Invasive vs. Non-Invasive Neural Interfaces: A Comparative Analysis for Researchers and Clinicians
This article provides a comprehensive comparative analysis of invasive and non-invasive neural interfaces (NIs), tailored for researchers, scientists, and drug development professionals.
Invasive vs. Non-Invasive Neural Interfaces: A Comparative Analysis for Researchers and Clinicians
Abstract
This article provides a comprehensive comparative analysis of invasive and non-invasive neural interfaces (NIs), tailored for researchers, scientists, and drug development professionals. It explores the fundamental principles, signal characteristics, and technological underpinnings of both approaches. The scope extends to their current methodological applications in clinical practice and research, an examination of the technical and optimization challenges each faces, and a direct, evidence-based comparison of their performance, market trajectories, and validation benchmarks. The goal is to offer a foundational resource for strategic decision-making in neurotechnology research and development.
Core Principles and Signal Foundations of Neural Interfaces
Brain-computer interfaces (BCIs) represent a rapidly evolving neurotechnology that enables direct communication between the brain and external devices [1] [2]. These systems create an alternative communication pathway by decoding neural signals associated with mental states or movement intentions, translating them into commands for controlling computers, prosthetic limbs, or other assistive devices [2]. The field has progressed substantially from early demonstrations in animals to human clinical trials, with potential applications spanning from restoring communication for paralyzed patients to revolutionary human-computer interaction paradigms [1] [3].
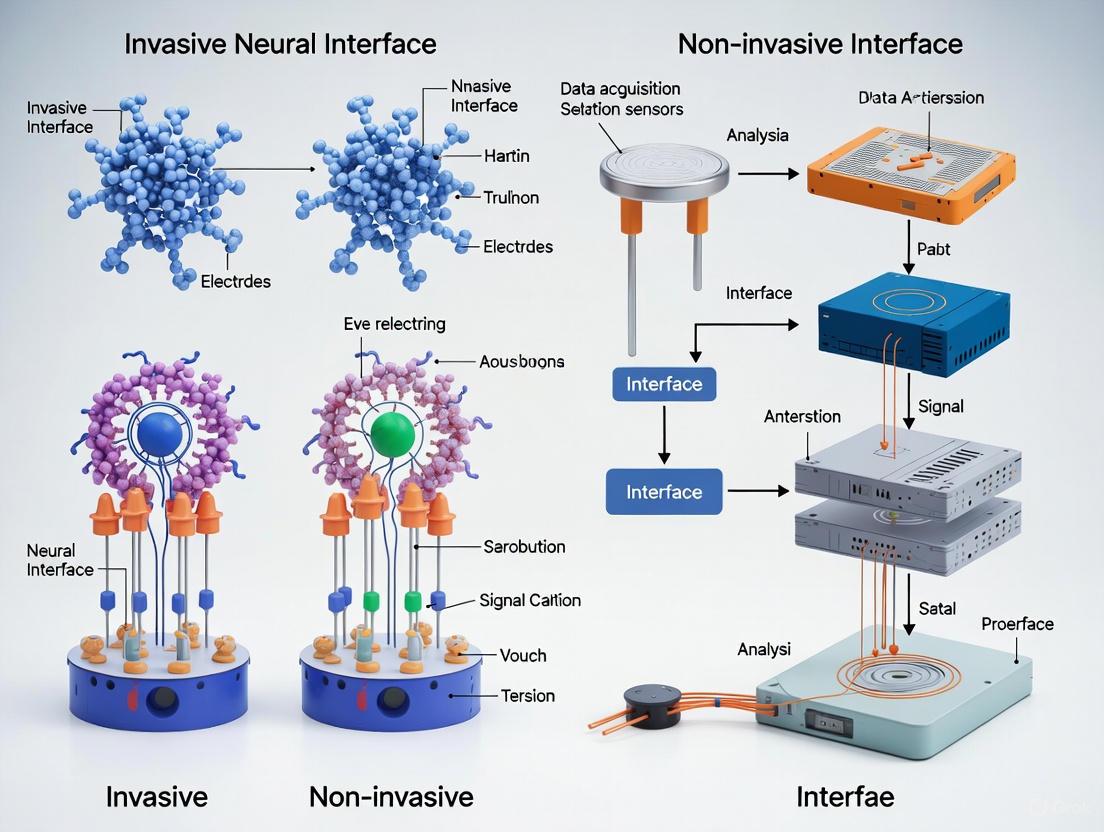
BCI technologies exist along a spectrum of invasiveness, each with distinct trade-offs between signal quality, risk, and clinical applicability [4] [2]. Non-invasive approaches record neural signals from outside the skull, typically using electroencephalography (EEG) or other external sensors [1] [5]. Invasive approaches require surgical implantation of electrodes directly onto or into brain tissue, providing higher-fidelity signals but carrying greater risk [1] [3]. A middle category of minimally invasive technologies has also emerged, including endovascular electrodes and thin-film cortical surfaces, which aim to bridge the gap between signal quality and safety [3] [2]. This review provides a comparative analysis of these approaches, focusing on their performance characteristics, experimental methodologies, and potential research applications.
Technology Classification and Signal Characteristics
Neural interfaces can be categorized based on their level of invasiveness, which directly correlates with their spatial resolution, signal-to-noise ratio, and clinical risk profile [4]. The fundamental distinction lies in whether the recording device requires penetration of the skull and/or neural tissue.
Table 1: Classification of Neural Interface Technologies by Level of Invasiveness
| Category | Technology Examples | Implantation Site | Spatial Resolution | Temporal Resolution | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|---|
| Non-Invasive | EEG [1] [5], fNIRS [4], Wearable MEG [4] | Scalp surface | Low (~1 cm) | High (ms) | Minimal safety risk, Easy application, Suitable for large populations [2] | Low signal-to-noise ratio, Limited spatial resolution, Susceptible to artifacts [1] [6] |
| Minimally Invasive | ECoG [2], Stentrode [2], Layer 7 Cortical Interface [3] | Brain surface or blood vessels | Medium (mm-cm) | High (ms) | Better signal quality than non-invasive, Reduced tissue damage compared to penetrating electrodes [3] [2] | Still requires surgical procedure, Limited long-term stability data |
| Invasive | Utah Array [1] [3], Neuralink [3], Neuropixels [2] | Brain parenchyma | High (μm-mm) | High (ms) | Highest signal quality, Access to single-neuron activity [3] [2] | Significant tissue damage, Scar formation over time, Ethical concerns [1] [3] |
The relationship between these technologies and their recording locations within the neural hierarchy can be visualized as follows:
Performance Comparison: Quantitative Metrics
The performance of neural interfaces is quantitatively evaluated using metrics such as information transfer rate (ITR), classification accuracy, and signal-to-noise ratio. These metrics enable direct comparison across technologies and research groups.
Information Transfer Rates Across Modalities
Information transfer rate (ITR), measured in bits per minute (bpm), provides a standardized measure of communication bandwidth that accounts for both speed and accuracy [1]. This metric allows direct comparison across different BCI technologies and experimental paradigms.
Table 2: Performance Comparison of Neural Interface Technologies
| Technology | Representative Study/System | Task | Information Transfer Rate | Classification Accuracy | Key Applications |
|---|---|---|---|---|---|
| Non-Invasive (EEG) | SSVEP Speller [5] | Character selection | 80.41 bpm (mean) | 75.37% (mean) | Communication, Environmental control [5] |
| Non-Invasive (sEMG) | Wristband Interface [6] | Handwriting | ~20.9 words/minute | >90% | Human-computer interaction, Handwriting decoding [6] |
| Minimally Invasive (ECoG) | WIMAGINE System [2] | Motor control for exoskeleton | N/A | Successful walking restoration | Robotic exoskeletons, Motor restoration [2] |
| Invasive (Utah Array) | BrainGate/Clinical Trials [1] [3] | Robotic arm control, Cursor control | Highly variable | High success in demonstrations | Prosthetic control, Communication for paralysis [1] |
| Invasive (Neuralink) | Neuralink [3] | Neural recording | Higher bandwidth than Utah arrays | High single-neuron resolution | High-density neural recording, Device control [3] |
Signal Characteristics and Resolution Trade-offs
The fundamental trade-offs between invasiveness and signal quality can be visualized through their relative spatial and temporal resolution characteristics:
Experimental Protocols and Methodologies
Non-Invasive BCI Protocols (EEG-based Systems)
Non-invasive BCI research typically employs standardized experimental paradigms to ensure reproducible results. The steady-state visual evoked potential (SSVEP) speller protocol represents a well-established methodology [5]:
Visual Stimulation Protocol: Participants focus attention on characters displayed on a screen that flicker at specific frequencies (typically 10.0-15.4 Hz range) [5]. The flicker period is typically 1.50 seconds followed by a 0.75-second flicker-free interval to reduce visual fatigue [5].
Signal Processing Workflow: EEG signals are processed using filter-bank canonical correlation analysis (CCA) to identify frequency components corresponding to the attended character [5]. This method improves signal-to-noise ratio by optimizing spatial filters for SSVEP detection.
Performance Assessment: Classification accuracy is calculated based on character selection success rate, with information transfer rate derived using the formula: ITR = [log₂N + Plog₂P + (1-P)log₂((1-P)/(N-1))]/T, where N represents number of choices, P represents classification accuracy, and T represents selection time per character [5].
Invasive BCI Protocols (Intracortical Systems)
Invasive BCI methodologies involve surgical implantation followed by signal acquisition and decoding:
Surgical Implantation: Utah arrays or similar multi-electrode arrays are surgically implanted in motor-related areas (primary motor cortex, posterior parietal cortex) [3] [2]. These arrays typically contain up to 100 needle-like electrodes that penetrate the cortical surface [3].
Neural Signal Acquisition: Systems record multi-unit activity (MUA) or single-unit activity from hundreds of recording sites simultaneously [2]. Modern systems like Neuralink contain over a thousand electrodes distributed over polymer threads implanted by specialized surgical robots [3].
Decoder Calibration: Participants perform imagined or attempted movements while neural activity is recorded [1]. Machine learning algorithms (typically linear decoders or neural networks) map neural patterns to movement parameters through closed-loop calibration [1] [2].
Performance Validation: Systems are tested using center-out reaching tasks where participants control robotic arms or computer cursors to acquire targets [1]. Performance is quantified by success rate, completion time, and path efficiency.
The complete experimental workflow for developing and validating neural interfaces follows a systematic process:
Research Reagent Solutions and Essential Materials
Successful neural interface research requires specialized materials and equipment. The following table details key components essential for experimental work in this field.
Table 3: Essential Research Materials for Neural Interface Studies
| Category | Specific Material/Device | Research Function | Key Specifications | Representative Examples |
|---|---|---|---|---|
| Electrode Technologies | Dry EEG Electrodes [4] | Non-invasive neural recording | No gel requirement, Rapid application | Consumer EEG devices |
| Wet EEG Electrodes [4] | High-quality non-invasive recording | Traditional gel-based, Higher signal quality | Research-grade EEG systems | |
| Utah Array [1] [3] | Invasive single-neuron recording | 100+ electrodes, Standardized manufacturing | Blackrock Neurotech [3] | |
| Flexible Thread Electrodes [3] | Minimally invasive recording | 1024+ electrodes, Reduced tissue damage | Neuralink, Precision Layer 7 [3] | |
| Signal Acquisition Systems | EEG Amplifiers [5] | Signal conditioning and digitization | High input impedance, Low noise | Research-grade EEG systems |
| Wireless ECoG Systems [2] | Minimally invasive chronic recording | Implantable, Wireless data transfer | WIMAGINE Device [2] | |
| Neuropixels Probes [2] | High-density neural recording | Thousands of recording sites, CMOS technology | Neuropixels [2] | |
| Decoding Algorithms | Filter-Bank CCA [5] | SSVEP frequency detection | Multi-frequency analysis, Enhanced SNR | SSVEP Speller Systems [5] |
| Deep Learning Networks [6] | sEMG gesture decoding | Cross-user generalization, Real-time processing | sEMG Wristband Decoders [6] | |
| Linear Decoders [1] | Motor parameter extraction | Real-time capability, Robust performance | Robotic Arm Control [1] | |
| Validation Tools | Motion Capture Systems [6] | Movement tracking for ground truth | High spatial precision, Multi-camera | sEMG validation [6] |
| Robotic Manipulanda [1] | Device performance assessment | Programmable targets, Precision control | Center-Out Task Equipment [1] |
The spectrum from non-invasive to invasive neural interfaces presents researchers with fundamental trade-offs between signal quality, clinical risk, and practical implementation. Non-invasive technologies offer safer, more accessible options but with limited information bandwidth, while invasive approaches provide superior signal quality at the cost of surgical risk and potential tissue damage [1] [2]. Emerging minimally invasive technologies aim to bridge this gap, showing promising results in recent clinical studies [3] [2].
Future development in neural interfaces will likely focus on improving information transfer rates through advanced signal processing and electrode design [1] [4]. For invasive systems, key challenges include improving long-term stability and reducing tissue damage [3]. For non-invasive systems, priority areas include enhancing signal-to-noise ratio and developing more intuitive control paradigms [6] [5]. The field continues to evolve rapidly, with both approaches finding complementary roles in the expanding landscape of human-machine interaction and clinical neurotechnology.
The advancement of neuroscience and neurotechnology hinges on the precise acquisition and interpretation of neural signals. Researchers and clinicians have at their disposal a spectrum of tools, each with distinct mechanisms for measuring brain activity. These techniques can be broadly categorized as non-invasive, such as electroencephalography (EEG) and functional near-infrared spectroscopy (fNIRS), which record from outside the skull, and invasive, such as electrocorticography (ECoG) and intracortical signals, which require surgical implantation to record from the brain's surface or from within its tissue. The choice between these methods involves critical trade-offs concerning signal origin, spatial and temporal resolution, invasiveness, and suitability for specific applications. This guide provides a comparative analysis of these four pivotal signal types, offering a structured overview of their acquisition, origins, and experimental use to inform research and development in academia and industry.
Fundamental Principles and Signal Origins
Understanding the biological and physical principles behind each signal is the first step in selecting the appropriate tool.
EEG (Electroencephalography): EEG measures the electrical activity of populations of neurons, primarily the postsynaptic potentials of cortical pyramidal cells. When these neurons fire synchronously, their summed electrical currents create potential differences that can be detected on the scalp [7] [8]. The signal is characterized by voltage fluctuations in the microvolt (µV) range.
fNIRS (functional Near-Infrared Spectroscopy): fNIRS is an optical technique that measures the hemodynamic response, or changes in blood oxygenation, coupled with neural activity. It uses near-infrared light to detect concentration changes in oxygenated (HbO) and deoxygenated hemoglobin (HbR) in the cortical vasculature [9] [7]. This provides an indirect measure of brain activity.
ECoG (Electrocorticography): ECoG records electrical signals from the surface of the cerebral cortex (electrocorticography). Like EEG, it captures population-level electrical activity, but without the signal attenuation and spatial blurring caused by the skull and scalp [10]. This results in signals with a higher amplitude and broader frequency bandwidth than EEG.
Intracortical Signals: These signals are acquired via microelectrodes implanted directly into the brain tissue. They can capture two primary types of signals: Local Field Potentials (LFPs), which are low-frequency signals representing the summed synaptic activity of a local neuronal population, and Action Potentials (APs or "spikes"), which are high-frequency signals from the firing of individual neurons near the electrode tip [10] [8].
The diagram below illustrates the anatomical origins of these different signals.
Figure 1: A cross-sectional view of the head showing the anatomical recording locations for EEG, fNIRS, ECoG, and intracortical signals.
Technical Specifications and Comparative Analysis
The fundamental differences in signal origin directly translate into varied technical performance profiles. The table below provides a quantitative and qualitative comparison of the four modalities.
Table 1: Comprehensive comparison of neural signal acquisition technologies.
| Feature | EEG | fNIRS | ECoG | Intracortical |
|---|---|---|---|---|
| Signal Origin | Postsynaptic potentials (Pyramidal neurons) [8] | Hemodynamic response (HbO/HbR) [7] | Cortical surface potentials [10] | Local Field Potentials (LFPs) & Action Potentials (Spikes) [10] |
| Spatial Resolution | Low (Centimeter-level) [7] | Moderate (Better than EEG) [7] | Medium (1-10 mm) [10] | High (50-100 μm) [10] |
| Temporal Resolution | High (Milliseconds) [7] | Low (Seconds) [7] | High (Milliseconds) | Very High (Milliseconds to kHz) [10] |
| Depth of Measurement | Cortical surface [7] | Outer cortex (1-2.5 cm) [7] | Cortical surface | Intracortical layers |
| Invasiveness | Non-invasive | Non-invasive | Invasive (Craniotomy, subdural) [10] | Highly Invasive (Penetrating tissue) [10] |
| Key Advantage(s) | Excellent temporal resolution, portable, low cost [7] | Good spatial resolution, motion-tolerant [7] | High signal quality, broad frequency range [10] | Highest spatial & temporal resolution, single-neuron access [10] |
| Primary Limitation(s) | Poor spatial resolution, sensitive to artifacts [7] | Low temporal resolution, indirect measure [7] | Requires craniotomy, limited spatial specificity [10] | Tissue response, signal stability over time [10] |
| Typical Applications | ERP studies, sleep research, brain-state monitoring [7] | Naturalistic studies, child development, rehabilitation [7] [11] | Surgical mapping, basic motor control [10] | Fine dexterous control, complex communication [10] |
Experimental Protocols and Methodologies
Robust experimental design is critical for acquiring high-quality data. Below are detailed protocols for a classic motor task across the different modalities, highlighting key methodological steps.
Protocol for a Motor Execution Task
A common paradigm for investigating motor system function involves simple motor acts. The following workflow outlines a typical experiment.
Figure 2: A generalized experimental workflow for a motor execution study, common to all neuroimaging modalities.
Step 1: Participant Preparation
- EEG/ECoG: Secure the electrode cap or subdural grid on the participant's head. For EEG, apply conductive gel to lower impedance. For ECoG, this is done during a surgical procedure [12].
- fNIRS: Position optodes on the scalp over the region of interest (e.g., primary motor cortex) using a head cap, ensuring good skin contact [12] [13].
- Intracortical: This involves the surgical implantation of a microelectrode array (e.g., Utah Array) into the target brain area, typically under general anesthesia [10].
Step 2: Baseline Recording A 2-5 minute resting-state recording is conducted where the participant remains relaxed with eyes open or closed. This baseline is used to contrast against task-induced activity [12].
Step 3: Task Execution & Data Acquisition The participant performs a blocked or event-related paradigm. For example:
- Cue (2s): A visual or auditory cue instructs the participant to prepare.
- Execution (3-5s): The participant repeatedly grasps and moves an object [12].
- Rest (10-15s): The participant remains still, allowing neural/hemodynamic activity to return to baseline. This sequence is repeated for multiple trials (e.g., 30-40 trials). For ECoG and intracortical recordings, this is often performed with patients undergoing monitoring for epilepsy [10].
Step 4: Data Preprocessing
- EEG/ECoG: Filtering (e.g., 0.5-40 Hz for ERPs, up to 200 Hz for higher frequencies), artifact removal (e.g., ocular, muscle), and re-referencing [14] [11].
- fNIRS: Converting raw light intensity to optical density, then to HbO and HbR concentrations using the Modified Beer-Lambert Law. Motion artifact correction is applied [9] [11].
- Intracortical: Filtering spikes (300-5000 Hz) and LFPs (0.1-300 Hz) separately. Spike sorting to isolate single-unit activity [10].
Step 5: Data Analysis & Interpretation
- EEG/ECoG: Time-frequency analysis (e.g., Event-Related Spectral Perturbation) to quantify power changes in specific frequency bands (e.g., mu/beta desynchronization during movement) [12].
- fNIRS: General Linear Modeling (GLM) is used to compare HbO/HbR concentrations during the task blocks against the rest blocks, generating statistical parametric maps of activation [9].
- Intracortical: Analyzing firing rates of individual neurons or LFP power in relation to movement kinematics (e.g., direction, force) [10].
The Scientist's Toolkit: Key Research Reagents and Materials
Successful experimentation relies on specialized hardware and software. The following table details essential components for a multimodal setup.
Table 2: Essential materials and reagents for neural signal acquisition experiments.
| Item Name | Function/Description | Example Use Case |
|---|---|---|
| Integrated EEG-fNIRS Cap | An elastic cap with pre-defined openings and fixtures to hold both EEG electrodes and fNIRS optodes, ensuring co-registration of modalities [14] [12]. | Simultaneously recording electrical and hemodynamic activity during a cognitive-motor task [12]. |
| Conductive Electrode Gel | A gel or paste applied to EEG electrodes to facilitate electrical contact between the scalp and the electrode, reducing impedance. | Essential for obtaining high-quality, low-noise EEG signals. |
| Microelectrode Array (e.g., Utah Array) | A grid of fine, sharp electrodes designed for intracortical implantation to record single-unit activity and LFPs [10]. | Investigating neural tuning properties in primary motor cortex for brain-computer interface control [10]. |
| Subdural Grid/Strip Electrodes | A flexible array of disc electrodes embedded in a silicone sheet, implanted under the dura mater for ECoG recording [10]. | Pre-surgical mapping of eloquent cortical areas (e.g., motor, language) in epilepsy patients. |
| Synchronization Hardware/Software | A system (e.g., TTL pulse generators, shared clock software) to precisely align data streams from different acquisition devices [14]. | Mandatory for temporal alignment of EEG and fNIRS data in a multimodal experiment. |
| Structured Sparse Multiset CCA (ssmCCA) | A data fusion algorithm used to identify correlated components across multimodal datasets (e.g., EEG and fNIRS) [12]. | Pinpointing brain regions where electrical and hemodynamic activity are jointly modulated by a task [12]. |
EEG, fNIRS, ECoG, and intracortical signals each provide a unique window into brain function, with inherent trade-offs defined by their origin and acquisition method. Non-invasive techniques (EEG, fNIRS) offer accessible and safe platforms for basic research and clinical monitoring in more naturalistic settings, with EEG leading in temporal resolution and fNIRS in spatial specificity for surface cortex. Invasive techniques (ECoG, Intracortical), while carrying surgical risks, provide unparalleled signal quality and specificity, enabling advanced brain-computer interfaces and detailed investigation of neural coding. The future of neural interface research lies not only in refining these individual technologies but also in their strategic integration. Multimodal approaches, such as combined EEG-fNIRS, are increasingly demonstrating that the synergistic use of complementary signals can overcome the limitations of any single modality, offering a more holistic and powerful tool for understanding the brain and developing novel clinical interventions.
Brain-Computer Interfaces (BCIs) represent a transformative technology that establishes a direct communication pathway between the brain and external devices [15]. These systems can be broadly categorized into invasive interfaces, which require surgical implantation of electrodes directly into brain tissue, and non-invasive interfaces, which measure brain activity from the scalp surface [4]. The performance and application potential of these neural interfaces are fundamentally governed by three core technical parameters: spatial resolution, temporal resolution, and signal-to-noise ratio (SNR).
Spatial resolution refers to the ability to distinguish neural activity from distinct brain regions, temporal resolution indicates how precisely neural activity can be tracked over time, and SNR represents the clarity of the neural signal against background noise [2] [16]. These three parameters form a critical trade-off triangle that dictates the capabilities and limitations of both invasive and non-invasive BCIs, influencing their suitability for research applications, clinical interventions, and consumer products.
This comparative analysis examines these fundamental trade-offs through the lens of current research and technological capabilities, providing researchers and drug development professionals with a structured framework for evaluating neural interface technologies.
Technical Comparison of Invasive vs. Non-Invasive Neural Interfaces
Table 1: Fundamental Performance Characteristics of Neural Interface Technologies
| Interface Type | Spatial Resolution | Temporal Resolution | Signal-to-Noise Ratio | Primary Signal Sources |
|---|---|---|---|---|
| Invasive (Intracortical) | Single neuron level (μm) [16] | Millisecond (kHz range) [16] | Very High [17] | Action potentials, local field potentials [16] |
| Minimally Invasive (ECoG) | ~1 mm (electrode spacing) [2] | Millisecond [2] | High [2] | Cortical surface potentials [2] |
| Non-Invasive (EEG) | ~1-3 cm [16] | Millisecond (but limited to <90 Hz) [16] | Low (attenuated by skull) [16] | Scalp potentials from pyramidal neurons [16] |
| Non-Invasive (fNIRS) | ~1 cm [4] | Seconds (hemodynamic response) [4] | Low to Moderate [4] | Hemodynamic changes [4] |
| Non-Invasive (MEG) | ~5 mm [4] | Millisecond [4] | Moderate (requires shielding) [4] | Magnetic fields from neural currents [4] |
Table 2: Information Transfer Capabilities and Applications
| Interface Type | Theoretical Information Transfer Rate | Medical Applications | Research Applications |
|---|---|---|---|
| Invasive | High (dozens of bits/min demonstrated) [16] | Paralysis, severe motor impairments [4] [17] | Motor control, speech decoding [2] |
| Non-Invasive | Low to Moderate (highly variable) [18] | Neurorehabilitation, basic assistive tech [2] [19] | Cognitive neuroscience, brain mapping [2] |
The performance disparities between invasive and non-invasive approaches stem from fundamental biophysical principles. Invasive electrodes directly access neural electrical activity, bypassing the signal-degrading effects of the skull and other tissues [16]. In contrast, non-invasive techniques like EEG measure attenuated signals that have passed through multiple biological layers, resulting in significantly reduced spatial resolution and SNR [16]. As one analysis notes, "The signals obtained through the scalp are often weaker and more susceptible to noise, which can affect the precision of device control" [17].
Temporal characteristics also differ substantially. While both EEG and invasive methods offer millisecond-level temporal resolution, non-invasive systems face inherent bandwidth limitations. As one researcher observes, "with the exception of AP bursts in neuronal populations, non-invasive signals mainly allow analysis of low-frequency neuronal activity (<≈90 Hz)" [16]. This high-frequency limitation restricts the types of neural phenomena accessible to non-invasive monitoring.
Experimental Protocols and Methodologies
Invasive BCI Motor Control Paradigm
Objective: To enable real-time control of external devices using motor intention signals decoded from intracortical recordings [2].
Methodology:
- Surgical Implantation: Utah array or similar multi-electrode arrays are implanted in motor cortical regions (e.g., primary motor cortex, posterior parietal cortex) [2] [16].
- Signal Acquisition: Neural activity (action potentials and local field potentials) is recorded from hundreds to thousands of neurons [2].
- Feature Extraction: Movement parameters (direction, velocity, grip force) are decoded from neural firing patterns using algorithms like Kalman filters or neural networks [2].
- Closed-Loop Control: Decoded movement commands are translated to robotic arm or computer cursor control in real-time, with visual feedback provided to the user [16].
- Adaptive Learning: Both the user and the decoding algorithm adapt through practice, with users learning to modulate neural activity and algorithms improving decoding accuracy [16].
Key Metrics: Task completion accuracy, information transfer rate, time to target acquisition [16].
Non-Invasive EEG-Based Motor Imagery
Objective: To control external devices through imagined movements without physical execution [15].
Methodology:
- Electrode Placement: EEG electrodes are positioned over sensorimotor cortex regions according to the International 10-20 system [18].
- Paradigm Design: Users imagine specific motor acts (e.g., hand grasping, foot movement) without physical movement [15].
- Signal Processing: Event-related desynchronization/synchronization (ERD/ERS) of mu (8-12 Hz) and beta (13-30 Hz) rhythms are extracted as control features [15].
- Classification: Machine learning algorithms (e.g., common spatial patterns, linear discriminant analysis) distinguish between different motor imagery states [15].
- Feedback: Real-time visual or tactile feedback is provided to facilitate user learning and system control [15].
Key Metrics: Classification accuracy, information transfer rate, false positive rate [18].
Emerging Protocol: Temporal Interference Stimulation
Objective: To achieve non-invasive deep brain stimulation for potential therapeutic applications [20].
Methodology:
- Electrode Configuration: Multiple electrode pairs are placed on the scalp to create interfering electric fields [20].
- Field Generation: Two high-frequency (kHz) electric fields with slight frequency difference (Δf) are applied, creating an amplitude-modulated envelope at the difference frequency [20].
- Focal Targeting: The interference pattern is steered to deep brain structures (e.g., hippocampus) by adjusting current ratios between electrode pairs [20].
- Validation: Electric field modeling and cadaver measurements verify focal stimulation of target structures [20].
- Physiological Assessment: Functional MRI and behavioral tests confirm target engagement and functional modulation [20].
Key Metrics: Envelope modulation amplitude, stimulation focality, behavioral effects [20].
Diagram 1: Signal Pathway Comparison (46 characters)
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Materials for Neural Interface Development
| Item | Function | Example Applications |
|---|---|---|
| Utah Array | Multi-electrode cortical implant for high-density neural recording [2] | Invasive motor BMI research [2] |
| Dry EEG Electrodes | Scalp electrodes that don't require conductive gel [4] | Consumer BCI, portable neuroimaging [4] |
| WIMAGINE Device | Implantable ECoG grid system for chronic recording [2] | Restorative neuroprosthetics [2] |
| Stentrode | Endovascular electrode deployed via blood vessels [2] | Minimally invasive motor BCI [2] |
| fNIRS Systems | Functional near-infrared spectroscopy for hemodynamic monitoring [4] | Brain activity monitoring in natural environments [4] |
| Digital Holographic Imaging | Non-invasive, high-resolution neural activity recording [21] | Novel signal detection through tissue deformation [21] |
| Temporal Interference Stimulation | Non-invasive deep brain stimulation [20] | Targeted neuromodulation without surgery [20] |
The fundamental trade-offs between spatial resolution, temporal resolution, and signal-to-noise ratio present researchers with critical choices when selecting neural interface methodologies. Invasive approaches provide superior signal quality and information transfer rates essential for complex control tasks, but require surgical intervention and carry associated medical risks [16] [17]. Non-invasive technologies offer safety, accessibility, and whole-brain coverage, but face inherent biophysical limitations that constrain their performance for precision applications [16].
Future directions in neural interface research focus on overcoming these trade-offs through technological innovation. Emerging approaches include minimally invasive techniques like the Stentrode [2], novel signal detection methods such as digital holographic imaging [21], and advanced stimulation paradigms like temporal interference [20]. The continued evolution of these technologies promises to expand both fundamental neuroscience research and clinical applications, potentially narrowing the performance gap between invasive and non-invasive approaches while mitigating their respective limitations.
The Historical Trajectory and Key Milestones in NI Development
Neural Interfaces (NIs) represent a revolutionary technology that enables direct communication between the human brain and external devices. This field has evolved along two primary trajectories: invasive approaches that require surgical implantation of electrodes into or onto brain tissue, and non-invasive approaches that record neural signals from outside the skull. The historical development of NIs has been characterized by continuous trade-offs between signal fidelity and accessibility, with invasive methods providing higher spatial and temporal resolution at the cost of surgical risk and limited participant pools, while non-invasive approaches offer greater safety and accessibility but with compromised signal quality [2]. This comparative analysis examines the key milestones, performance metrics, and experimental protocols that have defined the evolution of both invasive and non-invasive neural interfaces, providing researchers with a comprehensive framework for evaluating current technologies and guiding future development.
The fundamental dichotomy in NI approaches stems from the challenge of measuring minute electrical signals generated by neural activity through various biological barriers. Invasive technologies such as intracortical electrodes and electrocorticography (ECoG) provide direct access to neural signals but face challenges related to long-term stability, biocompatibility, and limited clinical translation due to their invasive nature [2]. Non-invasive technologies including electroencephalography (EEG), functional near-infrared spectroscopy (fNIRS), and magnetoencephalography (MEG) circumvent surgical risks but must contend with signal attenuation caused by the skull and other tissues [22]. Recent advancements in signal processing, machine learning, and sensor technology have progressively narrowed the performance gap between these approaches, enabling unprecedented applications in both clinical and recreational domains [23] [2].
Historical Trajectory and Technological Evolution
Key Milestones in Neural Interface Development
The development of neural interfaces follows a distinct historical pathway characterized by foundational discoveries, technological innovations, and paradigm-shifting applications. The trajectory began with the discovery of electrical activity in the brain and the development of EEG in the early 20th century, which established the foundation for non-invasive brain monitoring [22]. The 1950s-1970s saw the first direct recordings from animal and human neurons, paving the way for invasive approaches. The formal conceptualization of Brain-Computer Interfaces (BCIs) in the 1970s marked a critical milestone, establishing the framework for direct brain-to-device communication [2].
The 1990s-2000s witnessed significant advancement in invasive technologies, particularly with the development of the Utah Array and other multi-electrode systems that enabled stable recordings from hundreds of individual neurons [22]. This period also saw the first successful demonstrations of invasive BCIs for cursor control in humans. Concurrently, non-invasive technologies benefited from the integration of advanced signal processing techniques and the development of more portable, affordable EEG systems [2]. The 2010s marked the emergence of commercial non-invasive BCIs for gaming and wellness applications, while invasive approaches demonstrated increasingly complex control of robotic prosthetics and communication devices for paralyzed individuals [22] [23].
Recent developments (2020-2025) have been characterized by several transformative trends. Miniaturization and wireless connectivity have enabled more practical form factors for both invasive and non-invasive systems [6]. The application of deep learning and neural networks has dramatically improved decoding accuracy across all modalities [2]. Hybrid approaches that combine multiple signal acquisition methods have emerged to overcome limitations of individual technologies [23]. Particularly noteworthy is the recent development of a generic non-invasive neuromotor interface based on surface electromyography (sEMG) that demonstrates unprecedented cross-participant generalization while achieving high-bandwidth communication previously only possible with invasive interfaces [6].
Comparative Technological Analysis
Table 1: Comparative Analysis of Major Neural Interface Technologies
| Technology | Spatial Resolution | Temporal Resolution | Invasiveness | Primary Applications | Key Limitations |
|---|---|---|---|---|---|
| Intracortical Electrodes | Single neuron (~50-100μm) | Milliseconds (∼1kHz) | High (surgical implantation required) | Robotic arm control, speech decoding [2] | Limited long-term stability, tissue response [2] |
| ECoG | Local field potentials (~1mm) | Milliseconds (∼1kHz) | Medium (requires craniotomy) | Motor restoration, epilepsy monitoring [2] | Limited cortical coverage, lower spatial resolution than intracortical [2] |
| sEMG | Muscle group level (~5-10mm) | Milliseconds (∼2kHz) | Non-invasive | Handwriting transcription, gesture recognition [6] | Limited to motor commands, anatomical variability [6] |
| EEG | ~1-10cm | ~10-100 milliseconds | Non-invasive | Basic communication, gaming, rehabilitation [2] | Low signal-to-noise ratio, limited spatial resolution [2] |
| fNIRS | ~1-2cm | Seconds | Non-invasive | Brain state monitoring, neurofeedback | Low temporal resolution, indirect hemodynamic measure [22] |
| fUS | ~100μm | Seconds (~2-10Hz) | Minimally invasive (requires cranial window) | Motor intention decoding [2] | Low temporal resolution, requires surgical access [2] |
Table 2: Performance Benchmarks Across Neural Interface Types (2020-2025)
| Interface Type | Information Transfer Rate (bits/min) | Decoding Accuracy (%) | Typical Applications | Representative Performance |
|---|---|---|---|---|
| Invasive (Intracortical) | 100-500 | 90-99 | Speech decoding, robotic control | Speech decoding at 62-78 words/minute [2] |
| Invasive (ECoG) | 50-200 | 85-95 | Motor restoration, spelling | Walking restoration in paralyzed patients [2] |
| Non-invasive (sEMG) | 80-180 | 90-95 | Handwriting, gesture control | 20.9 words per minute handwriting [6] |
| Non-invasive (EEG) | 5-60 | 70-90 | Basic control, neurofeedback | 0.66 target acquisitions/sec in continuous navigation [6] |
| Non-invasive (fNIRS) | 5-20 | 65-80 | Brain state monitoring | Classification of motor imagery [22] |
Experimental Protocols and Methodologies
Protocol for Non-invasive sEMG-based Neuromotor Interface
Recent groundbreaking research has demonstrated a non-invasive surface electromyography (sEMG) interface that achieves performance metrics previously only associated with invasive systems [6]. The experimental methodology encompasses several meticulously designed components:
Hardware Configuration: The research team developed a custom dry-electrode, multichannel sEMG recording device (sEMG-RD) with a high sample rate (2 kHz) and low-noise characteristics (2.46 μVrms) [6]. The device was fabricated in four different sizes (10.6, 12, 13, or 15 mm circumferential interelectrode spacing) to accommodate anatomical variation, approaching the spatial bandwidth of EMG signals at the forearm (~5-10 mm) while minimizing form factor. A strategic gap in electrode placement allowed for tightening adjustments along the ulna bone where muscle density is reduced, enabling sensing of putative motor unit action potentials (MUAPs) during low-movement conditions.
Participant Recruitment and Data Collection: The study employed an unprecedented scale of participant recruitment, encompassing 162-6,627 participants across different tasks, selected to represent anthropometric and demographic diversity [6]. Participants wore sEMG bands on their dominant-side wrist and performed three distinct tasks: (1) wrist control, where participants controlled a cursor with position determined from wrist angles tracked via motion capture; (2) discrete-gesture detection involving nine distinct gestures performed in randomized order with variable intergesture intervals; and (3) handwriting, where participants held their fingers together as if holding a writing implement and "wrote" prompted text. A real-time processing engine recorded both sEMG activity and label timestamps while a custom time-alignment algorithm addressed variations in participant reaction time and compliance.
Signal Processing and Decoding Architecture: The researchers developed neural networks trained on the large-scale dataset to transform sEMG signals into commands for computer interactions [6]. The models were designed to generalize across participants without individual calibration, addressing a fundamental challenge in BCI systems. The architecture incorporated techniques to minimize online-offline shift and handle the substantial variability in sEMG patterns across participants and sessions resulting from differences in sensor placement, anatomy, physiology, and behavior.
Protocol for Invasive Intracortical Speech Decoding
Invasive approaches have demonstrated remarkable capabilities in decoding neural signals for communication applications. The experimental methodology for state-of-the-art speech decoding involves:
Surgical Implantation: Participants with severe paralysis undergo surgical implantation of high-density microelectrode arrays (such as the Utah Array) into regions of the motor cortex associated with speech production [2]. These arrays typically contain hundreds of microelectrodes that record single-unit and multi-unit activity with high temporal resolution (~30 kHz sampling rate). The implantation procedure requires precise stereotactic positioning based on pre-operative imaging and functional mapping.
Neural Signal Acquisition: Raw neural signals are amplified, filtered, and processed to extract features relevant to speech production [2]. The processing pipeline typically includes: (1) bandpass filtering to separate local field potentials (LFP) from spike activity; (2) spike detection and sorting to identify action potentials from individual neurons; and (3) feature extraction that may include firing rates, population vectors, or spectral power in specific frequency bands. The system requires physically wired connections between the brain implant and external decoding hardware, creating challenges for long-term use and portability.
Decoding Algorithm Training: Participants are asked to attempt to speak or imagine speaking words and sentences while neural activity is recorded [2]. The corresponding audio or textual representations serve as training labels for supervised learning algorithms. Recent approaches have utilized recurrent neural networks (RNNs) and long short-term memory (LSTM) networks that model temporal dependencies in speech production. The trained models learn to map patterns of neural activity to intended speech sounds, words, or directly to text.
Performance Validation: Decoding performance is evaluated using metrics such as word error rate, characters per minute, or information transfer rate [2]. State-of-the-art systems have achieved decoding rates of 62-78 words per minute with vocabularies of hundreds of thousands of words, approaching natural conversation speeds.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Neural Interface Development
| Item | Function | Example Specifications | Application Context |
|---|---|---|---|
| High-Density Microelectrode Arrays | Record neural activity at single-neuron resolution | 64-256 channels, 50-100μm electrode spacing, 1-4kHz sampling rate | Invasive intracortical recording for motor control and speech decoding [2] |
| Dry sEMG Electrodes | Record muscle electrical activity without conductive gels | 2kHz sampling, 2.46μVrms noise, multiple sizes for anatomical variation | Non-invasive gesture recognition and handwriting transcription [6] |
| ECoG Grids | Record from brain surface with higher resolution than EEG | 16-256 contacts, 1cm spacing, subdural placement | Motor restoration, epilepsy monitoring [2] |
| Neural Signal Amplifiers | Amplify microvolt-level neural signals | High input impedance, programmable gain, built-in filters | Essential for all recording modalities to amplify weak neural signals [2] |
| Data Acquisition Systems | Convert analog signals to digital format | 16-24 bit resolution, simultaneous sampling, USB or wireless interface | NI data acquisition systems set standards for accuracy and performance [24] |
| Biocompatible Encapsulants | Protect implanted electronics from body fluids | Parylene-C, silicone elastomers, ceramic packages | Long-term stability of invasive neural interfaces [22] |
| Open-Source BCI Toolboxes | Signal processing and machine learning pipelines | MATLAB, Python, or Julia-based with real-time capabilities | Accelerate algorithm development and standardization [2] |
Comparative Analysis and Future Trajectories
Performance Benchmarking Across Modalities
The comparative analysis of invasive versus non-invasive neural interfaces reveals distinct performance characteristics and application domains. Invasive approaches consistently demonstrate superior information transfer rates, with intracortical interfaces achieving speeds necessary for fluent speech decoding and dexterous robotic control [2]. These systems provide access to neural signals at the spatial and temporal resolution required for decoding complex motor commands and cognitive processes. However, this performance comes with significant limitations: restricted participant pools due to surgical risks, challenges with long-term signal stability, and substantial technical support requirements.
Non-invasive approaches have historically offered substantially lower bandwidth but greater accessibility [2]. Recent advancements, particularly in sEMG-based interfaces, have dramatically narrowed this performance gap. The demonstrated capability of non-invasive sEMG to achieve 20.9 words per minute for handwriting transcription and 0.88 gesture detections per second approaches the functional utility of some invasive systems while maintaining complete non-invasiveness [6]. This represents a significant milestone in NI development, suggesting that strategic focus on signal acquisition and processing innovations can yield substantial performance improvements without surgical intervention.
The trade-offs between these approaches are further illustrated by their generalization capabilities. Invasive systems typically require extensive per-participant calibration and show limited generalization across users due to individual neuroanatomical differences and precise electrode placement [6] [2]. In contrast, recent non-invasive approaches have demonstrated remarkable cross-participant generalization, with models trained on thousands of participants performing effectively for new users without individual calibration [6]. This scalability advantage represents a critical consideration for widespread implementation.
Emerging Trends and Future Development Trajectories
The historical trajectory of NI development suggests several convergent trends that will shape future research directions. Hybrid approaches that combine multiple signal acquisition modalities are increasingly demonstrating complementary advantages [23]. Systems that simultaneously record EEG and fNIRS, or combine sEMG with inertial measurement units (IMUs), overcome limitations of individual technologies while preserving non-invasiveness.
Advanced materials science is driving innovations in both invasive and non-invasive interfaces [22]. For invasive systems, development of more biocompatible electrodes with reduced foreign body response and improved long-term stability is a critical research frontier. For non-invasive systems, materials innovations focus on higher conductivity dry electrodes, comfortable wearables, and systems that maintain signal quality during movement.
Machine learning and signal processing advancements continue to enhance performance across all modalities [6] [2]. Transfer learning approaches that leverage data from multiple participants to improve performance for new users are particularly promising for addressing the generalization challenge. Personalization techniques that efficiently adapt generic models to individual users with minimal calibration data represent another important direction.
The commercialization and standardization of NI technologies is accelerating translation from research to application [23]. Increasing availability of open-source toolboxes, standardized performance metrics, and regulatory frameworks for clinical applications is creating an ecosystem conducive to rapid innovation. The projected growth of the BCI market from $2.41 billion in 2025 to $12.11 billion by 2035 reflects increasing investment and commercial interest in both invasive and non-invasive technologies [23].
The historical trajectory of neural interface development reveals a field in rapid transition, with traditional trade-offs between invasiveness and performance being redefined by technological innovations. Invasive approaches continue to set benchmarks for signal fidelity and decoding performance, particularly for complex applications like speech decoding and dexterous robotic control. Meanwhile, non-invasive approaches are achieving unprecedented levels of performance and cross-participant generalization, dramatically expanding potential user populations and application domains.
The comparative analysis presented in this guide provides researchers with a framework for selecting appropriate technologies based on specific application requirements, participant populations, and performance targets. As the field continues to evolve, the convergence of materials science, signal processing, and machine learning promises to further narrow the performance gap between invasive and non-invasive approaches while addressing persistent challenges related to scalability, accessibility, and long-term reliability. These advancements will undoubtedly unlock new possibilities for human-computer interaction, neurorehabilitation, and fundamental neuroscience research in the coming decade.
Methodologies, Real-World Applications, and Current Market Landscape
Brain-Computer Interfaces (BCIs) represent a revolutionary technology that enables direct communication between the human brain and external devices [25]. Unlike their invasive counterparts, which require surgical implantation, non-invasive BCIs measure brain activity from the scalp, offering a safer and more accessible alternative for a wide range of applications [17]. The global non-invasive BCI market is projected to capture a majority share of the overall BCI market, which is forecast to grow from USD 2.41 billion in 2025 to USD 12.11 billion by 2035 [25]. This growth is largely driven by the wide applicability of non-invasive technologies in healthcare, consumer wellness, and assistive technology, bolstered by their user-friendliness and lower risk profile [4] [25]. This guide provides a comparative analysis of the dominant non-invasive applications, detailing their performance, underlying experimental protocols, and the essential tools required for research and development.
Performance Comparison of Dominant Non-Invasive BCI Applications
The performance of non-invasive BCIs varies significantly across different application domains, primarily due to the distinct neural signals and decoding challenges inherent to each use case. The table below summarizes the key performance metrics and technological focuses for the three dominant applications.
Table 1: Performance Metrics and Technological Focus of Dominant Non-Invasive BCI Applications
| Application Domain | Primary Signal & Modality | Key Performance Metrics | Typical Information Transfer Rate (ITR) | Primary Technological Focus |
|---|---|---|---|---|
| Neurodiagnostics & Medical Monitoring | Spontaneous EEG/ERPs [2] | Sensitivity, Specificity, Spatial Resolution | Not Primary Focus | High-density scalp EEG systems for diagnosis of epilepsy, sleep disorders, and traumatic brain injury [4] [2] |
| Consumer Wellness & Neurofeedback | Oscillatory EEG (Alpha, Beta bands) [4] | Usability, Comfort, Long-term Stability | Low | Wearable EEG headsets for sleep monitoring, emotional state tracking, and meditation [4] [26] |
| Basic BCI & Assistive Technology | Sensorimotor Rhythms, SSVEP, P300 [2] | Classification Accuracy, Speed, Reliability | Medium | EEG-based systems for communication (e.g., text spelling) and control (e.g., wheelchair navigation) for individuals with paralysis [2] [27] |
Experimental Protocols & Methodologies
Robust experimental protocols are fundamental to the development and validation of non-invasive BCI technologies. The following section outlines standard methodologies employed across the dominant application domains.
Protocol for Motor Imagery-Based BCI Control
This protocol is typical for developing assistive technologies, such as controlling a computer cursor or a robotic arm [2].
- Participant Preparation & Setup: The participant is fitted with a multi-channel EEG cap, typically following the international 10-20 system. Electrode impedances are checked and reduced to below 10 kΩ to ensure high-quality signal acquisition. The participant is seated in a comfortable chair in a dimly lit, shielded room to minimize environmental artifacts [2].
- Signal Acquisition & Hardware: Neural signals are recorded using a high-density EEG system (e.g., 64-128 channels) with a sampling rate of at least 250 Hz. The hardware includes amplifiers and analog-to-digital converters to capture microvolt-level brain signals [2].
- Paradigm & Task: The participant performs a series of cued motor imagery tasks, such as imagining left-hand or right-hand movement without any physical execution. Each trial begins with a fixation cross, followed by a visual cue indicating the specific task, and an imagery period of several seconds [2].
- Data Processing & Decoding:
- Pre-processing: Acquired EEG signals are filtered (e.g., 8-30 Hz bandpass for sensorimotor rhythms) and artifacts from eye movements or muscle activity are removed using algorithms like Independent Component Analysis (ICA) [2].
- Feature Extraction: Features are extracted from the EEG signals, commonly focusing on changes in band power (e.g., Event-Related Desynchronization in the mu/beta rhythms over the sensorimotor cortex) [2].
- Classification: A machine learning classifier (e.g., Support Vector Machine or Linear Discriminant Analysis) is trained on the extracted features to discriminate between the different motor imagery states. This model is then used for real-time control [2].
- Output & Feedback: The decoder's output is translated into a command for an external device. The system provides real-time visual feedback to the participant, for instance, by moving a cursor on a screen, creating a closed-loop system that enables the user to learn and improve control [2].
Protocol for Neurodiagnostic Monitoring (e.g., Epilepsy)
This protocol is standard for clinical diagnosis and monitoring of neurological conditions like epilepsy.
- Patient Setup: The patient is fitted with a full-cap EEG electrode system in a clinical setting. The setup is like the research protocol but often with a strong emphasis on consistent electrode placement for longitudinal comparisons [4].
- Signal Acquisition: Long-term, continuous EEG is recorded, often over 24-48 hours, in an inpatient setting or at home with portable devices. The recording captures both resting-state activity and activity during potential seizure events [4].
- Data Analysis & Detection: The recorded data is analyzed, either by a trained clinician or automated software, to identify pathological patterns such as spikes, sharp waves, or seizure discharges. The analysis focuses on signal morphology and temporal patterns rather than intentional control signals [4].
The experimental workflow for a standard non-invasive BCI protocol, from participant setup to closed-loop feedback, is visualized below.
Signaling Pathways & Neural Correlates
The efficacy of non-invasive BCIs hinges on detecting specific neural signals that reflect user intention, cognitive state, or pathological activity.
Primary Neural Signals in Non-Invasive BCI
- Sensorimotor Rhythms (SMR): These are oscillatory patterns in the mu (8-12 Hz) and beta (13-30 Hz) frequency bands recorded over the sensorimotor cortex. During motor imagery or movement preparation, these rhythms exhibit Event-Related Desynchronization (ERD)—a decrease in power. Upon movement cessation, they show Event-Related Synchronization (ERS)—an increase in power. This predictable modulation is the cornerstone for motor-based BCIs [2].
- Event-Related Potentials (ERPs): ERPs are voltage fluctuations in the EEG signal that are time-locked to a specific sensory, cognitive, or motor event. The P300 potential, a positive deflection occurring about 300 ms after an infrequent target stimulus, is widely used in BCI spellers. The P300's amplitude is inversely related to stimulus probability, making it a robust marker for attention-based selection [2].
- Steady-State Visually Evoked Potentials (SSVEP): When a user gazes at a visual stimulus flickering at a fixed frequency, the visual cortex generates an oscillatory EEG response at the same frequency (and its harmonics). By detecting which frequency is present in the EEG, a BCI can determine which stimulus the user is attending to, enabling high-ITR communication systems [2].
- Pathological Patterns: In neurodiagnostics, the focus is on aberrant signals. For epilepsy, this includes interictal epileptiform discharges (spikes and sharp waves) and ictal rhythms (seizure activity characterized by rhythmic patterns that evolve in frequency and amplitude) [4].
The diagram below illustrates the relationship between external events, the resulting neural signals measured by EEG, and their characteristics.
The Scientist's Toolkit: Research Reagent Solutions
Advancing non-invasive BCI research requires a suite of reliable hardware, software, and analytical tools. The following table details essential components of a modern non-invasive BCI research toolkit.
Table 2: Essential Tools and Reagents for Non-Invasive BCI Research
| Tool/Reagent | Function/Description | Example Vendors/Platforms |
|---|---|---|
| High-Density EEG Systems | Records electrical potential from the scalp with high spatial resolution; the core hardware for signal acquisition. | ANT Neuro, CGX, G.Tec Medical Engineering [25] |
| Dry & Wet Electrodes | Interface with the scalp for signal transduction. Dry electrodes improve usability, while wet electrodes (with gel) offer better signal quality. | Material innovations are a key R&D area [4] |
| Open-Source BCI Software | Provides standardized pipelines for signal processing, feature extraction, and machine learning classification. | OpenBCI, BCILAB, Psychtoolbox [2] |
| Stimulation Hardware | Presents visual, auditory, or tactile stimuli to evoke measurable neural responses (ERPs, SSVEP). | |
| Artifact Removal Algorithms | Software tools to identify and remove non-neural signals from data (e.g., eye blinks, muscle activity). | Independent Component Analysis (ICA) is a standard method [2] |
| Machine Learning Libraries | Enable the development of custom decoders to translate neural features into control commands. | Scikit-learn, TensorFlow, PyTorch (as applied to neural data) [2] |
Non-invasive BCIs have carved out critical and distinct application niches in neurodiagnostics, consumer wellness, and basic assistive communication. Their dominance is secured by their safety profile, accessibility, and the maturity of supporting technologies like high-density EEG and advanced machine learning. While invasive interfaces may offer superior signal resolution for complex motor control, non-invasive technologies are unmatched for applications where risk, cost, and large-scale deployment are primary concerns. Future progress will likely stem from advancements in signal processing, dry electrode technology, and the integration of artificial intelligence, further solidifying the role of non-invasive BCIs in both clinical and consumer markets.
Invasive neural interfaces represent a cutting-edge frontier in neurotechnology, offering direct access to neural signals by placing electrodes within the skull—either on the brain's surface (epidural or subdural) or within brain tissue itself (intracortical). These technologies have evolved beyond experimental concepts into clinically validated solutions for severe neurological disorders, particularly for patients with motor disabilities who have exhausted conventional treatment options. The fundamental rationale for pursuing invasive approaches lies in their superior signal quality compared to non-invasive alternatives; intracortical electrodes and electrocorticography (ECoG) provide higher spatial resolution, broader bandwidth, and improved signal-to-noise ratio, enabling more precise decoding of neural intent for controlling external devices or modulating pathological neural circuits [4] [19].
The clinical landscape for these interfaces is rapidly evolving, with the overall brain-computer interface market forecast to grow to over $1.6 billion by 2045 [4]. This growth is propelled by advances in materials science, neural decoding algorithms, and minimally invasive surgical techniques. Invasive interfaces are primarily deployed for three principal applications: motor neuroprosthetics for restoring movement and communication, deep brain stimulation (DBS) for modulating dysfunctional neural circuits, and functional restoration for severe paralysis conditions. This comparative analysis examines the current state of these technologies, their relative performance metrics, and the experimental protocols validating their clinical efficacy, providing researchers and clinicians with a framework for evaluating their therapeutic potential.
Technology Comparison: Performance Metrics and Clinical Applications
Performance Benchmarking of Invasive Neural Interfaces
Table 1: Comparative Performance Metrics of Invasive Neural Interfaces
| Interface Type | Spatial Resolution | Temporal Resolution | Signal-to-Noise Ratio | Primary Clinical Applications | Key Limitations |
|---|---|---|---|---|---|
| Intracortical Microelectrodes | Very High (micron-scale) | Very High (milliseconds) | High | Motor control for paralysis, neural decoding for communication | Tissue response, signal stability over time |
| Electrocorticography (ECoG) | High (mm-scale) | High (milliseconds) | Moderate-High | Epilepsy monitoring, motor neuroprosthetics | Limited penetration depth, requires craniotomy |
| Deep Brain Stimulation (DBS) Electrodes | Medium (cm-scale) | Therapeutic stimulation | N/A | Parkinson's disease, essential tremor, dystonia | Invasive implantation, side effects from stimulation |
Invasive interfaces demonstrate distinct performance characteristics that determine their clinical applications. Intracortical microelectrodes, such as the Utah Array used by Blackrock Neurotech, provide the highest spatial and temporal resolution, enabling detailed decoding of movement intentions from individual neurons or small neural populations [4] [28]. This high-fidelity signal is essential for complex tasks such controlling robotic arms or enabling typing through neural signals. However, these interfaces face challenges with long-term signal stability due to the brain's tissue response to implanted microelectrodes [28].
Electrocorticography (ECoG) approaches offer a balance between signal quality and invasiveness. By placing electrodes on the surface of the brain (below the dura mater), ECoG systems capture neural population signals with higher spatial resolution and signal-to-noise ratio compared to non-invasive electroencephalography (EEG), while avoiding some of the long-term stability issues associated with intracortical implants [28] [19]. A fully implanted ECoG system demonstrated reliable decoding of movement-intent with approximately 90% accuracy in a subject with cervical quadriplegia, enabling volitional control of hand grasp both in laboratory and home environments [28].
Deep brain stimulation (DBS) electrodes represent a different class of invasive interfaces focused on therapeutic modulation rather than signal recording. These systems deliver electrical stimulation to specific deep brain structures to modulate pathological neural activity. DBS has received FDA approval for essential tremor (1997), Parkinson's disease (2002), and dystonia (2003), establishing it as the most clinically validated invasive neuromodulation approach [19].
Clinical Application Comparison
Table 2: Clinical Applications and Efficacy Metrics
| Application | Technology Implementations | Key Efficacy Metrics | Representative Clinical Outcomes |
|---|---|---|---|
| Severe Paralysis Restoration | Intracortical BMI, ECoG with FES | Decoding accuracy, Functional independence measures | 89-91% decoding accuracy for hand grasp [28]; Improved object transfer tasks |
| Parkinson's Disease Symptoms | Deep Brain Stimulation (DBS) | Tremor reduction, Medication reduction | Significant tremor suppression; Reduced levodopa requirements [29] [19] |
| Communication Restoration | Intracortical speech decoding | Characters per minute, Accuracy | Real-time decoding with >90% accuracy for 8-word vocabulary [19] |
| Spinal Cord Injury Rehabilitation | Epidural SCS with rehabilitation | Walking ability, Voluntary movement recovery | Independent overground walking with continuous SCS [29] |
For severe paralysis conditions, particularly cervical spinal cord injury, invasive brain-computer interfaces have demonstrated remarkable capabilities. In one landmark study, a fully implanted ECoG system allowed a participant with complete cervical quadriplegia to achieve volitional control of hand grasp with 89.0% accuracy in laboratory settings and 88.3% accuracy during closed-loop trials at home [28]. This performance remained stable throughout the 29-week laboratory study and subsequent home use, highlighting the potential for long-term functional restoration.
Deep brain stimulation has established itself as a transformative therapy for movement disorders, with well-documented efficacy in large patient populations. Unlike motor neuroprosthetics that primarily decode and execute motor commands, DBS works by modulating pathological neural circuits. For Parkinson's disease, high-frequency stimulation of the subthalamic nucleus or internal globus pallidus effectively suppresses tremors, rigidity, and bradykinesia, significantly improving quality of life and reducing medication requirements [29] [19].
Recent advances have also explored the application of invasive interfaces for cognitive disorders, though this represents a more nascent field. Preliminary studies suggest that electrical neuromodulation strategies might potentially alleviate some cognitive and memory deficits, particularly in the context of dementia, though the neural mechanisms underlying cognition are considerably more complex than those for sensorimotor functions [29].
Experimental Protocols and Methodologies
Implantable BCI for Hand Grasp Restoration
A comprehensive study published in 2021 detailed the methodology for restoring volitional control of hand grasp in a 21-year-old male with complete cervical quadriplegia (C5 ASIA Impairment Scale A) using a fully implanted brain-computer interface [28]. The experimental protocol encompassed several distinct phases:
Screening and Participant Selection: Twenty-one subjects with C5/C6 motor complete SCI underwent EEG-based screening to test their ability to trigger a functional electrical stimulation (FES) device through motor imagery of dominant hand movement versus rest states. Only one subject qualified for surgical implantation after completing 16 sessions of EEG screening, demonstrating the importance of careful participant selection [28].
Surgical Implantation Protocol: Pre-operative functional magnetic resonance imaging (fMRI) mapped cortical activation during imagined dominant hand movements and actual shoulder movements. Diffusion tensor imaging identified the location of corticospinal tract fibers previously controlling dominant hand movement. These merged images guided a small craniotomy over the left motor cortex using frameless stereotaxy. Intraoperative electrical stimulation and electromyogram (EMG) monitoring definitively identified motor cortex by evoking EMG activity in proximal muscles [28].
System Configuration and Signal Processing: The implanted system consisted of subdural surface electrodes placed over the dominant-hand motor cortex connected to a transmitter implanted subcutaneously below the clavicle, enabling continuous reading of electrocorticographic (ECoG) activity. Movement-intent was decoded from the ECoG signals to trigger functional electrical stimulation of the dominant hand during laboratory studies and subsequently control a mechanical hand orthosis during in-home use [28].
Assessment Metrics: The study employed multiple quantitative measures including decoding accuracy for movement intent, performance on upper extremity tasks (lifting small objects, transferring objects to specific targets), and temporal stability of functional outcomes. Laboratory decoding accuracy averaged 89.0% (range 78-93.3%), while at-home decoding reached 91.3% (range 80-98.95%) during open-loop trials and 88.3% (range 77.6-95.5%) during closed-loop trials [28].
Figure 1: Experimental workflow for fully implanted BCI deployment
Spinal Cord Stimulation for Locomotor Recovery
Multiple research groups have developed protocols for spinal cord stimulation (SCS) to restore motor function after spinal cord injury, employing distinct methodological approaches:
Conventional Continuous SCS: The Kentucky SCI Center implemented continuous SCS combined with intensive rehabilitation in participants with motor-complete SCI. Training included standing, body-weight-supported treadmill stepping, and overground walking, all with continuous SCS delivered via fully implanted leads in the posterior epidural space connected to an implantable pulse generator [29].
Spatiotemporal SCS: Courtine and Bloch's team developed a paradigm using real-time control capabilities to alternate stimulation between swing, weight acceptance, and propulsion phases of the gait cycle. Electrode configurations were triggered either at a pre-defined pace or in real-time by residual kinematic events. This approach was tested in nine participants with chronic incomplete SCI, including three with motor-complete SCI implanted with electrode arrays tailored for both leg and trunk motor functions [29].
Assessment Metrics: Studies measured the recovery of voluntary leg movements with and without stimulation, quantitative gait analysis, and functional independence measures. Notably, participants demonstrated significant improvement in assisted standing, trunk stability, and overground walking ability with assistive devices after extended training periods ranging from 15 to 85 weeks [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Invasive Neural Interface Studies
| Item Category | Specific Examples | Research Function | Implementation Notes |
|---|---|---|---|
| Electrode Technologies | Utah Array (Blackrock), Neuropixels, Custom ECoG grids | Neural signal acquisition | Intracortical arrays for single-unit recording; ECoG for population signals |
| Signal Acquisition Systems | Wireless transmitters, Implantable pulse generators | Signal transmission and power delivery | Subclavian implantation for cosmesis and reduced infection risk [28] |
| Stimulation Apparatus | Functional electrical stimulators, DBS pulse generators | Therapeutic neuromodulation | Multi-channel systems for targeted muscle activation or deep brain stimulation |
| Neural Decoding Algorithms | Support vector machines, Deep learning networks | Movement intent classification | Real-time processing of ECoG or spike signals for device control |
| Surgical Navigation | Pre-operative fMRI, DTI, Frameless stereotaxy | Precision electrode placement | Motor cortex localization for optimal signal acquisition [28] |
| Assessment Tools | Upper extremity task batteries, Gait analysis systems | Functional outcome measurement | Standardized metrics for decoding accuracy and clinical improvement |
The development and implementation of invasive neural interfaces requires specialized materials and instrumentation. Electrode technologies form the foundation, with intracortical microelectrode arrays providing the highest signal resolution but potentially facing long-term stability challenges, while ECoG electrodes offer a balance between signal quality and reduced tissue trauma [4] [28].
Signal acquisition systems have evolved toward fully implanted wireless platforms that enable continuous recording and processing outside laboratory environments. These systems include subcutaneous transmitters that communicate with external receivers, allowing participants to use the technology in home settings without direct clinical supervision [28].
Neural decoding algorithms represent the computational core of motor neuroprosthetics, translating raw neural signals into control commands for external devices. These typically employ machine learning approaches trained on individual participant data to classify movement intent with accuracies typically exceeding 85-90% in optimized systems [28].
Assessment methodologies include both performance metrics (decoding accuracy, speed of task completion) and functional outcome measures specific to the target clinical application. For motor restoration, these may include standardized upper extremity task batteries, while for locomotor recovery, quantitative gait analysis and independence measures are employed [29] [28].
Figure 2: Neural signal processing pathway for invasive BCIs
Comparative Analysis: Invasive versus Non-Invasive Approaches
The selection between invasive and non-invasive neural interfaces involves careful consideration of risk-benefit ratios, signal fidelity requirements, and target applications. Invasive technologies provide substantial advantages in signal quality, with ECoG and intracortical systems offering higher spatial resolution, temporal resolution, and signal-to-noise ratios compared to non-invasive alternatives like EEG [4]. This enhanced signal fidelity translates to superior performance in complex control tasks, higher information transfer rates, and reduced training requirements.
However, these advantages must be balanced against the surgical risks, potential for tissue response, and higher costs associated with invasive approaches [4]. Non-invasive systems, while limited in signal quality, offer safety and accessibility advantages that make them suitable for a broader range of applications, particularly in consumer neurotechnology and preliminary clinical assessment [19].
The evolving neurotechnology landscape suggests a future with multiple coexisting modalities tailored to specific clinical needs. Invasive interfaces will likely remain the gold standard for severe paralysis conditions requiring high-fidelity control, while non-invasive approaches may dominate in diagnostic, monitoring, and consumer applications. Future directions include the development of minimally invasive approaches, such as endovascular electrodes that can be delivered through blood vessels, potentially offering an intermediate solution with improved signal quality over non-invasive systems while reducing surgical risks [19].
The field of neural interfaces has long been defined by a fundamental trade-off: the pursuit of high-fidelity neural signals has necessitated invasive technologies that carry significant surgical risks and biological challenges. Invasive brain-computer interfaces (BCIs), such as the Utah Array, penetrate brain tissue to record from individual neurons but can trigger inflammatory responses and scar tissue formation, which degrade signal quality over time [27]. On the opposite end of the spectrum, completely non-invasive techniques like electroencephalography (EEG) offer safety and accessibility but are limited by poor spatial resolution and signal strength due to the damping effect of the skull and scalp [2].
Against this backdrop, minimally invasive technologies have emerged as a promising middle path. This guide provides a comparative analysis of two leading approaches: Stentrodes, which are endovascular electrodes, and functional ultrasound (fUS), which images neural activity through acoustic signals. Both aim to circumvent the skull barrier without penetrating delicate brain parenchyma, potentially offering superior signal quality compared to non-invasive methods while avoiding the key pitfalls of fully invasive implants. Their development represents a pivotal direction in neurotechnology, seeking to balance signal fidelity, procedural risk, and long-term stability for both research and clinical applications.
Technology Comparison: Stentrodes vs. Functional Ultrasound
The following table provides a direct, data-driven comparison of Stentrode and functional ultrasound technologies across critical technical and application parameters.
Table 1: Comparative Analysis of Stentrode and Functional Ultrasound Neural Interfaces
| Feature | Stentrode | Functional Ultrasound (fUS) |
|---|---|---|
| Fundamental Principle | Endovascular electrocorticography (ECoG); records electrical signals from within blood vessels [30] | Measures changes in cerebral blood volume (CBV) as a hemodynamic correlate of neural activity [31] |
| Key Physical Component | Self-expanding nitinol stent with platinum-iridium electrodes [30] | Miniaturized linear ultrasound transducer array [31] |
| Spatial Resolution | Millimeter-scale (limited by vessel location and electrode count) [30] | ~100 μm x 100 μm in-plane resolution [31] |
| Temporal Resolution | High (milliseconds, suitable for electrical potentials) [30] | Low (~1 Hz, limited by hemodynamic response) [31] [2] |
| Signal Type | Direct neural electrical activity (local field potentials) [30] | Indirect hemodynamic response (changes in blood volume) [31] |
| Primary Surgical Step | Endovascular deployment via jugular vein [27] [30] | Requires a cranial window or sonolucent skull prosthesis [2] |
| Chronic Biostability | Endothelialization anchors device; preserves venous patency [30] | Still under investigation for chronic human use [2] |
| Target Application | Motor intention decoding for communication and control [27] [30] | Mapping mesoscopic brain organization and real-time intention decoding [31] [2] |
| Representative Data | Enabled patients with paralysis to control digital devices for text communication [27] | Mapped directional tuning of saccadic eye movements in primate lateral intraparietal area (LIP) [31] |
Experimental Protocols and Methodologies
Stentrode Deployment and Motor Intent Decoding
The development and validation of the Stentrode involve a multi-stage process, from precise engineering to chronic implantation and decoding.
Table 2: Key Experimental Stages for Stentrode Development and Validation
| Stage | Key Objective | Methodology Overview |
|---|---|---|
| 1. Device Fabrication | Create a biocompatible, self-expanding electrode array. | A nitinol stent scaffold is laser-cut and electropolished. A polyimide-film electrode array with 16 platinum-iridium contacts is lithographically patterned and bonded to the stent [30]. |
| 2. Preclinical Biocompatibility | Assess long-term safety and integration within the venous environment. | The device is implanted in the superior sagittal sinus of ovine models. Endothelialization, vessel patency, and signal stability are monitored histologically and via imaging for over 12 months [30]. |
| 3. Clinical Deployment (Human Trials) | Implant the device in human participants via a minimally invasive procedure. | The stent is compressed and delivered to the superior sagittal sinus via a catheter inserted in the jugular vein. It is deployed under fluoroscopic guidance to appose the vessel wall adjacent to the motor cortex [27] [30]. |
| 4. Signal Acquisition & Processing | Capture and decode motor commands from within the vessel. | Local field potentials are acquired, amplified, and digitized by a subcutaneous telemetry unit. Signals are transmitted wirelessly to an external decoder that translates high-gamma band activity into control commands for external devices [30]. |
| 5. Performance Validation | Quantify the system's efficacy in restoring communication or control. | Participants with paralysis perform attempted limb movements or imagine typing. Decoding algorithms are trained to translate these recorded neural signals into cursor movements or text output, with success rates and speed measured [27]. |
Diagram 1: Stentrode experimental workflow from implantation to functional control.
Functional Ultrasound for Mesoscopic Brain Mapping
fUS neuroimaging has been powerfully applied to uncover the functional organization of neural circuits, as demonstrated in a 2025 study mapping saccadic eye movement control in the primate brain [31]. The core experimental protocol is as follows:
- Animal Preparation and Cranial Access: Two rhesus macaques were implanted with a recording chamber over the left posterior parietal cortex. This provided acoustic access for the ultrasound transducer, which was positioned normal to the brain surface above the dura mater [31].
- Behavioral Task Design: The animals were trained on a memory-guided saccade task. They fixated on a center point, were cued with one of eight peripheral target directions, maintained the location in memory, and then executed a saccade to the remembered location upon cue [31].
- fUSI Data Acquisition: A miniaturized linear ultrasound transducer (128 elements, 100 μm spatial pitch) was used to record images at 1 Hz. The key measured parameter was the change in cerebral blood volume (CBV), an indirect marker of neural activity. Data were collected from multiple coronal planes of the posterior parietal cortex across different sessions [31].
- Data Processing and Analysis:
- General Linear Model (GLM): A GLM was applied to identify voxels whose CBV responses were significantly modulated by saccade direction.
- Directional Tuning Analysis: For significant voxels, tuning curves were constructed to determine their preferred saccade direction and tuning width (e.g., broad vs. narrow).
- Mesoscopic Mapping: The spatial organization of these tuned voxels was analyzed to identify patches or subregions with similar directional preferences, revealing a heterogeneous, patchy topography within the lateral intraparietal area (LIP) that was stable over months to years [31].
Diagram 2: Functional ultrasound workflow from data acquisition to feature mapping.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details the key materials, reagents, and hardware essential for conducting research in these two specialized fields.
Table 3: Essential Research Tools for Stentrode and fUS Technologies
| Item | Function/Description | Relevance |
|---|---|---|
| Nitinol Tubing | Base material for the self-expanding stent scaffold; provides superelasticity and shape memory [30]. | Critical for Stentrode mechanical integrity and minimally invasive delivery. |
| Platinum-Iridium & Iridium Oxide | Conductive electrode material and coating; provides high corrosion resistance and enhanced charge injection capacity [30]. | Essential for Stentrode electrochemical performance and chronic recording stability. |
| Polyimide Film Substrate | A flexible, biocompatible substrate for lithographic patterning of microelectrodes and traces [30]. | Forms the thin-film electronic component of the Stentrode. |
| Linear Ultrasound Transducer Array | The core sensing hardware (e.g., 128 elements, 100 μm pitch) for transmitting and receiving ultrasonic waves [31]. | Fundamental component of fUS systems for high-resolution data acquisition. |
| Subcutaneous Telemetry Unit (IRTU) | An implantable unit that amplifies, digitizes, and wirelessly transmits neural data from the Stentrode [30]. | Enables chronic, untethered signal acquisition in freely behaving subjects. |
| Dual Antiplatelet Therapy (e.g., Aspirin/Clopidogrel) | Pharmacological regimen to prevent thrombus formation on the intravascular implant [30]. | Standard clinical protocol for managing thromboembolic risk post-Stentrode implantation. |
| General Linear Model (GLM) Software | Statistical framework for identifying voxels with significant hemodynamic responses to specific stimuli or tasks [31]. | Core analytical tool for extracting task-related neural signals from fUS data. |
Stentrodes and functional ultrasound represent two distinct and promising paths through the central challenge of neural interfacing. The Stentrode leverages established endovascular techniques and the high temporal resolution of electrical signals to create a clinically viable, minimally invasive motor BCI. In contrast, functional ultrasound offers unprecedented mesoscopic spatial resolution for brain mapping and basic research, albeit with a currently more limited temporal profile and greater cranial access requirement.
The choice between these technologies is not a matter of superiority but of alignment with research or clinical objectives. The Stentrode is engineered for chronic implantation and direct device control in patient populations, offering a tangible solution for restoring communication. Functional ultrasound, meanwhile, is a powerful discovery tool for elucidating fundamental principles of brain organization and function. Together, they significantly expand the neurotechnologist's arsenal, providing new avenues to explore the brain with reduced biological cost and accelerating the journey toward safe, effective, and high-performance brain-computer interfaces.
The field of neural interfaces is undergoing a transformative period, marked by a clear divergence between invasive and non-invasive brain-computer interface (BCI) technologies. These distinct technological pathways are progressing along different development timelines, targeting specific market segments, and facing unique adoption challenges. Invasive BCIs, which require surgical implantation directly into brain tissue, offer high-fidelity neural signal acquisition for severe medical conditions, while non-invasive approaches, utilizing external sensors placed on the scalp, provide safer, more accessible solutions for broader applications. This comparative analysis examines the market segmentation and growth forecasts for both invasive and non-invasive neural interfaces, tracing their progression from research environments to clinical adoption. The trajectory of these technologies is shaped by a complex interplay of technological innovation, clinical validation, regulatory oversight, and market forces that collectively determine their path toward widespread implementation and commercial viability. Understanding these dynamics is essential for researchers, investors, and healthcare professionals navigating the evolving neurotechnology landscape [22] [2] [32].
Technical Performance Benchmarks
The fundamental distinction between invasive and non-invasive neural interfaces lies in their technical capabilities for recording neural signals, which directly influences their appropriate applications and market positioning.
Signal Acquisition and Resolution Comparison
Table 1: Technical Performance Comparison of Neural Interface Technologies
| Parameter | Invasive BCIs | Non-Invasive BCIs |
|---|---|---|
| Spatial Resolution | Micrometer-scale (single neuron level) | Centimeter-scale (limited by skull, scalp tissues) |
| Temporal Resolution | Millisecond precision (neural spiking activity) | Millisecond to second range (EEG: ms; fNIRS: seconds) |
| Signal-to-Noise Ratio | High (direct neural recording) | Low to moderate (signals attenuated by skull) |
| Penetration Depth | Deep cortical layers and specific nuclei | Superficial cortical regions only |
| Typical Applications | Speech decoding, robotic arm control, movement restoration | Communication aids, basic device control, neurofeedback |
| Information Transfer Rate | High (up to 56 words per minute demonstrated) | Low to moderate (slow typing interfaces) |
Invasive BCIs provide unprecedented access to neural signals through microelectrode arrays implanted directly in brain tissue. These systems can record from hundreds to thousands of individual neurons, enabling fine-grained decoding of movement intentions, speech processes, and complex cognitive states. The high spatial and temporal resolution of invasive approaches has enabled remarkable demonstrations, including the restoration of communication for paralyzed individuals at speeds approaching 56 words per minute with 99% accuracy and the control of robotic arms for object manipulation [27] [33].
Non-invasive approaches, primarily using electroencephalography (EEG), functional near-infrared spectroscopy (fNIRS), and emerging technologies like wearable magnetoencephalography (MEG) and functional ultrasound (fUS), face fundamental physical constraints. The skull and scalp tissues significantly attenuate and spatially blur neural signals, resulting in lower spatial resolution and signal-to-noise ratios. However, continuous advancements in sensor technology, signal processing algorithms, and artificial intelligence are steadily improving the capabilities of non-invasive systems. Recent demonstrations show that AI-assisted non-invasive BCIs can significantly improve task completion times for robotic arm control and cursor tasks, with one study reporting a paralyzed participant completing a block-moving task in approximately 6.5 minutes with AI assistance compared to being unable to complete it without [34] [2].
Decoding Performance and Applications
The performance differences between these approaches directly influence their current and near-term applications. Invasive systems excel in applications requiring precise control and high information throughput, particularly for individuals with severe paralysis or communication impairments. Non-invasive systems, while less precise, offer immediate utility for basic communication, environmental control, rehabilitation, and emerging consumer applications in gaming and wellness [35] [2].
Application Segmentation Between BCI Types
Market Segmentation Analysis
The neural interface market has evolved into distinct segments based on technological approach, application areas, and end-user populations, with invasive and non-invasive technologies targeting largely complementary markets.
Technology-Based Segmentation
Table 2: Global BCI Market Segmentation by Technology, Product, and Application (2025-2033)
| Segment | 2025 Market Value | 2033 Projected Value | CAGR | Primary Applications |
|---|---|---|---|---|
| Non-invasive BCI | 87.5% market share [36] | Dominant position maintained | 14.4% [37] | Healthcare, rehabilitation, consumer gaming, research |
| Invasive BCI | Smaller market share | Fastest growth rate [36] | 8.4% [22] | Severe paralysis, communication restoration, advanced prosthetics |
| Healthcare Applications | 63.3% market share [36] | Continued dominance | N/A | Neurological disorder treatment, assistive technologies |
| Medical End-Users | 47.0% market share [36] | Leading segment | N/A | Hospitals, clinical research centers |
Market forecasts reveal distinct growth trajectories for invasive and non-invasive neural interfaces. The overall BCI market is projected to grow from USD 2.40 billion in 2025 to USD 6.16 billion by 2032, representing a compound annual growth rate (CAGR) of 14.4% [37]. Alternative projections suggest even stronger growth from USD 2.05 billion in 2023 to USD 10.65 billion by 2033, at a CAGR of 17.9% [36]. Non-invasive technologies currently dominate the market, accounting for 87.5% of revenue share in 2023, driven by their safety profile, ease of use, and broader applicability across healthcare, research, and consumer segments [36].
While representing a smaller portion of the current market, invasive BCIs are projected to grow at a significant pace, with IDTechEx forecasting the overall BCI market to surpass USD 1.6 billion by 2045, representing a CAGR of 8.4% since 2025 [22]. This growth is fueled by demonstrated clinical efficacy in restoring communication and mobility for severely disabled populations, with companies like Neuralink, Synchron, and Blackrock Neurotech advancing human clinical trials [27].
Application-Based Segmentation
The healthcare segment represents the largest application area for BCIs, accounting for 63.3% of market revenue, with medical end-users comprising 47.0% of the market [36]. Within healthcare, distinct subsegments have emerged:
Rehabilitation and Restoration: This segment addresses conditions such as spinal cord injury, stroke recovery, and amyotrophic lateral sclerosis (ALS). Invasive BCIs show remarkable success in this domain, with one study demonstrating a paralyzed ALS patient communicating over 237,000 sentences at approximately 56 words per minute with 99% accuracy using an implanted BCI over two years [33].
Neurological Disorder Treatment: BCIs are being developed for conditions including Parkinson's disease, epilepsy, and depression. The rising prevalence of neurological disorders is a significant market driver, with projections indicating 25.2 million people living with Parkinson's disease alone by 2050 [37].
Assistive Technologies: This segment includes communication devices, environmental control systems, and mobility aids for individuals with severe disabilities. Both invasive and non-invasive approaches compete in this space, with the choice dependent on the severity of impairment and performance requirements.
Beyond healthcare, emerging segments include consumer gaming (NeuroSky), workplace wellness (Neurable's fatigue detection), and military applications (DARPA-funded projects), though these remain smaller markets currently [37] [27] [19].
Regional Adoption Patterns
Significant geographical variations exist in neural interface adoption, reflecting differences in healthcare infrastructure, regulatory frameworks, research funding, and market readiness.
North America represents the largest regional market, accounting for 40.8% of global revenue in 2023 [36]. This dominance is fueled by strong R&D investment, a high concentration of clinical trials, advanced healthcare infrastructure, and the presence of leading BCI companies including Neuralink, Synchron, Blackrock Neurotech, and Paradromics. The region's market growth is further driven by the increasing prevalence of neurodegenerative diseases and significant government funding through initiatives like the NIH BRAIN Initiative [22] [27].
The Asia-Pacific region is projected to exhibit the highest CAGR during the forecast period, driven by rising healthcare expenditures, growing patient awareness, low-cost manufacturing advantages, and favorable government policies attracting foreign investment. Countries including China, Japan, and South Korea are actively promoting BCI development for both medical and industrial applications, such as driver alertness monitoring and workplace safety systems [37].
Europe maintains a significant presence in the neurotechnology landscape, with strong academic research institutions and medical device companies contributing to both invasive and non-invasive BCI development. The European market is characterized by robust regulatory oversight and ethical frameworks governing neural interface technologies [22].
Regional Adoption Drivers for Neural Interfaces
Experimental Protocols and Methodologies
Rigorous experimental protocols underpin the advancement of both invasive and non-invasive neural interfaces, with distinct methodologies tailored to their specific applications and technological constraints.
Invasive BCI Clinical Trial Protocols
Human trials for invasive BCIs follow stringent protocols designed to ensure patient safety and generate clinically meaningful data. The BrainGate2 trial, one of the longest-running and most extensive clinical trials for invasive BCIs, exemplifies this approach:
Participant Selection: Participants typically have severe paralysis resulting from spinal cord injury, brainstem stroke, or neurodegenerative diseases such as ALS. Criteria include intact cognitive function and the ability to provide informed consent [33].
Surgical Implantation: Microelectrode arrays (such as the Utah Array or Neuralink's N1 Implant) are surgically implanted in brain regions relevant to the target function—motor cortex for movement control, speech motor cortex for communication, or somatosensory cortex for sensory restoration. The procedure involves craniotomy and precise placement of electrodes using stereotactic guidance [27] [33].
Signal Acquisition and Processing: Neural signals are recorded from hundreds of microelectrodes, amplified, digitized, and processed in real-time. Custom decoding algorithms translate neural activity into control signals for external devices [2] [33].
Task Training and Calibration: Participants engage in structured training sessions where they attempt to perform specific tasks (cursor control, text entry, robotic arm movement) while the system adapts to their neural patterns. Modern systems increasingly maintain performance without daily recalibration [33].
Long-term Monitoring: Studies now extend over years, with continuous assessment of device performance, signal stability, and safety parameters. One study demonstrated stable performance over two years with a participant generating over 237,000 sentences without daily recalibration [33].
Non-Invasive BCI Experimental Framework
Non-invasive BCI protocols prioritize accessibility and scalability while addressing challenges related to signal quality and user variability:
Signal Acquisition Setup: Participants wear EEG caps or fNIRS headbands with electrode configurations ranging from 1-16 channels for consumer systems to 32-128+ channels for research-grade systems. Preparation includes skin abrasion and electrolyte gel application for traditional EEG, though dry electrodes are increasingly common [2].
Experimental Paradigms: Common paradigms include motor imagery (imagining limb movements without physical execution), evoked potentials (responses to visual/auditory stimuli), or mental state classification (focus, relaxation). Recent approaches incorporate AI as a "co-pilot" to interpret user intent and improve task performance [34].
Signal Processing Pipeline: Advanced algorithms filter artifacts, extract relevant features, and classify intended actions using machine learning techniques. Deep learning approaches have significantly improved decoding accuracy for non-invasive signals [34] [2].
Validation Metrics: Performance is quantified through information transfer rate, accuracy, completion time, and user experience measures. Recent studies demonstrate that AI assistance can significantly reduce task completion times, with paralyzed participants completing tasks that were impossible without assistance [34].
Research Reagent Solutions and Experimental Tools
The development and validation of neural interfaces rely on specialized tools, reagents, and experimental systems that enable precise measurement and manipulation of neural activity.
Table 3: Essential Research Tools for Neural Interface Development
| Tool/Category | Function | Example Implementations |
|---|---|---|
| Microelectrode Arrays | Record neural activity at single-neuron resolution | Utah Array (Blackrock Neurotech), N1 Implant (Neuralink), Neuropixels |
| Endovascular Electrodes | Minimally invasive recording through blood vessels | Stentrode (Synchron) |
| EEG Systems | Non-invasive recording of electrical brain activity | Research-grade systems (Brain Products GmbH), consumer headsets (NeuroSky, Muse) |
| fNIRS Systems | Measure hemodynamic responses via infrared light | Portable systems for movement-friendly brain monitoring |
| Neural Decoding Algorithms | Translate neural signals into device commands | Deep learning models, filter algorithms, classification techniques |
| Calibration Protocols | Adapt systems to individual users' neural patterns | Transfer learning approaches, subject-specific training |
| Experimental Software Platforms | Present stimuli, record responses, manage experiments | BCI2000, OpenVibe, PsychToolbox, custom MATLAB/Python frameworks |
| AI Co-pilot Systems | Augment BCI control with computer vision and intent inference | UCLA's AI-BCI system for robotic arm control [34] |
The toolset for neural interface research continues to evolve, with several key trends shaping experimental capabilities. For invasive approaches, materials science advancements are producing more biocompatible electrodes with reduced immune responses and longer functional lifetimes. Flexible "neural lace" designs and high-channel-count systems (such as Paradromics' 421-electrode array) are pushing the boundaries of recording capacity and tissue integration [27].
For non-invasive systems, the integration of multimodal sensing (EEG + fNIRS + MEG) provides complementary information that enhances decoding accuracy. Additionally, portable and wearable systems enable longer recording sessions in real-world environments, facilitating the transition from laboratory validation to clinical and consumer applications [35] [2].
Advanced signal processing represents another critical tool category, with deep learning approaches now routinely applied to both invasive and non-invasive data. Self-supervised learning techniques are particularly valuable for reducing calibration times and improving generalization across users and sessions [35] [2].
Challenges in Clinical Translation
The path from research demonstration to clinical adoption presents distinct challenges for invasive and non-invasive neural interfaces, spanning technical, regulatory, and commercial dimensions.
Invasive Interface Translation Barriers
Invasive BCIs face significant hurdles in achieving widespread clinical adoption:
Surgical Risks and Biocompatibility: Implantation requires brain surgery with associated risks of infection, inflammation, and tissue damage. Long-term biocompatibility remains challenging, with foreign body responses potentially leading to scar tissue formation that degrades signal quality over time [36] [32].
Long-Term Reliability and Stability: Maintaining stable performance over years or decades presents substantial engineering challenges. Device longevity is critical for clinical viability, yet few systems have demonstrated multi-decade reliability. Recent data shows promise, with one study reporting ICMS (intracortical microstimulation) remaining safe and effective in human subjects over years, with more than half of electrodes functioning reliably after a decade [33].
Regulatory Approval Pathways: Invasive neural interfaces face rigorous regulatory scrutiny due to their high-risk classification. The FDA and other regulatory bodies require extensive preclinical testing and clinical data demonstrating both safety and efficacy. Companies like Synchron and Neuralink are navigating these pathways through Breakthrough Device designations and controlled clinical trials [27] [32].
Reimbursement and Health Economics: Establishing viable reimbursement models is essential for commercial sustainability. High development costs, surgical expenses, and ongoing support requirements create significant economic barriers. Payers require compelling cost-effectiveness evidence, which necessitates larger clinical trials with meaningful patient outcome measures [36].
Non-Invasive Interface Translation Barriers
Non-invasive approaches face different, though equally significant, challenges:
Signal Quality Limitations: The fundamental physics of signal attenuation through the skull creates an inherent performance ceiling for non-invasive systems. Low signal-to-noise ratios and limited spatial resolution restrict the complexity of tasks that can be reliably controlled [35] [2].
User Variability and Training Requirements: Performance varies considerably across users, with a significant proportion of "BCI illiterate" individuals who struggle to achieve reliable control. Extensive training is often required, creating practical barriers to clinical implementation [36].
Clinical Validation and Standardization: While non-invasive systems face lower regulatory barriers, demonstrating clinically meaningful benefits remains essential for adoption. Standardized performance metrics and validation protocols are still evolving, making cross-study comparisons difficult [2].
Real-World Usability: Consumer-grade systems prioritize aesthetics and ease of use but may sacrifice signal quality. Achieving acceptable performance outside controlled laboratory environments remains challenging due to artifacts from movement, environmental noise, and variable setup conditions [36].
Future Outlook and Emerging Trends
The neural interface landscape continues to evolve rapidly, with several trends shaping the future trajectory of both invasive and non-invasive technologies toward clinical adoption.
The convergence of AI with BCI systems represents perhaps the most significant trend, with AI acting as an intelligent "co-pilot" that interprets user intent and compensates for limitations in signal quality or decoding algorithms. UCLA researchers demonstrated this approach by combining custom EEG decoding algorithms with a camera-based AI platform that interprets user direction and intent in real-time, significantly improving task completion times for both able-bodied and paralyzed participants [34].
Miniaturization and wireless connectivity are transforming both invasive and non-invasive systems. For invasive interfaces, fully implantable, wireless systems eliminate transcutaneous connectors that pose infection risks. For non-invasive approaches, miniaturized electronics and dry electrodes enable more practical, user-friendly designs suitable for daily use outside laboratory settings [27] [2].
Hybrid approaches that combine neural signals with other input modalities (eye tracking, muscle signals, contextual sensors) are creating more robust and intuitive systems. These multimodal interfaces can compensate for the limitations of any single signal source, potentially accelerating adoption across diverse user populations and application scenarios [22] [2].
The regulatory landscape is maturing alongside the technology, with agencies developing more nuanced frameworks for evaluating neural interfaces. Ethical considerations around neural data privacy, agency, and enhancement are receiving increased attention, with neuroethics becoming an integral component of technology development rather than an afterthought [32].
Market projections suggest a period of sustained growth and specialization, with invasive and non-invasive technologies increasingly targeting complementary applications and patient populations. While non-invasive approaches will likely dominate the broader market due to their accessibility and safety profile, invasive interfaces will continue to advance toward resolving the most severe disabilities where their risks are justified by their transformative potential [22] [37] [36].
As the field progresses, the distinction between research and clinical applications will continue to blur, with technologies gradually transitioning from proof-of-concept demonstrations to validated clinical tools that restore function, augment capabilities, and fundamentally expand our understanding of the human brain.
Technical Hurdles, Biocompatibility, and Optimization Strategies
In the rapidly advancing field of brain-computer interfaces (BCIs), a fundamental dichotomy exists between invasive and non-invasive approaches, creating a critical research axis for comparative analysis. Invasive neural interfaces, which involve surgically implanted electrodes, provide direct access to neural signals with high spatial and temporal resolution, enabling remarkable applications such as controlling robotic arms and decoding speech [27] [2]. However, these systems require neurosurgical implantation, carry risks of infection and tissue response, and may experience signal degradation over time due to scarring [38], limiting their widespread adoption.
Non-invasive approaches, particularly electroencephalography (EEG), offer a safer, more accessible alternative that avoids surgical risks. EEG measures electrical activity from the scalp surface, providing millisecond-level temporal resolution at relatively low cost and high portability [38] [2]. Despite these advantages, EEG-based systems face intrinsic challenges in signal fidelity and stability that have historically constrained their performance for precise control applications. The core limitation stems from the biological and physical barriers that separate scalp electrodes from neural sources - the cerebrospinal fluid, skull, and scalp - which attenuate and spatially blur electrical signals, resulting in poor spatial resolution and low signal-to-noise ratio (SNR) [39] [38].
This comparative guide objectively analyzes the performance gap between invasive and non-invasive neural interfaces, with particular focus on technological innovations that are advancing non-invasive EEG capabilities. We present experimental data and methodologies demonstrating how modern signal processing, hybrid sensing approaches, and novel hardware designs are progressively overcoming EEG's intrinsic limitations, bridging the fidelity chasm toward more robust, real-world BCI applications.
Comparative Performance Analysis: Invasive vs. Non-Invasive Interfaces
Table 1: Fundamental Characteristics of Neural Interface Technologies
| Parameter | Invasive BCIs (Cortical Implants) | Minimally Invasive BCIs (Stentrode, ECoG) | Non-Invasive EEG |
|---|---|---|---|
| Spatial Resolution | Single neuron level (microns) [27] | Mesoscale (mm-cm) [2] | Centimetres [39] |
| Temporal Resolution | Millisecond (neural spiking) [27] | Millisecond (local field potentials) [2] | Millisecond [38] |
| Signal Attenuation | Minimal (direct tissue contact) | Moderate | Significant (skull, tissues) [38] |
| Signal-to-Noise Ratio | High [38] | Moderate to High | Low [39] [38] |
| Clinical Risk Profile | High (surgical risk, infection) [38] | Moderate (minimal surgery required) | Negligible [38] |
| Long-Term Stability | Degrades over time (scarring) [38] | Good (WIMAGINE system demonstrated chronic use) [2] | Variable (depends on electrode type) [40] |
| Target Applications | High-precision control (robotic arms, speech decoding) [27] [2] | Motor command detection, walking restoration [2] | Rehabilitation, communication, basic control [38] |
Table 2: Quantitative Performance Metrics Across BCI Modalities
| Modality | Information Transfer Rate (bits/min) | Motor Imagery Classification Accuracy | Real-World Deployment | Key Limitations |
|---|---|---|---|---|
| Invasive (Intracortical) | ~300+ (handwriting decoding) [2] | N/A (direct neural command) | Limited to clinical trials | Requires brain surgery, signal stability [27] |
| Minimally Invasive (Stentrode) | Not reported | N/A (motor command detection) | Early human trials [27] | Limited brain coverage, vascular access [2] |
| ECoG | ~200+ [2] | >90% (finger movements) [2] | Limited clinical use | Requires craniotomy [2] |
| Traditional EEG | 5-25 [38] | ~70-80% (2-class MI) [41] | Widespread research use | Low SNR, susceptibility to artifacts [39] |
| Advanced EEG (Hybrid Models) | Not reported | 96.06% (4-class MI with CNN-LSTM) [41] | Emerging research use | Computational complexity, training data requirements [41] |
The performance differential between invasive and non-invasive approaches is substantial, particularly for applications requiring precise control. Invasive BCIs have demonstrated remarkable capabilities, such as decoding handwriting at speeds of approximately 20 words per minute directly from neural signals [2]. Non-invasive EEG traditionally lagged significantly in information transfer rates and classification accuracy, but recent advances in decoding algorithms have begun to narrow this gap, with hybrid deep learning models now achieving exceptional accuracy in motor imagery classification [41].
Experimental Approaches to Enhancing EEG Fidelity
Advanced Signal Processing Methodologies
The intrinsic limitations of EEG signals have prompted development of sophisticated processing pipelines to enhance signal fidelity. A typical advanced EEG processing workflow integrates multiple stages of artifact removal and feature extraction to maximize the extractable information content.
Experimental Protocol: Hybrid Deep Learning for Motor Imagery Classification
A landmark study demonstrating EEG's potential employed a hybrid deep learning approach to achieve unprecedented classification accuracy [41]. The methodology encompassed:
Dataset: Utilized the "PhysioNet EEG Motor Movement/Imagery Dataset" containing EEG recordings from multiple subjects performing actual and imagined movements.
Preprocessing Pipeline:
- Applied band-pass filtering (0.5-40 Hz) to remove non-physiological noise and DC drift
- Used Independent Component Analysis (ICA) to identify and remove ocular and muscular artifacts
- Implemented spatial filtering to enhance signal-to-noise ratio
- Normalized signals across channels to mitigate inter-session variability
Feature Extraction:
- Employed Wavelet Transform to capture time-frequency characteristics
- Applied Riemannian geometry approaches to analyze covariance matrices in Riemannian space
- Used dimensionality reduction techniques (PCA, t-SNE) to visualize and select discriminative features
Classification Models:
- Compared traditional machine learning classifiers (KNN, SVC, Logistic Regression, Random Forest, Naive Bayes)
- Evaluated individual deep learning models (CNN, LSTM)
- Developed a novel hybrid CNN-LSTM model combining spatial feature extraction (CNN) with temporal dependency modeling (LSTM)
Performance Metrics: The models were evaluated based on classification accuracy, with the hybrid CNN-LSTM achieving 96.06% accuracy for motor imagery classification, significantly outperforming traditional machine learning (91% with Random Forest) and individual deep learning models [41].
Hardware Innovations for Signal Acquisition
Beyond algorithmic advances, hardware innovations are critical for improving EEG signal quality at the acquisition stage. Traditional wet EEG systems require conductive gel and skin preparation, creating practical barriers to long-term monitoring. Recent developments have focused on dry electrode technology that eliminates the need for gels while maintaining signal quality.
QUASAR's dry electrode EEG sensors incorporate ultra-high impedance amplifiers (>47 GOhms) that handle contact impedances up to 1-2 MOhms, producing signal quality comparable to wet electrodes [40]. These systems enable recordings through hair without skin preparation, with mechanical isolation designs that stabilize electrodes for artifact-free recordings during movement. Practical advantages include significantly reduced setup time (4.02 minutes for dry electrodes versus 6.36 minutes for wet electrode systems) and stable signal quality over extended periods [40].
Ear-EEG systems represent another innovation, capturing EEG signals from within the ear canal using dry or wet electrodes [40]. The Naox device employs dry-contact electrodes with active electrode technology featuring 13 TΩ input impedance to minimize noise despite higher electrode-skin impedance. These systems enable discreet, long-term monitoring compatible with daily activities.
Emerging Approaches: Hybrid Systems and Transfer Learning
Hybrid EEG-fNIRS Integration
A promising approach to overcoming individual modality limitations involves combining EEG with complementary neuroimaging techniques. Functional near-infrared spectroscopy (fNIRS) measures hemodynamic responses in the brain, providing better spatial specificity and robustness to electrical noise and motion artifacts compared to EEG [39] [42].
Table 3: Hybrid EEG-fNIRS Integration Benefits
| Aspect | EEG Strengths | fNIRS Strengths | Hybrid Advantage |
|---|---|---|---|
| Temporal Resolution | Excellent (millisecond) [38] | Poor (inherent physiological delay) [39] | Preserves high temporal resolution |
| Spatial Resolution | Poor (centimetres) [39] | Good (localized hemodynamic response) | Enhanced spatial localization |
| Noise Immunity | Susceptible to electrical, motion artifacts [39] | Robust to electrical noise [39] | Improved robustness in real-world settings |
| Information Content | Direct neural electrical activity | Indirect metabolic activity | Complementary information enhances decoding |
| Real-World Use | Challenging due to artifacts | More feasible due to noise robustness | More reliable performance |
Hybrid EEG-fNIRS systems leverage the temporal precision of EEG with the spatial specificity of fNIRS, demonstrating enhanced classification performance compared to either modality alone [39] [42]. This approach is particularly valuable for neuroprosthetic control applications where both speed and precision of command decoding are essential.
Cross-User Generalization Techniques
A fundamental challenge in non-invasive BCIs is the variability of EEG signals across individuals and sessions, necessitating user-specific calibration that impedes practical deployment. Recent research has focused on transfer learning and domain adaptation techniques to develop models that generalize across users without individual calibration.
Experimental Protocol: Generic Non-Invasive Neuromotor Interface
A groundbreaking study published in Nature developed a generic non-invasive neuromotor interface using surface electromyography (sEMG) that demonstrates the feasibility of cross-user generalization [6]. While based on sEMG rather than EEG, the methodological approach provides a template for addressing similar challenges in EEG systems:
Data Collection at Scale: Collected training data from thousands of consenting participants (162-6,627 participants depending on task) to capture population-level variability [6].
Hardware Optimization: Developed a comfortable, wireless sEMG research device with dry electrodes that could be donned in seconds, manufactured in multiple sizes to accommodate anatomical diversity.
Generalized Model Architecture: Employed neural networks trained on diverse population data rather than individual users, demonstrating that generic models could achieve:
- 0.66 target acquisitions per second in continuous navigation tasks
- 0.88 gesture detections per second in discrete gesture tasks
- Handwriting transcription at 20.9 words per minute [6]
Personalization Potential: Showed that generic model performance could be further improved by 16% with limited user-specific calibration, providing a hybrid approach to balancing generalization and personalization [6].
This approach demonstrates that with sufficient training data diversity and appropriate model architecture, non-invasive interfaces can achieve cross-user generalization while maintaining high performance - a crucial advancement for practical BCI deployment.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagents and Solutions for Advanced EEG Research
| Category | Specific Solution | Function/Application | Key Characteristics |
|---|---|---|---|
| Signal Acquisition | Dry EEG Electrodes [40] | Scalp potential measurement without gel | High-input impedance amplifiers, mechanical stabilization |
| Ear-EEG Systems [40] | Discreet neural monitoring | In-ear placement, active electrode technology | |
| High-Density EEG Arrays | Improved spatial sampling | 64-256 channels, standardized placements | |
| Signal Processing | Independent Component Analysis (ICA) [38] | Artifact separation and removal | Blind source separation, requires manual component identification |
| Wavelet Transform [41] [38] | Time-frequency analysis | Multi-resolution analysis, preserves temporal and spectral information | |
| Riemannian Geometry Approaches [41] | Covariance matrix analysis | Manifold-based classification, enhanced feature discrimination | |
| Classification Algorithms | Convolutional Neural Networks (CNN) [41] | Spatial feature extraction | Learns hierarchical representations, effective for EEG topography |
| Long Short-Term Memory (LSTM) Networks [41] | Temporal sequence modeling | Captures long-range dependencies in time-series data | |
| Hybrid CNN-LSTM Models [41] | Spatiotemporal pattern recognition | Combined spatial and temporal feature learning | |
| Random Forest Classifier [41] | Traditional machine learning benchmark | Ensemble method, robust to noise, achieved 91% accuracy in MI | |
| Data Enhancement | Generative Adversarial Networks (GANs) [41] | Synthetic EEG data generation | Addresses limited dataset sizes, improves model generalization |
| Transfer Learning Frameworks | Cross-user and cross-session adaptation | Reduces calibration requirements, enables plug-and-play operation | |
| Validation Metrics | Cohen's Kappa Coefficient [40] | Inter-rater agreement assessment | Measures classifier performance relative to chance |
| Information Transfer Rate (ITR) | BCI communication efficiency | Bits per minute, accounts for speed and accuracy |
The comparative analysis between invasive and non-invasive neural interfaces reveals a rapidly evolving landscape where technological innovations are systematically addressing the intrinsic limitations of EEG. While invasive methods currently provide superior signal fidelity for high-precision applications, recent advances in non-invasive approaches demonstrate a promising trajectory toward closing this performance gap.
The integration of sophisticated deep learning architectures, hybrid multimodal systems, and novel hardware designs has enabled remarkable improvements in EEG-based BCI performance. The achievement of 96.06% classification accuracy for motor imagery using hybrid CNN-LSTM models [41] demonstrates that algorithmic advances can extract substantially more information from conventional EEG signals than previously possible. Similarly, the development of cross-user generalization techniques [6] addresses a critical barrier to practical BCI deployment.
Future research directions will likely focus on further refining these approaches, with particular emphasis on real-world validation, long-term stability assessment, and standardized performance metrics. As non-invasive EEG systems continue to evolve, they offer the potential for widespread BCI adoption across clinical, research, and eventually consumer domains, balancing performance requirements with practical accessibility and safety considerations.
The evolution of brain-computer interfaces (BCIs) represents a paradigm shift in neurotechnology, offering potential solutions for restoring sensory and motor functions in individuals with neurological impairments [27]. Biocompatibility—the ability of an implant to perform its desired function without eliciting any undesirable local or systemic effects in the host—stands as the fundamental determinant for the successful long-term deployment of neural interfaces [43] [44]. The widening gap between the mechanical and chemical properties of conventional implant materials and those of native neural tissue triggers a cascade of biological responses that ultimately compromise both stability and safety [43] [44]. This comparative analysis examines how both invasive and non-invasive neural interfaces address the core challenge of biocompatibility, evaluating the distinct material strategies and their implications for long-term performance.
Comparative Landscape of Neural Interfaces
Neural interfaces can be broadly categorized by their level of invasiveness, which directly correlates with their signal quality, biocompatibility challenges, and target applications.
Table 1: Comparison of Invasive and Non-Invasive Neural Interfaces
| Feature | Invasive Interfaces | Minimally Invasive Interfaces | Non-Invasive Interfaces |
|---|---|---|---|
| Placement | Penetrates brain tissue (e.g., Utah Array, Michigan Probe) [27] [2] | On cortical surface (ECoG) or in blood vessels (Stentrode) [27] [2] | On the scalp (EEG, fNIRS, MEG) [4] [2] |
| Signal Resolution | High spatial and temporal resolution [2] [44] | Moderate to High resolution (ECoG); Lower than invasive (Stentrode) [27] [2] | Low spatial resolution, variable temporal resolution [4] [2] |
| Primary Biocompatibility Challenge | Foreign Body Reaction (FBR), chronic inflammation, glial scar formation [43] [44] | Reduced FBR risk compared to invasive, but potential for encapsulation [27] [45] | Minimal safety risk; challenge is signal fidelity from non-contact recording [4] [2] |
| Longevity & Stability | Degradation over weeks/months due to FBR; active research on solutions [43] [44] | Potentially longer-lasting than invasive; Stentrode showed stability at 12 months [27] | Stable for acute use; not subject to biological rejection [4] |
| Key Players/Technologies | Neuralink, Blackrock Neurotech, Paradromics [27] [45] | Precision Neuroscience, Synchron [27] [45] | Various research labs and consumer neurotech companies [4] |
The central challenge for implantable neural interfaces is the mechanical mismatch at the tissue-device interface. Neural tissue is soft, with a Young's modulus approximately 1-10 kPa, while traditional electrode materials like silicon (≈102 GPa) and platinum (≈102 MPa) are orders of magnitude stiffer [43] [44]. This mismatch, combined with the implantation injury, activates the host immune system, initiating a Foreign Body Reaction (FBR) [43]. The FBR involves acute and subsequent chronic inflammatory responses, attracting immune cells like macrophages to the implant site and leading to the formation of a fibrotic glial scar around the electrode [43] [44]. This scar tissue insulates the electrode from nearby neurons, drastically increasing electrical impedance and causing a progressive decline in recording quality and stimulation efficacy, often within a month of implantation [43].
Material Strategies and Experimental Approaches for Enhanced Biocompatibility
To overcome the FBR, significant research focuses on developing new materials and coatings that better mimic the properties of neural tissue. The following experimental workflows and reagent toolkits are central to this endeavor.
Key Experimental Workflows
Diagram 1: Biocompatibility R&D Pipeline
The research pipeline for evaluating novel neural interfaces involves a multi-stage process, progressing from material design to human trials, with a consistent focus on assessing the foreign body response and functional stability.
Diagram 2: Foreign Body Reaction Pathway
The Foreign Body Reaction is a sequential biological process initiated by implantation, leading to scar tissue formation that diminishes the long-term performance of neural electrodes.
The Scientist's Toolkit: Research Reagents and Materials
Table 2: Essential Materials for Advanced Neural Interface Development
| Material/Reagent | Category | Primary Function | Key Consideration |
|---|---|---|---|
| Nature-Derived Materials (Chitosan, Alginate, Silk Fibroin, Hyaluronan) [43] | Biocompatible Coating/Substrate | Creates a bio-friendly interface; reduces immune activation and scar formation [43]. | Excellent biocompatibility and biodegradability; can be engineered to mimic the ECM [43]. |
| Conductive Polymers (PEDOT:PSS) [44] | Coating/Conductive Element | Improves charge injection capacity and signal-to-noise ratio; can be combined with soft substrates [44]. | Enhances electrical properties while allowing for softer, more tissue-conformable electrodes [44]. |
| Utah & Michigan Arrays (Silicon, Platinum, Iridium Oxide) [27] [44] | Traditional Rigid Electrode | Gold-standard for high-fidelity neural recording and stimulation in research [27]. | Significant mechanical mismatch with tissue; prone to inducing chronic FBR [43] [44]. |
| Flexible Polymer Substrates (Polyimide, Parylene C) [43] | Insulation/Structural Support | Provides a flexible and biocompatible backbone for microfabricated electrodes [43]. | More compliant than silicon, but still significantly stiffer than brain tissue (Epolyimide ≈ 2.5 GPa) [43]. |
| Carbon Fiber Electrodes [44] | Ultra-Small Electrode | Enables high-density neural interfaces with small diameters (e.g., 7 μm) for reduced tissue displacement [44]. | Offers a compromise between sufficient stiffness for insertion and reduced cross-sectional area. |
Analysis of Emerging Solutions and Performance Data
Coating and Material Strategies
Nature-derived materials (NMs) are promising for creating a favorable interface. For instance, layer-by-layer coatings of marine polysaccharides (chitosan, ulvan) on silicon surfaces have shown enhanced hippocampal neuron proliferation and reduced astrocyte adhesion in vitro, suggesting a potential to improve cortical electrode biocompatibility [43]. Silk fibroin has been ingeniously used as a supporting layer that dissolves after implantation, allowing for the transfer of a planar cortical NI that exhibits excellent conformability to the feline brain and stable recording performance [43].
Soft and conformable designs represent a shift from rigid probes. Precision Neuroscience's "Layer 7" device is an ultra-thin electrode array that slips between the skull and brain, conforming to the cortical surface without penetrating it, thereby reducing the risk of tissue damage [27] [45]. Similarly, the development of flexible lattice structures (e.g., Blackrock's Neuralace) and carbon fiber microelectrodes aims to minimize mechanical mismatch [27] [44].
Comparative Performance Metrics
Table 3: Quantitative Comparison of Interface Performance and Biocompatibility
| Interface Type | Typical Signal-to-Noise Ratio (SNR) | Spatial Resolution | Typical Longevity & Key Failure Mode | Recorded Signal Type |
|---|---|---|---|---|
| Invasive Utah Array [43] [27] [44] | High (direct neuron contact) | Single Neuron | Months to Years; Fibrotic Encapsulation [43] | Single-Unit & Multi-Unit Activity |
| Minimally Invasive ECoG (e.g., Precision) [27] [2] [45] | Moderate to High | Millimetres | Under investigation; potentially longer than invasive | Local Field Potentials |
| Endovascular Stentrode (Synchron) [27] [2] | Moderate | ~1-2 cm | Stable at 12-month follow-up [27] | Local Field Potentials |
| Non-Invasive EEG [4] [2] | Low (signal attenuation by skull) | ~1-2 cm | Limited by session use, not biocompatibility [4] | Scalp Potentials |
The performance data highlights a direct trade-off. Invasive interfaces provide the highest signal fidelity but face the steepest biocompatibility challenges, with recording performance often declining drastically after approximately one month due to fibrotic tissue formation [43]. Minimally invasive strategies like the Stentrode and surface ECoG seek a compromise, demonstrating stable medium-term performance in human trials with a potentially safer profile [27].
The pursuit of biocompatible neural interfaces is a multi-faceted endeavor defined by a fundamental trade-off: the pursuit of high-fidelity neural signals often necessitates greater invasiveness, which in turn provokes a more pronounced biological rejection response. Invasive technologies, while powerful, are fundamentally constrained by the chronic Foreign Body Reaction. The field's progress is therefore increasingly defined by innovative material science strategies—from nature-derived coatings to flexible and ultrasmall electrode designs—that aim to blur the line between the biological and the electronic. While non-invasive interfaces remain the safest, their utility is limited by poor signal quality. The future of long-term, high-performance BCIs likely rests on the continued development of minimally invasive platforms and advanced biomaterials that can reliably overcome the biocompatibility challenge, finally enabling the stable and safe neural integration that has long been envisioned.
A central challenge in modern brain-computer interface (BCI) research lies in developing algorithms that can accurately decode user intention from neural signals. This process is fundamentally a translation problem—converting the brain's complex electrical activity into commands for external devices. The core of this challenge stems from the fact that brain activity is highly subject-specific, with neural population activity varying considerably between and even within subjects, making universal decoding algorithms difficult to build [46]. Decoding models must overcome what is known as negative transfer in machine learning, where increasing dataset diversity can sometimes degrade performance rather than improve it, leading to counterintuitive results where models trained on smaller datasets outperform those trained on larger ones [46].
The field has witnessed a significant evolution in decoding approaches, moving from simple linear models to sophisticated deep learning architectures. While early BCIs relied on relatively straightforward signal processing techniques, contemporary systems increasingly leverage artificial intelligence as a co-pilot to help infer user intent and complete tasks [34]. This partnership between neuroscience and machine learning has enabled researchers to tackle one of the most formidable challenges in neuroscience: understanding how the brain works by deciphering the neural code that transforms sensory input into perception, cognition, and adaptive behavior [47].
Fundamental Differences in Signal Acquisition and Their Algorithmic Implications
The choice between invasive and non-invasive neural interfaces fundamentally shapes the subsequent algorithmic approaches and decoding challenges. These two pathways offer dramatically different starting points for signal processing, with implications throughout the machine learning pipeline.
Table 1: Fundamental Characteristics of Invasive vs. Non-Invasive Neural Signals
| Characteristic | Invasive Signals (APs/LFPs) | Non-Invasive Signals (EEG) |
|---|---|---|
| Spatial Resolution | Single neuron to local networks (micrometers) | Large neuronal populations (centimeters) |
| Temporal Resolution | Millisecond precision (up to kHz) | Millisecond to tenths of seconds |
| Signal-to-Noise Ratio | High | Low to moderate |
| Primary Signal Source | Extracellular action potentials, local field potentials | Post-synaptic extracellular currents, primarily from pyramidal neurons |
| Brain Coverage | Localized to implanted regions | Whole cortex (adjacent to neurocranium) |
| Information Transfer Rate | High | Lower |
Invasive recordings provide access to extracellular action potentials (APs) and local field potentials (LFPs) that reflect input to, local processing, and output of cortical areas [16]. The signals contain information up to several kHz, offering a rich data stream for decoding algorithms [16]. In contrast, non-invasive electroencephalography (EEG) signals are dominated by fields of pyramidal neurons and are subject to significant attenuation and spatial distortion as they pass through cerebrospinal fluid, skull, and scalp [16]. Furthermore, tissue acts as a low-pass filter that generally attenuates high-frequency signals to the extent that buries them in background noise, limiting non-invasive analysis mainly to lower frequency neuronal activity [16].
These fundamental differences create distinct algorithmic hurdles. Invasive decoder development must contend with the challenges of chronic signal instability as electrodes can be affected by biological responses, while non-invasive approaches must overcome the low signal-to-noise ratio and significant preprocessing requirements before meaningful decoding can even begin [2] [16].
Figure 1: Comparative signal processing workflows for invasive and non-invasive neural interfaces, highlighting distinct algorithmic challenges at each stage.
Algorithmic Approaches for Invasive Neural Interfaces
Signal Processing Foundations
Invasive neural interfaces typically begin with spike sorting algorithms that separate action potentials from different neurons, followed by extraction of firing rates and local field potential features [16] [47]. The high dimensionality of neural data from multi-electrode arrays (containing up to 1024 electrodes in systems like Neuralink's N1 Implant) necessitates sophisticated dimensionality reduction techniques before decoding can occur [19]. The mathematical foundation for these decoding models can be represented as:
P(x|K) - The probability of a stimulus or intent x given observed neural activity K [47]
This fundamental statistical relationship drives the development of decoders that can predict behavior from neural population activity.
State-of-the-Art Performance and Applications
Invasive BCIs have demonstrated remarkable capabilities in clinical applications. The Brain Gate clinical trial—the largest and longest-running clinical BCI trial—reported positive safety results in patients with quadriparesis from spinal cord injury, brainstem stroke, and motor neuron disease [19]. Researchers have achieved speech decoding from cortical activity, enabling communication for paralyzed individuals, with some systems approaching performance levels comparable to conventional computer input methods [6]. Motor decoding for robotic arm control has enabled patients with paralysis to perform complex tasks, representing some of the most advanced applications of invasive decoding technology [2].
Table 2: Performance Benchmarks for Invasive Neural Decoding
| Application Domain | Performance Metric | Reported Performance | Technical Approach |
|---|---|---|---|
| Speech Decoding | Word decoding accuracy | >90% accuracy for 8-word classification [19] | Cortical implant with bespoke decoders |
| Motor Control | Robotic arm manipulation | Complex task completion (e.g., block moving) [34] [2] | Utah array with population decoding algorithms |
| Cursor Control | Target acquisition rate | Significant improvement over non-invasive approaches [2] | Intracortical signals with continuous decoding |
| Clinical Translation | Long-term viability | Positive safety results in long-term trials [19] | Chronic implants with adaptive decoding |
Algorithmic Approaches for Non-Invasive Neural Interfaces
Overcoming the Signal Quality Challenge
Non-invasive interfaces face the fundamental constraint of lower signal-to-noise ratio, which has driven innovation in signal processing and machine learning approaches. Researchers have developed several strategies to overcome these limitations:
AI as a co-pilot systems combine decoded brain signals with a camera-based artificial intelligence platform that interprets user direction and intent in real time [34]. This approach has demonstrated significant performance improvements, with one study showing that a paralyzed participant completed a robotic arm task in approximately six and a half minutes with AI assistance, whereas without it, he was unable to complete the task [34].
Surface electromyography (sEMG) represents an alternative non-invasive approach that measures electrical signals from muscles, which reflect motor commands from the central nervous system [6]. Recent advances in sEMG include the development of generic decoding models that generalize across people, achieving remarkable performance including handwriting at 20.9 words per minute without person-specific training [6].
Novel Algorithms for Cross-Subject Generalization
The problem of negative transfer in multi-subject brain decoding has driven the development of specialized algorithms. Researchers have created novel computational frameworks that minimize negative transfer by reframing source selection as a mixture model parameter estimation problem [46]. This approach allows each source subject to contribute through a continuous mixture weight rather than being outright included or excluded, achieving state-of-the-art performance while using 62% less training data [46].
Deep learning techniques have shown significant success in addressing cross-session and cross-user generalization challenges for sEMG systems [6]. By training neural networks on data from thousands of consenting human participants, researchers have developed models that perform well across people without person-specific training or calibration [6].
Table 3: Performance Benchmarks for Non-Invasive Neural Decoding
| Application Domain | Performance Metric | Reported Performance | Technical Approach |
|---|---|---|---|
| Handwriting Decoding | Words per minute (WPM) | 20.9 WPM [6] | sEMG wristband with deep learning |
| Gesture Classification | Accuracy for held-out participants | >90% accuracy [6] | sEMG with cross-subject models |
| Continuous Control | Target acquisitions per second | 0.66 acquisitions/sec [6] | Wrist-based sEMG continuous control |
| Discrete Gesture | Detections per second | 0.88 detections/sec [6] | sEMG with discrete gesture decoding |
| AI-Assisted BCI | Task completion time | 6.5 minutes with AI vs. unable to complete without [34] | EEG with computer vision co-pilot |
Figure 2: Scalable non-invasive decoding workflow emphasizing cross-subject generalization techniques.
Comparative Analysis: Performance and Applications
Direct Performance Comparison
When comparing invasive and non-invasive approaches, the performance differences reflect the fundamental trade-offs between signal quality and practicality. Invasive interfaces currently demonstrate superior performance in applications requiring high precision and bandwidth, such as complex robotic arm control and speech decoding [2] [16]. However, non-invasive approaches have made significant strides in applications where cross-subject generalization and ease of use are prioritized, such as in the sEMG-based handwriting system achieving 20.9 WPM [6].
The information transfer rates possible with invasive technologies remain substantially higher due to direct access to neural signals [16]. As one researcher notes, "the great opportunity offered by invasive BMIs thus lies in accurate control, a prerequisite for user acceptance, combined with restoration of somatosensation" [16]. However, non-invasive approaches benefit from lower barriers to adoption and the ability to leverage large-scale data collection from thousands of participants to build robust models [6].
Application-Specific Considerations
Different applications necessitate different approaches to the invasive versus non-invasive decision:
Clinical motor restoration for paralyzed individuals has seen remarkable advances with both approaches. Invasive systems have enabled control of robotic arms and patients' own arms through functional electrical stimulation [2], while non-invasive systems have demonstrated impressive control of exoskeletons and computer interfaces [34] [6].
Communication systems have progressed along both pathways, with invasive speech decoding achieving high accuracy for limited vocabularies [19], while non-invasive handwriting systems now offer competitive performance for general text entry [6].
Consumer applications remain primarily the domain of non-invasive systems due to safety and regulatory considerations, with EEG headsets available for under $100 for applications in meditation support, sleep monitoring, and focus enhancement [19].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Neural Decoding Research
| Item Category | Specific Examples | Function/Purpose |
|---|---|---|
| Recording Hardware | Utah arrays, Neuropixels, sEMG wristbands, EEG headsets | Signal acquisition from neural tissue or peripheral nervous system |
| Signal Processing | Open-source toolboxes (EEGLAB, BCILAB), custom algorithms | Preprocessing, artifact removal, feature extraction |
| Decoding Algorithms | Generalized Linear Models (GLMs), Deep Neural Networks, Mixture Models | Translating neural signals to intended outputs |
| Validation Frameworks | Closed-loop BCI tasks, Real-time performance metrics | System evaluation and iterative refinement |
| Data Collection | Anthropometrically diverse participant pools, Behavioral prompting systems | Training data acquisition for robust model development |
The field of neural decoding stands at an exciting crossroads, with both invasive and non-invasive approaches benefiting from advances in machine learning and artificial intelligence. Future progress will likely focus on several key areas:
Hybrid approaches that combine the strengths of multiple signal modalities may offer pathways to overcome individual limitations. The integration of AI co-pilot systems with traditional BCIs represents one such hybrid approach that has already demonstrated significant performance improvements [34].
Advanced algorithms that better handle the cross-subject and cross-session generalization problem will be crucial for wider adoption of both invasive and non-invasive technologies. Approaches that minimize negative transfer while leveraging large-scale datasets show particular promise [46].
Closed-loop systems that provide sensory feedback through intracortical microstimulation or other neuromodulation techniques may enhance decoding performance by creating more naturalistic control paradigms [16].
In conclusion, while invasive and non-invasive neural interfaces present distinct algorithmic and processing hurdles, both approaches continue to advance rapidly through innovative applications of machine learning and AI. The choice between approaches ultimately depends on the specific application requirements, balancing factors such as performance needs, safety considerations, and practical constraints. As decoding algorithms become increasingly sophisticated, we move closer to realizing the full potential of brain-computer interfaces for both clinical and consumer applications.
Wireless Systems, Miniaturization, and Power Management for Next-Generation NIs
The evolution of neural interfaces (NIs) is fundamentally reshaping the landscape of neuroscience research and neurotechnology development. A central theme in this progression is the shift from tethered, bulky systems toward miniaturized, wireless, and intelligent platforms. This transition is critical for enabling naturalistic studies in animal models and developing viable clinical brain-computer interfaces (BCIs) for human patients [48] [49]. The design of next-generation NIs necessitates careful consideration of the trade-offs between invasiveness and performance, balancing signal fidelity against surgical risk and long-term stability [2]. Researchers and drug development professionals must navigate a complex field where advancements in material science, wireless power transfer, and neural decoding algorithms converge to create increasingly sophisticated neural interfacing tools [22] [50]. This guide provides a comparative analysis of current wireless NI architectures, detailing their experimental validation, technical specifications, and suitability for various research and clinical applications, with a particular focus on the critical balance between invasive and non-invasive approaches.
Performance Comparison of Invasive vs. Non-Invasive Wireless Neural Interfaces
The choice between invasive and non-invasive neural interfaces involves significant trade-offs across multiple performance parameters. The table below summarizes key comparative metrics essential for experimental design and technology selection.
Table 1: Performance Comparison of Invasive vs. Non-Invasive Wireless Neural Interfaces
| Performance Parameter | Invasive Interfaces | Non-Invasive Interfaces |
|---|---|---|
| Spatial Resolution | Single neuron level (microns) [2] | ~1-2 cm (scalp EEG) [2] |
| Temporal Resolution | Millisecond (neural spiking) [2] | Millisecond (EEG) [19] |
| Signal-to-Noise Ratio (SNR) | High (direct neural recording) [2] | Low (attenuated by skull, scalp) [2] |
| Surgical Risk | High (requires craniotomy) [2] | None [2] |
| Long-Term Stability | Degrades over months/years (glial scarring) [50] [2] | Stable with proper electrode maintenance [51] |
| Typical Applications | Motor control restoration, high-fidelity speech decoding [2] [19] | Neuroimaging, basic BCIs, cognitive monitoring [2] [52] |
| Key Technological Examples | Utah Array (Blackrock), Stentrode (Synchron), N1 Implant (Neuralink) [22] [19] | High-density EEG headsets (Emotiv, NeuroSky), fNIRS, MEG [22] [51] |
| Information Transfer Rate (ITR) | High (>200 bits/min demonstrated) [2] | Low to Moderate (<100 bits/min typical) [2] |
The experimental implications of these differences are profound. Invasive systems, such as the Utah Array or Neuralink's N1 Implant, provide unparalleled data quality for decoding complex motor intentions and have enabled paralyzed individuals to control robotic arms and communicate via imagined handwriting [2] [19]. However, they face challenges related to long-term biocompatibility and signal stability due to the body's inflammatory response [50]. Non-invasive systems, primarily using electroencephalography (EEG), offer a safe and accessible platform for studying brain dynamics and developing BCIs for communication and rehabilitation [2] [52]. Their limitations in spatial resolution, however, restrict their ability to decode more nuanced neural representations without advanced signal processing and machine learning [53] [52].
Table 2: Market and Adoption Forecast (2025-2035) for Wireless Neural Interfaces
| Category | 2025 Market Estimate (USD) | 2035 Market Projection (USD) | CAGR (%) | Primary Drivers |
|---|---|---|---|---|
| Overall Market | 324.0 Million [51] | 1,334 Million [51] | 15.2 [51] | Rising neurological disorders, AI-powered decoding [51] |
| Invasive Segment | Not Specified | Not Specified | 15.4 [51] | Clinical BCIs for paralysis, communication [51] [19] |
| Non-Invasive Segment | ~40% Market Share [51] | Not Specified | Not Specified | Consumer wellness, research, neurorehabilitation [22] [51] |
| United States | Not Specified | Not Specified | 14.3 [51] | Strong R&D ecosystem, venture capital [51] |
| China | Not Specified | Not Specified | 15.5 [51] | Government investment in AI & digital health [51] |
Experimental Protocols for Validating Neural Interface Performance
Robust experimental methodologies are essential for quantitatively assessing and comparing the performance of different NI technologies. The following section outlines standard protocols for evaluating key aspects of system functionality, from neural decoding accuracy to closed-loop control.
Protocol 1: Neural Decoding Algorithm Benchmarking
Objective: To systematically compare the accuracy and computational efficiency of different neural decoding algorithms on a standardized dataset.
Methodology (as derived from large-scale comparative studies):
- Dataset: Utilize a large-scale EEG dataset with multiple subjects performing tasks such as motor imagery or inner speech. The dataset should be preprocessed to remove artifacts and normalized [54] [53].
- Signal Processing: Apply and compare multiple signal processing methods, including Artifact Subspace Reconstruction (ASR), Surface Laplacian Filtering, and standard Data Normalization [54].
- Feature Extraction: Implement diverse feature extractors such as Common Spatial Patterns (CSP), Independent Component Analysis (ICA), and Short-Time Fourier Transform (STFT) to transform raw neural signals into discriminative features [54].
- Classification: Train and evaluate multiple machine learning classifiers, including Support Vector Machines (SVM), Linear Discriminant Analysis (LDA), Convolutional Neural Networks (CNN), and Long Short-Term Memory (LSTM) networks [54] [52].
- Evaluation Metrics: The primary metric is Classification Accuracy. Secondary metrics should include Computational Load and Memory Storage Requirements to assess feasibility for real-time, embedded computing [54].
Workflow Diagram: The following diagram illustrates the hierarchical experimental workflow for benchmarking neural decoding algorithms.
Diagram 1: Neural Decoding Benchmarking Workflow
Protocol 2: Behavioral Impact of Wireless vs. Tethered Systems
Objective: To quantitatively assess the effects of tethering on animal behavior and data quality in preclinical studies.
Methodology (as derived from optogenetics studies):
- Animal Model: Use a cohort of rodents (e.g., mice) expressing light-sensitive opsins in targeted neural circuits.
- Experimental Groups: Divide subjects into two groups: one using a traditional tethered optical fiber and another using a miniaturized, wireless, battery-free optogenetic device [48].
- Behavioral Paradigm: Subject all animals to a standardized behavioral battery in an open-field enclosure, including tests for social interaction, general mobility, and anxiety-like behaviors (e.g., time spent in the center vs. periphery) [48].
- Data Analysis:
- Behavioral Metrics: Measure total distance traveled, average velocity, time engaged in social interaction, and time spent in the center zone.
- Neural Data Quality: Record and compare the signal-to-noise ratio of neural recordings or the consistency of stimulation-evoked behaviors between groups [48] [49].
Key Findings from Prior Studies: Comparative studies have demonstrated that mice using wireless devices exhibit significantly increased social interaction (approximately 21 seconds vs. 14 seconds in tethered), greater total mobility (~100 meters vs. ~75 meters), and higher average velocity (~9 cm/s vs. ~6 cm/s), indicating reduced anxiety and more naturalistic behavior [48].
Technical Specifications and Power Management Architectures
The core of next-generation NIs lies in their miniaturization and innovative power solutions. The following table details the key components that form the "research reagent solutions" for building and testing these advanced systems.
Table 3: Research Reagent Solutions for Next-Generation Neural Interfaces
| Component Category | Specific Example / Material | Function & Rationale |
|---|---|---|
| Substrate/Encapsulation | Polyimide, Parylene, Polydimethylsiloxane (PDMS) [48] [50] | Provides flexible, stretchable, and biocompatible support for electronics, reducing mechanical mismatch with neural tissue. |
| Conductive Elements | Iridium Oxide, PEDOT:PSS, Graphene, Carbon Nanotubes [48] [50] | Forms low-impedance electrodes for recording and stimulation. Conjugated polymers and nanomaterials improve flexibility and charge injection capacity. |
| Power Source | Radio-Frequency (RF) Harvesting, Ultrasound Harvesting [48] [49] | Enables battery-free operation through remote wireless power transfer, critical for long-term implantation and miniaturization. |
| Core Chip Technology | Custom ASICs (Application-Specific Integrated Circuits) [19] | Miniaturizes control, data processing, and wireless transmission functions while maintaining ultra-low power consumption. |
| Neural Probes | Flexible penetrating probes (e.g., Neuropixels), Stentrode [2] [19] | Allows for high-density neural recording with minimal tissue damage (flexible probes) or minimally invasive implantation (endovascular Stentrode). |
| Decoding Software | EEGNet, Spectro-temporal Transformers (e.g., NeurIPT) [53] [52] | AI models for translating raw neural signals into commands or interpretations. Transformers show promise in handling long-range dependencies in EEG. |
Wireless and Battery-Free System Architecture
Fully implantable, battery-free devices represent the cutting edge of NI miniaturization. These systems rely on remote wireless power transfer via far-field radio frequency (RF) or near-field ultrasonic energy harvesting [48] [49]. This approach eliminates the need for bulky batteries, which are a major limiting factor for device size and longevity. The harvested power runs ultra-low-power microchips that manage neural signal acquisition (recordings) and delivery of stimuli (electrical, optical, or pharmacological). Processed data is then transmitted back to an external receiver via backscatter communication, a very low-power method of wireless data transfer [48]. The following diagram illustrates this integrated architecture.
Diagram 2: Battery-Free Implantable NI Architecture
The field of neural interfacing is advancing along several parallel trajectories. In the short term, the proliferation of miniaturized and wireless devices will continue to enhance the quality of behavioral neuroscience data by minimizing confounds [48] [49]. For clinical applications, the focus is on improving the long-term biocompatibility and stability of invasive implants through the use of flexible substrates and advanced electrode materials that mitigate the foreign body response [50].
The most transformative trend, however, is the deep integration of Artificial Intelligence (AI). Foundation models like NeurIPT, pre-trained on vast, diverse EEG datasets, are demonstrating remarkable generalization across different tasks and patient populations, addressing the critical challenge of inter-subject variability [53]. These models leverage sophisticated architectures, such as Amplitude-Aware Masked Pretraining (AAMP) and Progressive Mixture-of-Experts (PMoE), to learn robust representations of neural activity [53]. Furthermore, AI is enabling closed-loop neuromodulation systems that can adapt stimulation parameters in real-time based on sensed neural states, opening new frontiers for treating neurological and psychiatric disorders with unprecedented precision [50] [19].
In conclusion, the comparative analysis of invasive and non-invasive wireless NIs reveals a dynamic and rapidly evolving technological landscape. The choice between these platforms is not a matter of superiority but of application-specific suitability. Invasive interfaces offer unmatched fidelity for restoring complex motor and communication functions in severe paralysis, while non-invasive systems provide a safe, scalable pathway for basic research, cognitive monitoring, and consumer neurotechnology. The continued convergence of materials science, wireless engineering, and artificial intelligence promises to further blur the lines between these categories, leading to a future where seamless, robust, and bidirectional communication with the nervous system is a standard tool for both scientific discovery and clinical intervention.
Performance Benchmarking, Ethical Considerations, and Regulatory Pathways
The evolution of Brain-Computer Interfaces (BCIs) has bifurcated into two primary technological pathways: invasive and non-invasive systems. This comparative analysis objectively evaluates their performance along two critical dimensions: information transfer rate (ITR) and control dimensionality. These metrics directly determine a BCI's capability to restore complex functions for individuals with paralysis or neuromuscular disorders. Invasive BCIs, which require surgical implantation, are often reported to offer higher signal fidelity, while non-invasive approaches provide greater accessibility and safety [55]. This guide synthesizes recent experimental data and methodological approaches to provide researchers and clinicians with a clear, evidence-based framework for technology selection and evaluation.
Performance Metrics Comparison
Quantitative Performance Benchmarks
Table 1: Direct Performance Comparison of Invasive and Non-Invasive BCIs
| Performance Metric | Invasive BCIs | Non-Invasive BCIs | Notes & Context |
|---|---|---|---|
| Information Transfer Rate (ITR) | Up to 99% accuracy for speech decoding [33]; ~56 words per minute for text communication [33] | 20.9 words per minute for handwriting via sEMG [6]; Robotic finger control at 80.56% accuracy (binary) and 60.61% (ternary) [56] | Invasive ITR enables full-time communication; Non-invasive ITR is sufficient for discrete commands and slower typing |
| Control Dimensionality | High-dimensional control of computer cursors, robotic arms, and individual prosthetic fingers [2] [33] | Individual robotic finger control [56]; 9 distinct gestures via sEMG [6]; Continuous 1D navigation [6] | Invasive: Direct neural population decoding; Non-invasive: Decoding from musculature or scalp signals |
| Signal-to-Noise Ratio (SNR) | High (direct neural recording) [2] [16] | Lower (attenuated by skull, scalp) [2] [16] | Fundamental physical difference impacts all downstream decoding |
| Spatial Resolution | Single-neuron level (e.g., Utah Array, Neuralink) [2] [57] | Centimeter-scale (EEG) [2] [16]; Millimeter-scale (high-density sEMG) [6] | Invasive resolution allows decoding of fine-grained motor commands |
| Temporal Resolution | Millisecond (neural spiking) [2] | Millisecond (EEG) to second-scale (fNIRS) [22] [2] | Both EEG and invasive electrical methods offer fast response times |
| Typical Application Latency | <100 milliseconds for movement tasks [57] | Real-time for robotic control [56] | Sufficient for closed-loop control in both paradigms |
Key Research Reagent Solutions
Table 2: Essential Research Materials and Experimental Platforms
| Item / Platform | Function in BCI Research | Example Use Case |
|---|---|---|
| Utah Array / Blackrock Neurotech | Records multi-unit activity and local field potentials from cortex [2] [16] | Control of robotic arms, speech decoding [2] |
| Neuralink N1 Implant | 1024-channel fully implantable wireless device for intracortical recording [57] | PRIME Study: Cursor control in quadriplegic patients [57] |
| Synchron Stentrode | Endovascular ECoG electrode array implanted in superior sagittal sinus [2] [57] | SWITCH/COMMAND Trials: Digital interface control for paralysis [57] |
| High-Density sEMG Band | Records surface EMG signals from wrist muscles for gesture decoding [6] | Generic neuromotor interface for handwriting and gesture control [6] |
| 64-Channel EEG Cap | Records scalp potentials for non-invasive neural decoding [58] [56] | Real-time robotic hand control at individual finger level [56] |
| AI Copilot (CNN-Kalman Filter) | Decodes noisy non-invasive signals and provides shared autonomy [58] | Improved BCI performance 3.9x for paralyzed user [58] |
| Intracortical Microstimulation (ICMS) | Provides artificial somatosensory feedback via microelectrode stimulation [33] | Restoring touch sensation in prosthetic control [33] |
Experimental Protocols and Methodologies
Invasive BCI Protocol: Chronic Intracortical Recording for Communication
Objective: To evaluate the long-term stability and performance of an implanted BCI for speech and cursor control in a paralyzed individual [33].
Participant Profile: Single participant with amyotrophic lateral sclerosis (ALS) enrolled in the BrainGate2 trial.
Device & Implantation: Four microelectrode arrays (256 electrodes total) surgically implanted in the left ventral precentral gyrus [33].
Data Acquisition & Processing:
- Neural Recording: Continuous monitoring of single-unit and multi-unit activity.
- Signal Processing: Custom algorithms for spike sorting and feature extraction.
- Decoding Model: Machine learning models mapping neural activity to intended speech or cursor movement.
- Output: Text generation and computer cursor control.
Performance Metrics: Word output accuracy (% correct), words per minute (WPM), hours of independent use.
Key Findings: The system achieved 99% word accuracy and ~56 WPM over 4,800 hours of use, enabling full-time work and communication without daily recalibration [33].
Invasive BCI Experimental Workflow
Non-Invasive BCI Protocol: sEMG-Based Generic Neuromotor Interface
Objective: To develop a non-invasive interface that generalizes across users without per-person calibration for computer input tasks [6].
Participant Profile: 162-6,627 anthropometrically diverse participants across studies.
Device & Setup: Dry-electrode, multichannel sEMG wristband (sEMG-RD) with 2 kHz sample rate, low-noise (2.46 μVrms), wireless Bluetooth connectivity [6].
Experimental Tasks:
- Wrist Control: Continuous cursor control using wrist angles.
- Discrete Gesture Detection: Nine distinct finger gestures and thumb swipes.
- Handwriting: Imaginary writing of prompted text.
Data Collection & Processing:
- Signal Acquisition: High-density sEMG recording from wrist muscles.
- Time Alignment: Algorithm to align prompt labels with actual gesture times.
- Model Training: Neural networks trained on data from thousands of participants.
- Generalization Testing: Cross-user performance evaluation without personalization.
Performance Metrics: Target acquisitions per second, gesture detections per second, words per minute for handwriting.
Key Findings: The system achieved 0.66 target acquisitions/sec, 0.88 gesture detections/sec, and 20.9 WPM with out-of-the-box generalization across users [6].
Non-Invasive BCI Experimental Workflow
Technical and Clinical Considerations
Signal Acquisition Pathways
The fundamental difference between invasive and non-invasive approaches lies in their signal acquisition pathways, which directly impacts resulting performance characteristics [16].
Invasive Pathway: Microelectrodes directly record action potentials and local field potentials from cortical neurons. This provides high-frequency neural data (up to several kHz) with minimal attenuation or distortion from intervening tissues [2] [16]. Signals reflect input to, local processing within, and output from cortical areas, enabling decoding of detailed movement parameters and intentions.
Non-Invasive Pathway: Scalp electrodes (EEG) detect synchronized post-synaptic potentials that have been attenuated by skull and scalp tissues, which act as a low-pass filter [16]. Surface EMG records electrical signals from muscles, which represent the final output of the motor system after neural processing [6]. Both methods face inherent limitations in spatial resolution and signal-to-noise ratio compared to invasive approaches.
Signal Acquisition Pathways Comparison
Clinical Translation and Adoption Factors
The choice between invasive and non-invasive BCI approaches involves balancing performance against practical clinical considerations:
Risk-Benefit Profile: Invasive systems require neurosurgical implantation with associated risks, but offer higher performance for severely disabled users [33] [57]. Non-invasive systems have minimal risk but currently provide more limited functionality [6].
Long-Term Stability: Recent data demonstrates impressive longevity for both approaches. Invasive systems have shown stable function over years, with one ICMS study reporting reliable operation over 10 years [33]. Non-invasive systems benefit from easy replacement and upgrades without surgical intervention.
User Acceptance and Accessibility: Non-invasive BCIs have broader potential application beyond medical uses, extending to consumer, wearable, gaming, and general human-computer interaction markets [58]. Invasive interfaces remain primarily focused on medical applications for patients with severe disabilities.
The direct performance comparison between invasive and non-invasive BCIs reveals a consistent trade-off: invasive systems provide superior information transfer rates and control dimensionality, while non-invasive approaches offer greater accessibility and faster implementation. Invasive BCIs currently enable high-bandwidth communication and complex device control that approaches natural interaction speeds, with recent studies demonstrating 99% accuracy for speech decoding and long-term stability over years [33]. Non-invasive alternatives have made significant advances through sophisticated signal processing and AI augmentation, achieving robotic finger control and hands-free writing at practically useful speeds [6] [56].
The optimal choice depends fundamentally on the clinical or research context. For patients with severe paralysis requiring high-performance communication and environmental control, invasive systems may justify their surgical risks. For applications requiring moderate control dimensionality or broader accessibility, non-invasive interfaces present a compelling alternative. Future directions include the development of minimally invasive technologies that bridge this performance gap, hybrid systems that combine multiple signal modalities, and continued refinement of AI-driven decoding algorithms to enhance both approaches.
Analyzing User Acceptance, Surgical Risks, and Long-Term Reliability
The field of neural interfaces, often referred to as brain-computer interfaces (BCIs), is rapidly advancing, offering potential breakthroughs in restoring function for patients with neurological disorders and augmenting human capabilities. These systems can be broadly categorized as invasive, requiring surgical implantation into the brain, or non-invasive, utilizing external sensors to measure brain activity from the scalp [59] [17]. The choice between these pathways represents a fundamental trade-off between signal fidelity and clinical risk, a balance that is critical for researchers, clinicians, and developers to understand. This guide provides a comparative analysis of invasive and non-invasive neural interfaces, focusing on the core research considerations of user acceptance, surgical risks, and long-term reliability, supported by current experimental data and protocols.
Comparative Analysis: Core Performance Metrics
The following tables summarize key quantitative and qualitative differences between invasive and non-invasive neural interfaces across critical performance and risk parameters.
Table 1: Comparison of Key Performance and User Acceptance Metrics
| Metric | Invasive BCIs | Non-Invasive BCIs |
|---|---|---|
| Spatial Resolution | High (single neuron possible) [2] | Low (neural population-level) [2] |
| Temporal Resolution | Very High (milliseconds) | High (milliseconds) |
| Signal-to-Noise Ratio | High [17] | Lower, susceptible to noise [17] [2] |
| Typical Signal Modalities | Single/Multi-Unit Activity, Local Field Potentials (LFPs) [2] | Electroencephalography (EEG), functional Near-Infrared Spectroscopy (fNIRS), Magnetoencephalography (MEG) [59] [22] [2] |
| Information Transfer Rate | Potentially very high (e.g., for speech decoding) [2] | Lower, limited by signal fidelity [2] |
| Clinical Acceptability (Rehabilitative Use) | >80% among neurosurgical teams [60] | Generally high due to safety profile |
| Acceptability for Augmentation in Healthy Populations | Divides opinion among clinicians [60] | Generally higher, seen as more appropriate |
Table 2: Comparison of Surgical Risks and Long-Term Reliability
| Factor | Invasive BCIs | Non-Invasive BCIs |
|---|---|---|
| Surgical Risk Profile | Intracranial: Risk of bleeding, infection, tissue damage [60] [61] | No surgical risk [17] |
| Procedural Terminology | Intracranial (within skull) or Embedded (penetrative, not deeper than skull's inner table) [61] | Non-invasive [61] |
| Immune Response | Significant; leads to foreign body response, glial scarring, and signal degradation over time [62] | Not applicable |
| Primary Failure Modes | - Mechanical/Technical: Insulation failure, wire breakage, electrode degradation [62]- Biological: Encapsulation, chronic inflammation [62]- Electronic: Battery depletion, housing pressure sores [62] | - Low signal quality- Environmental noise interference- User discomfort during extended wear |
| Typical Longevity in Humans | Years to decades for some devices (e.g., DBS, Cochlear Implants) [62]; BCI recording quality can degrade in shorter timeframes [62] | Indefinite, subject to device hardware lifespan |
| Key Long-Term Challenges | Maintaining signal quality and stability amidst biological encapsulation; requires revision surgeries for battery/power [62] | Improving signal clarity and developing robust algorithms that compensate for low signal-to-noise ratio [17] [2] |
Experimental Protocols for Assessing Neural Interfaces
To generate the comparative data summarized above, the field relies on standardized experimental methodologies. Below are detailed protocols for key areas of investigation.
Protocol for Assessing Surgical Team Acceptability
Objective: To quantify the perceptions and acceptability of invasive BCIs among the neurosurgical teams responsible for their implantation.
Methodology (Based on a published international survey) [60]:
- Study Design: A two-stage, cross-sectional, mixed-methods survey.
- Participants: Members of the neurosurgical team, including neurosurgeons, anesthetists, and operating room nurses. The quantitative survey gathered 538 responses from 32 countries.
- Qualitative Stage: Initial open-ended questions assessed baseline understanding and attitudes. Responses were thematically analyzed to identify key concerns (e.g., stability, ethical implications) and potential benefits.
- Quantitative Stage: A structured survey was developed using themes from the first stage. Participants were presented with specific case vignettes (e.g., BCI for stroke rehabilitation, communication, military augmentation) and asked to rate their responses on a 5-point Likert scale.
- Key Metrics:
- "Do you agree or disagree that this is an appropriate use of BCI?"
- "Would you be happy to be involved as a member of the surgical team in this example?"
- Data Analysis: Quantitative data were analyzed using non-parametric inferential statistics (Mann-Whitney U, Kruskal-Wallis tests) to compare responses between groups (e.g., by occupation).
Protocol for Evaluating Long-Term Reliability of Implanted Systems
Objective: To characterize the failure modes and longevity of implanted neural interfaces in chronic in vivo settings.
Methodology (Based on a comprehensive review of clinical devices) [62]:
- Component-Level Analysis: Systematically examine each component of the implanted system for potential failure modes:
- Electrodes: Electrochemical impedance spectroscopy to track changes at the tissue-electrode interface. Histological analysis post-explantation to assess glial scarring and neuronal loss.
- Lead Wires: Mechanical fatigue testing (in vitro and in vivo) for breakage; inspection of insulation for cracks or degradation.
- Pulse Generator/DAQ: Monitor battery life and electronic failure rates. Track incidence of skin erosion, pressure sores, or infection at the implant site.
- Packaging: Conduct accelerated aging tests to validate hermeticity and prevent moisture ingress.
- Biological Response Monitoring: Use non-invasive imaging (MRI, CT) and/or terminal histology to quantify the extent of the foreign body response, including fibrosis and chronic inflammation.
- Functional Performance Tracking: In recording BCIs, monitor metrics like the number of recordable units, signal-to-noise ratio, and single-unit yield over time. In stimulating BCIs, track the stability of impedance and the efficacy of the therapeutic effect.
- Data Synthesis: Correlate technological and biological findings with clinical outcomes to determine the primary reasons for loss of efficacy or explantation.
Protocol for Benchmarking Non-Invasive BCI Performance
Objective: To evaluate the decoding performance and information transfer rate of non-invasive BCIs for complex control tasks.
Methodology (Based on state-of-the-art EEG-based systems) [2]:
- Signal Acquisition: Apply high-density EEG caps (e.g., 64-128 channels) following the international 10-20 system. Use commercial amplifiers with high sampling rates and synchronized data logging.
- Paradigm Design: Implement established BCI paradigms:
- Motor Imagery (MI): Participants imagine movements of specific limbs (e.g., left hand vs. right hand) without executing them. The associated Event-Related Desynchronization/Synchronization (ERD/ERS) in the sensorimotor cortex is the target signal.
- Event-Related Potentials (P300): Participants focus on rare target stimuli within a rapid sequence of non-target stimuli, eliciting a detectable P300 waveform.
- Signal Processing & Decoding:
- Preprocessing: Apply band-pass filters and artifact removal techniques (e.g., Independent Component Analysis) to mitigate noise from eye blinks and muscle movement.
- Feature Extraction: Calculate signal features such as band power for MI or temporal waveforms for P300.
- Classification: Employ machine learning algorithms (e.g., Common Spatial Patterns, Riemannian geometry, or deep learning models) to decode the user's intention from the features.
- Performance Metrics: Quantify accuracy, bit rate (bits per minute), and F1 score for closed-loop control tasks, such as controlling a robotic arm or a computer cursor.
Visualization of Neural Interface Technologies and Signal Pathways
The following diagrams illustrate the core concepts and data pathways in neural interface technologies.
The Scientist's Toolkit: Research Reagents & Essential Materials
This table details key materials and technologies used in neural interface research, providing a foundation for experimental design.
Table 3: Essential Research Tools for Neural Interface Development
| Item | Function/Application | Key Characteristics |
|---|---|---|
| Utah Array | Invasive recording; multi-unit activity from cortex [2] | Multi-electrode array with penetrating shanks; clinical and research use. |
| Neuropixels Probe | Invasive recording; large-scale, high-density single-unit recording [2] | CMOS-based probe with thousands of recording sites; primarily for research. |
| WIMAGINE Implant | Minimally invasive ECoG recording; chronic BCI for motor control [2] | Implantable ECoG grid with wireless data/power transfer. |
| Stentrode | Minimally invasive recording; endovascular BCI [63] [2] | Stent-based electrode array deployed in cortical blood vessels. |
| High-Density EEG System | Non-invasive recording; scalp-level brain potentials [2] | 64+ channel caps with high-quality amplifiers; standard for non-invasive BCI. |
| Dry EEG Electrodes | Non-invasive recording; improved usability [22] | Eliminate need for conductive gel; target for consumer and long-term use. |
| OpenBCI & BCI Toolboxes | Signal acquisition and processing [2] | Open-source software (e.g., BCILAB, MOABB) and hardware for accessible BCI research. |
| Functional Ultrasound (fUS) | Minimally invasive imaging; hemodynamic-based brain activity mapping [2] | Provides high-resolution neural activity readout; requires cranial window. |
The choice between invasive and non-invasive neural interfaces is not a matter of declaring a superior technology, but of aligning technology with application-specific requirements and risk-benefit calculations. Invasive BCIs offer unparalleled signal resolution for complex tasks like dexterous prosthetic control or speech decoding, but this comes at the cost of significant surgical risks and non-trivial long-term reliability challenges related to biocompatibility and device failure [62] [63]. Non-invasive BCIs provide a safe, accessible, and rapidly deployable platform, making them ideal for rehabilitation, basic research, and initial forays into consumer applications, though they are fundamentally limited by lower signal fidelity [17] [2].
The future of the field lies not in these approaches competing, but in their parallel evolution. Research continues to make invasive interfaces safer and more stable through novel materials and less invasive surgical techniques [61] [62]. Simultaneously, advances in signal processing and machine learning are steadily improving the performance of non-invasive systems [2]. For researchers and clinicians, this comparative analysis underscores the necessity of a deliberate, evidence-based approach to technology selection, guided by the intended user population, the specific functional outcome desired, and a clear-eyed assessment of the associated risks and long-term viability.
Navigating the Ethical and Regulatory Landscape for Clinical and Consumer NIs
Neural interfaces (NIs) represent a transformative technology that enables direct communication between the nervous system and external devices. These systems are broadly categorized as invasive, requiring surgical implantation, or non-invasive, utilizing external sensors [17]. The field stands at a critical juncture, balancing rapid technological advancement against complex ethical and regulatory considerations. As commercial applications expand beyond clinical settings to consumer markets, understanding this landscape becomes imperative for researchers, developers, and policymakers [64].
The fundamental distinction between interface types lies in their proximity to neural tissue. Invasive interfaces penetrate the brain parenchyma or rest on its surface, while non-invasive alternatives measure signals through the skull and scalp [8]. This physical difference creates inherent trade-offs between signal fidelity and procedural risk that ripple through ethical and regulatory frameworks.
Technical Performance Comparison
Signal Characteristics and Information Transfer
Table 1: Performance Characteristics of Invasive vs. Non-Invasive Neural Interfaces
| Parameter | Invasive NIs | Non-Invasive NIs |
|---|---|---|
| Spatial Resolution | Micrometer scale (single neurons) [8] | Centimeter scale (neuronal populations) [8] |
| Temporal Resolution | Millisecond precision (up to kHz range) [8] | Limited by signal filtering (<~90 Hz for meaningful analysis) [8] |
| Signal-to-Noise Ratio | High (direct neural contact) [8] | Low (attenuated by skull, scalp) [8] [65] |
| Primary Signal Sources | Action potentials (APs), local field potentials (LFPs) [8] | Post-synaptic currents, surface EMG [8] [6] |
| Information Transfer Rate | Theoretically high, but limited by decoding challenges [65] | Lower, but recently demonstrated up to 20.9 WPM for handwriting [6] |
| Signal Path Distortion | Minimal (direct measurement) [8] | Significant (multiple tissue layers cause spatial smearing) [8] |
| Neuronal Population Sampled | Limited cortical areas but specific cell types [8] | Large-scale activity but dominated by pyramidal neurons [8] |
Representative Performance Data from Current Platforms
Table 2: Performance Metrics of Contemporary Neural Interfaces
| Platform/Company | Interface Type | Key Performance Metrics | Primary Applications |
|---|---|---|---|
| Neuralink [27] | Invasive (intracortical) | 5 human patients (as of 2025) controlling digital devices | Severe paralysis, communication |
| Synchron Stentrode [27] | Minimally invasive (endovascular) | Patients texting via thought; no serious adverse events at 12 months | Paralysis, motor restoration |
| Precision Neuroscience [27] | Minimally invasive (cortical surface) | FDA 510(k) clearance for up to 30-day implantation (April 2025) | Communication for ALS patients |
| Surface EMG Wristband [6] | Non-invasive (sEMG) | 20.9 WPM handwriting; 0.66 targets/sec continuous navigation | Human-computer interaction |
| Research EEG Systems [8] | Non-invasive (scalp EEG) | Lower performance than invasive signals but safe for broad use | Basic communication, gaming |
Experimental Methodologies
Signal Acquisition Protocols
Key Research Reagents and Materials
Table 3: Essential Research Materials for Neural Interface Studies
| Item | Function | Example Specifications |
|---|---|---|
| Multi-electrode Arrays | Records extracellular potentials from neuronal ensembles [8] [27] | Utah arrays (Blackrock): 96 electrodes, 1.5mm length; Custom designs: 421+ electrodes [27] |
| High-Density EEG Systems | Measures scalp potentials via electrode caps [8] | 64-256 channels, dry/wet electrodes, 2kHz sampling rate [8] [6] |
| Surface EMG Sensors | Records muscle electrical activity as proxy for motor commands [6] | Wristband form factor, 2.46 μVrms noise, 2kHz sampling [6] |
| Neural Signal Processors | Real-time signal filtering, spike sorting, and feature extraction [8] | Custom ASICs or FPGA-based, processing delays <100ms [8] |
| Biocompatible Substrates | Encapsulation for chronic implants to minimize immune response [64] | Flexible polymers (e.g., polyimide), ceramic packages [27] [64] |
| Calibration Software | Aligns neural signals with behavioral tasks for decoder training [6] | Time-alignment algorithms, prompt-response labeling systems [6] |
Decoding Methodologies
The translation of neural signals into commands involves sophisticated decoding pipelines. For invasive systems, algorithms typically extract movement parameters (direction, velocity, grip force) from combinations of single-unit activity and LFPs [8]. The brain's remarkable plasticity enables users to learn to control BCIs through closed-loop feedback, gradually improving performance as neural tuning adapts to the device [8].
Non-invasive systems increasingly leverage large-scale datasets and deep learning. For example, the surface EMG platform achieving 20.9 WPM handwriting recognition was trained on data from "thousands of consenting participants" [6]. This data-driven approach enables generic models that generalize across users without individual calibration, though personalization can further improve performance by 16% [6].
Ethical Considerations
Risk-Benefit Analysis by Interface Type
Table 4: Ethical Risk Profile Comparison of Neural Interfaces
| Consideration | Invasive NIs | Non-Invasive NIs |
|---|---|---|
| Physical Risks | Surgical complications (infection, bleeding); tissue damage; immune response [64] | Minimal physical risk; potential skin irritation [17] |
| Long-Term Safety | Device degradation; scar tissue formation; unknown long-term effects [64] | Well-established safety profile [17] |
| Informed Consent | "Coercive optimism" may undermine autonomy for desperate patients [64] | Lower stakes enable more voluntary participation [64] |
| Privacy Concerns | Direct access to neural data revealing thoughts, emotions, intentions [64] | Indirect inference of mental states; still reveals sensitive data [66] |
| User Acceptance | Lower due to medical concerns and surgery [8] | Higher; present commercial NIs are all non-invasive [8] |
| Equity of Access | High cost limits availability; primarily research subjects currently [64] | Potentially lower cost and broader distribution [6] |
Neural Data Privacy and Commodification
The sensitive nature of neural data raises unprecedented privacy concerns. Neural information can reveal "mental health conditions, emotional states, and cognitive patterns" even when anonymized [66]. This creates risks of discrimination, manipulation, and exploitation if adequate safeguards are not implemented [64].
The process of neural commodification - transforming intimate brain activity into economic goods - prioritizes market value over individual autonomy and mental privacy [64]. This is particularly problematic in employment contexts, where employers might use neurotechnology to monitor productivity, fatigue levels, or cognitive states without adequate worker protections [67].
Regulatory Frameworks
Current Regulatory Landscape
Emerging Legislation and Standards
The MIND Act of 2025 (Management of Individuals' Neural Data Act) represents a significant federal response to neural data privacy concerns. The proposed legislation directs the FTC to study neural data processing and identify regulatory gaps, with a report due to Congress within one year [67]. The Act adopts a broad definition of neural data encompassing both central and peripheral nervous system information [67].
At the state level, California and Colorado have amended their privacy laws to explicitly include neural data as sensitive information, though with important definitional differences [66]. Colorado requires opt-in consent for neural data collection, while California provides only a limited right to opt-out [66]. This patchwork approach creates compliance challenges for companies operating across multiple jurisdictions.
Commercialization and Future Directions
Market Outlook and Adoption Barriers
The addressable market for clinical NI applications is substantial, with approximately 5.4 million people in the United States living with paralysis that could benefit from these technologies [27]. Current commercial activity is concentrated in the non-invasive sector, though multiple invasive platforms are advancing through clinical trials [27].
Barriers to widespread adoption differ significantly between interface types. For invasive systems, the primary challenges include surgical risk, long-term biocompatibility, and user acceptance [64]. Non-invasive systems face hurdles related to signal quality, generalization across users, and real-world robustness [6]. Both approaches must contend with emerging regulatory requirements and ethical concerns that could impact development timelines and market entry.
Responsible Innovation Framework
Responsible commercialization of neural interfaces requires proactive measures including:
- Transparent Governance: Developing clear accountability structures for neural data handling and use [64]
- Public Engagement: Meaningful dialogue with diverse stakeholders to align development with societal values [64]
- Ethical by Design: Integrating privacy, security, and ethical considerations into product development from inception [64]
- Beneficial Use Categorization: Identifying and promoting applications that serve public interest and improve quality of life [67]
The rapid pace of neurotechnology innovation necessitates flexible governance approaches that can adapt to emerging challenges while fostering beneficial applications for patients and consumers alike.
The comparative analysis of invasive and non-invasive neural interfaces reveals a field characterized by fundamental trade-offs. Invasive technologies offer superior signal quality and specificity for high-performance clinical applications but face significant ethical and regulatory hurdles related to safety and permanence. Non-invasive approaches provide greater accessibility and lower risk profiles but currently deliver more limited performance for complex control tasks.
The ethical and regulatory landscape is evolving rapidly, with neural data privacy emerging as a central concern across interface types. The patchwork of state regulations and proposed federal frameworks reflects growing recognition of the unique sensitivities of neural information. Researchers and developers must navigate this complex environment while maintaining focus on responsible innovation that prioritizes user welfare and societal benefit.
As the technology continues to advance, the distinction between invasive and non-invasive interfaces may blur with the development of intermediate approaches such as endovascular and minimally invasive cortical surface technologies. Whatever the technical trajectory, maintaining public trust through ethical development practices and robust privacy protections will be essential for realizing the full potential of neural interfaces to restore function and enhance human capabilities.
The field of neural interfaces is undergoing a transformative period, marked by a dynamic competition between invasive and non-invasive technologies. This ecosystem is fueled by significant investment and a clear medical imperative: to restore functions like movement and communication to millions of people living with paralysis and other neurological conditions [27] [45]. As of 2025, the global brain-computer interface (BCI) market is forecast to grow to over $1.6 billion by 2045, representing a compound annual growth rate (CAGR) of 8.4% since 2025 [22]. This growth is driven by a blend of established medical device companies, ambitious start-ups, and tech giants, all vying to overcome the fundamental trade-off between signal fidelity and invasiveness. This article provides a comparative analysis of the current competitive and research landscape, offering scientists and drug development professionals a clear overview of the technologies, key players, and experimental methodologies shaping the future of neurotechnology.
The Competitive Ecosystem: A Company Landscape
The neural interface market is a vibrant and rapidly evolving space, characterized by players employing distinct technological strategies. The table below summarizes the key companies, their technological approaches, and their developmental status.
Table 1: Key Players in the Neural Interface Competitive Landscape
| Company | Technology Approach | Key Differentiator | Development Stage (as of 2025) |
|---|---|---|---|
| Neuralink [27] [45] | Invasive (Intracortical) | Ultra-high-bandwidth implant with thousands of electrodes threaded into the cortex by a robotic surgeon. | First human clinical trials ongoing; at least five participants implanted. |
| Blackrock Neurotech [27] [19] | Invasive (Intracortical) | Pioneering Utah Array; extensive human experience. Developing new flexible lattice electrode (Neuralace). | Decades of human implantation in research; expanding trials, including in-home use. |
| Paradromics [27] | Invasive (Intracortical) | High-channel-count implants (Connexus BCI) for ultra-fast data transmission, focused on speech restoration. | First-in-human recording completed; planning full clinical trial for late 2025. |
| Precision Neuroscience [27] [45] | Minimally Invasive (ECoG) | Ultra-thin "brain film" electrode array placed on the brain's surface without penetrating tissue. | FDA 510(k) clearance for temporary (up to 30 days) cortical interface. |
| Synchron [27] [19] | Minimally Invasive (Endovascular) | Stentrode delivered via blood vessels, avoiding open-brain surgery. | Implanted in 10 patients across trials; demonstrated control of Apple Vision Pro. |
| Non-Invasive sEMG Interface [6] | Non-Invasive (Surface Electromyography) | A generic, high-performance interface using a wristband to decode neuromuscular signals for computer control. | Research stage; demonstrated high-performance, out-of-the-box generalization across users. |
The competitive dynamics are further clarified by analyzing key business metrics. The broader MedTech industry, which encompasses neural interfaces, recorded its seventh successive year of growth in 2025, reaching $584 billion in revenue [68]. Venture capital investment in the sector surged by 16%, with average financing rounds reaching $36 million—a 122% increase over 2024 [68]. This robust funding environment underpins the growth of neurotech startups.
Table 2: Funding and Market Analysis of Key BCI Companies
| Company / Metric | Funding / Market Data | Strategic Position & Market Outlook |
|---|---|---|
| Neuralink [27] [19] | Reportedly raised over $650 million to date; valued at approximately $5 billion. | High-profile, aiming for a high-bandwidth general-purpose neural interface. |
| Paradromics [27] | Secured more than $105 million in venture funding, plus $18 million from NIH and DARPA grants. | Focused on high-data-rate applications, particularly speech decoding. |
| Global BCI Market [22] [27] | Overall BCI market forecast to surpass $1.6B by 2045 (CAGR: 8.4%). Invasive BCIs estimated at $160.44 billion in 2024. | Driven initially by medical applications in paralysis, rehabilitation, and prosthetics. |
| MedTech M&A Trend [68] | Average M&A deal size of $497 million in 2025, up 11% from 2024. | Industry leaders are leveraging strong balance sheets for high-growth acquisitions. |
| Patent Landscape [22] | Patent analysis suggests filing numbers for "brain-computer interface" have peaked. | Indicates a maturing technology domain where competitive advantage may shift to clinical execution and manufacturing. |
Comparative Analysis: Invasive vs. Non-Invasive Neural Interfaces
The core trade-off in neural interfacing is between the high-fidelity signals obtained from invasive technologies and the safety and accessibility of non-invasive approaches. The following table provides a technical and functional comparison of the major technology categories.
Table 3: Technical Comparison of Invasive and Non-Invasive Neural Interfaces
| Parameter | Invasive (Intracortical) | Minimally Invasive (ECoG/Endovascular) | Non-Invasive (EEG/sEMG) |
|---|---|---|---|
| Spatial Resolution | Very High (microns) [2] | High (millimeters) [2] | Low (centimeters) [2] |
| Temporal Resolution | Very High (milliseconds) [2] | High (milliseconds) [2] | High (EEG: milliseconds) [2] |
| Signal-to-Noise Ratio | Highest [2] | High [2] | Low to Moderate [6] [2] |
| Typical Applications | Control of robotic limbs, speech decoding, complex device control [27] [45] [2] | Computer cursor control, text communication, control of external devices [27] [45] | Basic device control, neurofeedback, gaming, handwriting transcription [6] [2] |
| Key Advantage | Bandwidth and fidelity for complex control. | Compromise between signal quality and surgical risk. | Safety, accessibility, and ease of use. |
| Primary Challenge | Long-term biocompatibility, scar tissue formation, and requirement for neurosurgery [27] [2] | Limited brain coverage or specific target location, long-term stability [27] [2] | Low signal bandwidth, susceptibility to noise, variability across users [6] [2] |
| Representative Performance (2025) | Neuralink: Controlling digital devices with thoughts [27]. Speech decoding at >90% accuracy [2]. | Precision: Wireless device for smartphone/computer operation [45]. Synchron: Texting and computer control [27]. | sEMG: Handwriting at 20.9 words per minute with cross-user generalization [6]. |
Experimental Protocols and Methodologies
To illustrate the experimental rigor behind these technologies, this section details the protocols from two landmark 2025 studies: one for a non-invasive surface EMG interface and one representative of invasive intracortical research.
Protocol 1: Non-Invasive sEMG for Generic Computer Input
This study demonstrated a high-bandwidth neuromotor interface that generalizes across people without individual calibration [6].
- Objective: To develop a generic non-invasive neuromotor interface using surface Electromyography (sEMG) for high-performance computer input.
- Hardware: A custom, dry-electrode, multichannel sEMG wristband (sEMG-RD) with four sizes to fit different wrist circumferences. The device samples at 2 kHz with low noise (2.46 µVrms) and streams data wirelessly via Bluetooth [6].
- Data Collection: A large and diverse cohort of participants (ranging from 162 to 6,627 depending on the task) was recruited. Participants performed three tasks while wearing the sEMG band on their dominant wrist:
- Wrist Control: Controlling a cursor using wrist angles tracked by motion capture.
- Discrete-Gesture Detection: Performing nine distinct gestures in a randomized order.
- Handwriting: "Writing" prompted text while holding fingers together as if holding a pen [6].
- Signal Processing & Decoding: A real-time processing engine recorded sEMG data and prompt timestamps. A time-alignment algorithm was used to precisely align intended gesture times with the recorded sEMG signals. Deep learning models (neural networks) were trained on this large dataset to decode user intent [6].
- Outcome Metrics:
- Handwriting: 20.9 words per minute (WPM) with cross-participant generalization.
- Discrete Gestures: 0.88 detections per second.
- Continuous Navigation: 0.66 target acquisitions per second [6].
Figure 1: Experimental workflow for non-invasive sEMG interface development.
Protocol 2: Invasive BCI for Speech Decoding and Device Control
This protocol synthesizes the common methodology used in invasive BCI human trials, as reported by companies like Neuralink, Paradromics, and the academic BrainGate consortium [27] [45].
- Objective: To decode neural signals for the control of external devices or synthetic speech in individuals with paralysis.
- Hardware: Implantable microelectrode arrays (e.g., Neuralink's N1 Implant, Blackrock's Utah Array) are surgically placed in the motor or speech cortex. These arrays record multi-unit activity and local field potentials [27] [45] [2].
- Data Acquisition: The implanted electrodes record neural signals, which are transmitted wirelessly to an external decoding system. The sheer volume of data is a key challenge, requiring sophisticated compression [27] [45].
- Signal Processing & Decoding: Machine learning and deep learning algorithms are used to decode the user's intention. For speech, this involves mapping neural patterns to intended words or phonemes. For movement, it involves decoding kinematic parameters for cursor or prosthetic control [45] [2]. Artificial intelligence is critical for recognizing complex neural patterns.
- Closed-Loop Feedback: Many systems incorporate sensory feedback, such as adding a sense of touch to a prosthetic hand by stimulating the sensory cortex, which significantly improves performance [45].
- Outcome Metrics:
The Scientist's Toolkit: Key Research Reagents & Materials
For researchers designing experiments in this field, the following tools and materials are essential.
Table 4: Essential Research Tools for Neural Interface Development
| Item / Technology | Function / Application | Specific Examples / Notes |
|---|---|---|
| Dry Electrode sEMG Wristband [6] | Non-invasive recording of neuromuscular signals for human-computer interaction. | Custom research device (sEMG-RD) with multiple sizes, high sample rate (2kHz), and wireless operation. |
| Implantable Microelectrode Arrays [27] [2] | Invasive recording of high-fidelity neural signals (multi-unit activity, local field potentials). | Utah Array (Blackrock), Neuralink's N1 Implant, Paradromics' Connexus array. |
| Minimally Invasive Electrode Arrays [27] [45] | Recording from the brain's surface (ECoG) or via blood vessels, balancing signal quality and risk. | Precision's "Layer 7" brain film, Synchron's Stentrode. |
| Deep Learning Algorithms [6] [2] | Decoding intended movements or speech from complex neural or neuromuscular signals. | Trained on large datasets; can be generic or personalized for individual users. |
| Real-Time Processing Engine [6] | Handling high-volume data streaming and ensuring precise time-alignment of signals and prompts. | Critical for reducing "online-offline shift" and enabling closed-loop control. |
| Brain Modeling Toolkits & Simulations [69] | In silico testing of hypotheses and BCI paradigms using biophysically realistic brain models. | Allen Institute's Brain Modeling ToolKit; used with supercomputers for large-scale simulation. |
Figure 2: Core technology stack and signal pathway for modern neural interfaces.
The competitive ecosystem for neural interfaces in 2025 is marked by a diverse range of technological solutions, each with a distinct path to market and value proposition. Invasive technologies from leaders like Neuralink and Blackrock Neurotech offer unparalleled bandwidth for restoring complex functions but face higher regulatory and surgical hurdles. Minimally invasive approaches from Synchron and Precision Neuroscience present a compelling compromise, potentially enabling faster clinical adoption. Meanwhile, breakthrough non-invasive technologies, such as the generic sEMG interface, demonstrate that high-performance, accessible alternatives are on the horizon. For researchers and clinicians, the choice of technology is no longer a simple binary but a strategic decision based on the specific application, required bandwidth, and risk tolerance. The convergence of advanced hardware, sophisticated AI-driven decoding, and robust clinical protocols signals that the era of practical neural interfaces has arrived, with the potential to profoundly impact human health and capability.
Conclusion
The comparative analysis reveals that the choice between invasive and non-invasive neural interfaces is not a binary one but is dictated by a clear trade-off between signal fidelity and practical accessibility. Invasive technologies offer unparalleled control for restoring complex functions in severe neurological disorders but face significant hurdles in surgical risk, long-term biocompatibility, and user acceptance. Non-invasive methods provide a safer, more scalable pathway for diagnostics, wellness, and basic communication, though they are limited by lower information transfer rates. Future directions will be shaped by trends in miniaturization, AI-powered decoding, the development of robust minimally-invasive solutions, and the establishment of clear ethical and regulatory frameworks. For researchers and drug developers, this evolving landscape presents diverse opportunities to target specific clinical needs, from high-fidelity motor restoration to scalable neuromonitoring tools, ultimately driving personalized neurotherapeutics forward.
References
- 1. What limits the performance of current invasive brain machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4010778/]
- 2. Non-Invasive Brain-Computer Interfaces: State of the Art and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11861396/]
- 3. Designing Brain-Computer Interfaces That Connect Neurons ... [https://magazine.hms.harvard.edu/articles/designing-brain-computer-interfaces-connect-neurons-digital-world]
- 4. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/tw/research-report/brain-computer-interfaces/1024]
- 5. Optimising non-invasive brain-computer interface systems ... [https://www.nature.com/articles/s41598-019-55166-y]
- 6. A generic non-invasive neuromotor interface for human- ... [https://www.nature.com/articles/s41586-025-09255-w]
- 7. fNIRS vs EEG: Comparing Non-Invasive Brain Imaging ... [https://imotions.com/blog/learning/research-fundamentals/fnirs-vs-eeg/?srsltid=AfmBOoqBwnhmYq54YvX_EOk1uN-4zOSrHJGeNJ2ZhUN2vcIz__K2R9-N]
- 8. Invasive vs. Non-Invasive Neuronal Signals for Brain-Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4921501/]
- 9. Frontiers | fNIRS , EEG , ECG, and GSR reveal an effect of complex... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1459653/full]
- 10. of Comparison and ECoG signals | Fiveable intracortical [https://fiveable.me/brain-computer-interfaces/unit-5/comparison-ecog-intracortical-signals/study-guide/ahyTx7o9wtbS31R2]
- 11. fNIRS-EEG BCIs for Motor Rehabilitation: A Review [https://www.mdpi.com/2306-5354/10/12/1393]
- 12. Simultaneous multimodal fNIRS-EEG recordings reveal ... [https://www.nature.com/articles/s41598-023-31609-5]
- 13. Evaluating the effects of multimodal EEG - fNIRS neurofeedback for... [https://pubmed.ncbi.nlm.nih.gov/40934195/]
- 14. A Cross-Disciplinary Review of the fNIRS-EEG Dual-Modality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11506513/]
- 15. A Review of Brain-Computer Interface Technologies [https://arxiv.org/html/2503.16471v1]
- 16. Invasive vs. Non-Invasive Neuronal Signals for Brain- ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2016.00295/full]
- 17. How does invasive vs non-invasive BCI compare? [https://synapse.patsnap.com/article/how-does-invasive-vs-non-invasive-bci-compare]
- 18. Optimizing Computer–Brain Interface Parameters for Non- ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2020.00001/full]
- 19. Neurotechnology & Brain-Computer Interfaces in 2025 [https://www.ambula.io/neurotechnology-brain-computer-interfaces-in-2025/]
- 20. Non-invasive temporal interference electrical stimulation of ... [https://www.nature.com/articles/s41593-023-01456-8]
- 21. A New Path to Noninvasive Brain-Computer Interface [https://www.jhuapl.edu/news/news-releases/241114-noninvasive-brain-computer-interface]
- 22. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/en/research-report/brain-computer-interfaces/1024]
- 23. Brain Computer Interface (BCI) Research Report 2025-2035: [https://www.globenewswire.com/news-release/2025/10/01/3159276/0/en/Brain-Computer-Interface-BCI-Research-Report-2025-2035-EEG-MEG-and-fMRI-Integration-Enhances-Neural-Signal-Detection-and-Drives-Global-Growth.html]
- 24. NI Data Acquisition: The Accuracy and Performance ... [https://www.ni.com/en/shop/data-acquisition/ni-data-acquisition--the-accuracy-and-performance-difference.html?srsltid=AfmBOoq645byxUTODFTuXH1lVTS1t3mW7RnR3jBQZGgZWZP4r6qapY5i]
- 25. Brain Computer Interface (BCI) Research Report 2025-2035 [https://finance.yahoo.com/news/brain-computer-interface-bci-research-090400037.html]
- 26. Top Non-Invasive Brain Monitor Companies & How to ... [https://www.linkedin.com/pulse/top-non-invasive-brain-monitor-companies-how-compare-g6gnc/]
- 27. BCIs in 2025: Trials, Progress, and Challenges [https://andersenlab.com/blueprint/bci-challenges-and-opportunities]
- 28. Implantable brain–computer interface for neuroprosthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8637800/]
- 29. Neuroprosthetics: from sensorimotor to cognitive disorders [https://www.nature.com/articles/s42003-022-04390-w]
- 30. The Stentrode™ System by Synchron: Architectural Design ... [https://www.auctoresonline.org/article/the-stentrode-system-by-synchron-architectural-design-and-clinical-translation-of-a-minimally-invasive-braincomputer-interface]
- 31. Functional ultrasound neuroimaging reveals mesoscopic ... [https://www.nature.com/articles/s41467-025-63826-z]
- 32. Invasive Brain-Computer Interfaces: A Critical Assessment of ... [https://neuro.jmir.org/2024/1/e60151]
- 33. A new era of brain-computer interfaces: Restored touch ... [https://www.eurekalert.org/news-releases/1106526]
- 34. AI co-pilot boosts noninvasive brain-computer interface by ... [https://newsroom.ucla.edu/releases/ai-brain-computer-interface-interprets-user-intent-ucla]
- 35. Outlook for Noninvasive Brain-Computer Interfaces for AI [https://etcjournal.com/2025/09/21/outlook-for-noninvasive-brain-computer-interfaces-for-ai/]
- 36. Brain Computer Interface Market Surges to USD 10.65 ... [https://media.market.us/brain-computer-interface-market-news-2025/]
- 37. Brain Computer Interface Market Poised for Explosive [https://www.globenewswire.com/news-release/2025/11/20/3192028/0/en/Brain-Computer-Interface-Market-Poised-for-Explosive-Growth-Projected-to-Hit-USD-6-16-Billion-by-2032-Coherent-Market-Insights.html]
- 38. Recent applications of EEG-based brain-computer-interface in ... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-025-00598-z]
- 39. Exploring Imagined Movement for Brain–Computer Interface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468679/]
- 40. Why Brain Wearables Are Making Traditional EEG Labs ... [https://globalrph.com/2025/10/why-brain-wearables-are-making-traditional-eeg-labs-obsolete-in-2025/]
- 41. Enhanced EEG signal classification in brain computer ... [https://www.nature.com/articles/s41598-025-07427-2]
- 42. An fNIRS and EEG Review [https://pubmed.ncbi.nlm.nih.gov/41008372/]
- 43. Progress and challenges of implantable neural interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8077843/]
- 44. Revolutionizing brain‒computer interfaces: overcoming ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03573-x]
- 45. Brain computer interfaces are poised to help people with ... [https://www.npr.org/sections/shots-health-news/2025/06/30/nx-s1-5339708/brain-computer-interface-implants-disabilities-neuralink]
- 46. Brains, minds and machines: A new algorithm for decoding ... [https://news.engineering.utoronto.ca/brains-minds-and-machines-a-new-algorithm-for-decoding-intelligence/]
- 47. Decoding the brain: from neural representations to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11637322/]
- 48. Wireless and battery-free technologies for neuroengineering [https://pmc.ncbi.nlm.nih.gov/articles/PMC8423863/]
- 49. Wireless and battery-free technologies for neuroengineering [https://www.nature.com/articles/s41551-021-00683-3]
- 50. Multidimensional advances in neural interface technology ... [https://www.sciencedirect.com/science/article/pii/S2590006425006623]
- 51. Wireless Neural Interfaces Market Insights 2025 to 2035 [https://www.factmr.com/report/wireless-neural-interfaces-market]
- 52. Deep learning for inner speech recognition [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1668935/full]
- 53. NeurIPT: Foundation Model for Neural Interfaces [https://arxiv.org/html/2510.16548v1]
- 54. Comparative Analysis of Neural Decoding Algorithms for ... [https://pubmed.ncbi.nlm.nih.gov/40644105/]
- 55. Comparative accuracy of invasive versus non- ... [https://eureka.patsnap.com/report-comparative-accuracy-of-invasive-versus-non-invasive-brain-computer-interfaces-approaches]
- 56. EEG-based brain-computer interface enables real-time ... [https://www.nature.com/articles/s41467-025-61064-x]
- 57. Architectural Design and Implantation Strategies of Brain ... [https://www.auctoresonline.org/article/architectural-design-and-implantation-strategies-of-braincomputer-interfaces-a-comparative-review-of-neuralink-synchron-precision-neuroscience-and-paradromics]
- 58. AI Copilot Boosts Brain-Computer Interface's Performance [https://www.psychologytoday.com/us/blog/the-future-brain/202509/ai-copilot-boosts-brain-computer-interfaces-performance]
- 59. The history, current state and future possibilities of the non- ... [https://www.sciencedirect.com/science/article/pii/S2590093525000049]
- 60. Neurosurgical Team Acceptability of Brain–Computer Interfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC10444691/]
- 61. Defining Surgical Terminology and Risk for Brain ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.599549/full]
- 62. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 63. Brain-computer interfaces face a critical test [https://www.technologyreview.com/2025/04/01/1114009/brain-computer-interfaces-10-breakthrough-technologies-2025/]
- 64. Ethical imperatives in the commercialization of brain- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553070/]
- 65. What limits the performance of current invasive brain ... [https://www.frontiersin.org/journals/systems-neuroscience/articles/10.3389/fnsys.2014.00068/full]
- 66. Neural Data Privacy Regulation: What Laws Exist and ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/07/neural-data-privacy-regulation]
- 67. U.S. Senators Propose "MIND Act" to Study and ... [https://www.dwt.com/blogs/privacy--security-law-blog/2025/10/senate-mind-act-neural-data-ftc-regulation]
- 68. EY releases: Pulse of the MedTech Report 2025 [https://www.ey.com/en_us/newsroom/2025/09/ey-releases-pulse-of-the-medtech-report-2025]
- 69. One of world's most detailed virtual brain simulations is ... [https://alleninstitute.org/news/one-of-worlds-most-detailed-virtual-brain-simulations-is-changing-how-we-study-the-brain/]