Beyond the Cage: A Modern Framework for Validating Animal Behavior Assays in Human Disorder Modeling
This article provides a comprehensive guide for researchers and drug development professionals on the validation of animal behavior assays for modeling human neuropsychiatric disorders.
Beyond the Cage: A Modern Framework for Validating Animal Behavior Assays in Human Disorder Modeling
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the validation of animal behavior assays for modeling human neuropsychiatric disorders. It explores the foundational concepts of model validity, details methodological applications of common behavioral tests, addresses key challenges in reproducibility and translation, and presents modern frameworks for comparative model assessment. By synthesizing historical perspectives with current technological innovations and standardized validation tools, this resource aims to enhance the reliability and translational value of preclinical behavioral research, ultimately accelerating the development of effective therapeutics.
The Pillars of Validity: Understanding the Historical and Conceptual Foundations
In the pursuit of translating findings from basic animal research to clinical practice, the validity of animal models stands as a cornerstone of psychiatric and neurological drug development. The "triad of validity"—encompassing face, predictive, and construct validity—provides a critical framework for evaluating whether animal behavioral assays accurately model human psychiatric disorders [1] [2]. These criteria determine the extent to which preclinical findings can be meaningfully extrapolated to human conditions, thereby guiding resource allocation in drug development and reducing attrition rates in clinical trials. Within the specific context of animal behavior assays for human disorder modeling, each validity type interrogates a different aspect of the model's relevance: surface-level symptom resemblance (face), response to therapeutic interventions (predictive), and alignment with theoretical underpinnings (construct) [2]. This article deconstructs this triad, providing researchers with a comparative analysis of how these validity types function, their relative strengths and limitations, and their practical application in validating behavioral assays for drug discovery.
Deconstructing the Validity Triad: Definitions and Theoretical Foundations
The triad of validity was formally elaborated by Willner in 1984 and has since become the standard for evaluating animal models of psychiatric disorders [2]. Each component addresses a distinct dimension of the model's utility and biological relevance.
Face Validity is the most straightforward criterion, assessing whether the model appears to measure what it intends to measure based on superficial characteristics. In animal models, this translates to observable behavioral or biological outcomes that resemble the human condition [1]. For instance, anhedonic behavior (a core symptom of depression) in rodents, measured by a decreased preference for sucrose solution, is considered to have high face validity [1] [2]. However, face validity is often considered the weakest form of evidence because it is a subjective assessment based on appearance rather than underlying mechanisms [3] [4].
Predictive Validity evaluates how well performance on a test predicts performance on a criterion measured at a different time [3]. For animal models of psychiatric disorders, this primarily refers to the model's ability to correctly identify treatments that will be therapeutically effective in humans [1] [2]. Willner's original definition specified that a model with high predictive validity should identify pharmacologically diverse antidepressant treatments without making errors of omission or commission, and that potency in the model should correlate with clinical potency [2]. This validity is crucial for drug screening, as it directly impacts the pipeline of candidate compounds moving from preclinical to clinical stages.
Construct Validity is the most complex and theoretically grounded criterion. It assesses how well a test or measurement represents and captures an abstract theoretical concept, known as a construct [4]. A construct refers to an underlying trait (e.g., intelligence, anxiety) that cannot be directly observed but is measured through observable indicators [3] [5]. For an animal model, construct validity requires that the cognitive or biological mechanisms underlying the disorder are identical in both humans and animals [1] [2]. Establishing construct validity is an ongoing process that involves demonstrating the test's relationship with other variables and measures theoretically connected to the construct [4].
Table 1: Core Concepts of the Validity Triad
| Validity Type | Core Question | Key Strength | Primary Limitation |
|---|---|---|---|
| Face Validity | Does the model superficially resemble the human disorder? [2] | Intuitive and easy to assess initially [3] | Subjective; does not guarantee accuracy [4] |
| Predictive Validity | Does the model correctly predict treatment outcomes? [2] | Directly useful for drug screening and development [1] | Can be mechanistic; may not reflect etiology [2] |
| Construct Validity | Does the model accurately represent the theoretical construct? [4] | The most meaningful indicator of a model's true relevance [2] | Difficult and complex to establish fully [4] |
Comparative Analysis: Strengths, Limitations, and Interrelationships
While each validity type offers unique insights, a comprehensive animal model should strive to satisfy all three to maximize its translational value. The table below provides a detailed comparison of the three validity types, highlighting their role in animal behavior assays.
Table 2: Comparative Analysis of the Validity Triad in Animal Behavior Assays
| Aspect | Face Validity | Predictive Validity | Construct Validity |
|---|---|---|---|
| Primary Role in Research | Initial, superficial assessment of a model's plausibility [4] | Screening and prioritization of potential therapeutic compounds [2] | Understanding underlying disease mechanisms and etiology [2] |
| Evidence Required | Observable similarity in symptoms (e.g., anhedonia, reduced locomotion) or biomarkers (e.g., elevated corticosterone) [1] | Correlation between treatment effects in the model and known clinical effects in humans [1] [2] | Alignment with theoretical framework; shared biological and cognitive mechanisms [1] [4] |
| Dependence on Other Validity Types | Can exist independently but is weak alone; does not assure predictive or construct validity [4] | Often established independently for drug screening; may not require strong face or construct validity [2] | Considered the overarching form of validity; subsumes aspects of face and predictive validity [6] |
| Risk if Over-Relied Upon | Pursuing superficial symptom mimicry without relevance to the human condition's core pathology [2] | Developing "models" that are merely drug screening tools with no relevance to the human disease state [2] | Becoming mired in theoretical debates, hindering the practical development of useful models [2] |
The relationship between these validities is not always synergistic. A model can have high predictive validity without strong face or construct validity; for example, the Porsolt Forced Swim Test, a common assay for antidepressant activity, has good predictive validity but is often criticized for its poor construct and face validity regarding the human experience of depression [2] [7]. Conversely, a model might have high face validity but fail to predict treatment response. Construct validity is increasingly seen as the most fundamental, as it ensures that the model is truly engaging the neurobiological systems relevant to the human disorder, thereby increasing confidence that findings will translate [2].
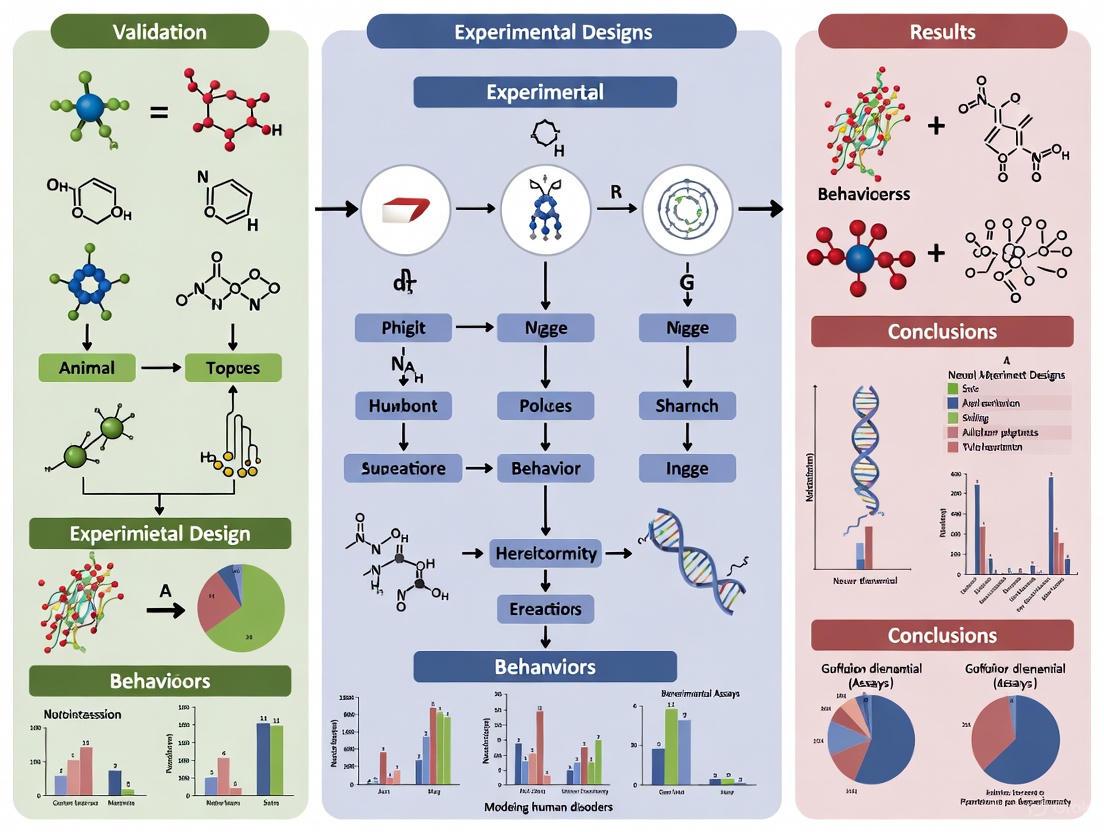
Figure 1: The Interrelationship of Validities in Animal Model Development. Construct validity is foundational, informing and supporting the establishment of face and predictive validity, with the collective goal of improving the model's translational relevance.
Experimental Protocols for Assessing Validity
Establishing the different types of validity requires distinct experimental approaches and protocols. Below are detailed methodologies for key behavioral assays that are central to validation in rodent models.
Assessing Face Validity: The Sucrose Preference Test for Anhedonia
Objective: To measure anhedonia, a core symptom of depression, by quantifying a rodent's inherent preference for a sweet-tasting sucrose solution over plain water [1] [2].
Protocol:
- Habituation: Animals are first habituated to the presence of two drinking bottles in their home cage, both containing plain water, for 48 hours.
- Water Deprivation: Following habituation, animals are mildly water-deprived for a short period (e.g., 4-18 hours) to ensure sufficient drinking motivation.
- Test Session: The two bottles are replaced—one with a 1-2% sucrose solution and the other with plain water. The positions of the bottles are counterbalanced between subjects to control for side preferences.
- Measurement: The animals are given free access to both bottles for a defined period (typically 1-24 hours). The consumption of sucrose solution and water is measured by weighing the bottles before and after the test.
- Calculation: Sucrose preference is calculated as: (Sucrose intake / Total fluid intake) × 100%. A significant reduction in this percentage in a test group compared to a control group is interpreted as anhedonic behavior, providing face validity for depression-like states.
Assessing Predictive Validity: The Elevated Plus Maze for Anxiety
Objective: To evaluate the anxiolytic (anxiety-reducing) effects of compounds by exploiting the natural conflict between a rodent's tendency to explore novel environments and its innate fear of open, elevated spaces [7].
Protocol:
- Apparatus: The maze consists of a plus-shaped platform elevated above the floor. It has two open arms (without walls) and two closed arms (with high walls), all connected by a central square.
- Pre-Test Handling: Animals are handled regularly for several days prior to testing to minimize stress.
- Test Session: The subject is placed in the central square, facing an open arm. Its behavior is recorded for a standard duration (e.g., 5 minutes).
- Key Behavioral Measures:
- Time spent in the open arms vs. closed arms.
- Number of entries into the open arms vs. closed arms.
- Risk-assessment behaviors (e.g., stretch-attend postures) at the entrance to the open arms.
- Validation: Anxiolytic drugs (e.g., benzodiazepines) are known to increase the proportion of time spent and number of entries into the open arms. A test compound that produces a similar behavioral profile demonstrates the assay's predictive validity for anxiolytic action [7].
Assessing Construct Validity: Fear Conditioning for Anxiety and Memory
Objective: To model the formation and expression of associative emotional memory, relevant to anxiety disorders (e.g., PTSD), by pairing a neutral stimulus with an aversive one [7].
Protocol:
- Apparatus: A specialized chamber with a grid floor for delivering mild foot shocks and features for presenting a conditioned stimulus (CS), such as a light or tone.
- Acquisition (Day 1): The animal is placed in the chamber. After a habituation period, a neutral CS (e.g., a 30-second tone) is presented, which coterminates with a mild, aversive unconditioned stimulus (US), such as a 1-second foot shock. This pairing is repeated several times.
- Contextual Memory Test (Day 2): The animal is placed back into the same chamber without any tone or shock. The amount of time spent freezing (a species-typical fear response) is measured. Freezing in this context indicates learning of the association between the environment (context) and the shock.
- Cued Memory Test (Day 2, later): The animal is placed in a novel, distinctly different chamber. After a habituation period, the CS (tone) is presented in the absence of the shock. Freezing during the tone presentation indicates learning of the association between the discrete cue and the shock.
- Construct Validation: This assay has strong construct validity because the neurocircuitry underlying this form of learning (heavily dependent on the amygdala and hippocampus) is highly conserved between rodents and humans, and the cognitive process of associative learning is directly relevant to the etiology of certain anxiety disorders [7].
Figure 2: Fear Conditioning Workflow for Construct Validity. This two-day protocol assesses the formation and expression of associative fear memory, tapping into specific, conserved neural circuits to provide strong construct validity for anxiety and memory disorders.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents, equipment, and software solutions essential for conducting and analyzing the behavioral assays discussed in this article.
Table 3: Essential Research Reagents and Solutions for Behavioral Assays
| Item Name | Specific Function | Application in Validity Assessment |
|---|---|---|
| Sucrose Solution (1-2%) | Serves as a hedonic stimulus to quantify anhedonia via consumption preference. | Core reagent for the Sucrose Preference Test, used to establish face validity for depression models [1]. |
| EthoVision XT Tracking Software | Automated video tracking system that quantifies locomotor activity, time in zones, and complex behaviors. | Used across multiple assays (Open Field, EPM, MWM) to provide objective, high-throughput behavioral data for face, predictive, and construct validity [7]. |
| Elevated Plus Maze Apparatus | Creates an approach-avoidance conflict; used to measure anxiety-like behavior based on time in open vs. closed arms. | Standard equipment for screening anxiolytic drugs, central to establishing predictive validity [7]. |
| Fear Conditioning Chamber | Controlled environment for administering precise conditioned (tone/light) and unconditioned (mild foot shock) stimuli. | Foundational apparatus for studying associative learning and memory, providing robust construct validity for anxiety and PTSD models [7]. |
| Morris Water Maze Pool | Apparatus for testing spatial learning and memory by requiring animals to find a submerged hidden platform using distal cues. | Key test for hippocampal-dependent learning, used to assess cognitive deficits and construct validity in models of neurodegenerative disorders [7]. |
| Known Psychoactive Compounds (e.g., Benzodiazepines, SSRIs) | Gold-standard therapeutics used as positive controls to verify that an assay responds to clinically effective treatments. | Critical for establishing predictive validity in any behavioral model intended for drug discovery [2]. |
| Rotarod Apparatus | Measures motor coordination and balance by testing the animal's ability to stay on a rotating rod. | Control assay to rule out motor deficits that could confound interpretation of primary behavioral tests, supporting internal validity [7]. |
The triad of face, predictive, and construct validity provides an indispensable, multi-faceted framework for deconstructing and evaluating animal behavior assays in psychiatric research. While face validity offers an intuitive check for symptom mimicry and predictive validity is paramount for efficient drug screening, construct validity remains the most rigorous standard for ensuring a model's true relevance to human disease mechanisms. A model strong in all three areas offers the greatest promise for translational success. As the field advances, with emerging technologies like artificial intelligence beginning to augment behavioral analysis [8], these core validity principles will continue to guide the development of more refined, reliable, and human-relevant animal models, ultimately accelerating the discovery of novel therapeutics for psychiatric and neurological disorders.
The development of effective treatments for human psychiatric disorders relies heavily on the availability of preclinical animal models that accurately recapitulate aspects of human disease. The value of these models is determined by specific validation criteria that have evolved significantly over the past half-century. This progression reflects the scientific community's deepening understanding of disease complexity and a growing emphasis on translational relevance. The validation framework began with relatively simple, pragmatic checklists and matured into a sophisticated, multi-dimensional system for evaluating how well animal models predict human therapeutic outcomes. Understanding this evolutionary pathway—from the initial criteria proposed by McKinney and Bunney to the widely adopted Willner framework and subsequent refinements—is essential for researchers designing robust experiments and accurately interpreting preclinical data in the context of human psychiatric conditions such as depression and anxiety [9] [10].
This guide objectively compares these foundational validation frameworks, providing researchers with a clear reference for evaluating animal models in their own work. The subsequent sections will detail the historical development, compare the core criteria, present experimental case studies, and outline contemporary methodological best practices.
Historical Development of Validation Criteria
The conceptual framework for validating animal models has shifted from a primary focus on internal consistency and pragmatic drug screening toward a greater emphasis on external and translational validity.
The Initial Framework: McKinney & Bunney (1969)
McKinney and Bunney were the first to formally propose criteria focused on the external validity of animal models, specifically for affective disorders. Their original paper outlined five key requirements for an animal model, which later literature often condenses and summarizes as focusing on four main areas [9] [10]:
- Similarity of Symptoms (Analogous Symptoms): The animal model should display behavioral changes analogous to human symptoms.
- Observable and Measurable Behavioral Changes: The behaviors must be quantifiable and consistent.
- Similar Response to Treatments: Effective treatments in humans should also be effective in the model.
- Biological Similarity: This includes similarities in etiology and underlying biochemistry, though these were not as explicitly detailed in their original list as commonly believed [9].
The Consolidation: Willner's Triadic Criteria (1984)
In 1984, Paul Willner simplified and restructured the existing ideas into a triad of validity criteria that have become the standard in the field. This framework drew inspiration from psychological validation concepts proposed earlier by Cronbach and Meehl. Willner's three criteria are [9] [10]:
- Predictive Validity: The model's ability to correctly identify therapeutic treatments.
- Face Validity: The phenomenological similarity of the model's manifestations to the human condition (symptoms).
- Construct Validity: The theoretical rationale behind the model—how well the model reflects the underlying theoretical constructs of the human disorder.
Modern Refinements: Belzung & Lemoine (2011)
Responding to the limitations of Willner's framework, Belzung and Lemoine proposed a more granular set of five criteria to better align with modern, multifactorial disease concepts like the diathesis model of depression [9]:
- Homological Validity: Appropriateness of the species and strain used.
- Pathogenic Validity: Similarity in the factors that trigger the disorder.
- Mechanistic Validity: Identity of the underlying biological and cognitive mechanisms.
- Face Validity: Similarity in observable behavioral and biological outcomes.
- Predictive Validity: Identity in the relationship between triggers/treatments and outcomes.
Table 1: Chronological Evolution of Animal Model Validation Criteria
| Timeline | Proponent(s) | Core Criteria | Primary Focus and Advancement |
|---|---|---|---|
| 1969 | McKinney & Bunney | • Similarity of Symptoms• Observable/Measurable Behavior• Similar Response to Treatments• Biological Similarity | Established the first structured set of external validity criteria, moving beyond simple pragmatic screens [9]. |
| 1984 | Willner | • Predictive Validity• Face Validity• Construct Validity | Consolidated prior concepts into a seminal, simplified tripartite framework that became the field standard [9] [10]. |
| 2011 | Belzung & Lemoine | • Homological Validity• Pathogenic Validity• Mechanistic Validity• Face Validity• Predictive Validity | Refined and expanded the criteria into a more nuanced, multi-factorial set to better capture complex disorder etiology [9]. |
Comparative Analysis of Core Validation Criteria
The following table provides a detailed comparison of the three main validation frameworks, highlighting their definitions, key components, and associated challenges.
Table 2: Detailed Comparison of Core Validation Criteria Across Frameworks
| Criterion | Definition & Key Aspects | McKinney & Bunney (1969) | Willner (1984) | Belzung & Lemoine (2011) |
|---|---|---|---|---|
| Predictive Validity | Definition: The model's ability to predict unknown aspects of the human condition, particularly therapeutic response. | Similar Response to Treatments: Focused on the model's correct identification of known effective therapies [9]. | Core Criterion: Explicitly defined as the ability to identify antidepressant treatments accurately [9]. | Subdivided into: • Induction Validity: Link between trigger and outcome.• Remission Validity: Effects of treatments [9]. |
| Challenges: A model with high predictive validity may lack mechanistic insight [10]. | ||||
| Face Validity | Definition: The superficial, phenomenological similarity between the model and the human disorder. | Analogous Symptoms: Explicitly included the need for symptom similarity in the model [9]. | Core Criterion: Similarity in symptoms between the animal model and the human condition [10]. | Subdivided into: • Ethological Validity: Observable behaviors (e.g., anhedonia).• Biomarker Validity: Biological measures (e.g., elevated corticosterone) [9]. |
| Challenges: Relies on surface-level comparisons; human psychiatric symptoms can be difficult to assess in animals [9]. | ||||
| Construct Validity | Definition: How well the model reflects the theoretical construct and known etiology of the human disorder. | Implied in "Cause": Similarity of cause was mentioned, but not as a fully developed criterion [9]. | Core Criterion: The theoretical rationale for the model—whether the mechanisms inducing the state in animals are analogous to those in humans [9] [10]. | Expanded into three criteria: • Homological Validity (Species/Strain)• Pathogenic Validity (Ontopathogenic/Triggering)• Mechanistic Validity (Biological/Cognitive mechanisms) [9]. |
| Challenges: Requires a well-understood and agreed-upon disease etiology, which is often lacking in psychiatry [9]. |
Diagram 1: The evolution of validation criteria from broad foundations to a consolidated triad and finally a detailed multifactorial system.
Experimental Validation: A Case Study in Depression Models
To illustrate the application of these validity criteria, we examine a direct comparative study of two rodent models of depression: the well-established Chronic Mild Stress (CMS) model and a newer Ultrasound-Induced (US) model [11].
Experimental Protocol and Methodologies
This study employed a standardized comparison of the CMS and US models in male Wistar rats (n=60). The detailed protocols were as follows [11]:
- Chronic Mild Stress (CMS) Protocol: Rats were exposed to a 3-week schedule of unpredictable, mild stressors. The protocol included periods of food deprivation, water deprivation, intermittent lighting, cage tilting, stroboscopic illumination, and housing in soiled cages or with unfamiliar partners. This variability prevents habituation and is a key feature of the CMS paradigm [11].
- Ultrasound-Induced (US) Protocol: Rats were continuously exposed for 3 weeks to variable-frequency ultrasound (20–45 kHz) at 50 ± 5 dB. The frequencies changed unpredictably every 10 minutes, simulating a state of "informational uncertainty" or a negative information flow, which is posited to mimic a core aspect of human psychological stress [11].
- Behavioral and Biological Endpoints: One day post-stress, animals underwent a battery of tests in this sequence: sucrose preference test (for anhedonia), social interest test, open field test, forced swim test (for behavioral despair), and the Morris water maze (for cognitive function). Plasma levels of corticosterone, epinephrine, norepinephrine, and dopamine were also measured [11].
Quantitative Results and Validity Assessment
The data from this comparative study were used to assess each model against the three primary validity criteria.
Table 3: Experimental Data Comparison: CMS vs. Ultrasound-Induced Model
| Test / Measure | Chronic Mild Stress (CMS) Model Outcomes | Ultrasound-Induced (US) Model Outcomes | Implication for Validity |
|---|---|---|---|
| Sucrose Preference | Decreased preference, indicating anhedonia [11]. | More pronounced decrease in preference, indicating stronger anhedonia [11]. | Face Validity: Anhedonia is a core symptom of depression. Both models show face validity, with the US model showing a stronger effect [11]. |
| Social Interaction Test | Reduced social interaction [11]. | More pronounced social isolation [11]. | Face Validity: Social withdrawal is a key symptom. The US model produced a more pronounced effect [11]. |
| Forced Swim Test | Increased immobility time [11]. | Increased immobility time [11]. | Face/Predictive Validity: Behavioral despair is a common endpoint; reversal by antidepressants confers predictive validity [11]. |
| Hormone & Neurotransmitter Levels | Dysregulation of the HPA axis and monoamines is known from literature. | Increased corticosterone, epinephrine, norepinephrine; reduced dopamine [11]. | Construct Validity: These biological changes mirror those seen in human depression, supporting the construct validity of both, and specifically demonstrated for the US model [11]. |
| Antidepressant Response | Reversal of behavioral deficits by known antidepressants (from established literature) [11]. | Reversal of behavioral deficits by various antidepressant classes [11]. | Predictive Validity: The ability to detect efficacy of standard treatments is a cornerstone of predictive validity. Both models demonstrate this [11]. |
The study concluded that while the established CMS model is valid, the novel US model is also suitable and meets all three required validity criteria, in some behavioral domains (anhedonia, social isolation) producing even more pronounced effects [11].
Essential Methodologies for Contemporary Behavioral Assays
Modern validation of animal models extends beyond theoretical criteria to incorporate rigorous methodological standards that ensure reliability and reproducibility.
The Pillars of Reproducible Experimental Design
To minimize bias and environmental variables, well-conceived behavioral experiments must adhere to several key principles [12]:
- Blinding: The technician conducting behavioral evaluations and analysis should be unaware of the treatment groups. If blinding is impossible due to visual cues, an independent technician should perform the final data interpretation [12].
- Randomization and Counterbalancing: Test subjects must be randomly assigned to treatment groups. When baseline testing is involved, groups should be counterbalanced for performance levels and body weight to avoid bias. The order of testing across days and apparatuses must also be randomized [12].
- Appropriate Controls: Vehicle control groups are essential and must be treated identically to the test compound group, including matching formulation excipients and injection procedures, to control for handling-induced stress [12].
- Sample Size Justification: Group sizes of 10-20 per sex per treatment are typically required to achieve statistical power. Small, underpowered pilot studies can be used for power calculations but should be confirmed in a second, independently powered cohort. Sexes should not be combined without statistical justification [12].
Technological Advances in Behavioral Data Capture
The move from manual observation to automated, computer-based systems has significantly improved the objectivity, throughput, and depth of behavioral analysis.
- Automated Video Tracking Systems: Software like EthoVision XT, AnyMaze, and TopScan uses pattern analysis of video images to extract quantitative measurements of animal behavior, such as location, distance traveled, and speed [13]. These systems are superior for measuring brief behaviors, long-duration activities, and precise spatial measurements that are difficult for human observers to estimate accurately [13].
- Custom and Open-Source Solutions: While commercial software is common, there is a growing demand for cost-effective and user-friendly alternatives. The development of in-house software, such as the Advanced Move Tracker (AMT), demonstrates the ability to produce data that correlates highly with both manual observation and commercial systems, providing a valid and accessible tool for researchers [13].
- Bio-logger Validation: For studies using wearable activity loggers on animals, validation is critical. A simulation-based methodology using synchronized video and raw sensor data allows researchers to validate data collection strategies (like intermittent sampling or data summarization) before deploying loggers in the field, ensuring the reliability of the inferred behavioral data [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Behavioral Validation Experiments
| Item Category | Specific Examples | Function in Validation |
|---|---|---|
| Animal Models | Wistar rats, C57BL/6 mice, Transgenic lines (e.g., Smn1/hSmn2 for SMA). | Subject for behavioral phenotyping. Strain/species choice is part of homological validity [10] [11] [13]. |
| Pharmacologic Agents | Diazepam (anxiolytic), Known Antidepressants (e.g., Imipramine, Fluoxetine), Test Compounds. | Positive controls for predictive validity (e.g., demonstrating an anxiolytic effect) and for testing novel treatments [12] [11]. |
| Hormone/Neurotransmitter Assay Kits | Corticosterone ELISA, Catecholamine (Epinephrine, Norepinephrine, Dopamine) ELISA/HPLC kits. | To measure biomarker-level changes for construct and face validity (biomarker validity) [9] [11]. |
| Automated Tracking Software | EthoVision XT (Noldus), AnyMaze, TopScan, Custom solutions (e.g., Advanced Move Tracker). | To provide objective, high-throughput, and reliable quantification of animal behavior, minimizing observer bias and fatigue [13]. |
| Specialized Behavioral Equipment | Sucrose Dispensers, Open Field Arenas, Elevated Plus Mazes, Forced Swim Tanks, Morris Water Maze. | To conduct standardized tests that operationalize and measure specific behavioral domains relevant to the human disorder (face validity) [11] [13]. |
Diagram 2: A modern workflow for validating animal behavior assays, integrating rigorous experimental design, technical proficiency, and advanced technology.
The field of psychiatric research is undergoing a fundamental transformation in how mental disorders are conceptualized and studied. For decades, the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD) framework has dominated psychiatric classification and research, operating on a neo-Kraepelinian assumption that mental disorders represent largely discrete entities characterized by distinctive signs, symptoms, and natural histories [15]. This DSM-ICD approach adopts an Aristotelian model of categorization, presuming that psychiatric disorders differ qualitatively from both normality and from each other [15]. While this system has provided a common language for clinicians and researchers and has demonstrated some treatment validity through the development of empirically supported therapies for specific disorders, growing anomalies within the DSM-ICD system have prompted a scientific reevaluation [15].
In response to these limitations, the National Institute of Mental Health (NIMH) launched the Research Domain Criteria (RDoC) initiative, which embraces a Galilean view of psychopathology as the product of dysfunctions in neural circuitry [15]. Central to this new approach is the concept of the endophenotype – heritable, quantifiable intermediate behavioral phenotypes that serve as a causal link between genes and observable symptoms in neuropsychiatric and neurological disorders [16]. This paradigm shift represents more than just a change in terminology; it constitutes a fundamental restructuring of how researchers conceptualize, measure, and investigate mental disorders, with profound implications for animal model development and validation in preclinical research.
Defining the Paradigms: Core Concepts and Criteria
The DSM-ICD Syndrome Approach
The DSM-ICD framework has served as the overarching model of psychiatric classification since at least the middle of the past century. This system is fundamentally syndromic, focusing on clinical symptom clusters that co-occur in ways that suggest underlying disorders. The approach emphasizes the differentiation of conditions based on their signs, symptoms, and natural history, providing standardized diagnostic criteria and algorithms for each diagnosis [15]. This model facilitated improved inter-rater reliability and created a common diagnostic language, but it suffers from significant limitations for research purposes, including heterogeneity within diagnostic categories, symptom overlap between disorders, and a lack of clear connection to underlying biological mechanisms [17] [15].
The Endophenotype Approach
Endophenotypes are defined as measurable components along the pathway between genotype and disease, requiring special processes or instruments for detection [16]. They can include neurophysiological, biochemical, endocrinological, neuroanatomical, cognitive, or neuropsychological measures and are believed to have a closer relationship to the underlying disease genotype than broader syndromic classifications [16]. The concept was originally introduced in psychiatry by Gottesman and Shields in the early 1970s to address the challenge of linking genes to complex psychiatric conditions by dividing behavioral symptoms into more stable phenotypes [16].
Table 1: Validation Criteria for Endophenotypes
| Criterion | Description | Research Application |
|---|---|---|
| Association with Illness | The endophenotype must be associated with the illness in the population | Serves as a measurable indicator linked to the disorder of interest |
| Heritability | The endophenotype must be heritable | Indicates a genetic component that can be systematically studied |
| State Independence | Manifest whether illness is active or in remission | Not merely an episode-dependent symptom but a stable trait |
| Familial Co-segregation | Co-segregates with illness within families | Higher prevalence in unaffected relatives of probands than in general population |
| Reliable Measurement | Amenable to reliable quantification and specific to illness | Provides objective, reproducible metrics for research |
Rigorous criteria define true endophenotypes, including association with illness, heritability, state independence (manifesting whether illness is active or in remission), co-segregation within families, and reliable measurement [18] [16]. These traits can be present in both affected individuals and their unaffected relatives, reflecting dimensional behavioral variation and genetic risk independent of actual disease manifestation [16]. This characteristic makes them particularly valuable for genetic studies and for investigating vulnerability mechanisms.
Comparative Analysis: Paradigm Strengths and Limitations
Table 2: DSM-Syndromic vs. Endophenotype Model Comparison
| Feature | DSM-Syndromic Model | Endophenotype Model |
|---|---|---|
| Classification Basis | Clinical symptom clusters | Neurobiological, cognitive, and neurophysiological measures |
| Genetic Connection | Indirect and heterogeneous | Direct, closer to genetic underpinnings |
| Measurement Approach | Clinical observation and patient report | Laboratory-based quantitative measures |
| Disorder Boundaries | Categorical divisions | Dimensional, often transdiagnostic |
| Research Utility | High clinical face validity, but heterogeneous groupings | Reduced heterogeneity, increased statistical power for genetic studies |
| Primary Limitations | Comorbidity, diagnostic overlap, biological heterogeneity | May not capture full clinical syndrome, requires specialized assessment |
The shift from DSM syndromes to endophenotypes addresses several fundamental challenges in psychiatric research. The endophenotype approach reduces heterogeneity by dissecting complex neurobiological traits and disorders into more elementary, quantifiable components [16]. This decomposition provides more direct links to biological pathways and increases statistical power in genetic studies by working with phenotypes closer to the gene effects [16]. Furthermore, endophenotypes facilitate translational research through cross-species compatibility, as many neurophysiological and cognitive measures can be assessed in both humans and animal models [16] [17].
However, the endophenotype approach is not without limitations. The lack of diagnostic specificity makes endophenotypes easier to detect but non-diagnostic [16]. Many endophenotypes are shared across various neuropsychiatric disorders, and boundaries between disorders dissolve when using an endophenotype approach [16]. This transdiagnostic characteristic enhances biological validity but complicates clinical application. Additionally, establishing endophenotypes requires rigorous validation, including longitudinal and family-based studies to establish trait stability and familial co-segregation [16].
Experimental Validation: Behavioral Assays and Their Neural Correlates
The validation of animal models in neuroscience requires a multidisciplinary approach with careful consideration of scientific criteria including replicability/reliability, predictive validity, construct validity, and external validity/generalizability [17]. Animal models are defined as living organisms used to study brain-behavior relations under controlled conditions, with the final goal of enabling predictions about these relations in humans [17]. The endophenotype approach facilitates this process by focusing on elemental phenotypes that are observable, measurable, and testable in both humans and animals [17].
Table 3: Representative Behavioral Assays for Key Endophenotypes
| Behavioral Assay | Measured Endophenotype | Neural Substrates | Translational Relevance |
|---|---|---|---|
| Prepulse Inhibition (PPI) | Sensorimotor gating | Complex brainstem-mediated reflex pathways | Schizophrenia, major depression |
| Morris Water Maze | Spatial navigation, reference memory | Hippocampus, entorhinal cortex | Alzheimer's disease, cognitive aging |
| Novel Object Recognition | Recognition memory | Dorsal hippocampus | Cognitive deficits across disorders |
| Conditioned Freezing | Fear conditioning, emotional memory | Amygdala (cued), hippocampus (contextual) | Anxiety disorders, PTSD |
| Social Preference Test | Sociability, social novelty | Multiple systems including prefrontal circuits | Autism spectrum disorder models |
| 5-Choice Serial Reaction Time | Attention, impulsivity, executive function | Prefrontal-striatal circuits | ADHD, cognitive control deficits |
Methodological Protocols for Key Behavioral Assays
Prepulse Inhibition (PPI) Protocol: PPI is an established method for testing sensorimotor gating that is abnormal in conditions such as schizophrenia [19]. The assay measures the reduction in startle response when a startling stimulus is preceded by a weaker, non-startling stimulus (prepulse). The acoustic startle response (ASR) and tactile startle reflex (TSR) evaluate complex brainstem-mediated reflex pathways [19]. Responses are similar in humans and rodents, offering homologous cross-species comparability [19]. Experimental sessions typically consist of multiple trial types including pulse-alone trials, prepulse-pulse trials, and no-stimulus trials, with startle magnitude measured using specialized equipment.
Morris Water Maze Protocol: This is the most widely used test for measuring spatial navigation and reference memory [19]. The animal is placed in an open, circular pool of room temperature water with a submerged platform. Over a series of trials, the animal learns to use distal cues located outside the maze to spatially navigate to the platform despite being placed in the maze at different starting positions [19]. Mice typically require a one-day training session to swim to a visible platform, followed by 5 days of learning to navigate to a hidden platform [19]. Rats typically do not require the initial training day. A probe trial with the platform removed assesses reference memory. The test relies on an intact hippocampus and entorhinal cortex [19].
Novel Object Recognition Protocol: This test uses the animal's reaction to a novel object within the context of familiar objects as a test of recognition memory [19]. First, the animal is familiarized with two or four identical objects. After a predetermined interval (which can be varied to test different memory retention periods), it is placed back in the test chamber with identical copies of the original objects and one new object [19]. Time spent exploring the novel object in preference to the familiar objects reflects memory of what has changed. This test is mediated by the dorsal hippocampus [19] and provides a measure of recognition memory that is translatable across species.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Materials for Endophenotype Investigation
| Research Tool Category | Specific Examples | Primary Research Application |
|---|---|---|
| Behavioral Apparatus | Acoustic startle chambers, Morris water maze, elevated zero maze, operant conditioning chambers | Quantitative assessment of specific behavioral endophenotypes |
| Pharmacological Agents | Indirect dopaminergic agonists, selective dopamine D1/D2 agonists/antagonists, cholinergic-muscarinic antagonists, glutamatergic-NMDA receptor antagonists | Manipulation of specific neurotransmitter systems to probe neural mechanisms |
| Video Tracking Systems | AnyMaze, EthoVision, custom SAS analysis programs [19] | Automated, objective behavioral quantification with minimal observer bias |
| Genetic Modification Tools | CRISPR-Cas9, transgenic animal models, selective breeding protocols | Investigation of genetic contributions to endophenotype expression |
| Neurophysiological Recording | EEG/ERP systems, in vivo electrophysiology, photometry systems | Direct measurement of neural activity correlates of behavioral endophenotypes |
The investigation of endophenotypes requires specialized research tools and approaches. Behavioral apparatus forms the foundation for endophenotype assessment, with specific tasks designed to measure particular neurobehavioral domains [19]. Pharmacological challenges are frequently employed to probe neurotransmitter systems involved in endophenotype expression, using targeted agonists and antagonists to temporarily alter neural function [19]. Advanced video tracking systems with associated analysis software enable precise, automated behavioral quantification that minimizes observer bias and enhances reproducibility [19]. Genetic manipulation tools allow researchers to investigate specific genetic contributions to endophenotypes, creating models with particular genetic variations associated with human disorders. Finally, neurophysiological recording techniques provide direct measures of neural activity that correlate with behavioral endophenotypes, bridging the gap between brain function and behavior.
Visualizing the Paradigm Shift: Conceptual Framework
Conceptual Framework of the Modeling Paradigm Shift
The diagram illustrates the fundamental differences between the traditional DSM-ICD syndrome model and the emerging endophenotype approach. The DSM model (red) begins with clinical symptom clusters as its foundation, which leads to challenges with heterogeneity and symptom overlap between disorders. In contrast, the endophenotype model (blue) is grounded in biological mechanisms, quantitative measures, and cross-species compatibility. Genetic risk factors (green) directly influence multiple categories of endophenotypes, including neurophysiological, cognitive, and neuroanatomical measures, which collectively contribute to the comprehensive endophenotype model. The dashed yellow arrow represents the paradigm shift from syndrome-focused to mechanism-focused approaches in psychiatric research.
The shift from DSM syndromes to endophenotypes represents more than a theoretical debate – it has practical implications for how researchers design studies, select animal models, and develop new therapeutics. This paradigm transition supports a more mechanistic approach to psychiatric research that emphasizes understanding the neurobiological pathways between genetic vulnerability and behavioral expression. The endophenotype approach facilitates the development of animal models with stronger translational validity by focusing on conserved biological and behavioral mechanisms that can be reliably measured across species [17].
For drug development professionals, this shift offers the potential for target engagement biomarkers that can guide early-stage clinical trials and help identify patient subgroups most likely to respond to specific mechanisms of action. The RDoC framework, which incorporates endophenotypes, aims to classify disorders based on biological and psychosocial features rather than clinical diagnosis alone, promoting integration from genes to neural systems to behavior [16]. As this paradigm continues to evolve, it promises to enhance the precision and efficacy of both basic research and therapeutic development in psychiatry and neurology.
Behavioral assays represent a cornerstone of preclinical neuroscience research, providing critical tools for investigating neuropsychiatric disorders, cognitive functions, and therapeutic interventions. These systematic procedures enable researchers to quantify behavioral responses in model organisms, bridging the gap between biological mechanisms and complex behavioral phenotypes. As the field moves toward dimensional approaches that focus on specific symptom clusters rather than attempting to model entire complex syndromes, the optimization and validation of these assays become increasingly important for translational success. This review examines the fundamental principles, applications, and methodological considerations of behavioral assays in neuroscience research, with particular emphasis on their validation for modeling human disorders and evaluating novel therapeutic agents. We compare established behavioral paradigms, detail experimental protocols, and provide a framework for assay implementation that ensures reliability and reproducibility across laboratories.
Behavioral assays are systematic procedures used in neuroscience to qualitatively assess and quantitatively measure specific behavioral responses in model organisms. Unlike chemical assays that detect substances or bioassays that measure biological activity, behavioral bioassays utilize whole-animal behavior as the primary readout, enabling researchers to investigate complex neurobiological processes, cognitive functions, and emotional states [20]. These tools are indispensable for preclinical investigation of neuropsychiatric disorders, where knowledge of underlying neurobiology often remains incomplete, making validation of animal models particularly challenging [21].
The fundamental purpose of behavioral assays in neuroscience extends beyond mere observation to answering specific questions about animal and human behavior. As outlined by Tinbergen's four categories, these questions span ontogeny (development), mechanism (causation), adaptive significance (function), and evolution [20]. In practice, this means behavioral assays allow researchers to address diverse questions such as how neural circuits generate specific behaviors, how genes and environment interact to shape behavioral outputs, and how pathological states alter normal behavioral patterns. The growing importance of testing novel CNS concepts and neuroactive drugs has spurred continued refinement of existing behavioral tests and the development of new assay paradigms [22].
In contemporary neuroscience research, there is an emerging trend toward dimensional approaches that define limited behavioral dimensions accounting for clusters of symptoms that co-vary within and across psychiatric illnesses. Rather than attempting to develop animal models that emulate all aspects of complex human neuropsychiatric syndromes such as depression, this approach focuses on modeling specific components or dimensions of an illness, representing specific symptom clusters that may share common underlying neurobiological mechanisms [21]. This methodological shift has increased the precision of behavioral assays while enhancing their translational relevance for understanding human disorders.
Fundamental Principles and Classification of Behavioral Assays
Defining Characteristics and Assay Types
Behavioral assays in neuroscience share common characteristics with other scientific assays, requiring standardized procedures, specific apparatuses, methods for detecting and quantifying variables of interest, and controls for confounding variables [20]. Three primary types of assays are utilized in neuroscience research: chemical assays that detect specific substances, bioassays that measure biological activity in response to specific stimuli, and behavioral bioassays that use whole-animal behavior as the measurement output. Behavioral bioassays may be further categorized based on their application for detecting external stimuli (such as environmental toxins or pheromones) or internal stimuli (such as hormones, drugs, neurochemicals, or disease processes) [20].
The design and implementation of behavioral bioassays require careful consideration of multiple factors: which specific behaviors to study, how to define behavioral units that serve as the assay's foundation, when to sample behavior, and how to record and analyze the resulting data [20]. Well-conceived behavioral assays must be reproducible and account for environmental variables while eliminating potential bias through key principles including blinding, randomization, counterbalancing, appropriate sample sizes, and inclusion of proper controls [12].
Pillars of Reproducibility
Reproducibility stands as a critical concern in behavioral neuroscience, with several methodological pillars essential for reliable data generation:
Blinding: At minimum, technicians responsible for behavioral evaluation and data analysis should be unaware of treatment groups. When visual clues make blinding challenging, independent technicians should perform analysis and interpretation before treatment codes are revealed [12].
Randomization and Counterbalancing: Test subjects must be randomly assigned to treatment groups, with considerations for counterbalancing performance levels and body weights evenly across groups. This principle extends to testing sessions, time of day, multiple testing equipment, and treatments within group-housed cages [12].
Controls: Vehicle controls should always be included in experimental designs, receiving identical treatment except for the test compound. This practice ensures that injection-related stress or handling effects don't confound interpretation of results [12].
Sample Size: Group sizes of 10-20 per sex per genotype/treatment typically represent minimal sample sizes required to achieve statistical significance in behavioral assays based on previous power analyses. Combining small sample sizes from separate experiments is methodologically inappropriate, though pilot data from small cohorts can inform power calculations for follow-up experiments [12].
Table 1: Key Methodological Principles for Behavioral Assay Validation
| Principle | Implementation Guidelines | Impact on Data Quality |
|---|---|---|
| Blinding | Technician unaware of treatment groups; independent analysis if visual cues present | Reduces observer bias in behavioral scoring and data interpretation |
| Randomization | Random assignment to groups; counterbalancing of performance levels across treatments | Minimizes systematic bias and ensures group comparability |
| Environmental Control | Minimize noise/vibration; consistent lighting, temperature, and humidity | Reduces external variables affecting behavioral responses |
| Technical Proficiency | Demonstrate ability to reproduce published data sets with positive controls | Ensures reliable assay execution and data collection |
| Appropriate Controls | Vehicle controls; wild-type controls in phenotyping experiments | Ispecific treatment effects from procedural artifacts |
Methodological Optimization of Behavioral Assays
Environmental and Technical Considerations
The behavioral testing environment requires careful optimization beyond simply placing equipment in available laboratory space. The testing environment must be sufficiently sensitive to detect expected behavioral outcomes, necessitating avoidance of high-traffic areas, elevator shafts, restroom facilities, or cage wash facilities to minimize disruptions from noise and vibration [12]. documented that high vibration levels can impact breeding and pup survival, suggesting similar potential effects on behavioral responses [12]. A consistent and rigorously controlled procedure space represents a major factor in achieving reliable, reproducible behavioral data.
Technical proficiency stands as another critical component in behavioral assay optimization. Researchers should demonstrate mastery of sensitive behavioral tests by reproducing published data sets with test compounds or established mouse models serving as positive controls [12]. This proficiency testing should be conducted with technicians blind to treatment groups or genotypes to eliminate potential bias and provide confidence in their technical capabilities. Failure to reproduce positive control data when all variables are known should caution investigators that their assay system requires further optimization before testing experimental unknowns [12].
Assay Validation and Positive Controls
The "great equalizer" across often uncontroll laboratory variables is demonstrating that a behavioral test possesses sufficient sensitivity to detect expected behavioral changes through proper validation [12]. Before testing experimental unknowns, initial experiments should establish the assay's ability to produce expected baseline results when positive or known standards are evaluated. For example, when establishing an assay sensitive to anxiolytic effects, technicians should demonstrate that a standard anxiolytic agent (e.g., diazepam) produces the expected anxiolytic-like effect [12]. This validation approach provides confidence that the test conducts under optimal conditions, distinguishing true negative results from methodological failures.
This validation principle should not be confused with expecting novel mechanisms of action to produce identical behavioral effects as known standards. Rather, it provides confidence that the test was conducted under conditions established to detect specific behavioral changes, allowing for proper interpretation of results for novel compounds or genetic manipulations [12]. The convergence of data from multiple behavioral tests, coupled with correlating biochemical data, strengthens the reliability of mouse models or compounds being tested and enhances translational utility [12].
Comparative Analysis of Established Behavioral Assays
Cognitive Function Assays
The Attentional Set-Shifting Test (AST) represents a sophisticated behavioral assay developed to assess prefrontal cortical function in rats, specifically targeting cognitive flexibility [21]. This test models the ability to "unlearn" an established contingency to learn a new one by shifting attention from a previously salient stimulus dimension to a previously irrelevant one. The rodent AST adapts the clinical Wisconsin Card Sorting Test (WCST) used to assess strategy-switching deficits in patients with frontal lobe dysfunction [21]. In this paradigm, rats progress through a series of discrimination stages where they must dig in small flower pots to locate food rewards, with the relevant dimension (odor or digging medium) changing across stages. The primary dependent measure is the number of trials required to reach criterion at each stage, with specific impairment in extradimensional shifting indicating medial prefrontal cortex dysfunction, while reversal learning deficits specifically implicate orbitofrontal cortex function [21].
Experimental Protocol for AST:
- Rats are food-restricted to approximately 85% of free-feeding weight to ensure motivation for food rewards.
- Animals are habituated to the testing arena and trained to dig in flower pots for food rewards.
- Testing proceeds through seven stages: simple discrimination (SD), compound discrimination (CD), first reversal (R1), intradimensional shift (ID), second reversal (R2), extradimensional shift (ED), and final reversal (R3).
- At each stage, rats must reach a criterion of six consecutive correct responses before advancing.
- All stimuli (odors and digging media) are changed for the ID and ED stages to prevent stimulus-specific learning.
- The number of trials to criterion at each stage is recorded, with specific attention to ED stage performance as a measure of cognitive flexibility [21].
Social Behavior Assays
The Three-Chamber Social Interaction Test (SIT) represents the most widely utilized behavioral assay for assessing sociability in rodents [23]. This test evaluates an animal's preference for social versus non-social stimuli in a three-chambered apparatus with a wired cup containing a social partner in one chamber and an identical empty cup or object in the opposite chamber. Following habituation, the experimental animal freely explores the apparatus while interaction time with both cups is quantified. Despite its widespread use, SIT has yielded inconsistent results across different rodent models of ASD, potentially pointing to methodological limitations [23].
The Reciprocal Interaction Test (RCI) provides an alternative approach to assessing social behavior by placing two freely interacting animals in an open field arena and quantifying specific social behaviors including nose-to-nose, nose-to-anogenital, and side sniffing, while also recording non-social behaviors such as evading, escaping, or freezing in contact [23]. Recent head-to-head comparisons between SIT and RCI in a SHANK3 mouse model of autism spectrum disorder revealed significant discrepancies, with Shank3B(-/-) mice displaying normative sociability in SIT but exhibiting less than half the social interaction and almost three times more social disinterest compared to wild-type controls in RCI [23]. This disparity suggests that RCI may offer greater sensitivity for detecting social deficits in certain genetic models, highlighting the importance of assay selection for specific research questions.
Table 2: Comparison of Social Behavior Assays in Rodent Models
| Assay Characteristic | Three-Chamber Social Interaction Test (SIT) | Reciprocal Interaction Test (RCI) |
|---|---|---|
| Apparatus | Three-chambered box with wired cups | Open field arena |
| Social Stimulus | Contained social partner in cup | Freely interacting social partner |
| Primary Measures | Time in chambers; interaction time with cup | Direct social behaviors (sniffing); non-social behaviors |
| Advantages | Controlled social exposure; minimal aggression | Naturalistic interaction; broader behavioral repertoire |
| Limitations | Limited behavioral complexity; constrained interaction | Dominance effects; more complex scoring |
| Sensitivity in ASD Models | Variable across models; potentially less sensitive | Potentially higher sensitivity for specific deficits |
Anxiety and Depression-Related Assays
Innovative approaches to behavioral assessment include the development of hybrid assays that combine elements of multiple tests. The Light-Dark Forced Swim Test represents one such novel hybrid assay combining features of the light-dark test and forced swim test to simultaneously assess anxiety-like and depression-like behaviors [22]. This paradigm evaluates light-dark preference during swimming as a measure of anxiety-like behavior while recording immobility as an indicator of behavioral "despair." Validation studies demonstrate that the anxiety-like dark preference in female white outbred mice is sensitive to physiological anxiogenic stressors, while clinically active antidepressants reduce despair-like immobility, supporting its utility for simultaneous evaluation of anxiety- and depression-like behaviors [22].
The Elevated Plus Maze, Social Interaction Test, and Shock-Probe Defensive Burying Test represent additional well-validated assays for anxiety-like components of depression and anxiety disorders [21]. Each test operationalizes anxiety through different behavioral manifestations: open arm avoidance in the elevated plus maze, decreased social investigation in the social interaction test, and burying behavior in response to a shock-producing probe in the defensive burying test. The convergent use of multiple anxiety assays provides a more comprehensive assessment of anxiety-like behavior than any single test alone.
Emerging Applications and Innovative Approaches
Cross-Species Behavioral Paradigms
Behavioral assays have expanded beyond traditional rodent models to include innovative approaches in diverse species such as Drosophila melanogaster. The fruit fly offers powerful genetic tools and well-characterized neurocircuitry for investigating molecular mechanisms underlying complex behaviors [24]. Drosophila behavioral paradigms for autism research include social space analysis, aggression assays, courtship behavior analysis, grooming behavior, and habituation assays [24]. These approaches leverage the conservation of fundamental neurobiological processes across species while enabling high-throughput screening of genetic manipulations and pharmacological treatments.
The utility of Drosophila models is particularly evident in research on neurodevelopmental disorders, where hundreds of genes have been associated with autism spectrum disorders. Rather than a single Drosophila ASD model, researchers employ targeted genetic manipulations of individual ASD-related genes, followed by comprehensive behavioral characterization [24]. This approach has identified conserved molecular pathways underlying social behavior, repetitive behaviors, and habituation learning, providing insights into the neurobiological basis of ASD-related behavioral dimensions.
Advanced Translational Neuroscience Assays
Recent advances in translational neuroscience have incorporated human iPSC-derived neurons from both peripheral and central nervous systems, employing electrophysiological readouts including manual patch clamping and multi-electrode array (MEA) platforms [25]. These approaches enable recording of changes in single cell and neuronal network activity, determining effects of test compounds on targets and signaling pathways relevant to CNS diseases such as epilepsy, depression, anxiety, and neurodegeneration [25].
MEA recordings specifically allow interrogation of effects at both single neuron and network levels, monitoring physiological activity from native tissue or human stem cell-derived neurons bearing patient-derived disease mutations. This creates translational "disease-in-a-dish" phenotypic assays that bridge molecular mechanisms and cellular function [25]. Similarly, peripheral neuron phenotypic assays utilizing DRG (dorsal root ganglion) neurons enable target validation and engagement studies for pain and inflammation research, expanding the toolkit for translational neuroscience.
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Key Research Reagent Solutions for Behavioral Neuroscience
| Reagent/Equipment | Primary Function | Application Examples |
|---|---|---|
| Automated Tracking Systems | Objective quantification of animal movement and behavior | EthoVision XT for social interaction tests, open field analysis |
| Multi-Electrode Array Platforms | Recording neuronal network activity | iPSC-derived neuron models for epilepsy, neurotransmitter effects |
| Biomarker Detection Assays | Quantification of neurological biomarkers in biological fluids | Ella platform for NF-L, NF-H in serum, plasma, CSF |
| Standard Anxiolytics/Antidepressants | Positive controls for assay validation | Diazepam for anxiety assays, fluoxetine for depression tests |
| Genetic Model Organisms | Investigation of gene function in behavior | SHANK3 models for ASD, Fmr1 models for Fragile X syndrome |
Behavioral assays remain indispensable tools in neuroscience research, providing critical bridges between biological mechanisms, neural circuits, and complex behavioral phenotypes. Their continued optimization and validation according to established methodological principles ensures the reliability and reproducibility necessary for translational success. As the field advances toward dimensional approaches that focus on specific symptom clusters and their underlying neurobiological mechanisms, behavioral assays will continue to evolve in sophistication and specificity. The integration of traditional behavioral paradigms with innovative approaches including cross-species models, human iPSC-based systems, and multi-electrode array technologies promises to enhance our understanding of neuropsychiatric disorders and accelerate the development of novel therapeutic strategies.
From Theory to Bench: A Guide to Key Assays and Model Organisms
Behavioral assays are indispensable tools in neuroscience and psychopharmacology research, providing critical windows into the cognitive and emotional states of animal models. The Open Field Test (OFT), Elevated Plus Maze (EPM), and Morris Water Maze (MWM) represent three foundational paradigms used extensively to evaluate anxiety-like behaviors, exploratory tendencies, and cognitive function in rodents. These tests leverage natural rodent behaviors—including thigmotaxis (wall-hugging), aversion to open spaces, and spatial navigation—to quantify complex behavioral outputs. Their validation against human disorders relies on careful experimental design, pharmacological sensitivity, and correlation with specific neural substrates. As the field moves toward increasingly sophisticated analysis techniques, understanding the comparative strengths, limitations, and optimal applications of these assays becomes paramount for researchers modeling human psychiatric and neurological conditions.
Comparative Analysis of Behavioral Assays
The table below provides a systematic comparison of the three behavioral assays, highlighting their primary applications, key behavioral measures, and neural correlates.
| Assay Name | Primary Behavioral Domain | Key Measured Parameters | Typical Testing Duration | Neural Substrates | Validity for Human Disorders |
|---|---|---|---|---|---|
| Open Field Test (OFT) [26] | Anxiety, locomotor activity, exploratory behavior | - Distance traveled [27]- Time in center vs. periphery [26]- Rearing frequency [26]- Defecation/urination events [26] | 5-60 minutes [28] | Striatum [27] | Contested; best used in conjunction with other tests [26] |
| Elevated Plus Maze (EPM) [29] | Anxiety-like behavior | - % time in open arms- % entries into open arms- Total arm entries (activity measure) [29] | 5 minutes [30] | Not specified in search results | Good for GABAergic drugs (e.g., benzodiazepines); mixed results for novel anxiolytics [29] |
| Morris Water Maze (MWM) [31] | Spatial learning & memory, reference memory | - Escape latency- Path efficiency- Time in target quadrant (Probe trial)- Platform crossings (Probe trial) [31] | Multiple days (e.g., 5-6 days of training + probe trial) [31] | Hippocampus, Entorhinal cortex [19] | Strongly correlated with hippocampal function and NMDA receptor-dependent synaptic plasticity [31] |
Analysis of Key Metrics and Sensitivity
A critical consideration in selecting a behavioral assay is the sensitivity and reliability of its output measures. For the Morris Water Maze, a comparative analysis of different probe trial measures has revealed significant differences in their ability to detect group differences. Proximity (P), or the average distance from the target platform location, has been consistently shown to be a more sensitive measure than percent time in the target quadrant (Q), time in a target zone (Z), or the number of platform crossings (X), regardless of sample or effect size [32]. This superior performance is attributed to proximity capturing the spatial precision of the animal's search pattern throughout the entire trial, rather than relying on arbitrary boundaries or single-location crosses.
Recent technological advancements are further enhancing the sensitivity of these assays. The traditional analysis of the Open Field Test, which often relies on individual parameters like line crossings or center time, can fail to capture the complexity of animal movement [26]. Advanced computational approaches, such as modeling movement with fractional Brownian motion (fBm), characterize complex movement patterns through distinct asymptotic scaling regimes, uncovering significant insights obscured by simpler metrics [26]. Similarly, in the Morris Water Maze, novel vector-field analyses that measure Spatial Accuracy, Uncertainty, and Intensity of Search have proven more sensitive than classical measures, successfully detecting previously hidden differences in mouse models of genetic disorders [33]. The integration of machine learning, particularly deep neural networks, is also proving superior to classical methods for classifying animal behavior from sensor data, promising more nuanced and powerful analysis pipelines [34].
Detailed Experimental Protocols
Open Field Test (OFT) Protocol
The OFT is designed to assess general locomotor activity and anxiety-like behavior in rodents by leveraging their natural aversion to open, brightly lit areas and their tendency to stay close to walls (thigmotaxis) [26].
- Apparatus: A square or circular arena with walls to prevent escape. The size varies by species; for pigs, a high variability in dimensions has been noted across studies [28]. The field is conceptually divided into a peripheral zone near the walls and a more anxiogenic center zone [26].
- Procedure: The test subject is placed in the periphery of the arena (often near a wall) and allowed to explore freely for a set period, typically 5-60 minutes depending on the species and experimental design [28]. The test is conducted under indirect lighting to avoid creating bright hotspots [30]. Behavior is recorded for subsequent analysis.
- Data Collection & Analysis: Key parameters are tracked, ideally using automated video tracking software (e.g., EthoVision XT) to minimize bias [27]. Primary measures include:
- Locomotor Activity: Total distance traveled and line crossings [26] [27].
- Anxiety-like Behavior: Time spent in the center zone versus the periphery, and the number of entries into the center [26]. A decrease in center activity indicates higher anxiety.
- Exploratory Behavior: Rearing frequency (standing on hind legs), which can be unsupported or against the walls [26].
- Emotionality: The frequency of defecation and urination, though the interpretation of these as direct measures of anxiety is controversial [26].
Elevated Plus Maze (EPM) Protocol
The EPM exploits the conflict between a rodent's innate curiosity to explore a novel environment and its unconditioned fear of heights and open, brightly lit spaces [30] [29].
- Apparatus: A plus-shaped apparatus elevated from the floor with two open arms (without walls) and two enclosed arms (with high walls) that are arranged opposite each other. A central square connects all four arms [29].
- Procedure: The animal is placed in the central square of the maze, facing an open arm. The session typically lasts for 5 minutes [30]. Behavior is recorded both manually by a blinded observer and via video tracking software. If an animal falls, it is immediately placed back on the maze at the point where it fell, though its data may be excluded from analysis [30].
- Data Collection & Analysis: The primary measures focus on the animal's exploration of the more "dangerous" open arms, which is interpreted as reduced anxiety.
- Primary Anxiety Indices: Percentage of time spent in the open arms and the percentage of entries made into the open arms [29].
- General Activity: The total number of arm entries is used as a control measure for overall locomotor activity [29].
- Automated Tracking: Video software (e.g., AnyMaze) is used to track the distance traveled in each arm type and the number of entries [30].
Morris Water Maze (MWM) Protocol
The MWM is a gold standard for assessing spatial learning and reference memory in rodents by requiring them to learn the location of a hidden platform using distal spatial cues [31].
- Apparatus: A large circular pool (e.g., 120 cm in diameter) filled with opaque water maintained at a specific temperature (e.g., 28 ± 1°C). A hidden escape platform is submerged just below the water surface in a fixed location [31] [32].
- Procedure: The test involves multiple phases over several days.
- Spatial Acquisition (Training): Over several days (e.g., 5 days), animals undergo multiple trials per day (e.g., 4-6 trials). On each trial, they are started from different, semi-randomly varied points around the pool's perimeter and must learn to find the hidden platform using distal cues. If an animal fails to find the platform within the allotted time (e.g., 60 s), it is guided to the platform [31] [32].
- Probe Trial (Memory Test): Typically conducted 24 hours after the last acquisition day, the platform is removed from the pool, and the animal is allowed to swim for a fixed time (e.g., 60 s). This tests the strength and precision of the spatial memory for the former platform location [31] [32].
- Reversal Learning (Cognitive Flexibility): Often, the platform is moved to the opposite quadrant, and training continues for additional days. This assesses the animal's ability to extinguish the old memory and learn a new location [31].
- Data Collection & Analysis: Performance is tracked using automated video systems.
- Acquisition Learning: Escape latency and path efficiency to find the hidden platform are measured across trials [31].
- Probe Trial Memory: Spatial bias is quantified using measures like:
- Proximity (P): The most sensitive measure, it is the average distance from the target location during the probe trial [32].
- Percent Time in Target Quadrant (Q): Time spent in the quadrant that previously contained the platform.
- Platform Crossings (X): Number of times the animal crosses the exact former platform location [31] [32].
Essential Research Reagent Solutions
The table below outlines key materials and tools required for the proper execution and analysis of these behavioral assays.
| Item Name | Function/Description | Specific Application Examples |
|---|---|---|
| Automated Video Tracking System (e.g., EthoVision XT, AnyMaze) | Automates the recording and analysis of animal movement, minimizing human bias and improving reproducibility [27]. | Tracks center of gravity, nose/tail points, and calculates parameters like distance traveled, time in zones, and arm entries in OFT, EPM, and MWM [30] [27]. |
| Open Field Arena | Provides a standardized, featureless environment to assess exploration and anxiety. | A square or circular arena with walls; size is scaled to the species (mice, rats, or pigs) [26] [28]. |
| Elevated Plus Maze | A plus-shaped apparatus with open and closed arms to create an approach-avoidance conflict. | Used to test anxiety-like behavior; typically elevated 50 cm from the floor [29]. |
| Morris Water Maze Pool | A large circular tank filled with opaque water for testing spatial navigation. | The pool is typically 120 cm in diameter for mice/rats, with a hidden platform [31] [32]. |
| Animal-borne Sensors (Bio-loggers) | Miniature sensors (accelerometers, gyroscopes) record kinematic and environmental data. | Used for computational analysis of behavior (e.g., using benchmarks like BEBE) in more naturalistic or long-term settings [34]. |
| Analysis Software (e.g., Pathfinder, custom software) | Specialized software for analyzing spatial navigation paths and strategies. | Used to analyze search strategies in the MWM and calculate novel metrics like vector fields [33]. |
The Open Field Test, Elevated Plus Maze, and Morris Water Maze form a cornerstone of behavioral phenotyping in animal models. The OFT and EPM provide insights into anxiety and locomotor profiles, while the MWM delivers a powerful and validated assessment of hippocampally dependent spatial learning and memory. A critical trend in the field is the move beyond traditional, simple metrics toward more sophisticated, model-based analyses—such as fractional Brownian motion for movement patterns and vector fields for search strategies—which offer greater sensitivity and richer biological interpretation [26] [33]. Furthermore, the integration of machine learning and bio-loggers is poised to revolutionize behavioral analysis, enabling the discovery of novel behavioral patterns and more accurate classification of states [34]. The continued refinement of these assays, coupled with advanced computational methods, ensures their enduring utility in validating animal models for human psychiatric and neurological disorders.
In preclinical research, animal models are indispensable for understanding the pathophysiology of human neuropsychiatric disorders and evaluating potential therapeutic interventions. The value of this research, however, is critically dependent on the validity of the behavioral assays used to quantify domains such as social interaction, depression-like states, and cognitive function. Validation provides the objective evidence that these assays consistently measure what they are intended to measure and that their results are meaningful for predicting human outcomes. The framework for validating animal models of human mental disorders has historically rested on three pillars: predictive validity (the ability to identify treatments known to be effective in humans), face validity (phenomenological similarity to the human condition), and construct validity (theoretical rationale linking the model to the human disorder) [35] [36].
This guide provides a comparative analysis of key behavioral assays within this validation framework, offering researchers a structured resource for selecting and implementing the most appropriate tests for their specific research objectives in modeling human disorders.
Validation Frameworks and Evolving Approaches
The interpretation of behavioral assay data is guided by the underlying validation philosophy, which has evolved significantly over time.
Traditional Validation Criteria
The established tripartite validation system offers a structured way to evaluate animal models [35] [36]:
- Predictive Validity: Assessed by whether a model correctly identifies pharmacologically diverse antidepressant treatments without errors of omission (false negatives) or commission (false positives), and whether potency in the model correlates with clinical potency [36].
- Face Validity: Requires that the model resembles the human disorder in specific, co-existing symptoms and that these effects are potentiated by chronic administration of treatments, as seen clinically. The model should also not show features absent in the human condition [36].
- Construct Validity: This is the most theoretical criterion, concerned with the quality of the rationale linking the model to the human disorder [35] [36].
The Shift to Endophenotypes and Technological Integration
A significant conceptual shift has moved the field from modeling entire psychiatric syndromes (e.g., major depressive disorder as defined in the DSM) toward modeling endophenotypes—discrete, component parts of a disorder such as specific behavioral traits or physiological markers [36]. This approach is driven by the recognition that complex human disorders are unlikely to be fully recapitulated in animal models, but their fundamental components can be effectively studied [36].
Concurrently, technological advances are revolutionizing data collection. Deep learning models, such as ResNet-50 and Random Forest classifiers, now enable markerless pose estimation and automated, high-accuracy classification of complex behaviors, reducing observer bias and enabling high-throughput analysis [37]. Integrated platforms like the JAX Animal Behavior System (JABS) provide end-to-end solutions, from standardized data acquisition hardware to software for machine learning-based behavior annotation and classification, facilitating reproducibility and sharing of validated classifiers across the research community [38].
Social Interaction Tests
Social interaction assays measure an animal's propensity to engage with a conspecific, which is relevant to disorders like autism spectrum disorder, schizophrenia, and social anxiety.
Prominent Social Interaction Assays
Table 1: Comparison of Key Social Interaction Assays.
| Assay Name | Experimental Protocol | Key Measured Parameters | Validation Strengths | Validation Limitations |
|---|---|---|---|---|
| Dyadic Social Defeat Stress [39] | An intruder mouse is placed in a resident aggressor's cage for repeated, brief physical encounters (e.g., 5 min/day), separated by prolonged sensory contact via a perforated partition for days or weeks. | Social interaction quotient (time investigating a social vs. non-social stimulus), urine scent marking, aggressive and submissive postures. | High face validity as a model of psychosocial stress; strong predictive validity for anxiety and depressive-like effects [39]. | The chronic stress component may model comorbid conditions rather than social deficits in isolation. |
| Social Interaction Test [39] | Typically follows social defeat. Test mouse is placed in an open field with two perforated Plexiglas cylinders, one containing an unfamiliar CD-1 mouse and the other empty. Session is recorded and tracked. | Duration and frequency of investigation of the social vs. empty cylinder. A lower ratio indicates social avoidance. | Direct and quantitative measure of social motivation; can be integrated with automated tracking (e.g., TopScan) for objectivity [39]. | May be confounded by general changes in locomotor or exploratory activity. |
Experimental Protocol in Focus: Social Defeat and Interaction Testing
The following workflow outlines a typical integrated social defeat and interaction test protocol in mice, based on the methodology described in [39].
Depression-like Behavior Tests
These assays aim to model core features of human depression, such as despair, anhedonia (loss of pleasure), and behavioral despair.
Prominent Depression-like Assays
Table 2: Comparison of Key Depression-like Behavior Assays.
| Assay Name | Experimental Protocol | Key Measured Parameters | Validation Strengths | Validation Limitations |
|---|---|---|---|---|
| Learned Helplessness [35] [36] | Animals are exposed to inescapable, uncontrollable stress (e.g., mild foot shocks). Later, they are tested in an environment where escape is possible. | Latency to escape, number of failures to escape. | Good predictive validity—reversed by diverse antidepressants; high face validity for helplessness and despair [35] [36]. | Symptoms may not be specific to depression; construct validity is debated [35] [36]. |
| Chronic Social Defeat Stress [39] | As detailed in Section 3.1. | Social interaction, sucrose preference (anhedonia), other depressive-like behaviors. | Induces a robust depressive-like state; good face validity from chronic psychosocial stress; useful for studying neuroimmune interactions (e.g., microglial activation) [39]. | Complex and lengthy setup; effects may involve multiple neural systems beyond those directly relevant to depression. |
| Sucrose Preference Test | Mice are presented with two bottles, one with water and one with a sucrose solution. | Percentage of sucrose solution consumed relative to total fluid intake. A decrease indicates anhedonia. | Strong face validity for anhedonia, a core symptom of depression; simple and inexpensive to run. | Can be confounded by changes in thirst or general appetite. |
Neurobiological Insights from Social Defeat
Research using the social defeat model has provided valuable insights into potential mechanisms underlying depression-like states. Studies show that chronic social defeat stress can induce microglial activation and increase phagocytic activity in the brain, without necessarily involving infiltration of peripheral macrophages [39]. This suggests that changes in CNS-resident microglia may represent a key immunological component of psychosocial stress-induced depressive states [39].
Cognitive Function Tests
Cognitive assays evaluate learning, memory, and executive function, which are impaired in disorders like Alzheimer's disease, schizophrenia, and major depressive disorder.
Prominent Cognitive Function Assays & Clinical Translation
Table 3: Comparison of Key Cognitive Function Assays and their Clinical Relatives.
| Assay Name (Animal) | Experimental Protocol | Key Measured Parameters | Related Human Test | Mediators in Cognition-Disability Link |
|---|---|---|---|---|
| MMSE-Based Assessment [40] | The rodent-adapted Chinese MMSE involves tasks for orientation, registration, attention/calculation, and language. | Scores for orientation (0-12), episodic memory (0-6), attention/calculation (0-6), and language (0-6). Total score 0-30. | Mini-Mental State Examination (MMSE) in humans, assessing global cognitive function. | Longitudinal studies show the cognition-IADL disability link is mediated by social interaction (46.3%), lifestyle (42.0%), and depressive status (8.3%) [40]. |
| Morris Water Maze | Rodents learn to find a hidden platform in a pool of opaque water using spatial cues. | Escape latency, path length, time spent in the target quadrant during a probe trial. | Tests of spatial memory and navigation. | Not specifically mentioned in search results, but models hippocampal-dependent learning. |
| Novel Object Recognition | Animals are exposed to two identical objects, then later one is replaced with a novel object. | Discrimination index (time exploring novel vs. familiar object). Measures recognition memory. | Visual recognition memory tasks. | Simple test for episodic-like memory without external reinforcement. |
The relationship between cognitive test performance in models and real-world functional outcomes is complex. As illustrated below, cognitive decline influences instrumental activities of daily living (IADL) through several modifiable mediators, highlighting the importance of a multi-faceted approach in translational research.
Table 4: Key Reagents, Models, and Platforms for Behavioral Research.
| Item Name/Type | Specific Examples | Function/Role in Research |
|---|---|---|
| Specialized Mouse Strains | Cx3cr1 wt/gfp (microglial reporter), Ccr2 wt/rfp (macrophage reporter), Ubc gfp/gfp (ubiquitous GFP) [39]. | Enable tracking and analysis of specific immune cell populations in the brain during behavioral experiments. |
| Validated Disease Models | Chronic social defeat stress model, learned helplessness model, various transgenic models (e.g., for Alzheimer's disease) [39] [41]. | Provide standardized, well-characterized systems for studying disorder mechanisms and testing therapies. |
| Automated Behavior Analysis Platforms | JAX Animal Behavior System (JABS), DeepLabCut, SLEAP, PsychoGenics' Cube technologies [37] [38] [41]. | Provide hardware and software for objective, high-throughput behavioral phenotyping using machine learning. |
| CRO Services & Expertise | MD Biosciences, PsychoGenics [42] [41]. | Offer access to validated models, specialized expertise, and GLP-certified facilities for preclinical testing. |
The selection of behavioral assays for research modeling human disorders is a critical decision that should be guided by a clear understanding of the strengths and limitations of each test within the established validation frameworks. No single assay is perfect, and the most compelling preclinical studies often employ a battery of tests to comprehensively assess a specific domain. The ongoing integration of sophisticated genetic tools and automated, AI-driven behavioral analysis promises to enhance the objectivity, reproducibility, and translational power of these assays. By carefully considering the comparative data presented in this guide, researchers can make more informed choices, ultimately strengthening the validity and impact of their findings in the pursuit of novel therapeutics for neuropsychiatric disorders.
The selection of an appropriate animal model is a fundamental decision in biomedical research, particularly in the study of human disorders and the development of therapeutic interventions. Animal models serve as indispensable tools for understanding disease mechanisms, identifying therapeutic targets, and evaluating potential treatments, providing a crucial bridge between basic scientific discovery and clinical application. Researchers must navigate a complex landscape of scientific and practical considerations when choosing between model organisms, balancing factors such as genetic similarity to humans, physiological relevance, experimental tractability, cost, and ethical implications. The three model systems discussed in this guide—rodents, zebrafish, and non-human primates—represent distinct points on this spectrum of trade-offs, each offering unique advantages and limitations for specific research applications. This comparative analysis aims to provide researchers with a structured framework for selecting the most appropriate model organism based on their specific scientific objectives, with particular emphasis on validating animal behavior assays for human disorder modeling.
Comparative Analysis of Model Organisms
The choice between rodent models, zebrafish, and non-human primates involves careful consideration of multiple scientific and practical parameters. The table below provides a systematic comparison of these three model systems across key dimensions relevant to biomedical research.
Table 1: Comprehensive Comparison of Model Organism Characteristics
| Parameter | Rodent Models (Mice, Rats) | Zebrafish (Danio rerio) | Non-Human Primates (NHPs) |
|---|---|---|---|
| Genetic Similarity to Humans | High genetic similarity; ~85-90% homology in protein-coding genes [43] | Significant genetic homology; ~70% of human genes have zebrafish orthologs [44] | Very high genetic homology; closest evolutionary relatives to humans [45] [46] |
| Brain Structure & Complexity | Lacks some human-specific features; less complex connectivity [43] | Simpler nervous system; lacks complexity of mammalian brains [43] [44] | Similar brain structure and function to humans [43] [45] |
| Generation Time & Lifespan | Short breeding cycle (2-3 months); maximum lifespan ~2-3 years [43] [47] | Rapid breeding cycle (~3 months); lifespan ~2-3 years in lab conditions [43] [44] | Long generation time; sexual maturity ~3-5 years; lifespan >35 years [46] [47] |
| Maintenance Costs | Relatively low cost [43] | Low cost; minimal space requirements [43] [44] | High cost and complexity of maintenance [43] [46] |
| Ethical Considerations | Moderate concerns; well-established oversight frameworks | Lower concerns due to simpler neuroanatomy [44] | Significant ethical concerns; stringent regulations [43] [46] |
| Genetic Manipulation | Highly tractable; extensive genetic tools available [43] [48] | Highly tractable; transparent embryos facilitate transgenics [49] [44] | Emerging genetic tools; complex and costly to implement [45] [46] |
| Behavioral Complexity | Limited cognitive abilities compared to NHPs [43] | Limited cognitive abilities [43] | Complex cognitive abilities similar to humans [43] [45] |
| Drug Screening Capacity | Suitable for mid-throughput screening | Excellent for high-throughput pharmacological screens [44] | Low throughput; used in final preclinical stages |
| Tissue Transparency | Not applicable without specialized clearing techniques [50] | Naturally transparent embryos; ideal for visualization [44] | Not applicable without specialized clearing techniques [50] |
| Key Research Applications | Genetic disorders, neurobiology, immunology, cancer [43] [48] | Developmental biology, genetics, high-throughput drug screening [44] | Complex behaviors, neurodegenerative diseases, translational therapeutics [49] [45] |
Experimental Protocols and Methodologies
Behavioral Assays for Neurological Disorder Modeling
Validating animal behavior assays is crucial for modeling human disorders, particularly in neuroscience research. Different model organisms offer complementary approaches for studying various aspects of neurological and psychiatric conditions:
Rodent Behavioral Assays for Autism Spectrum Disorder (ASD) Modeling Rodent models employ sophisticated behavioral test batteries to recapitulate core features of ASD. The three-chamber test for sociability and novel social preference assesses social interaction and preference, while the reciprocal social interactions assay observes how animals reciprocate social advances through behaviors including sniffing, following, chasing, grooming, and wrestling [48]. The social partition test similarly evaluates abnormalities in social behavior, and the scent marking test investigates non-verbal communication through olfactory signals [48]. These complementary approaches provide a comprehensive assessment of social behaviors relevant to ASD pathology, with researchers increasingly advocating for standardized scoring systems to enhance the validity of these models [48].
Zebrafish Pain Response Assays Zebrafish have emerged as valuable models for studying pain responses and screening analgesic compounds. These models employ various algogens and noxious stimuli including acetic acid, formalin, histamine, Complete Freund's Adjuvant, cinnamaldehyde, allyl isothiocyanate, and fin clipping to elicit measurable behavioral and physiological responses [44]. The transparency of zebrafish embryos enables real-time visualization of neural activity using fluorescent probes, while their genetic tractability facilitates the study of evolutionarily conserved pain pathways including the opioid system, transient potential receptor (TRP) family, endocannabinoid system, and acid-sensitive ion channels (ASIC) [44]. These features make zebrafish particularly suitable for medium-to-high throughput screens of potential analgesic therapies [44].
Non-Human Primate Models of Stress and Anxiety NHP models provide unique insights into complex emotional behaviors relevant to human psychiatric disorders. Studies utilizing rhesus monkeys have demonstrated lasting changes in cortisol and behavior following maternal separation, providing valuable models for investigating the neurobiological mechanisms underlying stress and anxiety [45]. These models capture aspects of emotional regulation and stress response that are difficult to fully recapitulate in rodent or zebrafish systems, highlighting the value of NHPs for studying complex behavioral phenomena with high translational relevance to human conditions.
Tissue Processing and Imaging Techniques
The CLARITY (Clear Lipid-exchanged Acrylamide-hybridized Rigid Imaging/Immunostaining/In situ-hybridization-compatible Tissue-Hydrogel) technique enables detailed visualization of neural circuitry across multiple species, providing a unified methodological approach for comparative neuroanatomy. This technique involves six principal steps that are applicable to zebrafish, rodent, and NHP brain tissue [50]:
- Tissue fixation and preparation using hydrogel-based stabilization
- Passive lipid removal to render tissue transparent
- Immuno-labeling with primary and secondary antibodies
- Optical clearing to enhance light penetration
- High-resolution 3D imaging of thick tissue specimens
- 3D visualization and quantification using analytical software tools
This methodology facilitates comparative neuroanatomical studies across species boundaries, allowing researchers to trace neuronal projections and quantify cellular populations in three dimensions within intact tissue specimens [50].
Diagram 1: Generalized workflow for model organism-based research, illustrating the iterative process from research question formulation to translational application.
Molecular Pathways and Experimental Applications
Evolutionarily Conserved Signaling Pathways
Despite anatomical differences, many molecular pathways relevant to human disease show remarkable evolutionary conservation across model organisms:
Opioid Signaling Pathways Zebrafish possess orthologs of all major opioid receptors found in humans, including zMOP (μ), zKOP (κ), two functional copies of zDOP (δ; oprd1a and oprd1b), and zNOP (nociceptin/orphanin FQ) receptors [44]. These receptors signal through Gi protein-coupled pathways similar to their mammalian counterparts and show conserved distribution in brain regions involved in analgesia and reward [44]. The genetic tractability of zebrafish enables detailed analysis of opioid system function and its modulation by pharmacological agents, providing insights relevant to pain management and addiction in humans.
Neurodevelopmental and Neurodegenerative Pathways Studies of amyotrophic lateral sclerosis (ALS) have demonstrated conserved pathogenetic mechanisms across species models. Mutations in SOD1, TARDBP (encoding TDP-43), FUS, and C9ORF72 recapitulate aspects of ALS pathology in models ranging from zebrafish to non-human primates [49]. Notably, large animal models including pigs and NHPs have revealed neurodegenerative features that more closely resemble human pathology than those observed in rodent models, highlighting how different model systems can capture distinct aspects of disease biology [49].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents and Their Applications in Model Organism Research
| Reagent/Category | Function/Application | Species Compatibility |
|---|---|---|
| CLARITY Solution | Tissue clearing for 3D visualization | Zebrafish, Rodents, NHPs, Human [50] |
| Primary Antibodies | Target protein labeling for immunohistochemistry | Species-specific variants available for all models [50] |
| Secondary Antibodies | Signal amplification with fluorescent tags | Compatible with diverse species [50] |
| Paraformaldehyde (PFA) | Tissue fixation and preservation | Universal application [50] |
| MS-222 (Tricaine) | Anesthesia for aquatic species | Primarily zebrafish [50] |
| Opioid Receptor Ligands | Pain pathway modulation and analysis | Zebrafish, Rodents, NHPs [44] |
| Algogens (e.g., formalin, acetic acid) | Nociception induction for pain studies | Primarily zebrafish and rodents [44] |
| CRISPR/Cas9 Systems | Genome editing and genetic manipulation | All species (with varying efficiency) [45] [46] [48] |
Diagram 2: Conserved molecular pathways mediating pain responses in zebrafish, showing similar organization to mammalian nociceptive circuits with modulation by opioid signaling systems.
The selection of an appropriate model organism requires careful consideration of the specific research question, with different models offering complementary strengths and limitations. Rodent models provide a balanced combination of genetic tractability, physiological relevance, and practical feasibility for most laboratory settings. Zebrafish excel in high-throughput genetic and pharmacological screens, leveraging their optical transparency and rapid development. Non-human primates offer unparalleled physiological and behavioral similarity to humans for validating therapeutic interventions, albeit with significant practical and ethical constraints. The most effective research programs often employ complementary approaches across multiple model systems, leveraging the unique advantages of each to build a comprehensive understanding of human biology and disease mechanisms. As technological advances continue to enhance the capabilities of each model system, researchers are increasingly positioned to select the most appropriate model based on specific scientific objectives rather than logistical constraints alone.
The pursuit of novel pharmacological treatments for human psychiatric and neurological disorders faces a significant challenge: the poor translatability of promising preclinical findings from rodents to successful clinical trials [51]. This translational crisis is partly driven by the overreliance on traditional behavioral tests that are brief, conducted during the animals' inactive light phase, and highly sensitive to external laboratory conditions and human interference [51]. Automated home-cage monitoring (AHCM) systems, empowered by sophisticated deep learning algorithms, represent a paradigm shift in preclinical behavioral phenotyping. By enabling continuous, longitudinal, and minimally invasive observation of animals in their familiar home-cage environments, these technologies generate rich, objective datasets that more accurately reflect an animal's behavioral state [51] [52]. This guide provides a comparative analysis of current AHCM technologies and methodologies, framing them within the critical context of validating animal behavior assays for modeling human disorders. We focus on the practical aspects of system selection, experimental design, and data interpretation for researchers and drug development professionals aiming to enhance the construct and predictive validity of their preclinical models.
Comparative Analysis of Automated Home-Cage Monitoring Platforms
Automated home-cage monitoring systems can be broadly categorized by their core sensing technology, which directly influences the type and quality of data collected. The table below summarizes the principal technologies, their capabilities, and their limitations.
Table 1: Comparison of Automated Home-Cage Monitoring Technologies
| Technology Type | Key Examples | Measured Parameters | Advantages | Limitations |
|---|---|---|---|---|
| Computerized Visual Systems (CVS) | PhenoTyper (Noldus), Envision (JAX), RodentWatch [53] [52] [54] | Locomotion, position, posture, complex behaviors (e.g., drinking, resting), social interaction [54] | High spatial resolution, rich behavioral data, can track multiple animals, requires no animal instrumentation [52] | Computational intensity, potential data storage issues, can be obscured by cage clutter [55] [53] |
| Operant Wall Systems (OWS) | IntelliCage (TSE Systems), Chora Feeder (AM Microsystems) [51] [53] | Cognitive tasks (learning, memory, flexibility), nosepoke responses, rewarded behaviors [51] | Excellent for high-throughput cognitive phenotyping, automated and programmable tasks [51] | Limited to measuring operant responses, device malfunction can disrupt data, may require single housing [51] [53] |
| Integrated Sensor Systems | PhenoMaster (TSE Systems), MotorMonitor (Kinder Scientific) [53] [56] | Gross locomotor activity (via IR beams), food/water consumption (via sensors), rearing [53] | Direct, precise metabolic data, less computationally demanding than video analysis [53] | Lower behavioral resolution, beam breaks can be ambiguous, sensors require unobstructed views limiting cage enrichment [53] |
The choice of system depends heavily on the research objectives. For instance, the IntelliCage system, which allows for complex cognitive testing in group-housed mice via RFID identification, has been instrumental in identifying circadian-specific cognitive deficits in mouse models of human genetic disorders like those involving β-catenin mutations [51]. In contrast, AI-powered video systems like JAX's Envision platform have demonstrated superior sensitivity in detecting early disease onset, identifying behavioral deviations in an ALS mouse model at 7 weeks—a full 7 weeks earlier than traditional methods [52].
Performance Benchmarks: Quantitative Validation of Deep Learning Models
The efficacy of deep learning-driven AHCM is quantitatively validated through robust performance metrics. The following table summarizes published performance data for several recently developed systems and algorithms.
Table 2: Performance Metrics of Deep Learning-Based Detection and Classification Models
| Model / System | Species | Key Task | Reported Performance | Reference |
|---|---|---|---|---|
| MacqD | Rhesus Macaques | Detection in complex home-cages (single animal) | Median F1-score: 99% (Same), 95% (Different) | [57] |
| MacqD | Rhesus Macaques | Detection in complex home-cages (two animals) | Median F1-score: 90% (Same), 81% (Different) | [57] |
| Deep Learning Accelerometer Model | Canine | Classification of drinking behavior | Sensitivity: 0.949, Specificity: 0.999 | [58] |
| Deep Learning Accelerometer Model | Canine | Classification of eating behavior | Sensitivity: 0.988, Specificity: 0.983 | [58] |
| RodentWatch (YOLOv5s) | Rat | Recognizing drinking and resting behaviors | F1-score > 0.8 across five behavioral categories | [54] |
These metrics highlight several key points. First, modern models like MacqD show remarkable robustness and generalizability, maintaining high performance even when tested on animals from a different facility [57]. Second, deep learning can be applied successfully across data types, from video (MacqD, RodentWatch) to accelerometer data [58]. Finally, high-specificity models are particularly valuable for preclinical research, as they minimize false positives in automated high-throughput screening.
Experimental Protocols for System Validation
Implementing an AHCM system requires rigorous validation to ensure data reliability and reproducibility. Below is a generalized workflow for establishing and validating a deep learning-based video monitoring system, synthesizing protocols from multiple sources [57] [54].
Figure 1: Workflow for developing and validating a deep-learning-based behavior analysis model.
Detailed Methodology
Data Acquisition: Video data is collected from the home-cage over extended periods (days to weeks) to capture a full range of behaviors and circadian rhythms [51] [54]. It is critical to capture footage under various lighting conditions (simulating day/night cycles) and from multiple angles if possible. For robust models, data should include a diverse set of animals, accounting for variations in coat color, strain, and presence of cage enrichment to improve model generalizability [57] [52].
Data Annotation: This is a crucial step where human experts label the data for the AI to learn from. This involves:
- Object Detection: Drawing bounding boxes around each animal in the frame [57].
- Instance Segmentation: A more precise approach using pixel-level masks to outline the exact shape of each animal, which is more resilient to occlusions [57].
- Behavior Classification: Labeling frames or video clips with specific behavioral categories (e.g., "drinking," "resting," "grooming") [54]. To ensure annotation quality and consistency, it is recommended to have multiple annotators and a validation process where a senior researcher reviews the labels [57].
Model Training: The annotated dataset is split into training, validation, and test sets. A deep learning architecture (e.g., YOLOv5 for real-time object detection, Mask R-CNN for instance segmentation) is trained on the training set [57] [54]. Techniques like contextual object labeling (expanding bounding boxes to include relevant context like a water bottle for "drinking" behavior) can significantly enhance accuracy for specific behaviors [54].
Performance Validation: The trained model is evaluated on the held-out test set, which contains data it has never seen before. Standard metrics like F1-score, Average Precision (AP), sensitivity, and specificity are calculated to provide a quantitative measure of the model's performance [57] [58] [54].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully deploying AHCM relies on a suite of hardware and software solutions. The table below details key components and their functions in a typical setup.
Table 3: Essential Research Reagents and Solutions for AHCM
| Item Name | Function / Description | Example Use-Case in AHCM |
|---|---|---|
| Home-Cage with Integrated Camera | A standard or specialized cage with a mounted camera (top, side, or internal) for continuous video acquisition. | The core unit for data collection; the RodentWatch system uses an internal 45-degree angle camera for a comprehensive view [54]. |
| RFID Transponder System | A chip implanted in or attached to the animal, paired with antennae in the cage, to uniquely identify individuals in a social group. | Used in the IntelliCage to track cognitive task performance of individual mice within a group-housed setting [51]. |
| AI Behavior Recognition Software | Cloud-based or local software (e.g., Envision, MacqD, RodentWatch) that runs deep learning models to analyze video footage. | Automates the scoring of behaviors like seizures, activity levels, and feeding/drinking from continuous video, replacing manual scoring [52] [54]. |
| High-Resolution IR Beam System | A system of closely spaced infrared beams surrounding the home-cage to detect fine-scale locomotor activity and position. | The Kinder Scientific MotorMonitor HD uses ¼" beam spacing for high-resolution positional tracking over 24-hour periods [56]. |
| Operant Conditioning Wall | A wall attachment with nose-poke holes, LED lights, and liquid/food dispensers for automated cognitive testing. | Used in systems like the Chora Feeder and IntelliCage to assess working memory, cognitive flexibility, and time-keeping in the home-cage [51]. |
The integration of deep learning with automated home-cage monitoring is fundamentally transforming preclinical behavioral research. These technologies address core limitations of traditional methods by providing continuous, objective, and high-dimensional data in a low-stress environment for the animals. As the field progresses, the focus will be on developing even more robust and generalizable models, standardizing data outputs across platforms, and further integrating AHCM data with other physiological and neurological measures. For researchers focused on validating animal models of human disorders, the adoption of these sophisticated tools is no longer a niche pursuit but a necessary step toward improving the reproducibility, translational utility, and ethical standards of preclinical drug discovery.
Navigating Pitfalls: Strategies for Enhancing Reproducibility and Translational Relevance
The reproducibility of experimental results is a fundamental tenet of the scientific method. However, biomedical research, particularly in the field of preclinical animal studies, is currently facing a significant "reproducibility crisis," characterized by a growing number of published findings that other researchers cannot reproduce [59]. This crisis undermines the credibility of scientific theories and has substantial downstream effects, including wasted resources and failed clinical trials [60] [61]. Surveys indicate that over 70% of researchers have failed to reproduce another scientist's results, and half have failed to reproduce their own [60]. A landmark project by the Brazilian Reproducibility Initiative, which focused on common biomedical methods, found that only 21% of experiments were replicable across multiple criteria, with original studies often overestimating effect sizes by an average of 60% [62]. This article identifies the major sources of variability and error contributing to this crisis within the context of validating animal behavior assays for human disorder modeling, and provides a comparative guide to methodological approaches for mitigating these issues.
Quantifying the Crisis: Key Evidence from Replication Studies
The scale of the reproducibility problem is revealed through large-scale, systematic replication efforts across different fields. The following table summarizes findings from major reproducibility projects.
Table 1: Summary of Large-Scale Replication Efforts
| Replication Project/Field | Replication Rate | Key Findings | Reference |
|---|---|---|---|
| Brazilian Reproducibility Initiative (Biomedical Science) | 21% (across multiple criteria) | Original studies showed effect sizes ~60% larger than replications; data were less variable in original papers, suggesting potential selective reporting. | [62] |
| Psychology (Open Science Collaboration) | 36% - 47% | Success rate varied based on the definition of replication. | [62] |
| Preclinical Cancer Research | < 50% | A review found that only a minority of landmark findings in cancer research could be replicated. | [62] [59] |
| Translational Stroke Research | Not applicable (Focus on translation) | While effective in animal models, neuroprotectants consistently failed in human trials, highlighting a translation crisis rooted in poor preclinical predictivity. | [61] |
The failure to reproduce findings stems from a complex interplay of statistical, methodological, environmental, and human factors.
Statistical and Design Flaws
- Low Statistical Power: Many preclinical studies use sample sizes that are too small to detect true effects reliably. The mean statistical power in stroke mouse studies, for example, is around 45%, leading to a high false-positive rate and substantial overestimation of true effects [61]. With low power, random variation inherently causes wide fluctuations in p-values and effect sizes between identical studies, making replication challenging even in the absence of other errors [63].
- Questionable Research Practices (QRPs): Practices such as p-hacking (manipulating data collection or analysis to achieve statistical significance) and HARKing (Hypothesizing After the Results are Known) inflate false-positive rates [59] [64].
- Publication Bias: The scientific publishing ecosystem often favors novel, positive results, while negative findings or replication studies remain in the "file drawer." This creates a skewed literature that does not reflect biological reality [64].
Methodological and Environmental Variability in Animal Behavior
Behavioral neuroscience is particularly susceptible to irreproducibility due to the sensitivity of animal behavior to subtle environmental and procedural factors.
- Environmental Conditions: Behavior can be influenced by vibration, noise, and circadian rhythms [12]. Standardized, homogenous laboratory environments (e.g., using specific pathogen-free, inbred young male animals) may produce results that are not robust and fail to generalize to more diverse, human-relevant conditions [61].
- Human Interference and Assay Limitations: Conventional behavioral tests like the open field are short-lasting and conducted in novel environments, which can induce anxiety and confound results [65]. Human handling during testing is a major source of stress and variability [65].
- Inadequate Experimental Control: Failures in blinding, randomization, and the inclusion of appropriate control groups introduce performance and detection bias [12] [61]. A lack of detailed reporting on these methods makes it difficult to assess the quality of published studies [61].
Table 2: Comparison of Traditional Behavioral Assays vs. Home-Cage Monitoring Systems
| Aspect | Traditional Out-of-Cage Assays (e.g., Open Field) | Automated Home-Cage Monitoring Systems (HCMS) |
|---|---|---|
| Environment | Novel, potentially anxiogenic | Familiar, ethologically relevant |
| Human Involvement | High (handling, direct observation) | Minimal after setup |
| Data Collection | Short-term snapshots (minutes) | Longitudinal, continuous (days to weeks) |
| Behavioral Measures | Often limited, apparatus-specific | Rich, spontaneous, across circadian cycles |
| Anxiety Confound | High due to novelty | Reduced |
| Throughput | Lower, requires manual intervention | Higher, automated |
Strategies for Improvement: Pathways to Robust Research
Addressing the crisis requires a multi-faceted approach focusing on rigorous design, technological innovation, and cultural change in research practices.
Pillars of Reproducible Experimental Design
The foundation of robust research is built on key methodological principles that minimize bias and account for variability [12].
Technological and Digital Solutions
- Automation and Digitalization: Replacing manual, error-prone tasks with automated systems (e.g., robotic liquid handlers, automated behavioral phenotyping) standardizes procedures and reduces human-induced variability [60]. Digital lab tools ensure rich metadata is captured systematically, enhancing transparency [60].
- Home-Cage Monitoring Systems (HCMS): As compared in Table 2, platforms like the PhenoTyper allow for automated, longitudinal recording of spontaneous behavior in a familiar environment [65]. This reduces novelty-induced stress and human interference, providing more reliable and ethologically relevant digital biomarkers of behavior [65].
Cultural and Reporting Shifts: The Open Science Framework
- Open Science Practices: These include publicly sharing data, methods, and analysis code (Open Data); publishing preprints to accelerate feedback; and submitting Registered Reports, where the study protocol is peer-reviewed before data collection to prevent publication bias [64].
- Systematic Reviews and Reporting Guidelines: Systematic reviews of animal studies help identify robust findings and highlight methodological weaknesses across the literature [61]. Adherence to reporting guidelines like the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines ensures that critical methodological details are disclosed, enabling proper evaluation and replication [61].
The following table details key solutions and resources that researchers can employ to enhance the reproducibility of their behavioral assays.
Table 3: Research Reagent Solutions for Reproducible Behavioral Assays
| Solution/Resource | Function & Purpose | Key Considerations |
|---|---|---|
| Automated Home-Cage System (e.g., PhenoTyper) | Automated, longitudinal recording of spontaneous behavior in a familiar home-cage environment. | Reduces human interference and novelty stress; provides large, continuous datasets of naturalistic behavior [65]. |
| Positive Control Compounds (e.g., Diazepam) | Used in assay validation to confirm the test's sensitivity to detect expected behavioral changes (e.g., anxiolytic effects). | Essential for demonstrating technical proficiency and assay functionality before testing novel compounds or models [12]. |
| Electronic Lab Notebooks & Data Capture Systems | Digital tools for rigorous, standardized recording of experimental protocols, conditions, and metadata. | Ensures data integrity, prevents loss of detail, and facilitates sharing and replication [60]. |
| Standardized Statistical Analysis Plans | Pre-defined plans for data analysis, including how to handle outliers and which tests to use. | Mitigates p-hacking and analytical flexibility; should be written before data collection begins. |
| ARRIVE Guidelines | A checklist of essential information to include in publications describing animal research. | Improves reporting quality and transparency, enabling critical evaluation and replication of studies [61]. |
The reproducibility crisis is a multi-faceted problem driven by statistical shortcomings, methodological inconsistencies, environmental variability, and systemic biases. In the specific context of animal behavior assay validation, the path forward requires a concerted shift towards more rigorous and transparent practices. This includes embracing the pillars of robust experimental design, leveraging technological solutions like automation and home-cage monitoring to reduce unwanted variability, and adopting the principles of Open Science. By systematically addressing these sources of error and variability, the research community can strengthen the foundation of preclinical science, enhance the predictive value of animal models for human disorders, and ultimately accelerate the development of effective therapeutics.
In the pursuit of modeling human neurodevelopmental and neuropsychiatric disorders, researchers rely heavily on behavioral data generated from animal models. The reliability of this data is paramount, as it forms the foundation for our understanding of disease mechanisms and the development of novel therapeutic agents. However, this field faces a significant crisis: the poor reproducibility of behavioral findings across laboratories threatens the validity and translational potential of preclinical research [66] [67]. A report from Bayer Healthcare highlighted this issue, noting that in two-thirds of projects based on exciting published data, the company's scientists could not sufficiently replicate the findings during target validation [66] [67]. Similarly, many published positive effects in animal models for amyotrophic lateral sclerosis (ALS) were likely "noise" rather than actual drug effects [66] [67]. This article will compare standardization approaches—ranging from strict protocol uniformity to systematic heterogenization—and provide the experimental data and methodologies necessary for researchers to make informed decisions in validating animal behavior assays.
Comparing Standardization Strategies: Benefits, Risks, and Experimental Outcomes
The debate on standardization is not about whether it is needed, but rather the degree and manner in which it should be applied. The goal is to navigate the delicate balance between reducing variability and maintaining the generalizability of research findings [67]. The table below compares the three primary standardization strategies explored in preclinical behavioral research.
Table 1: Comparison of Standardization Strategies in Behavioral Neuroscience
| Strategy | Key Features | Reported Outcomes | Advantages | Limitations |
|---|---|---|---|---|
| Strict Standardization [66] [67] | Controlling all possible environmental and procedural variables (apparatus, husbandry, testing order, time of day). | Significant site-specific effects persisted despite controls; sometimes produced opposite results for the same mouse strain between labs [66] [67]. | Reduces identifiable noise; ideal for initial assay validation [12]. | Risk of false positives/negatives; poor generalizability; can stifle innovation [66] [67]. |
| Standardized Protocols with Cross-Lab Validation [66] [67] | Different labs use their own established apparatus and some husbandry variables, but follow a clear standard operating procedure. | Preserved robust trends and strain differences across labs, despite variations in magnitude of effects [66] [67]. | Balances consistency with practical reality; more reproducible and robust results for some tests. | Inconsistent results for certain behavioral tests (e.g., elevated plus-maze) [66] [67]. |
| Systematic Heterogenization [66] [67] | Intentionally varying select environmental factors (e.g., housing cage size, illumination levels) across experiments. | Produced more consistent and reliable strain differences across experiments compared to standardized conditions [66] [67]. | Improves generalizability and real-world relevance; reduces spurious results. | Requires more complex experimental design; not yet a widely adopted practice. |
The experimental data supporting this comparison comes from landmark studies. Crabbe et al. (1999) demonstrated that even with extraordinary efforts to standardize test apparatus, protocols, and animal husbandry across three laboratories, significant site-specific effects were found for nearly all variables measured [66] [67]. In one test, BALB/c mice showed lower anxiety-like behavior than C57BL/6 mice at one site, but the exact opposite was found at another [66] [67]. In contrast, Richter et al. (2010) systematically varied two factors (housing cage size and illumination level) and found that this heterogenization approach led to remarkable consistency in strain differences across experiments, unlike the highly variable results seen under standardized conditions [66] [67]. This suggests that over-standardization can create a highly specific, artificial environment that inflates the sensitivity of a test, making findings less generalizable to other conditions.
Core Methodologies for Robust Behavioral Assay Validation
The Pillars of Reproducible Experimental Design
Before selecting a specific assay, the foundational elements of experimental design must be in place. These "pillars of reproducibility" are critical for minimizing bias and ensuring reliable data [12]:
- Blinding: The technician conducting behavioral assessments and analyzing data should be unaware of the treatment groups or genotypes. If physical differences (e.g., coat color) make this impossible, an independent researcher should handle the final data interpretation [12].
- Randomization and Counterbalancing: Subjects must be randomly assigned to treatment groups. When baseline testing is involved, groups should be counterbalanced for performance levels and body weight to avoid bias. This principle also applies to testing sessions, time of day, and across multiple pieces of equipment [12].
- Controls: Every experiment must include appropriate controls, typically vehicle-treated controls for compound screening or wild-type controls for phenotyping. These controls must be treated identically to the experimental groups in all aspects except for the variable being tested [12].
- Sample Size: Group sizes of 10-20 per sex per genotype/treatment are typically the minimum required to achieve statistical power. It is not methodologically sound to combine several small, underpowered experiments (e.g., n=2-8) after the fact [12].
Detailed Protocol: Validating an Anxiety-Related Behavioral Assay
The following workflow outlines the key steps for establishing a reliable behavioral assay, using a common test like the open field test or elevated plus maze as an example.
1. Optimize the Testing Environment: The behavioral testing space must be rigorously controlled. It should be located away from high-traffic areas, cage wash facilities, elevator shafts, and restrooms to minimize disruptions from noise and vibration, which are known to impact animal behavior and breeding [12]. Lighting, temperature, and humidity must be consistent and documented. Cages and bedding should not be changed for at least two days prior to testing, as this procedure can induce anxiety and alter activity levels [68].
2. Technician Training and Proficiency: A technician's mastery is demonstrated by their ability to reproduce published data sets or known phenotypes reliably while blind to treatment groups. Training requires significant investment in time and resources, but is essential. Failure to reproduce positive control data indicates that the assay is not yet optimized or the technician is not yet proficient, making it premature to test experimental unknowns [12].
3. Run a Positive Control Experiment: Before testing any novel compound or model, the assay's sensitivity must be confirmed using a positive control. For example, to validate an anxiety test, a known anxiolytic like diazepam should be administered to demonstrate that it produces the expected effect (e.g., increased time in the center of an open field or in the open arms of an elevated plus maze) under the specific laboratory conditions [12]. This step is the ultimate equalizer across uncontrollable variables.
4. Analysis, Interpretation, and Troubleshooting: Data should be analyzed with the pillars of reproducibility in mind. If the positive control fails to produce the expected result, investigators must systematically troubleshoot the testing environment, the protocol fidelity, and the technician's skills before proceeding [12].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key resources and their applications for conducting and validating behavioral assays in the context of neurodevelopmental disorder (NDD) research.
Table 2: Key Research Reagent Solutions for Behavioral Assay Validation
| Item / Reagent | Function / Application | Example Use-Case |
|---|---|---|
| Automated Tracking Software | Objectively quantifies movement, location, and specific behaviors from video recordings. Reduces experimenter bias. | Used in Open Field, Elevated Plus Maze, and Morris Water Maze tests for precise measurement of path, speed, and time in zones [7]. |
| Standard Anxiolytic (e.g., Diazepam) | Serves as a positive control drug for validating anxiety-related behavioral assays. | Administered before an Elevated Plus Maze test to confirm the assay can detect an expected increase in open-arm time [12]. |
| Valproic Acid (VPA) | A teratogen used to create an environmental model of Autism Spectrum Disorder (ASD) in rodents. | Injected in pregnant dams to induce autism-like phenotypes (e.g., social deficits, repetitive behaviors) in offspring for model validation [68]. |
| Touchscreen Cognitive Testing | Automated apparatus for assessing learning and memory using computographic stimuli. Enhances translation to human cognitive tests. | Used in visual discrimination or paired-associate learning tasks for models of Alzheimer's disease or schizophrenia, improving cross-species comparability [66]. |
| Inbred Mouse Strains (C57BL/6, BALB/c) | Genetically uniform populations used to control for genetic variability and test for baseline behavioral differences. | Comparing anxiety levels (e.g., C57BL/6 vs. BALB/c) on the Elevated Plus Maze to benchmark a new testing environment [66] [67]. |
The path to reliable data in animal behavior research does not lie in a rigid, one-size-fits-all standardization. Instead, it requires a more nuanced and pragmatic approach. The evidence suggests that systematic heterogenization—the controlled variation of key environmental factors—may enhance the generalizability and robustness of findings more effectively than strict standardization alone [66] [67]. Furthermore, the core of reliable data generation rests on the unwavering implementation of the pillars of reproducibility: blinding, randomization, controls, and appropriate sample sizes [12]. Ultimately, the most critical factor is assay validation within each laboratory's context. By requiring that a positive control produces the expected result before any experimental unknowns are tested, researchers can ensure their data is not only consistent internally but also holds the greatest potential for successful translation to the clinic.
In the pursuit of understanding human psychopathology, animal models serve as indispensable tools for unraveling the complex etiology of mental disorders and screening potential therapeutic compounds. However, a central challenge persists: how well do findings from controlled laboratory environments translate to the rich, complex tapestry of human experience? This challenge, encapsulated by the concept of ecological validity, represents a critical frontier in biomedical research. Ecological validity refers to whether research sufficiently represents real-world naturalistic conditions, determining how well experimental findings can be generalized beyond the laboratory [69] [70]. For researchers modeling human disorders in animal systems, this necessitates a careful balancing act between experimental control and real-world relevance. This guide examines the strengths and limitations of both artificial and naturalistic settings, providing a framework for selecting and validating animal behavior assays with greater translational potential for drug development.
Defining Ecological Validity in Preclinical Research
The term "ecological validity" is often used interchangeably with "mundane realism," but they represent distinct concepts. Mundane realism simply refers to how closely the experimental situation resembles situations encountered outside the laboratory, while ecological validity more specifically concerns the generalizability of study findings to real-world contexts [70]. Some scholars argue that the term has become so broadly and inconsistently applied that it risks losing meaning, suggesting instead that researchers should precisely specify the particular context of cognitive and behavioral functioning they aim to study [71].
In animal model research, ecological validity is formally assessed through established validity frameworks that evaluate how well a model recapitulates critical aspects of the human condition:
Table 1: Validity Criteria for Animal Models of Psychiatric Disorders
| Validity Type | Definition | Research Application |
|---|---|---|
| Face Validity | Resemblance to human disease symptoms or behaviors [72] [36] | Measuring anhedonia via sucrose preference test for depression modeling [72] |
| Construct Validity | Similar underlying etiology or biological mechanisms [72] [36] | Using chronic stress paradigms to model depression pathogenesis [36] |
| Predictive Validity | Ability to correctly identify therapeutic effectiveness [72] [36] | Reversal of behavioral deficits by known antidepressants [36] |
Contemporary approaches have refined these criteria further. Belzung and Lemoine (2011) developed an enhanced framework that incorporates technical advances and emphasizes the life course of the organism, requiring validity criteria to be met at each pivotal transition from healthy state to pathological and convalesced states [72]. This perspective acknowledges that a model valid for studying disease initiation might not adequately represent maintenance or recovery phases.
Artificial Laboratory Settings: Controlled but Simplified
Laboratory environments offer precise control over experimental variables, standardized procedures, and simplified data collection [73]. These reductionist approaches are particularly valuable for isolating specific mechanisms and establishing causal relationships.
Advantages of Artificial Settings
- Controlled Environment: Researchers can manipulate specific variables while holding others constant, enabling unambiguous causal inferences about drug effects or neural mechanisms [73] [74].
- Standardized Procedures: Protocols can be precisely replicated across laboratories, facilitating direct comparison of results and multi-site validation studies [73].
- Technical Accessibility: Sophisticed equipment (e.g., in vivo electrophysiology, fiber photometry) can be more readily implemented in controlled settings than in naturalistic environments [69].
Limitations and Concerns
- Artificial Environment: The sterile, controlled laboratory setting differs dramatically from an organism's natural habitat, potentially altering fundamental biological and behavioral processes [73] [71].
- Limited Generalizability: Findings from highly artificial settings may not translate to real-world contexts. For example, common behavioral decision-making tasks in laboratories rarely predict real-world risky behaviors [75].
- Demand Characteristics: Animals may adapt their behavior to artificial laboratory contingencies rather than exhibiting their natural behavioral repertoire [73].
Naturalistic Settings: Complex but Ecologically Relevant
Naturalistic approaches aim to study behavior within real-world contexts, providing access to authentic behaviors and complex environmental interactions that cannot be fully replicated in the laboratory [73] [74].
Advantages of Naturalistic Research
- Access to Real-World Context: Studying animals in environments that approximate their natural habitats or incorporating naturalistic elements into laboratory settings provides more authentic behavioral data [73] [69].
- Naturalistic Observation: Behaviors occur spontaneously rather than being experimentally elicited, potentially offering greater insight into natural behavioral patterns and sequences [73].
- Longitudinal Studies: Naturalistic designs more readily accommodate long-term observation of behavioral patterns, disease progression, and developmental trajectories [73].
Methodological Considerations
- Reduced Experimental Control: The complexity of natural environments introduces numerous uncontrolled variables that can complicate data interpretation [73].
- Technical Challenges: Implementing precise measurement technologies in field settings remains logistically challenging, though advances in wearable sensors and wireless monitoring are rapidly overcoming these limitations [74].
- Ethical Considerations: Field research may raise additional ethical concerns regarding wildlife disturbance, habitat preservation, and data privacy when studying animals in their natural ecosystems [73].
Experimental Paradigms: A Comparative Analysis
The tension between artificial and naturalistic approaches is particularly evident in specific experimental paradigms used for modeling human psychiatric disorders.
Social Defeat Stress in Mouse Models
The social defeat stress paradigm illustrates how ecological considerations can be incorporated into laboratory research. This model examines how aggressive confrontations between mice induce stress responses relevant to human depression and anxiety disorders [69].
Table 2: Ecological Validity in Social Defeat Stress Models
| Design Element | High Ecological Validity | Limited Ecological Validity |
|---|---|---|
| Housing | Groups with mixed sex and age structure | Single-sex, same-age groupings |
| Social Interaction | Unrestricted interaction with visual, auditory, olfactory, tactile contact | Physical separation or limited sensory modalities |
| Territory | Resident in home cage with familiar nesting material | Neutral arena without territory establishment |
| Duration | Continuous or repeated exposure over days | Single brief exposure |
Wild male mice naturally form territories inhabited by an adult male, one or more females, and their offspring. Young males are aggressively evicted from natal groups after sexual maturity and must navigate unfamiliar territories, creating naturalistic conditions of social conflict [69]. Laboratory models that incorporate these elements—such as resident-intruder paradigms in established territories—demonstrate greater ecological validity than those using neutral arenas or brief exposures.
Diagram 1: Ecological validity in social defeat stress models. The laboratory model (red) incorporates elements from natural mouse behavior (yellow) to produce relevant research outcomes (green).
Forced Swim Test and Learned Helplessness
The forced swim test (FST), a widely used screening tool for antidepressant compounds, demonstrates the limitations of artificial paradigms. In the FST, rodents are placed in inescapable water-filled cylinders, and their passive versus active coping strategies are interpreted as behavioral despair [72]. While the FST shows reasonable predictive validity for certain antidepressant classes, it has been modified multiple times to balance practical utility with ethological relevance [72].
The related learned helplessness model demonstrates how validity assessments are applied. In this paradigm, animals exposed to inescapable shock later fail to escape avoidable shock, modeling aspects of human depression [36]. According to Willner's criteria:
- Predictive validity: Moderate - various antidepressants reverse learned helplessness with few false positives [36]
- Face validity: Moderate - helpless animals exhibit symptoms analogous to depressed humans [36]
- Construct validity: Limited - helplessness is not specific to depression and occurs in other disorders [36]
The Scientist's Toolkit: Research Reagent Solutions
Diagram 2: Comprehensive toolkit for enhancing ecological validity in animal models.
Table 3: Essential Research Reagents and Tools for Ecological Validity
| Tool Category | Specific Examples | Research Application |
|---|---|---|
| Behavioral Assessment | Sucrose preference test, social interaction test, open field assay | Quantifying anhedonia, social avoidance, anxiety-like behaviors [72] |
| Physiological Monitoring | Telemetry systems, wireless EEG, cortisol/corticosterone assays | Measuring stress axis activation, sleep architecture, autonomic function [69] |
| Environmental Enrichment | Naturalistic bedding, nesting materials, tunnels, running wheels | Creating laboratory environments that approximate natural habitats [69] |
| Genetic Tools | CRISPR-Cas9, Cre-lox system, optogenetic/chemogenetic actuators | Dissecting causal mechanisms and modeling genetic vulnerabilities [69] |
Integrated Methodologies: Bridging the Divide
Rather than treating artificial and naturalistic approaches as mutually exclusive, contemporary research increasingly integrates both methodologies:
Graduated Validation Pipelines: Initial high-throughput drug screening in simplified assays followed by validation in progressively more naturalistic settings [72] [36].
Ethological Laboratory Design: Incorporating key naturalistic elements into controlled laboratory settings, such as establishing territories, mixed-sex housing, and graduated social hierarchies [69].
Experience Sampling Methods: Adapted from human research, these approaches collect repeated in-the-moment behavioral measurements as animals navigate semi-naturalistic environments [74].
Back-Translation: Using findings from human studies to refine animal models and validation criteria, creating an iterative cycle between clinical observation and preclinical modeling [9].
The challenge of ecological validity in animal behavior assays necessitates a thoughtful, balanced approach that acknowledges both the practical requirements of experimental control and the fundamental need for real-world relevance. Rather than seeking to completely eliminate artificiality, successful research programs strategically employ artificial settings for their specific advantages while systematically addressing their limitations through validation in more naturalistic contexts. The evolving frameworks for assessing multiple validity domains—face, construct, predictive, and ecological—provide crucial guidance for developing animal models that more accurately recapitulate human disorders. For drug development professionals, this integrated approach offers a more reliable pathway for translating preclinical findings into meaningful clinical applications, potentially reducing the high attrition rates that have long plagued psychiatric drug development. As technological advances continue to blur the boundaries between laboratory and field settings, the opportunity exists to create a new generation of animal behavior assays that combine experimental rigor with ecological relevance.
Mitigating Stress-Induced Variability with Home-Cage Monitoring
The reproducibility crisis in preclinical research represents a fundamental challenge in translational science, with estimates indicating that 50–90% of published findings cannot be replicated in subsequent studies [76]. This crisis carries tremendous financial implications, costing approximately $28 billion annually in the United States alone for irreproducible biomedical research [76]. A significant contributor to this problem lies in stress-induced variability introduced by traditional behavioral testing methods, where conventional handling procedures, novel environment exposure, and experimenter interaction confound experimental outcomes and compromise data integrity.
The validation of animal behavior assays for human disorder modeling requires meticulous attention to these confounding factors. Stress artifacts from handling and testing procedures present a particular challenge—mice subjected to traditional tail handling exhibit elevated corticosterone levels, reduced natural behaviors, and increased anxiety-like phenotypes that introduce substantial variability across laboratories [76]. Furthermore, standard behavioral tests are typically conducted during the light phase, conflicting with rodents' nocturnal activity patterns and distorting circadian-dependent metrics [76]. Within this context, Digital Home Cage Monitoring (DHCM) systems have emerged as transformative tools that mitigate stress-induced variability through continuous, non-invasive data collection in animals' native environments, thereby enhancing both animal welfare and data quality [76] [77].
Understanding Stress-Induced Variability in Animal Models
Physiological and Behavioral Impact of Stress
Animal models of stress are broadly categorized into physical stress (e.g., electric foot shock, forced swim) and psychological stress (e.g., maternal separation, predation, immobilization) [78]. These stressors activate complex neurobiological pathways, primarily through activation of the hypothalamic-pituitary-adrenal (HPA) axis and locus coeruleus-norepinephrine/autonomic systems [78]. When an animal encounters a stressor, it triggers a cascade of physiological responses that significantly alter behavior and cognition:
Neurobiological Changes: Chronic stress produces several critical modifications in the brain, including structural and functional impairments through altered neuronal structure, cell survival, and neurotransmission [78]. These changes include shrinkage in the apical dendritic arbors of CA3 pyramidal neurons in the hippocampus and reduced neurogenesis within the dentate gyrus [78].
Behavioral Manifestations: Exposure to stressful events alters key behaviors including increased anxiety-like behavior, depression-like behavior, reduced social interactions, and diminished sexual behaviors [78]. Stressful experiences also disrupt important cognitive functions, particularly learning and memory processes [78].
Neurochemical Alterations: Stress paradigms modify various dopaminergic, GABAergic, and excitatory amino acid transmission systems. In neuropeptide systems, corticotropin-releasing factor (CRF) and arginine vasopressin (AVP) pathways of the HPA axis are activated by stress, while extra-hypothalamic AVP and CRF circuits are inhibited and stimulated, respectively [78].
Methodological Artifacts in Traditional Behavioral Testing
Conventional behavioral assessment introduces numerous confounding variables that compromise data quality and translational validity:
Handling-Induced Stress: Traditional handling methods such as tail suspension induce acute stress responses that confound behavioral and physiological measurements. Studies comparing handling techniques have found that tunnel handling or cup techniques reduce corticosterone levels by 40% compared to tail suspension [76].
Experimenter Effects: Even subtle differences in experimenter identity, handling techniques, or testing environment can significantly influence behavioral outcomes, particularly for strain-specific behavioral traits [76].
Temporal Discordance: Standard behavioral tests conducted during the light phase conflict with rodents' nocturnal activity patterns, potentially masking important circadian-mediated behaviors and physiological processes [76].
The following diagram illustrates the pathways through which traditional testing methods introduce stress and how DHCM mitigates these effects:
Diagram: Comparative pathways of traditional behavioral testing versus digital home cage monitoring, highlighting how DHCM mitigates stress-induced variability by preserving natural behavioral states.
Home-Cage Monitoring Technologies: Comparative Analysis
Digital Home Cage Monitoring systems represent a paradigm shift in behavioral assessment, enabling continuous, non-invasive data collection in animals' native environments. These systems utilize various technological approaches, each with distinct advantages and limitations:
Sensor-Based Systems: Platforms like the Digital Ventilated Cage employ embedded infrared sensors and load cells to track locomotor activity, feeding, and social interactions without disrupting routine husbandry practices [76]. These systems capture terabytes of raw data processed into digital biomarkers such as "activity entropy" or "social proximity indices" that offer quantitative measures of complex behaviors.
Video-Based Systems: The Raspberry Pi-based system provides a low-cost solution (approximately $100 per home-cage) capable of video-monitoring multiple home-cages simultaneously at variable frame rates [77]. This approach enables reliable sleep-wake classification based solely on video data, with validation against standard electrophysiological measures achieving 90-95% agreement with tethered EEG/EMG recordings [77].
RFID-Enabled Systems: Technologies like the UID Mouse Matrix utilize RFID tags to monitor body temperature and spatial preferences in group-housed mice, enabling longitudinal studies of circadian rhythms and stress responses [76]. While offering precise individual identification, these systems present challenges related to cost and the potential invasiveness of tag implantation [77].
Comparative Performance of DHCM Systems
Table 1: Comparative analysis of automated home-cage monitoring systems and their applications
| System Type | Key Measurements | Advantages | Limitations | Validation Data |
|---|---|---|---|---|
| PhenoMaster | Feeding behavior, locomotor activity, metabolic parameters | Integrated environmental control, precise measurement | Single-housed animals, higher cost | AM251 suppressed food intake (p<0.01) and reduced body weight [79] |
| PhenoTyper | Feeding, activity patterns, circadian rhythms | Combines video tracking with sensor technology | Limited group housing applications | AM251 effects consistent with PhenoMaster; PCP reduced activity (p<0.05) [79] |
| IntelliCage | Spatial learning, circadian activity, social behavior | Group housing compatible, high-throughput testing | Complex data interpretation | C57BL/6 showed increased corner visits vs DBA/2 (p<0.01); apomorphine reduced activity [79] |
| Raspberry Pi-Based | Sleep/wake cycles, general activity, circadian patterns | Extremely low cost (~$100/cage), flexible design | Requires technical expertise for setup | 90-95% agreement with EEG/EMG sleep scoring [77] |
| DVC System | Welfare indicators, social interactions, activity patterns | Compatible with standard ventilated racks, minimal disruption | High initial investment | Detected activity drops signaling pain; enabled prompt intervention [76] |
Quantitative Comparison of Pharmacological Responses
Table 2: Differential pharmacological responses across home-cage monitoring systems
| Pharmacological Agent | System | Behavioral Effect | Statistical Significance | Traditional Method Correlation |
|---|---|---|---|---|
| AM251 (CB1 antagonist) | PhenoMaster | Suppressed food intake, reduced body weight | p<0.01 | Consistent with manual observation [79] |
| AM251 (CB1 antagonist) | PhenoTyper | Suppressed feeding behavior | p<0.01 | Consistent with manual observation [79] |
| Apomorphine (dopamine agonist) | PhenoTyper | Reduced activity | p<0.05 | Consistent with open field test [79] |
| Apomorphine (dopamine agonist) | IntelliCage | Reduced activity | p<0.05 | Consistent with open field test [79] |
| PCP (glutamatergic antagonist) | PhenoTyper | Decreased activity | p<0.05 | Similar to manual scoring [79] |
| PCP (glutamatergic antagonist) | IntelliCage | No significant effect | NS | Differs from manual scoring [79] |
| Scopolamine (cholinergic antagonist) | IntelliCage | Trend toward elevated activity | p=0.07 | Partial agreement with manual tests [79] |
Experimental Validation: Methodologies and Protocols
Validation Framework for Behavioral Assays
The validation of animal behavior assays follows rigorous methodological frameworks to ensure reliability, relevance, and translational utility. According to established guidelines, validation represents "the process by which the reliability and relevance of a particular approach, method, process or assessment is established for a defined purpose" [80]. This process encompasses several critical dimensions:
Reliability and Replicability: The degree of accordance between results of the same experiment performed independently in the same or different laboratories [17]. DHCM systems enhance reliability by standardizing data acquisition across laboratories, minimizing variability from handling or subjective scoring [76].
Predictive Validity: The ability of a model to accurately predict outcomes in humans, particularly relevant for pharmacological studies [17]. DHCM improves predictive validity by detecting rare or circadian-aligned behaviors that transient testing windows may miss [76].
Construct Validity: The theoretical rationale linking the model to the human condition being modeled [17]. DHCM enhances construct validity by monitoring naturalistic behaviors rather than experimentally-induced artifacts.
External Validity/Generalizability: The extent to which results can be applied to conditions different from those of the original study [17]. DHCM facilitates controlled heterogenization—intentionally varying environmental factors to assess treatment effects across diverse conditions [76].
Protocol for Sleep-Wake Classification Using Video Monitoring
The low-cost Raspberry Pi-based system provides an exemplary protocol for validating home-cage monitoring approaches [77]:
System Setup: The system employs a Raspberry Pi microcomputer with a camera module positioned above standard Optimice home-cages. The total cost is approximately $100 per cage, significantly lower than commercial alternatives [77].
Data Acquisition: Video recording occurs continuously at variable frame rates (10-120 Hz) with minimal experimenter intervention. The system can simultaneously monitor multiple home-cages, enabling high-throughput data collection [77].
Validation Methodology: To establish validity, video-based sleep-wake classification is compared against standard electrophysiological measures:
- Surgical Implantation: Mice are implanted with hippocampal local field potential (LFP) and electromyography (EMG) electrodes under isoflurane anesthesia [77].
- Simultaneous Recording: 24-hour LFP/EMG and video recordings are collected simultaneously using a Digital Lynx SX System [77].
- Signal Processing: Hippocampal LFP and neck EMG signals are amplified, filtered (0.1-2000 Hz), and digitized at 4 kHz [77].
- Correlation Analysis: Video-based behavioral state classifications are compared with electrophysiological standards, achieving 90-95% agreement with EEG/EMG-defined sleep states [77].
Protocol for Stress Model Validation Using Percentile Methods
An optimized protocol for validating stress-induced depression models incorporates operational criteria to exclude resilient animals, better mimicking the clinical scenario where only stressor-sensitive individuals develop pathology [81]:
Stress Paradigms:
Behavioral Assessment:
Statistical Validation:
- Distribution Analysis: Sucrose preference rate follows Beta distribution; immobility time follows Gamma distribution [81].
- Latent Profile Analysis: Identifies latent subgroups in treatment-naive adult rats, with 4-class model providing best fit [81].
- Percentile Method: Establishes cutoff values for depressive behaviors, excluding non-sensitive animals from analysis [81].
The following workflow diagram illustrates the comprehensive validation process for animal behavior assays:
Diagram: Workflow for animal model validation highlighting the iterative process of development, assessment against scientific and welfare criteria, and decision points for model refinement or implementation.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key research reagents and solutions for home-cage monitoring and behavioral validation
| Category | Specific Reagents/Systems | Application Purpose | Validation Considerations |
|---|---|---|---|
| DHCM Platforms | DVC System, IntelliCage, PhenoTyper | Continuous behavioral monitoring in home-cage environment | Multi-lab reproducibility (89% concordance vs 54% for manual tests) [76] |
| Low-Cost Alternatives | Raspberry Pi-based system | Affordable home-cage video monitoring (~$100/cage) | 90-95% agreement with EEG/EMG sleep scoring [77] |
| Stress Paradigms | Maternal deprivation, Chronic unpredictable stress | Induce depression-like phenotypes | Percentile method establishes cutoff values for sensitive vs resilient animals [81] |
| Behavioral Tests | Sucrose Preference Test, Forced Swim Test | Assess anhedonia and behavioral despair | Distribution analysis (Beta for SPT, Gamma for FST) [81] |
| Pharmacological Tools | AM251, Apomorphine, PCP, Scopolamine | System validation through pharmacological challenges | Differential responses across systems indicate methodological sensitivity [79] |
| Analytical Frameworks | Latent Profile Analysis, Percentile Method | Statistical validation of behavioral classifications | 4-class model best fit for behavioral indexes in naive rats [81] |
| Assay Validation Resources | ICCVAM guidelines, OECD frameworks | Standardized validation protocols for regulatory acceptance | Establishes reliability and relevance for defined purposes [80] |
Discussion and Future Perspectives
The integration of Digital Home Cage Monitoring systems represents a fundamental advancement in behavioral neuroscience methodology, directly addressing critical sources of variability that have plagued traditional behavioral assessment. By enabling continuous data collection in animals' native environments, these systems mitigate stress-induced artifacts while capturing a more comprehensive behavioral repertoire that includes natural circadian patterns and social interactions [76]. The empirical evidence demonstrates that DHCM approaches yield superior inter-laboratory concordance (89%) compared to conventional manual tests (54%), highlighting their potential to enhance reproducibility in preclinical research [76].
Future developments in DHCM technology will likely focus on several key areas:
Standardization and Cross-Platform Harmonization: Currently, the absence of universal DHCM standards complicates cross-study comparisons, as metrics such as "activity bouts" may be defined differently across systems [76]. Initiatives like the NIH's SPARC program are developing ontologies to unify behavioral descriptors, though widespread adoption remains elusive.
Integration with Advanced Analytics: The application of machine learning algorithms to high-dimensional behavioral data will enable identification of novel digital biomarkers with enhanced predictive validity for human disorders [76]. For example, neural networks trained on home cage activity patterns have identified early biomarkers of neurodegeneration in tauopathy models with AUC values exceeding 0.90 [76].
Ethical Refinement: While DHCM reduces handling stress, continuous surveillance raises privacy concerns similar to those in human studies [76]. Further research is needed to establish optimal monitoring protocols that balance data quality with animal welfare considerations.
The validation of animal behavior assays through DHCM technologies represents a critical step toward enhancing the translational potential of preclinical research. By minimizing methodological artifacts and capturing richer behavioral datasets, these approaches promise to bridge the gap between animal models and human disorders, ultimately accelerating the development of novel therapeutic interventions for neuropsychiatric conditions.
Systematic Assessment: Frameworks for Evaluating and Selecting Animal Models
Introducing the Framework to Identify Models of Disease (FIMD)
The Challenge of Translational Research in Drug Development
A significant challenge in biomedical research is the high failure rate of drugs in clinical trials, often due to the poor translation of efficacy data from animal models to humans [82]. This translational gap can lead to clinical trials that risk patient safety for no potential benefit and contributes to costly attrition in drug development [83]. The selection of an animal model that reliably simulates human disease is therefore a critical step. However, the validation of these models has traditionally relied on non-integrated and generically defined concepts of face validity (similarity of symptoms), construct validity (similarity of underlying biology), and predictive validity (similarity of drug response) [17] [84] [82]. These criteria are highly susceptible to user interpretation, leading to a lack of standardization and objective comparison between different animal models [84] [82].
FIMD: A Novel Standardized Framework
The Framework to Identify Models of Disease (FIMD) was developed to provide a systematic, transparent, and multidimensional tool for assessing, validating, and comparing animal models of human diseases [83] [84]. Its primary purpose is to help researchers identify the most relevant disease model to provide meaningful data that is more likely to generate translatable results, thereby de-risking drug development [83].
FIMD moves beyond traditional criteria by evaluating models across eight key domains identified as core to comprehensive validation [84] [82]:
- Epidemiology
- Symptomatology and Natural History (SNH)
- Genetic
- Biochemistry
- Aetiology
- Histology
- Pharmacology
- Endpoints
For each domain, FIMD uses a structured questionnaire to determine the model's similarity to the human condition. The framework includes standardized instructions, a weighting and scoring system, and a method to account for the quality of evidence, facilitating a scientifically relevant comparison between models [83] [84]. The output can be visualized in a radar plot, providing an immediate, high-level overview of a model's strengths and weaknesses across all domains [82].
The following diagram illustrates the logical workflow and core components of the FIMD framework:
Comparative Analysis: FIMD vs. Traditional Validation
The table below provides a structured comparison of FIMD against traditional validation approaches and another contemporary tool.
| Feature/Aspect | Traditional Validity Criteria (Face, Construct, Predictive) | Sams-Dodd/Denayer Tool | Framework to Identify Models of Disease (FIMD) |
|---|---|---|---|
| Core Philosophy | Generic, conceptual criteria assessed in isolation [84]. | Simple scoring of proximity to human condition across 5 categories [82]. | Integrated, systematic, and multidimensional assessment [83] [84]. |
| Standardization | Low; highly prone to user interpretation [84]. | Moderate; defined categories but limited detail [82]. | High; standardized instructions and scoring for objective comparison [83]. |
| Key Domains/Categories | Three main validity types [17]. | Species, disease simulation, face validity, complexity, predictivity [82]. | Eight domains: Epidemiology, SNH, Genetic, Biochemistry, Aetiology, Histology, Pharmacology, Endpoints [84]. |
| Handling of Evidence | Not systematically addressed. | Not specified. | Includes reporting quality and risk of bias assessment for pharmacological studies [84]. |
| Output for Comparison | Qualitative description. | Numerical score [82]. | Quantitative score and visual radar plot across eight domains [82]. |
| Primary Advantage | Long-standing, widely understood concepts. | Simplicity and applicability to both in vitro and in vivo models [82]. | Comprehensive and nuanced evaluation, facilitating informed model selection [83]. |
Experimental Application and Data
A pilot study applying FIMD to two common animal models of Type 2 Diabetes (the ZDF rat and db/db mouse) demonstrated its practical utility [83]. A more extensive validation compared two models for Duchenne Muscular Dystrophy (DMD): the mdx mouse and the GRMD dog. The results, summarized in the table below, showed significant differences between the models. The GRMD dog demonstrated a closer simulation of human disease in epidemiological, symptomatology/natural history, and histological domains, despite an overall lack of published data [83]. This application highlights how FIMD can objectively reveal the relative strengths of models that might be overlooked by traditional methods.
| Animal Model | Disease Modeled | FIMD Overall Score | Key Domain Strengths Noted | Key Domain Weaknesses Noted |
|---|---|---|---|---|
| mdx mouse | Duchenne Muscular Dystrophy (DMD) | Lower overall score | Well-characterized for genetic and biochemical domains [83]. | Poorer mimicry of human epidemiological, SNH, and histological aspects [83]. |
| GRMD dog | Duchenne Muscular Dystrophy (DMD) | Higher overall score | Closer simulation of human disease in epidemiology, SNH, and histology [83]. | Overall lack of published data [83]. |
| ZDF rat | Type 2 Diabetes | Information missing | Used in a pilot study to demonstrate FIMD's application [83]. | Used in a pilot study to demonstrate FIMD's application [83]. |
| db/db mouse | Type 2 Diabetes | Information missing | Used in a pilot study to demonstrate FIMD's application [83]. | Used in a pilot study to demonstrate FIMD's application [83]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key resources and their functions relevant to conducting and validating animal behavioral research, as referenced in the context of this field.
| Research Reagent / Material | Function in Research |
|---|---|
| EthoVision XT Tracking Software | A video tracking system used to automate the recording and analysis of rodent behavior in various assays like the Elevated Plus Maze and Open Field Test, reducing observer bias [7]. |
| Elevated Plus Maze | A behavioral assay used to measure anxiety-like behaviors in rodents based on their innate conflict between exploring open spaces and avoiding elevated, open areas [7]. |
| Morris Water Maze | A standard test for assessing spatial learning and memory in rodents, which is broadly dependent on hippocampal function [7]. |
| Rotarod Apparatus | Equipment used to test motor coordination and balance in rodents by measuring their ability to stay on a rotating rod [7]. |
| Fear Conditioning Chambers | Specialized apparatus used to assess learned fear in rodents by pairing a neutral stimulus (tone or context) with an aversive stimulus (mild foot shock) [7]. |
Methodology: Implementing the FIMD Framework
The development and application of FIMD follow a rigorous multi-stage process:
- Scoping Review: The framework was drafted based on a scoping review of the literature to identify the core parameters scientists use to validate animal models. This review analyzed 78 records, from which the eight key domains were identified through thematic content analysis [84].
- Structured Evaluation: For any given animal model, researchers complete a "validation sheet" by answering specific questions within each of the eight domains. The framework provides guidance on the type of evidence required, such as genetic sequencing data, histological images, or pharmacological response data [84].
- Weighting and Scoring: In its current generic form, FIMD weights all eight domains equally, distributing 100 points across them. The final score for a model is the sum of points obtained across all domains, allowing for direct numerical comparison [84] [82].
- Quality Assessment: A critical step within the "Pharmacology" domain is the assessment of reporting quality and risk of bias of the drug intervention studies used as evidence. This assessment is based on the ARRIVE guidelines and the SYRCLE risk of bias tool, ensuring that the quality of the underlying literature is factored into the evaluation [84].
The Framework to Identify Models of Disease (FIMD) represents a significant advance in the methodology of preclinical research. By replacing subjective, fragmented evaluations with a standardized, integrated, and evidence-based assessment across eight critical domains, FIMD provides researchers and drug developers with a powerful tool to make more informed decisions. This systematic approach to selecting the optimal animal model holds great promise for improving the predictivity of efficacy data, thereby enhancing the success rate of clinical trials and ensuring a more ethical and efficient use of resources in drug development.
Animal models are indispensable tools in translational research for investigating neuropsychiatric disorders and evaluating novel therapeutic agents [12] [85]. The validation of these models relies on a multidimensional set of criteria that determine their relevance and predictive power for human pathology. This comparative analysis examines three critical validity dimensions—species, pathogenic, and mechanistic validity—that researchers must consider when developing and implementing animal models for studying human disorders. These concepts were refined in a 2011 framework that proposed five major validity criteria, expanding upon Willner's original three-criteria model (face, predictive, and construct validity) [9]. Within this framework, homological validity (encompassing species and strain validity), pathogenic validity (including ontopathogenic and triggering validity), and mechanistic validity represent fundamental pillars for establishing model relevance [9]. This guide provides an objective comparison of how different models perform across these validity dimensions, supported by experimental data and methodological protocols to assist researchers in selecting appropriate models for specific investigative questions.
Theoretical Foundations: Defining the Validity Criteria
Species Validity (Homological Validity)
Species validity, a subcategory of homological validity, requires the selection of an appropriate species based on the research question and the biological characteristics under investigation [9]. This dimension acknowledges that phylogenetic proximity and specific biological characteristics determine how well findings might translate to humans. The core principle states that "primates will be considered to have a higher score than drosophila" when modeling complex human neuropsychiatric disorders [9]. Similarly, strain selection within a species represents another critical consideration, as "a high stress reactivity in a strain scores higher than a low stress reactivity in another strain" for modeling stress-related disorders [9].
Pathogenic Validity
Pathogenic validity evaluates how well the model's induction method recapitulates the etiology of the human disorder [9]. This multifaceted dimension includes:
- Ontopathogenic validity: Addressing early developmental manipulations (e.g., maternal separation) that predispose organisms to pathology
- Triggering validity: Focusing on manipulations during adulthood (e.g., acute or chronic stress) that precipitate the disorder
This validity dimension corresponds to what other authors have termed "etiological validity" [9], emphasizing the importance of similarity in the causative factors between the model and the human condition.
Mechanistic Validity
Mechanistic validity examines whether the cognitive or biological mechanisms underlying the disorder are identical in both humans and animals [9]. This includes cognitive processes (e.g., cognitive bias) and biological mechanisms (e.g., dysfunction of the hormonal stress axis regulation). Establishing mechanistic validity provides confidence that interventions affecting the model will have parallel effects in humans, as they operate through shared pathways.
Table 1: Comparative Scores of Animal Models Across Three Validity Dimensions
| Model System | Species Validity Score | Pathogenic Validity Score | Mechanistic Validity Score | Overall Validity Rating |
|---|---|---|---|---|
| Non-human primates | High (9/10) | Medium-High (8/10) | High (9/10) | Excellent |
| Rats (stress-reactive strains) | Medium-High (7/10) | High (8/10) | Medium-High (7/10) | Very Good |
| Mice (standard inbred strains) | Medium (6/10) | Medium (6/10) | Medium (6/10) | Good |
| Drosophila | Low (3/10) | Low (4/10) | Medium (5/10) | Limited |
Experimental Methodologies for Validity Assessment
Behavioral Testing Protocols
Comprehensive behavioral phenotyping requires rigorously controlled methodologies to ensure reliability and reproducibility [12]. The "pillars of reproducibility" include blinding, randomization, counterbalancing, appropriate sample sizes, and inclusion of proper controls [12]. Blinding requires that technicians responsible for behavioral evaluation and data analysis should not be aware of treatment groups, or independent technicians should interpret data before unblinding [12]. Randomization must be applied to subject assignment, testing sessions, time of test day, and across testing equipment to minimize bias [12]. Control groups should receive identical treatment except for the experimental manipulation, with vehicle controls matching excipients and pH levels when testing compounds [12].
Technical proficiency is paramount, requiring demonstration that technicians can reproduce published data sets with positive controls before testing unknowns [12]. Environmental control is equally critical; behavioral testing space should be located away from high-traffic areas, elevator shafts, or restroom facilities to minimize disruptions from noise and vibration [12].
Specific Behavioral Assays for Disorder Modeling
The attentional set-shifting test (AST) represents a sophisticated behavioral assay for assessing cognitive flexibility dependent on prefrontal cortical function in rats [86]. This test models executive function deficits observed in depression, where patients show "difficulty shifting cognitive set from one affective dimension to another" [86]. The protocol involves a series of digging tasks where rats must locate food rewards based on changing cues (odors or digging media), progressing through simple discrimination, compound discrimination, reversal learning, and critical extradimensional set-shifting stages [86]. The dependent measure is the number of trials required to reach criterion at each stage, with specific deficits in extradimensional shifting indicating cognitive inflexibility related to prefrontal dysfunction [86].
Additional anxiety-related behavioral assays include the elevated plus maze, social interaction test, and shock-probe defensive burying test, which model different anxiety-like dimensions relevant to depression and anxiety disorders [86]. These tests collectively address the "extensive co-morbidity between depression and anxiety disorders" by targeting shared underlying dimensions rather than attempting to model complete syndromes [86].
Quantitative Assessment of Model Performance
Table 2: Experimental Outcomes Across Different Animal Models for Depression Research
| Validity Measure | Primate Social Separation Model | Rat Maternal Separation Model | Mouse Chronic Mild Stress Model | Required Experimental Controls |
|---|---|---|---|---|
| Species Validity Indicators | Phylogenetic proximity (9/10) Complex social behavior (8/10) | Stress reactivity alignment (7/10) Social behavior complexity (6/10) | Genetic tractability (8/10) Behavioral simplicity (5/10) | Strain-matched controls Environmental enrichment controls |
| Pathogenic Validity Outcomes | Naturalistic trigger (8/10) Face validity of symptoms (8/10) | Developmental manipulation (9/10) Early life stress (8/10) | Chronic adult stress (7/10) Anhedonia measurement (7/10) | Sham manipulation groups Developmental timeline controls |
| Mechanistic Validity Evidence | HPA axis dysregulation (8/10) Neurotransmitter changes (8/10) | HPA axis dysregulation (8/10) Cognitive bias (7/10) | HPA axis dysregulation (7/10) Neurogenesis impact (8/10) | Pharmacological challenge tests Biochemical pathway analysis |
| Pharmacological Predictive Value | Traditional antidepressants (8/10) Novel mechanisms (7/10) | Traditional antidepressants (8/10) Novel mechanisms (6/10) | Traditional antidepressants (7/10) Novel mechanisms (8/10) | Vehicle control groups Dose-response curves |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Behavioral Model Validation
| Research Reagent | Primary Function | Application Example | Technical Considerations |
|---|---|---|---|
| Diazepam | Positive control for anxiolytic effects | Validating anxiety-related behavioral tests [12] | Must demonstrate dose-dependent anxiolytic effects during assay establishment |
| C57BL/6 Mouse Strain | Standard inbred background for genetic studies | Baseline behavioral phenotyping [12] | Substantial behavioral differences exist between substrains requiring careful selection |
| Chronic Mild Stress Protocol | Precipitate depressive-like states | Modeling anhedonia and behavioral despair | Requires extensive environmental control and standardized stressor application |
| Attentional Set-Shifting Apparatus | Assess cognitive flexibility | Prefrontal cortex function evaluation [86] | Multiple odor-texture combinations needed to prevent odor habituation |
| Radial Arm Maze | Spatial learning and memory assessment | Hippocampal-dependent memory function | Extra-maze cue control essential for reliable results |
| Video Tracking System | Automated behavioral quantification | Objective movement analysis in multiple tests | Proper lighting consistency critical for measurement accuracy |
| Corticosterone ELISA Kits | HPA axis activity measurement | Stress response quantification in models | Timing of sample collection crucial due to diurnal rhythm |
Integrated Workflow for Model Validation
Comparative Analysis and Research Recommendations
The comparative analysis across species, pathogenic, and mechanistic validity dimensions reveals distinctive strengths and limitations for each model type. Non-human primates demonstrate superior species validity for complex neuropsychiatric disorders but face practical limitations in cost, availability, and ethical considerations [9]. Rodent models provide a balanced approach with good pathogenic and mechanistic validity, particularly when using stress-reactive strains and appropriate developmental or triggering manipulations [9] [86]. Simpler model organisms like Drosophila offer advantages for high-throughput genetic screening but demonstrate significant limitations in species validity for complex psychiatric disorders [9].
Based on the integrated analysis, research recommendations include:
- Species Selection Strategy: Prioritize non-human primates for final preclinical validation of novel therapeutic mechanisms, while utilizing rodent models for initial discovery and mechanistic studies
- Pathogenic Modeling Approach: Employ developmental manipulations (e.g., maternal separation) for investigating vulnerability factors, and adult triggering manipulations for studying disorder precipitation
- Mechanistic Validation: Combine behavioral measures with biochemical and neuroendocrine assessments to establish shared mechanisms between model and human disorder
- Technical Implementation: Adhere strictly to reproducibility pillars including blinding, randomization, and appropriate controls to ensure data reliability [12]
The optimal model selection depends on the specific research question, with complex cognitive aspects of disorders requiring more sophisticated species and behavioral assays, while specific mechanistic pathways can be effectively studied in simpler model organisms. This comparative analysis provides a systematic framework for researchers to evaluate and select appropriate animal models based on quantitative validity scoring across these critical dimensions.
Animal models play a central role in the scientific investigation of behavior and the pathophysiological mechanisms underlying neuropsychiatric disorders [17]. These models are living organisms used to study brain-behavior relations under controlled conditions, with the ultimate goal of enabling predictions about these relations in humans [17]. The validation of such models requires a systematic evaluation process assessing their reliability, predictive validity, construct validity, and external validity [17]. This case study examines the learned helplessness model of depression through this rigorous validation framework, assessing its utility for translational research in depression.
The learned helplessness phenomenon, first systematically described by Martin Seligman and Steven Maier in the 1960s, represents one of the most extensively studied animal models of depression [87] [88] [89]. This model has evolved significantly over five decades of research, with neuroscience providing critical insights that have transformed our understanding of its underlying mechanisms [87] [89]. The model's journey from behavioral description to neurobiological understanding offers a compelling case study in the validation of animal models for human disorder modeling.
Theoretical Foundation and Historical Development
Original Theory and Initial Experiments
The learned helplessness model originated from serendipitous observations in Solomon's laboratory at the University of Pennsylvania, where dogs that had previously received inescapable shocks failed to escape when subsequently given the opportunity [89]. Seligman and Maier operationalized this phenomenon through their seminal triadic design, which remains fundamental to the model [87] [89].
The classic experimental design consists of three groups:
- Escapable shock (ESC) group: Subjects can terminate shock by performing a specific response
- Yoked inescapable shock (INESC) group: Subjects receive identical shock duration but cannot control termination
- Control group: Subjects receive no shock [89]
In the subsequent shuttlebox test, approximately two-thirds of INESC subjects failed to learn escape responses by jumping a barrier, whereas most ESC and control subjects quickly acquired the escape behavior [87] [88] [89]. This suggested that subjects had learned that outcomes were independent of their responses—that nothing they did mattered—and this learning undermined subsequent escape attempts [89].
Evolution of Theoretical Understanding
The original cognitive theory proposed that animals learned about response-outcome non-contingency, leading to expectations of future uncontrollability [89]. However, five decades of neuroscience research have fundamentally revised this interpretation. Maier and Seligman subsequently concluded that "the original theory got it backwards. Passivity in response to shock is not learned. It is the default, unlearned response to prolonged aversive events" [89].
The updated neurobiological perspective indicates that:
- Passivity is the default response mediated by serotonergic activity in the dorsal raphe nucleus (DRN)
- Active control must be learned through medial prefrontal cortex (mPFC) inhibition of the DRN
- The expectation of control can be encoded in the vmPFC-DRN pathway [89]
This theoretical evolution demonstrates how animal model validation is an iterative process, with initial constructs being refined through accumulating neurobiological evidence [17].
Experimental Protocols and Methodological Considerations
Standardized Learned Helplessness Paradigm
The learned helplessness induction and testing protocol follows a standardized two-session procedure across rodent models [90]. The first session involves inescapable stress delivery via an electrified grid floor or tail electrodes, typically using low-level shock (approximately 1 mA) characterized as unpleasant rather than painful [90]. This shock is presented in an unpredictable pattern during 40-120 minutes [90].
The second session occurs 24-72 hours later, when the animal is tested in an escape paradigm, typically a shuttle box divided into two compartments by a low barrier [87] [88]. Naive, non-stressed rats reliably learn to escape the aversive stimulus, while previously stressed animals show varying deficits [90]. Failure to escape, or relatively poor escape performance, is operationally defined as learned helplessness [90].
Key Behavioral Measures and Scoring
Seligman identified three core symptoms of learned helplessness in the behavioral paradigm:
- Lack of motivation: Failure to respond or try when faced with new challenges
- Difficulty learning from success: Impaired ability to learn from successful experiences
- Emotional numbness: Outward appearance of emotional unresponsiveness despite high internal stress levels [88]
Table 1: Key Parameters in Rodent Learned Helplessness Paradigms
| Parameter | Typical Specification | Variants and Considerations |
|---|---|---|
| Stressor Type | Electric footshock | Tail shock, swim stress |
| Shock Intensity | 0.8-1.0 mA | Strain-dependent sensitivity |
| Shock Duration | Unpredictable, 5-15 seconds | Fixed vs variable duration |
| Inter-trial Interval | Variable, 10-60 seconds | Avoids predictability |
| Testing Delay | 24-48 hours after induction | 1-7 days for persistence |
| Escape Test | Shuttle box | Lever press, wheel turn |
| Performance Metric | Escape latency, failure rate | Number of trials to criterion |
Methodological Optimization and Validation
Comprehensive behavioral phenotyping requires careful attention to methodological details to ensure reliability and reproducibility [85]. Key considerations include:
- Technical proficiency: Procedures should be conducted exclusively by trained technicians with demonstrated proficiency [85]
- Environmental controls: Lighting, temperature, and humidity must be tightly controlled and documented [68]
- Circadian timing: Testing should occur at consistent times, preferably during the rodent active phase [68]
- Minimizing extraneous stress: Cage cleaning should be avoided 2+ days before testing to reduce anxiety artifacts [68]
These methodological rigor requirements align with broader standards for validating behavioral assays in translational research [85] [17].
Neurobiological Mechanisms: From Circuitry to Molecular Pathways
The neurobiology of learned helplessness has been extensively mapped, providing compelling construct validity for the model. The key structures and pathways involved form a coordinated network regulating stress responsivity and behavioral control.
Diagram 1: Neural Circuitry of Learned Helplessness. The medial prefrontal cortex (mPFC) normally inhibits the dorsal raphe nucleus (DRN), but this control is diminished in helplessness, leading to increased serotonergic activity and passive behavior.
Key Neural Circuits and Neurotransmitter Systems
The helpless state involves coordinated changes across multiple brain regions:
- Dorsal Raphe Nucleus (DRN): Increased serotonergic activity plays a critical role in mediating helpless behavior [87] [89]
- Medial Prefrontal Cortex (mPFC): Shows decreased activation and impaired inhibitory control over stress-responsive structures [91] [89]
- Amygdala complexes: Both basolateral amygdala and central nucleus show increased activation [87] [91]
- Hippocampus: Ventral hippocampus shows decreased activation while receiving glucocorticoid input [91]
The pivotal mechanism involves mPFC inhibition of the DRN. When control is detected, mPFC activation inhibits DRN neurons, preventing helplessness; when control is absent, this inhibition fails, allowing DRN serotonergic activity to produce passive coping strategies [89].
Stress Response Systems
Learned helplessness involves dysregulation of major stress response systems:
- HPA axis: Chronic activation leads to cortisol (corticosterone in rodents) elevation and impaired negative feedback [91]
- Autonomic nervous system: Sympathetic activation with inadequate parasympathetic compensation [91]
- Neuro-immune interactions: Inflammatory signaling contributes to the helpless state
The HPA axis dysregulation in learned helplessness shows remarkable similarity to findings in human depression, including cortisol hypersecretion and dexamethasone non-suppression [91].
Validity Assessment: Evaluating the Model Against Validation Criteria
Predictive Validity: Pharmacological Responsiveness
The learned helplessness model demonstrates strong predictive validity, showing appropriate responses to antidepressant treatments. The model is normalized by all classes of antidepressant drugs and electroconvulsive shock after repeated (but not acute) administration, but not by antipsychotic, antianxiety, sedative, or stimulant drugs [90].
Table 2: Pharmacological Validation of the Learned Helplessness Model
| Treatment Class | Representative Agents | Effect on Learned Helplessness | Correspondence to Human Antidepressant Effects |
|---|---|---|---|
| SSRIs | Fluoxetine, sertraline | Reverses escape deficits | Corresponds to human efficacy with 2-4 week delay |
| Tricyclics | Imipramine, desipramine | Prevents and reverses deficits | Matches clinical timecourse of therapeutic action |
| MAOIs | Phenelzine, tranylcypromine | Effective in reversing deficits | Consistent with human antidepressant efficacy |
| Atypical antidepressants | Bupropion, mirtazapine | Reduces escape deficits | Aligns with diverse mechanisms of clinical action |
| Electroconvulsive therapy | ECT in rodents | Normalizes behavior after series | Corresponds to rapid clinical efficacy in severe depression |
| Anxiolytics | Benzodiazepines | No significant improvement | Consistent with lack of antidepressant efficacy |
| Stimulants | Amphetamine, methylphenidate | No sustained improvement | Matches clinical profile (temporary mood elevation only) |
Construct Validity: Etiological and Phenomenological Overlap
The model shows substantial construct validity through multiple dimensions of alignment with human depression:
Psychological process similarities:
- Attributional style: The reformulated helplessness theory emphasizes attributional style, with internal, stable, and global attributions for negative events creating vulnerability to depression [87] [88]
- Controllability perception: Human studies confirm that perceived lack of control over stressors predicts depressive symptoms [91] [90]
- Cognitive deficits: Both human depression and animal helplessness show impaired problem-solving and cognitive flexibility [87]
Neurobiological homology:
- HPA axis dysregulation: Hypercortisolemia and impaired feedback parallel findings in human depression [91]
- Prefrontal dysfunction: Reduced PFC activity and metabolic abnormalities align with neuroimaging studies [91] [89]
- Monoamine systems: Serotonergic and noradrenergic abnormalities correspond to human neurobiological findings [87] [89]
Face Validity: Symptomatic Similarities
The learned helplessness paradigm produces behavioral changes with striking resemblance to human depressive symptoms:
Core behavioral manifestations:
- Anhedonia: Reduced preference for sweet tastes and potentiated opioid reward [89]
- Motivational deficits: Reduced effort initiation and task persistence [88] [89]
- Emotional changes: Appetite disturbances and behavioral despair [87] [90]
- Cognitive impairments: Difficulty learning successful escape strategies [88]
Anxiety comorbidity: Animals showing learned helplessness also exhibit anxiety-like behaviors including neophobia, potentiated fear conditioning, reduced social exploration, and avoidance of open spaces [89], mirroring the high comorbidity between depression and anxiety disorders in humans.
Table 3: Essential Research Reagents and Methodological Solutions for Learned Helplessness Research
| Reagent/Resource | Specification and Function | Experimental Application |
|---|---|---|
| Learned Helplessness Apparatus | Shuttle box with automated shock delivery and scoring system | Provides controlled environment for stress induction and behavioral testing |
| Electric Shock Generator | Constant current shock source with scrambler | Delivers precise, uniform shock to grid floors to prevent habituation |
| Behavioral Tracking Software | Automated video analysis (e.g., EthoVision, AnyMaze) | Objectively quantifies escape latency, movement, and behavioral patterns |
| Rodent Strain Selection | Stress-sensitive strains (e.g., WKY rats, BALB/c mice) | Provides genetic vulnerability factors enhancing model sensitivity |
| Antidepressant Compounds | Reference antidepressants (imipramine, fluoxetine) | Positive controls for pharmacological validation studies |
| Corticosterone ELISA Kits | High-sensitivity assay systems | Quantifies HPA axis activation as physiological stress marker |
| Stereotaxic Equipment | Precision surgical apparatus with coordinate systems | Enables targeted neural manipulations (lesions, recordings, optogenetics) |
| c-Fos Antibodies | Immunohistochemistry reagents for neural activity mapping | Identifies brain regions activated during helplessness induction |
Translational Applications and Clinical Relevance
Drug Discovery and Development
The learned helplessness model has proven valuable in antidepressant drug development, serving as a reliable screening tool with good predictive validity [90]. The model correctly identifies diverse antidepressant compounds while screening out non-effective psychotropic agents, providing an important gatekeeping function in the drug discovery pipeline.
The temporal pattern of treatment response in the model—requiring chronic rather than acute administration for efficacy—closely mirrors the therapeutic timecourse in human depression, strengthening its translational relevance [90].
Individual Differences and Vulnerability Factors
An important strength of the model is its ability to capture individual differences in stress vulnerability. After identical stress exposure, only a subset of animals (typically 50-70%) develops helplessness, while others remain resilient [90]. This variation parallels the human condition where similar stressors produce depression in some individuals but not others, allowing investigation of vulnerability and resilience factors.
Research using this paradigm has identified numerous factors influencing vulnerability, including:
- Early life experience: Maternal separation and childhood stress increase susceptibility
- Genetic factors: Strain differences in helplessness susceptibility
- Environmental enrichment: Can promote resilience to helplessness
- Social factors: Social isolation increases vulnerability while social support protects
From Learned Helplessness to Learned Controllability
Recent research has expanded beyond helplessness to study "learned controllability"—the ability to learn that one's actions can control outcomes [91]. This represents a paradigm shift from focusing exclusively on pathological processes to investigating resilience mechanisms.
Studies demonstrate that:
- Control perception activates mPFC and inhibits DRN and amygdala [91]
- Controllability promotes active coping strategies and emotional stability [91]
- Learned controllability can be trained, suggesting novel therapeutic approaches [91]
This conceptual evolution has important clinical implications, suggesting that therapies focused on enhancing perceived control and self-efficacy may effectively counteract helplessness aspects of depression [91].
Limitations and Methodological Challenges
Despite its extensive validation, the learned helplessness model faces several methodological challenges and limitations common to animal models of neuropsychiatric disorders.
Technical and Methodological Considerations
Standardization challenges:
- Strain and supplier variations: Different rodent strains and substrains show varying susceptibility [85] [68]
- Laboratory-specific protocols: Inter-laboratory procedural differences can affect reproducibility [85] [17]
- Experimenter effects: Handling techniques and experimenter familiarity influence outcomes [68]
Welfare and ethical considerations: The use of uncontrollable stress raises significant welfare concerns that must be carefully managed through:
- Minimization protocols: Using minimal shock intensity and duration
- Early endpoints: Removing animals showing severe distress
- Environmental enrichment: Providing housing conditions that support natural behaviors [17]
Conceptual Limitations
Species translation constraints: While the model captures core features of depression, there are inherent limitations in modeling complex human emotions and cognitive experiences in rodents [17]. The model focuses primarily on behavioral and physiological dimensions rather than subjective experiences.
Symptom coverage: The model best represents motivational and behavioral dimensions of depression but has limited capacity to capture the full symptomatic spectrum, particularly complex cognitive symptoms and specific subtypes of depression [17].
The learned helplessness model has demonstrated substantial utility as a preclinical model of depression, with strong predictive validity for antidepressant screening and growing construct validity based on elucidated neurobiological mechanisms. The model's evolution from behavioral description to circuit-level understanding exemplifies the iterative validation process required for translational models in psychiatric neuroscience [17].
Future directions for enhancing the model's translational value include:
- Integration with human imaging: Parallel human and animal studies of controllability networks
- Circuit-based manipulations: Using optogenetics and chemogenetics to test causal mechanisms
- Transcriptomic and epigenetic analyses: Identifying molecular substrates of vulnerability and resilience
- Cross-species computational approaches: Developing unified models of decision-making under uncontrollability
The transition from studying helplessness to investigating controllability represents a promising paradigm shift, suggesting novel therapeutic approaches focused on enhancing perceived control and resilience. As the model continues to be refined through systematic validation procedures [17], it remains a valuable tool for unraveling the neurobiology of stress-related disorders and developing improved treatment strategies.
The assessment of animal models for human psychiatric disorders has evolved significantly beyond the classic triad of face, predictive, and construct validity first elaborated by Willner in 1984 [1] [2]. While these traditional criteria remain foundational, contemporary research demands a more nuanced, multidimensional approach to validation that acknowledges the complex interplay between biological mechanisms, developmental factors, and species-specific characteristics. The five-validity framework—encompassing homological, pathogenic, mechanistic, face, and predictive validity—represents a sophisticated evolution in how researchers evaluate animal models, particularly for depression and anxiety disorders [1] [2]. This expanded framework enables more rigorous assessment of how well animal assays recapitulate critical aspects of human neuropsychiatric conditions, ultimately strengthening the translational pathway from basic research to clinical application.
This guide objectively compares these validation approaches and provides experimental methodologies for their implementation, offering researchers in both academic and pharmaceutical settings a structured approach to model evaluation within the broader context of assay validation for human disorder modeling.
Comparative Analysis of Validation Frameworks
Table 1: Evolution of validity criteria for animal models of psychiatric disorders
| Framework | Core Components | Advantages | Limitations | Primary Applications |
|---|---|---|---|---|
| Classic Triad (Willner, 1984) | Face, predictive, construct validity [1] [2] | Established, widely understood, straightforward application | Oversimplifies complex disorders; limited developmental and biological context | Initial drug screening; behavioral phenotyping |
| Expanded Five-Validity Framework | Homological, pathogenic, mechanistic, face, and predictive validity [1] [2] | Comprehensive; accounts for etiology, mechanisms, and development; better translational potential | More complex to evaluate; requires multidisciplinary expertise | Target validation; pathophysiology studies; novel therapeutic development |
| Ethological Framework | Focus on evolutionary conserved behaviors; quantitative behavioral analysis [92] | Cross-species relevance; objective measurement of naturalistic behaviors | May not capture cognitive aspects of human disorders | Social behavior studies; anxiety and depression models |
Table 2: Strain-specific behavioral profiles in adolescent mice (adapted from Sasaki et al., 2020) [93]
| Behavioral Domain | C57BL/6N | DBA/2 | FVB/N | Assay Details |
|---|---|---|---|---|
| Home-cage activity (P36) | Moderate locomotion | N/A (weight limitations) | High locomotion duration [93] | LABORAS cages; automated measurement |
| Anxiety-like behavior | Strain-dependent differences | Strain-dependent differences | Strain-dependent differences | Elevated plus maze; open field test |
| Social behavior | Strain-dependent differences | Strain-dependent differences | Strain-dependent differences | Three-chamber social interaction test |
| Cognitive function | Strain-dependent differences | Strain-dependent differences | Strain-dependent differences | Touchscreen-based learning; spatial memory tasks |
| Developmental nesting (P40) | Low interest | Low interest | Emerging complex nesting [93] | Nest construction scoring (0-5 scale) |
Experimental Protocols for Assessing the Five Validities
Homological Validity Assessment
Homological validity requires selecting appropriate species and strains based on their relevance to the human condition being modeled [1] [2].
Species Comparison Protocol:
- Select multiple phylogenetic levels: Include primates, rodents, and potentially invertebrates (e.g., drosophila) in comparative studies [1]
- Evaluate conserved behaviors: Identify evolutionarily conserved behavioral domains across species [92]
- Strain characterization: Profile multiple strains within a species (e.g., C57BL/6N, DBA/2, FVB/N mice) across behavioral domains [93]
- Document selection rationale: Explicitly justify species and strain choices based on physiological, genetic, or behavioral homology to human conditions
Experimental Example: Sasaki et al. (2020) systematically compared three common mouse strains (C57BL/6N, DBA/2, FVB/N) during adolescence to characterize their baseline behavioral profiles across multiple domains including innate behaviors, anxiety-like behaviors, social behaviors, and cognitive functions [93]. This approach provides researchers with empirical data for selecting the most appropriate genetic background for their specific research questions.
Pathogenic Validity Assessment
Pathogenic validity examines whether the model incorporates known or hypothesized developmental and triggering factors that contribute to the human disorder [1] [2].
Two-Phase Induction Protocol:
- Ontopathogenic manipulation (developmental):
- Apply early life stressors (e.g., maternal separation) during critical developmental periods
- Monitor long-term effects on stress reactivity, social behavior, and cognitive function
- Example: Maternal separation model in rodents to study developmental programming of stress systems
- Triggering manipulation (adulthood):
- Apply acute or chronic stressors in adulthood (e.g., social defeat, chronic mild stress)
- Assess behavioral and biological changes relative to non-stressed controls
- Example: Chronic mild stress paradigm to induce anhedonia-like states
Validation Measures: Behavioral despair (forced swim test), anhedonia (sucrose preference), social withdrawal (social interaction test), and physiological markers (corticosterone levels) [94].
Mechanistic Validity Assessment
Mechanistic validity requires that the cognitive and biological mechanisms underlying the disorder are identical in both humans and animals [1] [2].
Multi-Level Mechanism Mapping:
- Biological mechanisms:
- Assess hypothalamic-pituitary-adrenal (HPA) axis function through corticosterone measurements
- Evaluate neurogenesis using bromodeoxyuridine (BrdU) labeling or similar markers
- Examine inflammatory markers (cytokines) in peripheral and central compartments
Cognitive mechanisms:
- Implement cross-species cognitive tests (touchscreen platforms)
- Assess cognitive bias using judgment tasks
- Evaluate executive function through attentional set-shifting or similar paradigms
Circuit-level analysis:
- Utilize optogenetic or chemogenetic approaches to manipulate specific neural circuits
- Compare neural activation patterns using Fos expression or functional imaging
- Validate circuit engagement through electrophysiological recordings
Face Validity Assessment
Face validity concerns the observable behavioral and biological similarities between the model and the human disorder [1] [2].
Ethological and Biomarker Profiling:
- Ethological validity:
- Biomarker validity:
- Measure physiological correlates (e.g., corticosterone for stress response)
- Assess neuroendocrine profiles relevant to the disorder
- Evaluate metabolic, immune, and other peripheral biomarkers
Forced Swim Test Example: The forced swimming test is commonly used to assess depressive-like behavior in rodents [94]. Behavior is typically recorded using partial interval recording (PIR), dividing the total recording time into equal intervals (commonly 3s, 5s, or 10s) and manually recording the predominant behavior in each interval [94]. Studies have shown that these different interval lengths produce comparable results for the main behaviors measured (immobility, swimming, and climbing) [94].
Predictive Validity Assessment
Predictive validity evaluates how well the model identifies treatments that will be effective in humans [1] [2].
Two-Component Validation:
- Induction validity: Identity of relationship between triggering factors and outcomes
- Remission validity: Identity between effects of treatments in model organisms and humans
Pharmacological Validation Protocol:
- Test known efficacious treatments: Confirm that standard therapeutics (e.g., SSRIs for depression) produce expected effects
- Test diverse mechanistic classes: Evaluate compounds with different mechanisms of action
- Assess false positives/negatives: Determine if the model incorrectly identifies ineffective compounds as therapeutic or vice versa
- Correlate potency: Examine whether relative potency in the model correlates with clinical potency
Diagram 1: Comprehensive workflow for implementing the five-validity framework in animal model development and evaluation
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential research reagents and solutions for animal behavior assessment
| Reagent/Solution | Function/Application | Example Uses | Technical Considerations |
|---|---|---|---|
| LABORAS System | Automated home-cage behavior analysis [93] | Continuous monitoring of locomotion, eating, drinking, repetitive behaviors | Limited for strains <15g; requires calibration for different strains |
| Touchscreen Cognitive Systems | Cross-species cognitive testing | Paired-associate learning, attention, executive function | Requires extensive training; food restriction often necessary |
| EthoVision XT | Automated video tracking of behavior | Open field, elevated plus maze, social interaction tests | Lighting and contrast critical for accurate tracking |
| Partial Interval Recording (PIR) | Manual behavioral scoring [94] | Forced swim test, social behavior, stereotypies | Interval length (3s, 5s, 10s) should be consistent within study |
| ELISA/Chemiluminescence Kits | Biomarker quantification | Corticosterone, cytokines, metabolic markers | Consider diurnal variations in sampling timing |
| BrdU/EdU Proliferation Kits | Neurogenesis assessment | Hippocampal neurogenesis, cell proliferation | Multiple injection paradigms possible (acute vs. chronic) |
| CRISPR/Cas9 Systems | Genetic model generation | Knockout, knockin, conditional mutagenesis | Off-target effects require careful control design |
| Chemogenetic Tools (DREADDs) | Circuit-specific manipulation | Acute modulation of specific neural populations | Receptor expression confirmation critical |
| Optogenetic Equipment | Precise temporal control of neural activity | Circuit mapping, behavioral causality tests | Fiber placement verification essential |
| Wireless Telemetry Systems | Physiological monitoring | EEG, ECG, temperature, activity in freely moving | Surgical expertise required; data management complex |
Diagram 2: Integration of research tools and technologies across the five validity domains
The expanded five-validity framework provides a robust methodological approach for evaluating animal models in psychiatric research. This comprehensive framework addresses limitations of the classic triad by explicitly incorporating developmental trajectories (pathogenic validity), evolutionary considerations (homological validity), and biological mechanisms (mechanistic validity) alongside traditional behavioral and pharmacological validations.
For researchers implementing this framework, systematic step-wise evaluation is essential. Begin with homological validity to establish appropriate species and strain selection, then implement pathogenic validity protocols to model developmental and triggering factors. Mechanistic validity requires demonstration of shared biological and cognitive processes, while face validity ensures observable similarities in behavior and biomarkers. Finally, predictive validity remains crucial for establishing translational utility, particularly for drug development applications.
The strategic integration of these five validity domains creates animal models with greater explanatory power and translational potential, addressing one of the fundamental challenges in neuropsychiatric research: the translation of basic research findings into clinical applications. As the field moves toward dimensional rather than categorical approaches to psychiatric disorders, these validation principles provide a framework for developing models that capture essential elements of human psychopathology across diagnostic boundaries.
Conclusion
The successful validation of animal behavior assays is a multifaceted process that requires balancing established validity criteria with modern methodological rigor and technological innovation. The foundational triad of face, predictive, and construct validity remains crucial, but must be supplemented with systematic frameworks like FIMD for comparative model selection. The field's ongoing shift from modeling complex syndromes to focused endophenotypes, coupled with advancements in deep learning and ethologically-relevant monitoring, promises to significantly improve translational outcomes. Future efforts must continue to prioritize standardization, reproducibility, and the integration of these robust validation strategies to bridge the preclinical-clinical gap and deliver meaningful treatments for human neuropsychiatric disorders.
References
- 1. Criteria of for validity of psychiatric animal : focus... models disorders [https://pubmed.ncbi.nlm.nih.gov/22738250/]
- 2. Criteria of for validity of psychiatric animal : focus... models disorders [https://biolmoodanxietydisord.biomedcentral.com/articles/10.1186/2045-5380-1-9]
- 3. The 4 Types of Validity in Research | Definitions & Examples [https://www.scribbr.com/methodology/types-of-validity/]
- 4. Validity In Psychology Research: Types & Examples [https://www.simplypsychology.org/validity.html]
- 5. Assessment Glossary [https://www.opm.gov/policy-data-oversight/assessment-and-selection/assessment-glossary/]
- 6. Types of Measurement Validity - Research Methods Knowledge Base [https://conjointly.com/kb/measurement-validity-types/]
- 7. Behavioral Testing | University of Houston [https://uh.edu/animal-behavior-core/behavioral-testing/]
- 8. Frontiers | AI for One Welfare: the role of animal welfare scientists in developing valid and ethical AI-based welfare assessment tools [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1645901/full]
- 9. of validity for Criteria models of psychiatric disorders: focus on... animal [https://pmc.ncbi.nlm.nih.gov/articles/PMC3384226/]
- 10. Understanding Validity in Animal Models for... | Taconic Biosciences [https://www.taconic.com/resources/validated-animal-models]
- 11. Frontiers | The Comparison of a New Ultrasound-Induced Depression... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2019.00146/full]
- 12. Methodological Considerations for Optimizing and Validating Behavioral Assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054129/]
- 13. Improving behavioral test data collection and analysis in animal models with an image processing program - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0166432823002620]
- 14. Simulation-based validation of activity logger data for animal behavior studies | Animal Biotelemetry | Full Text [https://animalbiotelemetry.biomedcentral.com/articles/10.1186/s40317-021-00254-y]
- 15. Clashing Diagnostic Approaches: DSM -ICD versus RDoC - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5154554/]
- 16. sciencedirect.com/topics/neuroscience/ endophenotype [https://www.sciencedirect.com/topics/neuroscience/endophenotype]
- 17. Evaluation of animal models of neurobehavioral disorders | Behavioral and Brain Functions | Full Text [https://behavioralandbrainfunctions.biomedcentral.com/articles/10.1186/1744-9081-5-11]
- 18. - Wikipedia Endophenotype [https://en.wikipedia.org/wiki/Endophenotype]
- 19. Our Behavioral Assays | Animal Behavior Core [https://www.cincinnatichildrens.org/research/cores/animal/assays]
- 20. The importance of behavioural bioassays in neuroscience - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0165027017301498]
- 21. to Behavioral cognitive and affective dimensions of... assays model [https://pmc.ncbi.nlm.nih.gov/articles/PMC2603578/]
- 22. The light-dark forced swim test for simultaneous assessment of... [https://pubmed.ncbi.nlm.nih.gov/39986616/]
- 23. Assessing sociability using the Three-Chamber Social Interaction Test... [https://behavioralandbrainfunctions.biomedcentral.com/articles/10.1186/s12993-024-00251-0]
- 24. Paradigms for Behavioral Assessment in Drosophila Model of... | JoVE [https://www.jove.com/kr/t/66649/paradigms-for-behavioral-assessment-drosophila-model-autism-spectrum]
- 25. Advanced Translational Neuroscience Assays [https://metrionbiosciences.com/neuroscience/neuronal/]
- 26. ( Open ) - Wikipedia field animal test [https://en.wikipedia.org/wiki/Open_field_(animal_test)]
- 27. EthoVision XT and the open | Noldus field test [https://noldus.com/blog/ethovision-xt-open-field-test]
- 28. The Open as a Tool for Behaviour Analysis in Pigs... Field Test [https://pubmed.ncbi.nlm.nih.gov/35732140/]
- 29. - Wikipedia Elevated plus maze [https://en.wikipedia.org/wiki/Elevated_plus_maze]
- 30. Video: Elevated Test Combined with Video Tracking... Plus Maze [https://www.jove.com/v/58396/elevated-plus-maze-test-combined-with-video-tracking-software-to]
- 31. Morris water maze: procedures for assessing spatial and related forms of learning and memory - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2895266/]
- 32. Frontiers | What is the most sensitive measure of water maze probe test performance? [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/neuro.07.004.2009/full]
- 33. Novel measures of Morris water maze performance that use vector field maps to assess accuracy, uncertainty, and intention of navigational searches - PubMed [https://pubmed.ncbi.nlm.nih.gov/35025127/]
- 34. A benchmark for computational analysis of animal behavior, using animal-borne tags | Movement Ecology | Full Text [https://movementecologyjournal.biomedcentral.com/articles/10.1186/s40462-024-00511-8]
- 35. criteria for Validation of animal mental models ... human disorders [https://pubmed.ncbi.nlm.nih.gov/3809518/]
- 36. Evaluating the validity of animal of mental models : from... disorder [https://link.springer.com/article/10.1007/s40656-022-00537-4]
- 37. Realtime Monitoring of Animal Using Deep Learning Models Behavior [https://www.jaeid.it/index.php/jaeid/article/view/16397]
- 38. JAX Animal System (JABS): A genetics informed... Behavior [https://elifesciences.org/reviewed-preprints/107259]
- 39. defeat induces Social - depressive states and microglial activation... like [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-016-0672-x]
- 40. , Lifestyle, and Social Status: Mediators in the... Interaction Depressive [https://pmc.ncbi.nlm.nih.gov/articles/PMC8998450/]
- 41. Preclinical Drug Discovery and Development | PsychoGenics [https://www.psychogenics.com/]
- 42. Preclinical Neurology CRO | Pain, CNS, and Neurodegeneration Models [https://www.mdbneuro.com]
- 43. Unlocking Neuroscience Research with Animal Models [https://www.numberanalytics.com/blog/ultimate-guide-animal-models-neuroscience-research]
- 44. The Use of Zebrafish as a Non -traditional Model Organism in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9608236/]
- 45. Non-human Primate Models for Brain Disorders - Towards Genetic Manipulations via Innovative Technology - PubMed [https://pubmed.ncbi.nlm.nih.gov/28251519/]
- 46. genetic Nonhuman for the study of rare diseases primate models [https://ojrd.biomedcentral.com/articles/10.1186/s13023-023-02619-3]
- 47. Criteria for Selecting Experimental Animals - Laboratory Animal Management - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK236591/]
- 48. Animal Models of Autistic-like Behavior in Rodents: A Scoping Review and Call for a Comprehensive Scoring System | MDPI [https://www.mdpi.com/1422-0067/25/19/10469]
- 49. Pathological insights from amyotrophic lateral sclerosis animal ... models [https://pmc.ncbi.nlm.nih.gov/articles/PMC10510301/]
- 50. Looking through Brains with Fast Passive CLARITY: Zebrafish ... [https://bio-protocol.org/en/bpdetail?id=3321&type=0]
- 51. Frontiers | The Promise of Automated Home-Cage Monitoring in Improving Translational Utility of Psychiatric Research in Rodents [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.618593/full]
- 52. Home Cage AI-Monitoring [https://www.genengnews.com/topics/artificial-intelligence/home-cage-ai-monitoring/]
- 53. Comparison of automated home-cage monitoring systems: Emphasis on feeding behaviour, activity and spatial learning following pharmacological interventions - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0165027014002258]
- 54. AI-powered home system for real-time tracking and analysis of... cage [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600061/]
- 55. Analysis Methods Using Animal : A Survey Behavior Deep Learning [https://arxiv.org/html/2405.14002v1]
- 56. Kinder Scientific – Industry Leading Animal Behavior, Drug Development and Drug Discovery Assays [https://kinderscientific.com/]
- 57. The MacqD deep - learning -based model for automatic detection of... [https://www.nature.com/articles/s41598-025-95180-x?error=cookies_not_supported&code=0e05dad3-f73e-494c-a4a1-99dbc1e65a63]
- 58. Classification of Canine Deep Using a Single... Learning Behavior [https://pubmed.ncbi.nlm.nih.gov/34070579/]
- 59. Replication crisis - Wikipedia [https://en.wikipedia.org/wiki/Replication_crisis]
- 60. Confronting the Preclinical Reproducibility with Digitalization... Crisis [https://www.linkedin.com/pulse/confronting-preclinical-reproducibility-crisis-damien-huzard-phd-uqszf]
- 61. 4 Reproducibility and Predictivity | Advancing Disease in... Modeling [https://nap.nationalacademies.org/read/25002/chapter/5]
- 62. Huge reproducibility project fails to validate dozens of biomedical studies [https://www.nature.com/articles/d41586-025-01266-x]
- 63. in science or unrealistic expectations? - PMC Reproducibility crisis [https://pmc.ncbi.nlm.nih.gov/articles/PMC5989743/]
- 64. The Reproducibility Crisis: How Open Science Can Save Research - Open and Universal Science (OPUS) Project [https://opusproject.eu/openscience-news/he-reproducibility-crisis-how-open-science-can-save-research/]
- 65. Frontiers | Measuring Behavior in the Home Cage: Study Design... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2021.735387/full]
- 66. Perspectives on Standardization - Improving the... - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK158942/]
- 67. 4 Perspectives on Standardization | Improving the Utility and... [https://nap.nationalacademies.org/read/13530/chapter/5]
- 68. Methods for Assessing Neurodevelopmental Disorders ... | Preprints.org [https://www.preprints.org/manuscript/202502.0040/v1]
- 69. Ecological validity of social defeat stressors in mouse ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763423000015]
- 70. Ecological validity [https://en.wikipedia.org/wiki/Ecological_validity]
- 71. The 'Real-World Approach' and Its Problems: A Critique of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7204431/]
- 72. Editorial: Animal models of neuropsychiatric disorders: validity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10213662/]
- 73. Field vs. Lab: Choosing the Right Environment for Your ... [https://research-rebels.com/blogs/rebelsblog/field-vs-lab-choosing-the-right-environment-for-your-research]
- 74. Conducting Psychology Research in the Real World [https://nobaproject.com/modules/conducting-psychology-research-in-the-real-world]
- 75. Ecological validity of common behavioral decision making ... [https://pubmed.ncbi.nlm.nih.gov/38591953/]
- 76. Solving Preclinical Reproducibility with Digital Home ... Cage Monitoring [https://www.linkedin.com/pulse/solving-preclinical-reproducibility-digital-home-cage-stefano-j1utf]
- 77. Low-cost solution for rodent home-cage behaviour monitoring | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0220751]
- 78. Animal Models of Stress - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/animal-models-of-stress]
- 79. Comparison of automated home-cage monitoring systems: emphasis on feeding behaviour, activity and spatial learning following pharmacological interventions - PubMed [https://pubmed.ncbi.nlm.nih.gov/24949557/]
- 80. Model and Assay Validation and Acceptance - Using 21st Century Science to Improve Risk-Related Evaluations - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK424977/]
- 81. Optimized animal model to mimic the reality of stress-induced depression in the clinic | BMC Psychiatry | Full Text [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1335-x]
- 82. Levelling the Translational Gap for Animal to Human Efficacy Data [https://www.mdpi.com/2076-2615/10/7/1199]
- 83. A standardised framework to identify optimal animal models for efficacy assessment in drug development - PubMed [https://pubmed.ncbi.nlm.nih.gov/31194784/]
- 84. A standardised framework to identify optimal animal models for efficacy assessment in drug development | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0218014]
- 85. Methodological Considerations for Optimizing and Validating ... [https://pubmed.ncbi.nlm.nih.gov/27906464/]
- 86. Behavioral assays to model cognitive and affective dimensions of depression and anxiety in rats - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2603578/]
- 87. - Wikipedia Learned helplessness [https://en.wikipedia.org/wiki/Learned_helplessness]
- 88. : Seligman's Theory of Learned Helplessness Depression [https://www.simplypsychology.org/learned-helplessness.html]
- 89. Learned Helplessness at Fifty: Insights from Neuroscience - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4920136/]
- 90. Learned Helplessness - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/learned-helplessness]
- 91. Frontiers | Learned and helplessness controllability: from... learned [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1600165/full]
- 92. Animal Models and Ethological Strategies for Early Drug-Testing in Humans - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0149763498000360]
- 93. Behavioral tests assessing neuropsychiatric phenotypes in adolescent mice reveal strain- and sex-specific effects | Scientific Reports [https://www.nature.com/articles/s41598-020-67758-0]
- 94. The effect of recording interval length on behavioral assessment using... [https://www.elsevier.es/es-revista-revista-iberoamericana-psicologia-salud-152-articulo-the-effect-recording-interval-length-S217120691500006X]