A Comprehensive Guide to Preventing, Detecting, and Troubleshooting Cell Culture Contamination in Neuronal Studies
This article provides a systematic framework for researchers and drug development professionals to manage cell culture contamination in neuronal studies.
A Comprehensive Guide to Preventing, Detecting, and Troubleshooting Cell Culture Contamination in Neuronal Studies
Abstract
This article provides a systematic framework for researchers and drug development professionals to manage cell culture contamination in neuronal studies. It covers the foundational knowledge of common contaminants and their specific impacts on neuronal cells, explores advanced detection methodologies, offers step-by-step troubleshooting and decontamination protocols, and establishes best practices for validation and quality control. By addressing the unique vulnerabilities of primary neurons, stem cell-derived cultures, and immortalized lines, this guide aims to safeguard experimental integrity, ensure reproducible results in neuroscience research, and protect valuable neuronal models.
Understanding Contamination: Threats to Neuronal Culture Integrity and Data Validity
Contamination in neuronal cell culture is not merely an inconvenience; it is a catastrophic failure that compromises data integrity, misdirects research resources, and ultimately undermines the validity of scientific discoveries. The unique vulnerability of primary neurons, their limited lifespan, and the profound consequences of subtle physiological changes caused by contaminants like mycoplasma make prevention and detection a critical mandate for every neuroscience laboratory. This technical support center provides targeted troubleshooting guides and FAQs to help researchers safeguard their invaluable neuronal studies.
Frequently Asked Questions (FAQs)
What makes neuronal cell cultures particularly vulnerable to contamination? Primary neuronal cultures are exceptionally sensitive because they are non-proliferating, finite cell lines derived directly from nervous tissue. They cannot be passaged indefinitely and are highly susceptible to subtle changes in their environment. Contaminants like mycoplasma can alter cellular metabolism and cause chromosomal aberrations, effects that are particularly devastating in experiments measuring precise neuronal signaling, synaptic function, or inflammatory responses [1].
Beyond cloudiness, what are the subtle signs of contamination I might miss? While bacteria and fungi often cause turbidity, mycoplasma contamination is stealthier. Key indicators include a persistent, unexplained drop in pH (medium turns yellow), subtle changes in cell morphology, poor cell health despite fresh medium, and a failure of cells to thrive. These signs can be easily mistaken for other experimental problems, which is why routine, specific testing is essential [1] [2].
My lab uses antibiotics routinely. Is this sufficient for preventing contamination? No. Reliance on antibiotics is a dangerous practice. Chronic antibiotic use can promote the development of resistant bacterial strains, mask low-level contamination, and has been shown to alter gene expression in cultured cells, which could confound your research results. Antibiotics should not be used as a substitute for rigorous aseptic technique [1].
How can I distinguish between contaminated primary neurons and unhealthy cultures due to isolation stress? This is a critical diagnostic challenge. Contamination often affects the entire culture uniformly and persists across subsequent medium changes. Stress from isolation is typically most severe immediately after plating and improves over time with proper care. Definitive distinction requires targeted tests: PCR for mycoplasma, Gram staining for bacteria, or culturing aliquots of medium on nutrient agar. Always culture a sample of your medium alone as a negative control [3] [1].
What is the most critical step in reviving a frozen vial of neuronal cells to minimize contamination risk? The most critical step is the rapid and complete removal of the cryoprotectant (e.g., DMSO) after thawing. DMSO is toxic to cells at room temperature. Thaw the vial quickly, immediately dilute the cell suspension in pre-warmed culture medium, and centrifuge to pellet the cells. Discard the supernatant containing the DMSO and resuspend the pellet in fresh, complete medium before seeding. This process minimizes cellular stress and prevents the carryover of potential contaminants from the freeze medium [2].
Troubleshooting Guides
Guide 1: Identifying Contamination Type and Source
| Observation | Potential Contaminant | Confirmation Test | Common Source |
|---|---|---|---|
| Rapid medium turbidity, pH change (yellow) | Bacteria | Gram stain, culture medium on nutrient agar | Non-sterile reagents, poor aseptic technique [2] |
| Cloudy medium with floating filaments or spots | Fungi/Yeast | Microscopy (visible structures), culture on agar | Laboratory air, contaminated water bath [1] |
| No turbidity, but unexplained cell death, altered metabolism, or poor growth | Mycoplasma | PCR, DNA staining (Hoechst/DAPI), ELISA | Fetal bovine serum, lab personnel, cross-contamination from other cell lines [1] |
| Rounded, detached cells; viral cytopathic effect (varies) | Virus | PCR, plaque assay, electron microscopy | Original tissue isolate, contaminated reagents [1] |
Guide 2: Proactive Prevention Checklist for Neuronal Cultures
- Personal Protective Equipment (PPE): Always wear a lab coat, gloves, and, in some cases, a face mask to protect samples from human aerosol droplets [4].
- Biosafety Cabinet Management: Work within a certified biosafety cabinet with uninterrupted airflow. Wipe down all items with 70% ethanol before introduction. Keep the cabinet uncluttered and avoid rapid movements that disrupt the air barrier [1].
- Aseptic Technique: Use sterile, single-use pipettes. Avoid touching the tip of pipettes or the necks of bottles. Perform all operations quickly and carefully to minimize exposure to the environment [1].
- Reagent and Equipment Quality: Use laboratory-grade water for all solutions. Source media and sera from reputable suppliers that provide sterility and endotoxin testing certification. Decontaminate equipment regularly with appropriate agents (e.g., 70% ethanol, sodium hypochlorite) [1].
- Routine Monitoring and Authentication: Check cultures daily under a microscope. Regularly test cell lines for mycoplasma (e.g., quarterly) and authenticate cell lines to rule out cross-contamination [1].
Experimental Protocols for Contamination Management
Protocol 1: Routine Mycoplasma Detection via DNA Staining
Principle: This method uses a fluorescent DNA-binding dye (e.g., DAPI or Hoechst) to stain DNA. Mycoplasma, which adheres to the surface of host cells, appears as punctate or filamentous fluorescence in the extranuclear regions.
Materials:
- Cell culture to be tested (test cell line)
- Known mycoplasma-negative cells (negative control)
- Phosphate-Buffered Saline (PBS), sterile
- Fixative (e.g., Methanol or Acetic acid:MeOH 1:3)
- DNA stain (e.g., 1 µg/mL Hoechst 33258 in PBS)
- Mounting medium
- Fluorescence microscope
Method:
- Seed Cells: Seed the test and control cells onto sterile coverslips in a multi-well plate and culture until sub-confluent.
- Wash and Fix: Aspirate the medium and gently wash the monolayer with PBS. Add fixative to cover the cells and incubate for 15-30 minutes at room temperature. Aspirate the fixative and allow to air dry completely.
- Stain: Add enough DNA stain solution to cover the cells and incubate for 15-30 minutes in the dark.
- Rinse and Mount: Aspirate the stain and rinse gently with PBS. Mount the coverslip onto a microscope slide with mounting medium.
- Visualize: Examine under a fluorescence microscope with appropriate filters. The nucleus of mammalian cells will be brightly stained. A positive mycoplasma contamination is indicated by the presence of small, bright extranuclear spots or a fibrous pattern on the cell surface or in between cells [1].
Protocol 2: Establishing Sterile Sampling and Handling for Primary Isolation
Principle: This protocol outlines decontamination steps to prevent contamination during the collection and processing of primary brain tissue, which is a high-risk step.
Materials:
- DNA-free dissection tools (or decontaminated)
- Personal protective equipment (PPE): gloves, mask, clean lab coat
- 80% Ethanol
- DNA decontamination solution (e.g., fresh 1-2% sodium hypochlorite)
- Sterile PBS or dissection medium
Method:
- Decontaminate Tools: Clean all dissection tools thoroughly. Ideally, use single-use, DNA-free tools. For re-usable tools, decontaminate with 80% ethanol (to kill organisms) followed by a nucleic acid degrading solution like sodium hypochlorite (to remove residual DNA). Rinse with sterile water and dry before use [4].
- Wear Appropriate PPE: Cover exposed body parts to limit sample contact with skin and aerosols from breathing [4].
- Dissection: Perform the brain dissection and meninges removal as quickly as possible in a sterile environment to minimize exposure [3].
- Tissue Processing: All subsequent steps—mechanical disruption, enzymatic digestion (e.g., with trypsin), and filtration—should be performed using sterile techniques and reagents in a biosafety cabinet [3].
- Include Controls: Process a sample of the dissection medium alone as a negative control to monitor for introduced contaminants during the procedure [4].
The Scientist's Toolkit: Essential Research Reagents
| Item | Function in Neuronal Research |
|---|---|
| DMSO (Dimethyl Sulfoxide) | A common cryoprotective agent used to preserve cells during freezing by preventing ice crystal formation. Must be removed after thawing [2]. |
| Accutase/Accumax | Milder enzymatic cell detachment agents used for passaging sensitive adherent cells. They are less toxic than trypsin and better preserve cell surface proteins for downstream analysis like flow cytometry [5]. |
| CD11b (ITGAM) Microbeads | Antibody-conjugated magnetic beads for the immunocapture of microglial cells from a mixed primary brain cell suspension [3]. |
| ACSA-2 Microbeads | Antibody-conjugated magnetic beads for the subsequent immunocapture of astrocytes from a cell suspension [3]. |
| Percoll Gradient | A density-based centrifugation medium used to isolate specific cell types (e.g., microglia, astrocytes) from a dissociated brain tissue homogenate without expensive antibodies or enzymes [3]. |
| Phenol Red | A pH indicator in cell culture media. A color change from red to yellow indicates acidification, a sign of high metabolic activity from cell overgrowth or microbial contamination [2]. |
| Hoechst 33258 / DAPI | Fluorescent DNA-binding dyes used to stain cellular DNA, crucial for detecting mycoplasma contamination that appears as extranuclear staining [1]. |
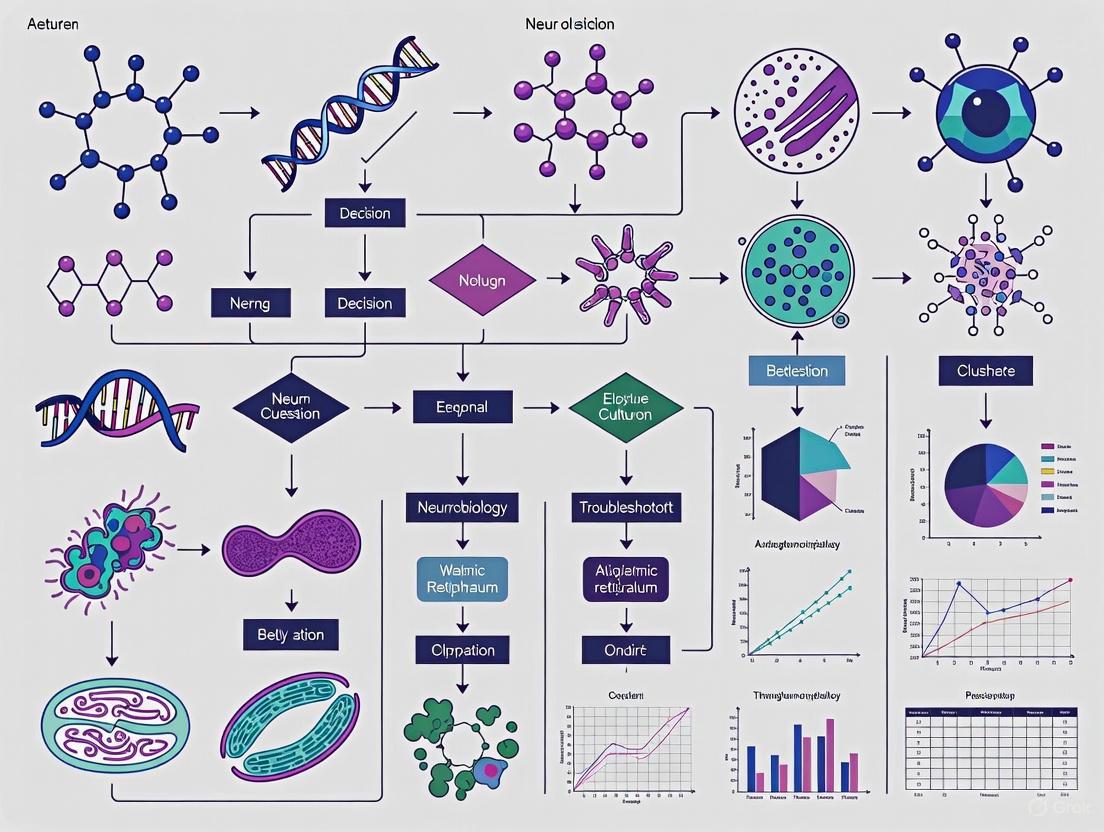
Experimental Workflow and Pathway Diagrams
Contamination Detection Pathway
Primary Neuron Isolation & Contamination Control
FAQ: Biological Contaminants in the Cell Culture Lab
What are the most common types of biological contaminants? Biological contaminants in cell culture are typically classified into broad categories: bacteria, fungi (which includes molds), and yeast [6]. Viruses, mycoplasma, and protozoa are also significant threats but are often harder to detect [5] [6].
How can I tell if my neuronal cell culture is contaminated? Visual inspection under a microscope is the first line of defense. Bacteria often appear as small, shimmering granules between cells and can cause the culture medium to become cloudy [7] [6]. Fungi form thin, filamentous structures called hyphae (mycelium) that can develop into fuzzy, cotton-like masses, sometimes with colored spores [7]. Yeast cells are oval or round and typically bud to form smaller daughter cells, appearing as small, separate colonies [7] [8].
My culture isn't cloudy, but the cells are dying. Could it still be contamination? Yes. Certain contaminants, like mycoplasma, do not cause visible cloudiness but can persist covertly, altering cell metabolism and growth and leading to unreliable experimental results [5] [6]. Mycoplasma is one of the most common and insidious contaminants in cell culture.
What is cross-contamination? Cross-contamination occurs when one cell line is overgrown by another, more robust cell line (e.g., HeLa cells). This is a form of biological contamination that can lead to invalid and irreproducible research data [5] [6]. It is crucial to obtain cell lines from reputable banks and perform periodic authentication [6].
Troubleshooting Guide: Identification and Analysis
Accurate identification is the first step in troubleshooting. The table below summarizes the characteristic signs of common contaminants.
Table 1: Identifying Common Biological Contaminants in Cell Culture
| Contaminant Type | Typical Signs of Presence | Common Examples | Potential Impact on Neuronal Cultures |
|---|---|---|---|
| Bacteria | Cloudy culture medium; fine, shimmering granules under phase-contrast microscopy; rapid pH change (yellow) [7] [6]. | Salmonella, Listeria, E. coli, Pseudomonas [9] [10]. | Nutrient depletion, altered pH, neurotoxic byproducts, rapid culture death. |
| Fungi / Mold | Fuzzy, cotton-like, or thread-like structures that grow over time; may produce pigmented spores (e.g., green, black) [7]. | Penicillium, Aspergillus [7]. | Overgrowth of culture, nutrient competition, possible mycotoxin production. |
| Yeast | Small, round or oval particles that bud off smaller particles; often appear as discrete colonies [7] [8]. | Candida spp., Saccharomyces cerevisiae [11] [8]. | Competition for nutrients, acidification of medium, potential to bud and spread rapidly. |
| Mycoplasma | No visible cloudiness; covert persistence often indicated by poor cell growth, abnormal morphology, or positive test results [5]. | M. pneumoniae, M. orale, M. hyorhinis [5]. | Altered gene expression, metabolism, and membrane integrity; unreliable neuronal signaling data. |
The Scientist's Toolkit: Key Reagents for Contamination Control
Table 2: Essential Reagents for Managing Biological Contaminants
| Reagent / Material | Function | Example Application in Neuronal Culture |
|---|---|---|
| Antibiotics | Inhibit or kill bacterial contaminants. | Used prophylactically in some media (e.g., Penicillin-Streptomycin) but can mask low-level infections [5] [7]. |
| Antimycotics | Inhibit the growth of fungal and yeast contaminants. | Amphotericin B or PPM can be added to media to prevent fungal overgrowth, especially in primary culture setups [7]. |
| PPM (Plant Preservative Mixture) | A broad-spectrum biocide effective against bacteria, fungi, and yeast [7]. | Heat-stable additive for culture media to prevent contamination from explants or during manipulation [7]. |
| Chromogenic Culture Media | Selective media that produce colored colonies for specific pathogens, allowing for rapid identification [10]. | Used diagnostically to identify specific bacterial contaminants (e.g., S. aureus, E. coli) from a contaminated culture [10]. |
| Mycoplasma Detection Kit | Specifically detects mycoplasma contamination via PCR, ELISA, or luciferase-based assays. | Essential for routine monthly screening of precious neuronal stock cultures to ensure data validity [5]. |
| DNA Profiling Kits | Authenticates cell lines via STR (Short Tandem Repeat) profiling. | Critical for confirming the identity of neuronal cell lines and ruling out cross-contamination [5]. |
Experimental Protocol: Systematic Workflow for Contamination Identification
The following diagram provides a logical workflow for diagnosing and responding to suspected contamination in your neuronal cultures.
FAQs: Understanding Contamination in Neural Cell Cultures
1. What are the most common signs that my neural cell culture is contaminated with mycoplasma?
Mycoplasma contamination is often called "silent" because it typically does not cause cloudiness in the culture medium. Common signs under the microscope include unexplained changes in cell growth rate or morphology, reduced transfection efficiency, and the presence of tiny black dots on the cells. For neuronal cultures specifically, you might observe impaired neurite outgrowth or aberrant synaptic activity, which can be mistaken for experimental treatment effects. These contaminants can affect virtually all aspects of cell physiology, including chromatin organization, gene expression, and metabolic pathways, ultimately compromising your experimental data [12] [13] [14].
2. Why are primary neural cultures particularly vulnerable to contamination?
Primary neurons and glial cells isolated from brain tissue are highly sensitive and have limited proliferative capacity. The isolation process itself, which involves multiple steps of dissection, enzymatic digestion, and mechanical trituration, represents a significant contamination risk. Furthermore, these primary cells require specific, nutrient-rich media and specialized substrate coatings, creating an ideal environment for microbial growth if contaminants are introduced. Unlike immortalized cell lines, primary neural cells cannot be easily "recovered" with antibiotics and are often sacrificed once contaminated, leading to significant losses of time and valuable tissue [3] [15].
3. What is the most reliable method to detect mycoplasma in my cultures?
While several methods exist, PCR-based detection is widely considered the most sensitive, specific, and rapid technique. It can identify over 60 species of Mycoplasma, Acholeplasma, Spiroplasma, and Ureaplasma, including the top eight species that account for 95% of cell culture contamination. This method can provide results within hours, allowing for a quick response. Other methods include direct culture (the gold standard but requiring 4-5 weeks) and indirect DNA staining with Hoechst 33258, which reveals characteristic filamentous patterns in the cytoplasm of infected cells [12] [13].
4. Can viral contamination be detected visually, and what are its impacts on neural research?
Viral contamination is notoriously difficult to detect visually, as it often does not cause obvious changes in medium clarity. However, some viruses may induce cytopathic effects (CPE), observable under a microscope as cell rounding, syncytia formation (cell fusion), or lysis. The impact on neural research is profound; viral contaminants can alter host cell immune responses, dysregulate hundreds of host genes, and integrate into the cellular genome. This can lead to misinterpretation of gene expression studies, such as RNA-seq or ATAC-seq data, where viral sequences can align to the host genome and create false positives [13] [16].
5. What are the most critical steps to prevent contamination when working with primary brain cells?
Prevention is the most cost-effective strategy. Key steps include:
- Strict Aseptic Technique: Always work in a certified biosafety cabinet, disinfect all surfaces and items with 70% ethanol, and avoid simultaneous handling of multiple cell lines.
- Reagent Quality Control: Use only certified, mycoplasma-free reagents, sera, and cell lines. Aliquot media and supplements to minimize repeated exposure.
- Quarantine and Testing: Isolate all new cell lines until they are confirmed to be contamination-free through rigorous testing.
- Environmental Control: Maintain clean incubators, change water pans regularly, and avoid creating aerosols that can disperse contaminants [12] [13] [14].
Troubleshooting Guides
Guide 1: Identifying Common Contaminants in Neural Cultures
The table below summarizes the key characteristics of major contamination types to aid in visual identification.
Table 1: Common Contamination Profiles in Cell Culture
| Contaminant Type | Visual Signs in Medium | Microscopic Appearance | Impact on Neural Cells |
|---|---|---|---|
| Mycoplasma | No cloudiness or color change [17] [14] | Tiny black dots; slow cell growth; abnormal cell morphology [17] | Chromosomal aberrations; changes in gene expression; disruption of neurotransmission [12] [13] |
| Bacteria | Turbid/yellowish; possible sour odor [14] | Small, motile particles (1-5 µm); "quicksand" movement [14] | Rapid pH shift; nutrient depletion; cell death [14] |
| Yeast | Clear initially, becomes yellow/turbid over time [17] | Round or oval budding cells [17] | Competes for nutrients; can acidify medium [17] |
| Mold | Cloudy or fuzzy appearance [17] | Thin, thread-like filamentous hyphae [17] | Forms dense, fuzzy colonies that overwhelm the culture [17] |
| Virus | Typically no change [14] [16] | May show cytopathic effects (cell rounding, syncytia) or no change [16] | Alters immune signaling & gene expression; compromises genomic & transcriptomic data [13] [16] |
Guide 2: Mycoplasma Prevention and Detection Workflow
This workflow outlines a standard operating procedure for maintaining mycoplasma-free neural cultures.
Detailed Protocol for PCR-Based Mycoplasma Detection [13]:
Principle: This protocol uses universal PCR primers targeted to the 16S rRNA gene to detect over 60 species of Mycoplasma, Acholeplasma, Spiroplasma, and Ureaplasma.
Reagents:
- PCR primers:
- Mycoplasma-F: GGGAGCAAACAGGATTAGTATCCCT
- Mycoplasma-R: TGCACCATCTGTCACTCTGTTAACCTC
- 2× Taq Plus Master Mix
- TAE buffer (40 mM Tris-Acetate, 1 mM EDTA, pH 8.3)
- Cell culture supernatant
Procedure:
- Sample Preparation: Culture cells for at least 12 hours. Transfer 200 µL of cell culture supernatant into a sterile 1.5 mL tube.
- Heat Inactivation: Incubate the sample at 95°C for 5 minutes to inactivate nucleases. The sample can be stored at -20°C at this point.
- PCR Setup: Prepare a PCR master mix on ice. For each reaction, combine:
- 12.5 µL of 2× Taq Plus Master Mix
- 1 µL of each forward and reverse primer (10 µM)
- 8.5 µL of Nuclease-Free Water
- 2 µL of the prepared template DNA (supernatant)
- PCR Amplification: Run the PCR using the following cycling conditions:
- Initial Denaturation: 95°C for 5 min
- 35 Cycles:
- Denaturation: 95°C for 30 sec
- Annealing: 60°C for 30 sec
- Extension: 72°C for 1 min
- Final Extension: 72°C for 5 min
- Analysis: Analyze the PCR products by running them on a 1.5% agarose-TAE gel containing 1× Gel stain. A positive result will show a band of the expected size (approximately 500 bp).
Guide 3: Decision Matrix for a Contaminated Neural Culture
Discovering contamination requires immediate and decisive action. Follow the logic below to determine the appropriate response.
Eradication Protocol for Mycoplasma (If Attempted) [13] [18]: If a culture is deemed worth saving, commercial mycoplasma removal agents (e.g., P-CMR-001) can be used. Treatment typically lasts 12-21 days. A clear effect is often observed after 3 days, but treatment should continue, and the culture must be retested with a mycoplasma detection kit to confirm complete eradication before returning to general use.
The Scientist's Toolkit: Essential Reagents for Contamination Control
Table 2: Key Research Reagents for Prevention, Detection, and Eradication
| Reagent / Kit | Primary Function | Brief Description & Application |
|---|---|---|
| Mycoplasma Detection PCR Kit [13] [17] | Detection | Contains primers targeting 16S rRNA genes for sensitive and specific identification of mycoplasma species via PCR. |
| Mycoplasma Removal Agent [17] [18] | Eradication | A specialized reagent (e.g., P-CMR-001) added to culture medium to eliminate mycoplasma over a 2-3 week treatment course. |
| Hoechst 33258 Stain [12] | Detection | A fluorescent DNA-binding dye used in indirect staining methods to visualize mycoplasma DNA in the cytoplasm of infected cells. |
| Antibiotic-Antimycotic (P/S) | Prevention | A mixture of Penicillin and Streptomycin used to prevent bacterial and fungal growth in non-critical applications. Note: Ineffective against mycoplasma. [12] |
| Zell Shield [13] | Prevention | A broad-spectrum reagent effective against mycoplasma, bacteria, and fungi, often used as an alternative to standard antibiotics. |
| MycoStrip [13] | Detection | A rapid, dipstick-style test for detecting mycoplasma contamination in cell culture samples. |
This technical support center provides targeted guidance for researchers troubleshooting contamination in neuronal cell culture studies. Endotoxins, or lipopolysaccharides (LPS), are pervasive contaminants derived from the outer membrane of Gram-negative bacteria. In neuronal research, their potent bioactivity can trigger neuroinflammatory and neurotoxic effects, potentially compromising experimental outcomes and leading to misleading conclusions [19] [20]. This resource offers practical, evidence-based protocols to identify, quantify, and mitigate these risks.
FAQ: Endotoxin Contamination in Neuronal Research
What are endotoxins and why are they a particular concern for neuronal studies?
Endotoxins are complex lipopolysaccharides (LPS) found in the outer membrane of Gram-negative bacteria. They are ubiquitous, thermostable contaminants that can persist in the environment and reagents even in the absence of live bacteria [19]. In neuronal studies, they are a critical concern because they can induce potent neuroinflammatory and neurotoxic responses. Endotoxin activates the Toll-like receptor 4 (TLR4) signaling pathway on innate immune cells in the brain, such as microglia, leading to the release of pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) [19] [20]. This inflammation can lead to secondary neurotoxicity, synaptic loss, and impaired neuronal function, which can confound the results of studies investigating primary neurotoxicants or therapeutic agents [20].
How can I determine if my neuronal cell culture is contaminated with endotoxin?
Direct observation of bacterial contamination (e.g., turbid media) may not be present with endotoxin, as the contaminant can be the LPS molecule itself without viable bacteria [21]. Specialized detection assays are required. The gold-standard method is the Limulus Amebocyte Lysate (LAL) assay, which is derived from horseshoe crab blood and comes in gel-clot, turbidimetric, and chromogenic formats [19]. Modern recombinant alternatives (rFC and rCR assays) are now recognized by regulatory bodies like the USP and offer a sustainable, animal-free method with high specificity and reduced batch-to-batch variability [22] [23]. It is crucial to validate that your nanomaterials or culture reagents do not interfere with the chosen assay's readout [19].
My reagents are sterile. How can they still be contaminated with endotoxin?
Sterility and the absence of endotoxin are not the same. Endotoxin is remarkably heat-stable and can survive standard autoclaving and many sterilization routines [19] [20]. It can be introduced through various sources, including:
- Water and raw materials used in culture media and buffers.
- Serum and other biological additives.
- Chemicals used to synthesize nanoparticles or other test compounds.
- Laboratory glassware and utensils that have not been properly depyrogenated (e.g., via dry-heat incineration at >250°C) [19].
What are the best practices for preventing endotoxin contamination in my experiments?
Prevention is the most effective strategy. Key practices include:
- Source Control: Use high-quality, endotoxin-tested reagents, water (WFI - Water for Injection), and serum.
- Aseptic Technique: Work in a laminar flow biosafety cabinet using strict sterile techniques.
- Depyrogenation: Use certified endotoxin-free plasticware. Depyrogenate glassware and tools by baking at 250°C for 30 minutes or 180°C for 3 hours [19].
- Synthesis in Clean Conditions: When producing nanomaterials, synthesize them under endotoxin-free conditions whenever possible, as depyrogenation post-synthesis can alter their physicochemical properties [19].
Troubleshooting Guides
Guide 1: Detecting and Quantifying Endotoxin in Nanomaterials and Reagents
Nanomaterials can often interfere with standard endotoxin detection assays, making accurate quantification challenging [19]. This protocol outlines a robust approach.
Materials:
- LAL reagent (chromogenic kinetic or gel-clot) or recombinant Factor C (rFC) assay kit [22] [23]
- Endotoxin-free water and consumables
- Control Standard Endotoxin (CSE)
- Heat block or water bath
- Microplate reader (for chromogenic/rFC assays)
Methodology:
- Sample Preparation: Prepare your nanomaterial or reagent suspension in endotoxin-free water. Create a series of dilutions to overcome potential interference.
- Interference Testing (Spike Recovery): This is a critical control.
- Split a sample into two aliquots.
- Spike one aliquot with a known amount of CSE (e.g., 0.1 EU/mL).
- Run the LAL or rFC assay on both the spiked and unspiked samples.
- Calculate % recovery = (Measured Endotoxin in Spiked Sample - Measured Endotoxin in Unspiked Sample) / Known Spike Concentration × 100.
- Acceptance Criterion: Recovery should be between 50% and 200% [23]. If outside this range, the sample is interfering, and further dilution or sample treatment is needed.
- Assay Execution: Perform the LAL or rFC assay according to the manufacturer's instructions. Always include a standard curve with CSE.
- Interpretation: Calculate the endotoxin concentration in your sample based on the standard curve and your dilution factor. Report in Endotoxin Units per milliliter (EU/mL) or per milligram (EU/mg) of nanomaterial.
Guide 2: Assessing Endotoxin-Induced Neurotoxicity in Vitro
This protocol uses high-content imaging to evaluate multiple facets of neuronal health, which is highly sensitive to inflammatory and toxic insults.
Materials:
- Human iPSC-derived neurons or primary neuronal cultures [24] [25]
- Cell culture plates (96- or 384-well, suitable for imaging)
- Purified endotoxin (LPS)
- Fixative (e.g., 4% PFA) and permeabilization buffer
- Antibodies: β-III-tubulin (neuronal marker), MAP2 (dendritic marker), Synapsin (synaptic marker)
- Nuclear stain (Hoechst or DAPI)
- Viability dye (e.g., Calcein AM) [24]
- ImageXpress Micro Confocal or similar high-content imaging system
- Analysis software (e.g., MetaXpress with Neurite Outgrowth Application Module) [24]
Methodology:
- Cell Treatment: Plate neurons and allow them to form mature networks (e.g., 14-21 days in vitro, DIV). Challenge the networks with a range of endotoxin concentrations for 24-72 hours.
- Endpoint Staining:
- Live-Cell Assay: Stain with Calcein AM (viability) and Hoechst (nuclei) to monitor real-time toxicity [24].
- Fixed-Cell Assay: Fix and immunostain for β-III-tubulin to visualize the entire neuronal network and a synaptic marker like synapsin.
- High-Content Imaging: Acquire images using a confocal high-content imager. Capture multiple fields and z-stacks per well for robust quantification.
- Image Analysis:
- Use the Neurite Outgrowth Application Module to quantify key parameters:
- Total Neurite Outgrowth: Sum of the area of all neurites.
- Average Neurite Length: Mean length of neurites per neuron.
- Branching Points: Number of branches per neuron.
- Use the Cell Scoring Application Module to:
- Count the total number of neurons.
- Quantify synaptic puncta density.
- Use the Neurite Outgrowth Application Module to quantify key parameters:
- Interpretation: A significant, dose-dependent reduction in neurite outgrowth, synaptic density, or cell viability indicates endotoxin-induced neurotoxicity. Compare the IC50 values for different endpoints to understand the compound's potency [24].
Data Presentation
Table 1: Endotoxin Limits and Detection Methods
| Product Type | Regulatory Limit (EU/mL) | Recommended Test Method | Key Advantages |
|---|---|---|---|
| Injectable Drugs / Medical Devices | 0.2 (for intrathecal) | LAL (Kinetic Chromogenic) [20] | FDA-approved, extensive historical data |
| 5.0 (general) [20] | Recombinant Factor C (rFC) [22] | Animal-free, superior batch consistency, specific for endotoxin | |
| Cell Culture Media / Reagents | Not regulated, but <0.1 is recommended for sensitive cells | rFC or LAL | Prevents immune activation in vitro |
| Engineered Nanomaterials | Not regulated; aim for <1.0 EU/mg for in vivo studies [19] | rFC with interference testing [19] | Reduced interference from nanomaterials |
Table 2: Key Reagents for Endotoxin and Neurotoxicity Research
| Reagent / Kit | Function / Application | Key Feature |
|---|---|---|
| Recombinant Factor C (rFC) Assay | Detects bacterial endotoxin without LAL [22] [23] | Sustainable, animal-free, high specificity |
| LAL Assay Kit | Traditional endotoxin detection [19] | Compendial method, widely accepted |
| iPSC-derived Human Neurons | Biologically relevant model for neurotoxicity screening [24] [25] | Human phenotype, available in large quantities |
| Neurite Outgrowth SW Module | Automated quantification of neurite parameters from images [24] | High-content, multiplexed data (length, branches, etc.) |
| Mitochondrial Dyes (e.g., JC-10, TMRM) | Assess mitochondrial health and membrane potential [24] [25] | Early indicator of cellular stress and toxicity |
Experimental Visualization
Diagram 1: Endotoxin-Induced Neuroinflammatory Signaling
The following diagram illustrates the TLR4-mediated signaling pathway activated by endotoxin, leading to neuroinflammation and potential neurotoxicity.
Diagram 2: Neurotoxicity Screening Workflow
This flowchart outlines a high-content screening workflow for assessing endotoxin-induced neurotoxicity in cultured neurons.
Cell culture contamination represents a significant threat to the integrity of biomedical research, particularly in the sensitive field of neuronal studies. Undetected contaminants can profoundly alter neuronal physiology, metabolism, and gene expression, leading to irreproducible results and erroneous scientific conclusions [26]. This technical support center provides a comprehensive troubleshooting guide for researchers navigating the challenges of contamination in neuronal cell cultures. The content is framed within a broader thesis on troubleshooting cell culture contamination, offering specific methodologies, detection protocols, and mitigation strategies to safeguard the validity of neuronal research and drug development applications.
FAQs: Addressing Critical Concerns in Neuronal Cell Culture
Q1: Our neuronal cultures show no obvious turbidity, but we observe slowed neurite outgrowth and premature cell death. What could be the cause?
This is a classic sign of mycoplasma contamination, which is often cryptic but exerts profound effects on neuronal health [21] [17]. Mycoplasma parasitizes cell culture media, competing for essential nutrients and altering the cellular environment [21]. This nutrient deprivation can impair neuronal metabolism, leading to the observed phenotypic changes. Diagnosis requires specific methods such as fluorescence staining with DNA-binding dyes like Hoechst 33258, PCR-based mycoplasma detection kits, or electron microscopy [21] [27].
Q2: We've detected bacterial contamination in a precious primary neuronal culture. Is it possible to rescue the cells?
The decision to rescue a contaminated culture is a trade-off between the value of the cells and the risk of unreliable data [27]. For primary neuronal cultures, which are often irreplaceable, a rescue attempt may be justified.
- Procedure: Immediately isolate the contaminated culture. Wash the cells gently with PBS containing high concentrations of antibiotics (e.g., penicillin-streptomycin or gentamicin) [21]. Replace with fresh, antibiotic-supplemented medium. Treatment should continue for at least 3-5 days, with daily monitoring. After the contamination appears cleared, culture the cells for several passages without antibiotics to ensure it is truly eliminated [28].
- Critical Consideration: Be aware that antibiotics can themselves induce changes in cell gene expression and physiology [27]. All experimental data generated from rescued cultures should be interpreted with caution, and validation in a clean culture is strongly recommended.
Q3: What are the most likely sources of contamination if we consistently practice aseptic technique but still encounter issues?
Even with good technique, contamination can arise from:
- Laboratory Equipment: Shared incubators and water baths are common hotspots [27]. Incubators should be cleaned monthly with Lysol and 70% ethanol, and water trays should be cleaned often with autoclaved, distilled water [27].
- Raw Materials: Contaminated media, serum, or reagents [27]. While suppliers perform sterility testing, the probability of a contaminant is never zero. For sensitive neuronal cultures, consider filter-sterilizing media prior to use.
- The Researchers Themselves: Humans are the most frequent source of contamination [28]. Avoid talking, coughing, or sneezing near cultures, bind long hair, and do not touch your face during cell handling [28].
Troubleshooting Guide: Identifying and Resolving Contamination
Common Microbial Contaminants and Their Signatures
Table 1: Characteristics of Common Cell Culture Contaminants
| Contaminant Type | Visual Culture Signs | Microscopic Signs (Neuronal Impact) | Recommended Detection Methods |
|---|---|---|---|
| Bacteria | Media turbidity; rapid yellow color shift (pH drop) [21] [17]. | Black sand-like particles in background; "quicksand" movement [21] [17]. Altered cell morphology, apoptosis [21]. | Direct observation, Gram staining, culture methods [21]. |
| Mycoplasma | No visible turbidity; premature medium yellowing; slowed cell growth [21] [17]. | Small black dots; abnormal neuronal morphology; stunted neurite outgrowth [21] [17]. | PCR, fluorescence staining (Hoechst), immunofluorescence [21] [27]. |
| Yeast | Media initially clear, turns yellow over time; possible white spots [21] [17]. | Round or oval budding particles [17]. Slowed cell growth, death [21]. | Direct observation, culture on antifungal plates, PCR [21]. |
| Mold | Fuzzy, filamentous structures on media surface [21] [17]. | Thin, thread-like hyphae [17]. | Direct observation, culture on antifungal plates [21]. |
Impact of Contaminants on Neuronal Function
Contaminants disrupt neuronal homeostasis through multiple interconnected pathways. The following diagram synthesizes how bacterial, mycoplasma, and fungal contaminants alter key neuronal functions, from physiology to gene expression.
Advanced Detection and Monitoring Protocols
Protocol: Mycoplasma Detection via Fluorescence Staining
Mycoplasma contamination is a pervasive problem that can drastically alter neuronal gene expression and function without causing media turbidity [21] [17]. This protocol uses a DNA-binding dye to visualize mycoplasma DNA adherent to the cell surface.
- Principle: Hoechst 33258 dye binds preferentially to DNA, staining both the host cell nucleus and any mycoplasma DNA attached to the cell's exterior [21] [27].
- Materials: Hoechst 33258 stain, positive control (known infected cells), negative control (mycoplasma-free cells), fixative (e.g., 3:1 methanol:acetic acid), fluorescence microscope [21].
- Procedure:
- Culture cells on a sterile glass coverslip until ~50% confluent.
- Rinse cells gently with PBS to remove serum, which can quench fluorescence.
- Fix cells with fixative for 10-15 minutes at room temperature.
- Rinse again with PBS to remove residual fixative.
- Stain with Hoechst 33258 (e.g., 0.5-1.0 µg/mL in PBS) for 15-30 minutes in the dark.
- Rinse with PBS to remove unbound dye.
- Mount the coverslip on a slide and visualize under a fluorescence microscope with a DAPI filter set.
- Interpretation: Mycoplasma-free cells will show only the bright, condensed nuclear DNA. Mycoplasma-contaminated cells will display a characteristic "halo" or speckled pattern of fluorescence in the cytoplasm, representing mycoplasma particles attached to the cell membrane [21].
Protocol: Routine Sterility Testing for Raw Materials
Ensuring the sterility of all culture components is critical for maintaining healthy neuronal cultures.
- Principle: A small sample of the material (e.g., media, serum, supplements) is inoculated into a nutrient broth and monitored for microbial growth [27].
- Materials: Trypticase soy broth or other general nutrient broth, sterile culture tubes, 37°C incubator.
- Procedure:
- Aseptically add 1-2 mL of the test material into 10 mL of sterile broth.
- Incubate the tube at 37°C for at least 14 days [27].
- Observe daily for signs of turbidity, which indicates microbial growth and contamination of the test material.
- Note: While this method is reliable, the 14-day incubation period can be a bottleneck. Newer methods, such as machine learning-aided UV absorbance spectroscopy, can provide results in under 30 minutes and are being developed for rapid sterility testing in cell therapy products [29].
The Scientist's Toolkit: Key Reagents for Contamination Management
Table 2: Essential Reagents for Contamination Prevention and Detection
| Reagent / Kit | Primary Function | Application Note |
|---|---|---|
| Penicillin-Streptomycin | Antibiotic mixture to prevent and treat bacterial contamination [21]. | Use as a short-term rescue agent; continuous use can mask contamination and affect gene expression [27] [28]. |
| Amphotericin B | Antifungal agent to treat yeast and mold contamination [21]. | Can be cytotoxic; use with caution for rescue operations only [17]. |
| Hoechst 33258 Stain | Fluorescent DNA dye for mycoplasma detection [21] [27]. | Requires fluorescence microscopy. A positive control is essential for result interpretation. |
| PCR-based Mycoplasma Detection Kit | Molecular method to detect mycoplasma-specific DNA sequences [21] [28]. | Highly sensitive and specific. Ideal for routine screening of master cell banks and valuable cultures. |
| Copper Sulfate | Additive for incubator water pans to inhibit fungal growth [17]. | A preventive measure to reduce contamination risk from the humidified incubator environment. |
| Mycoplasma Removal Agent | Reagent designed to eliminate mycoplasma from contaminated cultures [17]. | A specialized treatment for rescuing high-value cells; follow-up testing is mandatory. |
Best Practices for Preventing Contamination in Neuronal Cultures
Preventing contamination is always more effective than treating it. The following workflow outlines a comprehensive strategy, from initial cell handling to long-term storage, to minimize the risk of contamination in neuronal studies.
Implementing these structured protocols and vigilance plans is essential for producing reliable and reproducible data in neuronal cell culture research. Consistent adherence to detection and prevention strategies will safeguard your cultures from the profound and often cryptic impacts of contamination.
Proactive Defense and Advanced Detection Methods for Healthy Neuronal Cultures
In neuronal studies research, where cell cultures are invaluable and often irreplaceable, contamination can derail critical experiments, resulting in the loss of months of work. Aseptic technique within the biosafety cabinet (BSC) is not merely a best practice; it is the fundamental barrier protecting your research from microbial invasion. This guide provides targeted troubleshooting and FAQs to help you master this first line of defense, ensuring the integrity of your neuronal cultures.
Understanding Your Primary Tool: The Biosafety Cabinet
A Biosafety Cabinet is a ventilated enclosure that provides a sterile work area by directing HEPA-filtered air to protect the user, the cell culture, and the environment from particulate matter and aerosols [30]. Using the correct type of BSC is critical for successful cell culture.
Types of Biosafety Cabinets and Their Uses
The table below summarizes the common classes of BSCs and their appropriate applications [31]:
| Cabinet Class | Personnel Protection | Product Protection | Environmental Protection | Use Case in Neuronal Research |
|---|---|---|---|---|
| Class I | Yes | No | Yes | Not suitable for sterile cell culture; may be used for enclosing equipment like tissue homogenizers. |
| Class II | Yes | Yes | Yes | The standard for most neuronal cell culture work. Provides an aseptic environment for handling cultures, transfections, and other sensitive procedures. |
| Class III | Yes | Yes | Yes | Used for high-risk pathogens (BSL-4); typically not required for standard neuronal cultures. |
Critical Note: Horizontal laminar flow "clean benches" are not BSCs. They discharge HEPA-filtered air toward the user, protecting the product but exposing the user to any aerosols created, and must never be used for handling cell culture materials or other potentially hazardous agents [31].
The Workflow for Aseptic Technique in a BSC
The following diagram outlines the logical sequence of actions required to establish and maintain an aseptic field before, during, and after work in a Biosafety Cabinet.
The Scientist's Toolkit: Essential Reagent Solutions
Maintaining asepsis relies on more than just technique; it requires the correct use of sterilizing reagents and materials.
| Reagent/Material | Function | Key Consideration |
|---|---|---|
| 70% Ethanol | Primary disinfectant for gloves, work surfaces, and all items entering the BSC [32] [33]. | The water content increases efficacy by aiding in protein denaturation [33]. |
| HEPA Filter | High-Efficiency Particulate Air filter; removes 99.97% of particles ≥0.3 µm, ensuring sterile airflow [34]. | Integrity must be certified regularly. |
| Sterile Pipettes (Plastic/Glass) | For manipulating all liquids; prevent cross-contamination [32]. | Use each sterile pipette only once [32]. |
| Personal Protective Equipment (PPE) | Lab coat and gloves form a barrier between the user and the culture [32] [33]. | Gloves should be sprayed with 70% ethanol frequently during work [33]. |
| Pre-sterilized Reagents & Media | Provides a sterile foundation for cell culture work [33]. | Aliquot to prevent contamination of entire stock [33]. |
Troubleshooting Common Contamination Issues
This section addresses specific problems you might encounter, with guided solutions to correct them.
Problem: Cloudy culture media or unexplained pH shifts in neuronal cultures. Possible Cause & Solution:
- Bacterial Contamination: Check under a microscope for motile bacteria. Discard culture and media. Review your aseptic technique, ensure you are not pouring from media bottles, and confirm all reagents were sterile [32] [33].
- Mycoplasma Contamination: This is a common and often invisible contaminant. Test your cultures regularly using a PCR-based or other mycoplasma detection method [33].
Problem: Fungal growth (visible mycelia) in cultures. Possible Cause & Solution:
- Spores in the environment. Decontaminate incubators and water baths thoroughly and regularly. Ensure water baths have a biocide treatment. Wipe the outside of all media bottles with 70% ethanol before placing them in the BSC [32] [33].
Problem: Consistent contamination across multiple users' cultures. Possible Cause & Solution:
- Compromised BSC or shared reagents. Check the BSC for recent HEPA filter certification and integrity. Ensure shared reagents like trypsin or media are not the source by testing a new, unopened aliquot. Review the BSC placement for drafts from doors, windows, or high-traffic areas [34] [31].
Frequently Asked Questions (FAQs)
Q1: How long should I run the BSC before starting my work? A: You should purge the cabinet by turning it on and allowing it to run for at least 5 minutes before beginning work. This stabilizes the airflow and removes contaminants from the cabinet interior [34].
Q2: Is it necessary to use a Bunsen burner inside a modern Class II BSC? A: No, and it is generally not recommended. Open flames create turbulence that disrupts the protective laminar airflow pattern and can be a fire hazard. The BSC itself maintains a near microbe-free environment [34].
Q3: How often should I disinfect the incubator, and why is it so important? A: Incubators should be cleaned regularly according to the manufacturer's protocol. The warm, humid environment is an ideal breeding ground for microbes. Contamination in an incubator can spread to all cultures inside, leading to widespread loss [33].
Q4: I followed aseptic technique, but my culture is contaminated. What else could be wrong? A: Consider these often-overlooked sources:
- The Cell Line Itself: The original stock could be contaminated. Test a frozen aliquot.
- Aerosols: Moving quickly or splashing liquids can create aerosols that spread contaminants. Always work slowly and deliberately.
- Water Baths: If you warm media in a water bath, ensure the water is treated and changed regularly, and submerge the bottle fully to prevent contamination from being drawn in during cooling [33].
By integrating these protocols, troubleshooting guides, and best practices into your daily routine, you will fortify your first line of defense, ensuring the reliability and reproducibility of your neuronal research.
In cell culture, particularly for sensitive neuronal studies, the primary engineering control (PEC) is your first and most critical line of defense against contamination. These devices create the controlled environments where your cells are actually handled.
Biosafety Cabinets vs. Other Enclosures
It is crucial to distinguish between different types of enclosures, as using the wrong one can inadvertently introduce contaminants.
Table 1: Comparison of Laboratory Enclosures for Contamination Control
| Enclosure Type | Primary Function | Protects the User? | Protects the Cell Culture? | Air Filtration | Suitable for Infectious Agents? |
|---|---|---|---|---|---|
| Biosafety Cabinet (Class II) | Aerosol control for safe cell culture | Yes [35] | Yes [35] | HEPA-filtered supply and exhaust air [35] | Yes [35] |
| Laminar Flow Hood (Clean Bench) | Product protection only | No - air is blown toward the user [35] | Yes | HEPA-filtered supply air [35] | No [35] |
| Chemical Fume Hood | Removal of chemical fumes and vapors | Yes [35] | No | No HEPA filtration [35] | No [35] |
Cleanroom Classifications and Environments
The secondary engineering control (SEC), or the cleanroom in which your BSC is placed, is equally important. Cleanrooms are classified by the cleanliness of the air based on the number and size of particles permitted per volume of air.
Table 2: Cleanroom ISO Classifications and Particle Counts
| ISO Class | Former US FS 209E Name | Max Particles per Cubic Meter (≥ 0.5 µm) | Typical Garments and Applications [36] |
|---|---|---|---|
| ISO 5 | Class 100 | 3,520 [37] | Full sterile coveralls, hood, mask, boot covers, sterile gloves (double). Critical for aseptic compounding. |
| ISO 7 | Class 10,000 | 352,000 [37] | Hood, face mask, coveralls, gloves, boot covers. Used for medical device manufacturing and buffer areas. |
| ISO 8 | Class 100,000 | 3,520,000 [37] | Hair cover, beard cover, lab coat (frock), shoe covers. Used for packaging, assembly, and anterooms. |
Essential Protocols for Contamination Control
Proper Cleanroom Gowning Procedure
Personnel are the largest source of contamination in a cleanroom. A strict and systematic gowning procedure is non-negotiable [36] [38]. The following workflow ensures that you do not introduce particles from your street clothes into the critical environment.
Detailed Steps for ISO Class 5-7 Gowning:
- Preparation: Before entering the gowning area, remove all personal items such as jewelry, watches, and rings. Do not wear any cosmetics or nail polish [37] [36].
- Hand Hygiene: Wash hands thoroughly with soap and water for at least 15 seconds, covering all hand surfaces. Dry hands completely using a HEPA-filtered air dryer or approved wipes; paper towels are typically prohibited [37].
- Initial Donning (Pre-Gowning Side): In the initial section of the gowning room, don a bouffant cap (ensuring all hair is covered) and a face mask [37] [36].
- Transition: Use a step-over bench to move from the "dirty" side to the "clean" side of the gowning process. This bench acts as a physical barrier to prevent floor contaminants from crossing over [36].
- Don Coverall: Pick up the cleanroom coverall. Be careful to let it touch only the clean floor on the "clean" side of the bench. Tuck the bouffant hood inside the coverall [37] [36].
- Don Booties: Put on cleanroom boot covers, ensuring they overlap and cover the ankles of the coverall [37].
- Don Gloves: Finally, put on cleanroom gloves. The gloves must be pulled over the cuffs of the coverall to create a sealed system, preventing skin flakes from escaping [37] [36].
Biosafety Cabinet Filter Replacement Protocol
A BSC with compromised filters offers false security. Filter replacement is a critical maintenance procedure that must be performed by qualified personnel following a strict decontamination protocol [39].
Pre-Replacement Checklist:
- Qualified Personnel: Is a qualified engineer performing the work? [39]
- Decontamination: Has the BSC been thoroughly decontaminated (fumigated) using a method like Vaporised Hydrogen Peroxide (VHP)? [39]
- Disposal Plan: Has a safe method for disposing of the contaminated old filters been decided? [39]
- Power Off: Has the power to the BSC been completely switched off? [39]
Replacement Steps for Class II BSCs:
- Exhaust HEPA Filter Replacement:
- Remove the frame surround at the top of the BSC, taking care not to damage any airflow sensors.
- Unbolt the filter frame and carefully lift out the old HEPA filter.
- Position the new filter and reverse the process to fit it. Ensure all frame bolts are tightened equally to avoid warping the frame and causing leaks [39].
- Downflow HEPA Filter Replacement:
- From inside the work area, remove any UV light fittings and airflow sensors from the back wall.
- Remove the protective stainless steel mesh cover from the roof.
- Unbolt the HEPA filter frame while providing proper support, and lower it into the work area.
- Fit the new filter to the frame and lift it back into place, again tightening all bolts evenly [39].
- Post-Replacement Certification:
- After the new filters are installed, the cabinet must be re-certified before use. This includes:
- Airflow calibration.
- A DOP (or equivalent) test to check filter integrity and seals.
- A containment test (e.g., Ki-Discus test) to ensure the cabinet maintains containment in line with standards like EN12469 [39].
- All work and test results must be documented in the asset register [39].
- After the new filters are installed, the cabinet must be re-certified before use. This includes:
Troubleshooting Common Contamination Control Issues
FAQ 1: Our cell cultures are frequently contaminated with bacteria, even though we work in a BSC. What are we doing wrong?
- Possible Cause 1: Improper Aseptic Technique.
- Solution: Review and retrain all users on core techniques. Ensure no arms or materials pass over open sterile containers. Always work within the "clean" zone of the BSC (typically 6-8 inches from the grill). Avoid quick, turbulent movements that disrupt the laminar airflow.
- Possible Cause 2: Inadequate BSC Decontamination.
- Solution: Implement a strict decontamination routine. The BSC interior must be decontaminated with an appropriate disinfectant (e.g., 70% ethanol, diluted bleach) for a minimum of 10-15 minutes of contact time before and after every use. All surfaces, including the side and back walls, should be wiped down thoroughly.
- Possible Cause 3: Contaminated Reagents.
- Solution: Always sterilize media by filtration (0.2 µm) even if purchased as "sterile." Qualify your reagent sources. Aliquot reagents to avoid repeatedly using from the same stock bottle.
FAQ 2: We are seeing high particle counts in our ISO 7 cleanroom. Where should we focus our investigation?
- Possible Cause 1: Inadequate Gowning.
- Possible Cause 2: Gown Room Cross-Contamination.
- Possible Cause 3: Unsealed Notepaper or Non-Cleanroom Compatible Materials.
- Solution: Only use cleanroom-compatible paper and pens inside the cleanroom. Standard paper and cardboard are significant sources of particle generation and are prohibited.
FAQ 3: When should the HEPA filters in our Biosafety Cabinet be replaced?
- Answer: Filters are replaced based on one of two triggers, whichever comes first:
- Failed Certification: During the annual certification, if the filters fail the integrity (DOP) test or if the airflow cannot be calibrated to the required specifications due to a clogged filter [39].
- Physical Damage: Any visible physical damage to the filter media or its sealing gaskets.
- Important Note: Filter replacement is not a routine, time-based activity. It should only be performed after a failed test or evident damage, and always by a qualified professional following full cabinet decontamination [39].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Aseptic Cell Culture
| Item | Function in Contamination Control |
|---|---|
| 70% Isopropyl Alcohol | Primary disinfectant for wiping down all surfaces inside the BSC and all items introduced into it (flasks, media bottles, etc.). |
| Sterile, Filter-Tip Pipettes | Pre-sterilized and equipped with filters to prevent aerosol contaminants from being drawn into the pipette shaft, protecting both your samples and the instrument. |
| Single-Use, Sterile Centrifuge Tubes | Guarantees a sterile environment for sample preparation and storage, eliminating the risk of cross-contamination from improper washing of reusable tubes. |
| Sterile Cell Culture Media | The nutrient-rich solution for cells. Must be sterile and used with additives (e.g., antibiotics/antimycotics) as required by your protocol. |
| Sterile Phosphate Buffered Saline (PBS) | Used for washing cells without causing osmotic shock. Must be sterile to avoid introducing contaminants during wash steps. |
| Trypsin-EDTA Solution | A sterile enzyme solution used to detach adherent cells from culture vessels for subculturing or analysis. |
Frequently Asked Questions (FAQs)
Q1: What are the most common early signs of contamination I can see with a microscope? While some bacterial and fungal contamination is visible to the naked eye as turbidity or floating clumps, microscopic inspection reveals subtler signs. For phase-contrast microscopy, look for small, shimmering dots (bacteria) or thin, filamentous structures (fungi) moving in the spaces between cells. A sudden, unexplained change in cell morphology, such as granulation, vacuolization, or the retraction of neurites in neuronal cultures, can also indicate microbial presence, particularly mycoplasma [40] [41].
Q2: My culture medium is turning acidic (yellow) very quickly, but I see no contaminants. What could be the cause? A rapid pH drop in the absence of visible contamination can have several causes:
- Incorrect CO₂ levels: Verify that the CO₂ concentration in your incubator matches the bicarbonate concentration in your medium [41].
- Overly tight flask caps: Loosen the caps one-quarter turn to allow for proper gas exchange [41].
- High cell density: An over-confluent culture produces metabolic waste too quickly, acidifying the medium. Passage the cells at a lower density [41].
- Mycoplasma contamination: These organisms can alter cell metabolism and culture pH without being visible. Test your culture for mycoplasma [41].
Q3: Why are my primary neurons dying or failing to attach after thawing? Low viability post-thaw is often related to the freezing and thawing process itself.
- Incorrect thawing: Thaw cells quickly but dilute the freezing medium slowly using pre-warmed growth medium [41].
- Poor-quality freezer stock: Use low-passage cells to create new stocks and follow established freezing protocols precisely [41].
- Improper substrate: Ensure culture vessels are properly coated with a suitable attachment factor like poly-d-lysine to facilitate neuronal adhesion and growth [42] [15].
Q4: What do phase-contrast "halo" artifacts mean, and how do they affect segmentation? In positive phase-contrast microscopy, bright halos often appear along the boundaries between the specimen and the medium. These are optical artifacts and do not represent physical cell structures. The presence of these halos, along with "shade-off" effects, can cause automated image segmentation algorithms to fail by creating inaccurate cell boundaries. Advanced image analysis techniques now model this imaging mechanism to restore artifact-free images for more reliable analysis [40].
Troubleshooting Guide
Use the following table to diagnose and address common cell culture issues.
Table 1: Troubleshooting Common Cell Culture Problems
| Observed Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Rapid pH shift (medium yellow) | Incorrect CO₂ tension, overly tight flask caps, high cell density, bacterial contamination [41] | Check and adjust incubator CO₂, loosen caps, passage cells, test for mycoplasma/bacteria [41]. |
| Poor cell growth/viability | Incorrect or exhausted medium, poor-quality serum, mycoplasma contamination, over-confluency [41] | Use fresh, pre-warmed medium; test new serum lots; test for mycoplasma; passage at lower density [41]. |
| Cells detaching from substrate | Over-trypsinization, mycoplasma contamination, lack of attachment factors [41] | Reduce trypsinization time/amount; test for mycoplasma; ensure proper coating (e.g., poly-d-lysine) [42] [41]. |
| Phase-contrast halo artifacts | Optical effect from difference in refractive index between cells and medium [40] | Recognize as normal artifact; for automated analysis, use software with artifact-correction algorithms [40]. |
| Unexplained changes in cell morphology | Microbial contamination (esp. mycoplasma), incorrect osmotic pressure, toxic components [41] | Perform sterility tests; check osmolality of medium; review all reagent lots and conditions [41]. |
Advanced Monitoring and Detection Protocols
Quantitative Analysis of Automated Detection Systems
Automated systems, particularly those using artificial intelligence (AI), can significantly improve detection rates and accuracy. The following table summarizes performance metrics from a study on automated skin cancer detection, illustrating the potential of such approaches in biomedical image analysis [43].
Table 2: Performance Metrics of AI-Based Segmentation and Classification Algorithms [43]
| Algorithm Category | Specific Algorithm | Key Performance Metric | Result |
|---|---|---|---|
| Segmentation | Adaptive Snake (AS) | Accuracy | 96% |
| Segmentation | Region Growing (RG) | Accuracy | 90% |
| Classification | Artificial Neural Network (ANN) | Accuracy / Sensitivity (Recall) / Specificity | 94% / 92.30% / 95.83% |
| Classification | Support Vector Machine (SVM) | Accuracy / Sensitivity / Specificity | Not fully specified / Lower than ANN |
Protocol: Novel UV Spectroscopy for Early Contamination Detection
This protocol outlines a machine learning-aided method for rapid, non-invasive microbial detection [29].
Principle: Measure the ultraviolet (UV) light absorbance of cell culture fluids. Microbial contamination alters the fluid's absorption pattern. A machine learning model is trained to recognize these patterns, providing a definitive yes/no assessment [29].
Procedure:
- Sample Collection: Aseptically collect a small aliquot of culture supernatant at designated intervals.
- UV Absorbance Measurement: Transfer the sample to a spectrophotometer and measure its UV absorbance spectrum.
- Data Analysis: Input the spectral data into the trained machine learning model.
- Interpretation: The model provides a contamination assessment within 30 minutes.
- Action: If contamination is detected, initiate corrective actions (e.g., use confirmatory RMMs, discard culture). This method serves as a preliminary, continuous safety check to optimize resource use [29].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Primary Neuronal Culture and Monitoring [44] [42] [15]
| Reagent / Material | Function / Application |
|---|---|
| Poly-D-Lysine | Coating agent for culture surfaces to promote neuronal attachment [42] [15]. |
| Neurobasal Medium | A optimized, serum-free basal medium designed for the long-term survival of primary neurons [15]. |
| B-27 Supplement | A serum-free supplement essential for neuronal survival and growth, used in Neurobasal medium [44] [15]. |
| GlutaMAX Supplement | A more stable dipeptide substitute for L-glutamine, which reduces the accumulation of toxic ammonia in cultures [41]. |
| Papain | Proteolytic enzyme used for the gentle dissociation of neural tissues to isolate primary neurons [44]. |
| ROCK Inhibitor (Y-27632) | Improves the survival of dissociated neurons by inhibiting apoptosis [44]. |
| Neurotrophic Factors (e.g., BDNF, GDNF, NGF) | Proteins that support the growth, survival, and differentiation of neurons [44]. |
| HEPES Buffer | Provides additional buffering capacity to maintain physiological pH outside a CO₂ incubator [41]. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for the early detection and troubleshooting of cell culture contamination, integrating both routine and advanced methods.
Early Detection Workflow
In neuronal studies, where subtle changes in metabolism, gene expression, and cell signaling are critically examined, undetected contamination can compromise data integrity and lead to misleading conclusions. While bacterial and fungal contaminants are often readily apparent, mycoplasma and viral contaminants pose a significant challenge due to their cryptic nature [45] [46]. Mycoplasmas, which lack a cell wall, are common contaminants that can alter cell metabolism and cause chromosomal aberrations without causing visible turbidity in the culture medium [46] [47]. Viral contaminants are even more elusive, as they may not cause cytopathic effects yet can still interfere with experimental outcomes and pose a safety risk to laboratory personnel [46]. This guide details the primary methods for detecting these stealthy invaders.
Mycoplasma Detection Methods
PCR-Based Detection
PCR is a powerful molecular technique for amplifying specific DNA sequences, allowing for the sensitive detection of mycoplasma contaminants.
- Principle: This method targets conserved regions of the mycoplasma genome, such as the 16S rRNA gene. In real-time quantitative PCR (qPCR), the accumulation of amplified DNA is monitored each cycle using fluorescent markers, allowing for quantification [45] [48].
- Advantages:
- High Sensitivity: Capable of detecting a very low number of genome copies [45].
- Rapid Results: Provides results in hours, unlike traditional culture methods that can take weeks [45].
- Broad Detection Range: Assays can be designed to detect a wide spectrum of mycoplasma species common in cell culture [45].
- Disadvantages:
Experimental Protocol: SYBR Green qPCR for Mycoplasma Detection
This protocol is adapted from a study developing a sensitive assay for cell culture quality control [48].
- Sample Preparation: Collect supernatant from the cell culture under test. Extract genomic DNA using a commercial DNA extraction kit.
- Primer Design: Design primers to target the 16S-23S Internal Transcribed Spacer (ITS) region or the 16S rRNA gene of Mycoplasma, Acholeplasma, and Ureaplasma species. Validate specificity in silico before use.
- qPCR Reaction Setup:
- Prepare a reaction mix containing SYBR Green I fluorochrome, primers, and the extracted DNA template.
- Positive Control: Use genomic DNA from a known mycoplasma species (e.g., M. arginini, M. hyorhinis).
- Negative Control: Use nuclease-free water instead of template DNA.
- Thermal Cycling:
- Initial Denaturation: 94°C for 4 minutes.
- 35 Cycles of:
- Denaturation: 94°C for 30 seconds.
- Annealing: 54°C for 30 seconds.
- Extension: 72°C for 30 seconds.
- Final Extension: 72°C for 5 minutes.
- Analysis: Analyze the amplification curves and determine the cycle threshold (Ct) values. A positive signal indicates mycoplasma contamination.
DNA Fluorescence Staining
This method uses fluorescent dyes that bind to DNA to reveal mycoplasma contamination under a microscope.
- Principle: The bisbenzimidazole dye Hoechst 33258 or Hoechst 33342 binds preferentially to A-T-rich regions in DNA. When applied to a fixed cell culture, it stains both the host cell's nucleus and any mycoplasma DNA present in the cytoplasm and attached to the cell membrane [46] [47].
- Advantages:
- Relatively quick and simple protocol.
- Does not require specialized molecular biology equipment.
- Disadvantages:
Experimental Protocol: Enhanced Staining with Colocalization
A recent study describes an enhanced method that combines DNA and membrane staining to improve accuracy [49].
- Cell Seeding: Grow the test cells (e.g., neuronal cell lines) on confocal dishes.
- Staining:
- First, stain the cell membrane by incubating the live cells with Wheat Germ Agglutinin (WGA) Oregon Green 488 conjugate (5-10 µg/mL) for 15 minutes at 37°C.
- Then, without fixing, stain the DNA by adding Hoechst 33342 (1 µg/mL) and incubating for another 15 minutes at 37°C in the dark.
- Washing: Gently wash the cells twice with 1X PBS to remove excess dye.
- Imaging: Capture images using a confocal microscope with a 60x oil-immersion objective.
- Analysis: Look for the colocalization of the blue Hoechst signal (mycoplasma DNA) with the green WGA signal (cell membrane). True mycoplasma contamination appears as bright blue spots tightly associated with the green membrane outline. This helps distinguish it from free-floating cytoplasmic DNA debris [49].
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA is an immunoassay that detects specific antigens or antibodies. For mycoplasma, it can be used to detect species-specific antigens in a culture [47].
- Principle: A capture antibody specific to a mycoplasma antigen is coated onto a microplate. If the antigen is present in the test sample, it will bind. A series of enzyme-linked antibodies and substrates are then added, producing a color change that can be measured spectrophotometrically [47].
- Advantages:
- Can be used to screen a large number of samples at once.
- Good specificity and sensitivity [47].
- Disadvantages:
- Requires specific antibodies for different mycoplasma species.
- May not be as universally adopted for cell culture testing as PCR or DNA staining [47].
Experimental Protocol: Direct Antigen Detection ELISA
- Coating: Coat a 96-well plate with an anti-mycoplasma antibody. Incubate overnight, then wash and block the plate to prevent non-specific binding.
- Sample Addition: Add cell culture supernatant or lysate to the wells. Include positive (known mycoplasma antigen) and negative (culture medium only) controls. Incubate to allow antigen binding.
- Detection Antibody: Add an enzyme-conjugated detection antibody that also recognizes the mycoplasma antigen. Incubate and wash.
- Substrate Addition: Add a colorimetric substrate for the enzyme. If the antigen is present, the enzyme will catalyze a reaction, producing a color change.
- Signal Measurement: Stop the reaction and measure the absorbance of each well with a plate reader. A signal above the negative control indicates contamination.
Comparison of Mycoplasma Detection Methods
The table below summarizes the key features of the primary mycoplasma detection methods.
Table 1: Comparison of Mycoplasma Detection Techniques
| Method | Principle | Time to Result | Sensitivity | Key Advantage | Key Disadvantage |
|---|---|---|---|---|---|
| PCR/qPCR | Amplification of mycoplasma DNA | 2.5 - 5 hours [45] | Very High (as low as 50-100 copies/mL) [48] | High sensitivity and speed | Cannot distinguish viable from non-viable cells [45] |
| DNA Staining (Hoechst) | Fluorescent dye binding to DNA | 1 - 2 hours | Moderate | Simple and fast protocol | Prone to false positives from cellular debris [49] |
| Enhanced Colocalization | DNA & cell membrane co-staining | 1 - 2 hours [49] | High | Reduces false positives by localizing signal [49] | Requires confocal microscopy |
| ELISA | Antibody-based antigen detection | 4 - 6 hours (estimate) | Good [47] | High throughput for many samples | Requires species-specific antibodies [47] |
| Microbial Culture | Growth on enriched agar | 28+ days [45] | High (for cultivable species) | Considered a historical "gold standard" | Extremely slow; some species are non-cultivable [45] |
Virus Detection Methods
Viral contamination is a major concern, especially when working with primary neuronal tissues or cell lines derived from primates.
- Principle of PCR for Viruses: Reverse Transcription PCR (RT-PCR) or qRT-PCR is the most common method. It involves first converting the viral RNA genome into complementary DNA (cDNA) using reverse transcriptase, followed by amplification with virus-specific primers [51].
- Challenges: Viral contamination is notoriously difficult to detect without specific testing, as it may not cause visible changes in the culture. It can originate from the original tissue sample, serum, or other biological reagents [46].
Troubleshooting Guides & FAQs
PCR Troubleshooting Guide
Table 2: Common PCR/qPCR Issues and Solutions
| Problem | Potential Cause | Solution |
|---|---|---|
| No Amplification | Failed reaction components, incorrect thermal cycling conditions, or enzyme inhibitors [52]. | Check all component concentrations and prepare a fresh pre-mix. Verify the PCR program settings. Add BSA (0.3%) to neutralize potential inhibitors [52] [53]. |
| False Positive Signal | Contamination from amplicons (carryover) or other positive samples [53]. | Use aerosol-resistant pipette tips and physically separate pre- and post-PCR areas. Use a dedicated set of reagents and equipment. Employ uracil-DNA-glycosylase (UNG) to degrade carryover contaminants [53]. |
| High Background/Non-specific Bands | Non-specific primer binding, insufficiently optimized annealing temperature, or excessive template [53]. | Verify primer specificity and design. Optimize the annealing temperature using a gradient PCR. Titrate the template concentration to the recommended amount [53]. |
| Poor Replicate Reproducibility | Pipetting errors, uneven thermal block temperature, or incomplete sample mixing [52]. | Calibrate pipettes and ensure proper pipetting technique. Use a thermal cycler with a validated block. Thaw and mix all reagents thoroughly before use [52]. |
Frequently Asked Questions (FAQs)
Q1: My neuronal cell culture looks healthy and grows at a normal rate, but my experimental results are inconsistent. Should I test for mycoplasma? Yes. Mycoplasma contamination is often chronic and asymptomatic, not necessarily killing the cells but causing subtle yet significant changes in cell metabolism, gene expression, and function. These alterations can directly lead to inconsistent and unreliable data in sensitive neuronal studies [45] [47].
Q2: I got a positive Hoechst stain with many extranuclear spots, but my PCR test was negative. What does this mean? This discrepancy strongly suggests that the Hoechst stain is yielding a false positive. The fluorescent spots are likely due to cytoplasmic DNA from other sources, such as apoptotic nuclear fragmentation or micronuclei. The enhanced colocalization staining protocol (using Hoechst with WGA) is recommended to confirm if the DNA is truly associated with the cell membrane, which is characteristic of mycoplasma [49].
Q3: How often should I screen my cell cultures for mycoplasma? It is strongly recommended to implement a routine testing schedule. For frequently used and valuable cell lines, such as neuronal models, testing every two weeks to once a month is advisable. All new cell lines arriving in the lab and all cell banks should be tested before they are put into use [47].
Q4: Can I use antibiotics to eliminate mycoplasma from my precious neuronal cell line? While possible, treatment with specific anti-mycoplasma antibiotics (e.g., BM-Cyclin, Plasmocin) is not always successful and can be stressful to the cells. The treatment typically takes 1-3 weeks, and you must rigorously confirm eradication post-treatment. Prevention through strict aseptic technique and regular screening is far more reliable [54] [50].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Mycoplasma and Virus Detection
| Reagent / Kit | Function | Example Products |
|---|---|---|
| Hoechst 33342 / 33258 | DNA-binding fluorescent dye used in direct staining methods to visualize mycoplasma DNA under a fluorescence microscope [49] [47]. | Sigma-Aldrich, Thermo Fisher |
| WGA (Wheat Germ Agglutinin) Oregon Green 488 | A lectin that binds to cell membrane sugars; used in colocalization staining to outline the plasma membrane and distinguish true membrane-associated mycoplasma [49]. | Invitrogen |
| SYBR Green I | A fluorescent dye that intercalates into double-stranded DNA, used for detection in qPCR assays [51] [48]. | Applied Biosystems, Thermo Fisher |
| TaqMan Probes | Sequence-specific fluorescent probes that provide higher specificity in qPCR assays compared to DNA-binding dyes [51]. | Applied Biosystems, Thermo Fisher |
| Mycoplasma Detection Kits (qPCR) | Commercial kits providing optimized primers, probes, and controls for sensitive and rapid detection of a broad range of mycoplasma species [45]. | MycoSEQ (Thermo Fisher), MycoTOOL (Roche) |
| Universal Mycoplasma Detection Kit | A commercial kit designed to detect over 60 species of mycoplasma via endpoint or qPCR [45]. | ATCC |
Experimental Workflow Diagrams
Workflow for Mycoplasma Detection Strategy Selection
Workflow for Enhanced Colocalization Staining
Mycoplasma contamination is a pervasive and serious issue in cell culture, with studies suggesting that between 15% and 35% of continuous cell lines are affected, a figure that can reach up to 80% in some settings [55] [56] [45]. For researchers in neuronal studies, where subtle changes in cell metabolism and gene expression can drastically alter experimental outcomes, undetected mycoplasma presence poses a significant threat to data integrity [55] [56]. These bacteria, among the smallest self-replicating organisms (0.1–0.3 µm), lack a rigid cell wall, making them resistant to common antibiotics like penicillin and streptomycin and allowing them to pass through standard 0.2 µm sterilization filters [55] [56] [57].
The protocol described herein utilizes the polymerase chain reaction (PCR) to detect mycoplasma DNA in culture supernatant. This method targets the highly conserved 16S ribosomal RNA (rRNA) gene of mycoplasma species, a region that provides both the necessary sequence homology for broad detection and sufficient variation for specificity against mammalian and other bacterial DNA [58] [45]. This makes PCR a rapid, sensitive, and specific tool for routine screening, enabling the detection of low-level contaminations that could otherwise compromise critical neuronal research data [58].
Research Reagent Solutions
The following table lists the essential reagents and materials required to perform the mycoplasma detection PCR protocol.
| Item | Function/Description |
|---|---|
| PCR Master Mix | Contains DNA polymerase, dNTPs, Mg2+, and reaction buffers. Hot-start enzymes are recommended to enhance specificity [59]. |
| Mycoplasma-Specific Primers | Oligonucleotides designed to anneal to conserved regions of the mycoplasma 16S rRNA gene. A validated set is crucial for detecting a wide spectrum of species [58] [45]. |
| Nuclease-Free Water | The solvent for preparing reagent aliquots and master mixes, ensuring no enzymatic degradation of primers or templates occurs. |
| Template DNA | The test material, prepared from cell culture supernatant. Positive and negative control DNA are also required for assay validation [45]. |
| Agarose Gel Electrophoresis System | For visualizing the PCR amplicons post-amplification to confirm the presence or absence of the target band. |
Step-by-Step Protocol
Sample Collection and DNA Preparation
- Collect Supernatant: Take a 1 mL sample from the cell culture whose supernatant is to be tested. It is critical that the culture has not been passaged or had its medium changed for at least 2-3 days prior to sampling to allow potential contaminants to proliferate to detectable levels [57].
- Clarify: Centrifuge the supernatant at 500 × g for 5 minutes to pellet any detached cells or large debris. Transfer the clarified supernatant to a new microcentrifuge tube.
- Concentrate Mycoplasmas: Centrifuge the clarified supernatant at high speed (e.g., >12,000 × g for 30 minutes) to pellet the mycoplasma cells [45].
- Extract DNA: Resuspend the pellet in a suitable volume (e.g., 50-100 µL) of nuclease-free water or a commercial DNA extraction buffer. For a simple lysis protocol, heat the suspension to 95°C for 10 minutes, then immediately place on ice. Centrifuge briefly to pellet debris, and use the supernatant as the template DNA. For higher sensitivity and consistency, use a commercial DNA purification kit.
PCR Reaction Setup
The following workflow outlines the entire process, from sample preparation to result interpretation.
- Prepare Master Mix: Thaw all PCR reagents on ice. Prepare a master mix in a sterile, nuclease-free tube. The following table provides a sample reaction setup for a 25 µL total volume. Adjust volumes proportionally for more reactions, including extras to account for pipetting error.
| Component | Sample Volume (µL) | Final Concentration/Amount |
|---|---|---|
| PCR-Grade Water | To 25 µL | - |
| 2X PCR Master Mix | 12.5 | 1X |
| Forward Primer (10 µM) | 1.0 | 0.4 µM |
| Reverse Primer (10 µM) | 1.0 | 0.4 µM |
| Total Master Mix per Rxn | ~14.5 | |
| Template DNA | 10.0 | 1-100 ng |
- Aliquot and Add Template: Dispense the appropriate volume of master mix into each PCR tube or well.
- Add DNA: Add 10 µL of the prepared template DNA to the respective reactions. Include the following essential controls in every run:
- Negative Control: Nuclease-free water instead of template.
- Positive Control: DNA from a known mycoplasma species.
Thermal Cycling and Amplification
- Run PCR Program: Place the tubes in a thermal cycler and run a program similar to the following. Optimal annealing temperatures may need to be determined empirically for specific primer sets [59].
| Step | Temperature | Time | Cycles |
|---|---|---|---|
| Initial Denaturation | 95°C | 5 min | 1 |
| Denaturation | 95°C | 30 sec | |
| Annealing | 55-65°C | 30 sec | 35 |
| Extension | 72°C | 1 min | |
| Final Extension | 72°C | 5-10 min | 1 |
| Hold | 4-10°C | ∞ | 1 |
Analysis of PCR Products
- Gel Electrophoresis: After amplification, analyze 10 µL of each PCR reaction, including all controls, by agarose gel electrophoresis.
- Interpret Results:
- Positive Sample: A distinct band of the expected amplicon size.
- Negative Sample: No band present.
- The test is valid only if the positive control shows a band and the negative control (no-template) is blank. A band in the negative control indicates PCR contamination, and the results from the entire run are invalid [60].
Troubleshooting FAQs
Q1: My no-template control (NTC) shows a band of the expected size, invalidating my run. What is the cause and how can I resolve this?
- Cause: This is a definitive sign of PCR contamination, most likely from amplicons (PCR products) from previous runs or from contaminated reagents [60].
- Solution:
- Spatial Separation: Strictly physically separate pre-PCR (reagent preparation, master mix assembly) and post-PCR (gel electrophoresis, product analysis) areas. Use dedicated equipment, lab coats, and pipettes for each area [60].
- Aseptic Technique: Always use aerosol-resistant filter tips. Change gloves frequently. Aliquot all reagents to avoid repeatedly using stock solutions [60].
- Decontaminate: Clean workspaces and equipment with a 10% bleach solution and/or use UV irradiation in the PCR hood to cross-link contaminating DNA [60].
- Systematic Testing: To identify the contaminated reagent, set up a series of reactions where each component (water, master mix, primers) is substituted with a fresh, new aliquot until the NTC is clean [60].
Q2: I get no amplification band in my test samples or my positive control. What went wrong?
- Potential Causes and Solutions:
- Failed Reagents: Check the activity of your DNA polymerase and other master mix components. Use a fresh aliquot or a different batch [59].
- Insufficient Template or Poor Quality: Ensure an adequate amount of DNA was added. Re-precipitate or re-purify the DNA if inhibitors (e.g., residual salts, phenol) are suspected [59].
- Incorrect Thermal Cycling Conditions: Verify the thermal cycler calibration. Re-optimize the annealing temperature using a gradient cycler, typically testing 3-5°C below the primer's calculated Tm [59].
- Primer Degradation: Resuspend fresh primer aliquots. Verify primer concentration and integrity [59].
Q3: The PCR result is weak or inconsistent. How can I improve the sensitivity and reliability?
- Optimization Strategies:
- Increase Cycle Number: Moderately increasing the number of amplification cycles to 35-40 can enhance sensitivity for low-level contamination [59].
- Optimize Mg2+ Concentration: Mg2+ is a critical cofactor. Perform a titration of Mg2+ concentration (e.g., 1.5 mM to 4.0 mM) to find the optimal level for your specific primer-template combination [59].
- Use a Hot-Start DNA Polymerase: This reduces non-specific amplification and primer-dimer formation at lower temperatures, often resulting in a stronger specific signal [59].
- Switch to qPCR/RT-PCR: For quantitative results and even faster turnaround without the need for gel electrophoresis, consider transitioning to a quantitative PCR (qPCR) method, which also offers greater sensitivity and a lower risk of contamination since the tube remains sealed after setup [58] [45].
Q4: My cell culture is contaminated with mycoplasma. Should I try to eliminate it, or is discarding the culture the best option?
- General Rule: The safest and most recommended practice, especially for neuronal studies where cellular physiology is paramount, is to discard the contaminated culture and start anew from a clean, cryopreserved stock. This prevents the spread of contamination to other cultures and avoids the variable effects of antibiotic treatments on your cells [55] [57].
- Exception for Irreplaceable Cultures: If the cell line is unique and irreplaceable, eradication can be attempted using commercial Mycoplasma Removal Agents (MRAs), such as Plasmocin or BM Cyclin. Treatment typically takes several weeks, and cells must be rigorously quarantined and re-tested post-treatment to confirm eradication [55] [57]. Be aware that such treatments can induce cellular stress and other unintended effects on your model system.
Practical Strategies for Decontamination, Rescue, and Process Optimization
Immediate Action Protocol
Upon discovering suspected contamination in your cell culture, execute the following steps immediately to contain the issue and protect your research.
- Contain and Document: Close the culture vessel lid immediately. Clearly label it with "CONTAMINATED," the date, and your initials. Do not open the dish again inside the incubator or biosafety cabinet (BSC). Note the appearance of the contamination (e.g., cloudiness, unusual particles, pH change) for your records [61].
- Isolate and Remove: Keep the contaminated culture sealed inside the BSC while you work. Remove it from the incubator and any shared equipment immediately to prevent cross-contamination of other cultures [61].
- Decontaminate: Autoclave the entire contaminated culture vessel before disposal. Thoroughly decontaminate all surfaces within the BSC and any other equipment that may have been exposed, using appropriate disinfectants [61].
Contamination Identification Guide
Use the table below to identify the likely contaminant based on visual cues. This will inform your subsequent investigation and corrective actions.
| Contaminant Type | Common Sources | Key Visual/Microscopic Signs | Detection Methods |
|---|---|---|---|
| Bacteria | Poor aseptic technique, contaminated water baths [62] | Media turbidity (cloudiness); rapid color change (yellow) of phenol red medium [62] | Light microscope: small, vibrating dark spots moving independently of media flow [61] |
| Mold | Airborne spores, environment [62] | Fuzzy, filamentous structures (white, black, or green) in media or on vessel surfaces [62] | Visible to the naked eye and confirmed via light microscopy [62] |
| Yeast | Poor aseptic technique [62] | Media turbidity without initial color change; appears as oval particles smaller than cells [62] | Light microscope: budding reproduction visible [62] |
| Mycoplasma | Reagents of animal origin, operator cross-contamination [62] | No visible signs; may cause subtle changes in cell growth, morphology, or function [62] | PCR, DNA staining (e.g., Hoechst), ELISA, or commercial detection kits [62] [61] |
| Chemical (e.g., Endotoxins) | Media supplements, plasticware [62] [63] | No visible signs; can inhibit cell growth and replication, or cause unexpected differentiation [62] [63] | Limulus Amebocyte Lysate (LAL) test; human cell-based pyrogen test (HCPT) [63] |
Investigation and Troubleshooting Workflow
The following diagram outlines a systematic workflow for investigating the source of contamination after initial containment.
Experimental Protocols for Confirmation
Protocol 1: Microscopic Identification of Microbial Contamination
This is the first-line test for visible contaminants.
- Sample: Place your culture vessel under a light microscope.
- Observation: Examine at multiple magnifications (e.g., 10X, 20X, 40X). Look for movement.
- Differentiation: Distinguish cell debris from bacteria by observing motion. Cell debris moves with the media flow, while many bacteria exhibit independent, vibrating, or circular motion due to flagella [61].
- Identification: Look for fungal hyphae (mold) or budding particles (yeast) [62].
Protocol 2: PCR-Based Mycoplasma Detection
This method is recommended for its speed and sensitivity, detecting over 200 strains in under two hours [61].
- Sample Collection: Collect a small aliquot of your cell culture supernatant.
- DNA Extraction: Isolate total DNA from the sample.
- PCR Amplification: Use a commercial Mycoplasma PCR detection kit with primers that target conserved mycoplasma DNA sequences.
- Analysis: Run the PCR products on an agarose gel. Compare the bands to positive and negative controls provided in the kit. A band matching the positive control indicates contamination [61].
Protocol 3: Sterility Testing with Automated UV Spectroscopy
A novel, machine learning-aided method for rapid, non-invasive sterility checking.
- Sample: A small volume of cell culture fluid is placed in a spectrophotometer.
- Measurement: UV absorbance spectroscopy is performed on the sample.
- Analysis: A machine learning model analyzes the light absorption pattern.
- Result: The method provides a definitive "yes/no" contamination assessment within 30 minutes, significantly faster than traditional 14-day culture methods [29].
The Scientist's Toolkit: Key Reagent Solutions
| Reagent / Material | Function in Contamination Control |
|---|---|
| Penicillin/Streptomycin | Antibiotic solution added to media (0.5-1.0%) to prevent bacterial contamination. Test for cell line sensitivity before use [61]. |
| Amphotericin B | Antifungal agent used to prevent and treat yeast and mold contamination [61]. |
| Mycoplasma-Specific Antibiotics | Cocktails containing antibiotics like quinolones or macrolides for treating mycoplasma-contaminated irreplaceable cell lines. Treatment can take weeks [61]. |
| Mycoplasma PCR Detection Kit | Provides fast, reliable screening for mycoplasma DNA in cell culture samples, with results in under two hours [61]. |
| HEPA-Filtered CO2 Incubator | Maintains an ISO Class 5 clean environment by filtering airborne particles, preventing contaminants from entering when the door is opened [64]. |
| Cointerior Incubator | A 100% pure copper chamber naturally inhibits microbial growth, providing a passive and effective contamination control strategy [64]. |
Frequently Asked Questions (FAQs)
Q: I see dark spots in my culture under the microscope. Is it contamination? A: Not necessarily. Cell debris from apoptosis can appear as dark spots. To differentiate, observe the motion: debris moves with the media flow, while bacteria often move independently with a vibrating motion [61].
Q: Can I save a cell line with microbial contamination? A: For common bacteria or fungi, discarding the culture is often safest. For irreplaceable cell lines contaminated with mycoplasma, specialized antibiotic cocktails (e.g., containing quinolones) can be used, but decontamination is a lengthy process that can take weeks and is not always successful [61].
Q: My reagents are sterile-filtered. Why did I get contaminated? A: Filtration may not be effective against all contaminants. Mycoplasma, due to its small size (0.2-0.3 μm), can pass through standard filters. Furthermore, contamination can occur during handling post-filtration [61].
Q: Are "pyrogen-free" plasticwares truly clean? A: Not always. A 2025 study found that some commercially available "pyrogen-free" pipette tips, well plates, and tubes were contaminated with pyrogens (like endotoxins) above detectable limits. This can subtly influence cell behavior without causing visible contamination [63].
To Treat or to Discard? A Decision Matrix for Irreplaceable Neuronal Cultures
Within the context of a broader thesis on troubleshooting cell culture contamination in neuronal studies research, this guide addresses a critical dilemma faced by researchers: whether to attempt a rescue of a precious, irreplaceable neuronal culture or to discard it to safeguard other experiments. Contamination is a pervasive set-back in cell culture laboratories, and the decision carries significant consequences for project timelines, resource allocation, and data integrity [65]. This technical support center provides a structured framework, detailed protocols, and essential reagents to support informed decision-making.
FAQs on Neuronal Culture Contamination
1. What are the most common biological contaminants, and how can I identify them?
The table below summarizes the identification features of common contaminants in neuronal cultures [66] [17] [65]:
Table: Identification of Common Cell Culture Contaminants
| Contaminant Type | Visual Culture Inspection | Microscopic Appearance | Other Indicators |
|---|---|---|---|
| Bacteria | Medium appears cloudy (turbid); color may turn yellowish [17] [65] | Tiny, moving granules between cells; shapes (rods, cocci) may be resolvable at high power [65] | Sudden, sharp drop in medium pH [65] |
| Yeast | Medium may be clear initially, becoming cloudy and often yellow over time [17] | Individual ovoid or spherical particles; may show budding of smaller particles [17] [65] | pH usually stable initially, then increases with heavy contamination [65] |
| Mold | Fuzzy, filamentous patches floating in medium or on culture surface [17] | Thin, thread-like structures (hyphae); sometimes denser spore clusters [17] [65] | pH stable initially, then increases with heavy contamination [65] |
| Mycoplasma | No obvious change in medium clarity or color [17] | No definitive visual signs; cultures may show slow growth and abnormal cell morphology [17] | Requires specialized detection kits (e.g., PCR, DNA staining) for confirmation [66] [17] |
2. Should I use antibiotics and antimycotics routinely in my neuronal cultures?
No. The continuous use of antibiotics and antimycotics is not recommended for routine cell culture [65]. This practice encourages the development of antibiotic-resistant strains and can allow low-level, cryptic contaminants (like mycoplasma) to persist undetected. These cryptic infections can then develop into full-scale contamination once the antibiotics are removed and may interfere with your cellular processes under investigation [65]. These agents should be used as a last resort for short-term applications only.
3. My culture is contaminated. What are the immediate first steps I should take?
- Isolate Immediately: Move the contaminated culture away from your clean cultures and main work area to prevent cross-contamination [65].
- Identify the Contaminant: Use the table above to determine the type of contaminant [65].
- Thoroughly Clean: Disinfect the incubator, water pans, and laminar flow hoods where the contaminated culture was located [17] [65].
4. When is it absolutely necessary to discard a culture?
Discarding a culture is the safest and most recommended course of action in these scenarios:
- The culture is contaminated with multiple types of microorganisms.
- The contamination is heavy and widespread.
- The culture is not irreplaceable (e.g., readily available cell lines).
- The contaminant is a mold or yeast, which produce spores that easily spread [17].
- Attempts to decontaminate have failed.
Decision Matrix: To Treat or to Discard?
Use the following matrix to guide your decision-making process for irreplaceable cultures. This framework integrates contamination type and culture status to recommend an action plan.
Experimental Protocols for Assessment and Rescue
Protocol 1: Assessing Neuronal Culture Health Post-Contamination
The functionality of a neuronal culture is as critical as its purity. After any contamination event, especially before and after a rescue attempt, assessing electrophysiological health is crucial.
- Objective: To evaluate the functional integrity of the neuronal network using Micro-Electrode Arrays (MEAs) following a contamination incident or treatment [67] [68].
- Materials:
- Method:
- Culture primary neurons on 48-well MEA plates pre-coated with PEI and Laminin [67].
- Maintain cultures in an incubator (37°C, 5% CO2), replacing 25% of the media volume every 2-3 days [68].
- Record extracellular signals. Define an "active electrode" as one with more than 6 spikes per minute (0.1 Hz) and an "active well" as having more than 40% active electrodes [67].
- Analyze key parameters pre- and post-contamination/treatment. Critical parameters include:
- Interpretation: A significant drop in these parameters indicates compromised neuronal health, which may warrant discarding the culture even if the contaminant is eradicated [67].
Protocol 2: Decontamination Procedure for Irreplaceable Cultures
This protocol should only be attempted on cultures deemed "irreplaceable" after consulting the decision matrix.
- Objective: To eliminate bacterial or mycoplasma contamination from a neuronal culture with minimal toxicity to the cells [65].
- Materials:
- Method:
- Determine Antibiotic Toxicity: Dissociate the contaminated cells and dilute them to normal passage concentration in antibiotic-free medium. Dispense into a multi-well plate. Add a range of antibiotic concentrations to the wells. Observe daily for toxicity (sloughing, vacuoles, decreased confluency, cell rounding) for several days to determine the toxic concentration [65].
- Decontaminate Culture: Passage the contaminated culture using the antibiotic at a concentration one- to two-fold lower than the determined toxic level. Maintain the culture under these conditions for 2-3 passages [65].
- Verify Eradication: Culture the cells for one passage in antibiotic-free media, then return to the treatment concentration for another 2-3 passages. Finally, culture in antibiotic-free medium for 4-6 passages to confirm the contamination is gone [65].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Contamination Management in Neuronal Cultures
| Reagent Name | Function / Application | Key Considerations |
|---|---|---|
| Penicillin-Streptomycin (P/S) [17] | Antibiotic mixture used to combat bacterial contamination. | Use at high concentrations (e.g., 10X) only as a short-term rescue agent; can be toxic to some cells [17] [65]. |
| Amphotericin B [17] | Antifungal agent used against yeast and mold. | Highly toxic to cells; not recommended for routine use. Discarding is often preferable to treatment with this agent [17]. |
| Mycoplasma Removal Agent [17] | Specific reagents designed to eliminate mycoplasma contamination. | Essential for treating this hard-to-detect contaminant. Follow product protocols precisely. Prevention kits are available for long-term protection [17]. |
| Mycoplasma Detection Kit (e.g., MycAway) [17] | Kits for routine monitoring and confirmation of mycoplasma contamination. | Crucial for detection, as mycoplasma does not cause visible medium turbidity. Recommended for use every 1-2 months [17]. |
| CD11b (ITGAM) Microbeads [3] | Immunomagnetic beads for positive selection of microglial cells from a mixed brain cell culture. | Useful for isolating specific cell types to check for cell-type-specific contamination or to salvage a pure population. |
| Poly-L-Lysine / Laminin [67] [68] | Substrate coating for MEA plates and culture vessels to promote neuronal adhesion and growth. | Proper coating is critical for the health and functionality of primary neuronal cultures, especially after stressful events like contamination [67]. |
| Copper Sulfate [17] | Added to incubator water pans to inhibit fungal growth. | A preventative measure to reduce the risk of mold contamination in the humidified incubator environment [17]. |
The decision to treat or discard a contaminated neuronal culture requires a balanced consideration of the culture's value, the contaminant's nature, and the risks to the laboratory. A systematic approach—beginning with rapid identification and isolation, followed by a rational assessment using the provided decision matrix—is paramount. While the salvage of an irreplaceable culture can be attempted, it is a high-risk endeavor. Adherence to strict aseptic technique and a focus on prevention remain the most effective and reliable strategies for protecting your neuronal cultures and ensuring the integrity of your research data.
This technical support center provides targeted guidance for researchers, particularly in neuronal studies, on the appropriate use of antibiotics and antimycotics in cell culture. While these agents are valuable tools, their misuse can lead to hidden contamination, cellular toxicity, and the development of resistant strains, compromising experimental data. The following guides and protocols are designed to help you prevent and manage contamination effectively, safeguarding the integrity of your research.
Troubleshooting Guides
Guide 1: I suspect my neuronal cell culture is contaminated
Contamination can be a significant setback, but systematic identification is the first step toward resolution.
| Contamination Type | Visual Signs (Macro/Microscopic) | Culture Medium pH | Common Identification Methods |
|---|---|---|---|
| Bacterial | Cloudy/turbid medium; thin film on surface; tiny, moving granules between cells [65] | Sudden drop [65] | Microscopy, microbial culture [65] |
| Yeast | Turbid medium; ovoid or spherical particles that may bud [65] | Stable initially, increases with heavy contamination [65] | Microscopy [65] |
| Mold | Thin, wisp-like filaments (hyphae) or dense clumps [65] | Stable initially, increases with heavy contamination [65] | Microscopy [65] |
| Mycoplasma | Often no overt signs; potential for subtle changes in cell growth/metabolism [65] | No consistent change [65] | PCR, ELISA, specialized staining [65] [5] |
| Cross-Contamination | Changes in cell morphology, growth rate, or gene expression profiles [65] [5] | No consistent change [65] | DNA fingerprinting, karyotype analysis, isotype analysis [65] |
Recommended Actions:
- Immediate Isolation: Immediately isolate the contaminated culture from other cell lines to prevent spread [65].
- Decontaminate Equipment: Thoroughly clean incubators and laminar flow hoods with a laboratory disinfectant and check HEPA filters [65].
- Decide on Decontamination: Consider decontamination only if the culture is irreplaceable. For most cases, especially in neuronal studies where cellular responses are critical, autoclaving and disposing of the culture is the safest option to avoid unreliable data [65].
Guide 2: My cells are not thriving, and I routinely use antibiotics
Persistent use of antibiotics can mask low-level contamination and directly impact cell health.
| Potential Issue | Why It Happens | Corrective Action |
|---|---|---|
| Cryptic Contamination | Antibiotics suppress but do not eliminate all microbes, allowing low-grade infections to persist [65] [69] | Transition to antibiotic-free media to reveal contamination; culture new stocks without antibiotics [65] [69] |
| Cellular Toxicity | Antibiotics/antimycotics can be toxic to certain cell lines, interfering with cellular processes [65] [69] | Perform a dose-response test to determine toxicity; use antibiotics only for short-term applications [65] |
| Masked Mycoplasma | Continuous antibiotic use can hide mycoplasma infections, which are resistant to common antibiotics [65] | Test specifically for mycoplasma using PCR or ELISA and quarantine new cell lines [65] [5] |
Preventive Strategy: The most robust solution is to phase out routine antibiotic use and rely on strict aseptic technique. This includes working in a clean, uncluttered hood, regularly cleaning incubators and water baths, and using proper personal protective equipment [69] [5].
Frequently Asked Questions (FAQs)
Q1: When is it absolutely necessary to use antibiotics and antimycotics in my cell culture? Their use is justified in specific scenarios:
- During the establishment of primary cultures, which may harbor contaminants from the source tissue [69].
- When working with valuable, irreplaceable stocks where contamination would be a major loss [69].
- For short-term experiments where the risk of contamination is high and the duration is too brief for resistance to develop [65].
- In selection protocols, such as in gene targeting, where an antibiotic resistance gene is used as a marker [69].
Q2: What are the specific risks of using antibiotics in neuronal cell culture studies? Beyond general risks, certain antibiotics pose a neurotoxicity risk. Beta-lactam antibiotics (e.g., penicillin) have molecular structures similar to GABA and can impair GABAergic transmission and benzodiazepine receptor function, potentially leading to encephalopathy, behavioral changes, myoclonus, or seizures in vivo [70]. Fluoroquinolones are also associated with neurological adverse effects [70]. These mechanisms can directly interfere with the physiological processes under investigation in neuronal models.
Q3: What are the long-term consequences of continuously using antibiotics in my lab? The long-term consequences are severe and contribute to a global health crisis:
- Antimicrobial Resistance (AMR): Continuous use encourages the development of antibiotic-resistant bacterial strains, which can render first-line therapies ineffective [65] [71]. This "Silent Pandemic" poses a major threat to healthcare worldwide [71].
- Compromised Research Data: Data generated from chronically treated cells may be spurious, as low-level contaminants or the antibiotics themselves can alter cellular behavior and biochemical pathways [65] [69].
Q4: How do I test if an antibiotic is toxic to my neuronal cell line? Follow this empirical protocol to determine a safe, non-toxic concentration [65]:
Q5: What is the single most effective way to prevent cell culture contamination? Nothing replaces consistent and meticulous aseptic technique [65] [69]. This includes:
- Working within a properly maintained laminar flow hood.
- Regularly disinfecting all surfaces and equipment with agents like ethanol or Virkon [69].
- Avoiding simultaneous handling of multiple cell lines.
- Using sterile pipettes and reagents.
- Routinely cleaning incubators and culture areas [69].
The Scientist's Toolkit: Key Reagents for Contamination Control
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Penicillin-Streptomycin [69] | Broad-spectrum antibiotic combination against Gram-positive and Gram-negative bacteria. | Common working concentration: 50-100 IU/mL penicillin, 50-100 µg/mL streptomycin [69]. |
| Amphotericin B [69] | Antimycotic agent targeting fungal contaminants like yeast and mold. | Can be toxic to cells with long-term use; working concentration is typically 2.5 µg/mL [69]. |
| Virkon / Ethanol (70%) [69] | Laboratory disinfectants for surface decontamination of hoods, incubators, and equipment. | Use Virkon for cleaning followed by 70% ethanol; ethanol is a fixative so detergent cleaning should come first [69]. |
| Mycoplasma Detection Kit (PCR) [65] [5] | Essential for detecting cryptic mycoplasma contamination. | Should be used for routine screening, especially when introducing new cell lines into the lab [5]. |
| Cell Dissociation Reagents (e.g., Accutase) [5] | Milder enzymes for passaging adherent cells, preserving surface epitopes for assays like flow cytometry. | Preferable to trypsin for neuronal cells where surface receptor integrity is critical for experimental outcomes [5]. |
FAQs on Systemic Decontamination
Q1: What is the difference between cleaning, decontamination, and sterilization? These terms represent different levels of microbial control [72].
- Cleaning: The physical removal of dirt, debris, and organic material, which reduces the bioburden but does not necessarily kill microorganisms [72].
- Decontamination: The broader removal or neutralization of hazardous substances to make surfaces safe. It significantly lowers the microbial load to minimize experimental interference but does not guarantee the elimination of all organisms [72].
- Sterilization: The complete destruction of all forms of microbial life, including hardy bacterial spores, using rigorous, validated methods like high-heat cycles [72].
Q2: What are the common contamination hotspots in a CO₂ incubator? The warm, humid environment of an incubator is ideal for microbial growth. Key hotspots include [72]:
- Door Gaskets: Often accumulate moisture and nutrients, making them a common hiding spot for mold and bacteria that are frequently missed during cleaning.
- Water Pan/Humidification System: Standing water is a major reservoir for bacteria, mold, and algae biofilm.
- Fan and Sensor Openings: Contaminated components can spread microbes throughout the chamber.
- Interior Walls, Shelves, and Corners: These surfaces can collect condensation and splashes, harboring microorganisms.
Q3: How often should I decontaminate my cell culture incubator? Frequency depends on usage, but general guidelines are [72] [73]:
- Daily/Weekly: Quick wipe-downs of high-contact surfaces (door handles, gaskets, shelves) with 70% ethanol or a suitable disinfectant.
- Monthly: A full internal deep clean, including removing and cleaning shelves, disinfecting the water reservoir, and wiping all interior walls and ceiling.
- Between Experiments: In busy or critical labs, perform bio-decontamination (e.g., hydrogen peroxide fogging) between experiment cycles to prevent rapid recontamination.
- Immediately: Clean and decontaminate any spills or if you suspect contamination in a culture.
Decontamination Methods at a Glance
The table below compares common decontamination methods for laboratory equipment.
Table 1: Comparison of Common Decontamination Methods
| Method | Description & Process | Typical Log Reduction | Key Advantages | Key Disadvantages |
|---|---|---|---|---|
| Dry Heat Sterilization [74] | Uses high temperatures (e.g., 120-180°C) for 2-3 hours. | Log 6 of bacteria and bacterial spores [74] | No toxic residues; avoids moisture-related issues like rust [74]. | High temperatures can damage heat-sensitive components [74]. |
| Moist Heat Decontamination [74] | Uses high humidity at elevated temperatures (e.g., 90-95°C). | Log 6 of bacteria, Log 4 of bacterial spores [74] | Steam penetrates surfaces/crevices; no toxic residues [74]. | Residual moisture requires drying; longer process [74]. |
| Hydrogen Peroxide Vapor (HPV) [72] [74] | Uses vaporized H₂O₂ to clean surfaces. Process includes vapor generation, exposure, and aeration. | Log 6 of bacteria and spores [74] | Vapor penetrates crevices; rapid process (few hours) [74]. | Requires costly specialized equipment; hazardous to health; not suitable for all materials [74]. |
| Ultraviolet (UV) Light [74] | Uses UV light to destroy microbial DNA. Often used for surfaces and water pan disinfection. | Log 3 to Log 4 of bacteria and spores [74] | Can be integrated for continuous operation; low operational cost; low residue [74]. | Least effective method; limited penetration; light is harmful to skin/eyes [74]. |
| Chemical Disinfection [72] [73] | Manual wiping with agents like 70% ethanol, quaternary ammonium compounds, or diluted bleach. | Varies by chemical and contact time. | Readily available and easy to use for routine surface cleaning [72] [73]. | Prone to human error; hard-to-reach areas can be missed; does not achieve sterility [72]. |
Experimental Protocol: Monthly Deep Decontamination of a CO₂ Incubator
This protocol provides a detailed methodology for a comprehensive monthly clean, combining manual cleaning and a no-touch decontamination cycle [72] [73].
1. Preparation and Dismantling * Move all cell cultures to a sealed, sterile temporary container [73]. * Turn off the incubator and disconnect it from the power and gas supplies. * Remove all internal components: shelves, shelf supports, trays, and the water pan [73]. * Inspect door gaskets and seals for visible debris or damage.
2. Manual Cleaning of Components and Chamber * Clean removable components with a lint-free cloth, soapy water, and a non-corrosive disinfectant. Rinse thoroughly with distilled water if using alcohol-based disinfectants [73]. * Wipe the entire interior chamber (walls, ceiling, floor, door) with a suitable disinfectant, paying special attention to corners and the door gasket [72]. * Clean the external components of the incubator [73].
3. Water Pan and Humidification System Care * Empty and clean the water pan. If biofilm is present, clean it immediately [72]. * Use a 2% solution of an ammonium disinfectant in the water reservoir or refill it with sterile distilled water [73]. Avoid chlorine bleach, as it can cause corrosion [73].
4. No-Touch Decontamination Cycle * After manual cleaning, run a built-in decontamination cycle if your incubator has one (e.g., moist heat at 90°C) [74] or use a hydrogen peroxide fogger (e.g., MycoFog) [72]. This step is critical for reaching areas that wipes cannot access [72]. * Follow the manufacturer's instructions for the specific cycle.
5. Reassembly and Recommissioning * Once the chamber is cool and dry, reinstall all clean, dry components [74]. * Close the door, reconnect power and gas, and allow the incubator to stabilize to the required temperature, CO₂, and humidity levels before reintroducing cultures [73].
Decontamination Workflow
The following diagram illustrates the logical workflow for a systematic decontamination process.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Reagents and Materials for Decontamination
| Item | Function / Purpose | Example / Notes |
|---|---|---|
| 70% Ethanol (IPA) [72] [73] | General surface disinfection for routine wipe-downs. | Effective for daily and weekly cleaning; requires rinsing with distilled water if used before a heat cycle [73]. |
| Quaternary Ammonium Disinfectants [73] | Broad-spectrum disinfectant for interior chamber surfaces. | Non-corrosive; suitable for final wipe-down of the interior chamber [73]. |
| Hydrogen Peroxide (H₂O₂) [72] [74] | Vapor-phase decontamination for comprehensive, no-touch decontamination. | Used in foggers or built-in systems; penetrates crevices [72] [74]. |
| Sterile Distilled Water [72] [73] | Used for rinsing and in the humidification pan. | Prevents introduction of contaminants from tap water; essential for water pan [72]. |
| Lint-Free Cloths / Wipes [73] | For applying disinfectants and drying surfaces. | Prevents lint from contaminating the clean chamber [73]. |
| Heat-Resistant Gloves [73] | Personal protective equipment (PPE) for handling hot components and using chemicals. | Essential for safety during and after heat-based decontamination. |
Troubleshooting Common Decontamination Issues
Q: My cultures are still getting contaminated shortly after a decontamination cycle. What could be wrong?
- Cause 1: Rapid Recontamination. Every time the incubator door opens, airborne microbes can enter. In a busy lab, microbial load can rebound quickly if surfaces are not protected [72].
- Solution: Implement more frequent spot-cleaning and consider supplemental decontamination (e.g., hydrogen peroxide fogging) between full monthly cleans [72].
- Cause 2: Hidden Biofilm. The water pan can develop a slimy biofilm if not cleaned and refilled with sterile water frequently enough [72].
- Solution: Empty, clean, and refill the water pan with sterile distilled water weekly or biweekly. Use antimicrobial agents as recommended by the manufacturer [72].
- Cause 3: Contaminated Cultures. The source may not be the incubator itself, but the cultures placed inside it [72].
- Solution: Quarantine new cell lines and always use good aseptic technique. Disinfect the exterior of culture vessels before placing them in the incubator.
Q: Should I use UV light inside my biosafety cabinet (BSC) for decontamination? UV light is a common feature in BSCs, but it has significant limitations. It is only effective on surfaces directly in its line of sight and is not reliable for inactivating all microbial types [74]. UV light should never be used as a substitute for manual chemical decontamination of the work surface and interior walls of the BSC. Its primary use is for surface decontamination and disinfecting the water in the humidity pan when the cabinet is not in use [74].
FAQs: Troubleshooting Cell Culture Contamination in Neuronal Studies
FAQ 1: My neuronal culture medium is becoming acidic very quickly, and I notice tiny, moving particles under the microscope. What is this likely to be, and what should I do?
This is a classic sign of bacterial contamination [65] [75]. The bacteria metabolize components in the medium, producing acidic by-products that cause a sudden drop in pH (often indicated by a color change in the phenol red indicator) [76]. The cloudiness and moving particles are the bacteria themselves [65].
- Action Plan:
- Isolate Immediately: Move the contaminated culture away from your clean lines and other materials in the incubator and biosafety cabinet [65].
- Discard Safely: The most secure action is to autoclave the entire culture vessel to eliminate the contamination and prevent its spread [6].
- Decontaminate: Thoroughly clean the incubator, water bath (if the vessel was placed in it), and biosafety cabinet with an appropriate disinfectant, such as 70% ethanol or isopropanol [76] [28] [65].
FAQ 2: My dissociated cortical neurons are unhealthy and dying after more than two months in culture, even though I see no signs of contamination. What could be happening?
Long-term neuronal cultures are susceptible to subtle stressors. Beyond potential chemical contamination from endotoxins or detergent residues [65] [6], a significant but often overlooked factor is the gradual evaporation of culture medium [77]. This increases the osmotic strength of the medium, stressing the cells over time. Furthermore, mycoplasma contamination is a common culprit for chronic cell health issues without obvious cloudiness [5] [76] [75].
- Action Plan:
- Prevent Evaporation: For long-term studies, consider using culture dish lids that form a gas-tight seal and incorporate a hydrophobic membrane to minimize water loss [77].
- Test for Mycoplasma: Implement a routine screening protocol for mycoplasma using PCR, DNA staining, or commercial ELISA kits [76] [28].
- Quality Control Reagents: Use laboratory-grade water and ensure all media, sera, and supplements are certified low in endotoxins [76] [65].
FAQ 3: I am obtaining inconsistent results in my electrophysiology recordings from a well-established neuronal cell line. Could my culture be the issue?
Inconsistency can stem from cross-contamination, where your cell line has been overgrown by a faster-growing, unrelated cell line [5] [65] [6]. This is a widespread problem that can lead to erroneous and irreproducible data.
- Action Plan:
- Authenticate Cell Lines: Periodically check the identity of your cell lines using DNA fingerprinting, karyotype analysis, or isoenzyme analysis [5] [65] [6].
- Source Cells Reputably: Always obtain cell lines from recognized, reputable cell banks [65] [6].
- Handle One Line at a Time: Practice good aseptic technique by handling only one cell line at a time and using dedicated media for each to prevent cross-contamination [28].
Troubleshooting Guide: Identifying Common Contaminants
The table below summarizes the key visual and microscopic characteristics of common biological contaminants to aid in initial diagnosis.
Table 1: Identification Guide for Common Cell Culture Contaminants
| Contaminant | Macroscopic Appearance (Culture Medium) | Microscopic Appearance | Additional Clues |
|---|---|---|---|
| Bacteria [65] [75] | Cloudy (turbid), possible white film; rapid pH drop (yellow). | Tiny, shimmering granules; rods or cocci may be visible; may show motility. | Visible within a few days; distinct, unpleasant odor. |
| Yeast [65] [75] | Turbid; pH may remain stable initially, then increases. | Round or ovoid particles; often seen in the process of "budding" to form chains. | Slower growing than bacteria; particles are larger than bacteria. |
| Mold/Fungus [65] [75] | Fluffy, fuzzy, or powdery growths (white or black) on the surface; turbid. | Thin, filamentous structures (hyphae) forming a network (mycelium). | Grows more slowly; can survive harsh conditions as spores. |
| Mycoplasma [76] [75] | No change in turbidity or pH. | Not detectable by standard light microscopy. | Causes chronic effects: altered metabolism, slowed growth, chromosomal aberrations [5] [76]. |
Experimental Protocols for Routine Screening
Protocol 1: Routine Monitoring for Microbial Contamination
Principle: Regular visual and microscopic inspection is the first line of defense to catch contamination early.
Methodology:
- Daily Macroscopic Check: Observe the culture medium daily for cloudiness, unusual color changes, or any floating/filmy material [76] [65].
- Daily Microscopic Check: Examine cells under an inverted phase-contrast microscope at low power (e.g., 100x) to assess cell health and look for signs of bacteria or yeast between mammalian cells. Increase magnification (400x) for a more detailed view [65].
- Documentation: Record observations on a quality control checklist to track culture health over time.
Protocol 2: Detection of Mycoplasma by DNA Staining
Principle: Mycoplasma, lacking a cell wall, adheres to the surface of host cells. Fluorescent DNA-binding dyes like DAPI or Hoechst stain the mycoplasma DNA, revealing characteristic particulate or filamentous patterns on the cell surface under a fluorescence microscope [76].
Methodology:
- Grow test cells on a sterile coverslip in a culture dish until subconfluent.
- Fix cells with a fresh mixture of acetic acid and methanol (e.g., 1:3) for 5-10 minutes.
- Prepare a working solution of a DNA stain (e.g., Hoechst 33258 at 0.5 µg/mL in PBS or distilled water).
- Add the stain to cover the fixed cells and incubate for 15-30 minutes in the dark.
- Rinse gently with distilled water to remove excess stain and air dry.
- Mount the coverslip on a slide and examine under a fluorescence microscope with a DAPI filter. The presence of mycoplasma is indicated by small, bright extranuclear dots or filaments on the cell surface and in intercellular spaces (see Diagram 1).
Protocol 3: Novel UV Absorbance Spectroscopy with Machine Learning
Principle: This recently developed method uses ultraviolet (UV) light to create an absorbance "fingerprint" of the cell culture fluid. Machine learning models are then trained to recognize the specific patterns associated with microbial contamination, providing a rapid, label-free, and non-invasive assessment [29].
Methodology:
- Sample Collection: A small, automated sample of the cell culture fluid is taken at designated intervals during the manufacturing or culture process.
- UV Spectroscopy: The sample is subjected to UV absorbance spectroscopy without any additional preparation or staining.
- Machine Learning Analysis: The absorbance spectrum is analyzed by a pre-trained algorithm.
- Result: The method delivers a definitive "yes/no" contamination assessment in under 30 minutes, allowing for early corrective actions [29].
Visualizing the Quality Control Workflow
The following diagram outlines a logical workflow for integrating these protocols into a robust quality control system for neuronal cell culture.
Diagram 1: Integrated QC and Screening Workflow for Neuronal Cell Culture.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Cell Culture QC
| Item | Function/Application |
|---|---|
| DAPI / Hoechst Stains [76] | Fluorescent DNA-binding dyes used to detect mycoplasma contamination and for nuclear staining. |
| Mycoplasma Detection Kit (PCR-based) [28] | Provides reagents for sensitive and specific detection of mycoplasma DNA via polymerase chain reaction. |
| Cell Line Authentication Kit (STR) | Contains reagents for Short Tandem Repeat (STR) profiling to uniquely identify and confirm cell line identity. |
| Gentle Cell Dissociation Reagent (e.g., Accutase) [5] | A milder alternative to trypsin for detaching sensitive adherent cells (e.g., neurons) while preserving cell surface proteins. |
| Defined Fetal Bovine Serum (FBS) [76] | Provides essential growth factors and nutrients; selecting serum tested for viruses and low endotoxin levels is critical. |
| Penicillin-Streptomycin (Antibiotic-Antimycotic) [65] | Used to suppress bacterial and fungal growth. Note: Recommended for short-term use only to avoid masking contaminants. |
| 70% Ethanol / Isopropanol [76] [28] | Standard disinfectant for decontaminating surfaces, gloves, and equipment within the biosafety cabinet. |
| Sealed Culture Dish with Gas-Permeable Membrane [77] | Specialized dish that minimizes medium evaporation, crucial for the long-term health of neuronal cultures. |
Emergency Response to Contamination
When contamination is confirmed, a swift and systematic response is critical to contain the issue.
Diagram 2: Emergency Response Pathway for Contamination Events.
Ensuring Authenticity: Cross-Contamination Prevention and Culture Validation
HeLa cell cross-contamination represents a persistent and critical challenge in biomedical research, including the field of neuronal studies. Originating from Henrietta Lacks's cervical cancer tumor in 1951, HeLa cells are remarkably vigorous and adaptable, capable of outcompeting and completely replacing other cell lines in culture [78]. This contamination compromises data integrity, experimental reproducibility, and the validity of research findings, potentially leading to decades of misleading scientific literature [79]. For researchers in neuronal studies, where precise cellular models are paramount, understanding and preventing this issue is not just good practice—it is essential for scientific credibility.
FAQs on HeLa Cell Cross-Contamination
What is HeLa cell cross-contamination and why is it a particular problem?
Cross-contamination occurs when HeLa cells are inadvertently introduced into and overgrow another cell culture. This is a severe problem due to HeLa's aggressive growth rate, hardy nature, and ability to thrive in various culture conditions [80]. Once introduced, HeLa cells can completely displace the original cell population, leading to a culture that is genetically HeLa but misidentified as another cell type [81] [78]. It is estimated that 15-20% of cell lines in use may be misidentified, and HeLa is one of the most common contaminants [82].
How can I tell if my neuronal cell line has been taken over by HeLa cells?
Morphological changes under a microscope can be a first clue, but they are not definitive, as HeLa cells can appear similar to other epithelial cells [81]. Relying on morphology or cell behavior alone is insufficient. Unexpected changes in cell behavior, growth rates, or gene expression profiles in your neuronal cultures should raise suspicion, but conclusive identification requires authentic genetic authentication [14].
What are the most reliable methods to authenticate my cell lines?
The gold standard for intra-species cell line authentication is Short Tandem Repeat (STR) profiling. This method analyzes highly variable regions of the genome to create a unique DNA fingerprint for a cell line, which can be compared against reference databases [81] [82]. For specifically detecting HeLa contamination, a highly sensitive method is nested PCR for HPV-18, a virus integrated into the HeLa genome. This method can detect HeLa contamination at levels as low as 1% and can even be performed using cell culture supernatant, making it a rapid and "non-invasive" check [80].
The table below compares these two key methods:
| Method | Principle | Sensitivity | Key Advantage | Key Disadvantage |
|---|---|---|---|---|
| STR Profiling [81] [82] | DNA fingerprint of multiple genomic loci | ~10% [80] | Gold standard; provides a unique identifier for any human cell line | Requires specialized equipment and analysis; lower sensitivity |
| HPV-18 Nested PCR [80] | Amplification of HeLa-specific viral DNA | ~1% | High sensitivity and specificity for HeLa; can use culture supernatant | Only detects HeLa contamination, not other cell line mix-ups |
The primary source is human error during cell culture handling. This includes:
- Using the same media, reagents, or pipettes for different cell lines without adequate decontamination [14].
- Generating aerosols containing cells during pipetting, which can spread to other cultures [82].
- Working with multiple cell lines simultaneously in the same biosafety cabinet [14].
- Contamination from a known HeLa-positive cell line cultured in the same lab, as was the case with the HES cell line being contaminated via WISH cells [81].
My cell line is contaminated with HeLa cells. What should I do?
The only universally recommended course of action for a contaminated culture is immediate disposal by autoclaving or chemical disinfection [83] [17]. Attempting to "rescue" a contaminated culture is generally not advised, as it is extremely difficult to eradicate all HeLa cells, and the risk of spreading the contamination is high [17]. You must then decontaminate all associated equipment (incubators, biosafety cabinets) and quarantine and authenticate all other cell lines cultured in the same environment [83].
Troubleshooting Guide: Prevention and Detection
Preventing HeLa cross-contamination is a multi-faceted effort requiring strict discipline and routine monitoring. The following workflow outlines a comprehensive strategy for maintaining culture integrity.
Essential Research Reagent Solutions
A key component of contamination prevention is using the right tools for detection and maintenance. The following table details essential reagents for managing HeLa contamination risk.
| Reagent / Kit | Function | Application Note |
|---|---|---|
| STR Profiling Kit [81] | Amplifies core set of STR loci to generate a DNA fingerprint for a cell line. | The resulting profile should be matched against a reference database (e.g., ATCC, DSMZ) for authentication. |
| HPV-18 Specific Primers [80] | Used in PCR or nested PCR to detect the unique HPV-18 genome present in HeLa cells. | Ideal for rapid, specific, and highly sensitive screening of potential HeLa contamination. |
| Mycoplasma Detection Kit [17] | Detects mycoplasma contamination via PCR, fluorescence, or ELISA. | Regular screening is crucial, as mycoplasma infection can make cells more vulnerable to cross-contamination. |
| Validated Cell Line | A certified, uncontaminated cell line obtained from a reputable bank (e.g., ATCC, ECACC). | Serves as a positive control for STR profiling and ensures your starting material is authentic. |
Detailed Experimental Protocol: HPV-18 Nested PCR for HeLa Detection
This protocol, adapted from a 2018 study, provides a highly sensitive method to screen for low-level HeLa contamination directly from cell culture supernatant, minimizing the need to sacrifice valuable cells [80].
Principle: This nested PCR assay targets the HPV-18 E6 gene, which is integrated into the HeLa genome. The two-round amplification significantly increases sensitivity and specificity.
Materials:
- Cell culture supernatant from the test cell line.
- Positive control: HeLa cell culture supernatant.
- Negative control: Cell culture medium and supernatant from a known HeLa-free line.
- PCR primers for the first and second (nested) rounds of amplification (sequences as defined in the source publication [80]).
- PCR master mix, thermal cycler, and agarose gel electrophoresis equipment.
Procedure:
- Sample Collection: Centrifuge cell culture medium at 300 × g for 5 minutes to remove cells and debris. Use the clear supernatant directly as the PCR template without DNA extraction [80].
- First Round PCR:
- Set up a PCR reaction mix using the outer set of primers.
- Use 2-5 µL of the collected supernatant as the template.
- Run the PCR with the appropriate cycling conditions (denaturation, annealing, extension).
- Second Round (Nested) PCR:
- Take a small aliquot (e.g., 1 µL) of the first-round PCR product.
- Set up a new PCR reaction mix using the inner (nested) set of primers.
- Run the PCR with optimized cycling conditions.
- Analysis:
- Run the final PCR products on an agarose gel stained with ethidium bromide.
- Visualize under UV light. A positive result (a band of the expected size) indicates the presence of HeLa cells in the original culture.
Interpretation: The presence of the specific HPV-18 amplicon in the test sample, co-migrating with the HeLa positive control, confirms HeLa contamination. The negative controls should show no bands. This method is capable of detecting HeLa contamination when it constitutes as little as 1% of the total cell population [80].
Vigilance against HeLa cell cross-contamination is a fundamental aspect of responsible science, especially in precise fields like neuronal research where model integrity is paramount. By integrating strict aseptic techniques, meticulous lab practices, and routine cell line authentication using methods like STR profiling and HPV-18 PCR, researchers can safeguard their work. This proactive approach is the most effective strategy to ensure the validity, reproducibility, and long-term value of your scientific findings.
Core Concepts: Authentication Methods at a Glance
Cell line authentication is a critical quality control process that verifies the identity and purity of cell lines used in research. For neuronal studies, where the use of misidentified cells can invalidate findings on disease mechanisms and drug responses, authentication is indispensable. The table below summarizes the two primary techniques discussed in this guide.
| Method | Primary Function | Key Output | Detects |
|---|---|---|---|
| DNA Fingerprinting (STR Profiling) [84] [85] | Confirms cell line identity and origin | DNA profile based on specific loci (e.g., 13-24 STR markers) [86] [85] | Misidentification, cross-contamination with other human cell lines [87] |
| Karyotyping [87] | Analyzes chromosomal number and structure | Visual map of chromosomes (karyogram) | Large-scale genetic changes, chromosomal abnormalities, aneuploidy [87] |
Detailed Experimental Protocols
Protocol 1: Cell Line Authentication via Short Tandem Repeat (STR) Profiling
STR profiling is the gold-standard method for authenticating human cell lines. The following workflow is based on international guidelines (ANSI/ATCC ASN-0002-2022) [85].
Workflow: STR Profiling for Cell Line Authentication
- DNA Extraction: Purify high-quality genomic DNA (gDNA) from a cell pellet. The recommended DNA input is 1-5 ng for direct amplification or up to 500 ng for samples stored on cards [85].
- Multiplex PCR: Amplify the target STR loci in a single PCR reaction. Commercial kits, such as the GenePrint 24 System or ThermoFisher's CLA GlobalFiler, are available that target the core 13 loci recommended by the ANSI/ATCC standard, plus additional markers for higher discrimination power [86] [85] [88].
- Capillary Electrophoresis: The PCR products are separated by size using capillary electrophoresis. An instrument like the Spectrum Compact CE System detects the fluorescently labeled fragments and generates an electropherogram [85].
- Data Analysis: Software (e.g., GeneMapper) analyzes the electropherogram to determine the number of repeats at each STR locus, producing an allele table or a unique STR profile for the cell line [86] [85].
- Profile Comparison: Compare the obtained STR profile against a reference database such as ATCC, DSMZ, or Cellosaurus [85].
- Interpretation: A match of 80% or higher with the reference profile is generally considered authenticated. Lower percentages suggest misidentification or cross-contamination [85].
Protocol 2: Cell Line Validation via Karyotyping
Karyotyping provides a macroscopic view of the cell's chromosomal integrity, which is crucial for identifying genetic drift in cultured neuronal cells.
Workflow: Karyotyping Analysis
- Cell Arrest and Harvesting: Treat actively dividing cells with colcemid to arrest them in metaphase, when chromosomes are most condensed. Harvest the cells and treat them with a hypotonic solution to swell them, which helps spread the chromosomes apart [87].
- Fixation: Fix the cells in a mixture of methanol and acetic acid (Carnoy's solution). This preserves the chromosome structure.
- Slide Preparation: Drop the fixed cell suspension onto a microscope slide, causing the nuclei to rupture and chromosomes to scatter. Stain the chromosomes, typically with Giemsa stain (G-banding), to produce a characteristic banding pattern for each chromosome pair [87].
- Microscopy and Analysis: Capture images of complete metaphase spreads under a microscope. Use software to arrange the chromosomes into a standardized karyogram, ordered by size, centromere position, and banding pattern.
- Identification: Compare the karyogram to a normal reference for the species. Note any numerical abnormalities (e.g., aneuploidy) or structural abnormalities (e.g., translocations, deletions) [87].
Troubleshooting Common Issues in Neuronal Cell Lines
Problem: STR analysis shows multiple extra alleles at numerous loci.
- Cause: Cross-contamination of your neuronal cell line with another human cell line.
- Solution: If the contamination is recent, you may attempt to subclone single cells to isolate the original line. However, the most reliable action is to discard the culture and thaw a new, authenticated vial from your stock. Re-authenticate the new culture upon thawing [85].
Problem: STR profile matches the reference database but at a low percentage (~60-70%).
- Cause: Genetic drift due to long-term culture or high passage number. Neuronal progenitor lines are particularly susceptible to genomic changes over time.
- Solution: Always return to an early-passage, authenticated stock (master cell bank). Authenticate your working stocks regularly and do not use cells beyond a defined passage number (e.g., every 10 passages) [86] [85].
Problem: Karyotype reveals aneuploidy or new structural variants.
- Cause: Accumulation of genetic instability during extended in vitro culture. This can alter cell behavior and gene expression profiles.
- Solution: Establish a new working cell bank from an early-passage stock. For functional experiments, consider using isogenic cell lines with defined genetic backgrounds or primary neuronal cultures for more physiologically relevant, albeit short-term, studies.
Problem: STR authentication fails for a non-human neuronal cell line (e.g., rat or mouse).
- Cause: The core STR panels and databases are often optimized for human cell lines.
- Solution: For non-human cells, alternative methods such as DNA barcoding (using the cytochrome c oxidase I gene) or SNP genotyping are recommended for species verification and line identification [84].
Frequently Asked Questions (FAQs)
Q: Why is cell line authentication especially critical in neuronal research? Using a misidentified or contaminated cell line can lead to incorrect conclusions about neuronal development, disease mechanisms, or drug responses. This wastes resources and misdirects future research. Many funding agencies like the NIH and journals require authentication for grant applications and publications [89] [84].
Q: How often should I authenticate my neuronal cell lines? Best practices recommend authentication:
- When a new cell line is acquired or established.
- Upon creating a new working stock or freezing down a master cell bank.
- At regular intervals during continuous culture (e.g., every 10 passages or every 3 months).
- Before starting a new series of experiments or submitting a manuscript for publication [86] [85].
Q: My lab does not have a capillary electrophoresis instrument. How can I perform STR profiling? You can outsource authentication to core facilities or commercial service providers. Many companies offer fee-for-service STR profiling with fast turnaround times, often in CLIA-certified or ISO-accredited labs, ensuring high-quality results [86] [85] [88].
Q: What is the first step I should take before any lab work with a new cell line? Before even thawing a new vial, consult the ICLAC Register of Misidentified Cell Lines. This free database lists nearly 600 known problematic lines. Checking it is a quick, zero-cost step to avoid using a cell line known to be cross-contaminated [90] [85].
Q: Can mycoplasma contamination affect authentication results? While mycoplasma contamination does not directly alter the STR profile, it severely compromises cell health and experimental validity, potentially leading to irreproducible results. Regular mycoplasma testing is a complementary and essential practice for maintaining healthy, reliable cell cultures [84] [33].
| Item | Function | Example Products/Resources |
|---|---|---|
| STR Multiplex Kit | Amplifies multiple STR loci in a single PCR reaction for DNA profiling. | GenePrint 24 System, ThermoFisher GlobalFiler CLA [85] [88] |
| Capillary Electrophoresis System | Separates amplified DNA fragments by size to generate an STR profile. | Spectrum Compact CE System, ABI 3730xl DNA Analyzer [86] [85] |
| Reference Databases | Online repositories of STR profiles for comparing and authenticating cell lines. | ATCC STR Database, DSMZ Database, Cellosaurus [84] [85] |
| ICLAC Misidentified Cell Line Register | A critical checklist of nearly 600 known cross-contaminated or misidentified cell lines to avoid. | ICLAC Register [90] [85] |
| Cell Culture Contamination Prevention Kit | Essential supplies for maintaining aseptic technique and preventing microbial contamination. | 70% Ethanol, sterile filtered media, mycoplasma detection kits [33] |
FAQs on Contamination Recovery and Functional Validation
Q1: What are the immediate steps to take after suspecting a contamination in a neuronal culture? Your first actions are critical to save the experiment and prevent cross-contamination.
- Isolate: Immediately move the contaminated culture from the incubator and laminar flow hood to a designated quarantine area [65].
- Identify: Determine the contaminant type (e.g., bacteria, yeast, mold, mycoplasma) using microscopy and other specific tests [65] [5].
- Decontaminate: Thoroughly clean the incubator and laminar flow hood with a laboratory disinfectant. Check HEPA filters if applicable [65].
- Assess Value: Decide if the culture is irreplaceable. For unique primary neurons, decontamination may be attempted. For common cell lines, autoclaving and disposal is often the safest course [65].
Q2: How can I verify that my neuronal culture has recovered its true phenotype after a contamination event? Recovery is not just about the absence of contaminants; it's about restoring fundamental neuronal characteristics.
- Check Morphology: Use phase-contrast microscopy to confirm the re-establishment of typical neuronal morphology, such as elongated axons and dendritic arbors [3].
- Authenticate Identity: Perform immunostaining for neuron-specific markers like Microtubule-Associated Protein 2 (MAP-2) to confirm the cellular identity has not been lost or altered [3].
- Confirm Functionality: Proceed to validate synaptic activity, as a phenotypically correct neuron must also be functionally competent.
Q3: What are the highest-throughput methods for mapping synaptic connectivity in validated cultures? Recent advances focus on optical methods to greatly increase mapping throughput.
- All-Optical Mapping: Methods combining holographic optogenetics for presynaptic stimulation with optical postsynaptic readouts (e.g., using genetically encoded voltage or calcium indicators) are emerging. These can interrogate connectivity across dozens to hundreds of potential presynaptic cells within minutes [91] [92].
- Compressive Sensing: This computational approach can be combined with multi-cell optogenetic stimulation. It leverages the inherent sparsity of neural connections to recover synaptic maps with a significant reduction in the number of required measurements, boosting throughput [91].
Q4: My primary neurons are senescing quickly after recovery, limiting long-term experiments. What can I do? This is a common challenge with primary cells.
- Acknowledge Limitation: Primary neurons have a limited lifespan and undergo senescence after a few divisions, which restricts long-term experiments [3].
- Plan Experiments Accordingly: Perform functional validation experiments as soon as possible after recovery and confirmation of health [3].
- Consider Alternatives: For long-term studies, consider using genetically defined immortalized cell lines. However, be aware that their physiological relevance may be lower than that of primary cells [3].
Troubleshooting Guides
Troubleshooting Contamination Identification
Use the table below to quickly identify common contaminants and initial actions.
Table 1: Identification and Initial Response to Common Contaminants
| Contaminant Type | Visual Signs (Microscopy) | Culture Medium pH | Recommended Action |
|---|---|---|---|
| Bacteria | Tiny, moving granules between cells; turbid culture [65] | Sudden drop [65] | Disculture in most cases; if irreplaceable, attempt antibiotic decontamination [65] |
| Yeast | Ovoid or spherical particles, may bud off smaller particles [65] | Stable initially, increases later [65] | Disculture; antimycotics can be attempted for valuable cultures [65] |
| Mold | Thin, wisp-like filaments (hyphae) or dense spore clumps [65] | Stable initially, increases later [65] | Disculture immediately to prevent spore release. |
| Mycoplasma | No obvious visual change; can cause subtle cellular effects [5] | No obvious change [65] | Test with PCR or specialized kits; treat with specific antibiotics if culture is vital [5]. |
Troubleshooting Functional Validation Assays
After confirming phenotypic recovery, use this guide to address issues in functional assays.
Table 2: Troubleshooting Synaptic Activity and Connectivity Assays
| Problem | Potential Cause | Solution |
|---|---|---|
| No postsynaptic response upon stimulation | Culture is not synaptically mature. | Extend culture time (e.g., beyond 14-21 days for human neurons) and use immunostaining for synaptic markers (e.g., synapsin, PSD-95) to confirm maturity. |
| Presynaptic neurons are not firing action potentials (APs). | Validate optogenetic stimulation efficacy by performing cell-attached recordings to confirm reliable, temporally precise AP generation [91]. | |
| High variability in synaptic response strength | Fluctuating neuromodulatory environment or membrane potential in vivo [91]. | Increase the number of repeated trials for averaging to reduce noise [91]. |
| Instability of whole-cell patch-clamp recording. | Ensure recording health by monitoring access resistance and membrane potential. | |
| Inability to detect connections in a dense culture | The connectivity rate is very low (sparse). | Use high-throughput methods like compressive sensing, which is designed to efficiently find sparse connections [91]. |
| The postsynaptic responses are very small (e.g., a few pA). | Ensure healthy postsynaptic neurons and use recording conditions that enhance signal-to-noise ratio. |
Experimental Protocols for Validation
Protocol 1: Validating Neuronal Phenotype Post-Recovery via Immunostaining
This protocol confirms that cells have re-established their neuronal identity after a contamination event [3].
- Culture Fixation: Aspirate the medium from the recovered culture and wash with PBS. Fix cells with 4% paraformaldehyde for 15 minutes at room temperature.
- Permeabilization and Blocking: Permeabilize cells with 0.1% Triton X-100 in PBS for 10 minutes. Block non-specific binding with 5% normal serum (from the secondary antibody host species) for 1 hour.
- Primary Antibody Incubation: Incubate with a neuron-specific primary antibody (e.g., mouse anti-MAP-2) diluted in blocking buffer overnight at 4°C.
- Secondary Antibody Incubation: Wash and incubate with a fluorophore-conjugated secondary antibody (e.g., goat anti-mouse Alexa Fluor 488) for 1 hour at room temperature in the dark.
- Imaging and Analysis: Mount and image using a fluorescence microscope. A successful validation shows strong MAP-2 signal in the cell body and neuronal processes.
Protocol 2: In Vivo High-Throughput Synaptic Connectivity Mapping
This protocol, adapted from recent research, uses two-photon holographic optogenetics and electrophysiology to map multiple connections rapidly [91].
- System Setup: Use a custom-built optical system with paths for two-photon imaging and two-photon holographic stimulation via a spatial light modulator (SLM).
- Presynaptic Stimulation:
- Express a fast, soma-targeted opsin (e.g., ST-ChroME) in presynaptic neurons.
- Use the SLM to generate multiple holographic spots (e.g., for 100 neurons) within a ~350x350x400 µm³ field of view.
- Stimulate with 10 ms pulses at a power density of 0.15–0.3 mW/µm² to reliably induce single action potentials with low latency and jitter [91].
- Postsynaptic Recording: Perform whole-cell patch-clamp recordings from a postsynaptic neuron to detect postsynaptic currents (PSCs) or potentials (PSPs).
- Sequential vs. Compressive Sensing Modes:
- Sequential Single-Cell: Stimulate presynaptic neurons one at a time, repeating trials for averaging. This identifies connected pairs and their synaptic properties in about 5 minutes for 100 cells [91].
- Multi-Cell with CS: Stimulate random combinations of presynaptic neurons. Use compressive sensing algorithms to demix the postsynaptic responses, reducing the number of required measurements by up to threefold in sparsely connected networks [91].
The workflow for this high-throughput validation is summarized in the diagram below.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Neuronal Recovery and Functional Validation
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| Antibiotics/Antimycotics | To combat identified bacterial or fungal contaminants during recovery. | Use only as a last resort and for short durations to avoid cryptic infections and resistance [65]. |
| Neuron-Specific Antibodies | To authenticate neuronal phenotype post-recovery via immunostaining. | Anti-MAP-2: Confirms neuronal identity and health of processes [3]. Anti-Synapsin I/PSD-95: Confirms presence of pre- and post-synaptic compartments. |
| Soma-Targeted Opsin | For precise, reliable presynaptic stimulation in connectivity mapping. | ST-ChroME: A fast opsin restricted to the soma, allowing cellular resolution stimulation with millisecond precision [91]. |
| Magnetic Cell Separation Beads | For isolating specific primary brain cell types (e.g., neurons, microglia) from mixed cultures or tissue. | CD11b beads: Isolate microglia. ACSA-2 beads: Isolate astrocytes. Neuronal kits: Use negative selection to deplete non-neuronal cells [3]. |
| Percoll Gradient | A density-based, non-enzymatic method to isolate primary microglia and astrocytes. | An alternative to immunomagnetic beads that can help preserve cell surface proteins and viability [3]. |
| Compressive Sensing Software | For computationally efficient reconstruction of synaptic connectivity from multi-neuron stimulation data. | Custom algorithms that leverage sparsity to reduce measurement time by up to 3-fold [91]. |
In neuronal cell culture, "contamination" extends beyond mere microbial presence to include biological and chemical impurities that can compromise experimental integrity. For researchers working with neuronal models, understanding the distinct contamination profiles of primary neuronal cultures versus those derived from induced pluripotent stem cells (iPSCs) is crucial for accurate data interpretation and reproducible results. Primary neuronal cultures, directly isolated from animal or human tissue, face specific risks from their heterogeneous cellular composition and complex isolation procedures [93] [94]. In contrast, iPSC-derived neuronal cultures, while offering unprecedented access to human-specific models, introduce contamination challenges stemming from extensive in vitro manipulation, prolonged culture periods, and potential issues with differentiation efficiency [95] [96]. This technical guide provides a systematic framework for identifying, troubleshooting, and preventing contamination issues specific to these two fundamental neuronal culture systems, equipping researchers with practical strategies to maintain culture purity and experimental validity within the broader context of neuronal studies research.
Comparative Contamination Profiles
The table below summarizes the principal contamination types, their sources, and characteristic indicators in primary versus iPSC-derived neuronal cultures.
Table 1: Comparative Contamination Profiles in Neuronal Culture Systems
| Contamination Type | Primary Neuronal Cultures | iPSC-Derived Neuronal Cultures |
|---|---|---|
| Biological: Cellular | Innate Mixed Population: Inherently contain non-neuronal cells (astrocytes, microglia, fibroblasts, endothelial cells) without purification [93] [94]. | Differentiation Imperfection: Heterogeneous outcomes with variable neuronal content; potential persistent undifferentiated iPSCs or off-target cell types (e.g., fibroblast-like cells) [95] [96]. |
| Biological: Microbial | Introduction from Host Tissue: Risk from donor microbiota during dissection and tissue processing [94] [5]. | Prolonged Culture Risk: Extended in vitro culture increases exposure opportunities; often amplified by antibiotic-free protocols to avoid masked, low-grade infections [97]. |
| Biological: Viral | Risk from Donor: Source material potentially carries adventitious agents (e.g., HIV, Hepatitis B/C) [97]. | Risk from Source Cells & Reprogramming: Donor cells or viral vectors used for reprogramming can introduce viral contaminants [97]. |
| Chemical/Reagent | Enzyme & Reagent Residues: Enzymatic digestion mixes (papain, collagenase) or purification gradient media (OptiPrep) can carry through to cultures [94]. | Small Molecules & Factors: Residual differentiation factors (e.g., CHIR99021, LDN193189), coating matrices (Geltrex, laminin), and quality variability between reagent lots significantly impact differentiation efficiency and phenotype [96] [98]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: My iPSC-derived sensory neurons show high transcriptional variability in key neuronal markers compared to primary DRG. Is this a sign of problematic culture conditions?
A1: Not necessarily. Higher transcriptional variability, particularly in genes related to nervous system development, is a recognized characteristic of iPSC-derived sensory neurons compared to primary dorsal root ganglion (DRG) tissue. One study reported a median coefficient of variation (CV) of 0.37 in iPSC-derived sensory neurons versus 0.23 in primary DRG [95]. This can stem from variability in differentiation efficiency rather than microbial contamination. It is recommended to use single-cell RNA-seq or immunostaining to quantify the purity of your neuronal population and adjust differentiation protocols accordingly [95] [96].
Q2: I am observing cellular debris and inconsistent neuronal morphology in my primary murine sensory neuron cultures shortly after plating. What is the likely cause?
A2: This is a common challenge in primary culture preparation. The cause is often suboptimal enzymatic digestion or mechanical dissociation during the isolation process from trigeminal ganglia or DRG [94]. Over-digestion with enzymes like papain or collagenase/dispase can damage surface proteins and decrease viability, while under-digestion yields insufficient neuron yield. Precise timing, temperature control, and using well-clarified enzyme solutions are critical. Implementing a density gradient centrifugation step (e.g., using OptiPrep) can effectively purify neurons from debris and myelin [94].
Q3: How can the initial culture conditions of my iPSCs affect the subsequent differentiation into neurons and potential contamination?
A3: The starting culture conditions of iPSCs have a profound downstream impact. Research shows that iPSCs maintained in Essential 8 (E8) medium prior to differentiation yielded sensory neurons with an estimated 28-36% higher neuronal content compared to those derived from iPSCs maintained on mouse embryonic fibroblast (MEF) feeders [95]. Furthermore, the use of feeder cells introduces an additional biological variable and a potential source of microbial contamination (e.g., mycoplasma). A transition to feeder-free, chemically defined culture systems for iPSC maintenance is recommended to enhance reproducibility and minimize this risk [95] [97].
Troubleshooting Guide: Step-by-Step Problem Solving
Problem: Suspected Mycoplasma Contamination in an iPSC Neuronal Culture
Mycoplasma contamination is a common and serious issue that can alter cell metabolism and behavior without causing turbidity in the media [5].
- Step 1: Observation & Initial Action: Look for subtle signs like a slight granular appearance in the culture, unexplained changes in cell growth rates, or poor differentiation efficiency. Do not rely on media turbidity. Quarantine the suspect culture immediately [5] [97].
- Step 2: Confirmatory Testing:
- PCR-based Detection: Use a commercially available mycoplasma detection kit. This is the most sensitive and rapid method for routine screening [5].
- Hoechst Staining: Fix cells and stain with a DNA stain like Hoechst 33258. Visualize under fluorescence microscopy; mycoplasma will appear as tiny, speckled fluorescent dots in the cytoplasm and surrounding the cells, distinct from the intact nuclear DNA [5].
- Step 3: Decision Point & Decontamination:
- Recommended Action: The ISSCR and other guidelines strongly recommend discarding contaminated cultures whenever possible. Mycoplasma eradication is difficult, risks persistence, and can spread to other cultures [97].
- Last-Resort Treatment: If the cell line is irreplaceable, commercial antibiotic mixtures like Plasmocin can be attempted. Treat the contaminated culture according to the manufacturer's instructions. However, this may only suppress the infection and requires rigorous post-treatment validation [5].
- Step 4: Validation & Prevention: After treatment or upon establishing a new line, validate sterility by testing the culture after at least two passages without antibiotics. Implement routine, scheduled mycoplasma testing for all stock and active cultures [97].
Problem: Low Yield and Purity in Differentiated iPSC-Derived Dopaminergic Neurons
- Step 1: Quality Control of Starting Material: Ensure your iPSCs are healthy, have a high pluripotency marker expression, and are free of differentiation before beginning. Characterize your neural progenitor cells (NPCs) for key midbrain markers like FOXA2 and LMX1A to ensure proper patterning [98].
- Step 2: Review Protocol Specifics: Minor deviations in the concentration or timing of small molecules can drastically alter outcomes. Double-check the concentrations of key patterning factors like SHH (e.g., Sonic Hedgehog), Purmorphamine (a SHH agonist), and CHIR99021 (a GSK3 inhibitor) used during the neural induction and floor-plate patterning stages [98].
- Step 3: Assess Final Culture Composition: Characterize the differentiated neurons not just for a general neuronal marker (βIII-tubulin), but also for specific dopaminergic markers like Tyrosine Hydroxylase (TH) and nuclear markers like NURR1 (NR4A2). Quantify the percentage of TH-positive neurons to assess efficiency [98].
- Step 4: Mitigate Non-Neuronal Outgrowth: If the culture is overgrown with non-neuronal cells, consider using a defined, serum-free medium. For some protocols, a brief treatment with mitotic inhibitors like FUDR can be applied to suppress proliferating glial cells without harming post-mitotic neurons [94] [96].
Essential Methodologies for Contamination Control
Protocol: Purification of Primary Murine Sensory Neurons
This protocol, adapted from [94], is critical for obtaining a high-purity neuronal population from dissected tissue, minimizing non-neuronal cellular contamination.
- Dissection and Enzymatic Digestion: Euthanize adult mouse (6-10 weeks) and dissect trigeminal ganglia (TG) or DRG. Perfuse transcardially with cold HBSS before dissection if possible. Collect ganglia in cold HBSS. Incubate tissues in Papain solution (120 units in 3ml HBSS) for 30-45 minutes at 37°C on a rotator.
- Secondary Digestion: Remove papain and replace with Collagenase/Dispase solution (210 units collagenase + 1.1 units neutral protease in 3ml HBSS). Incubate for another 30-45 minutes at 37°C.
- Trituration and Gradient Centrifugation:
- Gently triturate the digested tissue 15-20 times using a fire-polished glass Pasteur pipette to create a single-cell suspension.
- Prepare a discontinuous OptiPrep density gradient in a 15ml conical tube: 1ml each of layers with densities 0.3 g/ml, 0.23 g/ml, 0.16 g/ml, and 0.1 g/ml.
- Carefully layer the cell suspension on top of the gradient.
- Centrifuge at 800 x g for 20 minutes in a swing-bucket rotor with slow acceleration and deceleration brakes turned off.
- Neuron Collection and Plating:
- After centrifugation, collect the neuronal cell band, typically found at the interface between the 0.16 g/ml and 0.23 g/ml layers.
- Wash the collected cells twice with warm Neurobasal-A Complete (NBA-C) medium to remove all traces of OptiPrep.
- Plate neurons on poly-D-lysine/laminin-coated coverslips at the desired density in NBA-C medium.
- Maintenance: After 24 hours, consider adding NBA-FUDR medium (containing mitotic inhibitors) for 2-3 days to suppress dividing non-neuronal cells, thereby enhancing long-term neuronal purity [94].
Workflow Diagram: Contamination Control in Neuronal Cultures
The diagram below visualizes the key decision points for identifying and addressing contamination in primary and iPSC-derived neuronal cultures.
Figure 1: Contamination Identification and Mitigation Workflow. This diagram outlines a systematic approach to diagnosing and addressing common issues in neuronal cultures, with specific paths for primary and iPSC-derived systems.
The Scientist's Toolkit: Essential Reagents & Materials
The table below lists critical reagents used in establishing and maintaining pure neuronal cultures, along with their specific functions and contamination control considerations.
Table 2: Key Research Reagent Solutions for Neuronal Culture Purity
| Reagent/Material | Function in Culture | Contamination Control Consideration |
|---|---|---|
| Accutase / Accumax [98] | A milder, enzyme-based cell detachment solution for passaging iPSCs and neurons. | Preserves cell surface proteins (vs. trypsin), enabling better FACS analysis for purity checks; less cytotoxic [5]. |
| LDN193189 & SB431542 [98] | Small molecule inhibitors used in dual SMAD inhibition for efficient neural induction of iPSCs. | Critical for generating pure neural progenitor populations; batch-to-batch variability can significantly impact differentiation efficiency and consistency [98]. |
| Poly-D-Lysine (PDL) / Laminin [94] | Coating substrates for promoting neuronal attachment and neurite outgrowth. | Essential for primary neuron survival; must be prepared sterilely. Laminin can crystallize and lose function if allowed to dry out after coating [94]. |
| OptiPrep [94] | Density gradient medium for purifying neurons from cellular debris and myelin after tissue dissociation. | Residual must be thoroughly washed post-purification as it can be toxic to cells [94]. |
| ROCK Inhibitor (Y-27632) [98] | Improves survival of single cells (e.g., after iPSC passaging or thawing). | Reduces selective pressure from massive cell death, which can otherwise lead to genetic drift in cultures [98]. |
| Chemically Defined Media (e.g., mTeSR, E8) [95] | Serum-free media for feeder-free maintenance of iPSCs. | Eliminates variability and microbial risk associated with serum and feeder cells, enhancing reproducibility and reducing biological contamination sources [95] [97]. |
| FuDR (5'-fluoro-2'-deoxyuridine) [94] | A mitotic inhibitor. | Selectively eliminates dividing non-neuronal cells (e.g., glia, fibroblasts) in primary neuronal cultures, thereby increasing neuronal purity over time [94]. |
Frequently Asked Questions (FAQs)
1. What are the most critical components of a reproducibility package for a manuscript? A successful reproducibility package must allow another researcher to independently reproduce all computations, tables, and figures starting from the rawest data possible [99]. Essential components include a comprehensive README file with a file overview and run instructions, all raw data and analysis code, data collection instruments for original data, and a codebook for all datasets [99]. The package should be structured with clear directories for code, data, and results.
2. My neuronal cell line is growing slowly and the medium turns yellow quickly. What should I suspect? This is a classic sign of mycoplasma contamination [21]. Key characteristics include premature acidification of the medium (yellowing), slowed cell proliferation, and eventual massive cell death. Other symptoms can include altered cell morphology, such as cells becoming more spread out or filamentous [21].
3. What guidelines exist for designing rigorous and reproducible animal studies? The ARRIVE guidelines (Animal Research: Reporting of in Vivo Experiments) are the established gold standard [100]. Many journals now require adherence to the ARRIVE Essential 10, which includes minimal recommendations for study design, sample size estimation, inclusion/exclusion criteria, randomization, blinding, outcome measures, statistical methods, and detailed information on experimental animals and procedures [100].
4. How can I make a complex flowchart or experimental workflow accessible and reproducible? For complex diagrams, provide a text-based alternative alongside the visual [101]. This can be achieved using nested lists with "If X, then go to Y" language for branching decisions or a structured heading format to communicate hierarchy [101]. Ensure the visual diagram itself is a single high-quality image with appropriate alternative text (alt text) that describes the overall relationship and purpose of the chart [101].
5. What is the minimum color contrast required for text in figures for publication? For standard text in figures, the enhanced contrast requirement is a contrast ratio of at least 7:1 between the text and its background [102]. For large-scale text (approximately 18pt or 14pt bold), a minimum contrast ratio of 4.5:1 is required [102].
Troubleshooting Guide: Common Cell Culture Contamination
The table below outlines common contaminants, their characteristics, and detection methods, which is critical for documentation in any reproducibility package.
Table 1: Identification of Common Cell Culture Contaminants
| Contaminant Type | Visual & Microscopic Characteristics | Culture Medium Indicators | Recommended Detection Methods |
|---|---|---|---|
| Bacterial [21] | Black sand-like particles or numerous dots under microscope; altered cell morphology. | Turbidity; color change to yellow/brown; rapid pH drop. | Direct microscopic observation; Gram staining; culture methods. |
| Fungal [21] | Visible filamentous structures (hyphae) or spores. | Color changes; white spots; yellow precipitates. | Direct microscopic observation; culture on antifungal plates. |
| Mycoplasma [21] | Cells may show spreading/filamentous growth; no overt microscopic debris. | Premature yellowing; slow cell growth. | Fluorescence staining (Hoechst 33258); PCR; electron microscopy. |
Experimental Protocols for Authentication and Contamination Detection
Protocol 1: Mycoplasma Detection via Fluorescence Staining
Principle: This method uses a DNA-binding fluorescent dye to detect mycoplasmal DNA, which adheres to the surface of infected cells, creating a characteristic particulate or filamentous pattern of fluorescence outside the cell nucleus [21].
Materials:
- Cell culture sample (test and clean control)
- Hoechst 33258 stain or equivalent
- Fixative (e.g., Methanol:Acetic Acid 3:1)
- Microscope slides and coverslips
- Fluorescence microscope
Method:
- Seed cells onto a sterile coverslip in a culture dish and incubate until 60-70% confluent.
- Rinse cells gently with PBS.
- Fix cells with fixative for 10-15 minutes at room temperature.
- Rinse again with PBS.
- Stain with Hoechst 33258 solution (e.g., 0.5 µg/mL in PBS) for 15-30 minutes in the dark.
- Rinse with PBS to remove excess stain.
- Mount the coverslip on a microscope slide with a mounting medium.
- Observe under a fluorescence microscope with a DAPI filter. A clean culture will show only nuclear fluorescence. A contaminated culture will show a particulate or filamentous pattern of fluorescence in the cytoplasmic and extracellular areas [21].
Protocol 2: Cell Line Authentication using STR Profiling
Principle: Short Tandem Repeat (STR) profiling analyzes highly polymorphic regions of the genome to create a unique genetic fingerprint for a cell line, preventing misidentification and cross-contamination, which are major sources of irreproducible data [5].
Materials:
- Cell pellet (~10^6 cells)
- DNA extraction kit
- STR PCR kit
- Genetic analyzer (capillary electrophoresis)
- STR profiling database (e.g., ATCC, DSMZ)
Method:
- Harvest cells and extract high-quality genomic DNA following the kit protocol.
- Amplify a standardized set of STR loci via PCR using a commercial kit.
- Separate and detect the amplified PCR fragments using capillary electrophoresis.
- Analyze the fragment sizes to generate an allelic profile for your cell line.
- Compare the generated profile against reference profiles in a database such as the one maintained by the International Cell Line Authentication Committee (ICLAC) [5]. A match of ≥80% is typically required for authentication.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Cell Culture and Contamination Management
| Reagent / Material | Function / Purpose | Example Use-Case |
|---|---|---|
| Antibiotic-Antimycotic Mixtures | Prevention and treatment of bacterial and fungal contamination. | Routinely added to culture media for primary neuronal cultures, which are particularly vulnerable [21]. |
| Amphotericin B | Antifungal agent targeting a broad spectrum of yeast and molds. | Used to treat or prevent confirmed fungal contamination [21]. |
| Hoechst 33258 Stain | DNA-binding fluorescent dye for detecting mycoplasma contamination. | Used in the fluorescence staining protocol to identify mycoplasma, a common and cryptic contaminant [21]. |
| Accutase/Accumax | Mild enzymatic cell detachment mixtures. | Passaging sensitive neuronal cell lines while preserving cell surface proteins for subsequent assays like flow cytometry [5]. |
| STR Profiling Kit | Standardized PCR-based kit for cell line authentication. | Periodically confirming the identity of neuronal cell lines (e.g., SH-SY5Y, PC12) to ensure research validity [5]. |
| Mycoplasma Detection PCR Kit | Molecular detection of specific mycoplasma gene sequences. | A highly sensitive and specific method for routine screening of cell cultures for mycoplasma [21]. |
Workflow Diagrams
Experimental Workflow for Ensuring Reproducibility
Contamination Suspectibility and Triage Workflow
Documentation and Peer Review Pathway
Conclusion
Effective management of cell culture contamination is not merely a technical task but a fundamental component of rigorous and reproducible neuroscience research. A proactive, integrated strategy—combining a deep understanding of contaminants, rigorous aseptic technique, advanced detection methods, and systematic validation—is essential to protect the integrity of valuable neuronal models. Adopting these practices safeguards against data invalidation, financial losses, and time-consuming repetitions. Future directions will involve the development of smarter, real-time contamination sensors integrated into incubators, the creation of more specific antibiotics with minimal neurotoxicity, and the establishment of universal authentication standards for stem cell-derived neuronal models. By embracing a culture of quality and vigilance, the neuroscience community can ensure that its foundational in vitro research continues to yield reliable and transformative insights into brain function and disease.
References
- 1. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOopuDUbU0lq9f2vxisJUp8ugdIaymwPhBM54MszC-IwEO0yKcEfF]
- 2. Cell culture and maintenance protocol [https://www.abcam.com/en-us/technical-resources/protocols/cell-culture-and-maintenance-protocol]
- 3. Isolation of Primary Brain Cells: Challenges and Solutions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12320896/]
- 4. Guidelines for preventing and reporting contamination in ... [https://www.nature.com/articles/s41564-025-02035-2]
- 5. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 6. The Simple Ways to Prevent Cell Culture Contamination [https://www.fishersci.com/us/en/science-social-hub/buying-guides/the-simple-ways-prevent-cell-culture-contamination.html]
- 7. How to Troubleshoot Contamination and Browning in Plant ... [https://plantcelltechnology.com/blogs/blog/how-to-troubleshoot-contamination-and-browning-in-plant-cultures?srsltid=AfmBOopuMgEqsIvwh7Lx2dfhwVLk-Do9FU4MDS9L7u7NMCuWGdDnb5MG]
- 8. Detection and Identification of Food-Borne Yeasts [https://www.mdpi.com/2076-2607/13/5/981]
- 9. Biological Contaminants [https://www.fda.gov/animal-veterinary/biological-chemical-and-physical-contaminants-animal-food/biological-contaminants]
- 10. A Decade of Development of Chromogenic Culture Media ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5355637/]
- 11. A Comprehensive Review of Identification Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10492613/]
- 12. | ATCC Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 13. Prevention, Diagnosis and Eradication of Mycoplasma ... Contamination [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668599/]
- 14. Cell Culture Contamination: 5 Common Sources and How ... [https://www.capricorn-scientific.com/knowledge-center/cell-culture-contamination]
- 15. Optimized Protocols for the Isolation and Culture of Primary ... [https://www.integrmed.org/journal/view.php?number=64]
- 16. Viral contamination in cell culture: analyzing the impact of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1442321/full]
- 17. Troubleshooting Cell Culture Contamination: A Practical ... [https://www.yeasenbio.com/blogs/cell/troubleshooting-cell-culture-contamination-a-practical-solution-guide]
- 18. Detecting and Managing Mycoplasma and Nanobacteria... [https://www.linkedin.com/pulse/detecting-managing-mycoplasma-nanobacteria-contamination-pricella-x6o1e]
- 19. Endotoxin Contamination in Nanomaterials Leads to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5420554/]
- 20. Mini review Safety assessment of endotoxin related to drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0378427425015735]
- 21. Troubleshooting Cell Culture Contamination [https://www.creative-bioarray.com/support/troubleshooting-cell-culture-contamination-a-comprehensive-guide.htm]
- 22. A new chapter in Quality Control – how USP Chapter <86 ... [https://www.biomerieux.com/us/en/blog/pharmaceutical-qc/new-chapter-Quality-Control-how-USP-Chapter-86-transform-approaches-endotoxin-testing.html]
- 23. Validating Recombinant Endotoxin Reagents [https://www.pda.org/pda-letter-portal/home/full-article/validating-recombinant-endotoxin-reagents]
- 24. High-content screening of neuronal toxicity using iPSC- ... [https://www.moleculardevices.com/en/assets/app-note/dd/img/high-content-screening-of-neuronal-toxicity-using-ipsc-derived-human-neurons]
- 25. Neuron-based high-content assay and screen for CNS active ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6949038/]
- 26. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://www.mdpi.com/2073-4409/12/5/682]
- 27. Cell Culture Contamination: Experts on How to Minimize ... [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/how-to-minimize-contamination-risk-and-protect-your-cultures.html]
- 28. Prevention of Contaminations in Cell Culture [https://ibidi.com/content/436-prevention-of-contaminations]
- 29. Novel method detects microbial contamination in cell cultures [https://news.mit.edu/2025/novel-method-detects-microbial-contamination-smart-0425]
- 30. The Role of the Biosafety Cabinet in Preventing Infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823295/]
- 31. Laminar Flow Hoods for Cell | Thermo Fisher Scientific - US Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-equipment/laminar-flow-hood.html]
- 32. Aseptic Laboratory Techniques and Safety in Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 33. and Avoiding Preventing Cell Culture Contamination [https://www.technologynetworks.com/cell-science/how-to-guides/preventing-and-avoiding-cell-culture-contamination-299231]
- 34. How to use a biosafety cabinet - Integra Biosciences [https://www.integra-biosciences.com/united-states/en/blog/article/how-use-biosafety-cabinet]
- 35. Biosafety Cabinets: Protection in Biological Labs [https://aspr.hhs.gov/S3/Pages/Biosafety-Cabinets.aspx]
- 36. Cleanroom Gowning Procedures & Garment Standards [https://encompasscleanrooms.com/blog/cleanroom-gowning-procedures-garment-standards]
- 37. Cleanroom Cleaning and Gowning Protocol Guide [https://blog.gotopac.com/2018/01/26/cleanroom-cleaning-procedure-contamination-control-iso-14644-1-protocol/]
- 38. Cleanroom Protocol: Gown Room Procedures [https://www.valutek.com/case-studies/gown-room-procedures]
- 39. Biosafety Cabinet Maintenance: How To Replace Your Filters [https://www.tion.co.uk/education/biosafety-cabinets-how-to-replace-your-filters/]
- 40. Phase Contrast Microscopy - an overview [https://www.sciencedirect.com/topics/computer-science/phase-contrast-microscopy]
- 41. Mammalian Cell Culture Basics Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/mammalian-cell-culture-basics-support/mammalian-cell-culture-basics-support-troubleshooting.html]
- 42. Using Cultured Mammalian Neurons to Study Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4917344/]
- 43. Early automated detection system for skin cancer diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11056372/]
- 44. Isolation and culture of functional adult human neurons from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7660143/]
- 45. Mycoplasma Detection in Cell Cultures [https://www.rapidmicrobiology.com/test-method/rapid-detection-of-mycoplasmas]
- 46. 细胞培养污染故障排除 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOorKNmK91rr_19eTQiJUgXpHm5voFHtbincidzAz5yL39ZIYWyUw]
- 47. How to Deal with Mycoplasma Contamination in Cell Culture [https://www.creative-biogene.com/blog/how-to-deal-with-mycoplasma-contamination-in-cell-culture]
- 48. Development of New PCR Assay with SYBR Green I for ... [https://www.mdpi.com/2075-4418/11/5/876]
- 49. A new method for detecting mycoplasma in cell cultures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270630/]
- 50. 实验技术(八):常见细胞污染及解决策略 [https://www.muhn.edu.cn/ecmd/info/1481/15455.htm]
- 51. 实时荧光定量PCR原理及基础知识 - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/essentials-real-time-pcr.html]
- 52. RT-PCR / RT-qPCR故障排除指南 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/genomics/pcr/troubleshooting?srsltid=AfmBOop07jTlPyzrLax4wKsGHfjONfzwGZL-DptrurnT65-j33Spu8vL]
- 53. 终点法PCR及PCR引物支持– 故障排除 - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/technical-resources/technical-reference-library/pcr-cdna-synthesis-support-center/end-point-pcr-primers-support/end-point-pcr-primers-support-troubleshooting.html]
- 54. 细胞培养常见问题_细胞污染原因_解决方法 [https://www.detaibio.com/topics/cell-culture-faq.html]
- 55. Mycoplasma Contamination in Cell Culture | Detection & ... [https://www.capricorn-scientific.com/knowledge-center/mycoplasma-contamination-cell-culture]
- 56. Prevention and Detection of Mycoplasma Contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584481/]
- 57. Mycoplasma Contamination: Where Does It Come From ... [https://blog.addgene.org/mycoplasma-contamination-where-does-it-come-from-and-how-to-prevent-it]
- 58. Simple, specific, rapid, and pharmacopoeia-compliant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441703/]
- 59. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 60. Your Ultimate Guide to PCR Contamination Troubleshooting [https://www.clyte.tech/post/guide-to-pcr-contamination-troubleshooting?srsltid=AfmBOorPRle5tXJtyWH7anQBndfPHvNDOEAJhMy0gf5KfYTN1G98XcZf]
- 61. Basics of Cell Culture Quality Control: Contamination [https://info.abmgood.com/cell-culture-quality-control-contamination]
- 62. Types of Cell Culture Contamination and How To Prevent ... [https://www.technologynetworks.com/cell-science/articles/types-of-cell-culture-contamination-and-how-to-prevent-them-397776]
- 63. Development of pyrogen-free utensils for cell culture by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182310/]
- 64. The Key to Contamination Prevention in CO₂ Incubators [https://www.thermofisher.com/blog/life-in-the-lab/key-to-contamination-prevention-in-co%E2%82%82-incubators/]
- 65. Cell Culture Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 66. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOoo9Cp3Qvk_ILYXU9PHe2CxLd8H3z-IiD8s3HcGA10L04N7yAWhc]
- 67. Development of a new hazard scoring system in primary ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1308547/full]
- 68. Early prediction of developing spontaneous activity in ... [https://www.nature.com/articles/s41598-021-99538-9]
- 69. Antibiotics and antimycotics in cell culture: how do they ... [https://bitesizebio.com/13679/antibiotics-antimycotics-cell-culture-how-do-they-work-when-to-use-them/]
- 70. Antibiotics and the Nervous System—Which ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8708917/]
- 71. Antimicrobial resistance: Impacts, challenges, and future ... [https://www.sciencedirect.com/science/article/pii/S2949916X24000343]
- 72. Keeping incubators and workstations contamination-free [https://www.oxford-optronix.com/resources/keeping-incubators-and-workstations-contamination-free]
- 73. Understanding Decontamination Cycles in CO2 Incubators [https://aresscientific.com/blog/understanding-decontamination-cycles-co2-incubators/]
- 74. Choosing the Most Effective Decontamination Method for ... [https://www.escolifesciences.com/news/choosing-the-most-effective-decontamination-method-for-your-co2-incubator]
- 75. Contaminant Help [https://unclineberger.org/tissueculture/contaminant/]
- 76. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOooefxBZPo8U-E3kxOWfmiIhn_k7bbRu0O2Ue0ad8lUns8XLfWQ3]
- 77. A new approach to neural cell culture for long-term studies [https://pubmed.ncbi.nlm.nih.gov/11564520/]
- 78. “HeLa Cells 50 Years On: The Good, The Bad, and The Ugly ... [https://embryo.asu.edu/pages/hela-cells-50-years-good-bad-and-ugly-2002-john-r-masters]
- 79. The ghosts of HeLa: How cell line misidentification ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0186281]
- 80. Rapid detection of low‐level HeLa cell contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6307787/]
- 81. Discovery of HeLa Cell Contamination in HES Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4126216/]
- 82. Cell Line Cross-Contamination and Misidentification [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-cell-line-misidentification?srsltid=AfmBOoru9e7rGJAjLszgH8PMs6ZCcH-EuG1x5kbWzlaOczbkWLzZEpM_]
- 83. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 84. Cell line authentication and validation is a key requirement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181071/]
- 85. Cell Line Authentication Resources [https://www.promega.com/resources/guides/cell-biology/cell-line-authentication/]
- 86. Why the Future of Biological Research Requires Cell Line ... [https://www.psomagen.com/blog/future-of-research-requires-cell-line-authentication]
- 87. Cell Line Authentication Methods: Ensuring Research ... [https://cellculturecompany.com/cell-line-authentication-methods-ensuring-research-integrity/]
- 88. Cell Line Authentication [https://www.psomagen.com/cell-line-authentication]
- 89. Journal & NIH funding guidelines - Cell Line Authentication [https://celllineauthentication.labcorp.com/resources/journal-nih-funding-guidelines]
- 90. Misidentified cell lines: failures of peer review, varying journal ... [https://researchintegrityjournal.biomedcentral.com/articles/10.1186/s41073-025-00170-2]
- 91. High-throughput synaptic connectivity mapping using in ... [https://www.nature.com/articles/s41593-025-02024-y]
- 92. A scalable, all-optical method for mapping synaptic ... [https://pubmed.ncbi.nlm.nih.gov/40667305/]
- 93. of Human Comparison with Human iPS Cell- Primary ... Derived [https://pmc.ncbi.nlm.nih.gov/articles/PMC4720696/]
- 94. Isolation, Purification, and Culture of Primary Murine Sensory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5613752/]
- 95. Molecular and functional variation in iPSC-derived sensory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5742539/]
- 96. How to differentiate induced pluripotent stem cells into ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03696-2]
- 97. Appendix 3: Cell Culture Hygiene Practices [https://www.isscr.org/basic-research-standards/appendix-3]
- 98. Preparation and Co‐Culture of iPSC‐Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9285934/]
- 99. Guidelines for Reproducibility [https://apsanet.org/publications/journals/american-political-science-review/guidelines-for-reproducibility/]
- 100. Key Factors for Improving Rigor and Reproducibility [https://pmc.ncbi.nlm.nih.gov/articles/PMC8965503/]
- 101. Key Considerations for Flowchart Accessibility - MN.gov [https://mn.gov/mnit/about-mnit/accessibility/news/?id=38-436349]
- 102. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]