Bregma and Lambda: Mastering Skull Landmarks for Precision Rodent Stereotaxic Surgery
This article provides a comprehensive guide to the critical skull landmarks, bregma and lambda, in rodent stereotaxic surgery.
Bregma and Lambda: Mastering Skull Landmarks for Precision Rodent Stereotaxic Surgery
Abstract
This article provides a comprehensive guide to the critical skull landmarks, bregma and lambda, in rodent stereotaxic surgery. Tailored for researchers, scientists, and drug development professionals, it covers the foundational neuroanatomy of these landmarks, detailed methodological protocols for their use in surgical targeting, strategies for troubleshooting common errors and optimizing accuracy, and a validation of techniques through comparison with modern digital atlases. The content synthesizes current research and best practices to empower scientists in achieving highly reproducible and precise intracranial interventions, thereby enhancing experimental validity and supporting the principles of the 3Rs (Replacement, Reduction, and Refinement) in animal research.
The Neuroanatomical Basis: Defining Bregma, Lambda, and the Stereotaxic Coordinate System
The advent of the stereotaxic apparatus by Victor Horsley and Robert Clarke in 1906 revolutionized neuroscience research by enabling precise three-dimensional navigation within the brain [1]. This foundational technology, based on a Cartesian coordinate system, allows researchers to target specific brain structures with remarkable accuracy. In rodent models, this technique relies critically on external skull landmarks, particularly the bregma and lambda points, to define the coordinate system origin and alignment [1] [2]. Despite its widespread adoption, challenges persist in consistently identifying these landmarks, with recent studies revealing significant discrepancies that can impact surgical outcomes [1] [2]. This technical guide explores the principles, applications, and refinements of stereotaxic technology, with emphasis on proper bregma and lambda identification to enhance precision in rodent neurosurgery.
Historical Development and Fundamental Principles
Origins of Stereotaxic Technology
The conceptual foundation for stereotaxic surgery emerged in 1889 when Professor Dmitry Nikolaevich Zernov introduced the "encephalometer," which used a geographical map concept around the head with an equator and meridian for spatial navigation [1]. However, the first stereotaxic apparatus in its modern form was developed by Victor Horsley (a neurosurgeon) and Robert Clarke (a physiologist) in 1906 [1] [3]. Their collaborative work produced an apparatus that allowed precise navigation along three axes in the monkey skull based on the Cartesian coordinate system [1]. This groundbreaking invention ignited the field of stereotactic neurosurgery, which Spiegel and Wycis later adapted for human procedures in 1947 [3].
The Cartesian Coordinate System in Stereotaxic Navigation
The Horsley-Clarke apparatus implements a 3D Cartesian system with three fundamental axes [1]:
- Mediolateral (ML) axis: x-axis representing left-right movement
- Anteroposterior (AP) axis: y-axis representing front-back movement
- Dorsoventral (DV) axis: z-axis representing up-down movement
This coordinate system enables researchers to define any point within the brain using three numerical coordinates relative to a defined origin point [3]. The mathematical foundation relies on affine conversions between coordinate systems using matrices that specify rotation, scaling, and translation parameters [3]. The relationship between different coordinate spaces (anatomical, frame-based, and head-stage) follows the transformation formula: T = R × S × P + t, where R is rotation, S is scaling, P is the original coordinate, and t is translation [3].
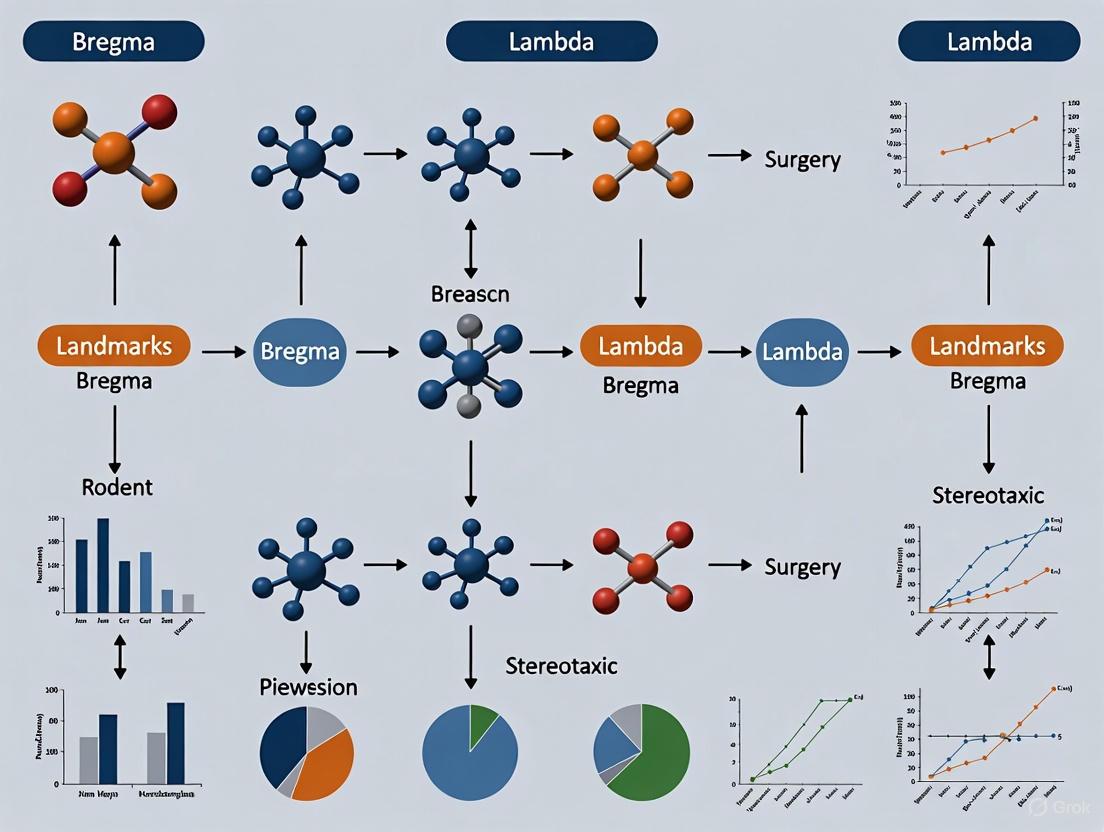
Figure 1: Stereotaxic Navigation Workflow. The process begins with identification of skull landmarks (bregma and lambda) to establish a 3D coordinate system, which is then translated through mathematical transformations into frame-based navigation parameters to reach target brain structures, often with reference to stereotaxic atlases.
Rodent Skull Landmarks: Bregma and Lambda
Anatomical Definitions and Significance
In rodent stereotaxic surgery, the skull provides the critical reference points for establishing coordinate systems. The adult mouse skull comprises 26 bones and joints connected by sutures [1]. Three key sutures are visible from a dorsal view:
- Coronal suture: A parabolic curve between the frontal and parietal bones
- Sagittal suture: Divides the skull into two halves along the medial line
- Lambdoidal suture: Resembles the Greek letter lambda at the posterior skull
The bregma point is defined as the intersection of the coronal and sagittal sutures, while the lambda occurs at the intersection of the sagittal and lambdoidal sutures [1]. The bregma serves as the most common origin point (0,0,0) for the stereotaxic coordinate system in rodents, while lambda is essential for aligning the dorsoventral coordinates and ensuring proper head leveling [1] [4].
Technical Challenges in Landmark Identification
A significant challenge in stereotaxic surgery is the accurate and consistent identification of the bregma point. The renowned Paxinos and Franklin brain atlases, while widely used, lack explicit instructions for bregma determination [1]. Compounding this problem, many researchers incorrectly assume the bregma is simply the crossing point of the coronal and sagittal sutures. However, Paxinos and Watson specifically define bregma as the "midpoint of the curve of best fit along the coronal suture" – a mathematically ambiguous definition that contributes to variability in identification [2].
Recent studies have revealed concerning discrepancies in skull and brain landmark measurements. Research comparing different identification methods found that in 44% of animals (11 out of 25), the traditional approach to locating bregma differed from a more precise mathematical method by ≥0.2 mm [2]. This variation exceeds the size of many rodent brain nuclei and subregions, potentially compromising experimental outcomes.
Enhanced Bregma Localization Methodology
To address these challenges, a novel computer-assisted method for bregma identification has been developed [2]:
- Digital Imaging: Capture a high-resolution digital picture of the exposed skull cap
- Mathematical Fitting: Mathematically fit a curve to the outline of the coronal suture
- Midline Determination: Delineate the brain midline based on the temporal ridges of the skull
- Point Calculation: Define the bregma as the intersection point of these two lines
This refined approach significantly decreases stereotaxic error compared to traditional visual estimation methods [2]. Implementation of this technique requires:
- Digital camera or microscope with imaging capabilities
- Image processing software capable of curve fitting
- Understanding of basic skull anatomy for landmark verification
Table 1: Comparison of Bregma Identification Methods
| Method | Technique | Precision | Error Rate | Advantages |
|---|---|---|---|---|
| Traditional Visual | Visual estimation of suture intersection | >0.2 mm in 44% of cases | High | Fast, requires no special equipment |
| Mathematical Fitting | Computer-assisted curve fitting to coronal suture | Significantly improved | Reduced by >50% | Objective, reproducible, higher accuracy |
| Paxinos Definition | Midpoint of curve of best fit along coronal suture | Variable interpretation | Moderate | Standardized reference |
Stereotaxic Apparatus and Instrumentation
Evolution of Stereotaxic Equipment
Modern stereotaxic instruments for rodents have evolved significantly from the original Horsley-Clarke design while maintaining the same fundamental principles. Contemporary systems typically include:
- A horizontal base plate
- One or two micromanipulators affixed to the frame
- Specialized holders for electrodes, syringes, or cannulas
- Species-specific ear bars and head holders for stabilization [1]
Several companies manufacture stereotaxic equipment, including Kopf Instruments, RWD Life Science, Harvard Apparatus, World Precision Instruments, and Stoelting Company [1]. Recent technological advances have introduced digital displays, motorized controls, and even integrated warming systems to maintain rodent body temperature during surgical procedures [5] [6].
Technical Specifications of Modern Systems
Contemporary stereotaxic instruments offer varying levels of precision to accommodate different research needs:
Table 2: Comparison of Modern Stereotaxic Instrument Specifications
| Manufacturer | Model Type | Precision Range | Key Features | Animal Applications |
|---|---|---|---|---|
| World Precision Instruments | Ultra Precise Digital | 1 micron (0.001 mm) | Digital LED display, integrated warming base, dual manipulator capability | Mice and small rodents (10-75g) |
| Stoelting Co. | Just for Mouse Series | 1-100 microns | Warmer-ready base, gas anesthesia compatible, small footprint (25×25cm) | Transgenic and knock-out mice |
| RWD Life Science | Automated Stereotaxic Instrument | 1 μm | Integrated brain atlas software, anti-collision function, automatic procedures | Mice, rats, and large animals |
| RWD Life Science | Digital Stereotaxic | 10 μm | Digital display module, displacement sensor, arbitrary origin setting | Rats and mice |
Modern innovations include 3D-printed headers that integrate multiple functions, significantly reducing surgical time. One study demonstrated that such modifications decreased total operation time by 21.7%, primarily by streamlining the bregma-lambda measurement process [7].
Experimental Protocols and Methodological Considerations
Standard Stereotaxic Surgical Procedure
A refined stereotaxic surgery protocol for rodents incorporates technical improvements that enhance survival and precision [4]:
Pre-surgical Preparation
- Pre-warm the heating pad to maintain body temperature (37.5-38.5°C)
- Administer anesthesia (e.g., ketamine/dexmedetomidine mixture)
- Shave the head area from ears to between the eyes
- Apply eye cream to prevent corneal dehydration
- Ensure adequate blood oxygenation (>90%) throughout procedure
Head Positioning and Landmark Identification
- Place the animal in the stereotaxic apparatus with equal ear bar readings on both sides
- Clean the skull surface and expose bregma and lambda
- Level the head by ensuring identical dorsoventral coordinates at bregma and lambda (difference <0.3 mm) [4]
- Record the anteroposterior and lateral coordinates at bregma
Coordinate Calculation and Targeting
- Calculate target coordinates relative to bregma using a stereotaxic atlas
- Mark the cannula locations on the skull
- Drill burr holes at calculated coordinates
- Gently puncture the meninges to allow unobstructed cannula insertion
Surgical Implementation and Recovery
- Lower the cannula or electrode carefully to the final ventral coordinate
- Apply dental cement to fix the implant in place
- Administer warm sterile saline (~10 ml/kg, subcutaneously) for rehydration
- Monitor the animal closely during recovery, maintaining thermal support
Impact of Technical Refinements on Surgical Outcomes
Implementation of refined techniques significantly improves surgical outcomes. Studies demonstrate that modified protocols incorporating active warming systems and improved landmark identification reduce non-survival rates and minimize postoperative weight loss [4] [7]. Specifically, the use of active warming pads to prevent hypothermia (a common complication of isoflurane anesthesia) increased survival rates from 0% to 75% in one severe TBI model study [7].
Furthermore, the implementation of continuous monitoring of blood oxygenation, heart rate, and body temperature throughout the procedure has been shown to significantly enhance postoperative recovery and reduce complications [4].
The Scientist's Toolkit: Essential Research Equipment and Reagents
Table 3: Essential Materials for Rodent Stereotaxic Surgery
| Item | Function | Technical Specifications | Example Applications |
|---|---|---|---|
| Stereotaxic Frame | Precise 3D navigation | Precision: 1-100 μm, Weight capacity: 10-75g (mice) | All stereotaxic procedures |
| Digital Coordinate Display | Accurate coordinate reading | Resolution: 1 μm, LED display for low-light conditions | High-precision targeting |
| Active Warming System | Maintain body temperature | PID controlled, target temperature: 37.5-38.5°C | Prolonged surgeries, prevention of hypothermia |
| Gas Anesthesia System | Maintain surgical anesthesia | Isoflurane with oxygen mixture (30-35% O₂) | All survival surgeries |
| Rodent Stereotaxic Atlas | Target coordinate reference | Paxinos & Franklin, Allen Brain Atlas | Coordinate determination |
| Microdrill | Create burr holes in skull | 0.5-1.0 mm drill bits, precise depth control | Access to brain structures |
| Dental Cement | Secure implants to skull | Fast-setting, biocompatible | Chronic implant fixation |
| Skull Screws | Anchor dental cement | 0.5-1.0 mm diameter, stainless steel | Chronic implant stability |
| Analgesics | Post-operative pain management | Carprofen (4.0-5.0 mg/kg) | Animal welfare compliance |
The Horsley-Clarke stereotaxic apparatus represents a foundational technology in neuroscience research, enabling unprecedented precision in accessing specific brain regions. The proper identification of bregma and lambda landmarks remains crucial for accurate targeting, with recent methodological refinements significantly improving precision through mathematical approaches to landmark identification. Contemporary technological advances, including digital displays, active warming systems, and computer-assisted planning, have further enhanced the capabilities of stereotaxic systems while improving animal welfare outcomes. As stereotaxic techniques continue to evolve, maintaining focus on accurate landmark identification and implementation of refined surgical protocols will ensure the continued utility of this powerful methodology in advancing our understanding of brain function and pathology.
The bregma is a fundamental cranial landmark defined as the point on the superior aspect of the skull where the coronal suture intersects perpendicularly with the sagittal suture [8] [9]. This anatomical junction marks the convergence of three skull bones: the frontal bone anteriorly and the two parietal bones posteriorly and laterally [8]. The term itself is derived from the Ancient Greek word brégma, meaning "the bone directly above the brain" [8]. In neonatal and infant anatomy, this location corresponds to the site of the anterior fontanelle, a membranous, unossified area that allows for skull flexibility during birth and rapid brain growth postnatally [8] [9]. This fontanelle typically closes between 18 and 36 months of life as the surrounding bones fuse, forming the definitive bregma point seen in adulthood [8]. Its consistent and identifiable nature makes it an indispensable reference point across multiple disciplines, including clinical neurology, neurosurgery, anthropology, and particularly in preclinical neuroscience research using rodent models.
Bregma in Rodent Stereotaxic Surgery
In experimental neuroscience, the bregma is the cornerstone of the stereotaxic coordinate system for targeting specific brain regions in rodent models. The stereotaxic apparatus operates on a three-dimensional Cartesian coordinate system, where the bregma most commonly serves as the origin point (0,0,0) for the anteroposterior (AP), mediolateral (ML), and dorsoventral (DV) axes [1] [10]. To establish a level skull position—a critical prerequisite for accurate coordinate translation—the lambda (the junction of the sagittal and lambdoid sutures) is aligned to the same dorsoventral height as the bregma [11]. This "flat-skull position" ensures that the horizontal plane is consistent with the reference planes used in stereotaxic brain atlases [11].
Despite its widespread adoption, used in 96% of stereotaxic surgery publications, targeting accuracy can be variable [10]. A critical review of practice reveals that while bregma is the optimal origin for rostral brain targets, for 27% of targets the skull entry point was closer to lambda, and for 38% the target itself was closer to the interaural line midpoint [10]. This indicates that the choice of the closest surgical landmark to the target can, in theory, improve precision. The accuracy of bregma-referenced targeting is influenced by several factors, including inter-animal anatomical variability, the skill of the operator in identifying the suture intersection, and the strain, sex, and age of the animal, which can cause significant deviations from the standard atlas brain [1] [10].
Table 1: Prevalence of Bregma as a Stereotaxic Origin in Rat Surgery (Analysis of 235 studies)
| Stereotaxic Origin | Prevalence in Studies | Closest to Target | Remarks |
|---|---|---|---|
| Bregma | 96% | 58% of targets | Optimal for rostral brain structures [10]. |
| Interaural Line Midpoint (IALM) | ~2% | 38% of targets | Yields shorter Euclidean distance for caudal targets [10]. |
| Lambda | ~1% | 5% of targets | Closer entry point for 27% of targets [10]. |
Quantitative Data on Targeting Accuracy and Challenges
Quantitative assessments of stereotaxic surgery outcomes highlight significant challenges in achieving consistent targeting. A systematic review of rat stereotaxic procedures found that in 39% of studies, no verification of implantation accuracy was performed at all, and only 8% of studies explicitly reported the number of on-target implants [10]. This reporting gap makes it difficult to assess the true efficacy and reproducibility of the technique across laboratories.
More objective, image-based analyses confirm these variability concerns. One study utilizing post-operative CT and MRI to reconstruct surgical trajectories found that only about 30% of electrodes were located within the targeted subnucleus structure, despite identical entry and target coordinates being used for all animals [12]. This inaccuracy can be attributed to multiple sources of error, including inter-individual anatomical differences, errors in establishing the flat-skull position, and crucially, inconsistencies in the precise identification of the bregma point itself [1] [12]. These discrepancies are not merely statistical; they have a direct impact on experimental outcomes, potentially leading to false negative results or misinterpretation of data due to off-target interventions. Furthermore, the conventional method of verification using 2D histology is susceptible to manual alignment errors, tissue distortion, and provides an incomplete picture of the full 3D trajectory [12].
Table 2: Sources of Error in Bregma-Referenced Stereotaxic Surgery
| Category of Error | Specific Examples | Impact on Accuracy |
|---|---|---|
| Anatomical & Biological | Inter-strain and inter-individual brain variability [10]; Age and sex differences [10]; Divergence from atlas reference brain [1] | Mismatch between atlas coordinates and actual brain structure location. |
| Surgical Procedure | Inaccurate identification of bregma and lambda [1]; Failure to achieve a true flat-skull position [11]; Incorrect calibration of stereotaxic apparatus | Systematic offset in all three coordinate axes (AP, ML, DV). |
| Verification & Reporting | Lack of post-operative verification [10]; Use of low-resolution 2D histology [12]; Failure to report off-target rates [10] | Inability to identify and exclude inaccurate data, perpetuating poor practice. |
Advanced Protocols and Methodological Refinements
Standard Protocol for Bregma Localization and Skull Alignment
A detailed protocol for establishing a reliable stereotaxic coordinate system is as follows:
- Anesthesia and Fixation: The rodent (rat or mouse) is anesthetized and securely placed in the stereotaxic frame using ear bars. The head is stabilized, and an incision is made to expose the skull surface.
- Skull Preparation and Suture Visualization: The periosteum and any connective tissue are gently cleared from the surface of the skull. To enhance the visibility of the cranial sutures, a cotton-tipped applicator with a small amount of hydrogen peroxide (H₂O₂) can be applied briefly to the skull, making the coronal and sagittal sutures more distinct [11].
- Identifying Bregma and Lambda: Using a stereotaxic microscope, the surgeon identifies the coronal suture, which runs transversely between the frontal and parietal bones, and the sagittal suture, which runs longitudinally along the midline between the parietal bones. Their intersection is the bregma [8] [1]. The lambda is identified posteriorly as the intersection of the sagittal suture with the lambdoid suture [1].
- Achieving Flat-Skull Position: The stereotaxic arm is used to position the tip of a fine needle or probe precisely on the bregma point, and the dorsoventral (DV) coordinate is recorded. The needle is then moved to the lambda point, and the DV coordinate is checked. The head position is adjusted (typically by tilting the nose clamp) until the DV readings for bregma and lambda are identical, confirming the skull is level in the anteroposterior plane [11]. This establishes the horizontal plane.
Image-Guided and Multi-Modal Verification
To address the limitations of traditional methods, advanced protocols using multi-modal imaging have been developed for retrospective assessment of targeting accuracy [12]. The workflow for this approach is as follows:
- Post-operative Imaging: After surgery, the animal is scanned using both in vivo Micro-CT (to visualize the physical implant or a radio-opaque marker) and in vivo MRI (to visualize the trace left by the electrode or needle in the brain tissue and to assess potential hemorrhage or damage).
- Image Co-registration and 3D Reconstruction: The post-operative CT and MRI images are fused together and then co-registered to a standard 3D reference brain atlas, such as the Allen Mouse Brain Common Coordinate Framework (CCFv3) [13] or other high-resolution atlases [14].
- Trajectory Reconstruction and Accuracy Quantification: The surgical trajectory is reconstructed in 3D from the imaging data. The Euclidean distance between the actual tip location and the intended target coordinate is calculated, providing an objective, quantitative measure of Target Localization Error [12].
- Benefit: This method allows for the early exclusion of off-target subjects in longitudinal studies, saving time and resources, and provides a more comprehensive and objective assessment of surgical outcome than 2D histology [12].
Diagram 1: Bregma-based stereotaxic surgery and verification workflow.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Solutions for Rodent Stereotaxic Surgery
| Item | Function / Application | Key Details |
|---|---|---|
| Stereotaxic Apparatus | Precise 3D navigation and head fixation. | Includes base plate, micromanipulators, ear bars, and a nose/incisor clamp [1]. |
| Stereotaxic Brain Atlas | Provides coordinate maps of brain structures. | e.g., Paxinos & Franklin's "The Mouse Brain in Stereotaxic Coordinates"; Paxinos & Watson's "The Rat Brain..." [1]. |
| Digital Stereotaxic Ruler | Enhances precision of coordinate measurement. | Reduces parallax error compared to manual vernier scales [10]. |
| Hydrogen Peroxide (H₂O₂) | Chemical aid for visualizing skull sutures. | Blunt scraping and application of H₂O₂ makes suture intersections (bregma/lambda) clearer [8] [11]. |
| High-Resolution 3D Reference Atlases | For advanced planning and verification. | e.g., Allen CCFv3 [13], STAM (1-μm resolution) [14]; used for co-registration with post-op images. |
| Multi-Modal Imaging (MRI/CT) | In vivo assessment of targeting accuracy. | Post-operative MRI shows electrode trace/lesion; CT visualizes physical implant; combined for 3D trajectory reconstruction [12]. |
The definition of bregma as the intersection of the sagittal and coronal sutures remains a bedrock principle in rodent stereotaxic surgery. However, the field is moving toward a more nuanced and sophisticated application of this landmark. Future directions focus on mitigating the documented variability in targeting accuracy. This includes the development of more comprehensive and high-resolution 3D digital atlases, such as the STAM atlas with its isotropic 1-μm resolution, which allows for arbitrary-angle slice generation and vastly improved structure delineation [14]. There is also a growing emphasis on the adoption of objective, image-based verification protocols to replace or supplement traditional histology [12]. Furthermore, the creation of standardized, population-averaged atlas templates across different developmental stages, as seen in the Developmental Mouse Brain Common Coordinate Framework (DevCCF), provides a more robust anatomical context for integrating data from diverse studies [13].
In conclusion, while bregma's anatomical definition is constant, its effective use in research requires a critical understanding of its limitations and the integration of modern techniques. By adhering to refined surgical protocols, employing the closest appropriate cranial landmark to the target, and utilizing advanced tools for planning and verification, researchers can significantly enhance the precision, reproducibility, and reliability of stereotaxic interventions in rodent models. This rigorous approach ensures that the foundational role of bregma in neuroscience research continues to be supported by evolving best practices.
In rodent stereotaxic surgery, a cornerstone of neuroscience and drug development research, precise navigation within the brain is paramount. This whitepaper defines the lambda, the cranial landmark formed by the intersection of the sagittal and lambdoid sutures, and details its critical role as a reference point in experimental protocols [15] [1]. While essential for aligning the skull in the stereotaxic apparatus, empirical data reveals significant variability in the spatial position of lambda relative to underlying brain anatomy, challenging its reliability as a sole fiducial marker [16] [17]. This guide provides an in-depth technical overview of lambda's anatomy, quantifies its limitations, outlines modern methodologies for its identification, and presents essential tools for researchers to enhance the accuracy and reproducibility of intracranial interventions.
Anatomical Definition and Landmark Context
The lambda is a defined craniometric point on the dorsal surface of the skull. It is located at the junction where the sagittal suture and the lambdoid suture meet [15] [18].
- Sagittal Suture: This is the fibrous joint that runs along the midline of the skull, connecting the left and right parietal bones [18] [19].
- Lambdoid Suture: This is the fibrous joint that separates the parietal bones from the occipital bone posteriorly. Its name is derived from its resemblance to the Greek letter lambda (λ) [15] [20].
The point where these two sutures converge is named after the same Greek letter [15]. In a developmental context, the lambda corresponds to the site of the posterior fontanelle in the fetal skull, a membranous area that later ossifies [15].
The lambda's anatomical counterpart in the stereotaxic system is the bregma, located anteriorly at the intersection of the sagittal suture and the coronal suture [1] [21]. Together, bregma and lambda serve as the two most critical external landmarks for establishing the stereotaxic coordinate system in rodents. The line connecting them defines the anteroposterior axis, and ensuring this line is level (i.e., both points are at the same dorsoventral coordinate) is a fundamental step before any surgical intervention [1] [21].
Table: Key Cranial Sutures and Landmarks in Rodent Stereotaxic Surgery
| Anatomical Feature | Description | Role in Stereotaxic Surgery |
|---|---|---|
| Lambda | Junction of the sagittal and lambdoid sutures [15] | Posterior reference point for aligning the skull in the stereotaxic apparatus [1] |
| Bregma | Junction of the sagittal and coronal sutures [1] | Anterior reference point; most common origin (zero point) for stereotaxic coordinates [1] |
| Sagittal Suture | Midline suture between the two parietal bones [18] | Defines the medial-lateral midline of the skull |
| Lambdoid Suture | Inverted V-shaped suture between parietals and occipital bone [15] [20] | Forms the posterior boundary for defining the skull-flat position |
| Coronal Suture | Suture between the frontal and parietal bones [1] | Forms the anterior boundary for defining the skull-flat position |
Lambda in Rodent Stereotaxic Research: Applications and Limitations
The stereotaxic apparatus, based on a 3D Cartesian coordinate system, allows for precise navigation along the mediolateral (x), anteroposterior (y), and dorsoventral (z) axes [1]. In this system, the lambda is indispensable for the initial skull-leveling procedure [21]. The established protocol involves measuring the dorsoventral coordinate at both bregma and lambda; the skull is considered level ("skull-flat position") when the difference between these two measurements is less than 0.1 mm [21] [22]. This ensures the skull is positioned in a standardized plane, a critical prerequisite for accurately targeting coordinates from a stereotaxic atlas.
However, a growing body of evidence highlights a significant limitation of lambda (and bregma) as fiducial markers. A key study coregistering 3D µCT skull datasets with brain MRI from five mice found that the positions of these skull landmarks vary considerably with respect to the underlying brain anatomy [16]. The study reported a maximum distance of 1.68 mm between the z-positions (dorsoventral) of lambda across different subjects, concluding that these two landmarks cannot be accepted as reliable fiducials for direct registration to a standard brain space like Waxholm Space (WHS) [16]. This inter-animal variability can be attributed to factors such as strain, sex, age, and body weight [1] [17].
Consequently, while lambda remains essential for mechanical alignment of the skull, the most accurate stereotaxic surgery for caudal brain structures is achieved when bregma is used as the reference for rostral structures and the interaural line is used for caudal structures, especially when animals of different weights are employed [17].
Table: Quantitative Variability of Skull Landmarks (Based on Coregistered µCT/MRI Data)
| Landmark | Nature of Variability | Reported Extent of Variation | Functional Impact |
|---|---|---|---|
| Lambda | Dorsoventral (z-position) variation between subjects [16] | Up to 1.68 mm [16] | Challenging for direct and accurate registration to standard brain atlases [16] |
| Bregma | Dorsoventral (z-position) variation between subjects [16] | Up to 1.2 mm [16] | Reduces reliability as a sole fiducial point for precise coordinate calculation [16] |
Advanced Detection and Validation Methodologies
Automated Detection via Deep Learning
To mitigate human error and improve repeatability, an automated framework using deep learning has been developed to locate bregma and lambda in rodent skull images [23]. This method addresses the challenge that, despite being theoretically easy to find, individual anatomical variations and obscured views make these points difficult to locate consistently in practice [23].
The framework employs a two-stage process:
- Skull Region Detection: A Region-Based Convolutional Neural Network (Faster R-CNN) is used to first detect the skull region of interest (ROI) in a raw input image, saving computing resources and focusing the subsequent analysis [23].
- Landmark Segmentation: A Fully Convolutional Network (FCN), modified with residual networks and batch normalization, then segments the precise locations of bregma and lambda within the skull ROI. The network is trained not with simple binary labels but with 2D Gaussian distributions centered on the true bregma and lambda points, which transforms the task into a regression problem for higher accuracy [23].
This automated system has demonstrated a mean error of less than 300 μm when compared to expert-placed landmarks and is robust to different lighting conditions and animal orientations in the images [23].
Validation of Internal Brain Landmarks
Given the variability of skull-based landmarks, research has validated a set of 16 internal brain landmarks as more reliable fiducials for registration to standard reference spaces like the Waxholm Space (WHS) [16]. These landmarks were identified to be reliably located by different individuals (both specialists and novices) across different MRI modalities and in various specimens, with a probability of being correctly found exceeding 95% [16]. The average deviations for these validated fiducials were 1.0, 0.6, and 1.5 voxels in the x, y, and z directions, respectively, demonstrating superior consistency compared to skull landmarks [16].
The Researcher's Toolkit: Essential Reagents and Materials
Table: Essential Materials for Stereotaxic Surgery based on Bregma and Lambda
| Item / Reagent | Function / Application | Experimental Context |
|---|---|---|
| Stereotaxic Apparatus (e.g., from Kopf Instruments, RWD Life Science) | Precise 3D navigation and fixation of the animal's head during surgery [1] | Fundamental hardware for all stereotaxic procedures. |
| Stereotaxic Atlas (e.g., Paxinos & Franklin's MBSC/RBSC, Allen Institute CCF 3D) | Provides 3D coordinates of brain structures relative to Bregma [1] | Used to determine target coordinates for injections, implants, or lesions. |
| Viral Vectors (e.g., AAV, Lentivirus) | Delivery of genetic material for gene expression manipulation (overexpression or knockdown via siRNA) in specific brain regions [21] | Used for optogenetics, chemogenetics, or functional gene studies. |
| Tracer Dyes | Visualization of neuronal projections and circuit connectivity [21] | Injected stereotaxically to map neural pathways. |
| Electrophysiology Probes/Electrodes | Recording of neural electrical signals in awake, behaving animals [21] | Implanted to monitor neuronal firing during behavior. |
| Microdialysis Probe | Continuous monitoring of neurotransmitters, drugs, or metabolites in the brain extracellular fluid [21] | Implanted for in vivo neurochemical sampling. |
| Deep Learning Framework (e.g., Faster R-CNN & FCN) | Automated, high-precision detection of Bregma and Lambda from skull images [23] | Used to reduce human error and improve surgical consistency. |
The Critical Role of Skull Landmarks as the Origin for Stereotaxic Coordinates
Stereotaxic surgery, a cornerstone technique in modern neuroscience and drug development, enables researchers to precisely navigate the intricate landscape of the rodent brain. This sophisticated approach relies on a three-dimensional Cartesian coordinate system—comprising mediolateral (ML), anteroposterior (AP), and dorsoventral (DV) axes—to target specific brain structures with remarkable accuracy [1]. The origin and reliability of this entire system are anchored to cranial sutures, the visible landmarks on the skull surface, with the intersection points known as bregma and lambda serving as the fundamental reference points [1] [24]. The precise identification of these landmarks is not a mere preparatory step but a critical determinant of surgical success, as even minor errors in establishing this origin point can propagate through the coordinate system, leading to significant deviations at the target site. This technical guide explores the paramount importance of skull landmarks within the context of rodent surgery research, detailing the protocols for their identification, the challenges in their consistent application, and the emerging technologies poised to enhance reproducibility in stereotaxic procedures for therapeutic development.
Fundamental Skull Landmarks in Rodent Stereotaxy
The rodent skull is composed of multiple bones that fuse at junctions called sutures. For stereotaxic surgery, two suture intersections are of paramount importance, Bregma and Lambda, serving as the anchor points for the entire coordinate system [1] [24].
Bregma is defined as the point where the sagittal suture (running mid-line along the skull, separating the two parietal bones) intersects with the coronal suture (which lies between the frontal and parietal bones) [1] [24]. In a top-down view, this forms a T-shaped junction. Bregma is the most commonly used origin point (zero point) for the anteroposterior and mediolateral coordinates in stereotaxic surgery [1].
Lambda is located posterior to bregma and is defined as the point where the sagittal suture meets the lambdoidal suture (which separates the parietal bones from the occipital bone) [1]. This junction often resembles the shape of the Greek letter lambda (λ). Lambda is primarily used to level the skull along the anteroposterior axis, ensuring the head is positioned flat in the stereotaxic apparatus [24].
Table 1: Key Skull Landmarks in Rodent Stereotaxic Surgery
| Landmark | Anatomical Definition | Primary Role in Stereotaxy |
|---|---|---|
| Bregma | Intersection of the sagittal and coronal sutures [1] [24] | Serves as the origin point (0,0) for the anteroposterior and mediolateral axes [1]. |
| Lambda | Intersection of the sagittal and lambdoidal sutures [1] [24] | Used to level the skull in the anteroposterior plane, ensuring proper alignment [24]. |
The following diagram illustrates the spatial relationship between these critical landmarks and the stereotaxic coordinate system they define.
Experimental Protocols for Landmark Identification and Skull Leveling
A rigorous and standardized protocol is essential for reliably identifying bregma and lambda and ensuring the skull is correctly positioned before any surgical intervention. The following detailed methodology, adapted from standard stereotaxic procedures, is critical for achieving this [24].
Materials and Setup
- Anesthetized Rodent: The animal is properly anesthetized and secured in a stereotaxic frame.
- Stereotaxic Apparatus: A standard stereotaxic instrument (e.g., from Kopf Instruments, RWD Life Science) equipped with ear bars and an incisor bar [1].
- Surgical Tools: Sterile scalpel, forceps, and scissors for exposing the skull.
- Probe or Needle: A fine-tipped probe attached to the stereotaxic manipulator.
- Sterile Saline: To keep the exposed skull moist during the procedure.
Step-by-Step Procedure
Scalp Incision and Skull Exposure: The scalp hair is shaved, and the skin is disinfected. A midline incision is made with a scalpel to expose the skull. The underlying connective tissue is gently separated to clearly visualize the sagittal, coronal, and lambdoidal sutures [24].
Initial Bregma Identification: Lower the probe tip to the suspected bregma point—the intersection of the sagittal and coronal sutures. Carefully note the dorsoventral (DV) coordinate at this position. This is the initial DV reading for bregma [24].
Skull Leveling - Lambda Check: Raise the probe and move it posteriorly to the lambda point (intersection of the sagittal and lambdoidal sutures). Lower the probe tip to touch lambda and record its DV coordinate [24].
Alignment Adjustment: Compare the DV readings from bregma and lambda. The skull is considered level in the anteroposterior plane if the difference between these two measurements is less than 0.1 mm. If the difference exceeds this tolerance, the incisor bar must be adjusted (raised or lowered) and the measurements repeated until the skull is level [24].
Setting the Origin: Once the skull is level, return the probe to bregma. The anteroposterior and mediolateral coordinates at this point are now set to zero, establishing the origin for all subsequent coordinate calculations for targeting brain structures [24].
Table 2: Common Commercially Available Stereotaxic Systems and Related Reagents
| Item Category | Specific Examples | Primary Function |
|---|---|---|
| Stereotaxic Apparatus | Kopf Instruments, RWD Life Science, Harvard Apparatus, Stoelting Co. [1] | Provides a rigid frame and micromanipulators for precise 3D navigation of the brain. |
| Surgical Consumables | Sterile scalpels, sutures, bone drill bits, absorbent gel foam. | Essential for performing the surgery, controlling bleeding, and closing the wound. |
| Anesthesia & Analgesia | Isoflurane (inhalant), Ketamine/Xylazine (injectable), Buprenorphine (post-op pain relief). | Ensures the animal is unconscious and pain-free during and after the procedure. |
| Viral Vectors & Tracers | AAV (for gene delivery), Lectins, Fluorescent Retrograde Tracers (e.g., Fluorogold) [24]. | Used to manipulate genes or map neural circuits by delivering agents to specific brain targets. |
Challenges and Limitations in Landmark Accuracy
Despite their foundational role, the use of skull landmarks is not without significant challenges, which can introduce variability and compromise experimental outcomes.
A primary concern is the inconsistency in how bregma is identified and measured across different laboratories. Renowned atlases like Paxinos and Franklin's "The Mouse Brain in Stereotaxic Coordinates," while indispensable, lack explicit, standardized instructions for determining the bregma point [1]. This omission can lead to subjective interpretations among researchers. Furthermore, inter-strain and intra-strain variations in craniometric parameters and brain volume due to factors like body size, weight, age, and sex can affect the relationship between the external skull landmarks and the underlying brain structures, making standardized coordinates less universally precise [1].
Compounding this issue, recent studies have revealed discrepancies when comparing measurements taken directly from the skull with those derived from brain atlases or even between different atlases themselves [1]. These inconsistencies pose a major challenge for scientists attempting to compare stereotaxic coordinates across different studies or replicate published findings. The problem is exacerbated by the nature of traditional 2D reference atlases, which are often constructed from brain sections spaced hundreds of micrometers apart. This prevents the observation of continuous structural changes and can hinder accurate three-dimensional reconstruction and boundary determination [25].
Advanced Approaches and Future Directions
To overcome the limitations of traditional landmarking, the field is evolving towards more precise and reliable methodologies.
High-Resolution and 3D Digital Atlases
A significant advancement is the creation of high-resolution, three-dimensional digital reference atlases. For example, the Stereotaxic Topographic Atlas of the Mouse Brain (STAM) was constructed using a Nissl-stained image dataset with an isotropic 1-μm resolution, allowing for visualization at a single-cell level [25]. This atlas provides the 3D topography of 916 brain structures and enables the generation of slice images at arbitrary angles, offering a far more precise tool for anatomical localization than traditional atlases with large intervals between sections [25]. Such atlases are interoperable with widely used stereotaxic atlases like Paxinos and Franklin's, supporting cross-atlas navigation and improving the accuracy of targeting small nuclei and complex fiber bundles [25].
Computational and AI-Driven Landmarking
Another promising direction is the application of artificial intelligence (AI) and deep learning to automate landmark identification. Recent research has developed models using optimized 3D U-Net networks to automatically detect craniometric landmarks on medical imaging such as spiral CT (SCT) and cone-beam CT (CBCT) scans [26]. These models have demonstrated high precision, with mean radial errors consistently below 1.3-1.4 mm, even in complex conditions involving malocclusion or metal artifacts [26]. While this technology is currently more advanced in human clinical applications, its principles showcase the potential for automating and standardizing the landmarking process in preclinical research, thereby reducing human error and subjective interpretation.
The logical workflow for integrating these advanced tools into a modern stereotaxic surgery pipeline is summarized in the following diagram.
The external skull landmarks, bregma and lambda, remain the indispensable foundation upon which the precise internal navigation of the rodent brain is built. Their correct identification and use in skull leveling are paramount for the accuracy and reproducibility of stereotaxic surgery, a technique critical to neuroscience research and pharmaceutical development. While challenges related to standardization and anatomical variability persist, the field is actively addressing these through the development of ultra-high-resolution 3D digital atlases and the exploratory application of AI-driven landmark detection. By adhering to meticulous protocols for landmark-based alignment and embracing these new technologies, researchers can significantly minimize stereotaxic errors, thereby enhancing the reliability of their data and the validity of their scientific conclusions.
In rodent stereotaxic surgery, the accurate targeting of specific brain structures is foundational to neuroscience research and drug development. This precision fundamentally relies on establishing a stable and reproducible coordinate system within the skull of the animal. The flat-skull position (FSP), achieved by leveling the bregma and lambda skull landmarks to the same vertical height, serves as this critical baseline. By defining a consistent horizontal plane, the FSP ensures that the three-dimensional coordinates derived from a brain atlas can be reliably translated to the live animal. This technical guide delves into the anatomical basis, detailed protocol, and significant impact of the flat-skull position, framing it within the broader context of using cranial landmarks for neuroscientific discovery. The renowned neuroanatomist George Paxinos, whose atlases are standard in the field, emphasized that the definition and implementation of the skull-flat position for their atlases significantly improved the reproducibility of stereotaxic procedures [22].
Anatomical Foundations: Bregma and Lambda as Cartesian Origins
The stereotaxic technique operates on a simple yet powerful principle: the spatial relationships between external skull landmarks and internal brain structures are consistent within a species and strain. This allows researchers to navigate the brain using a three-dimensional Cartesian coordinate system.
- Bregma: This is defined as the point where the coronal suture (running between the frontal and parietal bones) intersects perpendicularly with the sagittal suture (running along the midline of the skull) [8]. In practical terms for rodent stereotaxy, it is often identified as the midpoint of the curve of best fit along the coronal suture, rather than merely the visual intersection, to improve accuracy [2].
- Lambda: This is the analogous point posterior to bregma, defined as the intersection of the sagittal suture and the lambdoid suture [1] [21].
- The Coordinate System: In this system, the anteroposterior (AP) axis and mediolateral (ML) axis lie within the horizontal plane established by leveling bregma and lambda. The dorsoventral (DV) axis is then perpendicular to this plane [21]. Bregma is most frequently used as the origin (zero point) for the AP and ML coordinates, from which all target measurements are made [11].
Table 1: Key Skull Landmarks in Rodent Stereotaxic Surgery
| Landmark | Anatomical Definition | Role in Stereotaxic Coordinate System |
|---|---|---|
| Bregma | Intersection of the coronal and sagittal sutures [8]. | The most common origin point (0,0) for the anteroposterior and mediolateral axes [1] [11]. |
| Lambda | Intersection of the sagittal and lambdoid sutures [1] [21]. | Used in conjunction with bregma to define and level the horizontal plane; a secondary reference point [11]. |
| Sagittal Suture | Midline suture between the two parietal bones [1]. | Defines the mediolateral midline (ML = 0) of the skull. |
| Coronal Suture | Suture between the frontal and parietal bones [1]. | Defines the anterior landmark for the bregma point. |
The Flat-Skull Position Protocol: A Step-by-Step Methodology
The following section provides a detailed experimental protocol for achieving the flat-skull position, a critical prerequisite for any stereotaxic procedure involving intracranial injections, lesions, or device implantation.
Surgical Preparation and Landmark Identification
- Anesthesia and Positioning: After inducing anesthesia (e.g., with isoflurane), secure the rodent in the stereotaxic frame using the ear bars and incisor bar. Shave the scalp, disinfect the skin, and make a midline incision to expose the skull [21].
- Cleaning and Visualizing Sutures: Gently clean the surface of the skull with a sterile saline solution or hydrogen peroxide to remove connective tissue and clarify the suture lines. This step is crucial for accurately identifying bregma and lambda [8] [11].
- Initial Bregma Measurement: Using a stereotaxic probe or needle attached to the micromanipulator, lower the tip directly onto the bregma point. Record the dorsoventral (DV) coordinate from the Vernier scale on the manipulator. This reading represents the height of bregma [21].
The Leveling Procedure
- Lambda Measurement: Raise the probe, move it to the lambda point, and lower the tip onto lambda. Record the DV coordinate at this location [21].
- Assessing Levelness: Compare the DV readings from bregma and lambda. A skull is considered level, or in the flat-skull position, when the difference between these two measurements is less than 0.1 mm [21].
- Adjusting the Incisor Bar: If the difference exceeds 0.1 mm, adjust the height of the incisor bar—lower it if lambda is higher than bregma, or raise it if lambda is lower—and repeat the measurements at both bregma and lambda until the height difference is within the acceptable tolerance [21].
- Setting the Origin: Once the skull is level, return the probe to bregma and record the final AP and ML coordinates. These values now establish the origin (0,0) for your target coordinates as listed in the stereotaxic atlas [21].
The following workflow diagram summarizes the logical sequence and decision points in this leveling procedure.
Impact and Innovations in Precision Leveling
The rigorous implementation of the flat-skull position is not a mere formality; it is a primary determinant of surgical success. Inaccuracies at this stage propagate through the entire procedure, leading to target miss and compromised experimental integrity.
Quantifying the Cost of Error
Inconsistent or inaccurate identification of bregma is a significant source of stereotaxic error. A study dedicated to improving bregma detection found that a traditional "rough" method of visual identification differed from a more precise, computer-assisted method by ≥ 0.2 mm in 44% of animals [2]. When this error was corrected using the new method, the average total stereotaxic error in implanting a microprobe was significantly reduced [2]. This highlights that minor deviations in establishing the origin point can lead to major inaccuracies in reaching the intended target, especially given that many rodent brain nuclei and subregions are smaller than 0.5 mm [1].
Table 2: Impact of Bregma Identification Method on Stereotaxic Error
| Measurement Factor | Traditional 'Rough' Method | Precise Computer-Assisted Method |
|---|---|---|
| Bregma Identification | Visual estimation of suture intersection. | Mathematical curve-fitting to coronal suture and midline [2]. |
| Rate of Substantial Error | Differed from precise method by ≥ 0.2 mm in 44% of cases [2]. | N/A (Defined as the accurate standard). |
| Resulting Implantation Error | Higher average total stereotaxic error [2]. | Significantly decreased average total stereotaxic error [2]. |
Advanced Techniques and Tools
The field is evolving with new technologies aimed at standardizing and automating landmark identification to further enhance precision and reproducibility.
- Digital and 3D Atlases: Modern reference atlases, such as the Allen Mouse Brain Common Coordinate Framework (CCF) and the new Stereotaxic Topographic Atlas of the Mouse Brain (STAM) with isotropic 1-μm resolution, provide unprecedented detail and allow for arbitrary-angle sectioning, improving the interpretation of anatomical locations [25].
- Automated Landmark Detection: Machine learning approaches are being developed to automatically detect bregma and lambda in images of the rodent skull. One framework using a region-based convolutional network and a fully convolutional network achieved localizations with mean errors of less than 300 micrometers, demonstrating robustness to varying lighting and orientation [23].
- Surgical Workflow Innovations: Modified stereotaxic devices that integrate multiple tools (e.g., a measurement probe and an impactor) into a single header can reduce the number of instrument changes. This innovation has been shown to decrease the total operation time by 21.7%, specifically improving efficiency during the Bregma-Lambda measurement phase and reducing anesthesia time [27].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Rodent Stereotaxic Surgery
| Item | Function / Explanation |
|---|---|
| Stereotaxic Frame | A rigid apparatus with ear and incisor bars to immobilize the rodent's head in a fixed position [21]. |
| Micromanipulator | Device attached to the stereotaxic frame that allows precise, micrometer-scale movement of probes or injectors in 3D space [21]. |
| Stereotaxic Atlas | A reference (e.g., Paxinos and Franklin's Mouse Brain atlas) providing 3D coordinates of brain structures relative to skull landmarks [1] [22]. |
| Hamilton Syringe / Microinjector | For delivering precise, small-volume injections of viruses, tracers, or pharmaceutical agents into the brain [21]. |
| High-Speed Drill | For performing clean craniotomies in the skull to access the brain surface without causing undue trauma [21]. |
| Active Warming System | A heated pad or controlled circuit board to maintain the rodent's body temperature during anesthesia, preventing hypothermia and improving survival rates [27]. |
| Isoflurane Anesthesia System | A vaporizer and nose cone for delivering inhaled isoflurane, providing stable and controllable surgical anesthesia [27]. |
The meticulous leveling of bregma and lambda to achieve the flat-skull position remains a non-negotiable standard in rigorous stereotaxic surgery. It is the cornerstone upon which the entire Cartesian coordinate system for intracranial navigation is built. While the fundamental principles established by pioneers like Paxinos continue to guide the field, modern innovations in digital atlas technology, automated landmark detection, and refined surgical hardware are pushing the boundaries of precision and reproducibility. For researchers in neuroscience and drug development, a deep understanding and flawless execution of this technique are paramount for generating valid, reliable, and impactful data on brain function and therapeutic intervention.
From Theory to Practice: A Step-by-Step Surgical Protocol for Landmark-Based Targeting
Stereotaxic surgery in rodents is a cornerstone technique in modern neuroscience and drug development research, enabling investigators to target specific brain regions with a high degree of precision. The procedure's success fundamentally relies on a rigorous pre-surgical setup, which encompasses appropriate anesthesia, strict aseptic technique, and the meticulous exposure and preparation of the skull. Within this context, the accurate identification of the bregma and lambda skull landmarks is paramount, as these points form the anatomical basis of the three-dimensional Cartesian coordinate system used for surgical navigation [1] [21]. The bregma, defined as the point of intersection between the sagittal and coronal sutures, serves as the most common origin point (zero point) for stereotaxic coordinates [1] [28]. Despite its critical role, studies highlight that discrepancies in how bregma is measured exist among different laboratories, and renowned atlases like Paxinos and Franklin lack explicit instructions for its determination [1] [28]. This technical guide details the essential pre-surgical procedures, framing them within the critical need for consistent and accurate landmark identification to ensure experimental reproducibility and animal well-being.
Anesthetic Protocols and Physiological Management
Selecting and managing an appropriate anesthetic regimen is the first critical step in rodent stereotaxic surgery. The chosen protocol must provide a sufficient plane of anesthesia for the procedure's duration while minimizing physiological stress on the animal.
Table 1: Common Injectable Anesthetic Protocols for Rodent Stereotaxic Surgery
| Anesthetic Agent(s) | Dosage and Route | Surgical Duration | Key Considerations |
|---|---|---|---|
| Ketamine + Xylazine [29] | 40-90 mg/kg (Ketamine) + 5-10 mg/kg (Xylazine), IP | 45-90 minutes | Thermal support is crucial. To prolong anesthesia, supplement with ¼ - ½ dose of ketamine only. Xylazine can be reversed with atipamezole or yohimbine [29]. |
| Ketamine + Dexmedetomidine [29] | 75 mg/kg (Ketamine) + 0.25-0.5 mg/kg (Dexmedetomidine), IP | ~120 minutes | Reversible with atipamezole, facilitating faster recovery. Dosage may be lower if pre-medicated with an opioid [29]. |
| Pentobarbital [29] | 40-50 mg/kg IP for sedation; higher doses for surgery | Variable; poor analgesia | Not recommended as a sole agent due to poor analgesic properties. Can cause significant cardiovascular depression [29]. |
Table 2: Inhaled Anesthetic Protocol for Rodent Stereotaxic Surgery
| Anesthetic Agent | Induction | Maintenance | Key Considerations |
|---|---|---|---|
| Isoflurane [29] [30] | 3-5% in oxygen | 1-3% in oxygen [29] | Requires a calibrated vaporizer and proper gas scavenging. Rapid induction and recovery allow for better control of anesthetic depth [29]. |
Supportive Care and Physiological Monitoring
Preventing hypothermia is a critical aspect of supportive care. Rodents, due to their high surface-area-to-body-mass ratio, are highly susceptible to heat loss under anesthesia. Isoflurane, in particular, promotes hypothermia by inducing peripheral vasodilation [7]. Proactive thermal support is mandatory:
- Allowed Heating Methods: Use a warm circulating water blanket, thermal pad with temperature control, or isothermal heat source. The animal must be separated from the heat source by a towel or drape to prevent burns [29] [30].
- Prohibited Heating Methods: Avoid "over-the-counter" electric heating pads without precise temperature control, as they are prone to overheating [30].
Other essential supportive measures include [29] [30]:
- Eye Lubrication: Apply ophthalmic ointment (e.g., Paralube) to prevent corneal drying for any procedure longer than 5 minutes.
- Hydration: Administer warmed subcutaneous or intraperitoneal fluids (e.g., saline, lactated Ringer's solution at 5-10 ml/kg/hr) during prolonged surgeries to maintain hydration.
Physiological parameters must be monitored regularly (at least every 15 minutes) throughout the procedure [30]:
- Anesthetic Depth: Assessed by loss of response to a firm toe pinch (pedal reflex) and loss of blink reflex.
- Respiratory Function: Monitor rate and effort. A normal undisturbed respiratory rate for a rat is 70-110 breaths per minute; a fall of 50% is acceptable under anesthesia [29].
- Mucous Membranes: Should be pink, not blue (cyanotic), indicating adequate oxygenation.
- Pulse: Can be assessed by palpation of the chest wall.
Figure 1: Anesthetic Management and Monitoring Workflow. This diagram outlines the decision-making process for establishing and maintaining a proper surgical plane of anesthesia while providing essential physiological support.
Aseptic Technique and Surgical Field Preparation
Maintaining asepsis throughout the survival surgical procedure is non-negotiable. It prevents postoperative infections, reduces animal suffering, and ensures that research outcomes are not confounded by pathological variables.
Preoperative Preparation:
- Instrument Sterilization: All surgical instruments must be sterilized prior to the procedure using an approved method (e.g., autoclaving, cold sterilization) [31].
- Surgeon Preparation: The surgeon should don appropriate personal protective equipment (PPE), including a clean lab coat, sterile gloves, mask, and head cover [31].
- Surgical Site Preparation: The rodent's scalp must be shaved and then disinfected with a alternating scrubs of chlorhexidine or povidone-iodine and 70% alcohol, working from the center of the surgical site outward [31].
Sterile Field and Operative Technique:
- The stereotaxic apparatus and surrounding area should be disinfected with 70% alcohol or an appropriate disinfectant wipe [31].
- Use sterile drapes to isolate the surgical site and create a sterile field. Some stereotaxic frames are compatible with dedicated draping kits.
- Handle tissues gently and use sterile instruments to minimize tissue trauma and the risk of contamination.
Skull Exposure and Landmark Identification
With the animal securely positioned in the stereotaxic frame and a stable plane of anesthesia confirmed, the surgical procedure for exposing the skull and identifying critical landmarks begins.
Experimental Protocol: Skull Exposure and Landmark Identification
- Scalp Incision: Using a scalpel, make a midline incision through the skin along the skull, from just behind the eyes to the posterior end of the skull [21].
- Tissue Reflection: Gently separate the underlying connective tissue and muscle from the skull surface using a periosteal elevator or the blunt end of a scalpel handle [21].
- Skull Cleaning: Thoroughly clean the surface of the skull with sterile saline and a cotton-tipped applicator. Any residual tissue or blood can obscure the cranial sutures. Ensure the skull is dry for optimal visualization of the landmarks [32] [21].
- Landmark Identification: Identify the three key sutures under the stereotaxic microscope:
- Sagittal Suture: The prominent suture running along the midline of the skull.
- Coronal Sutures: The sutures that run perpendicular to the sagittal suture, roughly at the level of the eyes.
- Lambdoidal Suture: The suture at the posterior part of the skull that resembles the Greek letter "lambda" (λ) [1].
- Locate Bregma and Lambda:
Table 3: The Scientist's Toolkit - Essential Materials for Pre-surgical Setup
| Item/Category | Specific Examples | Function and Application |
|---|---|---|
| Anesthesia System | Precision vaporizer (for isoflurane), induction chamber, anesthetic machine with oxygen source [29] [30]. | Delivery and control of inhaled anesthetic agents. |
| Stereotaxic Apparatus | Kopf Instruments, RWD Life Science, Harvard Apparatus [1]. | Rigid head fixation and precise 3D navigation. |
| Thermal Support | Circulating warm water blanket, isothermal heating pad (e.g., Gaymar Stryker T/Pump) [7] [29] [30]. | Prevention of hypothermia during surgery and recovery. |
| Surgical Instruments | Scalpel handle and blades, fine forceps, tissue scissors, periosteal elevator, hemostats. | Performing the scalp incision, tissue reflection, and hemostasis. |
| Drilling System | Dental drill with assorted burrs (e.g., 0.5 mm - 1.0 mm). | Creating a clean craniotomy for access to the brain. |
| Skull Fixation | Jeweler's screws, dental acrylic (e.g., Jet Denture Repair Acrylic), dental adhesive (e.g., Super-Bond C&B) [32]. | Securing head-posts and implants to the skull. |
| Disinfectants & Lubricants | Povidone-iodine or chlorhexidine scrub, 70% alcohol, ophthalmic ointment (e.g., Paralube) [29] [30]. | Surgical site preparation and corneal protection. |
The pre-surgical phases of anesthesia, aseptic preparation, and skull exposure constitute the foundational pillars of a successful stereotaxic surgery. The rigorous application of the protocols outlined herein—from the selection of an appropriate anesthetic and diligent physiological monitoring to the maintenance of a sterile field—is essential for ensuring animal welfare and data integrity. Crucially, the entire process culminates in the accurate identification of the bregma and lambda landmarks. As the origin of the stereotaxic coordinate system, the correct setting of the bregma is a non-negotiable step that directly dictates the accuracy of all subsequent surgical interventions [1] [28]. Mastery of these pre-surgical elements not only enhances the wellbeing of the animal subject but also directly contributes to the reproducibility, reliability, and scientific validity of neuroscience and drug development research.
In rodent stereotaxic neurosurgery, the bregma and lambda points on the skull serve as the fundamental anatomical landmarks for establishing a three-dimensional Cartesian coordinate system. This system enables precise navigation to specific brain targets for interventions such as injecting fluids, implanting probes, cannulae, or optic fibers [28]. The advent of the stereotaxic apparatus revolutionized neuroscience research by allowing for this precise 3D navigation along the skull's mediolateral (ML), anteroposterior (AP), and dorsoventral (DV) axes [28]. The accuracy of defining these points is paramount, as even minor errors in setting the bregma as the coordinate origin can propagate into significant targeting inaccuracies, potentially compromising experimental results and their reproducibility [28].
Despite its importance, the specific procedure for measuring bregma is not consistently described across laboratories, and renowned brain atlases often lack explicit instructions for its determination [28]. Furthermore, discrepancies exist between different atlas coordinate systems, and individual anatomical variations between subjects make these points challenging to locate consistently in practice [28] [23]. This guide details both established manual techniques and emerging automated technologies designed to enhance the precision, efficiency, and reliability of bregma and lambda identification.
Established Manual Techniques and Inherent Challenges
The conventional method for identifying bregma and lambda relies on visual inspection and palpation of the rodent skull. Bregma is defined as the point of intersection between the sagittal suture (running along the midline of the skull) and the coronal sutures (which run transversely). Similarly, lambda is the intersection point of the sagittal suture with the lambdoid sutures on the posterior part of the skull [23].
While theoretically straightforward, this manual process involves estimation based on the investigator's experience, which introduces subjectivity and positioning errors [23]. Key challenges include:
- Anatomical Variability: The exact morphology of the skull and suture patterns can vary between individual animals, even within the same strain [23].
- Suture Ambiguity: In some subjects, the suture lines can be faint or partially obscured, making the exact point of intersection difficult to determine with high confidence [23].
- Operator Dependence: The skill and experience of the researcher play a significant role in the accuracy and repeatability of the landmark identification [23].
These challenges underscore the need for rigorous training and standardized protocols to minimize variability when relying on manual techniques.
Automated Detection: A Deep Learning Framework
To overcome the limitations of manual identification, a novel automated framework utilizing deep learning has been developed. This method aims to reduce localization error, improve repeatability, and simplify the procedure [23].
Experimental Protocol for Automated Detection
Dataset Preparation:
- Source: 93 images of sacrificed mice (male and female, age 8-28 weeks, various strains) [23].
- Acquisition: Images were captured using a handheld smartphone (iPhone 6) with dimensions of 2448 × 3264 × 3 pixels, under uncontrolled lighting conditions and mouse orientations to ensure model robustness [23].
- Labeling: An expert neurosurgeon provided the ground-truth coordinates for bregma and lambda on each full-resolution image. For training, these points were represented as 2D Gaussian distributions (standard deviation of 20 pixels) centered on the landmark, transforming the problem into a regression task [23].
Localization Framework Architecture: The framework employs a two-stage deep learning approach [23]:
- Stage One - Skull Detection: A Region-Based Convolutional Neural Network (Faster R-CNN) is used to detect the skull region within the full image. This crops and isolates the Region of Interest (ROI), improving computational efficiency for the next stage [23].
- Stage Two - Landmark Segmentation: A Fully Convolutional Network (FCN) modified with residual networks, bottleneck design, and batch normalization performs pixel-wise segmentation on the cropped skull image. The network outputs two channels representing the probability of each pixel being bregma or lambda. The final coordinates are determined as the pixel with the maximum probability value in each channel [23].
Implementation and Training:
- The 93 images were split into training (n=80) and testing (n=13) sets for the FCN.
- Extensive data augmentation (random flipping, rotating, shifting) was applied to the training set, generating 8000 augmented images from 80 originals to improve model robustness.
- The model was trained to minimize the error between its predicted Gaussian maps and the ground-truth maps provided by the expert [23].
Key Quantitative Performance Data
The automated deep learning framework demonstrated high accuracy in identifying bregma and lambda, as summarized in the table below.
Table 1: Performance Metrics of the Automated Landmark Detection Framework
| Metric | Performance Value | Experimental Context |
|---|---|---|
| Mean Localization Error | < 300 μm [23] | Tested on rodent skull images |
| Model Robustness | Effective under varying lighting conditions and animal orientations [23] | Images captured with handheld smartphone, conditions uncontrolled [23] |
| Skull Detection Rate | 100% in testing (n=33 images) [23] | Stage one Faster R-CNN performance |
This performance is achieved with a model designed to be robust to different lighting conditions and mouse orientations, making it a potentially valuable tool for standardizing stereotaxic procedures [23].
Technical Specifications and Visualization
Experimental Workflow Diagram
The following diagram illustrates the two-stage automated detection process.
Research Reagent Solutions and Essential Materials
A successful experiment, whether manual or automated, relies on specific tools and reagents. The following table details key materials used in the automated detection research.
Table 2: Essential Research Reagents and Materials for Automated Landmark Detection
| Item Name | Function / Role in the Experiment | Specifics / Examples |
|---|---|---|
| Rodent Subjects | Source of anatomical skull images for model training and validation. | Mice; various strains, sexes, 8-28 weeks old [23]. |
| Imaging Equipment | Captures high-resolution digital images of the exposed skull. | Handheld smartphone camera (e.g., iPhone 6) [23]. |
| Deep Learning Framework | Provides the software environment for building, training, and deploying the neural networks. | Frameworks supporting Faster R-CNN and FCN implementations (e.g., TensorFlow, PyTorch) [23]. |
| Region-Based CNN (Faster R-CNN) | First-stage neural network model that localizes and crops the skull region from the full image [23]. | -- |
| Fully Convolutional Network (FCN) | Second-stage neural network model that performs pixel-wise segmentation to identify bregma and lambda points [23]. | Modified with residual connections and batch normalization [23]. |
| Data Augmentation Pipeline | Artificially expands the training dataset by applying random transformations, improving model robustness [23]. | Includes random flipping, rotation, and shifting of images [23]. |
| Expert-Annotated Ground Truth | The definitive, accurate coordinates of bregma and lambda used to train and evaluate the model. | Provided by a trained neurosurgeon [23]. |
The precise identification of bregma and lambda is a cornerstone of reproducible rodent stereotaxic surgery. While manual techniques based on skull sutures remain prevalent, they are inherently subjective and susceptible to error. The emergence of automated, deep-learning-based frameworks offers a promising avenue for enhancing the accuracy, reliability, and throughput of this critical step. By achieving sub-300-micron precision and robustness to experimental variability, these technologies have the potential to standardize landmark identification across laboratories, thereby strengthening the validity of neuroscientific and drug development research.
In rodent stereotaxic surgery, the precise targeting of specific brain regions hinges on a Cartesian coordinate system that uses visible landmarks on the skull as its reference points [1]. The Bregma, defined as the point where the sagittal suture intersects the coronal suture, and the Lambda, identified as the intersection of the sagittal and lambdoidal sutures, are the two most critical landmarks for establishing this coordinate system [1] [21]. The primary origin for stereotaxic coordinates is most commonly the Bregma [1]. However, the accuracy of these coordinates is entirely dependent on the skull being positioned in a level plane. If the skull is tilted, the same set of coordinates will target a different, and incorrect, location in the brain. Therefore, the procedure of using a micromanipulator to ensure that Bregma and Lambda are at the same height along the dorsoventral axis is not merely a preliminary step; it is a fundamental prerequisite for ensuring the reproducibility and validity of any stereotaxic intervention, from viral vector injections to electrode implantations [21].
Recent studies continue to highlight that discrepancies in the measurement of these skull landmarks are a significant source of error in neuroscience research [1]. This technical guide will detail the leveling procedure, framing it within the broader context of a thesis on rodent cranial landmarks, and provide the detailed methodologies and tools required to execute it with precision.
Essential Concepts: Bregma, Lambda, and the Stereotaxic Frame
Anatomical Definitions and Their Significance
The adult rodent skull is composed of several bones that meet at joints known as sutures. For stereotaxic surgery, three key sutures are visible from a dorsal view [1]:
- Sagittal Suture: Runs medially along the midline of the skull, separating the two parietal bones.
- Coronal Suture: Has a parabolic curve between the frontal and parietal bones.
- Lambdoidal Suture: Resembles the Greek letter Lambda (λ) at the posterior part of the skull, between the parietal bones and the occipital bone.
The intersections of these sutures define our critical landmarks [1] [21]:
- Bregma: The point where the sagittal suture crosses the coronal suture. This is the most common origin point for the stereotaxic coordinate system.
- Lambda: The point where the sagittal suture crosses the lambdoidal suture.
The line connecting Bregma and Lambda defines the anteroposterior (AP) axis. Ensuring both points are at the same height in the dorsoventral (DV) axis confirms the skull is level in the AP plane.
Table 1: Key Skull Landmarks in Rodent Stereotaxic Surgery
| Landmark | Anatomical Definition | Role in Stereotaxic Surgery |
|---|---|---|
| Bregma | Intersection of the sagittal and coronal sutures | Most common origin point (zero point) for stereotaxic coordinates. |
| Lambda | Intersection of the sagittal and lambdoidal sutures | Used in conjunction with Bregma to level the skull and define the anteroposterior axis. |
| Sagittal Suture | Midline suture between the parietal bones | Provides a visual reference for medial-lateral alignment. |
The Stereotaxic Apparatus and Micromanipulator
The stereotaxic frame is the instrument that holds the animal's head in a fixed position. Its key components include [21]:
- Base Plate: The horizontal platform on which the animal is positioned.
- Ear Bars: Secure the animal's head by being gently placed in the external auditory meatus.
- Incisor Bar: Holds the animal's front teeth to stabilize the head.
- Micromanipulator: A precise moving assembly attached to the frame. It holds surgical probes, electrodes, or syringes and allows for controlled movement along the three Cartesian axes: mediolateral (ML), anteroposterior (AP), and dorsoventral (DV) [1] [21]. The manipulator is equipped with Vernier scales or digital readouts for exact distance measurements.
The Leveling Procedure: A Step-by-Step Technical Guide
This protocol is adapted from established stereotaxic surgical methods [21] and incorporates insights from recent technical modifications [7].
Pre-Surgical Preparation
- Anesthesia and Animal Setup: Deeply anesthetize the rodent using an approved anesthetic like isoflurane. Confirm the depth of anesthesia by the absence of a foot pinch reflex. Apply a lubricating ophthalmic ointment to prevent corneal drying. Place the animal on a warming pad to maintain body temperature throughout the procedure, a critical step for animal survival and physiological stability [7].
- Head Fixation in the Stereotaxic Frame: Position the animal's head in the frame by placing its upper incisors securely over the incisor bar. Gently insert the ear bars into the external auditory meatus, ensuring the head is symmetrically secured and does not move laterally [21].
- Surgical Exposure of the Skull: Shave and aseptically prepare the scalp. Make a midline incision with a scalpel to expose the skull. Gently clear away fascia and connective tissue from the surface of the skull using a sterile cotton-tipped applicator. If the suture lines are difficult to visualize, a small amount of hydrogen peroxide can be applied to the skull to improve contrast [21].
Leveling the Skull Using the Micromanipulator
The core of the leveling procedure involves using the micromanipulator to measure and equalize the DV height at Bregma and Lambda.
Diagram 1: Workflow for Skull Leveling
- Initial Measurement at Bregma:
- Attach a fine-tipped probe to the micromanipulator.
- Using the manipulator's controls, carefully lower the probe until its tip gently touches the skull at the precise point of Bregma.
- Record the dorsoventral (DV) coordinate from the Vernier scale or digital readout. To read a Vernier scale, first note the whole millimeter value, then find the line on the Vernier scale that aligns perfectly with a line on the main scale to determine the fraction of a millimeter [21].
- Measurement at Lambda:
- Raise the probe and move the manipulator to position the tip directly above Lambda.
- Carefully lower the probe until it just touches the skull at Lambda.
- Record the DV coordinate at this landmark.
- Assessment and Adjustment:
- Calculate the difference between the two DV measurements.
- Acceptance Criterion: The skull is considered level if the DV measurement at Lambda is within 0.1 mm of the measurement at Bregma [21].
- If the difference exceeds 0.1 mm, the skull is not level. To correct this, adjust the height of the incisor bar. If the Lambda reading is more ventral (lower), the nose is too high, and the incisor bar should be lowered. Conversely, if the Lambda reading is more dorsal (higher), the nose is too low, and the incisor bar should be raised.
- Iterative Process:
- After adjusting the incisor bar, return the probe to Bregma and re-measure the DV coordinate. Then, measure Lambda again. This process must be repeated until the DV measurements at both landmarks are within the 0.1 mm tolerance.
Table 2: Troubleshooting Common Leveling Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Large height difference (>0.5 mm) that is hard to correct. | Improper placement in ear bars, causing head tilt. | Remove and re-seat the animal in the ear bars, ensuring symmetrical and secure placement. |
| Suture lines are blurry and difficult to identify. | Tissue or fascia obscuring the skull. | Use a cotton swab with hydrogen peroxide to clean the skull surface gently. Use higher magnification on the surgical microscope. |
| Consistent drift in measurements. | Loose manipulator or unstable frame. | Check that all components of the stereotaxic frame and manipulator are tightly secured. Calibrate the equipment. |
The Scientist's Toolkit: Essential Materials and Reagents
Successful execution of the leveling procedure and subsequent stereotaxic surgery requires a specific set of tools and reagents.
Table 3: Essential Research Reagents and Equipment for Stereotaxic Surgery
| Item | Function / Description | Example Vendors / Sources |
|---|---|---|
| Stereotaxic Frame | Precision instrument for head fixation and 3D navigation. | Kopf Instruments, RWD Life Science, Harvard Apparatus, Stoelting [1] |
| Micromanipulator | Provides motorized or manual precise movement in ML, AP, and DV axes. | Integrated into stereotaxic systems; also available from New Scale Tech [33] |
| Isoflurane Anesthesia System | Vaporizer and tubing for delivery of inhaled anesthetic. | E-Z Systems, Pivetal [34] [7] |
| Animal Warming Pad | Active warming system to prevent hypothermia during surgery, critical for survival. | Kent Scientific, Custom PCB-based systems [34] [7] |
| Surgical Drill & Burrs | For performing craniotomy after leveling and coordinate marking. | Fine Science Tools (e.g., 0.5 mm burr) [34] |
| Stereotaxic Atlas | Reference for brain region coordinates relative to Bregma. | Paxinos & Franklin's Mouse Brain, Allen Institute CCF, STAM Atlas [1] [25] |
| Analgesics | Post-operative pain management (e.g., Meloxicam). | Pivetal, etc. [34] |
| Antiseptic Solution | For pre-surgical skin preparation (e.g., Betadine, 70% Ethanol). | Atlantis Consumer Healthcare, Fisher Scientific [34] |
Advanced Considerations and Recent Technical Advances
The fundamental principle of skull leveling remains unchanged, but recent technological advancements are enhancing its precision and integration into complex experimental workflows.
- Digital and Robotic Systems: Modern systems, like the Multi-Probe Micromanipulator System, incorporate Virtual Coordinate Systems (VCS). These software platforms allow for simulation, planning, and automated execution of probe insertions. They can integrate with open-source trajectory planning apps, providing real-time visualization of probe locations in a 3D brain model, which inherently relies on an accurately leveled skull [33].
- Integrated Workflows for Complex Interventions: Recent modified stereotaxic systems for models like severe Traumatic Brain Injury (TBI) aim to reduce surgery time. For instance, a 3D-printed header that combines the impactor and measurement probe can eliminate the need to change tool headers, thereby streamlining the process after the initial leveling is complete [7]. This highlights the importance of efficiency without compromising the foundational leveling step.
- High-Resolution Atlases for Validation: The development of ultra-high-resolution 3D reference atlases, such as the Stereotaxic Topographic Atlas of the Mouse Brain (STAM) with isotropic 1-μm resolution, provides an unprecedented level of anatomical detail [25]. While the surgical procedure still relies on skull landmarks, these atlases offer a powerful tool for post-hoc validation of targeting accuracy and for planning trajectories in complex anatomical contexts.
The procedure of using a micromanipulator to level the skull by ensuring Bregma and Lambda are at the same DV height is a cornerstone technique in rodent stereotaxic surgery. It is a direct and practical application of the theoretical framework that defines bregma and lambda as the key landmarks for establishing a reliable coordinate system. As the search results underscore, inconsistencies in measuring these landmarks are a significant source of error in neuroscience research [1]. Mastering this leveling procedure is therefore not a mere technicality but a critical factor in ensuring the accuracy, reproducibility, and overall success of sophisticated neuroscientific interventions, from basic lesion studies to advanced optogenetics and in vivo imaging. As technology evolves with more automated and digital systems, the fundamental requirement for a level plane of reference, established through this meticulous procedure, will remain unchanged.
The bregma point, defined as the intersection of the coronal and sagittal sutures on the rodent skull, serves as the fundamental origin (coordinate 0,0,0) for the three-dimensional Cartesian system used in stereotaxic neurosurgery [1] [35]. This technical guide details the principles and methodologies for accurately translating atlas-derived coordinates to in vivo surgical applications. Despite its widespread adoption—used in 96% of stereotaxic procedures—evidence indicates that inconsistent measurement practices and anatomical variations can introduce significant targeting errors, compromising experimental validity [1] [10]. This whitepaper, framed within a broader thesis on skull landmarks, provides an in-depth analysis of coordinate calculation, presents current error statistics, and outlines refined protocols and computational tools designed to enhance precision for researchers and drug development professionals.
Stereotaxic surgery enables precise navigation of the rodent brain for interventions such as drug delivery, lesioning, and neural recording [35]. The technique relies on a 3D Cartesian coordinate system, where the mediolateral (ML), anteroposterior (AP), and dorsoventral (DV) axes are anchored to cranial landmarks [1]. While lambda (the intersection of the sagittal and lambdoidal sutures) is critical for skull alignment, bregma is the predominant origin for the AP and ML axes [1] [10].
The renowned Paxinos and Franklin brain atlases are the gold standard for identifying target structures. However, a critical limitation is that these atlases are typically constructed from a single animal model (e.g., a 290g male Wistar rat), and they often lack explicit, detailed instructions for measuring the bregma point itself [1] [10]. This can lead to laboratory-specific variations in practice. Furthermore, anatomical differences between the atlas reference brain and experimental subjects in terms of strain, sex, age, and weight introduce another layer of systematic error [10] [35]. Recognizing these challenges is the first step in mitigating them and improving the reliability of stereotaxic targeting.
Quantitative Analysis of Stereotaxic Practices and Accuracy
Understanding the current state of the field is crucial for identifying areas for improvement. The following tables summarize key quantitative data on stereotaxic practices and their impact on accuracy.
Table 1: Current Stereotaxic Practice in Rat Models (Analysis of 235 publications) [10]
| Aspect of Practice | Finding | Percentage of Studies |
|---|---|---|
| Stereotaxic Origin | Use Bregma as the origin point | 96% |
| Atlas Referencing | Referenced the Paxinos Atlas | 57% |
| Subject Matching | Used subjects resembling the Paxinos Atlas rat | 10% |
| Accuracy Verification | Did not perform any implant accuracy check | 39% |
| Reporting of Accuracy | Clearly reported the number of on-target implants | 8% |
Table 2: Common Sources of Error in Stereotaxic Surgery [1] [10] [35]
| Error Category | Specific Source | Impact on Accuracy |
|---|---|---|
| Anatomical Variation | Strain, sex, age, and weight differences from atlas reference | Systematic error in coordinate calculation |
| Landmark Identification | Inconsistent identification of the bregma point | Incorrect setting of the coordinate system origin |
| Surgical Procedure | Skull misalignment after drilling or brain surface deformation post-craniotomy | DV coordinate errors; can exceed 100µm |
| Atlas & Tool Limitations | Discrepancies between different atlases; use of manual vs. digital rulers | Unavoidable random and systematic errors |
Established Experimental Protocols for Coordinate Calculation
Core Protocol: Standard Coordinate Translation from Bregma
This is the foundational method for most stereotaxic procedures [1] [35].
- Step 1: Atlas Coordinate Acquisition. Identify the 3D stereotaxic coordinates (AP, ML, DV) for your target brain structure from the appropriate reference atlas (e.g., Paxinos and Franklin). Note the specimen used to create the atlas.
- Step 2: Animal Preparation and Skull Exposure. Anesthetize the rodent and securely fix its head in the stereotaxic apparatus. Perform a midline incision to expose the skull and clean the surface to ensure the sutures are visible.
- Step 3: Skull Leveling (Critical Alignment). Using the stereotaxic manipulator, adjust the head position until the heights of the bregma and lambda points are identical in the DV axis. This ensures the skull is flat and aligned with the horizontal plane of the atlas.
- Step 4: Bregma Coordinate Zeroing. Carefully lower the tip of the stereotaxic probe or needle directly onto the bregma point. Set the readings of the AP, ML, and DV scales to zero.
- Step 5: Target Coordinate Calculation and Movement. Move the probe to the target coordinates relative to bregma. For example, to target a structure at AP +2.0mm, ML -1.5mm, you would move the probe 2.0mm anterior and 1.5mm lateral from bregma. The DV coordinate is typically measured from the dura or brain surface.
Advanced Protocol: Mathematical Adjustment for Surface Deformation
Installing a cranial window for optical imaging deforms the brain surface, invalidating standard DV coordinates. This protocol uses a mathematical approach to correct coordinates [36].
- Step 1: Pre-Craniotomy Landmark Registration. Before opening the skull, identify and record the stereotaxic coordinates of several (e.g., 4-6) vascular landmarks on the brain surface visible through the skull.
- Step 2: Cranial Window Implantation and Re-registration. Perform the craniotomy and implant the cranial window. After the brain stabilizes, re-identify the same vascular landmarks and record their new pixel coordinates from the microscopic image.
- Step 3: Conversion Function Calculation. Use a quadratic approximation model with L2 regularization to compute a mathematical function that maps the new pixel coordinates of the landmarks back to their original stereotaxic coordinates. This function accounts for the global deformation of the brain surface.
- Step 4: Target Coordinate Transformation. Apply the calculated conversion function to the pixel coordinates of your target region of interest (identified via optical imaging) to obtain its corrected stereotaxic coordinates for subsequent implantation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Equipment for Stereotaxic Surgery
| Item | Function / Application |
|---|---|
| Stereotaxic Apparatus (e.g., from Kopf Instruments, RWD Life Science) | Provides the rigid frame and micromanipulators for precise 3D navigation [1]. |
| Digital Stereotaxic Ruler | Offers higher precision in reading coordinates compared to manual vernier scales [10] [35]. |
| Paxinos & Franklin Brain Atlases | The standard anatomical reference for determining target coordinates in rats and mice [1]. |
| Anesthesia System (e.g., Isoflurane vaporizer) | Ensures the animal remains unconscious and immobile during the entire procedure. |
| Drill System | For performing a clean craniotomy at the calculated coordinates without damaging the underlying brain tissue. |
| Viral Vectors & Dyes | Used for targeted gene delivery (optogenetics, chemogenetics) or histological verification [35]. |
Visualizing Workflows: From Atlas to Accurate Implantation
The following diagrams illustrate the core workflow and an advanced automated method for landmark detection.
Stereotaxic Coordinate Workflow
Automated Bregma Detection
Discussion: Integrating Bregma and Lambda in a Coherent Thesis
The reliability of stereotaxic surgery hinges on the correct interpretation and application of cranial landmarks. While this guide focuses on bregma as the origin, its utility is defined in relation to lambda. The alignment of these two points establishes the critical horizontal plane for surgery [1] [35]. A key finding from recent literature is that bregma is not always the optimal origin. For caudal brain structures, selecting lambda or the interaural line midpoint as the origin can reduce error, as the target may be geographically closer to these alternative landmarks [10]. This demonstrates that a rigid, one-size-fits-all approach to coordinate calculation is flawed.
Furthermore, technological advancements are paving the way for a new paradigm. Automated detection of bregma and lambda using deep learning (Region-Based and Fully Convolutional Networks) can achieve a mean error of less than 300 μm, reducing human error and subjectivity [23]. These systems are robust to varying lighting conditions and animal orientation, offering the potential for greater standardization and reproducibility across laboratories. Integrating these computational tools with traditional surgical practice represents the future of high-precision stereotaxic research, strengthening the foundational thesis that accurate landmark identification is paramount.
The stereotaxic apparatus, based on a three-dimensional Cartesian coordinate system, revolutionized neuroscience research by enabling precise navigation within the skull along the mediolateral (ML), anteroposterior (AP), and dorsoventral (DV) axes [28]. In rodent models, the bregma and lambda skull landmarks serve as the fundamental anatomical reference points for this navigation system. The consistent use of these landmarks is paramount, as the correct setting of the bregma can significantly decrease stereotaxic errors [28]. Despite their importance, notable discrepancies exist in how different brain atlases describe and utilize these landmarks, and recent studies have found variances in skull and brain landmark measurements [28]. This technical guide details advanced applications of these landmarks for lesioning, viral vector delivery, and device implantation, framing these procedures within the broader context of reproducible and precise rodent neurosurgical research.
Fundamental Principles: Establishing a Stereotaxic Coordinate System
The stereotaxic coordinate system uses bregma as the typical origin point (0,0,0) for navigation [28]. The process begins with the precise leveling of the skull, a critical step to ensure coordinate accuracy. This is achieved by measuring the z-coordinates of both bregma and lambda and adjusting the position of the animal's head until these coordinates are equal [37]. Although the renowned Paxinos and Franklin brain atlas is a standard laboratory resource, it lacks explicit instructions on bregma determination, a gap that can lead to procedural variations between laboratories [28].
Table 1: Core Stereotaxic Landmarks and Their Functions
| Landmark | Anatomical Definition | Role in Stereotaxic Surgery |
|---|---|---|
| Bregma | The point of intersection between the coronal and sagittal sutures [37] | Serves as the most common origin point (0,0,0) for the anteroposterior and mediolateral coordinate axes [28] [37] |
| Lambda | The point of intersection between the interparietal and sagittal sutures [37] | Used in conjunction with bregma to level the skull in the anteroposterior plane, ensuring a flat surgical field [37] |
Advanced Application I: Viral Vector Delivery for Gene Therapy
Viral vectors, including adeno-associated virus (AAV), lentivirus, and herpes simplex virus (HSV), are powerful tools for introducing transgenes into specific cells of the central nervous system [38] [37]. Local delivery directly to the brain parenchyma is often preferred to overcome the challenge of the blood-brain barrier and reduce off-target effects [39]. The accuracy of this delivery is entirely dependent on the precise targeting afforded by the bregma-based coordinate system.
Protocol: Stereotaxic Surgery for Viral Vector Delivery
The following protocol is optimized for viral delivery into the mouse brain but can be adapted for rats and for various viral types, including AAV and lentivirus [37].
- Instrument Preparation: Clean and sterilize the stereotaxic instrument and surgical tools. Position Hamilton syringes in the instrument arms and clear any blockages by flushing with 100% acetone followed by sterile PBS [37].
- Animal Anesthesia and Positioning: Anesthetize the animal and secure it in the stereotaxic instrument using ear bars and an incisor adapter. Ensure the head is firmly secured and unable to move laterally [37].
- Skull Exposure and Leveling: Make a midline incision on the scalp and use surgical clips to retract the skin. Clean the skull to visualize bregma and lambda. Measure the z-coordinates of both landmarks and adjust the head position until they are equal, ensuring a level skull [37].
- Coordinate Calculation: Position the tip of the Hamilton syringe at bregma and record the x, y, and z coordinates. Subtract the atlas-derived coordinates of the targeted brain region to determine the precise injection site [37].
- Skull Perforation: Position the syringe at the calculated x and y coordinates. Using a dental drill with a 0.6 mm burr, carefully thin the skull at this location without damaging the brain [37].
- Viral Loading and Injection: Draw the viral solution (e.g., 0.5–1 μL of ~5 × 10⁵ infectious units/μL) into the Hamilton syringe, optionally separated from the PBS in the syringe by a small air bubble. Lower the syringe to the target z-coordinate and infuse the virus at a slow rate (e.g., 0.1 μL per minute). Allow 5 minutes post-infusion for diffusion before slowly retracting the syringe [37].
- Post-operative Care: Close the incision and provide analgesics. Monitor the animal during recovery. Maximal transgene expression for tools like HSV-delivered transcription factors typically occurs 2–3 days post-surgery and persists for 8-10 days [37].
Visualization and Validation of Viral Delivery
Advanced imaging techniques are crucial for validating the distribution of viral vectors. One approach co-infuses gadolinium-loaded liposomes (GDL) with the viral vector, allowing for real-time magnetic resonance imaging (MRI) visualization of the convective delivery process [40]. Studies have shown a close correlation between the distribution of GDL on MRI and subsequent transgene expression confirmed via immunohistochemistry, particularly for certain serotypes like AAV1 [40].
For high-resolution, quantitative analysis, computational pipelines can reconstruct and quantify the 3D distribution of viral vectors from 2D microscopy images of brain sections. These methods can distinguish between different viral vectors, such as Adeno virus (AdV) and AAV, which exhibit varying transport properties in the brain [39].
Advanced Application II: Device Implantation for Localized Drug Delivery
Beyond viral vectors, the bregma-lambda coordinate system is essential for the precise implantation of devices for localized and sustained drug delivery within the brain. This approach mitigates challenges associated with systemic administration, such as limited blood-brain barrier crossing and off-target effects [39].
Modalities for Localized Delivery
- Needle Injection: The standard method using a Hamilton syringe for simple bolus injections [39].
- Liquid-Filled Capsule Implantation: A method for passive, controlled drug release over several weeks. Custom capsules made from biocompatible polymers are implanted, allowing the drug to diffuse passively through side microports [39].
- Convection-Enhanced Delivery (CED): A technique that uses fluid pressure to generate bulk flow, propagating therapeutics over larger volumes within the extracellular space [40].
- Advanced Robotic Systems: Emerging platforms, such as remote-controlled millimeter-scale robots (Bionaut bots), are being developed for site-specific drug ejection or cargo drop-off, representing the next generation of precise local delivery [39].
Table 2: Key Reagents and Materials for Stereotaxic Procedures
| Research Reagent / Material | Function in Procedure |
|---|---|
| Hamilton Syringe (5 μL) with 33G RN Needle | Precise injection of nanoliter-to-microliter volumes of viral vectors or other agents into the brain parenchyma [37] |
| Adeno-Associated Virus (AAV) | A popular viral vector platform for gene therapy due to its safety profile and capacity for cell and tissue specificity [39] |
| Gadolinium-Loaded Liposomes (GDL) | Co-infused MRI contrast agent that acts as a surrogate to visualize the real-time distribution of convectively delivered therapeutics [40] |
| Liquid-Filled Polymer Capsule | An implantable device for passive, controlled release of a drug solution over an extended period (e.g., several weeks) [39] |
| Ketamine/Xylazine Mixture | Anesthetic combination administered via intraperitoneal injection to achieve a surgical plane of anesthesia for the duration of the procedure [37] |
Quantitative Analysis of Methodological Rigor in Preclinical Models
A systematic review of preclinical studies using rodent models of post-surgical pain reveals critical trends and gaps in methodological reporting that are relevant to all stereotaxic surgery applications [41]. An analysis of 674 studies found that 83% of studies used only male animals, most without providing a scientific rationale, introducing a significant sex bias [41]. Furthermore, methodological rigor remains limited; randomization and blinding were reported in just over half of the studies, and sample size calculations in only 18% [41]. These reporting trends highlight areas for improvement to enhance the translational relevance of stereotaxic neurosurgical research.
Table 3: Quantitative Trends in Preclinical Stereotaxic Surgery Models
| Methodological Category | Quantitative Finding | Implication for Translational Relevance |
|---|---|---|
| Sex Bias | 83% of studies used only male animals [41] | Limits generalizability of findings and fails to account for potential sex-based differences in treatment response |
| Behavioral Assessment | Mechanical outcomes dominated (87%); movement-evoked pain was rare (5%) [41] | A narrow focus on one outcome domain may overlook clinically relevant aspects of the condition being modeled |
| Methodological Safeguards | Randomization and blinding reported in ~50% of studies; sample size calculations in 18% [41] | Inadequate reporting of key safeguards raises the risk of bias and questions the robustness of the findings |
The bregma and lambda landmarks are the indispensable foundation for advanced stereotaxic procedures in rodent research, from basic lesioning to sophisticated viral vector delivery and device implantation. The accuracy of these procedures directly impacts the validity of experimental outcomes. While the techniques and tools continue to evolve—ranging from real-time MRI visualization to 3D computational reconstruction of drug distribution and advanced robotic delivery systems—the fundamental reliance on precise landmark identification remains constant. Addressing identified gaps in methodological rigor, such as justified sex inclusion and transparent reporting of randomization and blinding, will further enhance the translational value of research built upon this cornerstone technique.
Enhancing Precision: Troubleshooting Common Errors and Refining Surgical Techniques
In rodent stereotactic neurosurgery, the bregma point serves as the fundamental origin for the three-dimensional Cartesian coordinate system used to target specific brain structures. Despite its critical role, significant variability in the methodologies for locating the bregma across different laboratory practices and brain atlases introduces substantial targeting errors that confound experimental outcomes. This technical review examines the sources and magnitudes of these discrepancies, quantifying localization errors that can exceed hundreds of microns—dimensions greater than many rodent brain nuclei targeted in contemporary neuroscience research. We evaluate traditional manual approaches against emerging computational methods that leverage digital imaging and deep learning to standardize bregma identification. Furthermore, we present a synthesis of validated experimental protocols and software solutions that enhance reproducibility, providing researchers with practical frameworks for improving targeting accuracy in stereotactic procedures. Within the broader context of bregma and lambda landmarks in rodent surgery research, this analysis underscores the critical need for standardized methodologies to ensure experimental reliability and cross-study comparability in both basic neuroscience and drug development applications.
Stereotactic neurosurgery in rodents relies on a three-dimensional Cartesian coordinate system for precise navigation to specific brain targets, with the bregma point serving as the most commonly used origin for this system [1]. Defined anatomically as the midpoint of the curve of best fit along the coronal suture, bregma forms the intersection of the sagittal suture with the coronal suture on the rodent skull [1] [2]. In conjunction with the lambda point (the midpoint of the curve of best fit along the lambdoid suture), bregma enables the establishment of the anteroposterior (AP), mediolateral (ML), and dorsoventral (DV) axes fundamental to stereotactic targeting [1].
The accuracy of bregma localization carries profound implications for the validity of experimental outcomes across neuroscience research, particularly in studies investigating neurological disorders, circuit mapping, and therapeutic interventions. Despite its foundational importance, the process of bregma identification remains inconsistently implemented across research laboratories. The renowned atlases of Paxinos and Franklin lack explicit instructions for bregma determination, creating an methodological vacuum filled by variable laboratory practices [1]. This technical ambiguity has established an environment where targeting inaccuracies systematically compromise data quality and experimental reproducibility, presenting a critical challenge for researchers requiring precise anatomical placements in rodent brain studies.
Quantitative Analysis of Bregma Measurement Variability
Magnitude of Discrepancies in Bregma Localization
Empirical investigations reveal that methodological inconsistencies in bregma identification translate into substantial targeting errors with potentially severe consequences for experimental outcomes. A systematic study comparing traditional manual localization against a novel digital image analysis method demonstrated that in 44% of test subjects (11 out of 25 animals), the bregma position determined by these different approaches varied by ≥200 micrometers [2]. Given that many rodent brain nuclei and subregions measure less than 0.5mm in diameter, this discrepancy exceeds the size of many targeted structures in contemporary neuroscience research.
The quantitative impact of these localization errors becomes evident when examining stereotactic targeting accuracy. Histological analysis confirmed that the average total stereotaxic error was significantly reduced when the bregma point was determined using the digital image analysis approach compared to traditional methods [2]. These findings substantiate concerns that conventional bregma localization techniques introduce systematic variability that directly compromises targeting precision, potentially explaining the common observation that identical coordinates yield different actual target locations across experimental animals.
Comparative Analysis of Bregma Measurement Methodologies
Table 1: Comparison of Bregma Measurement Approaches
| Methodology | Error Range | Key Advantages | Key Limitations |
|---|---|---|---|
| Traditional Manual | ≥200μm in 44% of cases [2] | Rapid implementation, requires no specialized equipment | Subjective interpretation, dependent on operator expertise |
| Digital Image Analysis | Significantly reduced error [2] | Objective, mathematically defined reference point | Requires image capture and analysis setup |
| Deep Learning (Faster R-CNN + FCN) | <300μm mean error [23] | Automated, robust to lighting and orientation variations | Requires training dataset and computational resources |
The tabulated comparison reveals a clear progression in methodological sophistication, with automated approaches offering distinct advantages in objectivity and reproducibility. The deep learning framework, which integrates a region-based convolutional network (Faster R-CNN) with a fully convolutional network (FCN), demonstrates particular promise for standardizing bregma identification across laboratories and experimental conditions [23]. This approach maintains accuracy under varying lighting conditions and mouse orientations, addressing two significant sources of variability in traditional manual methods.
Experimental Protocols for Enhanced Bregma Localization
Digital Image Analysis Protocol
Based on methodologies validated in controlled studies, the following protocol establishes a standardized approach for precise bregma identification:
Skull Exposure and Preparation: Following standard surgical procedures, fully expose the skull cap and clean the surface to clearly visualize the coronal, sagittal, and lambdoidal sutures. Ensure proper lighting and minimize glare that could obscure suture boundaries.
Image Acquisition: Capture a high-resolution digital image (recommended minimum 2448 × 3264 pixels) of the exposed skull using a fixed-mount camera positioned perpendicular to the skull surface. Include a scale marker for spatial calibration [2].
Suture Identification and Curve Fitting:
- Import the image into analytical software (e.g., MATLAB, ImageJ) capable of curve-fitting algorithms.
- Manually or automatically identify points along the coronal suture.
- Apply a mathematical curve-fitting algorithm to determine the curve of best fit along the coronal suture.
Bregma Coordinate Calculation:
- Define the bregma point as the intersection between the mathematically fitted coronal suture curve and the midline sagittal suture [2].
- For enhanced accuracy, delineate the brain midline based on the temporal ridges of the skull rather than relying solely on the sagittal suture.
Coordinate System Establishment:
- Calculate the lambda point using a similar curve-fitting approach along the lambdoid suture.
- Establish the anteroposterior axis parallel to the midline plane crossing both bregma and lambda points [1].
This protocol's efficacy was demonstrated through experimental testing showing consistent reduction in stereotaxic error compared to traditional approaches [2].
Automated Detection Using Deep Learning
For laboratories with appropriate computational resources, an automated framework provides robust bregma localization:
Dataset Preparation: Compile a training dataset of rodent skull images with expert-annotated bregma and lambda points. The dataset should include variations in lighting conditions, mouse orientations, and skull morphologies to ensure model robustness [23].
Two-Stage Framework Implementation:
- Stage One (Skull Detection): Employ a Region-Based Convolutional Neural Network (Faster R-CNN) to detect the skull region within the raw input image, isolating the region of interest (ROI) from background elements [23].
- Stage Two (Landmark Segmentation): Utilize a Fully Convolutional Network (FCN) to segment bregma and lambda points within the identified skull ROI. The FCN is trained using Gaussian distribution labels centered on the true bregma and lambda points rather than binary classifications [23].
Coordinate Output: The system outputs the calculated coordinates of bregma and lambda relative to the image space, which can be transformed into stereotactic coordinates using a calibrated scale factor.
This automated approach achieved localizations with mean errors less than 300μm and demonstrated robustness to the anatomical variations that typically challenge manual identification [23].
Figure 1: Experimental Workflow Comparison for Bregma Localization. This diagram contrasts traditional, digital, and deep learning approaches to bregma identification, highlighting the progressive reduction in error rates with more computational methods.
Software Solutions for Registration and Analysis
Table 2: Software Tools for Atlas Registration and Bregma Localization
| Tool Name | Primary Function | Automation Level | Application Context |
|---|---|---|---|
| Brainways [42] | AI-based registration of coronal slices to 3D atlases | Automated with manual refinement | Fluorescence quantification, whole-brain activity mapping |
| QuickNII [43] | Affine spatial registration of brain sections to 3D reference atlases | Semi-automated | Spatial registration of serial section images |
| VisuAlign [43] | Non-linear refinement of atlas registration | Manual | Fine adjustment of section-to-atlas alignment |
| DeepSlice [43] | Linear atlas registration | Automated | Rapid registration of structurally intact sections |
| FCN + Faster R-CNN [23] | Bregma and lambda detection in skull images | Fully automated | Pre-surgical planning for stereotactic procedures |
Contemporary neuroscience research benefits from an expanding ecosystem of software tools designed to address registration challenges. Brainways exemplifies this progress with its over 93% atlas registration accuracy for coronal brain slices, leveraging deep learning algorithms trained on both mouse and rat brain atlases [42]. This cross-species training approach enhances model robustness, while the software's graphical interface enables manual refinement of automated registrations—a critical feature for addressing the tissue distortions common in histological processing.
For laboratories implementing automated bregma detection, the integrated framework combining Faster R-CNN for skull detection with FCN for landmark segmentation represents a specialized solution that directly addresses localization variability [23]. This approach transforms bregma identification from an expertise-dependent visual task to a standardized, quantifiable procedure, potentially reducing a significant source of inter-laboratory variability in stereotactic surgery.
Reference Atlases and Analytical Frameworks
The evolution of brain atlases continues to refine the anatomical context for stereotactic targeting. The Allen Mouse Brain Common Coordinate Framework (CCFv3) has emerged as a standard reference space, incorporating multimodal data from histology, immunohistochemistry, and gene expression to define anatomical boundaries [44]. Recent advancements include microenvironment-based atlases that nearly double the number of identifiable brain areas by incorporating dendritic morphological features, offering unprecedented granularity for anatomical targeting [44].
Complementing these structural resources, the Allen Mouse Brain Connectivity Atlas provides comprehensive wiring diagrams that inform functional targeting strategies, characterizing connection strengths varying over five orders of magnitude [45]. For developmental studies, newly available growth atlases capture dynamic changes in brain architecture during critical postnatal periods, enabling age-adjusted stereotactic planning [46]. These resources collectively provide the anatomical foundation upon which precise bregma-based coordinate systems depend.
The variability in bregma measurement methodologies across different brain atlases and laboratory practices represents more than a technical footnote in rodent stereotactic surgery—it constitutes a fundamental challenge to experimental reproducibility in neuroscience research. The evidence presented demonstrates that methodological inconsistencies generate targeting errors of sufficient magnitude to compromise interventions in small brain nuclei and confound functional analyses. The progression from traditional manual localization toward computationally-enhanced approaches offers a promising pathway for reducing this variability.
Looking forward, the integration of automated bregma detection with increasingly refined digital brain atlases presents an opportunity to establish new standards for stereotactic precision. The research community would benefit from consensus guidelines on bregma identification methodology, particularly for multi-center studies where consistency is paramount. Furthermore, the development of open-source automated tools could democratize access to precise localization methods, reducing the expertise barrier that currently contributes to inter-laboratory variability. As stereotactic techniques continue to enable increasingly sophisticated neuroscientific investigations, addressing the fundamental challenge of bregma measurement variability remains essential for ensuring both the validity of individual studies and the cumulative advancement of knowledge across the field.
Stereotaxic surgery in rodents, a cornerstone of neuroscience research, relies on the precise identification of cranial landmarks, primarily bregma and lambda, to establish a coordinate system for navigating the brain. Despite its widespread use, the technical procedure is susceptible to multiple sources of error that can compromise experimental validity and reproducibility. This whitepaper examines the critical impact of inter-animal variability—specifically strain, sex, and weight—and the inherent challenges of skull suture ambiguity on targeting accuracy. We synthesize current data to quantify these errors, present refined experimental protocols for mitigating them, and provide a toolkit for researchers to enhance the precision and reliability of stereotaxic surgery within the broader context of a thesis on rodent cranial landmarks.
The stereotaxic apparatus, developed by Horsley and Clarke, revolutionized neuroscience by enabling precise 3D navigation within the brain using a Cartesian coordinate system [1]. In rodents, the bregma, defined as the intersection of the coronal and sagittal sutures, is the most common origin for this coordinate system, while lambda, the intersection of the sagittal and lambdoidal sutures, is essential for aligning the skull in the dorsoventral plane [1] [10]. The renowned atlases of Paxinos and Franklin are the standard references for determining target coordinates from these points [1].
However, the assumption that bregma provides a stable and universally applicable origin is a significant oversimplification. Recent analyses highlight that discrepancies in skull and brain landmark measurements are common, and the specific procedure for measuring bregma varies considerably among laboratories [1]. Furthermore, stereotaxic atlases are typically constructed from a single animal of a specific sex, strain, and weight, creating a fundamental mismatch when applied to a genetically and physiologically diverse research population [10]. This paper delves into the specific sources of error stemming from this biological variability and the morphological challenges of the skull itself, providing a technical guide for achieving higher standards in stereotaxic research.
A systematic review of stereotaxic practices reveals the profound influence of biological factors and technical choices on experimental outcomes. The data in the tables below summarize key findings from the literature.
Table 1: Impact of Biological and Technical Factors on Stereotaxic Targeting
| Factor | Observed Impact / Prevalence | Source of Data |
|---|---|---|
| Animal Strain | Craniometric parameters and brain volume exhibit inter-strain variations. Only 10% of stereotaxically operated rats resemble the male Wistar "Paxinos atlas rat." [10] | Literature review of 235 publications (2019) [10] |
| Stereotaxic Origin Selection | Bregma was used as the origin in 96% of publications, even though for 27% of targets, the surgical entry point was closer to lambda. For 38% of targets, the midpoint of the interaural line was closer than bregma. [10] | Systematic review of 235 publications (2019) [10] |
| Accuracy Verification | 39% of studies did not perform any verification of implantation accuracy. Only 8% of studies clearly reported the number of on-target implants. [10] | Systematic review of 235 publications (2019) [10] |
| Skull Suture Development | In young rats, the width of the coronal suture decreases by 53.5% between 7 and 21 weeks of age, directly affecting landmark identification. [47] | Longitudinal μCT study of 12 rats (2025) [47] |
Table 2: Consequences of Suboptimal Stereotaxic Practices
| Practice | Consequence | Proposed Improvement |
|---|---|---|
| Using a single atlas for all strains/sexes | Systematic error in coordinate determination due to craniometric mismatches. [10] | Use strain-specific atlases or perform pilot studies to adjust coordinates. [48] |
| Always using bregma as the origin | Increased targeting error for caudal brain structures. [10] | Select the nearest stereotaxic origin (Bregma, Lambda, or Interaural Midpoint) to the target. [10] |
| Poor suture visualization | Inaccurate identification of Bregma/Lambda. [49] | Enhance suture visibility with dye (e.g., tissue marker) or dried blood. [48] |
| Inadequate post-op verification | Inability to correlate experimental data with accurate anatomical location, reducing data validity. [10] | Implement blinded histological verification of implant location and report exclusion rates. [10] |
Detailed Experimental Protocols for Error Mitigation
Protocol: Refinement of Stereotaxic Surgical Procedures
The implementation of comprehensive and refined protocols from pre- to post-surgery can drastically reduce animal morbidity, experimental error, and the number of animals required per group [50].
- Pre-Surgical Phase: Conduct a thorough clinical examination of the animal. Weigh the animal precisely to adjust anesthesia dosage and establish a baseline for post-operative recovery monitoring. Do not subject animals to food restriction before surgery [50].
- Preparation of the Surgeon and Asepsis: Implement a "go-forward" principle with distinct "dirty" (animal preparation) and "clean" (surgery) zones. The surgeon should perform a surgical handwash and wear a sterile gown, mask, and gloves. Surgical instruments must be sterilized, and the surgical site on the animal's head should be meticulously scrubbed with an iodine or chlorhexidine-based solution [50].
- Anesthesia and Animal Installation: Use blunt-tip ear bars for head fixation. Correct positioning is confirmed by observing a blink of the eyelids upon insertion into the external auditory canal. Apply ophthalmic ointment to prevent corneal desiccation. Maintain core body temperature with a feedback-controlled heating pad throughout the procedure [50].
- Skull Landmark Identification and Alignment: After a scalp incision and retraction, clean the skull surface. Enhance the visibility of the bregma and lambda sutures by applying a sterile tissue marker or using a small amount of dried blood from the incision [48]. Precisely level the skull by ensuring bregma and lambda are at the same dorsoventral coordinate.
- Coordinate Determination and Implantation: Use digital stereotaxic rulers and motorized arms to reduce manual errors [48]. For the dorsoventral coordinate, carefully note whether the reference is the skull surface, dura, or brain surface at the entry point [10].
- Post-Surgical Recovery and Verification: Provide appropriate analgesic care (e.g., buprenorphine) tailored to the procedure, noting that formulation can impact recovery [51]. Monitor weight and overall condition closely. Finally, perform histological verification of the implant site by a researcher blinded to the intended target to objectively assess accuracy [10] [48].
Protocol: Aseptic Technique for Stereotaxic Surgery
Maintaining asepsis is critical for animal welfare and data quality by preventing infections that can confound results.
- Environment and Materials: Sterilize all surgical tools (e.g., drapes, gowns, cannulas, drills, scalpels) via autoclaving (e.g., 30 minutes at 170°C). The stereotaxic frame, ear bars, and drill hand-piece should be thoroughly disinfected with appropriate wipes before surgery [50].
- Animal Preparation: Anesthetize the animal in a separate preparation area. Clean the paws and tail with a disinfectant scrub. In the surgical area, scrub the top of the head with an iodine foaming solution, rinse with sterile water, and then apply an iodine solution, allowing it to dry [50].
Visualization of Workflows and Relationships
Stereotaxic Coordinate Selection Workflow
Skull Suture Changes During Growth
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Precise Stereotaxic Surgery
| Item | Function / Explanation | Reference |
|---|---|---|
| Digital Stereotaxic Apparatus | Motorized arms and digital rulers (e.g., from Kopf Instruments) reduce human error in coordinate setting compared to manual systems. | [1] [48] |
| Strain-Specific Atlases | Brain atlases tailored to the specific rodent strain (e.g., C57BL/6 mouse) used in the experiment to account for craniometric differences. | [10] [48] |
| Tissue Markers / Surgical Dye | Used to stain the skull surface, enhancing the contrast and visibility of sutures like bregma and lambda for more accurate identification. | [48] |
| Blunt-Tip Ear Bars | Used for head fixation; designed to minimize trauma to the auditory canal. Correct placement is indicated by a blink reflex. | [50] |
| PEGylated-Peptide Nanoparticles | An advanced non-viral vector system for efficient delivery of genetic material (e.g., plasmid DNA for miR-200a) to cranial suture cells in gene therapy studies. | [52] |
| Buprenorphine SR Formulations | Slow-release (SR) analgesics for post-operative pain management. Note: The specific formulation (e.g., LAB vs. HCl) can significantly impact weight loss and recovery in TBI models. | [51] |
| Micro-CT Scanner | Enables high-resolution 3D imaging of the skull for ex vivo verification of implant placement or longitudinal study of suture morphology. | [47] |
The pursuit of precision in rodent stereotaxic surgery demands a critical acknowledgment of its inherent sources of error. As detailed in this whitepaper, the biological variables of animal strain, sex, and weight, coupled with the dynamic morphology and frequent ambiguity of the skull sutures bregma and lambda, are not minor complications but fundamental factors that can systematically bias experimental outcomes. The data and protocols presented provide a roadmap for elevating experimental standards. By adopting refined surgical techniques, selecting stereotaxic origins judiciously, employing modern tools, and rigorously verifying results, researchers can significantly enhance targeting accuracy. This commitment to methodological rigor is paramount for ensuring the validity, reproducibility, and ethical integrity of neuroscience research reliant on stereotaxic procedures.
Stereotaxic surgery in rodents is a cornerstone of modern neuroscience research, enabling precise interventions in specific brain regions for studies ranging from neurocircuitry analysis to the development of novel therapeutic strategies. The foundation of this technique rests upon a three-dimensional Cartesian coordinate system, where the skull landmarks bregma and lambda serve as the essential reference points for navigation [1]. The bregma, defined as the point where the coronal and sagittal sutures intersect, and the lambda, the junction of the sagittal and lambdoidal sutures, collectively establish the anterior-posterior and mediolateral axes, with their alignment critical for ensuring the skull is positioned in a standardized flat skull position [1] [22].
Despite the universal adoption of this system, a significant challenge persists: standardized atlas coordinates frequently fail to yield accurate targeting in practice. Discrepancies arise from multiple sources, including inter-strain neuroanatomical variations, differences in animal age and sex, and the inherent limitations of historical atlases that may not reflect true in vivo brain geometry [53] [54]. For instance, one study on Lister hooded rats found that to reach the ventral hippocampus, an anterior-posterior coordinate of 5.0 mm posterior to bregma was required, whereas the Paxinos and Watson atlas indicated a coordinate of 6.0 mm—a substantial 1.0 mm discrepancy that could critically impact experimental outcomes [53]. This paper details advanced methodological refinements, focusing on empirical coordinate determination and pilot surgeries, to overcome these challenges and achieve superior precision and reproducibility in stereotaxic procedures.
Limitations of Standard Atlas-Derived Coordinates
Over-reliance on standardized atlases without validation introduces systematic errors. The common practice of using a single atlas for determining stereotaxic coordinates is fraught with limitations that can compromise research validity.
- Strain and Sex-Based Variability: Brain morphology and craniometric parameters can exhibit considerable inter-strain and inter-sex differences. An atlas created from one strain (e.g., Sprague-Dawley rats) may not accurately represent the brain of another (e.g., Lister hooded rats) [53]. Similarly, differences in body size and weight between males and females of the same strain can lead to coordinate miscalculations [54].
- Atlas Creation Artifacts: Traditional histology-based atlases may be affected by tissue shrinkage or distortion during the fixation, sectioning, and staining processes. This means the published coordinates do not always correspond to the geometry of the living brain [53].
- Landmark Identification Ambiguity: The precise identification of bregma itself is not consistently described across atlases and can be challenging to pinpoint in practice due to suture anatomy, leading to variability in how the origin point is set by different surgeons [1].
Table 1: Common Sources of Error in Stereotaxic Coordinate Determination
| Error Source | Description | Impact on Targeting |
|---|---|---|
| Inter-strain Variation | Neuroanatomical differences between rat or mouse strains. | Systematic offset in coordinates; target region may be missed entirely. |
| Sex/Weight Differences | Brain size and skull shape vary with sex and body mass. | Incorrect scaling of coordinates, affecting depth and anterior-posterior placement. |
| Tissue Processing Artifacts | Shrinkage in histologically-derived atlas brains. | Coordinates overestimate the actual in vivo distance to the target. |
| Landmark Ambiguity | Inconsistent identification of Bregma and Lambda. | Incorrect setting of the coordinate system origin, leading to global inaccuracy. |
Empirical Coordinate Determination: A Methodological Framework
To address the limitations of standardized atlases, researchers can adopt a more tailored approach through empirical coordinate determination. This process involves refining target coordinates for a specific experimental setup using data collected from the actual animals and conditions being used.
Craniometric Measurement and Scaling
An initial adjustment can be made by measuring key distances on the subject's skull and comparing them to the atlas reference. This allows for a proportional scaling of coordinates.
Protocol for Craniometric Scaling:
- With the animal secured in the stereotaxic frame under anesthesia, accurately identify and record the precise distance between Bregma and Lambda.
- Compare this measured distance to the Bregma-Lambda distance reported in the reference atlas.
- Calculate a scaling factor:
Scaling Factor = Measured Distance / Atlas Distance. - Apply this scaling factor to the anterior-posterior (AP) coordinate of your target. For example, if your target is -4.0 mm AP from Bregma in the atlas and your scaling factor is 0.95, the adjusted coordinate would be -3.8 mm [54].
This method provides a first-order correction for overall skull size differences but may not account for all neuroanatomical variations.
Histological Validation and Error Analysis
The most definitive method for verifying targeting accuracy is post-mortem histological analysis. This process not only confirms successful injections or implantations but also creates a dataset for quantifying and correcting errors.
Protocol for Histological Validation and Error Correction:
- Surgery and Perfusion: Perform the stereotaxic surgery (e.g., tracer injection, device implantation) using your initial best-estimate coordinates. After an appropriate survival time, perfuse and fix the animal transcardially with paraformaldehyde.
- Brain Sectioning and Staining: Section the brain on a cryostat or microtome and stain the sections (e.g., Nissl stain) to visualize both the lesion/injection site and the surrounding neuroanatomy.
- Location Determination: Identify the actual location of the intervention by comparing the stained sections to the reference atlas. Precisely note the AP, ML, and DV coordinates of the center of the site.
- Error Calculation and Adjustment: Calculate the error vector by subtracting the target coordinates from the actual coordinates. This error can be random (variable between animals) or systematic (a consistent offset). A consistent systematic error indicates a need to adjust the baseline coordinates for future experiments [54]. For instance, if histological analysis consistently shows your injections are 0.3 mm too anterior, you would adjust your AP coordinate by -0.3 mm.
The Role of Pilot Surgeries in Technique Refinement
Pilot surgeries are an indispensable tool for refining complex stereotaxic procedures, optimizing coordinates, and improving surgical outcomes before commencing a full-scale experimental series. They are particularly valuable for establishing new targets, testing novel surgical protocols, or when working with a new animal strain.
Non-Survival Pilot Surgeries for Coordinate Optimization
Non-survival surgeries are a specific type of pilot study conducted to maximize data collection for coordinate refinement from a single animal, thereby adhering to the "reduction" principle of the 3Rs (Replacement, Reduction, Refinement).
Protocol for Non-Survival Pilot Surgery:
- Animal Model: Use an animal that has already been part of a previous, terminal experiment, where appropriate ethical approval is in place.
- Procedure: Under deep anesthesia, the animal is placed in the stereotaxic frame. Multiple tracts or injections can be made at slightly different coordinates surrounding the theoretical target.
- Immediate Perfusion and Analysis: Immediately after creating these tracts, the animal is perfused, and the brain is extracted, sectioned, and analyzed. This allows for the rapid assessment of which coordinate set most accurately hit the target structure without the need for a prolonged recovery period [55].
- Application: The data gathered from these procedures directly inform the final, refined coordinates to be used in survival surgeries for the main study, significantly reducing the number of animals discarded due to targeting errors.
Integration with Advanced Imaging and Atlasing
Modern neuroscience leverages high-resolution imaging to create more accurate, strain-specific brain templates. These resources can be integrated into the pilot surgery phase.
Utilizing Magnetic Resonance Imaging (MRI) Templates: Researchers can create or use existing in vivo MRI brain templates for their specific rodent strain. For example, the "Ratlas-LH" is an MRI-based atlas created specifically for the Lister hooded rat, providing stereotaxic coordinates that account for the in vivo dimensions of this strain's brain [53]. Using such a template for initial coordinate planning can drastically reduce initial targeting errors. Subsequent pilot surgeries with histological validation then serve to fine-tune these already improved coordinates.
Quantitative Validation of Refined Techniques
The implementation of empirical determination and pilot studies has demonstrated a tangible, positive impact on both animal welfare and research quality, as evidenced by longitudinal laboratory studies.
A long-term analysis of one laboratory's refinements in stereotaxic techniques from 1992 to 2018, which included the adoption of pilot surgeries and improved asepsis and analgesia, showed a clear and significant reduction in the proportion of animals excluded from final experimental groups due to surgical error or morbidity [55]. This success is directly attributable to the more reliable and reproducible surgical outcomes achieved through these refined methods.
Table 2: Impact of Technical Refinements on Experimental Outcomes
| Refinement Category | Specific Improvement | Measured Outcome |
|---|---|---|
| Surgical Precision | Use of pilot surgeries for coordinate refinement [55]. | Reduced rate of animal exclusion from final experimental groups. |
| Postoperative Care | Implementation of active warming systems to prevent anesthesia-induced hypothermia [7]. | Increase in survival rates from 0% to 75% in a severe TBI model. |
| Surgical Efficiency | Use of a modified stereotaxic device with a 3D-printed header to reduce instrument changes [7]. | 21.7% decrease in total operation time, reducing anesthesia exposure. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of these advanced techniques requires specific tools and reagents. The following table details key items for empirical coordinate determination and stereotaxic surgery.
Table 3: Essential Research Reagents and Materials for Stereotaxic Surgery
| Item | Function/Benefit | Application Notes |
|---|---|---|
| Isoflurane Anesthesia System | Provides safe and controllable inhalation anesthesia, allowing for adjustment of depth during long procedures. | Preferred over injectable anesthetics for survival surgeries due to better control and faster recovery [7] [56]. |
| Active Warming Pad | Maintains core body temperature during surgery, preventing anesthesia-induced hypothermia. | Critical for improving survival rates and post-operative recovery; can be PID-controlled [7]. |
| Digital Stereotaxic Instrument | Provides high-precision, digital readouts of coordinates, reducing manual reading errors. | Motorized arms can further enhance precision and ease of use [54]. |
| Sterile Surgical Instruments | Includes fine scissors, forceps, retractors, and drills for aseptic craniotomy. | Heat sterilization (e.g., 170°C for 30 min) is required to maintain asepsis [55]. |
| Antiseptic Solutions (Iodine/Chlorhexidine) | Pre-surgical skin preparation to prevent postoperative infection. | Applied as a scrub followed by a solution; allowed to dry before incision [55]. |
| Analgesics (e.g., Flunixine, Buprenorphine) | Pre-emptive and post-operative pain management. | Administration for at least 7 days post-surgery significantly improves welfare and recovery [56]. |
| Histological Stains (e.g., Nissl) | For post-mortem verification of target location. | Allows cytoarchitectural visualization to confirm the precise anatomical placement of an injection or implant [25]. |
Workflow and Logical Relationships
The following diagram illustrates the integrated workflow for planning and executing a precision stereotaxic surgery, incorporating the principles of empirical validation and pilot studies detailed in this guide.
Diagram 1: A workflow for precision stereotaxic surgery, showing how empirical adjustments and pilot studies integrate into the surgical planning process.
Refining Asepsis and Post-operative Care to Reduce Morbidity and Experimental Attrition
In rodent survival surgery, particularly for neuroscience and drug development research, the precise identification of the bregma and lambda landmarks on the skull is a foundational step in stereotaxic procedures. This precision directly influences both the success of experimental interventions and animal welfare. Inaccurate bregma measurement is a documented source of stereotaxic error that can compromise data quality, necessitate repeated procedures, and increase animal numbers to achieve statistical power—ultimately leading to increased experimental attrition [28]. Furthermore, breaches in aseptic technique during these sophisticated procedures introduce the risk of surgical site infections (SSIs), which are a significant cause of post-operative morbidity and mortality. SSIs not only cause pain and distress but also introduce uncontrolled variables that can alter physiological and behavioral responses, jeopardizing data integrity [57].
This guide integrates the critical technical aspects of stereotaxic surgery with robust aseptic and post-operative care protocols. Adherence to these refined methods ensures the welfare of animal subjects, enhances the reproducibility of experimental data, and aligns with the ethical and regulatory principles of the 3Rs, particularly Reduction.
Pre-Operative Asepsis: Foundation for Success
Preparation of the Surgical Environment
Aseptic technique is defined as methods used to reduce microbial contamination to the lowest practical level and is critical for minimizing the risk of post-operative infections [58] [59]. The surgical area must be a dedicated space that is easily sanitized and located away from high-traffic areas, doorways, and ventilation ducts to minimize air-borne contaminants [60] [61]. Benchtop surfaces should be smooth, non-porous, and disinfected before use with an appropriate agent such as 70% alcohol or a 10% bleach solution [60] [59]. It is recommended to separate the surgical area into three distinct zones: one for animal preparation, one for the surgery itself, and a separate quiet area for post-operative recovery [59].
Preparation of the Surgeon, Instruments, and Animal
Surgeon Preparation: The surgeon must wear a clean lab coat or gown, a surgical face mask, and a bouffant cap. A surgical hand scrub should be performed before donning sterile surgical gloves [58] [61]. For "tips-only" micro-surgeries, such as some stereotaxic procedures, sterile gloves may not be mandatory if approved by the IACUC; however, only the sterilized tips of the instruments may contact the surgical site [61].
Instrument Sterilization: All surgical instruments, including drill bits and cannulas, must be sterile at the start of the procedure. Steam autoclaving is the preferred method [58] [60]. When performing multiple surgeries, instruments must be re-sterilized between animals. A hot bead sterilizer (at 240–270°C for 15 seconds) is highly effective for this purpose, provided gross debris is wiped from the instrument tips first [58] [61] [59]. Chemical sterilization (e.g., with glutaraldehyde) is an alternative but requires thorough rinsing with sterile water afterwards [61] [59].
Animal Preparation: Hair should be removed from the surgical site with electric clippers, creating a margin of at least 1-2 cm around the planned incision [60] [59]. The skin is then aseptically prepared using a series of alternating scrubs. A common and effective protocol involves three alternating passes of a germicidal scrub (e.g., chlorhexidine or povidone-iodine) and a rinse (70% alcohol or sterile saline), moving in a concentric pattern from the center of the site outwards [58] [61] [59]. To prevent hypothermia, care should be taken to avoid oversaturating the animal with preparative solutions [61].
Table 1: Recommended Agents for Pre-operative Preparation
| Category | Agent Examples | Application Notes |
|---|---|---|
| Skin Antiseptic | Povidone-iodine, Chlorhexidine [57] [61] | Apply from center of incision site outward in concentric circles; repeat for 3 cycles [61]. |
| Rinse/Solution | 70% Isopropyl Alcohol, Sterile Saline [58] [61] | Used to rinse antiseptic scrub; chlorhexidine must be completely rinsed to avoid skin irritation [61]. |
| Instrument Sterilant | Steam Autoclave, Hot Bead Sterilizer, Chlorine Dioxide (e.g., Clidox) [58] [59] | Autoclaving is gold standard; bead sterilizers are for between-animal re-sterilization [58] [61]. |
Intra-Operative Techniques: Precision and Asepsis in Stereotaxic Surgery
Bregma and Lambda: The Foundation of Stereotaxic Accuracy
The stereotaxic apparatus relies on a 3D Cartesian coordinate system, with the bregma (the junction of the sagittal and coronal sutures) most commonly serving as the origin reference point [28] [37]. However, discrepancies exist in how different brain atlases and laboratories define and measure this landmark, which can significantly impact the accuracy of targeting specific brain regions [28]. The first critical step after securing the anesthetized animal in the stereotaxic instrument is to level the skull. This is achieved by adjusting the pitch of the incisor adapter until the dorsoventral coordinates of bregma and lambda are equal, ensuring the skull is flat in the anteroposterior plane [37]. Failure to properly level the skull is a major source of targeting error.
Aseptic Protocol During the Stereotaxic Procedure
Once the skull is leveled and the coordinates for the target brain region are calculated, a small incision is made along the midline of the scalp. The use of sterile drapes is highly recommended to prevent contamination of the surgical site and instruments [58] [60]. Commercial drapes or sterile Press'n'Seal wrap can be used to create a sterile field around the incision site [58]. A handheld dental drill with a sterile burr (e.g., 0.6 mm) is used to thin the skull above the injection site. The Hamilton syringe, which has been pre-cleared with acetone and sterile PBS, is then lowered through the burr hole to the target depth to deliver the viral vector or other injectate [37]. Throughout this process, the surgeon must avoid touching non-sterile surfaces (e.g., microscope controls, anesthetic tubing) with gloved hands or sterile instruments. If contamination occurs, gloves should be changed or instrument tips re-sterilized [58] [61].
The following workflow visualizes the integrated procedures for precise and aseptic stereotaxic surgery:
Post-Operative Care: Minimizing Morbidity and Promoting Recovery
Immediate Recovery and Analgesia
Post-operative care begins immediately after wound closure. Animals should be placed in a clean, warm, and quiet recovery cage. Supplemental heat via a circulating water blanket or a thermostatically controlled heating pad is critical to prevent hypothermia, a major risk in anesthetized rodents due to their high surface area to volume ratio [58] [60]. Animals must be monitored every 15 minutes until they regain sternal recumbency [61].
Analgesia is a mandatory component of post-operative care. The first dose of analgesics should be administered pre-emptively or immediately post-operatively, and treatment should continue for a minimum of 24-48 hours, though major procedures often require a longer duration (e.g., 1-5 days) [58] [61]. Withholding analgesics requires strong scientific justification and must be approved by the IACUC [58]. Supportive care, such as providing moistened food pellets on the cage floor, can enhance recovery by ensuring easy access to nutrition [37].
Surgical Site Infection (SSI) Monitoring and Assessment
Monitoring for SSIs should extend for at least 30 days post-surgery [62] [63]. The CDC criteria are commonly used for defining SSIs but can suffer from subjectivity, as they include "diagnosis by the attending physician" [63]. The ASEPSIS score is an alternative, more objective wound scoring system. It assigns points based on quantitative clinical findings: the percentage of wound area affected by serous exudate, erythema, purulent exudate, and separation of deep tissues, with additional points awarded for antibiotic use, drainage, and prolonged hospitalization [63]. A score greater than 20 defines an SSI, with higher scores indicating greater severity. One study found the ASEPSIS score had "very good" inter-rater agreement (α=0.856) compared to "moderate" agreement (α=0.587) for CDC criteria, making it a superior tool for consistent SSI identification in a research setting [63].
Table 2: Post-operative Monitoring and Intervention Guidelines
| Parameter | Recommended Practice | Rationale & Evidence |
|---|---|---|
| Analgesia Duration | At least 24-48 hours; 1-5+ days for major surgery [58] [61] | Prevents pain and distress, which are sources of uncontrolled experimental variation and morbidity. |
| Heat Support | Circulating water blanket or regulated heating pad during recovery [58] [60] | Prevents hypothermia, a common complication of anesthesia and surgery in rodents. |
| SSI Assessment | Use ASEPSIS score for objective, quantitative wound evaluation [63] | Provides "very good" inter-rater agreement (α=0.856), enhancing consistency and data quality [63]. |
| Suture/Clip Removal | 7 to 14 days after surgery [61] | Allows sufficient time for wound strength to develop, preventing dehiscence. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Rodent Survival Surgery
| Item | Function/Application | Technical Notes |
|---|---|---|
| Hot Bead Sterilizer | Rapid re-sterilization of instrument tips between surgeries in a multiple-surgery session. | 15-20 seconds at 240-270°C; instruments must be cooled before tissue contact [58] [61] [59]. |
| Hamilton Syringe | Precise microinjection of viral vectors (e.g., HSV, AAV) or other agents into the rodent brain. | Pre-cleared with acetone and sterile PBS before loading virus; allows for 0.1 μL/min injection rates [37]. |
| Tissue Adhesive (e.g., VetBond) | Closure of small, non-tension-bearing skin incisions. | Dissolves as the incision heals; does not require removal [58] [61]. |
| ASEPSIS Score Sheet | Objective, quantitative assessment of surgical wound healing and infection. | Scores >20 indicate SSI; superior inter-rater agreement vs. CDC criteria [63]. |
| Chlorhexidine or Povidone-Iodine Scrub | Pre-operative skin antisepsis to reduce bacterial load at the surgical site. | Apply in a "bullseye" pattern from center outward; alternate with alcohol or saline rinse [58] [57] [61]. |
Refining aseptic technique and post-operative care in rodent stereotaxic surgery is not merely an animal welfare imperative—it is a scientific necessity. The accurate identification of bregma and lambda ensures the precision of experimental interventions, while rigorous asepsis and comprehensive post-operative monitoring directly combat surgical site infections and post-operative morbidity. By adopting the evidence-based protocols outlined in this guide—from the objective ASEPSIS scoring system to the meticulous intra-operative aseptic techniques—researchers can significantly reduce experimental attrition, minimize uncontrolled variables, and enhance the reliability and reproducibility of their data. This integrated approach ultimately strengthens the validity of research outcomes in neuroscience and drug development.
In rodent stereotaxic surgery, the precise localization of intracranial structures is paramount. The canonical coordinate system, defined by bregma and lambda on the skull's midline, is the undisputed gold standard. However, this approach is not without limitations, including anatomical variability and the potential for error when bregma and lambda are not perfectly level. This whitepaper, framed within a broader thesis on optimizing cranial landmark usage, details the application of the interaural line (IAL) and temporal crests (TC) as supplemental landmarks. These alternatives provide a critical means of verification, enhancing the accuracy and reliability of stereotaxic targeting, which is crucial for reproducible research in neuroscience and drug development.
Landmark Definitions and Rationale
- Interaural Line (IAL): An imaginary line connecting the external auditory meatus (ear canals) on both sides of the head. It serves as a stable, externally referenceable axis that is independent of the sutures on the dorsal skull.
- Temporal Crests (TC): Bony ridges on the dorsal skull that form the lateral boundaries of the temporal muscles. They converge anteriorly and can be used as a secondary reference plane to assess skull tilt and alignment.
The primary value of these landmarks lies in their role as verifiers of the alignment established by bregma and lambda. A misalignment between the IAL/TC plane and the bregma-lambda plane indicates a skewed skull position, which would lead to significant stereotaxic error if uncorrected.
Quantitative Comparison of Landmark Systems
The following table summarizes key characteristics and comparative data for the standard and supplemental landmarks.
Table 1: Comparative Analysis of Rodent Cranial Landmarks
| Feature | Bregma-Lambda (Standard) | Interaural Line (IAL) | Temporal Crests (TC) |
|---|---|---|---|
| Anatomical Basis | Intersection of sagittal & coronal/lambdoid sutures | Line between external auditory meati | Bony ridges for temporal muscle attachment |
| Primary Use | Defining the anterior-posterior (AP) & medial-lateral (ML) axes | Verifying horizontal skull alignment; alternative zero point | Assessing rotational tilt and symmetry |
| Visibility/Access | Requires scalp incision and tissue clearing | External, but requires proper ear bar placement | Requires scalp incision |
| Reported Variability (AP Coordinate, SD in mm)* | ~0.2 - 0.4 mm | ~0.3 - 0.5 mm | Not typically used for direct coordinate calculation |
| Key Advantage | Gold standard, direct skull reference | Independent of suture visibility, good for vertical (DV) axis | Quick visual check for symmetry and tilt |
| Key Disadvantage | Sensitive to skull flatness error | Potential for ear bar trauma-induced misalignment | Less precise, more subjective |
*Note: Variability is species-, strain-, and age-dependent. Values are representative from published stereotaxic atlases.
Detailed Experimental Protocols
Protocol 1: Validating Skull Alignment Using the Interaural Line
This protocol ensures the skull is perfectly level in the stereotaxic frame before proceeding with bregma-lambda coordinate zeroing.
- Animal Anesthesia and Fixation: Anesthetize the rodent (e.g., using a ketamine/xylazine cocktail, 80/10 mg/kg i.p.) and securely place it in the stereotaxic instrument. Insert blunt ear bars into the external auditory meati. Ensure the incisor bar is set to the appropriate height (e.g., -3.3 mm for flat skull position in rats).
- Midline Landmark Exposure: Make a midline scalp incision and retract the tissue. Gently clear the periosteum and any connective tissue from the skull surface to expose bregma and lambda clearly.
- IAL Alignment Check: Lower the stereotaxic manipulator arm with a fine-tip probe attached. Position the probe tip directly over the IAL midpoint (theoretical point zero). Note the Dorsal-Ventral (DV) coordinate.
- Coordinate Comparison: Move the probe to a point directly over bregma. The DV coordinate reading should be identical (within a tolerance of ±0.05 mm) to the reading taken at the IAL midpoint. A discrepancy indicates that the skull is tilted along the AP axis.
- Correction: If a tilt is detected, adjust the angle of the head in the stereotaxic frame by very slightly loosening the ear bars and repositioning. Re-check the DV coordinates at IAL and bregma iteratively until they match.
Protocol 2: Assessing Symmetry and Rotation Using Temporal Crests
This protocol provides a rapid visual assessment to prevent rotational errors.
- Skull Exposure: Following steps 1-2 from Protocol 1, expose the dorsal skull.
- Visual Inspection: Identify the left and right temporal crests. They should appear as symmetrical, gently curving ridges.
- Manipulator-Assisted Verification: Using the stereotaxic manipulator, position the probe tip on the temporal crest at a fixed AP coordinate (e.g., at the level of bregma) on one side of the skull. Note the Medial-Lateral (ML) coordinate.
- Symmetry Check: Move the probe to the same AP coordinate on the contralateral temporal crest. The absolute value of the ML coordinate should be identical (e.g., +3.2 mm and -3.2 mm). Any significant difference indicates head rotation.
- Correction: Adjust the head rotation within the stereotaxic frame and re-verify until symmetry is achieved.
Workflow and Relationship Visualization
Landmark Verification Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Stereotaxic Landmark Verification
| Item | Function | Example Product / Specification |
|---|---|---|
| Sterotaxic Instrument | Precise 3D manipulation and head fixation | Kopf Model 940, RWD Life Science |
| Blunt Ear Bars | Secure placement in auditory meatus without trauma | Mouse/Rat specific, non-breakable tip |
| Anaesthetic Cocktail | Induce and maintain surgical anesthesia | Ketamine/Xylazine, Isoflurane vaporizer |
| Digital Stereotaxic Display | High-accuracy readout of AP/ML/DV coordinates | Software-integrated systems (e.g., Neurostar) |
| Fine Tungsten Probe | Precise landmark targeting for coordinate checks | Tip diameter: 50-100 µm |
| Surgical Micro-drill | Create craniotomy for intracranial access | High-speed (e.g., 40,000 RPM), foot-pedal controlled |
| Hamilton Syringe | Precise micro-injection of agents | 1-10 µL volume, 33-gauge needle |
| Bone Wax | Control bleeding from skull during drilling | Ethicon Bone Wax (Beeswax-based) |
Beyond the Basics: Validating Accuracy and Integrating Modern Digital Atlases
In rodent neuroscience research, stereotaxic surgery relies on external cranial landmarks, bregma and lambda, to target specific brain structures. However, biological variability introduces significant targeting errors that can compromise experimental validity. This technical guide details how post-hoc histological validation serves as an indispensable tool for confirming target accuracy, quantifying implantation errors, and ensuring the reliability of neuroscientific data. We present quantitative evidence of targeting variability, provide detailed protocols for histological verification, and discuss integrating this methodology within a rigorous experimental framework for drug development and basic research.
Stereotaxic coordinates, typically referenced from the bregma and lambda suture landmarks, are the cornerstone of targeted interventions in rodent brain research. The widespread assumption is that these coordinates, as defined in standardized atlases, reliably map to consistent functional domains across individual animals. However, a growing body of evidence challenges this assumption, revealing substantial inter-animal variability that limits targeting precision.
Critical studies have demonstrated that the location of functionally identified auditory cortices shows inter-animal variability as large as 1 mm along both the anteroposterior (AP) and dorsoventral (DV) axes when plotted in bregma-based stereotaxic coordinates [64]. This variability is not simply attributed to differences in brain size or suture irregularities but reflects fundamental differences in cortical geography across individuals [64]. Consequently, functional area boundaries in standardized brain atlases often correlate poorly with the true complexity of functional domains in living animals. Without direct validation, researchers risk misinterpreting experimental data, particularly when targeting small brain structures or when using techniques like optogenetics, fiber photometry, or electrophysiology that require precise anatomical placement.
Quantitative Evidence of Targeting Errors
The limitations of atlas-based targeting are not merely theoretical but have been quantitatively documented. The following table summarizes key findings from studies that have measured the magnitude of stereotaxic targeting errors.
Table 1: Quantified Stereotaxic Targeting Errors and Validation Methods
| Study Focus | Key Finding on Variability/Error | Validation Method Used | Implication for Targeting |
|---|---|---|---|
| Functional Auditory Cortex Mapping [64] | Inter-animal variability in functional area locations up to ~1 mm in AP and DV axes. | Intrinsic Signal Imaging | Atlas coordinates alone are insufficient for precise functional domain targeting. |
| Chronic Implant Localization [65] | In vivo micro-CT/MRI localization precision matches gold-standard post-mortem histology. | Micro-CT/MRI co-registration & Histology | Enables post-surgical verification and adjustment before lengthy experiments. |
| Vascular Phenotyping [66] | Active learning classifier (AUC=0.964) mines histology data to identify specific cell types. | Machine Learning on Histologic Images | Unlocks quantitative phenotypic data from histology for validation. |
These quantitative findings underscore a critical methodological imperative: reliance on bregma and lambda without subsequent confirmation is a high-risk strategy. Post-hoc histology provides the definitive evidence required to confirm that manipulations—whether injections, recordings, or lesions—were delivered to the intended neuroanatomical target.
Core Methodologies for Histological Post-hoc Validation
Perfusion, Fixation, and Sectioning
The validation process begins with proper tissue preparation. Following a terminal experiment, animals are transcardially perfused first with phosphate-buffered saline (PBS) to clear blood, followed by 4% paraformaldehyde (PFA) in PBS for fixation [67]. The brain is then extracted, post-fixed in PFA for 24-48 hours, and cryoprotected in a sucrose solution (typically 30%). Using a cryostat or vibrating microtome, the brain is sectioned into coronal slices 20-50 µm thick, with series of sections collected for different stains (e.g., every third section for Nissl stain and adjacent sections for immunohistochemistry).
Identifying Implantation Tracks and Lesion Sites
To visualize the trajectory of electrodes or optic fibers, sections are stained with standard histological dyes. Nissl staining (e.g., with Cresyl Violet) allows for the visualization of cytoarchitectonic boundaries and reveals physical tracks or glial scars caused by chronic implants [65]. The path of the implant and its terminal point can be traced through sequential sections and mapped onto corresponding atlas plates.
Immunohistochemistry (IHC) for Molecular Validation
IHC provides molecular specificity, confirming not just location but also the biological impact of an intervention.
- Primary Antibodies: Target-specific proteins such as c-Fos (for neuronal activity), GFAP (for astrocytic reactivity), Iba1 (for microglial activation), or tyrosine hydroxylase (for dopaminergic neurons) [68].
- Fluorescent Tags: Use fluorescently conjugated secondary antibodies (e.g., Alexa Fluor 488, 555, 647) for high-resolution imaging and multiplexing.
- Counterstaining: Nuclei are commonly counterstained with DAPI to provide anatomical context [67].
This workflow allows researchers to correlate the physical location of an implant or injection with changes in neuronal activity or neuroinflammatory responses, providing a multifaceted validation.
In Vivo Validation with Micro-CT and MRI
An advanced alternative or complement to traditional histology is the co-registration of micro-CT and MRI [65]. This method involves:
- Pre-operative micro-CT: Scanning the intact skull to establish a baseline 3D model of bone landmarks.
- Post-operative micro-CT: Scanning after implant placement. The post-op scan is co-registered to the pre-op scan, which is aligned to the stereotaxic coordinate system.
- MRI Integration: The micro-CT data is merged with an MRI scan, which provides soft-tissue contrast, allowing the implant to be visualized within the brain structure itself [65].
This non-invasive technique provides in vivo localization with precision comparable to histology, enabling researchers to verify targeting success shortly after surgery and adjust experiments accordingly, saving weeks or months of potentially wasted effort [65].
Table 2: Key Research Reagents and Materials for Histological Validation
| Item | Function/Description | Example Use Case |
|---|---|---|
| Paraformaldehyde (PFA) [67] | Cross-linking fixative that preserves tissue morphology. | Standard perfusion and immersion fixation for brain tissue. |
| Cresyl Violet | Nissl stain that labels neuronal cell bodies (Nissl substance). | Identifying cytoarchitectonic boundaries and lesion tracks. |
| DAPI Nucleic Acid Stain [67] | Fluorescent stain that binds strongly to DNA. | Counterstaining to label all cell nuclei in a section. |
| Primary Antibodies (e.g., anti-c-Fos, anti-GFAP) | Immunoglobulin proteins that bind specifically to a target antigen. | Detecting specific proteins of interest via IHC. |
| Fluorescent Secondary Antibodies | Antibodies conjugated to fluorophores that bind to primary antibodies. | Visualizing the location of primary antibodies. |
| Mounting Media with Antifade Agent [67] | Medium for preserving fluorescence under a coverslip. | Preparing slides for long-term storage and fluorescence imaging. |
| AAV.hSyn.GRAB.Ado1.0m [67] | Genetically encoded fluorescent sensor for detecting adenosine release. | Real-time monitoring of neuromodulator dynamics in specific circuits. |
Experimental Workflow and Data Interpretation
The following diagram illustrates the complete workflow from stereotaxic surgery based on skull landmarks to final histological confirmation.
Figure 1. Workflow for target validation, integrating both in vivo imaging and post-hoc histology pathways.
Principles of Valid Histopathologic Scoring
When analyzing histological data, adherence to principles of valid histopathologic scoring is essential for generating robust, quantitative data [69].
- Masking (Blinding): The pathologist or researcher scoring the histology should be masked to the experimental groups to prevent observational bias [69].
- Defined Scoring System: Use clear, objective definitions for each score. Avoid vague terms like "mild" or "severe"; instead, use quantitative thresholds (e.g., ">50% of the field of view") [69].
- Interpretation Consistency: Guard against "diagnostic drift" by periodically re-scoring initial samples to ensure intra-observer consistency throughout the scoring process [69].
Correlating Anatomy with Function
The ultimate goal of validation is to bridge anatomy and function. For instance, a study on cholecystokinin (CCK) demonstrated that high-frequency stimulation of the medial geniculate body (MGB) induced thalamocortical long-term potentiation (LTP) in the auditory cortex [68]. Histological verification of electrode and cannula placements in the MGB and ACx was crucial for interpreting the electrophysiological and behavioral results, confirming that the observed effects were due to specific modulation of the thalamocortical circuit [68].
Post-hoc histological validation is not merely a supplementary technique but a fundamental component of rigorous neuroscientific research, particularly when using bregma and lambda as primary surgical guides. The documented variability in individual brain anatomy makes it an essential practice for ensuring the accuracy, reliability, and interpretability of experimental data.
To maximize the effectiveness of histological validation, researchers should adopt the following best practices:
- Plan for Validation: Design experiments with histological verification in mind, including appropriate control groups and sample sizes for statistical power.
- Use Multiple Methods: Combine Nissl staining with immunohistochemistry to gain both anatomical and functional insights.
- Embrace Quantitative Methods: Utilize modern tools like machine learning-based image analysis [66] to extract objective, high-dimensional data from histologic sections.
- Report Validation Details: Transparently report methodological details of histological processing, scoring criteria, and the number of animals excluded due to off-target placements in scientific publications.
By systematically implementing robust post-hoc validation protocols, the research community can strengthen the foundation upon which our understanding of brain function and the development of novel neurotherapeutics is built.
Stereotaxic surgery in rodents, a cornerstone of modern neuroscience and drug development research, relies fundamentally on the precise identification of cranial landmarks, primarily bregma and lambda, to establish a three-dimensional coordinate system for brain navigation. Despite technological advancements, stereotaxic inaccuracies remain a significant source of experimental variability, potentially confounding results and impeding reproducible research. These inaccuracies manifest as two distinct types: systematic errors, which are reproducible deviations from the true value, and random errors, which are unpredictable fluctuations around the true value. This whitepaper provides an in-depth analysis of the sources and characteristics of these errors within the context of bregma and lambda landmark identification. We present quantitative data on the magnitude of these inaccuracies, detail robust experimental protocols for their identification and mitigation, and propose a standardized framework for error assessment. By providing researchers with the tools to differentiate, quantify, and minimize these errors, this guide aims to enhance the precision, reliability, and translational value of stereotaxic interventions in preclinical research.
The stereotaxic apparatus is predicated on a three-dimensional Cartesian coordinate system, enabling navigation along the anteroposterior (AP), mediolateral (ML), and dorsoventral (DV) axes [1] [21]. The origin of this system is not an intrinsic brain structure but is defined by visible landmarks on the skull. The most prominent of these is the bregma, defined as the point of intersection between the sagittal and coronal sutures [21]. A second critical landmark, the lambda, is located posteriorly, defined by the intersection of the sagittal and lambdoid sutures [21]. These two points form the anatomical basis for aligning the rodent skull into a standardized, level position, a prerequisite for accurate targeting [21] [70].
However, the reliance on these landmarks is a primary source of stereotaxic inaccuracy. Inter-animal biological variability introduces significant challenges, including irregularities in skull suture patterns, differences in brain size and shape due to factors such as strain, age, and sex, and variability in the relative positioning of functional areas within the cortex [71] [64] [70]. A fundamental issue is the discrepancy between standardized brain atlases and individual animal anatomy. Renowned atlases, such as those by Paxinos and Franklin, are constructed from average templates derived from a specific set of animals, which inevitably smooths over individual anatomical differences [1] [64]. Consequently, coordinates derived from any particular atlas should be considered only a first approximation for an experimental animal [71]. This whitepaper delineates how these foundational challenges manifest as either systematic or random errors and provides a strategic framework for their analysis and correction.
Theoretical Foundations: Systematic vs. Random Error
In the context of stereotaxic surgery, the concepts of accuracy and precision are paramount. Accuracy refers to how close a measurement is to the true value, while precision refers to how close repeated measurements are to each other [72]. These concepts are directly governed by the two types of experimental error.
Systematic Errors (Inaccuracy)
Systematic errors are reproducible, consistent deviations from the true value caused by flaws in the system, instrument, or methodology. They affect the accuracy of all measurements in a predictable way, meaning the measurements are consistently centred on the wrong target [73] [72].
- Causes in Stereotaxy: In stereotaxic surgery, systematic errors arise from biases inherent in the experimental setup.
- Atlas-Animal Mismatch: Using an atlas developed for one specific strain, sex, or age group on animals with different characteristics [71] [70]. For example, applying coordinates from a C57BL/6J atlas to a CD-1 mouse, which has a larger brain, will consistently lead to off-target placements in a predictable direction.
- Instrument Calibration Error: A miscalibrated stereotaxic frame or micromanipulator that consistently misreports positions [73].
- Incorrect Theory/Procedure: An operator consistently misidentifying the bregma point by a fixed vector (e.g., always 200 µm too anterior) or using an incorrect angle of entry [73] [70].
Random Errors (Imprecision)
Random errors are unpredictable fluctuations in measurements caused by unknown and unpredictable changes. They affect the precision or repeatability of measurements but do not necessarily cause inaccuracy if the measurements are averaged over a sufficient number of trials [73] [72].
- Causes in Stereotaxy: These are often stochastic and related to minor, uncontrollable variations.
- Inter-Animal Anatomical Variability: Inherent biological differences in skull suture morphology and brain geometry between individuals, even within the same strain, sex, and age [12] [64].
- Operator-Dependent Variations: Slight differences in how different researchers, or even the same researcher on different days, identify the exact center of bregma or level the skull [12].
- Unpredictable Environmental Factors: Minor fluctuations in the surgical environment, though these are typically minimal in a controlled setting [73].
The following diagram illustrates the relationship between these error types and their common sources in a stereotaxic workflow.
Quantitative Analysis of Stereotaxic Inaccuracies
Empirical studies have quantified the impact of these errors, revealing significant challenges in achieving precise targeting. The following tables summarize key findings on targeting variability and the biological factors contributing to it.
Table 1: Quantified Stereotaxic Targeting Errors from Experimental Studies
| Study / Target | Error Type | Magnitude of Variability / Inaccuracy | Key Finding |
|---|---|---|---|
| Image-based Assessment (Various targets) [12] | Overall Localization Error | Only ~30% of electrodes were within the targeted subnucleus. | Highlights a high rate of off-target placements even with standardized coordinates. |
| Functional Auditory Cortex Mapping [64] | Inter-Animal Variability (Random Error) | AP and DV coordinates varied by up to 1 mm across individuals. | Demonstrates substantial biological variability, limiting the accuracy of atlas-based targeting. |
| Comparison of Multiple Atlases [71] | Coordinate Discrepancies (Systematic Error) | Notable inconsistencies in structure boundaries across different atlas publications. | The coordinates from any single atlas are only a first approximation. |
Table 2: Biological Factors Contributing to Stereotaxic Variability
| Factor | Impact on Stereotaxic Accuracy | Manifests Primarily As |
|---|---|---|
| Strain, Age, & Sex [71] [70] | Differences in brain size and craniometric distances. | Systematic Error |
| Inter-Individual Anatomy [64] | Variability in functional area location and skull suture patterns. | Random Error |
| Suture Landmark Identification [1] [70] | Ambiguity in precisely defining bregma/lambda. | Both Systematic and Random Error |
Experimental Protocols for Error Assessment and Mitigation
Protocol 1: Standardized Stereotaxic Surgery with Skull Leveling
This core protocol is the foundation for minimizing initial errors [21] [70].
- Animal Preparation: Anesthetize the rodent and secure it in the stereotaxic frame using ear bars and an incisor bar. Apply eye ointment to prevent corneal drying.
- Surgical Exposure: Shave and disinfect the scalp. Make a midline incision and retract the skin and tissue to clearly expose the skull surface. Gently clean the skull to visualize the sagittal, coronal, and lambdoidal sutures.
- Landmark Identification: Identify bregma (intersection of sagittal and coronal sutures) and lambda (intersection of sagittal and lambdoid sutures). Use a sharpened needle or probe attached to the micromanipulator for precise measurement.
- Skull Leveling (Critical Step):
- Lower the probe to touch the skull at bregma and record the dorsoventral (DV) coordinate.
- Retract the probe, move it to lambda, and record the DV coordinate there.
- If the difference between the two DV measurements is greater than 0.1 mm, adjust the pitch of the head by raising or lowering the incisor bar. Repeat the measurements until bregma and lambda are within the 0.1 mm tolerance, ensuring the skull is level [21].
- Coordinate Calculation: With the skull level, return the probe to bregma and record the anteroposterior (AP) and mediolateral (ML) coordinates. Calculate the target coordinates relative to bregma based on the atlas.
- Drilling and Intervention: Move the probe to the calculated target coordinates, mark the skull, and drill a burr hole. Carefully incise the dura mater. Lower the surgical instrument (electrode, cannula, etc.) to the target DV coordinate to perform the intervention.
Protocol 2: Post-Operative Assessment of Targeting Accuracy Using Multi-Modal Imaging
This protocol, adapted from scientific studies, provides an objective, in vivo method for quantifying targeting accuracy, moving beyond traditional and often subjective histological verification [12].
- Post-Operative Image Acquisition:
- CT Imaging: If an implant is left in place (e.g., for DBS), acquire a post-operative CT scan. The metallic implant provides a high-contrast signal for precise 3D reconstruction of its physical location [12].
- MRI Imaging: Acquire a post-operative T2-weighted MRI. This will visualize the trace or lesion caused by the electrode/needle insertion, as well as any potential adverse effects like hemorrhage [12].
- Image Co-Registration and Spatial Normalization:
- 3D Trajectory Reconstruction and Error Quantification:
- Reconstruct the 3D path of the electrode or its trace from the imaging data.
- Precisely localize the tip of the electrode/trace in the normalized coordinate space.
- Quantify the target localization error by calculating the 3D Euclidean distance between the actual tip location and the intended target coordinates in the standard atlas [12].
- Error Type Diagnosis:
- Systematic Error: If the actual positions from a cohort of animals consistently cluster in a direction biased away from the target (e.g., all 200 µm too lateral), this indicates a systematic error, likely from an atlas mismatch or consistent landmark misidentification.
- Random Error: If the actual positions are scattered randomly around the target with no consistent directional bias, this indicates random error, primarily from inter-animal biological variability.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Stereotaxic Surgery
| Item / Reagent | Function / Application |
|---|---|
| Stereotaxic Frame & Micromanipulator [21] | Provides a stable platform and enables precise 3D movement of surgical tools. Essential for accurate coordinate targeting. |
| Vernier Scale [21] | Allows for exact distance measurements (to 0.1 mm or better) in all three dimensions. Critical for reproducible coordinate settings. |
| Anaesthetic (e.g., Isoflurane) [64] | Ensures animal immobility and analgesia during the surgical procedure, which is both an ethical requirement and a necessity for precision. |
| Viral Vectors (e.g., AAV) [21] [70] | Used for gene delivery, optogenetics, and chemogenetics. Precise stereotaxic injection is required for region-specific manipulation. |
| Histological Dyes (e.g., India Ink) [70] | Can be used to mark stereotaxic reference points on the skull or for post-mortem verification of injection sites. |
| Standardized Brain Atlases [1] [71] [64] | Provide the reference map and coordinates for brain structures. Must be appropriate for the animal's strain, age, and sex to minimize systematic error. |
The differentiation between systematic and random stereotaxic inaccuracies is not merely an academic exercise but a critical requirement for rigorous and reproducible neuroscience and drug development research. Systematic errors, often stemming from a mismatch between standardized atlases and experimental animals, can be proactively addressed by using appropriate animal models, validating coordinates through pilot studies, and employing advanced imaging for pre-operative planning. Random errors, inherent in biological systems, can be mitigated but not eliminated; they must be accounted for through robust experimental design, including adequate sample sizes and post-hoc verification of target placement using objective methods like the 3D imaging protocol outlined herein. A thorough understanding and application of these principles, centered on the critical appraisal of bregma and lambda landmarks, will significantly enhance the precision and translational impact of stereotaxic surgery.
The precision of stereotaxic surgery, a cornerstone of modern neuroscience and pre-clinical drug development, hinges on the accurate selection of a coordinate system origin. This origin point serves as the foundational reference from which all other brain targets are navigated. Within rodent models, the most prevalent skull landmarks used for this purpose are bregma, lambda, and the interaural line midpoint (IALM). The choice among these landmarks is not arbitrary but is influenced by factors including the target's location within the brain, the animal's anatomical characteristics, and the desired surgical accuracy. Framed within a broader thesis on the critical role of skull landmarks in rodent surgery research, this technical guide provides a comparative analysis of these three stereotaxic origins. We synthesize historical data, quantitative comparisons, and contemporary methodologies to equip researchers and drug development professionals with the evidence needed to select the most appropriate reference point, thereby enhancing the reliability and reproducibility of neuroscientific interventions.
The Anatomical and Historical Basis of Stereotaxic Landmarks
Anatomical Definitions
The rodent skull features several sutures—lines where bones articulate—that provide reliable landmarks for stereotaxic navigation.
- Bregma: Defined as the point where the coronal suture (running between the frontal and parietal bones) intersects the sagittal suture (the midline suture dividing the parietal bones) [1]. It is the most commonly used origin point for stereotaxic coordinates [11].
- Lambda: Located as the junction of the sagittal suture and the lambdoidal suture, which separates the parietal bones from the occipital bone [1]. Its appearance resembles the Greek letter lambda (λ) [1].
- Interaural Line Midpoint (IALM): An imaginary point located midway between the external auditory meatus (ear canals) of the animal [17] [11]. It is not a suture-based landmark but is defined by the stereotaxic apparatus's ear bars.
The Evolution of the Stereotaxic Apparatus
The foundational stereotaxic apparatus was developed by Victor Horsley and Robert Clarke in 1906, introducing a three-dimensional Cartesian coordinate system for precise navigation within the brain [1]. This system, which underpins all modern stereotaxic devices, allows for movement along three axes: anteroposterior (AP), mediolateral (ML), and dorsoventral (DV) [1]. The critical innovation was the use of stable, externally visible skull landmarks to infer the location of internal brain structures, a principle that remains unchanged. While early atlases for species like rats were established using the interaural line as the origin, the work of Paxinos and Watson popularized the use of bregma, especially with the introduction of the flat-skull position for standardization [74] [75].
Quantitative Comparison of Stereotaxic Origins
A key factor in selecting a stereotaxic origin is its spatial relationship to the intended target. Using an origin point closer to the target can theoretically reduce the error distance. An analysis of reported brain targets reveals the comparative advantage of each landmark.
Table 1: Comparative Analysis of Stereotaxic Origin Efficacy
| Stereotaxic Origin | Proportion of Targets with Shortest Euclidian Distance (ED) | Common Applications and Advantages | Key Limitations |
|---|---|---|---|
| Bregma | 170/295 (58%) of targets [11] | - Rostral (anterior) brain structures (e.g., prefrontal cortex, striatum) [17] [11].- Highest overall usage (225/235 studies) [11].- Demonstrates stable relationship with anterior commissure [11].- More stable than IALM across rats of different weights [74]. | - Accuracy decreases for caudal targets distant from bregma [11].- Can be difficult to localize precisely due to suture morphology [1] [28]. |
| Interaural Line Midpoint (IALM) | 111/295 (38%) of targets [11] | - Caudal (posterior) brain structures (e.g., cerebellum, brainstem) [17] [11].- Traditionally used in older stereotaxic atlases. | - High variability with changes in animal weight and skull length [74].- An electrode placement can recede by up to 4 mm as rats grow larger if IALM is used without adjustment [74]. |
| Lambda | 14/295 (5%) of targets [11] | - Alternative for caudal brain structures [11].- Essential for establishing the flat-skull position when leveled with bregma [1] [11]. | - Least commonly selected as the optimal origin [11].- The lambdoid suture can be difficult to visualize in vivo [11]. |
The data in Table 1 demonstrates that while bregma is the most versatile origin, a substantial portion of targets—particularly caudal ones—are more accurately referenced from IALM or lambda. This highlights the importance of a tailored approach rather than a one-size-fits-all use of bregma.
Experimental Protocols for Landmark Identification and Surgery
Establishing the Flat-Skull Position
The flat-skull (or horizontal) position is a critical prerequisite for accurate stereotaxic surgery, as it aligns the animal's skull with the plane used to create the stereotaxic atlas.
- Anesthesia and Fixation: The anesthetized rodent is securely placed in the stereotaxic frame using ear bars and a nose clamp [1].
- Landmark Exposure: A midline incision is made on the scalp to expose the skull and clearly visualize the bregma and lambda sutures [11].
- Skull Leveling: The dorsal-ventral (Z-axis) coordinate of both bregma and lambda is measured. The skull is then adjusted by raising or lowering the incisor bar until the dorsal coordinates of bregma and lambda are equal, ensuring the skull is flat [11]. Applying hydrogen peroxide (H₂O₂) to the skull can help better visualize the sutures if they are difficult to see [11].
Protocol for Targeting a Brain Structure
The following workflow, derived from established methodologies, outlines the key steps from planning to confirmation [76] [12].
- Selecting the Origin: The choice of origin (bregma, lambda, or IALM) should be guided by the data in Table 1. For a target near the cerebellum, using IALM would be more appropriate than bregma [17] [11].
- Calculating Coordinates: Once the origin point (e.g., bregma) is set to (0,0,0) in the stereotaxic manipulator, the target coordinates are calculated by applying the AP, ML, and DV offsets from the atlas.
- Accuracy Enhancements:
- Craniometric Adjustments: If the experimental animals differ in weight, strain, or sex from those used in the atlas, pilot studies and adjustments based on skull measurements (craniometrics) are necessary [17] [76].
- Digital Tools: Using digital stereotaxic rulers and motorized arms can reduce human error associated with manual adjustments [76].
- Image-Guided Surgery: For the highest precision, pre-operative MRI or CT scans of the individual animal can be co-registered to a 3D atlas (e.g., Allen CCF) for personalized coordinate planning, though this requires specialized equipment and software [12].
Post-Operative Verification of Targeting Accuracy
Confirming the final location of an implant or injection is crucial for validating experimental results.
- In Vivo Imaging: A robust method involves post-operative MRI to visualize the trajectory trace of a needle or electrode, or CT to image a physical implant like a DBS electrode [12]. These 3D images can be co-registered to a standard atlas template to quantitatively measure the Euclidean distance between the actual location and the intended target [12].
- Ex Vivo Histology: The traditional method involves perfusing the animal, sectioning the brain, and staining sections (e.g., with Nissl stain) to visually identify the electrode track or injection site and map it onto a corresponding atlas plate [1] [12]. This method is 2D, can be subject to tissue distortion, and is typically an end-point analysis.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Stereotaxic Surgery
| Item | Function & Application | Example Use Case |
|---|---|---|
| Stereotaxic Apparatus (e.g., Kopf, RWD) | Provides the physical framework for precise 3D navigation and head stabilization during surgery [1]. | Fundamental equipment for all stereotaxic procedures, including injections and implantations. |
| Reference Brain Atlas (e.g., Paxinos & Franklin, Allen CCF) | Provides the anatomical maps and standard coordinate sets for targeting specific brain regions [1] [75]. | Used to determine the AP, ML, and DV coordinates relative to a chosen origin for a target like the hippocampus. |
| Cresyl Violet (Nissl Stain) | Histological stain that labels Nissl substance in neuronal cell bodies, enabling visualization of cytoarchitectonic boundaries [1] [75]. | Used on brain sections post-surgery to verify the implantation site relative to anatomical structures. |
| Hydrogen Peroxide (H₂O₂) | A chemical agent used topically to clean the skull and enhance the contrast of cranial sutures for better landmark identification [11]. | Applied to the exposed skull during surgery to make bregma and lambda more visible. |
| Bromodeoxyuridine (BrdU) | A thymidine analog incorporated into DNA during synthesis, used as a marker for cell proliferation [11]. | Injected into animals post-surgery to label newborn cells in regions like the subventricular zone (SVZ) [11]. |
The selection of a stereotaxic origin—bregma, lambda, or the interaural line midpoint—is a fundamental decision that directly influences the accuracy and validity of neurosurgical interventions in rodent models. Quantitative evidence clearly demonstrates that bregma is the most stable and commonly used reference, especially for rostral brain structures. However, a dogmatic reliance on bregma for all targets is suboptimal. For caudal targets, the interaural line midpoint provides a theoretically shorter error distance, though it requires careful consideration of animal size. Lambda plays an indispensable role in establishing the flat-skull position but is less frequently the optimal surgical origin. The overarching recommendation is to align the choice of origin with the neuroanatomical target, use the animal's demographics to inform potential adjustments and employ post-operative verification techniques to quantify and account for targeting error. By adopting this nuanced, evidence-based approach, researchers in both academia and drug development can significantly enhance the precision and reproducibility of their stereotaxic procedures.
Stereotaxic surgery, a cornerstone of modern neuroscience, relies fundamentally on a Cartesian coordinate system anchored to cranial landmarks, with the bregma and lambda sutures serving as the principal reference points for rodent models [1]. The bregma, defined as the midpoint of the curve of best fit along the coronal suture, establishes the origin for anteroposterior (AP) and mediolateral (ML) coordinates, while the lambda ensures proper alignment of the skull [1] [2]. Despite its widespread use, this technique harbors inherent limitations. Rough determination of the bregma point can lead to targeting errors of hundreds of microns, a significant discrepancy given that many rodent brain nuclei are sub-millimeter in size [2]. Furthermore, traditional 2D stereotaxic atlases cannot fully represent the complex three-dimensional anatomy of the brain, creating a pressing need for more precise and integrative tools.
The Waxholm Space (WHS) atlas of the rat brain addresses these challenges by serving as a comprehensive open-access volumetric atlas resource [77]. It provides a detailed 3D map supporting data analysis and integration, bridging the gap between traditional surgical techniques and contemporary computational neuroscience. By including spatial coordinates for bregma and lambda, it facilitates conversion between conventional stereotaxic coordinates and its own standardized digital space, thus enabling researchers to leverage the precision of a 3D common coordinate framework while remaining grounded in established surgical practice [78]. This overview explores the core features, tools, and methodologies of the WHS atlas, framing it as an essential evolution in the infrastructure for rodent brain research.
Core Features of the Waxholm Space Rat Brain Atlas
The Waxholm Space atlas is a dynamic, evolving resource. Its fourth version, detailed in a 2023 Nature Methods publication, represents a significant expansion, featuring 222 annotated brain structures [77]. This includes 112 entirely new annotations and 57 revised structures compared to previous versions, achieving comprehensive coverage of all major brain systems [77].
The atlas is hierarchically organized, sorting brain structures into domains derived from the embryonic neural tube: telencephalon, diencephalon, mesencephalon, metencephalon, and myelencephalon [77]. This logical organization facilitates dynamic visualization and analysis at different levels of granularity. Key delineations include detailed subdivisions of the cerebral cortex, striatopallidal region, midbrain dopaminergic system, and thalamus, defined by combining structural magnetic resonance imaging (sMRI) and diffusion tensor imaging (DTI) with multimodal architectural data from histology and established literature [77].
Table 1: Key Specifications of the Waxholm Space Rat Brain Atlas (Version 4)
| Feature | Specification | Source |
|---|---|---|
| Template Subject | 80-day-old male Sprague Dawley rat | [78] |
| Primary Imaging Modalities | ex vivo sMRI and DTI | [77] [78] |
| Spatial Resolution | Isotropic (21.5 µm or 43 µm interpolated to 21.5 µm) | [79] |
| Total Annotated Structures | 222 | [77] |
| Hierarchical Organization | 5 main neural tube-derived domains | [77] |
| Stereotaxic Landmarks | Includes positions of bregma and lambda | [78] |
| License | CC BY 4.0 | [80] |
A critical feature for integration with existing methodologies is the atlas's inherent compatibility with traditional stereotaxic coordinates. The WHS coordinate system was defined using internal brain landmarks and explicitly includes the positions of bregma and lambda, allowing for straightforward conversion between its internal coordinates and the stereotaxic coordinates used in surgical procedures [78]. This design directly addresses the variability inherent in landmark identification, providing a stable digital foundation for planning and analyzing experiments.
Access and Visualization Tools
The WHS atlas is distributed as an open-access resource through platforms like the Neuroimaging Tools and Resources Collaboratory (NITRC) and is integrated into the EBRAINS research infrastructure [77] [78] [80]. As of October 2023, it had been downloaded over 33,000 times, reflecting its significant adoption by the research community [78].
The data is provided in the standard NiFTi format, ensuring compatibility with a wide array of neuroimaging software. Users can access the atlas through several pathways:
- Downloadable Files: The atlas can be downloaded with ready-to-use label and configuration files for popular software packages, including itk-SNAP for 3D inspection and rendering, the Mouse BIRN Atlasing Toolkit (MBAT), and the biomedical quantification tool PMOD [77] [80].
- Online Viewers: For users who wish to bypass local software installation, the EBRAINS platform offers an interactive atlas viewer. This web-based tool allows for arbitrary slicing of the brain in any plane, 3D surface rendering of selected structures, and navigation using either WHS or voxel coordinates [77] [78].
- Analysis Tools: The atlas is embedded in specialized tools for data analysis, such as the QuickNII tool for spatial registration of serial 2D images and the QUINT workflow for quantifying labeled objects in atlas-registered images [78].
Experimental Protocols and Methodologies
Atlas Construction and Registration Workflow
The creation of the WHS atlas and the registration of new data to its framework involve a meticulous, multi-stage protocol. The foundational template was constructed from a single perfusion-fixed Sprague Dawley rat brain, actively stained to enhance tissue contrast for MRI [79]. The brain was imaged within the cranium using multiple MRI protocols (T1, T2, T2*) at an isotropic resolution of 21.5 µm on a 9.4T magnet, producing high-contrast, low-distortion 3D image volumes [77] [79].
A pivotal aspect of the protocol is the integration of multimodal data. As a proof of principle, one study detailed a pipeline for registering cytoarchitecture, muscarinic M2 receptor distributions, and fiber architecture from histologically processed brains into the WHS [81]. This process involves:
- Tissue Sectioning and Blockface Imaging: The brain is cryosectioned, and a blockface image of each section is captured before it is removed from the microtome. These images provide an undistorted 3D reference volume for subsequent reconstruction [81].
- Histological Processing and Staining: Sections are processed for various modalities—e.g., silver staining for cytoarchitecture, receptor autoradiography for M2 receptors, or 3D Polarized Light Imaging (PLI) for nerve fibers [81].
- 3D Reconstruction and Registration: The blockface volume is first aligned to the WHS MRI template. The same transformation is then applied to the high-resolution histological image volumes, effectively mapping them into the standard WHS coordinate system [81]. This workflow enables the creation of 3D volumes of microscopic data within the common reference space.
The following diagram illustrates the workflow for integrating multimodal data into the Waxholm Space, a key process for enhancing the atlas's detail and utility.
Enhanced Surgical Targeting Protocol
The WHS atlas also informs improvements in conventional stereotaxic surgery. Recognizing that bregma identification is a major source of error, a refined protocol was developed. This method uses a digital image of the exposed skull cap, to which a curve is mathematically fitted to the coronal suture and the brain midline is delineated based on the temporal ridges. The intersection of these lines is defined as the bregma [2]. Systematic testing showed this computer-assisted method significantly decreased stereotaxic error compared to the "old, rough method" of visual estimation [2].
Furthermore, recent technical advances in the surgical procedure itself have been shown to enhance outcomes. The use of an active warming pad system to maintain rodent body temperature at 40°C during isoflurane anesthesia significantly improved survival rates in a severe traumatic brain injury model [7]. Additionally, modifying the stereotaxic apparatus with a 3D-printed header that integrates the needle for bregma-lambda measurement and the impactor/electrode insertion tool reduced the total operation time by 21.7%, thereby minimizing the duration of anesthesia and associated risks [7].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, tools, and materials essential for working with the Waxholm Space atlas and conducting related stereotaxic experiments.
Table 2: Essential Research Reagents and Tools
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| Stereotaxic Apparatus | Precise 3D navigation and fixation for rodent brain surgery. | Kopf Instruments, RWD Life Science; automated systems offer 1-micron resolution and motorized control [1] [82]. |
| Active Staining Solution | Enhances contrast for high-resolution MRI. | Mixture of formalin and ProHance (Gadoteridol) perfused into the brain [79]. |
| Histological Stains | Reveals specific architectural features in brain sections. | Silver stain for cytoarchitecture [81]; receptor autoradiography for neurotransmitter densities [81]. |
| 3D Polarized Light Imaging (PLI) | Visualizes the spatial orientation of nerve fibers and tracts at microscopic resolution. | Used to map fiber architecture into the WHS [81]. |
| Stereotaxic Alignment Tools | Precisely determine the bregma and lambda points. | Digital camera and image analysis software for mathematical fitting of sutures [2]. |
| Active Warming Pad | Maintains rodent body temperature during anesthesia, preventing hypothermia and improving survival. | Custom-made PCB heat pad with PID controller and thermal sensor [7]. |
Discussion and Future Directions
The Waxholm Space atlas represents a paradigm shift in rodent brain research, moving from static 2D plates to a dynamic, integrative 3D digital framework. It directly confronts the challenges of traditional stereotaxic surgery by providing a common coordinate system that mitigates the variability associated with landmark identification like bregma [2]. The ability to integrate diverse data types—from gene expression and receptor densities to connectivity and functional imaging—into a single reference space is accelerating multidisciplinary research and enabling more sophisticated computational models of brain structure and function [77] [81].
Future developments will likely focus on increasing the resolution and annotation detail of the atlas, potentially incorporating single-cell resolution data. Furthermore, the expansion of integrated multimodal datasets, such as the cyto- and receptorarchitectonic maps already demonstrated, will continue to enrich the atlas, transforming it from a purely anatomical guide into a multiscale platform for exploring the molecular and functional organization of the brain [81]. As these tools become more deeply embedded in the neuroinformatics ecosystem through platforms like EBRAINS, they promise to enhance reproducibility, data sharing, and collaborative discovery across the neuroscience community.
The following diagram summarizes the logical relationship between the challenge of traditional methods and the integrated solution provided by the Waxholm Space atlas and its associated tools.
Stereotactic neurosurgery in rodents, a cornerstone of preclinical neuroscience, has long relied on skull-based landmarks—bregma and lambda—for navigation. However, advancements in neuroimaging and computational biology are fundamentally reshaping this landscape. The integration of high-resolution magnetic resonance imaging (MRI) and sophisticated digital brain atlases is now supplementing, and in some contexts supplanting, traditional landmark-based approaches. This whitepaper examines the technical evolution of targeting methodologies, framing the transition within the persistent challenges associated with bregma and lambda. We detail how modern digital tools provide a more comprehensive, accurate, and standardized framework for navigating the rodent brain, thereby enhancing the precision and reproducibility of neuroscientific research and drug development.
The Established Standard: Landmark-Based Navigation and Its Limitations
The stereotaxic apparatus, based on a three-dimensional Cartesian coordinate system, has revolutionized neuroscience by enabling precise targeting of specific brain regions [1]. In rodents, the bregma and lambda points on the skull serve as the fundamental anatomical landmarks for establishing the coordinate origin.
- Role of Bregma and Lambda: The bregma, defined as the intersection of the coronal and sagittal sutures, is the most common origin point for stereotaxic coordinates. The lambda, the intersection of the sagittal and lambdoidal sutures, is essential for aligning the dorsoventral axis [1].
- Inherent Variability and Limitations: Despite their widespread use, these skull landmarks present significant challenges. Recent studies have identified substantial discrepancies in skull and brain landmark measurements. Coregistration of 3D µCT and MRI datasets from multiple mice revealed that the positions of bregma and lambda with respect to the underlying brain anatomy vary considerably between individuals. The largest distance between bregma z-positions was 1.2 mm, and between lambda z-positions was 1.68 mm, a degree of variability that precludes their use as reliable fiducials for high-precision registration [16]. Furthermore, renowned atlases like Paxinos and Franklin's often lack explicit instructions for bregma determination, leading to inconsistent application across different laboratories [1].
Table 1: Limitations of Traditional Skull Landmarks for Stereotactic Navigation
| Limitation | Description | Impact on Research |
|---|---|---|
| Anatomical Variability | The position of bregma and lambda relative to the brain varies significantly between subjects [16]. | Introduces targeting errors, reducing experimental consistency and reproducibility. |
| Ambiguous Definition | The specific procedure for measuring bregma is not consistently detailed in major brain atlases [1]. | Leads to inter-laboratory procedural differences, hindering cross-study comparisons. |
| Dependence on Skull Anatomy | Relies on the assumption of a fixed relationship between external skull sutures and internal brain structures. | Fails to account for individual neuroanatomical differences, strain, sex, or age-related variations [83]. |
The Digital Revolution: MRI and Digital Brain Atlases
The limitations of traditional methods have catalyzed the development of digital neuroanatomical tools. MRI-based brain atlases have emerged as pivotal resources, evolving from traditional printed histology atlases to sophisticated digital platforms that incorporate diverse, high-fidelity imaging datasets [84].
Technical Advantages of Digital Atlases
- Spatial Flexibility and Integration: Digital atlases provide an isotropic image volume, allowing interactive viewing of anatomical regions from arbitrary planes (coronal, sagittal, horizontal) without distortion. This enables seamless co-registration of individual experimental scans to a standardized template [83].
- Enhanced Accuracy and Standardization: By creating an average brain image from multiple subjects (e.g., 41 Fischer 344 rats), group-based MRI atlases minimize individual subject bias and capture population-level neuroanatomy. This approach provides a common spatial reference for the research community [83].
- Comprehensive Data Integration: Modern 3D reference atlases, such as the Allen Mouse Brain Common Coordinate Framework (CCF), incorporate multimodal datasets. These include histology stains, gene expression patterns, and mesoscale connectivity data, offering a richer context for experimental planning and analysis beyond simple structural anatomy [1].
Table 2: Comparison of Traditional and Digital Brain Atlas Approaches
| Feature | Traditional Printed Atlas | MRI-Based Digital Atlas |
|---|---|---|
| Spatial Representation | Fixed, 2D sectional planes | Flexible, interactive 3D volume |
| Underlying Data | Histology of a single subject | MRI from a group average (e.g., n=41) [83] |
| Standardization | Subject to individual anatomical variance | Population-based, reducing individual bias [83] |
| Integration Capacity | Limited | High (supports multi-modal data like genomics, connectomics) [1] |
| Automation Potential | Low; manual coordinate identification | High; enables automated segmentation and analysis [85] |
Creation of a Standardized Digital Atlas: A Methodological Workflow
The development of a high-resolution digital atlas, as exemplified for the Fischer 344 rat strain, involves a rigorous, multi-step protocol [83]:
- Animal Preparation and MRI Acquisition: A cohort of subjects (e.g., 41 rats at 4 months of age) is scanned in-vivo using a high-field MRI scanner (e.g., 7 Tesla Bruker Biospec). A 3D RARE (Rapid Acquisition with Relaxation Enhancement) sequence is used to acquire high-resolution T2-weighted images with an isotropic voxel size of 60 µm.
- Template Generation: The resulting individual scans are co-registered using an image registration pipeline (e.g., Pydpiper) to create an unbiased, high-resolution average template brain. This step statistically minimizes anatomical outliers and creates a representative model.
- Manual Segmentation and Labeling: The average brain image is manually segmented by trained raters. Structures and substructures (e.g., 71 regions) are delineated individually and bilaterally based on the image contrast and with reference to a canonical stereotaxic atlas (e.g., Paxinos and Watson).
- Validation and Dissemination: The finalized atlas, in both MINC and NIfTI file formats, is made publicly available. It includes summary statistics (e.g., mean and standard deviation of regional volumes) for the sample population, enabling future volumetric comparisons.
The Next Frontier: Deep Learning and Automated Registration
The integration of artificial intelligence (AI) is pushing the boundaries of digital atlasing further, enabling unprecedented speed and accuracy in brain parcellation and landmark identification.
AI-Powered Segmentation
Deep learning (DL) models, particularly convolutional neural networks like the nnU-Net, are now performing brain segmentation with accuracy comparable to established atlas-based methods but at a significantly faster rate. These models can be trained on diverse datasets encompassing different mouse strains, sexes, and ages, making them robust and widely applicable [85]. Once trained, such models can process new scans in minutes on a standard personal computer, bypassing the computationally intensive, non-linear registration steps required by traditional multi-atlas pipelines [85].
Automated Landmark Detection
To directly address the variability in identifying bregma and lambda, novel AI frameworks have been developed for their automated detection. One such method uses a two-stage deep learning approach [23]:
- Stage One - Skull Detection: A region-based convolutional network (Faster R-CNN) detects and isolates the skull region of interest (ROI) from a raw rodent skull image.
- Stage Two - Point Segmentation: A fully convolutional network (FCN), modified with residual networks and batch normalization, then segments the bregma and lambda points within the skull ROI. This system registers mean localization errors of less than 300 µm, demonstrating robustness to varying lighting conditions and animal orientations [23].
The following diagram illustrates the automated detection workflow.
The Scientist's Toolkit: Essential Research Reagents and Materials
The implementation of advanced targeting methodologies relies on a suite of specialized reagents and instrumentation.
Table 3: Key Research Reagents and Solutions for Advanced Neuro-Targeting
| Item / Solution | Function / Application | Example Use in Context |
|---|---|---|
| High-Field MRI Scanner | Generates high-resolution 3D anatomical images of the rodent brain. | Essential for creating baseline atlases and acquiring experimental subject scans (e.g., 7 Tesla Bruker BioSpec) [83] [85]. |
| Digital Brain Atlas | Serves as a standardized spatial reference for registration and segmentation. | Used as a template in software pipelines (e.g., ANTs, FSL) to map individual subject data into a common coordinate space [83]. |
| Deep Learning Segmentation Model | Enables fast, automated parcellation of brain structures from MRI data. | The nnU-Net framework can be trained on a labeled dataset to segment a new scan into major brain regions in minutes [85]. |
| Automated Landmark Detection Software | Accurately locates bregma and lambda from skull images, reducing human error. | A two-stage CNN/FCN framework can identify these points with a mean error of <300 µm, standardizing the surgical setup [23]. |
| Stereotaxic Apparatus with Digital Integration | Provides the physical platform for performing precise navigated surgeries. | Modern systems can integrate coordinate plans derived from digital atlases to guide probe, cannula, or optic fiber insertion [1]. |
The future of targeting in rodent models is unmistakably digital. While bregma and lambda will remain a foundational starting point for stereotactic surgery, their role is being redefined. The demonstrated variability in these skull landmarks [16] underscores the necessity for the more reliable and internally consistent framework offered by MRI-based digital atlases and AI. The convergence of high-resolution neuroimaging, standardized digital brain maps, and powerful deep learning algorithms is creating a new paradigm. This paradigm shift promises to enhance the precision, reproducibility, and throughput of neuroscientific experiments, ultimately accelerating the pace of discovery in basic research and therapeutic development. The ongoing challenge for the research community is to foster the widespread adoption of these tools and to develop even more integrated, user-friendly platforms that make high-precision targeting accessible to all.
Conclusion
Mastering the identification and application of the bregma and lambda landmarks remains fundamental to the success and reproducibility of stereotaxic surgery in rodents. While these sutural intersections provide the cornerstone of the 3D coordinate system, researchers must be aware of inherent challenges, including anatomical variability and atlas discrepancies. By adhering to refined surgical protocols, implementing rigorous troubleshooting measures, and validating results through histology, scientists can significantly reduce experimental errors and the number of animals required. The future of precise intracranial targeting lies in the integration of these classical anatomical skills with emerging technologies, such as high-resolution digital atlases and computational tools, which together will drive greater accuracy in neuroscience research and drug development.
References
- 1. Where do you measure the Bregma for rodent stereotaxic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10776314/]
- 2. A new approach to detection of the bregma point on the rat ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027009005317]
- 3. Coordinate Systems for Navigating Stereotactic Space [https://pmc.ncbi.nlm.nih.gov/articles/PMC7358954/]
- 4. Rodent Stereotaxic Surgery and Animal Welfare Outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3353515/]
- 5. Ultra Precise Mouse Stereotaxic [https://www.wpiinc.com/var-505313-just-for-mouse-stereotaxic-instruments.html?srsltid=AfmBOopv7EFH7o8DL9XezV9WlMidwrcWkdqtPQS5KT873Cuybdfy0MOg]
- 6. Stoelting's Just for Mouse™ Stereotaxic Instrument [https://stoeltingco.com/Neuroscience/Just-for-Mouse-Stereotaxic-Instruments~9640]
- 7. Modified stereotactic neurosurgery techniques for rodent ... [https://www.nature.com/articles/s41598-025-05328-y]
- 8. Bregma [https://en.wikipedia.org/wiki/Bregma]
- 9. Bregma [https://grokipedia.com/page/Bregma]
- 10. Stereotaxy in rat models: Current state of the art, proposals ... [https://www.sciencedirect.com/science/article/abs/pii/S0166432817315619]
- 11. Bregma - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/bregma]
- 12. Image-based in vivo assessment of targeting accuracy ... [https://www.nature.com/articles/srep38058]
- 13. Developmental mouse brain common coordinate framework [https://www.nature.com/articles/s41467-024-53254-w]
- 14. A mouse brain stereotaxic topographic atlas with isotropic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422980/]
- 15. Lambda (anatomy) [https://en.wikipedia.org/wiki/Lambda_(anatomy)]
- 16. 16 landmarks of the mouse brain have been validated as ... [https://www.frontiersin.org/10.3389/conf.fninf.2014.08.00028/event_abstract]
- 17. Bregma, lambda and the interaural midpoint in stereotaxic ... [https://pubmed.ncbi.nlm.nih.gov/3889509/]
- 18. Sutures of the skull: Anatomy [https://www.kenhub.com/en/library/anatomy/the-cranial-sutures]
- 19. The Skull | Anatomy and Physiology I [https://courses.lumenlearning.com/suny-ap1/chapter/the-skull/]
- 20. 3 Quick Tips to Remember the Sutures of the Skull [https://3d4medical.com/blog/quick-tips-to-remember-the-sutures-of-the-skull-anatomy-slices]
- 21. Video: Rodent Stereotaxic Surgery [https://www.jove.com/v/5205/rodent-stereotaxic-surgery]
- 22. Stereotaxic Atlases for Neuroscience Research [https://www.leicabiosystems.com/us/knowledge-pathway/navigator-through-the-brain-stereotaxic-atlases-for-neuroscience-research/]
- 23. Automatically detecting bregma and lambda points in rodent ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0244378]
- 24. Stereotaxic Rodent (artículo) | JoVE Surgery [https://www.jove.com/es/t/5205/rodent-stereotaxic-surgery]
- 25. A mouse brain stereotaxic topographic atlas with isotropic ... [https://www.nature.com/articles/s41586-025-09211-8]
- 26. Accuracy and reliability of 3D cephalometric landmark ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539169/]
- 27. Modified stereotactic neurosurgery techniques for rodent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12214793/]
- 28. Where do you measure the Bregma for rodent stereotaxic ... [https://www.sciencedirect.com/science/article/pii/S266724212300060X]
- 29. Guidelines for Anesthesia and Analgesia in Rats - IU Research [https://research.iu.edu/policies/animal-care/lar-guidelines/anesthesia-analgesia-guidelines-rats.html]
- 30. Anesthesia (Guideline) - Vertebrate Animal Research [https://animal.research.uiowa.edu/iacuc-guidelines-anesthesia]
- 31. Surgical Techniques for Chronic Implantation of Microwire ... [https://www.ncbi.nlm.nih.gov/books/NBK3895/]
- 32. Acrylic Resin Molding Based Head Fixation Technique in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4781350/]
- 33. Multi-Probe Micromanipulator System [https://newscaletech.com/multi-probe-micromanipulator/]
- 34. Protocol for GCaMP expression and in vivo calcium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305568/]
- 35. Techniques in Stereotaxic Surgery [https://conductscience.com/techniques-in-stereotaxic-surgery/?srsltid=AfmBOookYUCVvnsBiSWmAvyNdQz6JCTDaniU6jddZ4lSZDA8rJ-6nLTa]
- 36. Methods for calculating the stereotaxic coordinates of rat ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027021002089]
- 37. Viral Expression of Epigenome Editing Tools in Rodent Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5963503/]
- 38. Viral Vectors [https://landmarkbio.com/viral-vectors/]
- 39. Quantitative 3D reconstruction of viral vector distribution in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12172745/]
- 40. Real-time MR imaging of adeno-associated viral vector ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2730220/]
- 41. systematic review AND QUANTITATIVE TREND analysis of ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763425004233]
- 42. Mapping brain-wide activity networks: brainways as a tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518845/]
- 43. Software and pipelines for registration and analyses of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504246/]
- 44. A mouse brain atlas based on dendritic microenvironments [https://www.nature.com/articles/s41593-025-02119-6]
- 45. Publication in Nature Showcases Most Comprehensive ... [https://alleninstitute.org/news/publication-in-nature-showcases-most-comprehensive-wiring-diagram-of-the-mammalian-brain-to-date/]
- 46. New detailed brain growth atlas in mice offers insights into ... [https://pennstatehealthnews.org/2025/10/new-detailed-brain-growth-atlas-in-mice-offers-insights-into-brain-development/]
- 47. Three-dimensional cranial suture morphometric changes in ... [https://www.sciencedirect.com/science/article/pii/S8756328224003259]
- 48. Techniques in Stereotaxic Surgery [https://conductscience.com/techniques-in-stereotaxic-surgery/?srsltid=AfmBOooX8GzvyhEnvcupoEUJ-OwTM9DTU2FEOcvqlf3E9uisafWAJxo_]
- 49. Novel 3D Scanning and Multi-Angle Analysis Uncover the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561190/]
- 50. Improving Stereotaxic Neurosurgery Techniques and ... [https://www.mdpi.com/2076-2615/11/9/2662]
- 51. Increased incidence of weight-loss-associated humane ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2024.1467419/full]
- 52. Inhibition of craniosynostosis and premature suture fusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372882/]
- 53. Ratlas-LH: An MRI template of the Lister hooded rat brain with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8370892/]
- 54. Techniques in Stereotaxic Surgery [https://conductscience.com/techniques-in-stereotaxic-surgery/?srsltid=AfmBOoodwkCmB0tZvDCm9-jgeOpCwYXsfca6jVv6g7wFCTI4ktVb0O6R]
- 55. Improving Stereotaxic Neurosurgery Techniques and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8465152/]
- 56. Optimized surgical techniques and postoperative care ... [https://bmcvetres.biomedcentral.com/articles/10.1186/1746-6148-5-28]
- 57. Three steps to reduction surgical site infection [https://pmc.ncbi.nlm.nih.gov/articles/PMC10486815/]
- 58. Rodent Survival Surgery Guideline - Knowledge Base [https://ohiostateresearch.knowledgebase.co/article/rodent-survival-surgery-guideline-66.html]
- 59. Survival Surgery in Mice, Rats, and Birds [https://rsawa.research.ucla.edu/arc/mice-rats-birds-surgery/]
- 60. Surgery: Rodent | Office of Research [https://www.bu.edu/research/ethics-compliance/animal-subjects/animal-care/procedures/surgery-rodent/]
- 61. Standard on Rodent Survival Surgery - UNC Policies [https://policies.unc.edu/TDClient/2833/Portal/KB/ArticleDet?ID=132210]
- 62. Safety of early postoperative showering in level-1 and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465920/]
- 63. Inter-rater agreement of CDC criteria and ASEPSIS score ... [https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2023.1123193/full]
- 64. Biological constraints on stereotaxic targeting of functionally ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10016058/]
- 65. In vivo localization of chronically implanted electrodes and ... [https://www.nature.com/articles/s41467-020-18472-y]
- 66. Interactive phenotyping of large-scale histology imaging ... [https://www.nature.com/articles/s41598-017-15092-3]
- 67. Protocol to study adenosine release in the adult mouse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332273/]
- 68. Cholecystokinin modulates age-dependent thalamocortical ... [https://elifesciences.org/articles/101513]
- 69. Principles for valid histopathologic scoring in research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3795863/]
- 70. Techniques in Stereotaxic Surgery [https://conductscience.com/techniques-in-stereotaxic-surgery/?srsltid=AfmBOorP-QIcl4UyGTrarjXAbQ-3ffr4AAAlQnQuPPfnhi57PC8MIaxh]
- 71. Discrepancies in stereotaxic coordinate publications and ... [https://pubmed.ncbi.nlm.nih.gov/28392415/]
- 72. Accuracy and precision [https://web.chem.ox.ac.uk/teaching/Physics%20for%20CHemists/Errors/Precision.html]
- 73. Random vs. Systematic Error [https://www.physics.umd.edu/courses/Phys276/Hill/Information/Notes/ErrorAnalysis.html]
- 74. The variability of the interaural line vs the stability of ... [https://www.sciencedirect.com/science/article/abs/pii/0031938477903043]
- 75. The Rat Brain in Stereotaxic Coordinates - Google Livros [https://books.google.com.br/books/about/The_Rat_Brain_in_Stereotaxic_Coordinates.html?id=RiHLCQAAQBAJ]
- 76. Techniques in Stereotaxic Surgery [https://conductscience.com/techniques-in-stereotaxic-surgery/?srsltid=AfmBOopMn0cr1YQ4sMHKCCVrar7CwzNUUz53skWdUd4dz0BAXBa25Q1y]
- 77. Waxholm Space atlas of the rat brain: a 3D atlas supporting ... [https://www.nature.com/articles/s41592-023-02034-3]
- 78. Rat Brain Atlas - Tools [https://www.ebrains.eu/tools/rat-brain]
- 79. An image-based reference for coordinating mouse brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2930145/]
- 80. Waxholm Space Atlas of the Sprague Dawley Rat Brain [https://www.nitrc.org/projects/whs-sd-atlas]
- 81. 3D Reconstructed Cyto-, Muscarinic M 2 Receptor, and ... [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2016.00051/full]
- 82. Advancing Mouse Research with Precision Stereotaxic Tools [https://bplabline.com/blogs/industrial-news/advancing-mouse-research-with-precision-stereotaxic-tools]
- 83. An MRI-Derived Neuroanatomical Atlas of the Fischer 344 ... [https://www.nature.com/articles/s41598-020-63965-x]
- 84. Development and advancements in rodent MRI-based ... [https://www.sciencedirect.com/science/article/pii/S2405844024034522]
- 85. Deep Learning and Atlas-Based MRI Segmentation Enable ... [https://www.mdpi.com/2313-433X/11/11/418]