Beyond Amyloid: The Revolution Reshaping Alzheimer's Disease Research
Exploring the scientific renaissance redefining our understanding and treatment of Alzheimer's disease
The Silent Tsunami
Imagine a disease slowly erasing your most cherished memories, unraveling your personality, and ultimately stealing your independence. Alzheimer's disease (AD), affecting over 55 million people globally, represents one of humanity's most profound health challenges. By 2050, this number could triple, overwhelming healthcare systems and families alike . Yet, 2025 marks a pivotal moment: a surge of breakthroughs—from radical new theories to AI-powered diagnostics and promising therapies—is transforming our fight against this relentless foe. This article explores the scientific renaissance redefining Alzheimer's, offering unprecedented hope.
1. Paradigm Shifts: Rewriting the Alzheimer's Story
For decades, research was dominated by the "amyloid cascade hypothesis," which blamed sticky amyloid-beta (Aβ) plaques as the singular villain. While anti-amyloid drugs like lecanemab show promise, their modest benefits underscore AD's complexity. Two revolutionary frameworks now challenge old dogmas:
Chronic Neuronal Stress Theory
Aβ isn't the root cause but a response to prolonged neuronal stress. Factors like hypoxia, inflammation, or metabolic imbalances push brain cells into survival mode. Initially protective, sustained Aβ production becomes toxic, triggering tangles and inflammation. Critically, this stress stems from body-wide disorders (e.g., cardiovascular disease, sleep apnea), explaining why AD is uniquely human and tied to modern lifestyles 2 5 .
Unified Theory of Alzheimer's (UTAD)
This model positions Adult Hippocampal Neurogenesis (AHN)—the birth of new neurons—as central to brain resilience. Lifestyle risks (poor diet, inactivity, stress) impair AHN, weakening memory and stress regulation. This dysregulates the HPA axis, flooding the brain with cortisol. The cascade begins: Aβ accumulates, inflammation ignites, and insulin resistance sets in. Unlike aging-based theories, UTAD argues AD stems from preventable AHN sabotage 5 .
These theories reframe AD as a convergence of multiple pathologies—not a single amyloid "curse." This holistic view fuels today's most promising research.
2. In-Depth Look: The Key Experiment Cracking Early Detection
The Challenge: Distinguishing stable mild cognitive impairment (sMCI) from progressive amnestic MCI (aMCI)—a critical step for early intervention—is notoriously difficult.
Methodology: The SLLE-SVM Pipeline
A landmark 2025 study harnessed machine learning to classify MCI subtypes using structural MRI (sMRI) 3 6 :
Participants
412 adults (93 sMCI, 96 aMCI, 86 AD, 137 healthy controls).
Brain Imaging
High-resolution sMRIs processed via FreeSurfer to extract cortical thickness (CTH) and regional volume (VOI) data.
Feature Extraction
UMPCA (Uncorrelated Multilinear Principal Component Analysis): Analyzed 3D brain scans as "tensors," preserving spatial structure (unlike older vector-based methods).
Laplacian Score (LS) Filtering: Selected features with highest discriminative power (e.g., hippocampal atrophy patterns).
Classification
Support Vector Machines (SVM) trained to separate sMCI from aMCI.
| Step | Tool/Technique | Function |
|---|---|---|
| Preprocessing | FreeSurfer | Segments brain into gray/white matter, extracts CTH/VOI |
| Feature Extraction | UMPCA | Reduces 3D data dimensionality, retains spatial info |
| Feature Selection | Laplacian Score | Identifies most discriminative features |
| Classification | SVM | Classifies MCI subtypes (e.g., aMCI vs. sMCI) |
Results and Analysis
- Accuracy: The SLLE-SVM model achieved 65.16% accuracy in distinguishing aMCI from sMCI—a 7.91% improvement over standard SVM 3 .
- Biomarker Insights: Volume loss in the entorhinal cortex and hippocampus were top predictors, validating their role as early AD indicators.
| Method | Accuracy (%) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| SLLE-SVM (VOI) | 65.16 | 63.33 | 67.62 |
| LLE-SVM (VOI) | 64.08 | 66.14 | 62.77 |
| Standard SVM | 57.25 | 56.28 | 58.08 |
Impact: This approach offers a low-cost, non-invasive tool for identifying high-risk MCI patients years before dementia. It exemplifies the shift toward computational neurology—using AI to decode subtle brain changes invisible to the human eye.
| Reagent/Technology | Function | Application Example |
|---|---|---|
| Structural MRI (sMRI) | High-resolution 3D brain imaging | Detects cortical thinning, hippocampal atrophy |
| FreeSurfer | Automated brain segmentation & feature extraction | Quantifies gray matter volume, thickness |
| UMPCA | Tensor-based dimensionality reduction | Preserves spatial data in sMRI analysis |
| Plasma p-tau217 | Blood-based biomarker | Non-invasive AD diagnosis (90%+ accuracy) |
| SVM Classifiers | Machine learning algorithm | Classifies MCI/AD subtypes from imaging data |
3. Early Detection: Catching Alzheimer's Before It Strikes
The race to detect AD 10–20 years before symptoms is accelerating:
Digital Biomarkers
Penn State's NIH-funded study uses smartphone apps to track subtle cognitive shifts in 40–65-year-olds via memory games and symbol tests. Paired with blood tests for GFAP and neurofilament light, it aims to predict risk decades in advance .
Blood Biomarker Revolution
2025 AAIC guidelines endorsed blood tests (e.g., p-tau217) as triage tools for specialists. They require ≥90% sensitivity and 75% specificity, enabling wider screening without costly PET scans 4 .
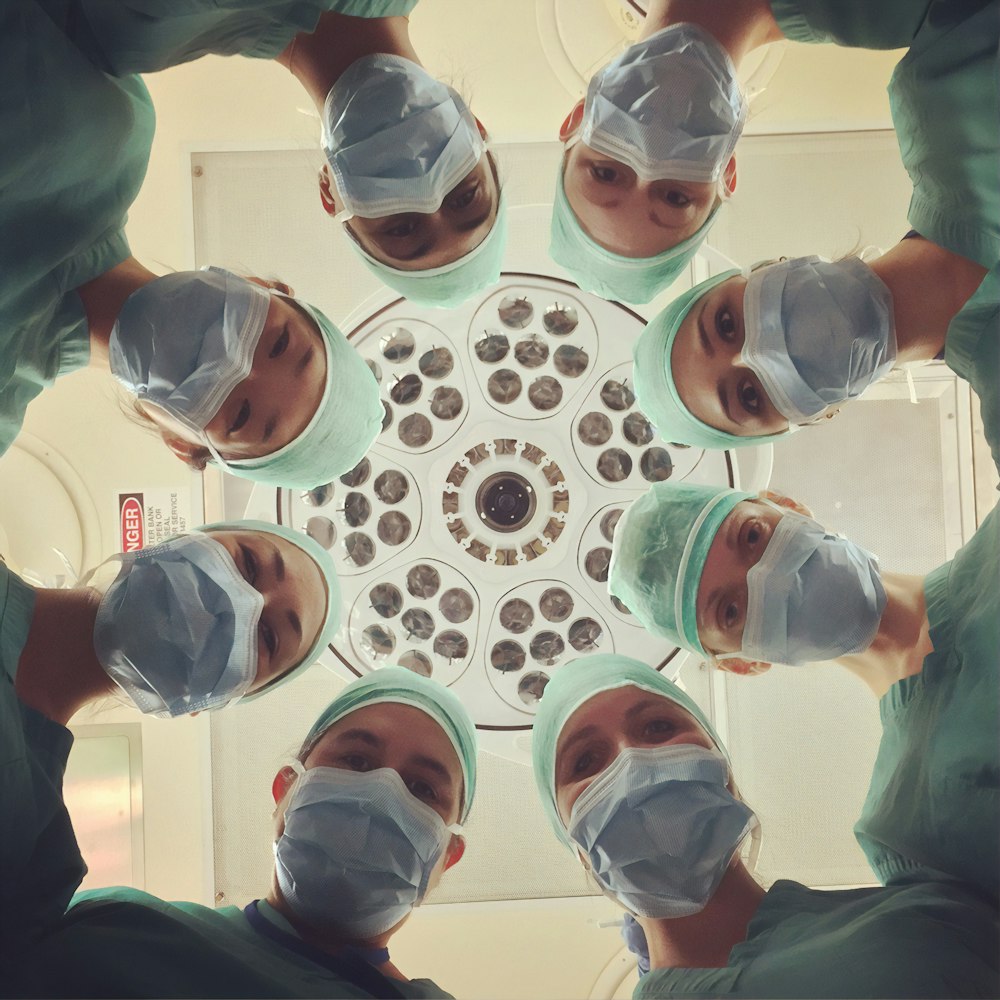
Advanced diagnostics combining imaging and digital tools are revolutionizing early Alzheimer's detection
4. Lifestyle as Medicine: The Power of Prevention
The U.S. POINTER trial confirmed that structured lifestyle changes significantly slow cognitive decline:
POINTER Trial Highlights
- Dual Interventions: 1,200 at-risk seniors received either self-guided (brochures) or structured (coaching, group activities) programs focusing on diet, exercise, and cognitive engagement.
- Results: The structured group showed cognition comparable to adults 1–2 years younger. Benefits were strongest in APOE4 carriers, proving genetics isn't destiny 4 .
- Beyond POINTER: SNAP (food assistance program) participants had 2–3 extra years of cognitive health over a decade, highlighting nutrition's role in brain resilience 4 .
Diet
Mediterranean or MIND diets reduce AD risk by 53%
Exercise
150 mins/week reduces amyloid buildup
Cognitive Engagement
Lifelong learning builds cognitive reserve
5. Therapeutic Frontiers: From Monoclonal Antibodies to Combo Therapies
The 2025 Drug Pipeline is the largest in history, with 138 drugs across 182 trials 1 :
Disease-Targeted Therapies (DTTs)
73% target Aβ, tau, or inflammation (e.g., lecanemab). Real-world data confirm their safety and patient satisfaction 4 .
Repurposed Drugs
33% are existing agents (e.g., diabetes/blood pressure drugs). Combining BP, cholesterol, and diabetes meds slowed decline equivalent to 3 fewer years of brain aging 4 .
Innovative Targets
Growth factors, circadian regulators, and gut-brain axis modulators reflect the field's diversification.
| Drug Type | % of Pipeline | Key Examples |
|---|---|---|
| Biological DTTs | 30% | Anti-Aβ mAbs, tau vaccines |
| Small Molecule DTTs | 43% | BACE inhibitors, inflammation modulators |
| Cognitive Enhancers | 14% | Glutamate regulators |
| Neuropsychiatric Symptom Drugs | 11% | Agitation/psychosis relievers |

The Alzheimer's drug development pipeline has never been more diverse
6. The Future: Precision Medicine and Global Equity
The NIH's $3.98B 2026 budget request targets:
Precision Prevention
Matching interventions to genetic profiles (e.g., APOE4 carriers benefit most from exercise) .
Health Equity
Projects like TIME-AD tackle disparities, studying why Black/Latino populations face higher AD risk but lower diagnosis rates .
Multimodal Integration
Combining blood tests, digital monitoring, and genomics for personalized risk scores.
Conclusion: A Future Reimagined
Alzheimer's research has transcended the simplistic "amyloid era." Today's science reveals a disease woven from threads of metabolism, inflammation, genetics, and lifestyle—a tapestry demanding equally nuanced solutions. From blood tests that detect whispers of pathology to lifestyle programs that fortify the brain, 2025's breakthroughs are not just lab curiosities but beacons of hope. As UTAD architect Dr. Bredesen aptly notes: "Alzheimer's is preventable, and for many, reversible—once we address all the holes in the roof." The path forward is clear: embrace complexity, act early, and leave no patient behind.
For Further Reading
Explore the Alzheimer's Association's ALZPro™ toolkit (alz.org) or the U.S. POINTER study updates.