Individual Differences in Addiction Neurobiology: From Genetic Risk to Personalized Treatment
This article synthesizes current research on the neurobiological basis of individual differences in addiction vulnerability, progression, and treatment response.
Individual Differences in Addiction Neurobiology: From Genetic Risk to Personalized Treatment
Abstract
This article synthesizes current research on the neurobiological basis of individual differences in addiction vulnerability, progression, and treatment response. Targeting researchers and drug development professionals, it explores the foundational genetic, developmental, and neural circuit mechanisms that create divergent pathways to addiction. The scope extends to methodological innovations in imaging and genetics, troubleshooting challenges in disease modeling and theoretical integration, and validating findings through comparative analysis of competing frameworks. The review emphasizes a consilience approach, arguing that integrating neuroscientific, behavioral, and clinical perspectives is crucial for advancing personalized addiction medicine.
The Biological Underpinnings of Addiction Vulnerability: Genetics, Circuits, and Early Risk
Frequently Asked Questions (FAQs)
1. What is the heritable component of addiction risk? Family and twin studies indicate that genetic factors contribute to approximately 40-60% of the risk for developing a substance use disorder. The specific heritability varies by substance [1] [2].
2. Are there genetic factors shared across different substance use disorders? Yes, multivariate genetic analyses reveal both shared and substance-specific genetic influences. For example, a cross-ancestry multivariate GWAS identified a shared genetic factor among alcohol, cannabis, opioid, and tobacco use disorders, while also highlighting specific loci like CHRNA2 that are more specific to cannabis use disorder [3] [4].
3. How do anxiety disorders and problematic alcohol use interact genetically? Recent genomic studies show a substantial genetic overlap and a bidirectional causal relationship between problematic alcohol use (PAU) and anxiety disorders (ANX). They share a significant number of genetic variants, many of which have concordant (same direction) effects on both conditions [5].
4. What are the primary molecular pathways implicated in addiction? Research has identified several key pathways, including dopaminergic signaling, cAMP signaling, long-term potentiation, MAPK signaling, and GnRH signaling. These are involved in synaptic plasticity, reward, and reinforcement [5] [2].
5. In which brain regions are addiction-related genes most active? Gene expression analyses show enrichment in brain regions critical for reward, decision-making, and emotion, including the prefrontal cortex, anterior cingulate cortex, hippocampus, hypothalamus, substantia nigra, and amygdala [5].
Quantitative Data on Heritability and Genetic Correlations
Table 1: Heritability Estimates and Key Genetic Findings for Substance Use Disorders
| Substance Use Disorder | Heritability (Twin/Family Studies) | SNP-based Heritability (h²snp) | Key Replicated Risk Genes / Loci |
|---|---|---|---|
| Problematic Alcohol Use (PAU) | ~50% [3] | 5.6% - 10.0% [3] | ADH1B, ADH1C, ADH4, ADH5, ADH7, DRD2 [3] |
| Cannabis Use Disorder (CUD) | ~50-60% [3] | Information Missing | CHRNA2, FOXP2 [3] |
| Tobacco Use Disorder (TUD) | ~30-70% [3] | Information Missing | CHRNA5-CHRNA3-CHRNB4, DNMT3B, MAGI2/GNAI1, TENM2 [3] |
| Opioid Use Disorder (OUD) | Information Missing | Information Missing | Information Missing |
Table 2: Genetic Correlations Between Problematic Alcohol Use and Comorbid Traits
| Trait | Genetic Correlation (rg) with Problematic Alcohol Use | Notes |
|---|---|---|
| Anxiety Disorders (ANX) | rg = 0.44 [5] | High effect direction concordance (86.4%) among shared variants [5]. |
| Other Substance Use Disorders | Strong positive correlations [4] | Strongest with opioid use disorder, cannabis use disorder, and problematic alcohol use [4]. |
| Psychiatric Traits | Strong positive correlations [4] | Notably with suicidality [4]. |
Experimental Protocols & Methodologies
Protocol 1: Mendelian Randomization to Test Causal Relationships
Objective: To assess whether a putative risk factor (e.g., anxiety) has a causal effect on an outcome (e.g., problematic alcohol use), or vice versa, using genetic variants as instrumental variables.
Workflow:
- Instrument Selection: Identify genetic variants (SNPs) that are strongly and reliably associated with the exposure trait (e.g., anxiety) from a large GWAS.
- Effect Size Extraction: Extract the association effects of these same genetic instruments on the outcome trait (e.g., problematic alcohol use) from an independent GWAS.
- Causal Estimation: Perform a two-sample Mendelian Randomization analysis (e.g., using inverse-variance weighted method) to estimate the causal effect of the exposure on the outcome [5].
- Bidirectional Analysis: Repeat steps 1-3, swapping the exposure and outcome to test for reverse causality [5].
- Sensitivity Analyses: Conduct pleiotropy-robust methods (e.g., MR-Egger, MR-PRESSO) to validate that results are not biased by horizontal pleiotropy.
Protocol 2: Conjunctional FDR for Identifying Shared Genetic Loci
Objective: To pinpoint specific genetic loci that are shared between two related traits (e.g., PAU and ANX) while increasing discovery power.
Workflow:
- Input Summary Statistics: Use GWAS summary statistics (p-values and effect directions) for both traits.
- ConjFDR Analysis: Apply the conjunctional false discovery rate (conjFDR) framework. This method identifies SNPs associated with either trait, then tests whether they are also associated with the other trait, conditioning on the first association.
- Identify Shared Loci: Declare a SNP as a shared locus if its conjFDR value falls below a specified significance threshold (e.g., < 0.05).
- Annotate and Map: Annotate the identified lead SNPs to genes and examine their effect direction (concordant or discordant) on both traits [5].
Table 3: Essential Resources for Investigating the Genetics of Addiction
| Resource / Reagent | Function / Application | Example / Source |
|---|---|---|
| GWAS Summary Statistics | Foundation for genetic correlation, MR, and polygenic score analyses. | Million Veteran Program (MVP), UK Biobank (UKB), Psychiatric Genomics Consortium (PGC) [3]. |
| Knowledgebase of Addiction-Related Genes (KARG) | A curated database of human addiction-related genes with extensive functional annotations. | http://karg.cbi.pku.edu.cn [2] |
| FUMA (FUctional Mapping and Annotation) | An online platform for the functional annotation of GWAS results, including gene mapping, tissue expression, and cell-type specificity analyses. | Used in recent studies to map SNPs to genes and conduct expression analyses [5]. |
| Mendelian Randomization Software | Statistical packages to perform MR analysis and sensitivity checks. | TwoSampleMR (R package), MR-Base. |
| Key Candidate Genes | Targets for functional validation experiments (e.g., in animal or cell models). | DRD2 (dopamine signaling), PDE4B (cAMP signaling), ADH1B (alcohol metabolism), CHRNA2 (cholinergic signaling) [5] [3]. |
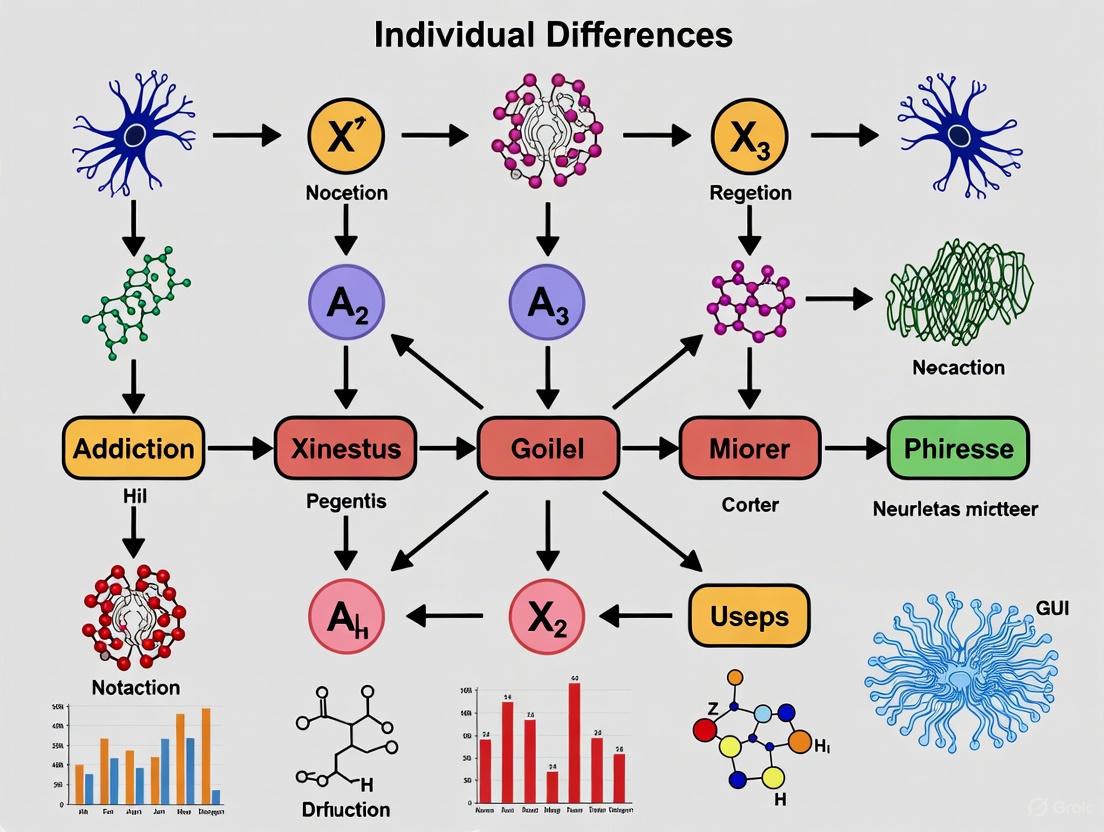
Visualization of Key Shared Molecular Pathways
The integration of genetic findings has highlighted several key molecular pathways that are shared across multiple substance use disorders and their comorbidities. The following diagram synthesizes these pathways into a core network, centered on dopamine signaling and its downstream effects on synaptic plasticity.
Core Concepts: The Neurobiological Basis of Sex-Specific Risk
Q: What is the central finding regarding sex-specific neural trajectories in youth with a family history of substance use disorder (SUD)?
A: A large-scale 2025 study analyzing nearly 1,900 children from the Adolescent Brain Cognitive Development (ABCD) Study found that a family history of SUD is associated with early, sex-divergent differences in brain activity dynamics, long before any substance use begins [6] [7]. The key finding is that girls and boys show opposing patterns of "transition energy"—a measure of the brain's effort to shift between different activity states—in distinct neural networks [6].
Q: What are the specific neural patterns observed in at-risk girls versus boys?
A: The patterns are opposing, as summarized in the table below [6] [7]:
| Sex | Neural Signature | Brain Network Affected | Proposed Behavioral Correlate |
|---|---|---|---|
| Females | Increased Transition Energy | Default-Mode Network (DMN) | Greater difficulty disengaging from internal states like stress or rumination; substance use may later serve as a way to escape [6]. |
| Males | Decreased Transition Energy | Dorsal and Ventral Attention Networks | Heightened reactivity to the environment and sensation-seeking; a tendency toward unrestrained behavior [6]. |
Q: How do these findings fit into the broader thesis of individual differences in addiction neurobiology?
A: This research underscores that sex is a critical biological variable shaping individual vulnerability to addiction. It demonstrates that the same familial risk factor can manifest as distinct neurobiological pathways in males and females [6]. This challenges homogeneous models of addiction and emphasizes the need for personalized prevention strategies that target these specific risk profiles—for instance, focusing on stress coping in girls and impulse control in boys [6] [7].
Experimental Protocols & Methodologies
Q: What was the primary experimental dataset and population used in this research?
A: The study analyzed data from the Adolescent Brain Cognitive Development (ABCD) Study, a large longitudinal NIH study in the United States [6]. The cohort included nearly 1,900 children aged 9 to 11 years, ensuring the observed differences predate substance use initiation [6] [7].
Q: What is the core methodology for quantifying brain activity dynamics?
A: The primary computational approach used is Network Control Theory (NCT) applied to resting-state functional MRI (fMRI) data [6].
- Protocol: When a subject lies in an MRI scanner at rest, the brain cycles through recurring patterns of activation. NCT calculates the "transition energy" required for the brain to shift between these different activity patterns [6].
- Measurement: This "transition energy" serves as a metric for the brain's flexibility or inertia. Higher energy implies less flexibility and more effort required to change states, while lower energy suggests greater ease of transition and potentially less cognitive control [6].
Q: Why is the analysis of sex-specific data critical in this protocol?
A: The researchers found that averaging data across both sexes masked the contrasting neural patterns. Conducting separate analyses for boys and girls was essential to reveal the opposing effects of family history on transition energy in attention versus default-mode networks [6]. This is a crucial methodological consideration for all research on individual differences.
Experimental Workflow Diagram
Troubleshooting & Experimental Replication
Q: What could lead to a failure to detect these sex-specific effects?
A: The most common error would be pooling data from males and females without stratification for the primary analysis. The study's authors explicitly note that these divergent patterns were only visible when data from boys and girls were analyzed separately [6]. Always include sex as a key biological variable in your experimental design and statistical models.
Q: How should "family history of SUD" be reliably defined and collected in a research setting?
A: The ABCD Study and other large cohorts typically use standardized, validated instruments such as structured interviews or detailed family history questionnaires. Best practices include:
- Using clear diagnostic criteria (e.g., based on DSM-5) to define SUD in family members.
- Gathering information on the degree of relation (first-degree vs. second-degree relatives).
- Employing multiple informants where possible to improve accuracy.
Q: Our analysis shows inconsistent results with the transition energy metric. What are potential sources of variance?
A: Inconsistencies can arise from several factors:
- Data Quality: Ensure high-quality fMRI pre-processing to minimize motion artifacts, a significant concern in pediatric populations.
- Parcellation Scheme: The definition of brain networks (like the DMN or Attention Networks) can vary. Test the robustness of your findings across different brain atlases.
- Computational Implementation: Verify the implementation of the NCT model, including the parameters used for defining brain states and calculating energy.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources and their functions for research in this domain.
| Research Tool / Reagent | Function & Application in Context |
|---|---|
| ABCD Study Dataset | A foundational, openly available resource providing longitudinal neuroimaging, genetic, behavioral, and environmental data from a large pediatric cohort, ideal for studying developmental trajectories [6]. |
| Network Control Theory (NCT) | A computational framework applied to fMRI data to model brain network dynamics and quantify the energy required for transitions between neural states [6]. |
| Resting-state fMRI | A non-invasive imaging technique that measures spontaneous brain activity to map functional connectivity networks without a task, crucial for studying intrinsic brain organization [6]. |
| Structured Clinical Interviews | Validated instruments (e.g., based on DSM-5 criteria) for consistently assessing substance use disorder in probands and their family members to define "family history" [6]. |
Neurobiological Pathways to Addiction
The sex-specific early vulnerabilities interact with the established three-stage cycle of addiction, which involves disruptions in three key brain regions [8] [9]. The following diagram integrates the early vulnerabilities with this broader framework.
Addiction Vulnerability Pathway
Frequently Asked Questions (FAQs)
Q1: What specific neurodevelopmental processes during adolescence increase vulnerability to substance use initiation? Adolescence is characterized by a mismatch in the development of subcortical limbic systems and the prefrontal cortex. Key processes include:
- Synaptic Pruning and Myelination: The brain undergoes significant refinement, reducing gray matter volume in prefrontal and temporal cortices while increasing white matter integrity through myelination, which improves neural conductivity [10]. Higher-order association areas mature only after lower-order sensorimotor regions, with frontal lobes being the last to complete development [10].
- Imbalanced Development: Subcortical limbic systems, which process rewards and emotions, mature earlier than the prefrontal cortex, which is responsible for executive control, impulse inhibition, and long-term planning [11] [10]. This imbalance creates a period of heightened reward sensitivity, novelty-seeking, and risk-taking, behaviors that can directly lead to substance use initiation [11].
Q2: How do individual differences in brain structure predict subsequent substance use? Pre-existing structural differences can serve as biomarkers for substance use vulnerability. Key predictors include:
- Prefrontal Cortex Volume: Smaller prefrontal cortex volumes, particularly in females, have been observed prior to or in conjunction with the onset of heavy drinking [10].
- Brain Maturation Patterns: Variations in the typical trajectories of cortical thinning and gray matter volume reduction may be associated with a predisposition to substance use [11]. Research is actively characterizing these individual differences to understand their role in the transition from use to dependence [12].
Q3: What are the most critical neuroimaging modalities for investigating the adolescent brain in the context of substance use? The primary non-invasive modalities used in human adolescents are:
- Structural MRI (sMRI): Used to investigate gross brain morphology, including cortical thickness, and gray and white matter volumes. For example, studies have linked adolescent alcohol use to smaller frontal cortices and hippocampal volumes [11] [13] [10].
- Functional MRI (fMRI): Infers brain region activity by measuring dynamic cerebral blood flow (BOLD signal). It is used to study reward processing, cue reactivity, and executive control in adolescent substance users [11].
- Diffusion Tensor Imaging (DTI): Investigates white matter microstructure by measuring water diffusivity across axon bundles, providing an index of neural connectivity and integrity [11].
Q4: What is the neurobiological mechanism underlying the transition from recreational use to addiction? The progression to addiction is conceptualized as a chronic, relapsing cycle with three core stages, each linked to specific neuroadaptations [8] [14]:
- Binge/Intoxication: Focused on the basal ganglia. Dopamine release reinforces drug use, and repeated use leads to "incentive salience," where cues associated with the drug trigger powerful motivational urges [8] [14].
- Withdrawal/Negative Affect: Centered on the extended amygdala (the "anti-reward" system). Chronic use leads to a downregulation of reward systems and an upregulation of brain stress systems (e.g., CRF, dynorphin), resulting in anxiety, irritability, and dysphoria when not using the drug [8] [14].
- Preoccupation/Anticipation: Governed by the prefrontal cortex. This stage is marked by executive dysfunction, including reduced impulse control and emotional regulation, and intense cravings, which drive the relapse cycle [8] [14].
Troubleshooting Common Experimental Challenges
Challenge 1: Accounting for Pre-Existing Vulnerabilities vs. Substance-Induced Effects
- Problem: It is methodologically difficult to determine whether observed neural differences in adolescent substance users are a consequence of drug exposure or a pre-existing risk factor.
- Solution:
- Implement Longitudinal Designs: The gold-standard approach is to recruit substance-naïve adolescents and perform repeated neuroimaging and neuropsychological assessments before and after substance use initiation [13]. The landmark ABCD Study is a prime example of this methodology [15].
- Careful Participant Screening: Rigorously match user and non-user groups on potential confounding variables such as family history of substance use disorders, prenatal exposure, conduct disorder symptoms, and other psychopathologies [10].
- Statistical Control: Use variables like age of first use, frequency, and quantity of use as covariates in analyses to help disentangle dose-dependent effects from predisposing traits [13].
Challenge 2: Controlling for Polysubstance Use
- Problem: Adolescents rarely use a single substance in isolation, making it challenging to attribute neurobiological findings to a specific drug.
- Solution:
- Stringent Inclusion Criteria: Recruit participants with well-characterized primary substance use patterns and minimal use of other drugs. This may reduce generalizability but improves interpretability.
- Statistical Modeling: Treat polysubstance use as a quantitative covariate or use data-driven approaches (e.g., factor analysis) to model the effects of multiple substances [13] [16].
- Targeted Recruitment: Focus on emerging trends, such as e-cigarette use (for nicotine and/or cannabis), and clearly define the primary substance of interest [11].
Challenge 3: Ensuring Valid and Reliable Neurocognitive Assessment
- Problem: Subtle neurocognitive deficits in adolescent users can be masked by generally high cognitive reserve or confounded by motivation, practice effects, or subclinical withdrawal.
- Solution:
- Abstinence Verification: For studies of current users, verify recent abstinence (e.g., 24-48 hours) using breathalyzer and urine toxicology screens to minimize acute intoxication or withdrawal effects [10].
- Battery Design: Use comprehensive, standardized neuropsychological batteries that assess multiple domains known to be affected, such as verbal and spatial memory, attention, speeded information processing, and executive functioning [10].
- Alternative Measures: Incorporate laboratory-based behavioral tasks (e.g., delay discounting, stop-signal task) that provide precise metrics of impulsivity and decision-making, which are core constructs in addiction [12].
Key Neuroimaging Findings in Adolescent Substance Use
Table 1: Long-term Neurostructural Correlates of Adolescent-Initiated Substance Use
| Substance | Key Structural Findings | Associated Cognitive/Behavioral Correlates |
|---|---|---|
| Alcohol | Smaller frontal cortex volumes; reduced gray matter volume decline over time; smaller left hippocampal volume [13] [10]. | Deficits in memory, attention, speeded information processing, and executive functioning; spatial functioning impairments linked to withdrawal history [10]. |
| Cannabis | Altered frontal cortex volumes; mixed findings on hippocampal volume (smaller with more years since initiation) [13]. | Poorer performance on learning, cognitive flexibility, visual scanning, and working memory; number of lifetime use episodes predicts poorer overall functioning [10]. |
| Tobacco/Nicotine | Smaller frontal cortices (especially OFC); altered white matter microstructure [13]. | Worsened attentional performance; symptoms of inattention; deficits in selective and divided attention [11]. |
| Stimulants | Trend towards altered volumes in putamen, insula, and frontal cortex [13]. | (Data less consolidated; often involves polysubstance use) |
| Opioids | Smaller subcortical and insular volumes [13]. | (Data less consolidated) |
Table 2: Core Neurobiological Stages of Addiction Relevant to Adolescent Development
| Stage of Addiction Cycle | Core Brain Region | Primary Neuroadaptations | Behavioral Manifestation |
|---|---|---|---|
| Binge/Intoxication | Basal Ganglia | Dopamine release & incentive salience; shift from goal-directed to habitual control (ventral to dorsal striatum) [8] [14]. | Positive reinforcement; drug-seeking for rewarding effects. |
| Withdrawal/Negative Affect | Extended Amygdala | Recruitment of brain stress systems (CRF, dynorphin); reduced reward system function [8] [14]. | Negative emotional state (anxiety, irritability); negative reinforcement. |
| Preoccupation/Anticipation | Prefrontal Cortex | Executive dysfunction; decreased inhibitory control; heightened craving [8] [14]. | Compulsivity; loss of control over drug use; cravings. |
Experimental Protocols & Workflows
Protocol 1: Longitudinal sMRI Analysis of Cortical Development
- Objective: To determine if adolescent substance use alters the normative trajectory of cortical brain development.
- Procedure:
- Acquisition: Collect high-resolution T1-weighted MRI scans at baseline (pre-initiation) and at regular follow-up intervals (e.g., annually).
- Preprocessing: Process images using standardized software (e.g., Freesurfer, SPM) for cortical reconstruction and volumetric segmentation. Key steps include noise correction, skull stripping, and tissue classification into gray/white matter.
- Analysis:
- Extract cortical thickness and surface area for regions of interest (e.g., prefrontal cortex, insula) and globally.
- Use mixed-effects modeling to compare the longitudinal trajectories of cortical measures between substance-use groups and matched controls, controlling for age, sex, and intracranial volume.
- Relate changes in brain structure to changes in substance use patterns (e.g., escalation) and neurocognitive performance over time.
Protocol 2: fMRI Task-Based Analysis of Reward Processing
- Objective: To assess neural responses to drug cues and monetary rewards in adolescent substance users.
- Procedure:
- Task Design: Implement a validated fMRI paradigm, such as a Monetary Incentive Delay (MID) task and a separate drug cue-reactivity task.
- Acquisition: Acquire T2*-weighted BOLD images during task performance. Monitor for head motion.
- Preprocessing: Use pipelines like fMRIPrep or SPM. Steps include realignment, slice-time correction, normalization to standard space, and smoothing.
- First-Level Analysis: Model the BOLD response for different task conditions (e.g., drug cue vs. neutral cue; reward anticipation vs. outcome) for each participant.
- Second-Level Analysis: Compare contrast images (e.g., [Drug Cue > Neutral Cue]) between user and control groups using a whole-brain or ROI-based approach (e.g., in the ventral striatum, OFC). Correlate neural activity with craving measures.
Signaling Pathways & Neurocircuitry
The following diagram illustrates the key neurocircuits and neurotransmitter systems involved in the three-stage addiction cycle, highlighting targets for adolescent vulnerability.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Methods for Adolescent Addiction Neuroscience
| Research Tool | Function/Application | Specific Examples/Considerations |
|---|---|---|
| Structural MRI Analysis Software | Quantifies brain volume, cortical thickness, and surface area from T1-weighted images. | FreeSurfer, FSL, SPM. Critical for tracking developmental trajectories and group differences [13] [10]. |
| fMRI Analysis Pipelines | Processes BOLD data to model brain activity during cognitive tasks or at rest. | fMRIPrep, SPM, FSL, AFNI. Essential for investigating reward, cue reactivity, and executive control [11]. |
| Diffusion Tensor Imaging (DTI) | Models white matter microstructure and structural connectivity (e.g., fractional anisotropy). | FSL's FDT toolbox, Tournier's MRtrix3. Used to assess the integrity of developing white matter tracts [11] [10]. |
| Standardized Neuropsychological Batteries | Assesses cognitive domains known to be impacted by substance use (memory, attention, executive function). | NIH Toolbox, Wechsler scales, and specific tasks for delay discounting (impulsivity) and stop-signal task (response inhibition) [12] [10]. |
| Animal Models of Adolescent Intermittent Access | Allows for controlled investigation of causal effects of adolescent drug exposure on adult outcomes. | Intermittent ethanol vapor or voluntary consumption (e.g., two-bottle choice) in rodents; allows for examination of molecular mechanisms (e.g., epigenetic changes) [16]. |
FAQs: Core Concepts and Common Experimental Challenges
Q1: What are the core neurocircuits and primary functions of the three-stage addiction cycle?
The addiction cycle is a framework for understanding the persistent neurobiological changes that drive compulsive substance use. It is characterized by three recurring stages, each mediated by distinct brain circuits and neurotransmitter systems [8] [14].
Binge/Intoxication Stage: This stage is dominated by the basal ganglia and its circuits. The initial pleasurable effects of a substance are linked to increased dopaminergic and opioid peptide release in the nucleus accumbens (NAcc) within the ventral striatum, a key part of the mesolimbic pathway [8] [14]. As use continues, a shift occurs from "liking" the substance to "wanting" it, a process known as incentive salience. Dopamine firing begins to respond more to substance-associated cues (people, places, things) than the substance itself, fueling reward-seeking behavior. The nigrostriatal pathway, involving the dorsolateral striatum, becomes increasingly involved in controlling these habitual behavior [8].
Withdrawal/Negative Affect Stage: This stage is primarily governed by the extended amygdala (including the bed nucleus of the stria terminalis and central nucleus of the amygdala), often termed the brain's "anti-reward" system [8] [14]. Chronic substance use leads to a downregulation of the brain's reward systems (e.g., decreased dopaminergic tone in the NAcc) and a recruitment of brain stress systems. This results in the increased release of stress mediators like corticotropin-releasing factor (CRF), dynorphin, and norepinephrine [8]. The clinical presentation includes irritability, anxiety, dysphoria, and a diminished capacity to feel pleasure from natural rewards, which creates a powerful negative reinforcement to resume substance use.
Preoccupation/Anticipation Stage: This stage, which occurs during abstinence, is marked by "cravings" and a loss of executive control, primarily mediated by the prefrontal cortex (PFC) [8]. Executive functions such as planning, emotional regulation, and impulse control are compromised. The PFC can be conceptualized as having a "Go system" (for goal-directed behaviors) and a "Stop system" (for inhibitory control); in addiction, this balance is disrupted, leading to executive dysfunction and powerful preoccupation with obtaining the substance [8] [14].
Q2: How does motivation shift from positive to negative reinforcement during the progression of addiction?
The progression from recreational use to addiction involves a critical transition in the primary motivation for substance use [14].
Early Stage: Positive Reinforcement. Initial use is typically driven by positive reinforcement. The substance produces a pleasurable "high" or euphoria (the a-process), which makes the individual more likely to use it again. Behavior at this stage is often impulsive, undertaken for the immediate pleasure with little regard for future consequences [8] [14].
Later Stage: Negative Reinforcement. With repeated use, the pleasurable effects diminish due to tolerance, while the opposing, negative b-process (withdrawal/negative affect) strengthens and appears earlier. Substance use then becomes driven by negative reinforcement—the need to alleviate the distressing symptoms of withdrawal and the underlying negative emotional state. The behavior shifts from impulsive to compulsive, characterized by perseverative use despite adverse consequences [14].
Q3: What are the key individual differences that influence vulnerability to addiction, and how can they be measured?
Individual differences in the neurobiological systems that process reward, incentive salience, habits, stress, and executive function can explain vulnerability to Substance Use Disorders and the diversity of clinical presentations [14] [17]. Key factors include:
- Genetic Variation: Functional polymorphisms in genes related to dopamine signaling (e.g., DRD2, DAT1) have been linked to individual differences in reward-related activation in the ventral striatum and traits like impulsivity, which can increase vulnerability [17].
- Neurofunctional Domains: The Addictions Neuroclinical Assessment (ANA) is a tool that translates the three neurobiological stages into measurable neurofunctional domains: incentive salience, negative emotionality, and executive dysfunction. Assessing these domains helps in characterizing an individual's specific addiction "biotype" [8].
- Circuit-Level Dysfunction: Research indicates there are at least two dissociable cortico-striatal circuits relevant to addiction. Some individuals may exhibit a weakened dorsolateral prefrontal cortex (dlPFC) pathway associated with poor executive control, while others may have a heightened ventromedial prefrontal cortex (vmPFC) pathway linked to exaggerated incentive valuation and stress sensitivity [18]. Modern techniques like functional magnetic resonance imaging (fMRI) and spectral dynamic causal modeling (spDCM) can be used to measure effective connectivity and identify these circuit-level differences [18].
Experimental Protocols: Targeting the Preoccupation/Anticipation Stage with Neuromodulation
The following is a detailed methodology from a recent clinical trial investigating deep Transcranial Magnetic Stimulation (dTMS) to modulate the dysregulated neurocircuitry of addiction, specifically targeting the preoccupation/anticipation stage [18].
Objective: To examine the capacity of two theta-burst stimulation (TBS) protocols to modify neuroimaging and behavioral indices of alcohol use disorder (AUD)-related neurocircuitry alterations, focusing on executive control and craving.
Background: The preoccupation/anticipation stage is characterized by executive dysfunction mediated by the prefrontal cortex. This protocol specifically targets two key nodes: the dorsolateral prefrontal cortex (dlPFC) (part of the "Go system" for executive control) and the ventromedial prefrontal cortex (vmPFC) (part of the limbic circuit for valuation and decision-making) [18].
Protocol Workflow
Detailed Methodology
1. Participant Selection and Eligibility:
- Inclusion: 30 adults (18-49) with current moderate to severe AUD per DSM-5 criteria [18].
- Exclusion: Current or past psychosis, mania, or major unstable psychiatric disorder; history of seizure/epilepsy; brain trauma with loss of consciousness in past 6 months; contraindications for MRI or TMS [18].
2. Trial Design:
- Type: Randomized, single-blind, sham-controlled crossover trial.
- Interventions: Two distinct dTMS protocols using an H-coil for deeper penetration [18]:
- Intermittent TBS (iTBS) to the dlPFC to increase neuronal excitability and strengthen top-down executive control.
- Continuous TBS (cTBS) to the vmPFC to decrease neuronal excitability and dampen hyperactive limbic drive.
- Control: Sham stimulation for placebo comparison.
3. Outcome Measures:
- Primary: Stimulation-induced changes in effective connectivity within targeted dlPFC and vmPFC circuits, measured with resting-state fMRI and spectral dynamic causal modeling (spDCM) [18].
- Secondary: Changes in performance on a cognitive test battery assessing executive control and value-based decision-making.
- Exploratory:
- Laboratory tasks measuring interoceptive processes related to craving.
- Experience Sampling Method (ESM): Daily fluctuations in craving and weekly alcohol consumption tracked for 90 days to assess long-term effects and relapse vulnerability [18].
Data Presentation: Neurotransmitter Systems in the Addiction Cycle
The table below summarizes the key neurotransmitter systems and their roles in the three stages of the addiction cycle, providing a reference for potential pharmacological targets.
Table 1: Key Neurotransmitter Systems and Neuroadaptations in the Addiction Cycle
| Addiction Stage | Primary Brain Region | Key Neurotransmitters/Neuromodulators | Direction of Change & Role |
|---|---|---|---|
| Binge/Intoxication | Basal Ganglia (Ventral Striatum, NAcc) | Dopamine [8] [14] | ↑ Release; mediates incentive salience and reward prediction. |
| Endogenous Opioids (e.g., via μ-opioid receptors) [14] | ↑ Release; contributes to hedonic "high" and reinforcement. | ||
| Endocannabinoids [8] | Modulates dopamine and opioid release. | ||
| Withdrawal/Negative Affect | Extended Amygdala | Corticotropin-Releasing Factor (CRF) [8] | ↑ Release; key driver of stress and anxiety-like responses. |
| Norepinephrine (NE) [8] | ↑ Release; contributes to hyperarousal and stress. | ||
| Dynorphin [8] | ↑ Release; acts on kappa opioid receptors to produce dysphoria. | ||
| Dopamine [8] | ↓ Tonic level in NAcc; leads to anhedonia and reduced motivation for natural rewards. | ||
| Preoccupation/Anticipation | Prefrontal Cortex (PFC) | Glutamate [8] | Imbalance; disrupted signaling underlies executive dysfunction and poor impulse control. |
| GABA [8] | Imbalance; contributes to the shift in excitatory/inhibitory tone in corticostriatal circuits. |
Signaling Pathways and Neurocircuitry
The following diagram illustrates the primary neuroadaptations occurring across the three stages of the addiction cycle, highlighting the within-system and between-system changes that perpetuate the cycle.
Table 2: Essential Research Tools for Investigating the Addiction Neurocircuitry
| Tool/Resource | Category | Primary Function in Research |
|---|---|---|
| Deep TMS (dTMS) with H-coil [18] | Neuromodulation Device | Non-invasive brain stimulation to directly modulate activity and connectivity of deep cortical and subcortical nodes (e.g., dlPFC, vmPFC) in addiction circuits. |
| Functional MRI (fMRI) with Spectral Dynamic Causal Modeling (spDCM) [18] | Neuroimaging & Analysis | Measures task-based and resting-state brain activity. spDCM analyzes the valence (excitatory/inhibitory) and directionality of neural connections within targeted circuits. |
| Experience Sampling Method (ESM) [18] | Behavioral Assessment | Captages real-time, longitudinal data on daily fluctuations in craving, mood, and substance use in a naturalistic setting, reducing recall bias. |
| Theta-Burst Stimulation (TBS) [18] | Neuromodulation Protocol | A patterned TMS protocol (iTBS for potentiation, cTBS for suppression) that mimics endogenous neural firing, offering efficient and potent modulation of cortical excitability. |
| Addictions Neuroclinical Assessment (ANA) [8] | Clinical Framework | A tool to translate the three neurobiological stages of addiction into measurable neurofunctional domains (incentive salience, negative emotionality, executive function) for patient stratification. |
Technical Support Center
The Scientist's Toolkit: Research Reagent Solutions
The following table details key assessment tools and technologies used to investigate trait-based vulnerabilities in addiction neuroscience.
| Item Name | Primary Function/Biological Target | Example Application in Research |
|---|---|---|
| Barratt Impulsiveness Scale (BIS-11) [19] | Assesses trait-level impulsive personality dimensions. | A 30-item self-report questionnaire used to measure attentional, motor, and non-planning impulsivity in study participants. |
| UPPS Impulsive Behavior Scale [19] | Dissects impulsivity into negative/positive urgency, lack of premeditation, lack of perseverance, and sensation seeking. | Used to determine which specific facet of impulsivity is most strongly associated with a substance use disorder (SUD). |
| Stop-Signal Reaction Time (SSRT) Task [19] | Objective measure of response inhibition (motor impulsivity). | Participants must inhibit a prepotent motor response; longer SSRT indicates poorer inhibitory control. |
| Kirby Delay-Discounting Task (KDDT) [19] | Quantifies choice impulsivity by measuring preference for smaller immediate rewards over larger delayed rewards. | A steeper discounting rate is used as a behavioral marker of impulsive decision-making in addiction. |
| Resting-State Electroencephalography (EEG) [20] | Non-invasive measurement of spontaneous brain activity and functional connectivity. | Used to identify neurophysiological correlates of trait impulsivity, such as specific power spectral and network connectivity patterns in the beta band. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the key distinction between "trait" and "state" impulsivity in the context of substance use disorders?
The relationship between impulsivity and Substance Use Disorders (SUDs) is complex and involves three key factors: the trait effect, which is a pre-existing vulnerability characterized by decreased cognitive and response inhibition; the state effect, which refers to acute or chronic changes in brain structure and function caused by substance use; and the influence of genetic and environmental factors like age and sex [19]. Trait impulsivity is a stable, underlying vulnerability marker, whereas state impulsivity is a transient condition influenced by drug intake or withdrawal.
FAQ 2: Our team is observing low correlations between self-report and behavioral measures of impulsivity in our dataset. Is this a methodological problem?
Not necessarily. It is common to find little overlap between self-report questionnaires (e.g., BIS-11) and objective behavioral tasks (e.g., SSRT, delay-discounting) [19]. These tools are understood to measure three conceptually related but quantitatively distinct domains of impulsivity: personality traits, discounting preferences, and response inhibition [19]. It is recommended to use a multi-method assessment battery to capture these different components.
FAQ 3: How does emotional dysregulation specifically contribute to addiction and relapse?
Emotional dysregulation is a core characteristic of substance dependence [21]. It involves disturbances in brain reward and stress systems. This can lead to a bias in emotional processing toward drug-related cues at the expense of natural rewards, enhancing drug craving. Furthermore, chronic drug use can sensitize the brain's stress systems, leading to negative emotional states that persist into abstinence. This negative state motivates drug-taking to achieve relief (negative reinforcement) and significantly increases the risk of relapse [21].
FAQ 4: Which neurophysiological marker from resting-state EEG is most informative for studying impulsivity?
Research indicates that power spectral density and functional connectivity in the beta band are particularly informative. Studies have shown that individuals with gambling addiction exhibit higher beta power, and those with methamphetamine addiction show less efficient network connectivity in this band compared to controls [20]. Furthermore, specific connectivity patterns in the beta band are correlated with impulsivity scores and can help differentiate individuals with addiction from healthy controls [20].
Troubleshooting Guides
Issue 1: Inconsistent or No Significant Findings in Neurophysiological Correlates of Impulsivity
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| High Participant Heterogeneity | Check for variations in SUD type, chronicity, and polydrug use history within your cohort. | Implement stricter participant inclusion criteria. Pre-stratify groups based on key clinical variables (e.g., primary drug of abuse, years of use) during the recruitment phase. |
| Comorbid Mental Health Conditions | Administer structured clinical interviews (e.g., SCID-5) to assess for comorbid disorders like ADHD, anxiety, or depression. | Include comorbidities as a separate experimental group or as a covariate in your statistical model to account for their confounding effects on impulsivity measures. |
| Medication Interference | Meticulously document all prescribed medications (e.g., methadone, buprenorphine, naltrexone) that participants may be taking [22]. | Either recruit medication-free participants or ensure that medication status is balanced across groups and included as a statistical covariate in analyses. |
Issue 2: Poor Participant Engagement or High Dropout Rates in Longitudinal Studies
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| High Burden of Testing Battery | Audit the total time required for all assessments (clinical, behavioral, neuroimaging). | Streamline the protocol by selecting the most sensitive and specific measures for your primary hypotheses. Consider breaking long sessions into shorter, more manageable visits. |
| Lack of Clinical Support | Assess whether participants feel their broader clinical needs are being met. | Integrate the research study within a treatment program or have clear, streamlined referral pathways to clinical care [22]. This demonstrates a commitment to participant well-being beyond data collection. |
| Insufficient Compensation or Rapport | Solicit anonymous feedback from past participants about their experience. | Implement a fair compensation schedule that increases for follow-up visits. Train research staff extensively on building rapport and communicating with empathy and respect. |
Experimental Protocols
Protocol 1: A Multi-Method Assessment of Impulsivity in Substance Use Disorders
I. Objective To comprehensively profile the different dimensions of impulsivity (trait, behavioral, and neurophysiological) in a cohort of individuals with Substance Use Disorders (SUDs) compared to healthy controls.
II. Materials
- Consent forms and demographic questionnaire
- Clinical Assessments: Mini-International Neuropsychiatric Interview (MINI) or Structured Clinical Interview for DSM-5 (SCID-5) to confirm SUD and assess comorbidities.
- Self-Report Impulsivity Measures:
- Behavioral Tasks (Computerized):
- Neurophysiological Recording:
- EEG system with a 32-channel (or higher) cap
- Electrically shielded, quiet room
III. Step-by-Step Methodology
- Screening & Consent: Obtain informed consent. Screen participants using clinical interviews to assign them to the SUD or control group based on pre-defined criteria.
- Self-Report Assessment: Administer the BIS-11 and UPPS-P questionnaires in a quiet room, counterbalancing the order of presentation across participants.
- Behavioral Task Setup: Seat the participant approximately 60 cm from the computer monitor. Provide standardized verbal instructions for each task.
- Behavioral Task Execution:
- SSRT Task: Conduct a practice block followed by the main experimental block. The task involves responding to "go" stimuli (e.g., arrows) and inhibiting the response when a "stop" signal (e.g., a tone) occurs shortly after the go stimulus. The stop-signal delay is adjusted dynamically.
- Delay-Discounting Task: Present participants with a series of choices between a smaller, immediate monetary reward and a larger, delayed reward (e.g., "Would you prefer $20 now or $60 in 30 days?").
- EEG Preparation and Recording:
- Prepare the scalp and apply the EEG cap according to the 10-20 system.
- Ensure impedances are kept below 5 kΩ.
- Record a 5-minute resting-state EEG with eyes closed, followed by a 5-minute recording with eyes open, in a seated position.
- Data Analysis:
- Behavioral: Calculate SSRT for the stop-signal task and a discounting parameter (e.g., k-value) for the delay-discounting task.
- Self-Report: Score the questionnaires according to their respective manuals.
- EEG: Preprocess the data (filtering, artifact removal). Compute power spectral density and functional connectivity metrics (e.g., Phase Lag Index) in standard frequency bands, with a focus on beta band activity [20].
Protocol 2: Investigating the Impact of Emotional Cues on Decision-Making
I. Objective To examine how emotional dysregulation biases decision-making processes in individuals with SUDs, using a modified gambling task with emotional stimuli.
II. Materials
- Software: Experiment builder (e.g., E-Prime, PsychoPy) for task programming.
- Stimuli: Standardized emotional images (e.g., from the International Affective Picture System - IAPS) categorized as neutral, positive, and negative.
- Task: A modified version of the Iowa Gambling Task (IGT) [19] where emotional images are presented as context during decision-making blocks.
III. Step-by-Step Methodology
- Participant Grouping: Recruit three groups: SUD group, a psychiatric control group with emotional disorders, and a healthy control group.
- Task Design: The task consists of three blocks, each preceded by a different emotional context (neutral, positive, or negative images). Each block uses the standard IGT structure where participants select cards from four decks with different reward/punishment contingencies.
- Procedure: Participants are seated and instructed to maximize their play money total. They complete the three IGT blocks in a randomized order.
- Data Collection: Record the number of advantageous vs. disadvantageous choices per block, reaction times, and psychophysiological measures (e.g., skin conductance response) if available.
- Data Analysis: Perform a mixed-model ANOVA with Group as a between-subjects factor and Emotional Context (and potentially Task Block) as within-subjects factors on the net score (advantageous - disadvantageous choices). This tests the hypothesis that the SUD group's decision-making is disproportionately impaired under specific emotional contexts, such as heightened risk-taking during positive states (positive urgency) [21].
Experimental Workflow and Signaling Pathways
Research Workflow for Trait Vulnerabilities
Pathways to Addiction Involving Traits
Advanced Methodologies for Deconstructing Heterogeneity: From Neuroimaging to GWAS
Applying Network Control Theory to Measure Brain Flexibility and State Transitions
Network Control Theory (NCT) provides a powerful framework for understanding how the brain's structural connectome informs and constrains its dynamic activity. This technical support guide explores how NCT can be applied to study individual differences in addiction neurobiology, offering researchers methodologies to quantify brain flexibility and state transitions relevant to the addiction cycle. By applying NCT, scientists can model the neuroadaptations that occur across the binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation stages of addiction, potentially identifying novel biomarkers and treatment targets [8].
Frequently Asked Questions (FAQs)
Q1: What is Network Control Theory and how is it relevant to addiction research?
Network Control Theory is a mathematical framework from engineering that models how external control signals can steer a system's dynamics toward a desired state. When applied to neuroscience, NCT uses the brain's structural connectome to understand how activity in one region influences others. For addiction research, this is particularly valuable for modeling transitions between the different stages of the addiction cycle and understanding how control energy requirements differ between individuals with and without substance use disorders [23]. Recent studies have shown that heavy alcohol use alters structural connectivity and functional brain dynamics, which can be quantified using NCT [24].
Q2: What are the key NCT metrics for studying brain flexibility in addiction?
The table below summarizes the primary NCT metrics used to study brain flexibility:
Table: Key NCT Metrics for Brain Flexibility Research
| Metric | Definition | Interpretation in Addiction |
|---|---|---|
| Control Energy | Amount of input required for state transitions [23] | Higher energy may indicate rigid, compulsive states [24] |
| Average Controllability | Node's ability to spread impulse across network [23] | Identifies hubs that may drive craving or relapse |
| Modal Controllability | Node's ability to drive difficult-to-reach states [23] | Potential for accessing non-habitual brain states |
| Intrinsic Neural Timescales (INTs) | Temporal specialization of brain regions [24] | May reflect tolerance to drug effects or recovery processes |
Q3: What are the data requirements for applying NCT to addiction neurobiology?
NCT requires both structural and functional neuroimaging data. The structural connectome is typically derived from diffusion tensor imaging (DTI), which maps white matter fiber tracts between brain regions. Functional data from fMRI provides information on brain states. For addiction research specifically, it's valuable to collect data during tasks or states relevant to the addiction cycle (e.g., cue exposure, withdrawal states) to define meaningful initial and target states for NCT analyses [23] [24].
Q4: How can NCT help identify individual differences in addiction vulnerability?
Individual differences in addiction vulnerability may manifest as variations in network controllability properties. NCT can quantify how efficiently individuals can transition between brain states, with potentially lower control energy requirements for state transitions associated with greater cognitive flexibility and resilience against addictive patterns. Conversely, higher control energy requirements might reflect the compulsivity and rigid behavioral patterns observed in later stages of addiction [14] [8] [24].
Troubleshooting Common Experimental Issues
Problem: Inconsistent control energy calculations across research sites
Solution: Implement standardized preprocessing pipelines for structural connectome construction. Key steps include:
- Use consistent parcellation schemes (e.g., AAL, Desikan-Killiany)
- Apply quality control metrics for tractography (e.g., fractional anisotropy thresholds)
- Normalize connection weights using standardized approaches (e.g., streamline count with proportional scaling)
- Validate NCT outputs with null network models to ensure results reflect true network properties rather than computational artifacts [23]
Problem: Relating NCT metrics to clinical measures of addiction severity
Solution:
- Collect comprehensive phenotypic data including addiction severity scales (e.g., AUDIT, DAST)
- Map NCT metrics to the three-stage addiction cycle model:
- Binge/Intoxication: Examine control energy for transitions to reward-related states
- Withdrawal/Negative Affect: Analyze transitions involving stress and emotion networks
- Preoccupation/Anticipation: Study controllability of executive control networks [8]
- Use multivariate approaches to account for comorbidities that may influence network dynamics [25]
Problem: Integrating NCT with molecular targets for drug development
Solution: Leverage transcriptomic and receptor distribution data from resources like the Allen Human Brain Atlas to connect NCT findings with potential pharmacological targets. Recent research has demonstrated relationships between NCT metrics and distributions of specific neurotransmitter receptors (e.g., serotonin 2a receptors), providing a bridge between network-level dynamics and molecular interventions [24].
Experimental Protocols
Protocol 1: Calculating Control Energy for State Transitions
Purpose: To quantify the energy required to transition between brain states relevant to addiction.
Materials:
- Structural connectome (n × n adjacency matrix)
- Definition of initial and target brain states (n × 1 vectors)
- NCT computational environment (e.g., NCTPy Python package) [23]
Procedure:
- Define State Vectors: Represent neural states using activity patterns from fMRI data. For addiction studies, define states relevant to the addiction cycle (e.g., craving state, satiety state).
- Formulate Control Problem: Use the discrete-time linear time-invariant system model:
x(t+1) = Ax(t) + Bu(t)[23] Where A is the structural connectome, x(t) is the state vector, and u(t) is the control input. - Compute Optimal Control Inputs: Solve for the control inputs that minimize the energy function:
E = Σ[u(t)ᵀu(t)][23] - Compare Groups: Calculate and compare control energy between individuals with substance use disorders and healthy controls for the same state transitions.
Table: Parameters for Control Energy Calculation
| Parameter | Description | Recommended Setting |
|---|---|---|
| System Matrix (A) | Structural connectome | Normalized by largest eigenvalue |
| Control Matrix (B) | Nodes receiving input | Identity matrix for full control |
| Time Horizon | Steps for transition | T = 10 for discrete model |
| State Constraints | Bounds on neural activity | -1 to 1 for normalized states |
Protocol 2: Assessing Regional Controllability in Addiction
Purpose: To identify brain regions with altered controllability properties in addiction.
Materials:
- Structural connectomes from participants with substance use disorders and matched controls
- Parcellated fMRI data during rest and task conditions
- Computational resources for network analysis
Procedure:
- Compute Average Controllability: For each brain region, calculate the average controllability metric, which measures a node's ability to steer the brain into easily reachable states [23].
- Compare Between Groups: Use appropriate statistical tests (e.g., ANCOVA controlling for age, sex) to identify regions with significant differences in controllability between groups.
- Relate to Addiction Stages: Map regions with altered controllability to the three-stage addiction model:
- Validate with Behavioral Measures: Correlate controllability metrics with clinical assessments of addiction severity and cognitive function.
NCT Data Analysis Workflow
The following diagram illustrates the complete workflow for applying NCT to addiction research:
NCT Analysis Workflow for Addiction Research
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for NCT Addiction Research
| Resource Type | Specific Examples | Application in NCT Addiction Research |
|---|---|---|
| Neuroimaging Data Repositories | Human Connectome Project, MICAMICs [24] | Source of standardized connectome data for control group comparisons |
| Computational Tools | NCTPy Python package [23] | Implementation of core NCT algorithms and metrics |
| Gene Expression Atlases | Allen Human Brain Atlas [24] | Linking NCT findings to molecular targets |
| Clinical Assessment Tools | Addiction Severity Index, Penn Alcohol Craving Scale | Correlating NCT metrics with clinical measures |
| Parcellation Schemes | AAL, Desikan-Killiany, Schaefer atlases | Standardized brain region definitions for cross-study comparisons |
Key Signaling Pathways in Addiction Neurobiology
The following diagram illustrates the primary neurocircuits involved in the addiction cycle, which serve as key systems for NCT analysis:
Neurocircuits of the Addiction Cycle
The Adolescent Brain Cognitive Development (ABCD) Study is a landmark longitudinal study on brain development and child health supported by the National Institutes of Health (NIH). This landmark research project aims to increase our understanding of environmental, social, genetic, and other biological factors that affect brain and cognitive development, ultimately seeking to identify factors that can enhance or disrupt a young person's life trajectory [26]. The study represents the largest long-term investigation of brain development and child health ever conducted in the United States, with nearly $290 million in new funding recently allocated for an additional seven years of research [26].
The ABCD Study's relevance to addiction neurobiology is profound, particularly in understanding individual differences in vulnerability to substance use disorders. The study was originally conceived to "examine risk and resiliency factors associated with the development of substance use" but has since expanded to inform our understanding of how biospecimens, neural alterations, and environmental factors contribute to both healthy behavior and risk for poor mental and physical outcomes [27]. By tracking participants from ages 9-10 into young adulthood, the ABCD Study provides unprecedented insight into the developmental trajectories that lead to substance use initiation, progression, and potential addiction, with a particular focus on individual differences in neurobiological susceptibility.
ABCD Study Design and Methodology
Cohort Composition and Recruitment
The ABCD Study employs a comprehensive, multi-faceted approach to recruitment and retention, ensuring a representative sample of the U.S. adolescent population:
Table: ABCD Study Cohort Characteristics
| Characteristic | Specification |
|---|---|
| Total Enrollment | 11,880 children [26] |
| Age at Baseline | 9-10 years old [26] |
| Recruitment Sites | 21 sites across the United States [27] |
| Study Duration | Planned follow-up for 10 years into young adulthood [26] [27] |
| Recruitment Method | Multi-stage probability sample including stratified random sample of schools [27] |
The study completed enrollment for the baseline sample in October 2018, with the goal of retaining approximately 10,000 participants into early adulthood [26]. The recruitment strategy employed a multi-stage probability sample including a stratified random sample of schools to ensure demographic diversity and representativeness [27].
Data Collection Domains and Assessment Schedule
The ABCD Study collects a wealth of multimodal data through repeated assessments at specified intervals:
Table: ABCD Study Data Collection Domains and Schedule
| Domain | Specific Measures | Assessment Schedule |
|---|---|---|
| Neuroimaging | Structural MRI (T1w, T2w), resting-state fMRI, task fMRI (Monetary Incentive Delay, Stop-Signal, Emotional N-Back), diffusion MRI [28] | Approximately every 2 years for neuroimaging; more frequently for behavioral assessments [29] |
| Cognitive Assessment | NIH Toolbox, neuropsychological tests [27] | Regular intervals (e.g., 6 months) [29] |
| Mental & Physical Health | K-SADS, ASEBA, mental health disorders, physical health metrics [27] | Regular intervals throughout study |
| Biospecimens | DNA, RNA, plasma, serum, cortisol, pubertal hormones [27] | Collected at baseline and follow-ups |
| Environmental Factors | Family history, cultural identification, school environment, neighborhood characteristics [27] | Ongoing assessment |
| Substance Use | Timeline Followback, substance use initiation and patterns [27] | Regular monitoring, especially during high-risk periods |
Behavioral and clinical assessments are administered at shorter intervals than neuroimaging assessments [29]. This comprehensive approach allows researchers to examine how various factors interact across development and how individual differences in these domains may predict substance use trajectories.
Technical Support Center: ABCD Data Access and Management
Data Access Frequently Asked Questions
How do I access ABCD Study data? ABCD data are publicly shared with eligible researchers with a valid research use of the data at a research institution. Researchers must visit the NBDC Datahub or the ABCD Study website for detailed information on how to access and download the data [28].
Can researchers from non-U.S. institutions access the data? Yes, researchers from international institutions with an active Federal Wide Assurance (FWA) can access ABCD data. Many international researchers have successfully accessed and published with ABCD Study data [28].
Is there a cost to access the data? No, there is no cost to access the ABCD Study dataset [28].
Do I need IRB approval to use ABCD data? Institutional requirements vary regarding de-identified datasets. Some institutions require expedited or exempt IRB reviews, while others do not consider working with de-identified data to constitute human subjects research. Researchers should consult their local IRB for guidance [28].
Can students or trainees access ABCD data? Lead investigators may obtain Data Use Certificates (DUCs) that include trainees, lab members, and collaborators at their institution. The lead investigator is responsible for ensuring compliance with DUC terms and conditions and must renew the DUC annually [28].
Data Analysis Troubleshooting Guide
Issue: Inconsistent imaging data quality across sites Solution: The ABCD Study has implemented rigorous quality control procedures including standardized acquisition protocols across all 21 sites. The minimally processed neuroimaging data have undergone standard modality-specific preprocessing stages including conversion from raw to compressed files, distortion correction, movement correction, alignment to standard space, and initial quality control [28]. Researchers should consult the imaging documentation for quality control metrics and exclude participants based on established QC criteria.
Issue: Cerebellum cutoff in fMRI and dMRI data Explanation: Due to relatively tight brain coverage for dMRI and fMRI acquisitions, the superior or inferior edge of the brain is sometimes outside of the stack of slices, a phenomenon called "field of view (FOV) cutoff" [28]. Solution: The ABCD Study provides automated post-processing QC metrics that include measures of superior and inferior FOV cutoff. Researchers can use these metrics to exclude participants with significant FOV cutoff from analyses. In tabulated imaging data, brain regions outside the FOV have missing values, but other regions remain usable [28].
Issue: Multiple dMRI series for Philips scanners Explanation: For imaging data from Philips scanners, the dMRI acquisition is split into two series due to a platform limitation. Both scans have the same phase-encode polarity and are meant to be concatenated together [28]. Solution: For minimally processed data, one scan is selected for each session based on QC ratings, except for Philips scanners, in which case two are selected for packaging and sharing. Researchers working with Philips scanner data should ensure proper concatenation of these series.
Issue: When should field maps be used? Solution: The "minimally processed" images have already been corrected for B0 distortion using field maps, so field maps are not necessary for these data. However, if researchers are working with "fast track" unprocessed data, they would need to perform distortion correction using the field maps provided in Fast Track [28].
Methodological Protocols for Key ABCD Experiments
Neuroimaging Acquisition and Processing Protocol
The ABCD Study employs a comprehensive neuroimaging protocol across all 21 sites:
Structural Imaging:
- High-resolution 3D T1-weighted (T1w) and T2-weighted (T2w) scans
- Parameters: Consistent across sites with standardized sequences
- Processing: Includes alignment to standard space and quality control metrics
Functional MRI:
- Resting-state fMRI: Eyes-open fixation
- Task-based fMRI: Monetary Incentive Delay (reward processing), Stop-Signal Task (response inhibition), Emotional N-Back (working memory and emotion regulation)
- Preprocessing: Distortion correction, movement correction, alignment to standard space
Diffusion MRI:
- Multiple b-values and directions for advanced diffusion modeling
- Processing: Diffusion gradients adjusted for head rotation, provided as bvecs.txt and bvals.txt files
- Registration: Rigid-body transformation matrix provided for registration between dMRI and corresponding T1w image
The minimally processed imaging data are shared in BIDS-formatted directory trees as NIfTI files, accompanied by JSON files containing imaging metadata derived from original DICOM files [28].
Genetic and Biospecimen Collection Protocol
The ABCD Study collects and processes various biospecimens through a standardized protocol:
- Blood samples: Processed for DNA, RNA, plasma, serum, and cryopreserved lymphocytes
- Saliva samples: Alternative source for genetic material
- Analysis coordination: RUCDR Infinite Biologics at Rutgers University provides materials for collecting samples and performs genetic/epigenetic analyses [29]
- Banking: Biospecimens are banked for future analyses to be determined later
For researchers interested in additional assays, NIDA has developed a mechanism for requesting biosamples through the NBDC biospecimen access program [28].
ABCD Neuroimaging Acquisition Workflow
Investigating Individual Differences in Addiction Neurobiology Using ABCD Data
Theoretical Frameworks for Individual Differences in Addiction
Understanding individual differences in addiction susceptibility requires comprehensive theoretical models that account for neurobiological variability:
The Opponent-Process Theory: Developed by Solomon and Corbit, this theory suggests that when a positive affective response is activated by drug use, an opposing negative response is simultaneously triggered to restore homeostasis. With repeated drug use, the opponent process intensifies, leading to tolerance and withdrawal symptoms [30]. Individual differences in the strength and timing of these processes may explain variability in addiction vulnerability.
Dopaminergic Hypothesis of Addiction: This framework posits that drugs of abuse act through a common mechanism of increasing dopamine in the brain's reward system, particularly the mesolimbic pathway projecting from the ventral tegmental area to the nucleus accumbens [30]. Individual differences in baseline dopamine function or receptor density may moderate susceptibility to addiction.
Three-Stage Addiction Cycle Model: Koob's model conceptualizes addiction as progressing through binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation stages, each with distinct neurobiological substrates [14]. Individual differences may manifest in the propensity to transition between these stages.
Oxytocin System Influence: Recent research indicates that individual differences in the endogenous oxytocin system, shaped by genetic variation and early environmental influences, may affect susceptibility to addiction through interactions with stress systems, neurotransmitter systems, and reward pathways [31].
Analyzing Individual Differences in ABCD Data
The ABCD Study provides unique opportunities to investigate individual differences in addiction neurobiology through several analytical approaches:
Twin Studies: The ABCD cohort includes twin pairs, allowing researchers to disentangle genetic and environmental contributions to substance use outcomes [27].
Longitudinal Growth Modeling: Repeated assessments enable tracking of individual trajectories in brain development, cognitive function, and behavior, identifying patterns associated with substance use initiation.
Machine Learning Approaches: Large sample size permits development of predictive models identifying neurobiological, cognitive, and environmental features associated with substance use outcomes.
Gene-Environment Interactions: Comprehensive genetic and environmental data allow examination of how specific genetic profiles interact with environmental factors to influence substance use risk.
Table: Key Research Reagent Solutions for ABCD Data Analysis
| Tool/Resource | Function | Access Point |
|---|---|---|
| NBDC Data Hub | Primary data access portal for ABCD data | https://data-archive.nimh.nih.gov/abcd |
| BIDS Format Data | Standardized neuroimaging data structure | ABCD Data Releases |
| PhenX Toolkit | Common measures for cross-study comparisons | https://www.phenxtoolkit.org/ |
| NIH Toolbox | Standardized cognitive assessment metrics | https://www.healthmeasures.net/ |
| FreeSurfer Output | Structural MRI processing outputs | Included in BIDS derivatives |
| ABCD Harmonized Code | Standardized processing pipelines | ABCD Study Resources |
Advanced Analytical Approaches for Individual Differences Research
Machine Learning Applications for Predicting Substance Use Outcomes
Recent research demonstrates the power of machine learning approaches for identifying individual differences in addiction susceptibility:
Functional Network Connectivity Predictive Models: Research by investigators outside the ABCD Study has shown that machine learning pattern classification models using functional network connectivity can predict with approximately 80% accuracy which individuals will complete substance abuse treatment programs [32]. Similar approaches can be applied to ABCD data to identify youth at highest risk for problematic substance use.
Key Predictive Features:
- Connectivity between anterior cingulate cortex, striatum, and insula
- Executive control network integrity
- Salience network function
- Default mode network regulation
These approaches highlight how neurobiological individual differences can be leveraged to predict real-world outcomes relevant to addiction.
Multilevel Modeling of Individual Differences
The ABCD dataset enables sophisticated multilevel modeling approaches:
Cross-Level Interactions: Examining how genetic factors moderate neural responses to environmental stressors Developmental Timing Effects: Investigating how the timing of substance use initiation interacts with neurodevelopmental trajectories Resilience Factors: Identifying protective factors that buffer against substance use despite high-risk profiles
Framework for Individual Differences in Addiction Vulnerability
Frequently Asked Questions on ABCD Study Applications
How can I propose new assays for collected biospecimens? NIDA has developed a mechanism for requesting biosamples through the NBDC biospecimen access program. All currently analyzed specimens are part of the data release, and researchers can petition for additional assays [28].
Are there assessments of autism spectrum disorder in the ABCD sample? The ABCD Study exclusion criteria included "a current diagnosis of schizophrenia, autism spectrum disorder (moderate, severe), intellectual disability, or alcohol/substance use disorder." While ABCD does not maintain comprehensive assessments related to diagnosed ASD, the KSADS includes diagnostic categories, including autism spectrum disorder based on parent report only [28].
Can I use AI tools like ChatGPT to analyze ABCD data? No, inputting ABCD data to generative AI tools such as ChatGPT is a violation of the terms of use outlined in the data use agreement [28].
Where can I find detailed information about specific measures used in ABCD? The ABCD Study provides extensive documentation on their website, including information about study design and protocols in the Scientist section. However, many specific measures are proprietary and cannot be shared [28].
How is substance use assessed in the ABCD Study? Substance use assessment includes the Timeline Followback method for detailed substance use history, along with regular monitoring of substance use initiation and patterns, particularly during high-risk developmental periods [27].
The ABCD Study represents an unprecedented resource for investigating individual differences in addiction neurobiology. By providing comprehensive, longitudinal data across multiple domains, it enables researchers to examine how genetic, neural, cognitive, and environmental factors interact across development to influence substance use trajectories. The technical support resources outlined in this article provide essential guidance for researchers navigating this complex dataset and leveraging it to advance our understanding of why individuals differ in their susceptibility to addiction.
As the ABCD cohort progresses through adolescence and into young adulthood—the period of highest risk for substance use initiation and progression—the value of this dataset will continue to grow. Future directions include examining the transition from initial substance use to regular use and disorder, identifying neurodevelopmental factors that predict treatment response, and elucidating the mechanisms underlying resilience despite high-risk profiles. Through continued analysis of this rich dataset, the research community moves closer to personalized prevention and intervention approaches that account for the fundamental individual differences in addiction neurobiology.
Genome-Wide Association Studies (GWAS) and the Genetically Informed Neurobiology of Addiction (GINA) Model
GWAS & GINA Model FAQ: Core Concepts for Researchers
FAQ 1: What is the primary objective of a Genome-Wide Association Study (GWAS) in addiction research?
A Genome-Wide Association Study (GWAS) is a research approach that tests hundreds of thousands of genetic variants across many genomes to identify those statistically associated with a specific trait or disease, such as substance use disorder [33] [34]. In addiction research, its goal is to pinpoint specific genomic loci and genetic architectures that contribute to an individual's liability for addiction, thereby providing insights into the underlying biology of this complex brain disorder [35] [36].
FAQ 2: How does the GINA model advance previous neurobiological theories of addiction?
The Genetically Informed Neurobiology of Addiction (GINA) model integrates findings from large-scale genomic studies with established brain-based models of addiction [35] [37]. It proposes that genetic liability to addiction is composed of two main components: a general, broad-spectrum liability that cuts across different substances and disorders, and substance-specific genetic risks [35] [38]. This model uses genomic evidence to inform our understanding of how addiction unfolds dynamically across the lifespan, moving beyond theories that focused predominantly on substance-induced neural changes [35].
FAQ 3: What is the key genetic distinction between substance use and a substance use disorder (SUD)?
GWAS results reveal a moderate to high genetic correlation between ever using a substance (e.g., ever smoking) and developing a disordered pattern of use (e.g., nicotine dependence) [35]. However, they are not genetically identical. Crucially, substance use and substance use disorders can show opposing genetic correlations with other outcomes like educational attainment and certain health conditions, highlighting the importance of carefully defining phenotypic traits in genetic studies [35].
FAQ 4: What is the polygenic architecture of addiction, and what does it imply for research?
Addiction is highly polygenic, meaning risk is influenced by many genetic variants, each with a very small individual effect size [33] [39]. This architecture explains why very large sample sizes are required for GWAS to have sufficient power to detect these variants reliably. It also underscores that there is no single "addiction gene"; rather, risk emerges from the aggregate of thousands of common and rare genetic variations [39] [36].
Troubleshooting Common GWAS Workflow Issues
Issue 1: Inflated Test Statistics and False Positives Due to Population Stratification
- Problem: A key quality control (QC) check reveals significant genomic inflation, potentially leading to false positive associations.
- Background: Population stratification occurs when a study sample contains subpopulations with different allele frequencies and different baseline rates of the trait (e.g., due to cultural or environmental factors). This can create spurious genetic associations if not corrected [39].
- Solution:
- Pre-Analysis Correction: Apply a standard method such as Principal Components Analysis (PCA) to genotype data. The top principal components can be included as covariates in the association model to correct for underlying population structure [33] [39].
- Post-Analysis Inspection: Calculate the genomic inflation factor (λ). A λ value significantly greater than 1.0 suggests confounding inflation. Examine quantile-quantile (Q-Q) plots to visually assess the deviation of observed p-values from the null expectation.
- Use of Family-Based Designs: Where possible, using within-family analyses (e.g., sibling controls) can effectively control for population stratification because family members share genetic ancestry [33].
Issue 2: Inconsistent Replication of Candidate Gene Findings in GWAS
- Problem: Historically reported associations from candidate gene studies often fail to replicate in well-powered GWAS.
- Background: Early candidate gene studies were typically underpowered and focused on biologically plausible genes (e.g., dopamine receptors) without a hypothesis-free scan of the genome. The polygenic nature of addiction means that individual effect sizes are very small, requiring large samples to detect them reliably [39] [36].
- Solution:
- Increase Sample Size: Prioritize participation in or meta-analysis of large consortia (e.g., GWAS & Sequencing Consortium of Alcohol and Nicotine Use (GSCAN)) to achieve sample sizes in the hundreds of thousands [33] [35].
- Ensure Stringent Quality Control: Adhere to strict QC pipelines for both genotype and phenotype data to minimize noise [39].
- Use Genome-Wide Significance Thresholds: Apply a multiple testing correction threshold of p < 5 × 10^-8 to declare statistical significance, which accounts for testing millions of independent common variants across the genome [39].
Issue 3: Handling Relatedness in Samples Assumed to Be Unrelated
- Problem: Standard GWAS assumes individuals are unrelated. The presence of unknown relatedness (cryptic relatedness) can bias association test results.
- Background: Relatedness refers to how closely genetically related a pair of individuals is. Including closely related individuals can inflate test statistics because their genotypes are not independent [39].
- Solution:
- Calculate Relatedness: Use software like PLINK to estimate identity-by-descent (IBD) between all sample pairs.
- Prune Related Individuals: Remove one individual from each pair that is more closely related than a predefined threshold (e.g., second-degree relatives).
- Use Robust Association Methods: For biobank-scale datasets with complex relatedness structures, use mixed-model association methods (e.g., BOLT-LMM, REGENIE) that can account for relatedness and population structure simultaneously by using a genetic relationship matrix [33].
Issue 4: Low SNP-Heritability and Discovery Yield for a Substance Use Disorder Trait
- Problem: A GWAS for a specific SUD yields a low SNP-heritability estimate and identifies very few significant loci.
- Background: SNP-heritability is the proportion of phenotypic variance explained by all common SNPs on the array. Low estimates can stem from a combination of factors, including a small sample size (low power), imprecise phenotype measurement, or a trait influenced largely by rare variants or environmental factors [35] [39].
- Solution:
- Refine Phenotyping: Use clinically validated, precise definitions for the disorder (e.g., DSM-5 criteria for severe SUD) rather than broad proxies. Misclassification of cases and controls dramatically reduces power [35].
- Increase Power via Meta-Analysis: Collaborate to combine results from multiple studies. Tools like METAL are designed for efficient meta-analysis of genome-wide association scans [33].
- Consider Rare Variants: For traits where common variants explain little heritability, consider sequencing-based studies and rare-variant association tests (e.g., SKAT) to investigate the role of less common genetic variations [33].
Quantitative Data on the Genetics of Substance Use Disorders
Table 1: GWAS Findings for Substance Use and Use Disorders (Adapted from [35])
| Substance | Phenotype | Largest GWAS Sample Size | SNP-Heritability (h²SNP) | Number of Independent Risk Loci | Genetic Correlation (rG) between Use and Disorder |
|---|---|---|---|---|---|
| Alcohol | Alcohol Use Disorder | 435,563 | 0.07 | 29 | 0.77 |
| Drinks per Week | 941,280 | 0.04 | 99 | ||
| Tobacco/Nicotine | Nicotine Dependence | 58,000 | 0.09 | 5 | 0.4 – 0.5 |
| Ever Smoked | 1,232,091 | 0.08 | 378 | ||
| Cannabis | Cannabis Use Disorder | 384,925 | 0.12 | 2 | 0.50 |
| Ever Used Cannabis | 184,765 | 0.11 | 8 | ||
| Opioids | Opioid Use Disorder | ~639,709 | 0.13 | 10 | N/A |
Table 2: Essential GWAS Software and Analytical Tools [33] [39]
| Tool Name | Primary Function | Application in Addiction Research |
|---|---|---|
| PLINK | Whole-genome association analysis, data management, and QC. | Core toolset for performing case-control and quantitative trait association analyses, data filtering, and basic QC steps. |
| PRSice | Polygenic Risk Score analysis. | Calculating individual-level genetic risk scores for addiction liability in independent target samples using summary statistics from a discovery GWAS. |
| METAL | Meta-analysis of GWAS results. | Combining summary statistics from multiple independent GWAS of addiction phenotypes to increase power and discover novel loci. |
| RICOPILI | Rapid Imputation for Consortia Pipeline. | A standardized pipeline for quality control, imputation, and analysis of GWAS data, often used in large psychiatric genetics consortia. |
| BOLT-LMM/REGENIE | Mixed-model association analysis. | Efficiently conducting GWAS in large biobank-scale datasets while accounting for relatedness and population structure. |
Key Experimental Protocols
Protocol 1: Standard GWAS Quality Control (QC) Pipeline
This protocol outlines the standard QC steps for genotype data prior to association analysis, crucial for generating reliable results [39].
Individual-Level QC:
- Missingness: Remove individuals with high genotype missingness rates (e.g., > 5%).
- Sex Discrepancy: Check for mismatches between genetically inferred sex and self-reported sex; exclude individuals with discrepancies.
- Heterozygosity: Exclude individuals with extreme heterozygosity rates (e.g., ±3 SD from the mean), which can indicate sample contamination or inbreeding.
- Relatedness: Calculate pairwise identity-by-descent (IBD) and remove one individual from each pair with a relatedness coefficient above a threshold (e.g., > 0.185, corresponding to second-degree relatives).
- Ancestry: Use PCA to project study participants onto reference panels (e.g., 1000 Genomes). Exclude outliers to ensure a genetically homogenous analysis cohort and control for population stratification.
Variant-Level (SNP) QC:
- Missingness: Exclude SNPs with high missingness rates (e.g., > 5%).
- Minor Allele Frequency (MAF): Remove SNPs with a low MAF (e.g., < 1%), as these provide low power for association in most studies.
- Hardy-Weinberg Equilibrium (HWE): Exclude SNPs that significantly deviate from HWE (e.g., p < 1 × 10^-6 in controls), as this can indicate genotyping errors.
Protocol 2: Conducting a Polygenic Risk Score (PRS) Analysis
PRS analysis aggregates the effects of many risk variants to estimate an individual's genetic liability for a trait [39].
- Obtain Discovery GWAS Summary Statistics: Secure the results (effect sizes, alleles, p-values) from a large, independent GWAS on your addiction phenotype of interest (the "base" dataset).
- Clump SNPs: To account for Linkage Disequilibrium (LD), perform clumping on the discovery summary statistics using an LD reference panel. This retains the most significant SNP in each correlated block of the genome.
- Calculate PRS in Target Sample: In your independent "target" sample with genotype data, calculate the score for each individual using the formula:
- ( PRS = \sum{i=1}^{n} (\betai \times G_i) )
- Where ( \betai ) is the effect size of SNP i from the discovery GWAS, and ( Gi ) is the number of effect alleles (0, 1, 2) the individual carries for SNP i. This is performed for a set of SNPs meeting a series of p-value thresholds from the discovery GWAS.
- Evaluate PRS Prediction Power: Test the association between the calculated PRS and the addiction phenotype in the target sample, typically using logistic (for case-control) or linear (for quantitative traits) regression, while including principal components as covariates.
Model and Workflow Visualizations
Diagram 1: The Genetically Informed Neurobiology of Addiction (GINA) Model
Diagram 2: Simplified GWAS and PRS Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Research Reagents and Resources for GWAS and Follow-up Studies
| Item Name | Function/Application | Example/Note |
|---|---|---|
| Genotyping Arrays | Genome-wide profiling of common single nucleotide polymorphisms (SNPs). | Illumina Global Screening Array, PsychArray (optimized for psychiatric traits). |
| Reference Panels | Provide haplotype information for genotype imputation to increase genomic coverage. | 1000 Genomes Project, NHLBI TOPMed [33]. |
| PLINK | Open-source whole-genome association analysis toolset. | Essential for data management, QC, and basic association testing [33] [39]. |
| METAL | Software for meta-analyzing GWAS results from multiple cohorts. | Critical for boosting power by combining studies [33]. |
| PRSice | Tool for calculating and applying polygenic risk scores. | Used to translate GWAS findings into individual-level genetic predictors [39]. |
| GWAS Catalog | Publicly available repository of published GWAS results. | Used for lookup and comparison of identified variants [34]. |
| Functional Mapping Tools | Tools to annotate non-coding GWAS hits and predict their functional consequences. | Used to move from statistical association to biological mechanism (e.g., for eQTL, chromatin interaction analysis) [33] [40]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: In our pharmacological fMRI studies, we often struggle with determining whether a functional signal change truly represents target engagement. What is the best practice? A1: A functional fMRI signal provides indirect evidence of target engagement. Best practice requires establishing a biologically plausible link between the fMRI response and your molecular target. For direct measurement of target engagement, use PET imaging when an appropriate tracer is available. For functional circuits, combine task-based fMRI with pharmacological challenges to demonstrate that your drug modulates the specific brain circuit in a dose-dependent manner [41] [42].
Q2: We are using focused ultrasound for BBB disruption in addiction models. How can we optimize parameters to avoid tissue damage while ensuring sufficient drug delivery? A2: Key parameters to optimize include ultrasound frequency, pressure amplitude, microbubble size, and dose. Use clinically relevant frequencies (0.2-1.5 MHz) and employ a real-time acoustic controller to monitor acoustic emissions and actively adjust pressure amplitude. This ensures consistent BBB disruption without damage. Always confirm opening and closure via contrast-enhanced MRI [43].
Q3: When combining TMS with behavioral pharmacology, how do we determine if TMS is effectively modulating the targeted circuit? A3: Implement a dose-response framework where you establish the behavioral effects of your pharmacological agent first, then assess how TMS shifts this dose-response function. Changes in efficacy, potency, or sensitivity of the drug effect after TMS reveal the importance of the stimulated region in the behavior. Use concurrent fMRI or EEG to verify circuit modulation [44].
Q4: What neuroimaging biomarkers show promise for patient stratification in addiction clinical trials? A4: Several biomarkers are emerging for stratification: Resting-state and task-based fMRI can identify patients with specific reward, stress, or executive function circuit abnormalities. EEG/ERP measures, particularly cognitive potential signals, can stratify patients based on cognitive impairment profiles. Molecular PET imaging may identify patients with specific neurotransmitter system dysregulations [41] [42].
Common Experimental Challenges and Solutions
Table 1: Troubleshooting Common Technical Issues in Non-Invasive Brain Imaging
| Problem | Possible Causes | Solutions |
|---|---|---|
| High variability in fMRI pharmacodynamic signals | Underpowered Phase 1 designs; Inconsistent task performance; Motion artifacts | Increase sample size (≥20 per group); Use robust task paradigms; Implement real-time motion correction; Apply rigorous quality control metrics [41] |
| Inconsistent BBB opening with FUS | Skull variability affecting beam focusing; Suboptimal microbubble administration; Incorrect acoustic parameters | Use MRI-guided targeting; Standardize microbubble preparation and injection; Implement real-time acoustic monitoring with feedback control [43] |
| Poor reproducibility of TMS effects on addiction behaviors | Inaccurate coil placement; Individual differences in brain anatomy; Variable drug levels | Use neuronavigation for precise targeting; Account for individual cortical anatomy; Monitor and control for drug plasma levels [44] |
| Weak translation from preclinical to clinical imaging biomarkers | Species differences in brain networks; Non-homologous behavioral tasks; Different pharmacokinetics | Establish homology in functional measures across species; Use cross-species comparable tasks; Model interspecies differences in drug distribution [42] |
Experimental Protocols for Key Methodologies
Protocol 1: Focused Ultrasound for Blood-Brain Barrier Disruption
Application: Targeted delivery of therapeutic agents to specific brain regions in addiction models.
Materials and Equipment:
- MRI-guided focused ultrasound system with integrated monitoring
- Gas-filled microbubble contrast agent (e.g., Definity)
- 3T MRI scanner with contrast-enhanced imaging capability
- Stereotaxic frame for precise targeting
Procedure:
- Pre-sonication Planning: Acquire high-resolution MR images for target identification (e.g., prefrontal cortex, striatum, extended amygdala).
- Microbubble Administration: Intravenously administer microbubbles at standardized dose (typically 10-20 μL/kg).
- Sonication Parameters: Apply ultrasound at frequency of 0.2-1.5 MHz, peak negative pressure of 0.3-0.6 MPa, pulse length of 10 ms, and repetition frequency of 1-5 Hz.
- Real-time Monitoring: Use acoustic emissions monitoring to provide feedback control of pressure amplitude.
- Confirmation of BBB Opening: Administer MRI contrast agent and perform T1-weighted imaging to verify localized BBB disruption.
- Therapeutic Administration: Immediately administer investigational therapeutic agent.
- Closure Verification: Repeat contrast-enhanced MRI at 6 hours post-sonication to confirm BBB restoration [43].
Safety Considerations:
- Monitor for inertial cavitation which may cause tissue damage
- Confirm BBB closure within 6-24 hours to prevent neurotoxicity
- Perform histological analysis for microhemorrhages in preclinical models
Protocol 2: Pharmaco-fMRI for Target Engagement in Addiction
Application: Assessing functional target engagement of novel therapeutics for substance use disorders.
Materials and Equipment:
- 3T MRI scanner with multiband EPI sequences
- Task paradigms (monetary incentive delay, emotional faces, go/no-go)
- Physiological monitoring equipment (pulse oximetry, respiration)
- Drug infusion apparatus for controlled administration
Procedure:
- Participant Stratification: Pre-screen participants using behavioral and cognitive measures to account for individual differences in addiction endophenotypes.
- Baseline Scanning: Acquire resting-state fMRI (10 min) and task-based fMRI using paradigms relevant to addiction (e.g., cue reactivity, inhibitory control).
- Drug Administration: Administer therapeutic compound using predetermined dosing regimen.
- Peak Effect Scanning: Repeat fMRI protocol during anticipated peak drug concentration.
- Data Analysis: Use generalized psychophysiological interaction (gPPI) to assess drug effects on functional connectivity within addiction-relevant circuits (basal ganglia, extended amygdala, prefrontal cortex).
- Individual Differences Analysis: Correlate drug-induced connectivity changes with baseline characteristics (craving severity, impulsivity, stress reactivity) [41] [42].
Analytical Considerations:
- Control for nonspecific vascular effects using global signal normalization
- Account for individual differences in drug metabolism through pharmacokinetic modeling
- Use robust motion correction algorithms (e.g., FSL FIX or ICA-AROMA)
Protocol 3: Integrated TMS and Behavioral Pharmacology
Application: Investigating neural mechanisms of addiction and testing novel therapeutics.
Materials and Equipment:
- TMS stimulator with figure-8 coil for focal stimulation
- Neuronavigation system for precise targeting
- Behavioral task software (e.g., E-Prime, PsychToolbox)
- Drug administration materials with safety monitoring equipment
Procedure:
- Target Identification: Use individual fMRI data to identify dorsolateral prefrontal cortex (DLPFC) or other target regions based on individual functional connectivity profiles.
- Baseline Behavioral Assessment: Establish dose-response function for abused drug (e.g., THC, nicotine) on relevant outcomes (subjective effects, cognitive performance, craving).
- TMS Parameter Selection: Apply excitatory (e.g., 10 Hz) or inhibitory (e.g., 1 Hz) stimulation protocols based on hypothesized circuit dysfunction.
- Combined Intervention: Administer active TMS to targeted region during peak drug effect.
- Outcome Assessment: Measure shifts in the drug dose-response function following TMS.
- Mechanistic Investigation: Use concurrent EEG or fMRI to assess neural correlates of TMS-drug interactions [44].
Individual Differences Considerations:
- Stratify participants based on addiction severity, comorbidities, and cognitive profiles
- Account for genetic polymorphisms affecting drug metabolism and TMS responsivity
- Consider menstrual cycle phase in female participants when studying hormonal influences
Research Reagent Solutions
Table 2: Essential Research Materials for Non-Invasive Brain Imaging Studies
| Category | Specific Items | Function/Application |
|---|---|---|
| Imaging Contrast Agents | Microbubbles (e.g., Definity) | Enable FUS-mediated BBB disruption through acoustic cavitation [43] |
| Gadolinium-based contrast agents | Validate BBB opening via contrast-enhanced MRI [43] | |
| Radiotracers for PET (e.g., [11C]raclopride) | Measure receptor occupancy and target engagement [41] | |
| Neurostimulation Equipment | TMS figure-8 coils | Provide focal brain stimulation for circuit modulation [44] |
| tDCS electrodes with conductive gel | Apply low-current electrical stimulation for neuromodulation [45] | |
| Neuronavigation systems | Precisely target brain stimulation based on individual anatomy [44] | |
| Pharmacological Tools | Receptor-specific compounds | Establish dose-response relationships and target validation [14] |
| Abuse liability assessment kits | Standardized measures of subjective drug effects [44] | |
| Pharmacokinetic monitoring equipment | Measure drug levels for exposure-response modeling [41] | |
| Computational Resources | Real-time processing software (e.g., improv) | Enable adaptive experimental designs and closed-loop interventions [46] |
| Quality control pipelines (e.g., fMRIPrep) | Ensure data reproducibility and minimize technical variability [42] |
Quantitative Data in Addiction Neuroimaging
Table 3: Key Quantitative Parameters in Non-Invasive Brain Imaging for Addiction Research
| Parameter | Typical Range/Values | Significance in Addiction | Measurement Technique |
|---|---|---|---|
| BBB Opening Volume | 50-200 mm³ | Determines drug delivery extent for targeted therapies [43] | Contrast-enhanced T1 MRI |
| BBB Closure Time | 4-24 hours | Affects therapeutic window and safety profile [43] | Serial contrast-enhanced MRI |
| Dopamine D2/3 Receptor Availability | 10-30% reduction in addiction | Marker of neuroadaptations in reward system [14] | PET with [11C]raclopride |
| Prefrontal Cortex Activity | Variable deactivation during cue exposure | Index of compromised executive control in addiction [14] | Task-based fMRI (BOLD signal) |
| Functional Connectivity (DLPFC-NAcc) | Reduced negative connectivity | Measure of disrupted top-down control [42] | Resting-state fMRI (correlation) |
| Error-Related Negativity (ERN) | Enhanced amplitude in addiction | Indicator of performance monitoring alterations [14] | EEG/ERP during cognitive tasks |
| Target Occupancy for Therapeutics | 30-80% for various targets | Guides dose selection for clinical trials [41] | PET imaging with target-specific tracers |
Methodological Workflows and Signaling Pathways
The Addictions Neuroclinical Assessment (ANA) is a neuroscience-based framework designed to address the profound clinical heterogeneity observed in Alcohol Use Disorder (AUD) and other addictive disorders. Traditional diagnostic systems, like the DSM-5, are based on clinical presentation and symptom counts, failing to capture the varied etiologies, neurobiological substrates, and prognoses among patients who meet criteria for the same disorder [47]. The ANA proposes a paradigm shift by grounding assessment in three core neurofunctional domains that reflect dysfunction in key brain circuits and correspond to the stages of the addiction cycle: Executive Function (EF) , Incentive Salience (IS) , and Negative Emotionality (NE) [47] [48]. Translating this framework from a research concept to a practical "bedside" tool is critical for advancing the study of individual differences and paving the way for personalized treatment in addiction medicine.
FAQ: The Scientist's Guide to the Addictions Neuroclinical Assessment
Q1: What are the three core domains of the ANA and which addiction cycle stages do they map onto? The ANA is built on three domains derived from the neurocircuitry of addiction. The following table outlines their focus and associated phase in the addiction cycle.
Table 1: Core Domains of the Addictions Neuroclinical Assessment
| ANA Domain | Primary Focus | Associated Addiction Cycle Stage |
|---|---|---|
| Executive Function (EF) | Cognitive control, inhibitory control, decision-making, planning [47] [48]. | Preoccupation/Anticipation (Craving) |
| Incentive Salience (IS) | Reward, motivational salience, habit formation [47] [48]. | Binge/Intoxication |
| Negative Emotionality (NE) | Negative affective states, stress, anxiety, dysphoria [49] [47]. | Withdrawal/Negative Affect |
Q2: Why is the ANA considered an improvement over traditional diagnostic criteria for researching individual differences? The DSM-5 and similar criteria classify individuals based on a count of behavioral symptoms. This groups together people who may have arrived at their diagnosis via different paths, obscuring meaningful neurobiological subtypes [47]. The ANA, by contrast, focuses on intermediate phenotypes—measurable neurofunctional domains—that are closer to the underlying biological mechanisms. This allows researchers to stratify study participants not just by diagnosis, but by the specific functional deficits driving their disorder, leading to a more nuanced understanding of individual differences [48].
Q3: What are the most common practical challenges when implementing the ANA battery in a clinical research setting? A primary challenge has been the time burden. The original comprehensive battery was estimated to take up to 10 hours to complete, which is impractical for most clinical and research settings [49]. Subsequent research has focused on developing streamlined batteries that retain scientific rigor while improving feasibility [48]. Other challenges include selecting standardized, reliable measures for each domain and ensuring the battery is sensitive enough to detect change over time, which is crucial for treatment studies [49].
Q4: How can I establish the validity of a streamlined ANA battery in my study? To validate a streamlined battery, researchers should:
- Perform Factor Analysis: Confirm that your selected measures for each domain (EF, IS, NE) load onto the expected latent constructs. Recent studies have shown these domains can be broken down into subfactors (e.g., EF comprises inhibitory control, working memory, and impulsivity) [48].
- Test for Invariance: Establish that your measurement model is equivalent across key groups (e.g., sex, gender) and over time. This ensures that observed differences reflect true differences in the construct and not measurement bias [49].
- Assess Construct Validity: Correlate your ANA domain scores with clinically relevant variables, such as drinking patterns, reasons for drinking, AUD severity, or treatment outcomes [49] [48].
Q5: Why is it critical to consider sex as a biological variable in ANA research? Emerging evidence shows that the neural pathways to addiction risk differ markedly between males and females. A 2025 study found that girls with a family history of substance use disorder showed brain patterns suggesting difficulty disengaging from internal states (e.g., stress), while boys showed patterns linked to heightened environmental reactivity [50]. These differences align with clinical presentations: women more often drink to relieve negative affect, while men more often drink for euphoria [50]. Averaging data across sexes can mask these distinct pathways, so ANA studies should be designed and analyzed with sex as a key variable.
Troubleshooting Common Experimental Issues
Table 2: ANA Implementation Guide: Troubleshooting Common Challenges
| Challenge | Potential Cause | Solution & Best Practices |
|---|---|---|
| High Participant Burden | Overly long assessment battery. | Streamline the protocol. Use abbreviated, validated measures and consider computer-adaptive testing. Break assessments into shorter blocks with mandatory breaks [51] [48]. |
| Data Inconsistency | Variation in administration protocols or participant state (e.g., acute withdrawal). | Standardize protocols. For outpatients, verify a negative breath alcohol concentration (BrAC) and absence of acute intoxication. For inpatients, test after completed detoxification and document absence of withdrawal symptoms [48]. |
| Poor Discrimination of Domains | Measures lack specificity or are influenced by multiple domains. | Conduct a pilot study to confirm the factor structure of your selected measures. Use a combination of neurocognitive tasks and self-report to triangulate constructs [48]. |
| Failure to Detect Change | Insensitive measures or testing at inappropriate timepoints. | Select measures known to be sensitive to change. Align assessment timepoints with theoretically expected periods of change (e.g., pre- and post-targeted intervention). Ensure longitudinal measurement invariance [49]. |
Experimental Protocols: Core Methodologies for ANA Domain Assessment
The following protocols are synthesized from recent studies that have successfully implemented the ANA battery [51] [48].
Protocol 1: General Administration Workflow for a Streamlined ANA Battery
Objective: To reliably assess the three ANA domains (Executive Function, Incentive Salience, Negative Emotionality) in a single session while minimizing participant fatigue. Pre-Session Requirements:
- Obtain informed consent.
- Breath Alcohol Test: Confirm a BrAC of 0.00% for all outpatient participants [51] [48].
- Clinical Assessment (Inpatients): Ensure completion of medical detoxification and confirm the absence of withdrawal symptoms using a standardized scale like the Clinical Institute Withdrawal Assessment (CIWA) [48].
Session Procedure:
- Blocked Administration: Divide the full assessment battery into four distinct testing blocks.
- Randomization: Randomize the order of these four blocks across participants to control for order effects.
- Fixed Internal Order: Within each block, administer behavioral neurocognitive tasks first, followed by self-report questionnaires.
- Mandatory Breaks: Provide a scheduled 15-minute break between each testing block. Allow for additional breaks upon participant request to mitigate fatigue [51] [48].
- Total Time: The entire protocol should be designed to be completed within approximately 6 hours, with the possibility of a second visit if absolutely necessary [51].
Diagram 1: ANA assessment workflow
Protocol 2: Assessing the Negative Emotionality (NE) Domain
Objective: To quantify the latent construct of negative emotionality using a concise set of self-report indicators. Rationale: Negative Emotionality is a key driver of relapse, particularly in individuals who drink to cope. A validated, brief model allows for efficient tracking of this domain [49]. Measures & Indicators:
- Beck Depression Inventory (BDI): Measures severity of depressive symptoms.
- Beck Anxiety Inventory (BAI): Measures severity of anxiety symptoms.
- State-Trait Anger Expression Inventory (STAXI) - Trait Anger Subscale: Measures predisposition to experience anger.
- Drinker Inventory of Consequences (DrInC) - Negative Affect Items: Three specific items assessing negative affective consequences of drinking [49]. Statistical Validation:
- Perform a Confirmatory Factor Analysis (CFA) to test the one-factor model where all indicators load onto a single "Negative Emotionality" latent factor.
- Establish longitudinal and gender invariance if using the measure across time or comparing sexes [49].
Protocol 3: Deconstructing the Executive Function (EF) Domain
Objective: To move beyond a unidimensional EF score and characterize its underlying subfactors. Rationale: EF is not a single entity. A 2024 study identified five subfactors, providing a more granular view of cognitive deficits in AUD [48]. Methodology:
- Administer a comprehensive neurocognitive battery targeting various aspects of executive function.
- Analytic Approach: Use Exploratory Factor Analysis (EFA) on a training dataset (n=150) to identify latent subfactors, followed by Confirmatory Factor Analysis (CFA) on a validation dataset (n=150) to confirm the model. Identified Subfactors [48]:
- Inhibitory Control
- Working Memory
- Rumination
- Interoception
- Impulsivity Correlation Note: The impulsivity subfactor has been shown to have strong cross-correlations with the "Alcohol Motivation" factor of Incentive Salience and the "Internalizing" factor of Negative Emotionality, highlighting the interconnectedness of the ANA domains [48].
Visualization of the ANA Theoretical Framework and Its Assessment
The following diagram illustrates the relationship between the addiction cycle, the corresponding ANA domains, and the practical level of assessment.
Diagram 2: ANA domains mapped to addiction cycle
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for ANA Research
| Tool/Reagent | Function in ANA Research | Specific Example / Note |
|---|---|---|
| Computerized Behavioral Tasks | Objective assessment of neurocognitive constructs like inhibitory control, decision-making, and reward processing. | Available through platforms like Millisecond Test Library. Used to assess EF and IS domains [48]. |
| Standardized Self-Report Scales | Capture subjective experience, affective states, and drinking motives. | Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI) for NE [49]. Alcohol Use Disorders Identification Test (AUDIT) for severity [48]. |
| Structured Clinical Interviews | Establish formal diagnoses and assess comorbidities. | Structured Clinical Interview for DSM-5 (SCID-5) to determine AUD and other DSM diagnoses [48]. |
| Breath Alcohol Analyzer | Ensure participant sobriety at time of testing for data integrity. | Critical for outpatient testing to rule out acute intoxication [51] [48]. |
| Withdrawal Assessment Scale | Quantify withdrawal symptoms in inpatient studies. | Clinical Institute Withdrawal Assessment (CIWA) scale to ensure testing occurs after detoxification [48]. |
| Data Analysis Software | For advanced statistical modeling of ANA domains and subfactors. | Software with Structural Equation Modeling (SEM) capabilities (e.g., R, Mplus) for factor and invariance analysis [49] [48]. |
Resolving Theoretical Disputes and Model Limitations in Addiction Research
Frequently Asked Questions (FAQs)
FAQ 1: How can the brain disease model of addiction (BDA) be deterministic, and why is this a problem for the field? The BDA is considered deterministic because an overly rigid interpretation can suggest that neurobiological changes inevitably lead to compulsive drug use, leaving no room for individual agency, behavior change, or recovery. This perspective fails to account for the well-documented heterogeneity in remission and recovery [52]. A strictly deterministic view can be harmful as it may reduce access to healthcare and treatment by fostering a belief that addiction is unchangeable, which can have catastrophic consequences for patients [52]. A more nuanced contemporary update of the BDA acknowledges the brain as the biological substrate for both addiction and the capacity for behavior change [52].
FAQ 2: If spontaneous remission is common, doesn't that invalidate the idea of addiction as a brain disease? No, the occurrence of spontaneous remission does not invalidate the BDA. The presence of a disease does not preclude the possibility of natural recovery or heterogeneity in outcomes. For example, conditions like hypertension or asthma also have variable courses and can sometimes be managed without formal treatment. The key is that the foundational premise of a neurobiological basis remains sound [52]. The brain possesses a capacity for change (neuroplasticity), and recovery, whether spontaneous or treatment-assisted, is a process that involves the brain re-adapting. Denying the brain disease aspect risks reducing access to treatments that could aid this natural recovery process [52] [53].
FAQ 3: What are the primary neurobiological circuits involved in addiction, and how do they relate to the critique of the BDA? Addiction involves a cycle of three stages that engage distinct but interconnected brain regions, which is crucial for understanding both the compulsive nature of addiction and the potential for recovery [53].
- Binge/Intoxication: This stage heavily involves the basal ganglia, particularly the reward system, which reinforces substance use through dopamine release.
- Withdrawal/Negative Affect: The extended amygdala drives the negative emotional state and stress of withdrawal, motivating continued use to relieve discomfort.
- Preoccupation/Anticipation (Craving): The prefrontal cortex, responsible for executive functions like decision-making and impulse control, is compromised, leading to intense cravings and compulsive drug-seeking [53].
Critics argue that the BDA overemphasizes the compulsive dimension driven by the basal ganglia and extended amygdala, while underplaying the role of the prefrontal cortex and an individual's preserved sensitivity to alternative reinforcements and choices [52].
FAQ 4: How do individual differences, such as biological sex, influence vulnerability to addiction? Individual differences significantly shape addiction risk and trajectory, challenging one-size-fits-all interpretations of the BDA. Research shows that the roots of addiction risk appear early in brain development and differ between sexes.
- Females: Girls with a family history of substance use disorder show higher "transition energy" in the brain's default-mode network, suggesting they may have a harder time disengaging from internal states like stress or rumination. This may lead to using substances as a way to escape [50].
- Males: Boys with a family history show lower transition energy in attention networks, making their brains more reactive to the environment and more drawn to rewarding experiences. This suggests they may find it easier to "step on the gas" regarding risky behaviors [50].
These findings confirm that boys and girls travel different neural roads toward addiction, which must be accounted for in the BDA to adequately explain heterogeneity [50].
Troubleshooting Common Experimental Challenges
Challenge 1: Unaccounted Variables Skewing Behavioral Assay Results Behavioral assays in addiction research can sometimes yield unexpected or inconsistent results due to "hidden variables" that are often overlooked in experimental design and reporting [54].
- Problem: Factors such as circadian cycles, transportation stress, and social housing conditions can dramatically impact physiological and behavioral outcomes relevant to addiction. For instance, the toxicity of amphetamine in male rats is much higher during their inactive (light) phase, and acquisition of learning tasks is faster during this period [54].
- Solution:
- Design: Conduct behavioral testing during the first half of the rodent's active (dark) phase. For dark-phase work, use dim, diffuse red lighting or, ideally, infrared light with cameras to avoid disturbing the animals' circadian rhythms [54].
- Reporting: Accurately report variables like time of testing, housing density, and transportation history in publications [54].
- Acclimation: Allow sufficient time for shipped animals to acclimate to new vivarium conditions before initiating experiments, especially if shipped during sensitive developmental periods like puberty [54].
Challenge 2: Modeling Heterogeneity in Recovery and Relapse A major critique of the BDA is its failure to account for heterogeneity in recovery, yet many animal models do not adequately capture this variability.
- Problem: Experimental designs often focus on group means, potentially masking the individual differences in neural plasticity that underlie spontaneous recovery or varied responses to treatment.
- Solution:
- Individualized Analysis: Move beyond group averages. Analyze data based on sub-populations, such as separating animals that exhibit resilience to relapse from those that are vulnerable, even within the same experimental group.
- Sex as a Biological Variable: Always include and analyze data from both sexes separately, as averaging can mask opposing neural patterns that explain different behavioral pathways [50].
- Longitudinal Studies: Implement study designs that track neural and behavioral changes over time within the same subjects throughout the addiction cycle and into extended abstinence to map the dynamics of recovery.
Table 1: Key Factors Influencing Vulnerability to Addiction
| Factor | Influence on Addiction Risk | Key Findings |
|---|---|---|
| Genetic Vulnerability | Accounts for ~50% of risk [1] | Individuals with a family history of addiction are more likely to develop substance use disorders. Specific genetic markers are under investigation [53]. |
| Early Life Exposure | Increases vulnerability [53] | The younger someone is when they start using a substance, the more likely and quickly they become addicted, as the brain is developing until about age 25 [1]. |
| Mental Health Conditions | Increases vulnerability [53] | Traits like impulsivity and conditions such as ADHD and bipolar disorder are significant risk factors [1]. |
| Environmental Influences | Contributes substantially to risk [53] | Exposure to substance use in one's community, unaddressed trauma, adverse childhood experiences, and high-risk environments increase vulnerability [53]. |
Table 2: Impact of Common "Hidden Variables" on Rodent Models of Addiction
| Hidden Variable | Potential Impact on Experiments | Recommended Mitigation Strategy |
|---|---|---|
| Circadian Phase | Drug toxicity, self-administration, learning, and pain perception are all modulated by time of day [54]. | Schedule testing during the rodent's active (dark) phase and use appropriate lighting (red or infrared) [54]. |
| Transportation Stress | Can cause enduring stress responses, disrupt immune function, and alter behavior, especially if animals are shipped during puberty [54]. | Breed on-site when possible or avoid shipping during sensitive developmental periods. Allow for an acclimation period post-transport [54]. |
| Social Housing | Alters hormone levels, aggressive behaviors, and stress responses, which can confound behavioral results [54]. | Record and report social ranking within cages. House animals according to species-specific needs and avoid testing immediately after cage changes [54]. |
Experimental Protocols & Methodologies
Protocol 1: Assessing Drug Self-Administration with Circadian Control
Objective: To accurately measure voluntary oral consumption of a substance like ethanol in mice, controlling for circadian influences on pharmacokinetics and behavior.
Methodology:
- Animal Housing: House mice on a reversed 12-hour light/12-hour dark cycle (e.g., lights off at 9:00 AM) for at least two weeks prior to experimentation to allow for full acclimation.
- Substance Access: Do not provide the substance ad libitum. Restrict access to the test substance to a defined window (e.g., 2-4 hours) at the beginning of the active dark phase.
- Justification: Ad libitum access leads to consumption spread over 24 hours, resulting in consistently low blood concentrations. Access at the start of the dark phase mimics natural feeding bouts and achieves clinically relevant blood concentrations necessary for modeling addiction [54].
- Testing Conditions: Perform all procedures during the dark phase under dim, diffuse red light or using infrared cameras to minimize disruption.
Protocol 2: Network Control Theory to Probe Individual Neural Vulnerability
Objective: To measure inherent brain flexibility in young individuals (e.g., children or adolescent rodents) before substance use begins, predicting later addiction risk.
Methodology:
- Data Acquisition: Collect resting-state functional MRI (fMRI) data from a large cohort (e.g., the ABCD Study) [50].
- Computational Analysis: Apply network control theory to the fMRI data. This calculates the "transition energy" required for the brain to shift between different intrinsic activity patterns [50].
- Group Stratification: Analyze data based on family history of substance use disorder and, critically, separate by biological sex.
- Interpretation:
- Outcome: This protocol identifies pre-existing neural vulnerabilities, moving beyond a deterministic model to one that explains heterogeneity in risk pathways.
Signaling Pathways & Experimental Workflows
Addiction Cycle Brain Circuits
Individual Vulnerability Research Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Investigating Individual Differences in Addiction Neurobiology
| Item | Function/Benefit in Research |
|---|---|
| Resting-state fMRI | Non-invasive method to measure intrinsic brain activity and functional connectivity in human subjects or animal models. Essential for studies using network control theory [50]. |
| Network Control Theory (Computational Model) | A computational framework applied to fMRI data to quantify the brain's energy requirements for shifting between states. It measures inherent brain flexibility and vulnerability to addiction [50]. |
| Conditioned Place Preference (CPP) | A behavioral assay used in rodent models to measure the rewarding effects of a substance. It can be adapted to test the strength of conditioned responses, a key component of addiction [52]. |
| Oral Self-Administration Paradigms | Allows for voluntary drug intake in rodents. Critical for modeling human consumption patterns, especially when timed to the active dark phase to achieve relevant blood concentrations [54]. |
| N-acetylcysteine | A compound studied for its potential to restore glutamate homeostasis and block drug reinstatement in animal models, representing a class of drugs targeting the neurobiology of craving [55]. |
| GLP-1 Receptor Agonists (e.g., Exenatide) | Medications developed for diabetes that have shown unexpected benefits in reducing alcohol, food, and nicotine use in early trials, highlighting new pathways for treatment [1]. |
What are the core neurobiological stages of addiction, and how do they interact?
Addiction is understood as a chronic, relapsing disorder that progresses through a three-stage cycle, each associated with specific neurobiological adaptations and brain regions. This framework is crucial for understanding the transition from casual use to compulsive behavior [14] [8].
The Three-Stage Addiction Cycle:
- Binge/Intoxication Stage: This initial stage is characterized by the acute rewarding effects of a substance. The primary neurobiological mechanism involves the release of dopamine and endogenous opioids in the ventral striatum and nucleus accumbens, part of the basal ganglia. This produces the subjective feeling of being "high" and reinforces the drug-taking behavior through positive reinforcement [14] [8].
- Withdrawal/Negative Affect Stage: When access to the drug is prevented, a negative emotional state emerges. This stage is driven by two key neuroadaptations: a within-system decrease in dopaminergic tone (leading to reward deficits) and a between-system recruitment of brain stress circuits in the extended amygdala (e.g., involving CRF and dynorphin). This creates a state of irritability, anxiety, and dysphoria, and drug use is continued to achieve negative reinforcement—to relieve this aversive state [14] [8].
- Preoccupation/Anticipation Stage: This stage involves intense craving and preoccupation with the drug during abstinence. It is primarily governed by the prefrontal cortex (PFC), where executive function, including impulse control and emotional regulation, becomes compromised. This "hijacking" of the PFC leads to a loss of control over drug-seeking behavior [14] [8].
These stages form an interactive cycle that intensifies with each repetition, driven by a progressive shift from positive to negative reinforcement and from impulsive to compulsive behavior [14].
Table: Neurobiological Correlates of the Addiction Cycle
| Stage of Cycle | Key Brain Region | Primary Neurotransmitters/Systems | Behavioral Manifestation |
|---|---|---|---|
| Binge/Intoxication | Basal Ganglia (Ventral Striatum, NAcc) | Dopamine, Endogenous Opioids | Pleasure, Reinforcement, Incentive Salience |
| Withdrawal/Negative Affect | Extended Amygdala | CRF, Dynorphin, Norepinephrine; Low Dopamine | Anxiety, Irritability, Dysphoria (Negative Reinforcement) |
| Preoccupation/Anticipation | Prefrontal Cortex | Glutamate, Dysregulated Dopamine | Craving, Loss of Executive Control, Compulsivity |
The following diagram illustrates the cyclical nature of these stages and their key drivers:
How can genetic data be integrated to account for individual differences in addiction risk?
Individual vulnerability to addiction is approximately 50-60% genetic. While traditional genome-wide association studies (GWAS) and polygenic risk scores (PRS) have identified common variants, they assume additive effects and often fail to capture the full complexity, including rare variants and gene-gene interactions [56]. Advanced computational methods are now enabling a more integrated approach.
Methodologies for Integrating Genetic Data:
- Polygenic Risk Scores (PRS): PRS summarize an individual's genetic liability by aggregating the effects of many common variants identified in GWAS. However, their predictive accuracy is currently moderate (e.g., AUC ~0.73 for schizophrenia, ~0.65 for bipolar disorder) and is not yet sufficient for standalone clinical diagnosis [56].
- Machine Learning (ML) and Advanced Integration: ML models (e.g., random forests, gradient boosting) can augment PRS by capturing non-additive genetic interactions (epistasis) and integrating heterogeneous data types. These models do not pre-specify a genetic model but learn the function that maps genotypes to disease status from the data, allowing for more flexible modeling of complex relationships [56].
- Bayesian Data Integration Frameworks: Tools like iGOAT represent a cutting-edge approach. They integrate GWAS data with other genomic information, such as long-range chromatin interactions from multiple brain cell types, to more accurately identify high-risk and low-risk genes for brain disorders. This method has been shown to have higher precision in identifying genes enriched in known brain disorder pathways compared to eQTL or TWAS-based methods [57].
Table: Comparison of Genetic Modeling Approaches for Addiction Risk
| Method | Core Principle | Key Strengths | Key Limitations |
|---|---|---|---|
| GWAS/PRS | Additive effects of common variants | Robust, reproducible, computationally efficient | Misses rare variants and interactions; moderate predictive accuracy |
| Machine Learning (ML) | Learns complex, non-additive functions from data | Can model epistasis; flexible; handles high-dimensional data | Computationally intensive; requires large sample sizes; "black box" |
| Bayesian Integration (e.g., iGOAT) | Integrates multiple genomic data types probabilistically | Higher precision; identifies biological pathways; incorporates epigenomics | Complex implementation; dependent on quality of input data |
The workflow for a multi-modal data integration approach is depicted below:
How do opponent-process and allostasis theories explain the transition to compulsive use?
The transition from recreational, positive-reinforcement-driven drug use to compulsive, negative-reinforcement-driven addiction is a central puzzle. The Opponent-Process Theory and the Allostasis Model provide a neurobiological explanation for this shift.
Experimental Protocol for Theory Validation:
- Paradigm: Repeated administration of a drug of abuse (e.g., cocaine, alcohol, opioids) in animal models (e.g., rodents), with measurement of affective and motivational states.
- Key Measures:
- Intracranial Self-Stimulation (ICSS) Threshold: Measures brain reward function. A elevated ICSS threshold indicates a decreased sensitivity to reward (anhedonia).
- Conditioned Place Aversion/Preference: Assesses the affective state associated with drug withdrawal or context.
- Self-Administration Behavior: Tracks the escalation of drug intake and motivation to work for the drug (e.g., using progressive ratio schedules).
Theoretical Explanation:
- Opponent-Process Theory: This theory posits that the initial pleasurable "a-process" (euphoria) triggered by a drug is automatically opposed by a "b-process" (dysphoria, craving) that restores homeostasis. With repeated drug use, the a-process weakens (tolerance), while the b-process strengthens, accelerates, and lasts longer. Consequently, drug use is increasingly motivated by the need to alleviate the unpleasant b-process (negative reinforcement) rather than to gain pleasure [14] [30].
- Allostasis Model: This model extends the opponent-process theory by proposing that chronic drug use leads to a persistent deviation of the brain's reward and stress systems to a new, pathological set point. It's not just a counter-reaction but a chronic dysregulation. The "allostatic load" results in a persistent reward deficit and a hyperactive brain stress system, which manifests as the negative emotional state of withdrawal and drives compulsive drug-taking to maintain this new, dysfunctional equilibrium [14].
The progression from acute reward to chronic allostatic state is shown in the following diagram:
What key reagents and tools are essential for studying addiction neurobiology?
A modern approach to addiction research requires a toolkit that spans molecular genetics, neuroimaging, and behavioral analysis. The table below details key research reagents and their applications.
Table: Research Reagent Solutions for Addiction Neurobiology
| Reagent/Tool | Primary Function/Utility | Application in Addiction Research |
|---|---|---|
| Polygenic Risk Scores (PRS) | Quantifies aggregate genetic liability from common variants | Stratifying research participants by genetic risk; studying gene-environment interactions [56]. |
| Bayesian Data Integration Tools (e.g., iGOAT) | Identifies disease-associated genes by integrating heterogeneous genomic data. | Pinpointing high-risk genes and uncovering shared genetic architecture between disorders [57]. |
| Dopamine Receptor Ligands | Selective agonists/antagonists for D1-like and D2-like receptors. | Probing the role of specific dopamine pathways in reward, reinforcement, and habit formation [14]. |
| Corticotropin-Releasing Factor (CRF) Antagonists | Block the CRF receptors in the extended amygdala. | Investigating the role of brain stress systems in the withdrawal/negative affect stage and testing potential therapeutics [14] [8]. |
| GLP-1 Receptor Agonists | Diabetes and weight loss medications. | Studying novel mechanisms for reducing alcohol, food, and nicotine use in preclinical and clinical trials [1]. |
| Varenicline / Cytisine | Partial agonists at α4β2 nicotinic acetylcholine receptors. | Reducing withdrawal symptoms and the rewarding properties of nicotine in smoking cessation studies [1]. |
How can we reconcile the brain disease model with behavioral and genetic frameworks?
Reconciling these frameworks requires viewing them not as competitors but as complementary levels of analysis. The core thesis is that genetic and environmental factors shape a vulnerable neurobiological substrate, which, through repeated drug exposure, undergoes allostatic changes that manifest as the maladaptive behaviors defining addiction.
Synthesized Model:
- Genetic Framework Sets the Stage: An individual's genetic makeup (e.g., via PRS, rare variants) confers a baseline level of vulnerability, influencing traits like impulsivity, stress reactivity, and initial reward sensitivity [56] [14].
- Behavioral Framework Drives the Process: The repeated cycle of drug use (behavior) is reinforced through the principles of positive and negative reinforcement. This behavioral engagement is the engine that drives neurobiological change.
- Brain Disease Framework is the Outcome: The relentless cycle of reinforcement and stress leads to the allostatic neuroadaptations in the basal ganglia, extended amygdala, and prefrontal cortex. These changes are the physical instantiation of the "disease"—they underlie the loss of behavioral control, compulsive seeking, and chronic relapse risk [1] [8].
This integrated view posits that behavior is the interface through which genes and environment interact to produce a diseased brain state, which in turn constrains and dictates future behavior. This reconciliation provides a more complete picture for developing personalized interventions, from pharmacological agents targeting specific neuroadaptations to behavioral therapies designed to re-normalize brain function and strengthen cognitive control.
Addiction neurobiology has traditionally focused on the compulsive, reward-driven aspects of substance use, often characterized as a breakdown of self-control mechanisms and the hijacking of the brain's reward system [58] [30]. However, a more nuanced understanding reveals that addiction does not entail a global impairment of reinforcement processing. Preserved sensitivity to alternative reinforcement—the capacity for non-drug rewards and punishments to influence behavior—remains a critical but underexplored facet of addiction [59] [60]. This phenomenon provides a vital key to understanding individual differences in vulnerability and recovery trajectories. This technical support center is designed to help researchers systematically investigate these preserved sensitivities within their experimental paradigms, framing the core issue not as a universal reward deficit, but as a competitive imbalance in behavioral allocation.
Core Theoretical Frameworks and Key Concepts
The following theories provide the foundational models for understanding reinforcement sensitivity in addiction. They are essential for formulating testable hypotheses about preserved sensitivity to alternative reinforcements.
Table 1: Key Neurobiological Theories of Addiction Relevant to Reinforcement Sensitivity
| Theory | Core Postulate | Implication for Alternative Reinforcement |
|---|---|---|
| Opponent-Process Theory [30] | A primary pleasurable drug response (A-process) triggers a countering opponent process (B-process). With repeated use, the B-process strengthens, dominating the affective state. | The aversive B-process can be mitigated by alternative, non-drug rewards, potentially restoring homeostatic balance. |
| Dopaminergic Hypothesis of Addiction [30] | Addictive drugs directly or indirectly increase dopamine in the mesolimbic pathway, the brain's primary reward system. | Alternative reinforcers also engage this system, though typically less intensely, creating a competitive dynamic for dopamine signaling. |
| Revised Reinforcement Sensitivity Theory (r-RST) [59] | Personality is governed by three systems: a Behavioral Approach System (r-BAS), a Behavioral Inhibition System (r-BIS), and a Fight/Flight/Freeze System (FFFS). | Individual variation in r-BAS (reward sensitivity), r-BIS (conflict anxiety), and FFFS (fear) predicts susceptibility to addiction and response to alternative rewards/punishments. |
| I-PACE Model [59] | A framework for addictive disorders positing interactions between Person-Affect-Cognition-Execution. | Specific predispositions (e.g., high r-BAS) interact with affective and cognitive responses to internet/ drug cues, influencing the effectiveness of alternative reinforcers. |
The Revised Reinforcement Sensitivity Theory (r-RST) is particularly instrumental for this research area. It differentiates the neurobiological substrates for responding to diverse stimuli [59]:
- The revised Behavioral Approach System (r-BAS) mediates reactions to conditioned appetitive stimuli and is associated with impulsivity and positive emotional experience.
- The Fight/Flight/Freeze System (FFFS) mediates reactions to all aversive stimuli (unconditioned and conditioned), provoking fear and avoidance.
- The revised Behavioral Inhibition System (r-BIS) is activated by goal-conflict (e.g., approach-avoidance conflict), generating anxiety and risk-assessment behavior.
Individual differences in the baseline sensitivity of these systems can predict how a person will respond to alternative reinforcements, such as monetary rewards or social approval, in the context of addiction [59].
The Scientist's Toolkit: Essential Research Reagents & Materials
To operationalize and investigate these theories, researchers rely on a suite of well-validated paradigms, tools, and measures.
Table 2: Key Research Reagents and Methodologies for Investigating Reinforcement Sensitivity
| Category/Item | Primary Function/Description | Application in Research |
|---|---|---|
| Probabilistic Reinforcement Learning Task [61] | A paradigm where participants learn stimulus-outcome associations that are probabilistic, not certain. | Dissociates learning from reward vs. punishment. Deficits in punishment learning, linked to insula dysfunction, are hallmarks of disorders like Conduct Disorder and may be relevant to addiction [61]. |
| fMRI Neurofeedback Setup [60] | A system providing real-time feedback on brain activity, allowing subjects to learn volitional control of a target region. | Used to test causality; e.g., training deactivation of the subgenual Anterior Cingulate Cortex (sgACC) to probe its role in emotional regulation and reward processing [60]. |
| Functional Localizer (Emotional) [60] | A short fMRI task using blocks of emotionally salient stimuli (e.g., negative pictures) to identify subject-specific emotion-related brain regions. | Defines a Region of Interest (ROI), like the sgACC, for subsequent neurofeedback or analysis tasks [60]. |
| Behavioral Inhibition/Activation Scales (BIS/BAS) [59] | Self-report questionnaires designed to measure the sensitivity of the BIS and BAS systems. | Provides a trait-level measure of reinforcement sensitivity to be used as a predictor variable in longitudinal or cross-sectional studies of addictive behavior [59]. |
| Dopamine Receptor Ligands (e.g., for D1, D2) | Radioactive molecules that bind to specific dopamine receptors for use with PET imaging. | Allows for the quantification of receptor availability in vivo, crucial for testing the Dopaminergic Hypothesis in human subjects [17]. |
Technical Support & Troubleshooting Guides
FAQ: My experimental group shows no behavioral difference in response to alternative rewards. What could be wrong?
Q: I am running a study comparing individuals with a substance use disorder and healthy controls on a task where they can work for monetary reward. I find no group difference in the amount of work expended. What are potential methodological issues?
- A: A null behavioral result can stem from several factors:
- Magnitude of Reinforcement: The alternative reward (e.g., a small monetary amount) may not be salient enough to compete with the anticipated value of the drug. The reward may need to be titrated to be subjectively equal in value [30].
- Probe the Underlying Neurobiology: Use fMRI to measure brain activity during the task. Even in the absence of overt behavioral differences, the ventral striatum may show a blunted response to the alternative reward in the clinical group, indicating a latent neurobiological deficit that the behavior is not capturing [17].
- State of the Subject: Ensure you account for the state of withdrawal or satiety. Sensitivity to alternative reinforcement may be severely dampened during acute withdrawal, as the "Allostasis" theory suggests a shift in reward thresholds [30]. Testing should be done in a controlled state.
- Task Design: The cognitive demands of your task might be confounded with the reinforcement process. A simple, cognitive-undemanding instrumental task is best for isolating motivational components.
FAQ: How do I design a neurofeedback protocol to test volitional control over reward circuits?
Q: I want to use real-time fMRI neurofeedback to train participants to upregulate brain regions involved in processing natural rewards. What are the key design considerations?
- A: The success of a neurofeedback protocol hinges on its design and the feedback provided.
- Feedback Valence Matters: Consider providing both Positive Reinforcement (PR) and Positive Punishment (PP). A study training control of the sgACC found that a group receiving PR+PP (a smiley that could become happy or sad) showed faster initial learning than a group receiving PR only (a smiley that was only neutral or happy) [60].
- Model the Dynamics: Learning is not static. Use modeling approaches (e.g., within-block and across-run trend analyses) to capture the dynamics of the learning process, as initial learning rates and consolidation over time can provide critical insights [60].
- Include Transfer Tests: Always include runs without feedback ("transfer runs") to test if the learned volitional control generalizes, which is the ultimate goal of neurofeedback as an intervention [60].
FAQ: How do I interpret a significant correlation between a dopamine gene and a behavioral trait?
Q: In my genetic study, I found a significant association between a polymorphism in a dopamine receptor gene and self-reported impulsivity. How can I strengthen the inference from this gene to behavior?
- A: The "imaging genetics" approach is designed to address this exact question.
- Find the Neural Intermediate Phenotype: Do not stop at the gene-behavior correlation. Use neuroimaging to identify the neural circuitry that links the two. For example, the same genetic variation might predict blunted reward-related activation in the ventral striatum, which in turn is associated with higher impulsivity [17].
- Convergent Evidence: This creates a more powerful, multi-level model: Gene → Brain Function → Behavior. This approach helps trace the path from basic molecular building blocks to complex behavioral phenotypes, reducing the potential for spurious findings [17].
Visualization of Key Workflows and Pathways
The following diagrams, generated using Graphviz DOT language, illustrate core experimental workflows and neurobiological pathways central to this field of research.
Diagram 1: Imaging Genetics Workflow
Diagram 2: Neurofeedback with Valenced Feedback
Diagram 3: Opponent-Process Theory & Allostasis
Moving beyond the concept of universal compulsion to a model that accounts for preserved sensitivity to alternative reinforcement opens new frontiers in addiction research and therapeutic development [62]. This shift demands rigorous, multi-method approaches that combine computational modeling of behavior, neuroimaging of circuit-level function, and genetic analysis [61] [17]. For professionals in drug development, this framework underscores the importance of targeting neurobiological systems that can enhance the salience and value of non-drug rewards, potentially through medications or neuromodulation techniques that re-calibrate the brain's reward thresholds [63]. The experimental protocols and troubleshooting guides provided here offer a concrete foundation for building a research program capable of dissecting the intricate balance of reinforcement systems that defines the individual experience of addiction.
Scientific Foundation: Individual Differences in Addiction Neurobiology
Addiction is not a uniform disorder; individuals exhibit significant variation in vulnerability, progression, and relapse susceptibility. This heterogeneity stems from a complex interplay of neurobiological, genetic, and environmental factors [64]. Preclinical research has shifted from studying averaged responses to focusing on the mechanisms underlying these individual differences, which is crucial for developing personalized treatment strategies [65] [66].
Key neurobiological theories provide the framework for understanding these differences. The Three-Stage Addiction Cycle (binge/intoxication, withdrawal/negative affect, preoccupation/anticipation) involves distinct neural circuits that are dysregulated to varying degrees across individuals [67] [64]. Furthermore, the Incentive-Sensitization Theory posits that vulnerable individuals experience a greater attribution of "wanting" to drugs and drug-associated cues [68] [65], while the Opponent-Process Theory explains the shift from positive to negative reinforcement driving compulsive use [68]. These varying neuroadaptations underscore why modeling individual differences is paramount.
The following diagram illustrates the core neurocircuitry and stages of addiction, highlighting the systems where individual differences are most pronounced.
Preclinical Models for Studying Individual Differences
Animal models are essential for investigating the neurobiological basis of individual differences in addiction vulnerability. The table below summarizes the primary models used, their core methodologies, and how they capture individual variation.
| Model Name | Core Experimental Methodology | Key Readout Parameters | How Individual Differences Are Captured |
|---|---|---|---|
| 3-Criteria Model [68] [66] | Self-administration with subsequent tests for motivation, persistence, and resistance to punishment. | 1. Motivation (Progressive Ratio)2. Persistence (Drug-seeking during non-availability)3. Resistance to Punishment | Animals are classified as "addiction-vulnerable" if they rank in the top percentile for all three criteria, versus "resilient" for those that do not. |
| Choice Models [68] [66] | A two-choice paradigm where animals select between a drug reward and a natural reward (e.g., sweet solution). | Percentage of choices for the drug over the alternative reward. | A minority of individuals (~10%) maintain a strong preference for the drug, identifying a vulnerable phenotype. |
| Extinction-Reinstatement Model [68] [65] | After self-administration and extinction, drug-seeking is reinstated by cues, stress, or a prime drug dose. | Number of active lever presses during reinstatement. | Individual animals show varying susceptibility to different relapse triggers, modeling heterogeneity in human relapse. |
| High-Responder/Low-Responder Model [65] | Screening based on spontaneous locomotor activity in a novel environment prior to drug exposure. | Locomotor counts; acquisition and escalation of drug self-administration. | Pre-existing neurobiological traits predict subsequent drug-taking behavior, modeling innate vulnerability. |
Model Validation and Workflow
For a model to be considered valid, it is evaluated against three key criteria [68]:
- Face Validity: The similarity of the observed behaviors in the model to the symptoms of the human disease.
- Predictive Validity: The model's ability to correctly predict treatment effects in humans.
- Construct Validity: The similarity between the mechanisms used in the model to induce the disease and the known etiology in humans.
The following diagram outlines a generalized workflow for utilizing these models to screen for and study individual differences in vulnerability.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Primary Function in Research | Key Considerations for Individual Differences Studies |
|---|---|---|
| Validated Antibodies (e.g., for pCREB, ΔFosB) [64] | Detect and quantify neuroplasticity-related protein expression changes in specific brain regions post-mortem. | Use antibodies validated for IHC on the specific tissue type (e.g., frozen vs. FFPE). Always include positive and negative controls from both vulnerable and resilient phenotypes. |
| SignalStain Boost IHC Detection Reagent [69] | Polymer-based detection system for amplifying immunohistochemistry signal, offering superior sensitivity over biotin-based systems. | Crucial for detecting subtle molecular differences between subgroups. Helps minimize background, especially in tissues with endogenous biotin (e.g., liver, kidney). |
| SignalStain Antibody Diluent [69] | Optimized buffer for diluting primary antibodies to preserve antibody stability and specificity during IHC incubations. | Using the recommended diluent is critical for reproducibility. Titration may be required when applying antibodies to different species or fixation conditions. |
| Phospho-Specific Antibodies [69] | Detect activated, phosphorylated forms of signaling proteins (e.g., Phospho-Akt, Phospho-STAT3) to study acute signaling events. | Staining may not be 100% uniform. Requires careful validation of antigen retrieval methods (microwave or pressure cooker preferred over water bath) and the use of appropriate positive control tissues. |
Technical Support Center
Troubleshooting Guides
Issue 1: Failure to Detect Meaningful Individual Variation in a Cohort
| Symptom | Possible Cause | Solution |
|---|---|---|
| All animals exhibit near-identical behavior with low standard deviation. | Insufficient behavioral challenge: The paradigm is not demanding enough to reveal phenotypic extremes. | Increase the behavioral challenge (e.g., use a Progressive Ratio schedule instead of Fixed Ratio, introduce a mild punisher, or offer a high-value alternative reward) [65]. |
| High variability within subjects, but no clear subgroup clustering. | Sample size is too small to reliably detect subpopulations with lower prevalence. | Increase cohort size (N). Perform a power analysis based on pilot data to determine the required N for identifying subgroups that may represent only 10-20% of the population [68]. |
| Inconsistent results upon model replication. | Environmental variables are not controlled: Factors like time of day, handler stress, or housing conditions are masking innate differences. | Strictly standardize all environmental conditions and experimental procedures across all subjects and testing days. |
Issue 2: Poor Predictive Validity for Human Treatment Outcomes
| Symptom | Possible Cause | Solution |
|---|---|---|
| Pharmacotherapies effective in the model consistently fail in clinical trials. | The model lacks construct validity: It may be modeling only one specific behavior (e.g., simple reinforcement) rather than the core compulsivity of addiction [70]. | Employ models that incorporate multiple addiction-like criteria (e.g., 3-criteria model) or compulsion (resistance to punishment) to better reflect the human disorder [68] [66]. |
| Ignoring population heterogeneity: The treatment may only be effective for a specific vulnerability subtype not represented in the model. | Use "reverse translation" [68]: Inform model development with human data. Test candidate therapies in multiple models representing different addiction phenotypes (e.g., stress-sensitive vs. impulse-driven). |
Issue 3: Molecular Analyses Confounded by Tissue Heterogeneity
| Symptom | Possible Cause | Solution |
|---|---|---|
| High background noise in IHC or Western blot data from brain tissue. | Non-specific antibody binding or inadequate blocking. | Use secondary antibodies pre-adsorbed against the species of your sample. Increase blocking time or change blocking reagent (e.g., 10% normal serum for sections) [71]. Always run a no-primary-antibody control. |
| Weak or absent staining in IHC. | Antigen masking from formalin/PFA fixation or antibody is not suitable for IHC [71] [69]. | Optimize antigen retrieval methods (HIER with microwave or pressure cooker is often superior to water bath) [69]. Confirm the antibody is validated for IHC and your specific tissue preparation (paraffin vs. frozen). |
| Inconsistent molecular results between vulnerable and resilient animals. | Sampling of different sub-regions within a brain structure (e.g., core vs. shell of NAc). | Use precise micropunches or laser-capture microdissection to ensure anatomical consistency across all subjects. Reference a detailed brain atlas for all dissections. |
Frequently Asked Questions (FAQs)
Q1: What is the single most important consideration when choosing a model to study individual differences? A: The key is to select a model that does not just produce an average group effect but has been demonstrated to reliably segregate a population into distinct phenotypic subgroups based on predefined, clinically relevant criteria (e.g., compulsion, motivation, choice) [65] [66]. The model should have a demonstrated neural correlate that differentiates these subgroups.
Q2: How can we improve the translation of findings from animal models to human addiction? A: Two strategies are crucial [68] [70]. First, employ cross-species translational measures (e.g., similar cognitive tests, fMRI/neuroimaging correlates) in both preclinical and clinical studies. Second, adopt a "phenotype-first" approach where the goal is not to find a universal cure, but to identify treatments effective for specific, well-defined vulnerability subtypes, which can then be validated in corresponding human subpopulations.
Q3: Our lab is new to this field. Which model should we start with? A: The 3-Criteria Model or a Choice Model are excellent starting points as they have strong face validity and directly operationalize the DSM diagnostic criteria of loss of control, compulsive use, and continued use despite negative consequences [68]. They provide a clear, behavioral basis for subgrouping animals before costly molecular analyses.
Q4: How critical are genetic factors in these models, and how can we control for them? A: Genetic background is a major source of individual differences [64] [66]. Using inbred rodent strains controls for genetic variability, allowing the study of environmental or pharmacological manipulations. Conversely, using outbred strains (like most standard rats) introduces genetic diversity similar to humans, which is essential for identifying genetic and phenotypic vulnerabilities. The choice depends on the specific research question.
Diagnostic Frameworks: DSM-5 and ICD-11
What are the core diagnostic criteria for Substance Use Disorders (SUDs) according to major classification systems?
The diagnosis of Substance Use Disorders is primarily guided by two major systems: the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the International Classification of Diseases, 11th Revision (ICD-11). Both systems recognize SUDs as patterns of substance use that cause significant health impairment, functional disability, or distress [72].
The DSM-5 defines a SUD as a problematic pattern of use leading to clinically significant impairment, manifested by at least two of eleven specified criteria occurring within a 12-month period [72]. These criteria encompass four main categories: impaired control, social impairment, risky use, and pharmacological criteria.
The ICD-11 categorizes disorders due to substance use into three main entities: Episode of Harmful Substance Use, Harmful Pattern of Substance Use, and Substance Dependence [72]. Substance Dependence, which corresponds most closely to the DSM-5's moderate-severe SUD, requires evidence of impaired regulation of substance use manifested by impaired control, increasing priority of substance use over other activities, and physiological features indicative of neuroadaptation.
Table 1: DSM-5 Diagnostic Criteria for Substance Use Disorders
| Criteria Category | Specific Manifestations |
|---|---|
| Impaired Control | Substance taken in larger amounts or over longer period than intended; Persistent desire or unsuccessful efforts to cut down; Great deal of time spent obtaining, using, or recovering; Craving or strong urge to use |
| Social Impairment | Failure to fulfill major role obligations; Continued use despite social/interpersonal problems; Important activities given up or reduced |
| Risky Use | Recurrent use in physically hazardous situations; Continued use despite physical/psychological problems |
| Pharmacological | Tolerance (need for increased amounts or diminished effect); Withdrawal (characteristic syndrome or substance taken to relieve withdrawal) |
Severity in DSM-5 is specified as mild (2-3 symptoms), moderate (4-5 symptoms), or severe (6+ symptoms). The term "addiction" is often used to correspond to moderate or severe SUDs where there is a progressive loss of control over drug-taking despite adverse consequences [72].
Core Neurobiological Mechanisms in Addiction
What are the key neurobiological stages and circuits involved in the transition to addiction?
Contemporary neuroscience research conceptualizes addiction as a chronic brain disorder that progresses through a three-stage cycle: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation [14] [8]. Each stage involves specific brain regions, neurotransmitters, and behavioral manifestations.
The Addiction Cycle: Neurocircuitry and Mechanisms
The transition from recreational drug use to addiction involves progressive changes in multiple brain circuits that mediate reward, motivation, stress response, and executive control [8].
1. Binge/Intoxication Stage This initial stage is characterized by the acute rewarding effects of substances and primarily involves the basal ganglia [8]. All major drugs of abuse increase dopamine release in the ventral striatum (particularly the nucleus accumbens), producing feelings of being "high" [14]. This stage also involves the release of endogenous opioids in the ventral striatum [14]. As addiction progresses, dopamine firing patterns shift from responding to the drug itself to anticipating drug-related cues, a phenomenon known as incentive salience [8]. The neurocircuitry of this stage involves both the mesolimbic pathway (reward and positive reinforcement) and the nigrostriatal pathway (habit formation) [8].
2. Withdrawal/Negative Affect Stage When access to the drug is prevented, a withdrawal syndrome emerges characterized by negative emotional states (irritability, anxiety, dysphoria) [14]. This stage involves the extended amygdala (the bed nucleus of the stria terminalis, central nucleus of the amygdala, and shell of the nucleus accumbens) and represents the brain's "anti-reward" system [8]. Key neuroadaptations include decreased dopaminergic tone in the nucleus accumbens and recruitment of stress circuits involving corticotropin-releasing factor (CRF), dynorphin, norepinephrine, and orexin [8]. This negative emotional state creates powerful negative reinforcement that drives continued drug use to alleviate discomfort.
3. Preoccupation/Anticipation Stage This stage is characterized by cravings and preoccupation with drug seeking, primarily involving the prefrontal cortex (PFC) [8]. Executive control systems in the PFC become dysregulated, leading to diminished impulse control, impaired emotional regulation, and poor decision-making [73]. Researchers have identified two key systems within the PFC: a "Go system" (involving dorsolateral PFC and anterior cingulate for goal-directed behaviors) and a "Stop system" (involving ventromedial and lateral orbital cortex for inhibitory control) [8]. In addiction, this balance is disrupted, with hyperactivity in the Go system and hypoactivity in the Stop system.
Addiction Cycle and Associated Brain Regions
Key Neurotransmitter Systems in Addiction
Multiple neurotransmitter systems interact across the addiction cycle, contributing to the complex phenotype of substance use disorders.
Table 2: Key Neurotransmitter Systems in Addiction Pathology
| Neurotransmitter/System | Primary Role in Addiction | Key Receptors |
|---|---|---|
| Dopamine | Incentive salience, reward prediction, motivation | D1, D2, D3 |
| Opioid | Hedonic value ("liking"), pain regulation, stress | μ-opioid (MOR), δ-opioid (DOR), κ-opioid (KOR) |
| GABA | Inhibition, sedation, anxiety reduction | GABAA, GABAB |
| Glutamate | Excitation, learning, memory, synaptic plasticity | NMDA, AMPA, mGluR |
| CRF | Stress response, negative affect | CRF1, CRF2 |
| Endocannabinoid | Appetite, mood, memory, pain modulation | CB1, CB2 |
| Norepinephrine | Arousal, stress response, attention | α1, α2, β |
Individual Differences in Vulnerability: Technical Guide
What methodological approaches can researchers use to study individual differences in addiction vulnerability?
Individual differences in vulnerability to addiction represent a core challenge in both research and clinical practice. The transition from drug use to addiction depends on a complex interplay of genetic, developmental, environmental, and neurobiological factors [73].
Key Experimental Paradigms for Studying Individual Differences
1. Self-Administration Models Self-administration paradigms in animal models allow researchers to study individual differences in the propensity to self-administer drugs [73]. Key methodologies include:
- Acquisition of drug self-administration under limited access conditions models early stages of drug use [73].
- Progressive ratio schedules measure motivation for drug seeking by requiring increasing effort for each subsequent drug delivery.
- Extended access models (long access or intermittent access) promote escalation of intake and capture transition to compulsive use.
2. Behavioral Trait Assessment Pre-existing behavioral traits can predict addiction vulnerability. Important assessments include:
- Impulsivity measures: Delay discounting tasks, 5-choice serial reaction time task, go/no-go tasks.
- Anxiety-like behaviors: Elevated plus maze, open field test, light-dark box.
- Sensation-seeking/novelty preference: Novelty-induced place preference, novel object recognition.
- Stress sensitivity: Social defeat stress, chronic mild stress paradigms.
3. Neuroimaging Correlates Human neuroimaging studies reveal structural and functional biomarkers of vulnerability:
- Prefrontal cortex function: Individual differences in prefrontal cortex activity and connectivity predict self-regulation capacity and treatment outcomes [73].
- Striatal responsiveness: Differential sensitivity of ventral and dorsal striatum to drug cues and rewards.
- Executive function assessments: Tasks measuring working memory, cognitive flexibility, and inhibitory control.
Factors Contributing to Individual Vulnerability in Addiction
Research Reagent Solutions for Addiction Neuroscience
What are the essential research tools and reagents for investigating addiction neurobiology?
Table 3: Key Research Reagents and Tools for Addiction Neuroscience
| Reagent/Tool | Primary Application | Research Utility |
|---|---|---|
| Selective receptor agonists/antagonists | Pharmacological manipulation of specific neurotransmitter systems | Testing causal roles of receptors in addiction behaviors |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic manipulation of specific neural circuits | Cell-type and circuit-specific modulation without permanent alterations |
| Channelrhodopsins/Archaerhodopsins | Optogenetic control of neuronal activity | Precise temporal control of neural activity in specific pathways |
| CRISPR-Cas9 systems | Gene editing for genetic models | Studying specific gene functions in addiction vulnerability |
| Viral vectors (AAV, lentivirus) | Gene delivery, circuit tracing, manipulation | Anterograde/retrograde tracing, pathway-specific manipulations |
| Radioactive and fluorescent ligands | Receptor autoradiography, in vivo imaging | Quantifying receptor density, distribution, and occupancy |
| Microdialysis probes | In vivo neurochemical monitoring | Measuring neurotransmitter release in behaving animals |
| Fast-scan cyclic voltammetry | Real-time dopamine detection | Monitoring phasic dopamine signals with high temporal resolution |
Technical Troubleshooting Guide: Common Experimental Challenges
How can researchers address common methodological challenges in addiction neuroscience studies?
Problem: High variability in self-administration behavior
Potential Causes: Individual differences in vulnerability, inconsistent training protocols, environmental factors. Solutions:
- Implement pre-screening for behavioral traits (novelty preference, impulsivity)
- Standardize training protocols across experimental batches
- Control for circadian rhythms by conducting experiments at consistent times
- Use within-subject designs when possible to control for individual differences
Problem: Lack of translational validity in animal models
Potential Causes: Overly simplified behavioral paradigms, species differences, inadequate modeling of human addiction criteria. Solutions:
- Incorporate multiple addiction criteria in models (escalation, motivation, persistence despite adverse consequences)
- Use longitudinal designs to model progression
- Include both males and females to study sex differences
- Validate models with pharmacotherapies known to work in humans
Problem: Inconsistent findings in neuroimaging studies
Potential Causes: Small sample sizes, heterogeneous patient populations, different analytical pipelines. Solutions:
- Collaborate for larger sample sizes
- Use standardized preprocessing and analytical pipelines
- Carefully characterize participant subgroups (severity, comorbidities, polysubstance use)
- Control for abstinence duration and withdrawal states
Problem: Difficulty interpreting circuit-specific manipulations
Potential Causes: Off-target effects, compensatory mechanisms, incomplete pathway characterization. Solutions:
- Use combination approaches (e.g., optogenetics with neurochemical measurements)
- Include appropriate controls (empty vector, wild-type viruses)
- Verify manipulation specificity with electrophysiology or fiber photometry
- Use multiple complementary techniques to validate findings
Frequently Asked Questions: Technical Aspects of Addiction Research
Q: How do we operationalize the transition from positive to negative reinforcement in animal models? A: The transition can be modeled by examining escalation of drug intake, development of compulsive use despite adverse consequences, and persistence of drug seeking during periods of anticipated non-availability. Behavioral markers include increased breakpoints on progressive ratio schedules, continued responding when drug is paired with footshock, and heightened motivation during withdrawal states [14].
Q: What are the key considerations when choosing between different self-administration paradigms? A: Selection depends on the research question. Limited access (1-2 hours) is suitable for studying acquisition and early drug use. Extended access (6+ hours) promotes escalation and models transition to addiction. Intermittent access schedules (e.g., 5 minutes on, 25 minutes off) can enhance motivation and may better model binge-like patterns [73].
Q: How can we best model individual differences in vulnerability in laboratory animals? A: Outbred rodent strains naturally exhibit variation in addiction-like behaviors. Pre-screening for traits like novelty reactivity, impulsivity, or stress sensitivity can identify vulnerable subpopulations. Longitudinal studies tracking the same animals across the addiction cycle can reveal predictive biomarkers [73].
Q: What are the current best practices for quantifying compulsion-like behavior in animal models? A: The three key criteria are: (1) persistence of responding when the drug is not available (resistance to extinction), (2) continued drug seeking despite adverse consequences (e.g., footshock-paired delivery), and (3) ability of drug-paired cues to reinstate seeking after extinction. Animals that meet all three criteria are considered to show addiction-like behavior [14].
Q: How has the brain disease model of addiction evolved in response to recent criticisms? A: Contemporary views acknowledge that while addiction has strong neurobiological foundations, this doesn't imply determinism. The current understanding emphasizes that neuroadaptations create vulnerability but don't eliminate capacity for change. Recovery involves harnessing neuroplasticity through pharmacological, behavioral, and social interventions [74]. The field is moving toward multidimensional models that integrate neuroscience with psychology, social context, and individual differences.
Validating Neurobiological Insights Through Comparative Frameworks and Clinical Translation
Drug addiction is a chronically relapsing disorder characterized by compulsion to seek and take the drug, loss of control in limiting intake, and emergence of a negative emotional state when access to the drug is prevented [75] [76]. Understanding the neurobiological mechanisms underlying this disorder has been the focus of extensive research, yielding several prominent theoretical frameworks. The Opponent-Process Theory, Dopamine Hypothesis, and Allostasis Model represent three foundational yet distinct frameworks for explaining the progression from recreational drug use to addiction.
These theories are not mutually exclusive but rather form an evolutionary progression of thought, each adding layers of neurobiological specificity to explain different aspects of the addictive process [30]. For researchers investigating individual differences in addiction vulnerability, recognizing how these theories intersect and diverge provides a critical foundation for designing experiments that account for the complex neuroadaptations occurring across different stages of the addiction cycle.
This technical resource integrates these theoretical perspectives with practical experimental guidance, specifically framed within the context of individual differences in addiction neurobiology research.
Theoretical Foundations and Core Mechanisms
Opponent-Process Theory
Historical Context and Core Principle: Proposed by Solomon and Corbit (1974), this theory posits that hedonic states are automatically opposed by central nervous system mechanisms that reduce the intensity of these states [75] [30]. The theory defines two opposing processes: the a-process (positive hedonic response) occurs shortly after presentation of a stimulus, correlates with intensity and duration of the reinforcer, and shows tolerance; the b-process (opponent response) appears after the a-process terminates, is opposite in direction, sluggish in onset and decay, and intensifies with repeated exposure [76].
Neurobiological Correlates: While the original theory was primarily psychological, contemporary research has identified potential neurobiological substrates. The initial acute drug effect (a-process) is opposed by the b-process as homeostatic changes in brain systems [14]. With repeated drug exposure, the b-process sensitizes, appears earlier, lasts longer, and masks the a-process, leading to apparent tolerance and creating a new motivational state that contributes to dependence [75].
Dopamine Hypothesis
Core Principle: This hypothesis centers on the mesolimbic dopamine system as the primary neural substrate for drug reward and reinforcement [30]. The theory posits that all addictive drugs, when administered acutely, increase dopamine release in the nucleus accumbens, and this neurochemical event is both necessary and sufficient for the reinforcing effects of drugs [75].
Mechanisms of Action: The mesolimbic dopaminergic system consists of dopaminergic cell bodies in the ventral tegmental area (VTA) and their projections to the ventral striatum (particularly the nucleus accumbens) [75]. The hypothesis suggests that dopamine encodes drug reward, attribution of incentive salience, and establishment of response habits [75]. However, more recent refinements indicate dopamine's role may be more related to reward prediction error and incentive salience rather than pleasure per se [14].
Allostasis Model
Core Principle: Allostasis, defined as the process of achieving stability through physiological or behavioral change, provides a framework for understanding the persistent changes in motivation associated with dependence [75] [77]. The model proposes that addiction involves a cycle of increasing dysregulation of brain reward/anti-reward mechanisms that results in a negative emotional state contributing to compulsive drug use [76].
Key Mechanisms: The allostatic model incorporates two types of biological processes: within-system adaptation (opposing, neutralizing reaction within the same system where the drug elicits its primary effects) and between-system adaptation (recruitment of different neurobiological systems from those initially activated) [75] [14]. This model extends opponent-process theory by suggesting that not only does the b-process get larger with chronic drug use, but the reward set point also progressively shifts downward, creating an allostatic state [14].
Comparative Analysis: Theoretical Distinctions and Convergences
Table 1: Core Theoretical Components and Neurobiological Substrates
| Theory Component | Opponent-Process | Dopamine Hypothesis | Allostasis Model |
|---|---|---|---|
| Primary Focus | Temporal dynamics of hedonic processing | Role of dopamine in reward/reinforcement | Chronic deviation of reward set points |
| Key Processes | a-process (primary) vs. b-process (opponent) | Dopamine release in NAc | Within-system & between-system adaptations |
| Neurobiological Substrates | Not specified in original theory | Mesolimbic dopamine pathway (VTA to NAc) | Extended amygdala; dopamine & CRF systems |
| View of Addiction | Strengthened b-process masks a-process | Hijacked reward system | Allostatic load from chronic adaptation |
| Explanatory Scope | Tolerance, withdrawal, craving | Acute reinforcement, incentive salience | Negative reinforcement in dependence |
Table 2: Experimental Evidence and Methodological Approaches
| Experimental Paradigm | Opponent-Process | Dopamine Hypothesis | Allostasis Model |
|---|---|---|---|
| Behavioral Measures | Conditioned place preference/aversion | Drug self-administration | Dependence-induced increased intake |
| Physiological Measures | Withdrawal symptom quantification | Microdialysis for dopamine | Brain stimulation reward thresholds |
| Neurological Measures | Not originally specified | Receptor binding studies | CRF measurements in extended amygdala |
| Key Supporting Evidence | Affective dynamics following stimulus | Dopamine antagonist effects | CRF antagonist effects in dependence |
Critical Theoretical Relationships
The three theories represent an evolutionary progression in addiction neuroscience. The Opponent-Process Theory established the fundamental motivational framework for understanding how counteradaptive processes drive addiction [30]. The Dopamine Hypothesis provided specific neurochemical mechanisms for the initial reinforcing effects of drugs [75]. The Allostasis Model integrates and expands both frameworks by incorporating both dopamine systems (within-system) and stress systems like CRF (between-system) to explain the persistent changes in motivation that characterize addiction [75] [77].
For researchers studying individual differences, these theoretical relationships highlight the importance of measuring neuroadaptations across different neural systems and stages of the addiction cycle. Individual vulnerability may manifest as variations in the intensity or time course of these adaptive processes.
Essential Experimental Protocols for Theory Testing
Protocol 1: Intracranial Self-Stimulation (ICSS) Reward Threshold Measurement
Purpose: To assess brain reward function and track the development of allostatic states in addiction models [75] [76].
Workflow:
- Surgical Preparation: Implant bipolar electrodes targeting the medial forebrain bundle at the level of the lateral hypothalamus in adult rats.
- Training Phase: Train animals to lever-press for varying intensities of brain stimulation using the method of limits.
- Baseline Establishment: Collect stable baseline reward thresholds (minimum current required to support self-stimulation) over 5-7 days.
- Drug Manipulation:
- Acute effects: Measure thresholds minutes after drug administration.
- Chronic effects: Measure thresholds at multiple time points (0.5, 2, 6, 24h) post-drug during repeated administration.
- Data Analysis: Compare reward thresholds across different phases of drug exposure; increased thresholds indicate decreased reward sensitivity.
Troubleshooting:
- Issue: High variability in baseline thresholds.
- Solution: Ensure consistent electrode placement coordinates and verify stable baselines before experimental manipulations.
- Issue: Non-responsive animals.
- Solution: Systematically adjust electrode placement during surgery; aim for coordinates that support rates of responding > 40 presses/min.
Protocol 2: In Vivo Microdialysis for Dopamine Measurement
Purpose: To quantify extracellular dopamine dynamics in specific brain regions during drug administration and withdrawal [75].
Workflow:
- Guide Cannula Implantation: Surgically implant guide cannulae targeting the nucleus accumbens (coordinates: AP +1.7 mm, ML ±1.5 mm, DV -5.0 mm from bregma).
- Probe Preparation: Construct dialysis probes with 2mm active membrane; calibrate in vitro recovery (>15%) prior to experiments.
- Sample Collection: Perfuse with artificial cerebrospinal fluid (1.0 μL/min); collect baseline samples every 10-20 minutes until stable (<10% variation).
- Drug Administration: Administer drug or vehicle after stable baseline establishment; continue sampling for 2-3 hours.
- Sample Analysis: Analyze dialysates using HPLC with electrochemical detection.
- Histological Verification: Verify probe placement after experiment completion.
Troubleshooting:
- Issue: Low dopamine recovery rates.
- Solution: Check membrane integrity, ensure proper flow rates, and verify HPLC detection sensitivity.
- Issue: High baseline variability.
- Solution: Allow sufficient acclimation time (2-3 hours) after probe insertion before baseline collection.
Protocol 3: Dependence-Induced Escalation of Drug Self-Administration
Purpose: To model the transition from controlled to compulsive drug use and measure negative reinforcement mechanisms [76].
Workflow:
- Catheter Implantation: Surgically implant intravenous catheters in jugular or femoral veins; maintain catheter patency with heparinized saline.
- Acquisition Training: Train animals to self-administer drug (e.g., cocaine, heroin) on fixed-ratio schedules during short access (1-2h) sessions.
- Baseline Establishment: Collect stable baselines of drug intake (variation <20% over 3 consecutive sessions).
- Induction of Dependence:
- Intermittent Access Model: Implement long access (6-12h) sessions multiple times per week.
- Chronic Drug Exposure: Administer additional drug injections between self-administration sessions.
- Measurement: Compare pre- and post-dependence drug intake patterns; escalated intake indicates negative reinforcement driving consumption.
Troubleshooting:
- Issue: Loss of catheter patency.
- Solution: Implement strict aseptic techniques; flush catheters daily with heparinized saline containing an antibiotic.
- Issue: Failure to escalate intake.
- Solution: Extend dependence induction period; verify drug concentrations and delivery system.
Signaling Pathways and Neural Circuits: Visual Synthesis
Figure 1: Neural Circuit Relationships Across Addiction Theories
Research Reagent Solutions: Essential Tools for Addiction Neurobiology
Table 3: Key Research Reagents and Their Applications
| Reagent/Category | Specific Examples | Research Application | Theoretical Relevance |
|---|---|---|---|
| Dopamine Receptor Agonists/Antagonists | SCH-23390 (D1 antagonist), Raclopride (D2 antagonist) | Probing dopamine system involvement in drug reward | Dopamine Hypothesis |
| CRF System Modulators | CRF receptor antagonists (e.g., antalarmin), CRF itself | Assessing stress system recruitment in dependence | Allostasis Model |
| Neurochemical Measurement Tools | In vivo microdialysis, Fast-scan cyclic voltammetry | Quantifying neurotransmitter dynamics in real-time | All Theories |
| Genetic Manipulation Tools | CRISPR-Cas9, Cre-Lox system, Viral vectors (AAV) | Investigating specific gene functions in addiction vulnerability | Individual Differences |
| Behavioral Assessment Platforms | Operant conditioning chambers, Place preference apparatus | Measuring reward, reinforcement, and motivational states | All Theories |
| Opto-/Chemogenetics | Channelrhodopsin (ChR2), DREADDs | Circuit-specific manipulation of neural activity | Circuit Mapping |
Frequently Asked Questions: Technical Troubleshooting
Q1: Our ICSS threshold measurements show high variability between animals, complicating interpretation of drug effects. What strategies can improve consistency?
A: Implement these specific protocols: (1) Extended shaping period - Ensure all animals reach stable baselines (<10% variation over 5 consecutive days) before experimental manipulations; (2) Rigorous surgical verification - Use precise stereotaxic coordinates and post-hoc histology to confirm electrode placement in medial forebrain bundle; (3) Standardized testing conditions - Conduct sessions at the same time daily in sound-attenuating chambers to minimize environmental disturbances [75] [76].
Q2: When testing the dopamine hypothesis, why don't dopamine receptor antagonists completely block drug self-administration in all models?
A: This limitation reflects theoretical complexities: (1) Multiple reinforcement mechanisms - While dopamine is crucial for psychostimulants, opioids and other drugs engage additional non-dopaminergic mechanisms in nucleus accumbens and amygdala [14]; (2) Dose-dependent effects - Partial blockade suggests complementary systems; (3) Stage-dependent involvement - Dopamine may be more critical for initial acquisition than maintained administration [14]. We recommend combining dopamine antagonists with manipulations of other systems (e.g., opioid, CRF) for comprehensive assessment.
Q3: How can we effectively model individual differences in addiction vulnerability in laboratory animals?
A: Implement these validated approaches: (1) Behavioral phenotyping - Identify high vs. low responders to novelty, sign-trackers vs. goal-trackers, or animals showing resilience vs. susceptibility to stress; (2) Longitudinal designs - Track the same animals across multiple addiction stages (bingeing, withdrawal, escalation, relapse); (3) Cross-species consistency - Align animal behavioral measures with human endophenotypes (e.g., impulse control, reward learning) [14] [78].
Q4: What are the most reliable measures of the "between-system" adaptations proposed in the allostasis model?
A: Focus on these multimodal assessments: (1) Neuroendocrine measures - Plasma corticosterone and ACTH responses to stress or drug challenge; (2) Central CRF function - Microdialysis measurements of CRF release in extended amygdala during withdrawal; (3) Behavioral indices - Anxiety-like behaviors in elevated plus maze or light-dark transition tests during abstinence; (4) Pharmacological challenges - Effects of CRF antagonists on dependence-induced drug taking [75] [77] [76].
Q5: How do we determine whether observed neuroadaptations represent "within-system" versus "between-system" changes?
A: Apply these operational criteria: Within-system adaptations include: (1) changes in the same neurotransmitter system that mediates initial drug effects (e.g., decreased dopamine D2 receptor sensitivity); (2) neuroadaptations localized to reward regions initially activated by drugs (e.g., VTA, NAc). Between-system adaptations involve: (1) recruitment of different neurotransmitter systems (e.g., CRF, norepinephrine, dynorphin); (2) neuroadaptations in brain regions not primarily involved in acute drug reward (e.g., extended amygdala) [75] [14].
The comparative analysis of these three foundational theories reveals both distinct focal points and important complementarities. The Opponent-Process Theory provides the fundamental motivational framework, the Dopamine Hypothesis identifies specific neurochemical mechanisms for positive reinforcement, and the Allostasis Model integrates both with stress neurocircuitry to explain the negative reinforcement that dominates later addiction stages.
For researchers investigating individual differences in addiction vulnerability, this theoretical integration suggests that individual variation may manifest differently across these mechanisms. Some individuals may show heightened sensitivity to initial drug rewards (Dopamine Hypothesis), others may demonstrate more rapid development of opponent processes, while still others may exhibit heightened between-system recruitment of stress mechanisms (Allostasis Model). The experimental protocols and troubleshooting guides provided here offer practical approaches for dissecting these complex interactions in future research aimed at understanding why only a subset of individuals transition from recreational drug use to addiction.
Troubleshooting Guide: Common Experimental Challenges
1. Issue: High Data Loss in Preclinical MRI Studies Due to Movement
- Problem Identification: Excessive head movement during MRI scans in rodent models, leading to blurred images and unusable data, particularly in longitudinal studies of withdrawal.
- Possible Explanations:
- Stress or anxiety in the animal due to the scanning environment.
- Inadequate acclimation to the scanning apparatus.
- Physiological discomfort or withdrawal symptoms causing increased agitation.
- Data Collection & Solutions:
- Habituation Protocol: Implement a multi-day mock scanner training regimen using a dedicated mock scanner with a head coil and recorded scanner sounds. This desensitizes animals to the scanning environment [79].
- Minimizing Discomfort: Ensure the animal is physiologically stable (e.g., normothermic, proper hydration) before scanning, especially during withdrawal phases. Use comfortable, non-restrictive padding to support the body and head [79].
- Monitoring and Feedback: Utilize a head-tracking device during mock sessions that provides real-time feedback (e.g., an audible tone) when movement is detected, training the animal to remain still [79].
2. Issue: Inconsistent Behavioral Phenotypes in Models of Relapse
- Problem Identification: High variability in cue-induced or stress-induced reinstatement of drug-seeking behavior between subjects, obscuring sex-specific effects.
- Possible Explanations:
- Uncontrolled environmental variables (e.g., light cycle, housing conditions).
- Inadequate characterization of the estrous cycle in female subjects.
- Variations in the potency of cues or stressors.
- Data Collection & Solutions:
- Standardize Environment: Strictly control housing conditions, including light/dark cycles, noise levels, and time of day for behavioral testing [80].
- Stratify by Estrous Phase: For female subjects, track and record the stage of the estrous cycle (e.g., via vaginal cytology) at the time of critical behavioral tests, such as the reinstatement session. Analyze data with estrous cycle as a co-variable to identify cycle-dependent effects on relapse behavior [81].
- Validate Stimuli Potency: Pre-validate all conditioned cues (e.g., tone, light) and stressors (e.g., footshock intensity, predator odor) to ensure they reliably elicit the intended response before use in the main experimental cohort.
3. Issue: Failure to Replicate Findings in Multi-Center Studies
- Problem Identification: A treatment that shows efficacy in a single-laboratory setting fails to confirm results in a larger, multi-center trial, as seen in a recent study on exosome treatment for alcohol relapse [81].
- Possible Explanations:
- Unstandardized protocols across research sites (e.g., differences in animal strain, drug administration paradigms, or outcome measures).
- Underpowered initial studies or inherent biases in single-lab experiments.
- Data Collection & Solutions:
- Pre-Consortium Standardization: Before initiating a multi-center study, collaborating labs should agree upon and publish a detailed common protocol specifying key parameters like species, strain, sex, age, and precise experimental procedures [82].
- Blinded Analysis: Implement fully blinded procedures for drug administration, behavioral scoring, and data analysis to minimize observer bias across all sites [81].
- Data Heterogeneity Analysis: Plan to collect and analyze data on potential sources of variability (e.g., genetic background, environmental factors) that may interact with the treatment effect, especially in relation to sex [82].
Frequently Asked Questions (FAQs)
Q1: Why is it methodologically critical to include both sexes in addiction neurobiology research?
Including both sexes is fundamental because research has consistently demonstrated sex-specific differences in the neurobiology of addiction. These differences impact vulnerability, progression, and treatment outcomes. For instance, a 2025 study found sex-dependent hippocampal atrophy specifically in males with methamphetamine-use experience, highlighting a clear anatomical divergence [81]. Furthermore, transcriptional signatures in the brain during oxycodone withdrawal are sex-specific [81]. Using only one sex provides an incomplete picture and risks developing treatments that are ineffective or lack optimal efficacy for a significant portion of the population.
Q2: What are the key neural circuits involved in addiction, and how do they relate to sex differences?
Addiction is conceptualized as a cycle involving three primary stages, each mediated by distinct but overlapping neural circuits [80]. The integration of sex as a biological variable has revealed that these circuits can be modulated differently in males and females.
Table 1: Key Neural Circuits in the Addiction Cycle
| Addiction Stage | Core Brain Regions | Primary Function | Documented Sex Differences |
|---|---|---|---|
| Binge/Intoxication | Ventral Tegmental Area (VTA), Ventral Striatum (Nucleus Accumbens) | Initial drug reward, reinforcement, and hedonic impact | Females often show enhanced dopamine release and more rapid development of conditioned responses. |
| Withdrawal/Negative Affect | Extended Amygdala (central nucleus), BNST | Negative emotional state (dysphoria, anxiety, irritability) during withdrawal | Withdrawal can be more intense in females, and the underlying neuroadaptations in GABA or CRF systems in the amygdala may be sex-dependent [81] [80]. |
| Preoccupation/Anticipation (Craving) | Prefrontal Cortex (PFC), Orbitofrontal Cortex, Dorsal Striatum, Hippocampus | Craving, executive function deficits, compulsive drug-seeking | The prefrontal cortex's regulation of relapse shows sex-specific neurophysiological adaptations, such as interneuron-specific changes during alcohol withdrawal [81]. |
Q3: How do we account for the estrous cycle in female rodents without making experiments prohibitively complex?
The estrous cycle, particularly fluctuations in hormones like estrogen and progesterone, can significantly influence drug responses. Ignoring it can add noise to your data and mask true effects. A balanced approach is recommended:
- For Initial Discovery Studies: It may be sufficient to record the estrous phase at the time of testing and include it as a covariate in statistical models. This controls for its variance without requiring a priori grouping.
- For Mechanistic Studies: If initial data suggests an effect, design experiments to explicitly test across cycle phases. This can be managed by staging females daily and running balanced cohorts across phases. The insight gained into the hormonal modulation of a drug effect or neural pathway is well worth the added effort.
Q4: What are some best practices for analyzing and reporting sex differences?
- Avoid Solely Reporting "Sex Differences": Move beyond simply stating that males and females are different. The goal is to define the specific mechanisms (e.g., hormonal, genetic, cellular) that underlie the divergence [81].
- Report Statistical Methods Clearly: Always indicate whether data from males and females were analyzed separately, together with sex as a factor, or with interaction effects.
- Deposit Data in Repositories: To contribute to population-level neuroimaging and meta-analyses, share your data with international consortia like ENIGMA, which pools data from tens of thousands of participants to identify robust, small-effect-size factors related to brain structure and function [82].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Item | Function/Application in Addiction Research |
|---|---|
| Cre-lox System | Enables cell-type-specific manipulation (knockout/activation) to define the role of specific neuronal populations (e.g., dopamine sub-circuits) in addiction behaviors [81]. |
| RNA Sequencing | Used for transcriptomic profiling to identify sex-specific gene expression patterns in brain tissue following drug exposure or during withdrawal (e.g., in the suprachiasmatic nucleus) [81]. |
| Fiber Photometry | Allows real-time measurement of neural activity (via calcium or neurotransmitter sensors) in freely behaving animals during specific behaviors, such as drug-seeking or relapse. |
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Permits remote control of specific neural pathways to establish causal links between circuit activity and behavior in a sex-specific manner. |
| GLP-1 Receptor Agonists (e.g., Exendin-4) | Originally developed for diabetes, these drugs are now investigated preclinically and clinically for their unexpected benefit in reducing alcohol, nicotine, and food consumption [1]. |
| Cytisine / Varenicline | Plant-derived and synthetic nicotinic receptor partial agonists, respectively, used as smoking cessation aids and to study the neurobiology of nicotine addiction [1]. |
Experimental Protocol: Validating a Sex-Specific Neural Pathway
This protocol outlines a comprehensive approach to investigate a hypothesized sex-specific pathway from the Prefrontal Cortex (PFC) to the Ventral Tegmental Area (VTA) mediating stress-precipitated relapse.
1. Hypothesis: Stress-induced relapse to opioid seeking is mediated by a distinct, hyperactive PFC→VTA projection in females, but not in males.
2. Subjects: Age-matched adult male and female C57BL/6J mice. Females will be monitored for estrous cycle phase.
3. Materials:
- Oxydocine or morphine for self-administration.
- Stereotaxic surgical apparatus.
- AAV vectors: Cre-dependent Gq-DREADD in PFC neurons projecting to VTA (retrograde Cre from VTA).
- Clozapine-N-oxide (CNO) or equivalent designer drug.
- Conditioned Place Preference (CPP) or operant self-administration chambers.
- Predator odor (e.g., TMT) or mild footshock as a stressor.
4. Methodology:
- Phase 1: Dependence Model & Behavior. Train all subjects to self-administer the drug. Subsequently, subject them to a prolonged abstinence period. After a set period, expose them to a standardized stressor and measure drug-seeking behavior in a reinstatement test. Expected Outcome: Females show a significantly greater stress-induced reinstatement of drug-seeking compared to males.
- Phase 2: Circuit Manipulation. Stereotaxically inject a retrograde Cre virus into the VTA and a Cre-dependent Gq-DREADD virus into the PFC of a new cohort. After recovery and the same abstinence period, administer CNO prior to the stress-induced reinstatement test to artificially activate the specific PFC→VTA pathway. Expected Outcome: Chemogenetic activation of this pathway potentiates relapse in females but has minimal effect in males, validating its functional role in the sex difference.
- Phase 3: Molecular Analysis. In a separate cohort, use RNAscope or similar in-situ hybridization on brain tissue from males and females after the reinstatement test. Probe for markers of immediate-early gene activation (e.g., c-Fos) and key genes of interest (e.g., opioid receptors, CRF) within the PFC and VTA neurons. Expected Outcome: Quantitatively greater co-localization of activation markers in the PFC→VTA pathway of females, providing molecular correlates of the observed behavioral and functional differences.
Signaling Pathways and Experimental Workflows
Technical Support Center: FAQs & Troubleshooting Guides
FAQ: Neuroendocrine-Targeting Pharmacotherapies
Q1: What is the scientific rationale for investigating gut-brain hormones like GLP-1 in substance use disorders?
A1: The investigation is grounded in the understanding that alcohol and other addictive substances share common neurobiological mechanisms with food intake, particularly in reward processing. Gut-brain hormones that regulate feeding and metabolism have been demonstrated to influence the reinforcing properties of both food and addictive substances. Targeting these feeding-related endocrine pathways represents a novel pharmacotherapeutic approach for alcohol and other substance use disorders (ASUDs) [83].
Q2: For which substance use disorders is there the most evidence supporting GLP-1 receptor agonists?
A2: Preclinical and clinical data availability varies by substance. The most extensive evidence exists for alcohol use disorder. Significant preclinical data also supports investigation for psychostimulants, opioids, and nicotine use disorders. Research on cannabis is currently limited to preclinical data [83].
Q3: How do the neurobiological mechanisms of addiction shift from initial use to a chronic disorder?
A3: Addiction progresses through a three-stage cycle: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. This involves a transition from positive reinforcement (seeking the drug's pleasurable effects) to negative reinforcement (seeking relief from a negative emotional state). Neurobiologically, this corresponds to a downregulation of brain reward systems and an upregulation of brain stress systems [14].
Q4: What are the primary barriers to the development of new pharmacotherapies for addiction?
A4: Key barriers include the high prevalence and significant global burden of ASUDs, coupled with a very low proportion of affected individuals receiving pharmacological treatment. The development of new treatments has been slow, with many existing medications dating back decades. Furthermore, there are no FDA-approved medications for stimulant or cannabis use disorders, highlighting a critical treatment gap [83].
Troubleshooting Guide: Experimental Design & Interpretation
Q1: Issue: Inconsistent behavioral responses to GLP-1R agonists in rodent models of alcohol seeking.
- Potential Cause: Individual differences in the baseline sensitivity of stress or reward systems. The relative contribution of the three addiction stages (binge/intoxication, withdrawal/negative affect, preoccupation/anticipation) can vary between subjects [14].
- Solution: Implement stratified group designs based on pre-test biomarkers. For instance, characterize subjects for indicators of anxiety-like behavior or reward sensitivity prior to drug testing. This allows for analysis of treatment efficacy in specific neurobiological subpopulations.
Q2: Issue: Difficulty in modeling the transition from controlled to compulsive drug use in preclinical studies.
- Potential Cause: Standard self-administration protocols may not adequately capture the negative reinforcement that drives addiction in its later stages.
- Solution: Employ progressive ratio schedules or punishment-based paradigms to measure motivation and compulsivity. This aligns with the theoretical framework that addiction involves a shift from impulsive to compulsive behaviors [14]. Ensure that the animal model reflects the "withdrawal/negative affect" stage, where the brain's stress systems (e.g., HPA axis, CRH) are hyperactive [83] [14].
Q3: Issue: Translational failure between robust preclinical data and modest clinical outcomes for a novel neuroendocrine compound.
- Potential Cause: The neuroadaptations in humans are complex and involve between-system changes, recruiting neurobiological systems different from those initially activated by the drug. Preclinical models may not fully capture this allostatic state [14].
- Solution: Prioritize compounds that demonstrate efficacy across multiple animal species and in models that incorporate chronicity and relapse. Furthermore, ensure clinical trial designs account for individual differences in neuropsychological profiles, such as stress reactivity or executive function [14].
Table 1: Summary of Preclinical and Clinical Evidence for Key Neuroendocrine Targets
| Neuroendocrine System | Addictive Substance | Preclinical Data Available | Clinical Data Available | Primary Proposed Mechanism |
|---|---|---|---|---|
| Glucagon-like peptide-1 (GLP-1) | Alcohol | Yes [83] | Yes [83] | Modulates dopamine release in reward regions (e.g., NAcc); reduces incentive salience. |
| Psychostimulants | Yes [83] | Yes [83] | ||
| Opioids | Yes [83] | Yes [83] | ||
| Nicotine | Yes [83] | Yes [83] | ||
| Ghrelin | Alcohol | Yes [83] | Yes [83] | Opposes GLP-1; enhances reward signaling. |
| Psychostimulants | Yes [83] | Yes [83] | ||
| Opioids | Yes [83] | Yes [83] | ||
| Fibroblast growth factor 21 (FGF-21) | Alcohol | Yes [83] | Yes [83] | Reduces alcohol consumption; mechanisms under investigation. |
| Amylin | Alcohol | Yes [83] | No [83] | Modulates mesolimbic dopamine pathways. |
| Stimulant | Yes [83] | Yes [83] | ||
| Glucocorticoid | Alcohol | Yes [83] | Yes [83] | Acts on HPA axis; high levels during stress can trigger relapse. |
| Opioids | Yes [83] | Yes [83] |
Table 2: Approved Pharmacotherapies for Substance Use Disorders (for context)
| Indication | Pharmacotherapy | Primary Mechanism(s) of Action |
|---|---|---|
| Alcohol Use Disorder | Acamprosate | Unclear; may interact with NMDA and GABA receptors [83]. |
| Disulfiram | Inhibition of aldehyde dehydrogenase [83]. | |
| Naltrexone | Antagonism of μ-, κ-, and δ-opioid receptors [83]. | |
| Opioid Use Disorder | Buprenorphine | Partial agonism of μ-opioid receptors [83]. |
| Methadone | Agonism of μ-opioid receptors [83]. | |
| Tobacco Use Disorder | Varenicline | Partial agonism of α4β2 nicotinic acetylcholine receptors [83]. |
| Bupropion | Inhibition of norepinephrine and dopamine reuptake [83]. |
Experimental Protocols for Key Methodologies
Protocol 1: Assessing Drug Seeking in a Rodent Model of Relapse (Reinstatement)
- Objective: To evaluate the efficacy of a novel compound (e.g., a GLP-1RA) in preventing cue- or drug-induced reinstatement of drug-seeking behavior.
- Workflow:
- Training: Subjects self-administer a drug (e.g., alcohol, cocaine) paired with a conditioned cue (e.g., light/tone).
- Extinction: The drug is removed, and lever presses no longer result in drug or cue delivery, leading to a reduction in seeking behavior.
- Reinstatement Test: Following extinction, seeking behavior is reinstated by either:
- A non-contingent presentation of the drug (e.g., a small priming dose).
- Response-contingent presentation of the conditioned cue.
- Exposure to a stressor (e.g., foot shock).
- Drug Testing: The test compound is administered prior to the reinstatement session. A significant reduction in lever presses compared to a vehicle-control group indicates a preventive effect on relapse-like behavior.
- Key Measurements: Number of active vs. inactive lever presses during the reinstatement test session.
Protocol 2: Evaluating Motivation for Drug Taking using a Progressive Ratio Schedule
- Objective: To measure the motivation or willingness to work for a drug reward following treatment with a potential therapeutic.
- Workflow:
- Training: Subjects acquire stable self-administration on a fixed-ratio (FR) schedule (e.g., FR1: one press = one infusion).
- Progressive Ratio (PR): The response requirement to receive a single drug infusion is progressively increased within a session according to a specific formula (e.g., exponential). For example: 1, 2, 4, 6, 9, 12, 15, etc.
- Endpoint: The session continues until the subject fails to meet the response requirement within a predetermined time limit (e.g., 1 hour). The last completed response requirement is recorded as the "break point."
- Drug Testing: The test compound is administered prior to the PR session. A significant reduction in the break point, compared to baseline or vehicle control, indicates a reduction in the drug's motivational value.
- Key Measurements: Final ratio completed (break point), total number of infusions earned.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Neuroendocrine Targets in Addiction
| Reagent / Tool | Function & Application in Addiction Research |
|---|---|
| Exenatide, Liraglutide, Semaglutide | GLP-1 Receptor Agonists (GLP-1RAs). Used to test the hypothesis that activating GLP-1 receptors reduces drug reward, reinforcement, and relapse-like behavior. Newer agents like semaglutide are longer-acting [83]. |
| DPP-4 Inhibitors | Inhibit the dipeptidyl peptidase-4 enzyme, which degrades endogenous GLP-1. Used to investigate whether elevating native GLP-1 levels has therapeutic potential [83]. |
| JNJ-31001074 (or similar) | Selective ghrelin receptor (GHS-R1a) antagonists. Used to study the role of the ghrelin system in promoting drug intake and reward [83]. |
| N-acetylcysteine (NAC) | A compound that normalizes extrasynaptic glutamate levels in the nucleus accumbens. Used in preclinical and clinical studies to reduce cue-induced craving and relapse, particularly for cocaine and nicotine [84]. |
| Mifepristone, Spironolactone | Glucocorticoid and Mineralocorticoid Receptor antagonists, respectively. Used to probe the role of stress hormones and the HPA axis in different stages of addiction, especially stress-induced relapse [83]. |
| Varenicline | A partial agonist at α4β2 nicotinic acetylcholine receptors. An approved smoking cessation aid that is also used as a reference compound in research to study its effects on other substances like alcohol [83]. |
Signaling Pathway: GLP-1 in Addiction Reward Circuitry
FAQ: Technical Challenges in Spontaneous Remission Research
Frequently Asked Questions
Q1: In human studies, how do you objectively define and measure "spontaneous remission" versus untreated recovery? A1: This is a fundamental methodological challenge. In research, "spontaneous remission" is typically identified retrospectively through longitudinal observational studies. It is operationalized as:
- Substance-specific: The absence of a Substance Use Disorder (SUD) diagnosis according to DSM-5 criteria for a sustained period (e.g., 1+ years) despite prior diagnosis [74].
- Treatment-independent: The remission occurs in individuals who have not participated in formal treatment or intervention programs during the recovery period [74] [85].
- Verified: Use of collateral reports or official records (e.g., driving, legal, or employment records) to corroborate self-reported abstinence and functional improvement.
Q2: What are the primary confounding factors when interpreting data on spontaneous remission rates? A2: Key confounders that must be controlled for in analysis include:
- Initial Addiction Severity: Individuals with less severe substance use disorders and fewer co-morbidities are more likely to experience remission [74].
- Environmental Context: Major life changes, such as new relationships, employment, or geographic relocation, can catalyze recovery and must be documented [74] [85].
- Neurobiological Heterogeneity: Individual differences in baseline neural circuitry, genetics, and neuroplasticity potential significantly influence outcomes. Failure to account for this can skew prevalence estimates [74] [86].
Q3: Our preclinical models show strong drug-seeking behavior even after extended abstinence. How does this reconcile with human data on spontaneous remission? A3: This discrepancy highlights a critical limitation of many animal models. Standard models often use continuous access and lack the rich environmental context present in human experience. To better model spontaneous remission, consider:
- Incorporating "Alternative Reinforcers": Implement behavioral paradigms where animals can choose between a drug and a potent natural reward (e.g., social interaction, sucrose). This models the human capacity to find new, rewarding pursuits [74] [87].
- Studying Incubation of Craving: The tendency to relapse can increase over time in animal models, which may model the persistent risk in humans rather than the resolution seen in remission [88].
- Environmental Enrichment: Housing animals in complex environments with toys, social partners, and exercise wheels can induce neuroplasticity that reduces drug-seeking, providing a model for recovery-promoting environments [89] [87].
Q4: Which neuroimaging biomarkers are most sensitive for tracking neuroplastic changes during spontaneous recovery? A4: A multi-modal approach is recommended, as no single biomarker provides a complete picture.
- fMRI (BOLD): Ideal for mapping large-scale network reorganization, such as restored activity in the prefrontal cortex (executive control) and reduced hyperactivity in the amygdala (stress/negative affect) [90] [58].
- PET Imaging: Use radioligands for dopamine D2/D3 receptors to quantify receptor availability in the striatum. Lower D2 receptor levels are associated with addiction, and recovery may involve their upregulation [58].
- Structural MRI: Can detect changes in cortical thickness and gray matter volume in regions like the prefrontal cortex that may occur with sustained abstinence and recovery [90].
Troubleshooting Guide: Experimental Pitfalls in Neuroplasticity Research
Common Issues and Solutions in Experimental Design
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High variability in behavioral reinstatement (relapse) data. | Uncontrolled environmental cues or stress; inconsistent animal handling. | Standardize pre-test conditions: implement a 7-day acclimation period to the testing room, handle all animals daily, and control for circadian rhythms by running experiments at the same time each day. |
| Inability to detect synaptic changes via electrophysiology. | Tissue degradation; failure to record from relevant circuits. | Ensure rapid brain extraction and optimal slicing conditions (correct sucrose-based ACSF for cutting, standard ACSF for recovery). Target specific pathways (e.g., prefrontal cortex to nucleus accumbens) based on your hypothesis. |
| Poor signal-to-noise ratio in fMRI data from recovering subjects. | Motion artifact; inadequate normalization due to structural differences. | Use a rigorous motion-correction protocol and include motion parameters as regressors in analysis. Employ advanced normalization algorithms that account for potential atrophy or structural changes in addicted brains. |
| Transcription factor or protein assays show no change despite behavioral evidence of recovery. | Incorrect timing for tissue collection; analyzing the wrong brain subregion. | Conduct a time-course pilot study to identify the peak expression window for your target molecule. Use precise micropunch dissection or laser-capture microdissection to isolate specific nuclei (e.g., core vs. shell of nucleus accumbens). |
Key Data on Spontaneous Remission and Recovery
Table 1: Quantitative Data on Recovery Trajectories in Substance Use Disorders
| Substance | Approximate Spontaneous Remission Rate (Annual) | Key Predictors of Remission | Common Neuroplasticity Correlates |
|---|---|---|---|
| Alcohol | Not precisely quantified, but significant spontaneous recovery is observed [74]. | Lower severity, strong social support, new negative consequences of use, "maturing out" [74]. | Prefrontal cortex gray matter recovery; restoration of inhibitory control networks [58] [86]. |
| Nicotine | Not precisely quantified in results. | Pregnancy, health diagnosis, cost [74]. | Reversal of nicotine-induced dendritic spine changes in the NAc; normalization of nAChR sensitivity [88] [91]. |
| Cocaine / Stimulants | Not precisely quantified in results. | Development of compelling alternative reinforcers; shift in social network [74] [87]. | Reduction in cue-induced dorsal striatal dopamine release; increased glutamate transporter GLT-1 expression in NAc [88] [58]. |
| Opioids | Not precisely quantified, generally considered low without intervention [74]. | Often associated with structural life changes (e.g., marriage, employment); access to non-drug rewards [74]. | Partial recovery of dopamine D2 receptor availability; functional rewiring of reward and stress circuits [58]. |
Table 2: Experimental Models for Probing Neuroplasticity in Recovery
| Model Type | Core Measurement | Utility for Studying Spontaneous Remission | Key Limitations |
|---|---|---|---|
| Incubation of Craving | Time-dependent increase in drug-seeking after forced abstinence. | Models persistence of craving, a barrier to remission. Allows study of underlying neuroadaptations (e.g., BDNF, mGluR dynamics) [88]. | Does not model the voluntary cessation or environmental context of spontaneous remission. |
| Abstinence / Extinction | Progressive reduction in operant responding when drug is no longer available. | Provides a clean baseline to study neural correlates of extinguished drug-seeking behavior [88]. | Extinction is an active learning process, not merely the absence of drug use, which differs from some remission trajectories. |
| Environmental Enrichment | Reduction in drug self-administration and reinstatement in enriched vs. standard housing. | Directly models how alternative reinforcers and a stimulating environment can compete with and suppress drug-seeking, a key mechanism in spontaneous remission [89] [87]. | Can be difficult to isolate the specific element (social, physical, cognitive) driving the protective effect. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Addiction Neuroplasticity
| Item | Function / Target | Example Application in Research |
|---|---|---|
| N-Acetylcysteine (NAC) | Cystine-glutamate exchanger activator; restores glutamate homeostasis in nucleus accumbens. | Used in reinstatement models to reduce cue-induced drug-seeking for cocaine, nicotine, and gambling [88]. |
| CEFTRI AXONE | Beta-lactam antibiotic that upregulates glutamate transporter GLT-1. | Prevents reinstatement of cocaine-seeking by enhancing glutamate clearance in the synapse, normalizing plasticity [88]. |
| Raclopride ([11C]) | Radioligand for Dopamine D2/D3 receptors for PET imaging. | Used to quantify striatal D2 receptor availability in addicted vs. control and recovered human subjects [58]. |
| BDNF Assays (ELISA/Western) | Quantifies Brain-Derived Neurotrophic Factor, a key mediator of structural plasticity. | Measures BDNF levels in the ventral tegmental area (VTA) and NAc during protracted abstinence, correlating with "incubation of craving" [88]. |
| Viral Vectors (e.g., DREADDs, ChR2) | Chemogenetic or optogenetic control of specific neuronal populations. | Used to causally test the role of specific circuits (e.g., PFC->NAc or VTA->Amygdala) in suppressing or promoting drug-seeking after abstinence [58] [86]. |
Experimental Protocols & Methodologies
Protocol 1: Assessing Glutamate Homeostasis in the Nucleus Accumbens During Recovery
Objective: To measure the restoration of glutamate signaling in the nucleus accumbens (NAc) following voluntary abstinence, as a correlate of spontaneous remission.
Workflow Diagram: Glutamate Homeostasis Assay
Method Steps:
- Animal Model: Use a rodent model of extended access to a drug of abuse (e.g., cocaine) followed by a period of forced or voluntary abstinence.
- Microdialysis & HPLC:
- Implant a guide cannula targeting the NAc core/shell.
- After recovery and abstinence, perfuse the NAc with artificial cerebrospinal fluid (aCSF).
- Collect microdialysate samples at baseline and in response to a drug-associated cue.
- Analyze extracellular glutamate concentration using High-Performance Liquid Chromatography (HPLC).
- Western Blot Analysis:
- After sacrifice, rapidly dissect the NAc.
- Homogenize tissue and quantify protein concentration.
- Probe for levels of the glutamate transporter GLT-1 and the cystine-glutamate antiporter (xCT). Compare to active-use and saline-control groups.
- Slice Electrophysiology:
- Prepare acute brain slices containing the NAc.
- Record from medium spiny neurons. Stimulate cortical afferents and calculate the AMPA/NMDA receptor current ratio, a key indicator of synaptic strength and plasticity.
- Integration: Correlate the molecular (protein levels) and neurochemical (glutamate levels) findings with the electrophysiological readout to build a comprehensive model of glutamate system recovery.
Protocol 2: A Behavioral Paradigm for Modeling Environment-Facilitated Remission
Objective: To test the hypothesis that environmental enrichment can compete with drug reinforcement and induce a remission-like state.
Workflow Diagram: Behavioral Model for Remission
Method Steps:
- Self-Administration Training: Train rats to self-administer intravenous cocaine or heroin on a Fixed-Ratio 1 schedule for 2-3 weeks. Pair a light/tone cue with each infusion.
- Motivation Assessment: Switch to a Progressive Ratio (PR) schedule to establish a baseline measure of motivation (breakpoint).
- Experimental Manipulation: Randomly assign animals to two housing conditions:
- Enriched Environment (EE): Large cages containing running wheels, tunnels, toys, and social partners (changed weekly).
- Standard Environment (SE): Standard laboratory housing.
- Abstinence Period: Remove drug access for an extended period (e.g., 4-6 weeks) while maintaining the housing conditions.
- Reinstatement Test: After abstinence, return animals to the operant chambers.
- Cue-Induced Reinstatement: Expose animals to the drug-paired cue (light/tone) without drug delivery. Measure non-reinforced lever presses.
- Outcome: A significant reduction in lever pressing in the EE group compared to the SE group models an environment-induced suppression of drug-seeking, a key feature of spontaneous remission [87].
Signaling Pathways in Neuroplasticity and Recovery
Diagram: Key Neuroadaptations in Addiction and Recovery The following diagram synthesizes core neuroadaptations from the search results, highlighting the opposing processes in chronic addiction versus recovery/remission.
Frequently Asked Questions (FAQs) for Addiction Neurobiology Research
This technical support center addresses common methodological challenges in research on individual differences in addiction neurobiology. The guidance below is framed within the three-stage addiction cycle (binge/intoxication, withdrawal/negative affect, preoccupation/anticipation) to help you isolate variables and interpret your data [8].
1. What are the primary neural circuits involved in the different stages of addiction, and how can I target them in my experiments?
The addiction cycle is supported by distinct, yet interacting, neural circuits. Understanding these is crucial for designing experiments that probe specific behavioral stages [8].
- Binge/Intoxication Stage: This stage involves the basal ganglia, particularly the mesolimbic dopamine pathway (ventral tegmental area to nucleus accumbens). Dopamine release here reinforces drug-taking behavior [8].
- Withdrawal/Negative Affect Stage: This stage is governed by the extended amygdala (including the bed nucleus of the stria terminalis and central amygdala). Recruitment of stress systems (e.g., CRF, norepinephrine) here leads to negative emotional states [8].
- Preoccupation/Anticipation Stage: This "craving" stage is primarily mediated by the prefrontal cortex. Dysfunction in this area leads to loss of executive control over impulses and compulsive drug-seeking [8].
2. How can I account for individual variability in incentive salience when studying drug-seeking behavior?
Individual differences in incentive salience—where cues associated with drug use become powerful motivators—are a key source of variability. To account for this:
- Behavioral Paradigms: Use well-established tasks like sign-tracking vs. goal-tracking or Pavlovian conditioned approach to classify subjects based on their propensity to attribute incentive salience to drug cues.
- Neurobiological Assays: Correlate behavioral performance with neurobiological measures. For example, subjects with high incentive salience may show stronger dopamine release in the nucleus accumbens upon cue exposure or differences in D1 vs. D2 receptor density in the striatum [8].
- Structured Assessment: Employ frameworks like the Addictions Neuroclinical Assessment (ANA) to translate the neurobiological stages of addiction into measurable neurofunctional domains for your subjects [8].
3. My animal model is not exhibiting expected behavioral phenotypes in the withdrawal/negative affect stage. What should I troubleshoot?
A failure to observe expected negative affect can stem from several methodological issues. Systematically isolate the problem [8] [92].
- Verify Model Induction: Confirm your substance administration protocol (dose, frequency, duration) is sufficient to induce dependence. Check plasma or tissue levels if possible.
- Refine Behavioral Tests: The measures of anxiety (elevated plus maze), anhedonia (sucrose preference), or irritability (e.g., von Frey filament test for mechanical allodynia in opioid withdrawal) must be sensitive and appropriate for your species/strain.
- Control for Environment: Ensure testing is conducted in a environment free of confounding stressors and that the experimenters are blinded to the subject groups.
- Physiological Measures: Supplement behavioral observations with physiological measures of stress, such as corticosterone/cortisol levels or heart rate variability, to objectively quantify the withdrawal state [8].
4. What are the best practices for integrating social stress paradigms into models of addiction relapse?
Social stress is a powerful predictor of relapse. To integrate it effectively:
- Choose a Validated Paradigm: Use established protocols like social defeat stress, chronic subordinate colony housing, or witness stress, depending on your species and research question.
- Time the Stressor: The impact of social stress may differ if applied before drug acquisition (vulnerability), during abstinence (provocation of relapse), or during development (epigenetic priming).
- Measure Neurobiological Endpoints: Focus on mechanisms within the addiction cycle. Social stress amplifies the "anti-reward" system in the extended amygdala (e.g., CRF, dynorphin) and impairs prefrontal cortex function, thereby increasing craving and reducing behavioral control [8] [93]. Measure these systems in your subjects.
5. How do I evaluate the strength of evidence for a new pharmacological treatment targeting a specific neurobiological stage?
Adopt a hierarchical framework to evaluate evidence, similar to models used in evidence-based medicine and drug development [94].
- Systematic Reviews/Meta-Analyses: Look for systematic reviews of existing randomized controlled trials (RCTs).
- Single RCTs: Evaluate the quality of individual RCTs, including blinding, randomization, and control groups.
- Observational Studies: Consider systematic reviews or single observational studies that address patient-important outcomes in real-world settings.
- Physiological Studies: Early-phase evidence often comes from physiological studies in controlled lab settings.
The table below summarizes the key criteria from different evaluation frameworks.
| Framework | Highest Level of Evidence | Key Criteria |
|---|---|---|
| Evidence-Based Medicine [94] | N-of-1 Randomized Trial | Direct, within-subject experimental evidence. |
| APA Division 12 [94] | Empirically Validated Treatment | Efficacy in two+ independent RCTs or single-case experiments. |
| FDA Phase Model [94] | Phase 3: Effectiveness RCT | Testing in routine conditions with typical patients and broad outcomes. |
Visualizing the Neurobiological Workflow
The following diagrams map the core concepts and experimental workflows in addiction neurobiology research.
Addiction Cycle Neurocircuitry
Experimental Troubleshooting Workflow
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and their applications for investigating individual differences in addiction neurobiology.
| Research Reagent / Tool | Primary Function | Application Context |
|---|---|---|
| Dopamine Receptor Agonists/Antagonists (e.g., SCH-23390, Raclopride) | Selectively activate or block D1-like or D2-like dopamine receptors. | Probing the role of specific dopamine pathways in the binge/intoxication stage and in incentive salience [8]. |
| CRF Receptor Antagonists | Block the corticotropin-releasing factor (CRF) receptors. | Testing the role of stress systems in the withdrawal/negative affect stage and in stress-induced relapse [8]. |
| Viral Vector Tools (e.g., DREADDs, Chemogenetics) | Allow precise, reversible control of specific neuronal populations. | Mapping and manipulating circuits (e.g., PFC to NAcc) to establish causality in behavior during the preoccupation/anticipation stage [8]. |
| Positron Emission Tomography (PET) Ligands for Dopamine Receptors | Quantify receptor availability and dopamine release in the living brain. | Correlating individual differences in D2/D3 receptor density in the striatum with vulnerability to addiction and treatment response [8]. |
| Social Stress Paradigms (e.g., Social Defeat) | Model the impact of social adversity on behavior and neurobiology. | Investigating how sociocultural factors (e.g., stress, isolation) interact with individual neurobiology to drive addiction cycles and relapse [93]. |
Conclusion
The investigation of individual differences in addiction neurobiology reveals that vulnerability and recovery are not monolithic but are shaped by a complex interplay of genetic predisposition, early brain development, sex-specific pathways, and environmental influences. A conclusive synthesis of the evidence necessitates moving beyond contentious debates between brain disease, behavioral, and genetic models toward an integrated, consilience framework. Future directions for biomedical research must prioritize the development of personalized intervention strategies that account for these individual differences. This includes tailoring prevention programs based on early neural risk markers, designing sex-specific treatments, and leveraging novel pharmacological targets informed by a deeper understanding of individual neurogenetic profiles. Ultimately, acknowledging and systematically studying this heterogeneity is the key to developing more effective, precise, and compassionate treatments for substance use disorders.
References
- 1. Why our brains are wired for addiction: What the science says [https://med.stanford.edu/news/insights/2025/08/addiction-science-human-brain-ancient-wiring.html]
- 2. Genes and (Common) Pathways Underlying Drug Addiction [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.0040002]
- 3. The genetic landscape of substance use disorders [https://www.nature.com/articles/s41380-024-02547-z]
- 4. Differences and similarities between the genetic ... [https://resolve.cambridge.org/core/journals/psychological-medicine/article/differences-and-similarities-between-the-genetic-architecture-of-lifetime-substance-use-across-different-substances/57ED52E17CCBB493E2EECD6B40F2E7B9]
- 5. Shared Genetic Architecture and Neurobiological ... [https://www.medrxiv.org/content/10.1101/2025.11.24.25339061v1.full-text]
- 6. Activity Early Predict Addiction Risk in Brain vs Differences Boys Girls [https://neurosciencenews.com/neurodevelopment-addiction-sex-differences-29965/]
- 7. , Boys may be predisposed to substance use... - The Hindu girls [https://www.thehindu.com/sci-tech/health/boys-girls-may-be-predisposed-to-substance-use-addiction-in-differing-ways-brain-scans-reveal/article70317486.ece]
- 8. Neurobiology of Addiction - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK597351/]
- 9. THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ... [https://www.ncbi.nlm.nih.gov/books/NBK424849/]
- 10. The Influence of Substance Use on Adolescent Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2827693/]
- 11. Adolescent Substance Use and the Brain: Behavioral ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2020.00298/full]
- 12. Individual differences in prefrontal cortex function and the ... [https://www.sciencedirect.com/science/article/pii/S0149763410000965]
- 13. Adolescent substance use initiation and long-term ... [https://www.nature.com/articles/s41380-024-02471-2]
- 14. Individual differences in the neuropsychopathology of addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741105/]
- 15. The Adolescent Brain and Substance Use - NIDA - NIH [https://nida.nih.gov/research-topics/adolescent-brain-substance-use]
- 16. Consequences of adolescent drug use [https://www.nature.com/articles/s41398-023-02590-4]
- 17. Imaging genetics and the neurobiological basis of ... [https://www.sciencedirect.com/science/article/pii/S0376871612000348]
- 18. A deep TMS/fMRI trial in people with alcohol use disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273219/]
- 19. The neurobiology of impulsivity and substance use disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC6450787/]
- 20. Neurophysiological correlates of trait and behavioral ... [https://www.sciencedirect.com/science/article/pii/S2405844024162433]
- 21. The detrimental effects of emotional process dysregulation ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2012.00101/full]
- 22. Drug addiction (substance use disorder) - Diagnosis and ... [https://www.mayoclinic.org/diseases-conditions/drug-addiction/diagnosis-treatment/drc-20365113]
- 23. A network control theory pipeline for studying the dynamics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12039364/]
- 24. Inferring intrinsic neural timescales using optimal control ... [https://www.nature.com/articles/s41467-025-66542-w]
- 25. Editorial: Individual differences in addictive behaviors [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2024.1386489/full]
- 26. Adolescent Brain Cognitive Development Study (ABCD Study®) [https://nida.nih.gov/research-topics/adolescent-brain/longitudinal-study-adolescent-brain-cognitive-development-abcd-study]
- 27. The ABCD study: understanding the development of risk for ... [https://www.nature.com/articles/s41386-020-0736-6]
- 28. FAQs [https://docs.abcdstudy.org/latest/info/faq.html]
- 29. Frequently Asked Questions - ABCD Study [https://www.addictionresearch.nih.gov/frequently-asked-questions-abcd-study]
- 30. Neurobiological Theories of Addiction: A Comprehensive ... [https://www.mdpi.com/2813-1851/3/1/3]
- 31. Individual differences underlying susceptibility to addiction [https://www.sciencedirect.com/science/article/pii/S0091305713002219]
- 32. Machine Learning of Functional Magnetic Resonance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5851466/]
- 33. Genome-wide association studies [https://www.nature.com/articles/s43586-021-00056-9]
- 34. Genome-Wide Association Studies (GWAS) [https://www.genome.gov/genetics-glossary/Genome-Wide-Association-Studies-GWAS]
- 35. The genetically informed neurobiology of addiction (GINA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10041646/]
- 36. Meta-analysis and genome-wide interpretation of genetic ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/1471-2164-12-508]
- 37. The Genetically Informed Neurobiology of Addiction (GINA ... [https://pubmed.ncbi.nlm.nih.gov/36446900/]
- 38. The Genetically Informed Neurobiology of Addiction ( GINA ) model [https://www.nature.com/articles/s41583-022-00656-8?error=cookies_not_supported&code=a31d71cb-07a7-4902-a3a3-316b256c66eb]
- 39. A tutorial on conducting genome‐wide association studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC6001694/]
- 40. BEYOND GWAS: THE GENETICS AND EPIGENETICS OF ... [https://www.sciencedirect.com/science/article/pii/S0376871623010244]
- 41. Opportunities for use of neuroimaging in de-risking drug ... [https://www.nature.com/articles/s41386-024-01970-8]
- 42. The role of fMRI in drug development - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931333/]
- 43. Noninvasive and Targeted Drug Delivery to the Brain Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3629738/]
- 44. Combining noninvasive brain stimulation with behavioral ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1150109/full]
- 45. Non-Invasive Brain Stimulation in Drug Addiction [https://www.frontiersin.org/research-topics/6524/non-invasive-brain-stimulation-in-drug-addiction/magazine]
- 46. A software platform for real-time and adaptive ... [https://www.nature.com/articles/s41467-025-64856-3]
- 47. Addictions Neuroclinical Assessment: A Neuroscience- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4870153/]
- 48. Factors underlying the neurofunctional domains of ... [https://www.nature.com/articles/s41398-024-02987-9]
- 49. The Addictions Neuroclinical Assessment Negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7069798/]
- 50. Early Brain Differences May Explain Sex-Specific Risks for ... [https://news.weill.cornell.edu/news/2025/11/early-brain-differences-may-explain-sex-specific-risks-for-addiction]
- 51. Protocol Details [https://clinicalstudies.info.nih.gov/protocoldetails.aspx?id=000406-AA&&query=]
- 52. Addiction as a brain disease revised: why it still matters, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8357831/]
- 53. The Disease Model of Addiction [https://sambarecovery.com/rehab-blog/the-disease-model-of-addiction/]
- 54. What's wrong with my experiment?: The impact of hidden ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9117327/]
- 55. Similarities and Differences in Neurobiology [https://pubmed.ncbi.nlm.nih.gov/41171560/]
- 56. unravelling brain disorders through data integration and ... [https://www.nature.com/articles/s41380-025-03330-4]
- 57. Accurate identification of genes associated with brain ... [https://pubmed.ncbi.nlm.nih.gov/39168091/]
- 58. The neurobiology of addiction - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6767400/]
- 59. The longitudinal impact of reinforcement sensitivity on ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2023.1298380/full]
- 60. Reinforcement and Punishment Shape the Learning ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2020.00304/full]
- 61. Altered Neural Responses to Punishment Learning in ... [https://www.sciencedirect.com/science/article/pii/S2451902225000254]
- 62. Beyond simple dichotomies in reinforcement learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7800310/]
- 63. Drug Discovery and Development: Overview of the End-to- ... [https://learn.hms.harvard.edu/programs/drug-discovery-and-development-overview-end-end-therapeutic-development-pipeline]
- 64. Conflicting theories on addiction aetiology and the ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2023.1166852/full]
- 65. Frontiers | Understanding Addiction Using Animal Models [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2019.00262/full]
- 66. Addiction: A preclinical and clinical analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5676458/]
- 67. of Neurobiology : a neurocircuitry analysis - PMC addiction [https://pmc.ncbi.nlm.nih.gov/articles/PMC6135092/]
- 68. From concepts to treatment: a dialog between a preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9492712/]
- 69. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopkaB6cCs1toQPjP0H5817BGfCH-Au8-btQJGEDoXXWlRX09nOa]
- 70. Removing Obstacles in Neuroscience Drug Discovery [https://www.nature.com/articles/npp2008173]
- 71. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopMbKvHgbbIZ2UK3uHKxJkAQ6RD2x4a3m1QEu7cIHN7hO6t-Rdx]
- 72. Substance use disorders - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10168177/]
- 73. Individual differences in prefrontal cortex function and the ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763410000965]
- 74. Addiction as a brain disease revised: why it still matters, ... [https://www.nature.com/articles/s41386-020-00950-y]
- 75. Allostasis and Addiction: Role of the Dopamine and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3288230/]
- 76. Neurobiological mechanisms for opponent motivational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2607326/]
- 77. Allostasis and addiction: Role of the dopamine and ... [https://www.sciencedirect.com/science/article/abs/pii/S0031938411005233]
- 78. Motivated Behaviors and Addiction [https://neurobiology.umaryland.edu/our-research/motivated-behaviors-and-addiction/]
- 79. Neuroimaging in Child Clinical Populations [https://pmc.ncbi.nlm.nih.gov/articles/PMC3652337/]
- 80. Neurocircuitry of Addiction | Neuropsychopharmacology [https://www.nature.com/articles/npp2009110]
- 81. Addiction Neuroscience | Vol 17, In progress (December ... [https://www.sciencedirect.com/journal/addiction-neuroscience/vol/17/suppl/C]
- 82. Neuroimaging in population - GIN-IMN [https://www.gin.cnrs.fr/en/current-research/axis1/]
- 83. Neuroendocrinology meets addiction - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522537/]
- 84. Neuroscience and Understanding Addiction [https://attcnetwork.org/neuroscience-and-understanding-addiction/]
- 85. Spontaneous Remission - Jackson House [https://www.jacksonhousecares.com/blog/posts/2023/october/spontaneous-remission/]
- 86. Neuroplasticity and Nervous System Recovery: Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025631/]
- 87. Natural rewards, neuroplasticity, and non-drug addictions [https://www.sciencedirect.com/science/article/abs/pii/S0028390811001195]
- 88. Neuroplasticity in addictive disorders - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181920/]
- 89. Mechanisms of neural plasticity following brain injury [https://www.sciencedirect.com/science/article/abs/pii/S0959438806000626]
- 90. Spontaneous & Therapeutic-Induced Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5079852/]
- 91. The Link Between Neuroplasticity and Addiction [https://neurowellnessspa.com/the-link-between-neuroplasticity-and-addiction/]
- 92. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 93. SOCIAL NEUROSCIENCE AND ITS RELATIONSHIP TO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3883133/]
- 94. Evidence-based practices for substance use disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC3678283/]