Beyond the Symptom Checklist: Neurobiological Validation of Next-Generation Addiction Assessment Instruments
This article synthesizes current advancements in the neurobiological validation of addiction assessment tools, charting a paradigm shift from purely behavioral checklists to mechanistically informed instruments.
Beyond the Symptom Checklist: Neurobiological Validation of Next-Generation Addiction Assessment Instruments
Abstract
This article synthesizes current advancements in the neurobiological validation of addiction assessment tools, charting a paradigm shift from purely behavioral checklists to mechanistically informed instruments. We explore the foundational neuroscience of addiction, highlighting frameworks like the Addictions Neuroclinical Assessment (ANA) that link core neurofunctional domains—executive function, incentive salience, and negative emotionality—to specific stages of the addiction cycle. The review details innovative methodological approaches, including gamified digital neurocognitive batteries, AI-driven predictive analytics, and integrated genetic-behavioral tools. We address key challenges in implementation and optimization, such as clinical heterogeneity and tool feasibility. Finally, we present a comparative analysis of validation evidence, underscoring how these neurobiologically-grounded instruments enhance predictive validity, enable personalized risk detection, and inform the development of targeted therapeutics for researchers and drug development professionals.
The Brain on Addiction: Foundational Neurocircuitry and the Case for a New Assessment Paradigm
Addiction is now understood as a chronic brain disorder, characterized by clinically significant impairments in health, social function, and voluntary control over substance use [1]. This represents a fundamental shift from historical views of addiction as a moral failing or character flaw. Research accumulated over several decades has revealed that addictive substances produce profound changes in brain structure and function that promote and sustain the condition [1]. The neurobiological understanding of addiction has opened new avenues for prevention and treatment, with a particular focus on three key brain regions: the basal ganglia, extended amygdala, and prefrontal cortex [1] [2].
This review adopts a comparative approach to examine the neurocircuitry of addiction through the lens of the Addictions Neuroclinical Assessment (ANA), a neuroscience-based framework designed to address the substantial heterogeneity observed among individuals diagnosed with the same substance use disorder [3] [4]. By deconstructing the addiction cycle into its constituent neurofunctional domains and their underlying neural substrates, we provide researchers and drug development professionals with a structured analysis of assessment methodologies, their experimental validation, and the standardized research tools available for investigating this complex disorder.
The Three-Stage Addiction Cycle: Core Neurocircuitry and Functions
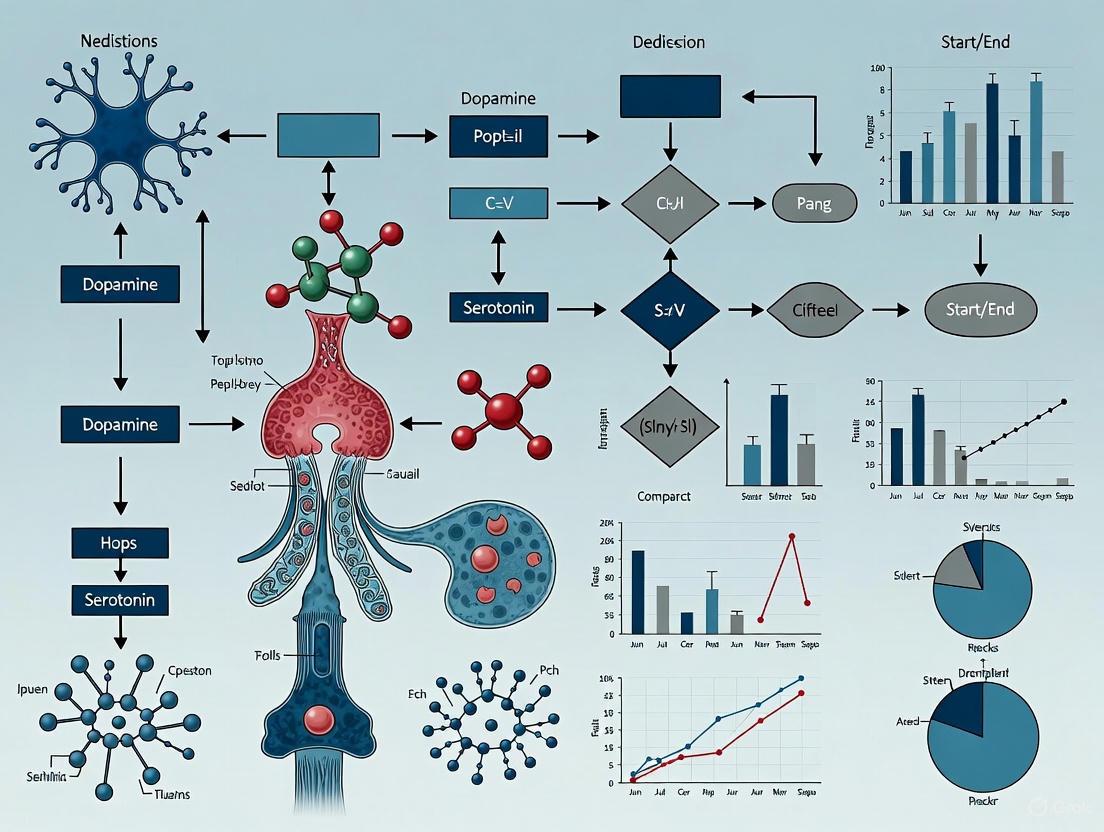
The addiction process is characterized by a three-stage cycle: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. This cycle becomes more severe with continued substance use, producing dramatic changes in brain function that reduce an individual's ability to control their substance use [1]. Each stage is mediated by specific brain regions and circuits, which are detailed below and visualized in Figure 1.
Binge/Intoxication Stage: Basal Ganglia
The binge/intoxication stage is primarily centered on the basal ganglia and its role in reward processing [1] [5]. Key structures within the basal ganglia, particularly the nucleus accumbens, are responsible for the acute rewarding or pleasurable effects of substance use [1] [2]. When drugs are taken, they can produce surges of neurotransmitters such as dopamine and the brain's natural opioids (endorphins) in the reward circuit, which are significantly greater than those produced by natural, healthy rewards [2]. These neurochemical surges powerfully reinforce the connection between drug consumption, pleasure, and associated environmental cues, teaching the brain to seek drugs at the expense of other goals [2].
Withdrawal/Negative Affect Stage: Extended Amygdala
The withdrawal/negative affect stage is dominated by the extended amygdala [1] [5]. This region plays a key role in stress responses and is responsible for the feelings of unease, anxiety, irritability, and physical discomfort that characterize withdrawal after the drug high subsides [5] [2]. With repeated drug use, this circuit becomes increasingly sensitive. Over time, the individual may use substances primarily to gain temporary relief from this aversive state rather than to achieve pleasure [2]. This represents a critical shift in the motivation for drug use.
Preoccupation/Anticipation Stage: Prefrontal Cortex
The preoccupation/anticipation stage, which drives relapse, is heavily influenced by the prefrontal cortex (PFC) [1] [5]. The PFC is essential for executive function, including the ability to organize thoughts and activities, prioritize tasks, manage time, make decisions, and exert self-control over impulses [1] [2]. In addiction, the function of the PFC is disrupted. This leads to reduced impulse control and a diminished ability to make rational decisions about drug-seeking, even after periods of abstinence [2]. The shifting balance between the PFC (executive control) and the circuits of the basal ganglia and extended amygdala (reward and stress) underlies the compulsive drug seeking that marks addiction [5].
Figure 1. The Three-Stage Cycle of Addiction and Associated Brain Regions. This diagram illustrates the recurrent cycle of addiction, highlighting the primary brain regions and key neurobiological processes involved in each stage. The cycle is driven by progressive neuroadaptations in the basal ganglia, extended amygdala, and prefrontal cortex [1] [5].
Comparative Analysis of Assessment Frameworks and Instruments
A significant challenge in addiction research is the clinical heterogeneity among patients, which has prompted the development of neuroscience-based assessment frameworks that move beyond traditional symptom-based diagnoses [3] [4]. This section compares the dominant framework, the Addictions Neuroclinical Assessment (ANA), with the broader Research Domain Criteria (RDoC) initiative.
The Addictions Neuroclinical Assessment (ANA) Framework
The ANA is a heuristic framework that incorporates three key neurofunctional domains derived from the neurocircuitry of addiction [3]. It was proposed specifically to address the limitations of existing diagnostic systems and to differentiate patients based on etiology, prognosis, and treatment response [3]. The three core domains are:
- Incentive Salience (IS): This domain encompasses processes involved in reward, motivational salience, and habit formation, tied to the binge/intoxication stage of the addiction cycle [3] [4]. It is primarily associated with the basal ganglia.
- Negative Emotionality (NE): This domain captures negative affective states resulting from withdrawal and long-term drug use, corresponding to the withdrawal/negative affect stage [3] [4]. It is linked to the extended amygdala.
- Executive Function (EF): This domain comprises cognitive functions such as inhibitory control, decision-making, and planning, which are relevant to the preoccupation/anticipation stage and relapse [3] [4]. It is primarily governed by the prefrontal cortex.
A recent validation study (N=300) using a standardized ANA battery identified subfactors within these domains, revealing a more complex structure [4]. The findings, including the psychometric properties of the assessments, are summarized in Table 1.
Table 1: ANA Domain Factors and Assessment Metrics from a Standardized Battery Study (N=300) [4]
| ANA Domain | Identified Subfactors | Key Assessment Instruments/Tasks | Critical Findings |
|---|---|---|---|
| Incentive Salience | 1. Alcohol Motivation2. Alcohol Insensitivity | Alcohol Cue-Reactivity Task, Monetary Choice Questionnaire, Self-Report | Alcohol Motivation and Insensitivity showed the strongest ability to classify individuals with problematic drinking and AUD. |
| Negative Emotionality | 1. Internalizing2. Externalizing3. Psychological Strength | State-Trait Anxiety Inventory, Positive and Negative Affect Schedule, Self-Report | Internalizing (e.g., anxiety) was strongly correlated with factors from other domains, like Alcohol Motivation. |
| Executive Function | 1. Inhibitory Control2. Working Memory3. Rumination4. Interoception5. Impulsivity | Stop-Signal Task, Digit Span Task, Delay Discounting Task, Self-Report | Impulsivity was a key factor in classifying AUD status and was strongly correlated with Alcohol Motivation. |
Comparative Framework: Research Domain Criteria (RDoC)
The RDoC is a broader framework initiated by the National Institute of Mental Health (NIMH) to create a research structure for studying all psychiatric diseases based on dimensions of observable behavior and neurobiological measures [3]. While not specific to addiction, the ANA domains align closely with the following RDoC constructs:
- Positive Valence Systems (similar to Incentive Salience)
- Negative Valence Systems (similar to Negative Emotionality)
- Cognitive Systems (similar to Executive Function) [3] [4]
The primary distinction is that ANA is a more focused framework specifically tailored to the neurobiology of addictive disorders and designed for clinical assessment, whereas RDoC provides a larger, transdiagnostic research matrix [3].
Experimental Protocols and Methodologies in Preclinical Research
To support the translation of neurobiological findings into treatments, standardized preclinical testing protocols are essential. The National Institute on Drug Abuse's (NIDA) Addiction Treatment Discovery Program (ATDP) provides a comprehensive suite of validated experimental protocols for evaluating potential pharmacotherapies [6]. These protocols are critical for generating reproducible and comparable data across different research programs. The methodologies are tailored to specific substance classes and target different aspects of the addiction cycle, as outlined in Table 2.
Table 2: NIDA ATDP Preclinical Testing Protocols for Substance Use Disorders [6]
| Target Substance | Key Behavioral Assays | Primary Measured Construct | Linked ANA Domain |
|---|---|---|---|
| Opioids | Oxycodone withdrawal (spontaneous/precipitated); Oxycodone cue-induced reinstatement of seeking | Physical dependence & negative affect; Relapse vulnerability | Negative Emotionality; Incentive Salience |
| Cocaine / Methamphetamine | Drug discrimination; Cue/Prime/Stress-induced reinstatement of cocaine seeking; Intracranial self-stimulation | Interoceptive drug effects; Relapse vulnerability; Reward function | Incentive Salience; Negative Emotionality |
| Nicotine | Withdrawal (spontaneous/precipitated); Cue-induced reinstatement of nicotine seeking | Physical dependence & negative affect; Relapse vulnerability | Negative Emotionality; Incentive Salience |
| Predictive Safety | Cytochrome P450 interactions; Ames test for mutagenicity; Comprehensive in vitro proarrhythmia assay (CiPA) | Drug metabolism & interactions; Genotoxicity; Cardiovascular risk | (General Safety Pharmacology) |
The experimental workflow for validating a novel compound typically follows a staged approach:
- In Vitro Screening: Initial assessment of compound binding and function at target receptors (e.g., opioid or dopamine receptors) [6].
- Lead Characterization: Selected compounds undergo behavioral testing in established models relevant to SUDs, such as:
- Self-Administration: Measures drug-taking behavior.
- Reinstatement: Models relapse by using cues, stress, or a small prime dose of the drug to re-initiate drug-seeking behavior after a period of extinction.
- Intracranial Self-Stimulation (ICSS): Assesses brain reward function; drugs of abuse typically lower the threshold for ICSS, while withdrawal raises it [6].
- Safety Pharmacology: Promising candidates are evaluated for potential toxicity, including mutagenicity and cardiac risk, using standardized in vitro and in silico assays [6].
Figure 2. Preclinical Compound Evaluation Workflow. This diagram outlines the multi-stage experimental protocol used by programs like NIDA's Addiction Treatment Discovery Program (ATDP) to evaluate the efficacy and safety of novel compounds for substance use disorders [6].
For researchers investigating the addiction cycle, a standardized set of tools and resources is critical for ensuring reproducibility and facilitating direct comparison of findings across studies. Table 3 details essential research solutions and platforms relevant to both preclinical and clinical research in this field.
Table 3: Essential Research Reagents and Resources for Addiction Neurobiology
| Resource Category | Specific Tool / Platform | Primary Function / Application |
|---|---|---|
| Preclinical Behavioral Assays | NIDA's Addiction Treatment Discovery Program (ATDP) [6] | Provides standardized, blinded preclinical testing of compounds for effects on drug taking, reinstatement, and withdrawal across multiple substance classes. |
| Human Brain Imaging | Ultra-High-Field MRI (e.g., 11.7T Iseult system) [7] | Enables unprecedented resolution for in vivo examination of human brain structure and function, allowing finer analysis of circuits like the basal ganglia and prefrontal cortex. |
| Digital Brain Models | Virtual Epileptic Patient; Digital Twins [7] | Personalized brain models and continuously updated digital twins can be adapted to simulate the effects of drugs or treatments on specific neural circuits involved in addiction. |
| Standardized Assessment Battery | ANA Battery (Computerized Tasks & Self-Report) [4] | A curated set of validated behavioral tasks and questionnaires designed to operationalize and measure the three core ANA domains (IS, NE, EF) in human subjects. |
| Data & Analysis Repositories | NIH BRAIN Initiative Data Archives [8] | Public, integrated repositories for large-scale neuroimaging and neurophysiological datasets, promoting data sharing and collaborative analysis. |
The deconstruction of the addiction cycle into its constituent neural circuits—from the reward-driven basal ganglia to the stress-responsive extended amygdala and the control-deficient prefrontal cortex—provides a robust neurobiological framework for understanding this disorder. The Addictions Neuroclinical Assessment (ANA) successfully translates this framework into a measurable, clinically relevant tool that addresses the critical problem of heterogeneity among affected individuals [3] [4]. The validation of its three core domains through standardized batteries confirms the utility of this approach and reveals additional dimensionality within each domain, such as the separation of "alcohol motivation" from "alcohol insensitivity" within the Incentive Salience domain [4].
Future research and drug development will be shaped by several key trends. The integration of genomic data and artificial intelligence, such as the use of polygenic risk scores, is poised to enhance the personalization of addiction medicine [9]. Furthermore, initiatives like the BRAIN Initiative 2025 are driving the development of innovative technologies to map and modulate neural circuits with ever-greater precision, which will undoubtedly refine our models of the addicted brain [8]. Finally, the emergence of digital therapeutics and device-based treatments (e.g., transcranial magnetic stimulation) offers new avenues for directly targeting the dysregulated circuits identified in the addiction cycle, providing hope for more effective and personalized interventions [6]. For researchers and drug development professionals, leveraging standardized frameworks like the ANA and validated preclinical protocols like those in the ATDP will be essential for translating these advancing technologies into tangible improvements in patient care.
Introducing the Addictions Neuroclinical Assessment (ANA) Framework
Theoretical Foundation and Neurobiological Basis
The Addictions Neuroclinical Assessment (ANA) is a neuroscience-informed framework designed to address the profound clinical and etiological heterogeneity observed among individuals diagnosed with addictive disorders (AD) [3]. Developed to translate advancements in neurobiology into clinical practice, the ANA proposes that addiction is driven by dysregulation in three core neurofunctional domains, each tied to a specific phase in the cycle of addiction [10] [4]. This model moves beyond traditional, purely symptom-based diagnostic systems like the DSM-5 by focusing on the underlying psychological processes and neurocircuitry that manifest as addictive behavior [3].
The framework is conceptually aligned with the Research Domain Criteria (RDoC) initiative and is directly built upon a well-validated three-stage neurobiological model of addiction: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation [3] [10]. The ANA maps specific neuroclinical domains onto these stages to characterize an individual's addiction phenotype more precisely [4].
Table: Core Neurofunctional Domains of the ANA Framework
| ANA Domain | Associated Addiction Stage | Primary Brain Circuitry | Core Neuropsychological Process |
|---|---|---|---|
| Incentive Salience | Binge/Intoxication | Basal Ganglia; Mesolimbic Pathway | Attribution of motivational value to substance-related cues; habit formation [10] [4] |
| Negative Emotionality | Withdrawal/Negative Affect | Extended Amygdala ("Anti-reward" System) | Stress, irritability, anxiety, and dysphoria during withdrawal; driven by negative reinforcement [10] [4] |
| Executive Function | Preoccupation/Anticipation | Prefrontal Cortex | Deficits in inhibitory control, decision-making, emotional regulation, and planning [10] [4] |
Experimental Validation and Domain Factorization
A pivotal 2024 cross-sectional study (N=300) systematically evaluated the ANA battery's construct validity, moving beyond prior validation efforts that relied on secondary data analysis [4]. This study employed a standardized collection of behavioral tasks and self-report measures to assess the three domains, followed by factor analyses to elucidate their underlying dimensionality.
The findings revealed that each broad ANA domain is composed of distinct, measurable subfactors, providing a more nuanced understanding of the addiction phenotype [4]. The study identified ten subfactors across the three domains, with specific subfactors showing superior utility in classifying individuals with problematic drinking and AUD.
Table: Factor Structure and Classification Utility of ANA Domains
| ANA Domain | Identified Subfactors | Key Assessment Examples | Strongest Classifiers for AUD |
|---|---|---|---|
| Incentive Salience | Alcohol Motivation; Alcohol Insensitivity | Alcohol Cue Reactivity Tasks | Alcohol Motivation; Alcohol Insensitivity [4] |
| Negative Emotionality | Internalizing; Externalizing; Psychological Strength | Negative Emotion Scales; Distress Tolerance Tasks | Internalizing [4] |
| Executive Function | Inhibitory Control; Working Memory; Rumination; Interoception; Impulsivity | Go/No-Go Task; N-Back Task; Self-Control Scales | Impulsivity [4] |
The experimental protocol was rigorous [4]. Participants across the drinking spectrum completed the ANA battery administered via computer in four randomized testing blocks. The battery integrated performance-based neurocognitive tasks with self-report questionnaires. All participants provided informed consent and had a negative breath alcohol concentration at testing; inpatient participants were tested post-detoxification. Statistical analyses included exploratory and confirmatory factor analysis on split-half samples to identify latent factors, and receiver operating characteristics (ROC) analyses to determine the classification power of each factor for AUD.
ANA Framework: From Addiction Cycle to Measurable Factors
Comparative Analysis with Alternative Assessment Approaches
The ANA framework differs fundamentally from other common assessment strategies in its theoretical grounding, structure, and objectives.
Table: Comparison of the ANA Framework with Other Assessment Approaches
| Assessment Approach | Theoretical Basis | Primary Measurement Focus | Advantages | Limitations |
|---|---|---|---|---|
| ANA Framework | Neurocircuitry-derived functional domains | Neuropsychological processes and behaviors linked to addiction stages | Captures etiological heterogeneity; potential for personalized treatment targeting; strong neurobiological validity [3] [4] | Longer assessment time; requires further validation for clinical deployment [4] |
| Diagnostic Criteria (e.g., DSM-5) | Clinical symptomatology and life impact | Presence or absence of pre-defined behavioral symptoms | High inter-rater reliability; diagnostic standardization; widely adopted [3] | Outcome-based rather than process-based; masks underlying heterogeneity [3] |
| Traditional Severity Scales (e.g., ASI) | Multidimensional psychosocial problems | Severity of consequences across life domains (e.g., employment, legal, family) | Comprehensive view of psychosocial functioning; tracks broad treatment outcomes [11] | Limited insight into specific neurocognitive mechanisms driving addiction [3] |
| Emerging Digital Tools (e.g., Cumulus Battery) | Classic neurobehavioral paradigms | High-frequency, repeatable cognitive performance metrics (e.g., reaction time, working memory) | Sensitive to subtle change; suitable for remote/decentralized trials; reduces participant burden [12] | May not fully cover motivational/affective ANA domains; often validated for specific impairments (e.g., alcohol challenge) [12] |
| Integrated ML Screening (e.g., CRAFFT 2.1 + Genetics) | Polygenic risk and behavioral screening | Aggregate risk score derived from genetic markers and self-reported behavior | Aims for early detection and prediction; potential for high-throughput screening [13] | Does not provide deep neuroclinical phenotyping for mechanistic intervention [13] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing the ANA framework in a research context requires a multi-modal toolkit designed to capture data across its core domains.
Table: Essential Research Materials for ANA Implementation
| Tool Category | Specific Instrument / Technology | Primary Function in ANA Research |
|---|---|---|
| Behavioral Task Software | Inquisit 5 (Millisecond Software LLC) | Administration and precise timing of standardized neurocognitive tasks (e.g., Go/No-Go, N-Back) [4] |
| Self-Report Metrics | Standardized Questionnaires (e.g., OCDS, ADS items) | Assess subjective experiences of craving, withdrawal, and emotional states that complement performance data [4] |
| Clinical Interview Schedule | Structured Clinical Interview for DSM-5 (SCID-5) | Determines formal AUD/SUD diagnosis and comorbid conditions for participant characterization [4] |
| Alcohol Use Assessment | Timeline Followback (TLFB); Alcohol Use Disorders Identification Test (AUDIT) | Quantifies past alcohol consumption patterns and screens for problematic use [4] |
| Digital Cognitive Platform | Cumulus Neuroscience Cognitive Assessment Platform | Enables high-frequency, remote assessment of cognitive domains relevant to Executive Function (e.g., DSST, N-Back) [12] |
| Biochemical Verification | Breathalyzer (e.g., Alco-Sensor) | Verifies a negative breath alcohol concentration (BAC) at the time of testing to ensure data integrity [4] |
ANA Validation Study Workflow
The ANA framework represents a significant paradigm shift in addiction assessment, moving from a syndromal classification to a neurofunctionally-grounded phenotyping approach. Its core strength lies in its ability to deconstruct the heterogeneity of addictive disorders into measurable, mechanistically relevant domains with established neural substrates [3] [4].
For researchers and drug development professionals, this framework offers a powerful tool for stratifying patient populations in clinical trials, potentially leading to more targeted and effective interventions. The identification of specific subfactors, such as alcohol motivation and impulsivity, provides a roadmap for developing therapies that target precise neurocognitive processes rather than the broad diagnosis of AUD [4]. As the field advances, integrating the ANA with emerging digital assessment platforms and genetic risk data holds the promise of creating a comprehensive, multi-level understanding of addiction, ultimately paving the way for truly personalized medicine in the treatment of substance use disorders.
Addiction is increasingly understood through a neurobiological framework that identifies three core neurofunctional domains which underlie the disorder's development and persistence. These domains—executive dysfunction, incentive salience, and negative emotionality—map onto specific neural circuits and represent distinct yet interacting mechanisms that drive the addiction cycle [10] [14]. Historically, addiction was misconceived as a moral failing, but contemporary neuroscience has revealed it to be a chronic brain disorder characterized by specific neuroadaptations that transcend mere substance use [10]. The identification and validation of these three domains have emerged from decades of animal and human research, providing a more nuanced understanding of why individuals persist in substance use despite negative consequences and why relapse rates remain persistently high [14] [15].
The neurobiological model of addiction describes a repeating cycle with three distinct stages: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation [10]. Each stage engages specific brain regions and corresponds to the core neurofunctional domains. The binge/intoxication stage primarily involves incentive salience processes centered in the basal ganglia, the withdrawal/negative affect stage engages negative emotionality systems in the extended amygdala, and the preoccupation/anticipation stage is governed by executive function circuits in the prefrontal cortex [10]. Understanding these domains and their interactions provides a framework for developing targeted assessment instruments and personalized treatment approaches for substance use disorders (SUDs) [14].
Domain Comparison: Neurocircuitry, Behavioral Manifestations, and Assessment
Table 1: Comparative Analysis of Core Neurofunctional Domains in Addiction
| Domain | Primary Neural Substrates | Key Neurotransmitters/Systems | Behavioral Manifestations | Associated Addiction Stage |
|---|---|---|---|---|
| Executive Dysfunction | Prefrontal cortex (PFC), dorsolateral PFC, anterior cingulate cortex [10] | Dopamine, glutamate imbalance [10] | Reduced impulse control, poor decision-making, inability to regulate drug-seeking behavior, diminished cognitive flexibility [10] [16] | Preoccupation/Anticipation [10] |
| Incentive Salience | Basal ganglia, nucleus accumbens (NAc), ventral striatum [10] [17] | Dopamine (mesolimbic pathway), opioid peptides [10] [17] | Cue-triggered "wanting," compulsive drug-seeking, motivation for drug rewards over natural rewards, habits [10] [17] | Binge/Intoxication [10] |
| Negative Emotionality | Extended amygdala (BNST, CeA), bed nucleus of stria terminalis, central nucleus of amygdala [10] [18] | CRF, dynorphin, norepinephrine, decreased dopamine in NAc [10] [18] [15] | Hyperkatifeia (heightened negative emotional state), irritability, anxiety, dysphoria, emotional pain [10] [18] [15] | Withdrawal/Negative Affect [10] |
Table 2: Quantitative Assessment of Domain Impairment in Substance Use Disorders
| Assessment Measure | Domain Measured | Key Findings in SUD Populations | Effect Size (Hedges' g or Comparable) | Reliability/Validity Metrics |
|---|---|---|---|---|
| Difficulties in Emotion Regulation Scale (DERS) | Negative Emotionality [19] | SUDs showed significantly greater emotion regulation difficulties vs. controls | g = 1.05 (95% CI: 0.86-1.24) [19] | Excellent internal consistency (α = 0.77-0.96) [19] |
| DERS Subscales Analysis | Negative Emotionality | Largest deficits in Strategies and Impulse subscales [19] | Mean difference: 21.44 (95% CI: 16.49-26.40) [19] | Good test-retest reliability (ρI = 0.88) [19] |
| Emotion Regulation Questionnaire (ERQ) | Negative Emotionality/Executive Function [19] | Greater use of expressive suppression in SUDs vs. controls | g = 0.76 (95% CI: 0.25-1.28) [19] | Established construct validity [19] |
| Latent Profile Analysis (NKI-RS Sample) | All Three Domains [14] | Identified three subtypes: Reward (27%), Cognitive (40%), Relief (20%) in past SUDs | Cohen's D range: 0.4-2.8 across domains [14] | Comprehensive phenotypic assessment (74 subscales) [14] |
Neurobiological Validation of Assessment Instruments
The Addictions Neuroclinical Assessment (ANA) Framework
The Addictions Neuroclinical Assessment (ANA) represents a significant advancement in translating the three-stage neurobiological model of addiction into clinical practice. Developed by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), this clinical instrument translates the three neurobiological stages of addiction into three measurable neurofunctional domains: incentive salience, negative emotionality, and executive dysfunction [10]. The ANA provides a structured approach to assess these domains at the bedside, allowing clinicians to move beyond generic diagnostic criteria and instead employ targeted treatments for specific clinical presentations [10]. This neurobiologically-informed framework represents a paradigm shift in addiction assessment, directly addressing the heterogeneous nature of SUDs by recognizing that different individuals may exhibit distinct patterns of impairment across these domains.
Validation of the ANA framework comes from empirical studies demonstrating that these domains represent meaningful subgroups within SUD populations. Research utilizing latent profile analysis in community samples has identified three distinct neurobehavioral subtypes corresponding to these domains: a "Reward type" with heightened incentive salience, a "Cognitive type" with executive dysfunction, and a "Relief type" with prominent negative emotionality [14]. These subtypes were equally distributed across different primary substance use disorders and genders, supporting the transdiagnostic nature of these domains and their relevance across the spectrum of addictive disorders [14].
Standardized Assessment Instruments and Methodologies
Several well-validated assessment instruments provide the methodological foundation for evaluating the core neurofunctional domains in research and clinical settings. These instruments vary in their structure, focus, and application, allowing researchers to select the most appropriate tools based on their specific objectives.
Table 3: Key Assessment Instruments for Addiction Research
| Instrument | Format | Primary Application | Domains Assessed | Administration Time | Training Requirements |
|---|---|---|---|---|---|
| Addiction Severity Index (ASI) | Semi-structured [20] | Treatment planning, service needs assessment [20] | Functioning in 7 domains (alcohol, drugs, psychiatric, etc.) [20] | 45-60 min + scoring [20] | 2-day classroom session [20] |
| Structured Clinical Interview for DSM-IV (SCID) | Semi-structured [20] | Diagnostic consistency for research [20] | Alcohol/drug dependence and abuse, psychiatric comorbidities [20] | 90 minutes [20] | User's guide, 1-2 days on-site training [20] |
| Composite International Diagnostic Interview (CIDI) | Fully structured [20] | Large-scale studies, epidemiological research [20] | DSM-IV and ICD-10 substance use and mental disorders [20] | 75 minutes [20] | 2.5-3 days classroom training [20] |
| Difficulties in Emotion Regulation Scale (DERS) | Self-report [19] | Emotion regulation capacity assessment [19] | Negative Emotionality (Strategies, Impulse subscales most sensitive) [19] | Not specified | Minimal (self-report) [19] |
The selection of appropriate assessment instruments is critical for both research and clinical applications. In research, proper instrumentation can determine the success or failure of clinical trials, as demonstrated by studies of tricyclic antidepressants for substance abusers with comorbid depression. Early trials that used limited assessment tools showed minimal benefit, while later studies employing more rigorous diagnostic instruments consistently demonstrated efficacy [20]. This highlights how assessment methodology directly impacts the validity and interpretation of research findings.
Experimental Protocols and Neural Circuit Mapping
Neuroimaging Protocols for Domain Assessment
Functional magnetic resonance imaging (fMRI) has become a cornerstone technology for investigating the neural substrates of the three core neurofunctional domains in addiction. Task-based fMRI protocols typically involve presenting emotionally salient stimuli while measuring blood-oxygen-level-dependent (BOLD) responses in specific brain regions [15]. These tasks can be passive (e.g., viewing emotional faces or aversive images) or active (e.g., requiring conscious emotion regulation strategies like reappraisal) [15]. The experimental workflow generally involves: (1) participant screening and diagnosis using structured clinical interviews; (2) abstinence verification (when relevant); (3) fMRI task administration; (4) preprocessing of neuroimaging data; and (5) statistical analysis of brain activation patterns.
For the negative emotionality domain, common paradigms include facial emotion processing tasks (e.g., identifying emotions in faces) and aversive stimulus viewing (e.g., unpleasant images) [15]. These tasks consistently engage the extended amygdala, anterior insula, anterior cingulate cortex (ACC), and medial prefrontal cortex (mPFC) [15]. Research has revealed substance-specific patterns of dysregulation, with alcohol dependence typically showing blunted activation in these regions, while cocaine dependence often demonstrates heightened reactivity [15]. These differential patterns highlight the importance of considering substance type when interpreting neuroimaging findings.
Behavioral Paradigms for Domain-Specific Assessment
Behavioral tasks provide crucial complementary data to neuroimaging for assessing the core neurofunctional domains. For executive dysfunction, common paradigms include the Go/No-Go task (measuring response inhibition), Stroop task (assessing cognitive interference), and Iowa Gambling Task (evaluating decision-making) [16]. These tasks probe the "Stop system" within the prefrontal cortex that is responsible for overriding strong urges to use substances [10].
For incentive salience, behavioral protocols often involve Pavlovian conditioning procedures where previously neutral stimuli are paired with drug rewards [16]. These paradigms measure the attribution of incentive salience to drug-paired cues, a process dependent on dopaminergic transmission in the mesolimbic pathway [17] [16]. Sign-tracking behavior (approaching and interacting with reward-predictive cues) provides a validated behavioral measure of excessive incentive salience in animal models, with parallels in human studies [17].
The negative emotionality domain is frequently assessed using stress reactivity paradigms, affective picture viewing tasks, and measures of distress tolerance [15] [19]. These protocols capture the hyperkatifeia (heightened negative emotional state) that emerges during withdrawal and drives negative reinforcement [18] [15]. The experimental workflow typically involves baseline assessment, stressor induction (e.g., social stress, individualized stress scripts), and measurement of subjective, physiological, and neural responses.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Research Reagent Solutions for Addiction Neuroscience
| Reagent/Material | Primary Application | Specific Function in Research | Domain Relevance |
|---|---|---|---|
| Structured Clinical Interview for DSM-IV (SCID) | Diagnostic assessment [20] | Ensures diagnostic consistency and participant characterization | All domains (patient stratification) |
| fMRI with BOLD contrast | Neurocircuitry mapping [15] | Measures neural activity during domain-specific tasks | All domains (neural substrates) |
| Difficulties in Emotion Regulation Scale (DERS) | Emotion regulation assessment [19] | Quantifies multiple aspects of emotional dysregulation | Negative Emotionality |
| Emotion Regulation Questionnaire (ERQ) | Emotion regulation strategies [19] | Measures cognitive reappraisal and expressive suppression | Negative Emotionality/Executive Function |
| Pavlovian Conditioning Apparatus | Incentive salience measurement [17] [16] | Assesses cue-reward learning and sign-tracking behavior | Incentive Salience |
| Corticotropin-Releasing Factor (CRF) Receptor Antagonists | Stress system manipulation [18] | Probes extended amygdala stress circuitry | Negative Emotionality |
| Dopamine Receptor Ligands | Dopamine system assessment [17] | Measures dopamine transmission and receptor availability | Incentive Salience |
| Go/No-Go and Stroop Tasks | Executive function assessment [16] | Measures response inhibition and cognitive control | Executive Dysfunction |
Implications for Targeted Treatment Development
The validation of three distinct neurofunctional domains in addiction has profound implications for developing targeted treatment strategies. Rather than applying one-size-fits-all approaches, this framework supports personalized interventions based on an individual's specific domain profile [14]. For those with prominent incentive salience dysregulation ("Reward type"), treatments might focus on managing cue reactivity and altering maladaptive reward learning processes [17] [14]. For individuals with executive dysfunction as their primary deficit ("Cognitive type"), cognitive remediation, working memory training, and interventions that strengthen prefrontal control systems may be most beneficial [14]. For those whose addiction is maintained primarily by negative emotionality ("Relief type"), treatments targeting the extended amygdala stress systems (e.g., CRF antagonists, neuropeptide Y enhancers) and emotion regulation skills training would be indicated [18] [14] [15].
This domain-based approach also informs medication development. Rather than seeking a single medication for all forms of addiction, pharmaceutical research can target specific neurochemical systems underlying each domain. For negative emotionality, compounds that modulate the brain's stress systems—including CRF receptor antagonists, neuropeptide Y enhancers, nociceptin agonists, and endocannabinoid system modulators—show particular promise [18]. For incentive salience, medications that normalize dopaminergic transmission without producing anhedonia represent a viable strategy [17]. For executive dysfunction, procognitive agents that enhance prefrontal function could improve self-regulation and treatment adherence [10] [14].
The recognition of these neurofunctional domains also supports the development of biomarker-driven clinical trials. By stratifying participants based on their domain profiles, researchers can achieve more homogeneous study populations and better detect treatment effects that might be obscured in heterogeneous samples [14]. This approach aligns with precision medicine initiatives and represents a promising path forward for addressing the high relapse rates that have persistently challenged addiction treatment [14] [15].
Limitations of Symptom-Based Nosology in DSM-5 and ICD-10
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the International Classification of Diseases, 10th Revision (ICD-10) represent the two predominant systems for classifying mental disorders worldwide. These symptom-based classifications have largely become an integral part of the body of knowledge of psychiatrists throughout the world and instruments they constantly refer to [21]. Both systems are descriptive classifications that categorize mental disorders based upon a constellation or syndrome of symptoms and signs, with symptoms representing the patient's reports of personal experiences and signs being observable behaviors [22]. The fundamental premise underlying these systems is that mental disorders can be identified through specific patterns of symptoms that cluster together, and that these patterns represent distinct diagnostic entities.
However, particularly in the case of psychiatry, equating nosological classification with diagnosis and validity is far from always being the case [21]. From a scientific point of view, these two most up-to-date classification systems in use today may be considered as the theoretical basis of current psychiatric nosology, yet they face significant challenges, especially in the context of addiction disorders and their neurobiological validation. The essential limitation lies in the fact that in the absence of biological markers for most psychopathological disorders, diagnostic features were based primarily on clinical descriptions, resulting in "official" nosological groupings that may not accurately reflect underlying neurobiological realities [21]. This paper examines the specific limitations of these symptom-based approaches, presents experimental data highlighting their deficiencies, and explores the neurobiological frameworks that may inform future diagnostic paradigms.
Comparative Analysis of DSM-5 and ICD-10 Diagnostic Approaches
Structural and Conceptual Differences in Classification
The DSM-5 and ICD-10 systems demonstrate significant structural and conceptual differences in their approach to diagnosing substance use and addictive disorders. The ICD-10 utilizes a categorical approach with two primary diagnoses: harmful use (F1x.1) and dependence (F1x.2). Harmful use is broadly defined as a pattern of psychoactive substance use that causes damage to mental or physical health, while dependence requires the presence of three or more of six specific criteria occurring within a 12-month period: strong desire or compulsion to take the substance; difficulties in controlling substance use; withdrawal; tolerance; neglect of alternative pleasurable activities or interests; and continued use despite clear evidence of harmful consequences [23].
In contrast, DSM-5 conceptualizes substance use disorder (SUD) classification through a dimensional approach with a single unified SUD category of graded clinical severity. The DSM-5 includes 11 total SUD criteria and features three severity specifiers based on the total number of positive criteria: mild (2-3 positive criteria), moderate (4-5 positive criteria), and severe (6 or more positive criteria) [23]. This represents a significant shift from the traditional categorical approach toward a more graduated conceptualization of substance-related problems.
Table 1: Diagnostic Criteria Comparison Between DSM-5 and ICD-10 for Substance Use Disorders
| Feature | DSM-5 | ICD-10 (Clinical Version) | ICD-10 (Research Version) |
|---|---|---|---|
| Conceptual Approach | Dimensional | Categorical | Categorical |
| Primary Diagnoses | Substance use disorder with severity specifiers | Harmful use, Dependence | Harmful use, Dependence |
| Number of Criteria | 11 | 6 for dependence | 6 for dependence |
| Severity Classification | Mild (2-3 symptoms), Moderate (4-5 symptoms), Severe (6+ symptoms) | Binary (presence/absence of dependence) | Binary (presence/absence of dependence) |
| Harmful Use Definition | Incorporated into mild SUD | Pattern causing mental/physical damage | Expanded to include impaired judgment/dysfunctional behavior |
| Diagnostic Focus | Continuum of severity | Distinct categories | Distinct categories with broader harmful use criteria |
Diagnostic Concordance and Empirical Validation
Empirical studies examining the concordance between DSM-5 and ICD-10 diagnoses reveal significant limitations in their alignment, particularly for moderate severity cases. Research conducted with a large state prison sample (n = 7,672) demonstrated that while prevalence rates of cannabis use disorders were comparable across classification systems, diagnostic concordance varied substantially by severity level [23].
The vast majority of inmates with no DSM-5 diagnosis continued to have no diagnosis per the ICD-10, and a similar proportion with a DSM-5 severe diagnosis received an ICD-10 dependence diagnosis. However, most of the variation in diagnostic classifications was accounted for by those with a DSM-5 moderate diagnosis, in that approximately half of these cases received an ICD-10 dependence diagnosis while the remaining cases received a harmful use diagnosis [23]. This discordance highlights fundamental differences in how the two systems conceptualize the threshold for dependence.
Table 2: Diagnostic Concordance for Cannabis Use Disorders Between DSM-5 and ICD-10 (N=7,672)
| DSM-5 Diagnosis | ICD-10 Dependence Diagnosis | ICD-10 Harmful Use Diagnosis | No ICD-10 Diagnosis | Concordance Level |
|---|---|---|---|---|
| Severe (6+ symptoms) | 92.3% | 6.1% | 1.6% | Excellent |
| Moderate (4-5 symptoms) | 48.7% | 47.2% | 4.1% | Poor |
| Mild (2-3 symptoms) | 12.4% | 72.6% | 15.0% | Fair to Good |
| No Diagnosis | 2.3% | 8.9% | 88.8% | Excellent |
The kappa coefficient analysis between algorithmic diagnoses and expert clinician diagnoses further reveals validity concerns. A study comparing DSM-IV and ICD-10 diagnoses of schizophrenia found only marginal correlation between expert clinician and algorithmic diagnoses (kappa = 0.34 for DSM-IV; kappa = 0.37 for ICD-10), where kappa values below 0.4 indicate marginal correlation [21]. This suggests that instrumentally generated diagnoses may have relatively low validity when compared with clinician expert diagnoses derived from holistic assessment.
Methodological Limitations in Diagnostic Validation
Experimental Protocols for Diagnostic Reliability Assessment
Research examining the validity of symptom-based nosology employs rigorous methodological approaches to compare diagnostic outcomes. One representative study protocol conducted at the Mental Health Clinical Research Center of the University of Iowa College of Medicine evaluated the reproducibility and validity of ICD-10 and DSM-IV clinical and operational diagnoses of schizophrenia [21]. The experimental workflow involved multiple structured components:
Subject Recruitment and Assessment: The study analyzed medical records of 43 subjects from the DSM-IV Field Trial Iowa Site. Each participant underwent comprehensive assessment through both unstructured clinical interviews conducted by experienced clinicians and structured diagnostic interviews using the Comprehensive Assessment of Symptoms and History (CASH) instrument.
Diagnostic Formulation: Two diagnostic methods were applied for each subject: (1) Clinical expert diagnoses derived from unstructured interviews employing a "holistic approach"; and (2) Algorithmic diagnoses generated through computer scoring of structured CASH interviews with diagnostic algorithms applied directly to the recorded symptoms.
Algorithm Development: Researchers prepared specific diagnostic algorithms for DSM-IV and ICD-10 diagnoses of schizophrenia, programming them for computerized scoring to ensure consistency and eliminate rater bias in application of diagnostic criteria.
Statistical Analysis: The correlation between algorithmic diagnoses and expert clinician diagnoses was quantified by calculating kappa coefficients, with established interpretive guidelines: kappa > 0.75 (excellent correlation), 0.4 < kappa < 0.74 (good correlation), and kappa < 0.4 (marginal correlation) [21].
This methodological approach allowed researchers to test the hypothesis that, assuming the expert clinician diagnosis represents a valid "gold standard," observation of a low correlation between clinician and algorithmic diagnoses would reflect low validity of the algorithmic diagnosis.
Key Research Reagents and Assessment Tools
The experimental assessment of diagnostic validity relies on specialized instruments and methodological tools. The following research reagents represent essential components for conducting diagnostic validation studies in psychiatry:
Table 3: Essential Research Reagents for Diagnostic Validation Studies
| Research Tool | Function | Application in Validation Studies |
|---|---|---|
| Comprehensive Assessment of Symptoms and History (CASH) | Structured interview for recording signs, symptoms, and history | Provides standardized data for algorithmic diagnosis [21] |
| Schedule for Clinical Assessment in Neuropsychiatry (SCAN) | Structured diagnostic interview for psychopathology | Enables systematic assessment of mental status [21] |
| Substance Use Disorder Diagnostic Schedule-IV (SUDDS-IV) | Automated diagnostic instrument for substance use disorders | Generates DSM and ICD compatible diagnoses [23] |
| Kappa Coefficient Statistics | Measures inter-rater reliability beyond chance agreement | Quantifies diagnostic concordance between systems [21] |
| Diagnostic Algorithms | Computerized criteria application for DSM/ICD diagnoses | Eliminates clinical judgment in operational diagnoses [21] |
| Addictions Neuroclinical Assessment (ANA) | Translates neurobiological stages to clinical domains | Bridges neurobiology and diagnostic assessment [10] |
Neurobiological Frameworks Challenging Symptom-Based Nosology
The Addiction Cycle and Neurobiological Stages
Contemporary models of addiction utilize a neurobiological framework that fundamentally challenges symptom-based diagnostic approaches. This framework defines addiction as a chronic and relapsing disorder marked by specific neuroadaptations that predispose an individual to pursue substances irrespective of potential consequences [10]. These neuroadaptations occur in three distinct neurobiological stages that cut across traditional diagnostic categories:
Binge/Intoxication Stage: During this initial stage, dopaminergic firing in the basal ganglia increases for substance-associated cues while diminishing for the substance itself, a phenomenon known as incentive salience [10]. The reward system activates two significant pathways: the mesolimbic pathway (responsible for reward and positive reinforcement via dopamine and opioid peptides) and the nigrostriatal pathway (controlling habitual motor function and behavior) [10].
Withdrawal/Negative Affect Stage: This stage involves two primary neuroadaptations. First, chronic reward exposure decreases dopaminergic tone in the nucleus accumbens while shifting the glutaminergic-GABAergic balance toward increased glutaminergic tone. Second, there is increased recruitment of stress circuits in the extended amygdala (the "anti-reward" system), leading to increased release of stress mediators including dynorphin, corticotropin-releasing factor, norepinephrine, and orexin [10].
Preoccupation/Anticipation Stage: The signature of this phase is preoccupation with using the substance ("cravings"), primarily involving the prefrontal cortex. Researchers have identified two systems within the PFC: a "Go system" (involving decisions requiring considerable attention and planning) and a "Stop system" (responsible for inhibitory control) [10]. In addiction, the balance between these systems becomes disrupted, leading to diminished executive control.
Neurobiological Theories of Addiction
Several neurobiological theories provide comprehensive explanations for addictive processes that transcend symptom-based classifications:
Opponent-Process Theory: Developed by Solomon and Corbit, this theory posits that when a positive affective response (primary process) is activated by drug consumption, mechanisms simultaneously initiate an opposite response (opponent process) to restore homeostasis [24]. Repeated drug consumption strengthens the opponent process, leading to tolerance (as the pleasurable primary process is counteracted) and withdrawal syndrome (as the strengthened opponent process creates prolonged discomfort after drug effects diminish) [24].
Dopaminergic Hypothesis of Addiction: This theory establishes that the reward level induced by a drug is directly related to the phasic increase in dopamine levels in the nucleus accumbens [24]. The mesolimbic cortical dopaminergic pathway, with projections from the ventral tegmental area to the nucleus accumbens and connections to hippocampus, prefrontal cortex, amygdala, and other structures, represents the common neural substrate for natural rewards and drugs [24].
Allostasis Theory: An extension of opponent-process theory, this model emphasizes the chronic dysregulation of brain reward and stress systems beyond homeostasis, creating a new set point that perpetuates addictive behavior through continued substance use [24].
These neurobiological models demonstrate that addiction involves specific, measurable alterations in brain structure and function that are not adequately captured by current symptom-based diagnostic criteria.
Emerging Alternatives to Traditional Nosology
The Hierarchical Taxonomy of Psychopathology (HiTOP)
The HiTOP framework was developed by a consortium of psychopathology researchers as an alternative to traditional diagnostic categories. This system provides an empirically based, fully dimensional organization of psychopathology by subjecting current diagnoses, syndromes, and symptoms to multivariate factor-analytic procedures [25]. HiTOP posits that psychopathology is hierarchically structured with symptoms/signs (level 1) nested within syndromes/traits (level 2), which are nested within factors (level 3), with broad spectra at the highest level (level 4) [25].
The model identifies several broad spectra, including internalizing pathology (encompassing fear, distress, eating pathology, and sexual problems), externalizing pathology (comprising disinhibited and antagonistic behaviors, substance abuse, and antisocial behavior), thought disorder (psychosis spectrum disorders), and detachment (pathological introversion) [25]. This dimensional approach addresses the substantial heterogeneity within traditional diagnostic categories and the problem of excessive comorbidity between putatively independent disorders.
Research Domain Criteria (RDoC)
The RDoC program was initiated by the National Institute of Mental Health as a dimensional and translational alternative to current psychiatric classification. Unlike the DSM/ICD top-down approach that defines disorders based on signs and symptoms, RDoC encourages a bottom-up approach that examines the normal distribution of traits or characteristics, the brain systems implementing these functions, and factors causing dysregulation that results in psychopathology [25].
The RDoC framework organizes research around five neurobiological domains: negative valence systems (acute threat, potential threat, sustained threat, loss, frustrative nonreward), positive valence systems (reward responsiveness, reward learning, habit), cognitive systems (attention, perception, memory, cognitive control), systems for social processes (attachment, social communication, perception of self/others), and arousal/modulatory systems (circadian rhythms, sleep/wake) [25]. This approach aims to address the lack of pathophysiological specificity within and between traditional psychiatric diagnoses.
Implications for Research and Drug Development
The limitations of symptom-based nosology have significant implications for research and pharmaceutical development. The inherent limitations of heterogeneous and fuzzy DSM/ICD diagnoses have been disclosed by functional neuroimaging studies demonstrating that no single pattern of aberrant brain activation consistently replicates across experiments [25]. Distinct pathophysiological mechanisms subsumed under the same diagnostic category are seen by the pharmaceutical industry as a major cause of the low-response rate of psychiatric drugs [25].
The neurobiological stages of addiction (binge/intoxication, withdrawal/negative affect, preoccupation/anticipation) offer an alternative framework for developing targeted treatments. The Addictions Neuroclinical Assessment (ANA) translates these three neurobiological stages into three neurofunctional domains: incentive salience, negative emotionality, and executive dysfunction [10]. This approach allows clinicians and researchers to employ targeted treatments for specific clinical presentations based on underlying neurobiology rather than symptom clusters.
Emerging evidence suggests that dimensional approaches like HiTOP and RDoC can advance etiological research, promote development of new treatments, and facilitate detection of genetic and neurobiological markers for application in diagnostic clinical tests [25]. These frameworks acknowledge that psychopathology is not organized according to the DSM/ICD scheme, and that adopting fully dimensional representations of mental disorders substantially improves reliability and validity beyond categorical measures [25].
The symptom-based nosology embodied in DSM-5 and ICD-10 demonstrates significant limitations when evaluated through the lens of contemporary neurobiological research. Empirical evidence reveals only marginal correlation between operational diagnoses and clinician expert diagnoses, poor diagnostic concordance for moderate severity cases, and inadequate representation of the underlying neurobiological processes in addiction. The emerging understanding of addiction as a cyclic process involving specific neuroadaptations in the basal ganglia, extended amygdala, and prefrontal cortex challenges the categorical, symptom-based approach of traditional diagnostic systems.
Alternative frameworks such as the Hierarchical Taxonomy of Psychopathology and Research Domain Criteria offer promising dimensional approaches that better align with the neurobiological evidence. For researchers and drug development professionals, these approaches provide opportunities to develop more targeted interventions based on specific neurofunctional domains rather than heterogeneous symptom clusters. Future diagnostic systems must integrate neurobiological dimensions with clinical observation to create more valid and clinically useful classifications that ultimately advance both treatment and research in addictive disorders.
Substance use disorders (SUDs) represent a significant global public health challenge, historically understood through categorical diagnostic systems that have limited biological validity and treatment personalization. The Research Domain Criteria (RDoC) framework, initiated by the National Institute of Mental Health, marks a paradigm shift by proposing a dimensional approach that links clinical presentations with their underlying biological foundations [26]. This framework organizes core dimensions of behavior across multiple levels of analysis, from genes to circuits to behavior, viewing these aspects as varying along a continuum rather than in distinct categories [27]. For addiction science, this translational approach offers unprecedented opportunities to identify functional mechanisms that transcend traditional diagnostic boundaries and align more precisely with the neurobiological evidence [28].
The contemporary understanding of addiction utilizes a neurobiological framework that defines it as a chronic and relapsing disorder marked by specific neuroadaptations which predispose an individual to pursue substances irrespective of potential consequences [10]. These neuroadaptations occur in three distinct neurobiological stages—intoxication/binge, withdrawal/negative affect, and preoccupation/anticipation—each involving specific brain regions and circuit dysfunctions [10]. The RDoC framework provides an ideal structure for investigating these stages as dimensional constructs rather than binary diagnoses, potentially revolutionizing both assessment and intervention strategies for addictive disorders.
Theoretical Foundation: RDoC Principles and Addiction Neurobiology
Core RDoC Concepts and Domain Structure
The RDoC framework is built upon several fundamental principles that distinguish it from traditional diagnostic systems. It employs a dimensional approach to psychopathology, viewing mental functioning as occurring along continuous valid dimensions ranging from functional to pathological [26]. This approach stands in contrast to the categorical systems of ICD and DSM, which define symptoms and symptom clusters but face significant limitations due to high comorbidity, clinical heterogeneity, and exclusion of biomarkers [26]. The framework spans multiple levels of analysis, from genes to behavior, promoting multi-level analysis and integrating disciplines from psychology to neuroscience to biology [27].
RDoC organizes psychological functioning into six major domains: Negative Valence Systems (e.g., fear, anxiety), Positive Valence Systems (e.g., reward processing), Cognitive Systems (e.g., attention, memory), Social Processes (e.g., social cognition), Arousal and Regulatory Systems (e.g., sleep-wake cycles), and Sensorimotor Systems [29]. Within each domain, specific constructs and sub-constructs represent biopsychological processes and mechanisms regarded as continua between functional and pathological states [26]. Importantly, these dimensions are not considered final or static but as dynamic constructs constantly adapted to and extended by current research findings [26].
Neurocircuitry of Addiction: The Three-Stage Cycle
Addiction neurobiology is characterized by a repeating cycle of three distinct stages, each with specific neural substrates and behavioral manifestations. The intoxication/binge stage begins when an individual consumes a rewarding substance, primarily involving the basal ganglia [10]. During this stage, dopaminergic firing increases for substance-associated cues while diminishing for the substance itself—a process known as incentive salience [10]. The mesolimbic pathway, facilitating communication between the ventromedial striatum and nucleus accumbens, is responsible for the reward and positive reinforcement via direct release of dopamine and opioid peptides [10].
The withdrawal/negative affect stage comprises acute and post-acute withdrawal phenomenology, characterized by two primary neuroadaptations [10]. First, chronic reward exposure decreases dopaminergic tone in the nucleus accumbens while shifting the glutaminergic-GABAergic balance toward increased glutaminergic tone. Second, stress circuits in the extended amygdala (the "anti-reward" system) become increasingly recruited, leading to elevated release of stress mediators including dynorphin, corticotropin-releasing factor, and norepinephrine [10]. The clinical consequences present as irritability, anxiety, and dysphoria, driving further substance use through negative reinforcement.
The preoccupation/anticipation stage occurs during abstinence periods and is characterized by cravings and preoccupation with substance use [10]. This stage primarily involves the prefrontal cortex (PFC), which is responsible for executive functions including planning, task management, and regulation of thoughts, emotions, and impulses [10]. Researchers have conceptualized two systems within the PFC: a "Go system" for goal-directed behaviors requiring attention and planning, and a "Stop system" for inhibitory control—both of which become dysregulated in addiction.
Table 1: RDoC Domains Relevant to Addiction Pathology
| RDoC Domain | Relevant Addiction Constructs | Associated Neural Circuitry | Behavioral Manifestations |
|---|---|---|---|
| Positive Valence Systems | Reward learning, incentive salience, habit formation | Mesolimbic dopamine pathway, ventral striatum, basal ganglia | Compulsive drug-seeking, cue reactivity |
| Negative Valence Systems | Acute threat (fear), sustained threat (anxiety), loss | Extended amygdala, BNST, HPA axis | Withdrawal symptoms, negative affect, stress-induced relapse |
| Cognitive Systems | Executive function, cognitive control, working memory | Prefrontal cortex, anterior cingulate, dorsolateral PFC | Poor decision-making, impaired inhibitory control, cravings |
| Arousal/Regulatory Systems | Arousal, sleep-wake regulation | Brainstem, hypothalamus, thalamocortical circuits | Sleep disturbances, emotional dysregulation |
Assessment Frameworks: From Traditional Tools to RDoC-Aligned Approaches
Conventional Addiction Assessment Instruments
Traditional addiction assessment has relied on structured interviews, self-report questionnaires, and clinical observations focusing primarily on behavioral symptoms and consumption patterns. These include broad-spectrum screening tools like the Tobacco, Alcohol, Prescription Medication and Other Substance Use (TAPS) tool, which offers validated, broad-spectrum screening specifically designed for adult populations [11]. For adolescent populations, specialized instruments such as the CRAFFT 2.1 questionnaire (with six questions exploring behaviors captured by the acronym CRAFFT: Car, Relax, Alone, Forget, Family/Friends, Trouble) and BSTAD effectively address developmental considerations while enabling systematic risk stratification [11]. These tools have demonstrated high diagnostic accuracy with area under the curve values between 0.89 and 1 in validation studies [11].
Advanced severity measurement instruments used in clinical settings include the Addiction Severity Index (ASI), which employs 0-9 scoring across seven domains to enable precise measurement of treatment urgency and progress [11]. Similarly, the ASAM's six-dimensional criteria drive treatment planning by replacing outdated single-symptom approaches with multidimensional risk assessment protocols [11]. While these instruments provide valuable clinical information, they primarily operate at the level of observed behavior and self-report without systematically incorporating neurobiological data across multiple units of analysis as encouraged by the RDoC framework.
Emerging Neuroscience-Informed Assessment Paradigms
The integration of neuroscientific principles with addiction assessment has led to the development of novel frameworks that align more closely with RDoC principles. The Addictions Neuroclinical Assessment (ANA) represents a significant advancement by translating the three neurobiological stages of addiction into three neurofunctional domains: incentive salience, negative emotionality, and executive dysfunction [10]. This clinical instrument, developed by the National Institute of Alcohol Abuse and Alcoholism, allows clinicians to employ targeted treatments for specific clinical presentations based on underlying neurofunctional impairments rather than symptom counts alone [10].
Complementing the ANA, alternative models like the ASPIRE framework propose a patient-centered, neuroscience-based approach for treating SUDs through shared decision-making [30]. This model tailors personalized medical care and precision medicine research to six neuroscience-based risk categories that patients report as most distressing: (A) Anhedonia/reward-deficit state; (S) Stressful/anti-reward state; (P) Pathological lack of self-control; (I) Insomnia associated with substance use; (R) Restlessness; and (E) Excessive preoccupation with seeking drug reinforcers [30]. Such approaches demonstrate how RDoC principles can be operationalized in clinical settings through concise assessment batteries that map onto biologically-based risk categories.
Table 2: Comparison of Traditional and RDoC-Aligned Assessment Approaches
| Assessment Characteristic | Traditional Assessment Tools | RDoC-Aligned Frameworks |
|---|---|---|
| Primary Focus | Behavioral symptoms, consumption patterns, psychosocial consequences | Neurofunctional domains, circuit-level dysfunctions, dimensional constructs |
| Theoretical Basis | Categorical diagnoses (DSM-5, ICD-11) | Dimensional psychopathology, neurocircuitry models |
| Typical Instruments | CRAFFT, ASI, TAPS, DSM-5 criteria | ANA, ASPIRE, neuroimaging, behavioral paradigms |
| Strengths | Standardized administration, established validity, clinical familiarity | Neurobiological validity, personalized treatment targets, transdiagnostic applicability |
| Limitations | Limited neurobiological integration, symptom focus rather than mechanisms | Assessment burden, translational challenges, limited clinical implementation |
Methodological Approaches: Experimental Protocols and Validation Studies
Latent Variable Approaches to RDoC Validation
Recent research has employed sophisticated statistical methods to empirically validate and refine the RDoC framework. A 2025 study published in Nature Communications utilized a latent variable approach with bifactor analysis to examine circuit-function relations in the RDoC framework [27]. The researchers examined 84 whole-brain task-based fMRI activation maps from 19 studies with 6192 participants, using a curated subset of 37 maps with balanced RDoC domain representation as a training set and remaining maps for internal validation [27]. External validation was conducted using 36 peak coordinate activation maps from Neurosynth, using terms of RDoC constructs as seeds for topic meta-analysis [27].
The study compared four distinct latent variable models, combining two methods of factor derivation (theory-driven RDoC factors or data-driven empirical factors) with two types of factor models (specific factor models or bifactor models) [27]. Results demonstrated that a bifactor model incorporating a task-general domain and splitting the cognitive systems domain provided better fit to task-based fMRI data than the current RDoC framework [27]. Additionally, the domain of arousal and regulatory systems was identified as underrepresented in the current framework [27]. These findings highlight how data-driven approaches can inform refinements to the RDoC structure to better reflect underlying brain circuitry.
Integrative Biopsychosocial Assessment Protocols
Comprehensive addiction assessment within an RDoC framework requires integration of data across multiple units of analysis. The TOPOWA Study (The Onward Project On Well-being and Adversity) exemplifies this approach by combining the RDoC framework with a social determinants lens to explore pathways linking social adversity to mental health challenges [29]. This study integrates diverse data sources, including biomarkers, wearable sensors, and self-report surveys, to capture multilevel influences on mental health in low-resource settings [29]. The approach demonstrates how RDoC can be adapted for community-based, context-sensitive research to support development of targeted mental health interventions.
The startle reflex potentiation method offers a low-cost, low-burden translational tool to study threat-related brain circuits in community settings where neuroimaging is not feasible [29]. This defensive response, common to all mammals, provides a practical method for examining neurobiological responses to environmental threat in individuals experiencing extreme poverty or other adverse conditions. Such methodological innovations are crucial for democratizing access to biologically informed mental health science and expanding RDoC-aligned research beyond well-resourced laboratory settings.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for RDoC-Aligned Addiction Studies
| Research Tool Category | Specific Examples | Primary Research Function | RDoC Alignment |
|---|---|---|---|
| Neuroimaging Platforms | task-based fMRI, resting-state fMRI, structural MRI | Circuit-level analysis, functional connectivity, structural correlates | Multiple units of analysis from circuits to behavior |
| Physiological Monitoring | Wearable sensors, startle reflex potentiation, heart rate variability | Arousal regulation, stress reactivity, real-world monitoring | Arousal/regulatory systems, negative valence systems |
| Genetic Analysis Tools | Polygenic risk scores, genome-wide association studies, epigenetic markers | Genetic vulnerability, gene-environment interactions, molecular mechanisms | Genetic levels of analysis, individual differences |
| Behavioral Paradigms | Monetary incentive delay task, emotional Stroop, fear conditioning | Reward processing, cognitive control, threat sensitivity | Positive/negative valence systems, cognitive systems |
| Self-Report Measures | PROMIS measures, PhenX Toolkit, ecological momentary assessment | Subjective experience, real-world functioning, symptom tracking | Self-report units of analysis, cross-level integration |
Data Integration and Analysis: Quantitative Findings and Comparative Validation
Empirical Validation of RDoC Framework
The 2025 latent variable analysis of RDoC domains provided compelling quantitative evidence regarding the framework's neural validity [27]. When conducting confirmatory factor analyses with RDoC factors, researchers found that most maps within each domain loaded significantly onto factors representing their domains (cognitive systems: 11/15; negative valence systems: 5/5; positive valence systems: 6/7; social processes: 6/6; sensorimotor systems: 4/4) [27]. Comparison of the RDoC-specific factor model with the bifactor model revealed that the bifactor model had a better fit according to all fit indices (Tukey's test, p < .001), suggesting that adding a general factor reflecting domain-general activation patterns improved model fit [27].
In data-driven analyses, parallel analysis indicated that models with eight factors or less had eigenvalues greater than expected by chance [27]. When extracting eight specific factors in data-driven confirmatory factor analyses, all but two maps across RDoC domains loaded on the general factor, indicating that maps across distinct studies and tasks showed overlap in activation patterns [27]. ANOVA results indicated significant differences in fit among all the RDoC and data-driven model types (robust RMSEA: F(3, 19588) = 108,961, p < .001; robust CFI: F(3, 19588) = 212,411, p < .001; robust TLI: F(3, 19588) = 209,379, p < .001) [27]. The data-driven bifactor model demonstrated greater overall fit to the data compared with both RDoC models and the data-driven specific factor model (Tukey's test, p < .001) [27].
Comparative Performance of Assessment Approaches
Modern addiction assessment tools show varying degrees of effectiveness across different populations and settings. Digital assessment platforms have demonstrated significant advantages in clinical implementation, with AI-driven tools analyzing electronic health records in real-time and reducing hospital readmissions by 47% [11]. These systems mimic brain-based pattern recognition to identify substance use indicators within clinical documentation, triggering immediate provider alerts when specialist consultations are needed [11].
For adolescent populations, specialized assessment tools have shown particularly strong performance characteristics. The CRAFFT screening tool offers rapid assessment through six targeted questions, while technology-focused instruments like the Internet Addiction Test provide granular analysis of online usage patterns with standardized scoring thresholds (40-69 for addiction, ≥69 for severe cases) ensuring reliable clinical intervention points [11]. The Comprehensive Inventory of Urges and Symptoms (CIUS) employs 5-point Likert scales to capture longitudinal severity patterns from "never" to "very often," while the Internet Severity and Addiction Questionnaire (ISAAQ) uses a 6-point system for more granular assessment of behavioral progression [11].
Table 4: Performance Metrics of Modern Addiction Assessment Tools
| Assessment Tool | Target Population | Administration Time | Key Performance Metrics | Clinical Utility |
|---|---|---|---|---|
| TAPS Tool | Adults | 5-10 minutes | Validated for broad-spectrum screening | Primary care integration, multiple substance assessment |
| CRAFFT 2.1 | Adolescents (12-21) | 2-5 minutes | High sensitivity/specificity for SUD risk | Pediatric settings, early intervention |
| Addiction Severity Index (ASI) | Adults with SUD | 10-20 minutes | 0-9 scoring across 7 domains | Treatment planning, progress monitoring |
| Digital Media Overuse Scale (dMOS) | Technology users | 5-7 minutes | Evaluates 5 online behavior categories | Emerging behavioral addictions |
| Addictions Neuroclinical Assessment | Research populations | Extensive (hours) | Three neurofunctional domains | Precision medicine, mechanism-targeted interventions |
Future Directions: Staging Models and Personalized Intervention
Implementing a Staging Paradigm for Substance Use Disorders
A promising direction for RDoC-aligned addiction research involves the development of comprehensive staging models that incorporate multidimensional factors including social determinants of health [31]. Such models would address the current limitation in which classification systems like DSM-5 diagnose mild, moderate, and severe SUDs based solely on the number of criteria without adequately addressing severity or treatment relevance [31]. A dynamic structured staging model for SUDs could transform clinical care by incorporating the reality of complex psychosocial contributions to patient outcomes [31].
This staging approach would incorporate multiple dimensions categorized into: clinical severity (accounting for cross-sectional severity), chronicity (duration of unresolved addiction and comorbidities), and social determinants of health status (adversity of patient circumstances) [31]. Unlike current diagnostic approaches, a comprehensive staging model would acknowledge that no single factor, irrespective of its severity, can solely determine the overall SUD stage [31]. The model would also incorporate the nonlinear nature of SUD whereby an individual's stage is expected to be dynamic and may change in response to treatment, illness remission or progression, or environmental elements [31].
Neuroscience-Informed Interventions and Precision Medicine
The ultimate translational application of RDoC-aligned addiction research lies in developing targeted, mechanism-focused interventions. Neuroscience-informed psychoeducation represents one such approach, utilizing connectivity-based neuromarkers or brain networks as a framework to provide non-judgmental insight for adolescents regarding the potential vulnerability of neurocognitive systems to continued substance use [28]. The Neuroscience-Informed Psychoeducation App (NIPA) exemplifies this approach, developed with the aim of increasing adolescents' awareness and resilience to the effects of drugs and other emotional triggers on brain and cognitive functions [28].
For treatment-refractory cases, palliative care models have been proposed as a holistic treatment paradigm involving long-term residential care, similar to skilled nursing facilities utilized for palliative care in medical conditions [31]. This may include hospice-type treatment and SUD-specific interventions such as supervised injection sites, or models of maintenance treatment with injected drugs (heroin maintenance or hydromorphone maintenance) [31]. While controversial, such approaches acknowledge the chronicity and treatment resistance of some severe SUD presentations and align with the RDoC emphasis on dimensional severity rather than binary diagnostic categories.
The alignment of addiction research with the RDoC framework represents a transformative approach that bridges decades of neurobiological findings with clinical assessment and intervention. By focusing on dimensional constructs across multiple units of analysis—from genetics and circuits to behavior and self-report—this approach offers a more nuanced understanding of addiction's underlying mechanisms [26] [27]. The validation of assessment frameworks like the Addictions Neuroclinical Assessment [10] [30] and the development of integrated staging models [31] demonstrate the translational potential of this approach.
Future research directions should prioritize the refinement of RDoC domains through continued data-driven validation [27], the development of feasible assessment protocols for diverse settings [29], and the testing of mechanism-targeted interventions [28] [31]. As the field progresses, the integration of social determinants of health with neurobiological vulnerability will be essential for comprehensive models that address the full complexity of substance use disorders [29]. Through these advances, the vision of precision medicine for addiction—with assessments and interventions targeted to specific neurofunctional domains and individual characteristics—moves closer to realization.
From Theory to Toolbox: Methodologies for Neurobiologically-Informed Assessment
The integration of digital technology and gamification into neurocognitive assessment represents a paradigm shift in the identification and monitoring of addiction risk. Traditional tools, often designed for neurological disorders, fail to capture the core neurocognitive constructs mechanistically linked to addictive behaviors and lack the ecological validity and scalability required for widespread early intervention. This guide objectively compares the performance of a novel, digitally gamified assessment battery—the BrainPark Assessment of Cognition (BrainPAC)—against established laboratory paradigms and other contemporary assessment frameworks. We synthesize validation data, detail experimental protocols, and situate these findings within the broader thesis of neurobiologically-validated addiction assessment, providing researchers and drug development professionals with a clear comparison of next-generation tools.
Addiction is understood as a chronic, relapsing disorder characterized by specific neuroadaptations that underpin a cyclical pattern of behavior, classically described in three stages: bingeing/intoxication, withdrawal/negative affect, and preoccupation/anticipation [10]. These stages are subserved by dysfunctions in distinct brain networks: the basal ganglia (reward and habit), the extended amygdala (stress and negative affect), and the prefrontal cortex (executive control and craving) [10] [24]. This neurobiological framework, exemplified by the Addictions Neuroclinical Assessment (ANA), posits that addiction heterogeneity can be understood through the prism of three core neurofunctional domains: Incentive Salience, Negative Emotionality, and Executive Function [4].
Traditional neurocognitive batteries are limited for addiction research and clinical practice. They often assess functions not core to addiction, such as processing speed or episodic memory, having been primarily designed for brain injury or dementia assessment [32] [33]. Furthermore, they are frequently lengthy, unengaging, and difficult to administer at scale, lacking ecological validity as their performance in sterile, clinical settings fails to predict real-world functioning [33]. This creates an urgent need for engaging, scalable, and purpose-built tools that validly assess the neurocognitive antecedents of addictive behaviors [32].
Methodology: Comparing Assessment Tools and Validation Protocols
To objectively compare BrainPAC against its alternatives, it is essential to understand the experimental protocols used for its validation and that of other instruments. The following section details these methodologies.
The BrainPAC Validation Protocol
The BrainPAC project aimed to develop and validate a gamified battery based on an international Delphi consensus of key neurocognitive constructs in addiction [32] [34].
- Study Design: A cross-sectional design was employed across three successive validation cohorts (total N=600) and a separate test-retest cohort (N=50).
- Participant Recruitment: Participants were recruited via Amazon's Mechanical Turk, restricted to users with >95% approval ratings to ensure data quality. Inclusion criteria were ages 18-55 and English fluency.
- Experimental Procedure: Participants completed both the original, standard laboratory paradigms and their newly developed gamified versions. The five core tasks were:
- Balloon Analogue Risk Task (BART): Measures action selection and risk-taking.
- Stop Signal Task (SST): Measures response selection and inhibition.
- Delay Discounting Task (DDT): Measures reward valuation.
- Value-Modulated Attentional Capture (VMAC) Task: Measures reward learning and cognitive flexibility (compulsivity).
- Sequential Decision-Making Task (SDT): Measures reward learning and reward prediction error.
- Gamification Process: The gamification was an iterative process involving neuropsychologists, game developers, and community focus groups to enhance engagement while preserving the core neurocognitive elements of the original tasks [32].
- Statistical Validation: The primary analyses focused on:
- Convergent Validity: Pearson correlations between metrics from the gamified and original tasks.
- Test-Retest Reliability: Intraclass correlation coefficients (ICC) calculated from the separate cohort.
- Criterion Validity: Associations between gamified task metrics and scores on behavioral inventories for addictive behaviors.
Validation Protocols for Other Frameworks
Other assessment models employ different validation approaches:
- The Addictions Neuroclinical Assessment (ANA): This framework was initially validated using factor analysis on secondary data from the NIAAA Natural History Protocol, primarily comprising self-report measures [4]. A more recent study [4] prospectively administered a standardized battery of behavioral tasks and self-reports to 300 participants across the drinking spectrum. Factor analyses (Exploratory and Confirmatory) were used to identify latent factors underlying the three ANA domains.
- Virtual Reality (VR) and Mobile Game Assessments: One study [33] compared cognitive assessment scores from 2 VR and 1 mobile 3D game against the traditional Addenbrooke's Cognitive Examination (ACE-III) in 82 young participants. The validation methods included correlational analysis, Z-score comparison, and multiple regression analysis to explore associations with cognitive health factors.
Results & Comparison: Quantitative Performance Data
The following tables summarize the key performance metrics of BrainPAC against the tools it aims to augment or replace.
Table 1: Comparison of BrainPAC's Psychometric Properties Against Standard Laboratory Paradigms [32] [34]
| Neurocognitive Construct | BrainPAC Task | Correlation with Lab Paradigm (r) | Test-Retest Reliability (ICC) |
|---|---|---|---|
| Action Selection | Gamified BART | 0.18 - 0.63* | 0.91* |
| Response Selection/Inhibition | Gamified SST | 0.18 - 0.63* | 0.84* |
| Reward Valuation | Gamified DDT | 0.18 - 0.63* (Excl. k function) | 0.72* |
| Reward Learning / Compulsivity | Gamified VMAC | 0.18 - 0.63* (Excl. total points) | 0.75* |
| Reward Learning / Prediction Error | Gamified SDT | 0.18 - 0.63* | Not Significant |
*p < .05 for most metrics; *p < .001
Table 2: Comparison of BrainPAC with Other Modern Assessment Approaches
| Assessment Feature | BrainPAC (Gamified Digital) | Traditional Lab Paradigms | ANA Framework (Standardized Battery) | VR/Mobile 3D Games |
|---|---|---|---|---|
| Primary Focus | Core addiction neurocognition | Basic cognitive science constructs | Neurofunctional domains (Incentive Salience, Negative Emotionality, Executive Function) | Real-world functional cognition |
| Ecological Validity | Designed to be engaging; moderate | Low; administered in sterile lab settings | Varies by measure; often includes self-report | High; simulates real-world environments |
| Scalability & Accessibility | High; designed for remote administration | Low; requires lab equipment & personnel | Moderate; requires structured administration | Potentially high with consumer hardware |
| Key Validation Metric | Correlation with lab tasks (r=0.18-0.63) [32] | N/A (Gold Standard) | Factor loadings of latent constructs [4] | Correlation with ACE-III (r=0.29-0.45) [33] |
| Engagement Strategy | Built-in gamification | None; repetitive tasks | None; standard questionnaires/tasks | Immersive, goal-oriented gameplay |
| Administration Time | ~60 minutes for full battery | Varies; often lengthy | Comprehensive battery (~several hours) [4] | Varies by game |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key components used in the development and validation of the BrainPAC model, which can serve as a guide for similar research and development efforts.
Table 3: Research Reagent Solutions for Digital Cognitive Assessment Development
| Item Name / Category | Function in Research & Development | Example from BrainPAC/Related Studies |
|---|---|---|
| Consensus-Defined Constructs | Provides a content-valid theoretical foundation for task selection. | International Delphi panel identified 7 key constructs (e.g., reward valuation, habit) [32]. |
| Gold Standard Laboratory Paradigms | Serves as the criterion for validating new assessment tools. | BART, SST, DDT, VMAC, SDT were used as the reference standards [32] [34]. |
| Gamification Software Platform | The digital environment for creating engaging task versions. | Developed in collaboration with professional game developers [32]. |
| Online Participant Recruitment Platform | Enables rapid recruitment of large, diverse cohorts for validation. | Amazon Mechanical Turk (with >95% approval rating filter) [32] [34]. |
| Data Quality Checks | Ensures the integrity of unsupervised, remote data collection. | Implementation of validity questions and screening for reduced effort [32]. |
| Standardized Behavioral Inventories | Provides measures for establishing criterion validity. | Used to correlate BrainPAC metrics with real-world addictive behaviors [32]. |
| Statistical Analysis Pipeline (e.g., R, Python) | For psychometric analysis (correlation, ICC, factor analysis). | Used to calculate convergence, reliability, and associations with behavior [32] [4]. |
Visualizing the Neurocognitive Workflow in Addiction
The following diagram illustrates the logical workflow of the addiction cycle and how modern assessment tools like BrainPAC and the ANA map onto the underlying neurobiology, providing a framework for their use in research.
Addiction Neurobiology and Assessment Mapping
This diagram delineates the foundational neurobiological model of addiction's three-stage cycle and maps the corresponding brain regions and the assessment domains of the ANA and BrainPAC frameworks onto this model, illustrating their targeted approach.
Discussion: Implications for Research and Drug Development
The validation of BrainPAC demonstrates that a digitally gamified battery can reliably assess core addiction-related neurocognitive processes, offering a tool that is both scalable and engaging [32]. Its significant correlations with laboratory paradigms and good test-retest reliability for most tasks provide a strong empirical foundation for its use. However, the model is not without limitations; the Sequential Decision-Making Task showed poor reliability, and the tool's sensitivity to change in longitudinal studies or clinical trials requires further investigation.
For researchers and drug development professionals, the shift towards tools like BrainPAC, the ANA, and VR assessments offers several advantages. They facilitate the early detection of at-risk individuals in community settings before diagnostic thresholds are met [32]. In clinical trials, they can serve as mechanistic biomarkers to evaluate whether a potential therapeutic agent specifically targets underlying neurocognitive dysfunctions, such as poor inhibitory control or aberrant reward valuation, rather than just reducing consumption [35] [4]. This aligns with the broader thesis in psychiatry of moving away from syndromal diagnoses towards dimensions of neurobehavioral function.
Future development should focus on enhancing convergence with established measures, collecting large-scale normative data for clinical comparison, and further integrating these tools with other digital phenotyping data, such as from wearables, to create a multi-modal, ecologically valid assessment system for addiction.
Behavioral tasks are fundamental tools in addiction neuroscience, providing objective measures of core cognitive and motivational processes disrupted in substance use disorders. This guide provides a comparative analysis of three key paradigms: the Stop-Signal Task (SST) for response inhibition, the Delay Discounting Task (DDT) for reward valuation, and the Balloon Analogue Risk Task (BART) for risk-taking and habitual behavior. Understanding the specific constructs, methodologies, and neurobiological correlates of these tasks is essential for researchers selecting appropriate assessments for addiction phenotyping and therapeutic development. This comparison is framed within the broader thesis that precise behavioral measurement, grounded in neurobiological validation, is critical for advancing addiction research and drug development.
The table below summarizes the core attributes, neurobiological substrates, and clinical applications of the SST, DDT, and BART.
Table 1: Core Characteristics of the SST, DDT, and BART
| Feature | Stop-Signal Task (SST) | Delay Discounting Task (DDT) | Balloon Analogue Risk Task (BART) |
|---|---|---|---|
| Primary Construct | Response Inhibition (Impulsive Action) | Reward Valuation (Impulsive Choice) | Risk-Taking / Probabilistic Decision-Making |
| Core Measurement | Stop-Signal Reaction Time (SSRT) | Discount Rate (k); Indifference Point | Adjusted Average Number of Pumps |
| Key Neural Circuits | Right Inferior Frontal Gyrus, Premotor Cortex, Subthalamic Nucleus [36] | Ventromedial Prefrontal Cortex, Striatum [37] | Orbitofrontal Cortex (OFC), Dorsolateral Prefrontal Cortex (DLPFC) [38] |
| Clinical Relevance in Addiction | Assesses ability to inhibit pre-potent responses; linked to relapse [36] | Measures preference for immediate rewards; associated with addiction severity [39] | Quantifies propensity for risky decision-making; predicts real-world risk behavior [40] |
| Task Variants | Stop-Signal Anticipation Task (SSAT) measures proactive control [36] | Fixed/Titrating Procedures; Probabilistic Designs; Real/Hypothetical Rewards [41] | Modified versions with addiction-relevant cues (e.g., short videos) [38] |
Detailed Experimental Protocols
Stop-Signal Task (SST) Protocol
The SST is a gold-standard measure of response inhibition, quantifying the ability to cancel an already-initiated motor response.
- Procedure: Participants perform a choice-reaction time task (the "go" task), such as indicating the identity of a frequently presented visual stimulus (e.g., X or O) with a button press. On a minority of trials (typically 25%), a "stop-signal" (e.g., an auditory tone or visual change) occurs shortly after the go stimulus, instructing participants to inhibit their response to that trial [36].
- The Horse-Race Model: The task is governed by an independent horse-race model between a "go" process and a "stop" process. The outcome of a stop trial depends on which process finishes first [36].
- Key Dependent Variable: The primary outcome is the Stop-Signal Reaction Time (SSRT), an estimate of the latency of the stop process. Longer SSRTs indicate worse response inhibition. It is typically calculated by subtracting the mean stop-signal delay from the mean go reaction time [36].
- Advanced Applications: The Stop-Signal Anticipation Task (SSAT) introduces cues that signal the probability of an upcoming stop-signal, allowing for the dissociation between reactive control (the ability to stop in response to a stop-signal, measured by SSRT) and proactive control (the ability to anticipate and prepare for a stop, measured by slowed go reaction times in high-probability stop conditions) [36]. Research in Gambling Disorder has found that while reactive control may be intact, deficits in proactive control are linked to specific traits like lack of premeditation [36].
Delay Discounting Task (DDT) Protocol
The DDT measures the devaluation of a reward's subjective value as a function of the delay to its receipt, a phenomenon known as delay discounting.
- Procedure: Participants perform a series of binary choices between a smaller-sooner reward (e.g., $10 now) and a larger-later reward (e.g., $100 in a month). The amounts and delays are systematically varied across trials to pinpoint the individual's indifference point—the value at which both options are subjectively equivalent [41].
- Common Variations:
- Fixed Sequence Procedures: The delayed reward amount is fixed while the immediate amount is titrated up or down (Fixed Delayed Reward), or vice versa (Fixed Immediate Reward) [41].
- Titrating Procedure: An adaptive "staircase" method where the immediate reward value is adjusted based on the participant's previous choice, efficiently converging on the indifference point [41].
- Stimuli and Framing: While monetary rewards are most common, other stimuli (food, alcohol) can be used and are often discounted more steeply. Framing of time (e.g., "4 weeks" vs. "one month") can also influence discounting rates [41].
- Key Dependent Variable: The primary outcome is the discount rate (k), typically modeled using a hyperbolic function. A higher k value indicates steeper discounting and a greater preference for immediate gratification, which is a hallmark of impulsivity in addiction [37]. Research shows that adolescents, who are often more impulsive, exhibit higher discount rates (k) than adults, and this is neurally underpinned by a reduced brain response (FRN) to delayed rewards, indicating their undervaluation [37].
- Methodological Considerations: Recent research highlights that perceived reward certainty declines with longer delays, and this perception can confound discounting measurements. Explicitly stating that rewards are "100% certain" in instructions may help isolate sensitivity to delay from sensitivity to uncertainty [39].
Balloon Analogue Risk Task (BART) Protocol
The BART is a behavioral measure of risk-taking propensity in a context where outcomes are uncertain and decisions are iterative.
- Procedure: Participants see a simulated balloon on a screen. Each pump of the balloon (via a button press) accrues a temporary monetary reward. However, the balloon has an unknown explosion point. If it explodes, the money earned for that balloon is lost. At any point, the participant can stop pumping and "cash out" the accumulated earnings for that balloon, transferring it to a permanent bank [38] [40].
- Key Dependent Variable: The primary metric is the Adjusted Average Number of Pumps, calculated as the mean number of pumps only on balloons that were successfully cashed out (i.e., did not explode). This measure reflects risk-taking propensity while accounting for trials terminated by explosions [40].
- Neurobiological Insights: Modern studies using fMRI and fNIRS have linked performance on the BART to activity in prefrontal regions. For example, a 2025 fNIRS study on short video addiction found that individuals with addiction showed higher risk-taking (shorter reaction times, more explosions) and heightened activation in the right orbitofrontal cortex (OFC) and right frontopolar area (FPA) when making risky decisions under the influence of addiction-related cues [38].
- Construct Validity: The BART has demonstrated strong construct validity, effectively differentiating known groups. For instance, it has been shown to account for significant incremental variance in differentiating MDMA users from non-users, even after controlling for self-reported impulsivity and polysubstance use [40].
Comparative Data and Neurobiological Validation
The following table synthesizes key experimental findings and effect sizes from studies utilizing these tasks in clinical and research populations.
Table 2: Comparative Experimental Data and Effect Sizes
| Task & Study Context | Key Experimental Findings | Effect Size / Statistical Data |
|---|---|---|
| SST: Gambling Disorder [36] | No significant group differences in reactive control (SSRT) between individuals with Gambling Disorder and controls. Lack of premeditation was associated with worse proactive control. | Association between premeditation and proactive control observed in the clinical group. |
| DDT: Adolescent vs. Adult Impulsivity [37] | Adolescents showed higher behavioral discount rates (k) than adults. ERP data revealed a smaller FRN effect for delayed outcomes in adolescents, indicating neural devaluation. | Discount rate: t(35) = -3.339, p = 0.003; FRN interaction: F(1,35) = 6.992, p = .012, η² = 0.167. |
| BART: Short Video Addiction [38] | Individuals with short video addiction had higher risk-taking (shorter reaction times, more explosions) under addiction-relevant cues. fNIRS showed cue-induced activation in right OFC and FPA. | Significant group-by-cue interaction for risk-taking behavior and specific neural activation patterns. |
| BART: MDMA Use [40] | BART score (risk-taking) significantly predicted MDMA use status after controlling for impulsivity, sensation seeking, and other substance use. | High classification accuracy in predicting MDMA use (91%) when combined with polysubstance use and age. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for deploying these tasks in a comprehensive addiction assessment battery, highlighting the distinct neurocognitive constructs they target.
Diagram 1: Experimental Workflow for Behavioral Assessment
The Scientist's Toolkit: Essential Research Reagents
This table details key materials and solutions required for implementing these behavioral paradigms in a research setting.
Table 3: Essential Research Reagents and Materials
| Item | Function/Description | Example Application |
|---|---|---|
| fNIRS/fMRI System | Non-invasive neuroimaging to measure brain activity (e.g., oxygenation, BOLD signal) during task performance. | Measuring OFC and DLPFC activation during risk-taking on the BART [38]. |
| EEG/ERP System | Records electrophysiological brain activity with high temporal resolution; used to measure components like FRN. | Capturing the FRN component during outcome evaluation in the DDT [37]. |
| Standardized Task Software | Software platforms (e.g., Labvanced, E-Prime, PsychoPy) for precise presentation of stimuli and recording of responses. | Administering the DDT with titrating procedures and catch trials [41]. |
| Eye-Tracker | Monitors gaze and pupil dilation, providing indices of attention and cognitive load. | Can be integrated to assess attentional bias towards addiction-related cues in modified tasks. |
| Validated Clinical Scales | Self-report questionnaires (e.g., UPPS, BIS-11) to measure trait impulsivity and correlate with behavioral data. | Controlling for self-reported impulsivity when validating the BART against substance use [40]. |
| Biometric Wearables | Devices to measure physiological data (e.g., heart rate, skin conductance) in real-time or during tasks. | Monitoring stress indicators during challenging SST or BART trials in ecological momentary assessment. |
Leveraging AI and Machine Learning for Risk Prediction and Pattern Recognition
This guide compares the performance of various artificial intelligence (AI) and machine learning (ML) methodologies in the field of addiction science, with a specific focus on risk prediction and neurobiological pattern recognition. The evaluation is framed within the critical context of validating addiction assessment instruments against measurable neurobiological criteria, moving beyond traditional symptom-based diagnoses.
The table below summarizes the performance and application of primary AI/ML modalities discussed in recent research for addiction risk prediction and pattern detection.
Table 1: Comparison of AI/ML Modalities in Addiction Research
| AI Modality | Primary Application | Reported Performance | Key Advantage | Neurobiological Target/Validation |
|---|---|---|---|---|
| Clinical NLP & EHR Analysis [42] | Screening for Opioid Use Disorder (OUD) in hospitals | 47% reduction in 30-day readmissions; 1.51% vs 1.35% consultation rate | Direct impact on real-world clinical outcomes and cost savings | Pragmatic validation via reduced readmissions; analyzes clinical notes and medical history. |
| Deep Learning on EEG (DSCnet) [43] | Detecting drug and alcohol addiction from brain signals | 85.1% accuracy (drug), 84.6% accuracy (alcohol) | Direct, physiological measure of brain dysfunction; high balanced accuracy | Validated against known patient groups; captures spatiotemporal neural activity patterns. |
| Predictive ML Models [44] | Predicting opioid-related adverse events (e.g., overdose, persistent use) | AUC range: 0.68 - 0.96 across studies | Handles complex, high-dimensional clinical data for prognostic risk | Focuses on clinically tangible outcomes (overdose, readmission); often uses EHR data. |
| Morphological Cell Analysis [45] | Mapping heroin-induced astrocyte changes | 80% accuracy in identifying astrocyte sub-populations | Provides novel, sub-cellular insight into addiction mechanisms | Direct ex vivo measurement of structural changes in brain cells (astrocytes) in reward circuits. |
| Gamified Digital Assessment (BrainPAC) [34] | Assessing neurocognitive functions linked to addiction | Correlations of r=0.18-0.63 with gold-standard lab tasks | Engages key neurocognitive constructs (e.g., reward valuation, inhibition) | Tasks are based on an expert-consensus RDoC framework; directly probes addiction neurocircuitry. |
Detailed Experimental Protocols and Methodologies
AI-Driven Clinical Screening for Opioid Use Disorder
This protocol outlines the methodology for a pivotal clinical trial demonstrating real-world efficacy [42].
- Objective: To determine if an AI screener embedded in the Electronic Health Record (EHR) can effectively identify patients at risk for OUD and prompt specialist consultation, thereby reducing hospital readmissions.
- Data Source & Cohort: The study screened 51,760 adult hospitalizations at a University Hospital. The cohort was split between a provider-only phase (66%) and an AI-screener phase (34%).
- AI Model & Workflow:
- Real-Time Analysis: The AI tool analyzed all available EHR documentation in real-time, including clinical notes and medical history.
- Pattern Recognition: It identified features and patterns associated with OUD, functioning similarly to visual information processing in the brain.
- Clinical Alert: Upon identification of risk, the system issued an alert to providers when they opened the patient's chart, recommending an addiction medicine consultation and monitoring for withdrawal.
- Outcome Measures:
- Primary: Rate of addiction medicine consultations and 30-day hospital readmissions.
- Secondary: Cost-effectiveness analysis based on estimated savings from avoided readmissions.
DSCnet for EEG-Based Addiction Detection
This protocol describes the development of a specialized deep learning model for classifying addiction using electroencephalography (EEG) data [43].
- Objective: To leverage a novel neural network (DSCnet) for differentiating between healthy individuals and those with substance addictions using EEG signals.
- Data Acquisition & Preprocessing:
- Drug Dataset: Resting-state EEG was collected from 60 drug addicts and 70 healthy controls, refined to 46 addicts and 54 controls after quality screening.
- Alcohol Dataset: The public UCI alcohol addiction dataset was used.
- Standardization: Data was standardized for consistent analysis.
- Model Architecture (DSCnet):
- Hybrid Representation: An embedding layer with skip connections was used to create a low-dimensional representation of EEG data, preserving critical features.
- Multi-Angle Feature Learning: The model integrates:
- Depthwise Separable Convolution: For efficient local feature extraction.
- Directional Adaptive Feature Modulation (DAFM) Module: A novel component for global feature extraction while preserving spatiotemporal information.
- CoTAttention Module: To capture dynamic and static features.
- Validation: Model performance was evaluated using standard metrics (accuracy, precision, recall, F1-score) on both the proprietary drug dataset and the public alcohol dataset, followed by an ablation study to confirm the contribution of each architectural innovation.
Machine Learning for Astrocyte Morphology Mapping
This protocol details a quantitative approach to study heroin-induced structural changes in non-neuronal brain cells [45].
- Objective: To apply machine learning-based object recognition to track and quantify changes in astrocyte structure in response to heroin use, withdrawal, and relapse.
- Experimental Model: The study used a rodent model of heroin relapse, focusing on the nucleus accumbens, a brain region critical to reward and relapse.
- ML Analysis Pipeline:
- Training: A machine learning model was trained to recognize astrocyte cells in microscopic images, similar to how software identifies objects in photographs.
- Feature Extraction: For each identified astrocyte, the computer measured 15 structural features, including size, elongation, and branching complexity.
- Classification & Quantification: The model was applied to identify subpopulations of astrocytes and quantify morphological differences between cells from saline- and heroin-exposed subjects.
- Outcome: The model could determine the experimental origin of astrocytes with 80% accuracy and revealed that astrocytes shrink and become less malleable after heroin exposure.
For researchers aiming to replicate or build upon these studies, the following table details key reagents, instruments, and computational tools.
Table 2: Essential Research Reagents and Solutions for AI-Driven Addiction Studies
| Resource Name | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| Electronic Health Records (EHR) [42] [44] | Data Source | Provides large-scale, real-world clinical data (notes, history, outcomes) for model training and validation. | Developing clinical risk prediction models for OUD and adverse events. |
| Electroencephalography (EEG) [43] | Instrument | Records electrical activity from the scalp, providing a direct, non-invasive measure of brain function. | Capturing neural correlates of addiction for classification models like DSCnet. |
| Structured Clinical Interviews (e.g., SCID, AUDADIS) [20] | Assessment | Provides reliable, standardized diagnostic classification for labeling data and validating model predictions. | Establishing ground truth for patient cohorts in supervised learning. |
| Gamified Neurocognitive Tasks (e.g., BrainPAC) [34] | Digital Tool | Engages participants to validly assess key addiction-related neurocognitive constructs (inhibition, reward learning). | Probing specific neurocognitive domains as mechanistic biomarkers. |
| Animal Models of Relapse [45] | Preclinical Model | Allows for controlled investigation of neural mechanisms of drug seeking and relapse. | Studying cellular and molecular changes in specific brain circuits. |
| UCI Machine Learning Repository Datasets [43] | Public Data | Provides benchmark datasets (e.g., EEG) for developing and comparing new algorithms. | Training and validating models like DSCnet on standardized, public data. |
| SHAP (SHapley Additive exPlanations) [46] | Computational Tool | Explains the output of ML models, identifying which features drove a particular prediction. | Interpreting "black box" models to gain insight into predictive factors. |
The integration of AI and ML with neuroscience is fundamentally advancing the validation of addiction assessment instruments. The compared modalities each offer distinct strengths: AI-driven EHR screening provides immediate clinical utility and cost-effectiveness [42]; deep learning on EEG offers a direct, physiological classification tool [43]; and ML analysis of cellular morphology unveils entirely novel therapeutic targets by quantifying the impact of addiction at a sub-cellular level [45]. The critical trend is a move away from purely behavioral diagnostics toward a multi-faceted, neurobiologically-validated framework for understanding and assessing addiction.
The pursuit of objective, biologically grounded assessment tools is a central theme in modern addiction research. The integration of polygenic risk scores (PRS), which aggregate an individual's genetic liability for a trait, with standardized behavioral questionnaires represents a paradigm shift towards multimodal, neurobiologically validated instruments. This approach moves beyond purely phenomenological diagnoses to anchor assessment in underlying genetic architecture and neurobiological processes, offering the potential for earlier identification of at-risk individuals and more personalized intervention strategies. This guide provides a comparative analysis of these methodologies, their experimental protocols, and their synergistic application in validating addiction assessment instruments.
Comparative Analysis of Assessment Modalities
The following tables provide a quantitative comparison of the predictive performance and characteristics of different assessment approaches, from genetic to nongenetic and purely clinical models.
Table 1: Predictive Performance of Polygenic, Polyexposure, and Clinical Risk Scores for Type 2 Diabetes
| Model Type | C-Statistic (AUC) | Top 10% Risk Fold-Increase | Continuous Net Reclassification Index (NRI) for Cases | Key Components |
|---|---|---|---|---|
| Polygenic Risk Score (PGS) | 0.709 [47] | 2.00 [47] | 15.2% [47] | >6 million genetic variants [47] |
| Polyexposure Score (PXS) | 0.762 [47] | 5.90 [47] | 30.1% [47] | 12 nongenetic exposure/lifestyle factors [47] |
| Clinical Risk Score (CRS) | 0.839 [47] | 9.97 [47] | Baseline [47] | Age, sex, family history, BMI, glucose, systolic BP, HDL, triglycerides [47] |
| CRS + PGS + PXS | Improved over CRS alone [47] | Not Reported | Combined NRI for cases: 45.3% [47] | Integration of all clinical, genetic, and environmental factors [47] |
Table 2: Performance of Polygenic Risk Scores for Substance Use and Related Behaviors
| Polygenic Risk Score (PRS) For | Phenotype Category | Key Findings and Performance Metrics |
|---|---|---|
| Externalizing Factor (PRSEXT) | Substance Use, Gambling, Eating, Internet Use | Strongest association across diverse addictive phenotypes; R² = 0.10–4.72% for substance use; R² = 0.18–1.50% for gambling [48]. |
| General Addiction Risk Factor | Substance Use Disorders | Derived from genomic structural equation modeling on substance use disorders; number of variants: 11,627 [49]. |
| Alcohol Use Disorder (AUD) | Alcohol Use Disorder | PRS explains ~2.5–3.5% of variance in AUD; individuals in top 5% of PRS had greater odds of AUD and other SUD criteria [50]. |
| Risky Behaviors | General Risk Behavior | Associated with shared genetic liability across substance use disorders and behaviors related to reduced inhibitory control [50]. |
Table 3: Characteristics of the Craving Assessment Scale for Behavioral Addictions and Substance-use Disorders (CASBAS)
| Characteristic | Description |
|---|---|
| Target Construct | Acute, subjective craving across substances and addictive behaviors [51]. |
| Factor Structure | Second-order model with a general craving factor and three sub-factors: Reward Craving, Relief Craving, and Urgency [51]. |
| Validity | High convergent validity with other craving measures (r > 0.58); low correlation with divergent measures [51]. |
| Sensitivity | Able to detect state changes (decrease after neutral cue, increase after behavior-specific cue) [51]. |
| Applicability | Validated for gaming, gambling, buying-shopping, pornography use, social network use, alcohol, cannabis, and nicotine use [51]. |
Experimental Protocols for Validation
A critical step in integrating genetic and behavioral data is the rigorous application of experimental protocols to generate and validate these tools.
Protocol for Polygenic Risk Score Development and Validation
The development of a PRS is a multi-stage process that requires large-scale genetic data and independent validation.
- Discovery Genome-Wide Association Study (GWAS): Conduct a GWAS on a large, well-phenotyped cohort to identify genetic variants associated with the trait of interest (e.g., addiction). Summary statistics from this study serve as the source of variant effect sizes [50].
- PRS Construction: In an independent target sample, calculate the PRS for each individual. This is typically done using methods like PRS-CS, which uses a Bayesian regression and continuous shrinkage approach to estimate posterior effect sizes for each single nucleotide polymorphism (SNP), improving predictive power [50]. The score is a weighted sum of an individual's risk alleles.
- Statistical Validation: Evaluate the predictive performance of the PRS by testing its association with the target phenotype. Common metrics include:
- Variance Explained (R²): The proportion of phenotypic variance explained by the PRS alone [50].
- C-statistic (AUC): The area under the receiver operating characteristic curve, measuring how well the score distinguishes between cases and controls [47].
- Odds Ratios (OR): The increased odds of having the disease for individuals in the top percentiles of the PRS distribution compared to the rest of the population [47] [50].
- Incremental Predictive Value: Test whether the PRS provides predictive value beyond established clinical or demographic factors by examining improvements in model fit and reclassification metrics like the Net Reclassification Index (NRI) [47].
Protocol for Behavioral Questionnaire Validation (CASBAS)
The development of a trans-diagnostic tool like the CASBAS follows a robust psychometric validation process.
- Factor Structure Analysis: In a large sample (e.g., n=1659), confirm the proposed factor structure of the scale using confirmatory factor analysis. For the CASBAS, a second-order model with a general craving factor and three first-order factors (Reward, Relief, Urgency) was confirmed [51].
- Validity Testing:
- Convergent Validity: Correlate scores on the new scale with established measures of the same or similar constructs (e.g., other craving questionnaires). High correlations (e.g., r > 0.58) support convergent validity [51].
- Divergent Validity: Demonstrate low correlations with measures of theoretically distinct constructs to ensure the scale is not measuring unrelated traits [51].
- Sensitivity Testing (Cue-Reactivity): In a controlled laboratory setting (e.g., n=287), use an experimental within-subjects design. Expose participants to both neutral cues (e.g., thinking about brushing teeth) and behavior-specific cues (e.g., exposure to gaming-related stimuli). Measure craving with the CASBAS before and after each exposure. A valid scale will show a significant increase in scores following behavior-specific cues but not neutral cues, demonstrating sensitivity to state changes [51].
Conceptual and Methodological Workflows
The integration of genetic and behavioral data, as well as the validation of new instruments, can be visualized through the following conceptual and methodological workflows.
The Transdiagnostic Genetic Architecture of Addiction
Figure 1: Shared Genetic Liability Across Addictive Behaviors. PRS for a broad externalizing factor (PRSEXT) demonstrates a common genetic influence underlying diverse substance and behavioral addictions, linked to specific biological pathways like synaptic function [48].
Integrated Risk Assessment Workflow
Figure 2: Multimodal Risk Assessment Workflow. Combining polygenic risk, real-time behavioral craving metrics, and clinical data creates a comprehensive risk profile for enhanced prediction and personalization [47] [51] [52].
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials and tools used in the featured research, providing a resource for experimental replication and extension.
Table 4: Key Research Reagents and Resources for Integrated Genetic and Behavioral Studies
| Item | Function/Description | Example Use in Research |
|---|---|---|
| UK Biobank | A large-scale biomedical database containing genetic, lifestyle, and health information from ~500,000 U.K. participants [47]. | Served as the primary cohort for developing and testing the polyexposure score (PXS) and for validating polygenic scores for type 2 diabetes [47]. |
| ALSPAC (Avon Longitudinal Study) | A longitudinal birth cohort study with genomic data and diverse health outcomes across the lifespan [48]. | Used to examine associations between polygenic scores for externalizing and addiction-related phenotypes across different developmental stages [48]. |
| PHESANT Software | A tool for automated phenome scan analysis in the UK Biobank; processes and categorizes exposure data for analysis [47]. | Used to process 111 nongenetic exposure and lifestyle variables from the UK Biobank in the PXS study [47]. |
| PRS-CS Method | A Bayesian polygenic prediction method that uses a continuous shrinkage prior to estimate effect sizes for PRS construction [50]. | Employed to create polygenic scores for alcohol use disorders and risky behaviors, improving predictive power over traditional methods [50]. |
| Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) | A comprehensive, polydiagnostic psychiatric interview that assesses substance use and other psychiatric disorders [50]. | Used in both the FinnTwin12 and COGA studies to derive lifetime DSM-5 criteria counts for alcohol and other substance use disorders [50]. |
| Craving Induction Paradigms | Experimental tasks (e.g., imagery-based desire thinking) used to provoke transient states of craving in a laboratory setting [51]. | Used to test the sensitivity of the CASBAS questionnaire, demonstrating its ability to detect increases in craving after behavior-specific cue exposure [51]. |
The integration of polygenic risk scores with standardized behavioral questionnaires represents a powerful, multi-modal approach for the neurobiological validation of addiction assessment instruments. While PRS currently offer modest standalone predictive power, their integration with nongenetic factors, as demonstrated by the polyexposure score, significantly enhances risk stratification. Similarly, tools like the CASBAS questionnaire provide a validated, trans-diagnostic method to quantify the core experience of craving across addictive behaviors. For researchers and drug development professionals, this integrated framework offers a more biologically-grounded and mechanistically informative path forward, promising improvements in early identification, prognostic stratification, and the development of targeted interventions. Future progress is contingent on increasing the diversity of genetic studies to improve the portability of PRS across ancestral populations [53] and on the continued development of evidence-based guidelines for communicating this complex information to effect behavior change [52].
The reliable identification of substance use disorders (SUDs) is a cornerstone of both clinical practice and research in addiction medicine. Structured screening instruments provide the methodological rigor necessary for diagnostic consistency, avoiding patient misclassification that can compromise the interpretation of research findings and treatment efficacy [20]. Within the context of neurobiological validation of addiction assessment instruments, these tools provide the critical behavioral phenotypes against which neural correlates—such as changes in reward pathway signaling or prefrontal cortex function—are measured. This guide offers a comparative analysis of three prominent broad-spectrum screening tools—TAPS, ASSIST, and CRAFFT 2.1—detailing their experimental validation, psychometric properties, and applicability for researchers and drug development professionals.
The Tobacco, Alcohol, Prescription medication, and other Substance use (TAPS) tool is a two-part instrument for screening and brief assessment in primary care adults [54]. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) was developed by the World Health Organization to detect psychoactive substance use and related risks [54] [55]. The CRAFFT 2.1 (Car, Relax, Alone, Forget, Friends, Trouble) is a screening tool designed specifically for adolescents and young adults aged 12-21 [56].
Table 1: Overview of Screening Tool Characteristics
| Feature | TAPS | ASSIST | CRAFFT 2.1 |
|---|---|---|---|
| Target Age Group | Adults (18+) [54] | Adults [55] | Adolescents & Young Adults (12-21) [56] |
| Administration Format | Self-administered or clinician-interview [54] | Interviewer-administered or computer-based [55] | Self-administered [57] |
| Substances Covered | Tobacco, alcohol, illicit drugs, prescription medication [54] | Alcohol, tobacco, drugs, non-medical use of prescription medications [55] | Alcohol, marijuana (including vaping), other drugs [56] |
| Number of Items | 4 initial screener (TAPS-1), 3-4 follow-up questions per substance (TAPS-2) [54] | Not explicitly stated in results | 6 items (Part B) [58] |
| Typical Administration Time | Brief (specific time not stated) | Not explicitly stated in results | Very brief (specific time not stated) |
| Recommended Setting | Primary Care [54] [55] | Primary Care [55] | Pediatric Emergency Departments, Primary Care [58] [56] |
Performance Data and Psychometric Properties
Validation studies for these instruments typically compare their performance against a reference standard, such as the Composite International Diagnostic Interview (CIDI), to determine sensitivity (ability to correctly identify true cases) and specificity (ability to correctly identify non-cases) [54] [59].
Table 2: Comparative Psychometric Performance of Screening Tools
| Tool | Population Studied | Criterion | Optimal Cut-off | Sensitivity | Specificity | Reference |
|---|---|---|---|---|---|---|
| TAPS | 2,000 primary care patients | Problematic Use (Tobacco) | 1+ | 0.93 | Not specified | [54] |
| Problematic Use (Marijuana) | 1+ | 0.82 | Not specified | [54] | ||
| SUD (Tobacco) | 2+ | 0.74 | ≥0.79 | [54] | ||
| SUD (Marijuana) | 2+ | 0.71 | ≥0.79 | [54] | ||
| SUD (Alcohol) | 2+ | 0.70 | ≥0.79 | [54] | ||
| ASSIST | Primary care patients | High-Risk Use | Varies by substance | High for tobacco, alcohol, illicit drugs | High for tobacco, alcohol, illicit drugs | [54] |
| CRAFFT | 16 PEDs, ages 12-17 | Problematic Use/SUD (1-3 year follow-up) | ≥1 | Good (exact value not specified) | Good (exact value not specified) | [58] |
| Moderate-Severe SUD (1-year) | ≥2 | Limited sensitivity | Good specificity | [58] | ||
| 23,248 young Asian males | Alcohol/Drug Disorder | ≥1 | Good (exact value not specified) | Good (exact value not specified) | [59] |
Detailed Experimental Protocols and Validation Methodologies
TAPS Tool Validation Protocol
A large-scale validation study involved 2,000 patients across 7 primary care clinics [54]. Participants were randomly assigned to first complete either the interviewer-administered or self-administered TAPS tool in clinic waiting areas. All participants subsequently completed the Composite International Diagnostic Interview (CIDI) as a reference standard. Researchers compared TAPS and CIDI responses to determine optimal cut-off scores that maximized combined sensitivity and specificity for identifying problematic substance use and SUDs. A subset of participants (n=1,802) also provided cheek swab samples for biochemical validation of self-reported substance use [54].
CRAFFT Predictive Validity Study Protocol
Researchers conducted a secondary analysis of a study across 16 pediatric emergency departments (PEDs) affiliated with the Pediatric Emergency Care Applied Research Network (PECARN) [58]. At baseline, 4,753 participants aged 12-17 years completed an assessment battery including the CRAFFT screen and the Diagnostic Interview Schedule for Children (DISC), which served as the gold standard for DSM-5 SUD diagnoses. A subsample was then re-administered the battery at 1-, 2-, and 3-year follow-ups to examine the predictive validity of the baseline CRAFFT score for future SUDs. Receiver operating characteristic (ROC) analysis was used to investigate optimal cut points for detecting DISC classifications [58].
ASSIST Feasibility Assessment Protocol
A systematic review of feasibility studies evaluated the ASSIST among other screening tools in primary care [55]. Physician feasibility was assessed using satisfaction questionnaires and qualitative studies, primarily measuring administration time. Patient feasibility was measured using criteria including "ease of use," comprehension, and format preference. The review analyzed completion rates and compared electronic versus interviewer-administered formats to determine practical implementation barriers [55].
Diagram 1: TAPS validation workflow
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials for Validation Research
| Item | Function in Research | Example Use |
|---|---|---|
| Composite International Diagnostic Interview (CIDI) | Fully structured diagnostic interview that generates DSM and ICD diagnoses [54]. | Served as the reference standard for validating the TAPS tool against DSM criteria for SUDs [54]. |
| Diagnostic Interview Schedule for Children (DISC) | Structured, DSM-based diagnostic interview designed for children and adolescents [58]. | Used as the gold standard for SUD diagnosis in the CRAFFT predictive validity study [58]. |
| Computer-Assisted Self-Interview (CASI) | Technology platform for self-administered surveys that standardizes administration and reduces missing data [55]. | Employed in feasibility studies of the ASSIST and TAPS tools to improve disclosure rates [55]. |
| Biochemical Verification Assays | Laboratory tests (e.g., saliva, urine) that provide objective measures of recent substance use [54]. | Used cheek swab samples to validate self-reported non-use of substances in the TAPS validation study [54]. |
| Receiver Operating Characteristic (ROC) Analysis | Statistical method for visualizing and selecting optimal cut-off scores by plotting sensitivity vs. 1-specificity [58]. | Used to determine optimal CRAFFT scores (≥1 or ≥2) for identifying SUDs at different severity levels [58]. |
Analysis of Tool Selection Considerations
Target Population and Setting
- TAPS: Optimized for adult primary care populations, with validation demonstrating good acceptability among patients and staff in these settings [54] [55]. Its two-stage design efficiently narrows the screening process.
- ASSIST: Appropriate for adult populations in primary care, with evidence supporting its use for detecting high-risk substance use [54] [55].
- CRAFFT 2.1: Specifically designed for adolescents and young adults (12-21), making it the preferred choice for pediatric, school-based, or young adult populations [56]. It is recommended by the American Academy of Pediatrics [56].
Psychometric Performance and Limitations
- TAPS shows strong sensitivity for tobacco and marijuana, but has limited sensitivity for detecting SUDs involving prescription opioids, sedatives, and stimulants [54]. This necessitates caution when screening for non-tobacco/non-marijuana substances.
- CRAFFT demonstrates good concurrent and predictive validity for problematic use and SUDs in adolescent populations, though studies note limited sensitivity for identifying moderate to severe SUDs at certain time points [58]. It has been validated across diverse ethnic groups [59].
- ASSIST shows high sensitivity and specificity for high-risk use of tobacco, alcohol, and illicit drugs, though sensitivity for moderate-risk use of some substances may be lower [54].
Diagram 2: Tool selection logic
The selection of an appropriate screening tool for substance use research depends critically on the target population, clinical setting, and specific substances of interest. For adult primary care populations, the TAPS tool provides a balanced combination of brevity and comprehensive substance coverage, though researchers should note its limitations with prescription medication misuse. For adolescent populations, the CRAFFT 2.1 remains the gold standard with extensive validation across diverse settings and ethnic groups. The ASSIST offers a well-validated option for detecting high-risk substance use in adults.
From a neurobiological validation perspective, these tools provide the essential behavioral assessment framework necessary for correlating clinical phenotypes with neural substrates. Future research should address the identified sensitivity limitations, particularly for prescription drug screening, and explore the integration of these tools with emerging biomarkers to create multimodal assessment platforms that enhance both clinical and research applications in addiction medicine.
Bridging the Gap: Troubleshooting Clinical Implementation and Optimizing Feasibility
Alcohol Use Disorder (AUD) represents a significant public health challenge characterized by substantial clinical heterogeneity, wherein individuals meeting identical diagnostic criteria based on behavioral symptoms may differ markedly in etiology, prognosis, and treatment response [3]. This heterogeneity has obstructed therapeutic advancements, as evidenced by the limited application and efficacy of existing pharmacotherapies—fewer than 4% of individuals with AUD utilize FDA-approved medications despite their availability [3]. The Addictions Neuroclinical Assessment (ANA) framework proposes that this clinical variation stems from distinct neurobiological dysfunctions manifesting in three primary domains: Executive Function, Incentive Salience, and Negative Emotionality [3]. These domains correspond to different phases in the addiction cycle and provide a neuroscientifically-grounded foundation for subtyping AUD that transcends the limitations of purely behavioral diagnostics.
Emerging evidence substantiates that these neurocognitive domains can be quantified through standardized methodologies, enabling objective stratification of what were previously considered homogenous clinical populations. Advances in multimodal assessment integrating neuroimaging, cognitive performance measures, and molecular biomarkers now permit researchers to delineate AUD subtypes with distinct neurocognitive profiles, pathological trajectories, and treatment needs [3] [60]. This paradigm shift toward mechanistically-informed subtyping mirrors approaches in other medical specialties, where diagnostic classification based on pathophysiology rather than clinical presentation alone has dramatically improved treatment outcomes [3]. This review systematically compares contemporary methodological approaches for AUD subtyping, evaluates their supporting empirical evidence, and provides a structured framework for implementing neurocognitive profiling in both research and clinical domains.
Neurocognitive Domains for AUD Subtyping: Theoretical Framework and Assessment
The ANA framework identifies three core neurofunctional domains that capture essential dimensions of addiction pathology and provide a structured approach to AUD subtyping. Each domain can be quantified through specific assessment protocols, creating a multidimensional profile for individual patients or research participants.
Table 1: Core Neurocognitive Domains for AUD Subtyping
| Domain | Neurocircuitry | Behavioral Manifestation | Primary Assessment Methods |
|---|---|---|---|
| Executive Function | Prefrontal cortex, anterior cingulate, dorsolateral striatum | Impaired response inhibition, cognitive flexibility deficits, poor decision-making | Trail Making Test (TMT) Part B, Grooved Pegboard Test, fMRI during cognitive tasks |
| Incentive Salience | Ventral tegmental area, nucleus accumbens, amygdala | Enhanced drug cue reactivity, craving, motivation for alcohol | fMRI cue-reactivity tasks, behavioral approach tasks, self-reported craving measures |
| Negative Emotionality | Amygdala, insula, bed nucleus of stria terminalis | Withdrawal-induced negative affect, anxiety, irritability, emotional dysregulation | Stress-induced craving paradigms, physiological stress measures, mood inventories |
Executive Function Domain
The executive function domain encompasses cognitive processes necessary for planning, impulse control, and flexible adaptation to changing environmental contingencies. Deficits in this domain reflect impaired prefrontal cortex regulation over subcortical reward and emotional structures [3]. In AUD populations, executive dysfunction manifests behaviorally as impaired performance on tasks requiring cognitive flexibility, such as the Trail Making Test (TMT), where individuals with AUD demonstrate significantly prolonged completion times for Part B compared to healthy controls [60]. The Grooved Pegboard Test further quantifies visual-motor coordination and fine motor control, with studies demonstrating that individuals with AUD risk show subtle performance deficits even before overt cognitive symptoms emerge [60]. Neuroimaging correlates include reduced prefrontal cortex activation during cognitive tasks and decreased integrity of white matter tracts connecting frontal regions with other brain areas.
Incentive Salience Domain
The incentive salience domain captures the pathological attribution of motivational value to alcohol-related cues at the expense of natural rewards, driven primarily by dysregulation in mesolimbic dopamine pathways [61]. This domain reflects the progressive neuroadaptation wherein alcohol-associated stimuli trigger compulsive motivation to drink, independent of conscious pleasure anticipation. Assessment methodologies include functional magnetic resonance imaging (fMRI) during exposure to alcohol-related cues, measuring activation in reward-processing regions like the nucleus accumbens and orbitofrontal cortex [61]. Behavioral measures include approach bias tasks that quantify automatic action tendencies toward alcohol stimuli. Neurochemical correlates involve dopaminergic signaling abnormalities, with evidence indicating that dopamine receptor mRNA expression levels in peripheral blood lymphocytes may serve as accessible biomarkers reflecting central nervous system changes [62].
Negative Emotionality Domain
The negative emotionality domain encompasses the negative reinforcement processes that maintain drinking through alleviation of withdrawal-induced dysphoria and stress sensitivity. This domain involves extended amygdala circuitry and is characterized by hyperarousal, irritability, and emotional dysregulation during abstinence [3]. Assessment approaches include measuring hypothalamic-pituitary-adrenal axis responses to stress provocation, fMRI during negative emotional processing, and self-report measures of negative affect. Neurobiological substrates include altered glutamatergic and corticotropin-releasing factor signaling, with evidence that the glutamate receptor GiuN3B subunit mRNA levels show stable elevation across different stages of heroin addiction, suggesting potential similar applications in AUD [62].
Diagram 1: Neurocognitive Domain Framework for AUD Subtyping. This diagram illustrates the three primary neurocognitive domains proposed for AUD subtyping, their associated neural substrates, and corresponding assessment methodologies. Dashed lines represent interactive connections between neural systems.
Comparative Methodological Approaches for AUD Subtyping
Multiple methodological approaches have emerged to operationalize and quantify the neurocognitive domains central to AUD subtyping. Each approach offers distinct advantages, limitations, and empirical support, necessitating careful consideration of their respective applications in research and clinical contexts.
Table 2: Methodological Approaches for AUD Subtyping
| Methodology | Domains Assessed | Key Metrics | Empirical Support | Implementation Considerations |
|---|---|---|---|---|
| Multimodal Deep Learning | Executive Function, Incentive Salience | T1-weighted MRI features, neuropsychological test scores | 79.88% classification accuracy in firefighter cohort [60] | Requires specialized computational expertise; high infrastructure needs |
| Neuropsychological Assessment | Primarily Executive Function | Trail Making Test completion time, Grooved Pegboard performance | Differentiated AUD risk in occupational cohort [60] | Accessible; standardized administration required |
| Structural MRI Morphometry | Cross-domain correlates | Cortical thickness, fractal dimension, sulcal depth | Associated with anxiety/depression in substance users [63] | Reveals persistent neural alterations; limited temporal resolution |
| Peripheral Biomarkers | Incentive Salience, Negative Emotionality | Dopamine receptor mRNA expression, glutamate receptor subunits | Differential expression in addiction stages [62] | Minimally invasive; peripheral-central correspondence uncertain |
Multimodal Deep Learning Framework
The multimodal deep learning approach represents a technologically advanced methodology for AUD subtyping that integrates neuroimaging data with clinical and cognitive measures. In a recent study targeting firefighters—a population with elevated AUD risk—researchers developed a deep learning framework that combined T1-weighted structural MRI with standardized neuropsychological assessments including the Grooved Pegboard Test and Trail Making Test [60]. This integrated model achieved a classification accuracy of 79.88% for identifying individuals with AUD risk, significantly outperforming models using either clinical (AUDIT scores) or neuroimaging data alone [60]. The methodological workflow involved systematic preprocessing of T1-weighted MRI data using FMRIB Software Library (FSL), including spatial normalization to MNI152 standard space and resampling to 2×2×2mm³ voxel resolution [60]. Critical implementation steps included employing a high-precision brain extraction tool (HD-BET) to isolate brain tissue from non-brain elements and applying data augmentation techniques (random affine transformations, color jitter) to enhance model generalizability [60].
Diagram 2: Multimodal Deep Learning Workflow for AUD Subtyping. This diagram outlines the integrated analytical pipeline for combining neuroimaging and neuropsychological data to classify AUD risk and subtype categories.
Structural Neuroimaging Approaches
Structural MRI morphometry provides valuable metrics for elucidating neuroanatomical correlates of AUD heterogeneity. Research comparing different substance use disorders has revealed distinct patterns of brain alterations associated with various addictive agents, suggesting analogous applications for AUD subtyping [63]. Quantitative morphometric analysis typically involves measuring four key parameters: cortical thickness (CT), fractal dimension (FD), gyrification index (GI), and sulcal depth (SD) across multiple brain regions [63]. In studies of heroin and methamphetamine addiction, researchers have employed Jensen-Shannon divergence (JSD) to construct morphological brain networks that reveal disrupted topological organization—specifically, heroin addiction was associated with global network efficiency reductions, while methamphetamine addiction showed more localized nodal efficiency decreases [63]. These differential patterns illustrate how structural network analysis might distinguish AUD subtypes with predominantly executive dysfunction versus incentive salience pathology.
Peripheral Biomarker Strategies
Peripheral blood biomarkers offer a minimally invasive approach to AUD subtyping that can be serially assessed to track dynamic changes across addiction stages. The fundamental premise is that molecular alterations in the central nervous system may be reflected in peripheral tissues, particularly blood lymphocytes [62]. Empirical evidence supports this approach, with studies demonstrating that dopamine receptor mRNA levels show differential expression patterns across stages of heroin and alcohol addiction [62]. Specifically, dopamine D4 receptor mRNA levels exhibit opposite directional changes during active dependence versus withdrawal phases, highlighting their potential for distinguishing AUD subtypes characterized by prominent incentive salience dysregulation [62]. Similarly, glutamate receptor subunits such as GiuN3B show stable elevation across heroin addiction stages and normalize with methadone treatment, suggesting applications for monitoring treatment response in specific AUD subtypes [62]. Standardized protocols for this approach require careful sample collection, RNA extraction, and quantitative real-time PCR analysis with appropriate normalization to reference genes.
Research Reagent Solutions for AUD Subtyping Protocols
Implementation of the methodological approaches described requires specific research reagents and tools designed to quantify neurocognitive domains with precision and reliability. The following table summarizes essential solutions for establishing AUD subtyping protocols.
Table 3: Essential Research Reagents for AUD Subtyping Studies
| Reagent/Tool | Primary Application | Specific Function | Example Implementation |
|---|---|---|---|
| FSL (FMRIB Software Library) | Structural MRI preprocessing | Spatial normalization, tissue segmentation, feature extraction | MNI152 spatial normalization of T1-weighted images [60] |
| HD-BET (Brain Extraction Tool) | Neuroimage preprocessing | Automated skull stripping of MRI data | Isolation of brain tissue from non-brain elements [60] |
| LCModel | Magnetic resonance spectroscopy analysis | Quantification of neurometabolite concentrations | Analysis of NAA/Cr, Cho/Cr, Glx/Cr ratios [64] |
| qPCR Assays | Peripheral biomarker analysis | Quantification of receptor mRNA expression | Dopamine receptor mRNA levels in lymphocytes [62] |
| Grooved Pegboard Test | Neuropsychological assessment | Fine motor coordination, visual-motor integration | Dominant and non-dominant hand completion time [60] |
| Trail Making Test | Executive function assessment | Cognitive flexibility, processing speed | Part A and B completion time difference [60] |
Integrated Subtyping Framework and Clinical Translation
The ultimate utility of AUD subtyping lies in its ability to inform targeted intervention strategies that address the specific neurocognitive dysfunctions underlying individual clinical presentations. Integration of the assessment methodologies described enables researchers and clinicians to construct multidimensional profiles that capture the heterogeneity of AUD more comprehensively than traditional diagnostic approaches.
Future directions should emphasize the development of standardized assessment batteries that efficiently capture all three neurocognitive domains with minimal participant burden. The ANA framework provides a conceptual foundation for such batteries, which might incorporate brief neuropsychological tests, targeted neuroimaging protocols, and strategically selected peripheral biomarkers [3]. Validation studies should establish test-retest reliability, sensitivity to change, and predictive validity for treatment outcomes across identified subtypes. Particularly promising is the integration of these subtyping approaches with pharmacogenomics to identify biological predictors of treatment response specific to different AUD subtypes.
Translation of these research protocols into clinical practice will require development of simplified algorithms that maintain neurobiological fidelity while accommodating practical constraints of clinical settings. The multimethod approaches compared in this review provide an empirical foundation for such algorithms, with the potential to transform AUD from a behaviorally-defined disorder into a neurobiologically-characterized condition with mechanistically-guided treatment pathways.
The integration of effective screening and brief intervention (SBI) into primary care represents a critical public health strategy for the early identification and management of substance use and behavioral health disorders. The "Make Every Contact Count" (MECC) paradigm emphasizes leveraging every patient-healthcare professional interaction as an opportunity for health promotion and behavior change [65]. However, significant barriers impede implementation, including time constraints, limited provider training, and concerns about workflow disruption [66]. Consequently, developing feasible, acceptable, and psychometrically sound brief screening instruments is paramount for overcoming these implementation challenges.
This review objectively compares the performance of contemporary brief screening tools within the context of advancing neurobiological validation research. As the field moves toward a more biologically-grounded understanding of addiction, assessing how these practical clinical tools perform against emerging neurobiological markers becomes increasingly relevant for researchers and drug development professionals seeking to bridge the gap between mechanistic understanding and clinical application.
Performance Comparison of Brief Screening Instruments
Broad-Spectrum Substance Use Screening Tools
Broad-spectrum screening tools are designed to evaluate multiple substance use domains simultaneously, making them highly efficient for primary care settings where time is limited. The performance characteristics of several key instruments are summarized in Table 1.
Table 1: Performance Characteristics of Broad-Spectrum Substance Use Screening Tools
| Tool Name | Target Population | Administration Time | Substances Covered | Key Performance Features |
|---|---|---|---|---|
| TAPS (Tobacco, Alcohol, Prescription Medication & Other Substances) | Adults | 5-10 minutes | Tobacco, alcohol, prescription medication, other substances | Validated for adult populations; integrates with clinical workflows; available in digital formats [11] |
| CRAFFT (Car, Relax, Alone, Forget, Friends, Trouble) | Adolescents | <5 minutes | Alcohol, marijuana, other drugs | 6-item rapid assessment; high sensitivity for adolescent substance use disorders [11] |
| BSTAD (Brief Screener for Tobacco, Alcohol, and other Drugs) | Adolescents | <5 minutes | Tobacco, alcohol, marijuana | High diagnostic accuracy (AUC 0.89-1.00); systematic risk stratification [11] |
| S2BI (Screening to Brief Intervention) | Adolescents | <5 minutes | Tobacco, alcohol, marijuana, other drugs | Categorizes use frequency (never, once or twice, monthly, weekly); guides intervention intensity [11] |
Substance-Specific and Behavioral Addiction Screening Tools
For targeted assessment or when specific substance use is suspected, substance-specific instruments provide detailed evaluation. Similarly, validated tools for behavioral addictions like gambling have been developed.
Table 2: Substance-Specific and Behavioral Addiction Screening Instruments
| Tool Name | Target Condition | Number of Items | Administration Time | Diagnostic Accuracy |
|---|---|---|---|---|
| AUDIT-C | Alcohol Use Disorders | 3 | 2-3 minutes | Integrated into the CliniCAP mSBI; demonstrates high feasibility in primary care [65] |
| BPGS-2 (Brief Problem Gambling Screen) | Problem and At-Risk Gambling | 2 | <1 minute | Satisfactory diagnostic accuracy for both problem and at-risk gambling [67] |
| NODS-CLiP | Problem and At-Risk Gambling | 3 | <2 minutes | Large volume of diagnostic data; satisfactory accuracy [67] |
| PGSI-SF (Problem Gambling Severity Index-Short Form) | Problem and At-Risk Gambling | 5 | 2-3 minutes | Meets criteria for satisfactory diagnostic accuracy [67] |
| Lie/Bet Questionnaire | Problem Gambling | 2 | <1 minute | Promising ultra-brief option [67] |
Implementation Feasibility and Acceptability Data
Recent studies provide quantitative data on the real-world implementation of mobile-assisted screening tools in healthcare settings. The CliniCAP mSBI (mobile Screening and Brief Intervention) demonstrated strong feasibility metrics during consultations for chronic conditions [65]:
- Completion Rate: 92% of patients could complete the screening with minimal assistance
- Time Efficiency: Average administration time of 20 minutes for the entire mSBI process
- Acceptability: Majority of patients rated the personalized feedback as comprehensible and useful
- Impact: Nearly half (48%) of participants reported intention to change behavior post-intervention
Critical implementation factors identified include the importance of medical doctor involvement for patient referral, adaptation for patients with low health literacy, and the system's ability to send feedback to both patients and doctors [65].
Experimental Protocols for Tool Validation
Protocol for Feasibility Assessment in Clinical Settings
The validation of screening tools requires rigorous assessment of their practicality in real-world clinical environments. The following protocol, adapted from recent studies, provides a framework for evaluating feasibility and acceptability.
Objective: To assess the feasibility and acceptability of brief screening instruments during routine primary care visits.
Population: Patients presenting for routine care, stratified by age, gender, and clinical presentation to ensure diverse representation.
Procedure:
- Recruitment: Research counselors approach patients in waiting rooms or through provider referral.
- Screening Administration: Participants complete the brief screening tool via tablet-based application with local storage to function without internet connection.
- Brief Intervention: Trained counselors provide structured feedback using the FRAMES (Feedback, Responsibility, Advice, Menu of options, Empathy, and Self-efficacy) blueprint based on motivational interviewing principles.
- Data Collection: Research staff record administration time, need for assistance (rated on a 4-point scale from "important for all questions" to "no assistance needed"), and any implementation barriers.
- Acceptability Assessment: Participants complete a post-intervention questionnaire adapted from the Technology Acceptance Model, rating statements on comprehensibility, usefulness, and behavioral intention on Likert-type scales.
Outcome Measures:
- Feasibility: Completion rates, administration time, level of assistance required
- Acceptability: Patient ratings of comprehensibility, usefulness, and relevance
- Clinical Impact: Proportion of patients expressing intention to change behavior
This protocol successfully demonstrated that 92% of patients could complete screening with minimal assistance, with an average completion time of 20 minutes for the entire process [65].
Protocol for Diagnostic Accuracy Validation
Establishing the sensitivity and specificity of brief screening tools against gold-standard diagnostic interviews is essential for their clinical implementation.
Objective: To determine the diagnostic accuracy of brief screening instruments against structured clinical interviews.
Design: Cross-sectional comparison of screening tools to criterion-standard evaluation.
Population: Community-based samples or clinical populations, depending on the target setting for implementation.
Procedure:
- Sampling: Participants are recruited through multi-stage sampling (stratified cluster simple random) to ensure representation.
- Screening Administration: All participants complete the brief screening instrument under investigation.
- Criterion Standard Assessment: Trained clinicians administer validated structured diagnostic interviews (e.g., MINI International Neuropsychiatric Interview) blinded to screening results.
- Data Analysis: Calculate sensitivity, specificity, likelihood ratios, and diagnostic odds ratios with confidence intervals.
Statistical Analysis:
- Receiver Operating Characteristic (ROC) curves are plotted for the screening instruments
- Area Under the Curve (AUC) values are calculated, with values ≥0.80 generally considered excellent discrimination
- Cronbach's alpha and intraclass correlation coefficients (ICC) assess reliability
This methodology was successfully employed in validating the 30-item Addiction Potential Questionnaire for Iranian children, demonstrating strong psychometric properties with four factors explaining 40% of total extracted variance and excellent reliability metrics [68].
Neurobiological Validation Framework
Neurobiological Correlates of Addiction and Assessment Implications
Advancements in understanding the neurobiology of addiction provide a framework for validating screening tools against objective biological markers. The addiction cycle encompasses three key stages, each with distinct neural substrates, that can inform assessment strategies.
Figure 1: Neurobiological Framework for Addiction Assessment. This diagram illustrates the three-stage addiction cycle and corresponding neural systems that can be measured through objective markers to validate screening tools.
Research demonstrates that patients with alcohol use disorder (AUD) show altered neurobiological markers even after extended treatment. A 2-year longitudinal study found that startle reflex response and salivary cortisol levels before and after exposure to alcohol-related stimuli did not normalize despite treatment, confirming the chronicity of moderate-severe AUD and the persistent risk of relapse [69]. These findings underscore the value of objective neurobiological measures in validating the predictive utility of clinical screening tools.
Experimental Protocol for Neurobiological Validation
Objective: To evaluate the relationship between brief screening tool results and objective neurobiological markers of addiction vulnerability.
Population: Patients with substance use disorders and matched healthy controls.
Procedure:
- Clinical Assessment: Participants complete brief screening instruments (e.g., AUDIT-C, BPGS-2).
- Startle Reflex Modulation: Eyeblink response magnitude is measured when participants view substance-related cues versus neutral or affective stimuli.
- Cortisol Reactivity: Salivary cortisol is collected before and after exposure to substance-related visual stimuli.
- Negative Emotionality Assessment: Standardized scales for anxiety, depression, and impulsivity are administered.
Outcome Measures:
- Correlation between screening scores and magnitude of startle reflex modulation
- Association between screening results and cortisol reactivity patterns
- Relationship between screening outcomes and negative emotionality scores
This approach has revealed that patients with AUD demonstrate significantly different startle reflex modulation when exposed to alcohol-related cues compared to controls, indicating the appetitive salience of these cues persists despite treatment [69]. Such protocols provide biological validation for screening tools aimed at identifying individuals with heightened addiction vulnerability.
Implementation Considerations in Primary Care
Barriers and Facilitators to Screening Implementation
Understanding implementation barriers is crucial for the successful integration of brief screeners into primary care workflows. Research with healthcare providers has identified key factors influencing adoption.
Table 3: Barriers and Facilitators to Screening Implementation in Primary Care
| Domain | Barriers | Facilitators |
|---|---|---|
| Outer Setting | Lack of reimbursement codes activation by Medicaid; Insufficient business case for payors [66] | Affordable Care Act mandates coverage; Potential healthcare cost savings from prevention [66] |
| Inner Setting | Burden on staff time and costs; Lack of training and referral networks [66] | Behavioral specialists embedded in primary care; Integrated electronic health records [11] |
| Provider Characteristics | Concerns about high false-positive rates; Fear of alienating patients [66] | Brief, psychometrically strong tools available; Evidence that patients and parents support screening [66] |
Survey research indicates that both pediatricians and family therapists recognize the widespread need for screening and brief intervention but cite lack of reimbursement, training, and inter-professional referral pathways as significant barriers [66]. Co-locating behavioral specialists in pediatric clinics has been proposed as a strategy to address many of these implementation challenges.
Workflow for Screening and Brief Intervention Implementation
Implementing screening successfully requires integration into existing clinical workflows with minimal disruption. The following diagram illustrates an optimized pathway for primary care settings.
Figure 2: Primary Care Screening and Brief Intervention Workflow. This diagram outlines a streamlined pathway for implementing brief screeners in primary care settings, from administration to appropriate intervention based on risk level.
The Scientist's Toolkit: Essential Research Reagents and Materials
To conduct rigorous validation studies of brief screening instruments, researchers require specific tools and assessment materials. The following table details key solutions for comprehensive validation protocols.
Table 4: Essential Research Reagents and Materials for Validation Studies
| Research Tool | Function | Application in Validation Studies |
|---|---|---|
| Tablet-Based Assessment Platform | Administration of screening tools with local storage | Enables standardized administration without internet connection; accommodates low health literacy through simplified language [65] |
| Startle Reflex Measurement System | Quantification of eyeblink response to substance-related cues | Provides objective measure of appetitive response to drug cues; correlates with addiction severity [69] |
| Salivary Cortisol Collection Kit | Non-invasive assessment of HPA axis reactivity | Measures stress system activation before/after exposure to substance cues; biomarker of stress reactivity [69] |
| Structured Clinical Interviews (e.g., MINI) | Gold-standard diagnostic assessment | Establishes criterion validity for brief screens against comprehensive diagnostic evaluation [70] |
| Negative Emotionality Scales | Assessment of anxiety, depression, impulsivity | Measures comorbid psychological dimensions that maintain addiction through negative reinforcement [69] |
| Technology Acceptance Questionnaire | Evaluation of user perceptions | Assesses patient comprehensibility, usefulness, and satisfaction with screening tools [65] |
Brief screening instruments demonstrate strong potential for overcoming implementation barriers in primary care settings, with recent studies confirming their feasibility, acceptability, and diagnostic accuracy. The integration of neurobiological validation approaches strengthens the scientific foundation of these practical tools, creating important bridges between biological mechanisms and clinical application. For drug development professionals and researchers, these advances offer opportunities to develop increasingly refined assessment tools that are simultaneously practical for clinical implementation and grounded in the neurobiological underpinnings of addiction. Future research directions should include further validation of brief screens against persistent neurobiological markers, development of integrated digital assessment platforms, and implementation studies to optimize workflow integration in diverse primary care settings.
Ensuring Data Quality in Digital and Self-Administered Formats
The integration of digital health technologies into substance use disorder (SUD) research represents a paradigm shift in data collection methodologies. This transition from traditional clinician-administered assessments to digital and self-administered formats offers unprecedented opportunities for scaling data collection while introducing significant challenges for ensuring data quality. The neurobiological framework of addiction, conceptualized as a repeating cycle of intoxication/binge, withdrawal/negative affect, and preoccupation/anticipation stages, provides a critical lens through which to evaluate the validity of these assessment tools [10]. As the field moves toward multidomain models that integrate psychological, social, and biological data, ensuring the quality of self-administered digital assessments becomes increasingly crucial for advancing our understanding of addictive disorders [71].
This guide objectively compares the performance of various digital assessment modalities against traditional methods, with particular emphasis on their application within neurobiologically-informed frameworks such as the Addictions Neuroclinical Assessment (ANA) [10] [30]. By examining experimental data across key data quality metrics including equivalence, completeness, and respondent engagement, we provide researchers with evidence-based recommendations for implementing digital assessments that maintain scientific rigor while leveraging technological advantages.
Comparative Performance of Assessment Modalities
Quantitative Comparison of Data Quality Metrics
Table 1: Comparative performance of digital versus traditional assessment formats across data quality metrics
| Assessment Format | Data Equivalence | Data Completeness | Completion Time | Break-off Rates | Respondent Enjoyment |
|---|---|---|---|---|---|
| Smartphone/Tablet Apps | No significant differences in mean scores or correlation coefficients [72] | Superior to paper formats; comparable to SMS [72] | Mixed results; potentially faster than paper/SMS [72] | Not reported in studies | Not specifically reported |
| Text-Based Digital | Established measurement invariance with paper formats [73] | High, with structured data capture | Baseline for comparison | No significant differences from video format [73] | Lower than video formats [73] |
| Video-Administered | Strict measurement invariance with text-based formats [73] | Comparable to text-based formats [73] | Male interviewer: faster; Female: comparable [73] | No significant differences from text-based [73] | Significantly higher than text-based [73] |
| Paper-Based | Reference standard for equivalence testing | Lower than digital formats [72] | Generally slower than digital alternatives [72] | Not systematically compared | Not specifically reported |
Neurobiological Alignment of Digital Assessment Tools
Table 2: Mapping of digital assessment tools to neurobiological addiction frameworks
| Assessment Tool | Target Population | Neurobiological Domain | Digital Implementation | Validation Evidence |
|---|---|---|---|---|
| Addictions Neuroclinical Assessment (ANA) | Adults with SUD | Incentive salience, negative emotionality, executive function [10] [30] | 10-hour comprehensive digital battery [30] | Links to cycle of addiction model; requires validation [30] |
| TAPS Tool | Adults | Broad-spectrum substance use [11] | Integrated with EHR systems [11] | Validated for adult populations [11] |
| CRAFFT 2.1 | Adolescents (12-21) | Substance use risk and behaviors [13] | Self-administered digital questionnaire [13] | High sensitivity/specificity for adolescent SUD [13] |
| BSTAD | Adolescents | Substance use patterns [11] | Brief digital screening | High diagnostic accuracy (AUC 0.89-1) [11] |
| ASPIRE Model | Patients with SUD | Six neuroscience-based risk categories [30] | Computer adaptive tests with skip patterns [30] | Incorporates PROMIS measures; reduces burden [30] |
Experimental Protocols for Validation Studies
Protocol for Mode Equivalence Studies
Objective: To determine whether digital administration modes produce equivalent results to traditional paper-based assessments while maintaining psychometric properties and measurement invariance [72] [73].
Methodology:
- Study Design: Randomized controlled trials (RCTs) or crossover designs comparing digital app delivery with paper, laptop, SMS, or other alternative delivery modes [72]
- Participants: Recruitment of both healthy volunteers and individuals with clinical diagnoses, with sample sizes sufficient for statistical power (e.g., N=2272 in included studies) [72]
- Procedure:
- Random assignment to assessment modalities
- Administration of identical survey content across modes
- Controlled for potential confounders (location, time of day, technology type, available assistance)
- Implementation in both controlled (research/clinical) and uncontrolled (home) settings [72]
- Measures:
- Data equivalence: Comparison of mean overall scores and correlation coefficients between modalities
- Data completeness: Percentage of completed items and overall survey completion rates
- Temporal metrics: Time taken for completion measured objectively
- Acceptability: Multi-dimensional assessment including preference, ease of use, willingness to reuse, satisfaction [72]
Analysis:
- Establishment of measurement invariance using confirmatory factor analysis
- Comparison of reliability coefficients (Cronbach's alpha) between modalities
- Evaluation of criterion validity against established clinical standards
- Assessment of completion rates and break-off patterns across modalities [73]
Protocol for Digital Phenotyping Validation
Objective: To validate machine learning-enhanced screening tools that integrate genetic and behavioral data for SUD risk prediction [13].
Methodology:
- Data Collection:
- Behavioral Assessment: Administration of CRAFFT 2.1 questionnaire with Part A (recent use) and Part B (risk behaviors) scoring [13]
- Genetic Sampling: Collection of saliva or blood samples for DNA analysis
- SNP Analysis: Identification of specific single nucleotide polymorphisms associated with SUD risk through genome-wide association studies [13]
- Polygenic Risk Scoring: Calculation of weighted PRS aggregating multiple SNP effects [13]
- Participant Sources:
- Utilization of longitudinal cohorts (e.g., Adolescent Brain Cognitive Development Study, National Longitudinal Study of Adolescent to Adult Health) [13]
- Tracking of participants from childhood to adulthood with comprehensive behavioral, genetic, and environmental measures
- Machine Learning Integration:
- Application of Random Forest algorithms to identify complex patterns among genetic and behavioral data
- Cross-validation techniques to ensure model generalizability and robustness
- Development of comprehensive risk score prediction models integrating genetic predispositions, behavioral indicators, and demographic variables [13]
Analysis:
- Evaluation of predictive accuracy through receiver operating characteristic curves
- Assessment of sensitivity and specificity enhancements compared to traditional methods
- Validation of clinical utility in identifying at-risk individuals for targeted interventions
Visualization of Methodological Frameworks
Digital Validation Neurobiological Alignment
Multidomain Quality Assessment Workflow
Essential Research Reagent Solutions
Table 3: Key research reagents and materials for digital assessment validation
| Research Reagent | Function | Application in Validation | Implementation Considerations |
|---|---|---|---|
| PROMIS Measures | Patient-reported outcomes with psychometric validation [30] | Computer adaptive tests with skip patterns to reduce burden [30] | Non-proprietary, open-source administration |
| PhenX Toolkit | Standardized data collection protocols [30] | Core measures for substance abuse and addiction research [30] | Ensures cross-study comparability |
| Electronic Health Record Systems | Integration with clinical data infrastructure [11] | Real-time data capture and provider alerts [11] | Requires interoperability standards |
| Random Forest Algorithms | Machine learning for pattern recognition [13] | Identifying complex genetic-behavioral interactions [13] | Cross-validation for generalizability |
| Digital Media Overuse Scale (dMOS) | Evaluates online behavior categories [11] | Assessment of technology-related behavioral disorders | Specific to digital addiction patterns |
| CRAFFT 2.1 | Adolescent substance use screening [13] | Behavioral component in integrated risk assessment | Self-administered digital formatting |
Discussion and Research Implications
The validation of digital and self-administered assessment formats requires multidimensional approaches that address both methodological and neurobiological considerations. Current evidence suggests that well-designed digital tools can achieve measurement invariance with traditional formats while offering advantages in data completeness and participant engagement [72] [73]. The integration of these tools with neurobiological frameworks such as the ANA provides a pathway for more precise assessment of addiction-related domains [10] [30].
Future research directions should prioritize the development of brief yet comprehensive digital assessments that minimize participant burden while maximizing clinical utility [30]. Additionally, further investigation is needed into how digital phenotyping approaches that integrate behavioral, genetic, and neurobiological data can enhance early identification of SUD risk [13]. As digital technologies continue to evolve, maintaining rigorous validation standards will be essential for ensuring that technological advances translate to improved assessment and treatment of addictive disorders.
The emerging evidence supporting video-administered questionnaires and AI-driven tools points toward increasingly sophisticated digital assessment platforms that can adapt to individual respondent characteristics while maintaining data quality standards [11] [73]. By grounding these technological advances in neurobiological models of addiction, researchers can develop assessment tools that not only capture behavioral manifestations but also align with the underlying biological mechanisms of addictive disorders.
The co-occurrence of substance use disorders (SUDs) and psychiatric conditions, often termed "comorbidity" or "dual diagnosis," represents one of the most significant challenges in both addiction research and clinical practice. This convergence of conditions is not the exception but the rule; recent studies indicate that approximately 26% of adults with psychiatric disorders and 37% of those with SUDs have a dual diagnosis [74]. The intricate interplay between addictive and psychiatric disorders complicates diagnosis, treatment selection, and prognosis, ultimately transforming the landscape of clinical practice and demanding a comprehensive grasp of the underlying neurobiological mechanisms [74]. The management of people who inject drugs (PWID) is particularly compounded by psychiatric comorbidities, leading to frequent relapses and poor treatment outcomes, with one study finding an 88.1% prevalence of psychiatric comorbidities among opioid injectors [75].
The diagnostic process is fraught with complexity due to overlapping symptomatology. For instance, stimulant use disorders can manifest symptoms of psychosis nearly identical to those of schizophrenia, creating a perplexing "chicken-or-egg" dilemma for clinicians [74]. This diagnostic challenge is further compounded by the fact that individuals with dual diagnoses often present with more severe symptoms, greater functional impairment, and increased service utilization compared to those with either condition alone [74]. Understanding the neurobiological underpinnings of these comorbid conditions is therefore not merely an academic exercise but an essential step toward developing targeted, effective interventions for a population that has proven difficult to treat successfully.
Neurobiological Frameworks for Deconstructing Comorbidity
The Addictions Neuroclinical Assessment (ANA) Framework
To address the pronounced heterogeneity within addictive disorders, researchers have developed the Addictions Neuroclinical Assessment (ANA), a neurobiologically-informed framework designed to understand the etiology and heterogeneity of disorders like Alcohol Use Disorder (AUD) [3] [4]. This framework shifts the focus from traditional, symptom-based diagnoses to a multidimensional approach centered on three core neurofunctional domains derived from the addiction cycle:
- Executive Function (EF): Comprises cognitive functions related to inhibitory control, decision making, and planning (preoccupation-anticipation stage) [4].
- Incentive Salience (IS): Encompasses processes involved in reward, motivational salience, and habit formation (binge-intoxication stage) [4].
- Negative Emotionality (NE): Captures negative affective states due to withdrawal and long-term drug use (withdrawal-negative affect stage) [4].
A recent study implementing the ANA battery through a combination of neurocognitive behavioral tasks and self-report assessments revealed that these domains are themselves multidimensional [4]. Factor analysis identified two factors for Incentive Salience (alcohol motivation and alcohol insensitivity), three for Negative Emotionality (internalizing, externalizing, and psychological strength), and five for Executive Function (inhibitory control, working memory, rumination, interoception, and impulsivity) [4]. These factors showed varying degrees of cross-correlation, with alcohol motivation, internalizing, and impulsivity exhibiting the strongest interrelationships, providing a more nuanced understanding of the neurofunctional disruptions in addiction [4].
Neuroimaging Evidence of Distinct Neurobiological Effects
Emerging neuroimaging research provides compelling evidence that co-occurring psychiatric disorders have distinct, measurable effects on the neurobiology of SUDs. A recent systematic review of neuro-imaging findings categorized these effects into four potential patterns [76] [77]:
Table 1: Neurobiological Effects of Psychiatric Comorbidities on Substance Use Disorders
| Comorbid Disorder | Effect Type | Key Neurobiological Impact |
|---|---|---|
| Schizophrenia | Amplifying & Unique | Amplifies neurobiological changes seen in SUD; exhibits unique neurobiological effects |
| Personality Disorder | Amplifying & Unique | Amplifies neurobiological changes seen in SUD; exhibits unique neurobiological effects |
| ADHD | Unique | Demonstrates unique neurobiological effects distinct from SUD alone |
| Depression | Attenuating or None | Shows dampening or no additional effects on neurobiological changes from SUD |
| PTSD | Contradictory | Findings are inconsistent and contradictory across studies |
The review, which analyzed 26 neuroimaging studies, found that schizophrenia and personality disorders not only amplify the neurobiological changes associated with SUD but also contribute unique alterations [76]. ADHD, while not necessarily amplifying SUD-related changes, demonstrates its own unique neurobiological signature in comorbid patients [76]. Conversely, depression appears to have either no additional effect or a dampening effect on the neurobiological changes observed in SUD [77]. The most inconsistent findings emerged for PTSD, highlighting the need for more targeted research on this specific comorbidity profile [76].
Methodological Approaches for Differential Assessment
Standardized Diagnostic Instruments
Accurate differentiation of comorbid conditions requires assessment tools that move beyond unstructured clinical interviews. Several validated, structured instruments provide the diagnostic consistency necessary for both research and complex clinical presentations [20].
Table 2: Key Structured Assessment Instruments for Comorbid Disorders
| Instrument | Primary Diagnostic Focus | Key Features | Administration Time |
|---|---|---|---|
| Addiction Severity Index (ASI) | Problem severity in 7 domains | Assesses functioning in alcohol, drugs, psychiatric, family/social, medical, employment, legal domains | 45-60 minutes |
| Structured Clinical Interview for DSM-5 (SCID-5) | DSM-5 Disorders | Semi-structured; allows clinical judgment; considered "gold standard" for research | ~90 minutes |
| Composite International Diagnostic Interview (CIDI) | DSM-IV & ICD-10 Disorders | Fully structured; can be administered by trained lay interviewers | ~75 minutes |
| Psychiatric Research Interview for Substance and Mental Disorders (PRISM) | Substance & Mental Disorders | Specifically designed for diagnosing comorbidities in substance-using populations | Variable |
| Alcohol Use Disorders and Associated Disabilities Interview Schedule (AUDADIS) | Alcohol, Drug, & Mental Disorders | Detailed assessment of substance use, mood, anxiety, personality disorders | Variable |
The PRISM instrument is particularly noteworthy for comorbid presentations as it was specifically designed to address the diagnostic complexities arising when substance use and psychiatric symptoms co-occur, helping clinicians disentangle substance-induced symptoms from independent psychiatric disorders [20]. When selecting an instrument, researchers and clinicians must consider factors including the population, training requirements, and the specific diagnostic questions being addressed.
Emerging Digital and Gamified Assessment Tools
Traditional neurocognitive assessments are often lengthy, unengaging, and difficult to administer at scale. To address these limitations, researchers have developed the BrainPark Assessment of Cognition (BrainPAC), a digitally gamified battery designed to assess the key neurocognitive constructs underpinning addictive behaviors [34].
The development and validation of BrainPAC followed a rigorous multi-stage protocol:
- Construct Identification: An international Delphi consensus study of addiction experts identified seven key neurocognitive constructs mechanistically implicated in addiction: response selection/inhibition, reward valuation, action selection, reward learning, expectancy/prediction error, habit, and compulsivity [34].
- Task Selection and Gamification: Gold-standard laboratory paradigms measuring these constructs were selected and redesigned with game elements through an iterative process involving neuropsychologists, industry partners, and community focus groups to enhance engagement while preserving cognitive demands.
- Psychometric Validation: The gamified tasks were validated against their original laboratory paradigms in a series of studies with over 600 participants recruited via Mechanical Turk. Four of the five tasks demonstrated adequate to excellent test-retest reliability (ICC 0.72-0.91), and most metrics significantly correlated with the original paradigms (r=0.18-0.63) [34].
This innovative approach represents a significant advancement for the scalable assessment of addiction-related neurocognition, with potential applications in early risk detection and intervention monitoring.
Research Reagents and Materials Toolkit
The following table details essential materials and methodological solutions for conducting research on addictive and psychiatric comorbidity.
Table 3: Essential Research Reagent Solutions for Comorbidity Studies
| Research Tool Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Structured Diagnostic Interviews | SCID-5, PRISM, CIDI, AUDADIS | Standardized assessment and reliable diagnosis of comorbid psychiatric and substance use disorders according to DSM/ICD criteria |
| Neurocognitive Assessment Batteries | ANA Battery, BrainPAC | Measurement of core neurofunctional domains (Executive Function, Incentive Salience, Negative Emotionality) through behavioral tasks and self-report |
| Specialized Behavioral Task Libraries | Millisecond Test Library (Inquisit) | Computerized administration of standardized neurocognitive tasks with precise timing measurement |
| Alcohol-Specific Assessment Tools | Alcohol Use Disorders Identification Test (AUDIT), Timeline Followback (TLFB) | Quantification of alcohol consumption patterns, problematic use, and treatment outcomes |
| Clinical Symptom Tracking | Clinician Institute Withdrawal Assessment (CIWA-Ar), Obsessive Compulsive Drinking Scale (OCDS) | Monitoring of alcohol withdrawal symptoms and craving intensity in study populations |
Experimental Workflow for Neurobiological Differentiation
The following diagram illustrates a comprehensive experimental workflow for differentiating addiction from other psychiatric disorders using neurobiological assessments, synthesizing methodologies from the ANA framework and validation studies.
This workflow implements a comprehensive assessment strategy as employed in recent ANA validation studies [4]. Participants are first characterized using standardized diagnostic instruments like the SCID-5 to establish baseline psychiatric and SUD diagnoses. The ANA battery is then administered in randomized blocks to mitigate order effects, with breaks to reduce fatigue-related bias [4]. The subsequent factor analysis identifies latent neurofunctional factors within each domain, with validation against clinical AUD status confirming the real-world relevance of identified factors [4].
Data Integration and Clinical Implications
Sex-Based Differences in Comorbidity Patterns
Large-scale clinical data sets reveal important demographic variations in comorbidity patterns. A recent analysis of a national US clinical dataset found significant sex-based differences in psychiatric comorbidities among individuals with opioid, alcohol, or cannabis dependence [78]. Males with these primary SUDs had lower adjusted odds of anxiety, bipolar, depression, and trauma/stressor disorders compared to females. However, males with opioid or cannabis dependence had higher adjusted odds of schizophrenia and other psychotic disorders (SPD) compared to females [78]. These findings highlight the need for sex-specific assessment and treatment approaches for dual diagnoses.
Toward an Integrated Treatment Approach
The complex nature of comorbidity necessitates a move away from serial treatment models (where one disorder must be "stabilized" before treating the other) toward integrated care that addresses both conditions simultaneously [74]. Evidence strongly supports integrated models, as substance withdrawal can exacerbate psychiatric symptoms, leading to a cycle of self-medication and resumed substance use [74]. Neurobiologically-informed assessments like the ANA can potentially guide targeted interventions by identifying an individual's specific profile of dysfunction across the three core domains, paving the way for personalized treatment approaches that address the unique neurobiological underpinnings of their condition.
The challenge of differentiating addiction from other psychiatric disorders requires a multifaceted approach that integrates neurobiological frameworks, standardized assessments, and emerging technologies. The ANA framework provides a promising structure for deconstructing the heterogeneity of addictive disorders through the lens of three core neurofunctional domains, each with its own underlying dimensionality. Neuroimaging evidence confirms that different comorbidities have distinct effects on the neurobiology of SUDs, ranging from amplification to attenuation of SUD-related changes.
Moving forward, the field must continue to develop and validate engaging, scalable assessment tools like BrainPAC that can efficiently measure the key neurocognitive constructs underpinning addictive behaviors. By combining these advanced assessment methodologies with integrated treatment approaches that address the full complexity of dual diagnosis, researchers and clinicians can work toward more personalized, effective interventions for those struggling with comorbid substance use and psychiatric disorders.
The neurobiological validation of addiction assessment instruments represents a critical frontier in advancing both clinical practice and therapeutic development. However, significant challenges emerge when applying these instruments across diverse populations without establishing measurement invariance—the statistical property confirming that an instrument measures the same underlying construct across different groups. The increasing recognition of addiction as a universal phenomenon worldwide necessitates assessment tools that demonstrate cross-cultural validity and reliability [79]. Without establishing measurement invariance, observed differences in addiction prevalence or severity across cultural, ethnic, or gender groups may reflect methodological artifacts rather than true phenotypic variations, potentially compromising the validity of neurobiological correlations and treatment outcome assessments [80] [81].
This comparison guide examines contemporary addiction assessment instruments through the dual lenses of measurement invariance and cultural adaptation, with particular emphasis on their applicability in global research contexts and drug development pipelines. We evaluate traditional substance use assessments alongside emerging instruments for behavioral addictions and innovative digital tools, focusing specifically on their cross-cultural validation status and implementation requirements.
Theoretical Framework: Neurobiological Foundations for Addiction Assessment
The Addictions Neuroclinical Assessment (ANA) framework proposes three core neurofunctional domains implicated across addictive disorders: executive function, incentive salience, and negative emotionality [3]. These domains, tied to different phases in the addiction cycle, provide a neurobiologically-grounded structure for assessment that transcends specific addictive agents or behaviors. This framework aligns with the Research Domain Criteria (RDoC) initiative from the National Institute of Mental Health, which advocates for a neuroscience-based research framework for psychiatric diseases [3].
Table 1: Neurofunctional Domains in the Addiction Cycle
| Addiction Phase | Core Neurofunctional Domain | Associated Processes | Assessment Examples |
|---|---|---|---|
| Binge/Intoxication | Incentive Salience | Reward valuation, reward learning | Delay Discounting Task, Value-Modulated Attentional Capture |
| Withdrawal/Negative Affect | Negative Emotionality | Stress reactivity, emotional regulation | Self-report measures of negative affect, stress tasks |
| Preoccupation/Anticipation | Executive Function | Response inhibition, decision making, cognitive control | Stop Signal Task, Balloon Analogue Risk Task |
The ANA framework emphasizes that addictive disorders are etiologically heterogeneous, and dichotomous affected/unaffected classifications fail to capture severity and distinctiveness [3]. A mechanistically-informed nosology may enable identification of improved treatment options and better matching to treatments, which is particularly relevant for drug development professionals seeking to validate therapeutic mechanisms across diverse populations.
Comparative Analysis of Addiction Assessment Instruments
Established Substance Use Disorder Assessments
Traditional substance use assessments have primarily been developed and validated within Western contexts, raising questions about their cross-cultural applicability. A systematic review identified 17 addiction screening tests validated in primary care settings, though notably none screened for non-substance addictive behaviors [82]. These instruments vary significantly in their structure, scope, and validation status across diverse populations.
Table 2: Comparison of Established Substance Use Disorder Assessment Instruments
| Instrument | Primary Constructs Measured | Cultural Validation Status | Measurement Invariance Testing | Key Psychometric Properties |
|---|---|---|---|---|
| Addiction Severity Index (ASI) | Functioning in 7 domains: alcohol, drugs, psychiatric, family/social, medical, employment/support, legal | Widused globally but limited cross-cultural validation | Limited formal measurement invariance testing | Administration: 45-60 minutes; Training: 2 days [20] |
| Composite International Diagnostic Interview (CIDI) | DSM-IV/ICD-10 substance use disorders, anxiety, mood disorders | Developed for international use | Extensive cross-cultural validation in WHO studies | Administration: 75 minutes; Fully structured format [20] |
| Alcohol Use Disorders Identification Test (AUDIT) | Alcohol consumption, drinking behavior, adverse reactions | Validated in multiple languages and cultures | Measurement invariance established for Hispanic vs Caucasian youth [80] | High sensitivity and specificity for alcohol use disorders |
| ASSIST | Substance use-related risks and problems | Validated in primary care across multiple countries | Limited formal measurement invariance testing | Brief administration (5-10 minutes); WHO-developed |
The search for a substance use assessment that demonstrates comprehensive cross-cultural measurement invariance continues, with most instruments showing variable performance across different ethnic and cultural groups. For instance, while the AUDIT demonstrates measurement invariance between Hispanic and Caucasian youth [80], this does not necessarily extend to other cultural groups or different substance use measures.
Emerging Behavioral Addiction Assessments
Behavioral addiction assessments represent a rapidly evolving field, with several instruments demonstrating progressive attention to cross-cultural validation.
Table 3: Behavioral Addiction Assessment Instruments and Cross-Cultural Validation
| Instrument | Target Behavior | Cultural Validation Status | Measurement Invariance Testing | Key Findings |
|---|---|---|---|---|
| International Work Addiction Scale (IWAS) | Work addiction/workaholism | Validated across 85 cultures, 31,352 participants [79] | Partial scalar invariance across 81 cultures (IWAS-7); Full scalar invariance across 85 cultures (IWAS-5) | 7-item and 5-item versions; Optimal cut-offs: 24 points (IWAS-7) and 18 points (IWAS-5) with 96% accuracy [79] |
| Mobile Phone Dependence Questionnaire (MPDQ) | Mobile phone dependence | Validated in mainland Chinese and Hong Kong adolescents [81] | Partial metric and partial scalar invariance achieved | Mainland Chinese adolescents reported higher scores on all MPD factors than Hong Kong counterparts [81] |
| Smartphone Application-Based Addiction Scale (SABAS) | Smartphone application addiction | Chinese version validated with college students [83] | Measurement invariance across gender demonstrated | Based on Griffiths' "Addiction Component Model"; 6 items assessing core addiction components [83] |
The International Work Addiction Scale (IWAS) represents a significant advancement in cross-cultural addiction assessment, with demonstrated scalar invariance across 85 cultures [79]. The development process involved administering an initial 16-item questionnaire to 31,352 employees from six continents alongside measures of job stress, job satisfaction, and self-esteem. The resulting brief versions (IWAS-7 and IWAS-5) maintain strong associations with these external validators across cultures, supporting their universal applicability [79].
Innovative Digital Assessment Tools
Digital assessment tools represent a paradigm shift in addiction measurement, leveraging technology to capture neurocognitive processes more directly.
Table 4: Digital Assessment Tools for Addiction-Related Neurocognition
| Tool | Assessment Approach | Target Constructs | Validation Status | Cross-Cultural Application |
|---|---|---|---|---|
| BrainPark Assessment of Cognition (BrainPAC) | Gamified neurocognitive tasks | Response selection/inhibition, reward valuation, action selection, reward learning, compulsivity [34] | Validated against standard laboratory paradigms (r=0.18-0.63); 4 of 5 tasks show adequate-excellent test-retest reliability (ICC 0.72-0.91) [34] | Initial validation in online samples; Cross-cultural validation ongoing |
| Traditional Laboratory Paradigms | Standard cognitive tasks | Executive function, reward processing, decision-making | Established reliability and validity primarily in Western samples | Limited cross-cultural validation; Potential cultural biases in task performance |
The BrainPAC digital assessment battery was developed through an international Delphi consensus study identifying key constructs mechanistically implicated in addiction outcomes [34]. The gamified approach addresses engagement challenges in neurocognitive assessment, potentially enhancing compliance in diverse populations, though comprehensive cross-cultural validation remains ongoing.
Methodological Protocols for Establishing Measurement Invariance
Statistical Procedures for Measurement Invariance Testing
Establishing measurement invariance involves a sequential testing process to ensure equivalent measurement properties across groups.
Table 5: Levels of Measurement Invariance and Their Interpretation
| Invariance Level | Statistical Test | Research Implications | Example from Literature |
|---|---|---|---|
| Configural | Same factor structure across groups | Basic construct similarity | Three-factor structure of MPDQ confirmed across mainland Chinese and Hong Kong adolescents [81] |
| Metric | Equivalent factor loadings across groups | Relationships between items and latent construct are similar | Peer norms measures showed equivalent factor loadings for Hispanic and Caucasian youth [80] |
| Scalar | Equivalent item intercepts across groups | Latent mean comparisons are valid | IWAS-5 demonstrated full scalar invariance across 85 cultures, enabling mean comparisons [79] |
| Strict | Equivalent residual variances across groups | Complete measurement equivalence | Rarely achieved in cross-cultural addiction research |
The protocol for establishing measurement invariance typically employs multiple group confirmatory factor analysis, evaluating model fit indices (e.g., CFI, RMSEA) at each successive level of constraint. A change in CFI ≤ .01 combined with a change in RMSEA ≤ .015 generally indicates invariance can be retained [80] [81].
Cultural Adaptation Methodologies
Cultural adaptation extends beyond linguistic translation to include contextual relevance of item content and response formats.
Table 6: Cultural Adaptation Protocol for Addiction Assessments
| Adaptation Phase | Key Procedures | Purpose | Exemplary Implementation |
|---|---|---|---|
| Forward Translation | Multiple independent translators; Reconciliation of discrepancies | Ensure linguistic equivalence | SABAS translation involved native Chinese speakers with expertise in English applied linguistics [83] |
| Back Translation | Blind back-translation by bilingual translators | Identify conceptual discrepancies | Preliminary Chinese version of SABAS back-translated to English [83] |
| Expert Review | Review by content and cultural experts | Evaluate cultural and contextual relevance | Two smartphone addiction experts reviewed SABAS-CV translations [83] |
| Cognitive Interviewing | Think-aloud protocols with target population | Assess comprehension and relevance | 45 college students interviewed after completing SABAS-CV [83] |
| Psychometric Validation | Factor analysis, reliability assessment, measurement invariance testing | Verify statistical properties | SABAS-CV tested with 644 Chinese college students; measurement invariance across gender established [83] |
The cultural adaptation process must balance maintaining assessment validity while ensuring cultural appropriateness. For instance, in adapting the Mobile Phone Dependence Questionnaire for mainland Chinese and Hong Kong adolescents, researchers considered differences in cultural environments, mental health literacy, pandemic policies, and language systems [81].
Table 7: Research Reagent Solutions for Cross-Cultural Addiction Assessment
| Tool/Resource | Function/Purpose | Implementation Considerations | Exemplary Applications |
|---|---|---|---|
| Multiple Group Confirmatory Factor Analysis | Statistical test of measurement invariance | Requires large sample sizes; Sensitive to model specification | Used to establish invariance of alcohol measures with Hispanic youth [80] |
| Computer-Assisted Assessment Platforms | Standardized administration across sites | Reduces administrator variability; Enables immediate data entry | Several structured interviews available in computer-assisted formats [20] |
| International Validation Samples | Cross-cultural comparison and norming | Resource-intensive; Enables detection of cultural variation | IWAS validation included 31,352 employees from 85 cultures [79] |
| Gamified Neurocognitive Tasks | Enhanced engagement in digital assessment | Potential for reduced cultural bias in performance-based measures | BrainPAC tasks developed to improve engagement in neurocognitive assessment [34] |
| Harmonized Assessment Batteries | Standardized cross-cultural comparison | Facilitates data pooling across international sites | NIDA Clinical Trials Network uses common assessment battery [20] |
The optimal approach to addiction assessment in diverse populations integrates multiple methodological frameworks: the neurobiological precision of the ANA framework, the cross-cultural robustness of instruments demonstrating measurement invariance like the IWAS, and the engaging assessment approach of digital tools like BrainPAC. For researchers and drug development professionals, this integrated approach enables more valid cross-cultural comparisons, enhances detection of neurobiological correlates, and ultimately supports the development of more precisely targeted interventions.
Future development should prioritize instruments that simultaneously capture the neurocognitive mechanisms underpinning addiction while demonstrating cross-cultural validity. The successful validation of the IWAS across 85 cultures provides a template for this approach, demonstrating that with rigorous methodology, universally applicable addiction assessment is an achievable goal [79]. As the field progresses, the integration of neurobiological markers with culturally-adapted behavioral assessments will likely yield the most comprehensive understanding of addictive disorders across global populations.
Evidence and Efficacy: A Comparative Review of Validation Outcomes
Predictive Validity of Neurocognitive Measures for Relapse and Treatment Outcomes
Addiction is increasingly understood as a chronic relapsing disorder characterized by specific neuroadaptations that drive compulsive substance use despite negative consequences [10]. A critical challenge in both clinical management and drug development is the high rate of relapse following treatment, with studies indicating that 40–80% of patients relapse within 1–6 months after treatment for heroin and cocaine dependence [84]. This persistent relapse risk underscores the urgent need for objective, biologically-based tools that can predict treatment outcomes and identify individuals at highest risk of recurrence.
Neurocognitive measures offer a promising approach by assessing brain functions mechanistically linked to the core processes of addiction. Unlike self-report measures, which can be influenced by poor insight or social desirability bias, neurocognitive assessments capture automatic, fast cognitive processes unavailable to conscious introspection [84]. This review synthesizes current evidence on the predictive validity of these measures across addictive disorders, comparing their relative strengths and providing researchers with standardized protocols for implementation.
Neurobiological Framework of Addiction
The neurobiology of addiction provides a critical foundation for understanding which cognitive domains most likely predict relapse. Contemporary models conceptualize addiction as a repeating cycle of three distinct stages, each mediated by specific neural circuitry [10]:
- Binge/Intoxication Stage: Focused on the basal ganglia, this stage involves dopaminergic firing for substance-associated cues (incentive salience) while diminishing for the substance itself.
- Withdrawal/Negative Affect Stage: Centered on the extended amygdala, this stage activates brain stress systems, leading to withdrawal symptoms and diminished baseline pleasure.
- Preoccupation/Anticipation Stage: Governed by the prefrontal cortex, this stage involves executive control system hijacking, presenting as diminished impulse control, executive planning, and emotional regulation.
This cyclic model has been translated into three neurofunctional domains through the Addictions Neuroclinical Assessment (ANA): incentive salience, negative emotionality, and executive dysfunction [10]. These domains provide the theoretical basis for selecting neurocognitive measures with the greatest potential predictive validity.
Comparative Predictive Validity of Neurocognitive Measures
Neurocognitive assessment in addiction research has evolved from traditional neuropsychological tests to include brain imaging during cognitive task performance (neurocognitive measures) and, more recently, engaging digital tools designed specifically for addiction-related constructs. The table below compares the predictive validity of established and emerging assessment approaches.
Table 1: Comparative Predictive Validity of Neurocognitive Assessment Approaches
| Assessment Approach | Specific Measures | Predicted Outcome | Predictive Strength | Key Findings |
|---|---|---|---|---|
| Brain Imaging during Cognitive Tasks [84] | fMRI during Attentional Bias Tasks | Substance relapse after treatment | Moderate to Strong | Dorsal anterior cingulate cortex (dACC) hyperactivity predicts relapse; associated with need for more top-down resources when substance cues are present [84] |
| fMRI during Cue-Reactivity Tasks | Substance relapse after treatment | Moderate | Enhanced prefrontal, sensory, motor, and limbic activity associated with relapse; different brain processes (cognitive control vs. reward) differently associated with outcomes [84] | |
| fNIRS during Verbal Fluency Task [85] | Alcohol dependence relapse within 3 months | Strong (AUC=0.951) | Significantly lower activation in frontal and bilateral temporal lobes predicts relapse with 92.4% sensitivity, 88.6% specificity [85] | |
| Digital Neurocognitive Assessment [34] | BrainPark Assessment of Cognition (BrainPAC) | Addictive behaviors in community samples | Moderate (correlation with lab tasks: r=0.18-0.63) | Gamified battery assessing response inhibition, reward valuation, action selection, reward learning, and compulsivity; adequate to excellent test-retest reliability (ICC=0.72-0.91) [34] |
| Neurophysiological Measures [69] | Startle Reflex Modulation | Long-term (2-year) treatment outcomes in alcohol use disorder | Limited change | Alcohol-related cues continue to facilitate motivational approach response even after 2 years of treatment, indicating persistent vulnerability [69] |
| Cortisol Response to Alcohol Cues | Long-term (2-year) treatment outcomes in alcohol use disorder | Limited change | Continued altered cortisol reactivity after sustained remission, suggesting persistent neurobiological dysregulation [69] |
Domain-Specific Predictive Relationships
Different neurocognitive domains demonstrate varying predictive relationships with relapse outcomes across substance use disorders. The following table synthesizes evidence for specific cognitive constructs and their prognostic value.
Table 2: Domain-Specific Neurocognitive Predictors of Relapse
| Neurocognitive Domain | Specific Construct | Associated Neural Substrate | Relationship to Relapse | Supporting Evidence |
|---|---|---|---|---|
| Cognitive Control | Response inhibition & error processing | Anterior cingulate cortex (ACC), inferior frontal gyrus (IFG), dorsolateral prefrontal cortex (DLPFC) | Strong predictor | Reduced brain activation during inhibitory control and error-processing predicts relapse; associated with event-related potentials (N2, ERN) [84] |
| Motivational Processes | Attentional bias to substance cues | Prefrontal areas, insula, nucleus accumbens, amygdala | Moderate predictor | Automatic orientation to drug-related stimuli due to incentive salience; associated with activity in ACC, DLPFC, insula, and subcortical regions [84] |
| Reward Processing | Reward valuation (delay discounting) | Prefrontal-striatal circuits | Moderate predictor | Preference for immediate smaller rewards over larger delayed rewards significant risk factor across addictive behaviors [34] |
| Executive Function | Verbal fluency & cognitive flexibility | Frontal and temporal lobes | Strong predictor in alcohol dependence | Reduced frontal and temporal lobe activation during verbal fluency tasks highly predictive of 3-month relapse (AUC=0.951) [85] |
| Self-Control Capacity | Subjective self-control | Prefrontal cortex | Moderate predictor (with fluctuations) | Temporal variability in self-control associated with craving intensity and substance use; single-item assessment captures cognitive self-control [86] |
Detailed Experimental Protocols
Functional Near-Infrared Spectroscopy (fNIRS) with Verbal Fluency Task
This protocol, adapted from the study predicting relapse in alcohol dependence [85], demonstrates how to assess prefrontal and temporal lobe function using fNIRS during a phonemic verbal fluency task.
Materials and Equipment
- fNIRS device (e.g., Hitachi ETG-4000) with 52 channels covering frontal and temporal lobes
- Sound-attenuated testing room with comfortable seating
- Task presentation software and timing apparatus
- Data recording and analysis system
Procedure
- Participant Preparation: Position participant in a comfortable chair in the testing room. Apply fNIRS cap ensuring proper probe contact with scalp.
- Baseline Recording (30 seconds): Instruct participant to repeat "1.2.3.4.5" following a metronome pace to establish hemodynamic baseline.
- Task Period (60 seconds): Present participants with specific phonemes (e.g., "big," "sky," "white" in original study) and instruct them to generate as many words as possible beginning with each phoneme.
- Post-Task Recording (30 seconds): Return to baseline condition with number repetition.
- Data Processing: Calculate oxygenated hemoglobin (oxy-Hb) concentration changes using modified Beer-Lambert law. Extract β-values using General Linear Model (GLM) representing degree of signal activation.
Outcome Measures
- Integral values: Area under the curve of oxy-Hb concentration in positive coordinate part
- β-values: Degree of signal activation corresponding to actual oxy-Hb concentration changes
- Channel-specific activation: Compare frontal (all channels except Ch13) and bilateral temporal lobe activation
Predictive Validation
In the validation study, this protocol successfully differentiated alcohol-dependent patients from controls and predicted 3-month relapse with 92.4% sensitivity and 88.6% specificity based on reduced frontal and temporal activation [85].
BrainPAC Digital Assessment Battery
The BrainPark Assessment of Cognition (BrainPAC) is a gamified digital battery developed through expert consensus to assess neurocognitive constructs mechanistically linked to addictive behaviors [34].
Materials and Equipment
- Computer or tablet with BrainPAC software installed
- Internet connection for data synchronization (optional)
- Quiet testing environment
Procedure
The battery consists of five gamified tasks administered in approximately 60 minutes:
- Balloon Analogue Risk Task (BART): Measures action selection; participants inflate virtual balloons to earn points while risking explosion.
- Stop Signal Task (SST): Assesses response selection and inhibition; participants respond to arrows unless a stop signal appears.
- Delay Discounting Task (DDT): Evaluates reward valuation; participants choose between smaller immediate and larger delayed rewards.
- Value-Modulated Attentional Capture (VMAC): Indexes reward learning and compulsivity-related cognitive flexibility; participants locate targets while ignoring distractors with previously rewarded features.
- Sequential Decision-Making Task (SDT): Measures reward learning and expectancy/reward prediction error; participants learn stimulus-outcome associations through trial and error.
Outcome Measures
- Task-specific metrics (e.g., Go Reaction Time for SST, discounting rate for DDT)
- Composite scores for key constructs: response selection/inhibition, reward valuation, action selection, reward learning, and compulsivity
Psychometric Properties
In validation studies, BrainPAC tasks showed significant correlations with original laboratory paradigms (r=0.18-0.63) and demonstrated adequate to excellent test-retest reliability (ICC=0.72-0.91 for 4 of 5 tasks) [34].
Neurocognitive Assessment Workflow
The following diagram illustrates a standardized workflow for implementing neurocognitive assessment in addiction treatment outcomes research, integrating both laboratory and digital approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Neurocognitive Addiction Research
| Category | Specific Tool/Reagent | Key Function | Example Use in Research |
|---|---|---|---|
| Brain Imaging Equipment | Functional Near-Infrared Spectroscopy (fNIRS) | Measures cortical hemodynamic changes during cognitive tasks | Assessing frontal and temporal lobe function during verbal fluency tasks to predict relapse in alcohol dependence [85] |
| Functional Magnetic Resonance Imaging (fMRI) | Measures brain activity through blood oxygen level-dependent (BOLD) signal | Identifying neural correlates of attentional bias and cue-reactivity associated with relapse risk [84] | |
| Electroencephalography (EEG) | Records electrical activity of the brain with high temporal resolution | Measuring event-related potentials (N2, ERN) during inhibitory control tasks [84] | |
| Digital Assessment Platforms | BrainPAC (BrainPark Assessment of Cognition) | Gamified battery assessing addiction-specific neurocognitive constructs | Scalable assessment of response inhibition, reward valuation, and other mechanistic targets [34] |
| CANTAB (Cambridge Neuropsychological Test Battery) | Computerized assessment of multiple cognitive domains | Standardized measurement of executive function, memory, and attention in addiction populations | |
| Physiological Measurement | Startle Reflex Paradigm Equipment | Eyeblink response measurement to assess motivational salience of cues | Determining appetitive responses to alcohol-related stimuli in alcohol use disorder [69] |
| Salivary Cortisol Collection Kits | Stress response biomarker measurement | Assessing hypothalamic-pituitary-adrenal axis reactivity to substance-related cues [69] | |
| Neuropsychological Tests | Delis-Kaplan Executive Function System (D-KEFS) | Comprehensive assessment of verbal and nonverbal executive functions | Measuring cognitive flexibility, response inhibition, and verbal fluency [86] |
| Conners' Continuous Performance Test (CPT-3) | Computer-based GO/NO-GO assessment of attention | Assessing impulsivity, inattention, sustained attention, and vigilance [86] | |
| Data Collection & Analysis | Mechanical Turk or similar platforms | Recruitment of diverse community samples for validation studies | Rapid recruitment for digital assessment validation [34] |
| Mixed-effects modeling software (R, Python) | Statistical analysis of intensive longitudinal data | Modeling temporal relationships between cognitive measures, craving, and relapse [86] |
Neurocognitive measures show significant promise for predicting relapse and treatment outcomes across substance use disorders, with particular strength in domains mapping onto the core neurobiological framework of addiction. Executive function assessments, particularly those measuring cognitive control and verbal fluency, demonstrate the most consistent predictive validity, while motivational processes like attentional bias offer complementary prognostic information.
Emerging digital assessment platforms represent a paradigm shift in neurocognitive measurement, offering engaging, scalable tools designed specifically for addiction-related constructs. These innovations address critical limitations of traditional laboratory assessments while maintaining strong psychometric properties.
For researchers and drug development professionals, integrating standardized neurocognitive assessment into clinical trials and treatment studies can provide objective biomarkers of treatment efficacy and identify individuals at highest relapse risk. Future research should focus on validating multimodal assessment approaches that combine neurocognitive measures with other biomarkers to enhance predictive accuracy and facilitate personalized intervention strategies.
Validation of the ANA Incentive Salience Domain in Multi-Site AUD Treatment Studies
The Addictions Neuroclinical Assessment (ANA) is a neuroscience-informed framework developed to address the profound heterogeneity observed in Alcohol Use Disorder (AUD) [3]. Moving beyond traditional symptom-counting diagnostic methods, the ANA proposes that addiction arises from dysfunctions in three core neurofunctional domains: Incentive Salience, Negative Emotionality, and Executive Function [3]. This review critically examines the validation evidence for the first domain—Incentive Salience—within multisite AUD treatment contexts. Incentive salience refers to the process whereby alcohol-related stimuli become disproportionately attractive and motivationally salient, driving compulsive alcohol seeking and use [87]. The validation of this domain across diverse populations and research settings is crucial for establishing a biologically grounded nosology for AUD and advancing personalized treatment approaches.
Experimental Validation of the Incentive Salience Domain
Psychometric Validation in Multisite Treatment Studies
The most compelling evidence for the incentive salience domain comes from a large-scale, multisite prospective study involving 563 participants seeking treatment for AUD [87] [88]. This research implemented a rigorous methodology to validate the latent construct of incentive salience.
- Experimental Protocol: Researchers used confirmatory factor analysis (CFA) to test a one-factor model of incentive salience. The model incorporated items from well-established clinical assessments measuring urges to drink: the Alcohol Dependence Scale, the Impaired Control Scale, and the Marlatt Relapse Interview [87] [88].
- Key Findings: The one-factor model demonstrated excellent fit to the data (χ²(12) = 19.42, p = .08; RMSEA = 0.034; CFI = 0.992), confirming that the various measures collectively tap into a single, unified construct [87]. Furthermore, the model was found to be measurement invariant across sex, indicating that the construct is measured equivalently in men and women, a critical feature for generalizable research and clinical application [87].
Table 1: Psychometric Properties and Correlates of the ANA Incentive Salience Factor
| Validation Metric | Result | Significance/Implication |
|---|---|---|
| Model Fit (CFA) | RMSEA = 0.034; CFI = 0.992 | Excellent fit for a one-factor model [87] [88]. |
| Measurement Invariance | Invariant across sex | Construct is measured equivalently across different demographic groups [87]. |
| Correlation with Drinks Per Day | r = 0.447 [0.379, 0.514] | Strong association with real-world drinking intensity [87]. |
| Correlation with Urge-Related Drinking | r = 0.529 [0.460, 0.599] | Strongly linked to drinking motivated by cravings [87]. |
| Predictive Validity | Surpassed pre-existing scales | Demonstrates superior utility in predicting drinking outcomes [87] [88]. |
The incentive salience factor demonstrated strong construct validity through significant correlations with drinking patterns and reasons for drinking. As shown in Table 1, it was strongly associated with the intensity of daily drinking and was particularly linked to drinking driven by internal urges and external social pressure [87]. This pattern of correlations affirms that the factor captures the core of incentive salience—the heightened motivational pull of alcohol-related cues.
Neurobiological Validation through Imaging Correlates
A critical step in validating a neuroscience-based framework is linking its constructs to specific neural circuitry. A 2024 functional neuroimaging (fMRI) study addressed this by investigating the neural correlates of the incentive salience factor in 45 individuals with AUD [89] [90] [91].
- Experimental Protocol: Participants completed a battery of behavioral assessments to compute their incentive salience factor score. They then underwent an fMRI session while performing an alcohol cue-reactivity task, which measures brain responses to alcohol-related images compared to neutral stimuli [89] [90].
- Key Findings: Contrary to the initial hypothesis, incentive salience was not correlated with cue-elicited activation in the ventral or dorsal striatum [89] [90]. Instead, whole-brain analyses revealed that higher incentive salience scores were significantly associated with greater activation in a distributed network of regions involved in reward-learning and affective processing [89] [90]. These regions included the insula, posterior cingulate cortex, bilateral precuneus, and bilateral precentral gyru[scitation:3] [90]. This finding suggests that the ANA incentive salience construct is subserved by a broader neural circuit that integrates interoceptive awareness (insula), self-relevance (precuneus/posterior cingulate), and motor preparation (precentral gyri), going beyond traditional reward pathways [90].
The following diagram illustrates the neural circuitry identified as correlating with the ANA incentive salience domain:
Elucidation of Subfactors in a Standardized Battery
Further refining the construct, a 2024 prospective study of 300 participants across the drinking spectrum used a standardized ANA battery to deconstruct the incentive salience domain into its underlying subfactors [4].
- Experimental Protocol: The study employed a comprehensive, standardized collection of neurocognitive tasks and self-report measures specifically selected to assess the ANA domains. Exploratory factor analysis (EFA) was then used to identify latent factors within the incentive salience domain [4].
- Key Findings: The analysis revealed that the incentive salience domain is not unidimensional but is composed of two distinct subfactors:
- Alcohol Motivation: This encompasses craving, desire, and the compulsive drive to seek and consume alcohol.
- Alcohol Insensitivity: This reflects a decreased sensitivity to the effects of alcohol, which is a known risk factor for developing AUD [4].
This two-factor structure provides a more nuanced understanding of the domain and helps explain some of the heterogeneity in clinical presentation. The study further found that these two subfactors, particularly when combined with an impulsivity factor from the executive function domain, showed a strong ability to classify individuals with problematic drinking and AUD [4].
Comparative Analysis of Validation Approaches
The multisite nature of the primary validation study underscores the real-world applicability and robustness of the ANA framework. Multisite trials are designed for external validity, intentionally embracing patient heterogeneity and community-based treatment settings to ensure findings are generalizable to real-world clinical populations [92]. This stands in contrast to highly controlled efficacy trials, which prioritize internal validity. The successful validation of the incentive salience factor across multiple sites indicates that it is a stable construct that transcends specific clinical contexts [87] [92].
Table 2: Key Methodologies in ANA Incentive Salience Validation
| Study Focus | Primary Method | Sample Characteristics | Core Outcome |
|---|---|---|---|
| Psychometric Validation [87] [88] | Confirmatory Factor Analysis (CFA) | n=563; treatment-seeking AUD; multisite | A unidimensional, sex-invariant factor with strong predictive validity. |
| Neurobiological Validation [89] [90] | Functional Neuroimaging (fMRI) | n=45; non-treatment-seeking AUD | Neural correlates in reward-learning/affective regions, not the striatum. |
| Subfactor Deconstruction [4] | Exploratory Factor Analysis (EFA) | n=300; across the drinking spectrum | Two distinct subfactors: Alcohol Motivation and Alcohol Insensitivity. |
The table above summarizes the complementary approaches used to validate the incentive salience domain. Together, they provide a multi-level validation from the psychological construct to its underlying neural circuitry and subdimensional structure.
The Scientist's Toolkit: Research Reagent Solutions
For researchers seeking to implement the ANA incentive salience domain in their own work, the following toolkit details the essential materials and assessments used in the featured studies.
Table 3: Essential Research Materials for Assessing the ANA Incentive Salience Domain
| Research Reagent / Instrument | Type | Primary Function in Validation |
|---|---|---|
| Alcohol Dependence Scale (ADS) | Self-report questionnaire | Provided items measuring perception of urges and loss of control over drinking for CFA [87] [88]. |
| Impaired Control Scale (ICS) | Self-report questionnaire | Contributed items on the inability to control alcohol consumption to the incentive salience factor model [87] [88]. |
| Marlatt Relapse Interview | Structured interview | Supplied indicators of urges and temptation in high-risk situations for factor analysis [87] [88]. |
| Alcohol Cue-Reactivity fMRI Task | Neuroimaging paradigm | Measured neural activation in response to alcohol versus neutral visual cues to identify biological correlates [89] [90]. |
| Standardized ANA Battery [4] | Integrated assessment battery | A curated set of computer-based tasks and questionnaires used to deconstruct the domain into subfactors (Alcohol Motivation, Insensitivity). |
The workflow for validating and applying the ANA incentive salience construct in a research setting typically follows a structured path, from participant recruitment to data synthesis:
The cumulative evidence from large-scale multisite psychometric studies, neuroimaging investigations, and deep phenotyping efforts provides robust support for the ANA incentive salience domain as a valid and clinically meaningful construct. Its validation across diverse samples and settings highlights its utility in capturing a core neurofunctional process in AUD. The identification of its distinct subfactors and associated neural circuits moves the field beyond syndromal diagnosis toward a precision medicine approach. This allows for the identification of a sub-phenotype of AUD characterized by heightened alcohol motivation and cue-reactivity, which could ultimately be targeted with specific interventions, such as those designed to dampen craving or modulate reward learning [89] [90] [4]. Future research focusing on the interplay between the incentive salience, negative emotionality, and executive function domains will be crucial for developing a fully integrated and biologically grounded nosology for addiction.
The field of addiction research is increasingly focused on identifying the neurocognitive processes that underpin addictive disorders. This shift towards a neurobiological validation of assessment instruments aims to move beyond symptom-based diagnoses and better capture the etiological and functional heterogeneity of these conditions [3]. Frameworks like the Addictions Neuroclinical Assessment (ANA) have been proposed to systematically evaluate core neurofunctional domains—such as executive function, incentive salience, and negative emotionality—that are implicated in the addiction cycle [3] [90].
A significant practical challenge in this endeavor is the assessment of these domains in an engaging, scalable, and psychometrically robust manner. Traditional standard laboratory paradigms, while considered the "gold standard," are often lengthy, unengaging, and difficult to administer at scale [93]. In response, gamified digital assessments have emerged as a promising alternative, designed to enhance participant engagement and enable broader deployment [93] [94]. This guide provides an objective, data-driven comparison of these two approaches, focusing on their test-retest reliability and convergent validity, to inform researchers and drug development professionals.
Comparative Psychometric Performance: Quantitative Data
The table below summarizes key psychometric data from a direct, head-to-head validation study of a gamified battery (BrainPAC) against established laboratory paradigms [93].
Table 1: Direct Psychometric Comparison of Gamified and Standard Laboratory Tasks
| Neurocognitive Construct | Example Laboratory Paradigm | Example Gamified Paradigm (BrainPAC) | Convergence (Correlation Coefficient) | Test-Retest Reliability (ICC) - Gamified Version |
|---|---|---|---|---|
| Response Inhibition | Stop Signal Task (SST) | Gamified SST | ( r = 0.18 - 0.63 ) * | Adequate to Excellent (ICC = 0.72-0.91) |
| Risk Taking | Balloon Analogue Risk Task (BART) | Gamified BART | ( r = 0.18 - 0.63 ) * | Adequate to Excellent (ICC = 0.72-0.91) |
| Delay Discounting | Delay Discounting Task (DDT) | Gamified DDT | ( r = 0.18 - 0.63 ) * | Adequate to Excellent (ICC = 0.72-0.91) |
| Reward Learning | Value-Modulated Attentional Capture (VMAC) Task | Gamified VMAC | ( r = 0.18 - 0.63 ) * | Adequate to Excellent (ICC = 0.72-0.91) |
| Sequential Decision-Making | Sequential Decision-Making Task (SDT) | Gamified SDT | ( r = 0.18 - 0.63 ) * | Poor (Exception) |
Note: * The validation study reported significant correlations (p<.05) across most metrics of the five tasks within this range. Specific correlation values vary by task and metric [93]. ICC = Intraclass Correlation Coefficient.
Detailed Experimental Protocols
Protocol: BrainPAC Validation Study
This cross-sectional study serves as a primary model for the direct validation of gamified cognitive tasks against their standard counterparts [93] [95].
- Objective: To psychometrically validate a purpose-built battery of gamified neurocognitive tasks (BrainPAC) against gold-standard laboratory paradigms and ascertain its test-retest reliability and sensitivity to addictive behaviors [93].
- Participant Cohort: The study utilized a total of 600 participants across three successive validation cohorts, plus a separate test-retest cohort of 50 individuals. Participants were recruited via Amazon's Mechanical Turk [93].
- Task Selection & Gamification: An international panel of addiction experts endorsed key neurocognitive constructs. Gold-standard laboratory paradigms (BART, SST, DDT, VMAC, SDT) were selected to measure these constructs. Professional game developers then collaborated with researchers to create engaging, user-friendly digital versions of these tasks [93].
- Procedure: Participants completed both the standard laboratory paradigms and their gamified equivalents. The test-retest cohort completed the gamified battery on two separate occasions to assess reliability [93].
- Key Outcomes:
- Convergent Validity: Performance on most gamified task metrics was significantly correlated with the original laboratory paradigms, with coefficients ranging from r=0.18 to 0.63 [93].
- Test-Retest Reliability: Four out of the five gamified tasks demonstrated adequate to excellent reliability (ICC: 0.72-0.91), with the Sequential Decision-Making Task being the exception [93].
- Sensitivity: Gamified metrics were significantly associated with addictive behaviors on behavioral inventories, supporting their real-world relevance [93].
Protocol: Densely Sampled Reliability Assessment
This study exemplifies a different approach, focusing on the repeated, longitudinal assessment of a single gamified construct in a naturalistic setting [96].
- Objective: To evaluate the test-retest reliability of reinforcement learning parameters through dense, repeated sampling in an ecologically valid context using a smartphone app [96].
- Participant Cohort: 384 participants with a wide range of psychopathology symptoms, who completed at least 10 runs of the gamified task (total of 9,729 valid runs) [96].
- Gamified Task: The "Influenca" app presented a reward learning task where players identified the most effective medication by integrating rewards with changing probabilities. The app included progress tracking to encourage replay [96].
- Procedure: Participants could complete up to 31 runs of the task (150 trials each) over time on their own devices. Reinforcement learning parameters (e.g., learning rate, reward sensitivity) were computed for each run [96].
- Key Outcomes: The study found that reinforcement learning parameters showed poor to fair intra-class correlations (ICC: 0.22–0.53) across runs. This highlights the substantial within-subject variance in these processes and underscores that a single lab-based measurement may not reliably capture trait-like differences. The quality of measurement and reliability improved over successive runs [96].
Conceptual Framework and Workflow
The Addictions Neuroclinical Assessment (ANA) Framework
The ANA is a heuristic framework designed to address clinical heterogeneity in addiction by grounding assessment in three core neurofunctional domains derived from the addiction cycle [3]. This framework provides the theoretical foundation for the neurocognitive constructs measured by the assessment paradigms discussed in this guide.
Experimental Workflow for Validation
The process of developing and validating a gamified cognitive task against a standard laboratory paradigm follows a systematic workflow.
The Scientist's Toolkit: Key Research Reagents
The following table details essential materials and methodological components frequently employed in this field of research.
Table 2: Essential Research Reagents and Methodological Components
| Item / Solution | Function in Research | Exemplars / Descriptions |
|---|---|---|
| Standard Laboratory Paradigms | Serves as the criterion or "gold standard" for validating new tools; measures specific neurocognitive constructs. | Stop Signal Task (SST), Balloon Analogue Risk Task (BART), Delay Discounting Task (DDT) [93]. |
| Gamified Digital Tasks | Provides an engaging, scalable alternative for assessing neurocognition; aims to improve ecological validity and participant engagement. | BrainPAC tasks [93], Influenca app [96]. |
| Computational Models | Quantifies latent cognitive processes from behavioral data; provides parameters that may serve as transdiagnostic biomarkers. | Reinforcement Learning models (e.g., estimating learning rate, reward sensitivity) [96]. |
| Functional Magnetic Resonance Imaging (fMRI) | Identifies neural correlates of neurocognitive domains and task performance; provides biological validation. | Used to link ANA "Incentive Salience" scores to cue-elicited activation in insula and cingulate cortices [90]. |
| Ecological Momentary Assessment (EMA) | Captures real-time, in-the-moment data on psychological states and behavior in natural environments. | Integrated into apps like Influenca to assess state fluctuations alongside cognitive task performance [96]. |
Critical Interpretation of Psychometric Data
- Convergence Validity: The observed correlation range (( r = 0.18 - 0.63 )) indicates that gamified tasks measure related, but not identical, constructs to their standard counterparts [93]. This suggests that gamification may introduce novel variance, potentially by enhancing engagement or altering task demands.
- Reliability in Context: The excellent test-retest reliability (ICC > 0.90) for some BrainPAC tasks is a robust result [93]. However, the poor to fair reliability (ICC = 0.22–0.53) found in the densely sampled Influenca study is not necessarily a failure [96]. Instead, it highlights that some neurocognitive processes, like reward learning, may have significant state-like components. This variability is a valid finding in itself and suggests that single, cross-sectional measurements in the lab may be insufficient to characterize an individual's trait-like functioning in these domains.
- Generalizability: The high completion rates and engagement reported for naturalistic tasks (including gamified and EMA-based ones) across multiple studies support their feasibility and acceptability for diverse participants, which is crucial for large-scale and longitudinal research [94].
The comparative psychometric data indicate that gamified paradigms are a valid and reliable alternative to standard laboratory tasks for assessing key neurocognitive domains in addiction. They offer a favorable balance of convergent validity, good test-retest reliability, and enhanced scalability and engagement [93] [94].
For researchers and drug development professionals, the choice of paradigm should be guided by the specific research question:
- Standard Laboratory Paradigms remain the benchmark for tightly controlled, mechanistic studies.
- Gamified Digital Assessments are highly suitable for large-scale screening, longitudinal monitoring, and studies where participant engagement and ecological validity are priorities.
Future development should focus on improving convergence with established measures, collecting large-scale normative data, and further exploring the state versus trait properties of neurocognitive measures through dense longitudinal designs [93] [96]. Integrating these tools with frameworks like the ANA holds promise for advancing a precision medicine approach to addictive disorders.
Substance use disorders (SUDs) represent a significant global public health challenge, characterized by high rates of relapse and considerable individual variation in treatment response [97]. The development of improved treatment options requires an advanced understanding of the neurocognitive heterogeneity underlying addiction [14]. Contemporary research has shifted from viewing addiction as a unitary disorder to recognizing it as a multi-faceted condition involving distinct neurobehavioral mechanisms that influence clinical trajectories. This systematic review synthesizes evidence on key neurocognitive constructs that predict addiction outcomes, focusing on their neural substrates, assessment methodologies, and implications for personalized intervention strategies. We examine three primary neurocognitive domains—approach-related behavior, executive function, and negative emotionality—and their interactions in shaping addiction vulnerability, maintenance, and recovery prospects.
Neurocognitive Constructs Predicting Addiction Trajectories
Key Domains and Their Predictive Value
Research consistently identifies three core neurocognitive domains that predict addiction trajectories, each with distinct neural substrates and behavioral manifestations [14].
1. Approach-Related Behavior (Reward Processing) This domain encompasses incentive salience attribution, reward sensitivity, and cue reactivity. It is mediated by a network including the ventral striatum, orbitofrontal cortex (OFC), and amygdala [98] [99]. Individuals with dominance in this domain show heightened neural responses to drug-related cues, which predicts craving intensity and relapse vulnerability. A machine learning model using fMRI drug cue reactivity successfully predicted craving intensity based on activity in the parahippocampal gyrus, superior temporal gyrus, and amygdala [100]. This "reward" profile is characterized by substance use driven by pleasure-seeking motives rather than coping mechanisms.
2. Executive Function (Cognitive Control) This construct involves working memory, inhibitory control, cognitive flexibility, and goal-directed planning. It primarily depends on the prefrontal cortex (PFC), particularly dorsolateral PFC (DLPFC) and anterior cingulate cortex (ACC) [98] [99]. Deficits in this domain predict poor treatment adherence, impaired decision-making, and inability to resist substance use impulses. The "cognitive type" subtype demonstrates lower executive function across multiple behavioral tasks and self-report measures [14]. Reduced activity in executive control networks is associated with compromised self-regulation in addiction.
3. Negative Emotionality (Stress Reactivity) This domain encompasses stress sensitivity, anxiety, negative affect, and emotional dysregulation. Key neural structures include the insula, amygdala, and medial PFC [99] [14]. Individuals with prominence in this domain often use substances to alleviate negative emotional states, forming a "relief" oriented pattern. The insula plays a crucial role in translating interoceptive signals into craving states, particularly during withdrawal or stress [99]. This profile predicts substance use in negative affective contexts and relapse during stressful life events.
Table 1: Neurocognitive Constructs Predicting Addiction Trajectories
| Neurocognitive Construct | Primary Neural Substrates | Behavioral Manifestations | Prediction Value for Trajectories |
|---|---|---|---|
| Approach-Related Behavior | Ventral striatum, OFC, amygdala | Enhanced drug cue reactivity, craving, reward sensitivity | Predicts cue-induced relapse, craving intensity [100] |
| Executive Function | DLPFC, ACC, frontoparietal network | Poor inhibitory control, decision-making deficits, cognitive rigidity | Predicts treatment adherence, ability to resist impulses [14] |
| Negative Emotionality | Insula, amygdala, medial PFC | Anxiety, stress reactivity, negative affect, emotional dysregulation | Predicts relapse during stress, negative reinforcement use [14] |
Neurobehavioral Subtypes and Their Trajectories
Latent profile analysis has empirically validated three distinct neurobehavioral subtypes in addiction, each with specific functional impairments and recovery trajectories [14]:
1. Reward Type (39.9% of SUD sample): Characterized by elevated approach tendencies, reward sensitivity, and cue reactivity. Neural connectivity alterations primarily involve Value/Reward, Ventral-Frontoparietal, and Salience networks.
2. Cognitive Type (40.5% of SUD sample): Defined by executive function deficits across multiple domains. Associated with connectivity patterns in Auditory, Parietal Association, Frontoparietal and Salience networks.
3. Relief Type (19.6% of SUD sample): Marked by high negative emotionality and affective dysregulation. Shows distinct connectivity in Parietal Association, Higher Visual and Salience networks.
These subtypes are distributed across different primary substances and genders, suggesting transdiagnostic applications [14]. Their identification enables more targeted interventions aligned with individual neurocognitive profiles.
Table 2: Neurobehavioral Subtype Characteristics and Implications
| Subtype | Prevalence in SUD | Primary Functional Impairment | Associated Neural Networks | Potential Intervention Focus |
|---|---|---|---|---|
| Reward Type | 39.9% | Elevated approach behavior, cue reactivity | Value/Reward, Ventral-Frontoparietal, Salience | Cue exposure therapy, neuromodulation of reward pathways |
| Cognitive Type | 40.5% | Executive function deficits | Auditory, Parietal Association, Frontoparietal, Salience | Cognitive remediation, executive function training |
| Relief Type | 19.6% | High negative emotionality | Parietal Association, Higher Visual, Salience | Emotion regulation skills, stress reduction techniques |
Assessment Methodologies and Experimental Protocols
Neuroimaging Approaches
fMRI Drug Cue Reactivity (FDCR) FDCR protocols measure brain responses to drug-related versus neutral cues using functional magnetic resonance imaging (fMRI). In a study with 69 participants with methamphetamine use disorder, participants completed an FDCR task while undergoing fMRI scanning [100]. They viewed drug-related and neutral cues while brain activity was recorded. Craving intensity was rated on a 1-4 scale after cue exposure. Machine learning pipelines employing multiple feature selection methods (ANOVA, PCA) and regression algorithms (linear regression, Lasso, Elastic Net, Random Forest, XGBoost) were evaluated to predict craving from brain activity patterns. Model performance was assessed using subject-level 5-fold cross-validation plus a 20% hold-out test set [100]. This approach achieved an RMSE of 0.983±0.026 and successfully classified high versus low craving levels (AUC-ROC=0.684±0.084).
Resting-State Functional Connectivity Resting-state fMRI captures intrinsic neural network architecture and identifies subtype-specific connectivity patterns. Participants undergo 6-10 minutes of rest while maintaining fixation, during which BOLD signal fluctuations are recorded [14]. Functional connectivity matrices are generated by correlating time series between brain regions. Network-based statistics then identify connectivity alterations associated with specific neurocognitive subtypes.
Computational Modeling of Temporal Dynamics
Dynamical systems theory (DST) applied to Ecological Momentary Assessment (EMA) data models the nonlinear relationships between cues, craving, and substance use in natural environments [101]. The protocol involves:
- EMA Data Collection: Participants receive electronic surveys 4 times daily for 14 days, reporting substance use, craving intensity (1-7 scale), and encountered cues.
- SARIMAX Modeling: Optimized linear Seasonal Auto-Regressive Integrated Moving Average with eXogenous variable models phenotype patients based on directionality between cues and craving.
- DST Model Implementation: Computational models replicate complex temporal dynamics, identifying either "maximum cue saturation" (cues→craving→use) or "maximum use saturation" (craving→cues→use) profiles [101].
This approach reveals craving as an essential modulator between cues and use, with distinct therapeutic implications for each profile.
Behavioral and Self-Report Measures
Comprehensive phenotypic assessment includes multiple instruments to capture the three core domains:
- Approach Behavior: Behavioral approach system (BAS) sensitivity, reward responsiveness, delay discounting tasks.
- Executive Function: Working memory tasks (n-back), inhibitory control (stop-signal, go/no-go), cognitive flexibility (task-switching).
- Negative Emotionality: Negative affect scales, distress tolerance measures, anxiety and depression inventories [14].
Factor analysis reduces these measures to latent constructs representing the core neurocognitive domains, enabling subtype classification through latent profile analysis.
Integration and Signaling Pathways
The triadic neurocognitive model conceptualizes addiction as arising from imbalanced interactions between three key systems [99]:
- Impulsive System: Amygdala-striatal circuits mediating automatic, habitual behaviors.
- Reflective System: Prefrontal circuits supporting self-regulation and future forecasting.
- Interoceptive System: Insula circuits translating bodily states into subjective experiences (craving).
This model proposes that the insula modulates dynamics between the impulsive and reflective systems, with insular hyperactivity during cue exposure exacerbating impulsive system activity while hijacking reflective system resources [99].
Diagram 1: Triadic neurocognitive model of addiction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Assessment Tools
| Tool/Category | Specific Examples | Primary Research Function | Domain Assessed |
|---|---|---|---|
| Neuroimaging Platforms | 3T fMRI, resting-state fMRI, task-based fMRI (FDCR) | Neural activity and connectivity mapping | All three domains (neural substrates) |
| Computational Modeling Tools | SARIMAX, Dynamical Systems Theory (DST) | Modeling temporal dynamics of cues, craving, use | Approach behavior, negative emotionality |
| Behavioral Tasks | Stop-signal, Go/No-Go, Delay Discounting, n-back | Objective executive function and decision-making assessment | Executive function, approach behavior |
| Self-Report Inventories | BAS/BIS scales, negative affect measures, craving ratings | Subjective experience and trait tendencies | All three domains (phenotypic expression) |
| Ecological Momentary Assessment | Mobile surveys, real-time tracking | Natural environment monitoring of symptoms | Negative emotionality, approach behavior |
Systematic evidence confirms that three neurocognitive constructs—approach-related behavior, executive function, and negative emotionality—robustly predict addiction trajectories through distinct yet interacting neural pathways. The identification of neurobehavioral subtypes (Reward, Cognitive, and Relief types) provides a validated framework for personalized addiction medicine [14]. Advanced assessment methodologies, including neuroimaging, computational modeling, and ecological momentary assessment, enable precise characterization of these constructs and their temporal dynamics.
Future research should focus on developing standardized protocols for subtype identification and matching interventions to individual neurocognitive profiles. Integration of multimodal assessment—combining neuroimaging, behavioral tasks, and real-time monitoring—holds particular promise for predicting treatment response and preventing relapse. The neurobiological validation of these assessment approaches strengthens their potential for transforming addiction care through mechanism-based subtyping and personalized intervention strategies.
Head-to-Head Comparison of Tool Feasibility in Primary Care Versus Specialist Settings
The feasibility of addiction assessment instruments is not merely a function of their psychometric properties but is profoundly shaped by the clinical environment in which they are deployed. In healthcare systems, a phenomenon termed "scope inversion"—where specialist physicians provide routine primary care—has been identified as a significant systems issue [102]. This practice is wasteful, diverting patients to more expensive care without improving outcomes and potentially creating environments where lengthy, complex assessments are less practical [102]. Quantitative studies reveal that specialists provide primary care in a substantial proportion of clinic visits, with estimates ranging from 2.6% to 65% depending on the specialty and healthcare system [102]. For instance, among children, 41.3% of visits with specialists were for routine follow-ups of conditions that could be managed in primary care [102].
This context is critical for understanding the divergent feasibility requirements of primary care versus specialist settings. Primary care is characterized by high patient volumes, shorter consultation times, and a broad scope of practice, necessitating instruments that are rapid, easy to administer, and minimally disruptive to clinical workflow [55]. In contrast, specialist settings, such as addiction treatment centers or academic research environments, often manage patients with more complex or severe disorders, potentially allowing for longer, more in-depth assessments [69] [103]. This comparative analysis examines the feasibility of various addiction assessment tools across these distinct clinical environments, focusing on administration time, format, user satisfaction, and integration into clinical workflow, all within the broader framework of neurobiological validation.
Comparative Feasibility Data of Assessment Instruments
Table 1: Head-to-Head Feasibility Comparison of Addiction Assessment Tools
| Instrument Name | Primary Setting Studied | Key Feasibility Metrics | Reported Administration Time | Recommended Format for Feasibility |
|---|---|---|---|---|
| TAPS (Tobacco, Alcohol, Prescription medication, and other Substance use) | Primary Care [55] | Good balance of ease of use, brevity, and comprehensive screening. | ~5-7 minutes | Self-administered (especially electronic) [55] |
| NIDA Phenotyping Assessment Battery (PhAB) | Specialist/Research [103] | Modular battery; 83% completion rate; high participant satisfaction. | ~3 hours (Core + Platform) [103] | Computer-based (e.g., Inquisit, REDCap) [103] |
| ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) | Primary Care [55] | Feasibility studied via audio-computer-assisted self-interview (ACASI). | Not specified | Audio-assisted self-interview (ACASI) [55] |
| BSTAD (Brief Screener for Tobacco, Alcohol, and other Drugs) | Primary Care (Adolescents) [55] | Brief screener for adolescent populations in primary care. | ~2-3 minutes | Ultra-brief (2-3 items) [55] |
| BrainPAC (BrainPark Assessment of Cognition) | Digital/Specialist [34] | Gamified tasks; validated for scalability and engagement. | ~60 minutes | Digitally gamified, self-administered [34] |
Table 2: User-Based Feasibility Criteria from Systematic Reviews
| Feasibility Criterion | Importance in Primary Care | Importance in Specialist Settings | Evidence Source |
|---|---|---|---|
| Administration Time | Critical; a major barrier [55] | Moderate; longer batteries accepted [103] | Systematic Review [55] |
| Format (Self-Admin vs. Interview) | Self-administered and electronic versions strongly preferred [55] | Flexible; can incorporate interviewer-led components [103] | Systematic Review [55] |
| Ease of Use/Comprehension | High priority for diverse patient populations | Important, but population may be more accustomed to assessments | Systematic Review [55] |
| Staff Training Required | Minimal training is a key facilitator [55] | More specialized training can be accommodated | Systematic Review [55] |
| Participant Satisfaction & Willingness | Contributes to long-term adherence | High satisfaction reported even for lengthy batteries (e.g., 90%+ in PhAB) [103] | Feasibility Study [103] |
Detailed Experimental Protocols & Methodologies
Protocol: Feasibility Testing in Primary Care (TAPS Tool)
Objective: To evaluate the feasibility of the TAPS tool for screening substance use disorders in primary care clinics [55].
Methodology Summary (Based on Wu et al., 2016 & McNeely et al., 2016):
- Setting & Population: Adult patients (≥18 years) in urban primary care clinics.
- Instrument Format: The TAPS tool was implemented as a self-administered, electronic instrument. This approach was selected to minimize staff involvement and integrate into clinical workflow.
- Feasibility Metrics Measured:
- Practicality: Administration time was a primary quantitative measure.
- Acceptability: Assessed via patient comprehension rates and ease-of-use ratings.
- Applicability: Determined by the tool's ability to be integrated into the standard clinical workflow without major disruptions.
- Implementation: The tool was designed for completion in waiting rooms or prior to consultations, leveraging electronic data capture to streamline the process.
Conclusion: The TAPS tool demonstrated a "good balance between ease of use, brevity of administration and more extensive screening," making it a feasible option for the high-volume, time-constrained primary care environment [55].
Protocol: Feasibility Testing in a Specialist Research Context (NIDA PhAB)
Objective: To assess the feasibility and participant burden of the NIDA Phenotyping Assessment Battery (PhAB) in a population including persons with Cocaine, Opioid, and Cannabis Use Disorders [103].
Methodology Summary (Based on Keyser-Marcus et al., 2021):
- Setting & Population: Participants (N=595) were recruited from various sources, including healthy controls and individuals with various SUDs, in a specialist research setting.
- Instrument Format: The PhAB is a modular battery comprising computer-based neurocognitive tasks (via Inquisit) and self-report scales (via REDCap). The "platform" design allows researchers to select relevant modules.
- Feasibility Metrics Measured:
- Completion Rate: The proportion of eligible participants who completed all assessments (83%).
- Participant Burden: Total administration time was meticulously recorded (average of 3 hours).
- Participant Satisfaction: A structured post-assessment interview quantified satisfaction and willingness to participate in similar future studies (over 90% endorsement).
- Implementation: Assessments were conducted over 1-3 study visits. The use of electronic data capture (REDCap) enhanced efficiency and data accuracy.
Conclusion: The NIDA PhAB was found to be an efficient and acceptable method for deep behavioral phenotyping in specialist addiction clinical trials, with high completion rates and satisfaction despite its longer duration [103].
Neurobiological Workflow & Feasibility Interface
The integration of neurobiologically validated tools into clinical practice requires a workflow that bridges biological mechanisms and practical constraints. The diagram below illustrates this interface, highlighting how core neurocognitive constructs map onto assessment tools and are filtered by the unique feasibility requirements of primary and specialist care settings.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Research Reagents and Digital Solutions for Feasibility Studies
| Item/Solution | Function in Feasibility Research | Exemplar Use in Literature |
|---|---|---|
| REDCap (Research Electronic Data Capture) | Electronic data capture platform for self-report measures; enhances efficiency, accuracy, and can include audio assistance for literacy/vision issues. | Used in NIDA PhAB study to administer self-report scales [103]. |
| Inquisit Millisecond Test Library | Software platform for deploying and running computerized neurocognitive tasks; allows for precise timing critical for cognitive assessment. | Hosts many tasks for the NIDA PhAB battery, promoting widespread adoption [103]. |
| Gamified Cognitive Tasks | Digitally redesigned neurocognitive paradigms that incorporate game elements to improve participant engagement and effort, especially in unsupervised settings. | Core principle of the BrainPAC battery, designed to enhance scalability and data quality [34]. |
| Audio-CASI (Computer-Assisted Self-Interview) | Technology that presents questions audibly to participants via headphones, reducing barriers related to literacy and potentially increasing honesty in self-report. | Studied as a feasible format for the ASSIST tool in primary care [55]. |
| Mechanical Turk (MTurk) | Online crowdsourcing platform used for rapid recruitment and validation of assessment tools in large, diverse community samples. | Used to validate the BrainPAC gamified tasks against standard laboratory paradigms [34]. |
Discussion: Integrating Neurobiology with Pragmatic Clinical Deployment
The head-to-head comparison reveals a clear divergence in feasibility parameters driven by fundamental setting constraints. Primary care demands ultra-brief, self-administered, and highly integrated tools like the TAPS, where a 5-minute administration time is a critical success factor [55]. The feasibility of these tools is paramount, as barriers like lack of time and integration into clinical workflow are major impediments to screening in this setting [55].
In contrast, specialist settings can leverage more comprehensive, neurobiologically-depthful instruments like the NIDA PhAB and BrainPAC, which require 60-180 minutes to complete but provide granular data on constructs like incentive salience, executive function, and negative emotionality [103] [34]. The high completion rates (83% for PhAB) and satisfaction ratings in these studies demonstrate that burden is relative to context and is acceptable when the assessment is perceived as relevant and is conducted in a supportive environment [103].
The future of addiction assessment lies in modular, scalable technologies that can bridge this gap. The NIDA PhAB's "platform" design and BrainPAC's gamified, digital nature are exemplars of this approach, allowing for tailored implementation [103] [34]. For a truly integrated care system, where the harmful effects of "scope inversion" are mitigated, tools must be developed with a clear understanding of the target environment's feasibility constraints, ensuring that validated, neurobiologically-informed assessments can be deployed effectively across the entire spectrum of care [102].
Conclusion
The neurobiological validation of addiction assessment instruments marks a critical evolution from descriptive phenomenology to an etiology-driven nosology. The synthesis of evidence confirms that frameworks like the ANA and tools such as digitally gamified batteries and AI-enhanced screeners provide a more precise, mechanistically grounded understanding of addictive disorders. These advances hold profound implications for biomedical and clinical research: they enable the identification of biologically distinct subtypes of addiction, which is a prerequisite for personalized medicine approaches in treatment development. Future research must focus on longitudinal studies to solidify the predictive power of these tools, the creation of normative datasets for clinical application, and the expansion of assessments to encompass behavioral addictions. Ultimately, this paradigm shift promises to de-stigmatize addiction, refine clinical trials, and catalyze the development of novel, neurobiologically-targeted therapeutics.
References
- 1. THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ... [https://www.ncbi.nlm.nih.gov/books/NBK424849/]
- 2. Drugs, Brains, and Behavior: The Science of Addiction - NIDA [https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain]
- 3. Addictions Neuroclinical Assessment: A Neuroscience- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4870153/]
- 4. Factors underlying the neurofunctional domains of ... [https://www.nature.com/articles/s41398-024-02987-9]
- 5. The Brain Disease Model of Addiction [https://www.hazeldenbettyford.org/research-studies/addiction-research/brain-disease-model]
- 6. DTMC Research Programs | National Institute on Drug Abuse [https://nida.nih.gov/about-nida/organization/divisions/division-therapeutics-medical-consequences-dtmc/research-programs]
- 7. Top 5 Trends in Neuroscience You Need to Know in 2025 [https://www.qmenta.com/blog/top-5-trends-in-neuroscience-you-need-to-know-in-2025]
- 8. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 9. Key Highlights from the 2025 American Neurological ... [https://www.neurologylive.com/view/key-highlights-from-2025-ana-annual-meeting]
- 10. Neurobiology of Addiction - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK597351/]
- 11. Which Are the Most Common Addiction Assessment Tools ... [https://metroatlantadetox.com/addiction-assessment-tools/]
- 12. Temporal Dynamics of Subtle Cognitive Change [https://www.jmir.org/2025/1/e55469]
- 13. Development and Validation of a Novel Screening Tool for ... [https://micronanoeducation.org/journal/volume-4-issue-1/development-and-validation-of-a-novel-screening-tool-for-predicting-substance-use-disorder-risk-using-machine-learning/]
- 14. Subtypes in addiction and their neurobehavioral profiles ... [https://www.nature.com/articles/s41398-023-02426-1]
- 15. emotional dysregulation is a critical driver of relapse to ... [https://www.nature.com/articles/s41398-024-03159-5]
- 16. The detrimental effects of emotional process dysregulation ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2012.00101/full]
- 17. Current perspectives on incentive salience and ... [https://www.sciencedirect.com/science/article/abs/pii/S2352154617301948]
- 18. The dark side of emotion: The addiction perspective [https://www.sciencedirect.com/science/article/abs/pii/S0014299915000151]
- 19. Emotion regulation in substance use disorders: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10087816/]
- 20. Assessing Addiction: Concepts and Instruments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2797097/]
- 21. Validity of nosological classification - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181576/]
- 22. DSM-5 Conceptual Changes: Innovations, Limitations and ... [https://tpcjournal.nbcc.org/dsm-5-conceptual-changes-innovations-limitations-and-clinical-implications/]
- 23. Diagnostic Concordance between DSM-5 and ICD-10 ... [https://www.sciencedirect.com/science/article/abs/pii/S0306460316300685]
- 24. Neurobiological Theories of Addiction: A Comprehensive ... [https://www.mdpi.com/2813-1851/3/1/3]
- 25. Frontiers | Why Psychiatric Research Must Abandon Traditional... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2017.00101/full]
- 26. Psychotherapy Research Domain Criteria: functional ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1549976/full]
- 27. A data-driven latent variable approach to validating the ... [https://www.nature.com/articles/s41467-025-55831-z]
- 28. Neuroscience-informed psychoeducation for addiction - PubMed [https://pubmed.ncbi.nlm.nih.gov/40012711]
- 29. Applying the Research Domain Criteria to Social ... [https://link.springer.com/article/10.1007/s10597-025-01508-2]
- 30. Commentary: Addictions Neuroclinical Assessment [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2017.00002/full]
- 31. Substance use disorders: a call for a staging paradigm [https://www.nature.com/articles/s41398-025-03484-3]
- 32. A Novel, Expert-Endorsed, Neurocognitive Digital Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7615064/]
- 33. Validation and comparison of virtual reality and 3D mobile ... [https://www.nature.com/articles/s41598-024-75065-1]
- 34. A Novel, Expert-Endorsed, Neurocognitive Digital ... [https://www.jmir.org/2023/1/e44414/]
- 35. Neurocognitive predictors of addiction-related outcomes [https://www.sciencedirect.com/science/article/pii/S0149763423002646]
- 36. Reactive and proactive control mechanisms of response ... [https://www.sciencedirect.com/science/article/abs/pii/S0165178118309983]
- 37. Undervaluing delayed rewards explains adolescents ... [https://www.nature.com/articles/srep42631]
- 38. How short video addiction affects risk decision-making ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1542271/full]
- 39. Perceived reward certainty in the assessment of delay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12419681/]
- 40. Construct Validity of the Balloon Analogue Risk Task (BART) [https://link.springer.com/article/10.1007/s10862-006-7487-5]
- 41. Delay Discounting Task | Overview, Applications, Data & ... [https://www.labvanced.com/content/research/en/blog/2025-06-delay-discounting-task/]
- 42. AI screening for opioid use disorder associated with fewer ... [https://nida.nih.gov/news-events/news-releases/2025/04/ai-screening-for-opioid-use-disorder-associated-with-fewer-hospital-readmissions]
- 43. DSCnet: detection of drug and alcohol addiction ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1607248/full]
- 44. A systematic review of machine learning applications in ... [https://www.nature.com/articles/s41746-024-01312-4]
- 45. UH/UC Researchers Use Machine Learning to Map Brain ... [https://www.uh.edu/news-events/stories/2025/april/04302025-heroin-brain-study.php]
- 46. Substance use prediction using artificial intelligence ... [https://link.springer.com/article/10.1007/s42001-024-00356-6]
- 47. Comparisons of Polyexposure, Polygenic, and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7985424/]
- 48. Externalizing as a common genetic influence for a broad ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586799/]
- 49. PGS005215 / Addiction risk factors (Polygenic Score) [https://www.pgscatalog.org/score/PGS005215/]
- 50. Using polygenic scores for identifying individuals at ... [https://www.nature.com/articles/s41398-020-00865-8]
- 51. The Craving Assessment Scale for Behavioral Addictions ... [https://pubmed.ncbi.nlm.nih.gov/41013925/]
- 52. Models of communication for polygenic scores and ... [https://www.sciencedirect.com/science/article/pii/S1098360022009467]
- 53. Analysis of polygenic risk score usage and performance in ... [https://www.nature.com/articles/s41467-019-11112-0]
- 54. Tobacco, Alcohol, Prescription Medication, and Other ... [https://www.c4tbh.org/program-review/tobacco-alcohol-prescription-medication-substance-use-taps-tool/]
- 55. Identifying available substance use disorder screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10874871/]
- 56. About the CRAFFT [https://crafft.org/about-the-crafft/]
- 57. Screening and Assessment Tools Chart - NIDA - NIH [https://nida.nih.gov/nidamed-medical-health-professionals/screening-tools-resources/chart-screening-tools]
- 58. Predictive Validity of the CRAFFT for Substance Use Disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC6855834/]
- 59. Validity of a brief screening instrument—CRAFFT in ... [https://www.sciencedirect.com/science/article/pii/S0306460310002406]
- 60. 使用多模态深度学习模型预测消防员的酒精使用障碍风险 [https://www.ebiotrade.com/newsf/2025-11/20251104000409883.htm]
- 61. 成瘾研究新纪元:神经生物学、社会影响与跨学科干预的深度 ... [https://www.forwardpathway.com/197456]
- 62. 外周血细胞生物标记物:成瘾诊疗新工具 [http://ibp.cas.cn/cb/kpbd/202508/t20250822_7908914.html]
- 63. 物质使用障碍患者的脑形态学改变与神经网络紊乱:海洛因与 ... [https://www.ebiotrade.com/newsf/2025-11/20251116000414726.htm]
- 64. a prospective study - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8690718/]
- 65. Feasibility and Acceptability of a Mobile-Assisted Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11663265/]
- 66. Addressing Barriers to Primary Care Screening and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8554188/]
- 67. The diagnostic accuracy of brief screening instruments for ... [https://www.sciencedirect.com/science/article/pii/S027273581930296X]
- 68. Design and Validation of an Addiction Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377693/]
- 69. Changes in neurobiological markers of reactivity to alcohol ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1613169/full]
- 70. A population study comparing screening performance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3235985/]
- 71. Moving Toward Neurobiological, Multidomain, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12516542/]
- 72. Comparison of self‐administered survey questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8152947/]
- 73. Psychometric properties and comparison with a text-based ... [https://www.sciencedirect.com/science/article/pii/S2451958825001290]
- 74. Navigating the Complex Intersection of Substance Use and ... [https://www.mdpi.com/2077-0383/13/4/999]
- 75. Psychiatric comorbidities and concurrent substance use ... [https://www.nature.com/articles/s41598-023-45633-y]
- 76. Psychiatric comorbidity in substance use disorders, a ... [https://www.sciencedirect.com/science/article/pii/S0149763425003264]
- 77. Psychiatric comorbidity in substance use disorders, a ... [https://pubmed.ncbi.nlm.nih.gov/40812726/]
- 78. Psychiatric comorbidities in substance use disorders: Sex- ... [https://www.medrxiv.org/content/10.1101/2025.09.11.25335563v1.full-text]
- 79. The International Work Addiction Scale (IWAS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC11974427/]
- 80. Measurement Invariance of Alcohol Instruments with Hispanic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4567959/]
- 81. Measurement invariance and comparison of the mobile phone ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-025-07057-y]
- 82. Identifying available addictive disorder screening tests ... [https://www.sciencedirect.com/science/article/pii/S0306460321003658]
- 83. Psychometric properties and measurement invariance across ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0323215]
- 84. The Clinical Relevance of Neurocognitive Measures ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2013.00185/full]
- 85. Clinical value of predicting relapse within 3 months in ... [https://www.nature.com/articles/s41598-025-89775-7]
- 86. Predicting Relapse in Substance Use [https://www.mdpi.com/2076-3425/12/7/957]
- 87. Validity and measurement invariance of the Addictions ... [https://pubmed.ncbi.nlm.nih.gov/33509416/]
- 88. Validity and measurement invariance of the Addictions ... [https://www.sciencedirect.com/science/article/abs/pii/S0740547220304840]
- 89. Neural correlates of the addictions neuroclinical assessment ... [https://pubmed.ncbi.nlm.nih.gov/38431152/]
- 90. Neural correlates of the addictions neuroclinical ... [https://www.sciencedirect.com/science/article/pii/S0166432824000822]
- 91. Neural Correlates of the Addictions Neuroclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11563703/]
- 92. The Design and Analysis of Multisite Effectiveness Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3232468/]
- 93. A Novel, Expert-Endorsed, Neurocognitive Digital ... [https://pubmed.ncbi.nlm.nih.gov/37624635/]
- 94. Naturalistic assessments across the lifespan: Systematic ... [https://www.sciencedirect.com/science/article/pii/S0149763424003841]
- 95. A Novel, Expert-Endorsed, Neurocognitive Digital ... [https://research.monash.edu/en/publications/a-novel-expert-endorsed-neurocognitive-digital-assessment-tool-fo]
- 96. Reliability of gamified reinforcement learning in densely ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10482292/]
- 97. Addiction and Substance Abuse [https://www.probiologists.com/article/ai-in-addiction-harnessing-technology-for-diagnosis-prevention-and-recovery-a-narrative-review]
- 98. A Systematic Review on Common and Distinct Neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10148787/]
- 99. Frontiers | A Triadic Neurocognitive Approach to Addiction ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2013.00179/full]
- 100. Craving Prediction From fMRI Drug Cue Reactivity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537833/]
- 101. a dynamical system analysis based on ecological ... [https://www.nature.com/articles/s41398-025-03531-z]
- 102. Provision of primary care by specialist physicians [https://pmc.ncbi.nlm.nih.gov/articles/PMC7046372/]
- 103. Development and feasibility study of an addiction focused ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8243823/]