In Vivo Techniques in Neuroscience: A Comprehensive Guide for Research and Drug Development
This article provides a comprehensive overview of current in vivo techniques for neuroscience research, tailored for researchers, scientists, and drug development professionals.
In Vivo Techniques in Neuroscience: A Comprehensive Guide for Research and Drug Development
Abstract
This article provides a comprehensive overview of current in vivo techniques for neuroscience research, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of methods like optical imaging and in vivo SELEX, details their practical applications in disease modeling and therapeutic discovery, addresses key troubleshooting and optimization challenges in translational settings, and offers a critical comparative analysis with in vitro and ex vivo approaches. The synthesis aims to bridge the gap between basic research and clinical application, empowering scientists to select appropriate methodologies and advance the development of novel therapeutics for neurological disorders.
Core Principles and the Power of In Vivo Brain Mapping
In vivo research, defined as investigations conducted within a living organism, is a cornerstone of biological and medical science. The term itself, derived from Latin meaning "within the living," encompasses studies performed in complex, integrated systems where all physiological processes remain intact [1]. This approach stands in contrast to in vitro ("in glass") methods, which are conducted in artificial environments outside of living organisms, such as petri dishes or test tubes [1].
The fundamental value of in vivo research lies in its capacity to reveal the true physiological behavior of biological systems, accounting for the intricate interplay between organs, tissues, cells, and molecular pathways that cannot be fully replicated in simplified in vitro settings [1] [2]. This is particularly critical in neuroscience research, where the complexity of the central nervous system, with its networked electrical signaling, blood-brain barrier dynamics, and multifaceted cellular interactions, demands investigation in intact organisms to generate clinically relevant insights [2]. In vivo models provide indispensable platforms for investigating pathophysiological mechanisms underlying neurological disorders and for conducting preclinical translational studies that may include the assessment of new treatments [1] [2].
Fundamental Principles and Physiological Relevance
Core Characteristics of In Vivo Systems
In vivo research operates on the principle that biological systems function as integrated wholes rather than as isolated components. This holistic approach captures the essential complexity of living organisms through several defining characteristics:
- Whole-organism complexity: Investigations account for systemic interactions between multiple organ systems, hormonal regulation, metabolic integration, and neural networking that collectively influence experimental outcomes [1].
- Intact physiological environment: Studies maintain natural barriers (e.g., blood-brain barrier), vascular perfusion, immune responses, and homeostatic mechanisms that significantly influence biological responses [2].
- Functional readouts: Researchers can measure complex behavioral, cognitive, and physiological endpoints that reflect integrated system function rather than isolated cellular responses [2].
Comparative Advantages and Limitations
The following table summarizes the key distinctions between in vivo research and alternative methodological approaches:
Table 1: Comparison of Research Methodological Approaches
| Parameter | In Vivo | In Vitro | In Silico |
|---|---|---|---|
| System Complexity | Whole living organism with intact physiology | Isolated cells, tissues, or organs in artificial environment | Computational models and simulations |
| Physiological Relevance | High - includes systemic interactions | Limited - lacks systemic context | Variable - depends on model accuracy |
| Throughput | Lower throughput, time-intensive | Higher throughput, rapid results | Highest throughput, instantaneous |
| Cost Implications | High (animal care, ethical oversight) | Moderate (reagents, cell culture) | Low (computational resources) |
| Regulatory Pathway | Required for preclinical drug development | Early screening and mechanism studies | Predictive modeling and hypothesis generation |
| Species Differences | Potential for cross-species translation bias | Human cells possible but lack systemic context | Species-specific parameters can be implemented |
While in vivo approaches offer unparalleled physiological relevance, researchers must acknowledge several methodological considerations. The selection of appropriate animal models is critical, as species with varying genetic backgrounds, environmental adaptations, and pathway differences can bias preclinical interpretations [1]. Additionally, the resource-intensive nature of in vivo studies, including costs, time investment, and ethical considerations, necessitates careful experimental design to maximize information yield while minimizing animal usage [3].
In Vivo Methodologies in Neuroscience Research
Advanced Neuroimaging and Modulation Techniques
Contemporary neuroscience employs sophisticated technologies for observing and manipulating neural activity in living organisms:
Optogenetics: This neurostimulation technique uses low-intensity light with different waveforms to produce or modulate electrophysiological responses in genetically modified neurons, opening promising revolutionary applications in neurological therapeutics in in vivo preclinical studies [2]. The approach involves viral vector-mediated expression of light-sensitive proteins (opsins) such as channelrhodopsin-2 (ChR2) in specific neuronal populations, enabling precise temporal control of neural activity with millisecond precision [2].
Chemogenetics: This forefront technique frequently uses the in vivo injection of a viral vector to induce the expression of genetically modified G-protein coupled receptors (GPCR), which are inert for endogenous ligands but specifically activated by "designer drugs" [2]. These expressed receptors are termed DREADDs (Designer Receptors Exclusively Activated by Designer Drugs), enabling remote control of neural activity without implanted hardware [2].
Two-photon laser scanning microscopy: This imaging method enables deep tissue imaging in living animals, allowing researchers to observe dynamic processes such as the emergence and disappearance of dendritic spines in adult mice and dynamic changes in dendrites and axons during development [2]. When combined with fluorescent calcium indicators, this technique permits functional imaging of neural activity in intact circuits [2].
Magnetic resonance imaging (MRI): This non-invasive multiplanar imaging technique helps investigate biological functions with both functional and structural images showing both activity and anatomy [2]. Recent development of MRI machines for laboratory animals has accelerated its use in in vivo preclinical investigations, providing critical information about neurological disorders [2].
Analytical and Monitoring Approaches
The quest for real-time monitoring of living systems has driven the development of specialized analytical approaches for in vivo measurements:
Solid phase microextraction (SPME): This non-exhaustive sample preparation technique involves using a small amount of extraction phase mounted on a solid support exposed for a defined time in the sample matrix [4]. Its unique features include combining sample preparation, isolation, and enrichment into a single step while reducing sample preparation time [4]. The miniaturized and minimally invasive nature of SPME makes it particularly suitable for in vivo applications in animal models and humans.
Microdialysis: This flow-through sampling technique involves implanting a small probe with a semi-permeable membrane into tissue to continuously collect analytes from the extracellular fluid [4]. The critical requirement for in vivo microdialysis is biocompatibility of all materials contacting extracellular fluids and perfusate to protect both the microdialysis probe and the specimen being sampled [4].
Wearable sensors and devices: These noninvasive, on-body chemical sensors interface with biological fluids like saliva, tears, sweat, and interstitial fluid instead of blood, enabling real-time monitoring of physiological parameters [4]. Modern technological advances in digital medicine and mobile applications have accelerated the development of new wearable devices with a multitude of applications in neuroscience research [4].
Table 2: Key In Vivo Analytical Techniques and Their Applications in Neuroscience
| Technique | Principle | Temporal Resolution | Key Applications | Materials Considerations |
|---|---|---|---|---|
| Solid Phase Microextraction (SPME) | Equilibrium-based extraction onto coated fiber | Minutes to hours | Monitoring neurotransmitters, metabolites, drugs | Biocompatible coatings: C18, PAN, carbon mesh |
| Microdialysis | Diffusion across semi-permeable membrane | Minutes | Neurochemical monitoring, pharmacokinetic studies | Biocompatible membranes: polycarbonate, polyether sulfone |
| Wearable Sensors | Electrochemical or optical detection | Continuous real-time | Physiological monitoring, biomarker tracking | Flexible substrates, biocompatible hydrogels |
| Two-photon Microscopy | Nonlinear optical excitation | Seconds to minutes | Cellular imaging in deep brain structures | Specialized cranial windows, fluorescent indicators |
Quantitative Frameworks and Experimental Design
Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling
The translation of in vitro findings to in vivo efficacy represents a significant challenge in drug development. Quantitative pharmacokinetic/pharmacodynamic (PK/PD) modeling establishes relationships among dose, exposure, and efficacy, enabling prediction of in vivo outcomes from in vitro data [3]. Remarkably, research has demonstrated that in vivo tumor growth dynamics may be predicted from in vitro data when linking in vivo PK corrected for fraction unbound with a PK/PD model that quantitatively integrates knowledge of relationships among drug exposure, pharmacodynamic response, and cell growth inhibition collected solely from in vitro experiments [3].
This approach requires diverse experimental data collected with high dimensionality across time and dose, including target engagement measurements, biomarker levels, drug-free cell growth, drug-treated cell viability, and pharmacokinetic parameters [3]. The implementation of such models can significantly reduce animal usage while enabling the collection of denser time course and dose response data in more controlled systems [3].
Research Reagent Solutions for In Vivo Neuroscience
Table 3: Essential Research Reagents and Materials for In Vivo Neuroscience Studies
| Reagent/Material | Function/Purpose | Example Applications |
|---|---|---|
| Viral Vectors (AAV, CAV2, Lentivirus) | Gene delivery for expression of sensors, opsins, or DREADDs | Selective transduction of specific neuronal populations [2] |
| Chemical Indicators (Calcium-sensitive dyes) | Monitoring neural activity via calcium flux | Functional imaging of circuit dynamics [2] |
| DREADDs (Designer Receptors) | Chemogenetic control of neural activity | Remote modulation of neuronal firing without implants [2] |
| Opsins (Channelrhodopsin, Halorhodopsin) | Optogenetic control of neural activity | Precise temporal control of neuronal activity with light [2] |
| Biocompatible Probes | Neural interface for recording or stimulation | Chronic implantation for electrophysiology [4] |
| MRI Contrast Agents | Enhance tissue contrast for structural and functional imaging | Tracking morphological changes in disease models [2] |
Experimental Protocols for Key In Vivo Methods
Protocol: Chemogenetic Modulation of Neuronal Circuits
This protocol outlines the use of chemogenetics for modulating specific neuronal populations in rodent models:
Stereotaxic Viral Injection:
- Anesthetize animal and secure in stereotaxic frame.
- Identify coordinates for target brain region using brain atlas.
- Perform craniotomy and inject recombinant viral vector (e.g., CAV2-hM3Dq) expressing DREADDs into target region [2].
- Optimal conditions identified include low and medium volume with 0.1 × 10^9 viral particles of CAV2 for safe and specific transduction [2].
Post-operative Recovery:
- Allow 2-4 weeks for adequate gene expression before experiments.
- Monitor animals for any signs of distress or neurological impairment.
Receptor Activation:
- Administer designer drug (e.g., Clozapine-N-oxide, CNO) via appropriate route (i.p. injection, oral gavage).
- Doses typically range from 0.1-5 mg/kg depending on the specific DREADD variant [2].
Functional Assessment:
- Conduct behavioral tests, electrophysiological recordings, or imaging studies to evaluate functional outcomes.
- Include appropriate controls (vehicle injection, empty vector controls).
Protocol: In Vivo Solid Phase Microextraction for Neurochemical Monitoring
This protocol describes the implementation of SPME for monitoring neurotransmitters and metabolites in living brain tissue:
SPME Probe Preparation:
- Select appropriate fiber coating based on target analytes (C18, PAN, carbon mesh).
- Condition fibers according to manufacturer specifications.
- Verify extraction efficiency and reproducibility in vitro before in vivo application [4].
Surgical Implantation:
- Anesthetize animal and secure in stereotaxic apparatus.
- Perform craniotomy at target coordinates.
- Slowly implant SPME probe into brain region of interest.
- Secure probe to skull using dental cement.
Sampling Period:
- Allow equilibrium period (typically 15-30 minutes) for analyte extraction.
- Maintain animal under anesthesia or use chronic implantation for freely moving samples.
Sample Processing:
- Carefully remove SPME probe from brain tissue.
- Desorb analytes using appropriate solvent (typically methanol or acetonitrile/water mixtures).
- Analyze extracts using LC-MS/MS or other appropriate analytical platforms [4].
Data Analysis:
- Quantify analytes using calibration curves generated with isotope-labeled standards.
- Normalize results to extraction time and probe characteristics.
- Perform statistical analysis comparing experimental groups.
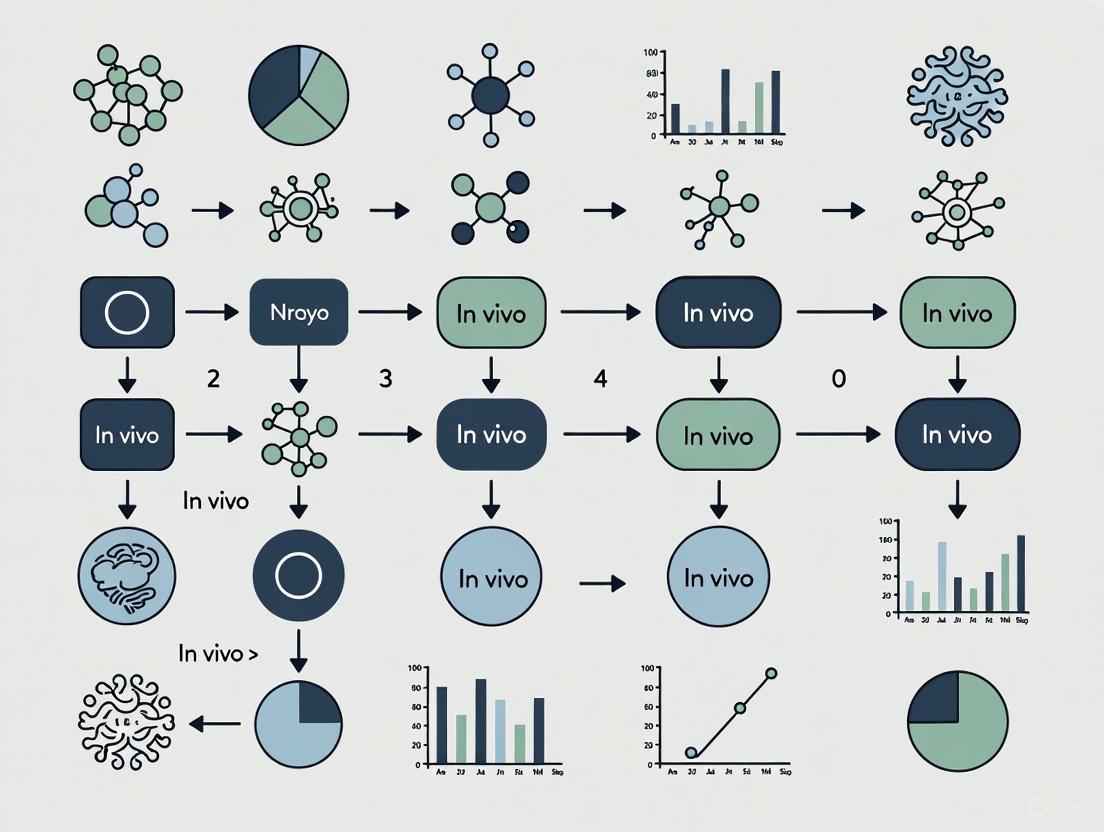
Visualization of In Vivo Research Concepts
Workflow for Integrating In Vitro and In Vivo Research
In Vitro to In Vivo Prediction Workflow
In Vivo Neural Circuit Investigation Techniques
Neural Circuit Investigation Methods
In vivo optical imaging has revolutionized neuroscience by enabling researchers to observe brain structure and function in living organisms. These technologies provide unparalleled sensitivity to functional changes through intrinsic contrast or a growing arsenal of exogenous optical agents, allowing scientists to study the dynamic processes of the brain in its native state [5]. The field encompasses a wide spectrum of techniques, each designed to overcome the fundamental challenge of light scattering in biological tissue, from non-invasive near-infrared imaging for human clinical applications to high-resolution microscopy for cellular-level investigation in animal models [5].
This technical guide provides neuroscientists and drug development professionals with a comprehensive overview of major in vivo imaging modalities, focusing on their operating principles, applications, and implementation considerations. We examine techniques ranging from macroscopic cortical imaging to microscopic cellular resolution methods, with particular emphasis on near-infrared spectroscopy (NIRS) and two-photon microscopy as cornerstone technologies in modern neuroscience research.
Core Imaging Modalities: Technical Principles and Applications
Comparative Analysis of Major Techniques
Table 1: Technical specifications of major in vivo optical imaging modalities
| Imaging Modality | Spatial Resolution | Penetration Depth | Temporal Resolution | Primary Applications in Neuroscience | Key Advantages |
|---|---|---|---|---|---|
| Functional NIRS (fNIRS) | ~1-3 cm (diffuse imaging) | 5-8 mm (cortical surface) [6] | 0.1-10 Hz [7] | Functional neuroimaging, hemodynamic monitoring, cognitive studies [7] [6] | Portable, non-invasive, compatible with other tasks, measures both HbO and HbR [7] [6] |
| Two-Photon Microscopy | Sub-micron to micron level [8] | Up to ~1 mm in neocortex [8] | Milliseconds to seconds (depending on scanning area) | Cellular and subcellular imaging, calcium dynamics, dendritic spine morphology [8] [9] | High-resolution deep tissue imaging, minimal out-of-focus photobleaching [8] |
| Macroscopic Cortical Imaging | 10-100 μm [5] | Superficial cortical layers | 0.1-10 Hz | Cortical mapping, hemodynamic response to stimuli, epilepsy focus identification [5] | Wide-field imaging, intrinsic contrast, simple implementation |
| Optoacoustic Neuro-tomography | Tens to hundreds of microns [10] | Several millimeters to centimeters | Seconds to minutes | Whole-brain functional imaging with calcium indicators [10] | Deep penetration, combines optical contrast with ultrasound resolution |
| Expansion Microscopy | ~15-25 nm (after expansion) [11] | Limited by physical sectioning | N/A (fixed tissue) | Ultrastructural analysis, protein localization, synaptic architecture [11] | Nanoscale resolution with standard microscopes, molecular specificity |
Table 2: Molecular contrast mechanisms in optical brain imaging
| Contrast Mechanism | Measured Parameters | Imaging Modalities | Typical Labels/Dyes |
|---|---|---|---|
| Hemodynamic | Oxyhemoglobin (HbO), deoxyhemoglobin (HbR) concentration changes [7] [5] | fNIRS, macroscopic imaging, DOT | Intrinsic contrast (no labels required) |
| Calcium Dynamics | Neuronal spiking activity via calcium flux [8] [10] | Two-photon microscopy, optoacoustic tomography | Genetically encoded indicators (GCaMP, NIR-GECO2G) [10], synthetic dyes |
| Voltage-Sensitive | Membrane potential changes [5] | Macroscopic cortical imaging, two-photon microscopy | Voltage-sensitive dyes (VSDs) |
| Structural/Morphological | Cell morphology, dendritic spines, synaptic structures [8] [11] | Two-photon microscopy, expansion microscopy | Fluorescent proteins, pan-staining dyes [11] |
| Metabolic | Cytochrome-c-oxidase, NADH fluorescence [5] | Multispectral imaging, fluorescence microscopy | Intrinsic contrast, exogenous dyes |
Fundamental Physical Principles of Light-Tissue Interaction
The effectiveness of different optical imaging modalities is largely determined by how light interacts with biological tissue. Two fundamental processes govern this interaction: absorption and scattering.
Absorption occurs when photons transfer their energy to molecules in the tissue, with hemoglobin being a dominant absorber in the brain. Critically, oxygenated hemoglobin (HbO) and deoxygenated hemoglobin (HbR) have distinct absorption spectra, particularly in the near-infrared range (700-900 nm). This spectral difference enables the quantification of relative changes in hemoglobin concentration through techniques like fNIRS [7] [5].
Scattering causes photons to deviate from their original path and represents the major obstacle to high-resolution deep tissue imaging. The degree of scattering is wavelength-dependent, with near-infrared light (700-900 nm) experiencing less scattering than visible light in neural tissue, creating an "optical window" for non-invasive imaging [7] [5].
The following diagram illustrates the fundamental principles of how different imaging modalities harness light-tissue interactions:
Figure 1: Fundamental principles of light-tissue interactions in optical brain imaging modalities
Detailed Modality Analysis
Near-Infrared Spectroscopy (NIRS) Platforms
Functional near-infrared spectroscopy (fNIRS) represents a cornerstone of non-invasive optical neuroimaging, particularly valuable for clinical populations and studies requiring naturalistic movement or portable monitoring solutions [6].
Technical Principles and Instrumentation
fNIRS operates on the principle that near-infrared light (700-900 nm) can penetrate biological tissues, including the scalp, skull, and brain, while being differentially absorbed by hemoglobin species. The modified Beer-Lambert law forms the mathematical foundation for relating changes in light attenuation to changes in hemoglobin concentration [7]:
Equation: OD = log(I₀/I) = ε · [X] · l · DPF + G
Where OD is optical density, I₀ and I are incident and detected light intensity, ε is extinction coefficient, [X] is chromophore concentration, l is source-detector separation, DPF is differential pathlength factor, and G is geometry-dependent factor [7].
Three primary fNIRS instrumentation approaches have been developed:
Continuous Wave (CW) Systems: Most common commercial systems using constant light intensity. Relatively simple and cost-effective but cannot provide absolute quantification of hemoglobin concentrations without additional pathlength modeling [7].
Frequency Domain (FD) Systems: Utilize amplitude-modulated light to directly measure photon pathlength, enabling absolute quantification of absorption and scattering coefficients [7].
Time Domain (TD) Systems: Employ short light pulses and time-of-flight measurements to directly resolve photon pathlength, offering the most comprehensive information but with greater technical complexity [7].
Experimental Protocol: fNIRS for Balance Task Monitoring
A representative fNIRS experimental protocol for studying cortical activation during balance tasks involves these key steps [6]:
Subject Preparation: Apply fNIRS head cap with source-detector array positioned over regions of interest (e.g., frontal, motor, sensory, temporal cortices) using International 10-20 system for registration.
System Setup: Configure continuous wave fNIRS instrument (e.g., TechEn CW6) with dual wavelengths (690 nm and 830 nm) and source-detector spacing of 3.2 cm to achieve appropriate penetration depth.
Data Acquisition: Record at 4 Hz sampling rate while subject performs balance tasks (e.g., Nintendo Wii Fit skiing simulation), with experimental paradigms typically structured as block designs with 30-second rest periods alternating with task periods.
Signal Processing: Convert raw light intensity measurements to optical density, then to hemoglobin concentration changes using modified Beer-Lambert law with appropriate differential pathlength factors.
Statistical Analysis: Apply general linear modeling to identify statistically significant hemodynamic responses correlated with task conditions, typically showing increased oxyhemoglobin and decreased deoxyhemoglobin in activated regions.
Two-Photon Microscopy
Two-photon laser scanning microscopy (TPLSM) represents the gold standard for high-resolution in vivo imaging in neuroscience, enabling visualization of cellular and subcellular structures in the living brain [8] [9].
Fundamental Principles and Advantages
The technique relies on the near-simultaneous absorption of two photons, each with approximately half the energy needed for electronic transition. This nonlinear process occurs only at the focal point where photon density is highest, providing inherent optical sectioning without the need for a confocal pinhole [8] [9].
Key advantages of two-photon microscopy include:
- Reduced scattering: Use of near-infrared excitation light (700-1000 nm) experiences less scattering in biological tissues [8]
- Deep tissue penetration: Enables imaging up to ~1 mm in neocortex, accessing cortical layers II/III and upper layer V [8]
- Minimal photodamage: Confined excitation volume reduces out-of-focus photobleaching and phototoxicity [9]
- Compatibility with diverse labels: Works with synthetic dyes, genetically encoded indicators, and fluorescent proteins [8]
The following diagram illustrates the experimental workflow for in vivo two-photon imaging:
Figure 2: Experimental workflow for in vivo two-photon microscopy in neuroscience research
Experimental Protocol: In Vivo Calcium Imaging
A standard protocol for two-photon calcium imaging of neuronal population activity includes [8]:
Cranial Window Installation: Under anesthesia, perform craniotomy over the region of interest (e.g., primary visual cortex) and implant a glass coverslip sealed with dental acrylic to create a stable optical window for chronic imaging.
Fluorescent Indicator Expression: Utilize one of several labeling approaches:
- Synthetic dyes: Bulk loading with AM-ester dyes (e.g., OGB-1 AM) using multicell bolus loading technique
- Genetically encoded indicators: Viral vector delivery (e.g., AAV-GCaMP) or transgenic mouse lines expressing calcium indicators under cell-type specific promoters
Two-Photon Microscope Setup: Configure laser-scanning microscope with tunable Ti:Sapphire laser (700-1000 nm range), high numerical aperture objective (20x-40x water immersion), and GaAsP photomultiplier tubes for high-sensitivity detection.
Image Acquisition: Collect time-series data at 4-30 Hz frame rate depending on field of view, with typical imaging volumes of 200×200×200 μm³ for population imaging or smaller fields for single-cell resolution.
Motion Correction and Signal Extraction: Apply computational algorithms to correct for brain motion artifacts, then extract fluorescence traces (ΔF/F) from regions of interest corresponding to individual neurons.
Data Analysis: Relate calcium transients to neuronal spiking activity, sensory stimuli, or behavioral parameters through correlation analysis and statistical modeling.
Emerging and Advanced Modalities
Shortwave Infrared (SWIR) Imaging Recent advances have extended fluorescence imaging into the shortwave infrared range (1000-1700 nm), which offers reduced scattering and autofluorescence compared to traditional NIR windows. SWIR imaging, enabled by novel emitters including organic dyes, quantum dots, and single-wall carbon nanotubes, provides improved tissue penetration and resolution for anatomical, dynamic, and molecular neuroimaging [12].
Multimodal and Optoacoustic Approaches Combining multiple imaging modalities addresses limitations of individual techniques. Functional optoacoustic neuro-tomography (FONT) with genetically encoded calcium indicators like NIR-GECO2G enables whole-brain distributed functional activity mapping with cellular specificity across large volumes [10]. This approach leverages the low vascular background and deep penetration of NIR light while providing ultrasound resolution.
Expansion Microscopy for Ultrastructural Context pan-ExM-t (pan-expansion microscopy of tissue) represents a revolutionary approach that combines ~16-24-fold physical expansion of brain tissue with fluorescent pan-staining of proteins and lipids [11]. This method provides electron microscopy-like ultrastructural context while maintaining molecular specificity through immunolabeling, enabling visualization of synaptic nanostructures including presynaptic dense projections and postsynaptic densities with standard confocal microscopes [11].
Research Reagent Solutions
Table 3: Essential research reagents for in vivo optical brain imaging
| Reagent Category | Specific Examples | Function/Application | Compatible Modalities |
|---|---|---|---|
| Genetically Encoded Calcium Indicators | GCaMP series, NIR-GECO2G [10] | Report neuronal activity via calcium concentration changes | Two-photon microscopy, optoacoustic tomography, widefield fluorescence |
| Synthetic Fluorescent Dyes | OGB-1 AM (calcium), sulforhodamine 101 (astrocytes) [8] | Cell labeling and functional imaging | Two-photon microscopy, widefield imaging |
| Voltage-Sensitive Dyes | RH795, Di-4-ANEPPS [5] | Report membrane potential changes | Macroscopic cortical imaging, two-photon microscopy |
| Fluorescent Proteins | GFP, RFP variants (e.g., tdTomato) [8] | Cell-type specific labeling, morphological analysis | Two-photon microscopy, expansion microscopy |
| Nanoparticle Contrast Agents | Quantum dots, single-wall carbon nanotubes [12] | Deep tissue imaging, SWIR contrast | SWIR imaging, optoacoustic tomography |
| pan-Staining Dyes | NHS ester dyes [11] | Bulk protein labeling for ultrastructural context | Expansion microscopy (pan-ExM-t) |
| Clinical Contrast Agents | Indocyanine green [12] | Vascular imaging, clinical applications | NIRS, diffuse optical tomography |
The landscape of in vivo optical imaging for neuroscience research encompasses a diverse and complementary set of technologies, each with distinct strengths and applications. From portable, non-invasive fNIRS for human studies to high-resolution two-photon microscopy for cellular investigation in animal models, these modalities collectively provide unprecedented access to brain structure and function across multiple spatial and temporal scales.
Current trends point toward continued technological refinement, including expansion into new spectral windows like SWIR, development of increasingly specific molecular probes, and integration of multiple modalities in hybrid approaches. These advances promise to further illuminate the complex dynamics of the living brain, accelerating both basic neuroscience discovery and therapeutic development for neurological disorders.
The optimal choice of imaging methodology depends critically on the specific research question, spatial and temporal resolution requirements, tissue depth of interest, and whether the application involves human subjects or animal models. As these technologies continue to evolve, they will undoubtedly remain indispensable tools in the neuroscientist's arsenal, providing unique windows into brain function in health and disease.
This technical guide explores the principles and applications of intrinsic contrast mechanisms for measuring hemodynamics and metabolism in living brains. Intrinsic contrast refers to the use of endogenous biological molecules that naturally interact with light or magnetic fields, enabling non-invasive or minimally invasive functional imaging. We focus on two primary endogenous contrast sources: hemoglobin for hemodynamic monitoring and cytochromes for metabolic activity assessment. This whitepaper details the underlying physics, instrumentation, experimental protocols, and data interpretation methods for researchers pursuing in vivo neuroscience studies and drug development applications.
Intrinsic contrast imaging leverages naturally occurring physiological contrasts rather than externally administered agents, providing unprecedented sensitivity to functional changes through endogenous biological signatures [13]. The fundamental advantage of this approach lies in its ability to monitor physiological processes without perturbing the system under investigation, making it particularly valuable for longitudinal studies and clinical applications.
In vivo optical brain imaging has seen 30 years of intense development, growing into a rich and diverse field that provides excellent sensitivity to functional changes through intrinsic contrast [13]. These techniques exploit the interaction of light with biological tissue at multiple wavelengths across the electromagnetic spectrum to retrieve physiological information, with the most significant advantages being excellent sensitivity to functional changes and the specificity of optical signatures to fundamental biological molecules [14].
The core physiological parameters measurable through intrinsic contrast include hemodynamic variables (blood volume, flow, oxygenation) and metabolic indicators (oxygen consumption, energy production). These measurements are particularly relevant for neuroscience research where understanding the coupling between neural activity, hemodynamics, and metabolism is essential for deciphering brain function in health and disease.
Physical Principles and Contrast Mechanisms
Light-Tissue Interactions
When light travels through biological tissue like the brain, it undergoes several interactions, with absorption and scattering being the two primary phenomena that generate intrinsic contrast [14]. Absorption by specific chromophores, particularly hemoglobin, provides the foundation for functional imaging, while scattering properties reveal structural information about the tissue microenvironment.
The absorption spectra of hemoglobin differ significantly between its oxygenated (HbO₂) and deoxygenated (HHb) states, enabling quantitative measurement of blood oxygenation through differential optical absorption [14]. This principle forms the basis for many intrinsic contrast imaging techniques, including hyperspectral imaging and near-infrared spectroscopy (NIRS).
Brain tissue exhibits relatively high transparency to light in the near-infrared (NIR) range between 650 and 1350 nm, a region known as the "optical window" [14]. This property enables non-invasive mapping of brain hemodynamics and functional activity, though depth penetration remains limited to superficial cortical layers in human applications due to scattering effects from extracerebral tissues (scalp and skull).
Hemodynamic Contrast Mechanisms
Hemodynamic intrinsic contrast primarily relies on the differential absorption properties of hemoglobin species. The molar absorption coefficients of HbO₂ and HHb vary significantly across the visible and NIR spectrum, with isosbestic points where their absorption is equal enabling concentration quantification [14].
The cerebral metabolic rate of oxygen (CMRO₂) can be estimated by combining hemoglobin concentration measurements with blood flow information, providing a crucial link between hemodynamics and metabolism [14]. This relationship forms the foundation for understanding neurovascular coupling and energy metabolism in the brain.
Table 1: Key Chromophores for Intrinsic Contrast Imaging
| Chromophore | Spectral Signature | Physiological Parameter | Measurement Technique |
|---|---|---|---|
| Oxy-hemoglobin (HbO₂) | Absorption peaks ~540, 580 nm; lower in NIR | Oxygen delivery, blood volume | Hyperspectral imaging, NIRS |
| Deoxy-hemoglobin (HHb) | Absorption peak ~555 nm; higher in NIR | Oxygen extraction, blood volume | Hyperspectral imaging, NIRS |
| Cytochrome c oxidase | Broad absorption in NIR | Mitochondrial metabolism, oxidative phosphorylation | Time-resolved spectroscopy |
| Water | Increasing absorption >900 nm | Tissue composition, edema | Multi-spectral imaging |
Metabolic Contrast Mechanisms
Beyond hemoglobin, intrinsic contrast can derive from molecules directly involved in cellular energy production. Cytochrome c oxidase, the terminal enzyme in the mitochondrial electron transport chain, has distinct optical absorption spectra that change with its oxidation state, providing a direct window into cellular metabolic activity [14].
The flavoprotein and NADH autofluorescence offers additional intrinsic contrasts for monitoring metabolic activity. These coenzymes involved in cellular respiration naturally fluoresce when excited with appropriate wavelengths, and their fluorescence intensity changes with metabolic state, enabling assessment of mitochondrial function and cellular energy production [14].
Imaging Modalities and Instrumentation
Hyperspectral Imaging (HSI)
Hyperspectral imaging (HSI) represents a powerful optical technology for biomedical applications that acquires two-dimensional images across a wide range of the electromagnetic spectrum [14]. HSI systems typically utilize very narrow and adjacent spectral bands over a continuous spectral range to reconstruct the spectrum of each pixel in the image, creating a three-dimensional dataset known as a hypercube (spatial x, y coordinates plus spectral information) [14].
The boundary between HSI and multispectral imaging (MSI) is not strictly defined, though HSI generally involves higher spectral sampling and resolution—typically below 10-20 nm—focusing on contiguous spectral bands rather than the discrete, relatively spaced bands characteristic of MSI [14]. This high spectral resolution enables precise identification and quantification of multiple chromophores simultaneously.
Table 2: Comparison of Intrinsic Contrast Imaging Modalities
| Modality | Spatial Resolution | Temporal Resolution | Depth Penetration | Primary Applications |
|---|---|---|---|---|
| Hyperspectral Imaging | 10-100 μm | Seconds-minutes | ~1 mm (exposed cortex) | Hemoglobin mapping, CMRO₂ estimation |
| Multispectral Imaging | 10-100 μm | Seconds-minutes | ~1 mm (exposed cortex) | Hemoglobin oxygenation monitoring |
| Near-Infrared Spectroscopy (NIRS) | 1-10 cm | Seconds | Several cm | Non-invasive human brain monitoring |
| Functional MRI (BOLD) | 1-3 mm | Seconds | Whole brain | Human brain activation mapping |
| Intrinsic Signal Imaging | 10-100 μm | Seconds | ~1 mm | Cortical mapping in animal models |
Functional MRI with Endogenous Contrast
Blood oxygen level-dependent (BOLD) functional MRI represents another powerful intrinsic contrast technique that exploits magnetic properties of hemoglobin without exogenous contrast agents [15]. Deoxygenated hemoglobin is paramagnetic and creates magnetic field inhomogeneities that affect T2*-weighted MRI signals, while oxygenated hemoglobin is diamagnetic and has minimal effect [15]. Neural activation triggers localized increases in blood flow and oxygenation, reducing deoxyhemoglobin concentration and increasing MRI signal.
Arterial spin labeling (ASL) provides another endogenous contrast mechanism for MRI by magnetically labeling arterial water protons as an endogenous tracer to measure cerebral blood flow without exogenous contrast agents.
Experimental Protocols and Methodologies
Hyperspectral Imaging of Cerebral Hemodynamics
Materials and Equipment:
- Hyperspectral imaging system with appropriate spectral range (500-600 nm for visible; 650-950 nm for NIR)
- Surgical tools for cranial window preparation (for animal studies)
- Stereotaxic frame for head stabilization
- Physiological monitoring equipment (body temperature, respiration)
- Data acquisition computer with appropriate storage capacity
Procedure:
- Animal Preparation: Anesthetize the animal using appropriate anesthetic regimen (e.g., urethane for rodents). Maintain body temperature at 37°C using a heating pad. Secure animal in stereotaxic frame.
- Cranial Window Installation: Perform craniotomy over the region of interest. For chronic studies, utilize a thinned-skull preparation or implant a transparent cranial window. Keep the dura mater intact and moist with artificial cerebrospinal fluid.
- System Calibration: Perform dark current calibration by acquiring images with the lens covered. Acquire images of a standard reflectance target for flat-field correction.
- Baseline Image Acquisition: Acquire hyperspectral image cubes of the baseline state across the selected spectral range. Ensure adequate signal-to-noise ratio by appropriate integration time settings.
- Functional Stimulation: Apply the designed stimulus (sensory, electrical, pharmacological) while continuously acquiring hyperspectral data.
- Data Collection: Continue acquisition during stimulation and for an appropriate post-stimulus period to capture the hemodynamic response.
Data Analysis:
- Spectral Unmixing: Apply algorithms to decompose the measured spectra into contributions from HbO₂ and HHb using their known extinction coefficients.
- Concentration Calculation: Convert optical densities to concentration changes using the modified Beer-Lambert law.
- Spatio-temporal Mapping: Generate maps of HbO₂, HHb, and total hemoglobin changes over time.
- CMRO₂ Estimation: Calculate the cerebral metabolic rate of oxygen using Fick's principle, combining hemoglobin oxygenation data with blood flow information from laser speckle contrast imaging or other modalities.
BOLD fMRI for Human Brain Activation
Materials and Equipment:
- MRI scanner with field strength ≥3T for improved signal-to-noise ratio
- Head coil appropriate for the study
- Stimulus presentation system (visual, auditory, or other)
- Response recording devices (button boxes, etc.)
- Physiological monitoring equipment (pulse oximeter, respiratory belt)
Procedure:
- Subject Preparation: Screen subjects for MRI compatibility. Position subject in scanner with comfortable head immobilization using foam padding.
- Localizer Scans: Acquire structural localizer images for precise positioning of functional slices.
- BOLD Protocol Optimization: Select appropriate pulse sequence parameters (TR, TE, flip angle, resolution) to maximize BOLD sensitivity.
- Task Paradigm Design: Implement block design or event-related design with appropriate baseline conditions.
- Data Acquisition: Acquire T2*-weighted images during task performance with whole-brain coverage and adequate temporal resolution.
- Physiological Monitoring: Record cardiac and respiratory fluctuations concurrently with BOLD data acquisition.
Data Analysis:
- Preprocessing: Apply slice timing correction, head motion correction, spatial smoothing, and temporal filtering.
- Statistical Analysis: Use general linear model (GLM) to identify voxels showing significant signal changes correlated with the task paradigm.
- Group Analysis: Implement random effects analysis to draw population inferences.
- Activation Mapping: Overlay statistical maps on high-resolution anatomical images for visualization.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Intrinsic Contrast Experiments
| Item | Function | Example Applications | Considerations |
|---|---|---|---|
| Hyperspectral Imaging System | Acquires spatial and spectral data simultaneously | Hemoglobin mapping, oxygen metabolism | Spectral range, resolution, and acquisition speed must match application needs |
| MRI Scanner with BOLD Capabilities | Detects hemoglobin oxygenation changes | Human brain activation studies | Field strength directly impacts sensitivity and spatial resolution |
| Cranial Window Chambers | Provides optical access to the brain | Long-term cortical imaging in animal models | Biocompatibility, optical quality, and chronic stability are crucial |
| Physiological Monitoring System | Monitors vital signs during experiments | Ensuring physiological stability | Should include temperature, respiration, and cardiovascular monitoring |
| Spectral Analysis Software | Processes hyperspectral data cubes | Chromophore quantification, spectral unmixing | Algorithms for accurate separation of overlapping spectral signatures |
Visualization of Signaling Pathways and Workflows
Neurovascular Coupling Pathway
Hyperspectral Imaging Workflow
Applications in Neuroscience and Drug Development
Intrinsic contrast imaging techniques provide powerful tools for basic neuroscience research and pharmaceutical development. In basic research, these methods enable investigation of neurovascular coupling—the fundamental relationship between neural activity, hemodynamics, and metabolism [14]. This understanding is crucial for interpreting functional imaging signals and understanding brain energy metabolism.
In drug development, intrinsic contrast methods offer valuable biomarkers for assessing therapeutic efficacy and understanding drug mechanisms. The ability to repeatedly measure hemodynamic and metabolic parameters non-invasively makes these techniques ideal for longitudinal studies of disease progression and treatment response [16]. This is particularly relevant for neuropsychiatric disorders where heterogeneous patient populations and unreliable endpoints have hampered drug development [16].
Hyperspectral imaging solutions have shown particular promise for monitoring brain tissue metabolic and hemodynamic parameters in various pathological conditions, including neurodegenerative diseases and brain injuries [14]. The identification of irregular tissue functionality through metabolic imaging potentially enables early detection and intervention for neurological disorders.
Challenges and Future Perspectives
Despite significant advances, intrinsic contrast imaging faces several challenges. Depth penetration remains limited for optical techniques, particularly in non-invasive human applications where the scalp and skull significantly scatter light [14]. The development of advanced reconstruction algorithms and hybrid approaches combining multiple imaging modalities may help address these limitations.
Another challenge involves the quantitative interpretation of intrinsic contrast signals, particularly disentangling the complex relationships between neural activity, hemodynamics, and metabolism [14]. Computational models that incorporate known physiology can help derive more specific physiological parameters from the measured signals.
Future developments will likely focus on improving spatial and temporal resolution, developing more sophisticated analysis methods, and integrating multiple contrast mechanisms for comprehensive physiological assessment. The combination of intrinsic contrast with targeted extrinsic agents may provide the specificity needed for molecular imaging while maintaining the advantages of endogenous contrast for functional assessment.
For drug development, the adoption of standardized intrinsic contrast biomarkers could significantly improve patient stratification and target validation in clinical trials [16]. As these techniques become more widely available and better validated, they have the potential to transform neuroscience research and therapeutic development for neurological and psychiatric disorders.
In vivo neuroscience research has been fundamentally transformed by optical imaging technologies that bypass the limitations of traditional electrode-based methods. While techniques like whole-cell patch-clamp electrophysiology provide precise measurements, they are inherently low-throughput, typically enabling investigation of only one or a handful of cells simultaneously [17]. The need to observe signal transfer across complex neural circuits created demand for approaches capable of recording from hundreds of neurons simultaneously. Although calcium imaging addressed some of these needs by enabling simultaneous recording from tens to hundreds of cells, it provides only indirect readout of membrane potential changes, lacks temporal resolution for dissecting individual depolarization events at high spiking frequencies, and cannot report on hyperpolarizing or subthreshold membrane potential changes [17]. These limitations created the opportunity for optical electrophysiology using voltage-sensitive dyes (VSDs) and genetically encoded fluorescent reporters, which now enable direct observation of electrical activity across neuronal populations with millisecond precision.
Fundamental Principles and Mechanisms
Photophysical Mechanisms of Voltage Sensing
Voltage-sensitive dyes function by embedding within the cell membrane where they directly experience the uneven charge distribution across the phospholipid bilayer. The two primary classes of modern organic VSDs employ distinct mechanisms to transduce membrane potential changes into optical signals:
- Electrochromic Mechanism: Membrane potential changes induce a spectral shift through alteration of the dye's HOMO-LUMO gap, resulting in voltage-dependent spectral changes that can be measured as absorption or fluorescence shifts [17].
- Photoinduced Electron Transfer (PeT) Mechanism: Changes in membrane potential alter the probability of electron transfer from a π-wire module to the chromophore unit, leading to measurable changes in fluorescence quantum yield [17].
Table 1: Major Classes of Voltage-Sensitive Dyes and Their Properties
| Dye Class | Representative Dyes | Mechanism | Excitation/Emission | Key Characteristics |
|---|---|---|---|---|
| Electrochromic | di-8-ANEPPS, di-4-ANEPPS | Spectral shift | Varies by specific dye | Fast response (<1 ms), rationetric capability [17] [18] |
| PeT-based | VoltageFluor (VF) series | Quantum yield change | Varies by specific dye | High brightness, improved targeting [17] |
| Styryl (Hemicyanine) | RH414, RH795, di-2-ANEPEQ | Multiple mechanisms | Visible spectrum | Widely used in embryonic CNS studies [19] |
| Merocyanine-rhodanine | NK2761 | Absorption change | ~703 nm | High signal-to-noise, low toxicity [19] |
Genetically Encoded Voltage Indicators (GEVIs)
In contrast to synthetic VSDs, genetically encoded voltage indicators are protein-based sensors derived from voltage-sensitive domains engineered to transform voltage responses into fluorescent signals. Early GEVI designs suffered from performance limitations, but recent developments have produced indicators with sufficient speed and sensitivity for in vivo applications [17] [20]. GEVIs typically employ either intrinsic fluorescence or coupling to fluorescent proteins/small-molecule fluorophores, enabling cell-type-specific expression through genetic targeting [20].
Figure 1: Fundamental operating principles of major voltage indicator classes
Experimental Methodologies and Protocols
Dye Loading and Tissue Preparation
Effective VSD imaging requires careful optimization of dye loading conditions and tissue preparation. For ex vivo brain slice preparations, the meningeal tissue is carefully removed to facilitate dye penetration [19]. Staining typically involves incubating tissue in physiological solution containing 0.04-0.2 mg/mL dye for 20 minutes, with the immature cellular-interstitial structure of embryonic tissue allowing better dye diffusion into deeper regions [19]. For in vivo applications, surgical preparation involves anesthetizing the animal, retracting the scalp, and thinning the skull over the region of interest. In some cases, a permanent cranial window can be implanted for repeated long-term imaging over periods exceeding one year [5].
Optical Imaging Hardware Configuration
Modern VSD imaging employs several specialized optical configurations optimized for different experimental needs:
- Epi-fluorescence Measurements: Use quasi-monochromatic light (510-560 nm excitation) reflected off a 575 nm dichroic mirror, with emission collected through a >590 nm long-pass filter [19].
- Ratiometric Measurements: Incorporate secondary dichroic beamsplitting and dual photodetectors (typically <570 nm and >570 nm) to detect voltage-dependent spectral shifts, enabling quantitative membrane potential determination with ~5 mV resolution without temporal or spatial averaging [18].
- High-Speed Imaging: Utilize CMOS-based cameras capable of recording at up to 1,923 frames per second at 256×256 pixel resolution to capture action potential propagation [21].
Table 2: Performance Characteristics of Selected Voltage-Sensitive Dyes
| Dye Name | Signal-to-Noise Ratio | Photobleaching Rate | Toxicity/Recovery | Recommended Applications |
|---|---|---|---|---|
| di-2-ANEPEQ | Largest among fluorescence dyes | Faster | Slower neural response recovery | High-fidelity recording where toxicity is less concern [19] |
| di-4-ANEPPS | Large | Moderate | Relatively long recovery time | General purpose voltage imaging [19] |
| di-3-ANEPPDHQ | Large | Moderate | Relatively long recovery time | Embryonic CNS studies [19] |
| di-4-AN(F)EPPTEA | Smaller | Slower | Faster recovery | Long-duration experiments [19] |
| di-2-AN(F)EPPTEA | Smaller | Slower | Faster recovery | Chronic imaging preparations [19] |
| NK2761 (absorption) | High | Small | Low toxicity, fast recovery | Embryonic nervous system population recording [19] |
Data Acquisition and Analysis
Functional imaging experiments typically involve presenting carefully controlled stimuli (visual, somatosensory, or auditory) during image acquisition, with responses averaged over multiple repetitions to improve signal-to-noise ratio [5]. Data analysis incorporates spatial and temporal filtering to enhance signals, with visualization of spatiotemporal activity patterns through pseudocolor representations and waveform analysis [21]. For ratiometric measurements, calibration is achieved using simultaneous optical and patch-clamp recordings from adjacent points [18].
Figure 2: Standard workflow for voltage-sensitive dye imaging experiments
Advanced Targeting Strategies for Cell-Type-Specific Recording
Synthetic Dye Targeting Approaches
A significant limitation of early VSDs was their non-specific labeling of all membranes in complex tissue environments. Recent innovations have produced sophisticated targeting strategies:
- Enzymatic Uncaging: Polar groups (e.g., phosphate esters) solubilize VSD precursors until activated by cell-specifically expressed phosphatases or esterases [17].
- Light-Directed Activation: "SPOT" sensors remain inactive until triggered by 390 nm light irradiation in defined locations [17].
- Self-Labeling Protein Tags: Hybrid chemogenetic approaches utilize VSDs linked to reactive groups captured by cell-selectively expressed enzymes (HaloTag, SpyTag, ACP-Tag) [17].
- Ligand-Directed Delivery: The VoLDe platform combines dextran polysaccharide carriers with small molecule ligands for cell-selective targeting via natively expressed protein markers, enabling cell-type-specific voltage imaging without genetic manipulation [17].
Organelle-Specific Voltage Imaging
Beyond plasma membrane potential measurements, specialized approaches now enable voltage recording from intracellular compartments:
- Mitochondrial Voltage Imaging: Modern dyes with esterase-mediated unmasking enable specific mitochondrial membrane potential measurements [17].
- Voltair Nanodevices: Nucleic acid-based systems with PeT-based VSDs measure potential across endosomes, lysosomes, and trans-Golgi networks [17].
- LUnAR RhoVR: Tetrazine-substituted PeT sensors activated by click chemistry with trans-cyclooctene-functionalized ceramide in the endoplasmic reticulum [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Equipment for Voltage-Sensitive Dye Imaging
| Category | Specific Examples | Function/Purpose | Notes |
|---|---|---|---|
| Voltage-Sensitive Dyes | di-4-ANEPPS, di-2-ANEPEQ, RH795, VoltageFluor dyes | Report membrane potential changes | Selection depends on signal size, photobleaching, and toxicity requirements [19] |
| Genetically Encoded Indicators | GEVIs based on voltage-sensitive domains | Cell-type-specific voltage reporting | Enable targeting to specific neuronal populations [20] |
| Imaging Systems | MiCAM05-N256, THT Mesoscope, two-photon microscopes | High-speed optical recording | Frame rates >1,000 fps needed for action potential resolution [22] [21] |
| Light Sources | ZIVA Light Engine, Lumencor solid-state engines | Provide excitation illumination | Millisecond control for optogenetics compatibility [22] |
| Targeting Tools | HaloTag ligands, VoLDe platform components | Cell-specific dye delivery | Enable recording from defined cell populations [17] |
| Analysis Software | BV_Ana, BV Workbench | Processing optical recording data | Spatial/temporal filtering, waveform analysis [21] |
Current Applications and Future Directions
Voltage-sensitive dyes and fluorescent reporters now enable diverse neuroscience applications from fundamental circuit mapping to drug screening. In cardiac research, VSDs visualize action potential propagation in isolated hearts and cultured cardiomyocytes at frame rates exceeding 1,800 fps [21]. In developmental neuroscience, specific dyes like NK2761 permit functional organization analysis during embryogenesis [19]. For systems neuroscience, VSD imaging reveals spatiotemporal dynamics of sensory processing across cortical areas in response to visual, somatosensory, or auditory stimuli [5] [21].
The field continues to evolve with several promising directions:
- Improved Targeting Specificity: Advanced chemical and genetic targeting strategies will enable more precise recording from defined neuronal subpopulations [17] [23].
- Integration with Optogenetics: Combined optical stimulation and recording permits all-optical electrophysiology [22].
- Multiparametric Imaging: Simultaneous recording of membrane potential, calcium transients, and metabolic indicators provides comprehensive functional profiling [21].
- Clinical Translation: Fluorescence-guided interventions using optical contrast agents are emerging for intraoperative neural monitoring [24].
Despite these advances, challenges remain in achieving robust in vivo performance with synthetic VSDs in complex environments, improving signal-to-noise ratios without averaging, and minimizing phototoxicity during long-term imaging sessions. The ongoing development of both synthetic dyes and genetically encoded indicators suggests a future where these complementary approaches will continue to expand our ability to observe electrical activity throughout the nervous system with unprecedented spatial and temporal resolution.
The quest to understand the brain requires tools capable of mapping its intricate structures and dynamic processes at the appropriate scale. Emerging technologies in super-resolution microscopy and molecular probes are fundamentally transforming neuroscience research by enabling visualization of neural components and activities at unprecedented resolutions. These advancements are particularly crucial for bridging the gap between molecular mechanisms and systemic brain functions, providing researchers with powerful means to investigate neural circuitry, synaptic plasticity, and molecular dynamics in living systems. Framed within the broader context of in vivo techniques for neuroscience, these technologies offer unparalleled opportunities to observe biological processes in intact organisms, thereby accelerating both basic research and pharmaceutical development [25] [26]. The integration of advanced optical methods with specifically engineered molecular probes is creating new paradigms for investigating neural function and dysfunction, offering insights that were previously inaccessible through conventional microscopy approaches limited by the diffraction barrier of light.
Super-Resolution Microscopy: Seeing Beyond the Diffraction Limit
Fundamental Principles and Technique Comparisons
Super-resolution microscopy (SRM) encompasses several advanced optical techniques that overcome the diffraction limit of conventional light microscopy, which traditionally restricts resolution to approximately 200-300 nanometers laterally and 500-800 nanometers axially [27]. These methods have significantly narrowed the resolution gap between fluorescence microscopy and electron microscopy, opening new possibilities for biological discovery by enabling visualization of subcellular structures and molecular complexes at the nanoscale [27].
The table below provides a technical comparison of the four main categories of commercially available super-resolution microscopy techniques:
Table 1: Comparison of Major Super-Resolution Microscopy Techniques
| Technique (Variants) | Super-Resolution Principle | Spatial Resolution (Lateral) | Temporal Resolution | Key Applications in Neuroscience |
|---|---|---|---|---|
| Pixel Reassignment ISM (AiryScan, SoRA, iSIM) | Reduced Airy unit detection with mathematical or optical fluorescence reassignment | 140-180 nm (120-150 nm with deconvolution) | Low (single-point) to High (multi-point) | Live-cell imaging of synaptic vesicles, organelle dynamics |
| Structured Illumination Microscopy (SIM) (Linear SIM, SR-SIM) | Moiré interference from patterned illumination with computational reconstruction | 90-130 nm (down to 60 nm with deconvolution) | High (2D-SIM) to Intermediate (3D-SIM) | Neural cytoskeleton organization, nuclear architecture |
| Stimulated Emission Depletion (STED) | PSF reduction using excitation with doughnut-shaped depletion beam | ~50 nm (2D STED), ~100 nm (3D STED) | Variable (low for cell-sized FOV) | Nanoscale protein organization in synapses, membrane dynamics |
| Single-Molecule Localization Microscopy (SMLM) (STORM, PALM, PAINT) | Temporal separation of stochastic emissions with single-molecule positioning | ≥2× localization precision (10-20 nm typical) | Very low (typically fixed cells) | Molecular counting, protein complex organization |
Each technique offers distinct advantages and limitations, making them suitable for different neuroscience applications. STED and SMLM provide the highest spatial resolution but often at the cost of temporal resolution, while SIM and ISM offer better balance for live-cell imaging [27]. The choice of technique depends on specific experimental requirements including resolution needs, sample type, imaging depth, and live-cell compatibility.
Recent Technical Innovations
Recent advancements continue to push the boundaries of super-resolution imaging. A novel approach termed Confocal² Spinning-Disk Image Scanning Microscopy (C2SD-ISM) integrates a spinning-disk confocal microscope with a digital micromirror device (DMD) for sparse multifocal illumination [28]. This dual-confocal configuration achieves impressive lateral resolution of 144 nm and axial resolution of 351 nm while effectively mitigating scattering background interference, enabling high-fidelity imaging at depths up to 180 μm in tissue samples [28].
The C2SD-ISM system employs a dynamic pinhole array pixel reassignment (DPA-PR) algorithm that effectively corrects for Stokes shifts, optical aberrations, and other non-ideal conditions, achieving a linear correlation of up to 92% between original confocal and reconstructed images [28]. This high fidelity is crucial for quantitative analysis in neuroscience research where accurate representation of nanoscale structures is essential.
Table 2: Advanced Super-Resolution Implementation Considerations
| Parameter | Technical Challenges | Emerging Solutions |
|---|---|---|
| Imaging Depth | Scattering background interference in tissue | C2SD-ISM dual-confocal configuration; adaptive optics |
| Live-Cell Compatibility | Phototoxicity and photobleaching | Spinning-disk systems; reduced illumination intensity |
| Multicolor Imaging | Channel registration and chromatic aberration | Computational correction; optimized optical design |
| Throughput | Trade-off between resolution and acquisition speed | Multi-focal approaches; advanced detectors |
| Sample Preparation | Fluorophore compatibility and labeling density | Improved synthetic probes; genetic encoding |
For researchers without access to specialized SRM facilities, computational approaches like the Mean Shift Super-Resolution (MSSR) algorithm can enhance resolution from confocal microscopy images, though these must be applied cautiously as selection of thresholding parameters still depends on human visual perception [29].
Molecular Probes for Neuroscience
Optical Sensors for Neural Activity Monitoring
Molecular and chemical probes represent indispensable tools for modern neuroscience, with optical sensors enabling researchers to monitor neural activity with high spatiotemporal resolution. These tools have been particularly transformative for observing activity in large populations of neurons simultaneously, leveraging optical methods and genetic tools developed over the past two decades [25].
The two primary categories of optical sensors are:
- Chemical sensors that directly interact with specific ions or neurotransmitters
- Genetically encoded sensors that can be targeted to specific cell types or subcellular compartments based on genetic promoters
These optical sensors offer several advantages for neuroscience research. They can report sub-cellular dynamics in dendrites, spines, or axons; probe non-electrical facets of neural activity such as neurochemical and biochemical aspects of cellular activities; and densely sample cells within local microcircuits [25]. This dense sampling capability is particularly promising for revealing collective activity modes in local microcircuits that might be missed with sparser recording methods.
Genetic tools further enhance these capabilities by enabling targeting of specific cell types defined by genetic markers or connectivity patterns. Perhaps most importantly, they allow large-scale chronic recordings of identified cells or even individual synapses over weeks and months in live animals, which is especially beneficial for long-term studies of learning and memory, circuit plasticity, development, animal models of brain disease, and the sustained effects of candidate therapeutics [25].
Current Capabilities and Future Directions
Most current in vivo optical recordings focus on monitoring neuronal or glial calcium dynamics, as calcium indicators track action potentials as well as presynaptic and postsynaptic calcium signals at synapses, providing important information about both input and output signals [25]. However, significant limitations remain, as these indicators have variable ability to report subthreshold or inhibitory signals, and while existing indicators can achieve single-spike sensitivity in low firing rate regimes, they cannot yet faithfully follow spikes in fast-spiring neurons [25].
The future of this field lies not only in improving calcium sensors but in generating a broad suite of optical sensors. Voltage indicators are particularly ripe for development, as they could in principle follow both spikes and subthreshold signals, including inhibition [25]. While several genetically encoded voltage indicators have been developed, they do not yet have the desired combination of signal strength and speed. The experience gained from optimizing calcium indicators is expected to be directly applicable to improving voltage indicators, with particular emphasis on developing indicators with ultralow background emissions for reliable event detection and timing estimation [25].
Integrated Experimental Workflows
The power of super-resolution microscopy is fully realized when combined with appropriate molecular probes in integrated experimental workflows. The following diagram illustrates a generalized workflow for super-resolution imaging in neuroscience research, from sample preparation to data analysis:
Diagram 1: Super-resolution Imaging Workflow
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of super-resolution imaging in neuroscience requires careful selection of reagents and materials. The table below outlines key components of the research toolkit for these advanced applications:
Table 3: Essential Research Reagents for Super-Resolution Neuroscience
| Reagent Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Fluorescent Probes | Synthetic dyes (ATTO, Cy dyes), FPs (GFP, RFP variants) | Target labeling for visualization | Photostability, brightness, switching characteristics |
| Immunolabeling Reagents | Primary/secondary antibodies, nanobodies | Specific protein targeting | Labeling density, specificity, accessibility |
| Genetic Encoders | Viral vectors (AAV, lentivirus), Cre-lox systems | Cell-type specific expression in model systems | Expression level, toxicity, delivery efficiency |
| Sample Preparation Materials | Fixatives, mounting media, coverslips | Sample preservation and optical properties | Refractive index matching, structural preservation |
| Imaging Buffers | STED depletion buffers, SMLM switching buffers | Control of fluorophore photophysics | Oxygen scavenging, thiol concentration, compatibility |
For studies focusing on functional imaging rather than structural analysis, molecular probes for monitoring neural activity are essential. The FLIPR Penta High-Throughput Cellular Screening System enables detailed studies of neural activity and disease mechanisms using human iPSC-derived models, which have become increasingly important for translational neuroscience [30]. These systems allow functional characterization of healthy and disease-specific neural models, such as Alzheimer's Disease (AD) organoids incorporating allelic variants of the ApoE gene (2/2, 3/4, and 4/4) to create disease-specific "neurospheres" [30].
Advanced three-dimensional neural organoids utilizing terminally differentiated iPSC-derived neural cells represent a groundbreaking cell-based assay platform with significant potential for neurotoxicity assessment, neuro-active effects of various neuromodulators, and disease modeling [30]. A critical feature of this platform is the use of kinetic calcium imaging, which provides reliable and accurate read-outs for functional neural activity, enabling evaluation of phenotypic changes and compound effects [30].
Applications in Drug Development and Neuroscience Research
Accelerating Pharmaceutical Development
The application of super-resolution microscopy and advanced molecular probes in pharmaceutical development has created significant opportunities for accelerating drug discovery pipelines. In vivo imaging techniques are recognized as valuable methods for providing biomarkers for target engagement, treatment response, safety, and mechanism of action [26]. These imaging biomarkers have the potential to inform the selection of drugs that are more likely to be safe and effective, potentially reducing the high attrition rates in late-phase clinical development where safety and lack of efficacy account for most failures [26].
A key advantage of in vivo imaging in pharmaceutical development is the ability to make repeated measurements in the same animal, significantly reducing the number of animals needed for preclinical studies while enhancing statistical power through intra-subject comparisons [26]. This aligns with the "3Rs" principle (Replacement, Reduction, and Refinement) in animal research, representing a more humane approach to pharmaceutical development [26].
Nuclear imaging techniques, particularly positron emission tomography (PET), have demonstrated significant utility in drug development. PET radionuclides such as 11C (20.4 min half-life) and 18F (109.7 min half-life) can be incorporated into drug candidates at high specific activities (1000-5000 Ci/mmol), enabling their injection at tracer levels (nmol injected) to measure biochemistry in vivo, especially at easily saturated sites like receptors [31]. The validation of receptor-binding radiotracers has been accelerated using gene-manipulated mice and liquid chromatography/mass spectrometry (LC/MS) to establish relevance to human metabolism and biodistribution [31].
Advancing Neuroscience Research
In basic neuroscience research, super-resolution techniques are enabling new discoveries about neural structure and function at the nanoscale. Recent studies have revealed:
- The functional diversity of over 40 different types of amacrine cells in the mouse retina [32]
- Both full-collapse fusion and the more transient 'kiss-and-run' fusion at hippocampal synapses, with the kiss-and-run form involving vesicle shrinkage between fusion events [32]
- How head-direction cells act as a stable 'neural compass' as bats navigate across large natural outdoor environments [32]
- That grid cells track a mouse's position in local reference frames instead of a global frame of reference during path integration tasks [32]
- How facial movements in mice provide a noninvasive readout of 'hidden' cognitive processes during decision-making [32]
These findings demonstrate how emerging mapping technologies are providing unprecedented insights into neural function across multiple scales, from molecular interactions to system-level processing.
The continuing evolution of super-resolution microscopy and molecular probes represents a transformative frontier in neuroscience research and drug development. These technologies are progressively breaking longstanding barriers in spatial and temporal resolution, while simultaneously improving compatibility with complex biological systems including living animals and human-derived models. The integration of advanced optical methods with specifically engineered molecular probes creates a powerful synergy that enables researchers to address fundamental questions in neuroscience with unprecedented precision.
As these technologies mature and become more accessible, they are poised to dramatically accelerate our understanding of brain function in health and disease. The ongoing development of improved voltage indicators, deeper tissue imaging capabilities, and more sophisticated computational analysis methods will further expand the applications of these approaches. For neuroscientists and drug development professionals, staying abreast of these rapidly advancing technologies is essential for leveraging their full potential in both basic research and therapeutic development.
From Bench to Bedside: Applications in Disease Research and Therapy
Exposed-cortex imaging represents a cornerstone of modern systems neuroscience, enabling researchers to visualize brain structure and function with exceptional resolution. This approach involves creating a cranial window or performing a craniotomy to allow optical access to the brain's surface and underlying structures, facilitating direct observation of neural activity in living animals. The development of exposed-cortex imaging techniques has been driven by the BRAIN Initiative's vision to generate a dynamic picture of the brain showing how individual cells and complex neural circuits interact at the speed of thought [33]. These methods have transitioned neuroscience from purely observational science to a causal, experimental discipline where researchers can not only monitor but also precisely manipulate neural circuit dynamics.
The fundamental advantage of exposed-cortex imaging lies in its ability to bypass the light-scattering properties of the skull, which significantly degrade image quality and resolution. Unlike non-invasive approaches that image through the skull, exposed-cortex techniques provide unobstructed optical access to neural tissues, enabling researchers to achieve cellular and even sub-cellular resolution while maintaining the brain's physiological integrity. This technical guide explores the core methodologies, applications, and quantitative comparisons of exposed-cortex imaging platforms, providing neuroscience researchers and drug development professionals with essential information for implementing these transformative technologies.
Core Imaging Modalities and Technical Specifications
Comparative Analysis of Exposed-Cortex Imaging Techniques
Table 1: Technical specifications and applications of major exposed-cortex imaging modalities
| Imaging Modality | Spatial Resolution | Temporal Resolution | Imaging Depth | Primary Applications | Key Advantages |
|---|---|---|---|---|---|
| Intrinsic Signal Imaging | 200-250 μm FWHM [34] | Seconds (hemodynamic-limited) [34] | Surface cortex | Mapping functional organizations (retinotopy, orientation) [34] | Non-invasive, wide-field, no indicators required |
| Two-Photon Microscopy | Sub-micron | Sub-second to seconds | ~400 μm [35] | Cellular & subcellular imaging, calcium dynamics [35] | High resolution, reduced phototoxicity, deep tissue imaging |
| Wide-Field Calcium Imaging | ~20 μm | Sub-second | Surface cortex | Large-scale network activity monitoring [34] | High speed, large field of view, genetically encoded indicators |
| Direct Electrocortical Stimulation (DECS) | 1-10 mm | Milliseconds | Direct surface contact | Functional mapping for surgical planning [36] | Gold standard for functional localization |
Performance Metrics and Quantitative Comparisons
Recent advances have enabled direct quantitative comparisons between exposed-cortex imaging and less-invasive approaches. The SeeThrough skull-clearing technique, developed through systematic screening of over 1,600 chemicals, represents a hybrid approach that achieves refractive index matching (RI = 1.56) while maintaining biocompatibility [35]. When compared to traditional open-skull cranial windows, SeeThrough provides equivalent imaging sensitivity and contrast for monitoring neuronal activity, including calcium transients in dendritic branches with comparable signal-to-noise ratios [35]. This demonstrates that under optimal conditions, minimally invasive methods can approach the performance of exposed-cortex preparations while better preserving brain physiology.
For functional mapping applications, quantitative comparisons reveal important methodological differences. Studies comparing task-based fMRI, resting-state fMRI, and anatomical MRI for locating hand motor areas found substantial variations (>20 mm) in determined locations across modalities in 52-64% of cases [37]. These discrepancies highlight the critical importance of selecting appropriate imaging techniques based on specific research questions and the continued value of direct cortical approaches for precise functional localization.
Experimental Protocols and Methodologies
Surgical Preparation for Chronic Cranial Window Implantation
The foundation of successful exposed-cortex imaging begins with precise surgical preparation. The following protocol outlines the key steps for creating a chronic cranial window preparation suitable for long-term neuronal imaging:
Anesthesia and Sterilization: Induce anesthesia using an appropriate regimen (e.g., isoflurane) and maintain at surgical depth. Administer analgesics and antibiotics preoperatively. Shave the scalp, disinfect with alternating betadine and ethanol scrubs, and maintain body temperature at 37°C using a heating pad.
Skin Incision and Craniotomy: Make a midline scalp incision and retract soft tissue to expose the skull. Identify the target region (e.g., visual cortex centered at 3.5 mm lateral from lambda). Use a high-speed dental drill to perform a craniotomy slightly larger than the intended coverslip, taking care not to damage the underlying dura.
Dura Management and Window Implantation: Based on experimental requirements, either preserve the dura or perform careful durotomy. Position a sterile coverslip (typically 3-5 mm diameter) over the craniotomy and secure using dental cement, creating a sealed preparation. Allow the cement to fully cure before proceeding.
Postoperative Recovery and Imaging: Monitor animals closely during recovery from anesthesia. Allow at least 1-2 weeks for surgical recovery and inflammation resolution before commencing imaging sessions. For chronic preparations, administer antibiotics and analgesics as needed throughout the study period.
Workflow for Large-Scale Neural Circuit Mapping
Table 2: Key reagents and materials for exposed-cortex imaging experiments
| Research Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Coverslip (Optical Window) | Optical access to cortex | 3-5 mm diameter, #1 thickness |
| Dental Acrylic Cement | Secure head frame and window | Self-curing, biocompatible formulation |
| GCaMP Calcium Indicators | Neural activity monitoring | jGCaMP8f for high-sensitivity detection [35] |
| tdTomato Fluorescent Protein | Structural imaging and labeling | Bright, photostable red fluorescent marker |
| Refractive Index Matching Solution | Optical clearing (SeeThrough) | BA/ANP combination (RI = 1.56) [35] |
| Aqueous Intermediate Solvent (AqIS) | Enhanced miscibility for clearing | 75% ethanol urea-saturated solution [35] |
The following diagram illustrates the integrated workflow for comprehensive neural circuit analysis using exposed-cortex imaging:
In Vivo Two-Photon Calcium Imaging Protocol
For monitoring neural population dynamics during behavior, two-photon calcium imaging through cranial windows provides unparalleled resolution. The following protocol details optimal implementation:
Indicator Expression: Transfert target cells to express genetically encoded calcium indicators (e.g., jGCaMP8f) using viral vectors or transgenic approaches. Allow 2-4 weeks for robust expression.
Imaging Setup Configuration: Utilize a two-photon microscope with tunable infrared laser (920 nm for jGCaMP8f). Set field of view to encompass target population (500×500 μm typical). Configure resonant scanners for high-speed acquisition (10-30 Hz).
Animal Positioning and Stabilization: Secure animal's head frame to custom-made stabilization apparatus. Ensure comfort and natural positioning for behavioral tasks. Minimize motion artifacts through proper restraint.
Data Acquisition Parameters: Set laser power to minimize photobleaching (typically 20-50 mW at sample). Use 16-bit detection for sufficient dynamic range. Acquire in continuous mode with 512×512 pixel resolution. Synchronize with behavioral task controllers and stimulus presentation systems.
Post-processing and Analysis: Perform motion correction using cross-correlation or feature-based algorithms. Extract calcium transients using constrained non-negative matrix factorization (CNMF) or similar approaches. Correlate neural dynamics with behavioral parameters and stimuli.
Integration with Broader Neuroscience Research Goals
Exposed-cortex imaging methodologies directly address several priority areas outlined in the BRAIN 2025 scientific vision, particularly "The Brain in Action" goal focused on generating dynamic pictures of brain function [33]. By enabling large-scale monitoring of neural activity with cellular resolution, these techniques facilitate the transition from observational neuroscience to causal circuit analysis. The integration of exposed-cortex imaging with targeted perturbation tools represents a powerful framework for establishing causal links between neural activity and behavior.
The MICrONS program exemplifies the potential of large-scale exposed-cortex imaging, having mapped 84,000 neurons, 500 million synapses, and 200,000 brain cells within a cubic millimeter of mouse visual cortex [38]. This unprecedented dataset, comprising 1.6 petabytes of information, provides a foundational resource for understanding circuit-level computation and validating more scalable, less invasive imaging approaches. Such efforts highlight how exposed-cortex imaging serves as both a primary research tool and a validation standard for emerging technologies.
For drug development applications, exposed-cortex imaging enables direct assessment of compound effects on neural circuit dynamics, cellular physiology, and disease progression in model systems. The ability to longitudinally monitor the same neuronal populations over time provides exceptional statistical power for detecting treatment effects and understanding mechanism of action at the circuit level.
Future Directions and Concluding Perspectives
The evolution of exposed-cortex imaging continues toward increasingly minimally invasive approaches that preserve physiological conditions while maintaining high-resolution access. Techniques like SeeThrough skull clearing demonstrate that imaging through the treated skull can achieve quality comparable to open-skull preparations while avoiding inflammatory responses and intracranial pressure changes associated with craniotomy [35]. Future developments will likely focus on improving the longevity, scalability, and multimodal integration of these platforms.
The combination of exposed-cortex imaging with novel molecular tools, high-throughput computing, and advanced behavioral paradigms will continue to drive discoveries in neural circuit function and dysfunction. As these technologies become more accessible and standardized, they will increasingly support both basic neuroscience discovery and translational drug development efforts aimed at treating neurological and psychiatric disorders. The ongoing development of shared data repositories and analysis platforms, as envisioned in the BRAIN Initiative, will further amplify the impact of these techniques across the neuroscience community [33].
Exposed-cortex imaging remains an essential methodology in the neuroscience toolkit, providing unparalleled access to the dynamic processes underlying brain function. While less invasive approaches continue to advance, the resolution, versatility, and proven track record of direct cortical imaging ensure its continued importance for understanding neural circuits in health and disease.
In vivo Systematic Evolution of Ligands by Exponential Enrichment (SELEX) has emerged as a transformative approach for directly identifying aptamers within living organisms. This technique addresses critical limitations of traditional in vitro methods by performing selection under physiological conditions, thereby enhancing the clinical translatability of selected aptamers for neurological disorders. By leveraging whole living organisms as selection targets, in vivo SELEX identifies aptamers with superior specificity, functionality, and physiological relevance for therapeutic, diagnostic, and imaging applications in neuroscience. This technical review comprehensively examines the principles, methodologies, applications, and future directions of in vivo SELEX, with particular emphasis on its growing significance in targeting neurological conditions such as Alzheimer's disease, Parkinson's disease, and spinal cord injury. We provide detailed experimental protocols, analytical frameworks, and practical resources to facilitate implementation of this groundbreaking technology in neuroscience research and drug development.
Nucleic acid aptamers are single-stranded DNA or RNA molecules, typically comprising 20-100 nucleotides, that fold into specific three-dimensional structures enabling high-affinity and specific binding to diverse targets [39] [40]. First discovered in 1990 through pioneering work by Tuerk and Gold, aptamers are often termed "chemical antibodies" but offer distinct advantages including higher specificity, stronger binding affinity, superior stability, easier chemical modification, lower immunogenicity, and synthetic production capabilities [39] [41]. The process of identifying aptamers, known as Systematic Evolution of Ligands by Exponential Enrichment (SELEX), involves iterative rounds of selection, enrichment, and amplification from random oligonucleotide libraries containing >10^15 sequences to isolate molecules with high affinity for specific targets [39].
The clinical potential of aptamers was established in 2004 with FDA approval of pegaptanib (Macugen) for age-related macular degeneration, followed by avacincaptad pegol (Izervay) in 2023 for geographic atrophy [39]. Currently, ClinicalTrials.gov lists 39 different clinical studies involving aptamers, with ocular diseases representing over 50% of these studies [39]. Despite this promise, many aptamers remain experimental due to challenges with physiological relevance, stability, and delivery efficiency [39].
Table 1: Comparison of In Vitro and In Vivo SELEX Approaches
| Parameter | In Vitro SELEX | In Vivo SELEX |
|---|---|---|
| Selection Environment | Controlled laboratory setting (test tubes) | Whole living organisms |
| Physiological Relevance | Limited; lacks complex physiological context | High; native physiological conditions maintained |
| Target Presentation | Purified molecules or cells | Targets in natural conformation and environment |
| Selection Pressures | Defined binding conditions | Complex biological factors (nucleases, protein competition, biological barriers) |
| Therapeutic Predictive Value | Moderate; requires extensive validation | High; directly identifies functional aptamers |
| Technical Complexity | Lower; simplified workflow | Higher; ethical considerations and biological variability |
| Duration and Cost | Faster and less expensive | Resource-intensive and time-consuming |
Fundamental Principles of In Vivo SELEX
In vivo SELEX represents a paradigm shift from conventional aptamer selection methods by using whole living organisms as selection environments. This approach fundamentally addresses the translational gap often encountered with in vitro selected aptamers, which frequently fail to function in complex biological systems due to unrecognized target interactions, nuclease degradation, and inability to navigate physiological barriers [42] [39].
The core principle of in vivo SELEX involves introducing a diverse library of chemically modified oligonucleotides directly into an animal model, allowing the molecules to circulate throughout the organism and interact with biological targets under authentic physiological conditions [39]. Aptamers that successfully localize to specific tissues or organs are recovered, while unbound sequences are cleared via renal filtration. This process inherently enriches for molecules with favorable pharmacokinetic properties, including stability against nucleases, appropriate biodistribution, and ability to reach intended targets despite biological barriers [39].
A particularly significant advantage for neuroscience applications is the ability of in vivo SELEX to identify aptamers capable of crossing the blood-brain barrier (BBB), a major obstacle for neurological therapeutics [42] [40]. The selection pressure imposed by the BBB means that aptamers recovered from brain tissue have inherently overcome this barrier, either through specific transport mechanisms or passive permeability [40]. Furthermore, by maintaining targets in their native conformation and biological context, in vivo SELEX minimizes off-target effects and enhances the functional relevance of selected aptamers [39].
Comparative Analysis: In Vivo vs. In Vitro SELEX
The selection environment fundamentally differentiates in vivo and in vitro SELEX approaches, with significant implications for the resulting aptamers and their clinical translation.
In Vitro SELEX: Controlled but Artificial
Traditional in vitro SELEX is conducted in controlled laboratory settings where aptamer libraries are exposed to purified target molecules, such as recombinant proteins, peptides, or cultured cells [39]. The process begins with incubation of the library with the target, followed by separation of bound and unbound sequences using techniques such as nitrocellulose filtration, affinity chromatography, or magnetic bead separation [39]. Bound aptamers are amplified via PCR and the process is repeated iteratively to enrich high-affinity sequences.
Key advantages of in vitro SELEX include:
- Precision: Controlled environment (temperature, pH, buffer composition)
- Speed: Rapid screening enabled by high-throughput approaches
- Simplified Workflow: No biological variability or ethical constraints [39]
However, critical limitations include:
- Artificial Conditions: Failure to account for nuclease degradation, ionic strength, pH shifts, and competition with proteins and biomolecules
- Limited Biological Relevance: Inability to replicate complex physiological environments of living organisms
- Unstable Target Binding: Poor compatibility with complex targets like membrane proteins that require specific cellular contexts [39]
In Vivo SELEX: Complex but Physiologically Relevant
In vivo SELEX addresses these limitations by performing selection within living organisms, offering several distinct advantages:
- Biological Relevance: Aptamers evolve under native physiological conditions, ensuring functionality in complex biological environments [39]
- Dynamic Selection: Maintains targets in their native conformation and location, significantly reducing off-target binding [42]
- Overcoming Biological Barriers: Identifies aptamers capable of crossing challenging barriers like the blood-brain barrier, enabling targeted drug delivery to previously inaccessible sites [42] [40]
- Therapeutic Potential: Selects for aptamers stable in complex environments like tumor microenvironments or inflamed neural tissue [39]
The primary challenges of in vivo SELEX include:
- Complexity: Logistical challenges of delivery into organisms and ethical/regulatory constraints
- Variable Outcomes: Biological noise from off-target binding and host immune responses
- Cost and Time: Resource-intensive and time-consuming due to iterative animal use [39]
Hybrid Approaches: Combined SELEX
Recognizing the complementary strengths of both approaches, researchers often employ combined strategies utilizing in vitro SELEX for initial rapid screening followed by in vivo validation and refinement [39]. This balanced approach leverages the speed of in vitro methods while ensuring biological relevance through subsequent in vivo optimization.
Technical Protocols for In Vivo SELEX in Neurological Research
Implementing in vivo SELEX for neurological targets requires specialized protocols to address the unique challenges of the central nervous system. The following section provides detailed methodologies for key experimental procedures.
Library Design and Preparation
The foundation of successful in vivo SELEX is a diverse, nuclease-resistant oligonucleotide library. For neurological applications, specific considerations enhance the probability of obtaining blood-brain barrier penetrating aptamers.
Library Composition:
- Random Region: 30-50 nucleotides provides sufficient structural diversity while maintaining synthetic feasibility [43]
- Constant Regions: 18-25 nucleotide primer binding sites flanking the random region enable PCR amplification
- Chemical Modifications: 2'-fluoro (2'-F) or 2'-O-methyl modifications on pyrimidines confer nuclease resistance without compromising polymerase compatibility [40] [44]
Library Synthesis and Quality Control:
- Synthesize modified oligonucleotides using phosphoramidite chemistry
- Purify by HPLC or PAGE to remove truncated sequences
- Quantify by spectrophotometry and verify integrity by analytical PAGE
- For RNA libraries, perform in vitro transcription with modified nucleotides
- Generate single-stranded DNA through strand separation or asymmetric PCR
In Vivo Selection Workflow for Neurological Targets
The following protocol outlines the specific steps for selecting aptamers against neurological targets:
Library Administration:
- Inject 1-5 nmol of modified oligonucleotide library via systemic route (intravenous, intraperitoneal) or direct CNS administration (intracerebroventricular, intrathecal) depending on target accessibility
- For blood-brain barrier penetration studies, intravenous administration with appropriate circulation time (minutes to hours) is essential
Circulation and Binding:
- Allow library to circulate for sufficient time to reach equilibrium binding (typically 15-60 minutes)
- Longer circulation times favor aptamers with higher stability and slower clearance
Tissue Collection and Processing:
- Euthanize animals and perfuse with cold buffer to remove blood-borne aptamers
- Harvest target tissues (specific brain regions, spinal cord) and homogenize in denaturing buffer
- For cell-specific aptamers, dissociate tissues and sort target cells before aptamer recovery
Aptamer Recovery and Amplification:
- Extract bound aptamers using phenol-chloroform or silica-based methods
- Amplify recovered sequences by PCR (DNA) or RT-PCR (RNA) with appropriate cycle control to minimize bias
- For RNA aptamers, include in vitro transcription step with modified nucleotides
Counter-Selection Strategies:
- Implement negative selection rounds by pre-incubating library with non-target tissues to remove non-specific binders
- For brain-targeted aptamers, pre-clear library against peripheral organs (liver, kidney, spleen) to enrich for CNS-specific binders
Iterative Rounds:
- Repeat process for 5-15 rounds with increasing stringency (reduced circulation time, increased wash stringency)
- Monitor enrichment by quantifying recovery rates after each round
Candidate Identification and Validation
Following completion of selection rounds, comprehensive analysis identifies lead aptamer candidates:
Sequencing and Bioinformatics:
- Perform high-throughput sequencing of early and late selection rounds
- Identify enriched sequences through frequency analysis and cluster similar sequences into families
- Analyze conserved motifs and predicted secondary structures
Binding Validation:
- Synthesize candidate aptamers with appropriate modifications
- Determine affinity (Kd) using surface plasmon resonance (SPR) or electrophoretic mobility shift assays (EMSA)
- Assess specificity through cross-reactivity studies with related targets and tissues
Functional Characterization:
- Evaluate ability to modulate target function in cell-based assays
- Assess stability in cerebrospinal fluid and relevant biological fluids
- Determine pharmacokinetic properties including half-life and biodistribution
Applications in Neuroscience and Neurological Disorders
In vivo SELEX has shown remarkable potential for addressing challenging neurological conditions by generating aptamers with enhanced therapeutic properties.
Neurodegenerative Diseases
For Alzheimer's disease (AD), aptamers targeting amyloid-beta (Aβ) and tau proteins have been developed to inhibit aggregation and promote clearance [40]. The in vivo selection approach ensures these aptamers can access pathological protein aggregates in their native environment within the brain. Similarly, for Parkinson's disease (PD), aptamers targeting α-synuclein have demonstrated efficacy in preventing fibril formation and reducing neurotoxicity in animal models [40].
A notable advancement is the development of aptamers capable of inhibiting protein-protein interactions involved in neurodegeneration. For instance, aptamers targeting the interaction between transcription factors and their binding partners can modulate gene expression pathways implicated in neuronal survival and function [45].
Neuropathic Pain Management
Recent research has demonstrated the successful application of RNA aptamers targeting ionotropic glutamate receptors (iGluRs) for spinal cord injury (SCI)-induced neuropathic pain [44]. In a rat SCI model, RNA aptamers (FN1008, FN1040, FB9s-b) targeting AMPA, kainate, and NMDA receptors showed significant efficacy in alleviating evoked and ongoing neuropathic symptoms without significant adverse effects [44].
Key findings from this application:
- Aptamers exhibited sustained antinociceptive effects that persisted for 2-3 weeks after termination of intrathecal injections
- Treatment efficacy strengthened during repeated administrations, suggesting cumulative therapeutic benefits
- Potential sex differences in aptamer response were noted, indicating possibilities for sex-specific pain therapeutics
- The water-soluble nature of RNA aptamers minimized off-target side effects common with lipophilic small molecules [44]
Blood-Brain Barrier Penetration
A critical application of in vivo SELEX in neuroscience is the identification of aptamers capable of crossing the blood-brain barrier. Transferrin receptor (TfR) binding aptamers have been developed that exploit receptor-mediated transcytosis to deliver therapeutic cargo across the BBB [40]. These aptamers serve as targeting moieties for drug delivery systems, enabling transport of neurotherapeutics that would otherwise be excluded from the brain.
Table 2: In Vivo SELEX Applications in Neurological Disorders
| Neurological Condition | Molecular Targets | Aptamer Functions | Development Status |
|---|---|---|---|
| Alzheimer's Disease | Amyloid-beta, tau proteins | Inhibit aggregation, promote clearance | Preclinical development |
| Parkinson's Disease | α-synuclein | Prevent fibril formation, reduce toxicity | Preclinical development |
| Neuropathic Pain | Ionotropic glutamate receptors | Receptor antagonism, pain relief | Animal models [44] |
| Multiple Sclerosis | Myelin components, immune markers | Immunomodulation, remyelination | Early research |
| Spinal Cord Injury | Growth inhibitors, inflammatory factors | Promote regeneration, reduce inflammation | Animal models |
| Brain Tumors | Tumor-specific antigens | Targeted drug delivery, diagnostics | Preclinical development |
Successful implementation of in vivo SELEX for neurological targets requires specialized reagents and resources. The following toolkit outlines essential components.
Table 3: Research Reagent Solutions for In Vivo SELEX
| Reagent Category | Specific Examples | Function and Importance | Technical Notes |
|---|---|---|---|
| Modified Nucleotide Libraries | 2'-fluoro-pyrimidines, 2'-O-methyl nucleotides | Enhanced nuclease resistance, maintained polymerase compatibility | Critical for stability in biological fluids [40] [44] |
| Animal Disease Models | Transgenic neurodegeneration models, spinal cord injury models | Provide physiologically relevant selection environment | Model choice dictates aptamer applicability to human disease |
| Specialized Amplification Reagents | Reverse transcriptases for modified RNA, thermostable polymerases | Efficient amplification of modified nucleic acids | Standard enzymes may have reduced efficiency with modified nucleotides |
| Blood-Brain Barrier Models | In vitro BBB co-cultures, microfluidic systems | Preliminary screening of BBB penetration capability | Complement but don't replace in vivo validation |
| Tracking and Identification Systems | Color-coded pre-labeled labware, barcoded tubes | Sample integrity maintenance throughout multi-step process | Prevents sample misidentification; withstands cryogenic storage [46] |
| Analytical Instruments | SPR systems, NGS platforms, confocal microscopy | Binding kinetics assessment, sequence analysis, localization studies | Essential for candidate characterization and validation |
Future Directions and Challenges
While in vivo SELEX represents a significant advancement in aptamer selection, several challenges and future directions merit consideration for neuroscience applications.
Current Limitations
Technical Challenges:
- Delivery Efficiency: Systemic delivery often results in minimal brain penetration (<1% of administered dose)
- Selection Resolution: Difficulty in distinguishing cell-type specific binding within complex neural tissues
- Immune Recognition: Modified nucleotides may still trigger innate immune responses affecting selection and function
Practical Constraints:
- Resource Intensity: Significant animal, time, and financial resources required
- Ethical Considerations: Increasing regulatory scrutiny on animal use in research
- Technical Expertise: Requirement for multidisciplinary skills spanning molecular biology, neuroscience, and bioinformatics
Emerging Innovations
Integration with Advanced Technologies:
- Single-Cell SELEX: Combination with single-cell sequencing to identify cell-type specific aptamers within complex tissues
- Spatial Selection: Incorporating spatial transcriptomics approaches to map aptamer binding within tissue architecture
- Microfluidic Platforms: Development of "organ-on-a-chip" systems that simulate physiological environments while maintaining controlled selection conditions
Novel Chemistry Approaches:
- Expanded Genetic Alphabets: Use of artificially expanded genetic information systems (AEGIS) to increase chemical diversity and binding properties [40]
- Structure-Guided Design: Implementation of computational approaches like Blocker-SELEX that integrate structural biology with selection to develop inhibitory aptamers targeting specific protein interfaces [45]
Clinical Translation Pathways
For neurological applications, successful clinical translation will require:
- Delivery Optimization: Development of efficient CNS delivery systems, including focused ultrasound, nanoparticle carriers, and receptor-mediated transcytosis enhancers
- Safety Profiling: Comprehensive assessment of immunogenicity, off-target effects, and long-term toxicity in relevant models
- Biomarker Integration: Companion diagnostics to identify patient populations most likely to respond to aptamer therapeutics
In vivo SELEX represents a transformative approach in aptamer development, particularly for challenging neurological targets. By performing selection within the complex physiological environment of living organisms, this methodology identifies aptamers with superior functional properties, enhanced specificity, and greater clinical translation potential compared to traditional in vitro methods. The ability to select for blood-brain barrier penetration, tissue-specific targeting, and functionality in disease-relevant contexts positions in vivo SELEX as a powerful tool for advancing neuroscience research and developing next-generation neurological therapeutics.
As technical innovations continue to address current limitations and enhance selection efficiency, in vivo SELEX is poised to make significant contributions to our understanding and treatment of neurological disorders. The integration of this technology with emerging fields such as single-cell analysis, spatial omics, and structure-guided design will further expand its applications and impact in neuroscience and beyond.
In vivo techniques represent a cornerstone of modern neuroscience research, providing indispensable tools for unraveling the pathophysiology of complex neurological diseases and evaluating novel therapeutic strategies. The use of animal models allows researchers to investigate molecular, cellular, and systemic processes within an intact living organism, capturing the dynamic interactions that define neurological function and dysfunction. Within the context of a broader thesis on in vivo techniques for neuroscience research, this technical guide focuses on three major neurological disorders: stroke, Alzheimer's disease (AD), and multiple sclerosis (MS). Each condition presents unique challenges that necessitate specific modeling approaches to recapitulate critical aspects of human pathology. Stroke models primarily focus on vascular disruption and subsequent ischemic cascades, AD models target proteinopathy and neurodegenerative processes, while MS models emphasize autoimmune-mediated demyelination. The selection of an appropriate animal model is paramount to experimental design, as each system offers distinct advantages and limitations in mimicking human disease mechanisms [47] [48] [49]. This review provides an in-depth analysis of current animal models for these disorders, detailing their pathological features, experimental methodologies, and applications in preclinical drug development, with the aim of guiding researchers in selecting the most appropriate systems for their specific investigative needs.
Animal Models of Stroke
Pathophysiology and Modeling Principles
Stroke, a leading cause of mortality and long-term disability worldwide, is characterized by the sudden interruption of cerebral blood flow, resulting in oxygen and nutrient deprivation to brain tissues. Animal models of ischemic stroke aim to replicate this cerebrovascular disruption and the subsequent cascade of excitotoxicity, oxidative stress, inflammation, and cell death [47]. The majority of human strokes (80-85%) are ischemic in nature, with large vessel atherosclerosis and cardioembolism representing the most common causes [47]. Successful modeling requires careful consideration of species, strain, sex, and comorbidity factors that significantly influence experimental outcomes and translational potential.
Core Modeling Techniques
Focal Ischemic Models are predominantly achieved through Middle Cerebral Artery Occlusion (MCAO), which mimics the most common form of human ischemic stroke. The transient or permanent intraluminal filament thread occlusion model is widely used due to its easy manipulation and accurately controllable reperfusion, making it suitable for studying pathogenesis of focal ischemic stroke and reperfusion injury [47]. The procedure involves inserting a silicone-coated nylon filament through the common carotid artery into the internal carotid artery until it blocks the middle cerebral artery origin. Embolic models involve injecting autologous blood clots or other embolic materials into the cerebral circulation, providing a more clinically relevant platform for investigating thrombolytic therapies, though with poorer reproducibility [47].
Global Ischemic Models simulate brain-wide ischemia as occurs during cardiac arrest. The four-vessel occlusion (4-VO) model involves permanent electrocoagulation of vertebral arteries followed by reversible occlusion of common carotid arteries, producing highly predictable brain damage but requiring a two-stage surgical procedure with high mortality [47]. The two-vessel occlusion (2-VO) model with hypotension induces forebrain ischemia through reversible bilateral common carotid artery occlusion combined with systemic hypotension, offering a one-stage procedure with lower mortality but poorer reproducibility [47].
Hemorrhagic Stroke Models include the whole blood injection model, which mimics hematoma mass effect and blood toxicity but produces uncontrollable hematoma size, and the collagenase model, where bacterial collagenase injection degrades basal lamina components leading to spontaneous bleeding with more controllable hematoma size, though bleeding is slow and diffuse [47].
Table 1: Key Animal Models of Ischemic Stroke
| Model Type | Common Species | Key Features | Advantages | Limitations |
|---|---|---|---|---|
| Transient MCAO | Rats, Mice | Temporary blockade of MCA with reperfusion | Controllable reperfusion; studies reperfusion injury | Endothelial damage; hyperthermia |
| Permanent MCAO | Rats, Mice | Permanent MCA blockade | Simple; consistent infarct | No reperfusion component |
| Embolic MCAO | Rats, Rabbits | Clot-induced occlusion | Clinically relevant; suitable for thrombolysis studies | Poor reproducibility; spontaneous recirculation |
| Photothrombosis | Rats, Mice | Light-induced thrombosis after dye injection | High reproducibility; minimal trauma | Lack of penumbra; poor response to tPA |
| Endothelin-1 | Rats | Vasoconstrictor-induced ischemia | Flexible infarct location; minimal invasion | Affected by anesthetics; neural modulation effects |
Experimental Protocol: Transient Intraluminal MCAO in Rats
Materials Preparation: Anesthetic (isoflurane or ketamine/xylazine), heating pad, physiologic monitoring equipment, silicone-coated nylon filaments (diameter adjusted to animal weight), surgical instruments, sutures.
Surgical Procedure:
- Anesthetize rat and secure in supine position. Maintain body temperature at 37°C throughout procedure.
- Perform midline neck incision and expose right common carotid artery (CCA), external carotid artery (ECA), and internal carotid artery (ICA).
- Ligate ECA and its branches permanently. Place temporary ligatures around CCA and ICA.
- Make a small incision in ECA stump and advance the silicone-coated filament (diameter 0.28-0.39 mm depending on rat strain and weight) through ICA until mild resistance indicates MCA occlusion.
- Secure filament position and close incision. For transient ischemia, remove filament after 30-120 minutes (depending on desired injury severity) to allow reperfusion.
- Monitor animals closely post-operatively with analgesic support (buprenorphine 0.05 mg/kg) and subcutaneous fluids if needed [50].
Outcome Assessment: Neurological deficit scores at 24h and 72h post-surgery (0=no deficit, 1=forelimb flexion, 2=decreased resistance to lateral push, 3=unidirectional circling, 4=longitudinal spinning, 5=no movement). Infarct volume quantification via TTC staining or MRI at 24-72h. Histopathological analysis for cellular death, inflammation, and blood-brain barrier integrity.
Animal Models of Alzheimer's Disease
Pathophysiology and Modeling Approaches
Alzheimer's disease is a progressive neurodegenerative disorder characterized by extracellular amyloid-β plaques, intracellular neurofibrillary tangles composed of hyperphosphorylated tau, synaptic loss, and eventual neuronal death. Animal models of AD aim to recapitulate these pathological hallmarks and the associated cognitive decline [48]. Modeling approaches have evolved from transgenic overexpression of familial AD mutations to more sophisticated knock-in models that better approximate the human disease state without artificial overexpression. The choice of model depends on the specific research question, whether focused on amyloid pathology, tauopathy, or their interaction.
Transgenic Mouse Models
Amyloid Precursor Protein (APP) Models include the Tg2576 model expressing human APP with the Swedish mutation (KM670/671NL), which develops Aβ plaques at 11-13 months and cognitive impairment around 9-10 months, showing sex-specific differences with more rapid progression in females [51]. The 5xFAD model carries five FAD mutations (Swedish, Florida, London on APP; M146L, L286V on PSEN1), exhibiting aggressive pathology with Aβ42 accumulation beginning at 1.5-2 months, plaques at 2 months, synaptic loss, gliosis, and significant neuronal loss by 9 months, with more severe phenotypes in females [51].
Tauopathy Models such as P301S and rTg4510 mice express mutant human tau protein, developing neurofibrillary tangles, neuronal loss, and brain atrophy. The rTg4510 model features regulatable expression of tau with the P301L mutation, showing tangle pathology by 5.5 months and significant cognitive deficits [51].
Multifactorial Models like the 3xTg-AD model harboring PSEN1M146V, APPSwe, and tauP301L transgenes develop both Aβ and tau pathology in a progressive, age-dependent manner, with intracellular Aβ accumulation at 3-6 months, extracellular plaques by 6 months, and tau pathology by 12 months, alongside synaptic dysfunction and LTP deficits [51].
Next-Generation and Non-Transgenic Models
Knock-In Models such as APP-KI and Tau-KI incorporate human mutations into the endogenous mouse genome without overexpression, resulting in more physiological expression levels and gradual development of pathology. The APPNL-G-F model with Swedish, Iberian, and Arctic mutations shows robust Aβ pathology, neuroinflammation, and cognitive deficits without overexpression [51].
Risk Factor Models include human APOE knock-in mice, where APOE4 knock-in mice display synaptic loss, gliosis, and tau hyperphosphorylation without overt Aβ pathology, and TREM2 models that explore the role of this microglial receptor in AD pathogenesis [51].
Table 2: Characteristics of Selected Alzheimer's Disease Mouse Models
| Model | Genetic Background | Pathology Onset | Key Features | Cognitive Deficits | Limitations |
|---|---|---|---|---|---|
| Tg2576 | APP Swe | Plaques: 11-13 months | Moderate plaque burden; cholinergic dysfunction | 9-10 months | No NFTs; minimal neuronal loss |
| 5xFAD | APP/PS1 with 5 FAD mutations | Aβ: 2 months; Plaques: 2 months | Aggressive amyloid pathology; neuronal loss | 4-6 months | Early, aggressive pathology |
| 3xTg-AD | PSEN1, APPSwe, tauP301L | Aβ: 3-6 months; Tau: 12 months | Both Aβ and tau pathology | 6 months (working memory) | Artificial chromosome integration |
| JNPL3 (P301L) | tau P301L | Tangles: 6.5 months | Motor deficits; NFT pathology | Not primary feature | Strong motor phenotype |
| APP-KI (NL-G-F) | Knock-in APP mutations | Plaques: 6 months | Physiological expression; no overexpression | 6-18 months | Less severe pathology |
Experimental Protocol: Behavioral Assessment in AD Models
Morris Water Maze (Spatial Learning and Memory):
- Equipment: Circular pool (120 cm diameter), opaque water (22°C), platform (10 cm diameter), tracking system.
- Acquisition Phase (4-5 days): Place platform submerged 1 cm below water surface in fixed quadrant. Perform 4 trials daily with different start positions. Measure latency to find platform, path length, and swimming speed.
- Probe Trial (Day 5-6): Remove platform. Allow mouse to swim for 60 seconds. Measure time in target quadrant, platform crossings, and search strategy.
- Data Analysis: Compare learning curves across genotypes and treatments. Impaired spatial learning manifests as longer latencies and poorer probe trial performance.
Y-Maze (Working Memory):
- Equipment: Y-shaped maze with three identical arms at 120° angles.
- Procedure: Allow mouse to freely explore all three arms for 8 minutes.
- Analysis: Record sequence of arm entries. Calculate spontaneous alternation percentage (number of triads containing entries into all three arms / maximum possible alternations). Reduced alternation indicates working memory deficits.
Contextual Fear Conditioning (Associative Memory):
- Training: Place mouse in conditioning chamber. Deliver mild footshock (0.7 mA, 2 seconds) after 3-minute exploration.
- Testing: Return mouse to same chamber 24 hours later without footshock.
- Analysis: Measure freezing behavior (complete immobility except breathing) for 3-5 minutes. Impaired memory manifests as reduced freezing compared to controls.
Animal Models of Multiple Sclerosis
Pathophysiology and Modeling Strategies
Multiple sclerosis is an immune-mediated demyelinating disorder of the central nervous system characterized by multifocal inflammatory lesions, myelin destruction, oligodendrocyte loss, and eventual axonal degeneration. The clinical course is heterogeneous, typically beginning with relapsing-remitting episodes that may evolve into progressive disability [49]. No single animal model captures the full spectrum of MS pathology, necessitating complementary approaches that emphasize different aspects of the disease process, including autoimmune inflammation, viral triggers, and primary demyelination.
Core Modeling Approaches
Experimental Autoimmune Encephalomyelitis (EAE) is the most widely used MS model, induced by active immunization with CNS antigens or passive transfer of autoreactive T-cells. The model reproduces key features of MS neuroinflammation, including blood-brain barrier disruption, immune cell infiltration, and demyelination [49]. Antigen Selection determines disease course and pathology: MOG35-55 peptide in C57BL/6 mice produces chronic progressive disease; PLP139-151 or MBP in SJL/J mice induces relapsing-remitting course [49]. Disease severity is typically assessed using a 0-5 clinical scoring scale: 0=no deficit; 1=limp tail; 2=hindlimb weakness; 3=hindlimb paralysis; 4=forelimb and hindlimb paralysis; 5=moribund or death.
Viral Models: Theiler's Murine Encephalomyelitis Virus (TMEV) infection in susceptible mouse strains (SJL/J) causes initial poliomyelitis followed by chronic progressive demyelinating disease with autoimmune components, suitable for studying viral triggers and progressive MS forms [49].
Toxin-Induced Demyelination Models include cuprizone feeding, which causes reproducible oligodendrocyte apoptosis and demyelination primarily in corpus callosum, followed by spontaneous remyelination upon toxin withdrawal, ideal for studying de/remyelination mechanisms independent of adaptive immunity [49]. Lysolecithin (LPC) focal injection produces discrete demyelinating lesions with robust subsequent remyelination, useful for screening promyelinating therapies [49].
Table 3: Multiple Sclerosis Animal Models Comparison
| Model | Induction Method | Clinical Course | Key Pathologic Features | Applications | Limitations |
|---|---|---|---|---|---|
| EAE (C57BL/6) | MOG35-55 + CFA + PTX | Chronic progressive | Inflammation, demyelination, axonal loss | Immunopathogenesis; drug screening | Less relevant to RRMS |
| EAE (SJL/J) | PLP139-151 + CFA + PTX | Relapsing-remitting | Multiple inflammatory flares | RRMS mechanisms; relapse therapies | Limited chronic progression |
| TMEV | TMEV intracranial injection | Chronic progressive | Demyelination; viral persistence | Viral etiology; progressive MS | Strain restrictions |
| Cuprizone | Toxin in feed | Demyelination: 4-6 weeks; Remyelination: after withdrawal | Oligodendrocyte apoptosis; microglia activation | De/remyelination mechanisms | No adaptive immunity role |
| Lysolecithin | Focal stereotaxic injection | Focal demyelination; remyelination in weeks | Focal demyelination; OPC recruitment | Remyelination therapies | Artificial lesion creation |
Experimental Protocol: Active EAE Induction in C57BL/6 Mice
Antigen Emulsion Preparation:
- Dissolve MOG35-55 peptide in PBS to 2 mg/mL concentration.
- Mix equal volumes of MOG35-55 solution and complete Freund's adjuvant (CFA) containing 4 mg/mL Mycobacterium tuberculosis H37Ra.
- Emulsify thoroughly using two syringes connected by a three-way stopcock until mixture is stable (drop of emulsion doesn't spread in water).
Immunization:
- Anesthetize mice (8-12 weeks old) with isoflurane.
- Subcutaneously inject 100 μL of emulsion (containing 100 μg MOG35-55 and 200 μg Mycobacterium) divided between two sites on the flank.
- Intravenously inject 200 ng pertussis toxin in 100 μL PBS via tail vein immediately after immunization and again 48 hours later.
Post-Immunization Monitoring:
- Monitor mice daily for clinical signs beginning day 7 post-immunization.
- Record clinical scores daily: 0=no disease; 1=limp tail; 2=hindlimb weakness; 3=hindlimb paralysis; 4=hindlimb and forelimb paralysis; 5=moribund.
- Provide supportive care including softened food on cage floor and subcutaneous fluids for mice with scores ≥2.5.
- Sacrifice at predetermined endpoints or upon reaching severity score of 4 for >24 hours.
Tissue Analysis: Perfuse mice with cold PBS followed by 4% PFA. Process spinal cords and brains for histology: H&E for inflammation, LFB for myelin, Bielschowsky silver for axons, Iba1 for microglia, GFAP for astrocytes. Analyze inflammatory foci, demyelination area, and axonal integrity.
Common Neuroinflammatory Pathways Across Disorders
Neuroinflammation represents a critical shared mechanism in stroke, AD, and MS pathogenesis, characterized by microglial activation, astrocyte reactivity, and cytokine production. Despite different initiating events, these disorders converge on similar inflammatory pathways that contribute to disease progression and neural damage [52].
Microglial Activation occurs in response to danger signals including Aβ (AD), myelin debris (MS), and damage-associated molecular patterns from necrotic cells (stroke). Microglia transition from homeostatic to activated states, adopting diverse functional phenotypes traditionally categorized as pro-inflammatory (M1) or anti-inflammatory (M2), though this represents a simplification of a continuous spectrum [52]. In AD, microglia cluster around amyloid plaques but become dysfunctional in clearance capacity. In MS, microglia phagocytose myelin and present antigens to T cells. In stroke, microglia contribute to both damage and repair processes.
Astrocyte Reactivity follows microglial activation, with astrocytes adopting neurotoxic (A1) or neuroprotective (A2) phenotypes. A1 astrocytes are induced by IL-1α, TNFα, and C1q released from activated microglia and lose normal synaptic supportive functions while gaining complement component secretion that mediates synapse elimination [52]. In AD, reactive astrocytes surround plaques and contribute to synaptic loss. In MS, astrogliosis forms glial scars in chronic lesions. In stroke, astrocytes participate in both the inflammatory response and tissue repair.
Inflammatory Mediators including TNF-α, IL-1β, IL-6, and complement components are elevated across these disorders. Key signaling pathways such as NF-κB and MAPK are activated in glial cells, propagating inflammatory responses that exacerbate neuronal damage [52]. The NLRP3 inflammasome is particularly important in AD, activated by Aβ to produce IL-1β and IL-18.
Diagram 1: Shared Neuroinflammatory Pathways. This diagram illustrates common neuroinflammatory mechanisms across stroke, Alzheimer's disease, and multiple sclerosis, highlighting microglial activation, astrocyte reactivity, and key inflammatory mediators.
Advanced In Vivo Techniques
Intravital Imaging of the Neurovascular Unit
The neurovascular unit - comprising neurons, astrocytes, pericytes, and cerebrovasculature - represents a dynamic interface critical for CNS homeostasis. Intravital imaging using two-photon laser scanning microscopy enables real-time visualization of cellular processes within the living brain, capturing dynamic responses to injury and disease progression [53].
Stroke Applications: In vivo imaging reveals thrombotic events, fibrin deposition, and BBB compromise within hours after MCAO. Following micro-occlusions, imaging has documented emboli extravasation through vascular walls and subsequent phagocytosis by microglia, demonstrating unique self-repair mechanisms [53]. Pericyte morphology alterations contribute to BBB weakening and persistent blood flow reduction after stroke.
AD Applications: Intravital imaging shows Aβ-mediated dendrite and spine loss, instability of vascular tone, and altered calcium signaling in astrocytes that affects cerebrovascular function. Microglial processes dynamically interact with dendritic spines, potentially regulating their stability in AD models [53].
MS Applications: In EAE models, in vivo imaging captures T cell dynamics at the cerebrovasculature, their migration across the BBB, and interactions with antigen-presenting cells. Focal axonal lesions and microglial involvement in axonal degeneration can be visualized in real time [53].
Multi-Table Methods for Network Neuroscience
Advanced analytical approaches like covSTATIS enable integrated analysis of multiple correlation/covariance matrices derived from neuroimaging data, identifying structured patterns in multi-table data while preserving data fidelity and enhancing interpretability [54]. This method is particularly valuable for comparing functional connectivity matrices across individuals or groups, characterizing similarity in connectivity profiles between brain regions, and assessing individual deviations from group-level patterns.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Neuroscience Disease Modeling
| Reagent Category | Specific Examples | Applications | Considerations |
|---|---|---|---|
| Anesthetics | Isoflurane, Ketamine/Xylazine, Pentobarbital | Surgical procedures, in vivo imaging | Effects on cerebral blood flow, neuroprotection |
| Analgesics | Buprenorphine, Carprofen | Post-operative pain management | Potential effects on inflammation; required ethically |
| Adjuvants | Complete Freund's Adjuvant, Pertussis Toxin | EAE induction to enhance immune response | Dose optimization critical for consistent disease |
| Antibodies | Anti-Aβ, Anti-MOG, Anti-CD3, Anti-GFAP, Anti-Iba1 | Immunotherapy, immunohistochemistry, flow cytometry | Species compatibility; validation required |
| Viral Vectors | AAV, Lentivirus, TMEV | Gene delivery, disease modeling, viral models | Tropism, expression level/duration, immune response |
| Tracers | Dextran conjugates, Sulforhodamine-101, Ca²⁺ indicators | BBB permeability, vascular imaging, cellular activity | Molecular weight, clearance, toxicity |
| Cytokines/Chemokines | TNF-α, IL-1β, IFN-γ, MCP-1 | Inflammation studies, cell recruitment assays | Short half-life; appropriate delivery methods |
| Transgenic Reporter Lines | GFAP-GFP, CX3CR1-GFP, Thy1-YFP | Cell-specific visualization, fate mapping, dynamics | Background strain; expression pattern consistency |
Animal models remain indispensable tools for advancing our understanding of stroke, Alzheimer's disease, and multiple sclerosis pathogenesis. The optimal choice of model depends critically on the specific research question, with each system offering unique advantages and limitations. Stroke models effectively capture acute vascular events and reperfusion injury, AD models replicate progressive proteinopathy and synaptic failure, while MS models reproduce immune-mediated demyelination. Recent advances including intravital imaging, sophisticated genetic models, and multi-table analytical methods have significantly enhanced our ability to investigate dynamic disease processes in real time. Looking forward, the development of more sophisticated models that better capture disease heterogeneity, incorporate multiple risk factors, and enable study of compensatory mechanisms will further strengthen translational research. The continued refinement of these in vivo techniques, coupled with careful experimental design and ethical considerations, promises to accelerate the development of novel therapeutic strategies for these devastating neurological disorders.
Functional near-infrared spectroscopy (fNIRS) and diffuse optical tomography (DOT) represent a class of non-invasive optical neuroimaging techniques that have rapidly evolved for human brain mapping. These technologies leverage near-infrared light to monitor cerebral hemodynamics and oxygenation, providing a bridge between the high temporal resolution of electroencephalography (EEG) and the high spatial resolution of functional magnetic resonance imaging (fMRI) [55] [5]. As the field of neuroscience increasingly focuses on in vivo techniques for studying brain function in naturalistic settings, NIRS and DOT offer unique advantages including portability, tolerance to motion artifacts, and the ability to separately quantify oxygenated and deoxygenated hemoglobin concentrations [56] [57]. This technical guide examines the fundamental principles, methodological considerations, and cutting-edge applications of these optical technologies within a broader thesis on in vivo neuroscience research, with particular relevance to researchers, scientists, and drug development professionals seeking practical neuroimaging tools.
Fundamental Principles and Technical Specifications
Core Imaging Mechanisms
fNIRS and DOT operate on the principle that biological tissues are relatively transparent to light in the near-infrared spectrum (650-900 nm) [55] [57]. Within this optical window, the primary chromophores—oxyhemoglobin (HbO) and deoxygenated hemoglobin (HbR)—exhibit distinct absorption spectra, enabling their selective quantification based on modified Beer-Lambert law principles [56] [5]. When neuronal activation occurs, neurovascular coupling mechanisms trigger localized changes in cerebral blood flow, volume, and oxygen metabolism, subsequently altering HbO and HbR concentrations [55] [57]. fNIRS measures these hemodynamic changes using source-detector pairs placed on the scalp, with typical source-detector separations of 2.5-4 cm for adults to ensure sufficient cortical penetration [57]. DOT extends this approach by employing high-density optode arrays and image reconstruction algorithms to generate three-dimensional tomographic maps of hemodynamic activity [58] [59] [60].
Figure 1: Fundamental Principles of fNIRS/DOT. Near-infrared light penetrates biological tissues following a banana-shaped path, with absorption primarily influenced by hemodynamic-dependent chromophores (HbO₂ and HbR) in the cerebral cortex.
Technical Comparison with Other Neuroimaging Modalities
Table 1: Technical comparison of fNIRS/DOT with other common neuroimaging modalities
| Parameter | fNIRS/DOT | fMRI | EEG | PET |
|---|---|---|---|---|
| Spatial Resolution | 1-3 cm [55] | 1-5 mm [5] | 5-9 cm [55] | 4-5 mm [5] |
| Temporal Resolution | 0.1-10 Hz [57] | 0.5-2 Hz [5] | 0.001-0.5 s [55] | Minutes [5] |
| Penetration Depth | 2-3 cm (cortical) [55] | Whole brain [5] | Cortical [55] | Whole brain [5] |
| Portability | High [56] [57] | Low [5] | High [55] | Low [5] |
| Measured Parameters | HbO, HbR [56] | BOLD signal [5] | Electrical potentials [55] | Metabolic activity [5] |
| Tolerance to Motion | Moderate-High [55] | Low [5] | Moderate [55] | Low [5] |
| Cost | Low-Moderate [55] | High [5] | Low [55] | High [5] |
Advanced Methodologies and Experimental Protocols
fNIRS/DOT Experimental Workflow
Figure 2: fNIRS/DOT Experimental Workflow. Comprehensive pipeline from experimental design to data interpretation, highlighting critical preprocessing and reconstruction steps.
Atlas-Guided DOT with GLM Analysis
Advanced DOT methodologies increasingly incorporate anatomical guidance for improved spatial accuracy. The atlas-guided volumetric DOT approach combines magnetic resonance imaging (MRI)-derived head templates with depth compensation algorithms to enhance three-dimensional image reconstruction [59]. This method addresses the fundamental depth sensitivity limitation in DOT by counter-balancing the exponential attenuation of sensitivity with increasing penetration depth [59]. When integrated with general linear model (GLM)-based analysis, this approach enables robust statistical mapping of brain activation without subjective selection of activation periods [59].
Protocol: Atlas-Guided DOT with GLM Analysis
Forward Model Computation: Generate a sensitivity matrix (Jacobian, J) that characterizes the relationship between changes in absorption at each voxel and measurements at each source-detector pair using a finite element method (FEM) mesh based on a head atlas [58] [59].
Depth Compensation: Apply depth compensation algorithms (DCA) to the sensitivity matrix to counterbalance the exponential signal attenuation with depth, producing a modified matrix (J#) [59].
Image Reconstruction: Reconstruct volumetric DOT images using the depth-compensated sensitivity matrix and continuous-wave fNIRS measurement data through inverse solution algorithms [58] [59].
GLM Statistical Analysis: Perform voxel-wise GLM analysis on the time-series of 3D DOT images using a design matrix that incorporates the experimental paradigm convolved with a hemodynamic response function (HRF) [59].
Activation Mapping: Generate statistical parametric maps of significant hemodynamic responses correlated with the experimental tasks, with appropriate multiple comparisons correction [59].
Hybrid Decomposition Frameworks
Modern analysis frameworks for fNIRS/DOT data increasingly adopt hybrid decomposition approaches that integrate spatial priors with data-driven refinement. The NeuroMark pipeline exemplifies this approach by using templates derived from large-scale datasets as spatial priors in a single-subject spatially constrained independent component analysis (ICA) [61]. This methodology preserves individual variability while maintaining correspondence across subjects, enhancing both sensitivity and generalizability [61]. Functional decompositions can be categorized across three key attributes: source (anatomic, functional, multimodal), mode (categorical, dimensional), and fit (predefined, data-driven, hybrid) [61].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential materials and reagents for fNIRS/DOT research
| Item | Function/Application | Technical Specifications |
|---|---|---|
| fNIRS/DOT System | Continuous-wave imaging systems most common for functional studies [62] | Laser diodes/LEDs (2+ wavelengths); photodetectors (APD/PMT); sampling rate: 0.1-100 Hz [55] |
| Optodes | Light sources (emitters) and detectors placed on scalp [62] | Source-detector separation: 1.5-5 cm depending on age; typically 3 cm for adults [57] |
| Headgear | Secure optode placement and positioning on scalp | Material: elastic fabric/neoprene; customizable for different head sizes [62] |
| Co-registration Equipment | Anatomical localization of optodes | 3D digitizers; MRI-compatible markers; photogrammetry systems [57] |
| SNIRF Format | Standardized data storage [62] | Community-developed format supporting continuous-wave, time-, frequency-domain data [62] |
| NIRS-BIDS Extension | Standardized data organization [62] | Hierarchical folder structure; JSON/TSV metadata files [62] |
| Anatomical Atlases | Guidance for image reconstruction | MRI-based head templates; brain parcellation atlases [59] |
Current Applications in Neuroscience and Clinical Translation
Clinical and Cognitive Neuroscience Applications
fNIRS and DOT have demonstrated significant utility across diverse neuroscience domains, particularly where traditional neuroimaging modalities face limitations. In neurological and psychiatric disorders, these technologies have been applied to study stroke, Parkinson's disease, epilepsy, and mental disorders [56] [55]. For example, in stroke rehabilitation, fNIRS can monitor cortical reorganization during recovery, while in epilepsy, it offers potential for seizure focus localization through hemodynamic response characterization [57]. The developmental neuroscience field has particularly benefited from fNIRS due to its tolerance to motion and quiet operation, enabling studies of language acquisition, social perception, and cognitive development in infants and children [55] [60]. DOT has revealed resting-state networks in neonates that mirror those observed in adults, providing insights into the early functional organization of the brain [60].
In cognitive neuroscience, fNIRS/DOT have been employed to investigate higher-order functions including risk decision-making, executive function, and language processing. A study utilizing atlas-guided DOT with the Balloon Analog Risk Task (BART) identified significant hemodynamic changes in the dorsolateral prefrontal cortex (DLPFC) during active decision-making, with distinct activation patterns between genders [59]. The portability of these systems enables ecological momentary assessment of brain function in real-world environments and during naturalistic behaviors, including social interactions [55].
Combined Neuromodulation and Imaging
The compatibility of fNIRS with electromagnetic neuromodulation techniques represents a particularly promising application. fNIRS can be coupled with transcranial magnetic stimulation (TMS) and transcranial electrical stimulation (TES) to monitor cortical responses during neurostimulation, providing real-time feedback for establishing closed-loop strategies that integrate evaluation, feedback, and intervention [56]. This combination offers opportunities to visualize spatiotemporal changes in brain activity during repeated TMS sessions, providing objective quantification of transient and prolonged cerebral functional responses to neurostimulation interventions [56]. Such approaches contribute to the development of individualized precise neurorehabilitation protocols for central nervous system diseases [56].
Technical Challenges and Innovative Solutions
Key Limitations and Advanced Mitigation Strategies
Table 3: Technical challenges and innovative solutions in fNIRS/DOT
| Challenge | Impact on Data Quality | Emerging Solutions |
|---|---|---|
| Superficial Contamination | Confounds brain signals with systemic physiology from scalp [58] | Short-distance channels; signal processing regression; principal/independent component analysis [57] |
| Depth Sensitivity | Exponential decay with penetration depth; poor localization accuracy [58] [59] | Depth compensation algorithms; spatial variant regularization; time-resolved systems [59] |
| Spatial Resolution | Limited by scattering; typically 1-3 cm [55] | High-density arrays; tomographic reconstruction; anatomical priors [59] [60] |
| Baseline Optical Parameters | Errors in chromophore quantification and localization [58] | Subject-specific MRI guidance; deep learning post-processing; multi-distance measurements [58] |
| Standardization | Reproducibility across sites and studies [62] | NIRS-BIDS extension; SNIRF file format; open-source processing tools [62] |
| Individual Anatomical Variation | Incorrect functional localization [61] | Atlas-guided reconstruction; co-registration with individual anatomy; hybrid decomposition frameworks [59] [61] |
Deep Learning and Computational Advances
Recent computational innovations have significantly addressed fundamental limitations in DOT image reconstruction. The ill-posed nature of the inverse problem in DOT means that small errors in measurements or modeling can cause large reconstruction errors [58]. Traditional perturbation models rely on approximate baseline optical parameters from literature, but inter-subject variations can reach 20-50%, leading to errors in activation contrast, localization, and area estimation [58]. Deep learning approaches, particularly model-based learning that combines neural networks with classical model equations, have demonstrated promise in marginalizing these errors while overcoming limitations of pure learning approaches such as training biases and large data requirements [58]. These computational advancements parallel improvements in experimental systems employing novel spatial, temporal, and frequency encoding strategies [58].
The clinical translation of non-invasive NIRS and DOT for human brain imaging continues to evolve through technological innovations and methodological refinements. Future developments will likely focus on whole-head, high-density optode arrays with enhanced depth sensitivity through time-resolved measurement systems [60]. The integration of complementary neuroimaging modalities, particularly EEG, will provide multi-parametric assessment of brain function by combining hemodynamic and electrophysiological information [57]. Standardization efforts through initiatives like NIRS-BIDS and SNIRF will enhance reproducibility and data sharing across the research community [62]. Computational advances in image reconstruction, particularly deep learning approaches that marginalize errors from uncertain baseline optical parameters, will improve quantitative accuracy [58]. Furthermore, the development of compact, wearable, and wireless systems will enable long-term monitoring of brain function in ecologically valid environments, opening new possibilities for understanding brain dynamics in real-world contexts [56] [55].
In conclusion, fNIRS and DOT have established themselves as valuable tools within the in vivo neuroscience research arsenal, offering unique capabilities for studying brain function across diverse populations and settings. While technical challenges remain, ongoing innovations in instrumentation, signal processing, and image reconstruction continue to expand the clinical and research applications of these optical neuroimaging technologies. For researchers, scientists, and drug development professionals, these modalities provide a versatile platform for investigating brain function, monitoring therapeutic responses, and developing novel biomarkers for neurological and psychiatric disorders.
Chimeric Antigen Receptor T-cell (CAR-T) therapy represents a paradigm shift in cancer treatment and is increasingly explored for autoimmune neurological diseases. While traditional ex vivo CAR-T therapy involves genetically engineering a patient's T cells outside the body, in vivo CAR-T represents a transformative innovation that delivers CAR genes directly into the patient to reprogram T cells inside the body [63] [64]. This emerging platform bypasses complex manufacturing processes associated with ex vivo approaches, offering potential for reduced costs, improved accessibility, and broader application across therapeutic areas, including neuroscience research [63] [64]. This technical guide examines the core principles, methodologies, and potential neuroscientific applications of in vivo CAR-T cell therapy, providing researchers with a comprehensive framework for exploring this innovative platform.
Fundamental Principles of CAR-T Technology
Chimeric Antigen Receptors (CARs) are engineered fusion proteins that redirect T cells to specifically target antigens expressed on disease-associated cells. The fundamental structure of a CAR consists of four key components [65] [66]:
- An extracellular antigen-binding domain (typically a single-chain variable fragment, scFv)
- An extracellular spacer or hinge region
- A transmembrane domain
- An intracellular T-cell signaling domain
CAR-T cells are classified into generations based on their intracellular signaling domains. Second-generation CARs, which incorporate one costimulatory domain (e.g., CD28 or 4-1BB), form the basis of all currently approved commercial products [66]. Later generations incorporate additional costimulatory domains or cytokine secretion capabilities to enhance persistence and efficacy [66].
Limitations of Ex Vivo CAR-T Manufacturing
Traditional ex vivo CAR-T therapy involves a complex, multi-step process: leukapheresis to collect patient T cells, activation and genetic modification ex vivo, expansion in culture, and finally reinfusion into the patient [65] [63]. This approach faces several significant limitations:
- Time-intensive processes: Manufacturing can take 3-5 weeks, limiting applicability for patients with rapidly progressing diseases [63] [64]
- High costs: Complex manufacturing in specialized GMP facilities results in treatments costing hundreds of thousands of dollars [63] [64]
- Logistical challenges: Requires specialized infrastructure for cell transport and handling [64]
- T-cell fitness impairment: Ex vivo manipulation can compromise T-cell function and persistence [63]
Table 1: Key Limitations of Ex Vivo CAR-T Manufacturing
| Limitation Category | Specific Challenges | Impact on Patients |
|---|---|---|
| Manufacturing Process | Time-intensive (3-5 weeks), Complex supply chain, Requires GMP facilities | Treatment delays incompatible with rapidly progressing diseases |
| Economic Factors | High manufacturing costs ($300,000-$500,000 per treatment) | Limited accessibility and reimbursement challenges |
| Technical Constraints | T cell fitness impairment during ex vivo culture, Variable product quality | Reduced efficacy potential, Inconsistent clinical outcomes |
| Infrastructure Requirements | Need for specialized treatment centers, Apheresis capabilities | Limited availability, Particularly in resource-limited settings |
The In Vivo CAR-T Paradigm
In vivo CAR-T therapy represents a fundamental shift in approach, delivering CAR genes directly into the body to reprogram the patient's own T cells in their native environment [63] [64]. This strategy eliminates the need for ex vivo manufacturing by using viral or non-viral vectors to transduce T cells directly within the patient's circulation or lymphoid tissues [63]. The approach potentially addresses multiple limitations of conventional CAR-T therapy by simplifying logistics, reducing costs, and preserving T-cell fitness through avoidance of ex vivo manipulation [63] [64].
Technical Foundations of In Vivo CAR-T Platforms
Vector Systems for In Vivo Gene Delivery
The success of in vivo CAR-T therapy depends critically on the efficiency and specificity of gene delivery systems. Multiple vector platforms are under investigation:
- Viral Vectors: Adeno-associated viruses (AAVs) are leading candidates due to their favorable safety profile and tropism for various tissues. Lentiviral vectors offer stable genomic integration but raise greater safety concerns for in vivo use [63] [64].
- Non-Viral Delivery Systems: Lipid nanoparticles (LNPs) have emerged as promising alternatives, particularly for mRNA-based transient CAR expression. Polymer-based nanoparticles and other synthetic delivery systems offer potential for improved targeting and reduced immunogenicity [64].
Recent advances in vector engineering focus on enhancing tropism for T cells through surface modifications with ligands or antibodies specific to T-cell markers (e.g., CD3, CD4, CD8) [63]. Optimization of vector pharmacokinetics and biodistribution is crucial to maximize transduction efficiency while minimizing off-target effects.
CAR Designs for In Vivo Application
CAR constructs for in vivo application require special considerations compared to ex vivo approaches:
- Transient vs. Persistent Expression: mRNA-based CAR delivery offers transient expression (days to weeks), potentially enhancing safety through limited persistence, while DNA-based approaches using integrating vectors aim for long-term expression [64].
- Safety Switches: Incorporation of suicide genes or other controllable safety switches provides an additional layer of safety control for in vivo approaches where products cannot be quality-tested before administration [64].
- Targeting Specificity: Enhanced specificity through logic-gated CAR designs may be particularly valuable for in vivo applications where precise control over which cells are modified is more challenging [66].
Table 2: Comparison of In Vivo CAR-T Delivery Platforms
| Delivery Platform | Genetic Payload | Expression Duration | Key Advantages | Major Limitations |
|---|---|---|---|---|
| AAV Vectors | DNA | Long-term (months to years) | Established manufacturing, Multiple serotypes for different tropisms | Pre-existing immunity concerns, Limited packaging capacity |
| Lentiviral Vectors | DNA (integrated) | Long-term/persistent | Stable genomic integration, Sustained expression | Insertional mutagenesis concerns, Complex safety profile |
| mRNA-LNP | mRNA | Transient (days to weeks) | Excellent safety profile, Rapid iteration potential | Repeated dosing may trigger immunogenicity, Limited persistence |
| Non-Viral DNA Vectors | DNA | Variable | Potential for reduced immunogenicity, Lower cost | Generally lower transfection efficiency |
Manufacturing and Quality Control
The manufacturing paradigm for in vivo CAR-T therapy shifts focus from cell products to vector production:
- Centralized GMP Vector Production: Enables large-scale, consistent lot production with comprehensive quality control testing before distribution [64]
- Distributed Administration Model: Vector products can be distributed to diverse clinical settings without specialized cell processing capabilities [64]
- Simplified Supply Chain: Eliminates need for patient-specific cell shipping and handling [63] [64]
This approach potentially addresses the "vein-to-vein" time and scalability limitations of autologous ex vivo CAR-T therapy while maintaining product consistency across treatment sites [64].
In Vivo CAR-T in Neuroscience Research and Neuro-Oncology
Overcoming Neurological Disease Challenges
The application of in vivo CAR-T platforms to neuroscience research and neurotherapeutics presents unique opportunities and challenges:
- Blood-Brain Barrier Penetration: Vector design must account for the need to cross or bypass the BBB, potentially through direct administration or receptor-mediated transcytosis [67]
- Target Antigen Selection: Ideal targets for neurological applications include disease-specific proteins with minimal expression on essential neural cells [65]
- Safety Considerations: The irreplaceable nature of neural tissue necessitates exceptional specificity to avoid on-target/off-tumor neurotoxicity [65]
Preclinical Advances in Neuro-Oncology
Recent research demonstrates promising applications of CAR-T technology for brain malignancies. A notable example comes from Mayo Clinic researchers who developed MC9999, a PD-L1-targeted CAR-T therapy tested in glioblastoma multiforme (GBM) models [67]. This approach strategically targets PD-L1, which is overexpressed on both GBM cells and immunosuppressive cells within the tumor microenvironment, potentially addressing a key resistance mechanism [67].
Notably, the GBM model utilized patient-derived CAR-T cells, exemplifying the potential for personalized approaches even within the in vivo paradigm [67]. The therapy demonstrated the ability to cross the blood-brain barrier and achieve significant tumor reduction in preclinical models [67].
Potential for Autoimmune Neurological Diseases
Emerging research explores CAR-T therapy for autoimmune neurological conditions, where targeted elimination of pathogenic immune cells could potentially reset immune tolerance [65] [64]. Conditions under investigation include:
- Multiple sclerosis - Targeting B cells expressing CD19 or other autoreactive markers [65]
- Myasthenia gravis - Directed against B cells producing pathogenic autoantibodies [65]
- Neuromyelitis optica - Elimination of aquaporin-4 autoantibody-producing cells [65]
The transient nature of some in vivo CAR-T approaches (particularly mRNA-based) may be especially suited to autoimmune applications, potentially providing temporary immune reset without permanent immunomodulation [64].
Experimental Protocols and Methodologies
In Vivo CAR-T Generation Workflow
The following diagram illustrates the core experimental workflow for in vivo CAR-T generation and validation:
Key Methodological Considerations
Vector Administration Protocols
Effective in vivo CAR-T generation requires optimization of administration parameters:
- Route of Administration: Intravenous injection provides systemic distribution, while local administration may enhance target tissue delivery. For neurological applications, intrathecal or direct CNS delivery may be considered [67]
- Dosing Strategy: Single versus multiple dosing regimens must be evaluated based on expression kinetics of the chosen platform [64]
- Pre-conditioning: The need for lymphodepleting chemotherapy in in vivo approaches requires investigation, as some platforms may function effectively without this prerequisite [64]
Analytical Methods for Validation
Comprehensive characterization of in vivo-generated CAR-T cells requires multiple analytical approaches:
- Flow Cytometry: Detection of CAR expression using target antigen recombinants or anti-idiotype antibodies
- Functional Assays: Standard chromium release assays or real-time cytotoxicity assays to measure target cell killing
- Cytokine Profiling: Multiplex ELISA or Luminex assays to quantify cytokine secretion upon antigen exposure
- Molecular Analyses: qPCR or ddPCR to quantify vector copy numbers in transduced cells
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for In Vivo CAR-T Development
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Vector Production | AAV serotypes, LNPs, Plasmids, Packaging cells | Delivery of CAR genetic payload to T cells in vivo |
| CAR Detection | Recombinant target antigens, Anti-idiotype antibodies, Protein L | Validation of CAR expression on transduced T cells |
| Functional Assay | Target cell lines, Cytokine detection antibodies, Cytotoxicity reagents | Assessment of CAR-T cell effector functions |
| Phenotypic Analysis | Fluorochrome-conjugated antibodies (CD3, CD4, CD8, memory markers) | Characterization of CAR-T cell populations and differentiation states |
| In Vivo Modeling | Immunodeficient mice, Humanized mouse models, Disease-specific models | Preclinical evaluation of efficacy and safety |
Current Landscape and Future Directions
Emerging Clinical Evidence
The in vivo CAR-T field is rapidly advancing from preclinical to clinical evaluation. Key developments include:
- Kelonia Therapeutics has initiated a Phase 1 study of anti-BCMA in vivo CAR-T therapy for relapsed/refractory multiple myeloma in Australia [64]
- Early-stage clinical trials for B-cell non-Hodgkin's lymphoma are generating first-in-human data [64]
- Preclinical data in animal models of cancer, autoimmune diseases, and cardiac fibrosis show promising results [64]
Technical Challenges and Research Frontiers
Despite promising advances, significant technical hurdles remain:
- Optimizing Vector Tropism: Enhancing specificity for T cells while minimizing off-target transduction [63] [64]
- Balancing Persistence and Safety: Achieving sufficient CAR-T cell persistence for durable efficacy while maintaining safety controls [64]
- Mitigating Immunogenicity: Preventing immune responses against vectors or CAR components that could limit repeated administration [63]
- Manufacturing Scalability: Developing robust, scalable processes for vector production to support broader clinical application [64]
Neuroscience-Specific Applications and Considerations
The intersection of in vivo CAR-T platforms with neuroscience research presents unique opportunities:
- Neuroimmunology Research: In vivo CAR-T could enable precise manipulation of specific immune cell populations involved in neuroinflammatory processes
- Neuro-oncology: Application for primary CNS malignancies requires optimization of delivery strategies to overcome the blood-brain barrier [67]
- Autoimmune Neurology: Targeted elimination of autoreactive B or T cells in conditions like multiple sclerosis or autoimmune encephalitis [65]
The following diagram illustrates the mechanistic action of in vivo CAR-T cells in targeting neurological disease:
In vivo CAR-T cell therapy represents a transformative approach that potentially addresses fundamental limitations of current ex vivo CAR-T platforms. By eliminating complex manufacturing processes, reducing costs, and simplifying administration, this technology could significantly expand access to sophisticated cell therapies across multiple disease areas, including neurological disorders and neuro-oncology [63] [64]. The ongoing clinical evaluation of in vivo CAR-T platforms will provide critical data on safety, efficacy, and practical implementation requirements. For neuroscience researchers and therapy developers, this innovative platform offers powerful new opportunities to target neurological diseases through in vivo immune reprogramming, potentially enabling novel treatment paradigms for conditions with significant unmet needs.
Navigating Translational Challenges and Optimizing Protocols
The blood-brain barrier (BBB) represents one of the most formidable challenges in neuroscience research and neurotherapeutic development. This sophisticated physiological interface separates the central nervous system (CNS) from systemic circulation, protecting the brain from harmful substances while maintaining a homeostatic environment for optimal neural function [68] [69]. From a research perspective, the BBB's selective permeability fundamentally limits our ability to deliver chemical probes, imaging agents, and therapeutic compounds to their intended CNS targets. The BBB restricts passage to over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics, creating a significant bottleneck in both neuroscience investigation and treatment development for neurological disorders [69] [70].
Understanding the BBB's structure and function is paramount for developing effective in vivo research methodologies. The vertebrate BBB is a complex, heterogeneous multicellular structure that not only protects the CNS from blood-borne neurotoxic and inflammatory threats but also actively regulates brain homeostasis through specialized transport mechanisms [68]. For neuroscience researchers, the imperative is to develop strategies that temporarily overcome or bypass these barrier functions without causing permanent damage or disrupting the delicate neural environment. This technical guide examines current approaches for delivering drugs and research probes across the BBB, with particular emphasis on methods compatible with in vivo neuroscience research paradigms.
BBB Structure and Physiological Function
Cellular Components of the Neurovascular Unit
The BBB's remarkable barrier properties emerge from the coordinated function of multiple cell types collectively termed the neurovascular unit. Brain endothelial cells (BECs) form the core structural component, differing significantly from peripheral endothelial cells through their absence of fenestrae, minimal pinocytic activity, and extensive tight junctions that limit both paracellular and transcellular transport [68] [69]. These specialized endothelial cells are interconnected by protein complexes including tight junctions (TJs, e.g., claudins, occludin) and adherens junctions (AJs, e.g., cadherins), which create high electrical resistance and severely restrict paracellular diffusion of molecules larger than 500 Da [68] [71].
Pericytes, embedded within the basement membrane, play crucial roles in BBB development, maintenance, and regulation. Through physical attachment via peg-and-socket junctions and paracrine signaling, pericytes influence tight junction formation, modulate microvascular tone, and contribute to angiogenesis and injury response [68] [69]. Astrocytes extend end-feet processes that extensively cover the cerebral vasculature, contributing to BBB integrity through the release of trophic factors and communication with endothelial cells [69] [70]. The collaborative function of these cellular elements creates a dynamic, regulated interface that poses significant challenges for research probe and drug delivery.
Transport Mechanisms Across the BBB
The BBB employs multiple specialized transport mechanisms that can be co-opted for research and therapeutic purposes, each with distinct advantages and limitations:
Table 1: Primary Transport Mechanisms at the Blood-Brain Barrier
| Mechanism | Description | Substrate Characteristics | Research Applications |
|---|---|---|---|
| Passive Diffusion | Non-energy-dependent movement along concentration gradient | Small (<400-500 Da), lipophilic (LogP>2), limited hydrogen bonds (<8-10) | Small molecule neuropharmaceuticals, lipophilic probes |
| Carrier-Mediated Transport | Protein-facilitated movement of essential nutrients | Structural similarity to endogenous substrates (glucose, amino acids) | Nutrient-mimetic probes, substrate-modified compounds |
| Receptor-Mediated Transcytosis (RMT) | Vesicular transport initiated by receptor-ligand binding | Macromolecules, nanoparticles with specific targeting ligands | Antibody delivery, nanoparticle-based systems |
| Adsorptive-Mediated Transcytosis | Vesicular transport triggered by charge interactions | Cationic proteins or nanoparticles | Cell-penetrating peptide conjugates |
| Efflux Transport | Active removal of compounds by transporter proteins | Diverse substrates recognized by P-gp, BCRP, MRPs | Understanding drug resistance, efflux inhibitor co-administration |
These transport pathways provide the foundational knowledge required to design effective BBB-penetrating research tools and therapeutics. The physicochemical properties of molecules—including molecular weight, lipophilicity, polar surface area, and hydrogen bonding capacity—critically determine their ability to traverse the BBB via these mechanisms [69] [70].
Strategic Approaches for Crossing the BBB
Physicochemical Optimization of Probe Molecules
Strategic modification of molecular properties represents the most straightforward approach to enhance BBB penetration. For small molecule probes and drugs, this involves optimizing key parameters to favor passive diffusion: molecular weight under 500 Da, appropriate lipophilicity (typically measured as clog P between 1.5-2.5), minimal hydrogen bond donors (<5) and acceptors (<10), and reduced topological polar surface area (tPSA <60-70 Ų) [72] [70]. Fluorescence probe design exemplifies this approach, where researchers systematically modify scaffold structures to achieve the necessary balance between optical properties and BBB permeability [72].
For example, in the development of ONOO⁻ detection probes, Cheng et al. employed a benzobODIPY scaffold with log P = 2.60, while Wang et al. utilized a Rhodol scaffold (log P = 2.16) to achieve sufficient BBB penetration for in vivo imaging applications [72]. These strategic modifications enable researchers to track neurochemical processes in real-time without physically disrupting the BBB integrity.
Receptor-Mediated Transcytosis (RMT) Strategies
RMT leverages the natural transport mechanisms of BBB endothelial cells to shuttle macromolecules and nanoparticles into the brain. This approach involves conjugating research probes or therapeutics to ligands that bind receptors highly expressed on the brain endothelium [69] [73].
Table 2: Key Receptors for Mediated Transcytosis Across the BBB
| Receptor | Ligand Examples | Advantages | Limitations | Research Applications |
|---|---|---|---|---|
| Transferrin Receptor (TfR) | OX26, 8D3 antibodies, transferrin | Extensive characterization, high expression | Peripheral expression, potential toxicity | Antibody delivery, nanoparticle targeting |
| Insulin Receptor | Insulin, specific antibodies | Effective brain uptake demonstrated | Risk of metabolic side effects | Enzyme replacement therapies |
| LDL Receptor Family | Angiopep-2, apolipoproteins | Diverse ligand options, high transport capacity | Complexity of receptor family | Nanoparticle delivery, gene therapies |
| CD98hc | Specific antibodies | High delivery efficiency demonstrated | Limited characterization | Bispecific antibody platforms |
| Glucose Transporter 1 (GLUT1) | Glucose conjugates | High expression, essential nutrient transporter | Competition with endogenous glucose | Glucose-conjugated nanocarriers |
The efficiency of RMT-based delivery varies significantly between receptor systems. Recent studies indicate that CD98hc-targeting bispecific antibodies achieve 80-90% greater brain delivery efficiency compared to TfR-targeted versions, highlighting the importance of receptor selection [73]. Additionally, receptor affinity must be carefully optimized—excessively high affinity can trap therapeutic agents on the endothelial cell surface, reducing transcytosis efficiency [73].
Nanoparticle-Based Delivery Systems
Nanocarriers provide versatile platforms for protecting therapeutic cargo and enhancing BBB penetration through multiple mechanisms. These systems typically range from 10-300 nm in diameter and can be engineered with specific surface properties to exploit various transport pathways [74] [70].
Liposomes, polymer nanoparticles, and solid lipid nanoparticles represent the most extensively studied nanocarrier systems for brain delivery. Their surfaces can be modified with targeting ligands (e.g., transferrin, insulin) to engage RMT pathways or with cell-penetrating peptides to facilitate adsorptive-mediated transcytosis [74] [70]. The nanocarrier composition also enables controlled release kinetics, potentially extending the duration of action within the CNS.
Recent advances include the development of biomimetic nanoparticles that incorporate native cellular membranes or exploit natural transport mechanisms. For instance, peptide 4F, which mimics high-density lipoprotein (HDL), has shown promise in reducing amyloid-β accumulation at the BBB in Alzheimer's disease models by modulating the p38 MAPK pathway [75].
Physical and Physiological Methods for BBB Disruption
Physical techniques to transiently open the BBB offer an alternative strategy for delivering impermeable research probes and therapeutics. These approaches create temporary disruption of tight junctions, allowing enhanced paracellular transport.
Focused ultrasound (FUS) combined with microbubble contrast agents enables localized, reversible BBB opening. The technique applies low-intensity ultrasound waves to targeted brain regions following intravenous microbubble administration. The microbubbles oscillate in response to ultrasound energy, mechanically disrupting tight junctions through stable cavitation. This method achieves precise spatiotemporal control over BBB permeability, with restoration of barrier integrity typically occurring within hours [75].
Other physical methods include:
- Intranasal administration: Exploits olfactory and trigeminal neural pathways for direct nose-to-brain delivery, completely bypassing the BBB [75] [72].
- BBB modulators (BBBMs): Compounds like HAVN1 peptide that temporarily loosen tight junctions through specific biological mechanisms [75].
- Osmotic disruption: Intra-arterial infusion of hypertonic solutions (e.g., mannitol) to shrink endothelial cells and separate tight junctions, though this approach is less specific than FUS [75].
Experimental Models and Methodologies for BBB Research
In Vitro BBB Models
In vitro BBB models provide cost-effective, high-throughput systems for preliminary screening of BBB permeability. The Transwell system, where endothelial cells are cultured on semipermeable membranes separating luminal and abluminal compartments, represents the most widely used approach [71]. These models enable measurement of transendothelial electrical resistance (TEER), permeability coefficients, and specific transport mechanisms.
Advanced in vitro systems incorporate multiple cell types (endothelial cells, pericytes, astrocytes) in increasingly physiological configurations. Three-dimensional models, including spheroids and microfluidic "organ-on-a-chip" devices, better recapitulate the native neurovascular unit architecture and function [71]. The NIH-funded "NVU-on-a-chip" project aims to create a comprehensive system incorporating CSF, neuronal, and vascular compartments with realistic flow conditions and cellular organization [71].
In Vivo Permeability Assessment Methods
In vivo models remain essential for validating BBB penetration due to the complex multicellular interactions impossible to fully replicate in vitro. Several well-established techniques enable quantitative assessment of BBB permeability:
Evans Blue (EB) Extravasation: The classic method for evaluating BBB integrity involves intravenous administration of Evans Blue dye, which binds serum albumin. Following circulation, animals are perfused with saline to remove intravascular dye, and brain EB content is quantified spectroscopically after formamide extraction [76]. This method provides a straightforward, quantitative measure of macromolecular leakage.
Fluorescent Probe Imaging: Advanced fluorescence imaging techniques utilize molecular probes designed for specific biological targets and BBB penetration. For example, Probe 6 (log P = 2.16) enabled visualization of age-dependent ONOO⁻ accumulation in Alzheimer's disease mouse models, while Probe 14 facilitated 3D photoacoustic imaging of NO in Parkinson's disease models at different brain depths [72].
Radiotracer and MRI Methods: Positron emission tomography (PET) and magnetic resonance imaging (MRI) with appropriate contrast agents enable non-invasive, longitudinal assessment of BBB permeability in both research and clinical settings [68]. These techniques are particularly valuable for tracking therapeutic delivery and disease progression.
Protocol: Evaluating Compound Permeability Using Evans Blue
Materials:
- Evans Blue dye (2% solution in saline)
- Formamide
- Spectrophotometer
- Surgical tools for transcardial perfusion
- Water bath (60°C)
Procedure:
- Administer Evans Blue (4 mL/kg) intravenously to experimental animals.
- Allow circulation for predetermined time (typically 30-180 minutes).
- Anesthetize animals and perform transcardial perfusion with saline (approximately 100 mL for mice) until effluent runs clear.
- Dissect brain regions of interest and weigh tissue.
- Homogenize tissue in formamide (1 mL/100 mg tissue).
- Incubate samples at 60°C for 24 hours with occasional mixing.
- Centrifuge at 10,000 × g for 20 minutes.
- Measure supernatant absorbance at 620 nm.
- Calculate Evans Blue content using a standard curve and normalize to tissue weight [76].
This protocol was employed in studies of Astragalus polysaccharide (APS), which demonstrated significantly reduced Evans Blue extravasation in middle cerebral artery occlusion (MCAO) models, indicating BBB protective effects [76].
Visualization: Signaling Pathways and Experimental Workflows
Signaling Pathways in BBB Protection and Regulation
APS Neuroprotective Mechanism
This diagram illustrates the mechanism by which Astragalus polysaccharide (APS) protects BBB integrity following ischemic injury, as demonstrated in MCAO model rats [76]. APS inhibits P2X7R receptor activation, subsequently downregulating MMP-9 expression and reducing BBB disruption.
Experimental Workflow for BBB Permeability Assessment
BBB Permeability Assessment Workflow
This workflow outlines the key steps in evaluating compound effects on BBB permeability using Evans Blue extravasation, a fundamental methodology in BBB research [76].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for BBB and Neurovascular Research
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| BBB Permeability Markers | Evans Blue, Trypan Blue, sodium fluorescein | Quantitative assessment of barrier integrity | Evans Blue binds albumin, indicating macromolecular leakage |
| Tight Junction Markers | Anti-claudin-5, anti-occludin, anti-ZO-1 antibodies | Immunohistochemical evaluation of BBB structure | Claudin-5 is predominant TJ protein at BBB |
| Endothelial Cell Models | Primary brain microvascular endothelial cells, hCMEC/D3 cell line | In vitro BBB models | Require co-culture for full BBB phenotype |
| Transport Assay Systems | Transwell plates, TEER measurement apparatus | Permeability and transport studies | TEER values >150 Ω·cm² indicate competent barriers |
| Neuroinflammatory Probes | Probe 6 (ONOO⁻), Probe 14 (NO) | In vivo monitoring of neuroinflammatory processes | Designed for BBB penetration and specific reactivity |
| Nanoparticle Systems | PEGylated liposomes, PLGA nanoparticles, solid lipid nanoparticles | Therapeutic/probe delivery vehicles | Size (50-200 nm) optimal for BBB penetration |
| FUS Equipment | Focused ultrasound transducer, microbubble contrast agents | Physical BBB disruption | Enables localized, reversible opening |
The field of BBB research continues to evolve with emerging technologies offering unprecedented opportunities for neuroscience investigation and therapeutic development. Advanced detection methods for nanoparticles in the brain, including high-resolution intravital microscopy and multimodal imaging approaches, are enhancing our understanding of delivery kinetics and distribution patterns [77]. The integration of sophisticated in vitro models with targeted delivery strategies promises to accelerate the development of effective neurotherapeutics while reducing reliance on animal models.
Future directions include the refinement of brain shuttle systems that more efficiently exploit endogenous transport mechanisms, the development of conditionally active biologics that minimize off-target effects, and the advancement of stimuli-responsive materials that release their cargo in response to specific pathological triggers. For neuroscience researchers, these innovations will provide increasingly powerful tools to probe neural function and intervene in neurological disorders, ultimately advancing our understanding of the brain in health and disease.
As these technologies mature, maintaining focus on the delicate balance between effective BBB penetration and preservation of neurovascular function will remain paramount. The most successful approaches will be those that achieve targeted delivery while respecting the BBB's crucial role in maintaining the precise neural environment required for optimal brain function.
In vivo techniques are indispensable in neuroscience research for elucidating the fundamental mechanisms of brain function, transport phenomena, and neurological disease pathology in a living system. Understanding molecular transport in the brain in vivo is essential for elucidating how the brain regulates its metabolism, how neurological pathologies develop, and why many brain-targeted drugs fail [78]. The high energy demands of the brain—consuming approximately 20% of the body's metabolic energy despite comprising only 2% of its mass—necessitate efficient transport systems for nutrients and waste removal, processes that can only be fully studied in living organisms [78]. The complexity of these investigations requires sophisticated imaging technologies and carefully designed experimental models that can capture the dynamic interactions within the brain's unique microenvironment while acknowledging the substantial costs and logistical challenges involved in such research.
Technical Complexities of In Vivo Neuroscience Models
Imaging Methodologies and Technical Challenges
Advanced optical imaging technologies form the cornerstone of modern in vivo neuroscience research, enabling high-resolution investigation of cerebral microvascular architecture, blood flow, and oxygenation [79]. Two-photon microscopy (TPM) has emerged as the gold standard for in vivo imaging in highly scattering tissues such as the brain, though its optimal implementation requires careful consideration of multiple technical factors [78]. The challenges of in vivo brain imaging include overcoming light scattering in turbid brain tissue, compensating for motion blur from both tracer diffusion and natural movement of cerebral vasculature, and managing the statistical analysis of noisy images that typically occur due to low-photon budgets or the need for fast image recording [78].
For imaging modalities to yield valuable data for neuroscience, they must meet several critical requirements: (i) capability to image several hundred micrometers into tissue to map three-dimensional microvascular structures across substantial cortical areas; (ii) high spatial resolution sufficient to resolve individual capillaries; (iii) capacity to estimate blood flow rates in individual microvessels; (iv) ability to estimate spatially resolved oxygen levels in microvessels and/or surrounding tissue; and (v) for neurovascular coupling studies, high temporal resolution (~1 second) to resolve hemodynamic changes [79].
Table 1: Comparison of Biodistribution Measurement Techniques for In Vivo Studies
| Method | Principle | Quantitative Capability | Sensitivity | Key Applications |
|---|---|---|---|---|
| ICP-OES | Elemental analysis of inorganic materials | Direct quantitative measurement (%ID/g) | High for specific elements | Porous silicon particle biodistribution [80] |
| IVIS | Fluorescence detection in near-infrared range | Qualitative to semi-quantitative | Limited by tissue attenuation | Iron-oxide nanoparticle localization, polymeric micelle distribution [80] |
| Confocal Microscopy | Optical sectioning of fluorescent samples | Qualitative spatial distribution | High spatial resolution | Cellular localization, particle co-localization with immune cells [80] |
| Fluorescence Homogenization | Fluorescence measurement in tissue homogenates | Quantitative with proper calibration | Moderate when attenuation eliminated | Organ-level biodistribution studies [80] |
| Radiolabeling | Radioactive isotope detection | Quantitative (%ID/g and %ID/organ) | Very high (gold standard) | Pharmacokinetic studies, particle clearance [80] |
Methodological Optimization for Accurate Data Acquisition
The spatial resolution in optical microscopy is fundamentally limited by the point-spread function (PSF), which defines the excitation volume within which fluorescence is generated [78]. For TPM, the PSF extends approximately one micrometer along the z-axis, which can limit the ability to distinguish finely spaced structures such as individual channels of the brain's extracellular space [78]. Proper characterization of the PSF is essential not only for defining optical resolution but also for predicting how specific geometrical structures will appear in recorded images, enabling more accurate interpretation of experimental data.
Practical strategies to mitigate motion artifacts include: optimizing temporal resolution based on the diffusion coefficient of tracers and natural movement of cerebral vasculature; implementing motion compensation algorithms; and employing statistical approaches designed to analyze noisy images characteristic of in vivo imaging conditions [78]. For studies of molecular transport in the brain extracellular space, integrative optical imaging (IOI) provides a valuable approach, though it relies on assumptions of molecular conservation during diffusion and homogeneous, isotropic brain tissue properties [78].
Quantitative Research Designs for In Vivo Studies
Hierarchy of Evidence and Experimental Designs
Quantitative research designs in in vivo research follow a hierarchy of evidence, with descriptive observational studies forming the foundation and randomized controlled trials representing the gold standard for establishing causal relationships [81]. The selection of appropriate research design depends on the research question, feasibility, ethical considerations, and the current state of knowledge in the field.
Table 2: Quantitative Research Designs for Preclinical and Clinical Research
| Research Design | Key Features | Strength of Evidence | Applications in In Vivo Research |
|---|---|---|---|
| Cross-Sectional | Data collected at single time point; "snapshot" of population | Low (identifies associations only) | Prevalence studies, initial biomarker characterization [81] |
| Case-Control | Compares cases with outcome to controls without; retrospective | Moderate (identifies risk factors) | Investigation of rare diseases, genetic factors [81] |
| Cohort | Follows groups over time; prospective or retrospective | Moderate-High (establishes temporal sequence) | Disease progression studies, natural history [82] |
| Quasi-Experimental | Intervention without random assignment | Moderate (suggests causality) | Preliminary efficacy studies, feasibility trials [81] |
| Randomized Controlled Trial (RCT) | Random assignment to intervention/control groups | High (establishes causality) | Gold standard for efficacy evaluation, registration trials [81] |
True experimental designs require several key elements: random assignment of participants to experimental and control groups, manipulation of an independent variable (the intervention), and strict control of all other variables to establish cause-effect relationships [83]. In contrast, quasi-experimental designs forfeit elements such as random assignment or control groups while still testing interventions, making them suitable for natural settings where full experimental control is impractical [83].
Ensuring Validity in Research Findings
The quality of a study's findings is determined by factors affecting its internal validity, while its application to other settings is gauged by its external validity [81]. Internal validity refers to the extent to which results are trustworthy and free from biases, accurately establishing cause-and-effect relationships between independent and dependent variables [81]. Common threats to internal validity include history (external events affecting the study), instrumentation changes, selection bias, attrition, testing effects, and natural maturation of participants over time [81].
External validity encompasses both population validity (generalizability to wider populations based on sample representativeness) and ecological validity (applicability to real-world settings beyond controlled laboratory environments) [81]. Maximizing both internal and external validity presents challenges, as overly controlled studies may undermine applicability to real-world settings, while insufficiently controlled studies may produce questionable causal findings [81].
Cost Analysis and Economic Considerations
Financial Dimensions of Drug Development
The development of new therapeutic agents involves substantial financial investment, with costs varying significantly by therapeutic area and development approach. Antimicrobial drug development serves as an informative comparator, with estimated capitalized costs accounting for failures and cost of capital reaching approximately $1.9 billion for drugs targeting multidrug-resistant pathogens [84]. This figure is comparable to the average cost of drug development across all therapeutic areas ($1.8 billion) but less than half the cost of developing oncology drugs ($4.5 billion) [84].
Breaking down development costs by phase provides greater transparency: Phase 1 trials represent an average out-of-pocket cost of $19.4 million, Phase 2 trials $71.5 million, and Phase 3 trials $237.4 million, with additional post-launch study costs of approximately $48.4 million [84]. Alternative estimates suggest slightly lower figures, with cash outlay for anti-infective agents at $0.4 billion and expected capitalized development costs at $1.3 billion [84]. Economic barriers, high costs, and low return on investment were cited by 80-84% of pharmaceutical companies as primary reasons for suspending antimicrobial clinical trial development [84].
Table 3: Clinical Trial Cost Components and Economic Challenges
| Cost Component | Typical Range | Factors Influencing Cost | Cost Reduction Strategies |
|---|---|---|---|
| Preclinical Research | $2 million+ | Compound screening, toxicity studies | High-throughput screening, in silico modeling |
| Phase 1 Trials | $12-19.4 million | Healthy volunteer recruitment, safety monitoring | Adaptive designs, optimized participant compensation |
| Phase 2 Trials | $7.5-71.5 million | Patient recruitment, dose-finding | Biomarker enrichment, precision medicine approaches |
| Phase 3 Trials | $35-237.4 million | Large sample sizes, multicenter operations | Noninferiority designs, surrogate endpoints, operational efficiency |
| Staff & Facilities | $250 million+ | Specialized personnel, regulatory compliance | Public-private partnerships, academic collaborations |
| Post-Marketing Studies | $48.4 million+ | Risk evaluation, additional indications | Integrated research programs, real-world evidence generation |
Cost-Benefit Analysis of Advanced Technologies
The integration of advanced diagnostic technologies can yield substantial economic benefits in medical research and clinical practice. In melanoma diagnosis, the adjunctive use of reflectance confocal microscopy (RCM) demonstrated a cost-benefit ratio of 3.89, meaning that for every €1 spent on RCM, there was a benefit of €3.89 [85]. This was achieved primarily through a 43.3% reduction in the number of unnecessary excisions while maintaining diagnostic sensitivity [85].
The cost per patient for standard care without RCM was €143.63, compared to €114.74 with adjunctive RCM, while the cost per melanoma excised with standard care (NNE 5.3) was €904.87, nearly double the cost for RCM (€458.96) [85]. Extrapolated to national healthcare systems, the estimated annual savings with adjunctive RCM were €425,844.05 regionally and €5,663,057.00 nationally in the Italian healthcare system [85]. These findings highlight how technological advancements that improve diagnostic accuracy can simultaneously address both complexity and cost challenges in medical research and practice.
Experimental Protocols and Methodologies
In Vivo Biodistribution Assessment Protocol
Accurate determination of in vivo biodistribution represents a critical step in evaluating the performance of inorganic particles for biomedical applications [80]. The following protocol outlines a systematic approach for comparing biodistribution measurement techniques:
Particle Preparation: Select appropriate particles (e.g., porous silicon particles) fabricated conforming to FDA cGMP regulations. Functionalize particles with APTES prior to injection to enhance loading capacity and facilitate conjugation [80].
Fluorescent and Radioactive Labeling: Employ established labeling protocols with high stability and reproducibility. For fluorescence methods, use near-infrared dyes (600-1000 nm) to minimize attenuation by biological tissue absorption [80].
Animal Administration: Administer particles via appropriate routes (intravenous or retro-orbital injection) using optimized dosing regimens based on previous safety studies [80].
Tissue Collection and Processing: At predetermined timepoints, collect all major organs (liver, spleen, lungs, kidneys, heart, brain). Divide each organ for analysis by different techniques to enable direct comparison [80].
Parallel Measurement: Analyze tissue samples using multiple complementary techniques: ICP-OES for direct elemental quantification, IVIS for whole-organ fluorescence imaging, confocal microscopy for cellular localization, fluorescence measurement of homogenized organs, and radiolabeling with gamma counting as a gold standard [80].
Data Analysis and Validation: Express results in terms of % injected dose per gram of tissue (%ID/g) and % injected dose per organ (%ID/organ) when possible. Compare methods in terms of absolute results, sensitivity (σ%), and practical considerations [80].
Cerebral Oxygen Transport Modeling Workflow
Network-level modeling of cerebral oxygen transport integrates in vivo microscopic imaging data with computational approaches to predict physiologically relevant properties [79]. The experimental workflow encompasses:
Diagram 1: Oxygen transport modeling workflow.
In Vivo Microscopic Imaging: Utilize high-spatial resolution optical imaging technologies (two-photon microscopy) capable of penetrating up to 1 mm into brain tissue to capture: (i) three-dimensional microvascular network structure; (ii) blood flow velocities in individual vessels; and (iii) oxygen levels in microvessels using phosphorescence quenching microscopy or other oxygen-sensitive techniques [79].
Data Extraction and Network Reconstruction: Extract quantitative data on vessel diameters, lengths, connectivity, and topological parameters. Reconstruct the complete three-dimensional microvascular network, typically containing hundreds to thousands of segments, representing a substantial fraction of the cortical thickness [79].
Blood Flow Modeling: Apply theoretical methods to compute blood flow distribution throughout the network based on vessel architecture and assumed flow resistance relationships. Account for the heterogeneity of structural and hemodynamic parameters in the microcirculation, which significantly impacts oxygen transport efficiency [79].
Oxygen Transport Simulation: Implement computational models that incorporate the convection of oxygen in blood, diffusion of oxygen from vessels to tissue, and oxygen consumption by the tissue. These "bottom-up" models generate spatially resolved predictions of oxygen distribution throughout the tissue volume [79].
Model Validation and Refinement: Compare model predictions with direct measurements of tissue oxygenation where available. Refine model parameters to improve agreement with experimental data, enhancing the predictive capability for investigating normal and disease states [79].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for In Vivo Neuroscience
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Porous Silicon Particles | Injectable delivery vector | Controllable design, biocompatibility, favorable degradation kinetics; size >20 nm accumulates in liver, spleen, lungs [80] |
| APTES Functionalization | Surface modification | Enhances loading/conjugation capacity; facilitates particle degradation/clearance; enables stable fluorescent/radioactive labeling [80] |
| Near-Infrared Fluorescent Dyes | Optical contrast agents | Emission 600-1000 nm minimizes tissue attenuation; enables IVIS, confocal imaging [80] |
| Radioactive Isotopes | Radiolabeling for biodistribution | High sensitivity detection; gold standard for quantitative biodistribution (%ID/g) [80] |
| Oxygen-Sensitive Probes | Tissue oxygenation measurement | Phosphorescence quenching microscopy; enables mapping of oxygen gradients in microvasculature [79] |
| Two-Photon Microscopy Tracers | In vivo imaging contrast | Fluorescent molecules for studying molecular transport in brain ECS, perivascular spaces [78] |
Integrated Logistics Management Framework
Diagram 2: Logistics management framework.
Successfully addressing the complexity and cost challenges in in vivo models and clinical trials requires an integrated framework that aligns technical capabilities with methodological rigor and economic sustainability. This framework encompasses: (1) strategic selection of imaging and measurement technologies balanced against capability requirements and operational constraints; (2) implementation of appropriate research designs that maximize validity while acknowledging practical limitations; (3) comprehensive economic analysis that considers both direct costs and long-term benefits of technological investments; and (4) development of standardized protocols that ensure reproducibility while allowing sufficient flexibility for adaptation to specific research contexts.
The interdependence of these elements necessitates careful planning and continuous evaluation throughout the research lifecycle. By applying this integrated framework, researchers can optimize the logistics of in vivo studies to maximize scientific output while responsibly managing the substantial resources required for such investigations. This approach ultimately enhances the translation of findings from basic neuroscience research to clinical applications that address pressing neurological disorders.
The development of effective therapeutics for neurological disorders represents one of the most challenging frontiers in modern medicine. A significant barrier to progress lies in the inconsistent definition and application of clinical endpoints across trials, which complicates the interpretation of results and hinders the reliable assessment of therapeutic efficacy. The National Institutes of Health Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative has identified this challenge, emphasizing the need to "develop innovative technologies to understand the human brain and treat its disorders" and to "create and support integrated human brain research networks" [33]. This technical guide examines the critical role of standardized clinical endpoints within the broader context of advancing in vivo neuroscience research techniques, providing a framework for researchers and drug development professionals to enhance the validity, reliability, and comparability of neurological trials.
The evolution of in vivo techniques, particularly high-resolution functional mapping and large-scale neural recording technologies, has created unprecedented opportunities to redefine clinical endpoints based on direct measures of neural circuit function [86] [33]. These technological advances coincide with growing recognition of the "curse of dimensionality" in neuroscience data visualization, where complex multivariate datasets require careful standardization to ensure clear interpretation and avoid misleading conclusions [87]. By establishing rigorous, biologically grounded endpoints, the neuroscience community can accelerate the translation of basic research findings into meaningful clinical applications.
Current Landscape and Challenges in Neurological Endpoints
The standardization of clinical endpoints in neurological trials faces multiple interconnected challenges that stem from both the complexity of the nervous system and methodological limitations in current assessment approaches.
Heterogeneity in Endpoint Measurement
Neurological clinical trials frequently employ disparate assessment tools and measurement techniques across studies, even when investigating similar conditions. This heterogeneity significantly complicates cross-trial comparisons and meta-analyses. A comprehensive survey of neuroscience literature revealed that fundamental elements of data presentation are often inadequately reported, with only 43% of 3D graphical displays properly labeling dependent variables and a mere 20% portraying the uncertainty of reported effects [87]. This lack of transparency in data reporting extends to clinical endpoint specification, where the precise definition of what is being measured and how it is quantified is frequently ambiguous.
The Dimensionality Problem in Neural Data
Modern neuroscience increasingly generates high-dimensional datasets that capture neural activity across multiple spatial and temporal scales. As noted in visualization research, "as datasets become more complex, displays should become increasingly informative, elucidating relationships that would be inaccessible from tables or summary statistics" [87]. However, the field often struggles with the opposite phenomenon: as data dimensionality increases, the clarity of reporting frequently decreases. This challenge is particularly acute for clinical endpoints derived from techniques such as large-scale electrophysiology or functional neuroimaging, where the relationship between raw data and clinically meaningful endpoints may involve complex analytical transformations that are poorly standardized across research groups.
In Vivo Techniques Informing Endpoint Development
Recent advances in in vivo neuroscience techniques provide unprecedented opportunities to develop clinical endpoints that are directly grounded in neural circuit function. These technologies enable researchers to move beyond symptomatic assessments to measures that reflect the underlying biological state of the nervous system.
High-Throughput Synaptic Connectivity Mapping
A groundbreaking approach published in Nature Neuroscience demonstrates the potential for high-throughput mapping of synaptic connectivity in living neural circuits [86]. This method combines two-photon holographic optogenetic stimulation of presynaptic neurons with whole-cell recordings of postsynaptic responses, enabling researchers to rapidly probe connectivity across up to 100 potential presynaptic cells within approximately five minutes in the visual cortex of anesthetized mice [86]. The technical specifications for this approach are detailed in Table 1.
Table 1: Technical Specifications for High-Throughput Synaptic Connectivity Mapping
| Parameter | Specification | Experimental Relevance |
|---|---|---|
| Stimulation Method | Two-photon holographic optogenetics | Enables precise activation of individual presynaptic neurons with minimal crosstalk |
| Recording Method | Whole-cell patch clamp | Provides direct measurement of postsynaptic responses with high signal-to-noise ratio |
| Presynaptic Neurons Probable per Session | Up to 100 cells | Increases mapping throughput by an order of magnitude compared to conventional methods |
| Time Required for Connectivity Scan | ~5 minutes | Enables rapid assessment of circuit connectivity within stable recording periods |
| Spatial Resolution | 12 µm temporally focused spots | Allows precise targeting of individual neurons within dense tissue |
| Temporal Precision | Sub-millisecond jitter in AP generation | Essential for correlating presynaptic activation with postsynaptic responses |
| Key Innovation | Compressive sensing reconstruction | Reduces required measurements threefold in sparsely connected populations |
This methodology represents a significant advance over previous approaches, which were limited to investigating connectivity among only a handful of neurons (maximum of 12 neurons in vitro) and characterized with low yield (~0.3 connections probed per mouse) in vivo [86]. The ability to rapidly characterize synaptic connectivity patterns in living organisms provides a potential framework for developing endpoints that directly reflect circuit-level dysfunction in neurological disorders.
Large-Scale Neural Population Recording
Complementing approaches that map anatomical connectivity, methods for large-scale recording of neural population activity offer insights into the dynamic functional properties of neural circuits. The BRAIN Initiative has emphasized the importance of producing "a dynamic picture of the functioning brain by developing and applying improved methods for large-scale monitoring of neural activity" [33]. These technologies include high-density electrophysiology, calcium imaging, and functional magnetic resonance imaging, each providing distinct insights into neural circuit function at different spatial and temporal scales.
The value of standardized data collection is exemplified by projects such as the "complete Liverpool SPN catalogue," which compiled 6,674 individual recordings of the sustained posterior negativity (SPN) brain response from 2,215 participants [88]. This comprehensive dataset enabled researchers to establish quantitative relationships between stimulus properties (such as visual symmetry) and neural response amplitudes, demonstrating that "SPN amplitude scales parametrically with the proportion of symmetry in the image" [88]. Such large-scale, standardized datasets provide robust normative references against which pathological neural responses can be compared, potentially serving as sensitive endpoints for detecting circuit dysfunction in neurological disorders.
Framework for Standardizing Clinical Endpoints
The development of standardized clinical endpoints for neurological trials requires a systematic approach that integrates technological capabilities with clinical relevance. The following framework provides guidance for endpoint selection and validation.
Hierarchical Endpoint Classification
Clinical endpoints for neurological trials should be conceptualized within a hierarchical framework that spans different levels of biological organization, from molecular through circuit to behavioral processes. The BRAIN Initiative has advocated for approaches that "integrate spatial and temporal scales," recognizing that "the nervous system consists of interacting molecules, cells, and circuits across the entire body, and important functions can occur in milliseconds or minutes, or take a lifetime" [33]. This perspective suggests that comprehensive assessment of therapeutic efficacy may require multiple endpoints capturing different aspects of neural function.
Methodological Standardization
Standardization of experimental protocols is essential for ensuring the reliability and comparability of endpoints across different research sites and studies. Detailed methodology reporting should include not only the parameters of data acquisition but also the complete data processing pipeline. The Liverpool SPN catalogue exemplifies this approach by providing "uniform data files from five subsequent stages of the pipeline: (i) raw BDF files; (ii) epoched data before ICA pruning; (iii) epoched data after ICA pruning; (iv) epoched data after ICA pruning and trial rejection; (v) pre-processed data averaged across trials for each participant and condition" [88]. This level of methodological transparency enables direct comparison of results across studies and facilitates the identification of sources of variability in endpoint measurement.
Table 2: Essential Research Reagents and Tools for Neural Circuit Mapping
| Tool Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| Optogenetic Actuators | ST-ChroME (soma-targeted opsin) | Encomes precise light-sensitive ion channels for controlled neuronal depolarization |
| Neural Activity Reporters | Genetically encoded calcium indicators (e.g., GCaMP), voltage-sensitive dyes | Provides optical readout of neural activity with cellular resolution |
| Holographic Stimulation Systems | Spatial light modulator (SLM), temporally focused two-photon excitation | Enables simultaneous photostimulation of multiple precisely defined neurons |
| Data Acquisition Systems | Whole-cell patch clamp rig, high-density electrophysiology systems | Records postsynaptic responses with high temporal resolution and sensitivity |
| Analytical Frameworks | Compressive sensing reconstruction, common data models | Reduces data dimensionality while preserving essential connectivity information |
Experimental Protocols for Endpoint Validation
The validation of novel clinical endpoints requires rigorous experimental approaches that establish their reliability, sensitivity, and clinical relevance. The following protocols provide templates for assessing the properties of potential endpoints.
Protocol for Synaptic Connectivity Assessment
The high-throughput synaptic connectivity mapping approach described by [86] provides a robust protocol for quantifying circuit-level dysfunction in disease models:
- Animal Preparation: Utilize transgenic mice expressing the fast, soma-restricted opsin ST-ChroME in defined neuronal populations.
- Optical System Configuration: Employ a custom-built system incorporating both two-photon imaging and holographic stimulation paths, using two-step phase modulation to generate 12 µm temporally focused spots.
- Stimulation Parameters: Apply photostimulation with power densities of 0.15–0.3 mW µm−2 and duration of 10 ms, parameters that yield action potential latency of 5.09 ± 0.38 ms, jitter of 0.99 ± 0.14 ms, and AP probability of 81.13 ± 5.34%.
- Recording Conditions: Maintain whole-cell recordings in voltage-clamp mode to detect postsynaptic currents resulting from presynaptic activation.
- Sampling Strategy: For densely connected populations, use sequential single-cell stimulation; for sparsely connected populations, employ multi-cell stimulation combined with compressive sensing reconstruction to improve sampling efficiency.
- Data Analysis: Identify connected pairs based on short-latency postsynaptic responses time-locked to presynaptic stimulation, quantifying both connection probability and synaptic strength.
This protocol enables the quantitative assessment of circuit connectivity alterations in disease models, providing a potential endpoint for evaluating therapeutics targeting synaptic dysfunction.
Protocol for Large-Scale Neural Response Characterization
The approach used to create the Liverpool SPN catalogue [88] provides a template for standardizing the assessment of evoked neural responses:
- Stimulus Presentation: Control visual stimulus parameters precisely, with presentation durations of at least one second to allow full development of sustained neural responses.
- Task Conditions: Systematically vary task demands, including active regularity discrimination versus task-irrelevant symmetry perception, to dissociate automatic from attention-modulated neural responses.
- Data Acquisition: Follow standardized electrophysiology recording protocols with consistent electrode placement and referencing.
- Signal Processing: Apply consistent preprocessing pipelines including filtering, artifact rejection, and independent components analysis to remove ocular and muscle artifacts.
- Response Quantification: Measure response amplitude in consistent time windows relative to stimulus onset, with explicit documentation of electrode sites and quantification methods.
- Data Sharing: Format data according to Brain Imaging Data Structure (BIDS) standards to enable cross-laboratory comparison and meta-analysis.
This systematic approach to neural response characterization facilitates the development of standardized endpoints that can be deployed across multiple research sites.
Data Visualization and Interpretation Standards
Effective standardization of clinical endpoints requires clear guidelines for data visualization and interpretation to minimize ambiguity and prevent misinterpretation.
Visualization Best Practices
Comprehensive surveys of neuroscience literature have identified common deficiencies in data presentation that can compromise the interpretation of clinical endpoints [87]. To address these limitations:
- Uncertainty Portrayal: Always include measures of uncertainty (e.g., confidence intervals, prediction intervals) appropriate to the study design and clearly define their meaning in figure legends.
- Color Mapping: Use color schemes that are perceptually uniform and accessible to individuals with color vision deficiencies, avoiding red-green contrasts and providing alternative coding methods when necessary.
- Axis Labeling: Clearly label all axes with the variable being displayed and its units of measurement, explicitly indicating whether scales are linear, logarithmic, or radial.
- Data Density Optimization: Choose visualization formats that maximize data density while maintaining clarity, such as violin plots that display full distributional information rather than bar plots that show only summary statistics.
Adherence to these visualization standards ensures that clinical endpoint data is presented in a manner that supports accurate interpretation and cross-study comparison.
Statistical Reporting Requirements
Complete statistical reporting is essential for evaluating the reliability of clinical endpoint measurements. This includes:
- Explicit Description of Statistical Procedures: Clearly identify all statistical tests used, their parameters, and any corrections for multiple comparisons.
- Sample Size Indication: Report the number of independent samples (e.g., subjects, neurons, connections) underlying each measurement.
- Effect Size Estimation: Provide quantitative estimates of effect sizes along with measures of statistical significance to facilitate power calculations for future studies.
- Model Assumption Verification: Document verification of statistical model assumptions, particularly for parametric procedures applied to neural data that may violate normality requirements.
These reporting standards align with the broader goal of enhancing the reproducibility and interpretability of neuroscience research [87] [88].
Implementation and Future Directions
The successful implementation of standardized clinical endpoints for neurological trials requires coordinated effort across multiple stakeholders in the research community. Several strategic initiatives can facilitate this process.
Data Sharing and Common Data Models
The establishment of "public, integrated repositories for datasets and data analysis tools, with an emphasis on ready accessibility and effective central maintenance" will have immense value for endpoint standardization [33]. The Common Data Model (CDM) proposed for neuroscience data provides a framework for federating disparate information resources through a structured set of superclasses—data, site, method, model, and reference—with relations defined between them [89]. Adoption of such common data models facilitates the pooling of data across studies to establish normative ranges for clinical endpoints and quantify their sensitivity to disease-related perturbations.
Technology Development and Validation
The BRAIN Initiative has emphasized that "new methods should be critically tested through iterative interaction between tool-makers and experimentalists" and that "after validation, mechanisms must be developed to make new tools available to all" [33]. This technology development cycle is essential for evolving clinical endpoints as new measurement techniques emerge. Particularly promising are approaches that "integrate new technological and conceptual approaches to discover how dynamic patterns of neural activity are transformed into cognition, emotion, perception, and action in health and disease" [33], as these integrated perspectives will enable the development of endpoints that more comprehensively capture the multi-level nature of neurological dysfunction.
The following workflow diagram illustrates the integrated experimental approach for standardizing clinical endpoints using in vivo techniques:
Integrated Workflow for Clinical Endpoint Development
The standardization of clinical endpoints for neurological trials represents a critical challenge with profound implications for the development of effective therapeutics. By leveraging advances in in vivo neuroscience techniques, particularly high-resolution circuit mapping and large-scale neural population recording, researchers can develop endpoints that are directly grounded in the biological mechanisms of neurological diseases. The frameworks, protocols, and standards outlined in this technical guide provide a roadmap for enhancing the validity and reliability of these endpoints, ultimately accelerating the translation of basic neuroscience discoveries into meaningful clinical applications. As the BRAIN Initiative has envisioned, the integration of new technological and conceptual approaches will enable a "comprehensive, mechanistic understanding of mental function" that transforms our approach to neurological drug development [33].
Within the context of in vivo techniques for neuroscience research, the selection of appropriate animal models is a cornerstone of experimental design. However, a critical variable often overlooked is the age and physiological maturity of the experimental subjects [90]. Much like the absurdity of conducting clinical trials for an adult drug exclusively in children, using animal models with brains that have not fully developed to study adult neurological function or age-related diseases presents a significant threat to model validity and translational outcomes [90]. This guide examines the profound impact of animal age and physiology on research findings, providing neuroscientists and drug development professionals with the frameworks and methodologies necessary to enhance the rigor and predictive power of their in vivo studies. Ignoring developmental stage can lead to data that is not only non-representative but also misleading, costing valuable time and resources in the quest to understand brain function and develop new therapies [91] [90].
The Prevalence of the Problem: A Systematic Look at Age Bias
Empirical evidence reveals a substantial bias towards the use of young animals in neuroscience research, particularly in specific experimental domains. A systematic review of hippocampal long-term potentiation (LTP) studies illustrates this point clearly, demonstrating a dominant reliance on immature models in ex vivo slice physiology [90].
Table 1: Use of Animal Ages in Neuroscience Research Domains
| Research Domain | Young Animals | Adult Animals | Age Not Specified |
|---|---|---|---|
| LTP: Ex Vivo (Voltage/Current Clamp) | 75% | 20% | 5% |
| LTP: Ex Vivo (Field Recordings) | 55% | 38% | 7% |
| LTP: In Vivo | 26% | 65% | 9% |
| Morris Water Maze (Behavior) | 17% | 77% | 5% |
Data derived from a systematic literature review [90].
This bias is frequently compounded by mislabeling, with approximately 42% of studies incorrectly defining young animals as "adults" [90]. The rationale for using young animals, especially in slice electrophysiology, often includes practical considerations such as improved cell visibility due to less advanced myelination [90]. However, this convenience comes at a high cost: the scarcity of studies in adult animals creates a significant disconnect, making it difficult to extrapolate findings from reductionist ex vivo work to in vivo physiology and behavior [90]. This gap fundamentally undermines the goal of a cohesive neuroscience research pipeline.
Defining Developmental Stages in Rodent Models
Accurate experimental design requires a precise understanding of animal development. Rats and mice, the most common models in neuroscience, share a similar developmental profile, yet many researchers erroneously consider a weaned animal to be an adult [90].
Table 2: Developmental Stages of the Laboratory Rat
| Developmental Stage | Approximate Age Range | Key Physiological Markers |
|---|---|---|
| Pre-weaning | Postnatal Day 0 (P0) - P21 | Dependent on dam; rapid initial growth. |
| Juvenile | P21 - ~P32 (females) / ~P45 (males) | Weaning; pre-pubertal. |
| Adolescence | ~P32 - ~P63 | Sexual maturity (vaginal opening in females, balano-preputial separation in males); characterized by risk-taking and social play. |
| Young Adult | >P63 | Transition to adulthood; brain maturation continues. |
| Adult | >P90 | Fully mature; ideal for modeling adult human conditions. |
| Aged | >P540 (18+ months) | Onset of age-related physiological and neural decline. |
Developmental timeline synthesized from neurobiological literature [90].
A critical mistake is using body weight as a surrogate for age. Data from major vendors and institutional colonies show that a male Sprague Dawley rat weighing 250-274g can be anywhere from 57 to 70 days old, depending on the source [90]. This variability is substantial enough to place animals in entirely different developmental categories, introducing a significant, unaccounted-for variable into experimental data.
Developmental Workflow in Research Models
The following diagram outlines key developmental stages and research considerations for rodent models in neuroscience:
Physiological and Mechanistic Consequences of Age
Brain development is an ongoing process that continues well beyond puberty, involving both quantitative changes and qualitative shifts in underlying mechanisms [90].
Quantitative Developmental Changes
These involve gradual changes, rapid switches, or inverted U-shaped curves in physiological processes. For example, the expression and subunit composition of neurotransmitter receptors, such as GABA-A and NMDA receptors, evolve significantly during early postnatal development and into adolescence, directly impacting neuronal excitability and synaptic plasticity [90]. These maturational changes mean that a pharmacological agent targeting a specific receptor may have profoundly different effects in an adolescent animal compared to an adult.
Qualitative Mechanistic Shifts
Perhaps more critically, some phenomena that appear unitary are governed by different mechanisms at different ages. A notable example is in the dopaminergic system. The regulation of prefrontal cortical dopamine shifts from being primarily dependent on the dopamine D2 receptor in juvenile rats to relying on the D1 receptor in adults [90]. This fundamental switch has staggering implications for research into psychiatric disorders like schizophrenia and for the development of psychotropic drugs, as a compound designed to modulate D2 receptors may appear ineffective if tested only in adult models, despite being critical during earlier developmental windows.
Methodologies for Age-Appropriate Experimental Design
Ensuring model validity requires integrating age as a core component of the experimental hypothesis and design.
Formulating an Age-Conscious Hypothesis
A strong hypothesis explicitly considers age as a variable. Rather than a generic question like "How does drug X affect memory?", an age-conscious hypothesis would be: "Chronic administration of drug X from P60 to P90 improves spatial memory retention in the Morris water maze in a model of early-stage neurodegeneration" [90] [92]. This specifies the independent variable (drug X administration), the dependent variable (memory retention), and the critical age variable (young adult, P60-P90), creating a testable framework with direct relevance to an adult human condition [92].
Determining Sample Groups and Frequency
Beyond standard demographic controls, subject groups must be defined by precise, narrow age windows that align with the research question [90] [92]. Studying adolescence? A range of P35-P40 is more appropriate than P30-P50. Studying aging? Animals should be definitively aged (e.g., >18 months) rather than simply "retired breeders" of variable age. Sampling frequency must also be developmentally informed; a study on adolescent development may require weekly behavioral tests, while a neurodegenerative study in adults might track progression monthly [92].
Incorporating Naturalistic Behavioral Analysis
Modern unsupervised computational methods for quantifying naturalistic behavior provide powerful tools for capturing subtle, age-related behavioral phenotypes that may be missed by constrained tasks [93]. Techniques like DeepLabCut for markerless pose estimation, coupled with machine learning models such as Hidden Markov Models (HMMs) or variational autoencoders (VAEs), can identify discrete, stereotyped behaviors and model the structure of behavioral sequences across different ages [93]. This data-driven approach minimizes human bias and can reveal robust behavioral biomarkers of development, aging, or disease progression.
The Scientist's Toolkit: Essential Reagents and Materials
Selecting the right tools is paramount for conducting rigorous, age-informed neuroscience research.
Table 3: Key Research Reagent Solutions for Age-Focused Neuroscience
| Item / Reagent | Function in Research | Application Note |
|---|---|---|
| Postnatal Rodents (P0-P21) | Model of neurodevelopment, synaptogenesis, and early-life insults. | Critical for studies of developmental plasticity; not suitable for modeling adult function. |
| Young Adult Rodents (P60-P90) | Model of fully matured adult brain function and early-stage disease processes. | The minimum recommended age for studies relevant to the adult human brain. |
| Aged Rodents (>18 months) | Model of age-related cognitive decline, neurodegeneration, and brain aging. | Essential for translational research on Alzheimer's, Parkinson's, and other aging-related diseases. |
| Unsupervised Behavioral Tracking Software | Automated, high-throughput quantification of naturalistic behavior from video. | Captures subtle age-specific behavioral motifs and dynamics beyond simple locomotion [93]. |
| Induced Pluripotent Stem Cells (iPSCs) | Generation of patient-specific neuronal cells; can be aged in culture. | An in vitro alternative for studying cellular aging mechanisms, though lacks circuit-level complexity [91]. |
| Microphysiological Systems (Organs-on-Chips) | 3D in vitro models that can mimic tissue- and organ-level physiology. | Emerging tool for modeling human biology; potential to incorporate aged cell lines [91]. |
Beyond Rodents: The Strength of Diversity in Model Systems
While this guide focuses on age, the principle of model validity extends to the choice of species. An over-reliance on a few inbred, laboratory-reared rodent strains limits the scope of neuroscience and fails to capture the evolutionary adaptations of nervous systems [94]. Exploring a rich diversity of animal model systems is fundamental to discovering evolutionarily conserved core mechanisms.
Songbirds provide exquisite models for vocal learning, foraging bats reveal complex three-dimensional spatial navigation algorithms, and the turtle's hypoxia-resistant nervous system allows for detailed ex vivo analysis of learning circuits [94]. Furthermore, core molecular mechanisms, such as CREB-dependent transcription and learning-related epigenetic modifications, are highly conserved from invertebrates to humans [94]. Research on diverse phyla helps distinguish general computational principles of neural circuits from species-specific specializations, ultimately strengthening the biological foundation of neuroscience.
Model Selection and Validation Workflow
The following diagram illustrates a strategic workflow for selecting and validating animal models in neuroscience research:
The age and physiology of an animal model are not mere methodological details; they are foundational to the validity and translational potential of neuroscience research. By systematically incorporating precise age considerations into experimental design—from hypothesis generation and model selection to behavioral analysis and data interpretation—neuroscientists can significantly enhance the rigor and relevance of their work. Moving beyond the convenience of young models and embracing both the complexity of development and the strength of diverse species will be crucial for unraveling the mysteries of the brain and developing effective treatments for neurological and psychiatric disorders.
Mitigating Off-Target Effects and Ensuring Specificity in Complex Environments
The pursuit of precise therapeutic intervention in neuroscience research faces a significant challenge: the inherent risk of off-target effects in complex biological systems. As molecular tools become increasingly sophisticated for investigating and treating neurological disorders, ensuring their specificity within the intricate environment of the living brain is paramount. Off-target effects—unintended interactions with non-target molecules, cells, or tissues—can compromise experimental validity, lead to misinterpretation of results, and pose substantial safety risks in therapeutic development [95] [96]. This technical guide provides an in-depth examination of the sources of off-target activity across key biotechnology platforms and presents a comprehensive framework of advanced strategies for their mitigation in preclinical neuroscience research.
The challenge is particularly acute for in vivo neuroscience applications, where delivery across the blood-brain barrier, cellular heterogeneity, and interconnected signaling pathways create a uniquely complex environment for achieving specificity. This guide details methodologies spanning from computational design and molecular engineering to sophisticated validation protocols, providing neuroscientists and drug development professionals with a systematic approach for enhancing the precision of their investigative and therapeutic tools.
Off-Target Effects Across Major Modalities
CRISPR-Cas Systems
CRISPR-Cas gene editing has emerged as a powerful tool for investigating gene function and developing therapies for neurological disorders. However, its application is associated with unintended alterations at both on-target and off-target genomic sites. These undesirable effects include small insertions and deletions (indels) and larger structural variations such as translocations, inversions, and large deletions, which present serious concerns for functional studies and therapeutic safety [96].
The primary source of CRISPR off-target activity stems from the tolerance of the Cas nuclease for mismatches between the guide RNA (gRNA) and genomic DNA, particularly in the seed region and when accompanied by microhomology. Furthermore, chromatin accessibility and epigenetic modifications significantly influence off-target susceptibility, creating cell-type-specific risk profiles that are particularly relevant in the heterogeneous cellular environment of the nervous system [96].
Advanced CRISPR Mitigation Strategies
Nuclease Engineering: The development of high-fidelity Cas9 variants represents a cornerstone strategy for reducing off-target effects. Enhanced specificity mutants include:
- Enhanced SpCas9 (eSpCas9): Engineered to reduce non-specific DNA interactions through positive charge neutralization [96].
- High-fidelity SpCas9 (SpCas9-HF1): Contains alterations to residue contacts with the DNA phosphate backbone [96].
- Hyper-accurate Cas9 (HypaCas9): Features mutations that stabilize the proofreading conformation of the REC3 domain [96].
- SuperFi-Cas9: Exhibits dramatically improved discrimination against mismatches, particularly in the PAM-distal region, without compromising on-target activity [96].
Guide RNA Optimization: Strategic modification of gRNAs significantly enhances specificity:
- Truncated gRNAs: Shortening the guide sequence by 2-3 nucleotides from the 5' end increases specificity by reducing binding energy [96].
- Chemical Modifications: Incorporation of 2'-O-methyl-3'-phosphonoacetate, bridged nucleic acids, or locked nucleic acids at specific gRNA positions reduces off-target editing while maintaining on-target efficiency [96].
- Hybrid DNA-RNA Guides: Systematic substitution of RNA nucleotides with DNA in the gRNA spacer region has been shown to dramatically reduce off-target editing while potentially increasing on-target efficiency in vivo [97].
Table 1: High-Fidelity CRISPR-Cas Variants for Neuroscience Research
| Nuclease Variant | Key Mutations | Specificity Improvement | On-Target Efficiency | Primary Applications |
|---|---|---|---|---|
| eSpCas9(1.1) | K848A, K1003A, R1060A | ~10-100-fold reduction | Moderate reduction | Gene knockout, neuronal lineage tracing |
| SpCas9-HF1 | N497A, R661A, Q695A, Q926A | ~10-100-fold reduction | Moderate reduction | Disease modeling in iPSC-derived neurons |
| HypaCas9 | N692A, M694A, Q695A, H698A | ~100-1000-fold reduction | Minimal reduction | Therapeutic gene correction studies |
| SuperFi-Cas9 | R221A, N394A, R661A, Q695A, Q926A | >3,000-fold for some mismatches | Variable by target | High-precision editing in complex genomic regions |
| HiFi Cas9 | R691A | Significant improvement as RNP | Maintained as RNP | Ribonucleoprotein delivery in primary neurons |
Small RNA Therapeutics
Small RNA therapeutics, including small interfering RNAs (siRNAs), microRNAs (miRNAs), and antisense oligonucleotides (ASOs), offer promising avenues for targeting neurological disorders at the post-transcriptional level. However, these molecules are susceptible to hybridization-dependent off-target effects, particularly miRNA-like off-target effects where the therapeutic RNA imperfectly pairs with non-target mRNAs, leading to their unintended degradation or translational repression [95].
The risk is particularly pronounced in neuroscience applications where prolonged exposure is often required, and slight alterations in neuronal gene expression networks can have profound functional consequences. Off-target effects can obscure experimental results in the preclinical phase and contribute to adverse events in therapeutic development [95].
Mitigation Approaches for Small RNAs
Chemical Modification Strategies: Strategic incorporation of chemically modified nucleotides can significantly enhance specificity:
- 2'-O-methyl (2'-O-Me) modifications: Improve nuclease resistance and reduce immune stimulation while modulating binding affinity [95].
- 2'-fluoro (2'-F) modifications: Enhance thermal stability and reduce off-target interactions [95].
- Phosphorothioate (PS) linkages: Improve metabolic stability and tissue distribution while potentially reducing non-specific protein binding [95].
- Locked Nucleic Acids (LNAs) and Bridged Nucleic Acids (BNAs): Dramatically increase binding affinity and specificity, allowing for shorter sequences that maintain potency while reducing off-target potential [95].
Computational Design and AI-Driven Approaches: Advanced bioinformatics pipelines are essential for predicting and minimizing off-target effects:
- Seed region analysis: Identification and modification of sequences with high complementarity to miRNA seed regions [95].
- Genome-wide target prediction: Implementation of algorithms that account for RNA secondary structure, accessibility, and binding energy thresholds [95].
- Network theory applications: Analysis of gene regulatory networks to identify nodes where off-target effects would have disproportionate functional consequences [95].
- Artificial intelligence and machine learning: Neural network models trained on transcriptomic data can predict sequence-specific off-target profiles with increasing accuracy [95].
Table 2: Comparison of Small RNA Chemical Modifications for Neuroscience Applications
| Modification Type | Key Properties | Specificity Impact | Stability Improvement | Delivery Considerations |
|---|---|---|---|---|
| 2'-O-Methyl (2'-O-Me) | Increased nuclease resistance, reduced immunogenicity | Moderate improvement | ~10-100x in serum | Compatible with various nanoparticle formulations |
| 2'-Fluoro (2'-F) | Enhanced binding affinity, metabolic stability | Significant improvement | ~50-200x in serum | Improved tissue distribution across BBB models |
| Phosphorothioate (PS) | Protein binding, improved pharmacokinetics | Can increase non-specific effects if overused | ~5-20x in tissue homogenates | Enhances neuronal uptake; optimize degree of modification |
| Locked Nucleic Acid (LNA) | Extremely high binding affinity, superior specificity | Dramatic improvement with proper design | >100x in biological fluids | Enables shorter sequences; monitor potential toxicity |
| Morpholino | Neutral backbone, nuclease resistance | High specificity due to unique chemistry | Highly stable | Effective in direct CNS applications; challenging delivery |
Targeted Delivery Systems
Achieving specificity through targeted delivery represents a complementary approach to molecular engineering. In vivo biopanning technologies have emerged as powerful methods for identifying ligands that home to specific cell types or tissues within complex biological environments [98]. For neuroscience applications, this approach holds particular promise for developing delivery vehicles that cross the blood-brain barrier and target specific neuronal populations.
In vivo biopanning mimics the natural immune selection process by screening large libraries of potential binding ligands (peptides, antibodies, aptamers) within living organisms, enabling the identification of motifs that specifically accumulate in target tissues despite the immense complexity of the in vivo environment [98]. The success of any biopanning strategy relies heavily on library design, selection stringency, and validation protocols to eliminate non-specific binders and identify genuinely specific targeting ligands.
In Vivo Panning Platforms
Bacteriophage Display: The most established platform, utilizing engineered bacteriophages to display peptide or protein libraries:
- M13 phage: Long, filamentous phage displaying 3-5 copies of peptide on pIII protein; library diversity ~10^9 [98].
- T7 phage: Smaller, icosahedral phage; higher library diversity up to ~10^11 [98].
- In vivo stability: Unmodified M13 persists ~4 hours in circulation; T7 ~10 minutes; modifications can enhance stability [98].
Aptamer Libraries: Nucleic acid-based ligands selected through Systematic Evolution of Ligands by EXponential enrichment (SELEX):
- Library diversity: Potentially enormous (10^10-10^60 depending on length) [98].
- Size: Approximately 10 kDa for unmodified aptamers [98].
- Stability: Low without chemical modification; various backbone modifications dramatically improve stability [98].
Viral Capsid Display: Engineering of viral vectors (AAV, lentivirus) to display targeting peptides:
- Library diversity: Typically 10^6-10^8 [98].
- Selection rounds: 2-5 rounds typically sufficient [98].
- Key advantage: Direct selection of functional delivery vehicles rather than separate targeting components [98].
Experimental Design for Off-Target Assessment
Comprehensive Risk Assessment Framework
A systematic approach to off-target assessment is essential for rigorous neuroscience research and therapeutic development. This multi-layered strategy combines computational prediction, experimental detection, and functional validation to comprehensively characterize off-target effects in biologically relevant models.
Hypothesis Formulation: Explicitly state the expected specificity profile of your molecular tool and the potential consequences of off-target activity in your experimental system. For neuroscience applications, this should include consideration of cell-type-specific expression patterns, neuronal connectivity, and potential impacts on circuit function [99].
Sample Group Design: Carefully define experimental and control groups that enable discrimination between on-target and off-target effects. For in vivo neuroscience studies, this includes consideration of age, sex, genetic background, and environmental factors that might influence off-target susceptibility [99].
Longitudinal Assessment: For therapeutic applications, implement multiple time points to assess whether off-target effects accumulate over time or manifest differently at various stages after intervention [99].
Detection Methodologies
In Silico Prediction Tools: Computational methods provide the first line of screening for potential off-target sites:
- Alignment-based methods: Identify potential off-target sites through genome alignment (e.g., Cas-OFFinder) [96].
- Scoring-based methods: Employ complex models to rank gRNAs or RNA therapeutics based on predicted specificity [96].
Cell-Free Methods: In vitro approaches using purified genomic DNA offer high sensitivity:
- CIRCLE-seq: Circularization of genomic DNA for highly sensitive, unbiased off-target site identification [96].
- SITE-seq: Capture and sequencing of cleaved genomic DNA fragments [96].
- CHANGE-seq: High-throughput method for mapping CRISPR nuclease off-target activities [96].
Cell-Based Methods: Approaches that maintain chromatin context and cellular environment:
- GUIDE-seq: Incorporation of double-stranded oligodeoxynucleotides to mark double-strand break sites [96].
- LAM-HTGTS: Linear amplification-mediated high-throughput genome-wide translocation sequencing [96].
- ONE-seq: Specifically adapted for base editor off-target profiling [97].
Table 3: Experimental Methods for Off-Target Detection in CRISPR Systems
| Method | Principle | Sensitivity | Bias | Detects SVs | Throughput | Neuroscience Application |
|---|---|---|---|---|---|---|
| GUIDE-seq | DSB tagging with double-stranded oligos | Moderate | Unbiased | No | Medium | Limited in post-mitotic neurons |
| CIRCLE-seq | In vitro cleavage of circularized DNA | High | Unbiased | No | High | Pre-screening before in vivo studies |
| SITE-seq | In vitro cleavage with biotinylated capture | High | Unbiased | No | High | Pre-screening before in vivo studies |
| LAM-HTGTS | Translocation sequencing | Moderate | Requires primer sites | Yes | Medium | Comprehensive risk assessment |
| ONE-seq | Competitive binding for base editors | High | Unbiased | No | High | Specific for base editing applications |
| UdiTas | Targeted sequencing with molecular barcodes | High | Biased (requires sites) | Yes | Medium | Focused validation of predicted sites |
Visualization of Experimental Workflows
Hybrid gRNA Optimization for Enhanced Specificity
Integrated Off-Target Assessment Strategy
In Vivo Biopanning Workflow for Targeted Neuroscience Applications
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Off-Target Assessment and Mitigation
| Reagent/Category | Specification | Function in Experimental Pipeline | Example Vendors/Resources |
|---|---|---|---|
| High-Fidelity Cas9 | SpCas9-HF1, eSpCas9, HypaCas9 variants | Core nuclease with reduced non-specific DNA interactions | Addgene, Integrated DNA Technologies, Thermo Fisher |
| Base Editor Systems | ABE8.8, BE4max with optimized gRNAs | Precision editing with reduced indel formation | Addgene, Beam Therapeutics |
| Chemically Modified gRNAs | 2'-O-methyl, phosphorothioate, DNA-RNA hybrids | Enhanced stability and specificity in complex environments | Synthego, Dharmacon, IDT |
| Off-Target Detection Kits | GUIDE-seq, CIRCLE-seq optimized reagents | Comprehensive mapping of unintended editing events | Integrated DNA Technologies, NEB |
| Next-Generation Sequencing | Amplicon-seq, hybrid capture panels | Sensitive quantification of editing frequencies | Illumina, PacBio, Oxford Nanopore |
| In Vivo Delivery Systems | AAV-PHP.eB, AAV9, LNPs optimized for CNS | Efficient delivery across biological barriers | Vigene, Aldevron, Precision NanoSystems |
| Bioinformatics Tools | Cas-OFFinder, CRISPOR, CCTop | Prediction and analysis of potential off-target sites | Open source, custom pipelines |
| Animal Models | Humanized murine models of neurological disorders | In vivo validation of specificity and efficacy | Jackson Laboratory, Taconic, Charles River |
The mitigation of off-target effects in complex biological environments requires a multi-faceted approach that integrates computational prediction, molecular engineering, and rigorous experimental validation. As neuroscience research increasingly employs sophisticated molecular tools for investigating and treating neurological disorders, ensuring their specificity becomes paramount for both scientific accuracy and therapeutic safety. The strategies outlined in this technical guide—from high-fidelity CRISPR systems and chemically modified RNAs to advanced targeting ligands identified through in vivo biopanning—provide a comprehensive framework for enhancing specificity in neuroscience applications. Implementation of these methodologies, coupled with the standardized reporting of off-target assessments, will advance the field toward more precise and reliable interventions for understanding and treating disorders of the nervous system.
Bridging the Gap: Comparative Analysis with Other Models
In biological and neuroscience research, two foundational methodologies provide the pillars for scientific discovery: in vivo and in vitro studies. These approaches represent a critical dichotomy in scientific inquiry—the tension between observing biological processes in their native, complex physiological context versus isolating them in a controlled environment to establish precise causal relationships. The terms, derived from Latin, meaning "within the living" (in vivo) and "within the glass" (in vitro), embody distinct experimental philosophies with complementary strengths and limitations [100].
For neuroscience research specifically, this dichotomy takes on particular significance. The brain's immense complexity, with its billions of interconnected neurons and diverse cell types operating across multiple spatial and temporal scales, presents unique challenges for researchers [33]. Understanding neural circuits requires observing them in action within intact organisms while also deciphering their fundamental mechanisms through reductionist approaches. This whitepaper provides an in-depth technical analysis of both methodologies, their applications in neuroscience, and emerging technologies that bridge these traditionally separate domains.
Fundamental Principles and Definitions
In Vivo Studies: The Whole-Organism Context
In vivo studies involve conducting experiments within living organisms, allowing researchers to observe biological processes in their natural, holistic context [100]. This approach preserves the intricate physiological interactions between different cell types, tissues, and organ systems that characterize biological function in health and disease. In neuroscience, this might involve studying neural circuit dynamics in behaving animals, monitoring neurotransmitter release during cognitive tasks, or investigating how systemic factors influence brain function.
The key advantage of in vivo studies lies in their high physiological relevance. By studying biological phenomena in intact organisms, researchers can observe how different systems interact and respond to stimuli in ways that mimic real-life situations [100]. This physiological fidelity offers a more comprehensive understanding of complex interactions and facilitates more accurate conclusions about biological processes, especially for translational research aimed at developing human therapies.
In Vitro Studies: The Controlled Reductionist Approach
In vitro studies are conducted outside of living organisms, typically using isolated cells, tissues, or biological molecules in controlled laboratory settings [100]. These experiments allow researchers to manipulate and analyze specific aspects of biological systems with precision and reproducibility unavailable in whole-organism studies. In neuroscience, in vitro approaches might include cultivating neurons in petri dishes, studying synaptic transmission in brain slices, or analyzing molecular pathways in isolated cellular components.
The primary advantage of in vitro systems is the ability to investigate biological phenomena under controlled conditions. By isolating specific components, researchers can simplify experimental setups and remove confounding factors present in complex organisms [100]. This controlled environment enables rigorous hypothesis testing and the establishment of direct causal relationships between variables—a capability often limited in whole-organism studies due to emergent complexity.
Comparative Analysis: Methodological Trade-offs
Table 1: Quantitative Comparison of In Vivo and In Vitro Methodological Attributes
| Attribute | In Vivo | In Vitro |
|---|---|---|
| Physiological Relevance | High (whole-system response) [101] | Low to Moderate (limited to specific cells/tissues) [101] |
| Experimental Control | Limited (many uncontrollable variables) | High (precise control over environment) [100] |
| Cost Factors | High (animal care, monitoring, equipment) [101] | Lower (simplified setup, no animal maintenance) [101] |
| Time to Results | Longer (extended study durations) [101] | Quicker (rapid, focused experiments) [101] |
| Throughput Capability | Low (limited number of subjects) | High (amenable to automation) [100] |
| Ethical Considerations | Significant (animal welfare concerns) [101] | Minimal (no live animals involved) [101] |
Table 2: Applications in Neuroscience and Drug Development Research
| Research Phase | In Vivo Applications | In Vitro Applications |
|---|---|---|
| Early Discovery | Hypothesis generation based on behavioral observations | High-throughput compound screening [101] |
| Mechanistic Studies | Circuit-level neural dynamics [33] | Molecular pathway analysis [100] |
| Therapeutic Development | Pharmacokinetics/ pharmacodynamics [101] | Target engagement and toxicity screening [3] |
| Disease Modeling | Complex behavioral phenotypes | Cellular pathophysiology [102] |
| Translational Research | Clinical trials (human subjects) [100] | Patient-derived cell models [102] |
Technical Methodologies and Experimental Protocols
In Vivo Experimental Approaches in Neuroscience
In vivo neuroscience methodologies have evolved significantly with technological advances, particularly through initiatives like the BRAIN Initiative that aim to produce dynamic pictures of the brain in action [33]. Key technical approaches include:
Large-Scale Neural Recording: Utilizing technologies based on electrodes, optics, molecular genetics, and nanoscience to monitor neuronal activity across multiple brain regions simultaneously in behaving organisms [33]. This enables researchers to observe how neural circuits process information and generate behavior.
Circuit Manipulation Tools: Employing optogenetics, chemogenetics, and biochemical and electromagnetic modulation to directly activate and inhibit specific neuronal populations [33]. These interventional approaches allow neuroscience to progress from observation to establishing causation between neural activity and behavior.
Anatomical Mapping: Generating circuit diagrams at multiple scales—from synapses to the whole brain—using advanced imaging and reconstruction technologies [33]. These maps reveal the relationship between neuronal structure and function, providing structural context for functional observations.
Clinical Neuroscience: Leveraging consenting humans undergoing diagnostic brain monitoring or receiving neurotechnology for clinical applications to conduct research on human brain function and disorders [33]. This approach provides unprecedented access to human brain activity but requires strict ethical standards.
In Vitro Experimental Approaches in Neuroscience
Modern in vitro neuroscience methodologies have progressed beyond simple cell cultures to increasingly complex models that better recapitulate in vivo conditions:
Advanced Cell Culture Models: Developing three-dimensional culture systems that more accurately mimic the brain's cellular environment. For example, MIT researchers recently created "miBrains"—multicellular integrated brain models that incorporate all six major brain cell types into a single culture, including neurons, glial cells, and vasculature [102].
Organ-on-a-Chip Technology: Using microfluidic culture devices that expose cells to biomechanical forces, dynamic fluid flow, and heterogeneous cell populations while providing three-dimensional cellular contacts [103]. These systems encourage cells to behave more naturally, bridging the gap between traditional in vitro culture and in vivo environments.
Patient-Derived Models: Generating in vitro systems from individual patients' induced pluripotent stem cells, enabling personalized disease modeling and drug testing [102]. This approach allows researchers to create customized models that reflect individual genetic backgrounds.
High-Content Screening: Implementing automated imaging and analysis systems to extract multiparametric data from cell-based assays. This enables quantitative analysis of complex cellular phenotypes in response to genetic or chemical perturbations.
Quantitative Framework: Predicting In Vivo Efficacy from In Vitro Data
A critical challenge in biomedical research is reliably predicting in vivo efficacy from in vitro data. Recent research has demonstrated promising approaches using quantitative pharmacokinetic/pharmacodynamic (PK/PD) modeling [3].
Table 3: Key Parameters for Translating In Vitro Findings to In Vivo Predictions
| Parameter | In Vitro Determination | In Vivo Scaling Factor | Application in PK/PD Modeling |
|---|---|---|---|
| Target Engagement | Direct measurement of drug-target binding [3] | Plasma protein binding (fu) [3] | Links plasma concentration to cellular effect |
| Biomarker Dynamics | Time- and dose-dependent response in cells [3] | Tissue penetration factors | Predicts pharmacodynamic response |
| Cell Growth/Tumor Dynamics | Proliferation rate in culture [3] | Growth rate modification (kP) [3] | Scales baseline growth characteristics |
| Drug Exposure | Concentration-response relationships [3] | Pharmacokinetic parameters (absorption, distribution, metabolism, excretion) | Models temporal drug availability |
In one demonstrated approach, researchers built a semimechanistic PK/PD model that successfully predicted in vivo antitumor efficacy from in vitro data with only a single parameter change—the parameter controlling intrinsic cell growth in the absence of drug (kP) [3]. This model integrated diverse experimental data collected across time and dose dimensions, under both intermittent and continuous dosing regimens, capturing the relationship between target engagement, biomarker levels, and cell growth dynamics.
The mathematical framework follows these core equations:
Target Engagement:
- LSD1 binding: dLSD1B/dt = kinact · ROC/(Ki + ROC) · LSD1U - Vmax/(Km + LSD1B) · LSD1B [3]
Pharmacokinetic Linking:
- Active drug concentration: ROC = CPL · fu [3]
- Where CPL is plasma concentration and fu is unbound fraction
This approach demonstrates how in vitro models, when properly designed and quantitatively analyzed, can reduce animal usage while providing predictive power for in vivo outcomes.
Diagram 1: PK/PD Modeling Workflow for translating in vitro data to in vivo predictions. The model integrates pharmacokinetic (PK) parameters with pharmacodynamic (PD) data from in vitro assays, with minimal parameter adjustment (k_P) for in vivo scaling [3].
Emerging Technologies and Future Directions
Advanced In Vitro Models for Neuroscience
Recent advances in in vitro modeling are dramatically improving their physiological relevance and predictive power for neuroscience applications:
Multicellular Integrated Brain Models (miBrains): Developed by MIT researchers, these 3D human brain tissue platforms integrate all major brain cell types—neurons, astrocytes, microglia, oligodendrocytes, pericytes, and endothelial cells—into a single culture system [102]. Derived from induced pluripotent stem cells, miBrains replicate key features of human brain tissue, including neurovascular units and blood-brain barrier functionality. Their modular design allows precise control over cellular inputs and genetic backgrounds, enabling researchers to study cell-type-specific contributions to disease pathology.
Organ-on-a-Chip Systems: Microfluidic devices that emulate the microenvironment of specific brain regions by incorporating physiological cues such as fluid shear stress, mechanical strain, and spatial organization [103]. These systems can model the blood-brain barrier with high fidelity and have demonstrated improved predictive accuracy for drug penetration into the CNS compared to traditional static cultures.
Case Study: Alzheimer's Disease Research with miBrains
The application of miBrains in Alzheimer's disease research illustrates the power of advanced in vitro systems. Researchers used miBrains to investigate how the APOE4 gene variant—the strongest genetic predictor for Alzheimer's—alters cellular interactions to produce pathology [102].
Key findings from this study demonstrate the value of complex in vitro systems:
APOE4 astrocytes cultured in isolation showed minimal immune reactivity, but when placed in multicellular miBrains environments, they expressed multiple measures of immune activation associated with Alzheimer's pathology [102].
By creating chimeric miBrains with APOE4 astrocytes in an otherwise APOE3 background, researchers isolated the specific contribution of astrocytic APOE4 to amyloid and tau pathology [102].
The study provided new evidence that molecular cross-talk between microglia and astrocytes is required for phosphorylated tau pathology—a discovery difficult to achieve with either traditional in vitro or in vivo approaches alone [102].
Diagram 2: miBrain Development Pipeline. Patient-derived induced pluripotent stem cells (iPSCs) are differentiated into six major brain cell types which self-assemble into functional units within a specialized "neuromatrix" hydrogel [102].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Neuroscience Studies
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific disease modeling [102] | Generating patient-derived neural cells for in vitro studies [102] |
| Extracellular Matrix Hydrogels | 3D structural support mimicking brain tissue [102] | Creating scaffold for complex 3D cultures like miBrains [102] |
| Selective Chemical Inhibitors | Targeted modulation of specific pathways | Studying causal relationships in signaling pathways (e.g., ORY-1001 for LSD1 inhibition) [3] |
| Optogenetic Tools | Light-sensitive proteins for neural control [33] | Precise temporal control of specific neuronal populations in vivo |
| Genome Editing Systems | Targeted genetic modifications | Creating disease-specific mutations in cellular models [102] |
| Molecular Biosensors | Real-time monitoring of cellular activity | Fluorescent reporters for neural activity or second messenger dynamics |
The dichotomy between in vivo and in vitro methodologies represents not a choice between superior and inferior approaches, but rather a strategic consideration of complementary scientific tools. In vivo studies provide essential physiological context and whole-system responses critical for understanding complex biological phenomena, while in vitro systems offer unprecedented control and analytical capabilities for mechanistic insights [100].
For neuroscience research specifically, the future lies in the intelligent integration of both approaches, leveraging their respective strengths while mitigating their limitations. Emerging technologies like miBrains [102], Organ-Chips [103], and sophisticated computational models [3] are creating new opportunities to bridge the gap between controlled simplicity and physiological relevance. These advanced systems enable researchers to address fundamental questions about brain function and dysfunction with increasing precision while reducing reliance on animal models through the principles of Replacement, Reduction, and Refinement (3Rs) [100].
As the BRAIN Initiative emphasizes, understanding the brain in health and disease requires cross-boundary interdisciplinary collaborations that link experiment to theory, biology to engineering, and tool development to experimental application [33]. By strategically employing both in vivo and in vitro approaches within this integrated framework, neuroscientists can accelerate the translation of basic discoveries into effective treatments for the myriad disorders that affect the nervous system.
The pursuit of understanding brain function relies heavily on the accuracy of our measurement techniques. While ex vivo approaches using postmortem tissue have provided invaluable anatomical insights, their utility for understanding dynamic brain functions remains fundamentally limited. This technical guide examines the critical limitations of ex vivo measurements through the lens of transcranial electric stimulation (TES) studies, presenting a cautionary tale for neuroscientists and drug development professionals. Within the broader context of in vivo techniques for neuroscience research, we demonstrate how death produces significant changes in the biophysical properties of brain tissues, making ex vivo to in vivo comparisons complex and often questionable [104]. These limitations are not merely academic—they directly impact the translational validity of preclinical research and the development of effective neuromodulation therapies.
The BRAIN Initiative has emphasized the importance of understanding the "brain in action" through innovative neurotechnologies that capture dynamic neural processes [33]. This vision aligns with the growing recognition that static ex vivo measurements cannot fully replicate the complexity of living neural systems. Through quantitative data comparison, detailed methodological analysis, and visual workflow documentation, this review provides researchers with a framework for critically evaluating measurement approaches in their own investigations of brain function and dysfunction.
Quantitative Comparison: Ex Vivo vs. In Vivo Biophysical Properties in TES
Direct comparative studies reveal substantial differences in TES-induced electric fields between living and postmortem conditions. A foundational study using nonhuman primate models demonstrated significant discrepancies in both the strength and frequency response dynamics of intracranial electric fields when measured pre- versus postmortem [104]. These differences persisted even while controlling for potentially confounding factors such as body temperature, indicating fundamental alterations in tissue electrical properties following death.
Table 1: Comparative Properties of In Vivo vs. Ex Vivo Brain Tissue in TES Studies
| Property | In Vivo Condition | Ex Vivo Condition | Functional Significance |
|---|---|---|---|
| Electric Field Strength | Dynamic, responsive | Significantly altered | Underestimates/overestimates stimulation intensity |
| Frequency Response | Intact dynamics | Differing dynamics | Misrepresents frequency-dependent effects |
| Tissue Conductivity | Physiological | Non-physiological | Alters current flow patterns |
| Cellular Environment | Homeostatic maintained | Degrading | Affects neuronal responsiveness |
| Fluid Compartments | Intact boundaries | Compromised | Distorts current paths |
| Metabolic Support | Active maintenance | Absent | Changes tissue impedance |
The implications of these discrepancies extend beyond basic research to clinical applications. TES protocols developed using ex vivo measurements may prove ineffective or require significant modification when translated to living human brains. The observed differences in electric field strength and frequency response dynamics suggest that ex vivo models cannot reliably predict the actual current distributions that occur during in vivo applications [104]. This limitation is particularly problematic for developing targeted neuromodulation therapies for neurological and psychiatric disorders, where precise electrical field delivery is critical for efficacy and safety.
Methodological Limitations: Understanding the Source of Discrepancies
Fundamental Biophysical Alterations in Postmortem Tissue
The transition from living to postmortem tissue involves profound biophysical changes that directly impact TES measurements. Key alterations include:
- Cessation of metabolic activity and disruption of ion homeostasis, affecting electrical conductivity
- Breakdown of cellular membranes and compromise of fluid compartments that guide current flow in living tissue
- Alterations in extracellular space geometry and composition, changing current paths
- Loss of blood flow and cerebrospinal fluid circulation, removing conductive pathways present in living brains
- Tissue fixation effects in processed specimens, including cross-linking that further alters electrical properties
These changes collectively create a fundamentally different biophysical environment that cannot adequately replicate the complexity of living neural tissue [104]. Consequently, measurements obtained ex vivo provide at best an approximation and at worst a significant misrepresentation of actual in vivo conditions.
Experimental Evidence from Direct Comparisons
The most compelling evidence comes from direct within-subject comparisons of pre- and postmortem measurements. In the seminal nonhuman primate study, researchers measured TES-induced intracranial electric fields in the same subject before and after death, controlling for variables such as electrode placement and body temperature [104]. This rigorous methodology revealed that ex vivo measurements differed significantly in both strength and frequency response dynamics, underscoring their limitations for predicting in vivo effects.
These findings challenge the common practice of using ex vivo data to calibrate or validate TES dosing parameters for human applications. They further question the utility of cadaver studies for precise targeting in clinical neuromodulation, suggesting that such approaches may lead to subtherapeutic stimulation or unexpected side effects when translated to living patients.
Advanced In Vivo Techniques: The Path Forward in Neuroscience
Cutting-Edge In Vivo Synaptic Connectivity Mapping
In contrast to static ex vivo approaches, emerging in vivo technologies enable unprecedented dynamic investigation of neural circuits. A recently developed framework combines two-photon holographic optogenetics with whole-cell recordings to map synaptic connectivity in living brains [86]. This approach allows researchers to:
- Probe connectivity across up to 100 potential presynaptic cells within approximately 5 minutes
- Identify synaptic pairs along with their strength and spatial distribution
- Combine multi-cell stimulation with compressive sensing reconstruction to improve sampling efficiency
- Recover most connections with a threefold reduction in required measurements compared to sequential approaches
This methodology demonstrates how in vivo techniques can achieve both high throughput and high resolution while maintaining physiological relevance—addressing a critical limitation of ex vivo approaches [86].
Table 2: Research Reagent Solutions for Advanced In Vivo Neuroscience
| Reagent/Technology | Function | Application in TES Validation |
|---|---|---|
| ST-ChroME opsin | Soma-restricted optogenetic actuator | Precise neuronal activation for connectivity mapping |
| Two-photon holographic system | Multi-cell photostimulation at cellular resolution | Controlled presynaptic spike induction |
| Compressive sensing algorithms | Reconstruction of sparse connectivity from limited measurements | Efficient analysis of neural circuit organization |
| Whole-cell patch clamp | Intracellular recording of postsynaptic responses | Direct measurement of synaptic responses to TES |
| Particle-filtering tractography | White matter pathway reconstruction | Anatomical validation of TES current paths |
Integrated In Vivo and Ex Vivo Mapping Approaches
While ex vivo methods have limitations for dynamic measurements, they can provide valuable anatomical context when integrated with in vivo approaches. A recent study on the superior longitudinal system (SLS) demonstrated how combining in vivo tractography with ex vivo dissection in the same radiological space can enhance anatomical characterization [105]. This integrated approach identified 45 SLS components, with 22 validated and refined through ex vivo dissection, while 17 were deemed anatomically plausible despite lacking ex vivo confirmation, and 6 were classified as anatomically implausible [105].
This hybrid methodology leverages the respective strengths of both approaches: the dynamic functional information from in vivo measurements and the high-resolution structural validation from ex vivo techniques. Such integration represents a more nuanced approach than relying exclusively on one methodology, acknowledging both the value and limitations of each.
Experimental Protocols for Validating TES Effects In Vivo
Protocol for Direct Pre-/Postmortem TES Comparison
To empirically validate the limitations of ex vivo measurements, researchers can implement the following protocol adapted from Opitz et al. [104]:
Surgical Preparation: Implant intracranial recording electrodes in target brain regions of an anesthetized nonhuman primate subject, ensuring stable placement for repeated measurements.
In Vivo Measurement: Apply TES at multiple frequencies and intensities while recording intracranial electric fields. Document precise electrode positions and stimulation parameters.
Postmortem Transition: Maintain the subject's physiological temperature during the transition to postmortem condition using regulated heating systems.
Ex Vivo Measurement: Precisely replicate the stimulation parameters from the in vivo condition, recording electric fields in the same locations.
Data Analysis: Compare electric field strength and frequency response dynamics between conditions using appropriate statistical methods (e.g., paired t-tests, frequency domain analysis).
This protocol directly tests the central hypothesis that ex vivo measurements differ significantly from in vivo conditions, providing crucial validation data for researchers relying on postmortem tissue.
Protocol for In Vivo Synaptic Connectivity Mapping
For investigators seeking to implement state-of-the-art in vivo validation of circuit-level effects, the following protocol adapted from high-throughput synaptic connectivity mapping can be applied [86]:
Viral Vector Expression: Express the fast, soma-targeted opsin ST-ChroME in presynaptic neurons using stereotaxic injection of AAV vectors.
Cranial Window Implantation: Install a chronic cranial window to allow optical access for both imaging and stimulation.
Two-Photon Guided Patching: Establish whole-cell recordings from postsynaptic neurons while simultaneously identifying opsin-expressing presynaptic cells via mRuby fluorescence.
Holographic Stimulation: Apply temporally focused holographic patterns to stimulate single or multiple presynaptic neurons with 10ms pulses at 0.15-0.3 mW/μm² power density.
Response Analysis: Record postsynaptic currents or potentials, averaging across trials to distinguish true synaptic connections from spontaneous activity.
Compressive Sensing Application: When probing sparse connectivity, use multi-cell stimulation patterns with compressive sensing reconstruction to improve sampling efficiency.
This approach enables direct investigation of how TES might modulate specific synaptic connections in living circuits, providing mechanistic insights beyond what is possible with ex vivo preparations.
Visualization of Experimental Approaches
Workflow for Validating TES Measurements
In Vivo Synaptic Connectivity Mapping
The evidence presented in this technical guide underscores a critical reality for neuroscience researchers and drug development professionals: ex vivo measurements provide fundamentally limited insights into the dynamic functioning of living neural circuits. The documented discrepancies in TES-induced electric fields between pre- and postmortem conditions [104] serve as a powerful cautionary tale about the potential pitfalls of over-relying on postmortem tissue for understanding brain function.
Moving forward, the field must prioritize the development and implementation of advanced in vivo techniques that can capture neural dynamics with increasing spatial and temporal resolution. The integration of cutting-edge approaches such as two-photon holographic optogenetics [86], combined with rigorous computational methods, offers a path toward more accurate and physiologically relevant understanding of brain function. Furthermore, the ethical deployment of these technologies in both animal models and human studies [33] will be essential for translating basic neuroscience discoveries into effective therapies for neurological and psychiatric disorders.
By acknowledging the limitations of ex vivo measurements and embracing the potential of in vivo approaches, researchers can avoid methodological pitfalls and generate more reliable, translatable knowledge about brain function in health and disease.
Organotypic brain slice cultures (BSCs) represent a sophisticated ex vivo experimental model that preserves the native three-dimensional cytoarchitecture, cellular diversity, and functional neural networks of living brain tissue. This bridging technology occupies a critical niche between simplified cell cultures and complex in vivo studies, enabling direct investigation of physiological and pathological processes in a controlled environment. With viability extending from days to several weeks, BSCs support a wide range of neuroscientific applications including disease modeling, drug screening, and mechanistic studies of neural circuit function. This technical guide examines the methodology, applications, and validation parameters of BSCs, with particular emphasis on their growing utility in translational neuroscience and drug development pipelines.
The central challenge in neuroscience research lies in capturing the complex interplay between diverse neural cell types within their native structural context while maintaining experimental accessibility. Organotypic brain slice cultures address this challenge by preserving the living brain's intricate organization outside the body, allowing for direct manipulation and observation not feasible in intact organisms [106]. Unlike dissociated cell cultures that lose native connectivity, BSCs maintain the three-dimensional architecture and multicellular environment of the original tissue, including neurons, glia, and vascular elements [107] [108].
These cultures serve as a pivotal bridge model in the neuroscience research continuum, offering a physiologically relevant system that complements both reductionist in vitro approaches and complex in vivo studies. The preservation of local circuitry and synaptic connections enables investigation of network-level phenomena with a precision impossible in whole-animal models [109] [106]. For drug development professionals, BSCs provide a human-relevant platform for therapeutic screening that predicts drug effects more accurately than monolayer cultures, particularly for compounds targeting complex neuronal interactions or requiring penetration through tissue barriers [108] [110].
Recent technical advances have extended the viability and applicability of BSCs, particularly through optimized culture media and preparation methods. The incorporation of human cerebrospinal fluid into culture systems has demonstrated significant benefits for neuronal survival and activity, enhancing the physiological relevance of these models [109] [110]. Furthermore, the successful establishment of cultures from post-mortem human tissue has expanded access to diverse neural tissues, enabling studies of age-related diseases and disorders not typically addressed through surgical specimens [110].
Technical Foundations: Methodologies for Slice Culture Preparation
Core Preparation Protocol
The successful establishment of viable organotypic slice cultures depends on meticulous attention to several critical steps throughout the preparation process. The following workflow outlines the key stages in generating and maintaining BSCs:
BSCs can be prepared from multiple tissue sources, each with distinct advantages and limitations:
Surgical Resections: Tissue obtained from epilepsy surgery or tumor resection procedures offers enhanced viability and functional activity, crucial for long-term studies. This tissue typically comes from patients with neurological conditions, which may influence generalizability of findings [108]. Common surgical sources include cortical tissue from epilepsy surgeries, tissue margins from tumor resections, and small biopsies from deep brain stimulation procedures [107].
Post-mortem Tissue: Donor tissue provides access to a wider range of age-matched controls and disease-specific tissues not available through surgical means. However, viability can be compromised by post-mortem interval (PMI), with shorter intervals (typically <4-6 hours) critical for maintaining tissue health [110].
Sectioning and Culture Conditions
Optimal sectioning parameters vary by tissue type and age:
Sectioning Thickness: Typical slices range from 150-400μm thickness, balancing diffusion limitations with structural preservation. Thinner slices (150-300μm) are often used for adult tissue to enhance viability [109] [110].
Sectioning Solutions: Choline-based slicing artificial cerebrospinal fluid (s-aCSF) is commonly used to diminish slicing-induced stress and excitotoxicity. This solution replaces sodium with choline to silence neuronal activity during preparation [109].
Culture Methodology: The interface method cultures slices on porous membrane inserts at the air-liquid interface, allowing nutrition from the medium below while maintaining gas exchange from above. This approach better preserves cytoarchitecture compared to roller-tube methods [106].
Research Reagent Solutions
Table: Essential Reagents for Organotypic Brain Slice Culture Maintenance
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Slicing Solutions | Choline-based s-aCSF (110mM choline chloride, 26mM NaHCO₃, 7mM MgCl₂, 0.5mM CaCl₂) [109] | Reduces excitotoxicity during sectioning by replacing sodium to silence neuronal activity |
| Culture Media | Minimum Essential Medium (50%) + Horse Serum (25%) + Earle's Balanced Salt Solution (25%) [110] | Provides nutritional support; serum contains essential growth factors |
| Medium Supplements | GlutaMAX-I, D-Glucose, Penicillin-Streptomycin, Amphotericin B [110] | Supports metabolic needs and prevents microbial contamination |
| Specialized Additives | Human Cerebrospinal Fluid [109] [110] | Enhances neuronal survival and activity; contains native growth factors |
| Viability Assessment | Propidium iodide, Lactate dehydrogenase assay [106] | Evaluates cell death and tissue health through membrane integrity markers |
Research Applications: From Basic Mechanisms to Therapeutic Discovery
Organotypic slice cultures support diverse experimental applications across neuroscience domains. The preserved tissue architecture enables studies of complex cellular interactions within a controlled environment.
Disease Modeling and Mechanistic Studies
Neurodegenerative Disorders
BSCs have proven particularly valuable for modeling proteinopathies such as Alzheimer's disease (AD), allowing investigation of Aβ plaque dynamics, tau phosphorylation, and neuroinflammatory responses in a preserved neural environment [111] [106]. Unlike monolayer cultures, BSCs maintain the complex cellular interactions essential for studying disease progression. For example, studies using okadaic acid treatment in BSCs have successfully induced tau hyperphosphorylation, replicating a key aspect of AD pathology [111]. The ability to introduce pathological proteins or observe disease progression in patient-derived tissue makes BSCs particularly valuable for studying sporadic neurodegenerative diseases, which constitute over 99% of AD cases [111].
Neuro-oncology
In neuro-oncology research, BSCs provide a unique platform for studying tumor-microenvironment interactions in a preserved human brain context. Models introducing patient-derived glioblastoma cells into human brain slices allow direct observation of tumor infiltration along white-matter tracts and blood vessels [108]. These systems preserve the resident astrocytes, microglia, neurons, and extracellular matrix, enabling investigation of tumor-host interactions that drive progression and therapeutic resistance [108]. Studies using this approach have revealed how gap junction inhibition can disrupt tumor network communication, highlighting how BSCs can reveal therapeutic effects on multicellular architecture [108].
Neuroimmunology and Infectious Disease
BSCs provide a human-relevant platform for studying host-pathogen interactions in the brain, overcoming ethical constraints of in vivo infection studies. The preserved innate immune environment allows investigation of microglial and astrocyte responses to pathogens in a context not possible with isolated cell cultures [108].
Therapeutic Development and Screening
The pharmaceutical application of BSCs spans multiple stages of therapeutic development:
Drug Efficacy Testing: BSCs enable direct assessment of compound effects on human brain tissue with preserved cellular complexity. Studies have demonstrated predictable antitumor effects of temozolomide in glioma-infiltrated slices, with the presence of blood-brain barrier elements enhancing translational relevance [108].
Immunotherapy Assessment: BSCs serve as testbeds for next-generation immunotherapies, including checkpoint inhibitors and CAR-T cells. Studies have analyzed how glioblastoma cells secrete immunosuppressive cytokines that suppress T-cell activity, guiding development of combination therapies [108].
Gene Therapy Validation: BSCs demonstrate successful cell-type dependent transduction with viral vectors, providing a platform for testing gene therapy approaches before advancing to in vivo models [110].
Validation and Assessment: Quantifying Culture Viability and Function
Rigorous assessment of slice health and functionality is essential for interpreting experimental results. Multiple complementary approaches are employed to validate BSC quality.
Viability and Functional Assessment Methods
Table: Viability and Functional Parameters of Organotypic Slice Cultures
| Assessment Method | Measurement Parameters | Typical Results | Interpretation Guidelines |
|---|---|---|---|
| Electrophysiology (Patch-clamp, MEA) [109] | Neuronal firing, synaptic responses, network activity | Sustained action potentials, spontaneous postsynaptic currents | Robust electrical activity indicates healthy, functional neurons |
| Viability Staining (Propidium iodide, live/dead assays) [106] | Membrane integrity, cell death quantification | <30% cell death in viable cultures | Higher percentages indicate culture compromise |
| Metabolic Assays (LDH release, MTT assay) [106] | Metabolic activity, cell death | Stable LDH levels, consistent metabolic activity | Rising LDH indicates increasing cell death |
| Morphological Analysis | Cytoarchitecture preservation, dendritic integrity | Maintained layered structure, complex dendritic arbors | Structural deterioration suggests culture decline |
| Immunohistochemistry | Cell-type specific markers, pathology markers | Preservation of neuronal and glial populations | Loss of specific cell types indicates selective vulnerability |
Culture Longevity and Success Rates
The viability of organotypic slice cultures varies based on preparation methods and tissue sources:
Surgical Tissue Cultures: Viability typically extends to 2-3 weeks, with some reports of functional maintenance up to 29 days in defined medium [109]. Success rates correlate with patient age and underlying pathology, with approximately 70% of cultures from epilepsy surgeries and 40% from tumor resections achieving high viability [109].
Post-mortem Cultures: Recent advances have extended viability of post-mortem-derived cultures to at least six weeks ex vivo when cultured at the air-liquid interface with appropriate medium supplements [110].
Culture success is influenced by multiple factors, with tissue quality at acquisition being paramount. For post-mortem tissue, shorter post-mortem intervals (<6 hours) significantly enhance viability, while for surgical tissue, rapid processing (<30 minutes post-resection) is critical [108] [110]. Medium composition also substantially impacts longevity, with human cerebrospinal fluid supplementation demonstrating beneficial effects on both survival and functional activity [109] [110].
Ethical Considerations in Slice Culture Research
The use of human brain tissue, particularly in long-term culture systems, raises important ethical considerations that must be addressed through appropriate guidelines and oversight. Key issues include:
Donor Consent: Ensuring proper informed consent for tissue use in research, with clear communication about potential applications including genetic manipulation and long-term maintenance [107] [108].
Consciousness Potential: The possibility of sustained neural activity in cultured slices prompts philosophical questions about consciousness that warrant careful consideration in experimental design [107].
Transparency and Oversight: Establishing clear ethical frameworks for tissue procurement, use, and eventual disposal, with particular attention to public transparency regarding research practices [107].
These considerations highlight the need for balanced guidelines that support scientific innovation while maintaining ethical responsibility in the use of living human neural tissue [107].
Organotypic slice cultures represent a powerful bridge technology in neuroscience research, offering unprecedented access to the complex cellular interactions within brain tissue while maintaining experimental control. The preservation of native cytoarchitecture and cellular diversity enables investigation of physiological and pathological processes in a context that balances physiological relevance with practical accessibility. As technical advances continue to extend culture viability and expand tissue sources, BSCs are poised to play an increasingly central role in both basic neuroscience and translational drug development. Their unique position in the research continuum makes them particularly valuable for validating findings from reductionist systems before advancing to complex in vivo models, potentially accelerating the pace of discovery in neurological disease research while reducing reliance on animal models.
The complexity of the human brain necessitates a multi-faceted approach to unlock its secrets. No single imaging modality can fully capture the intricate interplay of structure, function, and molecular biology that underpins both healthy cognition and neurological disease. Consequently, the integration of multiple neuroimaging techniques has emerged as a cornerstone of modern neuroscience research, enabling a more comprehensive and mechanistic understanding of brain function in vivo. This technical guide focuses on the core principles and methodologies for the cross-validation and integration of three powerful modalities: functional Magnetic Resonance Imaging (fMRI), Positron Emission Tomography (PET), and optical imaging data. Framed within a broader thesis on in vivo techniques, this whitepaper provides researchers, scientists, and drug development professionals with the experimental protocols and analytical frameworks needed to leverage these technologies synergistically, thereby accelerating biomarker discovery and the development of targeted therapeutics for neuropsychiatric disorders.
The Multimodal Imaging Landscape: Core Technologies and Complementary Data
The value of multimodal integration stems from the unique and complementary biological information each technique provides.
Functional Magnetic Resonance Imaging (fMRI): fMRI, particularly resting-state fMRI (rs-fMRI), infers brain activity by measuring hemodynamic changes related to neural activity. Its primary output is a map of functional connectivity (FC), which represents the statistical interdependence of neural activity between different brain regions [112] [113]. FC is a statistical construct rather than a direct physical measurement, and its estimation can be performed using a variety of pairwise interaction statistics, from simple Pearson correlation to more complex measures like precision or inverse covariance [114]. fMRI provides excellent spatial resolution and is non-invasive, making it ideal for investigating large-scale brain networks and their alterations in disease.
Positron Emission Tomography (PET): PET is a molecular imaging technique that uses radioactive tracers to quantify specific neurobiological targets in vivo. In neurodegenerative diseases like Alzheimer's, PET tracers for amyloid-beta (e.g., Florbetapir) and tau proteins (e.g., Flortaucipir) allow for the direct visualization of pathological aggregates [112]. PET can also map dopaminergic system integrity in Parkinson's disease, cerebral glucose metabolism with [18F]-FDG, and a wide array of neurotransmitter receptors [114]. This molecular specificity is crucial for linking functional and structural changes to their underlying biochemical pathways.
Optical Imaging Techniques: While less frequently integrated with fMRI and PET in human whole-brain studies, optical techniques like optogenetics are foundational to causal interrogation in animal models. They enable precise manipulation of specific neural cell types and circuits with millisecond precision, providing a ground truth for interpreting correlational data from fMRI and PET [33]. The translation of these principles is a key goal in neuroscience.
The synergy is clear: fMRI reveals when and where brain regions communicate, PET reveals why by identifying the molecular substrates, and optical data can causally test these relationships. For instance, amyloid PET can identify at-risk individuals, fMRI can track the subsequent disruption of functional networks, and targeted interventions can be designed based on this integrated profile [112] [115].
Table 1: Key Characteristics of Core Neuroimaging Modalities
| Modality | Primary Measurement | Spatial Resolution | Temporal Resolution | Key Biomarkers | Principal Advantages |
|---|---|---|---|---|---|
| fMRI | Hemodynamic response (BOLD signal) | 1-3 mm | ~1 second | Functional Connectivity (FC), Network Topology | Non-invasive, whole-brain coverage, excellent for network dynamics |
| PET | Radioligand binding / concentration | 4-5 mm | Minutes to hours | Amyloid-beta, Tau, Dopaminergic terminals, Glucose Metabolism | Molecular specificity, quantifies specific proteinopathies |
| Optical Imaging | Light scattering/fluorescence | Microns (invasively) | Milliseconds | Neural activity (via indicators), Circuit manipulation | High spatiotemporal resolution, causal interrogation (optogenetics) |
Quantitative Cross-Validation: Benchmarking and Establishing Ground Truth
Cross-validation ensures that findings from one modality are biologically meaningful and not methodological artifacts. This involves benchmarking against other imaging techniques and established biological truths.
Benchmarking fMRI Functional Connectivity
A critical step in validating fMRI findings is to benchmark FC metrics against the brain's structural anatomy and other neurophysiological networks. A comprehensive study evaluated 768 fMRI data-processing pipelines and found vast variability in their outcomes [113]. The optimal pipelines were those that minimized motion confounds and spurious test-retest discrepancies while remaining sensitive to individual differences and experimental effects.
Furthermore, benchmarking 239 different pairwise statistics for calculating FC revealed substantial qualitative and quantitative variation in derived network features [114]. Key validation criteria include:
- Structure-Function Coupling: The correlation between fMRI-based FC and diffusion MRI-based structural connectivity. Measures like precision and stochastic interaction show the strongest structure-function coupling [114].
- Alignment with Multimodal Neurophysiology: FC matrices can be validated by correlating them with interregional similarity matrices derived from other modalities, such as:
- Neurotransmitter receptor similarity (from PET)
- Gene expression profiles (from the Allen Human Brain Atlas)
- Electrophysiological connectivity (from MEG) [114]
Table 2: Performance of Select fMRI Connectivity Metrics in Benchmarking Studies
| Functional Connectivity Metric | Structure-Function Coupling (R²) | Correlation with Receptor Similarity | Sensitivity to Individual Differences | Key Strengths |
|---|---|---|---|---|
| Pearson's Correlation | Moderate | Moderate | Moderate | Standard, easily interpretable |
| Precision (Inverse Covariance) | High (up to ~0.25) | High | High | Accounts for shared network influence, emphasizes direct connections |
| Distance Correlation | Moderate | Moderate | High | Captures non-linear dependencies |
| Imaginary Coherence | High | Moderate | Moderate | Robust to zero-lag artifacts |
Validating PET Findings with Multimodal Data
PET findings are cross-validated by establishing their relationship with clinical and other imaging data. For example:
- Amyloid and Tau PET should show a strong association with downstream neuronal injury, such as hypometabolism on FDG-PET and atrophy on structural MRI [112].
- In drug development, a successful therapeutic that clears amyloid plaques (as verified by PET) should correspondingly slow the rate of functional network deterioration measured by fMRI and clinical cognitive decline [112] [115].
Experimental Protocols for Multimodal Integration
Successful integration requires meticulous planning at the acquisition, preprocessing, and analysis stages.
Data Acquisition and Preprocessing Pipeline
A standardized protocol is essential for generating coherent multimodal datasets.
- Subject Recruitment & Clinical Phenotyping: Recruit participants (e.g., Alzheimer's disease, Mild Cognitive Impairment, healthy controls) and collect comprehensive cognitive and clinical data.
- Multimodal Data Acquisition:
- MRI/fMRI Session: Acquire high-resolution T1-weighted structural MRI, resting-state fMRI (rs-fMRI), and diffusion MRI (dMRI) in a single session. Parameters: rs-fMRI (TR=0.72s, 2mm isotropic voxels, multiband acceleration); T1 (MPRAGE, 1mm isotropic) [113].
- PET Session: Perform amyloid/tau PET scanning on a separate visit. Parameters: Dynamic acquisition, bolus injection of [11C]PIB (amyloid) or [18F]Flortaucipir (tau), followed by a 60-90 minute scan. Monitor arterial input for quantitative modeling [112].
- Preprocessing:
- fMRI: Use tools like fMRIPrep or SPM. Steps include slice-timing correction, head motion realignment, normalization to standard space (e.g., MNI), and nuisance regression (e.g., aCompCor). Critically, the impact of global signal regression (GSR) must be evaluated [113].
- PET: Perform motion correction, co-registration to the subject's T1 MRI, spatial normalization, and partial volume correction. Standardized Uptake Value Ratio (SUVR) or full kinetic modeling (e.g., generating Distribution Volume Ratio, DVR) are used for quantification [112].
- Structural MRI: Process with FreeSurfer or CAT12 for tissue segmentation (GM, WM, CSF) and parcellation of Regions of Interest (ROIs) using an atlas like AAL or Schaefer [116].
Multimodal Data Processing Workflow
Multimodal Data Fusion Techniques
Once preprocessed, data from different modalities are integrated using fusion techniques, increasingly powered by deep learning [117] [116] [115].
- Input-Level Fusion (Early Fusion): Raw or minimally processed data from different modalities are combined into a single input for a model. This is less common due to differing data resolutions and dimensionalities.
- Intermediate-Level Fusion (Deep Learning-Based Fusion): This is the most prevalent approach in modern architectures. Features are extracted from each modality using separate neural network branches, which are then merged.
- Architectures: Frameworks like ADMV-Net use dual-pathway networks (e.g., Hybrid Convolution ResNet) to extract global and local features from sMRI and PET separately [116].
- Fusion Modules: Features are then integrated using mechanisms like:
- Multi-view Fusion Learning (MVFL): Combines features from global, local, and latent perspectives [116].
- Attention-based Fusion: Uses cross-modal attention modules (e.g., Bidirectional Cross-Attention) to dynamically weigh the importance of features from different modalities [117] [116].
- Hierarchical Fusion: Combines features from different network depths using structures like BiFPN [116].
- Decision-Level Fusion (Late Fusion): Separate classifiers are trained on each modality, and their predictions are combined (e.g., by averaging or voting) for a final decision.
Deep Learning Multimodal Fusion
Table 3: Key Research Reagent Solutions for Multimodal Neuroimaging
| Item / Resource | Function / Application | Example Specifications / Notes |
|---|---|---|
| fMRI Preprocessing Pipelines | Standardized data cleaning and preparation for FC analysis. | fMRIPrep [113], HCP Minimal Preprocessing Pipelines. Critical for reproducibility. |
| Brain Parcellation Atlases | Define network nodes (ROIs) for connectivity analysis. | Schaefer Atlas (functionally-derived), AAL3 (anatomically-derived), Brainnetome [116] [113]. Choice affects results. |
| PET Radioligands | Target specific molecular pathways in vivo. | [18F]Flortaucipir (Tau), [11C]PIB / [18F]Florbetapir (Amyloid), [18F]FDG (Glucose Metabolism) [112]. |
| Multimodal Fusion Software | AI-powered platforms for integrated data analysis. | ADMV-Net [116], PySPI (for FC statistics) [114], custom Transformer-based frameworks [117] [115]. |
| Reference Datasets | Provide large-scale, multimodal data for training and validation. | Alzheimer's Disease Neuroimaging Initiative (ADNI), Human Connectome Project (HCP), AIBL [116] [118]. |
The integration of fMRI, PET, and optical data represents a paradigm shift in neuroscience, moving beyond the limitations of single-modality studies. Through rigorous cross-validation and the application of sophisticated, AI-powered fusion techniques, researchers can now construct unified models of brain function that span molecular, circuit, and systems levels. This integrated approach is indispensable for deconstructing the mechanisms of neuropsychiatric disorders, identifying robust, multimodal biomarkers for early diagnosis, and ultimately guiding the development of precise, effective therapeutics. The future of this field lies in standardizing these methodologies, fostering open data sharing, and continuing to innovate in computational fusion to fully realize the promise of precision medicine for the brain.
The transition from promising preclinical results to successful human clinical trials represents one of the most significant challenges in modern biomedical research, particularly in neuroscience. This transition failure, often termed the "valley of death," persists as a major obstacle in drug development. A comprehensive understanding of this phenomenon requires examining quantitative data on failure rates, analyzing methodological weaknesses in preclinical design, and implementing rigorous experimental protocols to enhance translational success. Within neurology specifically, recent evidence indicates that statistical misapplication in animal studies is strongly associated with subsequent failure in human trials, revealing a critical modifiable factor in the translational pathway [119]. This whitepaper examines the multifaceted reasons behind these failures and provides methodological guidance for strengthening preclinical research design.
Quantitative Analysis of Clinical Trial Attrition Rates
The drug development pipeline suffers from substantial attrition rates across all phases. Recent data indicate that only 6.7% of drugs entering Phase I trials ultimately receive regulatory approval. Success rates decline precipitously at each stage: Phase I to Phase II transitions occur at a 52% rate, Phase II to Phase III at 28.9%, and Phase III to approval at 57.8% [120]. These statistics translate to massive financial losses, with failed Phase III trials alone costing sponsors an estimated $800 million to $1.4 billion [120].
Table 1: Clinical Trial Success Rates by Phase
| Development Phase | Transition Success Rate | Primary Failure Causes |
|---|---|---|
| Preclinical to Phase I | 60% pass preclinical safety | Preclinical toxicity, species differences |
| Phase I to Phase II | 52% | Human-specific toxicity, pharmacokinetic issues |
| Phase II to Phase III | 28.9% | Lack of efficacy, poor endpoint selection |
| Phase III to Approval | 57.8% | Inadequate statistical power, safety concerns |
Comprehensive analysis reveals that pure clinical trial design issues account for approximately 35% of all failures—a substantially larger contribution than previously recognized. Meanwhile, limitations in animal model translation contribute to approximately 20% of clinical failures [120]. This suggests that approximately 60% of clinical trial failures (design issues plus recruitment/operational problems) are potentially preventable through improved methodology and planning, compared to only 20% attributable to limitations in animal models [120].
Table 2: Root Causes of Clinical Trial Failures
| Failure Category | Contribution to Overall Failures | Specific Issues |
|---|---|---|
| Pure Clinical Trial Design Issues | 35% | Flawed study design, inappropriate endpoints, poor patient selection |
| Recruitment & Operational Issues | 25% | Failed enrollment, site selection problems, operational complications |
| Animal Model Translation Limitations | 20% | Poor translation from preclinical models, species differences |
| Intrinsic Drug Safety/Efficacy Issues | 20% | True drug toxicity, fundamental lack of efficacy |
Statistical and Methodological Deficiencies in Preclinical Neuroscience Research
Statistical Misapplication in Neurological Animal Studies
Recent research specifically examining neurological indications (multiple sclerosis, Parkinson's disease, and epilepsy) reveals compelling evidence linking statistical practices in animal studies to human trial outcomes. In a modified meta-research, case-control study, animal studies preceding negative human trials demonstrated significantly higher rates of methodological deficiencies [119].
Key findings from the analysis of 70 rodent studies associated with 24 clinical trials revealed:
- Misapplication of cross-sectional tests to longitudinal data: 93% (95% CI 83-100) in animal studies preceding negative human trials versus 66% (95% CI 47-82) for positive trials [119]
- Use of plots concealing continuous data distributions: 98% (95% CI 95-100) in negative-trial associated studies versus 71% (95% CI 51-91) for positive trials [119]
- General statistical practice was poor or poorly reported across both groups, though notably worse in studies preceding failed trials [119]
Internal and External Factors Compromising Study Design
Research design faces numerous challenges that can compromise validity. Internal factors—those under a researcher's direct control—include hypothesis composition, selection of animal strain, sex and age, definition of experimental and control groups, proper statistical powering, dosing regimens, and sample collection timelines [121]. External pressures, including publication bias and career incentives, further compound these issues, often encouraging practices that prioritize novel, statistically significant findings over methodological rigor [121].
Experimental Protocols for Enhancing Translational Rigor
Protocol for Systematic Evaluation of Preclinical-to-Clinical Translation
The following methodology, adapted from Hogue et al., provides a framework for evaluating the translational potential of preclinical research [119]:
Objective: To assess whether negative clinical trials show a higher prevalence of statistical misapplication in preceding animal experiments compared to positive human trials.
Systematic Search Methodology:
- Clinical Trial Identification: Identify Phase 2 clinical trials (e.g., completed January 1, 2010-October 31, 2020) via ClinicalTrials.gov for specific neurological indications
- Animal Literature Search: Employ best practice methods to systematically search MEDLINE and Embase for animal experiments preceding the start of each human trial for each intervention and disease
- Data Extraction: Gather statistical reporting and decision-making data from animal articles by collectors blinded to human trial outcome
- Analysis: Compare rates of statistical mistakes between animal articles preceding positive versus negative human trials using weighted percentages and confidence intervals
Key Metrics for Statistical Assessment:
- Appropriate handling of longitudinal data (e.g., use of repeated measures ANOVA versus cross-sectional tests)
- Data visualization practices (concealment versus transparent display of distributions)
- Sample size justification and power calculations
- Handling of missing data and dropouts
- Appropriate correction for multiple comparisons
Protocol for Enhancing Statistical Rigor in Preclinical Studies
To address the identified statistical deficiencies, implement the following experimental protocol:
Pre-Study Design Phase:
- Power Analysis: Conduct a priori sample size calculations based on pilot data or literature effect sizes
- Randomization Scheme: Develop and document randomization procedures for animal assignment to groups
- Blinding Procedures: Implement blinding protocols for outcome assessment, particularly for subjective endpoints
- Statistical Analysis Plan: Pre-specify primary and secondary endpoints, statistical methods, and handling of missing data
Data Collection Phase:
- Longitudinal Data Management: For repeated measures, implement appropriate tracking systems and planned analysis methods
- Outlier Management: Predefine criteria for handling outliers before data collection
- Data Quality Checks: Implement regular quality control checks during data collection
Analysis and Reporting Phase:
- Appropriate Statistical Tests: Select tests based on data structure (e.g., mixed models for longitudinal data)
- Transparent Visualization: Use data representations that show distributions rather than concealing them
- Complete Reporting: Document all experimental details, including attrition, protocol deviations, and statistical methods
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Robust Preclinical Neuroscience Research
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Properly Powered Animal Cohorts | Ensures adequate statistical power to detect true effects | Calculate sample size using power analysis; consider attrition in long-term studies [121] |
| Multiple Animal Models | Addresses species-specific differences and improves translational predictability | Employ both rodent and non-rodent species where possible; select models with strongest pathophysiological relevance [122] |
| Longitudinal Data Analysis Software | Enables proper analysis of repeated measures data | Alternatives to cross-sectional tests; includes mixed-effects models and appropriate post-hoc analyses [119] |
| Blinding Protocols | Reduces experimental bias in outcome assessment | Critical for behavioral assessments and histopathological analyses; document implementation [121] |
| Standardized Behavioral Assays | Provides consistent, reproducible outcome measures | Validate for specific neurological conditions; ensure consistency across testing sessions and experimenters |
| Data Visualization Tools | Enables transparent representation of data distributions | Avoid bar graphs alone; use scatter plots with measures of variance, violin plots, or similar distribution representations [119] |
The "valley of death" in translational neuroscience remains a significant challenge, but quantitative evidence now identifies specific, modifiable factors contributing to this problem. While animal model limitations contribute to approximately 20% of clinical failures, statistical misapplication and poor experimental design in preclinical studies represent a substantial and addressable contributor to translational failure. The higher prevalence of statistical deficiencies in animal studies preceding negative human trials underscores the critical importance of methodological rigor in preclinical research. By implementing robust experimental protocols, enhancing statistical training, and adopting more rigorous standards for preclinical research, the scientific community can meaningfully improve the translation of promising preclinical findings into successful clinical interventions for neurological disorders.
Conclusion
In vivo techniques are indispensable for neuroscience research, providing unparalleled physiological relevance for understanding brain function and developing treatments for neurological diseases. The integration of foundational imaging methods with innovative approaches like in vivo SELEX and CAR-T generation represents a powerful trend. However, the translational pathway is fraught with challenges, including biological barriers, model standardization, and the critical differences between in vivo, in vitro, and ex vivo data. Success in bridging the 'valley of death' will depend on a more rigorous and integrated strategy. Future progress hinges on developing more predictive animal models, standardizing clinical outcome measures, creating advanced probes for specific cellular targets, and fostering collaborative frameworks that seamlessly connect basic discovery with clinical application. By systematically addressing these areas, the field can accelerate the delivery of effective therapies to patients.
References
- 1. In Vivo - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/in-vivo]
- 2. Editorial: In vivo investigations on neurological disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC9623258/]
- 3. Predicting In Vivo Efficacy from In Vitro Data - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7070804/]
- 4. In vivo analytical techniques facilitated by contemporary ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993621001138]
- 5. Optical brain imaging in vivo: techniques and applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2435254/]
- 6. Functional Near-infrared Spectroscopy (fNIRS) of Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3294084/]
- 7. Functional near-infrared spectroscopy [https://en.wikipedia.org/wiki/Functional_near-infrared_spectroscopy]
- 8. Two-Photon Functional Imaging of Neuronal Activity - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK20230/]
- 9. Multiphoton fluorescence microscopy for in vivo imaging [https://www.sciencedirect.com/science/article/pii/S0092867424008304]
- 10. Multimodal fluorescence-optoacoustic in vivo imaging of ... [https://www.sciencedirect.com/science/article/pii/S2213597924000880]
- 11. All-optical visualization of specific molecules in the ... [https://www.nature.com/articles/s41587-025-02905-4]
- 12. In vivo near-infrared fluorescent optical imaging for CNS ... [https://pubmed.ncbi.nlm.nih.gov/32396023/]
- 13. Optical brain imaging in vivo: techniques and applications from animal to man - PubMed [https://pubmed.ncbi.nlm.nih.gov/17994863/]
- 14. Hyperspectral imaging solutions for brain tissue metabolic and hemodynamic monitoring: past, current and future developments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5964611/]
- 15. Contrast agents in functional MR imaging [https://pubmed.ncbi.nlm.nih.gov/9039593/]
- 16. Strategies to Address Challenges in Neuroscience Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6600465/]
- 17. The Future of Targetable Synthetic Voltage Sensors [https://pmc.ncbi.nlm.nih.gov/articles/PMC11882369/]
- 18. II. Fast Quantitative Measurements With Voltage-Sensitive ... [https://www.sciencedirect.com/science/article/pii/S0006349599773832]
- 19. Evaluation of voltage-sensitive fluorescence dyes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4096138/]
- 20. Probing neuronal activity with genetically encoded calcium ... [https://www.sciencedirect.com/science/article/pii/S0168010224000762]
- 21. Voltage Sensitive Dye Imaging of Membrane Potential [https://www.scimedia.com/applications/voltage-imaging/voltage-sensitive-dye-imaging/]
- 22. The latest Neurophotonics products in 2025 [https://www.electrooptics.com/article/latest-neurophotonics-products]
- 23. Fluorescent Molecular Tools for Brain-Wide Neuroscience ... [https://www.mdpi.com/journal/molecules/special_issues/6901RSE96B]
- 24. Optical Imaging Modalities: Principles and Applications in ... [https://jnm.snmjournals.org/content/61/10/1419]
- 25. Research Area II: Molecular and Chemical Probes ... [https://ntc.columbia.edu/neuro-chemistry/]
- 26. In Vivo Imaging in Pharmaceutical Development and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5886324/]
- 27. Resolution in super-resolution microscopy – facts, artifacts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12148039/]
- 28. High-fidelity tissue super-resolution imaging achieved with ... [https://www.nature.com/articles/s41377-025-01930-x]
- 29. Comparison of the SMLM technique and the MSSR ... [https://pubmed.ncbi.nlm.nih.gov/38420882/]
- 30. Neuroscience and Neurobiology Solutions [https://www.moleculardevices.com/applications/neuroscience-neurobiology-solutions]
- 31. Accelerating drug discovery and development through in ... [https://www.sciencedirect.com/science/article/abs/pii/S0969805102003451]
- 32. Research Highlights in 2025 | Nature Reviews Neuroscience [https://www.nature.com/nrn/articles?type=research-highlight&year=2025]
- 33. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 34. Automated identification of mouse visual areas with intrinsic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5381647/]
- 35. SeeThrough: a rationally designed skull clearing technique ... [https://www.nature.com/articles/s41467-025-62836-1]
- 36. Quantitative comparison of functional MRI and direct ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3733359/]
- 37. Quantitative comparisons on hand motor functional areas ... [https://www.sciencedirect.com/science/article/pii/S2213158216300444]
- 38. Scientists reveal advance in brain research once thought ... [https://www.cnn.com/2025/04/15/science/3d-brain-map-mouse-mammal-breakthrough]
- 39. Advantages, applications, and future directions of in vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173102/]
- 40. Aptamer Technologies in Neuroscience, Neuro-Diagnostics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10934870/]
- 41. Aptamers Against Live Targets: Is In Vivo SELEX Finally ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7321788/]
- 42. Advantages, applications, and future directions of in vivo ... [https://www.sciencedirect.com/science/article/pii/S2162253125001295]
- 43. Methods for cell- and tissue-specific DNA aptamer selection [https://www.sciencedirect.com/science/article/pii/S2329050125000774]
- 44. Isolation, characterization and testing of RNA aptamers ... [https://www.nature.com/articles/s42003-025-08772-8]
- 45. Blocker-SELEX: a structure-guided strategy for developing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11310338/]
- 46. Using Color-Coding for Organized Sample Tracking [https://computype.com/blog/color-coding-for-organized-sample-tracking/?srsltid=AfmBOooD624z95H_0x26rPHiLjdgN0LY22j7S3AbJgCyVDeTd4iiv42O]
- 47. Animal models of stroke - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8446711/]
- 48. Animal models of Alzheimer's disease - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9700500/]
- 49. Animal models of Multiple Sclerosis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7094661/]
- 50. Veterinary medical care in rodent models of stroke [https://www.sciencedirect.com/science/article/pii/S0306452225000569]
- 51. Updates on mouse models of Alzheimer's disease [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-024-00712-0]
- 52. Comparative analysis of neuroinflammatory pathways in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12069400/]
- 53. In vivo imaging of the neurovascular unit in CNS disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4155511/]
- 54. covSTATIS: A multi-table technique for network neuroscience [https://apertureneuro.org/article/124518-covstatis-a-multi-table-technique-for-network-neuroscience]
- 55. Application of Functional Near-Infrared Spectroscopy to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5582298/]
- 56. Functional near-infrared spectroscopy in non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10883499/]
- 57. Functional Near-Infrared Spectroscopy and Its Clinical ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00724/full]
- 58. Diffuse optical tomography of the brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC11427210/]
- 59. Atlas‐guided volumetric diffuse optical tomography enhanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4282392/]
- 60. Diffuse optical tomography to investigate the newborn brain [https://www.nature.com/articles/pr2017107]
- 61. Data-guided neuroimaging and visualization [https://apertureneuro.org/article/140427-data-guided-neuroimaging-and-visualization-from-functional-decomposition-to-dynamic-fusion]
- 62. NIRS-BIDS: Brain Imaging Data Structure Extended to ... [https://www.nature.com/articles/s41597-024-04136-9]
- 63. In vivo production of CAR T cell - ScienceDirect.com [https://www.sciencedirect.com/science/article/pii/S2352304225001011]
- 64. In vivo CAR-T Therapy Challenges the Cancer Treatment ... [https://www.isctglobal.org/telegrafthub/blogs/isct-head-office1/2025/10/07/scientific-spotlight-in-vivo-car-t-therapy-challen]
- 65. CAR T-cells meet autoimmune neurological diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12313632/]
- 66. CAR-T cell therapy for cancer: current challenges and ... [https://www.nature.com/articles/s41392-025-02269-w]
- 67. Major advance in use of CAR-T cell therapy to treat solid ... [https://www.mayoclinic.org/medical-professionals/cancer/news/major-advance-in-use-of-car-t-cell-therapy-to-treat-solid-tumors/mac-20588405]
- 68. In vivo methods for imaging blood–brain barrier function and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931809/]
- 69. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 70. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 71. Blood-brain barrier modeling: challenges and perspectives [https://pmc.ncbi.nlm.nih.gov/articles/PMC4498345/]
- 72. 探针穿越血脑屏障策略和脑动力学荧光成像的进展 [https://www.muhn.edu.cn/ecmd/info/1512/20275.htm]
- 73. 跨越血脑屏障的生物大分子递送策略|BBB|大脑 - CN-Healthcare [https://www.cn-healthcare.com/articlewm/20220523/content-1360683.html]
- 74. Drug Delivery Across the Blood–Brain Barrier: A New Strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11677317/]
- 75. 药物递送策略:穿越、靶向或绕过血脑屏障 [https://www.ebiotrade.com/newsf/2025-11/20251104174618492.htm]
- 76. 黄芪多糖减轻大脑中动脉闭塞模型大鼠的血脑屏障损伤 [https://pmc.ncbi.nlm.nih.gov/articles/PMC9742771/]
- 77. In vivo nanocarrier detection methods in the brain and their ... [https://www.sciencedirect.com/science/article/pii/S0168365924003286]
- 78. Transport in the brain studied with in vivo two-photon ... [https://www.spiedigitallibrary.org/journals/neurophotonics/volume-12/issue-S2/S22806/Transport-in-the-brain-studied-with-in-vivo-two-photon/10.1117/1.NPh.12.S2.S22806.full]
- 79. Modeling of Cerebral Oxygen Transport Based on In vivo ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2016.00082/full]
- 80. Systematic comparison of methods for determining the in vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9646250/]
- 81. Quantitative Research Designs, Hierarchy of Evidence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056466/]
- 82. Types of Quantitative Research Methods and Designs [https://www.gcu.edu/blog/doctoral-journey/types-quantitative-research-methods-designs]
- 83. Experiments and Quantitative Research [https://researchmethodscommunity.sagepub.com/blog/experiments-quantitative-methodologies]
- 84. DEVELOPMENT AND APPROVAL COST ANALYSIS - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK603192/]
- 85. Cost-benefit analysis of in vivo reflectance confocal ... [https://www.dovepress.com/costbenefit-analysis-of-in-vivo-reflectance-confocal-microscopy-for-me-peer-reviewed-fulltext-article-RMHP]
- 86. High-throughput synaptic connectivity mapping using in ... [https://www.nature.com/articles/s41593-025-02024-y]
- 87. Data visualization in the neurosciences - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4427844/]
- 88. Meta-Research: Lessons from a catalogue of 6674 brain ... [https://elifesciences.org/articles/66388]
- 89. Common Data Model for Neuroscience ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC134589/]
- 90. Age matters - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2761206/]
- 91. Animal models in neuroscience with alternative approaches [https://pmc.ncbi.nlm.nih.gov/articles/PMC11680486/]
- 92. Experimental Design: The Complete Pocket Guide [https://imotions.com/blog/learning/research-fundamentals/experimental-design/?srsltid=AfmBOorTsRqT9a3mieB1vCMFsOhTUzfwQ4hL6RUJ7fKwS27qji_PzQJv]
- 93. Unsupervised quantification of naturalistic animal ... [https://www.sciencedirect.com/science/article/abs/pii/S0959438821000891]
- 94. Putting the “Biology” Back into “Neurobiology” [https://www.frontiersin.org/journals/systems-neuroscience/articles/10.3389/fnsys.2016.00069/full]
- 95. Mitigating off-target effects of small RNAs [https://pubmed.ncbi.nlm.nih.gov/39293936/]
- 96. evaluating and mitigating off-target effects in CRISPR gene ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1339189/full]
- 97. Improved specificity and efficiency of in vivo adenine base ... [https://www.nature.com/articles/s41551-025-01545-y]
- 98. Current state of in vivo panning technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC6512807/]
- 99. Experimental Design: The Complete Pocket Guide [https://imotions.com/blog/learning/research-fundamentals/experimental-design/?srsltid=AfmBOooQffiKzvcnL8054rChvFBta-r09LvCtgxus_D0qxECRv0xsDzh]
- 100. In Vitro vs In Vivo: Complete Comparison + Selection Guide [https://www.assaygenie.com/in-vitro-vs-in-vivo-complete-comparison-selection-guide-research-methods/?srsltid=AfmBOor5LVeSc5s-i20Yg-wXF0YZgkXvhZAk_TLxuyIeccKbLN6DWFsb]
- 101. In Vivo vs. In Vitro Models: Key Differences and ... [https://liveonbiolabs.com/in-vivo-vs-in-vitro-models/]
- 102. MIT researchers invent new human brain model to enable ... [https://news.mit.edu/2025/researchers-invent-human-brain-model-to-enable-disease-research-drug-discovery-1105]
- 103. In Vitro vs In Vivo: A History of Modern Cell Culture [https://emulatebio.com/in-vitro-vs-in-vivo-cell-culture/]
- 104. Limitations of ex vivo measurements for in vivo neuroscience [https://pubmed.ncbi.nlm.nih.gov/28461475/]
- 105. Anatomical insights into the superior longitudinal system ... [https://www.nature.com/articles/s42003-025-08774-6]
- 106. Organotypic brain slice cultures to model neurodegenerative ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-019-0346-0]
- 107. Human brain slice cultures: translational applications and ... [https://www.life-science-alliance.org/content/8/12/e202403160]
- 108. Human brain slice cultures: translational applications and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511760/]
- 109. Human organotypic brain slice cultures: a detailed and ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027023002741]
- 110. Human post-mortem organotypic brain slice cultures: a tool to ... [https://actaneurocomms.biomedcentral.com/articles/10.1186/s40478-024-01784-1]
- 111. Three-dimensional organotypic mouse brain slices to study ... [https://www.frontiersin.org/journals/dementia/articles/10.3389/frdem.2025.1585124/full]
- 112. Advanced Imaging Techniques (PET, fMRI, DTI) in Early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245986/]
- 113. Systematic evaluation of fMRI data-processing pipelines for ... [https://www.nature.com/articles/s41467-024-48781-5]
- 114. Benchmarking methods for mapping functional connectivity ... [https://www.nature.com/articles/s41592-025-02704-4]
- 115. AI-powered integration of multimodal imaging in precision ... [https://www.sciencedirect.com/science/article/pii/S2666379125002058]
- 116. A multi-view multimodal deep learning framework for ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1658776/full]
- 117. A review of deep learning-based information fusion ... [https://www.sciencedirect.com/science/article/pii/S0010482524007200]
- 118. Brain functional connectivity analysis of fMRI-based ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1540297/full]
- 119. Association of Statistical Methodology and Design ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/41082697/]
- 120. Why the Majority of Clinical Trials Fail: Beyond Animal ... [https://www.linkedin.com/pulse/why-majority-clinical-trials-fail-beyond-animal-pure-stefano-lzdxf]
- 121. In Vivo Study Design Challenges [https://www.taconic.com/resources/in-vivo-study-design-challenges]
- 122. The 90% myth [https://www.understandinganimalresearch.org.uk/news/the-90-myth]