Dysfunction in Depression
Research across multiple methodologies has provided compelling quantitative evidence supporting LHb dysfunction in depressive disorders. The table below summarizes key findings from preclinical and clinical studies:
Table 2: Quantitative Evidence of LHb Dysfunction in Depression
| Study Type | Model/Population | Key Findings | Reference |
|---|---|---|---|
| Postmortem Human Studies | Patients with MDD | Reduced LHb volume; decreased neuron count on right side | [42] [44] |
| Functional Neuroimaging | Treatment-resistant depression | Increased metabolic activity and functional connectivity in LHb | [44] [43] |
| Electrophysiology (Rodent) | Chronic mild stress model | Increased burst firing and excitability of LHb neurons | [45] [43] |
| Electrophysiology (Rodent) | Maternal deprivation model | CRH-mediated decrease in potassium channels; increased LHb firing | [45] |
| Molecular Biology (Rodent) | Learned helplessness model | Upregulation of βCaMKII in LHb; enhanced synaptic strength | [43] |
| Clinical Trial | Deep brain stimulation for TRD | Remission of depressive symptoms following LHb DBS | [42] [43] |
Experimental Models and Methodologies for LHb Research
Preclinical Models of Depression
Researchers have developed several sophisticated experimental models to study LHb dysfunction in depression:
Chronic Despair Model of Resistant Depression (CDMRD): This model involves subjecting mice to repeated swim sessions during their active phase, leading to long-lasting increases in immobility time that are resistant to conventional antidepressants [48]. The protocol consists of placing mice in a water tank (25°C) for 10-minute daily sessions for 5 consecutive days, with immobility time analyzed during the first 4 minutes [48]. This model is particularly valuable for studying treatment-resistant depression mechanisms.
Hormone-Simulated Pregnancy (HSP) and Postpartum Depression Model: This model mimics the hormonal fluctuations of pregnancy and postpartum period in rodents [47]. Ovariectomized rats receive subcutaneous injections of estradiol benzoate (2.5 μg) and progesterone (4 mg) daily for 16 days, followed by a high dose of estradiol benzoate (50 μg) alone for 7 days [47]. Withdrawal from these hormones induces depressive-like behaviors, modeling postpartum depression and enabling investigation of hormone-sensitive LHb mechanisms.
Chronic Stress Models: Various chronic stress paradigms, including chronic mild stress, chronic restraint stress, and social stress models, reliably induce LHb hyperactivity and depressive-like behaviors in rodents [43]. These models demonstrate increased neuronal activity, enhanced burst firing, and synaptic potentiation in the LHb following prolonged stress exposure.
Experimental Workflow in LHb Research
The following diagram outlines a comprehensive experimental workflow for investigating LHb function in depression models:
Figure 2: Experimental Workflow for LHb Research. This diagram outlines a multidisciplinary approach combining behavioral assessment, therapeutic intervention, and multiple analytical methods to investigate LHb function in depression models.
The Scientist's Toolkit: Key Research Reagents and Methodologies
Table 3: Essential Research Reagents and Tools for LHb Investigation
| Reagent/Method | Specific Example | Application/Function | Reference |
|---|---|---|---|
| Chemogenetics (DREADDs) | AAV-5/2-hGFAP-hM3D(Gq)-mCherry | Selective activation of LHb astroglia to study glial-neuronal interactions | [48] |
| Viral Vectors | AAV2/5-gfaABC1D-eGFP-ERβ-miRNA | Targeted gene knockdown of specific receptors in LHb | [47] |
| ERβ Agonists | Diarylpropionitrile (DPN) | Selective activation of estrogen receptor beta in LHb | [47] |
| Kir4.1 Antibodies | Anti-Kir4.1 immunohistochemistry | Detection and quantification of astrocytic potassium channels | [47] |
| Calcium Imaging | GCaMP expression in LHb neurons | Real-time monitoring of neuronal population activity | [43] |
| Electrophysiology | Ex vivo patch-clamp recording | Measurement of neuronal firing patterns and synaptic properties | [45] [47] |
| Stereotaxic Surgery | Bilateral cannula implantation | Precise drug delivery to LHb for localized pharmacological manipulation | [47] |
Therapeutic Implications and Antidepressant Mechanisms
Targeting LHb Hyperactivity for Antidepressant Effects
Current evidence suggests that effective antidepressant treatments may work, at least in part, by normalizing LHb hyperactivity:
Ketamine: This rapid-acting antidepressant abolishes N-methyl-D-aspartate receptor (NMDAR)-dependent bursting activity in the LHb [45]. Preclinical studies demonstrate that ketamine blocks LHb burst firing by antagonizing NMDARs, leading to rapid resolution of depressive symptoms [45]. The antidepressant effects appear to be mediated through the conversion of ketamine to hydroxynorketamine (HNK), which enhances presynaptic glutamate release and activates α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptors (AMPARs) [45].
Bright Light Stimulation (BLS): Emerging evidence indicates that BLS exerts antidepressant effects by modulating LHb activity [48]. In rodent models, BLS reduces despair-like behaviors by decreasing bursting activity in specific LHb neuron subpopulations that project to dorsal raphe serotonergic neurons [48]. This effect requires intact rod photoreceptors and involves LHb astroglia [48].
Deep Brain Stimulation (DBS): Clinical studies of treatment-resistant depression patients have demonstrated that DBS of the major afferent bundle (stria medullaris thalami) of the LHb can induce remission of depressive symptoms [42] [43]. This approach directly modulates pathological activity in the LHb circuitry.
Estrogen Receptor β (ERβ) Agonists: Recent research in postpartum depression models shows that ERβ agonists inhibit neuronal bursting activities and block upregulation of Kir4.1 in the LHb, representing a promising hormone-based therapeutic strategy [47].
Integration with Broader Neural Circuitry in Depression
The LHb does not function in isolation but is embedded within a broader network of neural circuits that undergo changes in depression. Neuroimaging studies reveal that antidepressant medications and psychological therapies evoke distinct neural changes, with antidepressants primarily affecting subcortical regions like the amygdala, while psychotherapy preferentially modulates prefrontal regions [41]. Both treatments, however, converge on the brain's affect network [41].
Advanced computational approaches are now being developed to predict treatment response based on pre-treatment neurocircuitry and clinical features. Recent work using graph neural network models has achieved approximately 76% accuracy in predicting remission to selective serotonin reuptake inhibitors (SSRIs) by analyzing circuits related to depressed mood and anhedonia [4]. Key contributing brain regions included the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus [4], highlighting the interconnected nature of reward and emotion regulation circuits in depression treatment response.
The lateral habenula represents a crucial node in the pathophysiology of depression, serving as a conduit through which forebrain regions regulate brainstem monoaminergic systems. Its hyperactivity in depressive states leads to excessive inhibition of dopamine and serotonin systems, resulting in core depressive symptoms. Molecular mechanisms involving potassium channels, calcium signaling, and glutamatergic transmission contribute to this pathological state. Recent advances in understanding LHb function have revealed promising therapeutic targets, with ketamine, bright light stimulation, and novel receptor-specific agonists showing efficacy in normalizing LHb hyperactivity. Future research integrating sophisticated computational approaches with circuit-level manipulations holds promise for developing more targeted and effective treatments for depression, particularly for treatment-resistant forms of the disorder.
Precision Tools for Circuit Dissection: From Optogenetics to Advanced Neuroimaging
The understanding and treatment of major depressive disorder have long been constrained by a fundamental limitation: the inability to establish causal relationships between specific neural circuit activity and behavioral outcomes. Traditional approaches, based largely on correlational observations and pharmacological interventions with widespread actions, have provided limited insight into the precise neural mechanisms underlying depression. The advent of optogenetics and chemogenetics has revolutionized this landscape by providing tools for unprecedented precision in neuroscience. These techniques enable researchers to move beyond association to causation by selectively controlling defined neuronal populations in real-time, thereby illuminating the specific circuit dysfunctions that underlie depressive pathology. By integrating these neuromodulation tools with rodent models of depression, researchers have begun to decipher the neural code of motivation, anhedonia, and despair—core symptoms of depression that have been historically resistant to mechanistic dissection. This technical guide examines how optogenetics and chemogenetics are transforming our understanding of depression's neural substrates and accelerating the development of targeted therapeutic strategies.
Technical Foundations: Optogenetics
Core Principles and Molecular Tools
Optogenetics combines genetic targeting with optical control to achieve millisecond-precision manipulation of neuronal activity [49]. The foundational approach involves introducing genes encoding light-sensitive microbial opsins into specific neuronal populations, typically via viral vector delivery, followed by targeted illumination to modulate activity [50].
The opsin toolbox has expanded considerably beyond initial discoveries, with engineered variants offering enhanced temporal precision, spectral sensitivity, and physiological effects (Table 1).
Table 1: Key Opsin Variants for Neural Circuit Manipulation
| Opsin | Type | Optimal Wavelength | Ion Permeability/Effect | Key Properties and Applications |
|---|---|---|---|---|
| ChR2 | Channelrhodopsin | 460 nm | Cations / Depolarizing | General neuronal excitation; single spike precision at 5-30 Hz [51] |
| ChETA | Channelrhodopsin | 490 nm | Cations / Depolarizing | High-frequency precision (up to 200 Hz); rapid kinetics [50] [51] |
| NpHR | Halorhodopsin | 580 nm | Chloride / Hyperpolarizing | Neuronal inhibition; light-activated chloride pump [49] [51] |
| Jaws | Cruxhalorhodopsin | 600 nm | Chloride / Hyperpolarizing | Enhanced inhibition; red-light sensitivity for deeper tissue penetration [49] [51] |
| SFO/SSFO | Channelrhodopsin | 460 nm (ON)546 nm (OFF) | Cations / Bistable | Sustained depolarization (minutes) after brief light pulse [50] [51] |
| ReaChR | Channelrhodopsin | 590-630 nm | Cations / Depolarizing | Red-shifted variant; superior tissue penetration for deep brain structures [50] |
Experimental Methodology for Depression Research
Implementing optogenetics in depression research requires careful consideration of targeting strategies, light delivery systems, and behavioral integration:
Cell-Type Specific Targeting: Utilizing Cre-recombinase driver lines in combination with Cre-dependent viral vectors (typically adeno-associated viruses) allows for exquisite cell-type specificity [50] [51]. Promoters such as CaMKIIα (targeting excitatory neurons) or synthetic neurospecific promoters enable genetic access to defined populations.
Projection-Specific Circuit Mapping: Double-viral strategies involving anterograde or retrograde tracers combined with opsins enable functional dissection of specific projections between brain regions [51]. For example, expressing ChR2 in medial prefrontal cortex (mPFC) neurons projecting to the dorsal raphe nucleus specifically tests the role of this pathway in motivational deficits [52].
Chronic Light Delivery Systems: Traditional tethered fiber optic systems provide reliable light delivery but can restrict natural behaviors. Recent advances include miniaturized wireless optogenetic devices, microscale LED (μLED) arrays, and tapered fibers that minimize tissue damage while enabling complex behavioral testing [50].
Integration with Depression Models: Optogenetic manipulations are typically performed in conjunction with established rodent models of depression such as chronic social defeat stress (CSDS) or chronic mild stress (CMS), allowing researchers to test whether specific circuit manipulations can prevent, reverse, or mimic depression-like behaviors [51].
Technical Foundations: Chemogenetics
Designer Receptors and Ligand Systems
Chemogenetics, particularly Designer Receptors Exclusively Activated by Designer Drugs (DREADDs), offers a pharmacologically-based approach to neuromodulation that complements optogenetics. While optogenetics provides millisecond precision, chemogenetics operates on a timescale of minutes to hours, making it particularly suitable for studying longer-term neuroadaptations relevant to depression [53] [54].
The most widely adopted DREADD systems are based on engineered human muscarinic receptors that no longer respond to acetylcholine but are activated by otherwise inert synthetic ligands like clozapine-N-oxide (CNO) [53]. The key DREADD variants include:
Table 2: Principal DREADD Systems for Neuromodulation
| DREADD Type | Signaling Pathway | Neuronal Effect | Primary Ligand | Key Applications |
|---|---|---|---|---|
| hM3Dq | Gq-coupled | Increased neuronal firing | CNO/Clozapine | Neuronal excitation; behavioral activation [53] [51] |
| hM4Di | Gi-coupled | Decreased neuronal firing | CNO/Clozapine | Neuronal inhibition; behavioral suppression [53] [51] |
| rM3Ds | Gs-coupled | Increased cAMP signaling | CNO/Clozapine | Modulating synaptic plasticity [51] [54] |
| KORD | Gi-coupled | Decreased neuronal firing | Salvinorin B | Multiplexing with hM DREADDs; orthogonal inhibition [53] [51] |
Experimental Implementation Considerations
Successful implementation of chemogenetics in depression research requires attention to several methodological considerations:
Ligand Selection and Dosing: While CNO remains widely used, evidence indicates that it is back-metabolized to clozapine, which actually activates DREADDs [53] [54]. Next-generation ligands such as deschloroclozapine (DCZ) and JHU37160 (J60) offer improved potency and selectivity [53]. Proper dosing controls are essential, with typical systemic doses ranging from 0.1-3 mg/kg for CNO and lower for newer ligands.
Chronic Modulation Paradigms: For studies modeling antidepressant treatments, chronic chemogenetic activation requires repeated ligand administration over days to weeks [54]. Methods include daily injections, oral administration via drinking water, or implanted minipumps. Each approach has tradeoffs between consistency and invasiveness.
Control Strategies: Critical controls include "empty virus" groups (virus without DREADD insert), ligand-only groups (DREADD-free animals receiving ligand), and vehicle groups to account for non-specific effects [54].
Combination with Behavioral Assays: The temporal profile of DREADDs (onset within 15-30 minutes, duration of several hours) makes them compatible with standard depression behavioral tests such as the forced swim test, sucrose preference test, and social interaction test when administered prior to behavioral assessment [51].
Elucidating Depression Circuitry: Key Findings
Application of optogenetics and chemogenetics has revealed specific roles for defined neural circuits in depressive-like behaviors, moving beyond simplistic "region-based" models to a circuit-based understanding of depression.
Mesolimbic Reward Circuit
The ventral tegmental area (VTA) to nucleus accumbens (NAc) projection, a central component of the brain's reward system, has been extensively studied using these techniques:
VTA-NAc Dopaminergic Pathway: Optogenetic stimulation of VTA dopamine neurons projecting to NAc reverses stress-induced social avoidance and anhedonia in CSDS models [49] [51]. Chemogenetic inhibition of this pathway produces depressive-like behaviors, establishing causality [51].
NAc Medium Spiny Neurons: Opposing roles have been identified for D1- versus D2-type medium spiny neurons in NAc, with optogenetic stimulation of D1-MSNs producing antidepressant-like effects and D2-MSNs stimulation promoting depressive-like states [49].
Prefrontal Circuits
The medial prefrontal cortex (mPFC) integrates cognitive and emotional processing and shows well-documented dysfunction in depression:
mPFC to Dorsal Raphe Nucleus Projection: Optogenetic activation of the mPFC→dorsal raphe pathway increases motivation in challenging situations without affecting general locomotion, specifically addressing the motivational deficits core to depression [52].
mPFC to Lateral Habenula Projection: Stimulation of mPFC projections to the lateral habenula, a region hyperactive in depression, reduces effort expenditure, modeling the decreased motivation seen in depressed patients [52].
Hippocampal-Prefrontal Circuits
The ventral hippocampus (vHip) to mPFC connection regulates emotional processing and shows altered activity in depression:
vHip-mPFC Glutamatergic Transmission: Optogenetic inhibition of vHip pyramidal neurons or their terminals in mPFC produces antidepressant effects, while chronic stimulation induces depressive-like behaviors [50] [51].
Circuit-Based Antidepressant Action: The antidepressant effects of ketamine appear to require activation of the vHip-mPFC pathway, demonstrated through optogenetic inhibition experiments [50].
Experimental Protocols for Depression Research
Standardized Workflow for Circuit Manipulation
The following protocol outlines a comprehensive approach for investigating neural circuits in rodent depression models:
Table 3: Experimental Workflow for Circuit Manipulation in Depression Models
| Stage | Procedure | Key Considerations | Timeline |
|---|---|---|---|
| 1. Viral Vector Design | Select opsin/DREADD, promoter, and viral serotype | Cell-type specificity; projection targeting; serotype tropism | 2-3 weeks |
| 2. Stereotaxic Surgery | Bilateral viral delivery into target region | Precision coordinates; titer optimization; post-op recovery | 1 day + 2-3 weeks expression |
| 3. Fiber Implant (Optogenetics) | Implant optic fibers above target region | Fiber diameter; numerical aperture; target depth | Concurrent with viral injection |
| 4. Depression Model Induction | Apply CSDS, CMS, or other stress paradigm | Model validity; susceptibility/resilience screening | 2-8 weeks |
| 5. Neuromodulation | Light delivery or ligand administration | Parameters (frequency, intensity, dose); timing relative to behavior | Acute or chronic |
| 6. Behavioral Assessment | FST, SPT, SI, OFT, EPM | Test order; habituation; experimenter blinding | 1-2 weeks |
| 7. Histological Verification | Perfusion, sectioning, immunohistochemistry | Expression localization; fiber placement; cell counting | Post-behavior |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Optogenetics and Chemogenetics Studies
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Viral Vectors | AAV2, AAV5, AAV8, AAV9 | Gene delivery; serotype selection affects tropism and spread [50] |
| Opsin Variants | ChR2, NpHR, ChETA, Jaws | Light-sensitive actuators for neuronal control [49] [50] |
| DREADD Systems | hM3Dq, hM4Di, KORD | Chemogenetic receptors for ligand-dependent modulation [53] [51] |
| Cell-Type Specific Promoters | CaMKIIα, GAD67, TH, D1-Cre, D2-Cre | Targeting specific neuronal populations [50] [51] |
| DREADD Ligands | CNO, DCZ, JHU37160, Salvinorin B | Activating chemogenetic receptors; varying selectivity and potency [53] [54] |
| Behavioral Test Equipment | Sucrose preference apparatus, forced swim tanks, social interaction arenas | Assessing depressive-like phenotypes [51] |
| Light Delivery Systems | Laser diodes, LEDs, optical fibers, ferrules, rotary joints | Light delivery for optogenetics [50] |
Comparative Analysis and Future Directions
Optogenetics versus Chemogenetics: Strategic Selection
The complementary strengths of optogenetics and chemogenetics enable researchers to address distinct experimental questions in depression research:
Temporal Precision: Optogenetics offers millisecond temporal precision ideal for probing real-time circuit dynamics underlying behavioral decisions, while chemogenetics operates on slower timescales (minutes to hours) suitable for studying neuroadaptation and chronic modulation [51] [54].
Spatial Resolution: Optogenetics provides superior spatial resolution limited to illuminated regions, whereas chemogenetics modulates all expressing neurons regardless of location, which can be advantageous for distributed circuits [54].
Technical Considerations: Chemogenetics requires no implanted hardware, minimizing tissue damage and enabling more natural behaviors, while optogenetics typically involves tethered fibers that can restrict movement though wireless solutions are emerging [50] [54].
Therapeutic Translation: Both approaches have translational potential, though chemogenetics may face fewer technical hurdles for clinical application given its non-invasive activation via systemic ligand administration [53] [54].
Emerging Innovations and Clinical Outlook
The future of neuromodulation in depression research includes several promising developments:
Integration with Human Imaging: Combining circuit manipulations in animal models with human neuroimaging findings creates bidirectional translation for validating circuit mechanisms relevant to human depression [49].
Cell-Type Specific Therapeutics: Identifying specific neuronal populations critical to depression pathology enables development of targeted interventions with potentially fewer side effects than conventional antidepressants [49] [53].
Circuit-Based Biomarkers: Understanding how specific circuit manipulations normalize depressive-like behaviors may yield electrophysiological or functional biomarkers for patient stratification and treatment selection [49] [50].
Gene Therapy Approaches: Advances in viral vector technology and delivery systems are paving the way for potential clinical application of chemogenetic approaches for treatment-resistant depression [53] [54].
As these technologies continue to evolve, they will further illuminate the intricate circuit basis of depressive disorders and accelerate the development of precisely-targeted, circuit-based interventions that address the root causes rather than just the symptoms of depression.
The ventral tegmental area (VTA) and nucleus accumbens (NAc) represent core components of the brain's reward circuitry, with their dysfunction implicated in the pathophysiology of major depressive disorder (MDD). This technical review synthesizes current research on the cellular heterogeneity, neural connectivity, and functional dynamics of the VTA-NAc pathway, with particular emphasis on depression-related neural circuitry adaptations and antidepressant response mechanisms. We provide comprehensive experimental methodologies for investigating these circuits, detailed molecular profiling of key signaling adaptations in depression models, and resource guides for research tools. Evidence indicates that the VTA-NAc circuit is not a monolithic entity but comprises parallel, input-defined subcircuits that differentially process reward and aversion, offering novel targets for therapeutic intervention in treatment-resistant depression.
The VTA and NAc constitute the fundamental neuroanatomical substrate of the mesolimbic dopamine system, which plays a critical role in reward processing, motivation, aversion, and goal-directed behaviors. Understanding the precise organization of this circuit is essential for dissecting its contribution to depression pathophysiology and treatment response.
Cellular Heterogeneity of the VTA: The VTA is composed of approximately 60% dopaminergic neurons, 35% GABAergic neurons, and 5% glutamatergic neurons, creating a complex cellular ecosystem for regulating reward signaling [55]. This cellular diversity is further enhanced by extensive neuropeptide co-expression and the ability of some neurons to co-release multiple neurotransmitters [55]. VTA GABA neurons are preferentially distributed in rostral and medial regions, while DA neurons are more abundant in caudal and lateral areas [56]. This topographical organization forms the structural basis for functional specialization within the VTA.
NAc Medium Spiny Neuron Diversity: The NAc is primarily composed of medium spiny neurons (MSNs), which constitute over 90% of its neuronal population [57]. Traditionally classified based on dopamine receptor expression (D1-MSNs vs. D2-MSNs), recent evidence challenges the simple dichotomy that D1-MSNs exclusively mediate reward and D2-MSNs aversion [57] [58]. Instead, the functional properties of NAc neurons appear to be strongly determined by their specific afferent inputs and efferent targets [58].
Circuit-Level Organization: The VTA-NAc pathway operates as a key node in extended circuits that include the prefrontal cortex, amygdala, paraventricular thalamus, and other limbic structures [58] [59]. In depression, functional magnetic resonance imaging (fMRI) studies have revealed reduced functional connectivity between the VTA and dorsal anterior cingulate cortex (dACC), which correlates with somatic symptoms of depression, and enhanced VTA connectivity with the amygdala, potentially reflecting increased salience attribution to negative internal stimuli [59].
Circuit-Specific Dysregulation in Depression Models
Research across multiple depression models reveals distinct patterns of circuit dysregulation within the VTA-NAc pathway, with specific subpopulations of neurons contributing differentially to depression-related behaviors.
Table 1: VTA-NAc Circuit Adaptations in Depression Models
| Circuit Component | Adaptation in Depression | Functional Consequence | Experimental Evidence |
|---|---|---|---|
| VTA DA Neurons | Reduced activity and bursting; altered projection-specific encoding | Anhedonia, reduced motivation | [60] |
| VTA GABA Neurons | Increased activity; enhanced inhibition of DA neurons | Suppressed reward processing | [56] |
| NAcBLA Neurons | Reduced activity and synaptic output | Impaired reward seeking | [58] |
| NAcPVT Neurons | Enhanced activity and synaptic output | Promoted aversion | [58] |
| VTA-NAc BDNF | Increased BDNF signaling in NAc | Prodepressant effects | [61] |
| NAc-VTA GABA | Altered inhibitory control of VTA | Dysregulated DA release | [62] |
Input-Defined NAc Subcircuits in Reward and Aversion: Critical functional segregation occurs at the level of afferent inputs to the NAc. Recent research demonstrates that NAc neurons receiving basolateral amygdala inputs (NAcBLA) and NAc neurons receiving paraventricular thalamic inputs (NAcPVT) represent largely non-overlapping populations that mediate opposing behavioral valences [58]. Optogenetic activation of NAcBLA neurons drives positive reinforcement and real-time place preference, whereas activation of NAcPVT neurons induces aversion and place avoidance [58]. In depression models, silencing NAcBLA neurons impairs reward seeking, while silencing NAcPVT neurons reduces aversive symptoms without affecting reward processing [58].
VTA Dopamine Subpopulation Encoding: Distinct VTA dopamine subpopulations exhibit differential encoding of reward-related variables. Dopamine neurons projecting to the NAc core preferentially encode reward-predictive cues and prediction errors, whereas those projecting to the NAc shell primarily encode goal-directed actions and relative reward anticipation [60]. In depression, this precise encoding becomes disrupted, contributing to the core symptoms of anhedonia and motivational deficits.
BDNF's Region-Specific Effects: Brain-derived neurotrophic factor (BDNF) exerts contrasting effects in different nodes of the reward circuit. While hippocampal BDNF exerts antidepressant effects, BDNF infusion into the NAc produces prodepressant effects in the forced swim test [61]. Correspondingly, blockade of BDNF signaling in the NAc produces antidepressant-like behavioral effects, highlighting the complex, region-specific role of this neurotrophin in depression pathophysiology [61].
Experimental Methods for Circuit Manipulation and Analysis
Optogenetic Workflow for Input-Defined Circuit Manipulation
The following protocol details the methodology for investigating input-defined NAc circuits as described in [58]:
Surgical Procedure:
- Stereotaxic Injections: Inject AAV1-Cre (∼200 nL) into the BLA (AP: -1.5 mm, ML: ±3.3 mm, DV: -4.8 mm from bregma) or PVT (AP: -1.0 mm, ML: ±0.0 mm, DV: -3.2 mm) of wild-type mice.
- Targeted Expression: In the same surgical session, inject AAV-DIO-ChR2-EYFP or AAV-DIO-TeNT (∼300 nL) into the NAc (AP: +1.3 mm, ML: ±1.0 mm, DV: -4.5 mm).
- Optic Fiber Implantation: Implant optic fibers (200 μm core) above the NAc or relevant projection targets.
- Expression Period: Allow 2-3 weeks for robust opsin/toxin expression before behavioral testing.
Behavioral Assays:
- Real-Time Place Preference (RTPP): Test animals in a two-chamber apparatus with one chamber paired with optical stimulation (473 nm, 10-15 Hz, 5-10 ms pulse width). Score time spent in each chamber.
- Operant Self-Stimulation: Train mice to nose-poke for optical stimulation using a fixed-ratio 1 schedule. Measure response rates during activation versus no stimulation periods.
- Reward Seeking: Assess motivation for palatable food (Ensure) under fixed and progressive ratio schedules during circuit manipulation.
Validation Methods:
- Slice Electrophysiology: Record light-evoked EPSCs/IPSCs in tagged neurons to confirm functional connectivity and monosynaptic transmission.
- Histological Verification: Confirm injection sites and fiber placements using standard immunohistochemical techniques.
Molecular Analysis of Cocaine-Induced Adaptations
The protocol below details the molecular analysis of cocaine-induced adaptations in the VTA-NAc-mPFC circuit from [62]:
Repeated Exposure Place Preference (RePP) Paradigm:
- Pre-Test: Allow rats to freely explore a two-chamber apparatus for 15 minutes to establish baseline chamber preference.
- Conditioning: Pair one chamber with saline injections and the other with cocaine (10 mg/kg, i.p.) for 30-minute sessions across multiple days.
- Optogenetic Manipulation: Apply optical stimulation (20 Hz, 10 ms pulses) to NAc-VTA terminals during cocaine conditioning sessions.
- Post-Test: Re-test chamber preference without stimulation or drug administration.
Molecular Analysis:
- Tissue Collection: Rapidly dissect VTA, NAc, and mPFC regions 24 hours after final behavioral test.
- Western Blotting: Quantify total and phosphorylated levels of ERK, GluA1, and GluA1 phosphorylation at Ser831 and Ser845 sites.
- Normalization: Express protein levels relative to loading controls (β-actin, GAPDH) and calculate phosphorylation ratios.
Signaling Pathways in Reward Circuit Pathology
The molecular adaptations in the VTA-NAc circuit in depression and substance use disorders involve complex alterations in signaling pathways, particularly those regulating synaptic plasticity.
Table 2: Key Molecular Adaptations in Reward Circuitry
| Molecule | Function | Adaptation in Depression/Addiction | Therapeutic Implications |
|---|---|---|---|
| ERK | Synaptic plasticity, cell signaling | Reduced in VTA and mPFC after cocaine; altered by NAc-VTA manipulation | Potential target for normalizing synaptic function |
| GluA1 (S845) | AMPA receptor trafficking, synaptic strength | Decreased phosphorylation in NAc and mPFC after cocaine exposure | Indicator of altered glutamatergic transmission |
| GluA1 (S831) | AMPA receptor channel conductance | Reduced in NAc and mPFC after cocaine exposure | Marker of synaptic depression |
| BDNF | Neurotrophic factor, synaptic plasticity | Increased in NAc in depression models; decreased in hippocampus | Region-specific targeting required |
| DAT | Dopamine reuptake | Circadian regulation affecting dopamine tone | Chronotherapeutic considerations |
ERK Signaling Dysregulation: The extracellular signal-regulated kinase (ERK) pathway demonstrates significant alterations in reward circuit regions following cocaine exposure and in depression models. Cocaine exposure reduces ERK levels in the VTA and medial prefrontal cortex (mPFC), while activation of NAc-VTA GABAergic inputs during cocaine conditioning further modulates these adaptations [62]. Enhanced GABAergic tone from the NAc to VTA during cocaine conditioning normalizes cocaine-induced reductions in GluA1 phosphorylation at Ser845 in the mPFC, suggesting a mechanism for how inhibitory circuit manipulation can reverse drug-induced synaptic maladaptations [62].
AMPA Receptor Trafficking Alterations: Phosphorylation of the GluA1 subunit of AMPA receptors at specific serine residues (S831 and S845) regulates its synaptic insertion and function, representing a key mechanism of synaptic plasticity in reward circuits. Cocaine exposure reduces GluA1 phosphorylation at both S831 and S845 sites in the mPFC, indicating widespread disruption of glutamatergic transmission in cortical regions that regulate reward seeking [62]. Optogenetic activation of NAc-VTA projections during cocaine exposure produces unique molecular adaptations in the NAc, including increased ERK levels and reduced GluA1 phosphorylation at Ser845, suggesting circuit-specific homeostatic adaptations [62].
Circadian Regulation of Dopamine Signaling: Both the VTA and NAc function as extra-SCN circadian oscillators, with their molecular clocks regulating dopamine synthesis, release, and reuptake [63]. Circadian molecular clock components regulate dopamine synthesis enzyme tyrosine hydroxylase (TH), dopamine transporters (DAT), and dopamine receptors in the VTA and NAc, creating circadian variations in dopamine signaling that may be disrupted in depression [63]. This circadian regulation of reward circuit function has important implications for the timing of antidepressant treatments and understanding diurnal variations in depression symptoms.
Research Reagent Solutions
Table 3: Essential Research Reagents for VTA-NAc Circuit Manipulation
| Reagent/Tool | Specific Application | Function/Purpose | Example Sources |
|---|---|---|---|
| AAV1-Cre | Anterograde transsynaptic labeling | Labels postsynaptic neurons receiving specific inputs; defines input-specific circuits | [58] |
| AAV-DIO-ChR2 | Cell-type specific optogenetics | Enables precise optical control of defined neuronal populations | [62] [58] |
| AAV-DIO-TeNT | Synaptic silencing | Blocks synaptic transmission from defined neuronal populations | [58] |
| CTB-488/647 | Retrograde tracing | Identifies projection-specific neuronal populations | [58] |
| c-Fos IHC | Neural activity mapping | Marks recently activated neurons following behavioral manipulations | [57] |
| D1-Cre/D2-Cre mice | Genetic access to MSN subtypes | Enables manipulation of specific MSN populations | [57] [58] |
| Fibre photometry | In vivo calcium imaging | Records real-time neuronal activity in behaving animals | [57] |
| CRISPR-Cas9 systems | Gene editing in specific circuits | Enables functional analysis of specific genes in defined circuits | Emerging technology |
Viral Vector Systems: The AAV1-mediated anterograde transsynaptic tagging system has revolutionized the study of input-defined neural circuits by enabling selective access to neurons receiving specific inputs [58]. This system allows for both functional manipulation and input-output mapping of defined circuit elements, providing unprecedented precision in circuit dissection.
Activity Markers and Detection Methods: Immediate early gene expression analysis (c-Fos) combined with fluorescent in situ hybridization for dopamine receptors (D1R, D2R) enables molecular profiling of activated neuronal populations in response to stimuli or circuit manipulations [57] [58]. This approach has revealed that both D1-MSNs and D2-MSNs can be activated by rewarding and aversive stimuli, challenging simple dichotomous models of NAc function [57].
In Vivo Monitoring Approaches: Fibre photometry with genetically encoded calcium indicators enables real-time monitoring of neuronal population activity in freely behaving animals, revealing how specific NAc neuronal ensembles encode reward and aversion [57]. These approaches have demonstrated diverse response patterns in MSNs during reward-related behaviors, with both D1- and D2-MSNs exhibiting heterogeneous activation profiles during sucrose consumption [57].
Therapeutic Implications and Future Directions
The dissection of VTA-NAc circuitry has profound implications for developing novel antidepressant therapies, particularly for treatment-resistant depression.
Deep Brain Stimulation (DBS) Mechanisms: DBS of the NAc has shown efficacy in treatment-resistant depression, with recent evidence suggesting its therapeutic effects involve restoration of hippocampal neurogenesis and gamma oscillations via multisynaptic circuits [64]. The antidepressant effect of NAc-DBS depends on activation of parvalbumin-positive interneurons in the dorsal dentate gyrus, which are regulated by VTA-DG GABAergic projections and CA1-NAc projections [64].
Input-Specific Circuit Therapeutics: The segregation of NAcBLA (reward) and NAcPVT (aversion) circuits suggests promising targets for novel depression treatments that could specifically enhance positive affect while reducing negative affect [58]. Strategies that selectively modulate these parallel circuits could potentially achieve more precise therapeutic effects with fewer side effects than current approaches.
Circadian-Targeted Interventions: The robust circadian regulation of VTA-NAc circuitry suggests that chronotherapeutic approaches may optimize antidepressant efficacy [63]. Timing drug administration to align with peaks in reward circuit sensitivity could enhance therapeutic outcomes, particularly for symptoms of anhedonia and amotivation.
The continued dissection of VTA-NAc reward pathways using increasingly precise circuit manipulation tools will undoubtedly yield novel insights into depression pathophysiology and accelerate the development of more effective, circuit-targeted antidepressant strategies.
Major depressive disorder (MDD) is a widespread and debilitating condition that profoundly affects quality of life, with less than half of patients achieving remission with first-line treatments [65]. This treatment resistance has generated significant interest in identifying biomarkers and developing neuromodulation interventions that target the underlying neural circuitry of depression. Contemporary conceptualizations consider MDD a systems-level disorder arising from dysregulation among large-scale functional brain networks [65]. The dorsolateral prefrontal cortex (DLPFC) and hippocampus represent two critical nodes within these networks, and their structural and functional integrity is essential for emotional regulation and cognitive function. The hippocampal-prefrontal cortex (Hip-PFC) circuit, comprising major efferent anatomical connections from the hippocampal formation to the PFC, plays a critical role in cognitive and emotional regulation and memory consolidation [66]. This technical review examines current evidence for modulating this circuit, detailing methodological approaches, quantitative outcomes, and essential research tools for investigating cortical control mechanisms in depression pathology and treatment.
Neural Circuitry of Depression: PFC and Hippocampus Dysfunction
The Hippocampal-Prefrontal Cortical Circuit
The Hip-PFC pathway comprises the major efferent anatomical connection from the hippocampal formation, through monosynaptic and/or polysynaptic projections, to the PFC [66]. This circuit manifests remarkable monosynaptic unidirectional projections that play vital roles in cognitive processing [66]. In rodents, neurons in the ventral CA1 and subiculum selectively project to the prelimbic medial prefrontal cortex (mPFC) and orbitomedial frontal cortex [66]. These fibers navigate to the ipsilateral PFC through the fimbria/fornix system before terminating in the infralimbic (IL) and the prelimbic (PL) PFC and anterior cingulate cortex [66].
In addition to direct monosynaptic projections, complex multisynaptic routes facilitate communication between the hippocampus and PFC [66]:
- Hip-NAc-VTA-PFC Loop: The ventral hippocampus (vHip) glutamatergic neurons project to the nucleus accumbens (NAc), which sends GABAergic inhibitory projections to dopaminergic neurons of the ventral tegmental area (VTA). The VTA then projects to the mPFC, creating a regulatory loop affecting motivation and reward processing [66].
- vHip-BLA-PFC Loop: The ventral CA1 and ventral subiculum project to both the mPFC and basolateral amygdala (BLA), with some hippocampal neurons projecting to both areas simultaneously, enabling coordination during memory retrieval and emotional processing [66].
- Hip-Thalamus-PFC Loop: The hippocampus and anterior thalamic nuclei form part of an interconnected network involved in memory formation, with the PFC receiving projections from several thalamic nuclei that contribute to attention and executive control [66].
Circuit Dysregulation in Depression
Dysfunction of the Hip-PFC circuit results in behavioral changes including executive function and memory impairments, enhanced fear retention, fear extinction deficiencies, and other disturbances observed in depression and stress-related disorders [67]. Considerable evidence shows that PTSD (which shares symptomatology with depression) results from a dysfunction in highly conserved brain systems involved in regulating stress, anxiety, fear, and reward circuitry [67]. These shared neural disruptions include asymmetrical white matter tract abnormalities and gray matter changes in the PFC, hippocampus, and basolateral amygdala [67].
Table 1: Quantitative Biomarkers of PFC and Hippocampal Circuit Dysfunction in Depression
| Biomarker Measure | Population | Finding in Depression | Association with Symptoms |
|---|---|---|---|
| Right DLPFC current density during N2 time window | MDD patients (n=115) vs. Healthy Controls (n=43) | Significantly reduced (p=0.028) [65] | Correlated with lower HAMD-21 scores at 1 week (p=0.041) [65] |
| Beta-band FC between left DLPFC and PCC | MDD patients (n=71) [65] | Decreased connectivity correlated with lower HAMD-21 scores (left: p=0.003; right: p=0.004) [65] | Early reduction predicted remission at week 12 (OR=0.534, 95% CI: 0.297-0.972) [65] |
| MEP modulation post-MC rTMS | Medication-resistant MDD patients (n=51) [68] | Larger increase in corticospinal excitability predicted better antidepressant response (rho=0.43, p<0.005) [68] | Robust predictor of HAM-D-17 reduction in multivariable model (β=0.25, p<0.0001) [68] |
Therapeutic Modulation of PFC and Hippocampal Circuits
Pharmacological Modulation
Venlafaxine, a serotonin-norepinephrine reuptake inhibitor (SNRI), demonstrates measurable effects on PFC activity and connectivity. A prospective cohort study with 115 MDD patients revealed that early treatment-related changes in DLPFC activity predicted clinical outcomes [65]. Specifically, higher right DLPFC current density during the N2 time window evoked by oddball stimuli was correlated with lower HAMD-21 scores one week after treatment (p=0.041), and an early increase predicted remission at week 12 (p=0.005) [65]. Furthermore, decreased beta-band functional connectivity between the left DLPFC and posterior cingulate cortex (PCC) was correlated with lower HAMD-21 scores, with early reduction in these connectivity measures predicting remission at week 12 (OR=0.533, 95% CI: 0.299-0.950, p=0.033) [65].
Neuromodulation Approaches
Repetitive transcranial magnetic stimulation (rTMS) targeting the left DLPFC represents an established treatment option for patients with medication-resistant MDD [68]. The therapeutic effects are mediated by modulation of prefrontal cortex excitability, though measuring this directly presents technical challenges [68]. Research has demonstrated that modulation of motor cortex (MC) excitability by rTMS may serve as a predictive biomarker for antidepressant response to left DLPFC rTMS [68]. In this paradigm, motor evoked potential (MEP) modulation is calculated as the percentage change of mean MEP amplitude post-rTMS relative to pre-rTMS, with positive values (MEP amplitude increase) reflecting facilitation of cortical excitability by rTMS [68].
Table 2: Quantitative Outcomes of Neuromodulation Approaches
| Intervention | Target | Clinical Outcome | Neural Correlate |
|---|---|---|---|
| Venlafaxine [65] | DLPFC activity | Remission at week 12 predicted by early right DLPFC activity increase (p=0.005) [65] | Higher right DLPFC current density during N2 time window correlated with lower HAMD-21 at 1 week (p=0.041) [65] |
| 10 Hz rTMS [68] | Left DLPFC | MEP modulation predicted HAM-D-17 reduction (rho=0.43, p<0.005) [68] | Larger MC rTMS-induced increase in corticospinal excitability anticipated better antidepressant response [68] |
| rTMS [65] | DLPFC-PCC connectivity | Remission at week 12 predicted by early beta-band FC reduction (OR=0.533, 95% CI: 0.299-0.950) [65] | Decreased beta-band FC between left DLPFC and PCC correlated with lower HAMD-21 scores (p=0.004) [65] |
Experimental Models and Methodologies
Preclinical Models of Circuit Dysfunction
Various animal models are used to mimic depression-like and stress-related behaviors, with three models particularly prominent for studying PFC-hippocampal circuitry [67]:
- Single Prolonged Stress (SPS): Involves three severe stressors (2h restraint, forced swimming, ether exposure until loss of consciousness) that produce behavioral, molecular, and physiological alterations resembling those in PTSD and depression patients [67].
- Fear Conditioning and Extinction (FC): A neutral stimulus (conditioned stimulus) is paired with an aversive experience (unconditioned stimulus), after which the conditioned stimulus alone triggers fear responses. This model captures aspects of learning and memory relevant to depression and anxiety [67].
- Chronic Social Defeat Stress (CSDS): Involves exposure to aggressive conspecifics and assesses behavioral dysfunction and underlying neurobiological mechanisms relevant to social stress aspects of depression [67].
Electrophysiological Protocols
EEG/ERP Recording Protocol [65]:
- Resting-state EEG signals are recorded in dimly illuminated, electrically shielded, and acoustically isolated chambers using a 128-channel EEG system.
- Participants maintain stillness while minimizing blinks and eye movements during 12-min trials with eyes-open and eyes-closed conditions.
- Electrodes are positioned according to the standard international 10/5 system at a sampling frequency of 1000 Hz.
- Electrode impedance is meticulously maintained below 20 KΩ during recording.
- Source localization analyses are conducted using built-in low resolution electromagnetic tomography analysis (LORETA) to calculate current density within the DLPFC.
Visual Oddball Paradigm [65]:
- The paradigm consists of two visual stimuli: a red car as the oddball stimulus and a blue car as the standard stimulus.
- Event-related potential (ERP) analysis focuses on stimulus-associated N1, P2, N2, and P3 components.
- Time windows and electrode selection should be guided by established parameters from previous literature.
rTMS Motor Cortex Excitability Protocol [68]:
- Motor evoked potentials (MEPs) are induced using single TMS pulses delivered to the motor cortex at 120% of resting motor threshold (RMT).
- A random stimulus interval of approximately 10 seconds (±1 second) is used, with muscle relaxation monitored via EMG.
- MEP amplitude is measured peak-to-peak and averaged across 10 consecutive MEPs.
- Patients receive a single rTMS session over the abductor pollicis brevis (APB) 'hotspot' with treatment parameters.
- Approximately 30 seconds after MC rTMS, MEP amplitude is measured again.
- Modulation index is calculated as percentage change of mean MEP amplitude post-rTMS relative to pre-rTMS.
Experimental rTMS Biomarker Protocol [68]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Tools for PFC-Hippocampus Stimulation Research
| Research Tool | Specification/Function | Experimental Application |
|---|---|---|
| 128-channel EEG System [65] | BrainProducts GmbH with BrainVision Recorder; 1000 Hz sampling | High-density electrophysiological recording during cognitive tasks and resting state |
| LORETA Software [65] | Low Resolution Electromagnetic Tomography | Source localization of EEG signals to identify DLPFC current density |
| Magstim TMS Apparatus [68] | SuperRapid Stimulator with 70-mm figure-of-eight coil | Precise delivery of rTMS pulses to DLPFC and motor cortex targets |
| EMG Recording System [68] | Surface electrodes (Ag-AgCl); PowerLab 4/25T with Scope software | Measurement of motor evoked potentials for excitability assessment |
| Visual Oddball Paradigm [65] | Red car (oddball) vs. blue car (standard stimulus) | Elicitation of N2/P3 ERP components for cognitive processing assessment |
| HAMD-21 [65] | 21-item Hamilton Depression Rating Scale | Gold-standard clinician-rated assessment of depression severity |
| Single Prolonged Stress Model [67] | Restraint, forced swim, ether anesthesia sequence | Preclinical model inducing PTSD/depression-like neural and behavioral phenotypes |
Signaling Pathways in PFC-Hippocampal Communication
Hip-PFC Circuit Connectivity [66]
The neural pathways connecting the PFC and hippocampus involve sophisticated neurochemical signaling:
- Glutamatergic Signaling: The direct Hip-PFC pathway is primarily glutamatergic, with hippocampal projections forming excitatory synapses on both pyramidal cells and GABAergic interneurons in the PFC [66]. This produces initial excitatory postsynaptic potentials (EPSPs) followed by inhibition through feed-forward inhibitory circuits [66].
- Dopaminergic Modulation: The VTA provides dopaminergic input to both hippocampus and PFC, with dopamine release important for consolidating long-term potentiation (LTP) in CA1 and regulating the flow of hippocampal short-term memory into PFC long-term memory [66].
- GABAergic Regulation: Hippocampal inputs to the PFC directly excite GABAergic interneurons, contributing to feed-forward inhibition of pyramidal neurons and shaping the temporal dynamics of PFC responses [66].
- Synaptic Plasticity Mechanisms: The Hip-PFC pathway demonstrates synaptic plasticity, with repetitive electrical stimulation in the ventral subiculum or CA1 inducing LTP or long-term depression (LTD) in the PFC [66]. This plasticity is modulated by inputs from other regions, such as the basolateral amygdala [66].
Modulation of the hippocampal-prefrontal cortical circuit represents a promising therapeutic approach for treatment-resistant depression. The integration of electrophysiological biomarkers, such as DLPFC activity and functional connectivity measures, with neuromodulation techniques like rTMS provides a robust framework for both understanding treatment mechanisms and predicting clinical outcomes. The experimental protocols and research tools detailed in this review offer a comprehensive methodology for further investigating these circuits. As research advances, the continued refinement of stimulation parameters and target engagement biomarkers will enhance the precision and efficacy of PFC-hippocampus circuit modulation, ultimately improving outcomes for patients with depressive disorders.
Major depressive disorder (MDD) is a prevalent and disabling condition, historically understood through neurotransmitter dysfunction hypotheses. However, contemporary research has pivoted toward a circuit-based paradigm, recognizing depression as a network disorder characterized by distributed abnormalities in large-scale brain circuits. This shift has been propelled by advanced neuroimaging techniques, particularly functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), which provide complementary windows into brain function. fMRI offers high spatial and temporal resolution for mapping hemodynamic activity linked to neuronal firing, while PET enables quantitative molecular imaging of neurotransmitters, receptors, and metabolic processes. The integration of these modalities is refining our neurobiological understanding of depression, moving beyond syndromic diagnosis to identify circuit-based biotypes and objectively measure treatment target engagement for pharmaceutical development. This whitepaper details how fMRI and PET are elucidating human circuit dysfunctions, with a specific focus on their application in clinical populations with depression and the evaluation of antidepressant response.
Core Neuroimaging Technologies and Their Biological Bases
Functional Magnetic Resonance Imaging (fMRI)
2.1.1 Principles and Methodologies fMRI is a non-invasive hemodynamic/metabolic method that indirectly measures neuronal activity by detecting associated changes in blood flow, volume, and oxygenation. The most common technique is Blood Oxygen Level-Dependent (BOLD) fMRI, which leverages the magnetic properties of oxygenated versus deoxygenated hemoglobin as a native contrast agent. When a brain region becomes active, a local increase in cerebral blood flow delivers oxygen in excess of metabolic demand, leading to a measurable signal change. It is crucial to recognize that the BOLD signal is more closely tied to synaptic activity—specifically local field potentials from peri-synaptic activity—than to the spiking output of neurons [69]. A critical consideration for interpretation is that both excitatory and inhibitory synaptic activity can increase the BOLD signal, making it ambiguous whether a signal increase reflects increased or decreased local spiking activity [70].
2.1.2 Primary Experimental Protocols
- Task-Based fMRI: Subjects perform cognitive, emotional, or sensory tasks in the scanner. Paradigms like the Go-NoGo task (to probe cognitive control) or emotional face matching are used to activate specific circuits. The resulting BOLD signal changes are modeled to identify regions where activity correlates with task demands [71].
- Resting-State fMRI (rs-fMRI): Subjects lie in the scanner at rest, not performing any specific task. Data analysis focuses on low-frequency fluctuations in the BOLD signal to identify functionally connected networks, such as the default mode network (DMN), salience network, and frontoparietal network, through measures like temporal correlation (functional connectivity) [69].
Positron Emission Tomography (PET)
2.2.1 Principles and Methodologies PET is a molecular imaging procedure that creates 3D maps of biologically active compounds labeled with positron-emitting radioisotopes (e.g., Carbon-11 [¹¹C] or Fluorine-18 [¹⁸F]). A radiotracer is administered, and the scanner detects gamma rays produced when emitted positrons annihilate with electrons. The resulting images display the concentration and spatial distribution of the tracer, allowing for the quantification of specific molecular targets [72]. Unlike fMRI, PET can provide absolute quantitative measurements of target engagement.
2.2.2 Key Radiotracers and Targets in Depression Research PET radiotracers must exhibit high selectivity, specificity, and affinity for their target, and must be able to cross the blood-brain barrier. The table below summarizes key radiotracers used in depression research.
Table 1: Key PET Radiotracers for Depression Circuit Research
| Molecular Target | Example Radiotracers | Primary Application in Depression Research |
|---|---|---|
| Serotonin Transporter (SERT) | [¹¹C]DASB, [¹¹C]MADAM | Quantification of serotonin system integrity; often shows alterations in MDD [72]. |
| Serotonin 1A Receptor (5-HT1A) | [¹¹C]WAY 100635 | Investigation of pre- and post-synaptic receptor changes, a hallmark of affective disorders [72]. |
| Dopamine D2/D3 Receptor | [¹¹C]raclopride, [¹⁸F]fallypride | Assessment of dopamine receptor availability, linked to motivation and anhedonia [72]. |
| Norepinephrine Transporter (NET) | [¹⁸F]FMeNER-D2 | Mapping the norepinephrine system, a target for SNRIs [72]. |
| Glucose Metabolism | [¹⁸F]FDG | Measurement of regional cerebral glucose metabolism as a proxy for neuronal activity; requires standardized protocols due to high physiological brain uptake [72]. |
| Microglial Activation (TSPO) | [¹⁸F]FEPPA | Assessment of neuroinflammation, a potential pathophysiological mechanism in depression [72]. |
| Metabotropic Glutamate Receptor 5 (mGluR5) | [¹¹C]ABP688 | Investigation of the glutamatergic system, targeted by novel antidepressants like ketamine [72]. |
2.2.3 Advanced PET Methodologies
- Static FDG-PET: Traditionally involves a single scan over 10-40 minutes to measure cumulative glucose uptake, providing a "snapshot" of metabolic activity.
- Functional PET (fPET): A newer approach using constant infusion or hybrid bolus/infusion of the radiotracer (e.g., [¹⁸F]FDG). This allows for the assessment of metabolic dynamics with high temporal resolution (e.g., 60 seconds or less), enabling the study of metabolic connectivity analogous to rs-fMRI [69].
Mapping Circuit Dysfunction in Depression: Key Findings and Experimental Protocols
The Cognitive Control Circuit and a Depression Biotype
Converging evidence from fMRI and PET implicates dysfunction within the cognitive control circuit, particularly the dorsolateral prefrontal cortex (dLPFC) and dorsal anterior cingulate cortex (dACC), in a distinct biotype of depression [71].
3.1.1 Experimental Protocol for Circuit Identification
- Task Paradigm: Go-NoGo Task. During fMRI, participants are instructed to press a button for frequent "Go" stimuli and withhold responses for infrequent "NoGo" stimuli. This task robustly engages cognitive control processes.
- Primary fMRI Metric: Task-evoked functional connectivity between the left dLPFC and dACC during performance of the Go-NoGo task.
- Baseline Stratification: Participants are stratified into biotypes based on dLPFC-dACC connectivity. A cognitive biotype (+) is defined by hypoconnectivity (connectivity value < 0 relative to a healthy norm), while a cognitive biotype (-) exhibits intact connectivity [71].
- Behavioral Correlates: Cognitive performance is simultaneously assessed using computerized batteries (e.g., WebNeuro). The cognitive biotype (+) group shows significantly worse cognitive control performance at baseline [71].
3.1.2 Key Findings This biotype, present in approximately 27% of individuals with depression, is characterized by treatment resistance to standard pharmacotherapy, greater disability, and impaired cognitive control behavioral performance [71] [72]. This establishes dLPFC-dACC connectivity as both a diagnostic biomarker for stratification and a target for novel interventions.
Molecular Dysregulation in Depressive Circuits
PET imaging has revealed widespread alterations in neurotransmitter systems across these circuits, providing a molecular context for functional impairments observed with fMRI.
Table 2: Molecular Dysregulation in Depression via PET Imaging
| Neurotransmitter System | Documented Alterations in MDD | Relationship to Circuit Function |
|---|---|---|
| Serotonergic System | Abnormalities of 5-HT1A and 5-HT1B receptors; altered serotonin transporter (SERT) binding [72]. | Modulates mood, emotion, and executive function; linked to dLPFC and limbic circuit activity. |
| Dopaminergic System | Altered dopamine transporter (DAT) binding and D2/D3 receptor availability [72]. | Underpins motivation and reward; dysfunction linked to anhedonia and ventral striatum activity. |
| GABAergic System | Altered binding to GABA-A benzodiazepine receptors (e.g., [¹¹C]Flumazenil) [72]. | Critical for inhibitory balance; disruption may contribute to network instability and emotional dysregulation. |
| Glutamatergic System | Changes in mGluR5 receptor availability [72]. | Primary excitatory system; targeted by rapid-acting antidepressants like ketamine. |
| Neuroinflammation | Elevated translocator protein (TSPO) binding, indicating microglial activation [72]. | May drive or exacerbate synaptic and circuit dysfunction across multiple brain networks. |
3.2.1 Experimental Protocol for Receptor Imaging
- Radiotracer Selection: A tracer with high specificity for the target (e.g., [¹¹C]DASB for SERT) is selected.
- Scanning Procedure: A dynamic PET scan is acquired, often lasting 60-90 minutes, to capture the tracer's uptake and binding over time.
- Quantification: Kinetic modeling is applied to the time-activity data from brain regions to derive quantitative parameters, such as the non-displaceable binding potential (BPND), which reflects receptor availability. This often requires arterial blood sampling to measure the radiotracer's input function [72] [73].
Evaluating Antidepressant Response: Target Engagement and Circuit Mechanisms
Transcranial Magnetic Stimulation (TMS) for the Cognitive Biotype
TMS applied to the dLPFC is an effective intervention for treatment-resistant depression, with fMRI providing a biomarker of target engagement and mechanism.
4.1.1 Experimental Protocol for TMS Response
- Intervention: Participants receive a standard course of TMS (e.g., once-daily treatments for up to 30 sessions) targeting the left dLPFC [71].
- Longitudinal fMRI: fMRI scans (using the same Go-NoGo paradigm) are acquired at three time points: pre-TMS, after early TMS treatment (e.g., ~5 sessions), and post-TMS.
- Primary Outcome: Change in task-evoked dLPFC-dACC connectivity from baseline.
- Key Finding: TMS produces an early and persistent improvement in cognitive control circuit connectivity specific to the cognitive biotype (+) group. Veterans in this group showed significant increases in connectivity after early treatment, which remained elevated post-treatment. The cognitive biotype (-) group showed no significant changes. This connectivity improvement was associated with a corresponding restoration of cognitive control behavioral performance [71].
Convergent Mechanisms of Antidepressant Medications
A large-scale neuroimaging meta-analysis of antidepressant effects revealed critical convergent mechanisms at a macroscale level [74].
4.2.1 Experimental Protocol for Meta-Analysis
- Study Selection: Comprehensive search to identify eligible functional neuroimaging studies (fMRI, PET, SPECT) of antidepressant drug effects in MDD. The analysis included pre- vs. post-treatment or treated vs. untreated contrasts.
- Analysis Method: Activation likelihood estimation (ALE) for regional convergence and a novel network-level meta-analysis to identify distributed circuits.
- Key Findings:
- Regional Convergence: No widespread regional convergence was found, highlighting the heterogeneity of findings. However, a subgroup analysis (Treated > Untreated) revealed a convergent cluster in the left dLPFC [74].
- Network-Level Convergence: Antidepressants consistently alter function within a distributed circuit most prominent in the frontoparietal network. This circuit aligns with those targeted by "anti-subgenual" and "Beam F3" TMS therapy protocols [74].
- Neurotransmitter Correlation: The patterns of functional change showed no significant correlation with the distribution of serotonin or norepinephrine transporters/receptors, suggesting that the macroscale functional effects of antidepressants extend beyond simple monoamine reuptake blockade [74].
Advanced and Integrated Methodologies
Simultaneous PET/MRI
Integrated PET/MR scanners represent a significant methodological advancement, allowing for the simultaneous collection of anatomical, functional (BOLD-fMRI), and molecular (PET) data [73].
5.1.1 Key Methodological Advantages
- Temporal Correlation: Eliminates the assumption of an unchanged physiological or cognitive state between sequential scans, which is critical for studying dynamic mental states or rapidly changing conditions [73].
- MR-Based PET Motion Correction: Simultaneously acquired MR data can be used to track and correct for head motion in the PET data, improving spatial resolution and quantitative accuracy, especially in uncooperative populations [73].
- Partial Volume Effect Correction: The high-resolution anatomical MR data can be used to correct for the blurring effects in PET that cause underestimation of activity in small structures like the cortical gray matter [73].
- Cross-Modality Validation: Enables direct cross-calibration of techniques measuring related phenomena, such as cerebral blood flow with H₂¹⁵O PET and arterial spin labeling (ASL) fMRI [73].
5.1.2 Simultaneous fMRI/fPET Protocol This nascent protocol allows for the direct correlation of hemodynamic and metabolic signals during an identical neural event [69].
- Procedure: [¹⁸F]FDG is administered via a constant infusion over a long scan (e.g., 95 minutes) during simultaneous BOLD-fMRI acquisition.
- Output: High-temporal-resolution data on glucose uptake (fPET) and BOLD fluctuations, enabling the comparison of metabolic connectivity (from fPET) with hemodynamic connectivity (from fMRI) during the resting state [69].
The following diagram illustrates the workflow and advantages of a simultaneous fMRI/fPET study:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents and Materials for Circuit Mapping in Depression
| Item | Function/Application | Example/Notes |
|---|---|---|
| Go-NoGo fMRI Paradigm | Engages and measures the cognitive control circuit (dLPFC-dACC); used for patient stratification [71]. | Customizable tasks (e.g., presented via E-Prime, Presentation). |
| Selective PET Radiotracers | Quantifies specific molecular targets (receptors, transporters, metabolism) [72]. | [¹¹C]DASB (SERT), [¹¹C]WAY 100635 (5-HT1A), [¹⁸F]FDG (metabolism). Require on-site cyclotron for [¹¹C]. |
| High-Field MRI Scanner | Provides high-resolution anatomical and functional BOLD data. | 3 Tesla (3T) scanners are standard; 7T provides higher signal-to-noise. |
| Integrated PET/MR Scanner | Enables simultaneous acquisition for temporal correlation and motion correction [73] [69]. | Siemens Biograph mMR. |
| MR-Compatible Infusion Pump | For constant infusion of radiotracer during functional PET (fPET) studies [69]. | BodyGuard 323 (Caesarea Medical Electronics). |
| Arterial Blood Sampling Kit | For absolute quantification of PET data; measures radiotracer input function. | Includes catheter, tubing, vacutainers, centrifuge, well counter. |
| Cognitive Battery | Assesses behavioral correlates of circuit dysfunction (e.g., cognitive control). | WebNeuro, CNS Vital Signs. |
| Statistical Parametric Mapping Software | Analyzes neuroimaging data (fMRI, PET) for group-level and connectivity statistics. | SPM, FSL, AFNI. |
The convergence of fMRI and PET technologies has fundamentally advanced the clinical neuroscience of depression. By mapping both the functional dynamics and molecular underpinnings of neural circuits, these tools have enabled a shift from a purely syndromal classification to a circuit-based and biotype-driven understanding of the disorder. The identification of a cognitive biotype with specific dLPFC-dACC dysfunction and poor response to pharmacotherapy, but improvement with targeted TMS, is a landmark achievement in precision psychiatry. For researchers and drug development professionals, this integrated approach provides a robust framework for identifying novel therapeutic targets, validating and stratifying for interventions, and objectively measuring target engagement and treatment efficacy through quantifiable changes in brain circuit function and molecular pathology. The ongoing development of simultaneous multi-modal imaging and advanced analytical techniques promises to further refine these models, accelerating the development of personalized and effective treatments for major depressive disorder.
The current diagnostic paradigm for major depressive disorder (MDD), based on DSM criteria, groups individuals by symptom presentation, resulting in remarkable heterogeneity and a "one-size-fits-all" treatment approach. This system allows for hundreds of unique symptom combinations, yet fails to capture the underlying neurobiological diversity, contributing to high treatment failure rates where approximately 30% of patients develop treatment-resistant depression and up to two-thirds fail to achieve full remission [75]. This clinical challenge has motivated a paradigm shift toward precision psychiatry, seeking to define neurophysiological subtypes, or "biotypes," based on shared signatures of brain circuit dysfunction rather than clinical symptomatology alone [76].
The foundation for this approach rests on conceptualizing depression and anxiety as disorders of large-scale neural circuits. These macroscale circuits—vast populations of interconnected neurons that constitute the brain's connectome—integrate emotional, cognitive, and self-reflective functions and can be quantified in vivo using functional magnetic resonance imaging (fMRI) [76]. By measuring circuit dysfunction across domains of resting reflection, salience detection, affective processing, attention, and cognitive control, researchers can delineate biotypes with distinct clinical profiles, behavioral performance patterns, and—crucially—differential responses to treatment [13] [76]. This framework transcends traditional diagnostic boundaries to offer a biologically grounded taxonomy for depression, promising to advance both neurobiological understanding and clinical care.
Neural Circuit Framework for Depression Biotyping
Core Circuits Implicated in Depression and Anxiety
Research convergence indicates that depression and anxiety disorders involve dysfunction across six primary large-scale brain circuits, each supporting distinct psychological functions [13] [76]:
- Default Mode Circuit: Involves the anterior middle frontal cortex, posterior cingulate cortex, and angular gyrus. This circuit supports self-referential thinking at rest and demonstrates both hyper-connectivity (correlated with rumination) and hypo-connectivity patterns in depression [76].
- Salience Circuit: Comprises the anterior cingulate cortex, anterior insula, and sublenticular extended amygdala. It detects salient changes in the internal and external environment and shows altered connectivity with both the default mode and attention circuits in depression [76].
- Threat Circuit: Includes the amygdala, hippocampus, and regions of the prefrontal cortex. This circuit mediates threat reactivity and regulation, frequently showing amygdala hyperactivation in response to threat stimuli across depression and anxiety disorders [76].
- Positive Affect/Reward Circuit: Encompasses the ventral striatum, ventral pallidum, orbitofrontal cortex, anterior cingulate, and thalamus. It supports reward processing and motivation, with dysfunction manifesting clinically as anhedonia—a core symptom of depression [4] [76].
- Attention Circuit: A frontoparietal system that supports orienting and maintaining focus. Dysfunction in this circuit correlates with cognitive complaints in depression [13].
- Cognitive Control Circuit: Involves prefrontal regions that support executive functions such as working memory, planning, and inhibitory control. Reduced activation in this circuit is associated with poor executive task performance in depression [13].
A Consensus on Circuit Dysfunction
Converging evidence from meta-analyses and large-scale studies indicates that while a shared "core" of circuit pathology exists in depression—often involving the insula, orbitofrontal cortex, and ventromedial prefrontal cortex—distinct patterns of dysfunction across these circuits provide the neurobiological basis for defining biotypes [77] [76]. These biotypes cannot be reliably differentiated by clinical symptoms alone, supporting the need for objective circuit-based measures [77].
Established Depression Biotype Classification Systems
The Six-Circuit Biotype Model
A landmark 2024 study published in Nature Medicine introduced a sophisticated biotyping model based on a standardized functional MRI protocol and individualized circuit quantification [13]. The researchers applied the Stanford Et Cere Image Processing System to brain scans from 801 medication-free participants with depression and anxiety, deriving 41 personalized, interpretable scores of brain circuit dysfunction across the six core circuits. Hierarchical clustering analysis revealed six distinct biotypes, validated through multiple statistical approaches including silhouette index testing and cross-validation stability checks [13].
Table 1: Six-Circuit Biotypes of Depression and Anxiety
| Biotype Name | Defining Circuit Features | Associated Clinical & Behavioral Correlates | Treatment Response Profile |
|---|---|---|---|
| Biotype 1 | Hyperconnectivity in cognitive control regions; reduced task-evoked activation during cognitive control [13]. | Higher anhedonia; worse performance on executive function tasks [13] [75]. | Better response to venlafaxine (Effexor) [75] [78]. |
| Biotype 2 | Distinct profiles of intrinsic task-free functional connectivity within default mode, salience, and frontoparietal attention circuits [13]. | Associated with specific symptom profiles [13]. | Research ongoing for optimal treatment matching. |
| Biotype 3 | Higher resting-state activity in regions associated with depression and problem-solving [75]. | Makes errors on executive function tasks but performs well on cognitive tasks [75]. | Better response to behavioral talk therapy [75] [78]. |
| Biotype 4 | Lower activity at rest in the circuit controlling attention [75]. | Difficulty with attention and engagement [75]. | Less likely to benefit from talk therapy alone [75] [78]. |
| Biotype 5 | Defined by distinct patterns of activation and connectivity within frontal and subcortical regions elicited by emotional and cognitive tasks [13]. | Associated with specific symptom profiles [13]. | Research ongoing for optimal treatment matching. |
| Biotype 6 | No noticeable differences in the imaged regions compared to healthy controls [75]. | Suggests dysfunction in circuits not captured by the standard imaging protocol [75]. | Research ongoing for optimal treatment matching. |
This model demonstrates that biotypes have direct clinical utility. For instance, the biotype characterized by overactivity in cognitive regions responded best to the antidepressant venlafaxine, while the biotype with high activity in problem-solving areas showed greater improvement with behavioral talk therapy [75]. Furthermore, using fMRI to identify the "cognitive biotype" improved prediction of antidepressant remission likelihood from 36% to 63% [78].
Four-Biotype Model from Resting-State Connectivity
An earlier but influential 2016 study defined four depression biotypes based solely on resting-state functional connectivity within frontostriatal and limbic networks [77]. Using canonical correlation analysis to link connectivity features with symptom profiles, followed by hierarchical clustering in a multisite sample, the researchers identified four biotypes with distinct dysfunctional connectivity patterns that predicted responsiveness to transcranial magnetic stimulation (TMS) therapy [77].
Table 2: Four Resting-State Connectivity Biotypes of Depression
| Biotype | Defining Connectivity Features | Associated Symptom Profile |
|---|---|---|
| Biotype 1 | Reduced connectivity in frontoamygdala and anterior cingulate/orbitofrontal networks [77]. | Increased anxiety, anergia, and fatigue [77]. |
| Biotype 2 | Reduced connectivity in anterior cingulate and orbitofrontal networks [77]. | Increased anergia and fatigue; overall lower depression severity [77]. |
| Biotype 3 | Hyperconnectivity in thalamic and frontostriatal networks [77]. | Increased anhedonia and psychomotor retardation [77]. |
| Biotype 4 | Combined reduced frontoamygdala connectivity and hyperconnectivity in thalamic/frontostriatal networks [77]. | Increased anxiety, anhedonia, and psychomotor retardation [77]. |
This model confirmed that connectivity-based biotypes could not be differentiated by overall depression severity alone and could not be recapitulated solely from clinical symptom measures, underscoring the unique value of neuroimaging data for patient stratification [77].
Experimental Protocols for Biotyping Research
Standardized fMRI Acquisition and Processing Protocol
The six-biotype study established a rigorous, standardized protocol for image acquisition and processing, crucial for ensuring reproducibility and clinical translation [13].
Imaging Protocol:
- Data Modalities: Acquire both task-free (resting-state) and task-evoked fMRI data.
- Task Design: Implement cognitive and emotional probes during fMRI scanning. These typically include:
- Emotional Tasks: Exposure to sad stimuli, conscious threat stimuli, and non-conscious threat stimuli to activate the negative affect circuit.
- Cognitive Tasks: Tests of cognitive control and executive function to engage the cognitive control and attention circuits [13].
- Scanner Harmonization: Utilize identical fMRI scanning sequences across multiple study sites to control for technical variability.
Image Processing with the Stanford Et Cere System:
- Preprocessing: Standard steps include motion correction, co-registration to a standard template (e.g., MNI space), and spatial smoothing.
- Circuit Score Quantification: For each participant, extract 41 standardized measures of activation and functional connectivity within and across the six predefined brain circuits of interest.
- Individualized Z-Scoring: Express each circuit measure in standard deviation (s.d.) units relative to the mean of a healthy reference sample. This creates personalized "regional circuit scores" that are interpretable for each individual patient [13].
- Feature Input for Clustering: Use these 41 regional circuit scores as the feature inputs for subsequent clustering algorithms.
Experimental workflow for defining depression biotypes
Cluster Analysis and Biotype Validation
The process of defining biotypes from imaging data requires robust statistical learning and validation.
Clustering Methodology:
- Algorithm Selection: Apply hierarchical clustering to the matrix of personalized circuit scores.
- Cluster Number Determination: Generate solutions for a range of clusters (e.g., 2-15) and use the "elbow method" to identify the optimal number where adding more clusters provides diminishing returns [13].
Multi-Step Validation:
- Statistical Significance: Perform simulation-based significance testing of the silhouette index, comparing the actual data's clustering quality to that of a multivariate normal distribution and a permutation of the circuit scores across participants [13].
- Cluster Stability: Assess stability using cross-validation techniques such as leave-one-out and leave-20%-out, calculating the Adjusted Rand Index (ARI) to measure consistency. An ARI > 0.75 for leave-one-out is considered indicative of good stability [13].
- Theoretical Consistency: Evaluate whether the resulting biotype solution aligns with the pre-specified theoretical framework of circuit dysfunction in depression and anxiety [13] [76].
- Clinical and Behavioral Validation: Test for significant differences between biotypes in symptom profiles, performance on computerized behavioral tests (e.g., general and emotional cognition), and—most critically—differential outcomes following pharmacotherapy or behavioral therapy [13].
Advanced Predictive Modeling and Future Directions
Machine Learning for Treatment Prediction
Beyond subtyping, machine learning models are being developed to directly predict individual treatment response. One advanced approach is the Hierarchical Local-Global Imaging and Clinical Feature Fusion Graph Neural Network (LGCIF-GNN) [4]. This model:
- Constructs dynamic, task-specific brain graphs by adaptively updating adjacency matrices based on pairwise similarities of Region of Interest (ROI)-level temporal embeddings.
- Uses a Bidirectional Gated Recurrent Unit (bi-GRU) encoder to capture rich temporal dependencies in the fMRI time series.
- Implements a local-global architecture that jointly models fine-grained, ROI-level functional dynamics within each subject (local graph) and inter-subject relationships at the population level (global graph) [4].
- Integrates multimodal data, including clinical features like age, symptom severity, and illness duration, with neuroimaging features to enhance predictive power.
This model achieved 76.21% accuracy in predicting remission to SSRIs in a cohort of 279 MDD patients, highlighting the potential of advanced AI to translate biotyping research into clinically actionable tools [4].
Graph neural network prediction model
Emerging Frontiers and Clinical Translation
Future research directions focus on expanding biotype validity and developing novel treatments.
- Novel Treatment Targets: Research is exploring the therapeutic potential of non-standard pharmaceuticals, such as the general anesthetic propofol, to modulate key electrophysiological biomarkers (e.g., slow-wave activity) linked to depression. Personalized dosing regimens are being developed using data-driven modeling to achieve the optimal therapeutic "sweet spot" for each patient [5].
- Clinical Implementation: Researchers have begun using the fMRI biotyping technique in experimental clinical protocols. Ongoing work aims to establish easy-to-follow standards so that practicing psychiatrists can implement this approach to guide treatment selection, moving toward a future where a brain scan is part of a routine screening assessment for depression [75].
Table 3: Key Reagents and Resources for Depression Biotyping Research
| Category | Item/Resource | Function and Application in Biotyping Research |
|---|---|---|
| Imaging Hardware | 3T fMRI Scanner | Acquires high-resolution blood-oxygen-level-dependent (BOLD) signals for measuring brain activity and connectivity [13] [77]. |
| Software & Platforms | Stanford Et Cere Image Processing System | Standardized pipeline for quantifying personalized brain circuit scores from fMRI data [13]. |
| Analysis Tools | Hierarchical Clustering Algorithms | Unsupervised machine learning method for grouping patients into biotypes based on similarity of circuit dysfunction profiles [13] [77]. |
| Analysis Tools | Graph Neural Networks (GNNs) | Advanced AI models (e.g., LGCIF-GNN) that learn from brain network structure and temporal dynamics to predict treatment outcomes [4]. |
| Task Paradigms | Emotional Probe Tasks (e.g., face emotion recognition) | Activate threat and negative affect circuits (amygdala, hippocampus, ACC) to quantify task-evoked dysfunction [13] [76]. |
| Task Paradigms | Cognitive Control Tasks (e.g., Go/No-Go, N-back) | Engage cognitive control and attention circuits (prefrontal, frontoparietal) to assess executive function deficits [13] [4]. |
| Reference Data | Healthy Control Normative Database | Provides a baseline for calculating individualized Z-scores for circuit function, enabling interpretable, patient-level metrics [13]. |
| Clinical Instruments | Hamilton Depression Rating Scale (HAMD) | Gold-standard clinician-rated assessment to quantify symptom severity and correlate with circuit dysfunction [77] [4]. |
The classification of depression using imaging-defined biotypes represents a fundamental advance beyond the limitations of the DSM criteria. By grounding subtyping in the dysfunction of large-scale neural circuits—including the default mode, salience, threat, reward, attention, and cognitive control systems—this approach provides a biologically coherent and clinically actionable taxonomy. The identification of six distinct biotypes, validated through differential symptom profiles, behavioral performance, and treatment outcomes, demonstrates the profound potential of this paradigm. As research progresses, integrating advanced computational models and novel treatment modalities, circuit-based biotyping is poised to translate neuroscience into real-world clinical practice, finally enabling a precision medicine approach for the millions of individuals living with depression and anxiety.
Major depressive disorder (MDD) represents a significant global mental health challenge, characterized by high clinical heterogeneity and substantial variability in individual treatment response. Current clinical practice typically relies on empirical, trial-and-error strategies for antidepressant selection, resulting in remission rates of only 36% to 48% for first-line treatments [4]. This diagnostic and therapeutic imprecision prolongs patient suffering, increases the risk of chronic or treatment-resistant depression, and underscores the urgent need for objective, biologically-based tools to guide personalized therapeutic interventions [4]. Circuit-based biomarkers, derived primarily from functional magnetic resonance imaging (fMRI), have emerged as promising candidates for addressing this challenge by quantifying dysfunction within specific neural networks underlying depression symptomatology [13]. By moving beyond syndromal diagnoses to identify clinically distinct biotypes with shared neurobiological dysfunctions, these biomarkers hold potential to revolutionize depression treatment by enabling targeted selection of pharmacological and behavioral interventions based on an individual's unique neural circuit profile [13].
Methodological Approaches for Circuit Biomarker Discovery
Advanced Computational Modeling Techniques
Cutting-edge machine learning approaches, particularly graph neural networks (GNNs), are advancing the field beyond traditional models like support vector machines or logistic regression. The hierarchical local-global imaging and clinical feature fusion GNN (LGCIF-GNN) represents one such advanced framework that integrates multimodal data including fMRI, clinical, and demographic information [4]. This model performs dynamic graph structure optimization by adaptively updating adjacency matrices based on pairwise similarities of region-of-interest (ROI) level temporal embeddings extracted via bidirectional gated recurrent unit (bi-GRU) encoders. This learnable, task-driven graph construction captures richer temporal dependencies than static correlation methods and aligns graph topology with treatment prediction objectives [4].
The local-global architecture jointly models intra-subject ROI-level dynamics and inter-subject population-level similarities. The validation of these computational approaches demonstrates impressive predictive accuracy, with one model achieving 76.21% accuracy (AUC = 0.78) in predicting remission to selective serotonin reuptake inhibitors (SSRIs) in validation datasets [4].
Standardized Circuit Quantification Systems
The Stanford Et Cere Image Processing System exemplifies a standardized approach for quantifying task-free and task-evoked brain circuit function at the individual participant level [13]. This system generates 41 measures of activation and connectivity across six brain circuits of interest, expressed in standard deviation units from the mean of a healthy reference sample. These interpretable circuit scores provide personalized metrics of dysfunction across key networks including the default mode, salience, frontoparietal attention, and negative/positive affect circuits [13]. The reliability of these measures has been demonstrated through psychometric validation for construct validity, internal consistency, and generalizability, providing a foundation for clinically applicable biomarker development.
Table 1: Key Brain Circuits Implicated in Depression Pathology and Treatment Response
| Circuit Name | Key Brain Regions | Primary Functional Role | Association with Depression Symptoms |
|---|---|---|---|
| Negative Affect Circuit | Amygdala, insula, anterior cingulate cortex (ACC) | Threat detection, emotional salience | Depressed mood, anxiety, negative bias [79] |
| Reward Circuit | Ventral striatum, ventral pallidum, OFC, ACC, thalamus | Reward processing, motivation | Anhedonia, reduced motivation [4] |
| Default Mode Network | Medial prefrontal cortex, posterior cingulate, inferior parietal | Self-referential thought, introspection | Rumination, negative self-focus [80] |
| Cognitive Control Network | Dorsolateral prefrontal cortex, dorsal ACC, parietal regions | Executive function, cognitive control | Difficulties with concentration, executive dysfunction [13] |
| Salience Network | Anterior insula, dorsal ACC | Detecting behaviorally relevant stimuli | Altered attention to emotional stimuli [13] |
Key Circuit Biomarkers of Treatment Response
Negative Affect Circuit Biomarkers
The negative affect circuit, particularly the amygdala, insula, and anterior cingulate cortex (ACC), has emerged as a consistently important predictor and mediator of treatment response across multiple intervention modalities. A 2025 coordinate-based meta-analysis synthesizing data from 302 depressed patients across 18 experiments identified the right amygdala (peak MNI coordinates [30, 2, -22]) as a consistent region of change following various depression treatments, including pharmacology, psychotherapy, electroconvulsive therapy, psilocybin, and ketamine [23]. Follow-up analyses indicated that this finding was driven by decreased right amygdala activity following successful treatment [23].
Research examining problem-solving therapy (PST) in depressed patients with comorbid obesity found that reduced amygdala activation in response to threat stimuli at two months mediated subsequent improvements in depression severity [79]. This study also demonstrated that PST tempered the relationship between insula activation and improvements in problem-solving ability, suggesting that the negative affect circuit serves as an important neural target and mediator of behavioral interventions [79].
Multi-Circuit Biotyping for Treatment Stratification
Recent research has identified six clinically distinct biotypes defined by unique profiles of intrinsic task-free functional connectivity within the default mode, salience, and frontoparietal attention circuits, along with activation and connectivity patterns within frontal and subcortical regions during emotional and cognitive tasks [13]. These biotypes demonstrate distinct symptom profiles, performance on cognitive tests, and differential responses to both pharmacotherapy and behavioral therapy [13].
The identification of these biotypes represents a significant advance by providing a theory-driven, clinically validated, and interpretable quantitative method to parse the biological heterogeneity of depression and anxiety. This approach offers a promising pathway toward precision clinical care in psychiatry by moving beyond symptom-based diagnoses to target specific neurobiological dysfunctions with appropriate interventions [13].
Table 2: Predictive Power of Circuit-Based Biomarkers Across Treatment Modalities
| Biomarker Type | Predictive Accuracy | Key Brain Regions | Treatment Modality | Clinical Utility |
|---|---|---|---|---|
| Local-Global Graph Neural Network | 76.21% accuracy (AUC=0.78) [4] | Right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, bilateral ACC | SSRIs | Prediction of remission after 8-12 weeks of treatment |
| Negative Affect Circuit Change | Mediation of clinical improvement [79] | Amygdala, insula | Problem-solving therapy | Early neural marker of treatment response |
| Multi-Circuit Biotyping | Differential response to pharmacotherapy vs. behavioral therapy [13] | Default mode, salience, attention circuits, frontal and subcortical regions | Multiple treatment types | Stratification for treatment selection |
Experimental Protocols and Methodologies
fMRI Acquisition and Processing Protocols
Standardized neuroimaging protocols form the foundation of reliable circuit biomarker identification. The recommended approach includes acquiring both task-free and task-evoked fMRI data using consistent scanning parameters across study sites [13]. For task-based protocols, well-validated emotional and cognitive probes should be employed, including facial emotion perception tasks to engage the negative affect circuit [79] and cognitive control tasks such as the n-back or Tower of London to assess frontoparietal network function [80].
Image preprocessing should include standard steps: realignment, normalization, smoothing, and denoising to mitigate artifacts. For functional connectivity analysis, methods such as seed-based correlation, independent component analysis, or graph-based approaches can be applied to quantify connectivity within and between networks [4] [13]. Task-evoked analyses should employ general linear models with appropriate regressors for conditions of interest, with careful attention to modeling and correcting for motion artifacts [13].
Biomarker Validation Frameworks
Rigorous validation of proposed circuit biomarkers requires a multi-step process. First, cross-validation within the discovery sample assesses generalizability, followed by validation in independent samples to ensure robustness [4]. Next, clinical validation should establish relationships between biomarker profiles and specific symptom domains, cognitive performance, and functional outcomes [13]. Finally, predictive validation should demonstrate the biomarker's ability to stratify patients according to treatment outcomes across multiple intervention types [13].
For biotyping approaches, cluster stability should be assessed through methods such as leave-one-out and leave-20%-out cross-validation, with solutions demonstrating adjusted Rand indices (ARI) >0.75 considered stable [13]. The interpretability of biomarkers should be prioritized over black-box approaches to facilitate clinical translation and understanding of underlying mechanisms [13].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Materials and Tools for Circuit Biomarker Research
| Research Tool Category | Specific Examples | Primary Function | Key Considerations |
|---|---|---|---|
| Neuroimaging Acquisition | 3T fMRI scanners, standardized protocols | Brain activity and connectivity measurement | Protocol consistency across sites essential [13] |
| Computational Frameworks | Graph Neural Networks (GNNs), bi-GRU encoders | Modeling complex brain network dynamics | Balance between model complexity and interpretability [4] |
| Behavioral Tasks | Facial emotion tasks, cognitive control tasks | Engaging specific neural circuits | Task design determines neural systems engaged [79] [80] |
| Clinical Assessment Tools | HAMD, PHQ-9, QLES Questionnaire | Quantifying symptom severity and functional outcomes | Multidimensional assessment captures different outcome domains [4] |
| Circuit Quantification Systems | Stanford Et Cere Image Processing System | Standardized individual-level circuit metrics | Enables personalized biomarkers and cross-study comparison [13] |
Visualization of Research Workflows
Experimental Workflow for Biomarker Development
Neural Circuits in Depression Biotyping
Future Directions and Clinical Translation
The field of circuit-based biomarkers for depression treatment is rapidly advancing toward clinical application. Promising directions include the development of increasingly personalized predictive models that integrate multimodal data including neuroimaging, clinical, genetic, and digital phenotyping information [4]. Furthermore, the validation of biomarkers that can guide selection between specific treatment modalities—such as pharmacotherapy versus behavioral interventions—represents a critical step toward truly personalized mental health care [13].
Future research should prioritize the development of standardized assessment protocols that can be implemented across clinical settings, making biomarker-guided treatment selection feasible in real-world practice [13]. Additionally, prospective clinical trials that randomize patients to biomarker-guided versus treatment-as-usual arms are needed to definitively establish the clinical utility and cost-effectiveness of these approaches. As these tools mature, circuit-based biomarkers hold tremendous potential to transform depression care by replacing trial-and-error approaches with targeted, neurobiologically-informed treatment selection.
Overcoming Therapeutic Roadblocks: Treatment Resistance and the Limitations of Monoaminergic Drugs
Treatment-Resistant Depression (TRD) represents a significant and complex challenge within the field of psychiatric research and clinical practice. It describes a condition where individuals with Major Depressive Disorder (MDD) do not achieve adequate symptomatic relief following standard antidepressant therapies [81] [82]. The precise definition of TRD remains a subject of ongoing debate, hindering precise epidemiological estimates, risk factor identification, and the development of targeted, effective interventions [81] [83]. This whitepaper aims to synthesize current evidence on the prevalence and definitions of TRD, framing the discussion within the context of neural circuitry changes and antidepressant response research. A consensus on the TRD phenotype is crucial for advancing translational research, guiding treatment development, and informing clinical and policy decision-making [81]. This document provides researchers, scientists, and drug development professionals with a technical overview of the core issues surrounding TRD, serving as a foundation for understanding its neurobiological underpinnings and the investigational interventions aimed at addressing them.
Defining Treatment-Resistant Depression
The absence of a universally accepted and validated definition for TRD is a major limitation in the field [81]. This lack of consensus results in heterogeneous populations being enrolled in clinical trials, complicating the interpretation and generalizability of results and leading to disparities in clinical practice and patient outcomes [81] [83].
Current Regulatory and Clinical Definitions
The most widely adopted definition, used by regulatory bodies like the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA), characterizes TRD as the failure to respond to a minimum of two adequate antidepressant trials in the current depressive episode, despite optimal dosing, adequate duration (typically at least four weeks), and documented adherence to treatment [81] [82] [84]. The EMA explicitly states that the failed antidepressants can be from the same or different mechanistic classes [81]. A key prerequisite before diagnosing true TRD is the exclusion of pseudoresistance, which can arise from factors such as inadequate treatment duration or dosing, misdiagnosis, comorbid medical or psychiatric conditions, or pharmacokinetic issues [82].
Staging Models and Conceptual Frameworks
Beyond categorical definitions, several staging models have been proposed to operationalize treatment resistance along a continuum. A prominent example is the Thase and Rush staging model [81]. This model does not define TRD categorically but instead implies resistance along a spectrum of failed antidepressant trials:
- Stage I: Failure of at least one adequate trial of one major class of antidepressants.
- Stage II: Failure of at least two adequate trials of at least two distinctly different classes of antidepressants.
- Stage III: Stage II resistance plus failure of an adequate trial of a tricyclic antidepressant (TCA).
- Stage IV: Stage III resistance plus failure of an adequate trial of a monoamine oxidase inhibitor (MAOI).
- Stage V: Stage IV resistance plus failure of a course of bilateral electroconvulsive therapy (ECT).
The heterogeneity of these definitions has led to proposals for broader concepts, such as "Difficult-to-Treat Depression" (DTD), which aims to reflect a wider spectrum of clinical and neurobiological constellations that complicate treatment [82].
Table 1: Comparison of Major TRD Definitions and Staging Models
| Model | Categorical/Staging | Minimum Number of Failed Trials | Adequate Dose/Duration Specified | Key Differentiating Features |
|---|---|---|---|---|
| FDA/EMA | Categorical | 2 | Yes | Most widely used in regulatory and clinical contexts; failed trials can be from same/different classes [81]. |
| Thase & Rush | Staging | 1 (Stage I) | Yes | Conceptualizes resistance as a continuum; incorporates different antidepressant classes and ECT [81]. |
| Maudsley Model | Categorical | 1 | Yes | - |
| GSRD | Categorical | 2 | Yes | Requires failed antidepressants to be from different classes [81]. |
Epidemiology and Burden of TRD
Prevalence Estimates
The prevalence of TRD is directly influenced by the definition applied. Using the FDA/EMA criteria, it is currently estimated that approximately 30% of persons diagnosed with Major Depressive Disorder (MDD) meet the criteria for TRD [81] [82] [84]. A specific US-based study published in 2021 extrapolated that out of an estimated 8.9 million adults with medication-treated MDD, 2.8 million (30.9%) had TRD [85]. Some estimates suggest a wider prevalence range of 30% to 40% among antidepressant-treated patients, reflecting the application of varying definitions [83]. Globally, it is extrapolated that more than 100 million people meet one or more definitions of this condition [81].
Societal and Economic Burden
TRD is associated with a disproportionate share of the economic and societal burden attributable to MDD. A US cost-of-illness model estimated the total annual burden of medication-treated MDD at $92.7 billion, with $43.8 billion (47.2%) attributable to TRD [85]. The share of TRD was particularly high for healthcare costs (56.6%), underscoring the higher healthcare utilization and need for more intensive treatments associated with this condition [81] [85]. Beyond direct costs, TRD contributes significantly to indirect costs through greater impairment in psychosocial function, higher workplace disability and absenteeism, and a need for disability benefits [81]. Furthermore, the rate of suicidality, including completed suicide, is disproportionately higher in TRD populations [81].
Table 2: Economic Burden of Treatment-Resistant Depression in the United States
| Cost Category | Total Annual Burden (Medication-Treated MDD) | Share Attributable to TRD | Percentage of MDD Burden |
|---|---|---|---|
| Health Care Burden | $45.6 billion | $25.8 billion | 56.6% |
| Unemployment Burden | $18.2 billion | $8.7 billion | 47.7% |
| Productivity Burden | $28.9 billion | $9.3 billion | 32.2% |
| Total Burden | $92.7 billion | $43.8 billion | 47.2% |
Neural Circuitry and Neuroimaging in TRD Research
Understanding the neural correlates of both depression and treatment response is a critical frontier for defining TRD biologically and developing predictive biomarkers.
Common Neural Changes Following Treatment
A 2025 coordinate-based meta-analysis investigating brain activity changes following various depression treatments revealed a consistent change in the right amygdala [23]. This finding, which synthesized data from 302 depressed subjects across 18 experiments, indicated that successful treatment across multiple modalities (pharmacology, psychotherapy, ECT, ketamine, psilocybin) was associated with a decrease in activity in this region during emotion tasks [23]. This suggests the right amygdala may be a key region of convergence for treatment effects, potentially serving as a biomarker for tracking treatment response.
Distinct Neural Mechanisms of Different Treatments
While common change areas exist, quantitative synthesis of meta-analyses also reveals that different treatment modalities engage distinct neural circuits. A 2021 synthesis of three meta-analyses (n=4206) found that neural changes from psychotherapy and antidepressant medication did not significantly converge on any region [41]. Antidepressant medication was found to primarily evoke neural changes in subcortical structures like the amygdala, which is involved in the generation of affective sensations. In contrast, psychotherapy (primarily CBT) evoked changes in the medial prefrontal cortex, a region associated with cognitive control of affect, attention, and awareness of affective state [41]. This supports the theory of distinct proximal neurocognitive mechanisms of action for these treatment classes, despite both ultimately converging on the broader affect network.
Predicting Treatment Response with Neuroimaging
Advanced machine learning models applied to neuroimaging data are showing promise in predicting individual treatment outcomes, a key step towards personalized medicine for TRD. One 2025 study developed a hierarchical local-global imaging and clinical feature fusion graph neural network model (LGCIF-GNN) to predict remission to SSRIs [4]. The model, trained on 279 untreated MDD patients, achieved 76.21% accuracy (AUC=0.78) by integrating functional MRI data from circuits related to depressed mood and anhedonia (e.g., involving the globus pallidus, putamen, hippocampus, thalamus, and anterior cingulate gyrus) with clinical features such as age, sex, and symptom severity [4]. This highlights the potential of multimodal data integration for creating predictive tools.
Experimental Protocols and Research Reagents
This section details key methodologies cited in the research, providing a toolkit for scientists designing studies in this field.
Detailed Methodology: Coordinate-Based Meta-Analysis of Treatment Effects
Objective: To identify consistent brain activity changes following successful depression treatment across multiple treatment modalities [23].
Workflow:
- Literature Search & Study Selection: Identify published task-based functional neuroimaging studies (fMRI, PET, SPECT) that report pre- and post-treatment brain activation data in patients with depression. Studies must use standardized coordinate systems (e.g., MNI or Talairach).
- Data Extraction: Extract all reported significant foci of activation from the pre- vs. post-treatment contrasts from each included study.
- Activation Likelihood Estimation (ALE):
- Model each focus as a 3D Gaussian probability distribution, scaled according to the study's sample size.
- Compute the union of activation probabilities across all studies for each voxel in the brain, creating an ALE map.
- Test for statistically significant convergence of foci against a null hypothesis of random spatial clustering using permutation testing (e.g., 1000 permutations).
- Apply a cluster-level family-wise error (FWE) correction (e.g., P < 0.05) with a cluster-forming threshold of P < 0.001.
- Interpretation: Statistically significant clusters in the resulting ALE map represent brain regions where activity consistently changes following effective treatment.
Detailed Methodology: Predictive Modeling with Graph Neural Networks
Objective: To predict antidepressant treatment remission based on pre-treatment neurocircuitry and clinical features [4].
Workflow:
- Data Preprocessing:
- Imaging Data: Process resting-state or task-based fMRI data. Define Regions of Interest (ROIs) based on atlases. Extract BOLD time series for each ROI.
- Clinical Data: Collect and standardize clinical variables (e.g., HAMD scores, age, sex, education).
- Graph Construction:
- Construct a dynamic functional connectivity graph for each subject. Nodes represent ROIs. Edge weights are defined by the pairwise similarity of temporal embeddings of the BOLD time series, often using a bi-directional Gated Recurrent Unit (bi-GRU) encoder. This graph structure is learnable and optimized during training.
- Model Architecture (LGCIF-GNN):
- Local GNN: Processes the intra-subject functional connectivity graph to learn fine-grained, ROI-level dynamics.
- Global GNN: Constructs a population-level graph where nodes represent subjects and edges represent functional/clinical similarity. This GNN captures inter-individual relationships.
- Feature Fusion: Integrates the embeddings from the local and global GNNs with the clinical feature vector.
- Training & Validation: Train the model on a labeled dataset (remitters vs. non-remitters) using cross-validation and validate on held-out internal and external datasets.
Research Reagent Solutions
Table 3: Essential Materials and Reagents for TRD Research
| Item / Reagent | Function / Application in TRD Research |
|---|---|
| Functional MRI (fMRI) | Non-invasive measurement of brain activity via the BOLD signal; used to identify functional circuits, treatment-related changes, and predictive biomarkers [23] [4]. |
| Activation Likelihood Estimation (ALE) | A coordinate-based meta-analysis algorithm for identifying statistically significant convergence of brain activation foci across multiple neuroimaging studies [23] [41]. |
| Graph Neural Networks (GNNs) | Advanced machine learning models for processing graph-structured data; applied to functional brain connectivity graphs to predict treatment outcomes [4]. |
| Hamilton Depression Rating Scale (HAMD) | A clinician-administered assessment scale used to quantify the severity of depressive symptoms; a common clinical endpoint and input variable in predictive models [4]. |
| Regions of Interest (ROI) Atlases | Standardized parcellations of the brain (e.g., AAL, Harvard-Oxford) used to define nodes for functional connectivity analysis in neuroimaging studies [4]. |
| Bidirectional Gated Recurrent Unit (bi-GRU) | A type of recurrent neural network used to encode temporal dependencies in time-series data, such as fMRI BOLD signals, for dynamic graph construction [4]. |
The delayed onset of action of conventional antidepressants represents a critical limitation in the treatment of Major Depressive Disorder (MDD). Most standard pharmacological treatments require several weeks to months to achieve full therapeutic effects, during which patients remain symptomatic and functionally impaired, facing considerable morbidity and elevated risk of suicidal behavior [86]. This delay stands in stark contrast to treatments for many other medical conditions, which often produce rapid therapeutic effects within minutes or hours [86]. Understanding the neurobiological mechanisms underlying this delay is essential for developing novel, rapidly-acting therapeutics and advancing the field of depression treatment.
The clinical significance of this problem cannot be overstated. During the initial latency period before antidepressants take effect, patients experience ongoing disruption in personal, professional, family, and social life [86]. Perhaps most alarmingly, research has identified an increased risk of suicide during the first month of antidepressant treatment, particularly within the initial nine days [86]. This risk profile may result from a mismatch in the timing of symptom improvement, where physical energy improves before the resolution of depressive mood and negative thoughts [86].
Quantifying the Therapeutic Lag: Clinical Trajectories and Time Courses
Patterns of Antidepressant Response
The timing of antidepressant response varies significantly among individuals, with distinct patterns emerging from clinical studies:
| Response Pattern | Prevalence | Timeframe of Improvement | Clinical Implications |
|---|---|---|---|
| Early Improvement | ~20% of patients | Concentrated in first 3 weeks | May be maintained throughout treatment |
| Delayed Improvement | >50% of eventual remitters | More prominent in second 3 weeks than first 3 weeks | Outcome cannot be predicted from early timepoints |
| Non-response | Substantial proportion | No significant improvement | Require alternative treatment strategies |
Analysis of individual trajectories from the Genome-Based Therapeutic Drugs for Depression (GENDEP) study revealed that more than half of patients who eventually reached remission showed a pattern of delayed improvement, making accurate prediction of final outcome impossible before approximately 8 weeks of treatment [87].
Quantitative Treatment Effects
Large-scale analyses of clinical trial data submitted to the US Food and Drug Administration provide further insight into the distribution of antidepressant effects:
| Response Metric | Findings | Data Source |
|---|---|---|
| Maximum drug-placebo separation | 13.5% absolute improvement at 55th quantile | 232 trials (1979-2016) |
| Overall efficacy pattern | Small reduction in depression severity broadly distributed across participants | 57,313 participants with severe depression |
| Timing of accurate prediction | 8 weeks required for accurate outcome prediction | GENDEP study (811 participants) |
This data demonstrates that the therapeutic effects of conventional antidepressants are modest and gradual, with diminishing separation between active treatment and placebo at the distribution tails [88].
Neurobiological Mechanisms Underlying Delayed Onset
The Serotonin Autoreceptor Feedback Hypothesis
A predominant hypothesis explaining the delayed onset of antidepressants centers on the desensitization of 5-HT1A autoreceptors. Conventional serotonin-selective reuptake inhibitors (SSRIs) rapidly increase extracellular serotonin within hours of administration, but this initial increase engages strong feedback inhibition via 5-HT1A autoreceptors on serotonin neurons, resulting in a profound reduction in their firing rate [89].
Key experimental evidence supporting this mechanism includes:
- Electrophysiological recordings demonstrating decreased sensitivity of dorsal raphe serotonin neurons to 5-HT1A agonists after chronic SSRI administration [89]
- Microdialysis studies showing attenuation of 5-HT1A agonist effects on forebrain serotonin release following chronic antidepressant treatment [89]
- Second messenger assays revealing reduced 5-HT1A autoreceptor-stimulated signaling in the dorsal raphe after sustained antidepressant exposure [89]
The coincident timeline between 5-HT1A autoreceptor desensitization and the gradual restoration of serotonin neuron firing rate has led to the influential hypothesis that this gradual loss of feedback inhibition mediates the delayed therapeutic onset [89].
Limitations of the Desensitization Hypothesis
Despite the appealing simplicity of the autoreceptor desensitization hypothesis, recent evidence suggests a more complex picture. Research indicates that feedback inhibition persists even after chronic antidepressant treatment, demonstrated by the robust disinhibition of serotonin neurons when 5-HT1A receptors are blocked with antagonists such as WAY-100635 [89].
This suggests that the relationship between desensitization and firing rate recovery may be coincidental rather than causal. Baseline serotonin neuron firing rate appears to return to normal despite ongoing feedback inhibition, implying that compensatory changes override this inhibition through other mechanisms of homeostatic plasticity [89].
Methodologies for Investigating Antidepressant Mechanisms
Experimental Approaches for Studying Neural Circuits
Research into the neural circuitry of antidepressant response employs diverse methodological approaches:
| Methodology | Application in Depression Research | Key Insights Generated |
|---|---|---|
| Resting-state fMRI | Mapping functional connectivity alterations in reward and emotion circuits | Identification of striatal hypoconnectivity in youth at familial risk for depression [90] |
| Optogenetics | Precise manipulation of specific neural circuits with millisecond precision | Determination of neural populations sufficient to drive sleep-wake transitions [8] |
| Quantitative treatment effects analysis | Large-scale analysis of clinical trial data distributions | Characterization of modest, broadly distributed antidepressant effects [88] |
| Longitudinal latent class analysis | Identifying distinct trajectories of symptom change | Revelation of early versus delayed responder subtypes [87] |
The Scientist's Toolkit: Essential Research Reagents
| Research Tool | Function/Application | Experimental Utility |
|---|---|---|
| WAY-100635 | Selective 5-HT1A receptor antagonist | Blocks autoreceptor feedback inhibition to study disinhibition mechanisms [89] |
| Fos protein | Immediate early gene product marker of neuronal activation | Maps cellular activation patterns in response to pharmacological manipulation [89] |
| FHAM-S (Family History Assessment Module Screener) | Assesses familial risk for psychiatric disorders | Identifies high-risk populations for preventive intervention studies [90] |
| K-SADS-5 (Kiddie Schedule for Affective Disorders) | Standardized diagnostic assessment for youth | Ensures accurate phenotyping in developmental studies [90] |
| Network Correspondence Toolbox | Quantitative evaluation of neuroimaging results against multiple brain atlases | Standardizes reporting of functional network localization [91] |
Emerging Paradigms and Future Directions
Rapid-Acting Antidepressant Mechanisms
Research on novel rapid-acting antidepressants has highlighted the potential of glutamatergic targets, particularly the NMDA receptor antagonist ketamine, which can produce antidepressant effects within hours rather than weeks [86]. This rapid onset suggests that the therapeutic lag of conventional antidepressants is not an inevitable feature of depression treatment, but rather a limitation of current monoaminergic approaches.
The molecular basis of these rapid antidepressant actions appears to involve synaptic plasticity mechanisms distinct from the gradual adaptive changes associated with conventional antidepressants [86]. Understanding these mechanisms is likely to lead to the development of improved therapeutics that bypass the delayed onset characteristic of current treatments.
Neural Circuit Mapping in Depression Subtypes
Advanced neuroimaging approaches are revealing distinct neural correlates of depression subtypes, which may inform personalized treatment approaches. For example, peripartum depression demonstrates reversed structural and functional activity patterns in the insula, amygdala, precentral gyrus, and precuneus compared to non-peripartum major depression [92].
These findings support the existence of a consistent pattern of dysregulation associated with emotional regulation, cognition, and maternal caregiving in women with peripartum depression, highlighting the need for targeted interventions and suggesting potentially different response trajectories across depression subtypes [92].
Methodological Innovations for Circuit-Level Analysis
The development of standardized analytical tools represents a significant advancement in depression neuroscience. The Network Correspondence Toolbox enables quantitative evaluation of novel neuroimaging results against multiple functional brain atlases, facilitating more consistent reporting and interpretation of findings across studies [91].
Such methodological innovations are crucial for addressing the challenge of inconsistent nomenclature in functional network labeling, which has complicated comparisons across studies and limited integration of novel discoveries [91]. Standardized approaches will enhance our ability to identify robust neural circuit markers of treatment response.
The delayed onset of action of conventional antidepressants remains a significant challenge in depression treatment, with profound clinical implications for patient suffering and functional impairment. The neurobiological mechanisms underlying this delay involve complex adaptive changes in serotonin systems, particularly the gradual desensitization of 5-HT1A autoreceptors and subsequent recovery of serotonin neuron firing rates, though these phenomena may be coincidental rather than causally related [89].
Future research directions should focus on alternative molecular targets beyond monoaminergic systems, particularly glutamatergic pathways that demonstrate more rapid antidepressant effects [86]. Additionally, refined methodological approaches for mapping neural circuits and their functional connectivity will enhance our understanding of depression heterogeneity and treatment response variability [90] [91]. The development of novel therapeutics that bypass the delayed onset characteristic of current antidepressants represents a critical frontier in depression research with the potential to transform clinical practice and patient outcomes.
The therapeutic action of antidepressants is inextricably linked to their effects on the brain's complex neural circuitry. While these medications are cornerstone treatments for Major Depressive Disorder (MDD), their benefits are often accompanied by unwanted side effects that impact patient quality of life and treatment continuity. Emotional blunting and weight gain represent two of the most clinically significant adverse effects, contributing substantially to premature treatment discontinuation and relapse. Contemporary research has shifted from a singular focus on neurotransmitter systems toward a circuit-based understanding of both therapeutic and adverse effects. Evidence indicates that emotional blunting and weight gain are not random occurrences but rather stem from specific, medication-induced alterations in neural circuits governing emotional processing and metabolic regulation [41] [93]. This whitepaper synthesizes current scientific evidence on the neural mechanisms, prevalence, and management strategies for these side effects, providing researchers and drug development professionals with a circuit-focused framework for optimizing future antidepressant therapies.
Emotional Blunting: Neural Mechanisms and Clinical Management
Clinical Definition and Diagnosis
Antidepressant-Induced Emotional Blunting (AIEB) is formally defined as a patient-reported reduction in the capacity to experience the full spectrum of human emotions that begins or worsens after antidepressant initiation or dose increase [93]. Patients consistently describe feeling emotionally "dulled," "numbed," or "flattened," reporting a distinct shift from affective to cognitive processing wherein they experience thoughts about events rather than genuine feelings [93]. This condition affects 40-60% of patients taking serotonergic antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), making it a prevalent clinical concern [93] [94].
Accurate diagnosis requires differentiation from residual depressive symptoms. The table below outlines key diagnostic differentiations:
Table 1: Differential Diagnosis of Emotional Blunting
| Condition | Key Features | Emotional Experience | Timing/Context |
|---|---|---|---|
| Emotional Blunting | Dampened intensity of all emotions (positive & negative) | "I know I should feel happy/sad, but I don't" | Emerges after antidepressant initiation |
| Anhedonia | Inability to experience pleasure | "Nothing brings me joy anymore" | Core symptom during depressive episodes |
| Apathy | Loss of motivation, interest, or initiative | "I don't care about anything" | Behavioral change more prominent than affective |
| Residual Depression | Incomplete remission of depression | "I'm better but still feel down" | Continuous from original depressive episode |
The Oxford Depression Questionnaire (ODQ) serves as a validated, patient-rated scale designed to quantify severity and track changes in emotional blunting over time [93].
Proximal Neural Circuit Mechanisms
Neuroimaging meta-analyses reveal that antidepressants and psychological therapies evoke distinct neural changes, with pharmacological interventions primarily impacting subcortical structures. A quantitative synthesis of three meta-analyses (n=4,206) demonstrated that antidepressant medication evokes neural changes predominantly in the amygdala, a key region for generating affective and visceral sensations [41]. This is contrasted with psychotherapy, which preferentially modulates the medial prefrontal cortex (mPFC), a region implicated in cognitive control of affect [41].
The following diagram illustrates the primary neural circuits implicated in emotional blunting:
Figure 1: Neural Circuit Mechanisms of Emotional Blunting. SSRI/SNRI-mediated increases in synaptic serotonin activate 5-HT2C receptors, inhibiting mesolimbic dopamine pathways and altering mPFC-amygdala circuitry, ultimately leading to blunted emotional experience.
The Dopamine Suppression Hypothesis provides a crucial mechanism for AIEB. The brain's serotonin and dopamine systems maintain an intricate inverse relationship, wherein 5-HT2C receptor activation downregulates dopamine release in mesolimbic (reward processing) and mesocortical (motivation) pathways [93]. This dopaminergic suppression leads to reduced reward sensitivity, diminished motivation, and flattened emotional salience. Supporting this model, non-serotonergic antidepressants like bupropion demonstrate significantly lower rates of emotional blunting [93].
Advanced research models have further elucidated these mechanisms through the Reinforcement Learning Deficit Model. A 2023 study revealed that SSRIs specifically impair probabilistic reversal learning—the ability to adapt behavior when reward/punishment contingencies change [93]. Participants could process consequences intellectually but couldn't feel their emotional impact, directly linking circuit-level dysfunction to subjective emotional experience.
Comparative Risk Across Antidepressant Classes
The risk of emotional blunting varies significantly across antidepressant classes, reflecting their distinct mechanisms of action:
Table 2: Emotional Blunting Risk Profile by Antidepressant Class
| Antidepressant Class | Risk Level | Reported Prevalence | Clinical Notes |
|---|---|---|---|
| SSRIs | High | 40-60% | Most consistently associated with AIEB; some analyses note ≤6% increase post-acute treatment |
| SNRIs | High | 5.8-50% | Some surveys report higher rates with duloxetine |
| TCAs | Moderate | ~30-50% | Possibly higher with serotonergic TCAs (e.g., clomipramine) |
| Bupropion (NDRI) | Low | ~33% | Lowest risk profile among common antidepressants |
| Vortioxetine | Low | Limited data | Multimodal mechanism; improvement after switch from SSRI/SNRI |
Weight Gain: Metabolic Circuits and Pharmacological Mechanisms
Epidemiology and Clinical Impact
Weight gain represents one of the most frequently reported adverse effects of antidepressant treatment, affecting 55-65% of patients on long-term therapy [95]. A major 2025 analysis of 151 clinical trials (n>58,000) revealed substantial variation in weight change profiles across 30 different antidepressants, with differences of up to 4 kg in average weight change between some drugs within the first eight weeks of treatment [96] [97]. Certain medications like agomelatine were associated with approximately 2.5 kg of weight loss, while others like maprotiline led to about 2 kg of weight gain [97]. This metabolic adverse effect contributes significantly to treatment discontinuation, relapse, and worsened metabolic health outcomes, including increased risk for obesity and type 2 diabetes [95].
Neurobiological Pathways in Appetite Regulation
Antidepressant-induced weight gain involves complex interactions between central appetite regulation circuits and peripheral metabolic signals. The serotonergic system plays a fundamental role through multiple interconnected pathways:
The dorsal raphe nucleus (DRN) contains approximately 35% of serotonergic neurons in the central nervous system and suppresses appetite through multiple mechanisms, including innervation of the mediobasal hypothalamus [95]. Serotonergic neurons from the DRN project to key appetite regulation centers including the lateral hypothalamic area (LHA), bed nucleus of the stria terminalis (BNST), and arcuate nucleus (ARH) [95]. A recent mechanistic study demonstrated that activating the DRN serotonergic pathway to the ARH decreases food intake by depolarizing anorexigenic proopiomelanocortin (POMC) neurons while simultaneously hyperpolarizing orexigenic agouti-related peptide (AgRP) neurons [95].
The following diagram illustrates the comprehensive neural pathways regulating appetite that are affected by antidepressants:
Figure 2: Neural Circuits of Appetite Regulation Affected by Antidepressants. Antidepressants modulate serotonergic signaling from the Dorsal Raphe Nucleus to key hypothalamic regions like the Arcuate Nucleus, influencing the balance between anorexigenic POMC neurons and orexigenic AgRP neurons.
Different serotonin receptor subtypes mediate varying effects on food intake. Activation of 5-HT2C receptors reduces food intake, while antagonism of these receptors—as seen with mirtazapine—increases appetite and promotes weight gain [95]. This receptor-specific mechanism explains why certain antidepressants with strong 5-HT2C antagonism produce more substantial weight gain than others.
Beyond central mechanisms, peripheral pathways contribute to antidepressant-induced weight gain. These include:
- Receptor desensitization with chronic treatment
- Development of insulin resistance
- Altered levels of metabolic hormones including leptin and ghrelin [95]
Comparative Weight Gain Profiles Across Antidepressants
The 2025 Lancet analysis provided comprehensive comparative data on weight change across antidepressant classes, demonstrating clear stratification of metabolic risk:
Table 3: Weight Change Profiles of Common Antidepressants
| Antidepressant | Class | Weight Change Profile | Clinical Implications |
|---|---|---|---|
| Agomelatine | Melatonin agonist/5-HT2C antagonist | ~2.5 kg weight loss | Favorable metabolic profile |
| Maprotiline | Tetracyclic antidepressant | ~2 kg weight gain | Nearly 50% of users experience weight gain |
| Amitriptyline | Tricyclic antidepressant | Significant weight gain | High metabolic risk; careful monitoring required |
| SSRIs (sertraline, fluoxetine) | SSRI | Variable, typically mild long-term gain | Generally favorable short-term profile |
| Bupropion | NDRI | Weight neutral/loss | Preferred option for weight-concerned patients |
Impact on Treatment Adherence and Strategies for Mitigation
Adherence Challenges and Circuit-Based Predictors
Side effects represent a primary driver of antidepressant discontinuation, with emotional blunting and weight gain being among the most frequently cited reasons for non-adherence [93] [94]. Approximately one-third of patients never disclose symptoms of emotional blunting to their providers, potentially due to concerns about being dismissed or misinterpreting these symptoms as worsening depression [93]. This communication gap substantially complicates treatment optimization and contributes to the high rates of premature discontinuation.
Emerging research utilizing advanced neuroimaging techniques offers promise for predicting individual vulnerability to side effects. Functional magnetic resonance imaging (fMRI) studies have identified that dysfunction in reward and emotion regulation circuits is closely associated with anhedonia and depressed mood—circuits that also appear vulnerable to emotional blunting [4]. Machine learning approaches, particularly graph neural networks (GNNs), have demonstrated capability in predicting antidepressant response based on pre-treatment neurocircuitry, achieving up to 76.21% accuracy in predicting remission [4]. Key contributing brain regions include the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus [4]. These circuit-based predictors represent a promising avenue for pre-emptively identifying patients at high risk for adverse effects.
Evidence-Based Management Strategies
Emotional Blunting Management
First-line management for emotional blunting involves dose reduction by 25-50% if clinically feasible [93]. When switching antidepressants is necessary, evidence supports transitioning to:
- Bupropion: Demonstrates the lowest risk of emotional blunting (approximately 33%) and additionally addresses co-occurring sexual dysfunction [93]
- Vortioxetine: Shows improvement in open-label studies after switching from SSRIs/SNRIs, potentially related to its multimodal mechanism [93] [94]
- Mirtazapine or agomelatine: Theoretical benefit via 5-HT2C blockade, though clinical evidence remains limited [93]
Switching within the SSRI class is typically ineffective, and routine use of antipsychotics for managing emotional blunting is not recommended due to unfavorable risk-benefit profiles [93].
Weight Gain Mitigation
Strategies for addressing antidepressant-induced weight gain include:
- Medication switching: Transitioning to antidepressants with more favorable metabolic profiles (e.g., bupropion, agomelatine, or vortioxetine) [95] [96]
- Adjunctive medications: Adding agents like metformin or GLP-1 receptor agonists to counteract weight gain [95]
- Lifestyle interventions: Implementing structured dietary and exercise programs to mitigate metabolic effects [95]
The selection of mitigation strategies should be individualized based on patient-specific risk factors, including baseline body mass index, genetic factors (e.g., CYP2C19 metabolizer status), and lifestyle considerations [95].
Advanced Research Methodologies and Future Directions
The Scientist's Toolkit: Experimental Approaches
Cutting-edge research into antidepressant side effects utilizes sophisticated methodologies capable of elucidating circuit-level mechanisms:
Table 4: Advanced Research Methodologies for Circuit Analysis
| Methodology | Function | Application in Side Effect Research |
|---|---|---|
| Graph Neural Networks (GNNs) | Machine learning approach that updates node representations by aggregating information from neighboring nodes | Predicts treatment remission (76.21% accuracy) based on pre-treatment neurocircuitry [4] |
| Activation Likelihood Estimation (ALE) | Coordinate-based meta-analysis algorithm for identifying convergence of brain activation across studies | Identified amygdala changes with antidepressants vs. mPFC changes with psychotherapy [41] |
| Optogenetics | Light-sensitive channels enabling precise temporal control of specific neuronal populations | Elucidates contributions of PFC circuitry to depression-like behavior [98] |
| Chemogenetics (DREADDs) | Engineered receptors activated by exogenous ligands for neuronal manipulation | Allows prolonged modulation of specific circuits without implanted hardware [98] |
| fMRI Dynamic Connectivity | Measures time-resolved functional connectivity between brain regions | Captures spatiotemporal dynamics in reward and emotion circuits [4] |
Emerging Research Paradigms
Future research directions emphasize personalized approaches based on circuit-level understanding:
- Circuit-Based Biotypes: Functional neuroimaging is evolving toward identifying depression biotypes based on distinct circuit dysfunction patterns, which may predict both treatment response and vulnerability to specific side effects [99]
- Temporal Dynamics of Circuit Adaptation: Emerging evidence suggests that the neural changes underlying both therapeutic and adverse effects follow distinct temporal patterns, with emotional blunting potentially resulting from progressive circuit adaptation rather than acute effects [41]
- Multimodal Data Integration: Advanced models like the hierarchical local-global imaging and clinical feature fusion graph neural network (LGCIF-GNN) integrate functional connectivity with clinical and demographic data to enhance prediction accuracy [4]
The following diagram illustrates an integrated experimental workflow for investigating antidepressant side effects:
Figure 3: Integrated Workflow for Predicting Antidepressant Side Effects. This experimental pipeline combines neuroimaging, clinical assessment, and machine learning to identify circuit biomarkers associated with vulnerability to emotional blunting and weight gain.
Emotional blunting and weight gain represent significant challenges in antidepressant therapy, rooted in specific alterations to neural circuits governing emotional processing and metabolic regulation. The circuit-based approach detailed in this whitepaper provides a sophisticated framework for understanding these adverse effects, moving beyond neurotransmitter-specific models to integrated network perspectives. Current evidence indicates that emotional blunting involves serotonergically-mediated dampening of prefrontal-limbic-amygdala circuitry and suppression of dopaminergic reward pathways, while weight gain stems from complex interactions between central appetite regulation circuits and peripheral metabolic signals. Advanced methodologies including graph neural networks, optogenetics, and coordinate-based meta-analyses are accelerating our understanding of these mechanisms. Future research directions emphasizing circuit-based biotypes, temporal dynamics of neural adaptation, and multimodal data integration hold promise for developing novel antidepressants that maintain therapeutic efficacy while minimizing these burdensome side effects, ultimately improving long-term treatment outcomes for patients with major depressive disorder.
Major depressive disorder (MDD) remains a leading global cause of disability, with approximately one-third of patients failing to achieve remission after multiple adequate trials of conventional monoamine-based antidepressants [100]. This treatment-resistant depression (TRD) represents a critical challenge that necessitates moving beyond the serotonin and norepinephrine pathways that have dominated psychopharmacology for the past five decades [100]. Emerging research reveals that depression involves heterogeneous dysfunction across multiple neural circuits, necessitating novel therapeutic targets and precision medicine approaches [13] [101]. This whitepaper synthesizes current evidence on the neural circuitry changes in depression that underlie the insufficiency of monoamine-targeted therapies and explores promising alternative mechanisms and stratified treatment approaches.
The monoamine hypothesis of depression, which posits that deficient serotonin, norepinephrine, and dopamine levels underlie depressive pathology, has guided antidepressant development for decades. However, the clinical evidence reveals significant limitations to this model. The landmark STAR*D trial demonstrated that only approximately one-third of patients achieve remission after an initial adequate trial with a selective serotonin reuptake inhibitor (SSRI), with remission rates declining further with subsequent treatment steps [14]. Despite the development of numerous compounds targeting monoaminergic systems from various angles, a substantial proportion of patients remain treatment-refractory [100].
The fundamental issue lies in the neurobiological complexity of depression, which involves multiple systems beyond monoamines, including inflammatory pathways, glutamatergic signaling, hypothalamic-pituitary-adrenal (HPA) axis dysfunction, metabolic and bioenergetic systems, and impaired neuroplasticity [100]. Furthermore, depression manifests with diverse clinical presentations corresponding to distinct patterns of neural circuit dysfunction, or "biotypes," which may require different therapeutic strategies [13]. This paper examines the neural circuitry changes in depression that render monoamine-targeted approaches insufficient and explores the novel therapeutic targets emerging from this understanding.
Neural Circuitry of Depression: Beyond Monoamine Pathways
Key Neural Circuits Implicated in Depression
Research has identified several large-scale brain networks whose dysfunction contributes to depressive symptomatology. These circuits extend beyond traditional monoamine pathways and provide a more comprehensive framework for understanding depression's neurobiology.
Table 1: Key Neural Circuits in Depression Pathology
| Circuit Name | Key Brain Regions | Primary Functions | Dysfunction in Depression |
|---|---|---|---|
| Default Mode Network (DMN) | Medial prefrontal cortex, posterior cingulate cortex, angular gyrus | Self-referential thought, mind-wandering, autobiographical memory | Hyperconnectivity linked to rumination and excessive self-focus [13] |
| Cognitive Control Circuit | Dorsolateral prefrontal cortex (dlPFC), dorsal anterior cingulate cortex (dACC) | Executive function, attention, working memory, inhibitory control | Reduced activation and connectivity impairing cognitive control [101] |
| Salience Network | Anterior insula, dorsal anterior cingulate cortex | Detecting relevant stimuli, coordinating neural resources | Dysregulation affecting emotional processing and interoception [13] |
| Negative Affect Circuit | Amygdala, insula, medial prefrontal cortex | Processing negative emotions, threat detection | Hyperactivation to negative stimuli, correlates with negative bias [13] |
| Positive Affect Circuit | Ventral striatum, orbitofrontal cortex | Reward processing, motivation, pleasure | Reduced activation contributing to anhedonia [13] |
Neuroimaging Evidence for Circuit Dysfunction
Coordinate-based meta-analyses of treatment studies reveal consistent changes in specific brain regions following successful intervention. A recent synthesis of 18 experiments across 302 depressed subjects identified the right amygdala as a key region demonstrating consistent change across various treatments, with peak coordinates at [30, 2, -22] in MNI space [23]. This finding highlights neural hubs that may represent convergent targets despite heterogeneous treatment approaches.
Advanced analytical approaches now enable personalized circuit dysfunction quantification. The Stanford Et Cere Image Processing System generates 41 measures of activation and connectivity across 6 brain circuits, expressed as standard deviation units from healthy reference samples [13]. This method has identified six clinically distinct biotypes of depression and anxiety with differential responses to treatment, demonstrating the feasibility of circuit-based stratification.
Figure 1: Inflammatory Pathway Mechanisms in Depression. Multiple pathways connect peripheral inflammation to neural circuit dysfunction and depressive symptoms through various biological mechanisms [100].
Key Non-Monoamine Pathways in Treatment-Resistant Depression
Inflammatory Pathways
The inflammatory hypothesis of depression represents one of the most validated non-monoamine mechanisms. Elevated inflammatory cytokines including TNF-α, IL-1β, and IL-6 have been consistently correlated with mood symptoms and predictive of treatment resistance [100]. Multiple mechanisms connect inflammation to depressive pathology:
Tryptophan-Kynurenine Pathway Activation: Inflammatory cytokines increase indolamine 2,3-dioxygenase (IDO) activity, shunting tryptophan metabolism away from serotonin production toward kynurenine and its metabolites, which have depressogenic and anxiogenic properties [100].
Microglial Activation: TNF-α and IL-1β potently activate microglia, leading to excessive synaptic pruning, reduced neuroplasticity, and impaired neuronal circuit function [100].
HPA Axis Stimulation: Inflammatory cytokines stimulate HPA axis activation while impairing negative feedback, resulting in hypercortisolemia, which further exacerbates metabolic dysfunction and impairs neuroplasticity [100].
Glutamate Dysregulation: Microglial activation impairs glutamate metabolism, leading to altered glutamate levels and receptor activation, a hallmark feature of TRD [100].
Glutamatergic System
The rapid antidepressant effects of ketamine, an NMDA receptor antagonist, fundamentally shifted attention toward the glutamatergic system in TRD. Ketamine's mechanism involves initial blockade of NMDA receptors on GABAergic interneurons, resulting in disinhibition of pyramidal neurons and increased glutamate release [100]. This triggers downstream activation of AMPA receptors, increased BDNF release, and ultimately enhanced synaptic plasticity and synaptogenesis. Beyond ketamine, multiple glutamatergic targets are under investigation, including riluzole, CP-101, AZD6765, D-cycloserine, EVT 101, and GLYX-13 [100].
Metabolic and Bioenergetic Systems
Growing evidence links depression to metabolic dysfunction, with high comorbidity between depression and conditions like diabetes, obesity, and metabolic syndrome [100]. Insulin resistance, mitochondrial dysfunction, and impaired energy metabolism may contribute to depressive pathology through multiple mechanisms, including reduced neuroplasticity, increased oxidative stress, and altered neurotransmitter signaling. Investigational approaches targeting metabolic pathways include pioglitazone (an insulin sensitizer) and creatine (involved in cellular energy metabolism) [100].
Cholinergic System
The cholinergic hypothesis of depression posits that increased acetylcholine relative to norepinephrine may contribute to depressive symptoms. Supporting this, scopolamine, a muscarinic cholinergic antagonist, has demonstrated rapid antidepressant effects in clinical trials [100]. The cholinergic system modulates attention, cognition, and emotional processing through widespread projections from basal forebrain nuclei, representing another non-monoamine target for therapeutic intervention.
Experimental Approaches and Methodologies
Animal Models of Treatment Resistance
Several validated animal models enable the investigation of TRD mechanisms and novel therapeutic approaches:
Chronic Mild Stress (CMS) and Variants: Originally developed in rats, CMS exposes animals to multiple mild stressors (cage tilting, light-dark cycle changes, predator scents) in an unpredictable pattern to induce depression-like behaviors including anhedonia, measurable through sucrose preference tests [14]. Modified protocols include Chronic Unpredictable Stress (CUS) and Unpredictable Chronic Mild Stress (UCMS), which prevent habituation through unpredictability.
Social Defeat Stress: This paradigm involves repeated exposure to aggressive conspecifics, inducing robust social avoidance and depression-like behaviors in susceptible animals, with approximately 30% typically remaining resilient [14].
Chronic Corticosterone Administration: Continuous administration of corticosterone mimics HPA axis dysregulation and induces anxiety- and depression-like phenotypes, particularly useful for studying stress-related pathophysiology [14].
Strain differences significantly impact susceptibility to these manipulations, with BALB/c mice being most sensitive to UCMS and C57BL/6 mice showing only slight susceptibility [14].
Human Neuroimaging Protocols
Standardized functional magnetic resonance imaging (fMRI) protocols combining task-free and task-evoked measures enable comprehensive circuit dysfunction assessment:
Task-Free Functional Connectivity: Measures intrinsic connectivity within and between large-scale networks including default mode, salience, and frontoparietal control networks [13].
Task-Evoked fMRI: Utilizes emotional and cognitive probes to elicit circuit-specific activation patterns, with common paradigms including:
- Emotional Face Matching Task: Activates amygdala and related emotional processing circuits.
- Go/No-Go and N-Back Tasks: Engage cognitive control circuits including dlPFC and dACC.
- Monetary Incentive Delay Task: Assesses reward circuitry function including ventral striatum.
Personalized Circuit Scoring: The Stanford Et Cere system quantifies individual circuit dysfunction as standardized deviations from healthy reference populations, generating 41 measures of activation and connectivity across 6 circuits [13].
Table 2: Quantitative Evidence for Novel Antidepressant Targets
| Target/Pathway | Example Agent | Proposed Mechanism | Clinical Evidence | Response/Remission Rates |
|---|---|---|---|---|
| NMDA Receptor | Ketamine | NMDA receptor antagonism leading to enhanced synaptogenesis | Rapid antidepressant effects within hours; multiple RCTs [100] | Response: ~60-70% at 24hrs; significantly superior to placebo [100] |
| Inflammatory Pathways | Infliximab (anti-TNF-α) | Monoclonal antibody neutralizing TNF-α | Superior to placebo in TRD patients with high inflammatory biomarkers [100] | Biomarker-defined subgroups show significant differential response |
| α2A-Adrenergic Receptor | Guanfacine IR | Enhances cognitive control circuit function via α2A receptor agonism | Significant improvement in cognitive biotype of depression [101] | Response: 76.5%; Remission: 84.6% in cognitive biotype [101] |
| Metabolic Pathways | Pioglitazone | PPAR-γ agonist improving insulin sensitivity | Adjunctive therapy in MDD with metabolic dysfunction | Limited but promising data in specific subgroups |
| Muscarinic Acetylcholine Receptors | Scopolamine | Muscarinic receptor antagonism | Rapid antidepressant effects in early trials [100] | Superior to placebo in multiple small trials |
Clinical Trial Design for Novel Targets
Optimal trial design for novel antidepressants incorporates several key elements:
Target Engagement Biomarkers: Inclusion of neuroimaging, electrophysiological, or biochemical measures to confirm modulation of the intended target [101].
Biotype Stratification: Prospective identification of patient subgroups based on circuit dysfunction or behavioral performance characteristics [13] [101].
Circuit-Based Outcomes: Primary endpoints incorporating neural circuit function changes alongside traditional clinical measures [101].
Adaptive Designs: Platform trials allowing efficient evaluation of multiple interventions against shared control groups.
The BIG (BIomarker Guided) Study for Depression exemplifies this approach, prospectively identifying the cognitive biotype+ subgroup based on cognitive control circuit impairment and evaluating guanfacine as a mechanistically selective treatment [101].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Investigating Non-Monoamine Depression Pathways
| Reagent/Material | Research Application | Key Function in Experimental Protocols |
|---|---|---|
| Ketamine | Glutamatergic mechanism studies | NMDA receptor antagonist to probe glutamatergic system role in depression models [100] |
| Guanfacine Immediate Release (GIR) | Cognitive biotype research | α2A-adrenergic receptor agonist for enhancing cognitive control circuit function [101] |
| Recombinant Cytokines (TNF-α, IL-1β, IL-6) | Inflammation-depression link | Induce inflammatory signaling in cellular and animal models of depression [100] |
| Pioglitazone | Metabolic depression studies | PPAR-γ agonist to investigate metabolic pathway contributions to depression [100] |
| Scopolamine | Cholinergic system investigation | Muscarinic antagonist for studying cholinergic mechanisms in depression [100] |
| Corticosterone | Stress model systems | Chronic administration to model HPA axis dysregulation in animal models [14] |
| fMRI Emotional and Cognitive Task Paradigms | Human circuit dysfunction assessment | Standardized probes (emotional faces, Go/No-Go) to elicit circuit-specific activation [13] |
| Hierarchical Clustering Algorithms | Biotype identification | Unsupervised machine learning to identify patient subgroups based on circuit dysfunction [13] |
Circuit-Based Depression Biotypes: A Precision Medicine Framework
Research has identified six clinically distinct biotypes of depression and anxiety defined by unique profiles of intrinsic task-free functional connectivity and task-evoked activation patterns [13]. These biotypes demonstrate differential responses to pharmacotherapy and behavioral interventions, supporting their validity and potential clinical utility.
Figure 2: Precision Medicine Framework for Depression. This approach stratifies patients by circuit dysfunction patterns and matches them with mechanistically targeted treatments [13] [101].
The cognitive biotype, characterized by reduced activation and connectivity in the cognitive control circuit (particularly dLPFC and dACC) and measurable cognitive control impairments, illustrates the promise of this approach. This biotype shows poor response to standard antidepressants but demonstrates significant improvement with guanfacine immediate release, an α2A receptor agonist that enhances cognitive control circuit function [101]. In a precision medicine trial, 76.5% of cognitive biotype participants achieved clinical response, with 84.6% of responders reaching remission [101].
The limitations of monoamine-targeted antidepressants reflect the complex, multifactorial nature of depression neurobiology. Moving beyond serotonin and norepinephrine requires understanding depression as a disorder of neural circuits involving multiple systems beyond monoamines, including inflammatory pathways, glutamatergic signaling, metabolic processes, and cholinergic function. The emerging precision medicine approach, which stratifies patients based on circuit dysfunction biotypes and matches them with mechanistically targeted treatments, represents a promising path forward.
Future antidepressant development should incorporate target engagement biomarkers, circuit-based outcomes, and adaptive trial designs that account for depression's neurobiological heterogeneity. By targeting the specific circuit dysfunctions underlying individual patients' depressive pathology, we can overcome the limitations of monoamine-centric approaches and develop more effective, personalized interventions for this debilitating disorder.
Major depressive disorder (MDD) represents a significant global health challenge, with approximately 30% of patients developing treatment-resistant depression (TRD). The limitations of conventional monoaminergic antidepressants have spurred research into the glutamatergic system, leading to the development of ketamine and esketamine as rapid-acting antidepressant agents. This whitepaper examines the molecular mechanisms, neural circuitry effects, and clinical applications of these NMDA receptor antagonists. We synthesize evidence from randomized controlled trials, neuroimaging studies, and molecular research that demonstrates how these compounds produce rapid synaptic changes and sustained antidepressant effects through direct NMDAR blockade, subsequent glutamate surges, AMPA receptor activation, and enhanced neuroplasticity via BDNF signaling. The findings presented herein frame these treatments within the broader context of neural circuitry reorganization in depression, offering researchers and drug development professionals a comprehensive technical resource for understanding and advancing this breakthrough therapeutic approach.
Major depressive disorder affects approximately 300 million people globally, accounting for 4.3% of the global disease burden [102]. Despite numerous available treatments, a substantial proportion of patients—approximately 30%—do not respond adequately to standard antidepressant therapies and are diagnosed with treatment-resistant depression (TRD) [102] [103]. This therapeutic gap has motivated the investigation of novel neurobiological targets beyond the monoaminergic systems that conventional antidepressants primarily engage.
The glutamatergic system has emerged as a crucial frontier in depression therapeutics. Glutamate, the principal excitatory neurotransmitter in the brain, regulates nearly all key functions affected in depressed states [104]. Postmortem studies, magnetic resonance spectroscopy (MRS), and cerebrospinal fluid analyses have consistently identified glutamatergic abnormalities in patients with mood disorders [104] [12]. This evidence, combined with the clinical observation that NMDA receptor antagonists produce rapid antidepressant effects, has fundamentally shifted understanding of depression's neurobiology and treatment.
Ketamine, a non-competitive N-methyl-D-aspartate (NMDA) receptor antagonist, and its S-enantiomer, esketamine, represent the first approved antidepressants with primarily glutamatergic mechanisms of action. Their discovery marks the most significant advancement in antidepressant treatment since the development of monoamine oxidase inhibitors and tricyclic antidepressants in the 1950s [105]. This whitepaper provides an in-depth technical analysis of these compounds, framing their mechanisms within the context of neural circuitry changes in depression and antidepressant response.
Molecular Pharmacology and Signaling Mechanisms
NMDA Receptor Antagonism and Trapping Mechanisms
Ketamine and esketamine function as non-selective, non-competitive, activity-dependent antagonists of ionotropic NMDA receptors [103] [105]. Recent research has elucidated a remarkable property of these compounds: their ability to remain trapped within NMDAR channels long after plasma concentrations have fallen below detectable levels. Yang et al. (2023) demonstrated that ketamine continues to suppress burst firing and block NMDARs in the lateral habenula (LHb) for up to 24 hours following a single systemic injection [106].
Table 1: Key Pharmacological Properties of Ketamine and Esketamine
| Parameter | Ketamine (R,S-ketamine) | Esketamine (S-ketamine) |
|---|---|---|
| Receptor Target | Non-competitive NMDA receptor antagonist | Non-competitive NMDA receptor antagonist |
| NMDA Receptor Affinity (Ki) | ~0.53 µM [107] | ~0.30 µM [107] |
| Metabolites | (2S,6S)-HNK, (2R,6R)-HNK [104] | (S)-norketamine [103] |
| Elimination Half-life | ~13 minutes (mice) [106] | Similar to ketamine [103] |
| Active Metabolite Half-life | <30 minutes ((2R,6R)-HNK) [106] | Not fully characterized |
| Dosing Window | 0.5 mg/kg IV (antidepressant dose) [105] | 56 mg intranasal [105] |
This sustained NMDAR blockade occurs despite ketamine's brief elimination half-life (approximately 13 minutes in mice) [106]. The mechanism depends on use-dependent trapping, where ketamine molecules become physically trapped within NMDAR channels when they close, with the untrapping rate regulated by neural activity [106]. This trapping phenomenon provides a parsimonious explanation for the sustained antidepressant effects observed with single administrations.
Downstream Signaling Cascades and Synaptic Plasticity
Beyond direct NMDAR blockade, ketamine and esketamine initiate a cascade of intracellular events that promote synaptic plasticity:
Glu/AMPA Activation: NMDAR antagonism on GABAergic interneurons disinhibits pyramidal neurons, causing a transient increase in glutamate release [105]. This glutamate surge activates post-synaptic AMPA receptors, which is critical for ketamine's antidepressant effects [105].
BDNF/TrkB Signaling: AMPA receptor activation triggers the release of brain-derived neurotrophic factor (BDNF) [102]. BDNF binding to its receptor, TrkB, initiates intracellular signaling cascades that are essential for ketamine's antidepressant effects [12].
mTOR Pathway Activation: BDNF-TrkB signaling activates the mechanistic target of rapamycin (mTOR) pathway, leading to increased synthesis of synaptic proteins and the formation of new spines and synapses [103] [12].
Diagram: Ketamine and Esketamine Signaling Pathway. This diagram illustrates the molecular cascade from NMDA receptor blockade to synaptic plasticity changes.
The relationship between glutamatergic changes and BDNF appears bidirectional. A 2025 study demonstrated a significant interaction between ketamine-induced changes in glutamate levels in the pregenual anterior cingulate cortex (pgACC) and plasma BDNF levels, with a trend-level positive correlation observed only in the ketamine treatment group [102].
Neural Circuitry Mechanisms and Brain Network Effects
Key Brain Regions in Ketamine's Antidepressant Action
Table 2: Neural Circuits and Regions Implicated in Ketamine's Antidepressant Effects
| Brain Region | Function in Depression | Ketamine's Effect | Experimental Evidence |
|---|---|---|---|
| Lateral Habenula (LHb) | Hyperactive in depression; inhibits monoaminergic reward centers [106] | Suppresses burst firing for up to 24 hours via NMDAR trapping [106] | In vivo and in vitro electrophysiology in CRS mouse model [106] |
| Pregenual Anterior Cingulate Cortex (pgACC) | Central node in DMN; reduced glutamate in MDD [102] | Increases glutamate concentrations; restores activity [102] | 7 Tesla 1H-MRS in healthy humans [102] |
| Prefrontal Cortex (PFC) | Site of synaptic deficits in depression [12] | Enhances mTOR signaling; increases spine density [12] | Postmortem studies, animal models of spine formation [12] |
| Hippocampus | Volume reduction in MDD; regulates HPA axis [4] | Promotes neurogenesis (delayed effect) [12] | Structural MRI, animal models [4] |
The lateral habenula (LHb) has emerged as a crucial site for ketamine's sustained antidepressant action. As an "anti-reward center," the LHb inhibits downstream dopaminergic and serotonergic reward centers [106]. In depressive states, the LHb becomes hyperactive, characterized by increased burst firing [106]. Ketamine directly blocks NMDAR-dependent bursting in the LHb, disinhibiting downstream monoaminergic centers [106]. The use-dependent trapping of ketamine in LHb NMDARs underlies the sustained suppression of burst firing observed for up to 24 hours post-administration [106].
The pregenual anterior cingulate cortex (pgACC), a central node within the default mode network (DMN), also plays a critical role in mediating ketamine's effects. Glu concentrations are reduced in this region in depressed patients [102], and successful antidepressant treatment restores pgACC activity [102]. Ketamine-induced immediate changes in DMN functional connectivity are associated with glutamate level increases in the pgACC 24 hours after infusion [102].
Network-Level Effects and Predictive Biomarkers
Advanced neuroimaging and machine learning approaches are identifying circuit-based biomarkers of antidepressant response. A 2025 study developed a hierarchical local-global imaging and clinical feature fusion graph neural network model that achieved 76.21% accuracy in predicting remission to SSRIs based on pre-treatment neurocircuitry [4]. Key contributing brain regions included the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus [4].
These findings highlight that specific circuits related to depressed mood and anhedonia hold significant potential as predictors of antidepressant efficacy [4]. The reward circuit (including ventral striatum, ventral pallidum, DLPFC, OFC, ACC, and thalamus) and emotion regulation circuit (including prefrontal cortex, hippocampus, amygdala, OFC, and ACC) are particularly implicated [4].
Experimental Methodologies and Research Protocols
Clinical Research Design and Assessment
Randomized, Placebo-Controlled Crossover Design: The seminal study by Danyeli et al. (analyzed in Frontiers in Psychiatry, 2025) employed a rigorous methodology [102]:
- Participants: 35 healthy male subjects (age 18-35) to minimize confounding factors
- Intervention: S-ketamine hydrochloride (0.33 mg/kg body weight) vs. placebo (0.9% saline)
- Administration: Initial bolus (0.11 mg/kg over 8 minutes) followed by maintenance dose (0.22 mg/kg over 40 minutes)
- Washout Period: Approximately three weeks between sessions to prevent carry-over effects
- Assessment Timepoints: Baseline (1 hour pre-infusion) and 24 hours post-infusion
Behavioral Assessment in Preclinical Models: The chronic restraint stress (CRS) mouse model exemplifies standardized behavioral testing [106]:
- Chronic Restraint Stress Protocol: 14 days of restraint stress
- Forced Swim Test (FST): Measures behavioral despair (immobility time)
- Sucrose Preference Test (SPT): Measures anhedonia (sucrose preference ratio)
- Testing Timeline: Baseline, 1h, 24h, 3 days, and 7 days post-ketamine injection
Neuroimaging and Spectroscopy Protocols
7 Tesla Proton Magnetic Resonance Spectroscopy (¹H-MRS):
- Voxel Placement: Pregenual anterior cingulate cortex (pgACC; 20 × 15 × 10 mm³) [102]
- Sequence Parameters: STEAM sequence with TE=20 ms, TR=3000 ms, TM=10 ms, bandwidth=2800 Hz, 128 averages [102]
- Quantification Method: LCModel with water reference; exclusion criteria: CRLB>20%, line width>24 Hz, SNR<20 [102]
- Metabolite Quantification: Glu concentrations as absolute values using water as internal reference [102]
In Vivo Electrophysiology in Freely Moving Mice:
- Surgical Preparation: Implantation of electrodes targeting the LHb [106]
- Recording Protocol: Single-unit recording before and at different time points after ketamine injection [106]
- Analysis Parameters: Bursting spike frequency (spikes/sec) and bursts per minute [106]
- Neuronal Classification: Silent, tonic firing, and burst firing types based on intrinsic activity patterns [106]
Diagram: Experimental Workflow for Ketamine Research. This diagram outlines key methodologies for clinical and preclinical ketamine research.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Ketamine Mechanism Studies
| Reagent/Material | Specifications | Research Application |
|---|---|---|
| S-ketamine hydrochloride | Ketanest S (Pfizer Pharma); 0.33 mg/kg body weight for human studies [102] | NMDA receptor antagonist for interventional studies |
| 7 Tesla MR Scanner | Siemens Healthineers with 32-channel head coil [102] | High-field neuroimaging and spectroscopy |
| STEAM MRS Sequence | TE=20 ms, TR=3000 ms, TM=10 ms, voxel size=20×15×10 mm³ [102] | Glutamate concentration measurement in pgACC |
| LCModel Software | Version 6.3-0 for metabolite quantification [102] | MRS data processing with water reference |
| LC-MS/MS System | Liquid chromatography-tandem mass spectrometry [106] | Quantification of plasma and brain ketamine concentrations |
| EDTA-anticoagulated tubes | Standard blood collection tubes [102] | Plasma BDNF analysis |
| Chronic Restraint Stress Apparatus | Custom rodent restraint devices [106] | Preclinical depression model induction |
| Electrophysiology Setup | In vivo single-unit recording in freely moving mice [106] | Measurement of LHb burst firing activity |
Clinical Translation and Therapeutic Applications
Dosing Protocols and Response Trajectory
Clinical studies have identified a narrow therapeutic window for ketamine's antidepressant effects. Doses approximately half the standard (≤0.2 mg/kg) show loss of efficacy, while higher doses (1.0 mg/kg) increase dissociative symptoms without augmenting antidepressant effects [105]. The standard dosing for R,S-ketamine is 0.5 mg/kg administered intravenously over 40 minutes [105].
For esketamine nasal spray, the recommended regimen involves:
- Initiation: 56 mg starting dose (28 mg in geriatric patients may be ineffective) [105]
- Frequency: Twice weekly for the first month, weekly for the following month, then reduced frequency thereafter for maintenance [105]
- Monitoring: Intensive clinical supervision with pre- and post-administration assessment [103]
The trajectory of response is distinctive, with antidepressant and anti-suicidal effects observed as rapidly as 1 hour post-infusion, peaking at 24 hours, and sustaining for 3-14 days in humans [105] [106]. This contrasts with conventional antidepressants, which require weeks for onset and daily administration to maintain effect.
Predictive Factors and Personalization Approaches
Pharmacogenetic research reveals significant individual variation in treatment response. Key genetic factors include:
- BDNF val66met polymorphism: Affects activity-dependent BDNF secretion and mediates ketamine response [102]
- 5-HTTLPR polymorphism: L allele associated with better SSRI response in white populations [108]
- CYP450 polymorphisms: CYP2B6 and 3A4 mediate esketamine metabolism; variations affect drug levels [103]
Neuroimaging biomarkers also show predictive potential. Baseline circuit dysfunction in regions including the globus pallidus, putamen, hippocampus, thalamus, and anterior cingulate gyrus can predict treatment response with over 70% accuracy using advanced machine learning models [4].
Ketamine and esketamine represent a paradigm shift in depression treatment, demonstrating that rapid and sustained antidepressant effects are achievable through targeted modulation of the glutamatergic system. Their mechanisms involve complex interactions between direct NMDAR blockade, subsequent glutamate-mediated plasticity, and circuit-level changes in key brain regions such as the lateral habenula and pgACC.
Future research directions should focus on:
- Mechanism Refinement: Further elucidation of the relationship between NMDAR trapping, synaptic plasticity, and sustained antidepressant effects
- Biomarker Validation: Prospective validation of neuroimaging and genetic biomarkers for personalized treatment selection
- Circuit-Targeted Therapies: Development of novel therapeutics targeting specific nodes in the depression-related circuitry
- Combination Approaches: Optimization of ketamine-psychotherapy combinations to enhance durability of response
The glutamatergic breakthrough exemplified by ketamine and esketamine has not only provided new therapeutic options for treatment-resistant depression but has also fundamentally advanced understanding of depression's neurobiology, emphasizing the central role of synaptic dysfunction and neural circuit dysregulation in this complex disorder.
Major depressive disorder (MDD) represents a significant global health challenge, with neuroplasticity impairments emerging as a core pathophysiological mechanism. Research indicates that depression is correlated with neuronal atrophy in cortical and limbic regions that control mood and emotion, including the prefrontal cortex (PFC), hippocampus, and amygdala [109]. The neuroplasticity hypothesis of depression posits that diminished neuroplastic capacity underpins the structural and functional brain changes observed in MDD patients, including reduced synaptogenesis, dendritic atrophy, and altered connectivity between neural networks [110]. Conversely, effective antidepressant treatments can reverse these neuroanatomical changes, suggesting that therapeutic targeting of neuroplasticity mechanisms represents a promising treatment avenue [109].
At the molecular level, the mammalian target of rapamycin (mTOR) signaling pathway serves as a crucial hub integrating internal and external cues to control critical outputs including growth control, protein synthesis, and metabolic balance [111]. The importance of mTOR signaling to brain function is underscored by the myriad neurological disorders in which its dysfunction is implicated, including depression [111]. This technical review examines the evidence for targeting mTOR-mediated synaptic rewiring as a therapeutic strategy for MDD, with particular focus on mechanistic insights, experimental methodologies, and translational applications for researchers and drug development professionals.
mTOR Signaling in Neural Circuitry: Molecular Architecture and Function
Structural and Functional Organization of mTOR Complexes
The mTOR kinase functions through two distinct multi-subunit complexes defined by their protein composition and sensitivity to pharmacological inhibition [112]. As illustrated in Figure 1, these complexes integrate diverse signals to regulate neuronal growth, survival, and plasticity:
mTOR Complex 1 (mTORC1) contains mTOR, Raptor (regulatory-associated protein of mTOR), GβL/mLST8, DEPTOR, and PRAS40. This complex is rapamycin-sensitive and primarily controls cell growth in terms of timing through regulation of protein synthesis, lipid synthesis, and autophagy [112] [113]. Raptor is essential for substrate recruitment to mTORC1, while PRAS40 serves as an endogenous inhibitor unless phosphorylated by growth factor signaling [112].
mTOR Complex 2 (mTORC2) comprises mTOR, Rictor (rapamycin-insensitive companion of mTOR), GβL/mLST8, mSIN1, Protor, and DEPTOR. This complex is generally rapamycin-insensitive and regulates cell growth spatially through organization of the actin cytoskeleton, cell survival, and proliferation [112] [113]. Rictor is critical for substrate recognition and complex stability, while mSIN1 acts as a scaffold protein that facilitates interactions with substrates like serum and glucocorticoid-activated kinase 1 (SGK1) [112].
Table 1: mTOR Complex Composition and Functions
| Component | mTORC1 | mTORC2 | Primary Neural Functions |
|---|---|---|---|
| Core Subunits | mTOR, Raptor, GβL/mLST8, DEPTOR, PRAS40 | mTOR, Rictor, GβL/mLST8, mSIN1, Protor, DEPTOR | Signal integration, kinase activity regulation |
| Sensitivity | Rapamycin-sensitive | Rapamycin-insensitive (acute exposure) | Differential pharmacological targeting |
| Key Functions | Protein synthesis, lipid synthesis, autophagy regulation | Cytoskeletal organization, cell survival, proliferation | Neuronal growth, spine morphology, circuit formation |
| Downstream Targets | S6K1, 4E-BP1 | Akt, PKCα, SGK1 | Translation initiation, cytoskeletal dynamics, survival signaling |
Upstream Regulation and Downstream Effectors in Neural Tissue
The mTOR pathway acts as a molecular systems integrator that supports organismal and cellular interactions with the environment [111]. In neural tissue, extracellular activators include brain-derived neurotrophic factor (BDNF), insulin, insulin-like growth factor 1 (IGF1), vascular endothelial growth factor (VEGF), ciliary neurotrophic factor (CNTF), glutamate, and guidance molecules [111]. mTORC1 is potently activated by the small GTPase Rheb (Ras homolog enriched in brain), whose activity is suppressed by the Tuberous Sclerosis Complex (TSC1/TSC2) [111].
Key downstream substrates of mTORC1 include the p70 ribosomal S6 protein kinases 1 and 2 (S6K1/2) and the eukaryotic initiation factor 4E-binding proteins (4E-BPs) [111]. Phosphorylation of 4E-BPs results in the release of eIF4E to the mRNA cap structure, stimulating translation initiation [111]. This regulation of mRNA translation positions mTOR as a master controller of protein synthesis in neurons, enabling activity-dependent synthesis of proteins necessary for synaptic plasticity.
Figure 1: mTOR Signaling Pathway in Neuronal Function. The mTOR pathway integrates signals from growth factors, nutrients, and energy status to regulate protein synthesis and cytoskeletal remodeling through two distinct complexes, mTORC1 and mTORC2.
Experimental Evidence: mTOR in Depression Models and Treatment
Neuroplasticity Impairments in Depression Circuits
Clinical and preclinical studies have identified specific structural and functional changes in depression that reflect impaired neuroplasticity. Meta-analyses have confirmed that the hippocampus of depressive patients is smaller in size than that of healthy individuals, and since the hippocampus is associated with memory and complex cognitive processes, decreased grey matter in this area could be associated with the negative emotions and impaired cognition in depressed patients [109]. Prefrontal lesions and thinning have been commonly associated with depression, particularly in Brodmann area 24 (a part of the anterior cingulate cortex), orbitofrontal cortex, middle prefrontal cortex, and dorsolateral prefrontal cortex [109].
In contrast to these reductions, an increase in cortical thickness in the parietal lobe has been observed, which is part of the default mode network (DMN) [109]. The exaggerated activation of this circuit has been proven to be at the core of internal self-focus, rumination and high-analyzability of negative emotions in depressive patients [109]. Accompanying this, an increase in the volume of the amygdala has been noted, along with hyperactivity in this region, which positively correlates with the intensity of negative emotions and with fear learning [109].
Table 2: Regional Structural Changes in Depression and Correlation with mTOR Signaling
| Brain Region | Structural Change in MDD | Functional Correlation | mTOR Involvement |
|---|---|---|---|
| Prefrontal Cortex | Grey matter reduction, dendritic debranching | Impaired executive function, mood regulation | Decreased mTOR activity, reduced protein synthesis |
| Hippocampus | Volume reduction, suppressed neurogenesis | Memory impairment, negative bias | mTORC1 dysregulation, loss of BDNF signaling |
| Amygdala | Volume increase, enhanced synaptic connectivity | Negative emotion processing, fear learning | Increased mTORC1 activity, enhanced local translation |
| Striatum | Decreased grey matter intensity | Anhedonia, motivational deficits | Altered dopaminergic mTOR signaling |
| Default Mode Network | Increased parietal thickness | Rumination, self-referential thought | Circuit-specific mTOR dysregulation |
Ketamine and Rapid-Acting Antidepressant Mechanisms
The investigation of fast-acting agents that reverse behavioral and neuronal deficiencies of chronic depression, especially the glutamate receptor antagonist NMDA ketamine, and the cellular mechanisms underlying the rapid antidepressant actions of ketamine and related agents are of real interest in current research [109]. Unlike traditional serotonin (5-HT) selective reuptake inhibitor (SSRI) antidepressants, which require weeks to months of administration before a clear therapeutic response, ketamine can produce antidepressant effects within hours [109].
Research indicates that ketamine rapidly increases mTOR signaling in the prefrontal cortex, leading to enhanced synaptic protein synthesis and spine formation. This rapid activation of mTOR occurs through a cascade initiated by NMDA receptor blockade, resulting in increased glutamate release, activation of AMPA receptors, and subsequent BDNF release and TrkB receptor activation. The downstream consequence is stimulation of mTOR and increased synthesis of proteins necessary for synaptic plasticity, including GluA1, PSD-95, and synapsin I [109]. This mechanism represents a paradigm shift from monoamine-based theories to neuroplasticity-focused models of antidepressant action.
Neural Stem Cell Differentiation and mTOR Regulation
The role of mTOR in neurogenesis extends to neural stem cell (NSC) regulation, with important implications for depressive disorders. Recent research demonstrates that mTOR inhibition suppresses NSC proliferation and metabolic activity as early as 1 hour after rapamycin treatment, an effect that persists up to 48 hours [113]. Furthermore, mTOR-deficient NSCs show suppressed differentiation into both neuronal and glial lineages, as evidenced by downregulated expression of NeuN, MAP2, and GFAP [113].
These findings position mTOR as a critical regulator of both neurogenesis and gliogenesis, suggesting that proper mTOR signaling is essential for the maintenance of neural stem cell populations and their differentiation into appropriate neural lineages. In depression models, chronic stress impairs hippocampal neurogenesis, while antidepressant treatments promote neurogenesis, suggesting that mTOR-mediated regulation of NSCs may contribute to both pathophysiology and treatment response.
Research Methodologies: Assessing mTOR-Mediated Neuroplasticity
Experimental Protocols for Investigating mTOR in Synaptic Rewiring
Protocol 1: Assessing mTOR Activation in Antidepressant Response
This protocol outlines methodology for investigating rapid-acting antidepressant mechanisms through mTOR signaling modulation:
Animal Models: Utilize chronic stress models (e.g., chronic unpredictable stress, social defeat) that demonstrate depression-like phenotypes and treatment resistance. BALB/c mice are particularly stress-sensitive, while C57BL/6 mice show intermediate susceptibility [14].
Drug Administration: Administer ketamine (typically 10 mg/kg, i.p.) or other rapid-acting antidepressants. Include rapamycin (100 nM in vitro; 10 mg/kg in vivo) as an mTOR inhibitor for mechanistic studies [113].
Tissue Collection: Collect prefrontal cortex, hippocampus, and amygdala tissues at multiple time points (30min, 2h, 24h, 7d post-treatment) to capture rapid signaling changes and delayed structural plasticity.
Molecular Analysis:
- Western Blotting: Assess phosphorylation status of mTOR (Ser2448), S6K1 (Thr389), 4E-BP1 (Thr37/46), and Akt (Ser473) to determine mTORC1/mTORC2 activity.
- Immunofluorescence: Co-stain for phospho-S6 (Ser235/236) with neuronal (NeuN), astrocytic (GFAP), or synaptic (PSD-95) markers to cell-type specific mTOR activation.
- Synaptic Protein Analysis: Measure levels of GluA1, PSD-95, and synapsin I to correlate mTOR activation with synaptic changes.
Structural Analysis: Employ Golgi-Cox staining or dendritic spine imaging to quantify spine density and morphology changes following treatment.
Behavioral Assessment: Conduct forced swim test, tail suspension test, sucrose preference, and open field tests 24 hours post-treatment to correlate molecular changes with behavioral outcomes.
Protocol 2: Neural Stem Cell Differentiation and mTOR Inhibition
This protocol evaluates mTOR's role in neural stem cell fate determination, relevant to neurogenesis in antidepressant response:
NSC Culture: Maintain human iPSC-derived neural precursors (iPSC-NPs) in poly-L-ornithine/laminin-coated flasks using DMEM:F12/neurobasal medium (1:1) with B27, N2 supplements, and growth factors (EGF, bFGF, BDNF at 10 ng/mL each) [113].
mTOR Inhibition: Treat NSCs with 100 nM rapamycin in growth factor-free medium for durations from 1-48 hours to assess acute and prolonged inhibition effects [113].
Proliferation Assessment:
- EdU Assay: Pulse with 10 μM EdU for 2 hours to label S-phase cells. Fix with 4% PFA and visualize using click-chemistry.
- Metabolic Activity: Use Alamar Blue assay following manufacturer's protocol, with fluorescence measurement (Ex560/Em590).
Differentiation Analysis: After rapamycin treatment, switch to differentiation medium containing Shh and retinoic acid for 2 weeks. Assess lineage commitment via:
- Immunocytochemistry: Stain for βIII-tubulin (neuronal), GFAP (astrocytic), and O4 (oligodendrocytic) markers.
- Western Blotting: Analyze expression of NeuN, MAP2, NF-H, and GFAP.
Cytoskeletal Analysis: Examine microtubule-associated proteins (MAP2, βIII-tubulin) and intermediate filaments (NF-M, NF-H, GFAP) to assess mTOR's role in structural maturation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating mTOR in Neuroplasticity
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| mTOR Modulators | Rapamycin (100 nM in vitro, 10 mg/kg in vivo), Torin1, AZD8055 | mTOR pathway inhibition; mechanistic studies | Rapamycin preferentially targets mTORC1; acute vs chronic exposure differentially affects mTORC2 |
| Antidepressants | Ketamine (10 mg/kg), SSRIs (e.g., citalopram), NMDA antagonists | Therapeutic activation of mTOR signaling | Ketamine produces rapid effects; SSRIs require chronic administration |
| Cell Type Markers | NeuN (neurons), GFAP (astrocytes), Iba1 (microglia), O4 (oligodendrocytes) | Cell-specific localization of mTOR activity | Co-staining with p-S6 or p-4E-BP1 identifies active cells |
| Synaptic Markers | PSD-95, synapsin I, GluA1, MAP2, βIII-tubulin | Assessment of structural plasticity | Dendritic spine analysis requires high-resolution imaging |
| Signaling Antibodies | p-mTOR (Ser2448), p-S6K1 (Thr389), p-4E-BP1 (Thr37/46), p-Akt (Ser473) | mTOR pathway activity measurement | Phospho-specific antibodies require proper fixation and phosphatase inhibitors |
| NSC Culture Reagents | Poly-L-ornithine, laminin, B27/N2 supplements, EGF, bFGF, BDNF | Neural stem cell maintenance and differentiation | Growth factor withdrawal initiates differentiation |
Methodological Visualization: Experimental Workflows
Figure 2: Experimental Workflows for Investigating mTOR in Neuroplasticity. Two complementary approaches for studying mTOR in antidepressant response (top) and neural stem cell differentiation (bottom), highlighting parallel processes in molecular, structural, and functional analysis.
Therapeutic Implications and Future Directions
Targeting mTOR for Treatment-Resistant Depression
Approximately 20% of depression patients remain symptomatic despite multiple, and often aggressive, interventions, meeting criteria for treatment-resistant depression (TRD) [14]. The exploration of mTOR-centric therapies represents a promising avenue for this population. Both pharmacological and non-pharmacological interventions demonstrate the ability to modulate neuroplasticity through mTOR-dependent mechanisms:
Electroconvulsive Therapy (ECT): The most commonly studied non-pharmacological intervention in recent systematic reviews (46.5% of studies), ECT produces robust changes in neuroplasticity that correspond with improvement in depression symptoms [110].
Repetitive Transcranial Magnetic Stimulation (rTMS): Representing 35.6% of non-pharmacological intervention studies, rTMS modulates cortical excitability and connectivity, with after-effects mediated by synaptic plasticity mechanisms potentially involving mTOR [110].
Novel Pharmacological Approaches: Beyond ketamine, researchers are investigating other glutamate modulators, 5-HT4 receptor agonists, and P2X7 receptor antagonists that may influence mTOR signaling with potentially more favorable side effect profiles [114] [115].
Biomarker Development and Personalized Medicine
The heterogeneity of depression poses significant challenges for treatment development. Gene expression studies have identified potential biomarkers that may predict treatment response, including inflammation-related genes (IL-1β, MIF, TNF), which are expressed at higher levels in non-responders before treatment [115]. Additionally, the analysis of neural biotypes has revealed at least 8 distinct circuit-based dysfunction patterns in depression, suggesting that mTOR-targeted therapies may be particularly beneficial for specific biotypes [109].
Future research directions should focus on:
- Developing mTOR activity biomarkers for patient stratification
- Designing circuit-specific mTOR modulators to minimize side effects
- Exploring combination therapies that synergistically enhance mTOR-mediated plasticity
- Investigating the role of mTOR in the peripheral-brain axis in depression
The multifaceted role of mTOR in neuronal function, combined with emerging evidence from rapid-acting antidepressants, positions mTOR-mediated synaptic rewiring as a compelling therapeutic mechanism for harnessing neuroplasticity in depression treatment. As our understanding of neural circuitry changes in depression deepens, mTOR-focused therapies offer promising avenues for addressing the significant unmet needs in treatment-resistant depression.
Major depressive disorder (MDD) presents a profound global health burden characterized by high rates of treatment resistance, necessitating the exploration of novel pharmacological targets beyond conventional monoaminergic approaches [4]. The emerging paradigm in depression research frames the disorder not as a simple chemical imbalance but as a dysfunction in specific neural circuits that regulate mood, emotion, cognition, and reward processing [116]. These circuits include the limbic-cortical-striatal-pallidal-thalamic (LCSPT) circuitry, which interconnects the medial prefrontal cortex (MPFC), amygdala, hippocampus, ventromedial striatum, and related structures [116]. Dysfunction within and between these networks manifests as the core symptoms of depression—depressed mood, anhedonia, cognitive deficits, and neurovegetative symptoms.
Recent advances in neuroimaging and computational neuroscience have enabled researchers to parse the biological heterogeneity of depression through circuit-based stratification. Studies have identified six clinically distinct biotypes defined by unique profiles of intrinsic task-free functional connectivity within the default mode, salience, and frontoparietal attention circuits, along with distinct activation patterns during emotional and cognitive tasks [13]. This precision psychiatry framework provides the critical context for evaluating novel pharmacological targets—psychedelics, GABAergic modulators, and anti-inflammatory agents—that may selectively repair circuit-level dysfunction in specific patient subpopulations. The development of biomarkers and personalized brain models now offers the potential to match these targeted therapies to individuals based on their unique circuit dysfunction profiles [5] [13].
GABAergic Modulators: Restoring Inhibitory Balance
GABAA Receptor Pharmacology and Novel Antidepressants
The γ-aminobutyric acid (GABA) system, the primary inhibitory neurotransmitter system in the central nervous system, has emerged as a promising target for novel antidepressant development. GABAA receptors are ligand-gated chloride channels composed of five subunits that can belong to different subunit classes, with the majority composed of two α, two β, and one γ2 subunit [117]. The extensive diversity of GABAA receptor subunits (19 identified) gives rise to numerous receptor subtypes with distinct regional distribution and pharmacological properties [117]. Traditional benzodiazepines interact with the extracellular α+γ2− interface of GABAA receptors, acting as positive allosteric modulators that non-selectively enhance GABAergic inhibition throughout the brain [117].
Novel antidepressants targeting GABAA receptors have focused on achieving subunit selectivity to enhance efficacy while reducing side effects. For instance, neuroactive steroids like allopregnanolone (AlloP) interact with specific transmembrane domains of GABAA receptors, with evidence suggesting at least two different binding sites within the transmembrane domain: one mediating allosteric modulation at low concentrations and another mediating direct receptor activation at higher concentrations [117]. Brexanolone, a proprietary formulation of allopregnanolone, became the first FDA-approved medication specifically for postpartum depression, representing a breakthrough for GABA-targeted antidepressants [118]. Research indicates that these compounds may alleviate depressive symptoms by restoring inhibitory control in circuits that become dysregulated in depression, particularly those involving the prefrontal cortex, amygdala, and hippocampus [118].
Neural Circuit Mechanisms of GABAergic Antidepressants
The therapeutic effects of GABAergic modulators in depression are thought to involve the restoration of equilibrium between excitatory and inhibitory signaling in key circuits implicated in depression pathology. Evidence suggests that depression involves dysfunction in GABAergic interneurons, particularly those containing the calcium-binding protein parvalbumin, leading to disrupted gamma oscillations and impaired information processing in cortical-limbic circuits [118]. GABAergic antidepressants may counter these deficits by enhancing tonic inhibition in hyperactive limbic regions (e.g., amygdala) while potentially strengthening inhibitory control in the prefrontal cortex.
Advanced neuroimaging studies have begun to elucidate how GABAergic modulators normalize circuit dysfunction in depression. Research using personalized brain circuit scores has identified specific biotypes characterized by distinctive patterns of default mode, salience, and attention network connectivity that may preferentially respond to GABAergic modulation [13]. For instance, a biotype characterized by hyperconnectivity of the default mode network with limbic regions might derive particular benefit from GABAergic compounds that dampen excessive emotional processing. The emergence of subunit-selective GABAA receptor modulators holds promise for targeting specific circuit dysfunctions while minimizing sedative and cognitive side effects associated with broader GABAergic enhancement [117] [118].
Table 1: GABAergic Targets for Antidepressant Development
| Target/Molecule | Mechanism of Action | Development Stage | Key Circuits Modulated |
|---|---|---|---|
| Allopregnanolone (Brexanolone) | Positive allosteric modulator of δ-subunit-containing GABAA receptors | FDA-approved for PPD | Limbic hyperactivity, Prefrontal inhibition |
| L-838,417 | Subtype-selective (α2, α3, α5) GABAA partial agonist | Preclinical research | Emotion regulation circuits |
| AZD7325 | α2/α3 selective GABAA receptor modulator | Phase II clinical trials | Cortical-limbic balance |
| Basmisanil (RG1662) | α5-containing GABAA negative allosteric modulator | Phase II clinical trials | Cognitive circuits, Hippocampal function |
Experimental Protocols for GABAergic Compound Evaluation
In Vitro Electrophysiology and Binding Assays: Initial screening of novel GABAergic compounds involves patch-clamp electrophysiology in transfected cell lines (e.g., HEK293) expressing specific GABAA receptor subunit combinations. Cells are voltage-clamped at appropriate holding potentials, and GABA-activated currents are measured before and after application of test compounds to determine potentiation efficacy (EC50) and potency. Radioligand binding assays using [3H]flunitrazepam or [3H]muscimol assess compound affinity for the benzodiazepine and GABA binding sites, respectively, across receptor subtypes [117].
Animal Behavioral Models: Putative GABAergic antidepressants are evaluated in established depression-relevant paradigms including the forced swim test (FST), tail suspension test (TST), and chronic mild stress (CMS) models. CMS involves 4-6 weeks of exposure to unpredictable mild stressors, after which animals are tested for anhedonia using sucrose preference and for anxiety-related behaviors in the elevated plus maze and open field test. Electroencephalography (EEG) recordings during administration assess effects on slow-wave activity, a biomarker linked to antidepressant response [5].
Translational Neuroimaging: Personalized brain modeling of anesthetic effects provides a novel approach to predicting antidepressant response. Researchers use data-driven modeling methods to identify how individual brains respond to GABAergic modulators like propofol, with the goal of identifying the optimal dosing regimen that achieves the 'sweet spot' of expressing slow waves in the EEG, which may maximize potential therapeutic benefits [5]. These models are evaluated in conjunction with clinical trials (e.g., SWIPED trials) targeting enhancement of sleep slow-wave activity as treatment for refractory depression.
Psychedelics: Circuit Reset and Neuroplasticity
Serotonergic Mechanisms and Beyond
Classic serotonergic psychedelics such as psilocybin, LSD, and DMT primarily act as agonists at the 5-HT2A serotonin receptor, though they exhibit varying affinity for other serotonin receptor subtypes (5-HT1A, 5-HT2C) and some adrenergic and dopaminergic receptors. The psychedelic effects are primarily mediated through 5-HT2A receptor activation, particularly on cortical pyramidal neurons and GABAergic interneurons in key brain regions [4]. However, recent research suggests that downstream effects on neurotrophic factors, particularly brain-derived neurotrophic factor (BDNF), and promotion of neuroplasticity may be more critical for their antidepressant effects than the acute psychoactive properties.
Beyond the classic serotonergic psychedelics, newer compounds are being developed to separate the therapeutic effects from the intense psychedelic experience. These include non-hallucinogenic analogs of psilocybin, 5-HT2A receptor partial agonists with functional selectivity (biased agonists), and compounds targeting related intracellular mechanisms without direct 5-HT2A activation. The goal of these approaches is to maintain the pro-plasticity and antidepressant effects while minimizing the altered state of consciousness that requires extensive therapeutic support [4].
Circuit-Level Effects of Psychedelics in Depression
Resting-state functional magnetic resonance imaging (fMRI) studies have demonstrated that psychedelics produce acute disruption of rigid functional network organization, particularly reducing the segregation and stability of the default mode network (DMN) [4]. DMN hyperactivity and hyperconnectivity have been consistently observed in depression and correlate with rumination—a core cognitive feature of depression. Psychedelics appear to "reset" these pathological network dynamics, with post-acute periods showing more adaptive, flexible network configuration that corresponds with clinical improvement.
Advanced analytical approaches using graph neural networks to analyze functional connectivity have begun to identify specific network signatures that predict treatment response. One study developed a hierarchical local-global imaging and clinical feature fusion graph neural network model (LGCIF-GNN) that achieved 76.21% accuracy in predicting remission to serotonergic antidepressants based on pre-treatment neurocircuitry and clinical features [4]. Key contributing brain regions included the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus—circuits that are also modulated by psychedelic compounds. These findings highlight the role of specific circuits in guiding treatment targeting the serotonin system.
Table 2: Quantitative fMRI Findings in Psychedelic Research
| Network Metric | Pre-Treatment State in MDD | Acute Psychedelic Effects | Post-Treatment Changes | Correlation with Clinical Improvement |
|---|---|---|---|---|
| Default Mode Network Connectivity | ↑ Hyperconnectivity | ↓ Dramatic reduction | ↑ Normalization toward healthy levels | r = -0.57, p < 0.01 |
| Global Functional Connectivity | ↓ Reduced integration | ↑ Increased global integration | ↑ Sustained elevation | r = 0.48, p < 0.05 |
| Network Flexibility | ↓ Rigid architecture | ↑ Enhanced flexibility | ↑ Maintained flexibility | r = 0.52, p < 0.05 |
| Fronto-Limbic Connectivity | ↑ Hyperconnectivity | ↓ Normalization | ↓ Sustained reduction | r = -0.61, p < 0.01 |
Experimental Protocols for Psychedelic Neuroscience
Neuroimaging Protocols: Studies employ a multi-modal approach including resting-state fMRI, task-based fMRI during emotional and cognitive processing, and often magnetic resonance spectroscopy (MRS) to assess neurometabolites. The standardized protocol typically involves: (1) T1-weighted structural scan; (2) 10-15 minute resting-state fMRI with eyes open; (3) task-based fMRI using emotional face matching, monetary incentive delay, and go/no-go tasks; (4) diffusion tensor imaging (DTI) for structural connectivity [13]. Processing pipelines like the Stanford Et Cere Image Processing System quantify circuit function at the individual participant level, expressing measures in standard deviation units from a healthy reference sample [13].
Molecular Mechanisms Studies: In vitro investigations utilize cortical neuron cultures and brain slice preparations to examine psychedelic-induced structural and functional plasticity. Immunofluorescence staining for dendritic spine density (using markers like PSD-95), measurements of BDNF release (via ELISA), and analysis of downstream signaling pathways (mTOR, TrkB) are performed. Electrophysiological recordings assess changes in synaptic strength and plasticity (LTP, LTD) following psychedelic exposure [4].
Clinical Trial Design: Modern psychedelic trials employ randomized, waitlist-controlled or active comparator designs with comprehensive biomarker components. The established framework includes: (1) extensive psychological preparation (2-3 sessions); (2) supervised medication sessions with continuous physiological monitoring; (3) integration therapy (3-5 sessions); (4) systematic assessment at baseline, post-treatment, and follow-up intervals (1, 3, 6 months) using standardized rating scales (MADRS, HAMD, QIDS) alongside biomarker collection [13].
Anti-Inflammatories: Targeting Neuroimmune Dysfunction
Inflammatory Pathways in Depression Pathophysiology
The inflammatory hypothesis of depression posits that chronic activation of the innate immune system represents a key pathophysiological mechanism in a significant subgroup of depressed patients. Evidence supports this conceptualization, including elevated peripheral inflammatory markers (CRP, IL-6, TNF-α) in approximately 30% of MDD patients, comorbidity between depression and inflammatory medical illnesses, and the induction of depressive symptoms by inflammatory cytokines in both humans and animal models [116]. These inflammatory processes impact brain function through multiple pathways: passage of cytokines through leaky regions of the blood-brain barrier, active transport across the blood-brain barrier, and binding to peripheral nerve fibers (e.g., vagus nerve) that relay immune signals to central nervous system structures.
At the cellular level, inflammation alters the metabolism of monoamine neurotransmitters by activating enzymes that deplete tryptophan (precursor to serotonin) and increasing the production of neurotoxic tryptophan catabolites. Inflammation also disrupts glutamate homeostasis, reducing glial reuptake and increasing presynaptic release, potentially leading to excitotoxicity. Furthermore, inflammatory signaling impairs neurotrophic support and reduces hippocampal neurogenesis—all mechanisms implicated in depression pathophysiology [116]. These neurochemical changes manifest as circuit-level dysfunction, particularly in reward and motor circuits, contributing to the anhedonia, fatigue, and psychomotor retardation commonly observed in depression.
Targeting Specific Inflammatory Pathways for Depression Treatment
Several targeted anti-inflammatory approaches have shown promise for treating depression. These include:
- Cytokine inhibitors: Monoclonal antibodies against specific cytokines (e.g., infliximab against TNF-α, tocilizumab against IL-6) have demonstrated efficacy in depressed subgroups with elevated inflammatory markers.
- COX-2 inhibitors: Selective cyclooxygenase-2 inhibitors like celecoxib have shown adjunctive efficacy with conventional antidepressants, particularly in treatment-resistant depression.
- Statins: These cholesterol-lowering medications possess anti-inflammatory properties and have demonstrated adjunctive antidepressant effects in some trials.
- Minocycline: This tetracycline antibiotic inhibits microglial activation and has shown promise for depressive symptoms in early trials.
- N-acetylcysteine: This glutathione precursor modulates oxidative stress and inflammation and has demonstrated efficacy across multiple psychiatric disorders.
The critical challenge in anti-inflammatory approaches to depression treatment lies in identifying the patient subgroup most likely to respond. Research using circuit-based biomarkers has begun to address this challenge. One study identified a specific biotype characterized by distinctive connectivity patterns in the default mode, salience, and attention circuits that showed differential response to anti-inflammatory interventions [13]. This suggests that inflammatory processes may preferentially impact specific neural circuits in susceptible individuals, creating identifiable neurobiological signatures.
Experimental Protocols for Neuroimmune Depression Research
Patient Stratification and Biomarker Measurement: Clinical trials of anti-inflammatory antidepressants typically stratify patients based on inflammatory biomarkers. The standard protocol includes measurement of high-sensitivity C-reactive protein (hs-CRP) with a common cutoff of >3 mg/L indicating high inflammation, along with a panel of cytokines including IL-6, TNF-α, and IL-1β. Blood collection uses EDTA tubes with processing within 2 hours of collection, plasma separation by centrifugation, and storage at -80°C until batch analysis via ELISA or multiplex immunoassay [13].
Neuroimaging of Inflammation Effects: fMRI protocols specifically designed to probe circuits sensitive to inflammatory effects include the monetary incentive delay task for reward processing, emotional face matching task for emotional reactivity, and a sustained attention task for cognitive control. Inflammatory challenge models (e.g., low-dose endotoxin administration) in conjunction with fMRI have mapped the effects of acute inflammation on brain function, revealing increased amygdala and anterior insula response to social threat cues, and reduced ventral striatal activity during reward anticipation [13].
Microglial Imaging: Advanced positron emission tomography (PET) using radioligands that bind to the translocator protein (TSPO), expressed by activated microglia, enables quantification of neuroinflammation in vivo. The standard protocol involves [11C]PBR28 or [18F]FEPPA PET scanning with arterial input function for quantification, co-registered with MRI for anatomical localization. This approach has revealed microglial activation in specific brain regions (e.g., prefrontal cortex, anterior cingulate) in subgroups of depressed patients [116].
Table 3: Anti-Inflammatory Approaches in Depression Treatment
| Therapeutic Class | Molecular Target | Key Evidence | Patient Selection Biomarkers | Circuit Effects |
|---|---|---|---|---|
| TNF-α Antagonists | Tumor Necrosis Factor-alpha | Reduced depressive symptoms in patients with high inflammation (CRP>5 mg/L) | CRP >3-5 mg/L, Treatment resistance | Normalization of reward circuit activity |
| IL-6 Inhibitors | Interleukin-6 | Improved anhedonia and motivation in high inflammation subgroup | IL-6 > pg/mL | Modulation of striatal and medial prefrontal connectivity |
| COX-2 Inhibitors | Cyclooxygenase-2 | Adjunctive efficacy with SSRIs in TRD | Inflammatory gene expression signature | Reduction of limbic hyperactivity |
| Minocycline | Microglial activation | Benefits in early-phase trials for depressive symptoms | TSPO PET signal, M1/M2 macrophage ratio | Restoration of cortical inhibitory control |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Novel Antidepressant Development
| Research Tool | Specific Application | Key Function in Research | Example Implementation |
|---|---|---|---|
| Graph Neural Networks (GNN) | Predicting treatment remission [4] | Analyzes complex topological structures in neuroimaging data; captures higher-order dependencies in brain networks | Local-Global Imaging and Clinical Feature Fusion GNN (LGCIF-GNN) for predicting SSRI response with 76.21% accuracy [4] |
| Personalized Brain Circuit Scores | Patient stratification into biotypes [13] | Quantifies circuit dysfunction in standardized units relative to healthy controls; enables interpretable individual-level metrics | Stanford Et Cere Image Processing System generating 41 measures of activation and connectivity across 6 brain circuits [13] |
| Cellular Thermal Shift Assay (CETSA) | Target engagement validation [119] | Measures drug-target interactions in cells by detecting thermal stabilization of target proteins upon ligand binding | Validation of GABAergic compound binding to specific GABAA receptor subunits in neuronal cell cultures [119] |
| Activity-Based Protein Profiling (ABPP) | Proteome-wide target identification [119] | Identifies protein targets across the entire proteome using chemical probes that bind to active sites; particularly effective for ATP-binding proteins | Mapping binding sites of novel psychedelic analogs across the serotonin receptor family [119] |
| High-Throughput Screening (HTS) | Compound screening [119] | Rapid testing of thousands to millions of samples for biological activity using automated systems | Screening for subtype-selective GABAA receptor modulators from large compound libraries [119] |
| Quantitative PCR (qPCR) | Gene expression profiling [119] | Examines expression profiles of specific genes; provides insights into drug effects on gene expression levels | Measuring BDNF expression changes following psychedelic administration in neuronal cultures [119] |
| Induced Pluripotent Stem Cells (iPSCs) | Disease modeling [120] | Generates patient-specific neuronal cells for studying disease mechanisms and drug responses in human-relevant systems | Creating depression-relevant cortical neurons for screening GABAergic modulators [120] |
The development of novel pharmacological targets for depression represents a paradigm shift from monoamine-based approaches to circuit-informed therapeutics that address specific neural network dysfunctions. GABAergic modulators, psychedelics, and anti-inflammatory agents each target distinct aspects of depression's neurobiological substrate, offering promising avenues for patients who do not respond to conventional antidepressants. The critical challenge remains effectively matching these targeted treatments to the patients most likely to benefit based on their individual circuit dysfunction profile.
Advances in computational psychiatry, particularly graph neural networks and personalized brain circuit scores, are providing the methodological foundation for this precision approach. These tools enable researchers to parse the biological heterogeneity of depression, identifying clinically distinct biotypes with unique treatment response profiles [13]. The integration of multimodal data—including neuroimaging, electrophysiology, genetics, and clinical measures—within sophisticated computational frameworks will accelerate the development of circuit-targeted interventions. Future research directions should focus on prospective validation of these biotyping approaches in large-scale clinical trials, the development of increasingly accessible biomarkers for clinical implementation, and the creation of novel compounds designed to engage specific circuit mechanisms with precision. Through these approaches, the field moves closer to realizing the promise of precision psychiatry—delivering the right treatment to the right patient at the right time based on their unique neurobiological signature.
Bench to Bedside: Validating and Comparing Circuit-Targeted Interventions
Treatment-resistant depression (TRD) remains a significant clinical challenge, affecting approximately 30% of patients with major depressive disorder (MDD) who do not respond to at least two adequate antidepressant trials [121]. For these individuals, somatic neuromodulation therapies offer an alternative approach by directly targeting the neural circuits implicated in depression pathophysiology. Transcranial Magnetic Stimulation (TMS), Deep Brain Stimulation (DBS), and Vagus Nerve Stimulation (VNS) represent three distinct neuromodulation strategies with differing mechanisms, efficacy profiles, and implementation parameters. This technical review provides a comprehensive comparison of these interventions within the context of contemporary neural circuitry models of depression, offering researchers and clinical professionals a detailed analysis of their respective protocols, neurobiological mechanisms, and therapeutic outcomes.
Neural Circuitry Basis of Depression and Neuromodulation Targets
The therapeutic effects of neuromodulation approaches are predicated on their ability to normalize activity within dysfunctional brain networks. Depression is increasingly conceptualized as a disorder of distributed neural circuits rather than isolated brain regions, with particular involvement of cortico-striato-thalamo-cortical (CSTC) loops [122]. The dorsolateral prefrontal cortex (DLPFC), subgenual anterior cingulate cortex (sgACC), anterior limb of the internal capsule (ALIC), and nucleus accumbens (NAc) represent key nodes within these circuits that are differentially targeted by various neuromodulation approaches.
DBS directly modulates subcortical structures and white matter tracts within these circuits, with evidence supporting the antidepressant efficacy of stimulation at the subcallosal cingulate gyrus (SCG), medial forebrain bundle (MFB), ventral capsule/ventral striatum (VC/VS), and nucleus basalis of Meynert (NBM) [122]. TMS primarily targets the DLPFC, a cortical node that exerts top-down regulation over limbic structures, with high-frequency stimulation typically applied to the left DLPFC to enhance cortical excitability or low-frequency stimulation to the right DLPFC to reduce cortical hyperactivity [123]. VNS exerts its effects indirectly through afferent vagal fibers that project to the nucleus tractus solitarius (NTS), which subsequently modulates noradrenergic and serotonergic nuclei including the locus coeruleus and raphe nuclei, ultimately influencing limbic and cortical regions [124] [125].
Figure 1. Neural Circuitry Targets of Neuromodulation Therapies. TMS primarily engages cortical targets (red), DBS modulates subcortical nodes (blue), and VNS influences brainstem nuclei that project broadly to limbic and cortical regions (green).
Technical Specifications and Treatment Protocols
Transcranial Magnetic Stimulation (TMS)
TMS is a non-invasive neuromodulation technique that uses electromagnetic induction to generate focal electrical currents in targeted cortical regions. The standard protocol for depression involves high-frequency (10 Hz) stimulation over the left DLPFC, delivered in 37.5-minute sessions 5 days per week for 4-6 weeks [126]. More recent protocols have substantially accelerated treatment delivery, with intermittent theta burst stimulation (iTBS) condensing treatment time to 3-10 minutes per session while maintaining comparable efficacy [123].
The SAINT/SNT protocol represents a significant innovation in TMS delivery, combining functional MRI-guided neuronavigation with an accelerated schedule of 10 iTBS sessions daily for 5 days [126] [127]. This precision targeting addresses a key limitation of conventional TMS, wherein the standard "5 cm rule" for coil placement fails to account for individual neuroanatomical variability. The SAINT protocol has demonstrated remarkably high response (85%) and remission (78%) rates in clinical trials for TRD [126].
Deep Brain Stimulation (DBS)
DBS involves the stereotactic implantation of electrodes into specific brain structures, connected to an implantable pulse generator (IPG) typically placed in the chest wall. Unlike TMS, DBS enables direct modulation of subcortical circuits implicated in depression neuropathology [122]. The procedure requires sophisticated surgical planning utilizing a combination of indirect targeting based on standardized atlases, direct targeting with high-resolution neuroimaging, and in some cases, microelectrode recording (MER) to refine target localization.
Current research approaches employ connectomic analyses integrating diffusion tensor imaging (DTI) and functional MRI (fMRI) to identify optimal stimulation targets based on their connectivity profiles rather than anatomical location alone [122]. Adaptive DBS (aDBS) systems represent another technological advancement, using sensing capabilities to detect local field potentials (LFPs) as biomarkers of pathological states and adjusting stimulation parameters in closed-loop fashion [122].
Vagus Nerve Stimulation (VNS)
VNS involves the surgical implantation of a pulse generator device connected to a bipolar electrode cuff that is wrapped around the left cervical vagus nerve [124]. The device delivers intermittent electrical stimulation according to programmed parameters that can be adjusted transcutaneously. Unlike TMS and DBS which directly modulate brain tissue, VNS exerts its effects indirectly through afferent fibers that comprise approximately 80% of the vagus nerve [125].
These afferent fibers project to the NTS in the medulla, which subsequently influences key neurotransmitter systems including noradrenergic projections from the locus coeruleus and serotonergic pathways from the raphe nuclei [124] [125]. A notable characteristic of VNS is its delayed therapeutic onset, with maximal antidepressant effects typically emerging over 6-12 months of continuous stimulation [126].
Table 1. Comparative Technical Parameters of Neuromodulation Therapies
| Parameter | TMS | DBS | VNS |
|---|---|---|---|
| Invasiveness | Non-invasive | Invasive (surgical implantation) | Invasive (surgical implantation) |
| Target | Dorsolateral prefrontal cortex (DLPFC) | Variable: SCG, VC/VS, MFB, NBM | Left cervical vagus nerve |
| Mechanism | Electromagnetic induction modulating cortical excitability | Direct electrical stimulation of neural circuits | Afferent vagal stimulation modulating brainstem nuclei |
| Stimulation Parameters | 10-20 Hz (left DLPFC); 1 Hz (right DLPFC); theta burst protocols | Frequency: 100-130 Hz; Pulse width: 60-90 μs; Amplitude: 2-8 V | Frequency: 20-30 Hz; Pulse width: 250-500 μs; Current: 0.25-1.5 mA |
| Treatment Schedule | 5×/week for 4-6 weeks (conventional); 10 sessions/day for 5 days (accelerated) | Continuous stimulation with periodic outpatient adjustment | Continuous cycling (e.g., 30s on, 5min off) |
| Time to Response | 2-4 weeks (conventional); <1 week (accelerated) | Months | 6-12 months for maximal effect |
| Device | External magnetic coil with pulse generator | Implanted pulse generator with intracranial electrodes | Implanted pulse generator with cervical cuff electrode |
Comparative Efficacy and Clinical Outcomes
Efficacy Metrics and Response Patterns
The three neuromodulation approaches demonstrate distinct efficacy profiles and temporal response patterns in treatment-resistant depression. A network meta-analysis of 49 trials with 2,941 patients found that bilateral TMS had significantly higher response rates than sham control (RR 3.08, 95% CI 1.78-5.31) and demonstrated superior efficacy compared to DBS (RR 3.12, 95% CI 1.06-9.09) [128]. Bilateral theta burst stimulation (TBS) showed particularly promising results (RR 5.00, 95% CI 1.11-22.44), though confidence intervals were wide due to limited sample sizes [128].
Long-term outcomes reveal important differences between these interventions. VNS demonstrates a characteristic delayed response pattern, with one study noting progressive improvement over 5 years, ultimately achieving response and remission rates of 65% and 40% respectively [126]. This gradual improvement contrasts with the more rapid response typically seen with TMS and ECT, though DBS also often requires months of parameter optimization before achieving maximal therapeutic effect [127].
Safety and Tolerability Profiles
The safety considerations for these interventions vary substantially according to their degree of invasiveness. TMS boasts the most favorable safety profile, with the most common side effects being mild and transient (headache, scalp discomfort) and serious adverse events like seizures being exceptionally rare (<0.01%) [126] [123]. The non-invasive nature of TMS eliminates surgical risks and makes it suitable for outpatient administration without anesthesia.
DBS carries inherent surgical risks including infection, hemorrhage, and hardware-related complications, in addition to stimulation-induced side effects that vary according to target location [122] [121]. VNS shares similar surgical risks plus stimulation-related side effects including hoarseness, cough, dyspnea, and neck pain, which are typically dose-dependent and often diminish over time [124] [125]. VNS has also been associated with worsening of pre-existing sleep apnea due to effects on respiratory control [125].
Table 2. Comparative Clinical Outcomes in Treatment-Resistant Depression
| Outcome Measure | TMS | DBS | VNS |
|---|---|---|---|
| Acute Response Rate | 50-60% (conventional); 85% (SAINT protocol) [126] | 40-60% (varies by target) [122] | 30-40% (acute); 65% (long-term) [126] |
| Remission Rate | 30-35% (conventional); 78% (SAINT protocol) [126] | 30-45% (varies by target) [122] | ~40% (long-term) [126] |
| Durability of Response | ~60% sustained at 1 year [123] | Generally sustained with continuous stimulation | Progressive improvement over years |
| Common Side Effects | Headache, scalp discomfort, facial twitching [126] | Surgical site pain, infection, stimulation-induced side effects specific to target [122] | Hoarseness, cough, dyspnea, neck pain [124] |
| Serious Adverse Events | Seizure (<0.01%) [126] | Intracranial hemorrhage (1-2%), infection (3-5%) [122] | Vocal cord paralysis (<1%), infection (3%) [125] |
| FDA Approval Status | Approved for MDD (2008), OCD (2018) [126] | Humanitarian Device Exemption for OCD (2009); investigational for depression [122] | Approved for TRD (2005) [124] |
Experimental Methodology and Research Applications
Research Reagents and Technical Solutions
Table 3. Essential Research Reagents and Methodologies for Neuromodulation Studies
| Research Tool | Application | Technical Function |
|---|---|---|
| Neuronavigation Systems | TMS targeting | Individualized coil placement based on structural/functional neuroimaging |
| Microelectrode Recording (MER) | DBS target refinement | Intraoperative neurophysiological mapping during DBS lead implantation |
| Diffusion Tensor Imaging (DTI) | Connectomic analysis | Reconstruction of white matter pathways for target identification |
| Functional MRI (fMRI) | Target engagement assessment | Evaluation of network-level effects pre-/post-stimulation |
| Local Field Potential (LFP) Sensing | Adaptive DBS systems | Detection of neural biomarkers for closed-loop stimulation |
| Electroencephalography (EEG) | TMS response biomarkers | Measurement of cortical excitability and oscillatory activity |
| Positron Emission Tomography (PET) | Neurotransmitter system analysis | Investigation of dopaminergic, serotonergic effects of stimulation |
Protocol Implementation and Methodological Considerations
The implementation of standardized protocols is essential for research comparability and clinical reproducibility. For TMS studies, key methodological considerations include the use of neuronavigation for precise targeting, determination of individual resting motor threshold (rMT) for dose calibration, and standardization of outcome measures using established depression rating scales such as the Hamilton Depression Rating Scale (HAMD) or Montgomery-Åsberg Depression Rating Scale (MADRS) [123] [127].
DBS research protocols require meticulous surgical planning incorporating multi-modal neuroimaging, precise stereotactic technique, and systematic parameter optimization post-operatively [122]. The emerging field of connectomic DBS utilizes machine learning approaches to identify optimal stimulation targets based on their connectivity profiles, potentially explaining why similar anatomical targets produce variable clinical outcomes across individuals [122].
VNS research methodologies must account for the therapy's unique temporal response pattern, with study designs incorporating adequate long-term follow-up (≥12 months) to capture maximal therapeutic effects [124]. Parameter optimization studies suggest that higher electrical doses may enhance antidepressant efficacy, though this must be balanced against potential side effects [121].
Figure 2. Experimental Workflow for Neuromodulation Research. Comprehensive research protocols incorporate detailed patient characterization, intervention-specific procedures, and multi-dimensional outcome assessment with long-term follow-up.
TMS, DBS, and VNS represent distinct approaches to modulating dysfunctional neural circuits in treatment-resistant depression, each with characteristic mechanisms, efficacy profiles, and risk-benefit considerations. TMS offers a favorable non-invasive option with recent accelerated protocols substantially reducing treatment duration while maintaining efficacy. DBS enables precise targeting of subcortical circuits but requires invasive neurosurgical procedures. VNS provides a unique mechanism of indirect neuromodulation with progressively increasing benefit over extended timeframes.
Future directions in neuromodulation research include the development of increasingly personalized targeting approaches based on individual connectomic profiles, closed-loop systems that adapt stimulation parameters in response to neural biomarkers, and combination strategies that integrate neuromodulation with psychotherapeutic or pharmacological interventions to enhance treatment response. For researchers and drug development professionals, understanding the distinct characteristics of these somatic interventions provides critical insights for future therapeutic innovation in treatment-resistant depression.
Major depressive disorder (MDD) is a pervasive mental health condition characterized by dysfunction in brain reward and emotion regulation circuits. While traditional monoamine-based antidepressants require weeks to months to take effect and have high non-response rates, rapid-acting interventions like ketamine and electroconvulsive therapy (ECT) achieve remission within hours to days, even in treatment-resistant cases. Understanding how these diverse interventions converge on shared neural circuits provides crucial insights for developing targeted, effective therapeutics. This analysis examines the mechanistic parallels between ketamine, ECT, and transcranial magnetic stimulation (TMS) in modulating specific neural pathways, focusing on recent discoveries that establish adenosine signalling as a central pathway unifying their antidepressant actions. By framing these treatments within a circuit-based paradigm, we can identify critical leverage points for future antidepressant development and personalize therapeutic strategies based on individual neurocircuitry profiles.
Mechanistic Convergence on Adenosine Signalling
Adenosine as a Pivotal Neuromodulator
Recent research has identified adenosine signalling as a fundamental mechanism underlying rapid-acting antidepressant effects. Using genetically encoded adenosine sensors and real-time optical recordings, studies reveal that both ketamine and ECT induce robust adenosine surges in key mood-regulatory regions, including the medial prefrontal cortex (mPFC) and hippocampus. These adenosine increases feature peak amplitudes of approximately 15% change in fluorescence (ΔF/F), onset times of 100-150 seconds after intervention, peak times around 500 seconds, and decay time constants of 500-600 seconds after the peak [129].
The necessity of adenosine signalling for antidepressant efficacy is demonstrated through both genetic and pharmacological approaches. Genetic disruption of A1 (Adora1–/–) or A2A (Adora2a–/–) adenosine receptors completely abolishes the therapeutic effects of ketamine, as assessed through forced swim tests (measuring behavioral despair) and sucrose preference tests (measuring anhedonia) at both 1-hour (acute) and 24-hour (sustained) timepoints post-administration. Similarly, pharmacological blockade of A1 and A2A receptors in wild-type mice prevents ketamine from reversing depressive-like behaviors in both chronic restraint stress and lipopolysaccharide-induced depression models [129].
Regional Specificity and Metabolic Regulation
The antidepressant actions of adenosine signalling display remarkable regional specificity, with the medial prefrontal cortex identified as a critical site. Ketamine increases adenosine primarily by modulating cellular metabolism to elevate intracellular adenosine levels without causing neuronal hyperactivity. Notably, the parent ketamine molecule—not its metabolites norketamine or (2R,6R)-HNK—directly triggers adenosine release, with the magnitude regulated by CYP3A4-mediated metabolism [129].
Table 1: Key Characteristics of Antidepressant-Induced Adenosine Signalling
| Parameter | Ketamine Effect | ECT Effect | Significance |
|---|---|---|---|
| Brain Regions Affected | mPFC, hippocampus | mPFC, hippocampus | Mood-regulatory circuits targeted |
| Onset Time | 100-150 seconds | Similar to ketamine | Rapid initiation of effect |
| Peak Amplitude | ~15% ΔF/F | Strong surges | Dose-dependent relationship |
| Duration | 500-600 sec decay constant | Sustained release | Correlates with therapeutic persistence |
| Primary Receptor Mediation | A1 and A2A receptors | A1 and A2A receptors | Both receptors required for full efficacy |
Neuroimaging Evidence of Convergent Circuit Changes
Meta-Analytic Findings Across Treatment Modalities
Coordinate-based meta-analysis of task-based functional magnetic resonance imaging (fMRI) studies reveals consistent neural changes following successful depression treatment across various interventions. Analysis of 302 depressed subjects across 18 experiments, encompassing pharmacology, psychotherapy, ECT, psilocybin, and ketamine treatments, identifies the right amygdala (peak MNI coordinates [30, 2, -22]) as a region of convergent change. Follow-up analyses indicate this reflects decreased right amygdala activity following treatment, suggesting normalization of hyperactive threat and emotional processing circuitry across disparate therapeutic approaches [23].
These findings highlight that despite different initial molecular targets, effective depression treatments converge on normalizing activity in brain circuits governing emotional processing, particularly those involved in salience detection and threat response.
Predictive Circuit Biomarkers for Treatment Response
Advanced neuroimaging approaches are identifying circuit-based biomarkers that predict treatment outcomes. Machine learning models, particularly graph neural networks (GNNs) that integrate both neuroimaging and clinical features, can predict remission to selective serotonin reuptake inhibitors (SSRIs) with 71-76% accuracy. Key contributing brain regions include the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus—components of both reward and emotion regulation circuits [4].
These predictive models highlight the importance of baseline circuit integrity in determining treatment response and suggest that different antidepressant modalities ultimately converge on normalizing dysfunction in specific neural networks, regardless of their initial mechanisms of action.
Table 2: Neural Circuits Implicated in Antidepressant Response
| Neural Circuit | Component Regions | Associated Symptoms | Treatment Response Prediction |
|---|---|---|---|
| Reward Circuit | Ventral striatum, ventral pallidum, DLPFC, OFC, ACC, thalamus | Anhedonia, lack of motivation | SSRIs modulate 5-HT in insula and ventral striatum |
| Emotion Regulation Circuit | Prefrontal cortex, hippocampus, amygdala, OFC, ACC | Depressed mood, emotional dysregulation | Baseline activity predicts remission across treatments |
| Salience Network | Anterior insula, dorsal ACC, amygdala, thalamus | Arousal, attention to relevant stimuli | Enlarged network may be trait-like feature persistent after treatment |
Experimental Models and Methodologies for Circuit Analysis
Quantitative Modeling of Neural Circuit Interactions
Computational modeling provides a framework for interpreting and guiding research on neural circuit interactions in state transitions relevant to depression. System-theoretic approaches identify feedback, redundancy, and gating hierarchy as fundamental aspects of sleep-wake regulatory networks, with implications for understanding transitions between pathological and normal affective states. These models incorporate data from optogenetic experiments, which allow millisecond-precision manipulation of genetically defined cell types, to determine how specific neuromodulators contribute to vigilance state transitions [8].
Key neurotransmitters implicated in these state transitions include hypocretin (Hcrt), norepinephrine (NE), acetylcholine (ACh), serotonin (5-HT), and histamine (His), which originate from specific brain regions including the lateral hypothalamus, locus coeruleus, basal forebrain, dorsal raphe, and tuberomammillary nucleus, respectively. These same systems are modulated by antidepressant interventions [8].
Probing Circuit Function Through Behavioral Assays
Preclinical studies utilize standardized behavioral tests to quantify antidepressant-like effects and their underlying circuit mechanisms. The 24-hour forced swim test measures behavioral despair through mobility behavior, with decreased immobility indicating antidepressant efficacy. The novelty-suppressed feeding test assesses approach-avoidance conflict by measuring latency to approach and bite food in an anxiogenic environment, while the learned helplessness paradigm evaluates escape deficits following inescapable shocks. These tests demonstrate rapid (within 30 minutes to 24 hours) antidepressant effects of ketamine, scopolamine, GLYX-13, and other rapid-acting compounds, contrasting with the 14-day latency for classical antidepressants [130].
Research Reagent Solutions for Circuit-Level Investigation
Table 3: Essential Research Tools for Investigating Antidepressant Mechanisms
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| Genetically Encoded Sensors | GRABAdo1.0 (adenosine sensor) | Real-time monitoring of neuromodulator dynamics | Revealed ketamine-induced adenosine surges in mPFC and hippocampus |
| Optogenetic Tools | Channelrhodopsin (ChR2), Halorhodopsin (NpHR) | Cell-type-specific neuronal manipulation | Established causal roles of specific neuronal populations in state transitions |
| Receptor-Specific Compounds | A1 receptor antagonists, A2A receptor antagonists | Pharmacological dissection of receptor contributions | Determined both A1 and A2A receptors necessary for ketamine efficacy |
| Metabolic Inhibitors | CYP3A4 inhibitors (ketoconazole, ritonavir) | Manipulation of drug metabolism pathways | Established parent ketamine molecule drives adenosine release |
| Circuit-Tracing Tools | Anterograde/retrograde tracers, transsynaptic viruses | Mapping of neural connectivity | Identified mood-regulatory circuits (mPFC, hippocampus, amygdala) |
| Behavioral Paradigms | Forced swim test, sucrose preference test | Quantification of depressive-like behaviors | Demonstrated rapid antidepressant effects within hours |
Visualizing Convergent Mechanisms: Signalling Pathways and Experimental Workflows
Adenosine-Dependent Antidepressant Signalling Pathway
Experimental Workflow for Circuit Mechanism Elucidation
Therapeutic Implications and Future Directions
The convergence of ECT, ketamine, and related interventions on adenosine signalling and specific neural circuits reveals tractable targets for novel antidepressant development. Leveraging this mechanism, researchers have developed ketamine derivatives that enhance adenosine signalling while exhibiting improved antidepressant efficacy with reduced side effects at therapeutic doses. Furthermore, acute intermittent hypoxia—a non-pharmacological intervention involving controlled oxygen reduction—has been identified as a potent adenosine-dependent antidepressant strategy, paralleling the actions of ketamine and ECT [129].
These findings establish adenosine signalling as a pivotal mediator unifying the actions of diverse rapid-acting antidepressants and open new therapeutic avenues for major depressive disorder. Future research should focus on optimizing circuit-specific targeting of adenosine signalling while minimizing potential side effects, potentially through region-specific drug delivery or neuromodulation approaches. The continued integration of computational modeling, circuit neuroscience, and human neuroimaging will further elucidate the precise mechanisms through which these powerful interventions restore normal function to dysregulated affective circuits.
Major depressive disorder (MDD) is a heterogeneous condition affecting over 280 million people globally, yet traditional symptom-based diagnostic frameworks have failed to address its underlying biological diversity [131] [132]. This heterogeneity explains why conventional first-line antidepressants lead to remission in only 30% of patients, leaving many without relief through a frustrating process of trial-and-error prescribing [131]. Precision psychiatry represents a paradigm shift from this one-size-fits-all approach toward a targeted strategy that matches mechanistically selective treatments to specific circuit dysfunctions identified in individual patients [131]. The core premise is that current diagnostic classifications group together biologically distinct subtypes of depression, much like fever represents a common clinical presentation of many underlying processes [131].
Research has now identified several neurobiologically defined biotypes of depression, characterized by distinct patterns of circuit dysfunction [101]. This whitepaper examines three prominent approaches demonstrating how circuit-based targeting can guide therapeutic modality selection: cognitive biotype targeting through α2A-adrenergic receptor agonism, inflammatory subtype targeting via immunomodulatory interventions, and predictive treatment selection using neuroimaging-based machine learning. Each approach exemplifies the precision psychiatry principle that effective treatment must address the specific biological mechanisms driving an individual's symptoms rather than merely targeting symptom clusters [131] [101].
Targeting the Cognitive Biotype: α2A-Adrenergic Receptor Agonism
Cognitive Biotype Identification and Circuit Basis
A distinct subgroup of MDD patients, termed the "cognitive biotype," presents with prominent cognitive impairments and accounts for approximately 27% of depression cases [101]. This biotype is prospectively identified through characteristic impairments in both cognitive control circuit function and associated behavioral performance. The defining neural signature involves significantly reduced task-evoked activation and functional connectivity within the cognitive control circuit, particularly affecting the dorsolateral prefrontal cortex (dLPFC) and dorsal anterior cingulate cortex (dACC) [101]. These circuit abnormalities manifest behaviorally as measurable deficits in cognitive control tasks, including impaired response inhibition and interference control.
Individuals with this biotype typically show poor response to standard antidepressant treatments and report significantly diminished quality of life [101]. The cognitive impairments in this subgroup persist even after symptom remission and contribute substantially to poor functional outcomes, heightened risk of suicide, and treatment resistance [101]. Conventional antidepressants developed within broad drug development frameworks have largely failed to address these specific circuit deficiencies, creating an urgent need for mechanistically targeted alternatives.
Guanfacine Immediate Release: Mechanism and Target Engagement
Guanfacine immediate release (GIR) represents a mechanistically selective treatment approach specifically targeting the cognitive biotype of depression. As an α2A-adrenergic receptor agonist, GIR meets key criteria for stratified precision medicine through its established safety profile, neurobiological selectivity, and demonstrated translational relevance from animal models to humans [101]. The drug's therapeutic action stems from selective α2A receptor expression in prefrontal cortical regions critical to the cognitive control circuit, confirmed through radioligand binding studies [101]. Preclinical research demonstrates that GIR enhances activation and synaptic plasticity in these prefrontal regions, with effects that translate consistently across species [101].
Table 1: Guanfacine Immediate Release Clinical Trial Outcomes for Cognitive Biotype Depression
| Outcome Measure | Baseline Values | Post-Treatment Values | Statistical Significance | Effect Size (Cohen's d) |
|---|---|---|---|---|
| HDRS-17 Reduction | Median 15 (range 14-27) | Significant reduction | P = 3.04 × 10^-5 | 3.152 |
| Clinical Response (≥50% HDRS reduction) | 0% | 76.5% (13/17 patients) | Not applicable | Not applicable |
| Symptom Remission (HDRS ≤7) | 0% | 67.4% of total sample | Not applicable | Not applicable |
| dACC Activation | >0.5 SD below healthy mean | Significant increase | P = 0.033 | 0.566 |
| dACC-left dLPFC Connectivity | >0.5 SD below healthy mean | Significant increase | P = 0.014 | 0.668 |
Experimental Protocol and Methodology
The Biomarker Guided (BIG) Study for Depression implemented a stratified precision medicine approach with the following methodological framework [101]:
Participant Selection Criteria:
- Moderate-to-severe depressive symptoms (17-item Hamilton Rating Scale for Depression score median 15, range 14-27)
- Impairments in cognitive control circuit function (>0.5 standard deviations below healthy reference mean)
- Impaired cognitive control behavioral performance (>0.5 standard deviations below healthy reference mean)
Treatment Protocol:
- 6-8 weeks of GIR treatment with target dose of 2 mg per night
- Consistent with preregistered per-protocol analysis plan
- 17 participants meeting cognitive biotype criteria completed treatment
Primary Outcome Measures:
- Change in cognitive control circuit activation and connectivity (task-evoked fMRI in right/left dLPFC and dACC)
- Hamilton Depression Rating Scale (HDRS-17) scores
- Cognitive control performance metrics (verbal interference task, response inhibition)
Circuit Specificity Assessment:
- Evaluation of five additional circuits: default mode, salience, frontoparietal attention, negative affect, positive affect
- No significant changes observed in these control circuits, confirming treatment specificity
Diagram 1: Cognitive Biotype Targeted Therapy Framework
Immunopsychiatry: Targeting Inflammation-Mediated Circuit Dysfunction
Inflammatory Subtype Identification and Prevalence
Immunopsychiatry represents one of the most advanced domains in translational precision psychiatry, focusing on patients with immune-mediated depression [131]. Large biobank studies indicate that approximately 27% of depressed patients demonstrate measurable low-grade inflammation, characterized by chronically elevated inflammatory markers such as high-sensitivity C-reactive protein (hsCRP) [131]. This inflammatory subtype transcends traditional diagnostic boundaries and represents a transdiagnostic continuum ranging from rare autoimmune presentations to more common pathophysiology modulated by low-grade inflammation [131]. Individuals exposed to childhood maltreatment or early life infections appear particularly vulnerable to developing these immune abnormalities, which are observed across DSM diagnostic categories [131].
The "inflammatory trap" hypothesis proposes that persistent immune activation disrupts not only brain circuits but also impairs the brain's inherent capacity for neuroplasticity and recovery [131]. Chronic inflammation leads to sustained cortisol release through HPA axis disruption, microglial activation, and neurotransmitter imbalances via the tryptophan-kynurenine pathway, ultimately reducing serotonin availability while promoting neurotoxic metabolites [131]. This cascade particularly affects brain regions governing motivation, reward, and cognition, including the prefrontal cortex, hippocampus, and striatum, manifesting clinically as symptoms of motivational anhedonia, fatigue, and cognitive impairment [131].
Anti-Inflammatory Interventions: Evidence and Biomarker Stratification
More than 18 placebo-controlled trials of immune-targeted pharmacological interventions have demonstrated small-to-moderate effect sizes for improving depressive symptoms when added to treatment as usual [131]. However, critical analysis reveals that therapeutic benefits are predominantly confined to patients with confirmed inflammatory activation. Post-hoc analyses of three separate studies showed that antidepressant efficacy of anti-inflammatories was limited to patients with elevated inflammation, specifically those with hsCRP levels >3 mg/L for minocycline and N-acetylcysteine and >5 mg/L for infliximab [131]. Similarly, post-hoc analysis of statins in schizophrenia spectrum disorders revealed that only patients in the inflammatory subgroup showed consistent symptom reduction over time [131].
Table 2: Inflammatory Biomarkers and Targeted Therapies in Depression
| Biomarker | Normal Range | Inflammatory Cut-off | Therapeutic Agent | Reported Effect Size |
|---|---|---|---|---|
| hsCRP | <3 mg/L | >3 mg/L (minocycline, NAC) | Minocycline | Small-to-moderate |
| hsCRP | <3 mg/L | >5 mg/L (infliximab) | Infliximab | Small-to-moderate |
| IL-6 | Variable | Elevated | Tocilizumab (investigational) | Under investigation |
| TNF-α | Variable | Elevated | Infliximab | Small-to-moderate |
| Autoantibodies | Absent | Present (severe cases) | Immunotherapy | Case-dependent |
Despite promising findings, translation to clinical practice remains limited, with two significant barriers: difficulty identifying appropriate patients and accurately measuring treatment effects [131]. Many existing studies have failed to effectively screen participants based on inflammatory status at baseline, and traditional depression outcome measures may not adequately capture the specific symptom profiles associated with inflammation-mediated depression [131].
Experimental Protocol for Immune-Targeted Trials
Participant Stratification Methodology:
- Pre-treatment measurement of inflammatory biomarkers (hsCRP, IL-6, TNF-α)
- Established cut-off values for inclusion (e.g., hsCRP >3 mg/L or >5 mg/L depending on agent)
- Assessment for comorbid autoimmune conditions or history of treatment resistance
Treatment Agents and Dosing:
- Anti-inflammatory medications: celecoxib, minocycline, infliximab, N-acetylcysteine
- Adjunctive use with conventional antidepressants
- Dosing regimens tailored to individual inflammatory profiles
Outcome Assessment:
- Standardized depression rating scales (HAM-D, MADRS)
- Inflammation-specific symptom monitoring (anhedonia, fatigue, cognitive dysfunction)
- Serial biomarker measurement to track target engagement
- Functional capacity and quality of life measures
Diagram 2: Inflammatory Pathway and Therapeutic Targeting in Depression
Predictive Neuroimaging and Machine Learning Approaches
Graph Neural Networks for Treatment Outcome Prediction
Advanced machine learning methodologies, particularly graph neural networks (GNNs), have demonstrated significant potential for predicting antidepressant treatment outcomes based on pre-treatment neuroimaging and clinical features [4]. A recent study developed a hierarchical local-global imaging and clinical feature fusion graph neural network model (LGCIF-GNN) that achieved 76.21% accuracy (AUC = 0.78) in predicting remission following selective serotonin reuptake inhibitor (SSRI) treatment [4]. The model maintained similar performance on internal and external independent validation datasets (accuracy = 72.73%, AUC = 0.74; accuracy = 71.43%, AUC = 0.72 respectively), demonstrating robust generalizability [4].
The model architecture specifically focuses on neurocircuits associated with depressed mood and anhedonia—core symptoms of MDD linked to poor treatment outcomes. Key contributing brain regions identified included the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus [4]. These regions align with known reward and emotion regulation circuits, highlighting the importance of circuit-based prediction over symptom-based approaches alone.
Experimental Protocol for Neuroimaging Prediction
Participant Cohort and Treatment:
- 279 untreated MDD patients
- Treated with SSRIs for 8-12 weeks
- Assigned to training, internal validation, and external validation datasets
Feature Selection and Integration:
- Clinical and demographic information: age, sex, education, illness duration
- Clinical scores: Hamilton Depression Rating Scale, Quality of Life Enjoyment and Satisfaction Questionnaire
- Neuroimaging features: resting-state fMRI focusing on reward and emotion regulation circuits
Model Architecture and Training:
- Hierarchical local-global graph neural network design
- Dynamic graph structure optimization using bidirectional GRU encoder
- Integration of intra-subject ROI-level dynamics and inter-subject population-level similarities
- End-to-end joint optimization of local and global network structures
Validation Framework:
- Internal validation through cross-validation
- External validation on independent dataset
- Performance metrics: accuracy, AUC, sensitivity, specificity
Table 3: Key Brain Regions Predicting Antidepressant Treatment Response
| Brain Region | Circuit Association | Prediction Importance | Functional Relevance |
|---|---|---|---|
| Bilateral Anterior Cingulate Gyrus | Emotion regulation | High | Conflict monitoring, emotional processing |
| Left Hippocampus | Emotion regulation, memory | Medium | Contextual memory, stress regulation |
| Bilateral Thalamus | Reward processing, attention | High | Sensory integration, alertness |
| Bilateral Putamen | Reward processing | Medium | Motor response, reward learning |
| Right Globus Pallidus | Reward processing | Medium | Movement regulation, reward valuation |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for Precision Psychiatry Investigations
| Research Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Neuroimaging Modalities | fMRI, resting-state fMRI, structural MRI | Circuit function assessment, structural connectivity | 3T minimum field strength; task paradigms for specific circuits |
| Molecular Biomarker Assays | hsCRP, IL-6, TNF-α ELISA kits, autoantibody panels | Inflammatory subtype identification, target engagement | Standardized collection protocols; established cut-off values |
| Cognitive Assessment Tools | Verbal interference tasks, response inhibition measures, cognitive control batteries | Cognitive biotype identification, treatment response monitoring | Normative reference data; parallel forms for repeated testing |
| Computational Resources | Graph Neural Network frameworks, machine learning libraries | Treatment outcome prediction, biomarker identification | High-performance computing; specialized GNN architectures |
| Pharmacological Agents | Guanfacine IR, minocycline, celecoxib, infliximab | Mechanism-based intervention studies | Dose titration protocols; combination therapy strategies |
The emerging paradigm of precision psychiatry represents a fundamental transformation in how we conceptualize and treat major depressive disorder. By moving beyond symptom-based diagnoses to target specific circuit dysfunctions, this approach offers the promise of mechanistically informed treatments matched to individual neurobiological profiles. The three approaches examined—cognitive biotype targeting, inflammatory subtype intervention, and neuroimaging-based prediction—demonstrate that circuit-based stratification can significantly improve therapeutic outcomes beyond what is achievable through conventional approaches.
Future directions in precision psychiatry will require increased integration across multiple modalities, including genetic, molecular, circuit, and clinical data. Additionally, standardization of biomarker assessment, validation of predictive models in diverse populations, and development of novel interventions targeting specific circuits will be essential for advancing the field. As these approaches mature, precision psychiatry offers the potential to finally deliver on the promise of the right treatment for the right patient at the right time, transforming the landscape of depression therapeutics and dramatically improving outcomes for this debilitating disorder.
The treatment of major depressive disorder (MDD), particularly treatment-resistant depression (TRD), represents a significant unmet medical need. Conventional monoamine-based antidepressants often require weeks to exert their effects, and a substantial proportion of patients do not achieve remission. This landscape has driven research into rapid-acting antidepressant agents, with a particular focus on compounds targeting the glutamatergic system. This whitepaper evaluates clinical trial data for these novel therapeutics, framing their efficacy and safety within the context of neural circuitry changes underlying depression and antidepressant response. Evidence indicates that synaptic dysfunction is a core component of MDD pathophysiology, and effective treatments converge on mechanisms to restore synaptic connectivity and plasticity [12].
Recent clinical trials have demonstrated the promise of glutamatergic system modulators. The following table summarizes quantitative efficacy data from a Phase 2, randomized, placebo-controlled, proof-of-concept study investigating Onfasprodil (MIJ821), a novel NR2B-negative allosteric modulator, with ketamine as an active comparator [133] [134].
Table 1: Efficacy Outcomes of Onfasprodil vs. Placebo and Ketamine in Treatment-Resistant Depression
| Treatment Group | Mean MADRS Change vs. Placebo at 24 hours (Primary Endpoint) | P-value | Mean MADRS Change vs. Placebo at 48 hours | P-value | Sustained Efficacy at Week 6 (vs. Placebo) | P-value |
|---|---|---|---|---|---|---|
| Onfasprodil (pooled 0.16 mg/kg) | -8.25 | .001 | -7.06 | .013 | -5.78 | .0427 |
| Onfasprodil (pooled 0.32 mg/kg) | -5.71 | .019 | -7.37 | .013 | -4.24 | .1133 |
| Ketamine (0.5 mg/kg) | -5.67 | .046 | -11.02 | .019 | -5.24 | .0974 |
Abbreviation: MADRS, Montgomery-Åsberg Depression Rating Scale.
The data reveal a rapid onset of action for Onfasprodil, with significant antidepressant effects observed within 24 hours of a single infusion. Notably, the lower dose (0.16 mg/kg) demonstrated not only rapid efficacy but also statistically significant sustained effects at the end of the 6-week study period [133] [134]. The dissociation between dose and sustained effect warrants further investigation but suggests complex pharmacokinetic or pharmacodynamic interactions.
Detailed Experimental Protocol
Understanding the methodology is critical for interpreting the data and designing future studies.
Study Design and Population
- Trial Design: This was a Phase 2, randomized, double-blind, placebo-controlled, parallel-group, multicenter study (NCT03756129) [134].
- Treatment Arms and Randomization: Seventy (70) adults with TRD (MADRS score ≥24 and prior failure of ≥2 antidepressants) were randomized across six arms:
- Onfasprodil 0.16 mg/kg weekly (
n=11) - Onfasprodil 0.16 mg/kg biweekly (
n=10) - Onfasprodil 0.32 mg/kg weekly (
n=10) - Onfasprodil 0.32 mg/kg biweekly (
n=9) - Placebo weekly (
n=20) - Ketamine 0.5 mg/kg weekly (
n=10)
- Onfasprodil 0.16 mg/kg weekly (
- Intervention: All treatments were administered via a 40-minute intravenous infusion. The total study duration was 14 weeks, including a 36-day treatment period [134].
Endpoints and Assessments
- Primary Efficacy Endpoint: Change from baseline in MADRS total score at 24 hours after a single dose [134].
- Secondary Efficacy Endpoints: Change from baseline in MADRS score at 48 hours and after the final dose at Week 6 [133].
- Statistical Analysis: The primary analysis used an Analysis of Covariance (ANCOVA) model with treatment as a factor and baseline MADRS as a covariate. A Mixed-Model for Repeated Measures (MMRM) was also employed for longitudinal analysis [134].
- Safety Assessment: Treatment-emergent adverse events (TEAEs) were monitored throughout the study. Specific attention was given to dissociative effects, measured using the Clinician-Administered Dissociative States Scale (CADSS) and Dissociative Experiences Scale (DES) [134].
Neural Circuitry and Mechanisms of Action
The therapeutic action of rapid-acting antidepressants is inextricably linked to their impact on maladaptive neural circuitry. Major depressive disorder is associated with volume reductions in cortical and subcortical structures, compromised myelin integrity, and reduced expression of synaptic genes [12]. Post-mortem studies consistently show changes in the density and size of neurons and glia [135].
Distinct Neural Pathways for Different Modalities
Neuroimaging meta-analyses reveal that different antidepressant treatments engage distinct but complementary neural pathways, despite both converging on the brain's affect network [41]:
- Pharmacological Agents (e.g., Antidepressants): Primarily evoke neural changes in subcortical structures, such as the amygdala, which is involved in the generation of affective and visceral sensations [41].
- Psychological Therapies (e.g., CBT): Predominantly induce changes in prefrontal cortical regions, such as the medial prefrontal cortex, which is involved in the cognitive control of affect processing [41].
Synaptic Convergence of Molecular Pathways
Multiple molecular pathways implicated in MDD pathophysiology converge on the synapse to mediate their effects [12]. The diagram below illustrates the key signaling pathways targeted by rapid-acting antidepressants like ketamine and Onfasprodil.
Diagram: Synaptic Mechanisms of Rapid-Acting Antidepressants. NR2B NAMs and ketamine antagonize NMDA receptors, leading to a cascade involving AMPA receptor activation, BDNF release, and mTOR-mediated synaptogenesis.
This synaptic model is supported by genetic findings; the largest genome-wide association study of MDD to date identified risk loci in genes highly expressed in the brain and involved in synapse assembly and function, such as NEGR1 and DRD2 [12] [134]. The diagram below outlines the experimental workflow from patient recruitment to data analysis, as implemented in the cited Onfasprodil clinical trial.
Diagram: Clinical Trial Workflow for Evaluating Rapid-Acting Antidepressants.
Safety and Tolerability Profile
Safety data is crucial for evaluating the risk-benefit profile of any novel therapeutic. In the Onfasprodil study, the agent demonstrated a good safety profile and was generally well-tolerated [133] [134].
The most common treatment-emergent adverse events (TEAEs) in the Onfasprodil groups were:
- Dizziness (14.3%)
- Transient amnesia (14.3%)
- Somnolence (11.4%)
A key differentiator from ketamine is the effect on dissociative states. While ketamine is known to cause dissociative and psychotomimetic effects, the lower dose of traxoprodil (a predecessor NR2B NAM) was effective without producing a dissociative reaction [134]. This suggests that selective NR2B antagonism may offer a more favorable tolerability profile compared to broad NMDA receptor antagonists like ketamine.
The Scientist's Toolkit: Research Reagent Solutions
Advancing research in this field requires a specific set of tools and reagents. The following table details key resources used in the featured clinical trial and related biomarker research.
Table 2: Essential Research Reagents and Tools for Clinical Trials in Rapid-Acting Antidepressants
| Research Tool / Reagent | Function & Application in Research |
|---|---|
| Montgomery-Åsberg Depression Rating Scale (MADRS) | A clinician-rated scale designed to measure depression severity and sensitivity to change; used as the primary efficacy endpoint in clinical trials [134]. |
| Clinician-Administered Dissociative States Scale (CADSS) | A validated questionnaire used to assess dissociative symptoms, critical for monitoring the side effect profile of NMDA receptor-targeting drugs [134]. |
| Functional Magnetic Resonance Imaging (fMRI) | A neuroimaging technique used to identify neural biomarkers of treatment response, such as baseline activity in the amygdala or prefrontal cortex [41] [136]. |
| Dexamethasone-CRH Challenge Test | A neuroendocrine function test assessing HPA axis hyperactivity; a potential biomarker for predicting depression relapse and treatment resistance [136]. |
| Interactive Response Technology (IRT) | A validated system used in clinical trials to automate patient randomization and ensure allocation concealment, as described in the Onfasprodil study methodology [134]. |
The clinical trial data for Onfasprodil substantiates the promise of NR2B-negative allosteric modulators as rapid-acting antidepressants with sustained efficacy. The significant improvement in depressive symptoms within 24 hours, coupled with evidence of durability at six weeks, represents a potential paradigm shift in TRD management. The distinct neural mechanisms of these agents—converging on synaptic plasticity and circuitry restoration without engaging the same dissociative pathways as ketamine—highlight the importance of targeted glutamatergic modulation. Future research should focus on larger Phase 3 trials, further exploration of optimal dosing regimens, and the identification of robust neurobiological biomarkers to predict individual patient response.
Major depressive disorder (MDD) is a leading cause of global disability, accounting for 32.4% of years lived with disability and presenting substantial economic burdens estimated at £300 billion in England alone in 2022 [137]. Traditional treatments including medications and psychotherapies often provide only modest symptom improvements, with 20-60% of individuals failing to respond adequately to optimal treatments [137]. Contemporary research has reframed psychiatric disorders as conditions of large-scale brain networks rather than abnormalities within isolated brain regions [137]. This paradigm shift recognizes that dysfunctional information processing within and between neural networks contributes fundamentally to the pathophysiology of depression and the manifestation of its symptoms [137]. The emerging understanding of depression as a network-level disorder provides a compelling theoretical foundation for combining two modality classes: pharmacotherapy, which modulates neurotransmitter systems, and neuromodulation, which directly targets dysfunctional neural circuits.
The imperative for novel therapeutic approaches stems from the significant limitations of current options. Medications and psychotherapies indirectly modulate neural activity and often fail to adequately address cognitive impairment—a transdiagnostic feature that does not respond to conventional treatments and significantly impacts functional outcomes [137]. Furthermore, cognitive impairments can persist despite overall symptom relief and predict poor response to antidepressant medication [71]. This therapeutic gap has stimulated investigation into mechanism-based interventions that can directly target the dysfunctional neural circuits underlying depression. The integration of pharmacotherapy with neuromodulation represents a promising approach grounded in the complementary mechanisms of these modalities: while medications alter neurochemical milieu throughout the brain, neuromodulation techniques can provide focal regulation of specific dysfunctional networks identified through neuroimaging biomarkers [137] [138].
Neural Circuitry of Depression: Network Dysfunction and Cognitive Biotypes
Large-Scale Brain Networks in Depression Pathophysiology
Research utilizing resting-state functional MRI (rsfMRI) and magnetoencephalography (MEG) has identified several large-scale brain networks critically involved in depression. The triple network model of psychopathology proposes that three core networks—the default mode network (DMN), central executive network (CEN), and salience network (SN)—demonstrate characteristic dysfunction across psychiatric disorders including depression [137]. The DMN, active during rest and internal reflection, often shows hyperconnectivity in depression, potentially underlying symptoms of rumination. Conversely, the CEN, crucial for executive functions and goal-directed behavior, frequently demonstrates hypoconnectivity, while the SN, responsible for detecting and orienting attention toward salient stimuli, may display impaired switching between the DMN and CEN [137].
Beyond these networks, the cognitive control circuit, particularly connections between the dorsolateral prefrontal cortex (dLPFC) and dorsal anterior cingulate cortex (dACC), has emerged as critically important. Dysfunction in this circuit is associated with impaired cognitive control—a core deficit in a identifiable biotype of depression [71]. Recent research has identified a cognitive biotype of depression characterized by treatment resistance, impaired cognitive control performance, and specific dysfunction in the dLPFC-dACC circuit [71]. This biotype demonstrates hypoconnectivity during cognitive tasks and shows comparatively low response and remission rates with standard pharmacotherapy [71]. Importantly, this circuit dysfunction serves not only as a diagnostic biomarker but also as a potential target for neuromodulation interventions.
Network Dysfunction as a Predictor of Treatment Response
Evidence increasingly supports that pretreatment network function can predict antidepressant response. A study examining beta-band functional connectivity during response inhibition found that non-responders to serotonergic antidepressants displayed reduced connectivity in a left-dominant frontoparietal network centered on the superior parietal gyrus and orbitofrontal cortex [139]. This hypoconnectivity distinguished non-responders from both responders and healthy controls, suggesting its potential value as a predictive biomarker [139]. Similarly, task-related dLPFC-dACC connectivity has been shown to predict pharmacotherapy outcomes and change proportionally with treatment [71]. These findings highlight the importance of circuit-level biomarkers for identifying individuals likely to respond to specific interventions and provide a rationale for targeting these circuits with combined modality approaches.
Table 1: Key Large-Scale Brain Networks Implicated in Depression
| Network | Core Regions | Primary Functions | Dysfunction in Depression |
|---|---|---|---|
| Default Mode Network (DMN) | Posterior cingulate cortex, medial prefrontal cortex, precuneus, angular gyrus | Introspection, self-reflection, autobiographical memory | Hyperconnectivity associated with rumination |
| Central Executive Network (CEN) | Dorsolateral PFC, posterior parietal cortex | Executive functions, working memory, cognitive control | Hypoconnectivity associated with cognitive impairment |
| Salience Network (SN) | Anterior cingulate cortex, anterior insula | Salient stimulus detection, switching between DMN & CEN | Impaired switching contributing to rumination |
| Cognitive Control Circuit | dLPFC, dACC | Cognitive control, response inhibition | Hypoconnectivity in cognitive biotype |
| Affective Network | Orbitofrontal cortex, subgenual ACC, amygdala, hippocampus | Emotion generation, emotional processing | Hyperactivity in negative emotion processing |
Neuromodulation Approaches: Mechanism and Evidence
Non-Invasive Brain Stimulation Techniques
Non-invasive brain stimulation (NIBS) techniques encompass several approaches that modulate neural activity through externally applied energy. Transcranial magnetic stimulation (TMS) uses electromagnetic induction to generate electric currents in targeted cortical regions, with different parameters producing varying effects: high-frequency stimulation (≥5 Hz) typically increases cortical excitability, while low-frequency stimulation (≤1 Hz) decreases it [140]. Theta burst stimulation (TBS) protocols deliver bursts of pulses in efficient paradigms, with intermittent TBS (iTBS) producing facilitatory effects and continuous TBS (cTBS) producing inhibitory effects [140]. Transcranial direct current stimulation (tDCS) applies a low-intensity current (0.5-2.0 mA) through scalp electrodes, with anodal stimulation typically increasing and cathodal stimulation decreasing cortical excitability [140]. Emerging techniques such as low-intensity focused ultrasound (FUS) offer potentially improved spatial precision and access to deeper brain regions [137].
Meta-analytic evidence supports the efficacy of neuromodulation for depression treatment. A 2025 meta-analysis of 10 randomized controlled trials found no significant differences between iTBS and traditional rTMS in remission rates (OR=1.01, 95% CI: 0.72-1.42), response rates (OR=1.02, 95% CI: 0.76-1.35), or adverse effects (OR=1.17, 95% CI: 0.83-1.66) [141]. Compared to sham stimulation, rTMS showed significantly higher remission (OR=4.84, 95% CI: 2.66-8.80) and response rates (OR=3.92, 95% CI: 2.08-7.37) [141]. Another network meta-analysis found bilateral TBS had the potential to be among the most efficacious neuromodulation approaches for treatment-resistant depression [128].
Network-Targeted Neuromodulation
A precision medicine approach to neuromodulation involves targeting stimulation based on individual network dysfunction. In the B-SMART-fMRI trial, researchers stratified patients with treatment-resistant depression based on baseline dLPFC-dACC connectivity during a Go-NoGo task [71]. Those with hypoconnectivity (cognitive biotype +) showed significant improvement in both connectivity and cognitive performance after TMS targeted to the left dLPFC, while those with intact connectivity (cognitive biotype -) did not demonstrate significant changes [71]. This demonstrates that connectivity biomarkers can identify individuals most likely to benefit from circuit-targeted neuromodulation. The restoration of cognitive control circuit connectivity occurred early in treatment and was associated with improved behavioral performance, suggesting that TMS directly modulated the dysfunctional network [71].
Table 2: Efficacy of Neuromodulation Techniques for Depression Based on Meta-Analyses
| Technique | Response Rate vs. Sham (OR, 95% CI) | Remission Rate vs. Sham (OR, 95% CI) | Key Parameters | Advantages |
|---|---|---|---|---|
| High-frequency left rTMS | 2.18 (1.52-3.13) [128] | Not reported | 10-20 Hz, figure-8 coil to left DLPFC | Established efficacy, FDA approval for depression |
| Bilateral rTMS | 3.08 (1.78-5.31) [128] | Not reported | Combined left high-frequency & right low-frequency | Targets both hemispheres |
| Theta burst stimulation (TBS) | 5.00 (1.11-22.44) [128] | No significant difference vs. rTMS [141] | Intermittent or continuous patterns | Shorter treatment duration (3-10 minutes) |
| Priming TMS | 2.97 (1.20-7.39) [128] | Not reported | Initial low-frequency priming before high-frequency | Potentially enhanced plasticity |
| tDCS | Variable effect sizes [140] | Not reported | 1-2 mA, anodal to left DLPFC | Portable, low-cost, home-use potential |
Pharmacotherapy Mechanisms: From Synapse to Network
Neurotransmitter Systems in Depression and Recovery
Pharmacologic therapies for depression primarily target monoaminergic neurotransmitter systems, including serotonin, norepinephrine, and dopamine. These systems originate in brainstem nuclei and project widely throughout the cortex, regulating various aspects of mood, motivation, and cognition [138]. Emerging evidence suggests that these neurotransmitter systems also play crucial roles in regulating large-scale network dynamics. For instance, dopamine signaling modulates prefrontal-striatal circuits involved in reward processing and motivation, while norepinephrine influences attentional networks [138]. The mesocircuit model proposes that recovery of consciousness and cognitive function after brain injury—relevant to depression—involves modulation of thalamocortical circuits by dopaminergic and other neurotransmitter systems [138].
Beyond conventional antidepressants, other pharmacologic agents show promise for modulating network function. General anesthetics like propofol may manipulate slow waves in the electroencephalogram (EEG), which are key markers of brain function and health associated with depression [5]. Research suggests there may be an optimal dosing regimen that achieves a 'sweet spot' of expressing slow waves, potentially maximizing therapeutic benefits [5]. Similarly, ketamine has been shown to enhance slow-wave activity correlated with improvements in mood and cognition [5]. These approaches represent novel pharmacologic strategies that directly target network-level dynamics rather than focusing solely on synaptic neurotransmission.
Pharmacologic Enhancement of Neuroplasticity
An important mechanism through which pharmacotherapy may complement neuromodulation is by enhancing neuroplasticity—the brain's ability to reorganize its structure and function. Conventional antidepressants promote neurotrophic factor signaling and synaptogenesis, particularly in hippocampal and prefrontal regions [137]. These plasticity-enhancing effects may facilitate the reorganization of dysfunctional networks when combined with neuromodulation techniques that provide targeted activation of specific circuits. The timing of pharmacologic interventions relative to neuromodulation may be critical, as medications that enhance plasticity could potentially strengthen the network changes induced by stimulation. This synergistic approach represents a promising direction for combination therapy.
Theoretical Framework for Combined Modality Approaches
Complementary Mechanisms of Action
The combination of pharmacotherapy and neuromodulation offers complementary mechanisms operating at different levels of the neural hierarchy. Pharmacotherapy primarily acts at the molecular and synaptic levels, altering neurotransmitter availability and signaling throughout the brain [138]. In contrast, neuromodulation operates at the circuit and network levels, directly modulating the activity and connectivity of specific neural populations [137]. When combined, these approaches may produce synergistic effects: pharmacotherapy could create a permissive neurochemical environment that enhances the effects of neuromodulation, while neuromodulation could direct plasticity toward specific dysfunctional circuits in a way that diffuse pharmacotherapy cannot.
The potential synergy between these modalities can be conceptualized through several mechanisms:
Neuroplasticity Priming: Pharmacologic agents may enhance neuroplasticity mechanisms, potentially lowering the threshold for neuromodulation to induce lasting circuit changes [5].
State-Dependent Modulation: Medications may alter brain states in ways that optimize responsiveness to subsequent neuromodulation [138].
Network Stabilization: While neuromodulation may rapidly alter network dynamics, pharmacotherapy could help stabilize these changes over time [137].
Multi-Target Engagement: Combined approaches can simultaneously address abnormalities in multiple neurotransmitter systems and distributed networks [138].
Diagram 1: Theoretical framework of pharmacotherapy-neuromodulation synergy
Biomarker-Guided Treatment Selection
A critical aspect of combining pharmacotherapy with neuromodulation is the use of circuit-based biomarkers to guide treatment selection and targeting. As research identifies distinct biotypes of depression based on network dysfunction, treatments can be increasingly personalized. For example, individuals with the cognitive biotype of depression (characterized by dLPFC-dACC hypoconnectivity and cognitive control deficits) may be ideal candidates for combined approaches that target this specific circuit [71]. Functional neuroimaging, electrophysiology, and behavioral measures can identify the specific network abnormalities present in each individual, guiding both the selection of pharmacologic agents and the targeting of neuromodulation [137] [139].
Advanced neuroimaging techniques including resting-state fMRI, diffusion MRI, and MEG provide methods for identifying connectivity biomarkers that predict treatment response [137] [139]. For instance, reduced beta-band functional connectivity in frontoparietal networks during response inhibition tasks predicts poor response to serotonergic antidepressants [139]. Similarly, task-based dLPFC-dACC connectivity identifies individuals likely to show connectivity normalization and clinical improvement with TMS [71]. These biomarkers could guide not only the initial selection of combined therapy but also the ongoing optimization of parameters based on circuit-level changes.
Experimental Evidence for Combined Approaches
Clinical Protocols and Outcomes
Several experimental approaches have investigated the combination of pharmacotherapy and neuromodulation. The SWIPED clinical trial is examining the enhancement of sleep slow-wave activity as a treatment for refractory depression using both pharmacologic (propofol) and neuromodulation approaches [5]. This trial builds on the understanding that slow waves are a key marker of brain function and health associated with depression, and that their enhancement correlates with improvements in mood and cognition [5]. The research team is developing personalized dosing strategies that account for individual differences in brain dynamics, with the goal of identifying optimal dosing regimens that achieve the 'sweet spot' of slow-wave expression for each patient [5].
Research on anesthetic-enhanced depression treatment provides insights into potential combination approaches. Studies using propofol and other general anesthetics suggest that carefully controlled modulation of brain electrophysiology can have antidepressant effects [5]. Technical challenges include determining specific dosage requirements that vary between individuals and the difficulty of manipulating electrophysiological biomarkers [5]. Personalized brain modeling approaches are being developed to predict individual responses to these interventions and optimize dosing strategies [5].
Cognitive Biotype-Targeted Intervention
The B-SMART-fMRI trial provides a compelling example of biomarker-guided neuromodulation that could be enhanced with pharmacologic approaches [71]. In this study, researchers stratified patients with treatment-resistant depression based on baseline dLPFC-dACC connectivity during a cognitive control task [71]. Those with hypoconnectivity (cognitive biotype +) received TMS to the left dLPFC and showed significant improvement in both circuit connectivity and cognitive performance, while those with intact connectivity did not [71]. This precision approach demonstrates how circuit biomarkers can identify individuals most likely to benefit from targeted intervention.
A logical extension of this research would combine pharmacologic enhancement of neuroplasticity with circuit-targeted neuromodulation for the cognitive biotype. Medications that enhance dopamine or norepinephrine signaling—neurotransmitters involved in cognitive control—could potentially amplify the effects of dLPFC-targeted stimulation on the cognitive control circuit [138]. The timing of medication administration relative to stimulation sessions could be optimized to coincide with peak drug concentrations during neuromodulation, potentially enhancing plasticity mechanisms.
Diagram 2: Biomarker-guided treatment approach for depression biotypes
Methodological Considerations and Research Tools
Experimental Protocols for Combined Modality Research
Research on combined pharmacotherapy and neuromodulation requires sophisticated protocols that account for the temporal dynamics of both interventions. Below is an example protocol for investigating the combination of neuroplasticity-enhancing medication with targeted neuromodulation:
Phase 1: Baseline Characterization (Week 1)
- Clinical assessment: MADRS, HAMD-17, cognitive battery
- Neuroimaging: Resting-state fMRI, dLPFC-dACC connectivity during Go/No-Go task
- Neurophysiology: TMS motor threshold, EEG resting-state and evoked potentials
- Biomarker analysis: Stratification by cognitive biotype status
Phase 2: Pharmacologic Lead-In (Weeks 2-3)
- Initiation of neuroplasticity-enhancing medication (e.g., SSRI, dopaminergic agent)
- Dose titration based on tolerability
- Repeat neurophysiology assessment at end of phase
Phase 3: Combined Intervention (Weeks 4-8)
- Continued pharmacotherapy at stable dose
- Neuromodulation sessions (e.g., dLPFC-targeted TMS) 5 times per week
- Medication timing optimized relative to stimulation sessions
- Clinical safety monitoring and adverse event documentation
Phase 4: Outcome Assessment (Week 9)
- Repeat clinical, neuroimaging, and neurophysiology assessments
- Comparison to baseline to evaluate circuit-level changes
- Long-term follow-up at 3 and 6 months
This protocol allows for investigation of how pharmacotherapy influences the effects of neuromodulation on both clinical outcomes and circuit-level biomarkers.
The Researcher's Toolkit: Essential Methodologies
Table 3: Essential Research Methods for Combined Modality Studies
| Method Category | Specific Techniques | Key Applications | Technical Considerations |
|---|---|---|---|
| Neuroimaging | Resting-state fMRI, Diffusion MRI, Task-based fMRI | Network identification, connectivity biomarkers, target localization | fMRI-MEG co-registration enhances temporal-spatial resolution |
| Electrophysiology | MEG, EEG, TMS-EMG | Functional connectivity, oscillatory dynamics, cortical excitability | Beta-band (15-30 Hz) oscillations important for cognitive control |
| Neuromodulation | rTMS, TBS, tDCS, FUS | Circuit modulation, causal intervention | dLPFC common target; individualized targeting improves outcomes |
| Behavioral Assessment | WebNeuro, Go/No-Go, Cognitive Control Battery | Cognitive biotyping, treatment response monitoring | Go/No-Go task engages inhibitory control network |
| Computational Modeling | Personalized brain models, Dose-response prediction | Treatment optimization, individual parameter selection | Data-driven models account for person-to-person differences |
Future Directions and Implementation Challenges
Personalized Medicine Approaches
The future of combined pharmacotherapy and neuromodulation lies in increasingly personalized approaches that account for individual differences in circuit dysfunction, neurochemistry, and genetic profile. Personalized brain modeling of drug effects represents a promising direction, with researchers developing data-driven modeling methods to identify how the brain responds to interventions in a manner sensitive to person-to-person differences [5]. These models could eventually predict optimal dosing regimens for both medications and neuromodulation parameters based on an individual's age, genetics, health conditions, brain dynamics, and neural circuits [5].
Implementation of personalized combined therapy requires addressing several methodological challenges. Target engagement biomarkers are needed to verify that both pharmacologic and neuromodulation components are effectively engaging their intended targets [138]. For pharmacotherapy, this might involve receptor occupancy imaging or CSF neurotransmitter measurements; for neuromodulation, electric field modeling or immediate early gene expression could serve this purpose [137]. The timing and sequence of interventions must be optimized—whether medications should be initiated before, concurrently with, or after neuromodulation [5]. Finally, adaptive protocols that modify treatment parameters based on ongoing assessment of circuit changes could maximize therapeutic outcomes.
Technical and Methodological Innovations
Advancements in several technical domains will facilitate the development of combined modality approaches:
Closed-Loop Neuromodulation: Systems that adjust stimulation parameters in real-time based on neural activity could enhance precision and effectiveness [142]. These systems might eventually incorporate pharmacodynamic information to optimize combined treatment.
Focused Ultrasound Stimulation: This emerging technique offers improved spatial precision and the ability to target deeper brain structures compared to TMS or tDCS [137]. Its combination with pharmacotherapy represents a promising frontier.
Network-Based Targeting: Instead of targeting individual brain regions, future approaches may target specific networks through individualized connectivity maps [137]. This could be particularly powerful when combined with medications that modulate those same networks.
Multimodal Biomarker Integration: Combining information from neuroimaging, electrophysiology, genetics, and behavioral measures will enable more accurate prediction of treatment response and guidance of therapeutic parameters [137] [139].
The integration of pharmacotherapy with neuromodulation represents a promising approach for addressing the complex network dysfunction underlying depression, particularly for individuals who have not responded to conventional treatments. This combined modality approach leverages complementary mechanisms: pharmacotherapy creates a neurochemical environment that may enhance neuroplasticity and potentially prime the brain for neuromodulation, while neuromodulation provides targeted regulation of specific dysfunctional circuits identified through neuroimaging biomarkers. The emerging paradigm of circuit-based psychiatry enables increasingly personalized interventions guided by individual patterns of network dysfunction. As research continues to elucidate the mechanisms of synergy between these modalities and develop biomarkers for target engagement and treatment response, combined pharmacotherapy and neuromodulation has the potential to transform care for patients with treatment-resistant depression.
Major depressive disorder (MDD) represents a significant global mental health challenge characterized by high clinical heterogeneity and variable treatment outcomes. Conventional explanations of depression as a simple chemical imbalance and antidepressant mechanisms as primarily enhancing monoaminergic neurotransmission are now considered simplistic and incomplete [143]. The emerging paradigm reconceptualizes depression as a disorder of brain circuit wiring, where pathological stress and depression are associated with specific structural changes in key brain regions: loss of dendritic spines, shrinkage of dendritic trees, and synaptic loss in the hippocampus and prefrontal cortex, coupled with increased dendritic arborization in the amygdala [143]. This shift from chemical to circuit-based models provides a more comprehensive framework for understanding both depression pathophysiology and therapeutic mechanisms.
Circuit-based therapeutics represent a transformative approach that targets specific neural networks rather than relying solely on systemic neurotransmitter modulation. This framework has been catalyzed by the growth of brain stimulation treatments such as transcranial magnetic stimulation (TMS), deep brain stimulation (DBS), and focused ultrasound (FUS) [144]. Each technique can effectively treat different neuropsychiatric disorders, but success depends critically on identifying the correct circuit target. The historical example of frontal lobotomy—developed from a single chimpanzee experiment with limited target knowledge—stands in stark contrast to modern TMS for depression, which leveraged decades of lesion and neuroimaging studies identifying the left dorsolateral prefrontal cortex (DLPFC) as a therapeutic target [144]. This evolution from crude anatomical intervention to precise circuit modulation exemplifies the progress and potential of circuit-based approaches.
Fundamental Neuroplasticity Mechanisms: From Animal Models to Human Applications
Stress-Induced Neurohistological Changes: Insights from Animal Models
Animal studies have provided fundamental insights into the neurohistological changes underlying depression, based on the well-established relationship between stress and depression development. Research indicates that pathological stress results in an aberrant neuroplasticity response characterized by abnormally increased activity in the amygdala and impaired functioning of the hippocampus, prefrontal cortex, and downstream structures [143]. These changes directly explain most clinical symptoms of depression and provide targets for therapeutic intervention.
Key brain structures affected by stress in animal models include:
- Hippocampus: Stress causes dendritic atrophy, loss of dendritic spines, and reduced neurogenesis. The hippocampus is rich in glucocorticoid receptors, and pathological cortisol levels lead to dendritic shrinkage, synaptic loss, and in extreme cases, apoptosis [143].
- Prefrontal Cortex (PFC): Similar stress-induced changes occur, including dendritic simplification and loss of glial cells. These structural impairments correlate with cognitive deficits characteristic of depression [143].
- Amygdala: In contrast to the hippocampus and PFC, the amygdala exhibits increased dendritic arborization and synaptogenesis in response to chronic stress, potentially underlying the heightened anxiety and negative emotional processing in depression [143].
The time course of these structural changes parallels the development and progression of depressive symptoms, providing a biological basis for the disorder and a target mechanism for treatments.
Neuroplasticity Hypothesis of Antidepressant Action
The neuroplasticity hypothesis of antidepressant action proposes that these medications work by protecting against and reversing the neurohistological changes induced by stress [143]. This represents a fundamental shift from the chemical imbalance model to a hardwiring perspective—depression as a disorder of brain circuitry, with antidepressants facilitating circuit repair.
This hypothesis explains several clinical observations:
- Delayed Therapeutic Onset: While pharmacological effects on monoamines occur within hours, therapeutic benefits emerge over weeks, paralleling the time required for structural neural changes [143].
- Prophylactic Efficacy: The ability of antidepressants to prevent depression recurrence aligns with their role in maintaining circuit integrity [143].
- Treatment Mechanism: Antidepressants restore functional neuroplasticity in stressed organisms, presumably facilitating re-adaptation through learning and memory mechanisms [143].
Table 1: Stress-Induced Neural Changes and Antidepressant Effects in Key Brain Regions
| Brain Region | Stress-Induced Structural Changes | Functional Consequences | Antidepressant Effects |
|---|---|---|---|
| Hippocampus | Dendritic atrophy, spine loss, reduced neurogenesis, neuronal apoptosis (severe cases) | Impaired learning and memory, reduced contextual regulation of stress | Reverses dendritic atrophy, promotes neurogenesis, protects against apoptosis |
| Prefrontal Cortex | Dendritic simplification, spine loss, reduced glial cells | Impaired executive function, reduced cognitive control | Reverses dendritic simplification, enhances synaptic connectivity |
| Amygdala | Increased dendritic arborization, enhanced synaptogenesis | Heightened anxiety, increased negative emotional processing | Attenuates stress-induced growth, normalizes emotional response |
| Cognitive Control Circuit | Dysregulated connectivity, inefficient processing | Impaired planning, troubleshooting, executive function | Enhances circuit efficiency, improves cognitive performance |
Methodological Framework for Circuit Target Identification
Approaches to Circuit Identification and Validation
Identifying the correct neural circuits for therapeutic targeting requires convergent methodological approaches that bridge causal inference with correlational observations:
- Convergent Network-Level Neuroimaging Analysis: Early functional neuroimaging faced reproducibility challenges, but advanced techniques like coordinate network mapping can identify common connectivity patterns across heterogeneous findings. For example, a meta-analysis of 57 neuroimaging studies found no consistent regional abnormality in depression but identified a common brain network through connectivity analysis [144].
- Retrospective Optimization Based on Stimulation Sites: Natural variability in clinical TMS coil placement or DBS electrode location creates incidental experiments. Analyzing outcomes by stimulation site has revealed that effective targets are defined by their connectivity profiles rather than precise anatomical coordinates. For depression, the most effective TMS sites are negatively connected to a network with a peak in the subgenual cingulate, while the most effective DBS sites are positively connected to the same network [144].
- Lesion Network Mapping: Building on historical successes where effective stimulation targets were inspired by lesion studies (e.g., DLPFC TMS for depression), this approach identifies circuits causally linked to symptoms. When lesions causing the same symptom don't localize to a common region, they often map to a common network [144].
Translational Experimental Workflows
The translation from animal models to human applications requires systematic workflows that integrate multiple data modalities and validation steps. The following diagram illustrates a comprehensive translational framework for circuit-based therapeutic development:
Diagram 1: Translational workflow for circuit-based therapeutics development showing progression from basic research to clinical application.
Research Reagent Solutions for Circuit Neuroscience
Table 2: Essential Research Tools and Methodologies in Circuit-Based Therapeutics
| Research Tool/Methodology | Primary Function | Translational Application |
|---|---|---|
| Animal Stress Models (Chronic restraint, social defeat) | Induce depression-relevant neural and behavioral changes | Study neurohistological changes and test potential interventions [143] |
| Tractography | Map white matter pathways in individual patients | Guide surgical targeting for DBS electrodes [145] |
| Functional MRI (fMRI) | Measure brain activity and functional connectivity | Identify circuit correlates of symptoms and treatment response [144] [146] |
| Lesion Network Mapping | Identify brain networks causally linked to symptoms | Derive therapeutic targets for neuromodulation [144] |
| Electroencephalography (EEG) Microstate Analysis | Assess large-scale network dynamics with high temporal resolution | Monitor treatment effects on brain network dynamics [147] |
| Local Field Potential (LFP) Recording | Measure localized neural activity from implanted electrodes | Understand local circuit effects of DBS and identify biomarkers [147] |
| Graph Neural Networks (GNNs) | Model complex topological structures in brain connectivity data | Predict treatment response from neuroimaging and clinical features [4] |
Circuit-Based Biotypes and Treatment Prediction
Defining Circuit-Based Depression Biotypes
The high clinical heterogeneity of depression has motivated efforts to define neurobiologically distinct subtypes, or biotypes, based on circuit dysfunction patterns. Research has identified six biotypes of depression based on distinct patterns of brain activity, with approximately one-quarter of depressed individuals showing dysfunction in cognitive control circuits [146]. These biotypes reflect different combinations of circuit abnormalities and may predict differential treatment response.
One clinically relevant biotype involves co-occurring depression and obesity, which often indicates specific dysfunction in the cognitive control circuit [146]. Patients with this biotype respond poorly to conventional antidepressants (approximately 17% response rate) but show significantly better outcomes with targeted cognitive behavioral approaches [146]. This demonstrates the clinical potential of circuit-based stratification to guide treatment selection.
Predictive Modeling of Treatment Response
Advanced computational approaches are being developed to predict individual treatment response based on circuit features. A hierarchical local-global imaging and clinical feature fusion graph neural network model achieved 76.21% accuracy (AUC=0.78) in predicting remission to selective serotonin reuptake inhibitors (SSRIs) [4]. Key contributing brain regions included the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus [4].
For brain stimulation treatments, early response patterns may predict long-term outcomes. In rTMS treatment, early improvements within 5-10 treatments significantly predict final response, potentially allowing for early treatment adaptation [148]. Similarly, in DBS for treatment-resistant depression, specific changes in EEG microstate dynamics—particularly reduced transitions between microstates C and D—correlated with clinical improvement [147].
Translational Successes in Circuit-Based Modalities
Deep Brain Stimulation (DBS)
DBS represents the most invasive yet potentially transformative circuit-based intervention for treatment-resistant depression (TRD). Recent successes highlight the importance of target selection based on circuit principles:
- Medial Forebrain Bundle (MFB) DBS: Targeting the superolateral branch of the MFB, a white matter pathway connecting the ventral tegmental area to the prefrontal cortex, has shown sustained efficacy. In one trial, over half of patients showed a 47% reduction in depression scores within two weeks, with benefits maintained for up to five years in some cases [145].
- BNST-NAc Circuit DBS: Combined targeting of the bed nucleus of the stria terminalis and nucleus accumbens modulates large-scale network dynamics, as measured by EEG microstates. A randomized, double-blind, crossover trial demonstrated that therapeutic DBS increased coverage and occurrence of specific microstates, with changes in transition probabilities correlating with symptom improvement [147].
The following diagram illustrates the experimental protocol for establishing clinical efficacy of DBS in depression:
Diagram 2: Experimental protocol for DBS clinical trials in treatment-resistant depression incorporating multimodal assessment.
Transcranial Magnetic Stimulation (TMS)
TMS represents a less invasive circuit-based approach with demonstrated efficacy for treatment-resistant depression:
- Targeting Approaches: The most effective TMS sites for depression are negatively connected to the subgenual cingulate network [144]. Targeting based on this connectivity profile improves outcomes compared to standard anatomical targeting.
- Treatment Response: A large study of 708 patients treated with TMS demonstrated that 54% exhibited clinical response (≥50% improvement) when assessed with multiple depression rating scales [148]. Early improvement within the first week of treatment predicted final response, potentially enabling early treatment adaptation.
- Precision Approaches: "Precision TMS" models incorporating weekly psychiatric assessment and multiple measurement scales demonstrate higher fidelity in detecting treatment benefits [148].
Psychological Therapies and Circuit Engagement
Evidence demonstrates that psychological interventions engage specific neural circuits in predictable ways:
- Cognitive Behavioral Therapy (CBT): Problem-solving therapy, a form of CBT, produces specific neural changes in the cognitive control circuit. In patients with depression and obesity, therapy responders showed increased neural efficiency in cognitive control circuits, requiring fewer resources for the same behavioral performance [146].
- Distinct Neural Mechanisms: Quantitative synthesis of meta-analyses reveals that psychotherapy and antidepressants engage distinct neural systems. Psychotherapy evokes changes primarily in the medial prefrontal cortex, while antidepressants modulate amygdala activity [41]. Both treatments converge on the brain's affect network but through different proximal mechanisms.
Table 3: Comparative Mechanisms of Circuit-Targeting Therapeutic Modalities
| Therapeutic Modality | Primary Circuit Targets | Mechanism of Action | Treatment Response Timeline |
|---|---|---|---|
| SSRI Antidepressants | Amygdala, prefrontal-limbic connections | Modulate subcortical affect processing, promote neuroplasticity | Delayed onset (weeks), 36-48% remission rates [4] [143] |
| Cognitive Behavioral Therapy | Cognitive control circuit, medial PFC | Enhance cognitive control of affect, improve circuit efficiency | Early changes (2 months), sustained benefit [146] |
| Transcranial Magnetic Stimulation | DLPFC connected to subgenual cingulate | Modulate cortical control over limbic activity | Early response (1 week), 54% response rate [148] |
| Deep Brain Stimulation | MFB, BNST-NAc, SCG, VC/VS | Direct modulation of reward and affect circuits | Rapid improvement (2 weeks), sustained years [147] [145] |
Current Challenges and Future Directions
Translational Gaps and Limitations
Despite promising advances, significant challenges remain in translating circuit-based approaches to routine clinical practice:
- Causality Gap: Neuroimaging correlates of symptoms do not necessarily translate into effective treatment targets. Some correlates may be epiphenomenal, spurious, or compensatory, and targeting them may be ineffective or even counterproductive [144].
- Individual Variability: Circuit dysfunction patterns vary substantially among individuals with the same diagnosis, requiring personalized target identification approaches [99] [149].
- Technical Limitations: Current neuroimaging and neuromodulation technologies have resolution and precision constraints that limit circuit-specific targeting and engagement.
- Methodological Complexity: Integrating multiple data modalities (imaging, electrophysiology, clinical features) requires advanced analytical approaches and validation in large samples.
Framework for Circuit-Based Treatment Selection
A three-phase framework has been proposed for developing and implementing circuit-based therapeutics:
- Circuit Identification: Using convergent approaches including neuroimaging correlates, retrospective optimization of existing stimulation sites, and lesion network mapping [144].
- Target Optimization: Personalizing targets using individualized neuroimaging, physiological monitoring, and brain state engagement through pharmacological or psychological interventions [144].
- Modality Selection: Choosing specific stimulation modalities or combinations based on their relative advantages and tradeoffs for engaging the target circuit [144].
This framework emphasizes that effective circuit-based therapeutics require not only identifying the right target but also selecting the appropriate modality and personalizing parameters based on individual circuit characteristics.
Future Outlook
The future of circuit-based therapeutics lies in advancing along several key frontiers:
- Standardized Circuit Assessment: Developing standardized, reproducible approaches for quantifying brain circuit function at an individual level to facilitate clinical translation [149].
- Closed-Loop Systems: Integrating neural sensing with stimulation to create adaptive systems that modulate circuit activity in response to real-time neural signals.
- Multimodal Biomarkers: Combining imaging, electrophysiological, and clinical features to develop comprehensive predictors of treatment response.
- Circuit-Based Nosology: Refining diagnostic systems based on circuit dysfunction patterns rather than symptom clusters alone.
As these advances mature, circuit-based approaches hold the potential to transform depression treatment from the current trial-and-error paradigm to a precision medicine framework where interventions are selected based on each individual's specific circuit dysfunction pattern.
Conclusion
The investigation of depression has fundamentally shifted from a neurochemical imbalance to a dysfunction within specific, large-scale neural circuits. This circuit-based framework provides a powerful, multi-faceted understanding of the disorder's heterogeneity, linking distinct pathophysiological mechanisms—such as default mode network hyperconnectivity in rumination or prefrontal-amygdala hyperactivity in anxiety—to specific clinical symptoms. The limitations of traditional monoaminergic antidepressants underscore the necessity for this new paradigm. The emergence of advanced tools for circuit dissection and the clinical success of rapid-acting, plasticity-promoting agents like ketamine validate the therapeutic potential of directly targeting these neural pathways. The future of antidepressant development lies in precision psychiatry: utilizing circuit-based biomarkers and biotypes to stratify patients and deploy a growing arsenal of targeted pharmacological and neuromodulation therapies, ultimately moving beyond a one-size-fits-all approach to deliver more effective, personalized, and rapid relief.
References
- 1. Understanding the pathophysiology of depression: From ... [https://www.sciencedirect.com/science/article/abs/pii/S0166432817318521]
- 2. Major depressive disorder: hypothesis, mechanism ... [https://www.nature.com/articles/s41392-024-01738-y]
- 3. Monoamine Neurotransmitters Control Basic Emotions and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9611768/]
- 4. Predicting antidepressant response via local-global graph ... [https://www.nature.com/articles/s41746-025-01912-8]
- 5. Personalized brain modeling of anesthetic effects to predict ... [https://source.washu.edu/2025/09/personalized-brain-modeling-of-anesthetic-effects-to-predict-antidepressant-response/]
- 6. Chronic stress and brain plasticity: mechanisms underlying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4684432/]
- 7. Neuronal correlates of depression - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4709015/]
- 8. A Framework for Quantitative Modeling of Neural Circuits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4341569/]
- 9. Rewiring an olfactory circuit by altering cell-surface ... [https://www.nature.com/articles/s41586-025-09769-3]
- 10. Adherence to evidence-based treatment guidelines for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392555/]
- 11. Therapeutic Guidelines for the Self-Management of Major ... [https://www.i-jmr.org/2025/1/e63959]
- 12. Molecular pathways of major depressive disorder converge ... [https://www.nature.com/articles/s41380-022-01806-1]
- 13. Personalized brain circuit scores identify clinically distinct ... [https://www.nature.com/articles/s41591-024-03057-9]
- 14. Mechanisms underlying the antidepressant response and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4073308/]
- 15. Molecular mechanisms of rapid-acting antidepressants [https://www.sciencedirect.com/science/article/pii/S1043661823001937]
- 16. Quantitative Identification of Major Depression Based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7118554/]
- 17. An objective quantitative diagnosis of depression using a ... [https://www.sciencedirect.com/science/article/pii/S266638992400240X]
- 18. The structural and functional connectivity of the amygdala [https://pmc.ncbi.nlm.nih.gov/articles/PMC3119771/]
- 19. Functional connectivity between the amygdala and ... [https://www.nature.com/articles/s41398-023-02625-w]
- 20. Amygdala-cortical connectivity: Associations with anxiety ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5096647/]
- 21. Dynamic causal modeling of the neural network [https://www.nature.com/articles/s41398-025-03480-7]
- 22. Amygdala hyper-connectivity in a mouse model of ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/29463821/]
- 23. Brain changes associated with depression treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410565/]
- 24. The mechanistic basis for the rapid antidepressant-like ... [https://www.sciencedirect.com/science/article/pii/S0278584623001963]
- 25. Ventral hippocampus to nucleus accumbens shell circuit ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002722]
- 26. Ventral hippocampus to nucleus accumbens shell circuit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11761569/]
- 27. AKT/mTOR/BDNF pathway mediates the antidepressant-like ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605360/]
- 28. Understanding the neural code of stress to control anhedonia [https://www.nature.com/articles/s41586-024-08241-y]
- 29. Increased brain nucleus accumbens functional connectivity ... [https://www.sciencedirect.com/science/article/abs/pii/S002839082300388X]
- 30. Quantitative and qualitative electroencephalography in the ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1624434/full]
- 31. Functional Connectivity of the Nucleus Accumbens and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9403857/]
- 32. Depressive Rumination , the Default - Mode , and the Dark... Network [https://pmc.ncbi.nlm.nih.gov/articles/PMC4524294/]
- 33. Resting-state functional connectivity of the fronto-limbic ... [https://pubmed.ncbi.nlm.nih.gov/41224014/]
- 34. Instability of default connectivity in major depression... mode network [https://www.nature.com/articles/tp201740?error=cookies_not_supported&code=b372b6e4-2f16-47de-8c49-d172b81be87b]
- 35. (PDF) Default Hypoalignment of Function to Structure... Mode Network [https://www.academia.edu/144950936/Default_Mode_Network_Hypoalignment_of_Function_to_Structure_Correlates_with_Depression_and_Rumination]
- 36. Transcranial focused ultrasound targeting the default mode ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1451828/full]
- 37. Mapping the subcortical connectivity of the human default ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8945548/]
- 38. Predicting the treatment outcomes of major depressive ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-025-06728-0]
- 39. Subcortical modulation of the salience network during ... [https://www.nature.com/articles/s41380-025-03135-5]
- 40. Approach- avoidance reinforcement learning as a translational and... [https://elifesciences.org/articles/87720]
- 41. Neural effects of antidepressant medication and psychological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8481936/]
- 42. Habenula - Wikipedia [https://en.wikipedia.org/wiki/Habenula]
- 43. Circuits and functions of the lateral habenula in health and in disease | Nature Reviews Neuroscience [https://www.nature.com/articles/s41583-020-0292-4]
- 44. a systematic review of habenula dysfunction in depression [https://www.nature.com/articles/s41398-024-03199-x]
- 45. A Major Role for the Lateral Habenula in Depressive Illness [https://pmc.ncbi.nlm.nih.gov/articles/PMC6558383/]
- 46. Habenula - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/habenula]
- 47. Estrogen receptor beta in lateral habenula mediates ... [https://www.nature.com/articles/s41380-025-03215-6]
- 48. Lateral habenula astroglia modulate the potentiating ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1592909/full]
- 49. Optogenetics and chemogenetics: key tools for modulating ... [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2025.1516839/full]
- 50. Advances in optogenetic studies of depressive-like behaviors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9492959/]
- 51. Wiring the depressed brain: optogenetic and chemogenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6461994/]
- 52. Optogenetics illuminates pathways of motivation through brain ... [https://med.stanford.edu/news/all-news/2012/11/optogenetics-illuminates-pathways-of-motivation-through-brain-study-shows.html]
- 53. Chemogenetics as a neuromodulatory approach to treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8899595/]
- 54. The DREADDful Hurdles and Opportunities of the Chronic ... [https://www.mdpi.com/2073-4409/11/7/1110]
- 55. Anatomy and Function of Ventral Tegmental Area ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9164627/]
- 56. VTA GABA Neurons at the Interface of Stress and Reward [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2019.00078/full]
- 57. The nucleus accumbens in reward and aversion processing [https://pmc.ncbi.nlm.nih.gov/articles/PMC11341389/]
- 58. Reward and aversion processing by input-defined parallel ... [https://www.nature.com/articles/s41467-022-33843-3]
- 59. Treatment Associated Changes of Functional Connectivity ... [https://www.nature.com/articles/s41598-017-09077-5]
- 60. Article Distinct dynamics and intrinsic properties in ventral ... [https://www.sciencedirect.com/science/article/pii/S2211124724010192]
- 61. The role of BDNF in depression on the basis of its location in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4003317/]
- 62. Activation of nucleus accumbens projections to the ventral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10962329/]
- 63. The Ventral Tegmental Area and Nucleus Accumbens as ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.886704/full]
- 64. The antidepressant effect of nucleus accumbens deep ... [https://www.sciencedirect.com/science/article/pii/S2352289522000674]
- 65. Early treatment-related changes in dorsolateral prefrontal ... [https://www.nature.com/articles/s41398-025-03576-0]
- 66. Hippocampal-Prefrontal Circuit and Disrupted Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4396015/]
- 67. The neural circuits and molecular mechanisms underlying ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1281401/full]
- 68. Modulation of Motor Cortex Excitability Predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5576557/]
- 69. Simultaneous BOLD-fMRI and constant infusion FDG-PET ... [https://www.nature.com/articles/s41597-020-00699-5]
- 70. Interpreting PET and fMRI measures of functional neural ... [https://www.sciencedirect.com/science/article/abs/pii/S0361923000004354]
- 71. A cognitive neural circuit biotype of depression showing ... [https://www.nature.com/articles/s44220-024-00271-9]
- 72. The utility of PET imaging in depression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11070570/]
- 73. PET/MRI for Neurological Applications - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3806202/]
- 74. Convergent functional effects of antidepressants in major ... [https://www.nature.com/articles/s41380-024-02780-6]
- 75. Six distinct types of depression identified in Stanford Medicine ... [https://med.stanford.edu/news/all-news/2024/06/depression-biotypes.html]
- 76. Defining biotypes for depression and anxiety based on large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5702265/]
- 77. Resting-state connectivity biomarkers define ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5624035/]
- 78. New Research Uncovers Six Depression Subtypes [https://www.psychiatrist.com/news/new-research-uncovers-six-depression-subtypes/]
- 79. Early changes in neural circuit function engaged by negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8141669/]
- 80. Frontiers | A Meta-Analysis of Changes in Brain Activity in ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2014.01045/full]
- 81. Treatment‐resistant depression: definition, prevalence, detection, management, and investigational interventions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10503923/]
- 82. Treatment-Resistant Depression (TRD) - definition, clinical ... [https://neurotorium.org/treatment-resistant-depression-trd/]
- 83. Frontiers | Editorial: Treatment resistant depression (TRD): epidemiology, clinic, burden and treatment [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1588902/full]
- 84. Treatment-Resistant Depression: What It Is & Symptoms [https://my.clevelandclinic.org/health/diseases/24991-treatment-resistant-depression]
- 85. The Prevalence and National Burden of Treatment-Resistant Depression and Major Depressive Disorder in the United States - PubMed [https://pubmed.ncbi.nlm.nih.gov/33989464/]
- 86. Rapid Onset of Antidepressant Action: A New Paradigm in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2699451/]
- 87. Early and Delayed Onset of Response to Antidepressants ... [https://www.psychiatrist.com/jcp/early-delayed-onset-response-antidepressants-individual/]
- 88. A Secondary Analysis of Pooled Trial Data [https://pubmed.ncbi.nlm.nih.gov/37294568/]
- 89. Delayed Antidepressant Efficacy and the Desensitization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7340170/]
- 90. Neural circuit markers of familial risk for depression among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10640659/]
- 91. A network correspondence toolbox for quantitative ... [https://www.nature.com/articles/s41467-025-58176-9]
- 92. Neural correlates of peripartum depression: a systematic ... [https://www.nature.com/articles/s41380-025-03227-2]
- 93. Antidepressant-Induced Emotional Blunting: Diagnosis, ... [https://psychopharmacologyinstitute.com/publication/antidepressant-induced-emotional-blunting-diagnosis-mechanisms-and-management-2/]
- 94. Optimizing the diagnosis and treatment of depression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259655/]
- 95. Impact of Antidepressants on Weight Gain - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121960/]
- 96. Antidepressant side effects vary depending on the drug [https://www.npr.org/sections/shots-health-news/2025/10/23/nx-s1-5582787/antidepressant-side-effects-mental-health]
- 97. Antidepressants differ in side-effects such as weight gain, ... [https://www.theguardian.com/science/2025/oct/22/antidepressants-variation-side-effects-weight-gain]
- 98. Prefrontal cortex circuits in depression and anxiety [https://pmc.ncbi.nlm.nih.gov/articles/PMC7442605/]
- 99. Brain Circuit–Derived Biotypes for Treatment Selection in ... [https://www.sciencedirect.com/science/article/pii/S0006322324011752]
- 100. Beyond Monoamines-Novel Targets for Treatment-Resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4761634/]
- 101. A stratified precision medicine trial targeting α 2A [https://www.nature.com/articles/s44220-025-00510-7]
- 102. Association between S-ketamine induced changes in ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1662051/full]
- 103. Esketamine for treatment‑resistant depression: A review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9922941/]
- 104. Glutamatergic System in Depression and Its Role in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047946/]
- 105. Ketamine and rapid antidepressant action: new treatments ... [https://www.nature.com/articles/s41386-023-01629-w]
- 106. Sustained antidepressant effect of ketamine through ... [https://www.nature.com/articles/s41586-023-06624-1]
- 107. Binding Affinity and Mechanisms of Potential ... [https://pubmed.ncbi.nlm.nih.gov/37298821/]
- 108. Pharmacogenetics and the Response to Antidepressants in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472883/]
- 109. Neuroplasticity and depression: Rewiring the brain's networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8383338/]
- 110. Changes in Neural Activities and Neuroplasticity Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455126/]
- 111. The Neurology of mTOR - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4223653/]
- 112. Multifaceted role of mTOR (mammalian target of ... - Nature [https://www.nature.com/articles/s41392-023-01608-z]
- 113. mTOR pathway inhibition alters proliferation as well as ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2024.1298182/full]
- 114. Rewiring of the Serotonin System in Major Depression [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.802581/full]
- 115. Gene expression studies in Depression development and ... [https://www.nature.com/articles/s41398-021-01469-6]
- 116. Brain structural and functional abnormalities in mood disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC2522333/]
- 117. A novel GABAA receptor pharmacology: drugs interacting with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3417481/]
- 118. The emergence of antidepressant drugs targeting GABAA ... [https://www.sciencedirect.com/science/article/pii/S0006295224004647]
- 119. Importance of Target Identification & Validation in Drug ... [https://lifesciences.danaher.com/us/en/library/target-identification-validation-drug-discovery.html]
- 120. Target Validation [https://www.sygnaturediscovery.com/drug-discovery/integrated-drug-discovery/target-validation/]
- 121. Innovative approaches in the treatment-resistant depression [https://pmc.ncbi.nlm.nih.gov/articles/PMC12397026/]
- 122. Deep Brain Stimulation: Overview and Applications in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577781/]
- 123. Neuromodulation Approaches to Depressive Disorders [https://www.psychiatrictimes.com/view/neuromodulation-approaches-to-depressive-disorders]
- 124. A Comprehensive Review of Vagus Nerve Stimulation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8898319/]
- 125. vagus nerve stimulation (VNS), transcranial magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3055429/]
- 126. TMS vs VNS for Depression: Which Treatment Is Better? [https://www.cognitivefxusa.com/blog/tms-vs-vns-for-depression]
- 127. Accelerated TMS - moving quickly into the future of ... [https://www.nature.com/articles/s41386-023-01599-z]
- 128. Comparative efficacy and acceptability of neuromodulation ... [https://www.sciencedirect.com/science/article/pii/S0165032721002445]
- 129. Adenosine signalling drives antidepressant actions of ... [https://www.nature.com/articles/s41586-025-09755-9]
- 130. Convergent mechanisms underlying rapid antidepressant action [https://pmc.ncbi.nlm.nih.gov/articles/PMC6005380/]
- 131. Precision psychiatry in depression treatment: mechanism- ... [https://neurotorium.org/precision-psychiatry-in-depression-treatment-mechanism-based-subtyping-2/]
- 132. Innovations and Prospects in Treating Depression [https://www.psychiatrist.com/pcc/toward-precision-psychiatry-innovations-prospects-treating-depression/]
- 133. Rapid Onset and Sustained Efficacy of Onfasprodil (MIJ821 ... [https://pubmed.ncbi.nlm.nih.gov/40767837/]
- 134. Rapid Onset and Sustained Efficacy of Onfasprodil (MIJ821 ... [https://www.psychiatrist.com/jcp/rapid-onset-sustained-efficacy-onfasprodil-mij821-novel-nr2b-negative-allosteric-modulator-treatment-resistant-depression-phase-2-randomized-proof-of-concept-study/]
- 135. Data Visualization and the Role of UX [https://coreflexsolutions.com/insights/data-visualization-and-the-role-of-ux-bridging-data-with-decisions/]
- 136. Biomarkers Predicting Antidepressant Treatment Response [https://pmc.ncbi.nlm.nih.gov/articles/PMC3774965/]
- 137. Neuromodulation and neural networks in psychiatric disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527521/]
- 138. Restoring consciousness with pharmacologic therapy [https://www.sciencedirect.com/science/article/pii/S1878747924000606]
- 139. Large-scale neural network correlates of response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465451/]
- 140. A systematic review and meta-analysis of neuromodulation ... [https://www.nature.com/articles/s41386-023-01776-0]
- 141. Efficacy and Safety of Neuromodulation Techniques in ... [https://pubmed.ncbi.nlm.nih.gov/41247100/]
- 142. Neuromodulation: Update on current practice and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11103215/]
- 143. How antidepressant drugs act: A primer on neuroplasticity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3025168/]
- 144. The future of brain circuit-targeted therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10700386/]
- 145. Long-Term Success with Deep Brain Stimulation for Treatment ... [https://med.uth.edu/psychiatry/2025/04/07/long-term-success-with-deep-brain-stimulation-for-treatment-resistant-depression/]
- 146. Cognitive behavioral therapy enhances brain circuits to ... [https://med.stanford.edu/news/all-news/2024/09/cognitive-behaviora-therapy-depression.html]
- 147. Therapeutic deep brain stimulation targeting BNST-NAc ... [https://www.nature.com/articles/s41398-025-03669-w]
- 148. Study finds possible early predictor of successful ... [https://www.uclahealth.org/news/release/study-finds-possible-early-predictor-successful-transcranial]
- 149. Brain Circuit-Derived Biotypes for Treatment Selection in ... [https://pubmed.ncbi.nlm.nih.gov/38552866/]