Dopamine Challenge Studies: A Comprehensive Guide to Pharmacological Probing of Human Reward Pathways for Research & Drug Development
This comprehensive review explores pharmacological challenge studies as a critical tool for investigating dopamine-mediated reward functioning in humans.
Dopamine Challenge Studies: A Comprehensive Guide to Pharmacological Probing of Human Reward Pathways for Research & Drug Development
Abstract
This comprehensive review explores pharmacological challenge studies as a critical tool for investigating dopamine-mediated reward functioning in humans. Aimed at researchers, scientists, and drug development professionals, it covers foundational theories linking dopamine to motivation and hedonia, details methodological protocols using agonists (e.g., amphetamine, L-DOPA) and antagonists, and discusses advanced neuroimaging integration (PET, fMRI). The article addresses key troubleshooting considerations for safety, blinding, and individual variability. It further validates these methods by comparing them with genetic, lesion, and computational approaches, and examines their translational application in psychiatric disorders like depression, schizophrenia, and addiction. This synthesis provides a roadmap for designing rigorous studies to advance neuropharmacology and therapeutic innovation.
The Dopamine-Reward Nexus: Core Theories and Rationale for Pharmacological Probing in Humans
Historical Context
Pharmacological challenge studies involve the controlled administration of a psychoactive agent to probe neurochemical systems and observe resultant behavioral, physiological, or neurobiological changes. Their history is deeply interwoven with the evolution of psychopharmacology and neuropsychiatry.
- 1950s-1960s (Origins): Emerged from early experiments with lysergic acid diethylamide (LSD) and amphetamine, which were used to model psychosis and study monoamine systems.
- 1970s-1980s (Systematization): The paradigm formalized with challenges using specific receptor agonists/antagonists (e.g., apomorphine for dopamine, fenfluramine for serotonin) to test hypotheses about neurotransmitter dysfunction in psychiatric disorders.
- 1990s-Present (Integration with Neuroimaging): Revolutionized by coupling with PET, SPECT, and fMRI, allowing direct in vivo assessment of neurotransmitter release, receptor occupancy, and region-specific brain activity in response to a challenge. This period solidified its role in drug development for validating target engagement.
Within dopamine and reward research, challenges like amphetamine (dopamine releaser) or methylphenidate (dopamine transporter blocker) became key tools for probing the mesolimbic and mesocortical pathways, linking dopamine signaling to motivation, reinforcement, and hedonic response.
Core Principles
- Pharmacological Specificity: The challenge agent should have a well-defined and primary action on the target system (e.g., dopamine transporter blockade).
- Hypothesis-Driven: The study must test a clear hypothesis regarding the system's functional state or its role in a behavioral domain.
- Controlled Administration: Use of placebo-controlled, often double-blind, designs to isolate the drug's effect from expectancy.
- Multimodal Assessment: Measurement of response across levels: neurochemical (e.g., PET), physiological (e.g., heart rate), behavioral (e.g., task performance), and subjective (e.g., self-report).
- Safety & Ethics: Rigorous screening and monitoring are paramount due to the intentional induction of transient neurochemical alteration.
Application Notes & Protocols in Dopamine/Reward Research
Application Note AN-01: Assessing Dopaminergic Capacity with an Amphetamine Challenge
Objective: To measure dopamine release capacity and its correlation with reward task performance. Rationale: d-amphetamine induces dopamine release by reversing transport through the dopamine transporter (DAT). The magnitude of change in dopamine receptor binding potential (ΔBP) on PET or the change in BOLD signal in reward regions on fMRI serves as an index of presynaptic dopamine capacity.
Table 1: Representative Quantitative Data from Amphetamine Challenge PET Studies
| Brain Region (ROI) | Baseline BPND (Mean ± SD) | Post-Amphetamine BPND (Mean ± SD) | ΔBPND (%) | Associated Behavioral Change (r-value) |
|---|---|---|---|---|
| Ventral Striatum | 2.65 ± 0.41 | 2.15 ± 0.38 | -18.9 ± 5.2 | Reward Learning (r = 0.52) |
| Dorsal Caudate | 2.89 ± 0.35 | 2.55 ± 0.33 | -11.8 ± 4.1 | N/A |
| Anterior Cingulate | 1.12 ± 0.21 | 1.05 ± 0.20 | -6.3 ± 3.5 | Subjective "High" (r = 0.48) |
BPND: Non-displaceable binding potential; ΔBPND calculated as (Post-BP - Baseline BP) / Baseline BP. Data synthesized from recent literature (2020-2023).
Protocol P-01: Combined Amphetamine-fMRI Challenge for Reward Circuit Function
Title: Protocol for Assessing Dopamine-Mediated Reward Circuitry Reactivity.
1. Pre-Study Screening & Preparation
- Screening: Full medical/psychiatric evaluation, ECG, urine toxicology, pregnancy test. Exclude for cardiovascular risk, psychiatric history, or drug use.
- Pharmacological Agent: d-amphetamine (0.3 mg/kg oral). Prepare identical placebo capsules.
- Design: Randomized, double-blind, placebo-controlled, crossover (≥1-week washout).
2. Experimental Session Timeline
- T-60 min: Participant arrival, baseline vitals, final eligibility check.
- T-45 min: Administer capsule (amphetamine or placebo).
- T 0 min (Peak Plasma Time): Begin fMRI scan with reward task (e.g., Monetary Incentive Delay).
- T+90 min: Subjective effects scales (e.g., ARCI, VAS), debriefing.
- Continuous Monitoring: Heart rate and blood pressure every 30 minutes.
3. fMRI Acquisition & Task Parameters
- Scanner: 3T MRI.
- Sequence: T2*-weighted EPI, TR/TE = 2000/30 ms, voxel size = 3x3x3 mm.
- Task: Monetary Incentive Delay (MID). Block or event-related design. Contrast BOLD signal for reward anticipation (Cue) and outcome (Feedback) vs. neutral trials.
4. Data Analysis Pipeline
- Preprocessing: Slice-time correction, realignment, co-registration, normalization, smoothing (6mm FWHM).
- 1st Level: General Linear Model (GLM) for task conditions. Primary contrast: [Reward Anticipation > Neutral].
- 2nd Level: Flexible factorial model comparing the reward contrast between Amphetamine and Placebo sessions. Region of Interest (ROI) analysis for ventral striatum.
Protocol P-02: Dopamine Depletion Challenge via Acute Phenylalanine/Tyrosine Depletion (APTD)
Title: Protocol for Transient Reduction of Dopamine Synthesis.
1. Rationale & Mixture Preparation
- APTD uses an amino acid mixture lacking the dopamine precursors phenylalanine and tyrosine, acutely lowering central dopamine synthesis. A balanced control mixture (BAL) is identical but contains these precursors.
- APTD Mixture: ~100g mixture of 15 amino acids excluding Phe and Tyr. BAL Mixture: Contains 10.2g Phe and 6.7g Tyr.
2. Experimental Session
- Day Before: Low-protein diet.
- T-300 min (5 hrs pre-test): After overnight fast, consume amino acid mixture (flavored, chilled).
- T-60 to T 0 min: Rest period. Plasma amino acid levels can be sampled.
- T 0 min: Begin behavioral testing (e.g., probabilistic reinforcement learning task, effort expenditure task). Subjective mood ratings.
- Post-Test: High-protein meal provided.
3. Primary Outcome Measures
- Behavioral: Learning rate in reward vs. punishment conditions, choice of high-effort/high-reward options.
- Subjective: Profile of Mood States (POMS), visual analog scales for motivation/fatigue.
- Biochemical (Optional): Plasma Phe/Tyr levels to confirm depletion.
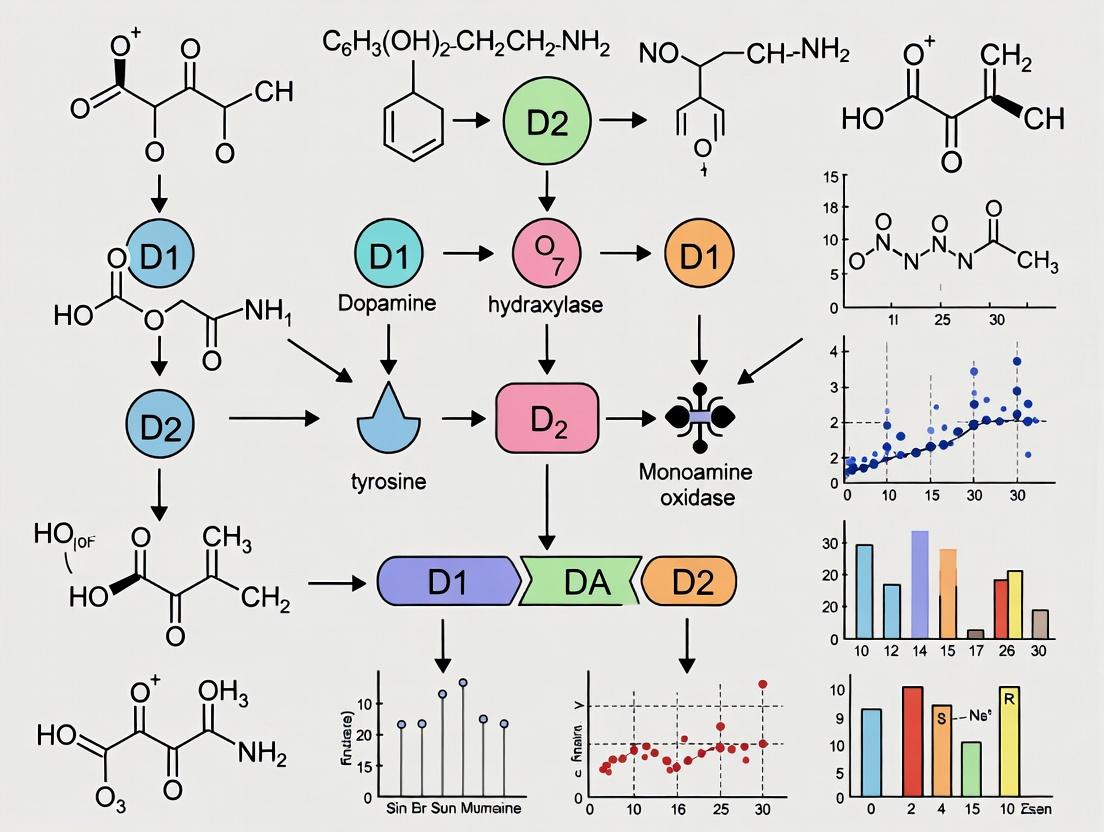
Visualizations
Title: Pharmacological Challenge Study Core Workflow
Title: Amphetamine Mechanism: Increased Synaptic Dopamine
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Dopamine Challenge Studies
| Item/Category | Example(s) | Function & Rationale |
|---|---|---|
| Challenge Agents | d-amphetamine sulfate; methylphenidate HCl; levodopa/carbidopa; α-methyl-p-tyrosine (AMPT); APTD amino acid mixtures. | Primary pharmacological tool to directly stimulate, block, or deplete the dopamine system in a controlled manner. |
| Radiotracers (for PET) | [¹¹C]Raclopride (D2/D3 antagonist); [¹¹C]PHNO (D3-preferring agonist); [¹¹C]-(+)-PHNO (for DA release). | Quantifies baseline receptor availability and changes (ΔBPND) following a challenge, indicating dopamine release. |
| fMRI Reward Tasks | Monetary Incentive Delay (MID); Probabilistic Reward Task; Reinforcement Learning Tasks. | Standardized behavioral probes to elicit BOLD activity in reward circuits (VS, vmPFC) during anticipation and outcome. |
| Subjective Effects Scales | Addiction Research Center Inventory (ARCI); Visual Analog Scales (VAS) for 'High', 'Wanting', 'Liking'; Profile of Mood States (POMS). | Measures the conscious, experiential effects of the challenge drug, linking neurochemistry to subjective state. |
| Biochemical Assays | HPLC/MS kits for plasma amphetamine, prolactin (indirect DA measure), and phenylalanine/tyrosine (for APTD). | Verifies compliance, pharmacokinetics, and biochemical efficacy of the challenge manipulation. |
| Safety Monitoring | ECG machine; automated sphygmomanometer; structured medical interview (e.g., SCID). | Ensures participant safety, a non-negotiable requirement when administering psychoactive drugs. |
Application Notes
Dopamine's role in reward has evolved from a simple "pleasure" signal to a complex neural currency for reward prediction error (RPE), motivation, and incentive salience. This conceptual shift is central to pharmacological challenge studies in humans, which probe the integrity of dopamine pathways to understand psychopathology (e.g., addiction, anhedonia, depression) and optimize therapeutic interventions.
Key Conceptual Shifts:
- From Hedonia to Motivation: Dopamine is less about conscious pleasure (liking) and more about wanting (motivation) and learning.
- Reward Prediction Error (RPE): Dopamine neurons signal the difference between received and predicted reward. Positive RPE (better than expected) increases firing; negative RPE (worse than expected) suppresses it.
- Pathway-Specific Functions: The mesolimbic, mesocortical, and nigrostriatal pathways mediate distinct aspects of reward processing, decision-making, and habit formation.
Thesis Context: Pharmacological challenges (e.g., agonists like amphetamine, antagonists like haloperidol, precursor depletion via AMPT) allow researchers to manipulate dopaminergic transmission and observe subsequent changes in behavior, neural activity (fMRI), and subjective states. This is crucial for testing computational models of RPE, quantifying motivational deficits, and evaluating novel drug targets.
Summarized Quantitative Data
Table 1: Effects of Pharmacological Challenges on Key Behavioral & Neural Measures
| Pharmacological Agent | Primary Action | Typical Dose in Human Studies | Effect on Subjective Reward | Effect on RPE Signaling (fMRI BOLD in Ventral Striatum) | Key Reference Paradigm |
|---|---|---|---|---|---|
| d-amphetamine | DA release agonist | 0.3-0.5 mg/kg (oral) | ↑ Euphoria, ↑ 'Wanting' | Significant potentiation of positive RPE signal | Monetary Incentive Delay (MID), Probabilistic Reward Task |
| Methylphenidate | DA reuptake inhibitor | 0.5 mg/kg (oral) | ↑ Alertness, mild euphoria | Moderate potentiation of RPE signal | Reinforcement Learning Task |
| Haloperidol (acute) | D2 receptor antagonist | 2-3 mg (oral) | ↓ Pleasure, ↓ motivation, anhedonia-like state | Attenuation of positive RPE signal | Effort Expenditure for Rewards Task (EEfRT) |
| Alpha-methyl-para-tyrosine (AMPT) | Catecholamine synthesis inhibitor | ~40-45 mg/kg over 24-48 hrs | Increased fatigue, reduced positive affect | Significant reduction in ventral striatal reward anticipation | MID Task, Pavlovian Conditioning |
| L-DOPA | DA precursor | 100/25 mg (w/ carbidopa) | Variable; can enhance learning | Can enhance neural learning signals in striatum | Instrumental Learning Task |
Table 2: Key Dopamine Pathway Characteristics & Functions
| Pathway | Origin | Primary Projections | Key Function in Reward | Dysfunction Implicated In |
|---|---|---|---|---|
| Mesolimbic | Ventral Tegmental Area (VTA) | Nucleus Accumbens (NAcc), amygdala, hippocampus | RPE, incentive salience, 'wanting', initial reward learning | Addiction, Schizophrenia (positive symptoms) |
| Mesocortical | Ventral Tegmental Area (VTA) | Prefrontal cortex (PFC), anterior cingulate cortex (ACC) | Executive control, value representation, goal-directed behavior, integrating RPE | Schizophrenia (cognitive symptoms), ADHD, Depression |
| Nigrostriatal | Substantia Nigra pars compacta | Dorsal striatum (caudate, putamen) | Habit formation, action selection, sensorimotor coordination | Parkinson's Disease, OCD |
Experimental Protocols
Protocol 1: Pharmacological fMRI Study of Dopamine and Reward Prediction Error
Objective: To assess how a dopaminergic agonist (e.g., d-amphetamine) modulates RPE signaling in the ventral striatum during a probabilistic reinforcement learning task.
Materials:
- Double-blind, placebo-controlled drug administration kit.
- Oral d-amphetamine (0.3 mg/kg) or matched placebo.
- 3T MRI scanner with compatible task presentation system.
- Physiological monitoring equipment (pulse oximeter, blood pressure cuff).
Procedure:
- Screening & Consent: Screen participants for MRI contraindications and medical/psychiatric exclusions. Obtain informed consent.
- Drug Administration: At time T=0, administer orally either d-amphetamine or placebo under double-blind conditions.
- Peak Plasma Timing: Allow 90-120 minutes for drug plasma concentration to peak.
- fMRI Task: Place participant in scanner. Perform structural scan. Conduct functional scans during a Probabilistic Reward Task:
- On each trial, participants choose between two abstract symbols with fixed, counterbalanced reward probabilities (e.g., 70/30).
- Choice is followed by visual feedback (reward or no reward).
- A computational model (e.g., Rescorla-Wagner) is used to trial-by-trial estimate the RPE for each participant.
- Data Analysis: Preprocess fMRI data (realignment, normalization, smoothing). Model the BOLD response in the ventral striatum using the time-series of estimated RPE as a parametric regressor. Compare the strength (beta weight) of this RPE signal between drug and placebo conditions using a second-level group analysis (e.g., SPM, FSL).
Protocol 2: Dopamine Depletion and Effort-Based Decision Making
Objective: To evaluate the causal role of dopamine in motivating effortful choices for rewards using the catecholamine depletion agent AMPT.
Materials:
- Alpha-methyl-para-tyrosine (AMPT).
- Placebo capsules (e.g., lactose).
- Effort Expenditure for Rewards Task (EEfRT) on a testing computer.
- Visual Analog Scales (VAS) for mood/fatigue.
- Actigraphy watch to monitor motor activity/sedation.
Procedure:
- Baseline & Depletion: Participants complete a 2-day inpatient protocol.
- Day 1 (Baseline): After acclimation, perform EEfRT task and complete VAS.
- Depletion Phase: Begin oral AMPT administration (e.g., 1g every 6 hours over 24-48 hours) to achieve steady-state depletion. Placebo group receives matched regimen.
- Post-Depletion Testing: On Day 2, after confirmed depletion (typically 24-48 hrs after first dose), repeat EEfRT task and VAS.
- EEfRT Task Design:
- On each trial, participants choose between a 'Hard Task' (e.g., rapid button presses within a short time) for a higher monetary reward ($1.00-$4.00) and an 'Easy Task' (slower button presses) for a lower, guaranteed reward ($0.50).
- Reward magnitude and probability of winning for the Hard Task are varied across trials.
- Data Analysis: Primary outcome is the proportion of Hard Task choices. Analyze using mixed-effects logistic regression with factors Drug (AMPT vs. Placebo), Reward Magnitude, and Reward Probability. Expect AMPT to selectively reduce Hard Task choices, particularly at intermediate reward probabilities, indicating reduced willingness to expend effort.
Diagrams
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Human Dopamine Challenge Studies
| Item / Reagent | Function in Research | Example Use Case & Notes |
|---|---|---|
| d-amphetamine | Potent dopamine/norepinephrine releaser. Increases synaptic DA. | Gold-standard agonist challenge to probe DA system capacity and RPE enhancement. Monitor cardiovascular effects. |
| Haloperidol | High-potency D2 receptor antagonist. Blocks DA signaling. | Used to acutely dampen DA transmission, modeling motivational deficits and anhedonia. |
| Alpha-methyl-para-tyrosine (AMPT) | Competitive inhibitor of tyrosine hydroxylase. Depletes DA/NE. | Chronic depletion model to study DA's role in effort, reward, and mood without acute receptor blockade side effects. |
| L-DOPA/Carbidopa | DA precursor (with peripheral decarboxylase inhibitor). Increases DA synthesis. | Used to study enhancement of learning-related DA signals, particularly in aging or Parkinson's disease. |
| [11C]Raclopride / [11C]PHNO | Radioligands for Positron Emission Tomography (PET). | Quantifies D2/D3 receptor binding potential (BPND). Used to measure receptor occupancy after drug challenge or in patient groups. |
| Monetary Incentive Delay (MID) Task | fMRI paradigm probing reward anticipation and outcome. | Evokes robust BOLD activity in ventral striatum. A standard for studying reward anticipation deficits. |
| Probabilistic Reinforcement Learning Task | Behavioral/fMRI paradigm for trial-by-toy RPE estimation. | Paired with computational modeling to extract a pure RPE signal for analysis of dopaminergic learning. |
| Effort Expenditure for Rewards Task (EEfRT) | Behavioral measure of effort-based decision making. | Sensitive to dopamine manipulations (AMPT, antipsychotics). Measures motivation, not just learning. |
| Computational Models (e.g., Rescorla-Wagner) | Algorithm to quantify latent variables like RPE and value. | Essential for moving beyond simple behavior to test theories of dopaminergic computation in the brain. |
Anhedonia, incentive salience, and effort-based decision-making are distinct but interconnected constructs for probing reward system dysfunction, particularly relevant to dopaminergic pharmaco-challenge studies. Anhedonia reflects a diminished capacity to experience pleasure (consummatory hedonia) or a lack of motivation to pursue rewards (motivational anhedonia). Incentive salience ("wanting") is a dopamine-dependent process attributing motivational value to cues predicting rewards. Effort-based decision-making evaluates the willingness to expend cognitive or physical effort for rewards. In pharmacological studies, these frameworks allow dissociation of dopamine's role in reward anticipation, valuation, and cost-benefit integration.
Table 1: Key Behavioral & Neuroimaging Tasks by Framework
| Framework | Primary Task(s) | Key Dependent Variable(s) | Associated Dopaminergic Pathway |
|---|---|---|---|
| Anhedonia | Snaith-Hamilton Pleasure Scale (SHAPS); Temporal Experience of Pleasure Scale (TEPS) | Self-reported anticipatory/consummatory pleasure scores | Mesolimbic (NAc to VTA) |
| Incentive Salience | Pavlovian Instrumental Transfer (PIT); Probabilistic Reward Task (PRT) | Response bias toward rewarded stimulus; cue-induced effort invigoration | Mesolimbic (VTA to NAc core) |
| Effort-Based Decision Making | Effort Expenditure for Rewards Task (EEfRT); Physical/Mental Effort Discounting | Proportion of high-effort choices; discounting rate for effort | Mesolimbic-mesocortical (NAc to ACC, VTA to dlPFC) |
Table 2: Typical Pharmacological Challenge Effects on Task Performance
| Drug (Dopaminergic Action) | Anhedonia (TEPS Score) | Incentive Salience (PIT Effect) | Effort Choice (EEfRT High-Effort %) |
|---|---|---|---|
| d-amphetamine (DA release promoter) | or slight ↑ in anticipatory | ↑↑ | ↑ (esp. at moderate reward) |
| Pramipexole (D2/D3 agonist) | ↑ (low dose) / ↓ (high dose) | ↓ (high dose causes aversion) | |
| Haloperidol (D2 antagonist) | ↓ anticipatory | ↓↓ | ↓↓ (blunts reward sensitivity) |
| Levodopa (precursor) | consummatory | ↑ | or slight ↑ |
Experimental Protocols
Protocol 1: Assessing Incentive Salience with Pavlovian Instrumental Transfer (PIT)
Objective: To measure the extent to which a reward-predictive cue invigorates instrumental responding, a proxy for incentive salience. Materials: Computer task, response box, pharmacological agent/placebo. Procedure:
- Pavlovian Training (Day 1): Participants learn associations between distinct visual cues (CS+, CS-) and a monetary reward (unconditioned stimulus, US). CS+ always predicts reward delivery; CS- predicts nothing.
- Instrumental Training (Day 2): Participants learn to perform a specific action (e.g., button press) to earn the same monetary reward (free of cues).
- Transfer Test (Day 3, post-drug administration): In an extinction phase (no rewards delivered), CS+ and CS- are presented while the instrumental action remains available. The critical measure is the rate of button pressing during CS+ vs. CS- periods. Analysis: Compare response rate difference (CS+ - CS-) between drug and placebo conditions. A greater difference indicates enhanced incentive salience.
Protocol 2: Effort-Based Decision Making using the Effort Expenditure for Rewards Task (EEfRT)
Objective: To quantify the effect of dopaminergic manipulation on willingness to expend physical effort for varying reward magnitudes and probabilities. Materials: Computer task, sequential button press device, pharmacological agent/placebo. Procedure:
- Task Structure: On each trial, participants choose between an "Easy Task" (low effort, 30 button presses in 7 seconds) for a small reward, or a "Hard Task" (high effort, 100 button presses in 21 seconds) for a larger reward.
- Independent Variables: Reward magnitude (low, high) and probability of winning (12%, 50%, 88%) are titrated across trials.
- Administration: Task is performed after drug plasma concentration peaks (e.g., 60-90 mins post oral amphetamine).
- Trial Count: Typically 150-200 trials, spanning ~45 minutes. Analysis: Use hierarchical logistic regression to model the probability of choosing the hard task as a function of reward magnitude, probability, drug condition, and their interactions. A significant drug × reward magnitude interaction indicates altered effort-cost computation.
Visualizations
Title: Dopamine, Brain Regions, and Reward Frameworks
Title: Pavlovian Instrumental Transfer (PIT) Protocol Flow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pharmaco-Challenge Reward Studies
| Item / Reagent | Function & Rationale | Example Product / Specification |
|---|---|---|
| d-Amphetamine Sulfate | DA/Norepinephrine releasing agent; gold standard for probing DA system responsivity in healthy controls. | Prescription-grade, compounded for precise dosing (e.g., 0.3-0.45 mg/kg oral). |
| Dopamine D2/D3 Agonist (e.g., Pramipexole) | Probes contribution of autoreceptor vs. post-synaptic receptor stimulation; low vs. high dose has biphasic effects. | Pharmaceutical grade, dose range 0.25-0.5 mg (low), 1.0-1.5 mg (high). |
| D2 Antagonist (e.g., Haloperidol) | Acute DA blockade model to induce transient anhedonia/blunted incentive salience for baseline comparison. | Low dose (1-3 mg oral) to minimize sedation/extrapyramidal effects. |
| Probabilistic Reward Task (PRT) Software | Quantifies reinforcement learning and response bias, a behavioral marker of reward sensitivity. | Open-source (e.g., Psytoolkit, PsychoPy) or commercial (E-Prime) implementations. |
| EEfRT Apparatus | Standardized hardware for measuring physical effort expenditure. | Customizable button box or validated software with dynamic response checking. |
| Salivary Cortisol/Alpha-Amylase Kits | Controls for stress/arousal confounds introduced by pharmacological challenge. | Salivette collection devices with ELISA/Luminescence analysis. |
| Plasma Catecholamine Analysis Kit | Verifies peripheral physiological impact of DA challenge (correlate with central effect). | LC-MS/MS based kits for plasma DA, NE, and metabolites (HVA, DOPAC). |
| fMRI-Compatible Reward Task Paradigms | Links behavioral measures (PIT, EEfRT) with BOLD signal in NAcc, ACC, VTA. | Pre-optimized task scripts for major scanner platforms (Siemens, GE, Phillips). |
Pharmacological challenge studies probing dopamine (DA) and reward functioning are central to understanding psychiatric and neurological disorders. Despite robust preclinical findings from animal models, a significant translational gap persists, with many candidate therapeutics failing in human clinical trials. This document outlines the rationale for integrating human and animal studies and provides practical application notes and protocols to enhance translational validity.
Quantitative Comparison: Key Disparities and Commonalities
Table 1: Comparative Metrics in DA Challenge Studies
| Metric | Rodent Models | Non-Human Primates (NHPs) | Human Studies | Translational Fidelity |
|---|---|---|---|---|
| DA Receptor Distribution (Striatum) | D1:D2 ~1.2:1 | D1:D2 ~1.5:1 | D1:D2 ~1.5:1 | NHP ≈ Human > Rodent |
| DA Synthesis Capacity (ng/mg tissue/hr) | ~3.5 (Striatum) | ~1.8 (Caudate) | ~1.5 (Caudate, PET estimate) | Quantitative, not qualitative, differences |
| Metabolic Rate (Basal) | High (~7x human) | Moderate (~2x human) | Baseline | Critical for dose extrapolation |
| Behavioral Paradigm | Lever pressing, maze navigation | Delayed response, social reward | Monetary incentive delay (MID), gambling tasks | NHP tasks more analogous to human fMRI paradigms |
| Pharmacokinetic Half-life (Example: Amphetamine) | ~1 hour | ~4 hours | ~10-12 hours | Major source of translational disconnect |
Table 2: Success Rates in Translational Phases for CNS Drugs (2020-2024)
| Phase Transition | Overall Success Rate | Success Rate with Integrated Human/Animal Biomarkers |
|---|---|---|
| Preclinical → Phase I | 62% | 68% |
| Phase I → Phase II | 52% | 59% |
| Phase II → Phase III | 29% | 41% |
| Phase III → Submission | 58% | 63% |
Experimental Protocols
Protocol A: Integrated Cross-Species DA Challenge with Biomarker Correlation Objective: To assess the dose-response of a novel D2/3 partial agonist on reward-related behavior and neurochemical release, correlating across species. Species: Mouse, Non-Human Primate (Rhesus macaque), Human. Part 1: Rodent Protocol (Fast-Scan Cyclic Voltammetry - FSCV)
- Animal Preparation: Implant a carbon-fiber microelectrode into the nucleus accumbens core of anesthetized adult C57BL/6J mouse.
- Pharmacological Challenge: Administer vehicle or test compound (0.1, 0.3, 1.0 mg/kg, i.p.) 30 min prior to experiment.
- Stimulation & Recording: Apply electrical stimulation (60 Hz, 60 pulses) to the medial forebrain bundle. Record DA transient via FSCV (waveform: -0.4 V to +1.3 V to -0.4 V, 400 V/s).
- Data Analysis: Quantify peak [DA] and signal decay constant (tau). Compare across doses.
Part 2: Non-Human Primate Protocol (PET with [¹¹C]Raclopride)
- Subject Preparation: Anesthetize NHP with ketamine/isoflurane. Position in PET scanner.
- Baseline Scan: Administer IV bolus of [¹¹C]Raclopride (~5 mCi). Conduct 60-minute dynamic PET scan.
- Challenge Scan: After 4-hour washout, administer test compound (dose scaled by allometric PK model). Repeat [¹¹C]Raclopride injection and scan 60 minutes post-drug.
- Data Analysis: Calculate binding potential (BP
ND) in ventral striatum using simplified reference tissue model (SRTM). Percent displacement indicates DA release.
Part 3: Human Protocol (fMRI with Pharmacological Challenge)
- Subject Screening: Healthy volunteers, genotyped for COMT Val158Met. Double-blind, placebo-controlled design.
- Session Design: Visit 1 (Placebo) and Visit 2 (Therapeutic dose from NHP PK/PD model). Oral administration 2 hours pre-scan.
- fMRI Task: Conduct Monetary Incentive Delay (MID) task in 3T scanner. Block design with Cue, Anticipation, and Outcome phases.
- Analysis: Model BOLD response in ventral striatum during anticipation of high reward vs. neutral cue. Compare drug vs. placebo.
Protocol B: In Vitro Binding Profile for Lead Candidate Objective: To establish receptor affinity and selectivity profile to de-risk translational planning.
- Membrane Preparation: Use HEK-293 cells stably expressing human DA receptors (D1-D5, others).
- Radioligand Binding Assay: Incubate test compound (10 pM–10 µM, 12 concentrations) with membrane homogenate and radioligand ([³H]SCH-23390 for D1, [³H]Spiperone for D2, etc.) in binding buffer for 1 hr at 25°C.
- Termination & Detection: Rapid vacuum filtration through GF/B filters. Measure bound radioactivity via scintillation counting.
- Data Analysis: Calculate Ki values using Cheng-Prusoff equation. Compile selectivity ratio table (D2/D1, D2/5-HT
2A, etc.).
Visualizing the Translational Workflow & DA Pathway
Diagram Title: Cross-Species Translational Workflow for DA Drugs
Diagram Title: Key Dopamine Signaling Pathways in Reward
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Integrated DA Studies
| Item/Catalog (Example) | Function & Application | Key Consideration |
|---|---|---|
| Carbon-fiber microelectrodes | In vivo detection of DA via FSCV in rodents. | Tip diameter (5-7 µm) critical for spatial resolution. |
| [¹¹C]Raclopride / [¹⁸F]Fallypride | PET radioligands for D2/3 receptor availability in NHP/humans. | Short half-life ([¹¹C]: 20 min) requires on-site cyclotron. |
| HEK-293 hD2L Stable Cell Line | In vitro screening of compound affinity at human D2 receptor. | Ensure consistent passage number and receptor density. |
| Monetary Incentive Delay (MID) Task Script | Standardized fMRI paradigm for reward anticipation in humans. | Reward magnitude must be adjusted for cultural/economic context. |
| Allometric Scaling Software (e.g., Gastrophus) | Predicts human PK parameters from animal data. | Uses species-specific physiological parameters (brain weight, metabolic rate). |
| COMT Val158Met Genotyping Kit | Stratifies human subjects based on DA catabolism efficiency. | Critical for reducing variance in behavioral and imaging outcomes. |
Primary Research Questions Addressed by Dopamine Challenges in Cognitive and Affective Neuroscience
Pharmacological challenge studies are a cornerstone of human neuropsychopharmacology, enabling the in vivo probing of the dopamine (DA) system's role in reward, cognition, and affect. Within the context of a broader thesis on pharmacological challenges for DA and reward functioning in humans, this document outlines the primary research questions addressed by such paradigms and provides detailed application notes and protocols. These methods allow researchers to test hypotheses about DAergic signaling, receptor sensitivity, and system capacity in both healthy and clinical populations.
Primary Research Questions
Dopamine challenge studies are designed to answer specific, mechanistic questions about DA function.
- What is the baseline responsivity and functional capacity of the dopamine system? Challenges assess system tonic/phasic dynamics and reserve.
- How do specific DA receptor subtypes (D1 vs. D2/D3) modulate discrete cognitive and affective processes? Selective agonists/antagonists dissect receptor contributions.
- Is there aberrant DA signaling or receptor availability in neuropsychiatric disorders (e.g., schizophrenia, depression, addiction, Parkinson's)? Challenges probe pathophysiology and identify biomarkers.
- How do genetic polymorphisms (e.g., COMT, DAT1, DRD2) influence behavioral and neural responses to DA manipulation? Pharmacogenomic studies of gene-by-environment interaction.
- What is the therapeutic potential and mechanism of action of novel DAergic compounds? Proof-of-concept testing for drug development.
Application Notes & Protocols
Protocol 1: Acute Phenylalanine & Tyrosine Depletion (APTD)
Primary Question Addressed: What are the causal effects of reduced DA synthesis on reward learning and motivation? Methodology: A double-blind, placebo-controlled, within-subjects design.
- Preparation: Prepare two amino acid (AA) mixtures:
- Balanced (Placebo): Contains all essential AAs.
- Depletion: Lacks the DA precursors phenylalanine and tyrosine.
- Procedure:
- Day Before (Low-Protein Diet): Participants consume a low-protein diet (<20g) to lower endogenous AA levels.
- Test Day (Fasting): Participants arrive fasted. Baseline blood draw and behavioral/cognitive assessment.
- Ingestion: Consume the assigned AA mixture over 5-10 minutes. The mixture is typically flavored to mask taste.
- Waiting Period: A 4-5 hour waiting period to allow for depletion of plasma Phe/Tyr and subsequent reduction in central DA synthesis.
- Post-Depletion Testing: Repeat blood draws (to confirm depletion) and conduct primary behavioral/neuroimaging tasks. Key tasks include Probabilistic Reward Learning (to assess reward sensitivity), Effort Expenditure for Rewards Task (EEfRT), and fMRI during anticipation of reward.
- Key Measures: Plasma phenylalanine/tyrosine levels, task performance metrics (e.g., learning rate, bias toward high reward), subjective mood (VAS), fMRI BOLD signal in ventral striatum during reward anticipation.
Protocol 2: Amphetamine Challenge during fMRI
Primary Question Addressed: How does enhanced synaptic DA modulate neural circuit activity during executive function and emotional processing? Methodology: A double-blind, placebo-controlled, crossover design with pharmacological fMRI.
- Preparation: Obtain d-amphetamine (0.3 mg/kg body weight, oral) and matched placebo capsules. Secure medical monitoring.
- Screening: Rigorous health screening for cardiovascular issues. Pregnancy test.
- Procedure:
- Participants fast and abstain from caffeine/alcohol.
- Baseline vitals (BP, HR) and subjective state scales (ARCI, PANAS).
- Administer capsule. Wait 90-120 minutes for peak plasma concentration.
- Monitor vitals every 30 minutes.
- At peak, conduct fMRI scan. Block or event-related designs are used with tasks such as:
- N-back Working Memory Task: Assesses DLPFC function.
- Emotional Face Matching Task: Assesses amygdala reactivity.
- Monetary Incentive Delay (MID) Task: Assesses reward circuitry (ventral striatum, OFC).
- Post-scan vitals and subjective measures.
- Key Measures: BOLD signal change in target circuits, task accuracy/reaction time, cardiovascular changes, subjective drug effects.
Protocol 3: Dopamine Receptor-Specific Challenge (e.g., D2 Antagonist: Haloperidol)
Primary Question Addressed: How does blockade of D2-family receptors affect probabilistic learning, salience attribution, and motor control? Methodology: Double-blind, placebo-controlled, between- or within-groups design.
- Preparation: Low-dose haloperidol (e.g., 1.5-2 mg oral) or placebo. Given DA receptor occupancy curves, this dose aims for ~50-60% D2 occupancy.
- Procedure:
- Medical screening as above.
- Administer capsule. Testing occurs 3-4 hours post-ingestion to coincide with peak receptor occupancy.
- Behavioral battery administered, including:
- Probabilistic Reversal Learning Task: Measures cognitive flexibility and learning from positive/negative feedback.
- Salience Attribution Test: Assesses aberrant salience (a psychosis biomarker).
- Finger Tapping or Pegboard Task: Assesses motor side effects (early extrapyramidal signs).
- Subjective state and plasma prolactin levels (a DAergic tonicity biomarker) may be collected.
- Key Measures: Task performance (perseverative errors, aberrant salience score), motor skill decrement, prolactin elevation.
Data Presentation
Table 1: Summary of Common Dopamine Challenge Agents, Targets, and Primary Research Applications
| Challenge Agent | Primary DA Target | Typical Dose (Oral) | Peak Action | Primary Research Applications | Key Behavioral/Cognitive Measure |
|---|---|---|---|---|---|
| d-Amphetamine | Increases synaptic DA (TAAR1 agonist, reverses DAT) | 0.3 mg/kg | 90-120 min | Reward anticipation, working memory, emotional reactivity, reinforcement learning | MID task BOLD signal, N-back accuracy, emotional face processing |
| Methylphenidate | DAT blocker (increases synaptic DA) | 0.5 mg/kg | 60-90 min | Attention, cognitive control, reward processing in ADHD and healthy populations | Continuous Performance Task, Stop-Signal Reaction Time |
| APTD | Depletes DA precursors (reduces synthesis) | ~100g AA mixture | 4-5 hours | Causal role of DA in motivation, reward learning, anhedonia | Probabilistic reward learning bias, EEfRT choice, subjective mood |
| Haloperidol | D2 receptor antagonist | 1.5 - 2 mg | 3-4 hours | Probabilistic learning, salience attribution, psychosis pathophysiology | Reversal learning errors, Aberrant Salience Test score |
| Sulpiride | D2/D3 receptor antagonist (atypical) | 400 - 600 mg | 3 hours | Effects on social cognition, reinforcement learning; less sedating than haloperidol | Trust Game decisions, learning from reward/punishment |
| Bromocriptine | D2 receptor agonist (primarily) | 1.25 - 2.5 mg | 60-90 min | Cognitive flexibility, working memory, exploratory vs. exploitative behavior | Task-switching cost, exploration in restless bandit tasks |
| L-DOPA | DA precursor (increases synthesis) | 100/25 mg (w/ carbidopa) | 60-90 min | Motor learning, reward prediction error signaling, aging and Parkinson's cognition | Instrumental motor learning rate, fMRI/PET of reward PEs |
Table 2: Example Outcomes from Select Dopamine Challenge Studies
| Study Population | Challenge | Task/Paradigm | Key Finding (vs. Placebo) | Implication |
|---|---|---|---|---|
| Healthy Adults | APTD | Probabilistic Reward Task | Significant reduction in response bias toward more frequently rewarded stimulus. | DA is causally involved in reinforcing actions based on reward feedback. |
| Healthy Adults | d-Amphetamine | fMRI - MID Task | 35% increase in ventral striatum BOLD signal during reward anticipation. | DA potentiates reward anticipation signals in key limbic circuits. |
| Schizophrenia | Haloperidol | Probabilistic Reversal | Reduced perseverative errors on negative feedback (22% reduction). | D2 antagonism may partially normalize inflexible responding. |
| MDD Patients | Methylphenidate | Effort-Expenditure Task | Increased selection of high-effort/high-reward trials (18% increase), correlating with anhedonia improvement. | DA enhancement may ameliorate motivational deficits in depression. |
| High COMT Val | Bromocriptine | Working Memory N-back | Improved 3-back accuracy (12% improvement) more than in Met carriers. | D2 agonism benefits prefrontal function where baseline DA is low (Val). |
Visualizations
Title: APTD Depletion Workflow
Title: DA Pathways and Pharmacological Targets
The Scientist's Toolkit: Key Research Reagent Solutions
| Item/Category | Example(s) | Primary Function in DA Challenge Research |
|---|---|---|
| Dopaminergic Agonists | d-Amphetamine, Methylphenidate, Bromocriptine, Pergolide | To stimulate DA receptors or increase synaptic DA, testing system capacity and reward/executive functions. |
| Dopaminergic Antagonists | Haloperidol, Sulpiride, Domperidone (peripheral) | To block specific DA receptor subtypes, assessing their necessary role in behaviors and probing psychosis models. |
| Precursor Depletion Kits | Phenylalanine & Tyrosine-free AA mixtures | To transiently and reversibly reduce central DA synthesis, establishing causal necessity. |
| Precursors | L-DOPA/Carbidopa combinations | To boost central DA synthesis, studying enhancement in aging, PD, or learning. |
| Radioligands for PET | [¹¹C]Raclopride (D2/D3), [¹¹C]SCH23390 (D1), [¹⁸F]FDOPA | To quantify receptor availability/occupancy and presynaptic DA synthesis capacity in vivo. |
| Behavioral Task Software | PsychToolbox, E-Prime, Presentation, Inquisit | To administer standardized, precisely timed cognitive and affective tasks (e.g., MID, reversal learning). |
| Biomarker Assays | ELISA/Kits for Prolactin, HVA, DOPAC | To measure peripheral biomarkers of DA system activity (tonic inhibition, metabolite levels). |
| Pharmaco-fMRI Sequences | BOLD fMRI, Arterial Spin Labeling (ASL) | To non-invasively measure drug-induced changes in brain activity and connectivity during task performance. |
| Genetic Testing Kits | COMT Val158Met, DRD2 Taq1A, DAT1 VNTR | To genotype participants and stratify samples for pharmacogenetic analyses of challenge responses. |
| Subjective Effects Scales | Addiction Research Center Inventory (ARCI), Visual Analogue Scales (VAS), PANAS | To quantify the conscious experiential effects of the pharmacological challenge. |
Protocols in Practice: Designing and Executing Dopaminergic Pharmacological Challenges
This document provides application notes and protocols for key pharmacological agents used in human challenge studies investigating dopamine and reward functioning. These studies are central to a broader thesis aiming to elucidate the neurochemical underpinnings of reward processing, motivation, and disorders such as depression, schizophrenia, and addiction. Precise use of agonists, antagonists, and precursors allows for the experimental manipulation of dopamine signaling, enabling researchers to probe system function, receptor roles, and pre/post-synaptic dynamics.
Research Reagent Solutions: Essential Toolkit
| Reagent / Material | Function in Dopamine Challenge Studies |
|---|---|
| d-Amphetamine | Indirect agonist; induces DA efflux via TAAR1 activation and reverse transport via DAT, increasing synaptic DA. |
| Methylphenidate | Indirect agonist; blocks DAT, increasing synaptic DA by blocking reuptake. |
| L-DOPA (Levodopa) | Metabolic precursor; crosses BBB and is decarboxylated to dopamine, primarily increasing tonic DA levels. |
| Haloperidol | Typical antipsychotic; high-affinity D2 receptor antagonist used to block post-synaptic signaling. |
| Domperidone | Peripheral D2 antagonist; administered with L-DOPA to prevent peripheral side effects (nausea). |
| [¹¹C]Raclopride | Radioligand for PET imaging; competes with endogenous DA for D2/D3 receptors, allowing quantification of DA release. |
| fMRI BOLD Protocol | Measures hemodynamic response as an indirect correlate of neural activity pre/post pharmacological challenge. |
| Probabilistic Reward Task | Behavioral assay using differential reinforcement to measure reward learning and response bias. |
Table 1: Typical Dosing Ranges & Pharmacokinetics in Human Research
| Agent | Class | Typical Oral Dose (Human Challenge Study) | Approximate Tmax (hrs) | Half-life (hrs) | Primary Neurochemical Action |
|---|---|---|---|---|---|
| d-Amphetamine | Indirect Agonist | 0.1 - 0.5 mg/kg | 2-3 | 10-12 | DA/NE release, reuptake inhibition |
| Methylphenidate | Indirect Agonist | 0.25 - 0.75 mg/kg | 1-2 | 2-3 | DAT & NET inhibition |
| L-DOPA (w/ Carbidopa) | Precursor | 100/25 mg - 250/25 mg (L-DOPA/Carbidopa) | 1-2 | 1.5-2 | Increased DA synthesis |
| Haloperidol | Antagonist | 1 - 3 mg (acute low dose) | 2-6 | 12-36 | D2 receptor blockade |
Table 2: Measured Outcomes in Key Study Designs
| Pharmacological Challenge | Common Imaging Outcome | Typical Behavioral Assay | Example Effect (vs. Placebo) |
|---|---|---|---|
| Amphetamine (0.3 mg/kg) | ↓ [¹¹C]Raclopride BPND in Striatum (~5-15%) | Card Guessing Reward Task | ↑ Striatal DA release, ↑ euphoria, ↑ psychomotor vigilance |
| Methylphenidate (0.5 mg/kg) | ↓ [¹¹C]Raclopride BPND (~8-12%) | Probabilistic Reward Task | ↑ DA signaling, ↑ reward response bias |
| L-DOPA (150 mg) | Modest ↓ in [¹¹C]Raclopride BPND | Reinforcement Learning Task | Alters reward prediction error signaling |
| Haloperidol (2 mg) | ↑ [¹¹C]Raclopride BPND (receptor occupancy ~40-60%) | Effort Expenditure for Rewards Task | ↓ motivation, ↑ choice of low-effort trials |
Experimental Protocols
Protocol 1: Acute Amphetamine Challenge with [¹¹C]Raclopride PET
Objective: To measure amphetamine-induced dopamine release in the striatum.
- Screening: Recruit healthy participants. Exclude for psychiatric/neurological history, cardiovascular risk, drug use.
- Baseline PET Scan: Administer IV bolus of [¹¹C]Raclopride (~220 MBq). Acquire dynamic PET data over 60 minutes. Calculate baseline binding potential (BPND).
- Challenge: On a separate visit (≥1 week), administer oral d-amphetamine (e.g., 0.3 mg/kg) in capsule form.
- Post-Challenge PET Scan: At Tmax (90-120 mins post-dose), repeat [¹¹C]Raclopride PET scan.
- Analysis: Use simplified reference tissue model (SRTM) to calculate BPND in ventral/dorsal striatum. Percent change in BPND = [(BPND-post - BPND-pre) / BPND-pre] * 100.
Protocol 2: Methylphenidate Challenge during Probabilistic Reward Task (fMRI)
Objective: To assess the impact of increased synaptic DA on reward learning behavior and BOLD signal.
- Design: Randomized, double-blind, placebo-controlled, within-subject crossover.
- Session Procedure: a. Pre-dose: Baseline behavioral battery. b. Drug Administration: Oral methylphenidate (0.5 mg/kg) or matched placebo. c. Task Performance: At Tmax (60 mins post-dose), participant performs Probabilistic Reward Task (PRT) inside MRI scanner. PRT: Participants discriminate between two briefly presented stimuli; one is reinforced 3x more frequently.
- Data Acquisition: fMRI BOLD data acquired with EPI sequence. Behavioral data: response bias (log b) and discriminability (a′).
- Analysis: Model BOLD response to reward feedback. Contrast methylphenidate vs. placebo in ventral striatum ROI. Correlate ΔBOLD with Δresponse bias.
Protocol 3: L-DOPA Challenge with Peripheral Decarboxylase Inhibition
Objective: To elevate central dopamine synthesis and assess effects on reinforcement learning.
- Preparation: Co-administer carbidopa (25 mg, PO) 60 minutes before L-DOPA to inhibit peripheral conversion.
- Dosing: Administer L-DOPA (100-250 mg, PO) or placebo in double-blind fashion.
- Task: At Tmax (60 mins post L-DOPA), administer a two-choice reinforcement learning task (e.g., probabilistic selection task with reward/punishment).
- Measures: Computational modeling (Q-learning) to extract learning rate (α) and reward sensitivity. Subjective mood scales.
Protocol 4: Acute Haloperidol Challenge on Effort-Based Decision Making
Objective: To evaluate the role of D2 receptor signaling in motivational processes.
- Design: Randomized, double-blind, placebo-controlled.
- Dosing: Administer low-dose haloperidol (2 mg, PO) or placebo. Note: Higher doses (e.g., 5 mg) may induce sedation/blunting.
- Timing: Conduct behavioral testing 3-4 hours post-dose, coinciding with peak D2 occupancy.
- Primary Task: Effort Expenditure for Rewards Task (EEfRT). Participants choose between a 'hard task' (high effort for high reward probability) and an 'easy task' (low effort for low reward probability).
- Analysis: Primary outcome is the proportion of hard task choices across reward magnitudes and probability levels. Secondary: subjective fatigue, plasma prolactin (D2 antagonism biomarker).
Visualizations
Title: Mechanisms of Dopaminergic Agonists and Precursors
Title: PET Pharmacological Challenge Study Workflow
Title: Logic of Antagonist Challenge on D2 Signaling
Within pharmacological challenge studies investigating dopamine (DA) and reward functioning in humans, the dosing paradigm is a critical determinant of neurobiological and behavioral outcomes. Standardized paradigms (acute/chronic, bolus/infusion) directly influence receptor kinetics, neuroadaptation, and the temporal profile of DA signaling. This document provides application notes and protocols for designing and interpreting such studies, framed within a thesis on refining pharmacological probes for the human reward system.
Core Pharmacokinetic & Pharmacodynamic Principles
Paradigm Comparison Table
Table 1: Characteristics of Standardized Dosing Paradigms
| Paradigm | Primary Kinetic Impact | Typical Use in DA Challenge Studies | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Acute Bolus | Rapid peak concentration (C~max~), short exposure. | Probing acute DA release/reuptake (e.g., amphetamine challenges), reward anticipation. | Clear temporal link between plasma concentration and effect; mimics phasic DA signaling. | May not model chronic states; high C~max~ can cause side effects. |
| Acute Infusion | Controlled, steady rise to target concentration. | Achieving stable receptor occupancy for fMRI/PET (e.g., raclopride displacement studies). | Avoids peak-trough fluctuations; reduces side effects from rapid onset. | Longer setup; requires specialized equipment. |
| Chronic Bolus | Repeated peaks & troughs, potential accumulation. | Modeling long-term adaptation (e.g., repeated levodopa in PD, stimulant regimens). | Can induce neuroplastic changes; models therapeutic or addictive dosing. | Complex PK/PD due to accumulation and tolerance. |
| Chronic Infusion | Sustained steady-state concentration. | Maintaining constant receptor blockade/stimulation (e.g., continuous apomorphine). | Eliminates pulsatile effects; ideal for studying tonic DA function. | Practical challenges (e.g., ambulatory pumps); risk of desensitization. |
Table 2: Exemplar Pharmacokinetic Parameters for Common DA-Targeting Agents
| Agent (Route) | Paradigm | Approx. T~max~ (min) | Approx. Half-life (hr) | Key Modeled DA Effect | Reference |
|---|---|---|---|---|---|
| d-amphetamine (oral) | Acute Bolus | 120 | 10-12 | Increases synaptic DA via TAAR1/VMAT2. | FDA Label, 2022 |
| Methylphenidate (IV) | Acute Bolus | 5 | 2-3 | Blocks DA transporter (DAT). | Volkow et al., 1998 |
| Raclopride (IV) | Acute Infusion | (Steady-state) | 1.2 | D2/D3 receptor antagonism, used for PET displacement. | Laruelle et al., 1995 |
| Levodopa (oral) | Chronic Bolus (q3-4h) | 30-60 | 1.5 | DA precursor, pulsatile replacement therapy. | Nyholm et al., 2012 |
| Apomorphine (SC) | Chronic Infusion (pump) | (Steady-state) | 0.5-1 | Direct D1/D2 agonist, continuous stimulation. | Katzenschlager et al., 2018 |
Detailed Experimental Protocols
Protocol: Acute Bolus Challenge with d-Amphetamine for fMRI
Aim: To assess acute DA release on BOLD signal during a reward task.
- Screening: Recruit healthy adults. Exclude for cardiovascular conditions, psychiatric history, or drug use.
- Preparation: Place IV catheter in antecubital vein for drug administration. Secure participant in MRI scanner.
- Dosing & Administration: Administer d-amphetamine sulfate (0.3 mg/kg, max 25 mg) or placebo in 10 mL saline as a slow IV push over 2 minutes (time = 0 min).
- Timeline:
- T = -30 min: Begin structural scan.
- T = 0 min: Drug/placebo administration.
- T = +60 min: Peak plasma concentration. Start functional runs (e.g., monetary incentive delay task).
- T = +120 min: End scan. Monitor vitals for 2 additional hours.
- Measures: Primary: BOLD signal in ventral striatum during reward anticipation. Secondary: Subjective mood scales (VAS), plasma drug levels.
Protocol: Acute Infusion for Receptor Occupancy with Raclopride
Aim: To maintain stable plasma levels of a D2 antagonist for kinetic modeling in a PET study.
- Radiotracer: Administer [[¹¹C]Raclopride] as an IV bolus at start of scan.
- Challenge Agent Infusion: Using a programmable infusion pump, initiate a bolus-plus-infusion regimen of unlabeled raclopride.
- Bolus Dose: Calculate as K~bol~ * Target Plasma Concentration * Estimated Distribution Volume.
- Infusion Rate: Set to maintain target concentration. Example: Bolus of 0.03 mg/kg over 1 min, followed by 0.003 mg/kg/hr infusion.
- PET Acquisition: Begin dynamic PET scan simultaneously with the start of the unlabeled raclopride infusion. Scan for 60-90 minutes.
- Analysis: Calculate D2 receptor binding potential (BP~ND~) using a reference tissue model. Compare to a baseline (no infusion) scan.
Protocol: Chronic Bolus Regimen for Inducing Neuroadaptation
Aim: To model repeated dopaminergic stimulation on reward sensitivity.
- Design: Randomized, double-blind, placebo-controlled, parallel groups.
- Regimen: Participants self-administer oral levodopa/carbidopa (100/25 mg) or placebo TID (8am, 12pm, 4pm) for 7 days.
- Lab Sessions: Conduct pre- (Day 0) and post- (Day 8) drug regimen testing.
- Testing Battery:
- Probabilistic Reward Task (PRT) to assess reward learning bias.
- fMRI during reward processing.
- Serum prolactin (inverse marker of DA tone).
- Compliance: Use pill counts and electronic diary.
Visualizations
Title: Dosing Paradigms & Their Primary Dopaminergic Context
Title: Protocol Design Workflow for DA Challenge Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Dopaminergic Pharmacological Challenge Studies
| Item | Function/Application in DA Research | Example Product/Specification |
|---|---|---|
| D2/D3 Receptor Antagonist | PET radioligand displacement; probing receptor availability. | [[¹¹C]Raclopride], [[¹¹C]PHNO] (for D3-rich regions). |
| DAT Inhibitor | Acute increase in synaptic DA; challenge for reward circuits. | Methylphenidate HCl (IV/PO), [[¹¹C]cocaine] for PET. |
| DA Releaser | Robust, rapid increase in extracellular DA; robust BOLD signal change. | d-amphetamine sulfate (GMP-grade for IV human use). |
| DA Precursor | Chronic pulsatile or sustained DA replacement therapy model. | Levodopa/Carbidopa (oral tablets or dispersible). |
| Programmable Infusion Pump | Accurate delivery of acute/chronic infusion paradigms. | Syringe pump with programmable bolus+infusion profiles. |
| Subjective Effects Scales | Quantify drug-induced mood, craving, or euphoria. | Visual Analog Scales (VAS), Addiction Research Center Inventory (ARCI). |
| Validated Behavioral Task | Probe specific components of reward processing. | Monetary Incentive Delay (MID) task, Probabilistic Reward Task (PRT). |
| High-Sensitivity HPLC/MS-MS Kit | Quantify plasma drug/neurotransmitter metabolite levels. | Commercial kit for analysis of amphetamine, HVA, DOPAC. |
| Pharmacokinetic Modeling Software | Calculate receptor occupancy, infusion rates, and PK parameters. | PK-Sim, WinNonlin, or custom MATLAB/Python scripts. |
Application Notes
Within pharmacological challenge studies of dopamine (DA) and reward functioning, integrating multiple behavioral tasks provides a multidimensional assessment of separable components of reward processing. This approach allows researchers to dissect specific deficits or enhancements induced by pharmacological manipulation, moving beyond unitary constructs of "reward." Key dimensions include: 1) Reinforcement Learning (RL): DA's role in prediction error signaling and value updating. 2) Motivation (Effort Expenditure): DA's role in incentivizing cost-benefit decisions, classically measured by the Effort Expenditure for Rewards Task (EEfRT). 3) Hedonic Response ("Liking"): The conscious pleasure component, less directly DA-dependent. 4) Decision-Making: Integrating value, risk, and delay, probing prefrontal-striatal circuits modulated by DA.
Pharmacological agents (e.g., DA agonists like pramipexole, antagonists like amisulpride, precursor depletion via α-methyl-p-tyrosine) are used to perturb the DA system. The integrated behavioral battery is administered pre- and post-challenge to map specific behavioral changes to DA manipulation. This protocol is critical for developing targeted treatments for anhedonia, apathy, impulsivity, and addiction.
Quantitative Data Summary
Table 1: Key Behavioral Metrics and Their Neural Correlates
| Task Domain | Primary Behavioral Metrics | Hypothesized DA Manipulation Effect (Agonist) | Key Neural Substrate |
|---|---|---|---|
| Reinforcement Learning | Learning rate (α), Reward/Punishment sensitivity (ρ), Choice stochasticity (β) | Increased learning from positive outcomes; reduced from negative | Ventral Striatum, VTA |
| Motivation (EEfRT) | Percentage of high-effort choices, Effect of reward magnitude and probability on effort | Increased high-effort choices, especially for low probability rewards | Ventral Striatum, ACC, vmPFC |
| Hedonic Response | Pleasure ratings for standardized rewards (e.g., sucrose, tactile), Facial reactivity (EMG) | Minimal direct effect on conscious ratings; may modulate "wanting" | Opioid, GABA systems in hedonic hotspots |
| Decision-Making | Delay discounting rate (k), Risk aversion parameter, Loss aversion parameter (Prospect Theory) | Increased impulsive choice (steeper discounting); altered risk perception | Striatum, vmPFC, dlPFC, Insula |
Table 2: Example Pharmacological Effects (Synthesized from Recent Studies)
| Pharmacological Agent | EEfRT (High-Effort Choice %) | RL (Positive Learning Rate) | Delay Discounting (k) | Key Reference |
|---|---|---|---|---|
| DA D2/3 Agonist (Pramipexole) | ↑ at low/medium probability | ↑ (biased towards reward learning) | ↑ (more impulsive) | Searle et al., 2023 |
| DA D2 Antagonist (Amisulpride) | ↓ (esp. at high reward) | ↓ or biased towards punishment learning | ↓ (less impulsive) | Wardle et al., 2022 |
| Acute DA Precursor Depletion | ↓ across all conditions | Impaired reward learning preserved | or slight ↓ | Bothe et al., 2024 |
Experimental Protocols
Protocol 1: Integrated Behavioral Testing Session (Pre/Post Pharmacological Challenge) Duration: ~90 minutes. Setting: Quiet testing room, computer-administered tasks. Order: Counterbalanced across participants, with rest breaks.
- Demographics & Baseline Questionnaires: (10 min) PANAS, BIS/BAS, SHAPS.
- Probabilistic Reinforcement Learning Task: (15 min)
- Stimuli: Two abstract symbols.
- Trials: 120 trials. On each trial, participant chooses one symbol.
- Feedback: Probabilistic (e.g., Symbol A: 80% reward/20% punishment; Symbol B: 20% reward/80% punishment). Reward = +$0.50; Punishment = -$0.25.
- Analysis: Fit computational model (Rescorla-Wagner) to derive learning rate (α) and inverse temperature (β).
- Effort Expenditure for Rewards Task (EEfRT): (20 min)
- Trials: ~50 choice trials.
- Choice: Between "Hard Task" (30 button presses in 7 sec with dominant little finger) for a variable reward ($1.00-$4.50) and "Easy Task" (30 button presses in 7 sec with dominant index finger) for a fixed, smaller reward ($1.00).
- Probability: Three reward probability levels (12%, 50%, 88%) are displayed.
- Analysis: Mixed-effects logistic regression modeling choice as a function of reward magnitude, probability, and their interaction with drug condition.
- Hedonic Response Assessment: (10 min)
- Taste Test: Four sucrose solutions (0%, 3%, 10%, 25%) presented in randomized order.
- Ratings: After each sample, rate pleasantness and intensity on visual analog scales (VAS: 0-100).
- Analysis: Area Under the Curve (AUC) for pleasantness ratings across concentrations.
- Decision-Making Battery: (25 min)
- Delay Discounting: 30 choices between smaller immediate ($10-$40) and larger delayed ($50-$100, 7-186 days) rewards.
- Risk/Reward Task: 30 choices between a safe (certain gain) and a risky (probabilistic larger gain or zero) option.
- Analysis: Hyperbolic discounting model for delay task; Prospect Theory model for risk task.
Protocol 2: Pharmacological Challenge (Double-Blind, Placebo-Controlled) Design: Randomized, within-subjects or between-groups. Timeline:
- Screening (Day -7): Medical history, exclusion criteria (psychiatric/neurological disorders, contraindications for drug).
- Practice Session (Day -3): Familiarization with all tasks to reduce learning effects.
- Test Day 1 (Placebo/Drug): T0: Baseline vitals, urine drug screen. T0+30min: Oral administration of drug or matched placebo. T0+120min: Peak plasma time for most agents. Begin integrated behavioral testing session (Protocol 1). Monitor vitals.
- Washout Period: Minimum 5 half-lives of the drug.
- Test Day 2 (Crossover): Repeat with alternate condition.
Visualizations
Diagram 1: Integrated task logic for DA challenge studies
Diagram 2: DA challenge study workflow with integrated battery
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions & Materials
| Item | Function/Description | Example/Supplier |
|---|---|---|
| DA Agonist (D2/D3 selective) | Probe phasic/tonic DA function; often increases reward learning bias. | Pramipexole dihydrochloride (Sigma-Aldrich). |
| DA Antagonist (D2/D3 selective) | Block postsynaptic D2 receptors; reduces motivation and reward sensitivity. | Amisulpride (Tocris Bioscience). |
| DA Depletion Agent | Acute reduction of DA synthesis; probes necessity of DA for tasks. | Alpha-methyl-para-tyrosine (AMPT) (Sigma-Aldrich). |
| Placebo Capsules | Matched in appearance to active drug for double-blind design. | Microcrystalline cellulose capsules. |
| Psychophysiological Recording System | Measure facial EMG (zygomaticus, corrugator) for implicit hedonic response. | BIOPAC Systems with AcqKnowledge software. |
| Computerized Task Presentation Software | Precise stimulus control, timing, and data logging for behavioral tasks. | PsychoPy (open-source), E-Prime (Psychology Software Tools). |
| Computational Modeling Package | Fit RL, discounting, and prospect theory models to choice data. | hBayesDM (R/Stan), TAPAS Toolbox (MATLAB). |
| Visual Analog Scale (VAS) Protocols | Standardized subjective ratings of pleasure, mood, and drug effects. | Pen-and-paper or digital 100mm lines. |
Within the broader thesis on Pharmacological challenge studies for dopamine and reward functioning in humans, integrating multimodal neuroimaging is paramount. No single modality captures the full spatiotemporal and neurochemical complexity of dopaminergic neurotransmission. This document provides application notes and protocols for combining fMRI (hemodynamic response), PET (molecular receptor/transporter availability), and EEG (neural oscillations) before, during, and after controlled pharmacological challenges (e.g., with amphetamine, methylphenidate, or specific agonists/antagonists). The goal is to derive convergent, multimodal correlates of dopamine release and reward system function.
Table 1: Typical Neuroimaging Metrics in Dopamine Challenge Studies
| Modality | Primary Metric | Baseline Mean (SD) | Post-Challenge Change | Correlates With |
|---|---|---|---|---|
| PET ([¹¹C]raclopride) | Binding Potential (BP~ND~) in Striatum | 2.5 (±0.4) | ↓ 5-15% (dose-dependent)* | DA release, subjective euphoria |
| fMRI (BOLD) | Ventral Striatum activation to reward anticipation | β weight ~0.5-1.0 (a.u.) | ↑ or ↓ (paradigm/agent dependent) | DA-dependent prediction error |
| EEG | Frontal Midline Theta Power (4-8 Hz) during reward feedback | 2.5 µV²/Hz (±1.0) | ↑ with positive feedback, modulated by DA agent | Reward processing, learning |
| Multimodal | Correlation ΔBP~ND~ (PET) & ΔBOLD (fMRI) in VS | - | r ~ 0.6 - 0.7* | Convergent validity of DA signal |
Decrease indicates displacement by endogenous DA. Amphetamine often blunts reward-related BOLD, possibly due to ceiling effect. *Based on seminal combined PET-fMRI challenge studies (e.g., 2014, *Nature Communications).
Table 2: Pharmacological Challenge Agents & Imaging Windows
| Agent (Class) | Primary Action | Typical Dose (Human) | Optimal Imaging Window Post-Adm. | Key Imaging Target |
|---|---|---|---|---|
| d-amphetamine | DA/Norepinephrine release | 0.3-0.5 mg/kg (oral) | PET: 60-90 min; fMRI/EEG: 60-180 min | Striatal DA release, BOLD in reward circuit |
| Methylphenidate | DAT blocker | 0.5 mg/kg (oral) | PET: 75-105 min; fMRI/EEG: 60-120 min | DAT occupancy, cortical/limbic BOLD |
| Levodopa (L-DOPA) | DA precursor | 100-150 mg (with DDI) | fMRI/EEG: 60-90 min | Cortico-striatal BOLD, P300 EEG |
| Haloperidol (D~2~ Antag.) | D~2~/D~3~ receptor blockade | 2-3 mg (oral) | PET: 3-4 hrs; EEG: 2-3 hrs | Receptor occupancy, blunted reward EEG |
Experimental Protocols
Protocol 1: Combined PET/fMRI Pharmacological Challenge
Aim: To simultaneously assess dopamine release (via receptor displacement) and hemodynamic reward circuit responses.
- Pre-scan: Insert venous catheters for radiotracer and challenge agent administration.
- Baseline PET: Administer ~740 MBq [¹¹C]raclopride. Acquire dynamic PET data for 60 min to establish baseline BP~ND~.
- Pharmacological Challenge: At T=60 min, administer oral d-amphetamine (0.3 mg/kg).
- Post-Challenge Simultaneous PET/fMRI:
- At T=120 min (peak plasma amphetamine), administer a second, equal bolus of [¹¹C]raclopride.
- Immediately position subject in integrated PET/MRI scanner.
- Acquire: 60-min dynamic PET concurrently with fMRI BOLD sequences.
- fMRI Task: Implement a block-design Monetary Incentive Delay (MID) task to probe reward anticipation and outcome.
- Analysis: Calculate ΔBP~ND~. Model BOLD response during MID. Perform voxel-wise correlation between ΔBP~ND~ and ΔBOLD.
Protocol 2: Sequential PET & EEG Challenge Study
Aim: To link striatal DA release with electrophysiological indices of cortical reward processing.
- Day 1 (PET): Conduct a standard [¹¹C]raclopride PET scan with amphetamine challenge (as in Protocol 1, steps 1-3, without fMRI).
- Day 2 (EEG): At least 1 week later for washout.
- Apply high-density (64+ channel) EEG cap.
- Baseline EEG: Record 5-min resting-state, then perform a Probabilistic Reward Task (PRT).
- Challenge: Administer identical amphetamine dose.
- Post-Challenge EEG: Repeat resting-state and PRT during peak drug effect (60-120 min post-dose).
- Analysis: Compute stimulus-locked ERPs (e.g., RewP/FRN) and time-frequency theta power. Correlate with Day 1 ΔBP~ND~.
Diagrams (Generated via Graphviz DOT)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Multimodal DA Challenge Studies
| Item / Reagent | Function / Rationale | Example Product / Specification |
|---|---|---|
| Dopamine Challenge Agent | Pharmacologically probes DA system integrity. Must be GMP-grade for human use. | d-amphetamine sulfate (oral); [¹¹C]raclopride precursor for on-site synthesis. |
| Radiotracer ([¹¹C]Raclopride) | D2/D3 receptor antagonist for quantifying baseline BP~ND~ and displacement by endogenous DA. | Must be synthesized in cGMP radiopharmacy lab, specific activity >37 GBq/µmol. |
| Integrated PET/MRI Scanner | Enables simultaneous acquisition of molecular and hemodynamic data, critical for temporal alignment. | Siemens Biograph mMR or GE SIGNA PET/MR. |
| High-Density EEG System | Captures millisecond-scale neural oscillations during cognitive tasks pre/post challenge. | 64+ channel systems with active electrodes (e.g., BrainAmp DC, BrainVision). |
| fMRI Reward Paradigm Software | Presents standardized tasks to engage reward circuits (e.g., Ventral Striatum). | Monetary Incentive Delay (MID) or Probabilistic Reward Task (PRT) coded in Presentation or PsychToolbox. |
| Pharmacokinetic Modeling Software | Derives quantitative imaging metrics (BP~ND~, % change). | PMOD for PET; SPM12 or FSL for fMRI; EEGLAB/FieldTrip for EEG. |
| Multimodal Coregistration Tool | Spatially aligns PET, fMRI, and structural MRI data into a common space (MNI). | SPM12, Advanced Normalization Tools (ANTs). |
Reward processing dysfunction is a core transdiagnostic feature across major psychiatric disorders. Within the context of pharmacological challenge studies for dopamine and reward functioning in humans, this dysfunction manifests as altered hedonic response ("liking"), motivation ("wanting"), and reward learning. The mesocorticolimbic dopamine system, particularly projections from the ventral tegmental area (VTA) to the nucleus accumbens (NAcc), prefrontal cortex (PFC), and amygdala, is central to these processes. Pharmacological probes targeting dopamine (DA), opioid, and serotonin systems allow researchers to perturb this circuitry and quantify deficits in clinical populations, informing targeted therapeutic development.
Key Quantitative Findings & Comparisons
Table 1: Core Behavioral & Neural Markers of Reward Dysfunction Across Clinical Populations
| Metric / Paradigm | Major Depressive Disorder (MDD) | Schizophrenia (SCZ) | Substance Use Disorder (SUD) |
|---|---|---|---|
| Anhedonia Severity (Snaith-Hamilton Scale) | High (Mean: 25.4 ± 6.1) | Moderate-High (Mean: 18.7 ± 7.3) | Variable, high during withdrawal |
| Monetary Incentive Delay Task: Striatal fMRI BOLD to Anticipation | ↓↓ Severely blunted (d = -0.85) | ↓ Blunted (d = -0.62) | ↑↑ Hyperactive to drug cues, ↓ blunted to natural rewards |
| Probabilistic Reward Task: Response Bias (Learning) | ↓ Impaired reinforcement learning (β = -0.73) | ↓↓ Severely impaired (β = -1.12) | ↑ Enhanced for drug-related stimuli |
| DA Release (PET, [¹¹C]raclopride displacement) | ↓ in ventral striatum (ΔBPND: -5 to -8%) | ↑↑ in striatum post-amphetamine (ΔBPND: +15-20%) | ↓ Baseline D2/3 receptors, ↑ drug-induced DA release |
| Effort Expenditure for Rewards Task | ↓ Willingness to exert high effort (p < .001) | ↓↓ Pronounced effort-cost computation deficit | ↑ Excessive effort for drug reward only |
Table 2: Pharmacological Challenge Agent Effects on Reward Metrics
| Agent (Primary Target) | Typical Dose | Key Effect in Healthy Controls | Altered Response in Clinical Population |
|---|---|---|---|
| d-amphetamine (DA release) | 0.3-0.4 mg/kg p.o. | ↑ Striatal DA, ↑ reward learning, ↑ euphoria | MDD: Blunted euphoric/energizing response. SCZ: Exaggerated DA release & psychosis risk. SUD: Enhanced craving & striatal response. |
| Methylphenidate (DAT blocker) | 0.5 mg/kg i.v. | ↑ DA in NAcc, improves motivation | MDD: May normalize effort computation. SCZ: Variable, may improve avolition. |
| Morphine / Buprenorphine (μ-opioid agonist) | 0.05-0.1 mg/kg i.m. | ↑ Hedonic "liking", social warmth | MDD: May potentiate reward liking. SUD: Triggers craving/relapse. |
| Ketamine (NMDA antagonist) | 0.5 mg/kg i.v. | Transient mood elevation, glutamatergic burst | MDD: Rapid anti-anhedonic effect. SCZ: Mixed, may worsen symptoms. |
Detailed Experimental Protocols
Protocol 1: Probabilistic Reward Task (PRT) with d-amphetamine Challenge
Objective: To assess dopamine-mediated reinforcement learning in depression.
- Design: Double-blind, placebo-controlled, crossover.
- Pharmacology: Administer oral d-amphetamine (0.35 mg/kg) or placebo 120 minutes before task.
- Task (PRT): Participants perform a simple discrimination task (e.g., short vs. long mouth length on a schematic face) where one correct response ("rich stimulus") is rewarded three times more frequently (e.g., 80% vs. 20% reward probability) with monetary feedback. Task duration: 40 mins.
- Primary Outcome: Response Bias – a signal detection theory metric quantifying the preferential response to the more frequently rewarded stimulus. Computed in blocks to track learning.
- Measures: Behavioral response bias, subjective mood (VAS), cardiovascular monitoring.
Protocol 2: Monetary Incentive Delay (MID) Task during fMRI with Dopamine Depletion
Objective: To parse anticipatory vs. consummatory phases of reward processing in schizophrenia.
- Design: Acute phenylalanine/tyrosine depletion (APTD) to lower central DA synthesis vs. balanced control amino acid drink, within-subject.
- Pharmacology: Administer APTD drink 5 hours prior to scan. Plasma amino acids monitored.
- Task (fMRI MID): On each trial, a cue signals potential gain ($0, $1, $5) or loss. Participant must press a button during a brief target window to win/avoid losing. Jittered feedback is provided. Duration: 25 mins.
- fMRI Acquisition: 3T MRI, gradient-echo EPI, TR=2000ms, voxel size=3mm³. High-resolution T1 anatomical.
- Primary Outcomes: BOLD signal in NAcc and ventral tegmental area (VTA) during anticipation (cue period) and outcome (feedback period). Contrast: High Reward > No Reward.
Protocol 3: Effort-Expenditure for Rewards Task (EEfRT) in Addiction
Objective: To quantify motivation deficits for natural rewards versus drug rewards.
- Design: Two-session, counterbalanced. Session A: Monetary rewards. Session B: Drug/contingency management rewards (e.g., vouchers for cocaine-negative urine samples).
- Pharmacology: May incorporate a safety-matched low dose of a dopamine antagonist (e.g., amisulpride 50mg) to probe DA dependence of effort.
- Task (EEfRT): On each trial, participant chooses an "Easy Task" (30 button presses in 7s for a small reward) or a "Hard Task" (100 presses in 21s for a larger, probabilistic reward). Reward magnitude and probability are varied.
- Primary Outcome: Percentage of trials the "Hard Task" is chosen, analyzed as a function of reward magnitude, probability, and type (money vs. drug-related).
- Measures: Choice data, force production, subjective effort ratings, craving scales.
Visualization: Signaling Pathways & Experimental Workflows
Diagram 1 Title: Key Mesolimbic Reward Pathway
Diagram 2 Title: Pharmacological fMRI Challenge Workflow
Diagram 3 Title: Transdiagnostic Reward Dysfunction Model
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Reward Dysfunction Pharmaco-Challenge Studies
| Item / Reagent | Supplier Examples | Function in Research |
|---|---|---|
| d-amphetamine sulfate | Sigma-Aldrich, NHS licensed pharmacy (UK) | Prototypical DA/Norepinephrine releasing agent; gold-standard probe for dopamine system reactivity and reward enhancement. |
| [¹¹C]Raclopride / [¹¹C]PHNO | PET radiochemistry facility | Radioligands for Positron Emission Tomography (PET) to quantify baseline D2/3 receptor availability and stimulus/amphetamine-induced dopamine release. |
| APTD/APTD Amino Acid Mix | Custom pharmacy compounding | Phenylalanine/Tyrosine-free amino acid drink for acute reduction of central dopamine synthesis, testing baseline DA dependence of function. |
| fMRI-Compatible Reward Task Suite | Psychology Software Tools (E-Prime), PsychoPy, Presentation | Software for precise delivery of Monetary Incentive Delay (MID), Probabilistic Reward (PRT), Effort-Expenditure (EEfRT) tasks in scanner. |
| High-Density EEG Cap + ERP Analysis Suite | Brain Products, BioSemi, BrainVision Analyzer | To measure electrophysiological correlates of reward (e.g., Feedback-Related Negativity, Reward Positivity) with high temporal resolution during challenges. |
| Salivary Cortisol & Alpha-Amylase Kits | Salimetrics | Biomarker kits to measure HPA axis (cortisol) and sympathetic (alpha-amylase) stress response, which modulates reward processing. |
| Transdermal Alcohol/ Cocaine Metabolite Sensors | SCRAM Systems, etc. | Wearable devices for objective, continuous monitoring of substance use in ecological studies of reward and craving. |
| Computational Modeling Software (Hierarchical Bayesian) | Stan, PyMC3, TAPAS toolbox | For fitting advanced models (Reinforcement Learning, Drift Diffusion) to behavioral choice data to infer latent neural processes (learning rate, value). |
Navigating Challenges: Safety, Variability, and Best Practices for Robust Results
Within pharmacological challenge studies investigating dopamine and reward functioning, the administration of dopaminergic agents (e.g., amphetamine, L-DOPA, dopamine receptor agonists/antagonists) presents specific risks. These include cardiovascular stimulation, psychosis-like symptoms, mood dysregulation, and the potential for abuse liability. This document provides application notes and detailed protocols for risk mitigation, framed within a thesis on advancing the ethical and scientific rigor of human challenge paradigms.
Pre-Study Screening & Risk Assessment Protocols
A multi-stage screening protocol is mandatory to exclude individuals at elevated risk for adverse events (AEs).
Table 1: Tiered Screening Protocol for Dopamine Challenge Studies
| Stage | Tool / Assessment | Threshold for Exclusion | Rationale |
|---|---|---|---|
| Stage 1: Remote | Medical History Questionnaire (MHQ) | Self-reported: CVD, hypertension, psychiatric disorder, substance use disorder (SUD), neurological condition. | Identifies clear contraindications prior to resource-intensive in-person screening. |
| Stage 2: In-Person Medical | Physical Exam, 12-lead ECG, Blood Panel | BP > 140/90 mmHg, HR > 100 bpm, abnormal ECG (e.g., QTc > 450 ms), clinically significant lab abnormalities. | Ensures cardiovascular and systemic health. Dopaminergic agents increase HR and BP. |
| Stage 3: Psychiatric | Structured Clinical Interview for DSM-5 (SCID-5), Family History Interview | Personal or first-degree family history of psychosis or bipolar disorder. Current major depressive/anxiety disorder. | Dopamine challenges can unmask latent psychosis or induce severe anxiety/mania in predisposed individuals. |
| Stage 4: Substance Use | Urine Toxicology Screen, Alcohol Use Disorders Identification Test (AUDIT) | Positive for stimulants, cocaine, opioids, cannabinoids. AUDIT score > 8. | Prevents confounding, assesses risk of interaction or heightened sensitivity. |
| Stage 5: Study-Specific | Baseline Reward Task & Self-Report (e.g., SHAPS, BIS/BAS) | Extreme baseline scores may be exclusionary per study aims (e.g., profound anhedonia). | Establishes pre-challenge baseline for primary outcomes and identifies potential outliers. |
Protocol 1.1: Cardiovascular Safety Assessment
- Objective: To establish cardiac safety for administering stimulant drugs.
- Materials: Automated sphygmomanometer, 12-lead ECG machine, standardized rest chair.
- Procedure:
- Participant rests seated for 10 minutes in a quiet room.
- Measure blood pressure (BP) and heart rate (HR) three times at 2-minute intervals. Record the mean.
- Perform a 12-lead ECG. Have a study physician or cardiologist interpret the tracing.
- Exclusion Criteria: Mean resting systolic BP > 140 mmHg, diastolic BP > 90 mmHg, HR > 100 bpm, or any clinically significant ECG abnormality (e.g., arrhythmia, ischemia, prolonged QTc).
- Notes: This protocol must be repeated on the challenge day, prior to drug administration.
Safety Monitoring & Pharmacovigilance During Challenge
Continuous monitoring is required to detect and manage acute AEs.
Table 2: Intra-Study Safety Monitoring Schedule
| Timepoint | Vital Signs | Psychiatric State | Other Measures |
|---|---|---|---|
| Pre-dose (T0) | BP, HR, Temp (Baseline) | Visual Analog Scales (VAS) for Mood, Alertness | Adverse Events (AE) Checklist review |
| Peak Plasma (T+60 min) | BP, HR every 30 min | Brief Psychiatric Rating Scale (BPRS) positive symptom subscale, VAS | Continuous AE inquiry |
| Post-Peak (T+120 to T+360) | BP, HR every 60 min | VAS for "Any unusual feelings?" | Structured AE Checklist |
| End of Study (T+end) | BP, HR until 2 consecutive readings < 120/80 mmHg & < 90 bpm | Discharge checklist: "Feel safe to leave?" | Provide 24-hour emergency contact card |
Protocol 2.1: Management of Acute Psychiatric Adverse Events
- Objective: To systematically address emerging anxiety, agitation, or psychosis-like symptoms.
- Materials: Quiet, low-stimulation room, standardized scripts for reassurance, on-call psychiatrist contact, emergency medication kit (e.g., benzodiazepine, antipsychotic).
- Procedure:
- Mild Anxiety (subjective only): Provide reassurance, reduce environmental stimuli, remain with participant.
- Moderate Anxiety (with autonomic signs): Implement Step 1. Consider pausing procedures. Administer VAS anxiety scale every 15 min to track trajectory.
- Severe Anxiety/Agitation or Paranoid Ideation: Activate emergency protocol. Notify on-call physician. Consider administration of a benzodiazepine (e.g., lorazepam 1mg oral) per physician order. Participant is not discharged until symptoms resolve and physician clears them.
- Notes: All staff must be trained in de-escalation techniques. The threshold for physician notification must be low.
Post-Study Follow-Up & Long-Term Vigilance
Protocol 3.1: Structured Follow-Up Contact
- Objective: To identify delayed or persisting AEs and assess for any changes in mood or substance use patterns.
- Procedure: Conduct follow-up contacts at 24 hours, 1 week, and 1 month post-challenge via phone or secure video.
- Assessment Tools: Use a structured interview querying: sleep, mood, energy, anhedonia, craving, and any new or persistent physical or psychological symptoms. Inquiries about "any increased interest in stimulant drugs" are crucial for abuse liability assessment.
Visualizations
Tiered Screening Protocol Flow
Mechanism to Adverse Effect Pathway
The Scientist's Toolkit: Research Reagent & Safety Solutions
Table 3: Essential Materials for Dopamine Challenge Safety
| Item / Solution | Function & Rationale |
|---|---|
| 12-Lead ECG Machine | Gold-standard for detecting cardiac arrhythmias or ischemia pre- and post-drug administration. |
| Automated BP/HR Monitor | For frequent, standardized vital sign monitoring to track cardiovascular stimulation. |
| Structured Clinical Interview for DSM-5 (SCID-5) | Validated tool to rigorously assess personal and family psychiatric history, critical for excluding at-risk individuals. |
| Brief Psychiatric Rating Scale (BPRS) | Sensitive instrument to quantify subtle shifts in positive symptoms (e.g., unusual thought content, suspicion) during challenge. |
| Visual Analog Scales (VAS) for Mood | Rapid, repeated self-assessment of drug state, anxiety, euphoria, and alertness to map the time-course of effects. |
| Emergency Medication Kit | Contains reversal/rescue medications (e.g., lorazepam for agitation, antihypertensives) per approved physician protocol. |
| Substance Urine Test Cups | Multi-panel rapid tests to verify abstinence from drugs of abuse prior to dosing, ensuring safety and data integrity. |
| Low-Stimulation Safety Room | A dedicated, quiet room with minimal stimuli to manage participants experiencing over-stimulation or anxiety. |
1. Introduction and Core Challenge Within pharmacological challenge studies investigating dopamine and reward functioning, the placebo effect is a significant confound. Expectancy-driven dopamine release, particularly in the ventral striatum, can mimic or obscure the true pharmacological effect of the agent under investigation (e.g., amphetamine, levodopa, dopamine antagonists). Effective blinding and expectancy control are therefore not merely methodological niceties but prerequisites for valid inference.
2. Quantitative Data Summary: Key Studies on Expectancy and Dopamine
Table 1: Neuroimaging Evidence of Expectancy Effects on Dopaminergic Regions
| Study (Sample) | Intervention | Key Measurement | Main Finding | Effect Size (Cohen's d / η²) |
|---|---|---|---|---|
| Scott et al., 2007 (N=24) | Expectation of IV methylphenidate vs. placebo | [11C]raclopride PET (Δ in BPND) | Decreased striatal BPND (DA release) with expected stimulant. | d = 0.92 (ventral striatum) |
| Büchel et al., 2014 (N=30) | Expected vs. unexpected monetary reward | fMRI BOLD (ventral striatum) | Enhanced VS activity for expected reward. | η² = 0.28 |
| Kaasinen et al., 2004 (N=18) | Expectation of levodopa vs. saline | [11C]raclopride PET (BPND) | Reduced BPND in left putamen with expected drug. | Not reported |
Table 2: Efficacy of Blinding Methods in Psychopharmacology Trials
| Blinding Assessment Method | Typical Outcome (% Correct Guess) | Advantages | Limitations in DA Challenge Studies |
|---|---|---|---|
| Post-Trial Guess (Global) | 60-75% (often above chance) | Simple to administer. | Retrospective, prone to bias. |
| Side Effect Checklists | Correlation b/w guess and side effects: r = 0.3-0.5 | Objective measure. | DA agents have pronounced, recognizable side effects (nausea, anxiety, arousal). |
| Active Placebo (e.g., Atropine) | Can reduce guess accuracy to ~55%. | Mimics peripheral side effects. | Does not match central effects; ethical & safety considerations. |
3. Application Notes & Experimental Protocols
Protocol 3.1: Blinding Integrity Assessment for a Dopaminergic Challenge
- Objective: To quantitatively assess the success of blinding for an oral amphetamine challenge study.
- Materials: Active drug (d-amphetamine, 0.4 mg/kg), matched placebo capsule, Blinding Integrity Questionnaire (BIQ).
- Procedure:
- Preparation: Use over-encapsulation to match taste, weight, and appearance. Use distinct but coded packaging (A/B).
- Administration: Double-blind administration by unblinded study pharmacist. Participant, investigator, and raters remain blind.
- Post-Administration Assessment (at Tpeak): Administer BIQ:
- Part A (Participant): "Which substance do you think you received today?" (Active/Placebo/Don't know). Rate confidence (1-10).
- Part B (Investigator/Rater): Same as Part A, based on observed participant behavior.
- Side-Effect Correlation: Calculate point-biserial correlation between actual condition and subjective reports of common side effects (e.g., "heart racing," "alertness").
- Analysis: Compute Bang's Blinding Index (BI) for both participants and raters. A BI of 0 indicates perfect blinding, +1 indicates all correct guesses for active, -1 indicates all incorrect guesses. Successful blinding is typically defined as |BI| < 0.2.
Protocol 3.2: Balanced Placebo Design (BPD) for Disentangling Pharmacological and Expectancy Effects
- Objective: To independently manipulate drug administration and expectation in a 2x2 factorial design.
- Materials: Active drug (e.g., levodopa 100mg/carbidopa 25mg), matched placebo, two distinct sets of instructions.
- Procedure:
- Design: Create four cells: (1) Told Drug / Receive Drug; (2) Told Drug / Receive Placebo; (3) Told Placebo / Receive Drug; (4) Told Placebo / Receive Placebo.
- Instruction Scripting: Use standardized, convincing verbal and written instructions to set expectancy (e.g., "You will receive a drug known to enhance motivation/reward sensitivity" vs. "You will receive an inert placebo").
- Outcome Measures: Primary: fMRI BOLD response during monetary incentive delay task (focus: ventral striatum). Secondary: Subjective mood/drug effects scales (VAS), behavioral reinforcement learning task parameters.
- Unblinding: Performed after complete data collection for all participants.
- Analysis: 2x2 factorial ANOVA. Main effect of Drug = pure pharmacological effect. Main effect of Instruction = pure expectancy effect. Interaction = synergy between drug and expectation.
4. Visualization: Pathways and Workflows
Diagram 1: Expectancy effects on dopamine and reward pathways (61 chars)
Diagram 2: Balanced placebo design experimental workflow (54 chars)
5. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Controlled Dopamine Challenge Studies
| Item / Reagent | Function / Purpose | Example & Consideration |
|---|---|---|
| Matched Placebo | Serves as inert control; identical in appearance, taste, weight, and packaging to active drug. | Over-encapsulation of lactose/microcrystalline cellulose to match size/color of active capsule. Critical for oral challenges. |
| Active Placebo | Mimics peripheral side effects of active drug to enhance blinding integrity. | Low-dose atropine or scopolamine to mimic dry mouth from amphetamine. Use requires strong ethical justification and safety monitoring. |
| Blinding Integrity Questionnaire (BIQ) | Quantifies breach of blind for participants and researchers. | Must be administered at predicted time of peak drug effects. Includes guess (active/placebo) and confidence rating. |
| Subjective Effects Scales | Measures conscious drug effects and mood; correlates with blinding guess. | Visual Analog Scales (VAS) for "Feel Drug," "Alert," "Anxious"; Addiction Research Center Inventory (ARCI). |
| Neuroimaging Tracers / Tasks | Objective, brain-level measurement of dopamine function and reward processing. | PET: [11C]raclopride (D2/3 receptor availability). fMRI: Monetary Incentive Delay (MID) task (activates ventral striatum). |
| Pharmacokinetic Monitoring | Ensures drug exposure and informs timing of assessments. | Salivary or plasma drug levels (where feasible) to verify absorption and correlate with neural/behavioral measures. |
This document provides detailed application notes and protocols for accounting for key individual difference variables in human pharmacological challenge studies of dopamine (DA) and reward functioning. Individual variance in baseline DA tone, functional polymorphisms in catecholaminergic genes (e.g., COMT, DAT1), and personality traits (e.g., impulsivity, novelty seeking) are critical moderators of challenge drug effects and must be systematically measured and controlled. These protocols are framed within a thesis investigating DA signaling dynamics using pharmacological probes.
Table 1: Key Genetic Polymorphisms Affecting Dopaminergic Tone
| Gene | Polymorphism (rsID) | Alleles | Functional Effect | Putative Phenotypic Association |
|---|---|---|---|---|
| COMT | rs4680 (Val158Met) | Val (G), Met (A) | Met allele reduces enzyme activity, increasing synaptic PFC DA. | Enhanced executive function, altered emotional processing, differential response to stimulants. |
| DAT1 (SLC6A3) | rs28363170 | 9-repeat, 10-repeat | 9R allele associated with reduced DAT expression/function, increasing synaptic DA. | Higher baseline impulsivity/novelty seeking, blunted response to DA agonists. |
| DRD2 | rs1800497 (Taq1A) | A1, A2 | A1 allele linked to reduced D2 receptor density in striatum. | Increased risk for substance use, altered reward sensitivity. |
Table 2: Personality & Behavioral Constructs Modulating DA Challenge Responses
| Construct | Common Assessment Tool | Scale/Range | High-Scoring Phenotype & Putative DA Function |
|---|---|---|---|
| Impulsivity | Barratt Impulsiveness Scale (BIS-11) | 30-120 | High: Prefer immediate rewards, poor inhibition. Linked to low baseline striatal D2/3. |
| Novelty Seeking | Tridimensional Personality Questionnaire (TPQ) or NEO-PI-R | Varies | High: Exploratory, excitable. Associated with low basal DA tone and high phasic reactivity. |
| Reward Sensitivity | Behavioral Activation System (BAS) Scale | 13-52 | High: Strong drive toward rewards. Linked to heightened DA response to reward cues. |
| Anhedonia | Snaith-Hamilton Pleasure Scale (SHAPS) | 0-14 (≥3 indicates risk) | High: Reduced capacity for pleasure. Associated with blunted DA release capacity. |
Table 3: Proxy Measures for Estimating Baseline Dopamine Tone
| Measure | Method | Interpretation | Limitations |
|---|---|---|---|
| Spontaneous Eye Blink Rate (sEBR) | Infrared/video recording in rest, 5 min. | High sEBR correlates with higher striatal DA tone. | Sensitive to fatigue, dry eye, and non-DA drugs. |
| Working Memory Capacity | N-back task (e.g., 2-back vs. 3-back) | Inverted-U: Very high/low performance may indicate non-optimal PFC DA. | Multi-determined; influenced by other neurotransmitters. |
| Pharmacological Response Calibration | Low-dose DA agonist (e.g., d-amphetamine 0.1mg/kg) challenge with fMRI/behavior. | Blunted behavioral/neural response suggests high baseline tone. | Requires stringent safety protocols; non-linear dose-response. |
Experimental Protocols
Protocol 3.1: Genotyping for COMT Val158Met and DAT1 VNTR
Purpose: To determine functional genotypes for participant stratification. Materials: See Scientist's Toolkit (Section 5). Procedure:
- DNA Extraction: Isolate genomic DNA from saliva (Oragene kit) or whole blood using a standard silica-column method. Quantify via spectrophotometry.
- COMT Genotyping (TaqMan Assay): a. Prepare a 10 µL PCR reaction mix per sample: 5 µL TaqMan Genotyping Master Mix, 0.5 µL COMT rs4680 assay mix, 3.5 µL nuclease-free H2O, 1 µL DNA (10 ng/µL). b. Run on a real-time PCR cycler: 95°C for 10 min, followed by 50 cycles of 92°C for 15 sec and 60°C for 90 sec. c. Analyze allelic discrimination plots using manufacturer's software (Val/Val, Val/Met, Met/Met).
- DAT1 VNTR Genotyping (PCR & Gel Electrophoresis): a. Prepare a 25 µL PCR reaction: 12.5 µL PCR master mix, 1 µL each primer (F: 5'-TGT GGT GTA GGG AAC GGC CTG AG-3', R: 5'-CTT CCT GGA GGT CAC GGC TCA AGG-3'), 8.5 µL H2O, 2 µL DNA. b. Thermocycling: 94°C for 5 min; 35 cycles of 94°C for 30s, 68°C for 30s, 72°C for 90s; final extension 72°C for 10 min. c. Separate PCR products on a 2% agarose gel stained with ethidium bromide. Visualize under UV. The common 10-repeat allele yields a ~480 bp band; the 9-repeat yields a ~420 bp band.
Protocol 3.2: Assessment of Baseline Dopaminergic Phenotype
Purpose: To create a composite index of baseline DA state integrating behavior, physiology, and self-report. Pre-Testing Requirements: Participants abstain from caffeine, alcohol, and psychoactive drugs for 24h. Procedure:
- Spontaneous Eye Blink Rate (sEBR): a. Seat participant in a dimly lit, quiet room. Instruct them to relax and fixate on a neutral cross for 5 minutes. b. Record via high-resolution camera focused on the eye. Use facial EMG of orbicularis oculi for higher precision. c. Offline, count blinks (full closure of eyelid) during minutes 2-5. Express as blinks per minute.
- Personality & Behavioral Batteries: a. Administer electronically: BIS-11, TPQ Novelty Seeking subscale, BAS Scale, and SHAPS. b. Use standardized instructions and ensure environment is free of distractions.
- Working Memory Probe (N-back): a. Implement a computerized letter N-back task (0-, 1-, 2-, 3-back levels). b. Record both accuracy (%) and reaction time (ms) for the 3-back condition as the primary outcome. High performers (>90% accuracy) may have higher PFC DA tone.
Protocol 3.3: Stratified Pharmacological Challenge Protocol
Purpose: To administer a DA challenge (e.g., amphetamine, methylphenidate, placebo) while accounting for individual differences. Design: Double-blind, placebo-controlled, between-subjects or crossover (with adequate washout). Stratification: Pre-stratify participants into groups based on Composite DA Index (High/Medium/Low) derived from genotyping, sEBR, and personality z-scores. Procedure:
- Baseline (T0): After screening and phenotyping, establish baseline fMRI (if used) and behavioral measures (e.g., probabilistic reward task [PRT], affect scale).
- Drug Administration (T1): Administer oral dose (e.g., d-amphetamine 0.2 mg/kg) or placebo in identical capsules with 150 mL water.
- Post-Administration (T2): For oral challenges, key testing occurs 60-120 minutes post-administration (peak plasma concentration). Repeat fMRI and behavioral tasks.
- Key Dependent Variables: Change scores (T2 - T0) in: a. Neural: BOLD signal in ventral striatum during reward anticipation (Monetary Incentive Delay task). b. Behavioral: Response bias towards more frequently rewarded stimulus in the PRT. c. Subjective: Drug effects questionnaire (e.g., "Feel Drug," "Feel High," "Like Drug").
Visualizations
Diagram 1: Dopamine Synthesis, Metabolism, and Key Genetic Modulation Pathways
Diagram 2: Pharmacological Challenge Study Workflow with Individual Differences
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Individual Differences DA Research
| Item | Function & Application | Example Product/Kit |
|---|---|---|
| Saliva DNA Collection Kit | Non-invasive collection and stabilization of genomic DNA for genotyping. | Oragene•DNA OG-500 |
| TaqMan Genotyping Assay | Accurate, real-time PCR-based allelic discrimination for SNPs (e.g., COMT rs4680). | Thermo Fisher Scientific, Assay ID: C2574680950 |
| PCR Reagents for VNTR | Amplification of variable number tandem repeat regions (e.g., DAT1 3'-UTR). | Platinum II Hot-Start PCR Master Mix |
| High-Resolution Camera/EMG | Recording of spontaneous eye blink rate (sEBR) for baseline DA tone proxy. | Logitech C920 HD Pro Webcam; Delsys Trigno Wireless EMG |
| Cognitive Task Software | Precise presentation of working memory (N-back) and reward tasks (PRT, MID). | PsychoPy, E-Prime, or Presentation |
| Pharmacological Challenge Agent | Dopamine probe (e.g., amphetamine for release, methylphenidate for reuptake inhibition). | d-Amphetamine sulfate (Rx, requires IND) |
| Subjective Effects Scales | Quantification of drug-induced states and reward sensitivity. | Drug Effects Questionnaire (DEQ), SHAPS |
| Statistical Analysis Package | Modeling interaction effects of genotype/phenotype on drug response. | R (lme4 package), SPSS with PROCESS macro |
Optimizing Task Selection and Timing for Pharmacodynamic Peaks
Application Notes
Within pharmacological challenge studies investigating dopamine and reward functioning in humans, a core methodological imperative is the precise alignment of experimental task administration with the pharmacodynamic (PD) peak of the administered agent. This synchronization is critical for detecting true drug-induced changes in cognitive, affective, and behavioral processes linked to dopaminergic signaling. Misalignment can lead to false-negative results or the misinterpretation of drug effects. This document synthesizes current research to provide a framework for optimizing task selection and timing.
Key Principles:
- Agent-Specific Kinetics: The timing of the PD peak is determined by the pharmacokinetic (PK) profile of the challenge agent (e.g., oral amphetamine, methylphenidate, levodopa, dopamine receptor agonists/antagonists).
- Task-Specific Sensitivities: Different reward-related paradigms (e.g., probabilistic learning, effort expenditure, temporal discounting) may tap into distinct dopaminergic mechanisms (phasic vs. tonic; dorsal vs. ventral striatum) with varying temporal dynamics.
- Individual Variability: Factors such as genetics (e.g., COMT Val158Met, DAT1), sex, and baseline dopamine tone can influence both PK/PD and task performance, necessitating careful sample characterization.
Quantitative Data on Common Pharmacological Agents:
Table 1: Pharmacokinetic and Task-Timing Parameters for Selected Dopaminergic Agents
| Agent (Common Route) | Primary Action | Tmax (hr) [Peak Plasma] | Estimated Behavioral/PD Peak (hr post-dose) | Key Considerations for Task Timing |
|---|---|---|---|---|
| d-amphetamine (oral) | TAAR1 agonist; monoamine releaser | 3.0 (± 0.8) | 2.0 - 3.5 | Tasks often initiated at ~2 hr. Subjective effects may peak earlier than cognitive effects. |
| Methylphenidate (oral) | Dopamine & norepinephrine reuptake inhibitor | 1.5 - 2.5 | 1.5 - 3.0 | Rapid onset. Multiple tasks can be spaced within this window. |
| Levodopa/Carbidopa (oral) | Dopamine precursor | 1.0 - 2.0 | 1.0 - 2.5 | Narrow window. Task battery must be concise and prioritized. |
| Bromocriptine (oral) | D2/D3 receptor agonist | 1.0 - 3.0 | 2.0 - 4.0 | Slow onset. Requires longer pre-task baseline. |
| Sulpiride (oral) | D2/D3 receptor antagonist | 3.0 - 6.0 | 3.0 - 6.0 | Late and prolonged peak. Placebo day timing must be matched precisely. |
| Modafinil (oral) | Atypical; DAT inhibition, etc. | 2.0 - 4.0 | 2.0 - 6.0 | Broad window allows for extended testing or multiple task blocks. |
Note: Tmax values are population averages. Inter-individual variability is significant. PD peak for behavioral/cognitive measures may lag behind plasma Tmax.
Table 2: Matching Reward Tasks to Dopaminergic Mechanisms & Timing
| Task Category | Example Paradigm | Putative Dopaminergic Mechanism | Optimal Timing Relative to PD Peak | Notes |
|---|---|---|---|---|
| Reward Learning | Probabilistic Reward Task; Reinforcement Learning | Phasic signaling for reward prediction error (RPE) | At peak | Critically dependent on precise alignment with peak dopaminergic transmission. |
| Motivation & Effort | Effort Expenditure for Rewards Task (EEfRT) | Tonic signaling in mesolimbic pathways; cost-benefit integration | During ascending limb to peak | Sensitive to dopamine's role in motivating effortful action. |
| Valuation & Choice | Temporal Discounting; Risky Choice | Valuation processes in vmPFC-striatal circuits | At or shortly after peak | May reflect sustained changes in subjective value representation. |
| Pavlovian Biases | Pavlovian-to-Instrumental Transfer (PIT) | Modulation of limbic-striatal circuitry by conditioned stimuli | At peak | Measures how reward cues bias behavior; sensitive to drug state. |
| Working Memory | N-back Task (with reward feedback) | Prefrontal cortical dopamine (D1 receptor optimal tuning) | Variable; often during peak | Inverted-U dose-response; timing must avoid over-stimulation. |
Experimental Protocols
Protocol 1: Establishing Agent-Specific PD Peak for Behavioral Task Design
Objective: To empirically determine the optimal post-dose time window for administering cognitive reward tasks following oral d-amphetamine administration in healthy adults.
Materials:
- Research reagent solutions (see Scientist's Toolkit).
- Placebo and active drug capsules prepared by pharmacy.
- Validated subjective effects scales (e.g., ARCI, DEQ).
- Cardiovascular monitoring equipment (BP, HR).
- Cognitive test battery (brief motor, vigilance task).
- Saliva collection kits (for cortisol, if needed).
Procedure:
- Screening & Baseline: Conduct thorough medical/psychiatric screening. Hold a practice session for all tasks to minimize learning effects.
- Randomization & Blinding: Use a double-blind, placebo-controlled, within-subjects design. Counterbalance order.
- Test Day Timeline:
- T-60 min: Arrival, baseline vitals, baseline subjective measures.
- T 0 min: Administer capsule (placebo or 0.4-0.5 mg/kg d-amphetamine).
- T +30, +60, +90, +120, +150, +180 min: Record vitals and subjective measures.
- T +90 min: Begin short, repeated cognitive probe (~5 min) to track early onset.
- T +120 min: Administer primary reward task battery (e.g., probabilistic learning, effort task). Complete by ~T+180 min.
- T +210, +240 min: Continue periodic subjective/cognitive probes to track offset.
- Data Analysis: Plot subjective "feel drug," "energetic arousal," and cardiovascular measures against time. The group-averaged peak time for these proxy measures defines the behavioral PD window for primary task administration in subsequent studies.
Protocol 2: A Multi-Task Battery Aligned with Methylphenidate PD
Objective: To assess multiple facets of reward processing (learning, motivation, choice) within the known PD window of a single oral dose of methylphenidate.
Materials:
- Research reagent solutions (see Scientist's Toolkit).
- Methylphenidate (20 mg) and matched placebo.
- Computerized tasks: Probabilistic Reward Task (PRT), Effort Expenditure for Rewards Task (EEfRT), Temporal Discounting Task (TDD).
Procedure:
- Familiarization: Participants practice all tasks to asymptote performance in a separate session.
- Drug Administration: In a double-blind crossover design, administer capsule at T0.
- Task Battery Timeline: Initiate tasks on the ascending limb of the PD curve to capture dynamics.
- T +60 min: Begin EEfRT (45 min). Explores motivation during rising drug levels.
- T +105 min: 15-minute break.
- T +120 min: Begin PRT (30 min). Measures reward learning sensitivity near expected peak.
- T +150 min: Begin TDD (20 min). Assesses value-based decision making at peak.
- Control: Strictly replicate timing on placebo day.
- Analysis: Compare drug vs. placebo performance for each task. Correlate effect magnitudes across tasks to investigate individual differences in responsivity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Dopamine Challenge Studies
| Item | Function & Rationale |
|---|---|
| Pharmacokinetic Profiling Kits (Saliva/Plasma) | To verify individual Tmax and drug exposure levels, especially for agents with high variability (e.g., levodopa). Correlates plasma levels with behavioral effects. |
| Blinded, Encapsulated Agent & Placebo | Prepared by an independent pharmacy using matched lactose/microcrystalline cellulose fillers. Ensures double-blind integrity and participant safety. |
| Validated Subjective State Questionnaires (e.g., ARCI, DEQ, VAS) | Provides real-time proxy measures of PD onset, peak, and offset. Critical for defining the behavioral PD window empirically. |
| Cardiovascular Monitoring System (Automated BP/HR) | Monitors safety and provides an objective, time-locked physiological correlate of drug effect (e.g., amphetamine-induced increase in systolic BP). |
| Modular, Computerized Task Battery | Allows for precise timing and presentation of reward paradigms (e.g., Presentation, PsychoPy, E-Prime). Ensures consistency and accurate data capture. |
| Participant Compliance Aids (Timeline Followback, SMS reminders) | Ensures adherence to pre-study restrictions (fasting, caffeine, alcohol, medications) which can profoundly influence drug metabolism and response. |
Visualizations
Title: Aligning Task Timing with Pharmacodynamic Peaks
Title: Research Workflow for Optimizing Task-Drug Timing
Application Notes
Within pharmacological challenge studies of human dopamine (DA) function, a primary pitfall is the conflation of DA's role in incentive salience ("wanting") with hedonic impact ("liking") and general task performance confounds (e.g., psychomotor speed, attention, learning). Accurate interpretation requires paradigms that dissociate these constructs. Pharmacological agents (e.g., DA agonists/antagonists, catechol-O-methyltransferase [COMT] inhibitors, tyrosine/phenylalanine depletion) manipulate DA transmission, but their effects on subjective and behavioral measures are often ambiguous.
Table 1: Key Constructs, Their Operationalizations, and Confounding Factors
| Psychological Construct | Operationalization in Tasks | Primary DA Circuit | Common Performance Confounds |
|---|---|---|---|
| 'Wanting' (Incentive Salience) | Effort Expenditure for Rewards (EEfRT), Progressive Ratio Breakpoint, Cue-Induced Craving Ratings, Pavlovian-Instrumental Transfer | Mesolimbic (VTA → NAcc) | Motor fatigue, differential reinforcement learning, perceived task difficulty. |
| 'Liking' (Hedonic Reaction) | Affective Facial Expressions (e.g., taste reactivity), Explicit Pleasure Ratings of Reward Consumption, Pleasantness Ratings | Ventral Pallidum, Opioid Systems | Expectation effects, scale use bias, social desirability in reporting. |
| Task Performance Confound | Reaction Time, Trial Accuracy, Learning Rate, Motor Coordination | Nigrostriatal, Mesocortical | Non-specific drug effects (sedation, arousal), baseline cognitive ability, practice effects. |
Table 2: Example Pharmacological Agent Effects on Behavioral Measures
| Pharmacological Manipulation | Theoretical DA Effect | Reported Effect on 'Wanting' Measures | Reported Effect on 'Liking' Measures | Common Performance Confound Observed |
|---|---|---|---|---|
| D2/D3 Agonist (e.g., Pramipexole) | ↑ DA receptor stimulation | ↑ Motivation for reward, ↑ cue-induced craving | Minimal change or slight ↓ in pleasure ratings | ↑ Impulsivity, ↓ motor learning, nausea. |
| DA Depletion (AMP/ATD) | ↓ DA synthesis, release | ↓ Effort expenditure, ↓ cue-induced 'wanting' | Minimal change to explicit pleasure ratings | ↓ Psychomotor speed, ↑ fatigue, working memory impairment. |
| COMT Inhibitor (e.g., Tolcapone) | ↑ Cortical DA (via reduced degradation) | Context-dependent effects on motivation | Potential subtle ↑ in reward anticipation ratings | Improved executive function, may alter reversal learning. |
Experimental Protocols
Protocol 1: Dissociating 'Wanting' from Performance Using the Effort Expenditure for Rewards Task (EEfRT) Under DA Challenge
- Objective: To assess dopaminergic modulation of incentive motivation independent of motor capability.
- Design: Randomized, double-blind, placebo-controlled, within-subject pharmaco-challenge.
- Procedure:
- Screening & Baseline: Participants complete practice EEfRT and motor speed/coordination battery (e.g., finger tapping, simple reaction time).
- Pharmacological Challenge: Administration of study drug (e.g., DA antagonist like amisulpride) or placebo.
- Task Administration (EEfRT): At peak plasma drug concentration, participants perform the EEfRT. On each trial, they choose between a "Hard Task" (high effort, e.g., rapid button presses) for a larger monetary reward and an "Easy Task" (low effort) for a smaller reward. Reward magnitude and probability are titrated.
- Control Measures: Concurrently administer a psychomotor vigilance task (PVT) and a subjective fatigue/arousal scale.
- Critical Analysis: The primary outcome is the proportion of hard-task choices. A drug-induced reduction in this proportion, uncorrelated with changes in PVT performance or simple motor speed, supports a specific effect on 'wanting'. Correlation with motor slowing suggests a performance confound.
Protocol 2: Assessing 'Liking' vs. 'Wanting' Using the Sweet Taste Test with Facial Electromyography (EMG)
- Objective: To separate dopaminergic effects on hedonic reactions from reported desire.
- Design: Randomized, double-blind, placebo-controlled.
- Procedure:
- Preparation: Apply facial EMG electrodes over the zygomaticus major ("smile") and corrugator supercilii ("frown") muscles.
- Challenge: Administer drug (e.g., mixed D1/D2 agonist) or placebo.
- Taste Test: Present small, controlled volumes of sweet (sucrose) and neutral (water) solutions via syringe.
- Measures:
- Implicit 'Liking': Record EMG activity (zygomatic response to sweet vs. water).
- Explicit 'Liking': Collect immediate subjective pleasantness ratings on a visual analog scale.
- Explicit 'Wanting': Collect desire-to-consume-more ratings for each solution.
- Critical Analysis: Compare drug effects on EMG-defined hedonic reactivity (implicit 'liking') versus desire ratings ('wanting'). A drug that alters desire ratings without changing zygomatic responses suggests a specific effect on 'wanting' rather than core pleasure.
Visualizations
Title: Interpreting DA Challenge Outcomes: Core Constructs
Title: EEfRT Protocol to Isolate 'Wanting'
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in DA Challenge Studies |
|---|---|
| Selective DA Agonists/Antagonists (e.g., Pramipexole, Amisulpride) | To probe the role of specific DA receptor subtypes (D1-like, D2-like) in reward processing. |
| Acute Phenylalanine/Tyrosine Depletion (APD/ATD) | A dietary method to transiently reduce central DA synthesis, creating a temporary DA-deficient state. |
| COMT Inhibitors (e.g., Tolcapone, Entacapone) | To increase synaptic DA, primarily in the prefrontal cortex, by inhibiting its enzymatic degradation. |
| Validated Effort-Based Decision-Making Tasks (e.g., EEfRT, Progressive Ratio) | Standardized paradigms to quantify motivational drive ('wanting') independent of reward consumption. |
| Facial Electromyography (EMG) System | To objectively measure implicit affective ('liking') reactions via facial muscle activity (e.g., zygomaticus). |
| Psychomotor Vigilance Task (PVT) | A simple reaction time task to control for non-specific effects of drugs on arousal and motor speed. |
| Subjective State Scales (e.g., Profile of Mood States [POMS], visual analog scales for desire/pleasure) | To quantify self-reported drug effects, craving, mood, and hedonic experience. |
Converging Evidence: Validating and Contrasting Pharmacological Probes with Alternative Approaches
Within the thesis on pharmacological challenge studies for dopamine (DA) and reward functioning in humans, a central methodological question arises: how do insights from acute pharmacological manipulations compare with those from studies of stable genetic polymorphisms? This document details application notes and protocols for these complementary strategies, focusing on the canonical example of D2 dopamine receptor (DRD2) and the linked ANKK1 Taq1A polymorphism.
Table 1: Comparison of Pharmacological vs. Genetic Strategies for DA Research
| Aspect | Pharmacological Challenge | Genetic Polymorphism Study |
|---|---|---|
| Primary Manipulation | Acute administration of a DA receptor agonist/antagonist (e.g., Cabergoline, Haloperidol). | Natural grouping based on inherited genotype (e.g., DRD2/ANKK1 Taq1A: A1+ vs. A1-). |
| Temporal Resolution | High (acute, within-session effects). | Low (trait-like, lifetime influence). |
| Mechanistic Target | Direct, reversible binding to pre- or post-synaptic DA receptors. | Indirect, proxy for lifelong alterations in DA receptor density or function. |
| Causal Inference | Strong for acute DA role in task. | Correlational; linkage disequilibrium and pleiotropy complicate causality. |
| Key Confounds | Non-specific effects (other receptor systems), pharmacokinetics, baseline DA tone. | Population stratification, small effect sizes, epigenetic and environmental moderators. |
| Typical Outcome Measures | BOLD fMRI signal during reward anticipation, behavioral shift in reinforcement learning. | Baseline BOLD fMRI signal, structural MRI (striatal volume), clinical association odds. |
Table 2: Meta-Analytic Summary of Key Findings for DRD2/ANKK1 Taq1A Polymorphism
| Phenotype | Effect Size (Cohen's d or Odds Ratio) | Notes |
|---|---|---|
| Striatal D2 Receptor Availability | d = -0.74 [95% CI: -0.99, -0.49] | A1+ carriers show ~30% lower BPND in striatum in PET studies. |
| Reward Anticipation fMRI (VS Activity) | d = -0.50 [95% CI: -0.78, -0.22] | Reduced ventral striatal BOLD signal in A1+ carriers. |
| Risk for Substance Dependence | OR = 1.46 [95% CI: 1.28, 1.67] | A1 allele associated with increased risk across multiple substances. |
| Antipsychotic Response (Prolactin) | d = 0.62 | A1+ carriers show greater D2 blockade response. |
Experimental Protocols
Protocol 1: Acute D2 Receptor Pharmacological Challenge with fMRI
Title: Assessing Dopamine’s Acute Role in Reward Processing. Objective: To measure the effect of acute D2 receptor modulation on neural correlates of reward anticipation and outcome. Design: Randomized, double-blind, placebo-controlled, crossover.
Materials & Reagents:
- Drug: Cabergoline (D2/D3 agonist, 0.5-1 mg oral) or Haloperidol (D2 antagonist, 2-3 mg oral). Placebo: Matched lactose pill.
- fMRI: 3T MRI scanner with compatible head coil.
- Task: Monetary Incentive Delay (MID) task programmed in Presentation/ Psychtoolbox.
Procedure:
- Screening & Consent: Obtain IRB-approved informed consent. Screen for contraindications (cardiovascular, psychiatric, pregnancy).
- Session 1 (Drug/Placebo):
- Participant fasts for 4 hours.
- Administer drug or placebo. Wait 2-3 hours for peak plasma concentration.
- Pre-scan Training: Complete 20 practice trials of the MID task outside scanner.
- fMRI Acquisition: Perform structural (T1-weighted) and functional (T2*-weighted EPI) scans during the MID task (~30 mins). The MID task includes cues signaling potential gain, loss, or neutral outcome, followed by a target response and feedback.
- Safety Monitoring: Monitor vitals and subjective state (e.g., Profile of Mood States).
- Washout & Session 2: Allow >=1 week washout. Repeat procedure with alternate treatment (drug/placebo).
- Data Analysis:
- Preprocess fMRI data (realignment, normalization, smoothing).
- Model BOLD response for reward anticipation (cue period) and outcome (feedback period) using GLM.
- Contrast activity in Drug vs. Placebo conditions in a priori Regions of Interest (ROI: ventral striatum, substantia nigra/VTA).
Protocol 2: Genotyping and Group Comparison for DRD2/ANKK1 Taq1A
Title: Assessing Trait-like Dopamine Function via ANKK1/DRD2 Genotyping. Objective: To compare reward-related phenotypes between carriers and non-carriers of the Taq1A A1 allele. Design: Cross-sectional, genetic association study.
Materials & Reagents:
- DNA Source: Saliva (Oragene kits) or blood.
- Genotyping Kit: TaqMan SNP Genotyping Assay (Assay ID: C748667510 for rs1800497) or PCR-RFLP primers.
- PCR Thermocycler & Real-Time PCR System (for TaqMan).
- Restriction Enzyme Taq1 (for RFLP).
Procedure:
- Sample Collection & DNA Extraction: Collect saliva/blood. Extract genomic DNA using standardized commercial kits. Quantify DNA via spectrophotometry.
- Genotyping (TaqMan Example):
- Prepare reaction mix: 10 ng DNA, 1x TaqMan Genotyping Master Mix, 1x TaqMan Assay.
- Run on Real-Time PCR System: 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min.
- Use allelic discrimination plot to assign genotypes: A1/A1, A1/A2, A2/A2.
- Group Assignment: Categorize participants into A1+ (A1/A1 + A1/A2) and A1- (A2/A2) groups.
- Phenotypic Assessment: All participants (genotyped blind) complete the MID task in the fMRI scanner without pharmacological manipulation.
- Data Analysis:
- Compare BOLD signal during reward anticipation between A1+ and A1- groups using a two-sample t-test in the ventral striatum ROI.
- Covary for potential confounds (age, sex, ancestry principal components).
Visualizations
Title: Comparison of Pharmacological and Genetic Research Strategies
Title: Pharmacological fMRI Challenge Study Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Dopamine Challenge & Genetic Studies
| Item | Function/Description | Example Product/Catalog |
|---|---|---|
| Selective D2 Agonist | Acute, reversible activation of D2 receptors to probe system function. | Cabergoline (Dostinex); also used: Bromocriptine. |
| Selective D2 Antagonist | Acute, reversible blockade of D2 receptors. | Haloperidol (Haldol); Sulpiride (limited central access). |
| Placebo Matched Tablets | Critical for double-blind design in pharmacological studies. | Custom compounded lactose tablets identical in appearance. |
| DNA Collection Kit | Non-invasive, stable collection of buccal cells/saliva for genotyping. | DNA Genotek • Oragene DISCOVER (OGD-500). |
| TaqMan SNP Genotyping Assay | Accurate, high-throughput allelic discrimination for specific polymorphisms. | Thermo Fisher • TaqMan Assay for rs1800497 (C748667510). |
| Monetary Incentive Delay (MID) Task | Standardized fMRI paradigm to dissect reward anticipation vs. outcome. | Open-source code available via PsychoPy/Psychtoolbox repositories. |
| fMRI Analysis Software | Processing and statistical analysis of BOLD data. | SPM12, FSL, AFNI. |
| Ancestry Informative Markers | Control for population stratification in genetic association studies. | AIMs Panels (e.g., from Thermo Fisher). |
This document provides application notes and protocols for the cross-validation of Positron Emission Tomography (PET) and functional Magnetic Resonance Imaging (fMRI) biomarkers within pharmacological challenge studies on dopamine (DA) and reward functioning. A core thesis in this field posits that individual differences in baseline dopaminergic tone, as quantified by D2/3 receptor availability (BPND), predict the magnitude of task-induced ventral striatal BOLD signal during reward anticipation. Cross-validating these multimodal biomarkers is critical for developing non-invasive predictive models of individual response to dopaminergic drugs in neuropsychiatric disorders.
Table 1: Representative Findings from Pharmacological Challenge Studies Correlating PET D2/3 and fMRI BOLD
| Study (Example) | PET Radioligand | fMRI Task | Key Brain Region | Correlation (BPND vs. BOLD) | Effect of DA Challenge |
|---|---|---|---|---|---|
| Baseline Studies | [¹¹C]raclopride | Monetary Incentive Delay (MID) | Ventral Striatum | r ≈ -0.60 to -0.70 (Negative) | Not Applied |
| Acute Depletion (αMPT) | [¹¹C]raclopride | MID | Ventral Striatum | r ≈ -0.50 (Negative) | Correlation strength modulated by depletion |
| Acute Agonist (Amphetamine) | [¹¹C]raclopride | Gambling Task | Ventral Striatum | Pre-drug: r ≈ -0.55 | Amphetamine reduces BPND (DA release) and alters BOLD correlation |
| Genetic Moderation (DRD2 Taq1A) | [¹¹C]FLB 457 | MID | Ventral Striatum | A1+ carriers show lower BPND and blunted BOLD | Highlights combined biomarker sensitivity |
Table 2: Typical Parameter Ranges for Cross-Validation Analyses
| Parameter | PET D2/3 (BPND) | fMRI BOLD (% Signal Change) |
|---|---|---|
| Typical Range in VS | 2.0 - 3.5 ([¹¹C]raclopride) | 0.2% - 0.8% (Reward > Neutral) |
| Test-Retest Variability | 5-10% (within-subject CV) | 15-25% (within-subject CV) |
| Critical Sample Size | N ≥ 20 for correlation power >0.8 | N ≥ 25 for robust group-level BOLD |
| Optimal Analysis Window | 30-60 min post-injection (equilibrium) | 4-8 sec post-cue (hemodynamic response) |
Experimental Protocols
Protocol 1: Concurrent PET/fMRI Data Acquisition for Cross-Validation
- Objective: To acquire matched, within-session PET D2/3 and fMRI BOLD data from the same individual.
- Materials: See "The Scientist's Toolkit" (Section 5).
- Procedure:
- Subject Preparation: Insert venous catheter for radioligand injection. Screen for MRI contraindications.
- Attenuation Scan: Position subject in PET-MR scanner. Perform low-dose CT or MR-based attenuation correction scan.
- Radioligand Bolus Injection: Initiate dynamic PET acquisition. Inject ~740 MBq (20 mCi) of [¹¹C]raclopride or [¹⁸F]fallypride as an intravenous bolus.
- Simultaneous fMRI Task: 40 minutes post-injection (during tracer equilibrium), initiate the fMRI reward task (e.g., MID) while PET acquisition continues. Total PET acquisition: 60-90 min.
- Image Reconstruction: Reconstruct PET data into dynamic frames (e.g., 1 min frames). Reconstruct fMRI data into time-series volumes.
Protocol 2: Pharmacological Challenge with Multimodal Imaging
- Objective: To assess the impact of altered DA transmission on both receptor availability and BOLD signal.
- Design: Double-blind, placebo-controlled, within-subject crossover.
- Procedure:
- Session 1 (Baseline): Perform Protocol 1 under placebo (saline injection administered prior to scanning).
- Session 2 (Challenge): After a suitable washout period (≥1 week), pre-administer the pharmacological agent (e.g., oral d-amphetamine 0.5 mg/kg or intravenous amphetamine 0.3 mg/kg) 60-90 minutes before scanning. Repeat Protocol 1.
- Key Analysis: Calculate the change in striatal BPND (ΔBPND) between sessions as an index of DA release. Correlate ΔBPND with the change in task-evoked BOLD signal (Δ%BOLD).
Visualization Diagrams
Title: Cross-Validation Informs Thesis on Drug Response
Title: Concurrent PET/fMRI Acquisition Protocol Workflow
Title: DA Challenge Impacts BPND and BOLD Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PET/fMRI Cross-Validation Studies
| Item | Function & Relevance | Example/Details |
|---|---|---|
| D2/3 PET Radioligands | Quantifies receptor availability (BPND). High affinity for striatum is key. | [¹¹C]Raclopride: Gold standard for striatum. [¹⁸F]Fallypride: Higher affinity, allows extrastriatal imaging. |
| Pharmacological Challenge Agent | Manipulates dopamine transmission to test biomarker sensitivity. | d-Amphetamine: Potent DA releaser. Sulpiride: D2/3 antagonist for blockade studies. |
| fMRI Reward Paradigm | Evokes dopamine-dependent ventral striatal BOLD signal. | Monetary Incentive Delay (MID): Standardized reward anticipation task. |
| Simultaneous PET/MR Scanner | Enables truly simultaneous, temporally aligned data acquisition. | Siemens Biograph mMR, GE SIGNA PET/MR. Critical for cross-validation. |
| Kinetic Modeling Software | Estimates BPND from dynamic PET data. | PMOD: Commercial solution. SRTM: Simplified Reference Tissue Model algorithm. |
| fMRI Analysis Suite | Preprocessing and GLM analysis of BOLD data. | SPM, FSL, AFNI: Standard packages for modeling task-evoked responses. |
| Multimodal Registration Tool | Precisely co-registers PET and fMRI data to anatomical MRI. | Advanced Normalization Tools (ANTs): For high-precision non-linear alignment. |
Comparing Challenge Studies to Lesion Models (Parkinson's Disease) and Computational Modeling of DA Signals
This document provides application notes and protocols for three interconnected methodologies used to investigate dopamine (DA) function: pharmacological challenge studies in humans, neurotoxic lesion models of Parkinson's Disease (PD), and computational modeling of DA signals. Within the broader thesis on human pharmacological challenge studies, lesion models offer causal validation of DA's role in observed behaviors, while computational models provide a formal framework to quantify DA signals (e.g., reward prediction error) that challenges are designed to perturb. Together, they form a translational triad for understanding DA in reward and motor functioning.
Comparative Analysis: Methodologies and Applications
Table 1: Core Comparison of Methodological Approaches
| Feature | Human Pharmacological Challenge Studies | Neurotoxic Lesion Models (PD) | Computational Modeling of DA |
|---|---|---|---|
| Primary Objective | Probe DA system function & receptor dynamics in vivo in healthy or clinical populations. | Establish causal link between DA depletion & behavioral/motor phenotypes; test therapeutic interventions. | Formally describe DA neuron activity or DA release dynamics (e.g., RPE) to predict behavior. |
| Typical Subjects | Human volunteers (healthy, patients with psychiatric/neurological conditions). | Rodents (rats, mice), non-human primates. | In silico agents; parameters often fit to human/animal data. |
| Key Manipulation | Administration of DAergic agents (e.g., agonist/antagonist, precursor, releaser). | Unilateral or bilateral striatal injection of 6-OHDA or systemic MPTP. | Algorithmic specification of learning rules and DA responses to stimuli/rewards. |
| Measured Outcomes | Neuroimaging (fMRI, PET), behavior (cognitive tasks, motor), subjective reports, physiology. | Motor asymmetry (rotation, forelimb use), cognitive-behavioral tasks, post-mortem DA cell counts. | Simulated DA signal traces, value estimates, choice probabilities; model fit to empirical data. |
| Temporal Resolution | Minutes to hours post-administration; acute effects. | Days to weeks post-lesion; chronic degeneration. | Milliseconds (neural) to seconds (behavioral) within the model. |
| Strengths | Direct human relevance; can assess receptor-specific functions. | Strong causal inference; enables histological verification; high control over DA depletion. | Precise, mechanistic theories; can disentangle latent variables; links neural to behavioral levels. |
| Limitations | Indirect measure of DA; systemic effects; pharmacokinetic variability. | Limited translational validity to human PD progression; species differences. | Model is only as good as its assumptions; requires validation against empirical data. |
| Complementarity | Provides human behavioral/imaging phenotypes for model fitting. | Validates the necessity of DA for behaviors inferred from challenge studies. | Provides quantitative framework to interpret both challenge & lesion study results. |
Table 2: Quantitative Data from Key Paradigms
| Model/Paradigm | Typical DA Depletion (%) | Key Behavioral Metric | Representative Value (Mean ± SEM or Range) |
|---|---|---|---|
| Unilateral 6-OHDA Rat (Medial Forebrain Bundle) | >95% (Striatum) | Net Contraversive Rotations (apomorphine, 0.05 mg/kg) | 300 - 600 turns/90 min |
| MPTP-treated Mouse (Acute) | 70-90% (Striatum) | Locomotor Activity (total beam breaks/60 min) | 65% decrease vs. control |
| Human DA Challenge (Amphetamine) | N/A (DA Release ↑) | Striatal DA Release (∆ Binding Potential via PET) | 15-25% ∆ [¹¹C]raclopride BPND |
| Computational Model (TD Learning) | N/A | Learning Rate (α) fitted from Probabilistic Reward Task | 0.05 - 0.3 (range) |
Experimental Protocols
Protocol 1: Human Pharmacological Challenge with fMRI
Title: Assessing DA Modulation of Reward Prediction Error with Levodopa and fMRI. Objective: To measure the effect of enhancing DA transmission on the neural correlates of reward prediction error (RPE) during a reinforcement learning task. Materials: Levodopa/Carbidopa (100/25 mg), placebo, fMRI scanner, probabilistic reward task. Procedure:
- Design: Randomized, double-blind, placebo-controlled, within-subject crossover.
- Pharmacology: Administer levodopa/carbidopa or identical placebo orally 60 minutes prior to scan.
- Task: Subjects perform a probabilistic reversal learning task in the scanner. Choices lead to probabilistic monetary rewards or losses.
- fMRI Acquisition: Use T2*-weighted EPI sequence (TR=2s, TE=30ms, voxel size=3x3x3mm). Acquire high-resolution T1 anatomical scan.
- Computational Modeling: Fit a Temporal Difference (TD) learning model to each subject's choice data to trial-wise RPE estimates.
- fMRI Analysis: Use the model-derived RPE time series as a parametric regressor in a GLM analysis of BOLD signal. Compare levodopa vs. placebo in a priori regions (ventral striatum, substantia nigra/VTA).
Protocol 2: Unilateral 6-OHDA Mouse Model of PD
Title: Induction of Hemi-Parkinsonism via Striatal 6-Hydroxydopamine. Objective: To create a stable, unilateral DA lesion for assessing motor deficits and therapeutic interventions. Materials: C57BL/6 mouse, 6-OHDA hydrobromide, desipramine, apomorphine, stereotaxic apparatus, Hamilton syringe. Procedure:
- Pre-treatment: Inject desipramine (25 mg/kg, i.p.) 30 min pre-surgery to protect noradrenergic neurons.
- Anesthesia: Induce and maintain surgical anesthesia (e.g., isoflurane 1-3%).
- Stereotaxic Surgery: Secure mouse in stereotaxic frame. Target coordinates for right striatum (from bregma): AP +1.0 mm, ML -2.0 mm, DV -3.0 mm (from dura). Drill burr hole.
- 6-OHDA Infusion: Prepare 6-OHDA (3 µg/µl in 0.02% ascorbic acid/saline). Load into a 5 µl Hamilton syringe. Lower needle to target and infuse 2 µl at 0.5 µl/min. Leave needle in place for 5 min post-infusion before slow withdrawal.
- Recovery: Monitor animal post-operatively for 7 days.
- Lesion Verification (3-4 weeks post-surgery):
- Apomorphine Rotation Test: Inject apomorphine (0.5 mg/kg, s.c.). Place mouse in cylindrical enclosure. Record contralateral rotations for 40 min. >7 full turns/min indicates successful lesion.
- Post-mortem Validation: Perfuse animal; process brain for immunohistochemistry against Tyrosine Hydroxylase (TH). Quantify TH+ fiber density in striatum.
Protocol 3: Fitting a TD Learning Model to Behavioral Data
Title: Quantifying DA-like RPE Signals from Choice Behavior. Objective: To derive trial-by-trial estimates of reward prediction error (RPE) using a computational model for correlation with neuroimaging or DA challenge data. Materials: Behavioral trial data (choices, outcomes), modeling software (e.g., Python, R, MATLAB). Procedure:
- Model Specification: Implement a basic TD Rescorla-Wagner model.
- Value update:
V(stimulus)t+1 = V(stimulus)t + α * (rewardt - V(stimulus)t) - RPE on trial t:
δt = rewardt - V(stimulus)t - Choice rule: Use softmax
P(choice A) = exp(β * V(A)) / [exp(β * V(A)) + exp(β * V(B))]
- Value update:
- Data Preparation: Format choice (0/1) and reward (e.g., +1/0) data.
- Parameter Estimation: Use maximum likelihood or Bayesian estimation to find the parameters (learning rate
α, inverse temperatureβ) that best explain the subject's choices. - Model Validation: Compare to alternative models (e.g., hidden Markov model) using cross-validation or information criteria (AIC/BIC).
- RPE Extraction: Generate the time series of
δtusing the best-fit parameters. This RPE signal can be used as a regressor in fMRI analysis or compared across drug/lesion conditions.
Visualizations
Title: The Translational Triad for Studying Dopamine Function
Title: Computational Model of DA Reward Prediction Error
Title: 6-OHDA Lesion Model Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials
| Item | Function/Description | Example Use Case |
|---|---|---|
| 6-Hydroxydopamine (6-OHDA) | Catecholaminergic neurotoxin; selective for DA & NE neurons when combined with NE reuptake inhibitor. | Creating stable, unilateral striatal lesions in rodent PD models. |
| MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) | Prodrug neurotoxin causing selective destruction of nigrostriatal DA neurons. | Inducing systemic Parkinsonism in mice and non-human primates. |
| Levodopa/Carbidopa | DA precursor (levodopa) with peripheral DOPA decarboxylase inhibitor (carbidopa). | Pharmacological challenge to enhance central DA in human fMRI studies. |
| [¹¹C]Raclopride | Radiolabeled D2/D3 receptor antagonist for Positron Emission Tomography (PET). | Measuring changes in synaptic DA levels following amphetamine challenge. |
| Apomorphine | Non-selective DA receptor agonist (D1/D2). | Inducing contralateral rotations in unilateral 6-OHDA lesioned rodents to verify lesion. |
| Desipramine | Norepinephrine reuptake inhibitor. | Pre-treatment to protect NE neurons from 6-OHDA toxicity in lesion models. |
| Anti-Tyrosine Hydroxylase Antibody | Primary antibody for immunohistochemistry targeting the rate-limiting DA synthesis enzyme. | Visualizing and quantifying DA neuron survival and fiber density post-lesion. |
| Temporal Difference (TD) Learning Model | Computational algorithm that learns to predict future reward, generating a phasic RPE signal. | Quantifying trial-by-trial DA-like learning signals from behavioral choice data. |
Introduction In pharmacological challenge studies investigating dopamine (DA) and reward functioning in humans, a core assumption is that a drug's primary action on a specific molecular target (e.g., the D2 receptor) directly translates to a specific, isolable neurochemical and behavioral output. This article critiques this assumption by examining two intrinsic limitations: 1) the imperfect selectivity of agents for receptor subtypes, and 2) the inevitable network-level effects that emerge from modulating a node within a highly interconnected neural system. These limitations are critical for interpreting data from studies using drugs like amphetamine, methylphenidate, or selective DA receptor agonists/antagonists.
1. Quantitative Data on Pharmacological Selectivity The following tables summarize binding affinity (Ki) data for commonly used dopaminergic challenge agents, illustrating their cross-reactivity.
Table 1: Receptor Binding Profiles of Selected Dopaminergic Agents
| Agent (Primary Target) | D1 Ki (nM) | D2 Ki (nM) | D3 Ki (nM) | 5-HT2A Ki (nM) | NET Ki (nM) | References |
|---|---|---|---|---|---|---|
| Raclopride (Antagonist) | >10,000 | 1.1 - 2.4 | 3.5 - 7.4 | >10,000 | >10,000 | Seeman et al. (2005), Synapse |
| Pramipexole (Agonist) | >10,000 | 2,500 - 5,000 | 0.5 - 5.4 | >10,000 | >10,000 | Millan et al. (2002), J. Pharmacol. Exp. Ther. |
| d-Amphetamine (Releaser) | >10,000 | >10,000 | >10,000 | >10,000 | 16 - 40 | Rothman et al. (2001), Synapse |
| Levo-DOPA (Prodrug) | N/A (Metabolite) | N/A (Metabolite) | N/A (Metabolite) | N/A (Metabolite) | N/A (Metabolite) | N/A (Non-selective DA increase) |
| Aripiprazole (Partial Agonist) | >10,000 | 0.8 - 1.5 | 8.5 | 8.7 (Antag.) | >10,000 | Shapiro et al. (2003), Neuropsychopharmacology |
Table 2: Network-Level Outcomes in Human Challenge Studies
| Challenge Paradigm | Intended Specific Effect | Observed Network-Level Correlates (fMRI/PET) | Potential Confound |
|---|---|---|---|
| D2 Antagonism (e.g., Haloperidol) | Block striatal D2 receptors, reduce reward signaling. | Altered connectivity in fronto-striatal circuits; modulated amygdala & insula reactivity to aversive stimuli. | Mood/anxiety changes indirectly affect reward tasks. |
| DA Releaser (e.g., d-Amphetamine) | Increase synaptic DA, enhance reward learning. | BOLD signal decrease in striatum (due to DA-ergic modulation of vascular tone); widespread cortical activation. | Vascular vs. neuronal signal ambiguity; noradrenergic effects on attention. |
| D3-Preferential Agonism (e.g., Pramipexole) | Modulate limbic DA function. | Altered reactivity in ventral striatum and default mode network; sleep architecture changes. | Off-target D2 effects at higher doses; secondary network adaptation. |
2. Experimental Protocols
Protocol 1: In Vitro Receptor Selectivity Validation for a Novel Ligand Purpose: To accurately determine the binding affinity (Ki) of a putative selective D3 agonist across a panel of human cloned receptors. Materials: Cell membranes expressing human D1, D2L, D3, 5-HT1A, 5-HT2A, α2A-AR receptors; [³H]-7-OH-DPAT (D3 radioligand) and respective radioligands for other receptors; test compound; assay buffer (50 mM Tris-HCl, pH 7.4, 120 mM NaCl, 5 mM KCl, 4 mM MgCl2, 1.5 mM CaCl2); GF/B filter plates; scintillation cocktail. Procedure:
- Prepare serial dilutions of the test compound (typically 10^-5 to 10^-11 M) in assay buffer.
- For each receptor, combine in triplicate: 100 µL membrane suspension, 50 µL of appropriate radioligand (at ~Kd concentration), and 50 µL of test compound dilution or buffer (for total binding) or 50 µL of high-concentration reference antagonist (for nonspecific binding).
- Incubate for 120 minutes at room temperature to reach equilibrium.
- Terminate binding by rapid filtration onto GF/B filter plates pre-soaked in 0.3% PEI, followed by 3x washes with ice-cold buffer.
- Dry plates, add scintillation fluid, and quantify bound radioactivity using a microplate scintillation counter.
- Analyze data: Calculate % inhibition. Use nonlinear regression (e.g., one-site competition model) to determine Ki values from IC50 using the Cheng-Prusoff equation. Analysis: A compound is considered "D3 selective" if its Ki at D3 is at least 100-fold lower than at D2 and other screened receptors.
Protocol 2: fMRI Pharmacological Challenge Study of Reward Prediction Error Purpose: To assess the effect of a D2/D3 antagonist on the neural correlates of reward prediction error (RPE) in humans. Materials: Double-blind, placebo-controlled design; oral dose of drug (e.g., amisulpride 400 mg) or placebo; 3T MRI scanner with gradient-echo EPI capability; computational task (e.g., probabilistic reinforcement learning task); analysis software (SPM, FSL, or similar). Procedure:
- Screening & Consent: Recruit healthy participants; obtain informed consent; conduct medical/psychiatric screening and MRI safety check.
- Session: Participants ingest drug or placebo capsule 3 hours prior to scanning (Tmax for amisulpride).
- Task: In the scanner, participants complete a task where they choose between abstract symbols with differing, probabilistic reward feedback (e.g., 80/20% chance).
- Imaging: Acquire T1-weighted structural scan. During task, acquire T2*-weighted BOLD fMRI (TR=2000 ms, TE=30 ms, voxel size=3x3x3mm).
- Computational Modeling: Fit trial-by-trial behavioral choice data with a Q-learning model to derive a participant-specific RPE signal (δ) for each trial.
- fMRI Analysis: Preprocess data (realignment, normalization, smoothing). Model the first-level GLM with the parametric modulator of RPE (δ) at the time of feedback. Create contrast images for the RPE regressor.
- Group Analysis: Perform second-level random-effects analysis (drug vs. placebo) on the RPE contrast images. Use whole-brain correction (e.g., cluster-level FWE p<0.05). Interpretation Caveats: Any observed BOLD signal change in striatum may reflect direct D2 blockade and/or downstream network adaptation (e.g., altered prefrontal input). Correlations with drug plasma levels can strengthen inference.
3. Diagrams (Generated with Graphviz)
Diagram 1 Title: How Drug Off-Target Effects Lead to Confounded Phenotypes
Diagram 2 Title: DA Reward Network: A Target Node Affects the Whole Circuit
4. The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Relevance to Challenge Studies |
|---|---|
| High-Affinity, Subtype-Selective Radioligands (e.g., [³H]-(+)-PHNO for D3/D2high) | Crucial for in vitro binding assays to definitively quantify a challenge drug's receptor selectivity profile before human use. |
| PET Radiotracers with Different Sensitivity (e.g., [¹¹C]Raclopride for D2/3, [¹¹C]SCH23390 for D1) | Allows probing of drug occupancy at intended vs. off-target sites in vivo and assessing downstream receptor adaptations. |
| Selective Chemical or Genetic Probes (e.g., DREADDs or novel ultra-selective tool compounds like PG01037 for D3) | Used in preclinical models to disentangle the effects of modulating a specific receptor subtype from network effects. |
| Computational Modeling Software (e.g., MATLAB with COGENT, hBayesDM, or Stan) | Essential for deriving computational phenotypes (e.g., RPE, learning rate) from behavioral data, linking drug effects to specific algorithmic processes. |
| Simultaneous Multi-modal Acquisition Platforms (e.g., combined fMRI/pupillometry or EEG/fMRI) | Enables capturing network-level brain activity (fMRI) alongside real-time indices of arousal/attention (pupillometry) or neural oscillations (EEG) to deconvolve direct vs. indirect drug effects. |
Application Notes
Pharmacological challenge studies are a critical translational bridge in neuroscience drug development. By administering a compound (e.g., a dopamine agonist, antagonist, or precursor) to healthy volunteers or patient populations and measuring multi-modal responses, these studies provide a controlled model of system engagement. The core translational value lies in linking acute, mechanism-based neurobiological and behavioral readouts to the long-term therapeutic outcomes sought in clinical trials for disorders like schizophrenia, depression, addiction, and Parkinson's disease.
Key Translational Links:
- Target Engagement Verification: Neuroimaging (e.g., fMRI, PET) during a challenge can confirm that a novel drug reaches and modulates its intended neural target (e.g., striatal dopamine release), de-risking Phase II trials.
- Biomarker Validation: Challenge-induced changes in electrophysiology (EEG), neuroendocrine response (prolactin, cortisol), or task-based behaviors (reinforcement learning, effort expenditure) serve as quantifiable biomarkers. These can be used to stratify patients, guide dosing, and provide early efficacy signals.
- Dose-Ranging and Safety: Controlled challenges help establish a compound's pharmacodynamic profile, identifying a window between minimally effective and maximally tolerable doses for neurological and psychiatric indications.
- De-risking Novel Mechanisms: For drugs acting on novel or complex systems (e.g., trace amine-associated receptor 1 [TAAR1]), challenge paradigms can provide the first in-human evidence of functional central activity, informing go/no-go decisions.
The following protocols and data tables outline standardized methodologies for implementing dopamine-focused challenge studies within a drug development pipeline.
Protocol 1: Acute Dopamine Precursor Challenge with Behavioral and Neuroendocrine Readouts
Objective: To assess central dopamine system capacity and its behavioral correlates using an acute oral dose of levodopa (L-DOPA) combined with a reward motivation task.
Detailed Methodology:
Participant Screening & Preparation:
- Recruit N=20-30 healthy volunteers (or patient cohort matched to study objectives). Exclude for major medical, psychiatric, or neurological conditions, current medications, or substance abuse.
- Conduct a baseline session for practice on cognitive tasks and acclimatization.
- Fasting & Restrictions: Participants fast overnight (water allowed) and abstain from caffeine, nicotine, and alcohol for 24 hours prior to the test session.
Experimental Session Timeline (Double-Blind, Placebo-Controlled, Crossover Design):
- T-60 min: Arrival, compliance check, insertion of intravenous cannula for blood sampling.
- T-30 min: Baseline blood sample (for prolactin/cortisol), baseline mood/arousal scales (e.g., Visual Analogue Scales [VAS], Positive and Negative Affect Schedule [PANAS]).
- T0 min: Administration of oral capsule: Placebo or L-DOPA (100/25 mg levodopa/carbidopa). Co-administration of carbidopa (peripheral DOPA decarboxylase inhibitor) is standard to minimize peripheral side effects.
- T+60 min: Post-dose blood sample and mood scales. Begin Effort Expenditure for Rewards Task (EERT).
- T+90 min: Post-task blood sample and debrief.
Key Outcome Measures:
- Primary Behavioral: Proportion of "hard task" choices in the EERT as a function of reward magnitude and probability. Dopamine augmentation is expected to increase willingness to expend effort for higher rewards.
- Primary Neuroendocrine: Plasma prolactin levels. Dopamine (via tuberoinfundibular pathway) tonically inhibits prolactin secretion; effective central DA increase should reduce prolactin from baseline.
- Secondary: Subjective state changes (VAS), cardiovascular monitoring (BP, HR).
Data Analysis:
- Use mixed-effects models with condition (Placebo vs. L-DOPA), time, and their interaction as fixed effects, and subject as a random effect.
- Correlate change in prolactin with change in hard-task choices to link neuroendocrine and behavioral effects.
Table 1: Representative Data from an L-DOPA Challenge Study (Hypothetical Cohort, N=24)
| Measure | Baseline (Mean ± SEM) | Placebo (T+90 min) | L-DOPA (T+90 min) | Effect Size (Cohen's d) | p-value |
|---|---|---|---|---|---|
| Plasma Prolactin (μg/L) | 8.2 ± 0.7 | 8.5 ± 0.8 | 5.1 ± 0.6* | 1.45 | <0.001 |
| EERT: Hard Task Choice (%) | -- | 62.3 ± 4.1 | 78.9 ± 3.5* | 0.92 | 0.005 |
| Systolic BP (mm Hg) | 118 ± 2 | 119 ± 2 | 122 ± 2 | 0.15 | 0.32 |
| VAS "Energy" (0-100) | 52 ± 3 | 50 ± 4 | 65 ± 4* | 0.81 | 0.01 |
Significantly different from Placebo (p < 0.05, corrected).
Protocol 2: Dopamine Receptor Antagonist Challenge with Functional MRI
Objective: To characterize target engagement and circuit-level effects of a novel dopamine D2/D3 receptor antagonist using a pharmacological fMRI paradigm with a monetary incentive delay (MID) task.
Detailed Methodology:
Design: Randomized, double-blind, placebo-controlled, between-groups design in healthy volunteers (N=15 per group).
Drug Administration:
- Experimental Arm: Single oral dose of a novel D2/D3 antagonist (e.g., 3 mg) or a reference compound (e.g., amisulpride 200 mg).
- Control Arm: Matched placebo.
- Administration occurs 3 hours prior to scan to align with expected Tmax.
fMRI Acquisition & Task:
- Acquire T1-weighted structural and T2*-weighted echo-planar imaging (EPI) scans on a 3T MRI scanner.
- MID Task: Participants complete a block-design task with cues predicting potential monetary gain, loss, or neutral outcomes, followed by a rapid target response to "win" or "avoid loss."
- Contrast of Interest: "Anticipation of Reward vs. Neutral" (Reward Cue > Neutral Cue).
Primary & Secondary Outcomes:
- Primary: BOLD signal attenuation in the ventral striatum (nucleus accumbens) during reward anticipation in the drug group vs. placebo. This demonstrates target engagement at the circuit level.
- Secondary: Correlation between striatal BOLD attenuation and drug plasma levels; modulation of reward prediction error signals in the ventral tegmental area (VTA); behavioral performance (reaction time) on the MID task.
Analysis Pipeline:
- Preprocess data (realignment, normalization, smoothing) using standard software (SPM, FSL).
- First-level analysis models BOLD response to cue types. Second-level group analysis uses a full factorial design.
- Region-of-Interest (ROI) analysis for the ventral striatum with small-volume correction.
Table 2: Key fMRI Findings from a D2 Antagonist Challenge (Hypothetical Data)
| Brain Region (ROI) | Placebo Group Beta (Reward-Neutral) | Drug Group Beta (Reward-Neutral) | Group Difference (t-value) | p-value (SVC) |
|---|---|---|---|---|
| Ventral Striatum | 0.85 ± 0.12 | 0.31 ± 0.10 | 3.45 | 0.008 |
| Ventral Tegmental Area | 0.42 ± 0.08 | 0.15 ± 0.07 | 2.51 | 0.035 |
| Medial Prefrontal Cortex | 0.58 ± 0.09 | 0.50 ± 0.11 | 0.55 | 0.58 |
SVC: Small-Volume Corrected.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in Challenge Studies |
|---|---|
| Levodopa/Carbidopa (Sinemet) | Gold-standard dopamine precursor challenge. Carbidopa inhibits peripheral conversion, increasing central L-DOPA availability. Used to probe DA system capacity. |
| d-Amphetamine | Potent dopamine/norepinephrine releaser and reuptake inhibitor. Used to evoke robust DA release, validated with PET, to test system responsiveness or "stress" the system. |
| Haloperidol / Amisulpride | Typical (D2 antagonist) and atypical (D2/D3 antagonist) antipsychotics. Used to acutely blunt DA signaling, establishing a model of hypodopaminergia and testing novel compound efficacy. |
| [11C]Raclopride / [11C]PHNO | PET radioligands for D2/D3 receptors. Used concurrently with DA-releasing challenges (e.g., amphetamine) to quantify endogenous dopamine release via displacement binding. |
| Monetary Incentive Delay (MID) Task | Well-validated fMRI paradigm isolating reward anticipation and consummation phases. Sensitive to pharmacological manipulation of the dopamine system. |
| Effort Expenditure for Rewards Task (EERT) | Behavioral probe of motivation and cost-benefit decision-making. DA agonists typically increase willingness to exert effort for larger rewards. |
| Prolactin ELISA Kit | Standard neuroendocrine readout. Plasma prolactin is inversely related to tuberoinfundibular dopamine tone, providing a peripheral proxy for central D2 receptor occupancy. |
| Positive and Negative Affect Schedule (PANAS) | Validated subjective mood scale to track affective state changes induced by pharmacological challenges. |
Visualizations
Title: L-DOPA Challenge Mechanism and Readouts
Title: Translational Pathway from Challenge Study to Trial
Title: Dopamine Antagonist fMRI Challenge Protocol
Conclusion
Pharmacological challenge studies remain an indispensable, though complex, methodology for directly probing the causal role of dopamine in human reward processing. This review synthesizes insights from foundational theory, methodological execution, troubleshooting, and cross-method validation. The future of the field lies in leveraging more selective receptor-targeting compounds, integrating multimodal neuroimaging and computational psychiatry frameworks, and designing personalized challenge paradigms that account for genetic and phenotypic variability. For drug development, these studies provide a critical experimental medicine bridge, enabling target engagement verification and mechanistic subtyping of disorders characterized by reward dysfunction, ultimately paving the way for more precise and effective therapeutics.