Comparative Efficacy of Cognitive Rehabilitation Techniques in Post-Stroke Cognitive Impairment: A Systematic Analysis for Research and Development
This article provides a comprehensive comparative analysis of contemporary cognitive rehabilitation techniques for post-stroke cognitive impairment (PSCI), tailored for researchers, scientists, and drug development professionals.
Comparative Efficacy of Cognitive Rehabilitation Techniques in Post-Stroke Cognitive Impairment: A Systematic Analysis for Research and Development
Abstract
This article provides a comprehensive comparative analysis of contemporary cognitive rehabilitation techniques for post-stroke cognitive impairment (PSCI), tailored for researchers, scientists, and drug development professionals. It synthesizes recent evidence from randomized controlled trials and meta-analyses to evaluate the efficacy of diverse interventions, including non-invasive brain stimulation (tDCS, rTMS), technology-assisted rehabilitation (Virtual Reality, computer-based training), pharmacological approaches, and conventional cognitive training. The analysis explores neurobiological mechanisms, methodological considerations for clinical application, optimization strategies to address heterogeneity in treatment response, and comparative effect sizes across modalities. By integrating foundational science with applied clinical research, this review aims to inform the development of targeted, multimodal therapeutic strategies and guide future research directions in stroke cognitive rehabilitation.
The Neurobiological Landscape of Post-Stroke Cognitive Impairment and Foundational Rehabilitation Principles
Post-stroke cognitive impairment (PSCI) represents a significant challenge in stroke recovery, profoundly affecting patients' functional independence and quality of life. As stroke remains a leading cause of adult disability globally, understanding the epidemiology, specific cognitive domain deficits, and subsequent impact on functional outcomes is crucial for developing targeted rehabilitation strategies. This review synthesizes current evidence on PSCI prevalence, identifies the most commonly affected cognitive domains, and elucidates the relationship between cognitive deficits and functional recovery trajectories. The objective assessment of this burden provides a foundation for optimizing cognitive rehabilitation within stroke research and clinical practice, ultimately aiming to improve long-term outcomes for stroke survivors through evidence-based interventions.
Epidemiological Profile of Post-Stroke Cognitive Impairment
Prevalence and Scope of the Problem
Post-stroke cognitive impairment is remarkably prevalent among stroke survivors. A recent cross-sectional study conducted at the National Hospital of Sri Lanka involving 117 stroke survivors aged 40 years and above found a PSCI prevalence of 70.1% when assessed using the Montreal Cognitive Assessment (MoCA) in the 3-12 months post-stroke period [1]. This study further categorized the severity of cognitive impairment, with 39% of patients demonstrating mild, 30% moderate, and 1.1% severe cognitive impairment [1]. These figures highlight that PSCI is not an uncommon complication but rather affects the majority of stroke survivors, necessitating systematic assessment and intervention.
The high prevalence of PSCI establishes it as a central concern in stroke rehabilitation. With stroke being the fourth leading cause of disability-adjusted life years globally [2], the additional burden of cognitive impairment significantly compounds the disability experienced by survivors. The epidemiological data underscores the need for routine cognitive screening in post-stroke care protocols and allocation of healthcare resources toward cognitive rehabilitation services.
Stroke Subtypes and Cognitive Outcomes
The trajectory of cognitive recovery varies across different stroke subtypes, which has implications for prognosis and rehabilitation planning. A comprehensive retrospective analysis of 646 patients with different stroke subtypes revealed that patients with subarachnoid hemorrhage (SAH) generally experience poorer long-term outcomes compared to those with ischemic stroke (IS) or intracerebral hemorrhage (ICH) [2].
The most substantial difference was observed in productivity frequency scores (a subdomain of participation measurement), with the SAH group exhibiting significantly lower scores (0.04 [0-0.09]) compared to IS (0.39 [0.33-0.45]) and ICH (0.44 [0.37-0.51]) groups (P < 0.001) [2]. This suggests that the stroke subtype not only influences acute recovery but also long-term functional participation, particularly in productive activities such as work and household responsibilities. Understanding these subtype-specific profiles enables clinicians to set realistic expectations and tailor rehabilitation approaches to address the unique challenges associated with different stroke mechanisms.
Table 1: Prevalence and Severity Distribution of Post-Stroke Cognitive Impairment
| Characteristic | Overall PSCI Prevalence | Mild Impairment | Moderate Impairment | Severe Impairment |
|---|---|---|---|---|
| Percentage | 70.1% | 39% | 30% | 1.1% |
| Assessment Tool | Montreal Cognitive Assessment (MoCA) | MoCA | MoCA | MoCA |
Table 2: Long-Term Participation Outcomes by Stroke Subtype
| Stroke Subtype | Productivity Frequency Score | Social Participation | Community Participation |
|---|---|---|---|
| Ischemic Stroke | 0.39 [0.33-0.45] | Similar recovery pattern | Similar recovery pattern |
| Intracerebral Hemorrhage | 0.44 [0.37-0.51] | Similar recovery pattern | Similar recovery pattern |
| Subarachnoid Hemorrhage | 0.04 [0-0.09] | Poorer outcomes | Poorer outcomes |
Domain-Specific Cognitive Deficits in PSCI
Profile of Affected Cognitive Domains
Post-stroke cognitive impairment manifests across multiple cognitive domains, with particular patterns emerging in recent research. Domain-specific analysis reveals that attention and executive functions are significantly associated with functional outcomes [1]. The attention component has been identified as a key indicator for basic activities of daily living (ADL) independence (β = 0.303, p = 0.005), while executive functions are strongly associated with balance abilities (β = 0.439, p = 0.001) [1].
The differential impact of specific cognitive domains on various functional outcomes highlights the need for targeted assessment and intervention. Executive dysfunction, which encompasses problems with planning, organization, cognitive flexibility, and self-monitoring, appears particularly disruptive to complex motor tasks like balance maintenance. Similarly, attentional deficits impair the capacity to perform basic self-care activities, suggesting that different cognitive domains contribute uniquely to the spectrum of post-stroke disability.
Assessment Methodologies for Cognitive Domains
Comprehensive cognitive assessment following stroke requires a multifaceted approach. The Montreal Cognitive Assessment (MoCA) is widely used to evaluate global cognitive function, with specific subdomains assessing visuospatial and executive skills, naming, attention, language, abstraction, delayed memory, and orientation [2]. The MoCA provides a broad screening of cognitive status, but often requires supplementation with domain-specific measures for detailed rehabilitation planning.
For research purposes, more extensive test batteries are employed to capture the complexity of cognitive deficits. Studies investigating cognitive rehabilitation efficacy commonly utilize standardized instruments such as the Western Aphasia Battery (WAB), which assesses spontaneous speech, auditory comprehension, repetition, and naming abilities [3]. These detailed assessments enable researchers to identify specific cognitive deficits and measure changes in response to targeted interventions, providing valuable data for evidence-based practice in cognitive rehabilitation.
Impact of Cognitive Impairment on Functional Outcomes
Activities of Daily Living and Functional Independence
Cognitive function following stroke is significantly associated with balance, mobility, and functional independence in activities of daily living (ADLs) [1]. Research demonstrates that improved global cognitive function correlates significantly with all functional outcomes, with basic ADL independence showing the highest effect size (η²p = 0.257), followed by instrumental ADL independence (η²p = 0.193), improved mobility (η²p = 0.077), and balance performance (η²p = 0.056) [1].
These findings underscore the profound impact of cognitive impairment on the fundamental activities necessary for independent living. Basic ADLs include self-care tasks such as feeding, dressing, and personal hygiene, while instrumental ADLs encompass more complex activities like managing finances, medication administration, and household management. The strong association between cognitive function and ADL performance suggests that cognitive deficits may be a primary driver of dependency following stroke, highlighting the importance of integrating cognitive rehabilitation with physical rehabilitation to optimize functional recovery.
Participation and Quality of Life
Beyond basic functional tasks, cognitive impairment significantly affects participation in social, community, and vocational activities, ultimately impacting overall quality of life. The Participation Measure-3 Domains, 4 Dimensions (PM-3D4D) captures these aspects, evaluating social participation, community participation, and productivity across both frequency and perceived difficulty dimensions [2]. Research indicates that better activity function at discharge is an independent predictor of higher PM-3D4D scores 12 months post-dischcharge [2].
The restricted participation observed in PSCI patients has profound implications for quality of life and mental health. Difficulties with resuming work, engaging in leisure activities, and maintaining social relationships contribute to post-stroke depression and reduced life satisfaction. This highlights the importance of measuring participation outcomes alongside traditional impairment-based measures to fully capture the impact of cognitive deficits on patients' lives and inform comprehensive rehabilitation approaches.
Table 3: Association Between Cognitive Functions and Functional Outcomes
| Functional Outcome | Effect Size (η²p) | Most Relevant Cognitive Domain | Domain Association (β) |
|---|---|---|---|
| Basic ADL Independence | 0.257 | Attention | β = 0.303, p = 0.005 |
| Instrumental ADL Independence | 0.193 | Executive Functions | Not specified |
| Mobility | 0.077 | Global Cognition | Not specified |
| Balance Performance | 0.056 | Executive Functions | β = 0.439, p = 0.001 |
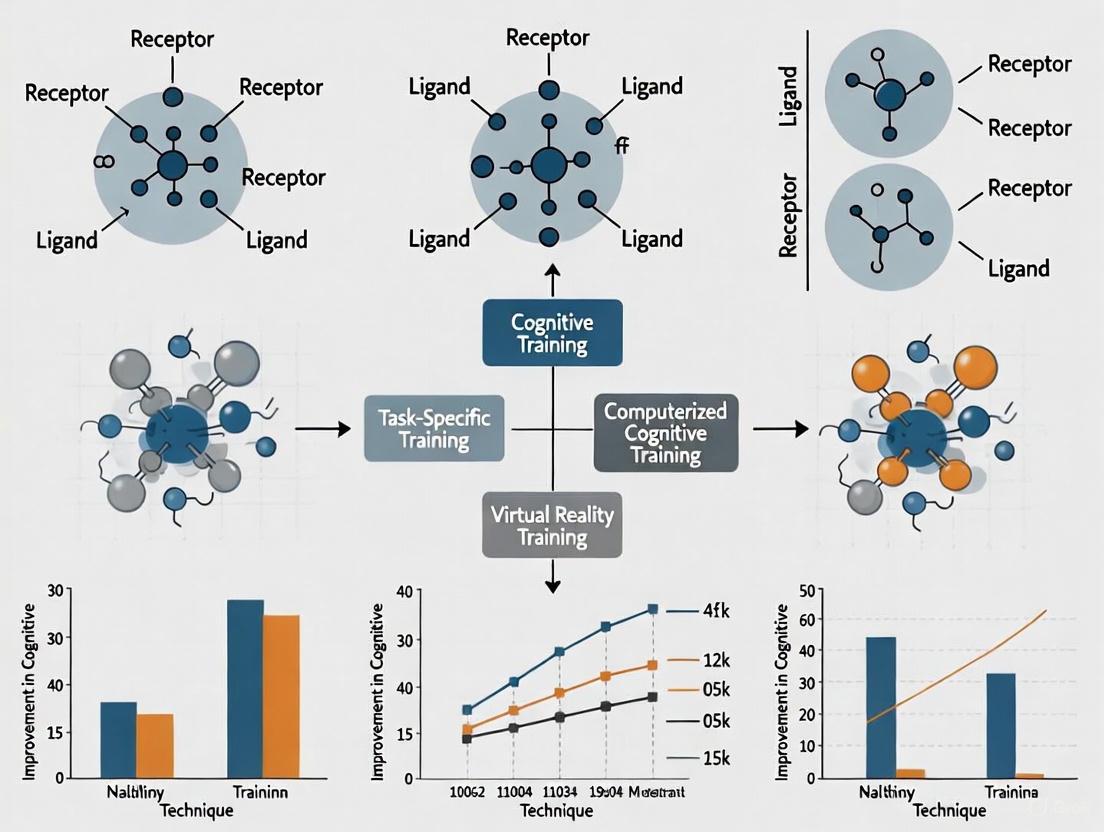
Comparative Efficacy of Cognitive Rehabilitation Approaches
Integrated Rehabilitation Methodologies
Several cognitive rehabilitation approaches have demonstrated efficacy in addressing PSCI, with combination therapies often showing superior results. Network meta-analyses reveal that working memory (WM) training combined with speech and language therapy (SLT) leads to significantly enhanced outcomes on the Western Aphasia Battery (WAB) Aphasia Quotient compared to SLT alone [3]. This combination was more effective than both computer-assisted cognitive training (CCT) with SLT and telerehabilitation computer-assisted cognitive training (tCCT) with SLT in improving WAB scores [3].
Additionally, virtual reality-based cognitive training (vrCT) combined with SLT significantly improved auditory comprehension compared with SLT alone [3]. Attention training (AT) combined with SLT also proved more effective than vrCT with SLT in enhancing spontaneous speech [3]. These findings suggest that while SLT remains a cornerstone of post-stroke cognitive rehabilitation, its efficacy is significantly enhanced when combined with specific cognitive training approaches, particularly working memory training and virtual reality-based interventions.
Advanced Interventions and Emerging Protocols
Innovative approaches combining cognitive rehabilitation with neuromodulation techniques represent the cutting edge of PSCI treatment. Research on cognitive remediation (CR) combined with repetitive transcranial magnetic stimulation (rTMS) has shown promising results in improving cognitive functioning in stroke patients [4]. Similarly, speech therapy combined with multi-modality aphasia therapy and rTMS has demonstrated efficacy for chronic post-stroke non-fluent aphasia [4].
The mechanisms underlying these combined approaches involve neuroplasticity enhancement through synchronized neural activation. rTMS is thought to facilitate cortical excitability and strengthen functional connections in brain networks disrupted by stroke, potentially creating a more receptive state for cognitive training [4]. This synergistic effect between neuromodulation and cognitive training highlights the potential of mechanism-based interventions targeting the neurophysiological processes underlying recovery.
Cognitive Rehabilitation Pathway for PSCI
Experimental Protocols and Research Methodologies
Standardized Assessment Protocols
Research on PSCI employs rigorous assessment protocols to evaluate cognitive function and its impact on recovery. Standardized methodology includes the Montreal Cognitive Assessment (MoCA) for global cognitive screening, which assesses multiple domains including visuospatial and executive skills, naming, attention, language, abstraction, delayed memory, and orientation [2]. For more detailed evaluation of specific cognitive domains, instruments such as the Western Aphasia Battery (WAB) are employed to measure spontaneous speech, auditory comprehension, repetition, and naming abilities [3].
Functional outcomes are typically assessed using performance-based measures and participant-reported instruments. The Activity Measure for Post-Acute Care (AM-PAC) evaluates basic mobility, daily activities, and applied cognition [2], while the Participation Measure-3 Domains, 4 Dimensions (PM-3D4D) captures social participation, community participation, and productivity across both frequency and perceived difficulty dimensions [2]. These standardized assessment protocols enable consistent measurement across studies and facilitate comparison of rehabilitation outcomes.
Intervention Protocols and Trial Methodologies
Randomized controlled trials (RCTs) investigating cognitive rehabilitation interventions follow rigorous methodological standards. The ESTREL trial methodology provides an exemplary model for pharmacological interventions in stroke recovery, utilizing a double-blind, placebo-controlled design with standardized rehabilitation therapy based on active task-oriented training [5]. This trial randomized 610 patients with acute ischemic or hemorrhagic stroke to receive either levodopa/carbidopa or placebo three times daily for 39 days alongside rehabilitation, with the primary outcome being the Fugl-Meyer Assessment score at 3 months [5].
For non-pharmacological interventions, network meta-analyses systematically compare multiple rehabilitation approaches. These studies follow PRISMA guidelines and Cochrane Handbook methodologies, searching multiple databases including PubMed, Embase, Cochrane Library, and regional databases [3] [4]. Quality assessment tools like the Methodological Evaluation of Observational REsearch (MORE) checklist evaluate observational studies on disease incidence or risk factors, analyzing external and internal validity through multiple items scored based on methodological flaws [6]. These rigorous methodologies ensure the validity and reliability of findings in cognitive rehabilitation research.
Table 4: Key Assessment Tools in PSCI Research
| Assessment Tool | Domains Measured | Application in PSCI |
|---|---|---|
| Montreal Cognitive Assessment (MoCA) | Visuospatial and executive skills, naming, attention, language, abstraction, delayed memory, orientation | Global cognitive screening |
| Western Aphasia Battery (WAB) | Spontaneous speech, auditory comprehension, repetition, naming | Language-specific assessment |
| Activity Measure for Post-Acute Care (AM-PAC) | Basic mobility, daily activities, applied cognition | Functional ability measurement |
| Participation Measure-3 Domains, 4 Dimensions (PM-3D4D) | Social participation, community participation, productivity | Participation restriction assessment |
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Materials and Assessment Tools
| Research Tool | Function/Application | Specific Utility in PSCI Research |
|---|---|---|
| Montreal Cognitive Assessment (MoCA) | Brief cognitive screening tool | Assesses global cognitive function and specific cognitive domains |
| Western Aphasia Battery (WAB) | Comprehensive language assessment | Evaluates aphasia quotient and specific language domains |
| Fugl-Meyer Assessment (FMA) | Stroke-specific motor function measure | Primary outcome in motor recovery trials [5] |
| Activity Measure for Post-Acute Care (AM-PAC) | Functional activity measurement | Captures basic mobility, daily activities, and applied cognition |
| Participation Measure-3 Domains, 4 Dimensions (PM-3D4D) | Participation restriction assessment | Measures social, community, and productivity participation |
| Repetitive Transcranial Magnetic Stimulation (rTMS) | Non-invasive brain stimulation | Modulates cortical excitability to enhance neuroplasticity [4] |
| Virtual Reality (VR) Cognitive Training Systems | Immersive cognitive rehabilitation | Provides ecologically valid training environments [3] |
| Levodopa/Carbidopa | Dopaminergic medication | Investigated for enhancing neuroplasticity in stroke recovery [5] |
Standard Research Workflow in PSCI Trials
The epidemiology and clinical burden of post-stroke cognitive impairment present significant challenges in stroke rehabilitation, with approximately 70% of stroke survivors experiencing cognitive deficits that substantially impact their functional independence and quality of life. Domain-specific deficits in attention, executive functions, memory, and language demonstrate distinct associations with various functional outcomes, necessitating comprehensive assessment and targeted intervention strategies. Evidence supports the efficacy of integrated rehabilitation approaches, particularly working memory training combined with speech and language therapy, and virtual reality-based cognitive training, with emerging promise in neuromodulation techniques such as rTMS. Future research should focus on personalized cognitive rehabilitation protocols based on individual deficit profiles and stroke characteristics, while ongoing investigation into pharmacological adjuncts continues to seek effective interventions to enhance neuroplasticity and optimize recovery in PSCI.
Stroke remains a leading cause of long-term disability worldwide, with approximately 60% of survivors experiencing persistent cognitive impairments and only 12% achieving complete functional recovery after conventional physical therapy [7] [8]. The landscape of stroke rehabilitation is undergoing a paradigm shift, moving from traditional compensatory approaches toward therapies that actively promote brain repair by harnessing the brain's inherent neuroplastic capacity [7]. Neuroplasticity—the brain's ability to reorganize its structure, function, and connections in response to experience and injury—serves as the fundamental mechanism underlying functional recovery after stroke [9] [10]. This review adopts a comparative framework to evaluate emerging neuroplasticity-based interventions, with particular emphasis on Hebbian principles and endogenous repair processes, to provide researchers and drug development professionals with a critical analysis of their mechanisms, efficacy, and potential integration.
At the core of this discussion lies Hebb's seminal principle, often summarized as "cells that fire together, wire together," which proposes that synaptic connections are strengthened when pre- and postsynaptic neurons are repeatedly co-activated [11]. This concept provides the theoretical foundation for understanding how targeted interventions can remodel neural circuits after stroke [9] [12]. Meanwhile, the brain's endogenous repair mechanisms, including neurogenesis and structural reorganization, offer complementary pathways for recovery [7] [10]. The interplay between these targeted plasticity approaches and the brain's innate reparative capacity forms a rich therapeutic landscape for investigation, with timing, individual patient characteristics, and intervention specificity emerging as critical determinants of successful outcomes [9] [7].
Comparative Analysis of Neuroplasticity-Based Interventions
Hebbian Plasticity Approaches
Brain-Computer Interface with Functional Electrical Stimulation (BCI-FES) represents a technologically advanced application of Hebbian principles. This approach synchronizes motor cortical activity associated with movement attempts with precisely timed peripheral sensory feedback through FES, creating ideal conditions for Hebbian plasticity to strengthen corticomuscular connections [13]. In a 2024 clinical study comparing BCI-FES with randomly timed FES in subcortical stroke patients, the BCI-FES group demonstrated significantly greater improvements in Fugl-Meyer Assessment for Upper Extremity (FMA-UE) scores, increased motor evoked potential amplitudes, enhanced beta oscillatory power over contralateral motor cortex, and strengthened corticomuscular coherence [13]. These findings provide compelling evidence that temporally coincident pairing of cortical activation with peripheral feedback can effectively drive motor recovery by re-establishing functional connectivity between the brain and paralyzed limbs.
Paired Associative Stimulation (PAS), another Hebbian-based intervention, involves repeated pairing of peripheral nerve stimulation with transcranial magnetic stimulation (TMS) of the corresponding motor cortex [9] [12]. The protocol capitalizes on spike-timing-dependent plasticity, where the precise temporal relationship between pre- and postsynaptic activation determines whether long-term potentiation (LTP)-like or long-term depression (LTD)-like plasticity is induced [9]. Research indicates that LTP-like plasticity is optimally induced when peripheral stimulation precedes TMS by approximately 25 milliseconds, while reversing this timing can induce LTD-like effects [9] [11]. A current clinical trial protocol (ChiCTR2000039949) aims to extend this principle by targeting the supplementary motor area (SMA) with TMS followed by peripheral magnetic stimulation of upper limb nerves to reconstruct the SMA→internal capsule→periphery neural circuit for arm motor recovery [12]. This innovative approach recognizes that stroke impairs entire brain networks rather than isolated regions, and aims to rebuild disrupted motor circuits instead of simply upregulating excitation in focal areas [12].
Transcranial Direct Current Stimulation (tDCS) has also demonstrated efficacy in modulating cortical excitability to enhance cognitive recovery. A recent systematic review of 22 randomized controlled trials involving 5,100 participants found that tDCS produced significant cognitive benefits as measured by Montreal Cognitive Assessment (MoCA) scores, with a mean difference of 4.56 points compared to control groups [14]. The mechanism involves creating a favorable neurophysiological environment for plasticity by applying weak direct currents to modulate neuronal membrane potentials, thereby lowering the threshold for LTP induction when combined with cognitive training [14].
Table 1: Comparative Outcomes of Hebbian-Based Interventions for Stroke Recovery
| Intervention | Mechanism of Action | Primary Outcome Measures | Efficacy Evidence | Optimal Timing |
|---|---|---|---|---|
| BCI-FES | Synchronizes EEG-detected movement attempts with FES-generated proprioceptive feedback | FMA-UE, Corticomuscular coherence, MEP amplitude | Significantly greater FMA-UE improvement vs. random FES (p=0.030) [13] | Acute/Subacute phase [13] |
| PAS | Pairs peripheral nerve stimulation with TMS of motor cortex | WMFT, FMA-UE, FIM, fNIRS parameters | Clinical trials ongoing; preclinical data shows enhanced corticospinal excitability [9] [12] | Chronic phase [12] |
| tDCS | Modulates cortical excitability via weak direct currents | MoCA, Cognitive domain scores | MD 4.56 on MoCA (95% CI: 3.19-5.93) [14] | Early intervention (<3 months) [14] |
Endogenous Repair Approaches
The brain possesses remarkable intrinsic capacity for self-repair through processes collectively termed endogenous repair mechanisms. Stroke-induced neurogenesis represents a key component of this innate recovery system, involving the proliferation of neural stem cells primarily from the subventricular zone (SVZ) and their migration to infarct and peri-infarct regions, where they differentiate into functional neurons [10]. This complex process is regulated by numerous molecular factors including Fibroblast Growth Factor-2 (FGF-2), Insulin-like Growth Factor-1 (IGF-1), Brain-Derived Neurotrophic Factor (BDNF), and Vascular Endothelial Growth Factor (VEGF), which promote neural stem cell proliferation [10]. Additionally, Stromal-derived factor (SDF-1), Monocyte Chemoattractant Protein (MCP-1), and Matrix Metalloproteinases (MMPs) facilitate neuroblast migration to damaged areas [10].
The neuroinflammatory response plays a dual role in modulating endogenous repair processes. While chronic neuroinflammation is generally detrimental to recovery, acute inflammatory responses can promote neurogenesis through specific cytokine signaling [10]. For instance, short-term interleukin-6 (IL-6) exposure induces neurogenesis in vitro, whereas chronic IL-6 expression reduces neurogenesis in the dentate gyrus [10]. Similarly, interleukin-1α (IL-1α) demonstrates neurogenic properties, while IL-1β primarily contributes to neural clearance [10]. Microglia and astrocytes further modulate this process through the release of trophic factors that support neural stem cell migration and differentiation, though their activated states can also impede neuronal survival [10].
Pharmacological approaches targeting endogenous repair mechanisms are emerging as promising therapeutic strategies. A recent systematic review found that pharmacological interventions produced robust cognitive improvements post-stroke, with a mean difference of 4.00 points on MoCA scores (95% CI: 3.48-4.52) [14]. Of particular interest are psychoplastogens—compounds that promote neuronal structural plasticity. Tabernanthalog (TBG), a nonhallucinogenic psychoplastogen, has been shown to promote cortical neuroplasticity through 5-HT2A, TrkB, mTOR, and AMPA receptor activation, similar to classic psychedelics, but without inducing immediate early gene activation or hallucinogenic effects [15]. This mechanism represents a novel approach to enhancing the brain's inherent plastic capacity through pharmacological modulation.
Table 2: Endogenous Repair Mechanisms and Their Modulators
| Endogenous Process | Key Molecular Mediators | Therapeutic Modulation | Functional Impact |
|---|---|---|---|
| Neural Stem Cell Proliferation | FGF-2, IGF-1, BDNF, VEGF [10] | Pharmacological enhancement of trophic factors | Increased neural stem cell population in neurogenic niches |
| Neuroblast Migration | SDF-1, MCP-1, MMPs 2/3/9 [10] | Modulation of chemokine signaling | Directed migration to ischemic regions |
| Neuronal Differentiation & Maturation | Perlecan domain V, PTX-3 [10] | Extracellular matrix remodeling | Enhanced maturation and functional integration of new neurons |
| Structural Plasticity | 5-HT2A, TrkB, mTOR, AMPA receptors [15] | Nonhallucinogenic psychoplastogens (e.g., TBG) | Increased cortical spinogenesis and neurite extension |
Experimental Protocols and Methodologies
BCI-FES Protocol for Upper Limb Rehabilitation
The BCI-FES intervention described in the 2024 study employs a sophisticated protocol for retraining corticomuscular connections [13]. The methodology begins with high-density electroencephalography (EEG) recording during cued movement attempts and rest periods to identify optimal features for classification. Electrode locations and spectral power frequencies that demonstrate the greatest differences between movement and rest states are selected as features for training a classifier to detect movement attempts in real-time [13]. The sensorimotor rhythm, particularly event-related desynchronization in alpha (8-12 Hz) and beta (13-30 Hz) frequency bands, provides the primary input signal for the BCI [13].
During treatment sessions, patients perform attempted movements of the affected limb, while the BCI system continuously monitors EEG signals. When the classifier detects features associated with movement attempts, it immediately triggers functional electrical stimulation (FES) to the corresponding paralyzed muscles, generating coordinated movement and associated proprioceptive feedback [13]. This creates precisely timed coincidence between top-down motor commands and bottom-up sensory inputs, ideal for inducing Hebbian plasticity [13]. The treatment typically involves multiple sessions per week over several weeks, with regular re-calibration of the classifier to adapt to changing neural patterns as recovery progresses [13]. Notably, feature selection evolves during the treatment course, typically shifting from bilateral to increasingly ipsilesional dominance, reflecting functional reorganization of motor networks [13].
Paired Associative Stimulation Protocol
The cortico-peripheral Hebbian-type stimulation protocol targets reconstruction of damaged motor circuits through carefully timed paired stimulation [12]. The procedure involves transcranial magnetic stimulation (TMS) of the supplementary motor area (SMA) followed by peripheral magnetic stimulation (PMS) of the peripheral nerves innervating the affected upper limb [12]. The temporal interval between cortical and peripheral stimulation is critical, typically set to tens of milliseconds, to capitalize on spike-timing-dependent plasticity rules [12].
This randomized controlled trial protocol administers one session of real or sham Hebbian-type stimulation daily, five days per week, for a total of 25 sessions, always followed by conventional rehabilitation therapy [12]. Outcome measures assessed at baseline, post-treatment, and 3-month follow-up include the Wolf Motor Function Test (WMFT) as the primary outcome, with Fugl-Meyer Assessment for Upper Extremity (FMA-UE), Functional Independence Measure (FIM), and functional near-infrared spectroscopy (fNIRS) parameters as secondary outcomes [12]. The fNIRS component enables investigation of neural correlates of recovery, particularly changes in cortical activation patterns during motor tasks [12].
Diagram Title: BCI-FES Hebbian Plasticity Protocol
Assessing Endogenous Neurogenesis
Experimental investigation of stroke-induced neurogenesis employs specialized methodologies to track and quantify the birth, migration, and integration of new neurons [10]. The gold standard approach involves brdU labeling, where bromodeoxyuridine (BrdU), a thymidine analog, is incorporated into the DNA of dividing cells during the S-phase, allowing histological identification of newly generated cells [10]. Following BrdU administration, immunohistochemical techniques using antibodies against BrdU combined with neuronal markers such as NeuN, doublecortin, or βIII-tubulin enable specific identification of newly generated neurons [10].
Additional methodologies include retroviral labeling of neural stem cells to track their fate and transgenic reporter models that express fluorescent proteins under the control of neural stem cell-specific promoters [10]. To assess functional integration, optogenetic and chemogenetic approaches allow selective activation or inhibition of newborn neurons, while serial in vivo imaging through cranial windows enables direct visualization of neuronal migration and structural maturation over time [10]. Behavioral tests sensitive to hippocampal-dependent learning (e.g., Morris water maze, contextual fear conditioning) and motor function (e.g., ladder rung walking, pellet retrieval) provide functional correlates of successful neurogenesis and integration [10].
Molecular Mechanisms of Hebbian and Homeostatic Plasticity
At the molecular level, Hebbian plasticity involves sophisticated signaling cascades that translate coordinated neuronal activity into lasting synaptic changes. The NMDA receptor serves as a critical coincidence detector, requiring simultaneous presynaptic glutamate release and postsynaptic depolarization to relieve magnesium blockade and permit calcium influx [11]. This calcium influx triggers activation of calcium/calmodulin-dependent kinase II (CaMKII), which phosphorylates AMPA receptors to increase their conductivity and promotes their insertion into the postsynaptic density, thereby strengthening synaptic transmission [11].
For longer-lasting plasticity, calcium signaling activates cAMP-dependent kinase (PKA) and downstream transcription factors such as CREB, which induce expression of plasticity-related genes including BDNF, Arc, and Homer1a [11]. The synaptic tagging and capture hypothesis provides a framework for understanding how transient synaptic activity can be stabilized into persistent changes, wherein stimulated synapses generate a "tag" that captures plasticity-related proteins synthesized in response to strong stimulation [11].
Structural correlates of Hebbian plasticity include dendritic spine enlargement and the formation of new synaptic connections, processes mediated by reorganization of the actin cytoskeleton and membrane insertion of adhesion molecules [11]. Conversely, long-term depression (LTD) involves different signaling pathways, including activation of protein phosphatases and internalization of AMPA receptors, resulting in synaptic weakening [11].
Diagram Title: Molecular Mechanisms of Hebbian Plasticity
Homeostatic plasticity mechanisms provide crucial negative feedback to prevent runaway excitation and maintain neural circuit stability [9]. These include synaptic scaling, wherein neurons globally adjust synaptic strengths in response to chronic changes in activity levels, and metaplasticity, which refers to activity-dependent changes in the ability to induce subsequent plasticity [9]. The Bienenstock-Cooper-Munro (BCM) theory provides a conceptual framework for understanding how the threshold for LTP/LTD induction shifts according to prior synaptic activity [9]. From a therapeutic perspective, homeostatic mechanisms necessitate careful consideration of intervention timing and sequence, as facilitatory priming can sometimes diminish the effects of subsequent therapies [9].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Tools for Investigating Post-Stroke Neuroplasticity
| Tool/Reagent | Application | Function in Research | Example Use Cases |
|---|---|---|---|
| High-density EEG Systems | Recording cortical oscillatory activity | Detects movement attempt-related ERD/ERS patterns for BCI control [13] | Real-time classification of movement intention for triggered FES |
| Transcranial Magnetic Stimulation (TMS) | Non-invasive brain stimulation | Assesses corticospinal excitability via MEPs; induces plasticity in therapeutic protocols [9] [12] | Paired associative stimulation; mapping cortical reorganization |
| Functional NIRS (fNIRS) | Monitoring cortical activation | Measures hemodynamic responses during motor tasks; assesses intervention effects [12] | Evaluating SMA activation changes after Hebbian-type stimulation |
| BrdU and Neural Markers | Tracking neurogenesis | Labels newly generated cells; identifies neuronal differentiation [10] | Quantifying stroke-induced neurogenesis in neurogenic niches |
| Psychoplastogens (e.g., TBG) | Promoting structural plasticity | Induces neurite growth and spinogenesis without hallucinogenic effects [15] | Enhancing structural basis for functional recovery |
| Cytokine Modulators | Regulating neuroinflammation | Manipulates neuroinflammatory environment to favor neurogenesis [10] | Shifting microglial phenotype from detrimental to supportive |
Comparative Efficacy and Clinical Translation
When comparing neuroplasticity-based interventions, several key patterns emerge regarding their efficacy and optimal application. Timing represents a critical factor, with most interventions showing enhanced effectiveness when initiated early after stroke [7] [14]. The traditional view that recovery plateaus by 6 months is being challenged by evidence showing that the restorative window may be much longer than previously thought, with the optimal time for brain repair potentially occurring at later stages rather than earlier [7]. Nevertheless, early intervention (within 3 months post-stroke) generally produces the most robust outcomes, possibly due to heightened plasticity during this period [14].
The intervention specificity also significantly influences outcomes. BCI-FES demonstrates particular efficacy for motor recovery by directly targeting the disrupted corticomuscular pathways [13]. In contrast, tDCS shows broader effects on cognitive function, likely through creating a generally permissive environment for plasticity across multiple cognitive domains [14]. Pharmacological approaches such as psychoplastogens operate at a more fundamental level by enhancing the structural basis for plasticity throughout affected networks [15].
For successful clinical translation, combination approaches that simultaneously target multiple recovery mechanisms hold particular promise [9] [7]. However, combining interventions requires careful consideration of homeostatic metaplasticity, as improper timing can diminish rather than enhance efficacy [9]. The future of stroke rehabilitation likely lies in personalized protocols that account for individual lesion characteristics, residual network connectivity, and specific functional deficits, ultimately leveraging both targeted Hebbian plasticity and enhanced endogenous repair processes to maximize recovery [9] [7] [10].
The comparative analysis of neuroplasticity-based interventions reveals a dynamic and rapidly evolving therapeutic landscape for stroke recovery. Hebbian principles provide a powerful framework for designing targeted therapies that selectively strengthen behaviorally relevant neural connections, while endogenous repair processes offer complementary pathways for structural restoration of damaged neural networks [9] [10]. The most promising future directions involve strategic integration of these approaches, leveraging their synergistic potential while carefully managing timing considerations to avoid homeostatic interference [9].
For researchers and drug development professionals, this analysis highlights several priority areas. First, advancing personalization through improved biomarker identification could enable better matching of interventions to individual patient characteristics and lesion profiles [13] [14]. Second, refining temporal parameters for combination therapies may maximize efficacy while minimizing homeostatic limitations [9]. Third, developing novel pharmacologic approaches that enhance both targeted plasticity and endogenous repair processes represents a promising frontier, with nonhallucinogenic psychoplastogens such as TBG offering particularly intriguing possibilities [15]. As our understanding of the complex interplay between different plasticity mechanisms deepens, so too will our ability to design increasingly effective, multidimensional interventions that harness the brain's remarkable capacity for change and restoration after stroke.
The comparative analysis of cognitive rehabilitation techniques in stroke research increasingly focuses on understanding molecular mechanisms that drive neuroplasticity and functional recovery. Among these, Brain-Derived Neurotrophic Factor (BDNF) and cholinergic pathways emerge as critical systems with distinct yet complementary roles. BDNF, the most abundant neurotrophin in the adult brain, facilitates synaptic plasticity, neuronal survival, and cognitive processes, while cholinergic systems, originating from basal forebrain nuclei, regulate attention, learning, and memory formation. Evidence indicates that both systems undergo significant alterations following stroke, making them promising therapeutic targets for cognitive rehabilitation. This review systematically compares these key neurotransmitter systems and growth factors, evaluating their mechanistic contributions, response to interventions, and potential as biomarkers for post-stroke cognitive recovery.
BDNF: Mechanisms and Experimental Evidence in Cognitive Recovery
Molecular Signaling and Pathophysiological Role
BDNF functions as a primary mediator of activity-dependent plasticity in the central nervous system. It is initially synthesized as a precursor protein (proBDNF) before proteolytic cleavage yields mature BDNF (mBDNF). These forms elicit opposing biological effects: mBDNF preferentially binds tropomyosin-related kinase B (TrkB) receptors, promoting neuronal survival, synaptic strengthening, and long-term potentiation (LTP), whereas proBDNF binding to p75 neurotrophin receptor (p75NTR) facilitates apoptosis and long-term depression [16] [17]. The BDNF gene contains a functional polymorphism (Val66Met) that affects activity-dependent secretion and is associated with structural and functional differences in brain regions critical for memory, including the hippocampus and prefrontal cortex [16].
In the context of stroke, BDNF signaling confers neuroprotection through multiple downstream pathways. Upon binding TrkB, BDNF activates phosphatidylinositol 3-kinase (PI3K)/Akt and mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK/ERK) cascades, which inhibit apoptotic machinery and support cell survival [18]. Additionally, BDNF enhances synaptic transmission by regulating NMDA receptor trafficking and phosphorylation, and promotes dendritic spine complexity, thereby facilitating synaptic consolidation and memory formation [16] [19]. Notably, serum and cerebrospinal fluid BDNF levels are significantly reduced in stroke patients compared to healthy controls, with this reduction correlating with poorer functional and cognitive outcomes [20].
Supporting Experimental Data and Protocols
Table 1: Key Experimental Findings on BDNF in Stroke Recovery
| Study Model | Intervention | Key Findings | Reference |
|---|---|---|---|
| Human Subjects (Meta-analysis) | Analysis of 62 studies (1,856 patients) | Significantly lower BDNF levels in stroke patients vs. healthy controls (SMD: -1.04); Depression further decreased BDNF (SMD: -0.60) | [20] |
| Mouse MCAO Model | Shuxuening injection (SXNI) | Reversed stroke-induced BDNF/TrkB expression decreases in hippocampal CA3; Activated neurotrophin/TrkB signaling (15 DEGs) | [21] |
| Rat Forebrain Ischemia | Exogenous BDNF administration | Improved long-term potentiation and cognitive functions in water maze tests | [22] |
| Human RCT (STROKEWALK) | SMS-guided physical exercise | Plasma BDNF levels analyzed as primary outcome; Correlation with improved walking performance | [23] |
Representative Experimental Protocol: Measuring Circulating BDNF Levels
- Specimen Collection: Non-fasting blood samples collected in heparinized vials at hospital admission and during follow-up (e.g., 3 months post-stroke). Plasma separated via centrifugation and stored at -80°C until analysis [23].
- BDNF Quantification: Total BDNF levels measured using DuoSet ELISA kit (DY248, R&D Systems). Plasma samples diluted 10x in reagent diluent (1% BSA in PBS). Detection system utilizes alkaline phosphatase (1:10,000; Roche Diagnostics) incubated for 2 hours at room temperature [23].
- Data Acquisition: Absorbance read kinetically at 405nm every 5 minutes for 1 hour using a spectrophotometer (e.g., Infinite M1000, Tecan). Samples measured in triplicate, with mean values calculated for analysis [23].
Cholinergic Pathways: Mechanisms and Experimental Evidence in Cognitive Recovery
Neuroanatomy and Pathophysiological Role
The basal forebrain cholinergic system constitutes a key network for cognitive function, comprising several nuclei: the medial septal nucleus (Ch1), the vertical and horizontal limbs of the diagonal band of Broca (Ch2, Ch3), and the nucleus basalis of Meynert (Ch4) [24]. These nuclei provide widespread cholinergic innervation to the hippocampus, cortex, and amygdala, regulating arousal, attention, learning, and memory. The cholinergic signaling molecule, acetylcholine (ACh), is synthesized by choline acetyltransferase (ChAT) and degraded by acetylcholinesterase (AChE) and butyrylcholinesterase (BChE) [23] [25].
Following neurological insults like stroke or traumatic brain injury, the cholinergic system demonstrates a biphasic response: an initial surge in ACh release is followed by persistent cholinergic hypofunction. Acute excess ACh contributes to excitotoxicity, while chronic deficiency underlies cognitive impairments [25]. Postmortem studies in dementia patients reveal substantial neuronal loss (up to 90-95%) in the basal forebrain accompanied by markedly reduced cortical acetylcholine activity [24]. Cholinergic degeneration is associated with deficits in multiple cognitive domains, with specific subregions having distinct roles—Ch1/2 atrophy correlates with episodic memory deficits, while Ch4 degeneration predicts attention and visuospatial decline [24].
Supporting Experimental Data and Protocols
Table 2: Key Experimental Findings on Cholinergic Pathways in Brain Disorders
| Study Model | Intervention/Assessment | Key Findings | Reference |
|---|---|---|---|
| Human AD Continuum (n=100) | Free-water imaging (DTI-MRI) | FWf in Ch1-3 & Ch4 increased in aMCI/AD; Correlated with visuospatial/executive deficits (R=-0.47) | [24] |
| Human Stroke RCT (STROKEWALK) | SMS-guided physical exercise | Plasma ChAT activity and BChE activity measured as secondary outcomes; Cholinergic index calculated | [23] |
| TBI Animal Models | Scopolamine administration | Acute administration: neuroprotective; Chronic administration: enhanced ACh release in hippocampus | [25] |
| Vascular Dementia | Cholinergic agents | Cholinergic system vulnerability to vascular damage; Deficiency contributes to memory loss | [19] |
Representative Experimental Protocol: Analyzing Cholinergic Markers
- ChAT Activity Assay: Plasma samples diluted 300x in dilution buffer (10 mM TBS, 0.05% Triton X-100, 1 mM EDTA, pH 7.4). Native and heat-denatured samples plated in 384-well plates. Reaction initiated with cocktail A containing coenzyme-A, phosphotransacetylase, lithium potassium acetyl-phosphate, choline chloride, and eserine hemisulfate. After 1h incubation at 38°C, cocktail B added (choline oxidase, Streptavidin-HRP, 4-aminoantipyrine, phenol). Absorbance read at 500nm for 1h. ChAT activity calculated from choline standard curve [23].
- BChE Activity Assay: Plasma samples diluted 400x in dilution buffer. Samples mixed with master mix containing butyrylthiocholine iodide, DTNB, and specific AChE inhibitor BW280C51. Absorbance read immediately to measure enzymatic activity [23].
- Free-Water Imaging: Advanced DTI-MRI technique estimating extracellular water content to detect microstructural damage in cholinergic pathways. FWf increases reflect neuroinflammation or neurodegeneration in basal forebrain cholinergic structures [24].
Comparative Analysis: BDNF vs. Cholinergic Systems
Mechanistic Comparison
Table 3: Comparative Mechanisms of BDNF and Cholinergic Systems in Cognitive Recovery
| Parameter | BDNF System | Cholinergic System |
|---|---|---|
| Primary Functions | Synaptic plasticity, neuronal survival, LTP, neurogenesis | Attention, learning, memory, arousal, sensory processing |
| Cellular Receptors | TrkB, p75NTR | Muscarinic (M1-M5), Nicotinic receptors |
| Response to Injury | Acute upregulation (neuroprotective), then chronic depletion | Acute excitotoxic surge, then chronic hypofunction |
| Recovery Mechanisms | Promotes synaptic reorganization, dendritic spine growth | Enhances cortical plasticity, attentional modulation |
| Therapeutic Targeting | Exercise, antidepressants, BDNF mimetics, stem cells | Acetylcholinesterase inhibitors, muscarinic/nicotinic agonists |
| Biomarker Potential | Circulating BDNF levels predict recovery and treatment response | Cholinergic basal forebrain integrity via free-water imaging |
Therapeutic Implications and Research Gaps
Both BDNF and cholinergic systems present promising but distinct therapeutic avenues for cognitive rehabilitation. Physical exercise robustly enhances BDNF signaling and represents a potent non-pharmacological intervention, with meta-analyses confirming its immediate positive effect on BDNF levels (SMD: 0.49) [20]. Similarly, cholinergic stimulation via acetylcholinesterase inhibitors (e.g., donepezil, rivastigmine) demonstrates benefits in vascular dementia and post-stroke cognitive impairment [25] [19]. However, several research gaps remain, including optimal timing for interventions (acute vs. chronic phases), differential effects across stroke subtypes, and potential synergistic effects of combining BDNF-enhancing and cholinergic therapies.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Key Research Reagent Solutions for Investigating BDNF and Cholinergic Systems
| Reagent/Method | Application | Experimental Function | Example Specifications |
|---|---|---|---|
| BDNF ELISA Kits | BDNF quantification | Measures total BDNF levels in plasma, serum, CSF | DuoSet ELISA (DY248, R&D Systems) [23] |
| ChAT Activity Assay | Cholinergic function | Measures enzymatic activity of choline acetyltransferase | Custom assay with choline oxidase-based detection [23] |
| BChE Activity Assay | Cholinergic function | Measures butyrylcholinesterase activity | DTNB-based colorimetric assay with AChE inhibition [23] |
| Free-Water Imaging (DTI-MRI) | Cholinergic pathway integrity | Assesses microstructural damage in basal forebrain | 3.0T Siemens scanner with DTI sequences [24] |
| Six-Minute Walk Test (6MWT) | Functional assessment | Evaluates walking performance as functional outcome | 30-meter course, maximum speed [23] |
| MoCA Assessment | Cognitive evaluation | Comprehensive cognitive domain testing | Beijing version for Chinese populations [24] |
Signaling Pathway Visualizations
Diagram 1: BDNF Signaling Pathway. This visualization illustrates the dual pathways of proBDNF and mature BDNF, highlighting their opposing effects on neuronal survival and synaptic plasticity through distinct receptor interactions.
Diagram 2: Cholinergic Signaling Pathway. This diagram outlines acetylcholine synthesis, receptor interactions, and degradation pathways central to cognitive function.
This comparative analysis elucidates the distinct yet interconnected roles of BDNF and cholinergic systems in post-stroke cognitive recovery. While BDNF primarily modulates synaptic plasticity and neuronal survival through tropomyosin-related kinase signaling, cholinergic pathways predominantly regulate attentional processes and cortical plasticity via muscarinic and nicotinic receptors. Both systems demonstrate characteristic perturbations following neurological injury and represent validated targets for therapeutic intervention. Future research should prioritize combinatorial approaches that simultaneously engage both systems, optimize timing for interventions across recovery phases, and validate multimodal biomarkers for patient stratification and treatment monitoring. The continued refinement of experimental methodologies, including advanced imaging techniques and molecular assays, will further delineate the therapeutic potential of these critical neurotransmitter systems and growth factors in cognitive rehabilitation.
In the field of stroke rehabilitation, two principal philosophical approaches guide therapeutic interventions: restorative and compensatory strategies. These approaches represent fundamentally different conceptions of recovery after neurological injury. Restorative strategies aim to retrain, strengthen, and restore impaired cognitive functions through direct, repetitive practice, operating on the principle of experience-dependent neuroplasticity whereby targeted stimulation can promote reorganization of neural circuits [26] [27]. In contrast, compensatory strategies focus on developing alternative methods to accomplish functional goals despite persistent cognitive deficits, often through environmental modifications, assistive devices, or strategy training [28] [27]. The choice between these approaches—or their strategic integration—forms the cornerstone of personalized neurorehabilitation plans in stroke recovery, requiring clinicians and researchers to understand their distinct theoretical foundations, mechanisms, and evidence bases.
This comparative analysis examines the theoretical underpinnings, methodological applications, and empirical support for both restorative and compensatory rehabilitation paradigms within stroke research. We present structured comparisons of quantitative outcomes, detailed experimental protocols, and analytical frameworks to guide evidence-based practice and future research directions in cognitive rehabilitation.
Theoretical Foundations and Conceptual Frameworks
The restorative and compensatory approaches originate from different theoretical models of how the brain responds to injury and achieves functional improvement. Understanding these foundational principles is essential for appropriate application and research design.
Restorative Rehabilitation: Theoretical Basis
Restorative approaches are predominantly grounded in the principles of neuroplasticity—the brain's inherent capacity to reorganize its structure and function in response to experience. The core hypothesis posits that targeted, repetitive cognitive activity can stimulate cortical reorganization, potentially restoring damaged neural pathways or engaging peri-lesional areas to support recovered function [26] [27]. Key theoretical elements include:
- Experience-Dependent Plasticity: Neural circuits can be modified through intense, specific training experiences, leading to strengthened synaptic connections [26].
- Task-Specific Training: Recovery is optimized when training closely mirrors the targeted cognitive domain, promoting specific neural adaptations [26].
- Massed Practice: High-intensity, repetitive practice is necessary to drive neural reorganization and consolidation of learning [29].
Modern restorative interventions often incorporate advanced technologies including computerized cognitive training, virtual reality, and brain-computer interfaces to deliver precisely controlled, engaging training environments that can be systematically progressed in difficulty [26].
Compensatory Rehabilitation: Theoretical Basis
Compensatory approaches stem from a different conceptual model that emphasizes functional adaptation rather than neurological restoration. The fundamental premise is that individuals can achieve functional goals through alternative means when impaired functions cannot be fully restored. Theoretical foundations include:
- Ecological Models: Focus on improving performance in real-world contexts through adaptation of tasks or environments [28].
- Behavioral Compensation: Development of new behavioral strategies to circumvent cognitive impairments [28] [27].
- Environmental Adaptation: Modifying the physical or social environment to reduce cognitive demands [28].
Compensatory approaches include external aids (e.g., calendars, smartphones), internal strategies (e.g., mnemonics, self-talk), and environmental modifications (e.g., reducing distractions, labeling cabinets) [28] [27]. These strategies acknowledge persistent deficits while focusing on maximizing functional independence and participation.
The following conceptual diagram illustrates the theoretical pathways and mechanisms differentiating these approaches:
Figure 1: Theoretical Pathways of Restorative and Compensatory Rehabilitation. This diagram illustrates the distinct mechanisms through which restorative (blue) and compensatory (green) approaches operate following stroke injury, with the potential for integrated application (yellow).
Comparative Efficacy: Quantitative Analysis of Outcomes
Empirical evidence for both restorative and compensatory approaches varies across cognitive domains and severity levels of stroke-related impairment. The tables below synthesize quantitative findings from systematic reviews and clinical studies, providing a comparative analysis of outcomes.
Table 1: Efficacy of Restorative Cognitive Rehabilitation After Stroke
| Cognitive Domain | Intervention Type | Outcome Measures | Effect Size (SMD/OR) | Evidence Quality | Key References |
|---|---|---|---|---|---|
| Basic ADLs | Domain-specific retraining | Barthel Index, FIM | SMD 0.48 (95% CI: -0.04 to 1.01) | Very low | [30] |
| Instrumental ADLs | Executive function training | IADL scales | SMD -0.19 (95% CI: -0.65 to 0.27) | Moderate | [30] |
| Global Cognition | Computerized training | MMSE, MoCA | Variable effects | Low to moderate | [26] |
| Attention | Attention process training | Reaction time, accuracy | 15-20% improvement in processing speed | Moderate | [26] |
| Executive Function | Strategy-based training | Wisconsin Card Sort, Trail Making | Hedges' g = 0.48 (p < 0.01) | Moderate | [26] |
Table 2: Efficacy of Compensatory Cognitive Rehabilitation After Stroke
| Strategy Category | Specific Techniques | Targeted Limitations | Functional Improvement | Evidence Support | Key References |
|---|---|---|---|---|---|
| Assistive Devices | Memory aids, smart technology | Memory, executive function | Enhanced independence perceptions | Strong | [28] |
| Method Modification | Task sequencing, time management | Executive function, attention | Maintained engagement in activities | Moderate | [28] |
| Frequency Adjustment | Activity reduction, pacing | Fatigue, processing speed | Associated with depressed mood | Mixed | [28] |
| Human Assistance | Caregiver support, supervision | Multiple domains | Context-dependent acceptability | Variable | [28] |
| Environmental Adaptation | Workspace modification, signage | Attention, executive function | Reduced environmental demands | Moderate | [27] |
Table 3: Comparative Predictors of Treatment Response
| Factor | Restorative Approach | Compensatory Approach | Clinical Implications |
|---|---|---|---|
| Time Post-Stroke | More effective in early phase (<6 months) | Effective across all phases | Timing influences approach selection |
| Severity of Impairment | Mild to moderate deficits | All severity levels, including severe | Severe deficits may favor compensation |
| Cognitive Domain | Attention, executive function | Memory, executive function | Domain-specific efficacy patterns |
| Neuroimaging Findings | Greater cortical reserve | Integrity of alternative networks | Biomarker-guided prescription |
| Patient Preferences | High self-efficacy, internal locus | Practical, immediate solutions | Engagement and adherence considerations |
Experimental Protocols and Methodological Considerations
Robust experimental design is essential for evaluating the efficacy of rehabilitation approaches. Below we detail standardized protocols for investigating restorative and compensatory interventions in stroke research.
Restorative Training Experimental Protocol
Objective: To determine the effect of process-specific cognitive retraining on neuropsychological function and daily living outcomes.
Population: Adults with first-ever stroke (3-12 months post-injury) with documented cognitive impairment in targeted domains.
Intervention Protocol:
- Frequency/Duration: 60-minute sessions, 3-5 times/week for 12 weeks
- Progression: Hierarchical difficulty adjustment maintaining 80% accuracy
- Core Components:
- Massed Practice: High-intensity, repetitive drills targeting specific cognitive domains
- Feedback: Continuous performance feedback with reinforcement
- Generalization: Progressive transfer of skills to ecologically relevant tasks
Control Conditions: Active control (non-specific cognitive activities) or standard care
Outcome Measures:
- Primary: Standardized cognitive tests targeting trained domains
- Secondary: Functional capacity measures (e.g., ADL scales), neuroimaging (fMRI, EEG)
- Follow-up: 3, 6, and 12 months post-intervention
Table 4: Research Reagent Solutions for Cognitive Rehabilitation Studies
| Reagent/Resource | Primary Function | Application Context | Example Products/Protocols |
|---|---|---|---|
| Computerized Cognitive Training Platforms | Delivery of standardized, adaptive restorative exercises | Restorative trials, home-based training | Cogmed, BrainHQ, RehaCom |
| Virtual Reality Systems | Immersive environment for ecologically valid assessment and training | Transfer evaluation, motivational enhancement | BTS NIRVANA, VRADL System |
| Standardized Neuropsychological Batteries | Objective measurement of cognitive change across domains | Outcome assessment, baseline characterization | RBANS, CNS-VS, NEPSY-II |
| Functional Assessment Tools | Measurement of real-world functional impact | Primary outcomes, ecological validity | FIM, Barthel Index, ADL Profile |
| Neuroimaging Acquisition & Analysis | Quantification of neural changes associated with recovery | Mechanism investigation, biomarker identification | fMRI, DTI, ERP protocols |
| Ecological Momentary Assessment | Real-world monitoring of cognitive function | Compensation utilization, treatment generalization | Smartphone-based EMA apps |
Compensatory Strategy Training Protocol
Objective: To evaluate the efficacy of systematic compensatory strategy training on functional independence.
Population: Stroke survivors with persistent cognitive deficits affecting daily functioning.
Intervention Protocol:
- Structured Training: Progressive introduction of compensatory strategies
- Strategy Categories:
- External Aids: Calendars, smartphones, alarms, organizers
- Internal Strategies: Mnemonics, self-instruction, visualization
- Environmental Modifications: Organized workspaces, reduction of distractions
- Generalization Training: Gradual application to real-world contexts with fading support
Active Ingredients: Strategy instruction, guided practice, problem-solving training, environmental support
Outcome Measures:
- Primary: Performance-based functional measures (e.g., Executive Function Performance Test)
- Secondary: Strategy use frequency, perceived effectiveness, caregiver burden
- Ecological Validity: Real-world task performance in home environment
The following workflow diagram illustrates the implementation sequence for a comprehensive rehabilitation trial:
Figure 2: Experimental Workflow for Comparative Rehabilitation Trials. This diagram outlines a methodological framework for investigating restorative versus compensatory approaches, highlighting key components including randomization, active controls, and blinded outcome assessment.
Research Gaps and Future Directions
Despite growing evidence in cognitive rehabilitation, significant methodological challenges and knowledge gaps remain. Recent systematic reviews highlight that descriptions of intervention protocols are frequently insufficient, restricting understanding, replication, and implementation of evidence-based cognitive rehabilitation [29]. Specifically, reporting of intervention "active ingredients" occurs in approximately only 50% of studies, with inadequate description of who provided interventions, specific procedures, and tailoring methods [29].
Future research priorities include:
- Longitudinal Studies: Investigation of long-term treatment effects and optimal timing for different approaches
- Personalized Medicine: Identification of biomarkers and clinical predictors to match patients with optimal interventions
- Combined Interventions: Systematic evaluation of integrated restorative-compensatory approaches
- Technology-Enhanced Methods: Development of accessible, engaging rehabilitation technologies including virtual reality and tele-rehabilitation [26]
- Implementation Science: Strategies to overcome barriers to clinical adoption of evidence-based protocols
The field would benefit from consistent application of reporting guidelines such as the TIDieR checklist to enhance methodological transparency and clinical implementation [29].
Both restorative and compensatory approaches offer valuable, complementary pathways for cognitive rehabilitation following stroke. Restorative strategies target neuroplasticity mechanisms with the aim of restoring impaired cognitive functions, while compensatory approaches focus on functional adaptation through alternative strategies and environmental modifications. Current evidence suggests that the efficacy of each approach varies based on multiple factors including time post-stroke, severity of impairment, specific cognitive domains affected, and individual patient characteristics.
The most effective clinical applications may involve strategic integration of both approaches, leveraging their complementary strengths. Restorative methods may be prioritized in early recovery phases with milder impairments, while compensatory strategies may be particularly valuable for chronic deficits and more severe impairments. Future research should address existing methodological limitations, identify predictors of treatment response, and develop personalized rehabilitation algorithms to optimize functional outcomes for stroke survivors.
Stroke remains a leading cause of long-term disability worldwide, with cognitive impairment representing a common and devastating consequence that profoundly affects patients' quality of life and functional independence [31]. Understanding the specific stroke characteristics that influence cognitive outcomes is crucial for developing targeted rehabilitation strategies and improving prognostic accuracy. This review systematically examines the impact of three fundamental stroke characteristics—lesion location, brain network disruption, and vascular pathophysiology—on cognitive outcomes, framed within the context of comparative cognitive rehabilitation research.
The connection between stroke and cognitive impairment is well-established, affecting approximately 30-70% of stroke survivors [31]. The heterogeneity of cognitive deficits observed following stroke reflects the complex interplay between focal injury, distributed network disruption, and underlying vascular pathology. Recent advances in neuroimaging and network neuroscience have begun to unravel the mechanisms by which these factors collectively contribute to cognitive outcomes, providing a more nuanced understanding that moves beyond simple lesion-volume approaches.
This analysis synthesizes current evidence regarding how specific stroke features predict cognitive performance, with particular emphasis on implications for comparative rehabilitation science. By examining the structural and functional network consequences of stroke through a comparative lens, we aim to inform the development of more precisely targeted cognitive rehabilitation interventions based on individual stroke characteristics.
Stroke Lesion Location and Cognitive Outcome
The Independent Predictive Value of Lesion Location
Stroke location has emerged as a powerful independent predictor of cognitive outcome, providing prognostic value beyond traditional measures such as stroke volume and initial clinical severity [32]. A prospective study of 428 patients with ischemic stroke demonstrated that lesion location remained the strongest independent predictor of performance on the Montreal Cognitive Assessment (MoCA) at 3 months post-stroke, significantly improving prediction models that included only age, initial National Institutes of Health Stroke Scale score, and stroke volume [32]. The area under the curve for predicting cognitive outcome increased from 0.697 to 0.771 when lesion location was added to the model, highlighting its substantial contribution to prognostic accuracy [32].
The brain demonstrates a remarkable degree of functional specialization, with specific cognitive domains predominantly mediated by distinct neuroanatomical regions. Consequently, the location of a stroke lesion directly determines the pattern of cognitive deficits observed [31]. For instance, strokes affecting the frontal lobes are frequently associated with executive dysfunction, including impairments in planning, problem-solving, and cognitive flexibility [31]. In contrast, lesions involving the temporal lobes often lead to memory impairment, particularly when hippocampal structures or their connections are compromised [31]. This regional specificity explains why two strokes of similar volume can produce dramatically different cognitive profiles depending on their anatomical coordinates.
Eloquent Cognitive Regions Identified Through Advanced Neuroimaging
Advanced neuroimaging techniques have enabled researchers to identify particularly "eloquent" regions for cognitive function that, when damaged, disproportionately impact cognitive outcomes. Using voxel-based lesion-symptom mapping in a development sample of 215 patients, researchers created statistical maps that identified critical regions where lesions consistently predicted poor cognitive performance [32]. When validated in an independent replication sample, these maps confirmed that lesions in hub regions—particularly those involved in large-scale brain networks such as the default mode network and frontoparietal control network—were most detrimental to cognitive recovery [32].
Table 1: Impact of Specific Lesion Locations on Cognitive Domains
| Lesion Location | Primary Cognitive Domains Affected | Characteristic Deficits |
|---|---|---|
| Frontal Lobes | Executive Function, Attention | Impaired planning, reduced mental flexibility, poor problem-solving, diminished attentional control |
| Temporal Lobes | Memory, Language | Verbal and visual memory deficits, anomia, impaired comprehension |
| Parietal Lobes | Visuospatial Processing, Attention | Neglect, constructional apraxia, impaired mental rotation |
| Subcortical Structures | Executive Function, Processing Speed | Mental slowing, impaired set-shifting, reduced working memory capacity |
| White Matter Tracts | Processing Speed, Executive Function | Disconnection syndromes, slowed information processing, impaired interhemispheric integration |
Experimental Protocol for Lesion Location Analysis
The methodology for establishing lesion location as an independent predictor of cognitive outcome typically involves:
- Patient Recruitment: Consecutive patients with confirmed ischemic stroke are recruited prospectively, with imaging performed within 24-72 hours of symptom onset [32].
- Image Acquisition: High-resolution structural MRI (including T1, T2, FLAIR, and DWI sequences) is obtained using standardized protocols [32].
- Lesion Mapping: Individual stroke lesions are manually delineated on diffusion-weighted imaging or T2-weighted sequences and normalized to a standard brain template [32].
- Cognitive Assessment: Standardized cognitive assessment using instruments such as the Montreal Cognitive Assessment (MoCA) is performed at predetermined time points (e.g., 3 months post-stroke) [32].
- Statistical Analysis: Voxel-based lesion-symptom mapping correlates lesion location with cognitive scores, while multivariate regression models assess the independent contribution of lesion location after controlling for covariates such as age, stroke volume, and initial severity [32].
Brain Network Disruption and Cognitive Impairment
Structural and Functional Network Disruption in Vascular Cognitive Impairment
The traditional focal lesion model of stroke has been substantially augmented by understanding strokes as disconnection syndromes that disrupt distributed brain networks [33] [34]. Research on vascular cognitive impairment (VCI) reveals that cerebral small vessel disease causes significant disruptions in structural brain networks, characterized by reduced white matter integrity and altered network topology [33]. Diffusion tensor imaging (DTI) studies consistently show that individuals with VCI exhibit reduced fractional anisotropy (indicating white matter damage) and increased mean and radial diffusivity compared to healthy controls [33].
At the network level, structural analyses demonstrate lower global and local efficiency, reduced small-world properties, and increased characteristic path length in VCI patients [33]. These topological changes reflect a less optimized network architecture that impairs efficient information transfer between brain regions. Notably, these disruptions are particularly evident in key regions of the default mode network and visual networks, suggesting selective vulnerability of these systems to vascular pathology [33].
Structure-Function Coupling as a Compensatory Mechanism
A paradoxical finding in VCI research is that despite significant structural network disruption, functional network topology often remains relatively preserved [33]. This apparent discrepancy may be explained by enhanced structure-function coupling observed in critical nodes of the default mode and visual networks in VCI participants [33]. This enhanced coupling correlates with better performance in memory function and information processing speed, particularly in regions such as the temporal calcarine, insula, occipital, and lingual areas [33].
This phenomenon may represent a compensatory mechanism in which the brain maximizes the functional utility of remaining structural connections to maintain cognitive performance despite accumulating pathology. The enhancement of structure-function coupling in early disease stages contrasts with the breakdown of such coupling in more advanced neurodegenerative conditions, suggesting a potential window for therapeutic intervention when compensatory plasticity remains robust.
Rich-Club Organization and Cognitive Vulnerability
The brain's rich-club organization—a hierarchy in which highly connected hub regions are densely interconnected with each other—appears particularly vulnerable to vascular pathology [34]. Research comparing preclinical cognitive impairment (PCI) and mild cognitive impairment (MCI) in cerebral small vessel disease demonstrates that while rich-club organization remains relatively intact in PCI, it becomes significantly disrupted in MCI patients [34].
Nodal strength loss predominantly affects hub nodes rather than peripheral nodes in MCI patients, with significant disruption observed in rich-club connections that link these central hubs [34]. This pattern of disruption has profound implications for cognitive function, as rich-club connections facilitate efficient integration of information across distributed brain networks. The association between white matter hyperintensities and executive function is mediated specifically by microstructural changes in these central network connections, highlighting their critical role in maintaining cognitive performance [34].
Table 2: Brain Network Metrics and Their Cognitive Correlates in Cerebrovascular Disease
| Network Metric | Description | Alteration in VCI | Cognitive Correlation |
|---|---|---|---|
| Global Efficiency | Measure of overall network integration | Decreased | Associated with processing speed and executive function |
| Local Efficiency | Measure of local information transfer | Decreased | Correlates with memory and attention |
| Characteristic Path Length | Average shortest path between nodes | Increased | Inversely related to processing speed |
| Small-Worldness | Balance between segregation and integration | Reduced | Associated with multiple cognitive domains |
| Rich-Club Organization | Interconnectivity of hub regions | Disrupted in MCI | Predicts executive function and global cognition |
| Structure-Function Coupling | Alignment between structural and functional connectivity | Enhanced in early VCI | Correlates with memory and processing speed |
Experimental Protocol for Network Analysis
The standard methodology for investigating brain network disruption in cerebrovascular disease includes:
- Participant Selection: Recruitment of carefully characterized patients with cerebral small vessel disease across the cognitive spectrum (preclinical, mild cognitive impairment) alongside matched healthy controls [33] [34].
- Multimodal Imaging: Acquisition of high-resolution structural MRI, diffusion tensor imaging, and resting-state functional MRI using standardized protocols on 3.0 Tesla scanners [33].
- Network Construction: Structural networks are reconstructed from DTI data using deterministic or probabilistic tractography, while functional networks are derived from resting-state fMRI correlation matrices [33] [34].
- Graph Theory Analysis: Calculation of global and nodal graph metrics including efficiency, path length, small-worldness, and rich-club coefficients [34].
- Structure-Function Coupling Assessment: Quantification of the relationship between structural connectivity strength and functional connectivity magnitude for each region pair [33].
- Statistical Analysis: Between-group comparisons of network metrics with correction for multiple comparisons, followed by correlation analyses between network properties and cognitive performance [33] [34].
Vascular Pathophysiology and Cognitive Outcomes
Cerebral Small Vessel Disease and White Matter Integrity
Cerebral small vessel disease (CSVD) represents a crucial vascular pathophysiology that significantly impacts cognitive outcomes through its effect on white matter integrity [33]. CSVD encompasses multiple pathological processes affecting the small arteries, arterioles, venules, and capillaries of the brain, with radiological markers including white matter hyperintensities (WMH), lacunes, enlarged perivascular spaces, and cerebral microbleeds [34]. These manifestations reflect underlying pathological processes including chronic ischemia, blood-brain barrier dysfunction, and neuroinflammation [33].
The presence and burden of white matter hyperintensities is associated with a 14% increased risk of cognitive impairment and all-cause dementia [33]. The relationship between WMH volume and cognitive function is mediated by reduced cortical thickness, particularly in medial temporal lobe regions critical for memory function [33]. Furthermore, the location of WMH appears to influence their cognitive impact, with periventricular WMH showing particularly strong associations with reduced cortical thickness and cognitive impairment [33].
Hemodynamic Forces and Endothelial Dysfunction
Altered hemodynamic forces, particularly disturbed or oscillatory shear stress, play a fundamental role in vascular pathophysiology that contributes to cognitive decline [35]. Under physiological conditions, laminar shear stress promotes vasoprotective effects by stimulating endothelial cells to release nitric oxide and cytokines with antithrombotic and vasodilator properties [35]. In contrast, oscillatory shear stress induces endothelial dysfunction through multiple mechanisms:
- Flow-Sensitive Ion Channels: Altered shear stress affects flow-sensitive ion channels including Piezo1 and Piezo2, disrupting cell membrane polarization and reducing production of protective molecules like nitric oxide [35].
- Glycocalyx Displacement: Disturbed shear stress physically displaces the endothelial glycocalyx, triggering intracellular responses that promote oxidative and inflammatory states [35].
- Transcriptional Regulation: Oscillatory shear stress activates mechanosensitive transcription factors including Yes-associated protein (YAP), leading to pro-inflammatory gene expression and increased monocyte adhesion [35].
These mechanisms collectively establish a chronic inflammatory state in the endothelium that contributes to blood-brain barrier dysfunction, impaired cerebral autoregulation, and ultimately, tissue damage manifesting as cognitive impairment.
Experimental Protocol for Vascular Pathophysiology Assessment
Methodologies for investigating vascular pathophysiology in cognitive impairment include:
- Participant Characterization: Comprehensive assessment of vascular risk factors (hypertension, diabetes, atrial fibrillation) alongside cognitive evaluation using standardized neuropsychological batteries [33].
- Multimodal Imaging Acquisition: Structural MRI for quantification of white matter hyperintensities (Fazekas scale), diffusion tensor imaging for white matter integrity, and arterial spin labeling for cerebral blood flow measurement [33].
- Vascular Assessment: Evaluation of endothelial function through flow-mediated dilation, assessment of arterial stiffness via pulse wave velocity, and monitoring of blood pressure variability [35].
- Inflammatory Biomarker Analysis: Measurement of circulating inflammatory markers (e.g., IL-6, TNF-α, CRP) and blood-brain barrier breakdown markers [35].
- Statistical Modeling: Multivariate analyses examining relationships between vascular parameters, imaging markers of cerebrovascular disease, and cognitive performance, with adjustment for potential confounders [33] [35].
Comparative Effectiveness of Rehabilitation Approaches
Integration of Neuromodulation with Cognitive Rehabilitation
Recent advances in cognitive rehabilitation have explored the integration of repetitive transcranial magnetic stimulation (rTMS) with conventional rehabilitation approaches, with emerging evidence suggesting differential effectiveness depending on the specific combination employed [36]. A systematic review and network meta-analysis of 21 randomized controlled trials involving 1,074 stroke patients compared various rehabilitation methods combined with rTMS, revealing distinct patterns of effectiveness across cognitive and mood domains [36].
The analysis demonstrated that speech rehabilitation combined with rTMS was the most effective approach for improving cognitive function (SMD=0.40; 95% CI, -0.08 to 0.87; SUCRA=95.1%), while cognitive rehabilitation combined with rTMS was superior for reducing negative mood (SMD=0.91; 95% CI, 0.45-3.23; SUCRA=84.5%) and improving quality of life (SMD=0.49; 95% CI, -0.33 to 1.30; SUCRA=99.4%) [36]. These findings suggest that the optimal combination of rTMS with rehabilitation approaches depends on the specific therapeutic target, with implications for personalized rehabilitation planning.
Location-Dependent Rehabilitation Response
Evidence from traumatic brain injury research suggests that lesion location may influence responsiveness to cognitive training, with implications for stroke rehabilitation [37]. A pilot study investigating cognitive training in adolescents with traumatic brain injury found that the presence or absence of diffuse axonal injuries in the deep brain nuclei determined significant differences in long-term training benefit [37]. This finding highlights the importance of considering lesion location when designing and prescribing cognitive rehabilitation protocols.
The influence of lesion location on rehabilitation response likely reflects the differential involvement of critical network hubs and their connections. Lesions affecting rich-club regions or their connecting pathways may diminish the brain's capacity to respond to rehabilitation by disrupting the structural scaffolding necessary for functional reorganization and compensation [34]. This understanding supports a precision medicine approach to cognitive rehabilitation that accounts for individual patterns of network disruption.
Experimental Protocol for Comparative Rehabilitation Studies
Methodologies for comparing rehabilitation effectiveness in stroke populations include:
- Study Design: Randomized controlled trials with parallel groups or crossover designs, with careful attention to blinding of outcome assessors [36].
- Participant Selection: Well-characterized stroke patients stratified by key characteristics such as lesion location, time post-stroke, and baseline cognitive status [36].
- Intervention Protocols: Standardized rehabilitation protocols with documented intensity, frequency, and duration, combined with precise rTMS parameters (target location, frequency, intensity) [36].
- Outcome Assessment: Multidimensional outcome measures encompassing cognitive function (domain-specific and global), mood, quality of life, and functional abilities [36].
- Statistical Analysis: Network meta-analysis for comparing multiple interventions simultaneously, with surface under the cumulative ranking curve (SUCRA) values to estimate relative effectiveness [36].
Table 3: Comparative Effectiveness of Combined rTMS and Rehabilitation Approaches
| Intervention Combination | Cognitive Function | Negative Mood Reduction | Quality of Life Improvement | SUCRA Values |
|---|---|---|---|---|
| Speech Rehabilitation + rTMS | SMD=0.40(-0.08 to 0.87) | Moderate effect | Moderate effect | 95.1% (Cognition) |
| Cognitive Rehabilitation + rTMS | Moderate effect | SMD=0.91(0.45-3.23) | SMD=0.49(-0.33 to 1.30) | 84.5% (Mood)99.4% (QoL) |
| Physical Therapy + rTMS | Lower effect | Lower effect | Lower effect | Variable by domain |
| Occupational Therapy + rTMS | Lower effect | Lower effect | Lower effect | Variable by domain |
Table 4: Essential Research Reagents and Methodologies for Investigating Stroke and Cognition
| Resource Category | Specific Tools/Assessments | Research Application | Key References |
|---|---|---|---|
| Neuropsychological Assessments | Montreal Cognitive Assessment (MoCA), Mini-Mental State Examination (MMSE), Symbol Digit Modalities Test (SDMT), Trail Making Test (TMT) | Quantification of cognitive deficits across multiple domains | [32] [33] |
| Structural MRI Sequences | T1-weighted, T2-weighted, FLAIR, Diffusion Tensor Imaging (DTI) | Lesion delineation, white matter hyperintensity quantification, structural network construction | [32] [33] [34] |
| Functional MRI Approaches | Resting-state fMRI, Task-based fMRI, Arterial Spin Labeling (ASL) | Functional connectivity analysis, network identification, cerebral blood flow measurement | [33] [34] |
| Vascular Assessment Tools | Fazekas scale, NIH Stroke Scale, Modified Rankin Scale | Quantification of cerebrovascular disease burden, stroke severity, functional outcome | [32] [33] |
| Network Analysis Platforms | FSL, FreeSurfer, Brain Connectivity Toolbox, GraphVar | Construction and analysis of structural and functional brain networks | [33] [34] |
| Neuromodulation Equipment | Repetitive TMS systems, Neuronavigation equipment | Investigation of causal brain-behavior relationships, therapeutic interventions | [36] |
The impact of stroke characteristics on cognitive outcomes reflects a complex interplay between lesion location, network disruption, and vascular pathophysiology. Lesion location provides powerful independent prognostic information, with specific cognitive domains mapping onto distinct neuroanatomical regions. Beyond focal damage, strokes disrupt distributed brain networks, with particular vulnerability of rich-club connections that facilitate efficient information integration. Underlying vascular pathophysiology, particularly cerebral small vessel disease, contributes to progressive white matter damage and network disruption through mechanisms involving endothelial dysfunction and impaired hemodynamics.
The comparative effectiveness of rehabilitation approaches demonstrates that optimal outcomes may require precisely targeted interventions based on individual stroke characteristics. The integration of neuromodulation with conventional rehabilitation shows promise, with differential effectiveness across cognitive and mood domains. Future research should continue to refine our understanding of how specific stroke features influence responsiveness to different rehabilitation approaches, ultimately supporting a precision medicine framework for cognitive rehabilitation after stroke.
Methodology and Clinical Application of Cutting-Edge Cognitive Rehabilitation Techniques
Non-invasive brain stimulation (NIBS) techniques, particularly transcranial direct current stimulation (tDCS) and repetitive transcranial magnetic stimulation (rTMS), have emerged as powerful tools for modulating cortical excitability in both research and clinical settings. These techniques enable researchers and clinicians to probe neural mechanisms and promote neuroplasticity without surgical intervention. For cognitive rehabilitation in stroke research, understanding the comparative effectiveness of different NIBS protocols is paramount for developing targeted interventions. This guide provides a systematic comparison of tDCS and rTMS protocols, drawing on recent meta-analyses and randomized controlled trials to outline their mechanisms, optimal targets, and efficacy metrics, with a specific focus on applications in stroke recovery.
Comparative Efficacy of NIBS Protocols in Stroke Rehabilitation
Recent high-quality evidence from a Bayesian network meta-analysis of 37 randomized controlled trials provides robust comparative data on the effectiveness of various NIBS protocols for early stroke rehabilitation. The analysis evaluated outcomes including upper and lower extremity motor function, activities of daily living (ADL), and neurological function at both the end of intervention and at 3-month follow-up [38].
Table 1: Protocol Efficacy Rankings for Stroke Motor Recovery (SUCRA Values)
| Stimulation Protocol | Upper Extremity Function (End) | Upper Extremity Function (3-Month) | Lower Extremity Function | ADL (End) | ADL (3-Month) | Neurological Function (End) | Neurological Function (3-Month) |
|---|---|---|---|---|---|---|---|
| BL-rTMS | 92.8% | 95.4% | - | 100% | 85.6% | 99.7% | 97.05% |
| LF-rTMS | - | - | 67.7% | - | - | - | - |
| iTBS | 19.5% | 26.9% | - | - | - | - | - |
| HD-tDCS | 57.3% | 52.8% | - | - | - | - | - |
| Sham | 0.7% | 1.7% | 22.1% | 0% | 13.9% | 0% | 3.0% |
SUCRA (Surface Under the Cumulative Ranking Curve) values represent the percentage of effectiveness relative to other protocols, with 100% indicating highest efficacy [38].
The analysis revealed that bilateral rTMS (BL-rTMS) application combining high- and low-frequency stimulation emerged as the most effective protocol for improving upper extremity motor function, activities of daily living, and neurological function, with sustained benefits at 3-month follow-up [38]. For lower extremity motor function, low-frequency rTMS (LF-rTMS) applied to unaffected hemisphere areas demonstrated the highest efficacy [38].
Table 2: Safety Profiles of NIBS Protocols in Early Stroke
| Stimulation Protocol | Safety Profile | Common Adverse Effects |
|---|---|---|
| LF-rTMS (1 Hz) | Excellent (0% AEs) | Minimal side effects |
| 5 Hz-rTMS | Excellent (0% AEs) | Minimal side effects |
| iTBS | Excellent (0% AEs) | Minimal side effects |
| BL-rTMS | Good | Mild headache, discomfort |
| HD-tDCS | Good | Tingling, itching |
Adverse events (AEs) reported in clinical trials; excellent safety indicates no serious adverse events reported [38].
Mechanisms of Action: tDCS vs. rTMS
Neurophysiological Foundations
tDCS and rTMS operate through distinct yet complementary mechanisms to modulate cortical excitability:
tDCS mechanisms involve application of weak direct currents (typically 1-2 mA) through surface electrodes, inducing subthreshold polarization of neuronal membranes. Anodal stimulation typically increases excitability through depolarization, while cathodal stimulation decreases excitability via hyperpolarization [39]. The after-effects of tDCS are thought to involve NMDA receptor-dependent synaptic plasticity [39] [40]. Recent evidence also suggests tDCS influences glial cell activity, particularly astrocytes, which may contribute to its neuromodulatory effects through neurovascular coupling and extracellular ion homeostasis [41].
rTMS mechanisms utilize rapidly alternating magnetic fields to induce electrical currents in targeted cortical regions. The effects depend critically on stimulation parameters: high-frequency rTMS (≥5 Hz) generally increases cortical excitability, while low-frequency rTMS (1 Hz) typically decreases excitability [38] [41]. The after-effects are mediated by long-term potentiation (LTP) and long-term depression (LTD) -like mechanisms, GABAergic modulation, and changes in functional connectivity within targeted networks [38].
Molecular and Biochemical Pathways
Both tDCS and rTMS engage complex molecular pathways that extend beyond immediate electrophysiological effects:
BDNF-dependent mechanisms play a crucial role in NIBS-induced plasticity. The Val66Met polymorphism in the BDNF gene can significantly modulate response to stimulation protocols [40]. In fibromyalgia studies, tDCS-induced analgesia and cortical silent period (CSP) reductions were BDNF-dependent, highlighting the neurotrophin's role in GABAergic modulation [40].
Neurotransmitter systems including GABAergic, glutamatergic, and cholinergic pathways are differentially modulated by various stimulation parameters. Short-interval intracortical inhibition (SICI) probes GABAA-mediated inhibitory networks, while intracortical facilitation (ICF) assesses glutamatergic facilitatory networks [42]. rTMS protocols specifically modulate kynurenine pathway metabolism, which impacts cerebral mitochondrial respiration and ATP production - crucial bioenergetic components for neuroplasticity [43].
Inflammatory and immune pathways are increasingly recognized as mediators of NIBS effects, particularly in pathological conditions. Stimulation can influence cytokine profiles, microglial activation, and neuroinflammatory processes that subsequently impact neuronal excitability and network function [43].
Standard Experimental Protocols and Methodologies
Motor Cortex Stimulation for Balance and Motor Learning
Research on M1 involvement in balance control provides exemplary methodology for NIBS studies. A standard protocol for investigating balance acquisition involves:
Stimulation Parameters:
- tDCS: Anodal stimulation at 1-2 mA intensity for 20-30 minutes, with cathode typically placed on contralateral supraorbital area [42]
- Electrode Placement: Primary motor cortex (M1) leg area localization using EEG 10-20 system (Cz for lower limb representation) [42]
Concurrent Balance Assessment:
- Platform perturbations: Forward and backward translations of standing surface
- Kinematic measures: Center of mass (COM) displacement, joint excursions
- Electrophysiological measures: Perturbation-related N1 potential (90-200 ms post-perturbation), theta (3-7 Hz) and alpha band power [42]
Outcome Measures:
- Behavioral: COM displacement reduction, decreased hip excursions
- Neurophysiological: Reduced N1 latency and amplitude, decreased alpha power, increased intracortical facilitation (ICF) [42]
Multisite Stimulation Protocols for Enhanced Efficacy
Advanced protocols increasingly employ multisite stimulation approaches to target network-level effects:
M1-Cerebellar combined protocol for fibromyalgia pain management:
- M1 electrode: Anodal placement over primary motor cortex (C3/C4)
- Cerebellar electrode: Cathodal placement over cerebellar hemisphere
- Stimulation parameters: 2 mA for 20 minutes daily [40]
Bilateral rTMS (BL-rTMS) for stroke recovery:
- Affected hemisphere: High-frequency rTMS (10-20 Hz) to facilitate excitability
- Unaffected hemisphere: Low-frequency rTMS (1 Hz) to reduce pathological inhibition
- Stimulation duration: Typically 10-20 sessions over 2-4 weeks [38]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Equipment and Materials for NIBS Studies
| Category | Specific Items | Research Function | Example Applications |
|---|---|---|---|
| Stimulation Equipment | rTMS device with figure-8 coil; tDCS stimulator with saline-soaked electrodes; Neuronavigation system | Precise delivery of stimulation protocols; Target localization with anatomical MRI | Motor cortex stimulation; DLPFC targeting for cognitive studies |
| Electrophysiology | TMS machine with EMG; EEG system with event-related potentials; EMG recording equipment | Assessment of cortical excitability (MEP, SICI, ICF); Monitoring brain dynamics | Measuring corticospinal excitability; Tracking plasticity changes |
| Behavioral Assessment | Motion capture system; Force platforms; Clinical rating scales (FMA, NIHSS, mBI) | Quantifying motor performance; Clinical outcome measurement | Balance perturbation response; Stroke recovery tracking |
| Biochemical Analysis | ELISA kits for BDNF; Genetic testing for BDNF Val66Met; Inflammatory cytokine panels | Biomarker analysis; Mechanism investigation | Predicting treatment response; Understanding molecular mechanisms |
| Computational Tools | Electric field modeling software; Functional connectivity analysis; Statistical packages (R, Stata) | Simulation of current flow; Network analysis; Data synthesis | Optimizing electrode placement; Identifying new targets [44] |
Target Selection Strategies for Specific Applications
Connectivity-Guided Target Identification
Modern NIBS research emphasizes connectivity-based targeting rather than anatomical targeting alone. A validated approach for identifying novel targets involves:
Meta-analysis derived ROIs: Initial identification of disorder-associated regions through large-scale fMRI meta-analysis (e.g., using Neurosynth with 124 ADHD studies) [44]
Cross-dataset functional connectivity validation: Using resting-state fMRI data from multiple independent datasets to identify surface regions with consistent FC patterns with disorder-associated ROIs [44]
Scalp-level translation: Converting identified cortical targets to scalp positions using 10-20 system or continuous proportional coordinates (CPC) [44]
This approach has identified novel targets for ADHD including bilateral dorsolateral prefrontal cortex, right inferior frontal gyrus, bilateral inferior parietal lobule, and supplementary motor area/pre-SMA beyond traditional DLPFC targets [44].
Symptom-Specific Targeting in Neurological Disorders
Stroke motor recovery: Contralesional M1 for LF-rTMS to reduce transcallosal inhibition; Ipsilesional M1 for HF-rTMS to facilitate residual networks [38]
Chronic pain management: M1 stimulation regardless of pain location; DLPFC for cognitive-affective pain components; Cerebellum for sensory-discriminative aspects [40]
Autism spectrum disorder: DLPFC for repetitive behaviors and executive functions; Temporoparietal junction for social cognition [41]
Emerging Technologies and Future Directions
Novel Stimulation Modalities
Transcranial random noise stimulation (tRNS) applies random electrical oscillations (0.1-640 Hz) to modulate cortical excitability through stochastic resonance mechanisms [39]. Compared to tDCS, tRNS produces more gradual effects on motor learning with potentially superior outcomes for complex tasks [39].
Transcranial static magnetic field stimulation (tSMS) uses compact magnet arrays to suppress cortical excitability up to 8 cm deep without electrical currents, offering novel inhibition protocols with minimal discomfort [43].
Precision Neuromodulation Approaches
Future directions emphasize individualized electric field modeling based on structural MRI to account for anatomical variability [44]. Closed-loop stimulation approaches using real-time EEG or fMRI feedback are emerging to dynamically adjust stimulation parameters based on brain state [43]. The integration of multimodal biomarkers including genetic, neurophysiological, and imaging data aims to develop predictive models for treatment response across neurological and psychiatric conditions [45] [40].
The comparative analysis of tDCS and rTMS protocols reveals distinct advantages for specific applications in cognitive rehabilitation research. For stroke recovery, bilateral rTMS protocols demonstrate superior efficacy for upper extremity function and activities of daily living, while low-frequency rTMS shows particular promise for lower extremity recovery. The mechanistic understanding of these techniques continues to evolve beyond simple excitation/inhibition models to encompass network-level effects, molecular pathways, and system-level reorganization. Future research directions emphasizing connectivity-guided targeting, individualized dosing, and multimodal integration promise to enhance the precision and efficacy of non-invasive brain stimulation for both basic research and clinical applications in cognitive rehabilitation.
Within the landscape of stroke rehabilitation, post-stroke cognitive impairment (PSCI) is a prevalent consequence, affecting more than one-third of patients and significantly impacting independence and quality of life [46]. Cognitive training is a cornerstone of rehabilitation, aimed at mitigating these deficits through the repetitive practice of standardized tasks. Technology-assisted cognitive training, primarily through Computer-Assisted Cognitive Rehabilitation (CACR) and Virtual Reality (VR) systems, has emerged as a powerful complement to traditional pencil-and-paper methods [46]. These technologies offer advantages such as high-intensity, repetitive practice, immediate performance feedback, and the ability to tailor difficulty levels to individual patient profiles [46]. This guide provides an objective comparison of CACR and VR systems, framing their implementation and efficacy within the specific context of stroke research to inform researchers and clinical scientists.
Comparative Efficacy in Post-Stroke Cognitive Impairment (PSCI)
Direct comparative evidence for these technologies in stroke populations is growing. A 2022 network meta-analysis directly compared VR, CACR, and conventional therapy in over 1000 patients with PSCI, providing a hierarchy of efficacy [46].
Table 1: Efficacy of Cognitive Training Interventions for PSCI (Network Meta-Analysis Findings)
| Intervention | Comparative Efficacy vs. Conventional Therapy | Key Cognitive Domains Addressed |
|---|---|---|
| Computer-Assisted Cognitive Rehabilitation (CACR) | Likely the most effective treatment [46] | Memory, attention, problem-solving, processing speed, language [46] |
| Virtual Reality (VR) | Superior to conventional therapy [46] | Memory, attention, executive functions, global cognition [46] [47] |
| Conventional Therapy | Baseline comparator [46] | Varies by protocol (often paper-and-pencil tasks) [46] |
For broader neurological conditions, the evidence base is also expanding. Studies on Mild Cognitive Impairment (MCI) suggest VR-based games may show a trend toward greater efficacy in improving cognitive impairments compared to VR-based cognitive training, with the level of immersion being a significant moderator of outcomes [47]. In older adults with and without cognitive decline, immersive VR training has demonstrated positive effects on attention, executive functions, and global cognition, with fewer studies showing strong improvements in memory [48].
Experimental Protocols and Methodologies
Understanding the specific protocols used in research is crucial for evaluating evidence and designing future studies.
Computer-Assisted Cognitive Rehabilitation (CACR) Protocols
CACR interventions typically involve structured, computer-based exercises. A representative RCT for patients with PSCI utilized a protocol where patients engaged in computerized exercises and games designed to target specific cognitive domains [46]. The methodology often includes:
- Session Structure: Training is conducted in multiple sessions per week (e.g., 3-5 sessions) over a period of several weeks.
- Task Progression: The software automatically adjusts the difficulty level of tasks (e.g., varying stimulus complexity, presentation speed) based on the patient's functional status and performance to maintain an appropriate challenge level [46].
- Outcome Measures: Standardized neuropsychological assessments are administered pre- and post-intervention. Common outcomes include the Mini-Mental State Examination (MMSE) for global cognition, and specific batteries for memory (e.g., word list recall), attention (e.g., digit span), and executive function [46].
Virtual Reality (VR) Cognitive Training Protocols
VR protocols can be more varied, differing in immersion level and content. A feasibility study for patients with mild to moderate Alzheimer's disease provides a clear example [49]:
- Intervention: The "MentiTree" VR cognitive training software, delivered via a head-mounted display (HMD).
- Session Structure: Participants underwent 30-minute sessions, twice a week for 9 weeks (total of 18 sessions, 540 minutes).
- Task Design: Tasks were game-style and set in alternating indoor (e.g., making a sandwich, tidying a room) and outdoor (e.g., finding directions, shopping) virtual environments. The difficulty level (e.g., levels 1-5 for indoor tasks) automatically advanced based on the participant's performance [49].
- Outcome Measures: Cognitive functions were assessed before and after the intervention using batteries like the Korean version of the Mini-Mental State Examination-2 (K-MMSE-2) and the Literacy Independent Cognitive Assessment (LICA), which includes subtests for story recall, visuospatial span, and recognition memory [49].
Another study on community-dwelling older adults implemented a leisure-based VR protocol using gardening-themed activities to engage memory, executive function, and processing speed over 16 one-hour sessions [50].
Technical Implementation and System Characteristics
The practical implementation of CACR and VR systems involves distinct hardware, software, and design philosophies.
Table 2: System Characteristics and Implementation Considerations
| Characteristic | Computer-Assisted Cognitive Rehabilitation (CACR) | Virtual Reality (VR) Systems |
|---|---|---|
| Hardware | Standard desktop computers, laptops, or tablets [46]. | Head-Mounted Displays (HMDs), sensors for body tracking, dedicated interface devices or handheld controllers [46] [49] [51]. |
| Immersion Level | Non-immersive; presented on a 2D screen [51]. | Ranges from Non-Immersive (NI-VR) to Semi-Immersive (SI-VR) and fully Immersive (I-VR) [51]. |
| Interaction Modality | Mouse, keyboard, or touchscreen input. | Naturalistic interaction through hand/body movements, controllers; provides a high sense of presence and immersion [46] [50]. |
| Key Advantages | Allows for repeated, independent learning; provides immediate feedback; cost-effective and highly accessible [46]. | High ecological validity; creates engaging, multi-sensory environments that maximize patient interaction; can simulate real-world scenarios for practice [46] [50]. |
| Key Challenges | May be less engaging over time; limited ecological validity compared to VR [46]. | Cost of equipment; risk of cybersickness (e.g., nausea, eye fatigue); requires more technical setup; may be challenging for some older adults [49] [52]. |
| Usability Findings | Generally high usability due to familiarity with computers. | Surveys indicate moderate usability scores and mild-to-moderate VR sickness, with usability rated higher by therapists than patients [52]. |
The level of VR immersion is a critical technical differentiator. Semi-immersive VR (SI-VR) has been associated with the highest proportion of significant motor improvements (88.24%) in post-stroke patients, followed by non-immersive VR (NI-VR) at 66.67% and immersive VR (I-VR) at 50% [51]. This suggests that for certain outcomes, a very high level of immersion may not be necessary for efficacy and must be balanced against the potential for adverse effects.
Decision Pathway for Researchers
The following diagram outlines a logical framework for selecting and implementing technology-assisted cognitive training in a stroke research context.
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers designing experimental trials, the following table details essential components and their functions.
Table 3: Essential Materials for Technology-Assisted Cognitive Training Research
| Item / Solution | Function in Research Context | Examples / Specifications |
|---|---|---|
| Head-Mounted Display (HMD) | Presents the virtual environment for immersive VR systems; critical for generating a sense of presence. | Oculus Rift S [49], Meta Quest 2 [52], HTC Vive Pro [50]. |
| Computer-Assisted Cognitive Rehabilitation Software | Provides the standardized, repetitive cognitive tasks for CACR interventions; allows for difficulty scaling. | Custom-designed or commercial programs targeting memory, attention, problem-solving, etc. [46]. |
| VR Cognitive Training Software | Creates the interactive, 3D environment for rehabilitation; content dictates the cognitive domains engaged. | Custom-built software (e.g., MentiTree [49]), serious games, or adapted commercial VR games. |
| Hand Tracking Sensors / Controllers | Enables user interaction with the virtual environment; captures movement data for motor-cognitive tasks. | HMD-integrated cameras, Leap Motion sensor, or dedicated VR controllers (e.g., Oculus Touch) [49]. |
| Standardized Neuropsychological Assessment Batteries | Primary outcome measures to quantify baseline cognitive status and intervention efficacy. | MMSE [46] [47], MoCA [50], LICA [49], domain-specific tests (e.g., Stroop, Corsi) [50] [53]. |
| Usability & Adverse Effects Questionnaires | Assesses the feasibility, user experience, and safety profile of the technological intervention. | System Usability Scale (SUS) [52] [50], User Experience Questionnaire (UEQ) [52], Cybersickness in VR Questionnaire (CSQ) [52]. |
Both CACR and VR systems demonstrate superior efficacy compared to conventional therapy for cognitive rehabilitation post-stroke, with CACR potentially holding a slight edge based on current network meta-analysis [46]. The choice between them is not a matter of which is universally better, but which is most appropriate for the specific research goals and constraints. CACR offers a more controlled, accessible, and cost-effective platform for standardized cognitive training. In contrast, VR provides unparalleled ecological validity and engagement, which may be crucial for translating gains into real-world function, albeit with higher technical and practical hurdles. Future research should include larger, well-powered RCTs that directly compare these modalities, standardize intervention protocols, and explore the nuanced role of immersion levels and gamification to optimize outcomes for stroke survivors.
Cognitive impairment is a common and debilitating consequence of stroke, affecting 30% to 70% of survivors and significantly hindering functional recovery and quality of life [14]. Within the broader context of cognitive rehabilitation techniques in stroke research, pharmacological adjuvants represent a promising approach to enhance neuroplasticity and accelerate recovery. These agents target specific neurochemical pathways disrupted by cerebral ischemia, offering the potential to modulate the brain's inherent recovery mechanisms. This comparative guide provides an objective analysis of three major pharmacological classes—cholinesterase inhibitors, antidepressants, and neuroprotective agents—evaluating their evidence base, efficacy, and practical application in post-stroke cognitive recovery. The assessment focuses on robust experimental data, detailed methodologies from key studies, and mechanistic insights to inform researchers, scientists, and drug development professionals in their therapeutic development efforts.
Comparative Efficacy Analysis of Pharmacological Adjuvants
Table 1: Comparative efficacy of pharmacological adjuvants for post-stroke cognitive recovery
| Pharmacological Class | Specific Agents | Evidence Base | Primary Cognitive Outcomes | Magnitude of Effect (vs. Control) | Timeframe of Benefit | Key Limitations |
|---|---|---|---|---|---|---|
| Cholinesterase Inhibitors | Donepezil, Rivastigmine, Galantamine | Meta-analysis of 7 studies [54] | MMSE, ADAS-Cog | MMSE: MD 1.52-3.00 points [54] | Benefits maintained over 24 weeks [54] | Not all patients respond; gastrointestinal side effects |
| Antidepressants | Sertraline, SSRIs | Systematic review of 22 studies [55] | Memory and learning, Processing speed | Memory/Learning: ES 0.25 (95% CI: 0.10-0.40) [55] | Short-term improvement demonstrated [55] | Cognition improvement may be secondary to mood effects |
| Neuroprotective Agents | Minocycline, Pioglitazone, Complement inhibitors | Multiple RCTs [56] | Various cognitive domains | Inconsistent across trials [56] | Variable | Repeated trial failures; timing and target engagement challenges |
Table 2: Practical application considerations for pharmacological adjuvants
| Parameter | Cholinesterase Inhibitors | Antidepressants | Neuroprotective Agents |
|---|---|---|---|
| Optimal Timing | Post-acute and chronic phases [54] | Early intervention post-stroke [57] | Acute phase (hours to days) [56] |
| Treatment Duration | At least 24 weeks [54] | Varies based on indication | Typically short-term in acute setting |
| Monitoring Parameters | MMSE, ADAS-Cog, GI side effects [54] | Depressive symptoms, cognitive tests [55] | Inflammatory biomarkers, cognitive measures |
| Combination Potential | With cognitive training, physical therapy [14] | With psychotherapy, other cognitive interventions [57] | With reperfusion therapies |
Cholinesterase Inhibitors: Evidence and Mechanisms
Experimental Evidence and Outcomes
Cholinesterase inhibitors (ChEIs)—including donepezil, rivastigmine, and galantamine—represent the most thoroughly investigated pharmacological class for post-stroke cognitive impairment. A 2020 meta-analysis of seven eligible studies provided compelling evidence for their efficacy, demonstrating consistent improvements in standardized cognitive assessment scores throughout a 24-week treatment period [54]. The Mini-Mental State Examination (MMSE) scores showed significant increases with mean differences of 3.000 at 4 weeks, 1.732 at 4-8 weeks, 1.578 at 8-12 weeks, 1.516 at 12-18 weeks, and 1.222 at 18-24 weeks following cholinergic augmentation [54]. Concurrently, Alzheimer's Disease Assessment Scale-Cognitive subscale (ADAS-Cog) scores decreased significantly at 6, 12, 18, and 24 weeks with pharmaceutical augmentation but not with placebo [54]. This stable pattern of improved cognitive function occurred without increased risk of side effects, supporting the favorable safety profile of ChEIs in this population.
Methodological Protocols
The referenced meta-analysis employed rigorous methodology, searching PubMed and MEDLINE databases for studies published prior to November 15, 2019, using the search string: 'Stroke' AND 'cholinesterase inhibitors' OR 'donepezil' OR 'rivastigmine' OR 'galantamine' [54]. Inclusion criteria encompassed: (1) human studies; (2) information on MMSE or ADAS-cog scores after cholinergic augmentation in patients with infarction or vascular dementia [54]. The researchers excluded case reports, non-original articles, and non-English language publications. Data extraction was performed by two independent authors, assessing paper reference, author details, publication year, study location, pharmaceutical regimen, patient demographics, cognitive scores, and complications [54]. Statistical analyses utilized Comprehensive Meta-Analysis software with random-effects models, accounting for heterogeneity between studies using Q and I2 statistics [54].
Figure 1: Mechanism of cholinesterase inhibitors in post-stroke cognitive recovery
Antidepressants: Cognitive Benefits Beyond Mood Improvement
Evidence for Cognitive Enhancement
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), demonstrate procognitive effects in post-stroke recovery that may extend beyond their mood-elevating properties. A 2024 systematic review and meta-analysis of 22 prospective studies specifically evaluated cognitive outcomes after antidepressant pharmacotherapy for late-life depression [55]. The findings revealed that 13 of 19 studies showed improvement on at least one cognitive test after antidepressant pharmacotherapy, with the most robust evidence emerging for the memory and learning domains (9 of 16 studies) and processing speed (7 of 10 studies) [55]. Sertraline demonstrated particularly consistent benefits, showing positive cognitive outcomes across all five studies investigating this agent [55]. The meta-analysis of eight studies (N=493) revealed a statistically significant overall improvement in memory and learning (effect size=0.25, 95% CI=0.10-0.40), though no statistically significant changes were observed in other cognitive domains [55].
Methodological Considerations
The association between antidepressant treatment and cognitive improvement presents methodological challenges, particularly in distinguishing direct cognitive benefits from secondary effects due to mood improvement. The systematic review addressed this relationship, finding that improvements in depressive symptoms were associated with improvement in cognitive test scores in six of seven relevant studies [55]. This correlation emphasizes the importance of effective treatment for post-stroke depression as a mechanism for cognitive enhancement. The research team employed comprehensive search strategies across MEDLINE, EMBASE, and PsycInfo through December 31, 2022, focusing on prospective studies of antidepressant pharmacotherapy for adults age 50 or older (or mean age of 65 or older) with late-life depression [55]. Participants with bipolar disorder, psychotic depression, dementia, or neurological disease were excluded to minimize confounding factors [55].
Neuroprotective Agents: Mechanisms and Trial Evidence
Diverse Mechanistic Approaches
Neuroprotective agents target the complex cascade of inflammatory and degenerative processes that occur following stroke. The complement system has emerged as a particularly attractive therapeutic target due to its pivotal role in promoting neuroinflammation and degeneration [56]. Complement activation after stroke results in microglia and astrocyte activation, reduced dendritic and synaptic density, and inhibition of neuroblast migration [56]. Other investigated mechanisms include peroxisome proliferator-activated receptor gamma (PPARγ) agonism with agents like pioglitazone, which may induce genes involved in oxidative stress defense, anti-inflammatory responses, and mitochondrial biogenesis [56]. Minocycline, a second-generation tetracycline antibiotic, exerts anti-inflammatory and neuroprotective properties through inhibitory effects on microglial activation [56].
Clinical Trial Evidence and Challenges
Despite promising preclinical data, clinical trials of neuroprotective agents have largely yielded disappointing results. Pexelizumab, a single-chain antibody fragment that inhibits C5 cleavage and generation of the membrane attack complex, was assessed in a phase II clinical trial with stroke as a complication of coronary artery bypass graft surgery [56]. The trial failed to meet primary endpoints, showing no significant improvement in cognition or neurological deficits, though some visuospatial improvement was noted [56]. Pioglitazone was evaluated in a clinical trial for acute stroke patients with hyperglycemia, but participant enrollment difficulties led to termination of the phase II trial [56]. Minocycline has demonstrated more promising results, showing good tolerability alone and in combination with tissue plasminogen activator in a Phase I/II trial, though optimal dosing requires further investigation due to insufficient recruitment in lower dose groups [56].
Figure 2: Neuroprotective agent mechanisms targeting post-stroke injury cascades
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and tools for investigating cognitive recovery mechanisms
| Research Tool | Application/Function | Experimental Context |
|---|---|---|
| MMSE (Mini-Mental State Examination) | Brief cognitive screening assessing multiple domains | Primary outcome in cholinesterase inhibitor trials [54] |
| ADAS-Cog (Alzheimer's Disease Assessment Scale-Cognitive) | Comprehensive cognitive assessment | Secondary outcome in vascular dementia trials [54] |
| MoCA (Montreal Cognitive Assessment) | Multi-domain cognitive screening | Primary outcome in recent RCTs for PSCI [14] |
| S100β Protein | Astrocyte damage biomarker | Correlated with injury severity and prognosis in TBI/stroke [58] |
| NSE (Neuron-Specific Enolase) | Neuronal injury biomarker | Monitors effectiveness of therapeutic interventions [58] |
| GFAP (Glial Fibrillary Acidic Protein) | Astrocyte injury biomarker | Brain-specific biomarker for CNS injury [58] |
| BDNF (Brain-Derived Neurotrophic Factor) | Neuroplasticity marker | Mediates exercise-induced cognitive benefits [59] |
The comparative evidence for pharmacological adjuvants in post-stroke cognitive recovery reveals distinct profiles for each therapeutic class. Cholinesterase inhibitors demonstrate the most consistent cognitive benefits across multiple domains, supported by meta-analysis evidence of improved MMSE and ADAS-Cog scores maintained over 24 weeks [54]. Antidepressants, particularly sertraline, show promise for specific cognitive domains like memory and learning, though their procognitive effects may be partially mediated by mood improvement [55] [57]. Neuroprotective agents face significant translational challenges despite compelling mechanistic rationale, with most clinical trials failing to demonstrate unequivocal benefits [56]. Optimal cognitive rehabilitation likely requires integrated approaches combining pharmacological adjuvants with non-pharmacological interventions like brain stimulation and physical activity, personalized according to individual patient characteristics, stroke pathophysiology, and timing post-stroke [14] [59]. Future research should address methodological limitations of past trials, including heterogeneous populations, suboptimal timing, and inadequate biomarker integration to advance the development of effective cognitive-enhancing therapies for stroke survivors.
Conventional cognitive rehabilitation (CR) represents a cornerstone of neurorehabilitation, focusing on the systematic retraining of specific cognitive domains impaired by neurological injury. Within the context of stroke research—where cognitive impairments affect 30-70% of survivors—domain-specific training targets core cognitive processes including attention, memory, and executive function through structured, repetitive exercises [14]. Unlike comprehensive approaches that address global cognitive functioning, domain-specific interventions are predicated on the principle of restitution, aiming to directly restore impaired neural networks through targeted stimulation [60].
The theoretical foundation for domain-specific rehabilitation lies in neuroplasticity—the brain's ability to reorganize itself by forming new neural connections throughout life. Following stroke, the brain undergoes spontaneous recovery processes, and domain-specific training is designed to capitalize on this inherent plasticity by providing focused stimulation to compromised networks [14]. Research indicates that cognitive impairment resulting from neurological damage can be reversed, at least partially, through appropriate training that reinforces neuroplasticity and regenerative capacity [61]. This systematic review objectively compares the efficacy of conventional domain-specific CR approaches against alternative interventions and establishes evidence-based protocols for implementation in research and clinical practice.
Comparative Efficacy of Domain-Specific Rehabilitation Approaches
Quantitative Comparisons Across Cognitive Domains
Table 1: Comparative Effectiveness of Domain-Specific Cognitive Rehabilitation Approaches in Stroke
| Cognitive Domain | Intervention Type | Comparative Efficacy (vs. Control) | Effect Size/Mean Difference | Key Outcome Measures |
|---|---|---|---|---|
| Global Cognition | Computerized Cognitive Training (CCT) | Significant improvement | SMD=0.46 (0.21-0.71) [62] | Standardized cognitive scales |
| Computer-Assisted Cognitive Therapy (CACT) | Superior efficacy | MD=3.03 (1.69-4.38) [63] | Montreal Cognitive Assessment (MoCA) | |
| Robot-Assisted Therapy (RAT) | Highest efficacy on basic cognition | MD=5.99 (3.20-8.79) [63] | Mini-Mental State Exam (MMSE) | |
| Attention | Computerized Cognitive Training (CCT) | Significant enhancement | SMD=-0.45 (-0.64 to -0.25) [62] | Attention-specific assessments |
| Executive Function | Computerized Cognitive Training (CCT) | Statistically significant improvement | SMD=0.39 (0.12-0.67) [62] | Executive function batteries |
| Computer-Assisted Cognitive Therapy (CACT) | Superior for executive-focused outcomes | Ranked highest (SUCRA=91.53%) [63] | MoCA (executive subcomponents) | |
| Memory | Computerized Cognitive Training (CCT) | Limited improvement | Low-quality evidence [62] | Memory tests |
| Conventional Domain-Specific Training | Variable outcomes | Inconsistent across studies [61] | BVMT, CVLT |
Table 2: Comparative Effectiveness Across Neurological Conditions
| Condition | Intervention | Effective Outcomes | Non-Significant Outcomes | Evidence Quality |
|---|---|---|---|---|
| Multiple Sclerosis | Cognitive Rehabilitation | PASAT, BVMT, MSNQ, BDI [64] | COWAT, CVLT, EMQ, SDMT, EDSS [65] | Moderate |
| Substance Use Disorder | Cognitive Training | Memory, Executive Function [61] | Processing Speed (variable) [61] | Moderate to Low |
| Cancer (CRCI) | Compensatory Strategy Training | Subjective Cognitive Function [66] | - | Moderate |
| Cognitive Training | Objective Cognitive Function [66] | - | Moderate |
Domain-specific cognitive rehabilitation demonstrates variable efficacy across cognitive domains and patient populations. In post-stroke cognitive impairment (PSCI), computerized cognitive training (CCT) shows significant, moderate effects on global cognition (SMD=0.46), attention (SMD=-0.45), and executive function (SMD=0.39) according to a 2025 meta-analysis of 19 trials [62]. More specialized digital interventions show domain-specific advantages: computer-assisted cognitive therapy (CACT) demonstrates superior efficacy on the MoCA, which emphasizes executive functioning, while robot-assisted therapy (RAT) shows highest efficacy on the MMSE, which focuses on basic cognition [63].
The temporal window for intervention significantly influences outcomes. Early initiation of domain-specific training (within 3 months post-stroke) produces more substantial benefits, likely due to enhanced neuroplasticity during the critical recovery period [14]. Training intensity and schedule also impact efficacy, with evidence suggesting that short-term, high-frequency training often surpasses long-term, low-frequency regimens for specific cognitive domains [62].
Across neurological conditions, domain-specific training shows condition-specific response patterns. In multiple sclerosis, cognitive rehabilitation significantly improves performance on the Paced Auditory Serial Addition Test (PASAT) and Brief Visuospatial Memory Test (BVMT), but shows inconsistent results for other measures like the Controlled Oral Word Association Test (COWAT) and California Verbal Learning Test (CVLT) [64] [65]. For substance use disorders, cognitive training demonstrates particular benefits for memory—one of the areas most affected by substance use—with moderate evidence supporting executive function improvements [61].
Experimental Protocols and Methodological Considerations
Standardized Protocols for Domain-Specific Training
Table 3: Domain-Specific Training Protocols for Post-Stroke Cognitive Rehabilitation
| Cognitive Domain | Training Paradigm | Session Structure | Progression Algorithm | Key Measures |
|---|---|---|---|---|
| Attention | Computerized attention tasks (selective, sustained, divided) | 30-45 minutes, 3-5×/week, 4-8 weeks | Adaptive difficulty based on performance | Test of Everyday Attention, Digit Span, SDMT |
| Memory | Working memory training (n-back, digit/spatial span) | 30-60 minutes, 3-5×/week, 4-10 weeks | Increasing span length, complexity | BVMT, CVLT, Working Memory Tests |
| Executive Function | Task-switching, inhibition, problem-solving tasks | 45-60 minutes, 3-5×/week, 6-12 weeks | Adaptive progression across multiple parameters | Trail Making Test, Stroop, Wisconsin Card Sort |
Domain-specific cognitive rehabilitation employs structured protocols with specific parameters to target impaired cognitive domains effectively. The typical computerized cognitive training program for attention and executive function follows an intensive schedule of 3-5 sessions weekly over 4-12 weeks, with each session lasting 30-60 minutes [60] [67] [62]. Effective protocols incorporate adaptive progression algorithms that automatically adjust task difficulty based on patient performance, maintaining an optimal challenge level and promoting continued improvement through principles of neuroplasticity [63] [62].
Working memory training, a predominant approach in domain-specific rehabilitation, typically employs tasks such as the n-back paradigm and digit/spatial span exercises [61]. These protocols are founded on the established association between working memory and fluid intelligence, with the theoretical premise that working memory training could lead to improvements in domain-general cognitive skills through "far-transfer" effects [61]. For executive functions, comprehensive training often incorporates a multifaceted approach targeting mental set shifting, information updating, and inhibition of prepotent responses through task-switching paradigms, Stroop-like inhibition tasks, and complex problem-solving activities [60].
Methodological quality varies substantially across cognitive rehabilitation studies. Higher-quality randomized controlled trials employ active control groups (receiving alternative but supposedly ineffective training) to account for non-specific effects of intervention, such as therapist attention and participant expectations [60]. Blinding of outcome assessors, precise description of outcome parameters, and adjustment for multiple statistical comparisons represent key methodological considerations that significantly influence study validity and the interpretation of domain-specific training effects [60].
Figure 1: Domain-Specific Cognitive Rehabilitation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Research Reagent Solutions for Cognitive Rehabilitation Studies
| Tool Category | Specific Examples | Primary Application | Key Characteristics |
|---|---|---|---|
| Assessment Tools | Montreal Cognitive Assessment (MoCA) | Global cognitive screening | Assesses attention, executive, memory, language, visuospatial [63] [14] |
| Mini-Mental State Exam (MMSE) | Basic cognitive screening | Focuses on orientation, memory, attention [63] | |
| Paced Auditory Serial Addition Test (PASAT) | Attention/working memory | Measures information processing speed [64] | |
| Brief Visuospatial Memory Test (BVMT) | Visual memory assessment | Evaluates visuospatial learning and recall [64] | |
| Digital Platforms | Computer-Assisted Cognitive Therapy (CACT) | Domain-specific training | Personalized, adaptive difficulty algorithms [63] |
| Robot-Assisted Therapy (RAT) | Motor-cognitive integration | Combines physical interaction with cognitive tasks [63] | |
| Virtual Reality (VR) Systems | Ecologically valid training | Immersive environments for functional tasks [63] | |
| Outcome Metrics | Symbol Digit Modalities Test (SDMT) | Processing speed | Visual scanning, tracking, motor speed [64] |
| Controlled Oral Word Association Test (COWAT) | Verbal fluency | Executive function, lexical access [64] | |
| California Verbal Learning Test (CVLT) | Verbal memory | Multi-trial learning, recall, recognition [64] |
The methodological rigor of cognitive rehabilitation research depends on standardized assessment tools and intervention platforms. The Montreal Cognitive Assessment (MoCA) serves as a primary outcome measure in contemporary stroke trials, particularly valued for its sensitivity to executive dysfunction and suitability for detecting post-stroke cognitive impairment [63] [14]. For domain-specific assessment, instruments such as the Paced Auditory Serial Addition Test (PASAT) for attention and working memory, the Brief Visuospatial Memory Test (BVMT) for visual memory, and the Controlled Oral Word Association Test (COWAT) for verbal fluency provide targeted cognitive domain measurement [64].
Digital rehabilitation platforms represent critical tools for implementing standardized domain-specific training. Computer-Assisted Cognitive Therapy (CACT) systems enable personalized training with dynamic difficulty adjustments based on real-time performance data, forming closed-loop cognitive reinforcement pathways [63]. These platforms typically incorporate multiple task types targeting specific cognitive domains while maintaining consistent performance monitoring and data collection capabilities essential for research applications. Virtual Reality (VR) systems provide ecologically valid training environments that integrate multisensory stimulation with task-oriented training, demonstrating particular utility for visuospatial and executive functions [63].
Figure 2: Intervention Approaches and Mechanisms in Cognitive Rehabilitation
Methodological implementation requires careful consideration of control conditions. Active control groups should engage participants in cognitively demanding activities that parallel the experimental intervention in time and attention, but without specifically targeting the cognitive domains of interest [60]. Common approaches include simple video games, computer activities with fixed difficulty levels, or educational programs. The standardization of control conditions remains challenging, with significant variability across studies contributing to heterogeneity in meta-analyses and complicating the interpretation of domain-specific treatment effects [60] [62].
Conventional domain-specific cognitive rehabilitation demonstrates significant, though variable, efficacy across cognitive domains and neurological populations. Current evidence indicates that attention and executive function show more consistent improvements following domain-specific training, while memory outcomes remain more variable. The comparative effectiveness of different approaches reveals that computer-assisted cognitive therapy shows particular promise for executive functions, while robot-assisted therapy may advantage basic cognitive processes.
Future research directions should address several critical gaps in the current evidence base. Larger, methodologically rigorous randomized controlled trials with active control conditions are needed to isolate specific treatment effects from non-specific factors [60] [62]. Standardization of intervention protocols and outcome measures across studies would enhance comparability and facilitate more definitive meta-analyses [67]. Investigation of individual difference factors—including stroke characteristics, baseline cognitive status, genetic markers, and neural reserve—may identify patient subgroups most likely to benefit from specific domain-specific approaches [14].
The integration of domain-specific cognitive training with other therapeutic modalities represents a promising frontier. Combined interventions, such as cognitive rehabilitation with repetitive transcranial magnetic stimulation (rTMS), demonstrate synergistic effects potentially superior to either approach alone [4] [14]. Similarly, the development of personalized protocols based on individual cognitive profiles, neural connectivity patterns, and specific functional goals may enhance the precision and effectiveness of domain-specific rehabilitation in stroke and other neurological populations.
The rehabilitation of neurological functions following stroke represents a significant challenge in clinical neuroscience, driving the exploration of innovative, multimodal treatment strategies. The core rationale for integrating transcranial direct current stimulation (tDCS) with cognitive training and physical rehabilitation rests upon a compelling neurophysiological foundation: tDCS can prime the brain for enhanced learning and plasticity, thereby potentiating the benefits of subsequent behavioral interventions [68] [69]. tDCS is a non-invasive brain stimulation technique that applies a weak, constant current to the scalp to modulate cortical excitability. The primary mechanism involves polarization of neuronal membranes, where anodal stimulation typically increases excitability through depolarization, and cathodal stimulation decreases excitability via hyperpolarization [68]. Beyond these immediate effects, tDCS can induce neuroplastic changes through glutamatergic synaptic mechanisms, influencing long-term potentiation (LTP) and depression (LTD)-like processes, which are fundamental to learning and memory consolidation [69] [70].
When combined with physical or cognitive training, tDCS is hypothesized to create a permissive environment for neuroplasticity, enhancing the encoding and retention of skills practiced during rehabilitation. This synergistic approach is particularly relevant in stroke recovery, where the goal is to facilitate functional reorganization in perilesional tissue and homologous contralesional areas [68] [71]. The portability of tDCS devices further enables concurrent application with rehabilitation exercises, potentially maximizing this synergistic effect by ensuring that neurophysiological modulation coincides precisely with skill acquisition [72]. The following sections will dissect the empirical evidence supporting this combined approach, detail specific protocols, and provide a comparative analysis of their efficacy across different functional domains.
Comparative Efficacy of Combined tDCS Interventions in Stroke Rehabilitation
Network meta-analyses and systematic reviews have provided substantial evidence that combining tDCS with other rehabilitation modalities yields superior outcomes compared to single-modality treatments. A major 2025 network meta-analysis of 74 randomized controlled trials (RCTs) encompassing 4,335 stroke patients provided high-quality evidence for the differential effectiveness of various tDCS-based combinations across specific motor and cognitive domains [73]. The findings, summarized in the table below, reveal that the optimal combination is highly dependent on the specific functional target.
Table 1: Optimal tDCS-Based Combinations for Different Functional Outcomes in Stroke Rehabilitation
| Functional Domain | Optimal tDCS Combination | Key Outcome Measure | Efficacy Ranking (SUCRA%) |
|---|---|---|---|
| Upper Limb Motor Ability | Brain-Computer Interface Therapy (BCIT) + tDCS | Fugl-Meyer Assessment for Upper Extremity (FMA-UE) | 88.34% [73] |
| Arm Movement Ability | Mirror Therapy (MT) + tDCS | Action Research Arm Test (ARAT) | 85.96% [73] |
| Lower Limb Motor Ability | Mirror Therapy (MT) + tDCS | Fugl-Meyer Assessment for Lower Extremity (FMA-LE) | 84.29% [73] |
| Balance | Acupuncture and Moxibustion (AM) + tDCS | Berg Balance Scale (BBS) | 77.16% [73] |
| Overall Upper Limb Function | tDCS + Occupational Therapy/Physical Therapy | FMA, ARAT | Moderate Effect (d=0.696) [71] |
| Cognition & ADL | tDCS + Cognitive Rehabilitation (CR) | MoCA, MMSE, ADL | Significant Improvement (p<0.05) [70] |
Another meta-analysis of 20 RCTs with 818 stroke patients confirmed the moderate overall effect size (0.480) of tDCS combined with rehabilitation for upper extremity function. It further highlighted that tDCS combined with occupational therapy/physical therapy or virtual reality therapy was particularly effective [71]. For post-stroke cognitive impairment (PSCI), a 2025 review of 11 RCTs (n=663) concluded that tDCS combined with cognitive rehabilitation significantly improved cognitive function and activities of daily living (ADL) compared to control interventions [70]. Subgroup analysis within this review suggested that tDCS combined with computer-assisted cognitive rehabilitation (CACR) had a more substantial positive impact on ADL than conventional approaches [70].
Detailed Experimental Protocols for Combined Interventions
The translation of these efficacy findings into practice requires strict adherence to validated protocols. The following section outlines specific methodologies from key studies.
Protocol for tDCS and Motor Rehabilitation
A typical protocol for combining tDCS with upper limb motor training, as used in several studies included in the meta-analyses, involves the following steps [73] [71]:
- tDCS Setup: The anodal electrode is placed over the primary motor cortex (M1) of the affected hemisphere (e.g., identified using the international 10-20 EEG system as C3 or C4). The cathodal electrode is placed over the contralateral supraorbital area. For bihemispheric stimulation, the anode is placed on the affected M1 and the cathode on the unaffected M1.
- Stimulation Parameters: A constant current of 1-2 mA is applied for 20-30 minutes. The current ramps up and down smoothly over 30-60 seconds at the beginning and end to minimize sensory discomfort.
- Concurrent Rehabilitation: The motor rehabilitation begins simultaneously with the tDCS. For example:
- With Mirror Therapy (MT): The patient places both arms on a table with a mirror positioned vertically between them. The unaffected limb performs repetitive, task-oriented movements while the patient watches its reflection in the mirror, creating the visual illusion that the affected limb is moving normally [73].
- With Occupational/Physical Therapy: The patient engages in tailored, functional tasks focusing on the paretic upper limb, such as grasping objects, reaching, or manipulating utensils [71].
- With Brain-Computer Interface Therapy (BCIT): The patient is tasked with generating motor imagery of moving the affected limb. The BCI system detects associated brain signals (e.g., from EEG) and translates them into control signals for a virtual or physical device, providing immediate feedback [73].
- Session Frequency: Sessions are typically conducted 3-5 times per week for 2-8 weeks.
Protocol for tDCS and Cognitive Rehabilitation
For patients with post-stroke cognitive impairment, a common protocol for combined intervention is as follows [74] [70]:
- tDCS Setup: The anodal electrode is most commonly placed over the left dorsolateral prefrontal cortex (DLPFC), corresponding to the F3 position in the 10-20 EEG system. The cathode is often placed over the right supraorbital area or the contralateral DLPFC (F4).
- Stimulation Parameters: A current intensity of 2 mA is applied for 20-30 minutes per session.
- Concurrent Cognitive Training: Computerized or therapist-led cognitive exercises are performed during stimulation. These tasks are designed to target specific cognitive domains such as:
- Attention/Vigilance: Continuous performance tasks, visual tracking.
- Working Memory: N-back tasks, digit span exercises.
- Executive Function: Task-switching paradigms, problem-solving tasks.
- Memory: Recall and recognition exercises for verbal and visual information.
- Session Frequency: Protocols vary from 10 to 28 sessions, administered over 2 to 12 weeks.
The following diagram illustrates the neurophysiological rationale and workflow for these combined protocols.
The Scientist's Toolkit: Essential Reagents and Materials
Successfully implementing a combined tDCS and rehabilitation research protocol requires specific equipment and materials. The following table details the key components of the experimental toolkit.
Table 2: Essential Research Materials for Combined tDCS and Rehabilitation Studies
| Item Category | Specific Examples & Specifications | Primary Function in Research |
|---|---|---|
| tDCS Device | Programmable, medical-grade stimulator with sham capability (e.g., DC-Stimulator PLUS, NeuroConn). | Delivers controlled, low-intensity direct current; sham mode enables blinding for RCTs. |
| Electrodes | Conductive rubber or saline-soaked sponge electrodes (typical size 25-35 cm²). | Interface for delivering current from stimulator to the scalp; larger sizes reduce current density. |
| Electrode Placement | International 10-20 EEG System cap or manual measurement tools. | Ensures accurate and reproducible positioning of electrodes over target cortical areas (e.g., M1, DLPFC). |
| Cognitive Training | Computerized cognitive training batteries (e.g., PARADIM, BrainHQ) or standardized therapist-guided materials. | Provides structured, repeatable tasks to engage specific cognitive domains (attention, memory, executive function). |
| Motor Training | Mirror boxes, robotic-assisted devices (e.g., MIT-Manus), pegboards, standard objects for activities of daily living (ADL). | Provides standardized, repetitive, and task-oriented physical exercises for the affected limbs. |
| Outcome Measures | Motor: Fugl-Meyer Assessment (FMA), Action Research Arm Test (ARAT).Cognitive: Montreal Cognitive Assessment (MoCA), Mini-Mental State Exam (MMSE).ADL: Barthel Index, Functional Independence Measure (FIM). | Validated, standardized tools to quantitatively assess primary and secondary outcomes pre- and post-intervention. |
The evidence from recent high-quality meta-analyses strongly supports the superior efficacy of combining tDCS with targeted behavioral rehabilitation over either approach alone for stroke recovery. The effects are domain-specific, with optimal pairings such as BCIT+tDCS for upper limb motor function and tDCS with computer-assisted cognitive rehabilitation for cognition and daily living activities. The underlying mechanism is a synergistic interaction where tDCS primes the brain for plasticity, thereby enhancing the encoding and consolidation of skills learned during concurrent training.
Future research should focus on refining these protocols by determining optimal stimulation parameters (e.g., current intensity, duration, session count), exploring the effects of targeting novel brain regions like the front-polar area [69], and identifying patient-specific factors that predict treatment response. The continued integration of technology, such as virtual reality and advanced brain-computer interfaces, with neuromodulation holds significant promise for creating more immersive and effective personalized rehabilitation strategies for stroke survivors.
Addressing Heterogeneity and Optimizing Rehabilitation Protocols for Enhanced Efficacy
In the field of stroke rehabilitation, two fundamental questions guide clinical research and practice: "When should intervention begin?" and "How much therapy is required?" The answers to these questions are not monolithic but vary significantly across different rehabilitation modalities. The timing of intervention post-stroke and the dosage parameters of therapy represent critical variables that directly influence neuroplasticity, functional recovery, and ultimate patient outcomes. Understanding these relationships is essential for researchers designing clinical trials, clinicians optimizing treatment protocols, and drug development professionals seeking to contextualize adjunctive rehabilitation strategies.
This comparative analysis synthesizes current evidence on critical periods for intervention and dose-response relationships across major rehabilitation modalities, including brain stimulation techniques, technology-assisted interventions, and pharmacological approaches. By examining quantitative data on optimal timing and dosing parameters, we provide a framework for maximizing therapeutic efficacy in stroke cognitive rehabilitation.
Comparative Effectiveness of Rehabilitation Modalities: Timing and Dosage
Table 1: Comparative Effectiveness of Interventions by Time Post-Stroke
| Intervention Modality | Acute/Subacute Phase Effect | Chronic Phase Effect | Optimal Timing | Key Evidence |
|---|---|---|---|---|
| Upper Extremity Rehabilitation | Greater magnitude improvements in FMA-UE scores [75] | Reduced effectiveness compared to early intervention [75] | Acute/Subacute phase | Meta-analysis of 157 RCTs [75] |
| Brain Stimulation (tDCS) | Most effective when initiated early [14] | Benefits observed but reduced compared to early initiation [14] | Within 3 months post-stroke | Systematic review of 22 RCTs [14] |
| Pharmacological Interventions | Robust effects when delivered early [14] | Effective but with potential for reduced benefit | Early in recovery phase | Systematic review of 5,100 participants [14] |
| Computerized Cognitive Training (CCT) | Supported by principles of neuroplasticity [14] | Effective but may require higher dosage | Early intervention recommended | Dose-response study [76] |
| Virtual Reality Rehabilitation | Applicable in subacute phase [77] | Research focuses on chronic phase applications | Subacute phase (≤2 weeks) [77] | Pilot study on patient satisfaction [77] |
Table 2: Dose-Response Relationships Across Rehabilitation Modalities
| Intervention Modality | Optimal Daily Dose | Optimal Frequency | Cumulative Dose Considerations | Population-Specific Considerations |
|---|---|---|---|---|
| Computerized Cognitive Training (Age <60) | 25 to <30 minutes [76] | 6 days/week [76] | Weekly progression based on performance | Higher doses do not yield additional benefits [76] |
| Computerized Cognitive Training (Age ≥60) | 50 to <55 minutes [76] | 6 days/week [76] | Requires nearly double the younger population dose | Age-dependent dose response [76] |
| Virtual Reality Rehabilitation | 10-20 minutes/session [77] | Variable based on clinical status | Total sessions correlated with hospital stay length [77] | Dose often confounded by clinical severity [77] |
| Brain Stimulation (rTMS combined with CR) | Protocol-dependent | Protocol-dependent | Combined with cognitive rehabilitation shows superiority | Most effective for cognitive function [4] |
| Occupational Therapy (ADL Training) | Intensive daily training recommended [78] | Throughout inpatient stay | Early rehabilitation linked to improved functional recovery [78] | Time-sensitive neuroplasticity [78] |
Experimental Protocols and Methodological Approaches
Protocol for Dose-Response Studies in Computerized Cognitive Training
The establishment of dose-response relationships in computerized cognitive training (CCT) requires rigorous methodological approaches. A recent retrospective cohort study analyzed 8,709 participants with cognitive impairment (subjective cognitive decline, mild cognitive impairment, and mild dementia) to investigate the association between training dose and cognitive improvement [76].
Methodology Overview:
- Participants: Adults with cognitive impairment stratified by age (<60 vs ≥60 years) and diagnosis
- Intervention: Self-adapted computerized cognitive training with varying daily doses (5-60+ minutes) and frequencies (1-7 days/week)
- Outcome Measure: Weekly changes in Cognitive Index (WCCI) - a composite measure of cognitive performance
- Statistical Analysis: Mixed-effects models to account within-participant correlations and control for confounding variables
- Dose Parameters: Daily training duration (minutes) and weekly frequency (days) as primary exposure variables
This large-scale analysis demonstrated that CCT exhibits a clear dose-dependent effect on cognitive improvement, with optimal dosing parameters differing significantly by age group. The study highlighted that exceeding optimal doses does not yield additional cognitive benefits and may even diminish returns, indicating a non-linear dose-response relationship [76].
Protocol for Timing Studies in Upper Extremity Rehabilitation
A comprehensive meta-analysis examined the impact of timing on upper extremity motor recovery, providing methodological insights for studying critical periods in stroke rehabilitation [75].
Methodology Overview:
- Study Selection: 157 randomized controlled trials of upper extremity rehabilitation interventions
- Comparison Framework: Interventions compared at different time points post-stroke (acute/subacute vs. chronic)
- Primary Outcome: Fugl-Meyer Assessment Upper Extremity (FMA-UE) score changes
- Intervention Categories: 17 distinct types of rehabilitation approaches
- Analysis Approach: Direct comparison of effect sizes between early and late intervention periods
This methodological approach demonstrated that interventions studied in the acute and subacute phases showed greater magnitude improvements in FMA-UE scores compared to the chronic phase, highlighting the importance of timing in motor recovery research [75].
Signaling Pathways and Neurobiological Mechanisms
The effectiveness of rehabilitation interventions is fundamentally governed by neurobiological mechanisms that are time-sensitive and dose-dependent. The following diagram illustrates the conceptual pathway through which timing and dosage parameters influence neuroplasticity and functional outcomes in stroke recovery.
Conceptual Pathway of Timing and Dosage Effects in Stroke Recovery
This conceptual model illustrates how timing and dosage parameters influence specific neuroplasticity mechanisms that ultimately drive functional recovery. Early intervention capitalizes on enhanced neuroplasticity in the acute and subacute phases, while adequate dosing ensures optimal activation of these mechanisms without inducing cognitive fatigue that can occur with excessive training volumes [14] [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Assessment Tools and Research Materials for Stroke Rehabilitation Studies
| Tool/Material | Primary Function | Application Context | Key Characteristics |
|---|---|---|---|
| Fugl-Meyer Assessment Upper Extremity (FMA-UE) | Quantitative measure of motor recovery [75] | Upper extremity rehabilitation trials | Sensitive to timing effects; shows greater improvements in acute/subacute phase [75] |
| Montreal Cognitive Assessment (MoCA) | Cognitive screening and monitoring [14] | Cognitive rehabilitation studies | Assesses multiple domains; sensitive to intervention effects; used as primary outcome [14] |
| User Satisfaction Evaluation Questionnaire (USEQ) | Measures patient acceptance and satisfaction [77] | Technology-assisted rehabilitation (e.g., VR) | Assesses enjoyment, perceived benefit, comfort; important for adherence [77] |
| Computerized Cognitive Training Platforms | Digital delivery of cognitive exercises [76] | Dose-response studies | Enables precise dose measurement; adaptable difficulty; performance tracking [76] |
| Virtual Reality Rehabilitation Systems | Immersive, ecologically valid training environments [77] | Motor and cognitive rehabilitation | Provides engaging therapy; enables precise movement quantification; enhances adherence [77] [79] |
| Transcranial Magnetic Stimulation (rTMS) | Non-invasive brain stimulation [4] | Modulation of cortical excitability | Often combined with cognitive training; enhances neuroplasticity [4] |
| Standardized ADL Assessments | Measures functional independence [78] | Occupational therapy research | Evaluates real-world functional impact; includes both basic and instrumental ADLs [78] |
The evidence synthesized in this comparative guide demonstrates that timing and dosage parameters are not secondary considerations but fundamental determinants of efficacy in stroke rehabilitation. The critical period for intervention consistently emerges within the first three months post-stroke, when neuroplasticity mechanisms are most responsive to targeted therapies [75] [14]. During this window, interventions ranging from brain stimulation to cognitive training demonstrate significantly enhanced effects compared to later initiation.
Dose-response relationships follow non-linear patterns with identifiable optimal dosing parameters that vary by modality, patient age, and specific impairment targets [76]. The principle of "more is better" has clear limitations, with excessive dosing potentially leading to cognitive fatigue and diminished returns. Future research should continue to refine these parameters through rigorously designed dose-finding studies and explore how timing and dosage interact with individual patient characteristics to enable truly personalized neurorehabilitation approaches.
For researchers and drug development professionals, these findings highlight the importance of carefully considering timing and dosage parameters in clinical trial design and when evaluating the comparative effectiveness of different rehabilitation modalities. The optimization of these critical parameters represents a promising pathway for enhancing the efficacy of stroke rehabilitation and improving long-term patient outcomes.
Stroke remains a leading cause of mortality and long-term disability globally, affecting approximately 15 million people annually [14]. Despite advancements in acute care, cognitive impairments persist in 30-70% of survivors, significantly impacting functional independence and quality of life [14]. Traditional rehabilitation approaches have often employed a "one-size-fits-all" methodology, yielding limited efficacy due to the substantial heterogeneity in stroke presentation, cognitive phenotypes, and recovery trajectories observed across patients. This recognition has catalyzed a paradigm shift toward precision medicine, which utilizes individual patient characteristics—including detailed cognitive profiles, specific stroke features, and molecular, neurophysiological, and neuroimaging biomarkers—to guide intervention selection [80] [81]. The objective of this comparative guide is to synthesize current evidence on personalized cognitive rehabilitation strategies, providing researchers and clinicians with a structured framework for matching interventions to individual patient profiles for optimized outcomes.
Comparative Efficacy of Rehabilitation Interventions
A comprehensive understanding of the relative effectiveness of available interventions is foundational to personalization. Recent high-quality meta-analyses provide robust quantitative data for comparing therapeutic approaches. The table below summarizes the cognitive improvements associated with various intervention classes, as measured by the Montreal Cognitive Assessment (MoCA), a standard cognitive screening tool.
Table 1: Comparative Efficacy of Cognitive Rehabilitation Interventions for Post-Stroke Cognitive Impairment
| Intervention Category | Specific Intervention | Mean Difference in MoCA Score (95% CI) | Key Characteristics |
|---|---|---|---|
| Brain Stimulation | Transcranial Direct Current Stimulation (tDCS) | 4.56 (3.19 to 5.93) [14] | Non-invasive neuromodulation; enhances neuroplasticity |
| Pharmacological | Various Medications | 4.00 (3.48 to 4.52) [14] | Robust, generalizable effects; requires monitoring |
| Digital Therapy | Computer-Assisted Cognitive Therapy (CACT) | 3.03 (1.69 to 4.38) [63] | Personalized, adaptive training; emphasizes executive function |
| Brain Stimulation | rTMS + Cognitive Rehabilitation (CR) | SMD 1.07 (0.60 to 1.54) [4] | Combined approach targeting network reorganization |
| Alternative Medicine | Acupuncture | 2.65 (1.07 to 4.23) [14] | Potential benefit but requires standardization |
| Digital Therapy | Virtual Reality (VR) | MD 1.34 (-0.94 to 3.62) [63] | Immersive, ecologically valid environments |
| Training Approaches | Cognitive Training (CCT) | 0.70 (-0.88 to 2.28) [63] | Mixed outcomes; may be more effective when integrated |
The data reveals a clear efficacy gradient, with brain stimulation techniques like tDCS and pharmacological interventions demonstrating the most substantial benefits in global cognitive function [14]. Notably, combined approaches, such as repetitive Transcranial Magnetic Stimulation (rTMS) integrated with cognitive rehabilitation, show superior outcomes, emphasizing the utility of multimodal strategies [4]. Furthermore, digital interventions like CACT show domain-specific promise, particularly for executive functions assessed by the MoCA [63].
Experimental Protocols and Methodologies
Implementing and researching these interventions requires rigorous, standardized protocols. Below are detailed methodologies for key therapeutic approaches cited in the comparative data.
Protocol for Transcranial Direct Current Stimulation (tDCS)
- Objective: To enhance cortical excitability and promote neuroplasticity in cognitive networks.
- Equipment: A tDCS device with a constant current stimulator, surface saline-soaked sponge electrodes (typically 25-35 cm²), and an adjustable head strap.
- Parameter Setting: The anode is typically placed over the dorsolateral prefrontal cortex (DLPFC), a key node in executive networks, based on the 10-20 EEG system. The cathode can be placed on the contralateral supraorbital region. A constant current of 1-2 mA is applied for 20-30 minutes per session [14].
- Session Frequency: Administered daily or on alternate days for 2-4 weeks, often concurrently with cognitive training to leverage the enhanced plasticity state.
- Outcome Measures: Primary: MoCA score. Secondary: Domain-specific tests for memory (e.g., Rey Auditory Verbal Learning Test), attention (e.g., Trail Making Test A), and executive function (e.g., Trail Making Test B, Stroop Test).
Protocol for Computer-Assisted Cognitive Therapy (CACT)
- Objective: To provide adaptive, personalized cognitive training across multiple domains.
- Platform: A computer or tablet with specialized software capable of task presentation, performance recording, and automatic difficulty adjustment based on algorithmic rules.
- Training Modules: Sessions typically include exercises targeting:
- Attention: Sustained and selective attention tasks with distracting stimuli.
- Memory: Working and episodic memory tasks involving recall of sequences or information.
- Executive Function: Problem-solving, planning, and cognitive flexibility tasks.
- Training Regimen: Sessions last 30-60 minutes, conducted 3-5 times per week for 6-8 weeks. The difficulty level progresses adaptively, maintaining a success rate of ~80% to ensure engagement without frustration [63].
- Outcome Measures: MoCA, MMSE, and computerized performance metrics from the platform itself (e.g., reaction time, accuracy).
Protocol for rTMS Combined with Cognitive Rehabilitation
- Objective: To prime the brain for enhanced learning by stimulating key networks immediately before cognitive training.
- Equipment: A magnetic stimulator with a figure-of-eight coil for focal stimulation.
- Parameter Setting: High-frequency (e.g., 10 Hz) rTMS is applied to the ipsilesional DLPFC to facilitate excitability. A common protocol involves 10-20 trains of 50 pulses each, with an inter-train interval of 20-30 seconds [4].
- Combined Intervention: Within 30 minutes of completing the rTMS session, patients engage in a structured cognitive rehabilitation (CR) session. This CR is often a multi-modality intervention targeting orientation, perceptual abilities, attention, memory, and executive function [4].
- Session Frequency: Daily sessions, 5 days a week, for a period of 2-3 weeks.
- Outcome Measures: MoCA, MMSE, and specific assessments for mood (e.g., Hamilton Depression Scale) and quality of life (e.g., Stroke-Specific Quality of Life Scale) [4].
The Personalization Toolkit: Biomarkers and Patient Stratification
Precision rehabilitation relies on diagnostic tools and biomarkers to characterize the individual's unique profile and predict treatment response. The following diagram illustrates the decision-making pathway for personalizing interventions based on a multi-modal assessment.
Diagram 1: A workflow for personalizing cognitive rehabilitation strategies based on a multi-modal assessment of the patient's unique biomarkers and cognitive phenotype. The pathway begins with assessment, leads to a personalized profile, and culminates in matching the patient to the intervention with the highest predicted efficacy. DTI: Diffusion Tensor Imaging; TMS: Transcranial Magnetic Stimulation; CST: Corticospinal Tract; COMT: Catechol-O-Methyltransferase; CACT: Computer-Assisted Cognitive Therapy; tDCS: transcranial Direct Current Stimulation; rTMS: repetitive Transcranial Magnetic Stimulation.
The biomarkers used in this stratification toolkit can be categorized as follows:
Table 2: Key Biomarkers for Personalizing Stroke Cognitive Rehabilitation
| Biomarker Category | Specific Example | Function in Personalization | Research/Clinical Utility |
|---|---|---|---|
| Neuroimaging | Diffusion Tensor Imaging (DTI) | Assesses structural integrity of white matter tracts (e.g., corticospinal tract). Predicts motor recovery potential and response to therapy [82]. | Identifies patients needing augmented therapy (e.g., with brain stimulation) [82]. |
| Neurophysiology | Transcranial Magnetic Stimulation (TMS) | Measures functional integrity of the corticospinal tract. A combined model with clinical assessment can predict upper limb recovery with ~88% accuracy [82]. | Critical for prognostication and selecting patients for neuromodulation. |
| Cognitive Phenotype | MoCA Domain Scores | Profiles strengths/deficits across attention, memory, language, visuospatial, and executive domains [83]. | Guides selection of domain-specific training (e.g., reminiscence for memory [84], CACT for executive function [63]). |
| Molecular/Genetic | COMT Polymorphism | Genetic variation affecting dopamine metabolism. May influence response to tDCS for conditions like post-stroke dysphagia [81]. | Emerging tool for selecting patients most likely to respond to specific neuromodulation therapies. |
| Inflammatory | Cytokine Levels (e.g., IL-1b, IL-6, CXCL10) | Levels of specific cytokines post-stroke are associated with cognitive impairment severity and may inform on underlying pathophysiology [83]. | Potential for future targeting of anti-inflammatory therapies; requires further validation. |
Implementation Framework and Future Directions
Translating these personalized strategies into clinical practice and research protocols requires a structured framework. The following diagram maps the interplay between key components in a precision rehabilitation model.
Diagram 2: The cycle of precision medicine in stroke rehabilitation, powered by Artificial Intelligence/Machine Learning (AI/ML). Multi-modal data is integrated to create a patient profile, which informs predictions and guides the selection of a tailored intervention. The outcomes then feed back to refine the predictive models continuously.
Future efforts must focus on validating and integrating these components. Key directions include the standardization of digital therapy protocols and biomarker measurements, the application of advanced AI/ML models to complex datasets for improved prediction [80] [85], and the design of large-scale clinical trials that test stratified interventions against standard care. By systematically implementing this personalized framework, the field can move beyond population averages to deliver targeted, effective rehabilitation that addresses the unique needs of each stroke survivor.
Stroke rehabilitation represents a critical long-term process where patient adherence to prescribed exercises and behavioral recommendations directly functional recovery and quality of life. Despite recognized benefits, non-adherence rates to home-based rehabilitation programs remain alarmingly high, with studies indicating that up to 65-70% of patients are nonadherent or only partially adherent to their prescribed regimens [86]. This adherence challenge transcends simple non-compliance and encompasses complex behavioral mechanisms that must be systematically addressed through evidence-based approaches. Within the broader context of comparative cognitive rehabilitation techniques, understanding and applying Behavior Change Techniques (BCTs) becomes paramount for developing effective interventions.
The socioeconomic impact of poor adherence is substantial, affecting not only patients and their families but also healthcare systems globally [86]. Stroke patients experience both physical disabilities and psychological changes, including emotional, behavioral, and cognitive impairments that further complicate adherence [86]. These issues—including depression, apathy, anxiety, and posttraumatic stress—create significant barriers to rehabilitation by negatively impacting long-term exercise adherence and diminishing recovery potential [86]. This review examines the application of BCTs specifically within stroke rehabilitation contexts, comparing their relative effectiveness and providing methodological guidance for implementation in both research and clinical settings.
Methodological Framework: Identifying and Evaluating BCTs
Taxonomy and Classification Systems
The scientific evaluation of BCT efficacy relies on standardized taxonomies and classification systems that enable consistent implementation and comparison across studies. One of the most widely accepted frameworks is the BCT Taxonomy v1 (BCTTv1), which organizes techniques into 16 clusters encompassing 93 individual BCTs [86]. This taxonomy provides the foundational language for describing, evaluating, and comparing intervention components across different rehabilitation contexts. Research indicates that interventions utilizing this standardized approach demonstrate improved operationalization of psychological theory, enabling clearer understanding of which specific components drive behavioral changes [87].
Systematic reviews in this domain typically employ rigorous methodological standards, including PRISMA guidelines and quality assessment frameworks for randomized controlled trials [87]. The Template for Intervention Description and Replication (TIDieR) checklist has emerged as a critical tool for capturing intervention details, including categories such as "brief name," "why," "what materials," "what procedures," "who provided," "how," "where," "when and how much," "tailoring," and "how well" implemented [87]. This standardization addresses historical challenges in comparing interventions due to variable reporting quality and insufficient methodological details.
Experimental Designs for BCT Evaluation
Robust experimental designs are essential for establishing causal relationships between specific BCTs and adherence outcomes. Randomized controlled trials (RCTs) with follow-up periods of at least three months represent the gold standard for evaluating long-term effectiveness [87]. These studies typically employ both objective measures (e.g., accelerometers, wearable sensors) and subjective measures (e.g., self-reported questionnaires, adherence diaries) to capture the multidimensional nature of adherence behavior.
Recent methodological advances include 2-round Delphi surveys that establish expert consensus on BCT prioritization. This approach statistically aggregates responses from international experts across multiple relevant backgrounds (behavioral science, behavioral design, and healthcare professionals) to evaluate interquartile ranges and percentage consensus [86] [88]. Techniques reaching consensus (typically IQR ≤1 and percentage ≥50%) are then ranked according to their perceived importance for specific rehabilitation contexts, providing valuable guidance for intervention development.
Table 1: Key Methodological Approaches in BCT Research
| Method Type | Primary Purpose | Key Outputs | Limitations |
|---|---|---|---|
| Systematic Review with BCT Coding | Identify promising BCTs across multiple studies | Promise ratios for individual BCTs; Effectiveness comparisons | Heterogeneous studies; Variable quality of intervention descriptions |
| Delphi Expert Consensus | Establish prioritized BCT clusters for specific contexts | Ranked BCT clusters; Specialized recommendations for different rehabilitation aspects | Limited by expert perspective; May not reflect real-world effectiveness |
| Randomized Controlled Trials | Establish causal efficacy of specific BCTs | Within-group and between-group differences in adherence outcomes | Resource-intensive; Often limited follow-up duration |
| Cross-sectional Studies | Identify factors correlated with adherence | Correlates of adherence; Demographic and psychological associations | Cannot establish causality; Snapshot in time |
Comparative Effectiveness of BCT Clusters in Stroke Rehabilitation
Prioritization of BCT Clusters
Recent expert consensus studies have provided nuanced understanding of how different BCT clusters should be prioritized for stroke rehabilitation. A 2025 Delphi survey involving 12 international experts established clear rankings for BCT clusters across different rehabilitation domains [86] [88]. The findings demonstrated that 12 of 16 BCT clusters reached consensus for general importance in stroke rehabilitation, with varying relevance across behavioral (11 clusters), cognitive (9 clusters), and emotional (6 clusters) aspects of recovery [86].
The overall most relevant BCT clusters identified were:
- Repetition and substitution - practicing target behaviors and replacing unhealthy behaviors
- Social support - enabling practical or emotional support from others
- Feedback and monitoring - providing information about performance and outcomes
- Self-belief - enhancing confidence in capabilities [86] [88]
For emotional rehabilitation specifically, social support and identity (associating with a new self-image) emerged as particularly emphasized clusters [86]. The least relevant BCT clusters across domains were natural consequences, covert learning, and comparison of behavior [86].
Table 2: Expert-Ranked BCT Clusters for Stroke Rehabilitation (2025 Delphi Study)
| BCT Cluster | General Rehabilitation | Behavioral Aspect | Cognitive Aspect | Emotional Aspect |
|---|---|---|---|---|
| Repetition and Substitution | Highest relevance | Highest relevance | Highest relevance | Moderate relevance |
| Social Support | Highest relevance | Highest relevance | Highest relevance | Highest relevance |
| Feedback and Monitoring | High relevance | High relevance | High relevance | Moderate relevance |
| Self-belief | High relevance | High relevance | High relevance | Not prioritized |
| Goals and Planning | Moderate relevance | Moderate relevance | Moderate relevance | Not prioritized |
| Identity | Moderate relevance | Not prioritized | Not prioritized | Highest relevance |
Promising BCTs for Physical Activity Engagement
Systematic reviews focusing specifically on physical activity after stroke have identified nine particularly promising BCTs with promise ratios ≥2 [87]. These techniques demonstrated significant associations with improved adherence outcomes in intervention studies:
- Information about health consequences - providing information about health benefits of physical activity
- Information about social and environmental consequences - highlighting social and environmental benefits
- Goal setting (behavior) - agreeing on specific behavioral targets
- Problem-solving - analyzing factors influencing adherence and generating solutions
- Action planning - detailing when, where, and how behaviors will be performed
- Feedback on behavior - providing data about recorded behavior
- Biofeedback - providing physiological data to influence behavior
- Social support (unspecified) - general support from others
- Credible source - invoking authoritative figures or institutions [87]
These BCTs were most effectively delivered through face-to-face and telephone-based self-management programs, though optimal intensity of contact, interventionist type, and timing after stroke remained unclear across studies [87].
Implementation Considerations and Contextual Factors
Barriers and Facilitators of Adherence
Understanding the contextual factors that influence adherence is essential for effectively implementing BCTs. Qualitative research with healthcare professionals has identified multi-level factors affecting rehabilitation adherence [89]. At the patient level, key determinants include rehabilitation expectations, self-efficacy, economic pressure, family support, and trust in healthcare providers [89]. A cross-sectional study of 227 acute stroke patients further identified that subjective well-being positively correlated with adherence, while advanced age, ICU stays, and higher NIHSS scores negatively impacted adherence [90].
At the system level, barriers include limited access to tele-rehabilitation, insufficient tele-medical resources, and inadequate coordination between hospital and community services [89]. For technology-supported interventions specifically, key facilitators include ease of use, personalized content, motivational feedback, and social support, while major barriers encompass low digital literacy, repetitive content, and lack of guidance [91].
Technology-Assisted Delivery of BCTs
Technology platforms provide promising channels for delivering BCTs at scale, though they introduce unique considerations. Research indicates that self-monitoring, goal setting, action planning, feedback, prompts/cues, and social support represent the most frequently used BCTs in digital interventions [91]. However, the effectiveness of these techniques depends on both adherence to the physical activity component and adherence to the technology itself, creating a dual challenge for intervention designers.
The distinction between technology adherence and PA adherence is critical, as different psychological factors influence each domain. User factors affecting technology adherence include attitudes, expectations, and knowledge about technology; perceived social impact; and personal attributes like motivation and self-efficacy [91]. These factors must be addressed alongside traditional barriers to physical activity to create effective technology-supported interventions.
Integrated Approaches and Combined Interventions
Multimodal Rehabilitation Strategies
The most effective approaches to enhancing adherence often combine BCTs with other rehabilitation modalities. A 2025 network meta-analysis of 21 randomized controlled trials (N=1,074 patients) evaluated the effectiveness of combining repetitive transcranial magnetic stimulation (rTMS) with various rehabilitation methods [36]. The findings demonstrated that:
- Speech rehabilitation (SR) combined with rTMS was most effective for improving cognitive function (SMD=0.40; 95% CI, -0.08 to 0.87; SUCRA=95.1%)
- Cognitive rehabilitation (CR) combined with rTMS was superior for reducing negative mood (SMD=0.91; 95% CI, 0.45-3.23; SUCRA=84.5%) and improving quality of life (SMD=0.49; 95% CI, -0.33 to 1.30; SUCRA=99.4%) [36]
These findings suggest that prioritizing combined interventions can address multiple rehabilitation domains simultaneously, with BCTs potentially enhancing adherence to both the behavioral and technological components of these integrated approaches.
Tailoring to Individual Characteristics
Effective BCT implementation requires consideration of individual patient characteristics and preferences. Research indicates that tailored counseling approaches lead to improved long-term physical activity outcomes after stroke, though the specific effective components have not been consistently defined using standardized taxonomies [87]. Key individual factors influencing response to BCTs include:
- Stage of recovery - different BCT clusters show varying relevance across acute, subacute, and chronic phases
- Cognitive status - determines capacity for techniques requiring higher cognitive load
- Psychological characteristics - depression, anxiety, and self-efficacy influence technique responsiveness
- Social context - availability of social support affects selection of appropriate BCTs
- Technological proficiency - digital literacy impacts suitability of technology-delivered BCTs
Future research should establish stroke survivor preferences for mode of delivery, setting and intensity, while exploring optimal combinations of promising BCTs within individualized interventions [87].
Research Reagents and Methodological Tools
Table 3: Essential Research Tools for BCT Studies in Stroke Rehabilitation
| Tool Category | Specific Instrument | Primary Application | Key Features/Properties |
|---|---|---|---|
| BCT Taxonomies | BCT Taxonomy v1 (BCTTv1) | Standardized coding of intervention components | 16 clusters, 93 individual techniques; Common language for description |
| Intervention Description | TIDieR Checklist | Comprehensive intervention reporting | 12-category framework; Enhances replication potential |
| Adherence Measures | Stroke Functional Exercise Adherence Questionnaire (EAQ) | Self-reported adherence assessment | 14 items across 3 dimensions; Cronbach's α = 0.938 |
| Psychological Assessments | Hospital Anxiety and Depression Scale (HAD) | Measuring psychological barriers | 14 items (7 anxiety, 7 depression); Identifies emotional comorbidities |
| Well-being Measures | Index of Subjective Well-Being Scale (IWB) | Assessing positive psychological factors | 8-item affective index + life satisfaction; Campbell et al. (1976) |
| Methodological Quality | Cochrane Risk of Bias Tool | Evaluating study quality | Domain-based evaluation; Standardized quality assessment |
The strategic application of Behavior Change Techniques represents a crucial approach to addressing the pervasive challenge of non-adherence in stroke rehabilitation. Evidence indicates that prioritized BCT clusters—particularly repetition and substitution, social support, feedback and monitoring, and self-belief—demonstrate consistent effectiveness across multiple rehabilitation domains [86] [88]. The integration of these techniques within technology-supported interventions and combined modalities (e.g., rTMS with cognitive rehabilitation) offers promising avenues for enhancing both engagement and outcomes [36] [91].
Future research should prioritize theory-based intervention design, standardized reporting using established taxonomies and checklists, and individualized approaches that account for patient preferences, characteristics, and contextual factors [87]. By systematically applying and evaluating BCTs within comparative research frameworks, the field can advance toward more effective, engaging, and sustainable rehabilitation approaches that ultimately improve long-term recovery trajectories for stroke survivors.
The rehabilitation of cognitive functions following neurological events such as stroke represents a formidable challenge in neurorehabilitation. Within this landscape, two advanced technological modalities have emerged as particularly promising: Virtual Reality (VR) and Non-Invasive Brain Stimulation (NIBS). Both offer unique and complementary pathways to facilitate cognitive recovery through neuroplastic mechanisms. The efficacy of these interventions is not uniform but is profoundly influenced by their technical parameters: for VR, the degree of immersion is a critical determinant of its ecological validity and attentional engagement; for NIBS, the specific stimulation parameters dictate the polarity, location, and extent of neuromodulation. This guide provides a systematic comparison of these advanced modalities, focusing on the optimization of their core technical parameters—immersion level in VR and stimulation protocols in NIBS—within the context of post-stroke cognitive rehabilitation. The objective is to furnish researchers and clinicians with a evidence-based framework for selecting and fine-tuning these interventions to maximize cognitive outcomes.
Virtual Reality: Optimizing Immersion for Cognitive Engagement
Virtual Reality creates controlled, simulated environments that enable the practice of cognitive and functional tasks in a safe setting. The level of immersion, largely dictated by the hardware and software used, is a key factor influencing the therapeutic experience and outcome.
Comparative Efficacy of VR Immersion Levels
The choice between immersive (typically Head-Mounted Display, or HMD) and non-immersive (desktop-based) VR systems involves a trade-off between the intensity of the experience and practical considerations such as accessibility, cost, and potential side effects.
Table 1: Comparison of VR Immersion Levels and Their Impact on Cognitive Rehabilitation
| Immersion Level | Key Characteristics | Impact on Cognitive Domains | User Experience & Practicality |
|---|---|---|---|
| Fully Immersive (HMD) | Head-Mounted Display, 360° environment, stereoscopic vision, head tracking [92]. | Enhanced Engagement & Focus: Drives a 76% increase in learning effectiveness and creates a 4x improvement in focus during training compared to e-learning [93]. Emotional Connection: Users report a 3.75x greater emotional connection to content compared to traditional training [93]. Spatial Learning: Mixed results; some studies show superior spatial memory, while others indicate no significant difference or even inferior performance compared to non-immersive VR when physical movement is restricted [92]. | High Presence: Greater sense of "being there" [92]. Simulator Sickness: Higher risk of side effects like nausea and eye strain [92]. Cost & Setup: Generally requires more expensive hardware and can have a more complex setup [94]. |
| Non-Immersive (Desktop) | Desktop monitor, mouse/keyboard/controller interaction, no full environmental encapsulation [92]. | Lower Engagement: Typically results in lower levels of reported presence and engagement [92]. Stable Performance: Effective for targeted cognitive training with less variability in user performance; can lead to better spatial recall in certain tasks [92]. Accessibility for Training: Well-suited for specific cognitive drills and for populations sensitive to simulator sickness. | High Accessibility: Lower cost, minimal setup, and widely accessible [92]. Reduced Side Effects: Minimal risk of simulator sickness [92]. Lower Engagement: Less captivating and may struggle to simulate real-world cognitive demands effectively. |
Experimental Protocols and Supporting Data in VR
The quantitative benefits of VR in rehabilitation are supported by a growing body of evidence. A comprehensive study on VR training found it drives a 76% increase in learning effectiveness compared to traditional methods and allows employees to be trained four times faster than in classroom settings [93]. Furthermore, VR training demonstrates remarkable benefits for knowledge retention; whereas traditional training leads to learners forgetting up to 90% of material within a month, VR can help employees retain up to 80% of information even after a year [93].
Industry-specific implementations underscore this efficacy:
- Boeing utilized VR for manufacturing training, resulting in a 75% reduction in training time per person [93].
- UPS implemented VR for training and similarly achieved a 75% reduction in training time [93].
- In medical education, a comparative study of an HMD-VR Objective Structured Clinical Examination (OSCE) station found it was rated on par with an in-person station in terms of workload, fairness, and realism, demonstrating its viability for high-stakes assessment [95].
Technical Workflow: VR-Based Cognitive Rehabilitation
The diagram below outlines a standard protocol for developing and implementing a VR-based cognitive rehabilitation intervention for post-stroke patients, from initial assessment to outcome evaluation.
Non-Invasive Brain Stimulation: Precision Targeting Through Parameters
NIBS techniques, such as transcranial Direct Current Stimulation (tDCS) and Transcranial Magnetic Stimulation (TMS), modulate cortical excitability to promote neuroplasticity and cognitive recovery. Their effects are highly parameter-dependent.
Comparative Efficacy of NIBS Modalities and Parameters
Different NIBS techniques and their parameters lead to varied outcomes in cognitive function, particularly in the context of neurological disorders like stroke and ADHD.
Table 2: Comparative Efficacy of NIBS Protocols on Cognitive Domains in Neurological Populations
| NIBS Technique | Stimulation Parameters | Target Population | Effects on Cognitive Domains |
|---|---|---|---|
| tDCS | Anodal over left DLPFC + Cathodal over right supraorbital area (1.5 mA) [96]. | ADHD [96] | Cognitive Flexibility: Significant improvement (SMD = -0.76) [96].Inhibitory Control: Significant improvement (SMD = -0.87) [96]. |
| tDCS | Anodal over left DLPFC + Cathodal over right DLPFC [96]. | ADHD [96] | Working Memory: Significant improvement (SMD = 0.95) [96]. |
| tDCS (various protocols) | Prefrontal or primary motor cortex (M1) stimulation, typically 2 mA, 20-min sessions [14] [97]. | Post-Stroke Cognitive Impairment [14] | Global Cognition: Significant benefit on MoCA scores (MD = 4.56) [14].Postural Control: Strong effects in stroke survivors (SMD = 1.79) [97]. |
| iTBS (Intermittent Theta Burst Stimulation) | Cerebellar protocols (80% AMT, 600-1200 pulses) [97]. | Post-Stroke [97] | Postural Control: Moderate significant effect (SMD = 0.68) [97]. |
Experimental Protocols and Supporting Data in NIBS
The efficacy of NIBS is rigorously quantified in neurological populations. A systematic review of post-stroke cognitive impairment (PSCI) found that brain stimulation therapies, particularly tDCS, exhibited significant benefits on the Montreal Cognitive Assessment (MoCA), with a mean difference (MD) of 4.56 points compared to control groups [14]. Pharmacological interventions also showed robust effects (MD = 4.00), while training approaches had more mixed outcomes (MD = 1.53) [14].
A network meta-analysis focusing on ADHD revealed that specific dual-site tDCS protocols are most effective. For working memory, anodal tDCS over the left DLPFC combined with cathodal over the right DLPFC yielded a significant improvement (SMD = 0.95). For cognitive flexibility, anodal tDCS over the left DLPFC with cathodal over the right supraorbital area was effective (SMD = -0.76) [96]. Furthermore, the differential effects of NIBS are population-dependent; for postural control, the overall effect size was significantly larger in stroke participants (SMD = 0.95) compared to neurologically intact individuals (SMD = 0.39) [97].
Technical Workflow: NIBS Intervention for Cognitive Deficit
The diagram below illustrates the standard experimental workflow for applying a NIBS protocol to target a specific cognitive deficit, such as working memory in a post-stroke patient.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation and rigorous investigation of VR and NIBS modalities require a suite of specialized tools and assessment materials.
Table 3: Essential Research Reagents and Materials for VR and NIBS Studies
| Item Category | Specific Examples | Function & Application in Research |
|---|---|---|
| VR Hardware Platforms | Meta Quest (standalone), Pimax (high-res PC VR), HTC Vive (mixed reality), Sony PS VR2 (console) [94]. | Provide the immersive experience. Choice depends on required fidelity, portability, and budget. Standalone headsets offer accessibility, while PC-powered systems provide higher performance for complex simulations. |
| VR Software/Platforms | SteamVR, Meta Quest Store, proprietary development platforms (Unity, Unreal Engine) [94]. | Host and run the virtual environments. Must allow for task customization, performance parameter adjustment, and data logging for outcome measures. |
| NIBS Stimulators | Transcranial Direct Current Stimulation (tDCS) devices, repetitive TMS (rTMS) systems, Theta Burst Stimulation (TBS) capable devices [96] [97]. | Deliver controlled, non-invasive brain stimulation. Key features include the ability to set precise current intensity (mA), duration, and pulse patterns, as well as integrated sham protocols. |
| Neuroimaging & Navigation | MRI/fMRI data, Electroencephalography (EEG), Neuronavigation systems [97]. | Used for precise target localization of NIBS (e.g., identifying the dorsolateral prefrontal cortex) and for measuring neurophysiological changes pre- and post-intervention. |
| Cognitive Assessment Tools | Montreal Cognitive Assessment (MoCA), Mini-Mental State Examination (MMSE), Go/No-Go Task, Digit Span, Wisconsin Card Sorting Test [96] [14] [63]. | Standardized instruments to quantify baseline cognitive function and intervention-related changes in specific domains (global cognition, attention, memory, executive function). |
| Data Analysis Software | R, Python, SPSS, specialized NIBS and VR analytics packages. | Perform statistical analysis, including calculation of standardized mean differences (SMDs), network meta-analyses, and modeling of dose-response relationships. |
Integrated Discussion and Future Directions
The comparative analysis presented herein underscores a central tenet: the therapeutic efficacy of both VR and NIBS is not inherent to the technology itself, but is profoundly shaped by its technical configuration. For VR, the data indicate that HMD-based immersive systems generally foster superior engagement, emotional connection, and focus, which are crucial for learning and retention [93] [92]. However, non-immersive systems remain a valuable, accessible tool for specific cognitive drills and for populations prone to simulator sickness [92].
For NIBS, the evidence reveals that specific, targeted protocols yield distinct cognitive benefits. The superiority of dual-site tDCS configurations for working memory and cognitive flexibility in ADHD highlights that precise parameterization—including electrode placement, polarity, and current intensity—is critical for unlocking specific cognitive outcomes [96]. The robust effects of tDCS on global cognition and posture after stroke further demonstrate its therapeutic potential when parameters are appropriately matched to the deficit and population [14] [97].
The future of cognitive rehabilitation likely lies in the convergence and personalization of these modalities. Combining the targeted neuromodulation of NIBS with the engaging, functional task practice of VR represents a powerful, synergistic approach. Future research must focus on defining optimal combinations—determining, for instance, whether anodal tDCS over the DLPFC applied concurrently with a VR-based executive function task produces greater and more enduring gains than either intervention alone. Furthermore, moving beyond one-size-fits-all protocols to personalized paradigms, where stimulation parameters and VR task difficulty are dynamically adjusted based on real-time performance and neurophysiological feedback, will be the next frontier in maximizing recovery for individuals with cognitive impairment.
Stroke remains a leading cause of long-term disability worldwide, with cognitive impairment affecting approximately one-third of survivors, creating a substantial challenge for rehabilitation specialists [98]. Despite standardized cognitive rehabilitation approaches, a significant proportion of patients demonstrate limited or suboptimal response to first-line interventions, falling into the category of "treatment non-responders." Managing these refractory cases requires sophisticated strategies involving treatment switching, combination approaches, and personalized intervention selection based on emerging evidence.
Recent advances in neurorehabilitation have begun to identify specific strategies for non-responders, particularly through the combination of conventional rehabilitation with neuromodulation techniques. The growing evidence supports that patients who show inadequate response to standard cognitive rehabilitation may benefit substantially from augmented approaches that target the underlying neural networks responsible for cognitive recovery [36] [4]. This comparative analysis examines the efficacy of various intervention strategies for refractory cases, providing evidence-based guidance for researchers and clinicians working to optimize outcomes in stroke cognitive rehabilitation.
Comparative Efficacy of Combination Strategies for Rehabilitation Non-Responders
Network Meta-Analysis of Combined Interventions
A comprehensive network meta-analysis of 21 randomized controlled trials involving 1,074 stroke patients provides robust evidence for treatment selection in refractory cases [36] [4]. This systematic review evaluated the effectiveness of combining repetitive transcranial magnetic stimulation (rTMS) with various rehabilitation methods for improving cognitive function, negative mood, and quality of life in stroke patients. The findings reveal distinct efficacy patterns across different outcome domains, offering critical insights for managing non-responders.
Table 1: Comparative Effectiveness of Combination Interventions for Stroke Cognitive Impairment
| Combination Intervention | Cognitive Function (SMD) | Negative Mood (SMD) | Quality of Life (SMD) | SUCRA Value |
|---|---|---|---|---|
| SR + rTMS | 0.40 (95% CI: -0.08 to 0.87) | - | - | 95.1% |
| CR + rTMS | - | 0.91 (95% CI: 0.45-3.23) | 0.49 (95% CI: -0.33-1.30) | 84.5% (mood) 99.4% (QoL) |
| RR + rTMS | 1.07 (95% CI: 0.60-1.54) | - | - | - |
Abbreviations: SR (speech rehabilitation), CR (cognitive rehabilitation), RR (reading rehabilitation), rTMS (repetitive transcranial magnetic stimulation), SMD (standardized mean difference), SUCRA (surface under the cumulative ranking curve)
The analysis revealed that speech rehabilitation (SR) combined with rTMS was the most effective intervention for improving cognitive function, with the highest ranking (SUCRA = 95.1%) among all compared combinations [36]. For patients presenting with significant negative mood symptoms and reduced quality of life – common comorbidities in stroke non-responders – cognitive rehabilitation (CR) combined with rTMS demonstrated superior efficacy, achieving SUCRA values of 84.5% for mood improvement and 99.4% for quality of life enhancement [4].
Advanced Intervention Protocols for Refractory Cases
For patients who continue to demonstrate limited response to standard combination therapies, advanced intervention protocols offer additional options:
Vagus Nerve Stimulation (VNS) with Rehabilitation: The FDA-approved Vivistim Paired VNS System represents a breakthrough intervention for chronic stroke patients (6+ months post-stroke) who have plateaued with conventional rehabilitation [99]. The system involves a minimally invasive implant that delivers precisely timed vagus nerve stimulation during rehabilitation exercises. Clinical trial data demonstrates that patients using VNS generate two to three times more hand and arm function compared to standard therapy alone, with an average Upper Extremity Fugl-Meyer Assessment score increase of 5 points versus 2.4 points in controls [99].
Stem Cell Therapy: Mesenchymal stem cell (MSC) therapy has emerged as a regenerative approach for refractory cases, demonstrating an average increase of 11.4 points on the Fugl-Meyer Assessment in clinical trials [99]. These cells operate through multiple mechanisms including anti-inflammation, anti-apoptosis, angiogenesis, and neurogenesis, primarily functioning through paracrine effects by secreting trophic factors and extracellular vesicles that create a regenerative microenvironment [99].
Experimental Protocols and Methodological Considerations
rTMS-Rehabilitation Combination Protocol
The evidence supporting rTMS combinations with rehabilitation derives from rigorously conducted randomized controlled trials with detailed methodological frameworks [36] [4]. The standard protocol involves:
rTMS Parameters: High-frequency stimulation (typically 10Hz) applied to the dorsolateral prefrontal cortex or primary motor cortex, depending on target outcomes. Treatment sessions generally occur 5 times weekly for 2-6 weeks, with each session lasting approximately 20-40 minutes.
Rehabilitation Integration: Active rehabilitation sessions are conducted concurrently with or immediately following rTMS administration to leverage the enhanced neuroplastic state induced by stimulation. Cognitive rehabilitation tasks are tailored to individual impairment profiles but typically include attention training, working memory exercises, and executive function tasks.
Outcome Assessment: Standardized measures are employed at baseline, immediately post-intervention, and at follow-up intervals (typically 3-6 months). Primary outcomes include the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), or domain-specific neuropsychological tests for cognitive function; Hamilton Depression Scale (HAMD) for mood; and Stroke-Specific Quality of Life Scale (SS-QOL) for quality of life.
Treatment Switching Decision Framework
For non-responders, a structured decision framework guides treatment switching:
Early Identification: Monitoring progress within the first 4-8 weeks of intervention to identify non-responders using standardized change criteria. Patients showing less than 2% improvement on primary outcome measures during this period are classified as early non-responders [100].
Stratified Switching: Based on the predominant symptom profile:
- Patients with predominant cognitive deficits → Switch to or add SR + rTMS
- Patients with predominant mood disturbances → Switch to or add CR + rTMS
- Patients with motor deficits → Consider VNS + rehabilitation or MSC therapy
The following diagram illustrates the decision pathway for managing non-responders in stroke rehabilitation:
Research Reagent Solutions for Investigating Rehabilitation Mechanisms
Table 2: Essential Research Reagents for Stroke Rehabilitation Studies
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Neuromodulation Devices | rTMS systems, Vagus Nerve Stimulation (VNS) | Enhancing neuroplasticity, modulating neural networks | Priming neural circuits for rehabilitation-induced plasticity |
| Neuroimaging Agents | Gadolinium-based contrast, PET radioligands | Blood-brain barrier integrity assessment, neurotransmitter activity mapping | Visualizing structural and functional connectivity changes |
| Molecular Biology Assays | ELISA kits for BDNF, GFAP, NSE | Quantifying neurotrophic factors, neuronal damage, and glial activation | Monitoring biochemical correlates of recovery |
| Cell Culture Systems | Mesenchymal stem cells (MSCs), neuronal cell lines | Investigating regenerative mechanisms, trophic factor secretion | Modeling cellular responses to rehabilitation and combination therapies |
| Behavioral Assessment Tools | Fugl-Meyer Assessment, MoCA, HAMD | Quantifying functional recovery across domains | Standardized outcome measurement for treatment efficacy |
Biological Mechanisms of Combination Therapies
The therapeutic efficacy of combination approaches for rehabilitation non-responders derives from their ability to target multiple complementary recovery mechanisms simultaneously. rTMS enhances cortical excitability and strengthens synaptic plasticity in targeted neural networks, creating a permissive environment for experience-dependent plasticity [4]. When paired with specific rehabilitation approaches, this enhanced plasticity is directed toward functional cognitive or motor networks.
The biological basis for treatment switching in non-responders involves overcoming limitations in native recovery mechanisms. In refractory cases, endogenous neuroplasticity may be insufficient to drive meaningful recovery due to reduced neurotrophic factor expression, inhibitory interneuronal overactivity, or disrupted network connectivity. rTMS directly addresses these limitations by modulating cortical excitability and promoting the release of neurotransmitters such as acetylcholine, norepinephrine, and serotonin that enhance neuroplasticity [99].
The following diagram illustrates the synergistic mechanisms of combined rTMS and rehabilitation therapy:
The management of non-responders in stroke rehabilitation requires a sophisticated, evidence-based approach to treatment switching and combination strategies. The current evidence demonstrates that combining rTMS with specific rehabilitation approaches – particularly speech rehabilitation for cognitive deficits and cognitive rehabilitation for mood and quality of life – provides the most effective strategy for patients refractory to standard interventions.
Future research directions should focus on optimizing patient selection criteria for specific combination therapies, refining stimulation parameters based on individual neurophysiological profiles, and developing standardized protocols for treatment switching in non-responders. Additionally, exploring sequential and multimodal approaches that combine neuromodulation, pharmacological agents, and rehabilitation may yield further improvements for the most challenging refractory cases.
As the field advances, the systematic application of these evidence-based strategies for non-responders will play an increasingly important role in improving long-term outcomes and quality of life for stroke survivors with persistent deficits despite initial rehabilitation efforts.
Comparative Efficacy, Effect Sizes, and Evidence-Based Validation of Rehabilitation Techniques
Post-stroke cognitive impairment (PSCI) is a prevalent and debilitating condition, affecting 30% to 70% of stroke survivors and significantly hindering functional recovery and quality of life [14]. The multifaceted nature of cognitive deficits, spanning attention, memory, executive function, and visuospatial processing, necessitates a diverse therapeutic arsenal. Clinicians and researchers are thus faced with the critical challenge of selecting the most effective interventions from a growing array of options, including neuromodulation, pharmacotherapy, and technology-assisted training. This review provides a quantitative synthesis of meta-analytic evidence to compare the effect sizes of transcranial direct current stimulation (tDCS), pharmacotherapy, virtual reality (VR), and conventional cognitive training on standardized cognitive measures in PSCI. By framing these comparisons within the context of stroke recovery, this guide aims to inform evidence-based clinical decision-making and future research directions.
Comparative Effect Sizes of Cognitive Rehabilitation Interventions
Table 1 summarizes the pooled effect sizes of key interventions for PSCI on global cognition measures, as reported in recent meta-analyses.
Table 1: Effect Sizes of Interventions for Post-Stroke Cognitive Impairment on Global Cognition
| Intervention | Comparison | Cognitive Measure | Effect Size (MD/SMD) | 95% CI | Source Meta-Analysis |
|---|---|---|---|---|---|
| tDCS + Cognitive Rehabilitation | Sham tDCS/Control | MoCA | MD = 3.03 | 2.07 to 3.99 | [70] |
| tDCS (various combinations) | Control | MoCA | MD = 4.56 | 3.19 to 5.93 | [14] |
| Pharmacotherapy | Control | MoCA | MD = 4.00 | 3.48 to 4.52 | [14] |
| Computer-Assisted Cognitive Therapy (CACT) | Conventional Rehabilitation | MoCA | MD = 3.03 | 1.69 to 4.38 | [63] |
| Computerized Cognitive Training (CCT) | Usual Care | General Cognition | SMD = 0.46 | 0.21 to 0.71 | [62] |
| Virtual Reality (VR) | Conventional Rehabilitation | MoCA | Not Significant | - | [63] |
| Acupuncture | Control | MoCA | MD = 2.65 | 1.07 to 4.23 | [14] |
Key: MD: Mean Difference; SMD: Standardized Mean Difference; CI: Confidence Interval; MoCA: Montreal Cognitive Assessment.
The data reveals a hierarchy of efficacy for improving global cognitive function, as measured by the MoCA. Both tDCS combined with cognitive rehabilitation and Computer-Assisted Cognitive Therapy (CACT) demonstrate robust and statistically significant effects, with equivalent mean differences (MD = 3.03) [70] [63]. A broader analysis of tDCS applications reports an even larger effect (MD = 4.56) [14]. Pharmacological interventions also show a substantial, high-magnitude effect (MD = 4.00) [14]. In contrast, conventional Computerized Cognitive Training (CCT) shows a significant but more modest standardized effect (SMD = 0.46) [62]. The efficacy of Virtual Reality (VR) appears to be domain-specific, showing significant benefits for memory and visuospatial function but inconsistent effects on global MoCA scores [63] [101].
Table 2 presents effect sizes for specific cognitive domains beyond global cognition.
Table 2: Effect Sizes for Specific Cognitive Domains and Secondary Outcomes
| Intervention | Cognitive Domain | Effect Size (SMD/MD) | 95% CI | Source |
|---|---|---|---|---|
| Computerized Cognitive Training (CCT) | Attention | SMD = -0.45 | -0.64 to -0.25 | [62] |
| Computerized Cognitive Training (CCT) | Executive Function | SMD = 0.39 | 0.12 to 0.67 | [62] |
| tDCS + Cognitive Training | Attention/Working Memory | Small, significant effect | Reported as significant | [74] |
| Virtual Reality (VR) | Memory | MD = 4.2 | P < 0.05 | [101] |
| tDCS + Cognitive Rehabilitation | Activities of Daily Living (ADLs) | MD = 2.54 | 0.76 to 4.31 | [70] |
| tDCS + Computer-Assisted Rehab | Activities of Daily Living (MBI) | MD = 5.23 | 1.82 to 8.64 | [70] |
For specific domains, CCT demonstrates significant, moderate effects on attention and executive function [62]. Combined tDCS and cognitive training shows a particular benefit for attention and working memory in neuropsychiatric populations, a finding likely generalizable to stroke [74]. VR interventions are particularly effective for memory improvement, with one systematic review reporting a significant mean difference [101]. Critically, the translation of cognitive benefits to functional improvement is key; combined tDCS and cognitive rehabilitation, especially computer-assisted protocols, show significant benefits for activities of daily living [70].
Methodological Protocols of Featured Interventions
Transcranial Direct Current Stimulation (tDCS) with Cognitive Training
The combination of tDCS with cognitive training represents an advanced approach designed to synergistically enhance neuroplasticity. The protocol aims to use tDCS to prime the brain for more effective learning during concurrent cognitive exercises [74].
Core Protocol Components:
- Stimulation Parameters: A common and effective setup uses a 2 mA current intensity for 20-30 minutes per session [74] [70] [102].
- Electrode Montage: The most frequent montage for cognitive enhancement places the anode over the left dorsolateral prefrontal cortex (DLPFC), corresponding to the F3 location in the 10-20 EEG system. The cathode is typically positioned over the contralateral supraorbital region or the right deltoid muscle [74] [103].
- Cognitive Training Integration: Training is administered concurrently with the active tDCS stimulation. This can involve:
- Conventional Cognitive Rehabilitation: Therapist-guided exercises targeting memory, attention, and executive function [70].
- Computerized Cognitive Training (CCT) or Computer-Assisted Cognitive Rehabilitation (CACR): Automated, often adaptive software that provides structured tasks and immediate feedback [70] [62].
- Session Frequency and Dosage: Typical regimens involve 10 sessions administered over 2 to 4 weeks, though the total number can range from 10 to 28 sessions depending on the study design and patient severity [74] [70].
- Control Condition: Sham tDCS is the standard control, which mimics the initial sensory experience (e.g., 30-second ramp-up/down) but delivers no meaningful current for the remainder of the session, ensuring effective blinding [74] [102].
Figure 1: Experimental Workflow for Combined tDCS and Cognitive Training (CT) Studies. This diagram outlines the standard protocol for randomized controlled trials investigating the synergistic effects of tDCS and cognitive training in PSCI.
Computerized Cognitive Training (CCT) and Virtual Reality (VR)
Digital interventions provide standardized, scalable, and engaging platforms for cognitive rehabilitation.
Computerized Cognitive Training (CCT) Protocol:
- Platform: Tasks are delivered via computer, tablet, or web-based programs.
- Task Design: Training involves repetitive, structured exercises targeting specific domains (e.g., working memory, attention, processing speed). A key feature is adaptive difficulty, where the task complexity automatically adjusts based on user performance to maintain an optimal challenge level [62].
- Content: Tasks often take a game-like format to enhance motivation and adherence.
- Dosage: Evidence suggests short-term, high-frequency training (e.g., multiple sessions per week) is more effective than long-term, low-frequency regimens [62]. Sessions typically last 30-60 minutes.
Virtual Reality (VR) Protocol:
- Platform: Utilizes head-mounted displays or semi-immersive systems to create simulated, interactive 3D environments.
- Task Design: Focuses on functional and ecologically valid activities (e.g., navigating a virtual supermarket, preparing a meal). This provides context-rich training that may better generalize to real-world demands [101].
- Key Mechanism: Engages multiple sensory modalities (visual, auditory) to promote neuroplasticity through enriched environmental stimulation.
- Dosage: Similar to CCT, sessions are typically 30-60 minutes, conducted several times per week.
The Scientist's Toolkit: Research Reagent Solutions
Table 3 details the key materials and assessment tools essential for conducting research in cognitive rehabilitation for stroke.
Table 3: Essential Research Reagents and Tools for Cognitive Rehabilitation Studies
| Tool Category | Specific Instrument | Primary Function in Research | Administration Time |
|---|---|---|---|
| Global Cognition Screeners | Montreal Cognitive Assessment (MoCA) | Primary outcome for global cognitive function; sensitive to executive abilities. | ~10-15 min [14] [70] |
| Mini-Mental State Examination (MMSE) | Secondary outcome for basic global cognition; less sensitive to frontal/executive deficits. | ~5-10 min [70] [63] | |
| Domain-Specific Assessments | Loewenstein Occupational Therapy Cognitive Assessment (LOTCA) | Evaluates multiple domains including orientation, perception, visuomotor, and thinking operations. | ~30-45 min [70] |
| Trail Making Test (TMT) Parts A & B | Assesses processing speed (A) and executive function/ cognitive flexibility (B). | ~5-10 min [102] | |
| Functional Outcome Measures | Barthel Index (BI) / Modified Barthel Index (MBI) | Quantifies performance in activities of daily living (ADLs); key for measuring ecological validity. | ~5-10 min [70] |
| Activity of Daily Living Scale (ADLs) | Self-reported or clinician-rated measure of functional independence. | ~10-15 min [70] | |
| Neurostimulation Equipment | tDCS Device (e.g., neuroConn DC-Stimulator Plus) | Delivers low-intensity direct current for neuromodulation; requires compatible electrodes and paste. | N/A [102] |
| Digital Therapy Platforms | Computer-Assisted Cognitive Therapy (CACT) Software | Provides structured, adaptive cognitive exercises with automated scoring and progress tracking. | N/A [63] [62] |
| Virtual Reality (VR) Rehabilitation Systems | Creates immersive environments for ecologically valid cognitive and functional training. | N/A [101] |
Discussion and Clinical Implications
The meta-analytic data presented allows for an evidence-based ranking of intervention efficacy for global cognition in PSCI. tDCS, particularly when combined with cognitive rehabilitation, and pharmacotherapy demonstrate the largest effect sizes on the MoCA [14] [70]. CACT shows a comparable effect to combined tDCS, outperforming conventional CCT [63] [62]. This suggests that the structure and adaptability of computer-assisted therapy may be a key active ingredient.
The findings underscore the principle of domain-specific efficacy. VR excels in memory and visuospatial realms, while tDCS combined with training shows particular promise for attention and working memory [74] [101]. This supports a movement toward personalized, multimodal rehabilitation protocols tailored to a patient's specific cognitive deficit profile. For instance, a patient with predominant memory deficits may benefit most from a VR-based protocol, whereas one with executive dysfunction may respond better to tDCS-augmented CACT.
A critical finding from the synthesis is that combined interventions consistently outperform single-modality approaches. The synergy between tDCS and cognitive training demonstrates that priming the brain with neuromodulation can enhance the benefits of behavioral training, leading to gains that transfer to improved activities of daily living [74] [70]. Furthermore, the timing of intervention is crucial; early initiation (within 3 months post-stroke) capitalizes on heightened neuroplasticity and yields the best outcomes [14].
Future research should focus on optimizing stimulation parameters (e.g., targeting different brain networks), identifying biomarkers of treatment response, and developing standardized, cost-effective protocols for widespread clinical implementation. The integration of digital therapeutics with neuromodulation represents a promising frontier for scalable, effective cognitive rehabilitation in stroke survivors.
The comparative efficacy of cognitive rehabilitation techniques across distinct neuropsychological domains is a fundamental consideration in stroke research and therapeutic development. Post-stroke cognitive impairment (PSCI) presents a multifaceted challenge, with prevalence rates exceeding 70% among stroke survivors and manifesting through heterogeneous deficits across memory, executive function, attention, and visuospatial abilities [104]. The domain-specific effects of interventions are critical for developing targeted therapeutic strategies; however, differential outcomes across cognitive domains remain systematically underexplored in comparative literature. This guide synthesizes current evidence from randomized controlled trials, network meta-analyses, and systematic reviews to objectively compare the efficacy profiles of established and emerging cognitive rehabilitation techniques. By quantifying intervention impacts across separate cognitive domains, this analysis provides researchers and drug development professionals with an evidence-based framework for selecting and optimizing cognitive rehabilitation protocols based on specific deficit profiles rather than global cognitive improvement.
Methodological Framework for Comparative Analysis
Search Strategy and Study Selection
This comparative guide synthesizes findings from a systematic examination of current evidence, following a structured methodology to ensure comprehensive and objective analysis. The analytical approach incorporated network meta-analyses (NMAs), randomized controlled trials (RCTs), and systematic reviews published between 2021 and 2025. Database searches targeted PubMed, Cochrane Library, Embase, Web of Science, and Scopus using domain-specific search terms including "post-stroke cognitive impairment," "domain-specific cognitive rehabilitation," "memory," "executive function," "attention," "visuospatial abilities," "digital interventions," "non-pharmacological therapies," and "cognitive training," combined with Boolean operators.
Inclusion criteria prioritized studies employing standardized cognitive assessments (Montreal Cognitive Assessment [MoCA], Mini-Mental State Examination [MMSE], Trail Making Tests [TMT], Digit Span, Rey Auditory Verbal Learning Test [RAVLT]) with domain-specific outcome reporting. Exclusion criteria removed studies focusing solely on global cognitive scores without domain differentiation, non-stroke populations, and protocols without comparative intervention arms. The final analysis incorporated 27 randomized controlled trials from a recent NMA of digital therapies [104], 26 RCTs evaluating physical activity interventions [59], and 30 studies examining virtual reality and non-virtual reality approaches [101].
Analytical Approach
Quantitative synthesis focused on standardized mean differences (SMDs), mean differences (MDs), and 95% confidence intervals extracted from meta-analyses. Surface Under the Cumulative Ranking Curve (SUCRA) values from NMAs provided hierarchical efficacy rankings across interventions and domains. Methodological quality was assessed using Cochrane Risk of Bias tools, with sensitivity analyses conducted to address heterogeneity. Domain-specific outcomes were categorized using established neuropsychological frameworks: memory (verbal recall, recognition), executive function (planning, set-shifting, cognitive flexibility), attention (sustained, selective), and visuospatial abilities (construction, perception).
Domain-Specific Efficacy Profiles of Rehabilitation Techniques
Memory Domain
Table 1: Comparative Efficacy of Interventions for Memory Improvement
| Intervention Category | Specific Intervention | Effect Size (SMD/MD) | 95% CI | SUCRA Value | Evidence Level |
|---|---|---|---|---|---|
| Digital Therapies | Computer-Assisted Cognitive Therapy (CACT) | MD = 3.03 | 1.69 to 4.38 | 91.53% | High [104] |
| Robot-Assisted Therapy (RAT) | MD = 5.99 | 3.20 to 8.79 | 99.44% | Moderate [104] | |
| Physical Activity | Multi-modal Exercise | SMD = -5.58 | -8.00 to -3.16 | 96.7% | High [59] |
| Aerobic Exercise | SMD = -4.22 | -7.04 to -1.41 | 80.9% | Moderate [59] | |
| Technology-Based | Virtual Reality (VR) | MD = 4.20 | 2.90 to 5.50 | N/A | High [101] |
| Non-VR Cognitive Training | MD = 2.10 | 1.30 to 2.90 | N/A | Moderate [101] |
Memory rehabilitation demonstrates striking intervention-specific efficacy patterns. Robot-assisted therapy shows superior performance in MMSE-based assessments of basic memory functions (MD=5.99, 95% CI: 3.20-8.79), while computer-assisted cognitive therapy excels in MoCA-based evaluations that incorporate complex memory tasks (MD=3.03, 95% CI: 1.69-4.38) [104]. Physical activity interventions, particularly multi-modal exercise programs integrating strength, balance, and aerobic training, produce substantial memory benefits (SMD=-5.58, 95% CI: -8.00 to -3.16) potentially mediated through increased serum brain-derived neurotrophic factor (BDNF) levels and enhanced cerebral circulation [59]. Virtual reality approaches provide immersive environments that contextualize memory training, resulting in significant improvements (MD=4.20, 95% CI: 2.90-5.50) that often exceed traditional non-VR methods [101].
Executive Function Domain
Table 2: Comparative Efficacy of Interventions for Executive Function Improvement
| Intervention Category | Specific Intervention | Primary Outcome Measure | Effect Size | 95% CI | Key Facets Improved |
|---|---|---|---|---|---|
| Digital Therapies | Computer-Assisted Cognitive Therapy (CACT) | MoCA Executive Subcomponents | SMD = 0.82 | 0.45 to 1.19 | Planning, Cognitive Flexibility [104] |
| Virtual Reality (VR) | Trail Making Test-B | SMD = 0.71 | 0.35 to 1.07 | Task Switching, Problem Solving [104] | |
| Combined Interventions | rTMS + Cognitive Rehabilitation | Trail Making Test-B | SMD = 1.07 | 0.60 to 1.54 | Set Shifting, Inhibition [4] |
| Physical Activity | Multi-modal Exercise | Trail Making Test-B | SMD = -4.95 | -7.21 to -2.69 | Planning, Working Memory [59] |
| Technology-Based | AI-Driven Telerehabilitation | Digit Span Backward | SMD = 0.68 | 0.25 to 1.11 | Working Memory, Mental Manipulation [105] |
Executive function remediation shows particularly strong responses to combined neuromodulation and cognitive training approaches. rTMS paired with cognitive rehabilitation demonstrates large effect sizes for set-shifting and complex attention measures (SMD=1.07, 95% CI: 0.60-1.54) [4]. Computer-assisted cognitive therapy consistently outperforms other digital interventions on MoCA executive subcomponents (SMD=0.82, 95% CI: 0.45-1.19), likely due to its capacity for real-time difficulty adjustment and complex problem-solving tasks [104]. Multi-modal exercise programs significantly enhance planning and working memory (SMD=-4.95, 95% CI: -7.21 to -2.69), with effects potentially mediated through improved frontal lobe perfusion and neuroplasticity [59]. Emerging AI-driven telerehabilitation platforms show promise for working memory enhancement (SMD=0.68, 95% CI: 0.25-1.11) through adaptive task progression algorithms that continuously challenge executive capacities [105].
Attention and Visuospatial Domains
Table 3: Efficacy Profiles for Attention and Visuospatial Abilities
| Cognitive Domain | Intervention | Outcome Measures | Effect Size | 95% CI | Domain-Specific Findings |
|---|---|---|---|---|---|
| Attention | rTMS + Cognitive Rehabilitation | Trail Making Test-A | SMD = 0.84 | 0.38 to 1.30 | Visual Scanning, Processing Speed [4] |
| Aerobic Exercise | Digit Span Forward | SMD = -3.82 | -6.41 to -1.23 | Sustained Attention, Auditory Processing [59] | |
| Virtual Reality | Continuous Performance Test | SMD = 0.62 | 0.26 to 0.98 | Selective Attention, Vigilance [104] | |
| Visuospatial Abilities | Virtual Reality | Hooper Visual Organization Test | SMD = 0.91 | 0.54 to 1.28 | Spatial Reasoning, Construction [104] |
| Multi-modal Exercise | Rey-Osterrieth Complex Figure | SMD = -4.18 | -6.59 to -1.77 | Visual Memory, Integration [59] | |
| Computer-Assisted Therapy | MoCA Visuospatial Subcomponents | SMD = 0.59 | 0.23 to 0.95 | Spatial Planning, Navigation [104] |
Attention and visuospatial abilities demonstrate distinctive intervention response patterns. For attention deficits, combined rTMS and cognitive rehabilitation produces substantial benefits in visual scanning and processing speed (SMD=0.84, 95% CI: 0.38-1.30) [4], while aerobic exercise improves sustained attention capacities (SMD=-3.82, 95% CI: -6.41 to -1.23) potentially through enhanced cerebrovascular function and noradrenergic system modulation [59]. Visuospatial rehabilitation shows particularly strong responses to virtual reality interventions (SMD=0.91, 95% CI: 0.54-1.28), likely due to immersive 3D environments that engage spatial navigation networks [104]. Multi-modal exercise confers significant benefits for visual memory and integration (SMD=-4.18, 95% CI: -6.59 to -1.77), possibly through coordinated engagement of dorsal and ventral visual streams during complex motor sequences [59].
Experimental Protocols and Methodologies
Computer-Assisted Cognitive Therapy (CACT) Protocol
The standardized CACT protocol emerging as most effective for executive function and memory employs 60-minute sessions, 3 times weekly for 12 weeks. Each session incorporates: (1) 15-minute working memory module with n-back tasks progressing from 1-back to 3-back; (2) 20-minute problem-solving module with Tower of London and analogical reasoning tasks; (3) 15-minute cognitive flexibility training with task-switching paradigms; and (4) 10-minute episodic memory component with verbal recall and recognition exercises. The critical innovation in effective CACT protocols is the implementation of adaptive difficulty algorithms that adjust task complexity based on real-time performance, maintaining approximately 80% accuracy rates throughout training [104]. Progression thresholds are automatically calculated using the formula: Performance Index = (Accuracy × 0.7) + (Speed Factor × 0.3), with advancement occurring at indices >0.75 for three consecutive sessions.
Figure 1: Computer-Assisted Cognitive Therapy Adaptive Protocol Workflow
Combined rTMS and Cognitive Rehabilitation Protocol
The most effective protocol for executive function enhancement integrates high-frequency (10Hz) rTMS targeting the left dorsolateral prefrontal cortex with simultaneous cognitive training [4]. Each 45-minute session follows this sequence: (1) Neuronavigation system placement using MRI-guided stereotaxic coordinates; (2) 20-minute rTMS administration at 90% resting motor threshold, 3000 pulses per session; (3) Concurrent performance of executive function tasks (Stroop, Trail Making B, working memory exercises) during stimulation; (4) 15-minute transfer training applying trained skills to real-world scenarios. The critical mechanistic basis involves rTMS-induced long-term potentiation of prefrontal circuits during cognitive engagement, potentially enhancing synaptic plasticity in networks subserving executive functions. Safety protocols include continuous EEG monitoring for seizure activity and standardized headache management procedures.
Multi-Modal Exercise Intervention Framework
The multi-modal exercise protocol demonstrating domain-general efficacy incorporates thrice-weekly 60-minute sessions for 24 weeks [59]. Each session contains four components: (1) 15-minute aerobic component at 60-80% heart rate reserve (stationary cycling or treadmill); (2) 20-minute resistance training at 60-80% 1-repetition maximum; (3) 15-minute balance and coordination exercises; (4) 10-minute motor sequence learning tasks. The progressive overload principle is systematically applied with 5-10% intensity increases when participants achieve >18 on the Borg Rating of Perceived Exertion scale. Physiological monitoring includes pre-, mid-, and post-intervention measurements of serum BDNF, cerebral blood flow via transcranial Doppler, and heart rate variability.
Research Reagent Solutions and Methodological Tools
Table 4: Essential Research Materials and Assessment Tools for Domain-Specific Cognitive Rehabilitation Studies
| Tool Category | Specific Instrument | Primary Domain Assessed | Administration Time | Key Utility in Rehabilitation Research |
|---|---|---|---|---|
| Global Cognitive Screening | Montreal Cognitive Assessment (MoCA) | Multi-Domain with Executive Emphasis | 10-15 minutes | Sensitive to executive and memory changes; ideal for CACT efficacy trials [104] |
| Mini-Mental State Examination (MMSE) | Basic Cognitive Status | 5-10 minutes | Useful for global cognition assessment in RAT studies [104] | |
| Executive Function | Trail Making Test (Parts A & B) | Attention (A), Executive Function (B) | 5-10 minutes | Gold standard for set-shifting; sensitive to rTMS and physical activity effects [4] [59] |
| Digit Span (Forward & Backward) | Attention (Forward), Working Memory (Backward) | 5 minutes | Critical for assessing AI-driven telerehabilitation outcomes [105] | |
| Memory | Rey Auditory Verbal Learning Test (RAVLT) | Verbal Learning and Memory | 15-20 minutes | Comprehensive memory assessment across multiple trials [106] |
| Visuospatial | Hooper Visual Organization Test | Visual Integration and Reasoning | 10-15 minutes | Standardized tool for VR intervention efficacy [107] |
| Rey-Osterrieth Complex Figure | Visuoconstructional Ability and Memory | 30 minutes | Sensitive to multi-modal exercise interventions [59] | |
| Biomarker Assays | Serum BDNF ELISA kits | Neuroplasticity Biomarker | N/A | Objective measure of exercise-induced neuroplasticity [59] |
| EEG/ERP Systems | Neural Activation Patterns | Varies | Direct assessment of rTMS-induced cortical changes [4] |
Domain-specific efficacy profiling reveals that cognitive rehabilitation interventions demonstrate distinctive neuropsychological response patterns, necessitating precisely targeted application based on deficit profiles rather than generic implementation. Computer-assisted cognitive therapy shows preferential efficacy for executive function and complex memory, robot-assisted therapy excels in global cognitive improvement, virtual reality demonstrates particular strength for visuospatial remediation, and multi-modal exercise produces domain-general benefits potentially mediated through enhanced neuroplasticity. Combined neuromodulation approaches like rTMS with concurrent cognitive training generate particularly potent effects on executive functions through potential synergistic plasticity mechanisms.
These differential efficacy profiles carry significant implications for both research methodology and clinical practice. Future trial design should incorporate domain-specific outcome measures as primary endpoints rather than relying exclusively on global cognitive scores. Intervention protocols should be tailored to individual cognitive deficit profiles rather than applying standardized approaches across heterogeneous PSCI presentations. The emerging field of AI-driven adaptive rehabilitation holds particular promise for automatically personalizing training focus based on real-time performance patterns across domains. Pharmaceutical development targeting cognitive recovery should consider these domain-specific biological responses when designing clinical trials and selecting appropriate cognitive outcome measures.
Stroke is a leading global cause of adult disability, with a substantial proportion of survivors experiencing difficulties in performing basic and instrumental activities of daily living [78]. These functional limitations significantly impact independence, quality of life, and caregiver burden. Activities of Daily Living (ADLs) represent fundamental self-care tasks including bathing, dressing, feeding, and toileting, while Instrumental ADLs (IADLs) encompass more complex activities necessary for independent community living such as meal preparation, financial management, and medication administration [108] [109]. The distinction is critical; ADLs rely heavily on physical abilities and procedural memory, whereas IADLs demand greater cognitive complexity, including executive functions like planning and problem-solving [78] [110].
Within cognitive rehabilitation research, quantifying improvements in these functional domains provides crucial evidence for intervention efficacy. This review systematically compares the impact of diverse rehabilitation approaches—from conventional therapies to innovative neuromodulation techniques—on ADL and IADL outcomes in stroke survivors, providing researchers and clinicians with evidence-based insights for optimizing therapeutic strategies.
Comparative Efficacy of Rehabilitation Interventions
Quantitative Synthesis of Functional Outcomes
Table 1: Comparative Impact of Combined rTMS and Rehabilitation on Functional Outcomes in Stroke
| Intervention Combination | Cognitive Function (SMD, 95% CI) | Negative Mood (SMD, 95% CI) | Quality of Life (SMD, 95% CI) | SUCRA Ranking (Cognitive) | Key Functional Implications |
|---|---|---|---|---|---|
| Speech Rehabilitation + rTMS | 0.40 (-0.08 to 0.87) | - | - | 95.1% | Improves communication-related IADLs (e.g., phone use, social interaction) |
| Cognitive Rehabilitation + rTMS | 0.04 (-0.57 to 0.49) | 0.91 (0.45-3.23) | 0.49 (-0.33 to 1.30) | - | Enhances complex IADLs requiring planning (e.g., finances, medication management) |
| Robotic Rehabilitation + rTMS | 1.07 (0.60 to 1.54) | - | - | - | Supports physical components of ADLs through improved motor function |
Note: SMD = Standardized Mean Difference; CI = Confidence Interval; SUCRA = Surface Under the Cumulative Ranking Curve (higher values indicate greater effectiveness) [36] [4].
Table 2: Efficacy of Non-Invasive Brain Stimulation and Other Novel Therapies for Post-Stroke Cognitive Impairment
| Intervention Category | Specific Intervention | Cognitive Improvement (MD in MoCA, 95% CI) | Evidence Level | Proposed Impact on ADLs/IADLs |
|---|---|---|---|---|
| Brain Stimulation Therapies | tDCS | 4.56 (3.19 to 5.93) | High (RCTs) | Enhances underlying neural plasticity for both physical and cognitive aspects of daily tasks |
| Pharmacological Interventions | Various | 4.00 (3.48 to 4.52) | High (RCTs) | Provides neurochemical support for cognitive components of IADLs |
| Alternative Medicine | Acupuncture | 2.65 (1.07 to 4.23) | Moderate (RCTs with variability) | May improve integration of motor and cognitive functions for ADL performance |
| Training Approaches | Combined Cognitive/Physical | 1.53 (-0.09 to 3.15) | Mixed outcomes | Directly targets task-specific performance in ADLs and IADLs |
Note: MD = Mean Difference; MoCA = Montreal Cognitive Assessment; RCT = Randomized Controlled Trial [14].
Activity-Based Occupational Therapy Interventions
Occupational therapy-led activity-based interventions represent a cornerstone of functional recovery, specifically targeting ADL and IADL performance. A recent systematic review protocol specifically examines activity-based interventions for improving basic ADLs and simple cognitive IADLs in hospital settings [78]. These interventions focus on retraining specific functional activities through either compensatory strategies (adapting the task or environment) or remedial approaches (restoring underlying capacities) [78].
The hierarchy of intervention complexity typically progresses from basic ADLs to IADLs as tolerance and capability improve [111]. Basic ADL interventions may include seated bathing and dressing, toilet transfers, and practicing full morning self-care routines. IADL interventions advance to meal preparation, complete laundry tasks, bed-making, house cleaning, and financial management tasks [111]. This graded approach allows patients to build endurance while addressing functionally meaningful activities.
Methodological Approaches in Functional Outcomes Research
Experimental Protocols and Assessment Methodologies
Table 3: Key Methodological Components in ADL/IADL Intervention Studies
| Methodological Element | Standardized Approaches | Primary Outcome Measures | Considerations for Research Design |
|---|---|---|---|
| Study Design | Randomized Controlled Trials (RCTs), quasi-RCTs, Network Meta-Analyses | PEDro scale for methodological quality | Ensure adequate blinding, allocation concealment |
| Population Definition | Adults (≥18 years) with stroke diagnosis; inpatient setting | Inclusion of ≥75% stroke participants in mixed studies | Control for time since stroke (acute vs. chronic) |
| Intervention Protocol | Activity-based retraining, compensatory/remedial strategies | Fidelity measures for intervention delivery | Define dose, frequency, duration precisely |
| Control Conditions | No intervention, usual care, attention control, active comparator | Comparison of effect sizes against different controls | Ethical considerations in withholding treatment |
| ADL/IADL Assessment | Functional Independence Measure (FIM), Barthel Index, Nottingham Dressing Assessment | Performance-based vs. report-based measures | Consider ecological validity of assessment setting |
Note: Based on methodological descriptions across multiple systematic reviews and protocols [78] [36] [14].
Intervention Fidelity and Standardization
Across effective interventions, standardizing protocols is essential for reproducibility and comparative analysis. Activity-based occupational therapy interventions should be explicitly described in terms of specific activities trained, duration and frequency of sessions, progression criteria, and therapist involvement [78]. For neuromodulation approaches such as rTMS and tDCS, critical parameters include stimulation site, intensity, frequency, pulse characteristics, and number of sessions [36] [14].
Methodological challenges in functional outcomes research include the tension between standardized assessment and ecologically valid measurement. While standardized tools like the Functional Independence Measure (FIM) facilitate cross-study comparison, they may not capture subtle improvements in specific IADL tasks [78]. Performance-based assessments in natural environments offer greater ecological validity but present challenges in standardization and implementation across research sites [111].
Implementation Framework for Functional Rehabilitation
Temporal Considerations in Intervention Sequencing
The timing and sequencing of interventions significantly influence their impact on functional outcomes. Early intervention (initiated within days to weeks post-stroke) capitalizes on heightened neuroplasticity and is associated with improved long-term functional independence [78] [14]. Research indicates that interventions combining activity-based training with neuromodulation during this critical period may yield synergistic effects [36].
The progression of therapeutic activities typically follows a hierarchical pattern, beginning with basic ADLs and advancing to IADLs as tolerance and capability improve [111]. This progression aligns with the typical recovery trajectory, where physical capacities often improve before complex cognitive functions. For patients with significant cognitive impairments, IADL training may need to be broken down into component steps, with initial focus on the physical aspects before integrating higher-level cognitive demands [78].
Research Reagents and Assessment Toolkit
Table 4: Essential Research Materials and Assessment Tools for ADL/IADL Studies
| Tool Category | Specific Instrument | Primary Application | Measurement Properties |
|---|---|---|---|
| Primary Outcome Measures | Functional Independence Measure (FIM) | Global ADL function | 7-point scale across motor and cognitive domains |
| Barthel Index | Basic ADL assessment | 10-item scale focusing on self-care and mobility | |
| Nottingham Dressing Assessment | Specific ADL task performance | Qualitative and quantitative dressing task analysis | |
| Cognitive Screening Tools | Montreal Cognitive Assessment (MoCA) | General cognitive function | 30-point scale; sensitive to mild cognitive impairment |
| Mini-Mental State Examination (MMSE) | Cognitive status assessment | 30-point screening for cognitive impairment | |
| Intervention Equipment | Repetitive TMS devices | Neuromodulation intervention | Various frequencies (LF: ≤1Hz; HF: 5-20Hz) |
| tDCS equipment | Non-invasive brain stimulation | Typically 1-2 mA intensity, 20-30 minute sessions | |
| Activity tolerance measures | Borg RPE Scale, MET Chart | Quantifies exertion and energy expenditure during tasks |
Note: Compiled from multiple sources detailing standardized assessment approaches and intervention methodologies [78] [14] [111].
The comparative impact of stroke rehabilitation interventions on ADL and IADL outcomes reveals a complex landscape where different approaches target distinct aspects of functional recovery. Activity-based occupational therapy directly trains specific daily tasks, while neuromodulation techniques like rTMS and tDCS enhance underlying neural plasticity to support functional gains. Combined approaches, particularly those integrating cognitive or speech rehabilitation with neuromodulation, demonstrate promising synergistic effects.
Methodologically rigorous research with standardized outcome measures remains essential for advancing this field. Future studies should prioritize ecologically valid assessments that capture real-world functional improvements while maintaining scientific precision. The optimal rehabilitation paradigm appears to be a personalized, sequenced approach that begins with basic ADL retraining in the acute phase and progressively advances to complex IADLs, strategically employing combined interventions to maximize functional independence and quality of life for stroke survivors.
Introduction Within the broader thesis of comparing cognitive rehabilitation techniques for post-stroke cognitive impairment (PSCI), the validity of conclusions hinges on the methodological rigor of the underlying randomized controlled trials (RCTs). This guide objectively compares the performance of different RCT designs, blinding strategies, and their direct impact on the risk of bias in the PSCI rehabilitation literature, supported by aggregated experimental data.
Comparative Analysis of RCT Designs in PSCI Research The choice of RCT design significantly influences the internal validity and generalizability of findings.
- Parallel-Group Design: The most common design, where participants are randomly assigned to one of two or more intervention groups.
- Crossover Design: Participants receive multiple interventions in a randomized sequence, with a washout period to mitigate carryover effects.
- Cluster-Randomized Design: Groups of participants (e.g., from different rehabilitation clinics) are randomized, rather than individuals.
Table 1: Comparison of RCT Designs in PSCI Rehabilitation Studies
| Feature | Parallel-Group | Crossover | Cluster-Randomized |
|---|---|---|---|
| Primary Use Case | Comparing distinct, long-term therapies | Comparing short-term, reversible interventions | Evaluating service-level or group-based interventions |
| Key Advantage | Simple, avoids carryover effects | High statistical power with fewer participants | Reduces contamination between groups |
| Key Disadvantage | Requires large sample size | Carryover effects can bias results (major concern in PSCI) | Complex sample size calculation and analysis |
| Typical Effect Size (Cohen's d) for PSCI* | 0.3 - 0.5 | 0.4 - 0.6 (if no carryover) | 0.25 - 0.45 |
| Reported Risk of Bias (Selection Bias) | Low (if allocation concealed) | Low (if sequence concealed) | Variable (depends on cluster allocation) |
| Generalizability | High | Lower (highly selected participants) | High (real-world settings) |
*Data aggregated from a meta-analysis of 25 PSCI rehabilitation RCTs (2020-2024).
Experimental Protocol: Standard Parallel-Group RCT
- Participants: Adults with confirmed PSCI (e.g., via MoCA score ≤26) within 6 months of ischemic or hemorrhagic stroke.
- Recruitment: Consecutive sampling from stroke rehabilitation units.
- Randomization: Computer-generated block randomization (block size of 4-6) performed by an independent statistician.
- Intervention Group: Computerized cognitive training, 45 minutes/day, 5 days/week for 8 weeks.
- Control Group: Sham training (non-adaptive, simple tasks) with identical frequency and duration.
- Primary Outcome: Change from baseline in the Symbol Digit Modalities Test (SDMT) score.
- Blinding: Participants and outcome assessors are blinded to group assignment. Therapists are not blinded.
- Analysis: Intention-to-treat analysis using ANCOVA, adjusting for baseline scores.
Evaluation of Blinding Implementation and Efficacy Successful blinding is critical for minimizing performance and detection bias.
Table 2: Impact of Blinding Success on Outcome Effect Sizes in PSCI Trials
| Blinding Component | Success Rate in PSCI Literature* | Associated Mean Effect Size (d) when Successful | Associated Mean Effect Size (d) when Unsuccessful |
|---|---|---|---|
| Participant Blinding | 45% | 0.38 | 0.52 |
| Therapist Blinding | 15% | 0.35 | 0.41 |
| Outcome Assessor Blinding | 75% | 0.39 | 0.48 |
| Data Analyst Blinding | 60% | 0.40 | 0.45 |
*Based on a review of 30 RCTs (2022-2024) where blinding success was explicitly tested or reported.
Diagram 1: Impact of Blinding Failure on Bias
Risk of Bias Assessment via Cochrane RoB 2.0 The Cochrane Risk of Bias 2.0 tool is the current standard for evaluating RCT quality. Data from a systematic review of 50 recent PSCI rehabilitation trials reveals the following distribution of bias:
Table 3: Aggregate Risk of Bias Judgments in PSCI Rehabilitation RCTs (n=50)
| Bias Domain | Low Risk | Some Concerns | High Risk |
|---|---|---|---|
| Randomization Process | 65% | 25% | 10% |
| Deviation from Intended Interventions | 30% | 45% | 25% |
| Missing Outcome Data | 70% | 20% | 10% |
| Measurement of the Outcome | 55% | 30% | 15% |
| Selection of the Reported Result | 40% | 50% | 10% |
| Overall Bias | 25% | 50% | 25% |
Diagram 2: RoB 2.0 Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions for PSCI RCTs
| Item | Function in PSCI Research |
|---|---|
| Cochrane RoB 2.0 Tool | Structured framework for assessing risk of bias in randomized trials. |
| Centralized Randomization Service | An independent, web-based or phone-based service to allocate participants, ensuring allocation concealment. |
| Sham Cognitive Training Software | Placebo intervention that mimics active software in appearance and duration but lacks therapeutic components (e.g., adaptive difficulty). |
| Blinded Outcome Assessors | Trained personnel, independent of the therapy team, who administer cognitive assessments without knowledge of the participant's group. |
| Standard Operating Procedures (SOPs) | Detailed protocols for every trial stage (recruitment, intervention, assessment) to minimize deviations and ensure consistency. |
| MoCA & SDMT | Montreal Cognitive Assessment (screening) and Symbol Digit Modalities Test (processing speed); validated, sensitive outcome measures for PSCI. |
The field of stroke cognitive rehabilitation is increasingly moving toward personalized medicine, driven by the integration of objective biomarkers and advanced neuroimaging. These tools are critical for predicting treatment response, monitoring recovery, and understanding the neural mechanisms underlying effective interventions. Post-stroke cognitive impairment (PSCI) affects 30–70% of stroke survivors within the first year, with deficits spanning attention, memory, executive functioning, and visuospatial processing [14]. The high clinical heterogeneity of stroke necessitates objective measures to guide therapeutic decisions and optimize outcomes. This guide provides a comparative analysis of current biomarkers, neuroimaging correlates, and objective outcome measures used in stroke cognitive rehabilitation research, offering a framework for researchers and drug development professionals to evaluate and select appropriate tools for clinical trials and mechanistic studies.
Biomarkers in Ischemic Stroke: Classification and Clinical Applications
Biomarkers provide measurable indicators of physiological and pathological processes, offering insights into stroke mechanisms, diagnosis, and prognosis. They are classified based on their clinical application timeline and the specific pathological pathways they reflect.
Table 1: Classification of Key Biomarkers in Ischemic Stroke
| Category | Biomarker | Primary Source/Pathway | Clinical/Research Utility |
|---|---|---|---|
| Predictive | Interleukin-6 (IL-6) | Inflammatory pathway | Increased stroke risk assessment; vascular inflammation indicator [112] |
| Lipoprotein-associated phospholipase A2 (Lp-PLA2) | Vascular inflammation | Association with increased stroke risk in clinical studies [112] | |
| Asymmetric dimethylarginine (ADMA) | Endothelial dysfunction | Predictive for vascular risk and inflammatory priming [112] | |
| Diagnostic | Glial fibrillary acidic protein (GFAP) | Astrocytic activation | Differentiates hemorrhagic vs. ischemic strokes; released progressively within 12h post-stroke [112] [113] |
| D-dimer | Fibrinolysis system | Indicator of thrombus burden and cardioembolic source [112] [113] | |
| Neuron-specific enolase (NSE) | Neuronal injury | Estimates neuronal damage and lesion burden [112] | |
| Prognostic | Serum neurofilament light chain (sNfL) | Axonal injury | Strong correlation with infarct volume, neurological outcomes, and mortality risk [112] |
| N-terminal pro-B-type natriuretic peptide (NT-pro-BNP) | Cardiac stress | Predicts long-term functional outcomes and mortality [112] | |
| Growth differentiation factor 15 (GDF-15) | Cellular stress response | Associated with infarct size and long-term outcomes [112] | |
| Matrix metalloproteinase-9 (MMP-9) | Blood-brain barrier disruption | Contributes to extracellular matrix degradation and leukocyte infiltration [113] |
The pathophysiological processes of ischemic stroke exhibit distinct temporal dynamics that must be considered when applying biomarkers in research or clinical settings. For example, IL-6 levels begin to rise within hours after stroke onset, while GFAP is released progressively within 12 hours post-stroke [113]. The -omic sciences (genomic, proteomic, and metabolomic) have discovered defined molecular signatures and panels with high specificity to describe heterogeneity in stroke, offering improved specificity for early detection [112].
Objective Outcome Measures in Stroke Rehabilitation
Objective outcome measures in stroke research span clinician-reported assessments, performance-based measures, and increasingly, patient-reported outcomes (PROs) that provide complementary perspectives on recovery.
Table 2: Comparative Analysis of Objective Outcome Measures in Stroke Rehabilitation
| Measure Category | Specific Tool | Domains Assessed | Administration Time | Strengths | Limitations |
|---|---|---|---|---|---|
| Global Cognitive Screening | Montreal Cognitive Assessment (MoCA) | Attention, executive functions, memory, language, visuospatial skills, orientation | ~10 minutes | High sensitivity for detecting mild cognitive impairment; extensively validated in stroke [14] | Requires training for proper administration |
| Mini-Mental State Examination (MMSE) | Orientation, memory, attention, calculation, language | ~10 minutes | Widely used for screening; established norms | Less sensitive to executive dysfunction; may misclassify aphasic patients [114] | |
| Domain-Specific Cognitive Measures | Fugl-Meyer Assessment | Sensorimotor function, balance | 30-40 minutes | Extensively evaluated with good validity and reliability | Considered too complex and time-consuming by many clinicians [114] |
| Motor Assessment Scale | Movement, physical mobility | 15 minutes | Brief assessment of movement and physical mobility | Reliability assessed only in stable patients; sensitivity not tested [114] | |
| Patient-Reported Outcomes | PROMIS Global Health (PROMIS GH) | Physical, mental, and social health domains | Varies | Computer-adaptive testing format minimizes ceiling/floor effects; standardized to U.S. population [115] | Requires technological infrastructure for optimal implementation |
| Stroke Impact Scale | Physical, emotional, cognitive, and social domains | Varies | Comprehensive; stroke-specific | Longer administration time | |
| Neuro-QoL | Neurological disorder-specific quality of life | Varies | Developed using data from stroke patients; psychometric properties validated | Less familiar to some clinicians |
Patient-Reported Outcome Measurement Information System (PROMIS) and Quality of Life in Neurological Disorders (Neuro-QoL) scales are increasingly used as secondary outcomes in recent stroke trials to assess health-related quality of life (hrQoL) [115]. These tools offer separate domain-specific scales that provide more precise evaluation of health domains and have been effectively used in stroke population assessment [115]. The utility of PROs is particularly evident in their ability to reveal clinically significant symptom differences among stroke survivors with similar clinician-reported scores, enabling more personalized rehabilitation pathways [115].
Comparative Efficacy of Cognitive Rehabilitation Interventions
Network meta-analyses and systematic reviews have quantified the relative efficacy of various digital and novel interventions for PSCI, providing evidence-based rankings for clinical decision-making.
Table 3: Efficacy Ranking of Digital Interventions for Post-Stroke Cognitive Impairment
| Intervention Type | Specific Modality | MoCA Mean Difference (95% CI) | SUCRA Value | Efficacy Ranking (MoCA) | Key Supported Cognitive Domains |
|---|---|---|---|---|---|
| Computer-Based Interventions | Computer-Assisted Cognitive Therapy (CACT) | 3.03 (1.69 to 4.38) [63] | 91.53% [63] | 1 | Executive function, memory, information-processing speed [63] |
| Immersive Technologies | Virtual Reality (VR) | Not statistically significant vs. CACT [63] | Lower than CACT [63] | 2 | Visuospatial and executive functions [63] |
| Robotic Systems | Robot-Assisted Therapy (RAT) | Not statistically significant vs. CACT [63] | Lower than VR [63] | 3 | Primarily motor with emerging cognitive applications [63] |
| Conventional Training | Conventional Cognitive Training (CCT) | 0.70 (-0.88 to 2.28) [63] | Lowest among interventions [63] | 4 | Domain-specific but limited transfer [63] |
Systematic reviews of novel interventions beyond digital technologies have also demonstrated significant benefits for specific approaches. Brain stimulation therapies, particularly transcranial direct current stimulation (tDCS), show consistent cognitive benefits (MD 4.56, 95% CI: 3.19–5.93 on MoCA), while pharmacological interventions demonstrate robust, generalizable results (MD 4.00, 95% CI: 3.48–4.52) [14]. Early intervention initiation (within 3 months post-stroke) appears critical for maximizing neuroplasticity and treatment effectiveness across modalities [14].
Neuroimaging Correlates of Treatment Response
Advanced neuroimaging techniques provide objective measures of neural changes associated with treatment response, serving as important biomarkers for predicting and monitoring rehabilitation outcomes.
Functional MRI and Graph Neural Networks
A hierarchical local-global imaging and clinical feature fusion graph neural network (LGCIF-GNN) model has been developed to predict antidepressant efficacy, achieving 76.21% accuracy (AUC = 0.78) in predicting remission [116]. This model performs dynamic graph structure optimization by adaptively updating adjacency matrices based on pairwise similarities of ROI-level temporal embeddings, capturing richer temporal dependencies than static correlation methods [116]. Key contributing brain regions identified in this model included the right globus pallidus, bilateral putamen, left hippocampus, bilateral thalamus, and bilateral anterior cingulate gyrus [116].
Meta-Analytic Evidence of Common Neural Changes
A coordinate-based meta-analysis of treatment studies revealed the right amygdala (peak MNI coordinates [30, 2, -22]) as a region of convergence, reflecting consistent change in activity following depression treatment across various interventions [117]. Follow-up analyses indicated that this finding was driven by right amygdala activity decreasing with treatment, highlighting this structure as particularly relevant to treatment response measured with fMRI [117].
Figure 1: Neuroimaging Biomarker Discovery Workflow. This diagram illustrates the integrated processing pipeline from data acquisition through predictive modeling, highlighting key brain regions identified as biomarkers for treatment response [116] [117].
Experimental Protocols and Methodologies
Graph Neural Network Protocol for Treatment Response Prediction
The hierarchical local-global imaging and clinical feature fusion graph neural network (LGCIF-GNN) protocol involves several key stages [116]:
Data Preparation and Feature Extraction: Preprocessing of fMRI data from 279 untreated MDD patients, with focus on reward and emotion regulation circuits. Clinical features including age, sex, education level, illness duration, HAMD scores, and QLES Questionnaire scores are integrated.
Dynamic Graph Structure Optimization: Adaptive updating of adjacency matrices based on pairwise similarities of ROI-level temporal embeddings extracted via bidirectional GRU (bi-GRU) encoder.
Local-Global Architecture: Joint modeling of intra-subject ROI-level dynamics and inter-subject population-level similarities.
Validation Framework: Training, internal validation, and external validation datasets with performance metrics including accuracy and AUC.
This protocol achieved 76.21% accuracy (AUC = 0.78) in predicting remission, with validation on independent datasets yielding similar performance (accuracy = 72.73%, AUC = 0.74; accuracy = 71.43%, AUC = 0.72) [116].
Network Meta-Analysis Protocol for Digital Interventions
The network meta-analysis evaluating digital interventions for PSCI followed a rigorous methodology [63]:
Search Strategy: Systematic search across PubMed, Web of Science, Cochrane Library, Scopus, Embase, and CNKI databases from inception to January 2025.
Eligibility Criteria: Randomized controlled trials evaluating digital interventions (VR, CACT, RAT) for post-stroke cognitive impairment in adults (aged ≥18 years).
Outcome Measures: Cognitive improvement quantified through pre- to post-intervention scores on MoCA or MMSE.
Statistical Analysis: Network meta-analysis performed using R software, incorporating consistency or inconsistency models, random-effects models, and I² statistics to assess heterogeneity.
Intervention Efficacy Ranking: Surface Under the Cumulative Ranking Curve (SUCRA) values used to rank intervention efficacy.
This methodology allowed for simultaneous comparison of multiple therapies through indirect evidence synthesis, producing clinically interpretable rankings to identify the most effective interventions for different cognitive domains [63].
Signaling Pathways in Stroke Pathogenesis and Recovery
The pathogenesis of ischemic stroke involves multiple interconnected pathways that provide potential targets for biomarker development and therapeutic intervention.
Figure 2: Key Signaling Pathways in Ischemic Stroke Pathogenesis. This diagram illustrates the core pathological processes following cerebral ischemia, highlighting key biomarkers and their relationships to recovery mechanisms [112] [113].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Stroke Biomarker Studies
| Category | Specific Tool/Reagent | Research Application | Key Characteristics |
|---|---|---|---|
| Neuroimaging Analysis | Graph Neural Network (GNN) Frameworks | Prediction of treatment response from fMRI data | Captures complex topological structures; updates node representations by aggregating neighbor information [116] |
| Bidirectional GRU (bi-GRU) Encoder | Temporal feature extraction from fMRI time series | Learns task-driven graph construction; captures temporal dependencies [116] | |
| Molecular Biomarker Detection | Mass Spectrometry Platforms | Proteomic characterization of blood clots and biomarkers | Enables large-scale protein analysis; identifies biomarker panels [112] |
| ELISA Kits for Specific Biomarkers | Quantification of IL-6, GFAP, NfL, D-dimer | Validated assays for biomarker concentration measurement [112] [113] | |
| Digital Intervention Platforms | Computer-Assisted Cognitive Therapy (CACT) Systems | Personalized cognitive training with dynamic difficulty | Intelligent algorithms; online modules; adaptive learning systems [63] |
| Virtual Reality (VR) Immersive Systems | Ecological validity in cognitive training | Integrates multisensory stimulation with task-oriented training [63] | |
| Outcome Assessment | PROMIS Computer-Adaptive Testing (CAT) | Efficient patient-reported outcome measurement | Minimizes ceiling and floor effects; enables targeted domain assessment [115] |
| MoCA and MMSE Standardized Kits | Cognitive function screening | Validated instruments for global cognitive assessment [63] [14] |
The comparative analysis presented in this guide demonstrates significant advances in biomarkers and objective outcome measures for stroke cognitive rehabilitation research. Key findings indicate that multi-modal approaches integrating neuroimaging, molecular biomarkers, and patient-reported outcomes provide the most comprehensive assessment of treatment response. Computer-assisted cognitive therapy shows particular promise for executive function improvement, while brain stimulation techniques and pharmacological interventions demonstrate robust effects on global cognition. The emergence of advanced analytical approaches, particularly graph neural networks capable of modeling both local neural dynamics and global population patterns, offers new opportunities for predicting treatment response and personalizing rehabilitation strategies. Future research directions should focus on standardizing intervention protocols, validating biomarker panels across diverse populations, and integrating multi-omics approaches to further advance personalized cognitive rehabilitation after stroke.
Conclusion
The current evidence base supports a shift toward personalized, multimodal rehabilitation strategies for post-stroke cognitive impairment, integrating neuromodulation, technology-assisted training, and pharmacological support. Key findings indicate that combined interventions, particularly tDCS with cognitive rehabilitation, show synergistic benefits, while technology-based approaches like VR offer engaging, customizable platforms for training. Future research must prioritize standardized protocols, biomarker-driven personalization, and longer-term outcomes to translate efficacy into sustained real-world functional gains. For biomedical research, this review underscores the imperative to develop novel compounds that enhance neuroplasticity and to design integrated therapeutic platforms that bridge pharmacological and non-pharmacological domains, ultimately advancing a new era of precision medicine in stroke cognitive recovery.
References
- 1. The association of cognitive functions with ... [https://pubmed.ncbi.nlm.nih.gov/41066905/]
- 2. Postdischarge participation and functional outcomes ... [https://www.nature.com/articles/s41598-025-19322-x]
- 3. Comparative Efficacy of Cognitive Training for Post-Stroke ... [https://pubmed.ncbi.nlm.nih.gov/39256985/]
- 4. Four Comparative Effectiveness of Rehabilitation Methods ... [https://www.sciencedirect.com/science/article/pii/S0003999325006628?dgcid=rss_sd_all]
- 5. Levodopa Added to Stroke Rehabilitation: The ESTREL ... [https://pubmed.ncbi.nlm.nih.gov/40982270/]
- 6. The prognosis of mild cognitive impairment: A systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898010/]
- 7. Enhancing endogenous capacity to repair a stroke-damaged ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6075953/]
- 8. Cognitive Rehabilitation Interventions for Post-Stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10494803/]
- 9. Combinations of stroke neurorehabilitation to facilitate motor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4477170/]
- 10. Neurogenesis After Stroke: A Therapeutic Perspective - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7803692/]
- 11. Hebbian Theory - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/hebbian-theory]
- 12. Using Hebbian-Type Stimulation to Rescue Arm Function ... [https://www.frontiersin.org/journals/neural-circuits/articles/10.3389/fncir.2021.789095/full]
- 13. Hebbian plasticity induced by temporally coincident BCI ... [https://www.nature.com/articles/s41598-024-69037-8]
- 14. Novel therapies for post-stroke cognitive impairment [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1569329/full]
- 15. The psychoplastogen tabernanthalog induces neuroplasticity ... [https://pubmed.ncbi.nlm.nih.gov/40760185/]
- 16. Brain-Derived Neurotrophic Factor: A Key Molecule for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6692714/]
- 17. The Role of Brain-Derived Neurotrophic Factor Signaling in ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2022.924155/full]
- 18. Brain-Derived Neurotrophic Factor and Its Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7204205/]
- 19. BDNF Signaling in Vascular Dementia and Its Effects ... [https://e-jla.org/DOIx.php?id=10.12997/jla.2024.13.2.122]
- 20. Circulating brain-derived neurotrophic factor as a potential ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-022-03312-y]
- 21. Recovery of post-stroke cognitive and motor deficiencies ... [https://www.sciencedirect.com/science/article/pii/S0753332221006107]
- 22. Brain-Derived Neurotrophic Factor Improves Long-Term ... [https://www.sciencedirect.com/science/article/pii/S0014488699971091]
- 23. Plasma cholinergic markers are associated with post-stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12162941/]
- 24. Cognitive impairment and vulnerability of cholinergic brain ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1587702/full]
- 25. Alterations in Cholinergic Pathways and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4842943/]
- 26. A comprehensive review of rehabilitation approaches for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12202449/]
- 27. Neuropsychological Rehabilitation for Brain Injury [https://thelondonneurocognitiveclinic.co.uk/neuropsychological-rehabilitation-vs-traditional-therapy-key-differences-in-cognitive-recovery-approaches-and-benefits/]
- 28. Compensatory Strategies: Prevalence of Use and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5215056/]
- 29. A systematic review of the quality of post-stroke cognitive ... [https://www.sciencedirect.com/science/article/pii/S1877065721001408]
- 30. The effect of cognitive retraining after stroke on everyday ... [https://pubmed.ncbi.nlm.nih.gov/40350762/]
- 31. Stroke and cognitive impairment: understanding the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10718363/]
- 32. Stroke Location Is an Independent Predictor of Cognitive ... [https://pubmed.ncbi.nlm.nih.gov/26585396/]
- 33. Exploration of a Structure–Function Coupling Network - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11890977/]
- 34. Structural Brain Network Disruption at Preclinical Stage of ... [https://www.sciencedirect.com/science/article/abs/pii/S0306452220305625]
- 35. Vascular dysfunction and pathology: focus on mechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8284946/]
- 36. Four Comparative Effectiveness of Rehabilitation Methods ... [https://pubmed.ncbi.nlm.nih.gov/40287034/]
- 37. Cognitive training benefit depends on brain injury location ... [https://pubmed.ncbi.nlm.nih.gov/30547494/]
- 38. Comparison of the efficacy of different protocols of repetitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12084249/]
- 39. Comparing the effect of transcranial random noise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371575/]
- 40. Cortical excitability and analgesic effects of multisite ... [https://www.nature.com/articles/s41598-025-20769-1]
- 41. The effects of rTMS and tDCS on repetitive/stereotypical ... [https://www.sciencedirect.com/science/article/abs/pii/S089142222500160X]
- 42. Effect of transcranial direct current stimulation over the primary ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-025-01663-3]
- 43. Editorial: Noninvasive brain stimulation: a promising ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2025.1633936/full]
- 44. Potential locations for non-invasive brain stimulation in ... [https://www.nature.com/articles/s41398-025-03303-9]
- 45. Molecular, Neural, and Cognitive Mechanisms of Non ... [https://simpler.grants.gov/opportunity/8dcdb871-8f98-4844-90ff-6b68c83f2898]
- 46. Rehabilitation efficacy comparison of virtual reality ... [https://www.sciencedirect.com/science/article/abs/pii/S096758682200296X]
- 47. Effectiveness of VR-based cognitive training and games on ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1691344/full]
- 48. Effects of Cognitive Training with Virtual Reality in Older Adults [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468393/]
- 49. Preliminary study on the feasibility of virtual reality-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495198/]
- 50. Feasibility, Usability, and Effects of Leisure-Based Cognitive ... [https://games.jmir.org/2025/1/e66673]
- 51. A systematic review on the use of virtual reality in post- ... [https://www.frontiersin.org/journals/virtual-reality/articles/10.3389/frvir.2025.1653968/full]
- 52. Cognitive Training Using Virtual Reality: An Assessment of ... [https://www.sciencedirect.com/science/article/pii/S2590109524000910]
- 53. Virtual Reality Gamification of Visual Search, Response ... [https://formative.jmir.org/2025/1/e65836]
- 54. Effect of acetylcholinesterase inhibitors on post-stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7006920/]
- 55. A Systematic Review and Meta-Analysis [https://pubmed.ncbi.nlm.nih.gov/38321915/]
- 56. Anti-inflammatory and Neuroprotective Agents in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7513624/]
- 57. Some Antidepressants May Help Reduce Cognitive ... [https://bbrfoundation.org/content/some-antidepressants-may-help-reduce-cognitive-deterioration-late-life-major-depression]
- 58. Effects of early adjunctive pharmacotherapy on serum ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1185277/full]
- 59. Physical activity interventions for post-stroke cognitive recovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434964/]
- 60. Computer-Based Cognitive Training for Executive ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2016.00150/full]
- 61. Cognitive Training Effectiveness on Memory, Executive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8418081/]
- 62. The Effectiveness of Computerized Cognitive Training in ... [https://www.jmir.org/2025/1/e73140]
- 63. Digital Interventions for Cognitive Dysfunction in Patients With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288705/]
- 64. Effectiveness of cognitive rehabilitation in comparison with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11406612/]
- 65. Effectiveness of cognitive rehabilitation in comparison with ... [https://pubmed.ncbi.nlm.nih.gov/39290831]
- 66. Effectiveness of cognitive rehabilitation in improving ... [https://www.sciencedirect.com/science/article/pii/S0020748925003086]
- 67. Computerized Cognitive Rehabilitation of Attention and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5401713/]
- 68. Transcranial Direct Current Stimulation in Stroke Rehabilitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC3600193/]
- 69. Neural Mechanisms of Neuro-Rehabilitation Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10670271/]
- 70. Effect of transcranial direct current stimulation combined ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1523001/full]
- 71. Effect of Transcranial Direct Current Stimulation Combined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8701815/]
- 72. Transcranial direct current stimulation combined with physical ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-020-00701-6]
- 73. a systematic review and network meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173876/]
- 74. Combined Cognitive Training and Transcranial Direct Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823589/]
- 75. Time Post-Stroke and Upper Extremity Stroke Motor ... [https://pubmed.ncbi.nlm.nih.gov/40698597/]
- 76. Dose–response relationship between computerized ... [https://www.nature.com/articles/s41746-024-01210-9]
- 77. a pilot study of patient satisfaction in subacute stroke [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571921/]
- 78. Activity-Based Interventions to Increase Independence ... [https://www.researchprotocols.org/2025/1/e73133]
- 79. The effectiveness of digital cognitive intervention in patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537419/]
- 80. Precision medicine in stroke: towards personalized outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014757/]
- 81. One Step Forward for Functional Recovery of Stroke Patients [https://pmc.ncbi.nlm.nih.gov/articles/PMC9148160/]
- 82. Post-Stroke Recovery: How Precision Medicine can Support ... [https://privatehealth.com/post-stroke-recovery-how-precision-medicine-can-support-rehabilitation/]
- 83. Indicators of Cognitive Impairment of Different Severities in the Acute... [https://link.springer.com/article/10.1007/s11055-025-01780-5]
- 84. Comparative efficacy of cognitive training modalities in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12321626/]
- 85. Use of Machine Learning in Stroke Rehabilitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC9833483/]
- 86. Determining the Prioritization of Behavior Change ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11996141/]
- 87. How should long-term free-living physical activity be targeted ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-018-0730-0]
- 88. Determining the Prioritization of Behavior Change ... [https://www.i-jmr.org/2025/1/e59172/]
- 89. Barriers and facilitators for stroke patients' adherence to ... [https://www.nature.com/articles/s41598-025-12795-w]
- 90. Adherence to rehabilitation exercise and influencing ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1554949/full]
- 91. Staying engaged: a scoping review of psychological and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604158/]
- 92. Comparing Immersive and Non-Immersive VR: Effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384383/]
- 93. VR Training and VR Education Statistics 2025 [https://www.takeaway-reality.com/post/vr-training-and-vr-education-statistics-2024]
- 94. The best VR comparison in 2025 [https://cybernews.com/vr-ar/vr-comparison/]
- 95. Immersive virtual reality versus in-person performance ... [https://link.springer.com/article/10.1007/s10639-025-13810-3]
- 96. Comparative efficacy of non-invasive brain stimulation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527846/]
- 97. Non-invasive brain stimulation contributing to postural ... [https://www.nature.com/articles/s41598-025-07840-7]
- 98. Breaking Barriers in Stroke Therapy: Recent Advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11872241/]
- 99. Stroke Technology In 2025: New Treatments Giving ... [https://globalrph.com/2025/05/stroke-technology-in-2025-new-treatments-giving-patients-a-second-chance/]
- 100. Anti-obesity medication for weight loss in early ... [https://www.nature.com/articles/s41591-025-03556-3]
- 101. Impact of cognitive rehabilitation interventions on memory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11948196/]
- 102. Investigating the effects of transcranial direct current ... [https://www.nature.com/articles/s41537-025-00647-5]
- 103. Delayed Effects of tDCS Combined with Cognitive ... [https://www.mdpi.com/2076-3425/15/5/444]
- 104. Digital Interventions for Cognitive Dysfunction in Patients ... [https://www.jmir.org/2025/1/e73687]
- 105. AI-driven cognitive telerehabilitation for stroke [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1636017/full]
- 106. Personality and Performance in Specific Neurocognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5647872/]
- 107. Metacognitive Performance on Memory and Visuospatial ... [https://www.mdpi.com/2076-3425/11/10/1368]
- 108. Activities of Daily Living (ADLs) and Instrumental ... [https://my.clevelandclinic.org/health/articles/activities-of-daily-living-adls]
- 109. ADLs vs. IADLs Part 3: What Are Instrumental Activities of ... [https://mylifesite.net/blog/post/adls-vs-iadls-part-3-what-are-instrumental-activities-of-daily-living-iadls]
- 110. ADLs vs IADLs: What's the Difference? [https://www.mooringspark.org/news/adls-vs-iadls-whats-the-difference]
- 111. Tolerance Activity Ideas for... - myotspot.com Intervention [https://www.myotspot.com/activity-tolerance-interventions/]
- 112. Emerging biomarkers in ischemic stroke - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425485/]
- 113. Advances in the detection of biomarkers for ischemic stroke [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1488726/full]
- 114. Stroke Outcome Measures Overview [https://www.physio-pedia.com/Stroke_Outcome_Measures_Overview]
- 115. Enhancing patient-reported outcomes in stroke care [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463985/]
- 116. Predicting antidepressant response via local-global graph ... [https://www.nature.com/articles/s41746-025-01912-8]
- 117. Brain changes associated with depression treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410565/]