A Comprehensive Guide to Electrophysiology Methods for Measuring Neuronal Activity
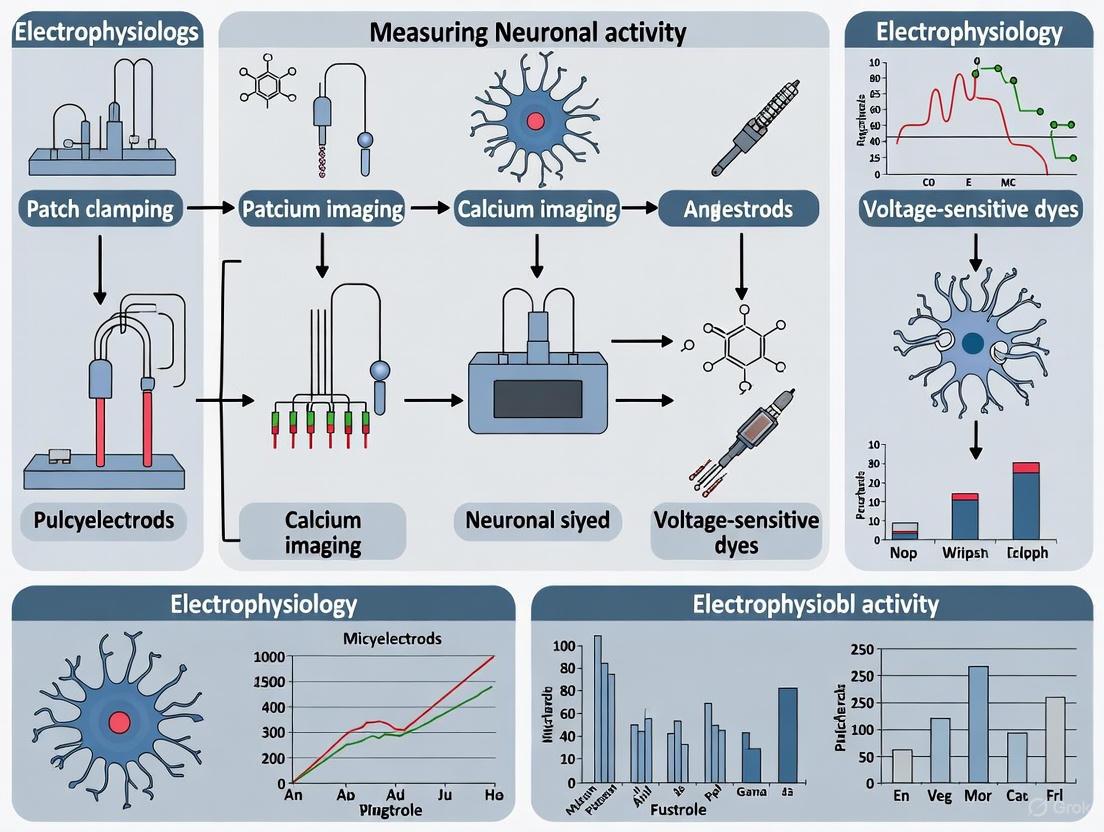
This article provides a comprehensive overview of electrophysiology techniques for measuring neuronal activity, tailored for researchers, scientists, and drug development professionals.
A Comprehensive Guide to Electrophysiology Methods for Measuring Neuronal Activity
Abstract
This article provides a comprehensive overview of electrophysiology techniques for measuring neuronal activity, tailored for researchers, scientists, and drug development professionals. It covers foundational principles, from the basic electrical properties of neurons to the role of ion channels. The guide details core methodologies like patch-clamp recording, microelectrode arrays (MEAs), and voltage/current-clamp, alongside their applications in basic research, drug discovery, and disease modeling. It also offers practical troubleshooting advice for improving experimental outcomes and discusses frameworks for validating results and comparing the strengths of various techniques. By synthesizing traditional methods with recent advancements in automation and high-throughput screening, this resource aims to be an essential reference for designing and executing robust electrophysiology studies.
Understanding the Fundamentals: The Electrical Language of Neurons
Fundamental Concepts of Neuronal Excitability
Neuronal excitability is a fundamental property of neurons, defined as their ability to generate action potentials in response to various stimuli [1]. This capability enables neurons to transmit and process information throughout the nervous system. The excitability of a neuron determines how it responds to synaptic inputs, generates action potentials, and communicates with other neurons [1].
Types of Neuronal Excitability
There are two primary types of neuronal excitability [1]:
- Intrinsic excitability: The ability of a neuron to generate action potentials in the absence of synaptic inputs, determined by its intrinsic membrane properties and ion channel composition.
- Synaptic excitability: The ability of a neuron to generate action potentials in response to synaptic inputs from other neurons.
Ion Channels in Neuronal Excitability
Ion channels play a crucial role in regulating neuronal excitability by controlling ion flow across the neuronal membrane, influencing membrane potential and action potential generation [1]. Their opening and closing are regulated by voltage, ligands, and neuromodulators.
Table: Major Ion Channel Types and Their Functions in Neuronal Excitability
| Ion Channel Type | Function in Neuronal Excitability |
|---|---|
| Voltage-gated sodium channels | Generate and propagate action potentials |
| Voltage-gated potassium channels | Repolarize the membrane after action potentials |
| Voltage-gated calcium channels | Regulate neurotransmitter release |
| Ligand-gated ion channels | Mediate synaptic transmission |
Key Research Reagent Solutions
Essential materials and reagents for studying neuronal excitability include:
Table: Essential Research Reagents for Neuronal Excitability Studies
| Reagent/Material | Function/Application |
|---|---|
| Acute brain slice preparation solutions | Maintain neuronal viability during slice preparation and recording [2] |
| Whole-cell patch clamp solutions | Intracellular and extracellular solutions for patch clamp recordings [2] |
| Enzymes for tissue dissociation (e.g., proteases) | Dissociate neuronal tissue for single-cell recordings |
| Ion channel modulators (agonists/antagonists) | Investigate specific ion channel contributions to excitability |
| Fluorescent indicators (e.g., voltage-sensitive dyes) | Visualize neuronal activity and membrane potential changes |
| Mechanosensitive compounds | Study mechanosensitive properties in chordotonal neurons [3] |
Electrophysiology Protocols for Assessing Neuronal Excitability
Acute Brain Slice Preparation for Electrophysiology
This protocol describes preparing live brain slices for extracellular and intracellular electrophysiology recordings [2].
Materials:
- Artificial cerebrospinal fluid (ACSF)
- Sucrose-based cutting solution
- Vibratome or tissue slicer
- Oxygenation system (95% O₂, 5% CO₂)
- Recording chamber with temperature control
Procedure:
- Rapidly extract brain tissue following approved institutional guidelines.
- Dissect region of interest and glue to vibratome stage.
- Prepare 300-400 μm thick slices in ice-cold, oxygenated cutting solution.
- Incubate slices in oxygenated ACSF at 32-34°C for 30 minutes.
- Maintain slices at room temperature for at least 1 hour before recording.
- Transfer individual slices to recording chamber perfused with oxygenated ACSF at 28-32°C.
Whole-Cell Patch Clamp Recording of Pyramidal Neurons
This protocol enables assessment of neuronal excitability and synaptic function in identified cell types [2].
Materials:
- Patch pipettes (3-6 MΩ resistance)
- Intracellular pipette solution
- Oxygenated extracellular solution
- Vibration isolation table
- Faraday cage
- Amplifier with data acquisition system
Procedure:
- Pull borosilicate glass capillaries to appropriate tip diameter.
- Fill pipettes with filtered intracellular solution.
- Position pipette near target neuron using micromanipulators.
- Apply gentle positive pressure while advancing pipette.
- Form gigaseal (>1 GΩ) by applying gentle suction.
- Compensate pipette capacitance and rupture membrane with additional suction or voltage pulses.
- Record in current-clamp or voltage-clamp mode based on experimental needs.
- For excitability assessment, inject current steps (e.g., -100 to +300 pA in 10-20 pA increments).
- Analyze resting membrane potential, input resistance, and action potential properties.
Extracellular Recording of Compound Action Potentials (CAPs)
This protocol measures synchronized electrical activity from multiple neurons [2].
Materials:
- Extracellular recording electrodes
- Stimulating electrodes
- Oxygenated extracellular solution
- Data acquisition system with stimulator
Procedure:
- Position stimulating and recording electrodes in region of interest.
- Deliver electrical stimuli of varying intensities (0.1-10 mA, 0.1-1 ms duration).
- Record evoked responses at 10-50 kHz sampling rate.
- Analyze CAP amplitude, latency, and conduction velocity.
- For long-term potentiation studies, apply high-frequency stimulation (e.g., 100 Hz for 1 second).
Extracellular Recordings of Mechanically Stimulated Neurons
This protocol, adapted from Drosophila studies, records neuronal activity from mechanically stimulated sensory neurons [3].
Materials:
- Dissection tools for fine tissue preparation
- Extracellular recording setup for small specimens
- Mechanical stimulation apparatus
- Vibration damping system
Procedure:
- Dissect larvae in appropriate physiological solution.
- Identify and access pentascolopidial chordotonal organs (lch5).
- Position recording electrode on lch5 neurons.
- Apply controlled mechanical stimulation while recording.
- Quantify action currents and response properties.
Emerging Technologies and Future Directions
Quantum Computing in Neural Excitability Modeling
Emerging approaches are exploring quantum computing to model ion channels and action potentials, leveraging the inherently quantum mechanical properties of ion movement at atomic scales [4]. Quantum algorithms show potential for revolutionizing simulations of ion channel behavior and neuronal signaling, though practical challenges including qubit coherence, error rates, and hardware scalability remain [4].
The BRAIN Initiative and Neural Circuit Analysis
Large-scale initiatives are prioritizing the analysis of neural circuits, requiring identification and characterization of component cells, definition of synaptic connections, observation of dynamic activity patterns during behavior, and perturbation testing [5]. This integrated approach spans spatial and temporal scales to understand how dynamic neural activity patterns transform into cognition, emotion, perception, and action [5].
Experimental Workflows and Signaling Pathways
The Critical Role of Ion Channels in Regulating Neuronal Activity
Ion channels are transmembrane protein pores that facilitate the selective flow of ions such as sodium (Na⁺), potassium (K⁺), calcium (Ca²⁺), and chloride (Cl⁻) across cellular membranes [6]. These channels are fundamental to electrical signaling throughout the nervous system, controlling processes ranging from fundamental neuronal communication to complex cognitive functions. In recent years, advanced techniques including single-cell transcriptomics, biophysical modeling, and high-throughput screening have dramatically enhanced our understanding of how diverse ion channel genes dictate neuronal physiology and enable the rich diversity of neuronal behaviors observed in the brain [7] [8]. This document provides detailed application notes and experimental protocols for studying ion channel function within the context of modern electrophysiology research, with particular emphasis on bridging molecular genetics with physiological outcomes.
Ion Channel Diversity and Neuronal Excitability
The brain contains an extraordinary diversity of neuronal cell types, each exhibiting distinct genetic signatures and functional properties [7]. This physiological diversity stems largely from the specific composition and density of ion channels expressed in the neuronal membrane. Voltage-gated ion channels (VGICs), including those for Na⁺, K⁺, and Ca²⁺, are critical regulators of membrane potential and cellular excitability, making them important drug targets for neurological, cardiovascular, and immunological diseases [9].
Table 1: Major Voltage-Gated Ion Channel Families and Their Neuronal Functions
| Ion Channel Family | Primary Ions | Activation Mechanism | Key Physiological Roles in Neurons | Associated Channelopathies |
|---|---|---|---|---|
| Voltage-Gated Sodium (Naᵥ) Channels | Na⁺ | Voltage-dependent | Action potential initiation and propagation | Epilepsy, chronic pain, neuropathies |
| Voltage-Gated Potassium (Kᵥ) Channels | K⁺ | Voltage-dependent | Action potential repolarization, firing frequency modulation | Episodic ataxia, epilepsy |
| Voltage-Gated Calcium (Caᵥ) Channels | Ca²⁺ | Voltage-dependent | Neurotransmitter release, synaptic plasticity, gene expression | Migraine, cerebellar ataxia |
| Transient Receptor Potential (TRP) Channels | Na⁺, K⁺, Ca²⁺ | Multiple (chemical, thermal, mechanical) | Pain sensation, sensory transduction, cellular signaling | Neurodegeneration, pain disorders |
Different neuronal cell types express characteristic combinations of these channels, which shape their distinctive firing patterns. For example, fast-spiking parvalbumin (Pvalb)-positive interneurons exhibit high densities of certain potassium channels (specifically, a high maximal conductance of the delayed rectifier K⁺ current, gKd), which enables their rapid spiking capability and supports high-frequency signaling in neuronal networks [8]. In contrast, pyramidal neurons display different ionic conductances that result in broader action potentials and lower maximum firing rates. Understanding these relationships is crucial for deciphering the functional building blocks of neural circuits.
Experimental Protocols for Ion Channel and Neuronal Characterization
Protocol 1: Patch-seq for Multimodal Neuronal Profiling
The Patch-seq technique allows for the integration of electrophysiological recordings, single-cell RNA sequencing (scRNA-seq), and morphological reconstruction from the same individual neuron [8]. This protocol enables the direct investigation of how a neuron's gene expression relates to its functional and structural properties.
Workflow Diagram for Patch-seq Analysis:
Detailed Methodology:
- Tissue Preparation: Prepare acute brain slices (300-350 μm thickness) from the region of interest (e.g., mouse motor cortex) using a vibrating tissue slicer. Maintain slices in oxygenated (95% O₂/5% CO₂) artificial cerebrospinal fluid (aCSF) at approximately 30°C for 1-5 hours before recording [8] [10].
- Electrophysiological Recording: Transfer a slice to the recording chamber and identify neurons using differential interference contrast (DIC) optics. Perform whole-cell patch-clamp recordings using pipettes with a resistance of 2.5-4 MΩ.
- Intracellular Solution (example): potassium gluconate (130 mM), KCl (10 mM), HEPES (10 mM), MgATP (4 mM), NaGTP (0.3 mM), phosphocreatine (10 mM) [10].
- Record neuronal responses to a series of current injections to characterize intrinsic excitability, including action potential properties and firing patterns.
- Cellular Content Harvesting: Upon completion of electrophysiological recording, gently aspirate the cytoplasmic content into the patch pipette by applying negative pressure. Expel the contents into a collection tube for subsequent RNA sequencing [8].
- Library Preparation and Sequencing: Convert the harvested RNA into a sequencing library using a single-cell RNA-seq platform (e.g., SMART-seq2 for higher sensitivity). Sequence the libraries to obtain full-transcriptome data from the recorded cell.
- Data Analysis and Integration:
- Electrophysiology Analysis: Calculate standard electrophysiological features (e.g., resting membrane potential, input resistance, spike amplitude, adaptation index) from the recorded traces.
- Transcriptomics Analysis: Process sequencing data to quantify gene expression levels, focusing on ion channel genes and neuronal markers.
- Multimodal Integration: Use statistical models, such as sparse reduced-rank regression (sRRR), to identify correlations between the expression levels of specific ion channel genes and the electrophysiological properties of the neuron [7] [8].
Protocol 2: Recursive Piecewise Data Assimilation (RPDA) for Ionic Current Estimation
Recursive Piecewise Data Assimilation (RPDA) is a computational method that infers the underlying ionic current waveforms and channel properties from current-clamp recordings [10]. Its strength lies in its ability to simultaneously estimate all major ionic currents in a neuron from a small set of high-quality electrophysiological data.
Workflow Diagram for RPDA Analysis:
Detailed Methodology:
Informative Stimulation Protocol Design:
- A key prerequisite for RPDA is using a current stimulation protocol that is sufficiently informative to constrain all model parameters [10].
- The protocol should probe neuron dynamics across different states: depolarized (eliciting action potentials), sub-threshold (near resting potential), and hyperpolarized.
- Incorporate a mix of positive/negative current pulses and complex oscillations (e.g., chaotic signals from the Lorenz system) to cover a wide range of time constants (e.g., 0.1 ms to 500 ms) relevant to neuronal ion channels [10].
- Example: A protocol combining square pulses with a chaotic signal generated by the Lorenz system (σ=10, β=8/3, ρ=28) [10].
Electrophysiological Recording:
- Perform whole-cell current-clamp recordings as described in Protocol 3.1, using the optimized stimulation protocol.
- Synaptic transmission should be pharmacologically inhibited (e.g., using kynurenate, picrotoxin, and strychnine) to isolate intrinsic neuronal properties [10].
Data Assimilation and Parameter Estimation:
- The voltage time series data (
V(t)) is assimilated into a Hodgkin-Huxley-type model of the neuron. - The RPDA algorithm works by recursively synchronizing the model equations to the observed voltage trace over short, sequential time windows.
- It adjusts model parameters (ionic conductances, activation thresholds, gate time constants) to minimize the difference between the model output and the experimental data.
- This process yields estimates of the unobserved state variables, including the gating parameters and the time-course of individual ionic currents (e.g., sodium, potassium, calcium) [10].
- The voltage time series data (
Validation and Application:
- The method can be experimentally validated by applying known ion channel blockers and confirming that RPDA correctly identifies the change in the targeted current.
- RPDA can quantify compensatory changes in non-targeted ion channels, demonstrating its utility as a drug toxicity counter-screen [10].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Tools for Neuronal Ion Channel Research
| Tool / Reagent | Category | Primary Function | Example Application |
|---|---|---|---|
| Patch-seq Platform | Integrated Methodology | Concurrently profiles transcriptome and physiology from single neurons | Linking ion channel gene expression to electrophysiological phenotypes [8] |
| Automated Patch Clamp (APC) | Instrumentation | High-throughput electrophysiology screening | Drug discovery campaigns on recombinant ion channels (e.g., hNaV1.7) [11] |
| Planar Lipid Bilayer System | Instrumentation | Functional characterization of purified ion channels in a defined membrane environment | Studying gating and permeation properties unbiased by cellular components [12] |
| Protein Language Models (e.g., ESM-2) | Computational Tool | Predicts functional effects of missense variants on ion channel function | Classifying variants as gain-of-function (GOF) or loss-of-function (LOF) [13] |
| Fluorescent Indicators (e.g., from ION Biosciences) | Chemical Reagent | Optical measurement of ion dynamics and membrane potential | High-throughput assay development and screening services [14] |
| Cryo-Electron Microscopy (Cryo-EM) | Structural Tool | High-resolution structure determination of ion channels in near-native states | Investigating ion channel regulation by lipids and chaperones [6] |
Data Analysis and Interpretation
Linking Gene Expression to Biophysical Parameters
Advanced computational approaches are required to move beyond correlations and establish mechanistic links between transcriptomic data and electrophysiological properties. One powerful method involves using conductance-based models as an intermediate layer [7] [8].
- Procedure: First, fit a Hodgkin-Huxley (HH)-based model with interpretable parameters (e.g., maximal ionic conductances) to the electrophysiological recording of a neuron. Then, use a statistical model (e.g., sparse linear regression or a neural network) to predict these best-fitting HH-model parameters from the cell's gene expression profile [7] [8].
- Outcome: This creates an interpretable, two-step mapping from genes to function. For example, this approach has revealed mechanistically plausible links, such as the association of the
Kcnc1gene with potassium channel conductance (gKv3.1) and theCacna2d1gene with calcium channel conductance [8].
Functional Prediction of Genetic Variants
Accurately classifying the functional impact of ion channel variants is critical for diagnosing channelopathies. Protein language models (pLMs) like Evolutionary Scale Modeling (ESM) offer a significant advance.
- Procedure: The "MissION" classifier uses pLM embeddings (latent representations of amino acid sequences) to predict whether a missense variant will cause GOF or LOF [13].
- Implementation: The model is trained on thousands of variants with known functional consequences. It processes the sequence embedding of the variant, cropped to a window around the substitution site, through a neural network classifier [13].
- Performance: This approach achieves high predictive performance (ROC-AUC: 0.925), generalizing well even to ion channel genes with little available experimental data [13].
Ion channels are the fundamental regulators of neuronal excitability, and modern research tools now allow us to dissect their roles with unprecedented precision. The integration of advanced electrophysiology, single-cell genomics, and sophisticated computational models is bridging the long-standing gap between neuronal gene expression and physiological function. The protocols and applications detailed here—from the multimodal Patch-seq and powerful RPDA analysis to the predictive power of protein language models—provide a roadmap for researchers to deepen the mechanistic understanding of neuronal diversity, disease-associated channelopathies, and accelerate the development of targeted therapeutics for neurological disorders.
Electrophysiology provides the foundational framework for understanding neuronal excitability and communication. The core principles of resting membrane potential, action potentials, and synaptic transmission form the essential trilogy that enables the nervous system to process and transmit information. For researchers measuring neuronal activity, a precise understanding of these concepts is paramount for designing experiments, interpreting data, and developing novel therapeutic agents. These electrical events are not merely isolated phenomena but are intricately linked processes that convert chemical gradients into electrical signals and back into chemical messengers, allowing for the complex computation that underpins all nervous system function [15] [16] [17].
This article details these core concepts with a specific focus on their relevance to experimental protocols in neuronal research. We synthesize classic physiological understanding with contemporary research findings, such as a recent study revealing the role of extracellular phosphorylation in synaptic plasticity, thereby updating the textbook model of synaptic function [18].
Resting Membrane Potential: The Foundation of Excitability
The resting membrane potential (RMP) is the stable, electrical potential difference across the plasma membrane of a non-excited cell, typically measured at -70 mV in neurons relative to the extracellular environment. This negative interior is the baseline from which all electrical activity arises [16] [19].
Biophysical Basis and Ion Dynamics
The RMP is generated and maintained by the interplay of ionic concentration gradients and selective membrane permeability. The key ions involved are potassium (K+), sodium (Na+), and chloride (Cl-), alongside impermeant intracellular anions (e.g., proteins) [20].
Table 1: Ionic Concentrations and Equilibrium Potentials in a Typical Mammalian Neuron
| Ion | Intracellular Concentration | Extracellular Concentration | Equilibrium Potential (Eion) | Primary Role in RMP |
|---|---|---|---|---|
| Potassium (K+) | 120-130 mM | 4-5 mM | -90 mV | Dominant influence; high permeability at rest pulls potential toward EK |
| Sodium (Na+) | 14-15 mM | 140-145 mM | +60 to +65 mV | Minor influence; low permeability at rest slightly depolarizes the cell |
| Chloride (Cl-) | 5-10 mM | 110-120 mM | -65 to -70 mV | Stabilizes potential near rest; permeability varies by cell type |
The Nernst equation is used to calculate the equilibrium potential for a single ion, the point at which its concentration gradient is exactly balanced by the electrical gradient [16] [20]:
E_ion = (RT/zF) * ln([ion]_outside / [ion]_inside)
Where R is the gas constant, T is temperature, z is the ion's valence, and F is Faraday's constant. At body temperature (37°C) for a monovalent cation, this simplifies to E_ion ≈ 61.5 * log([out]/[in]).
Since the membrane is permeable to multiple ions simultaneously, the Goldman-Hodgkin-Katz (GHK) voltage equation provides a more accurate prediction of the RMP by incorporating the relative permeabilities (P) of the major ions [16] [19]:
V_m = (RT/F) * ln( (P_K[K+]_out + P_Na[Na+]_out + P_Cl[Cl-]_in) / (P_K[K+]_in + P_Na[Na+]_in + P_Cl[Cl-]_out) )
Because the membrane at rest is approximately 20-100 times more permeable to K+ than to Na+, the RMP is close to, but slightly more positive than, EK [19].
The Role of the Sodium-Potassium Pump
The Na+/K+ ATPase pump is critical for maintaining the long-term stability of the RMP. This electrogenic pump actively transports 3 Na+ ions out of the cell and 2 K+ ions in for every molecule of ATP hydrolyzed, thereby directly contributing a small hyperpolarizing current and, more importantly, constantly maintaining the concentration gradients that K+ leaks down [16] [20] [19].
Diagram 1: Ion dynamics generating the resting membrane potential.
Action Potential: The Electrical Signal
An action potential (AP) is a rapid, all-or-nothing, self-regenerating wave of depolarization that travels along the axon, serving as the fundamental unit of neuronal communication [15] [21]. Its stereotypical shape is consistent within a given cell type but can vary in duration between cell types, from less than a millisecond in fast-spiking neurons to over 100 milliseconds in cells dominated by voltage-gated calcium channels [15].
Phases and Ion Channels
The initiation and propagation of an AP can be dissected into distinct phases driven by the sequential activation and inactivation of voltage-gated ion channels.
Table 2: Phases of the Neuronal Action Potential and Underlying Mechanisms
| Phase | Membrane Potential | Key Permeability Change | Ionic Flow | Governing Mechanism |
|---|---|---|---|---|
| 1. Resting State | -70 mV | PK+ >> PNa+ | K+ leak outward > Na+ leak inward | Membrane at RMP; voltage-gated Na+ and K+ channels closed. |
| 2. Depolarization to Threshold | Rising to ~ -55 mV | Stimulus-gated or synaptic Na+ channels open. | Net inward Na+ current. | Sufficient depolarization opens enough voltage-gated Na+ channels to reach the threshold for positive feedback. |
| 3. Rapid Depolarization (Rising Phase) | Rapid rise to +30 to +40 mV | P_Na+ increases dramatically. | Massive, rapid Na+ influx. | Voltage-gated Na+ channels activate (open) rapidly, driving Vm toward ENa. |
| 4. Repolarization (Falling Phase) | Falls back toward RMP | PNa+ inactivates; PK+ increases. | Na+ influx stops; K+ efflux increases. | Na+ channels inactivate; delayed voltage-gated K+ channels open, driving Vm back toward EK. |
| 5. After-Hyperpolarization | Briefly more negative than RMP (e.g., -80 mV) | P_K+ remains elevated. | Continued K+ efflux. | Delayed K+ channels close slowly; Na+ channels reset from inactivation. |
| 6. Refractory Period | Returns to RMP | P_Na+ is inactivated. | Ionic gradients restored by pumps. | Absolute refractory period: No new AP can be initiated. Relative refractory period: A stronger-than-normal stimulus is required. |
The Hodgkin-Huxley Model and All-or-Nothing Principle
The biophysical properties of the AP are classically described by the Hodgkin-Huxley model, a set of differential equations that quantify the conductance changes of voltage-gated Na+ and K+ channels [15]. A critical feature of the AP is its all-or-nothing nature. Once the membrane potential at the axon initial segment reaches the threshold (typically -55 mV), the positive feedback cycle of Na+ channel activation proceeds explosively and independently of the initial stimulus strength [21]. This ensures the faithful, non-decremental propagation of the signal along the axon.
Propagation and Saltatory Conduction
APs propagate along the axon because the depolarizing current from the active region depolarizes adjacent membrane segments to threshold. In myelinated axons, the process of saltatory conduction significantly increases speed and metabolic efficiency. The myelin sheath, formed by oligodendrocytes or Schwann cells, insulates the axon. APs actively regenerate only at the unmyelinated Nodes of Ranvier, "jumping" from node to node [21].
Diagram 2: Action potential initiation decision tree.
Synaptic Transmission: Bridging the Gap
Synaptic transmission is the process by which an AP in a presynaptic neuron is converted into an electrical or biochemical signal in a postsynaptic cell. This occurs at specialized junctions called synapses, most commonly via the release of chemical neurotransmitters [17].
The Synaptic Vesicle Cycle
The core mechanism of neurotransmitter release is the Ca2+-dependent synaptic vesicle cycle [17] [22]:
- Docking and Priming: Synaptic vesicles loaded with neurotransmitter are docked at the presynaptic active zone and molecularly "primed" for release by proteins including SNARE complexes (syntaxin-1, SNAP-25, synaptobrevin-2) and Munc13 [17] [22].
- Calcium Influx and Fusion: An arriving AP depolarizes the presynaptic terminal, opening voltage-gated calcium channels (VGCCs). The rapid influx of Ca2+ triggers a conformational change in the calcium sensor protein synaptotagmin, leading to the fusion of the vesicle membrane with the presynaptic membrane and exocytosis of neurotransmitter into the synaptic cleft.
- Recycling: The vesicle membrane is retrieved via endocytosis and refilled with neurotransmitter for future rounds of release.
Postsynaptic Receptors and Potentials
Released neurotransmitters bind to ligand-gated ion channels (ionotropic receptors) or G-protein coupled receptors (metabotropic receptors) on the postsynaptic membrane.
- Ionotropic Receptors mediate fast synaptic transmission. For example, glutamate binding to AMPA-type receptors opens cation channels, leading to Na+ influx and excitatory postsynaptic potentials (EPSPs), which depolarize the neuron. Conversely, GABA binding to GABAA receptors opens Cl- channels, leading to inhibitory postsynaptic potentials (IPSPs), which hyperpolarize or shunt excitation [17].
- Metabotropic Receptors act through second messenger systems to produce slower, longer-lasting, and more modulatory effects on neuronal excitability and synaptic strength [17].
Emerging Mechanism: Extracellular Phosphorylation in Synaptic Plasticity
Recent research has unveiled a novel layer of regulation in synaptic transmission: extracellular phosphorylation within the synaptic cleft. A 2025 study identified that the ectokinase Vertebrate Lonesome Kinase (VLK) is secreted by presynaptic neurons following injury [18]. VLK then phosphorylates the extracellular domain of Ephrin type-B receptor 2 (EphB2) on the postsynaptic membrane. This phosphorylation event promotes the clustering of NMDA receptors with EphB2 receptors, a key mechanism for strengthening synaptic connections and mediating injury-induced pain hypersensitivity [18]. This discovery updates the traditional model of the synapse by showing that kinase activity within the cleft itself is a critical regulator of receptor function and synaptic plasticity.
Diagram 3: Synaptic transmission with the novel VLK pathway.
Experimental Protocols for Electrophysiological Investigation
Protocol: Extracellular Recording of Mechanically Stimulated Neurons
This protocol, adapted from recent methodology, is designed for recording action currents (the extracellular correlate of APs) from sensory neurons in Drosophila larvae, useful for studying mechanotransduction [3].
Application: Investigating the molecular mechanisms of mechanosensation, auditory transduction, and the function of specific ion channels in a genetically tractable model system.
Key Steps:
- Dissection: Isolate the intact nervous system of the Drosophila larva in a physiological saline solution to maintain tissue viability.
- Stimulation and Recording: Position an extracellular recording electrode (e.g., sharp glass microelectrode or suction electrode) near the cell body or axon of the target chordotonal neuron (lch5). Apply controlled mechanical stretch to the neuron using a micromanipulator.
- Signal Acquisition: Record the resulting electrical activity (action currents) using a standard extracellular amplifier. Signals are typically band-pass filtered (e.g., 300 Hz to 3 kHz) to isolate spiking activity.
- Data Analysis: Quantify neuronal activity by measuring parameters such as firing rate, latency to first spike, and spike adaptation in response to the mechanical stimulus. Compare these metrics across genetic manipulations or pharmacological treatments.
Protocol: Investigating Synaptic Plasticity via the VLK Pathway
Based on the recent discovery of VLK's role [18], this protocol outlines a methodology to probe this novel signaling pathway in a pain research context.
Application: Elucidating mechanisms of synaptic strengthening in pain pathways, learning, and memory; screening for potential analgesic drugs targeting VLK or EphB2.
Key Steps:
- Preparation: Utilize ex vivo spinal cord slices or primary cultures of sensory neurons co-cultured with spinal cord neurons. Alternatively, use human sensory neuron cultures for translational impact.
- Genetic/Pharmacological Manipulation:
- Knockdown/Knockout: Use transgenic mice or viral vectors to delete or silence the Vlk gene specifically in sensory neurons.
- Inhibition: Apply a selective VLK inhibitor to the synaptic preparation.
- Activation: Apply recombinant VLK protein to normal tissue.
- Stimulation and Measurement:
- Induce synaptic plasticity using electrical stimulation protocols (e.g., high-frequency stimulation) or chemical LTP induction.
- Measure postsynaptic potentials using whole-cell patch-clamp electrophysiology in the postsynaptic neuron.
- Quantify NMDA receptor clustering via immunohistochemistry (e.g., anti-NMDAR and anti-EphB2 antibodies) and super-resolution microscopy.
- Behavioral Correlation (in vivo): In parallel mouse experiments, assess pain hypersensitivity (e.g., using von Frey filaments for mechanical allodynia) following injury in control vs. VLK-deficient animals.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Electrophysiology and Synaptic Research
| Reagent / Tool | Function / Application | Specific Examples / Notes |
|---|---|---|
| Patch-Clamp Amplifiers (Axon Instruments) | High-fidelity recording of transmembrane currents (whole-cell, single-channel) and membrane potential. | Essential for quantifying AP properties, postsynaptic currents, and ion channel kinetics. [23] |
| Tetrodotoxin (TTX) | Selective blocker of voltage-gated sodium channels. | Used to isolate Na+ current contributions or silence neuronal firing. |
| Tetraethylammonium (TEA) | Broad-spectrum blocker of voltage-gated potassium channels. | Used to isolate K+ current contributions and prolong the AP duration. |
| Selective Kinase Inhibitors | Pharmacological disruption of specific signaling pathways. | Emerging tools for novel targets like VLK inhibitors to probe synaptic plasticity and pain mechanisms. [18] |
| Recombinant Proteins (e.g., VLK) | To directly activate or supplement a specific pathway. | Application of recombinant VLK is sufficient to induce pain hypersensitivity and NMDA receptor clustering in studies. [18] |
| SNARE Complex Modifiers (e.g., Botulinum Toxin) | Proteolytic cleavage of SNARE proteins to inhibit vesicle fusion. | Used to dissect the fundamental mechanisms of neurotransmitter release. [17] |
| Agonists/Antagonists for Neurotransmitter Receptors (e.g., CNQX, AP5, Bicuculline) | To selectively activate or block specific ionotropic or metabotropic receptors. | Critical for determining the receptor subtypes mediating synaptic responses. [17] |
| Caged Compounds (e.g., Caged Glutamate, Caged Ca2+) | Precursors of bioactive molecules that are activated by UV light. | Allows for precise spatial and temporal control of neurotransmitter application or intracellular signaling. |
Electrophysiology is the field of research studying current or voltage changes across a cell membrane, and it is a fundamental tool for investigating neuronal activity [24]. Neurons communicate via action potentials—rapid electrical signals that travel along axons and trigger the release of neurotransmitters across synapses [25]. When neurotransmitters bind to receptors, they enable the flow of ions (such as Na+ or K+) across membrane channels, changing the neuron's membrane potential [25]. Measuring these minute electrical signals requires a suite of highly specialized equipment capable of extreme precision, low noise, and stable mechanical operation. The core instruments of any electrophysiology lab include microscopes for visualization, amplifiers for signal detection, micropipette pullers for electrode fabrication, and Faraday cages for noise shielding [24]. This application note details the function, key specifications, and experimental protocols for these essential tools, providing a framework for reliable measurement of neuronal activity in research and drug development.
The Core Electrophysiology Setup
An electrophysiology setup is an integrated system where each component plays a critical role in obtaining high-quality measurements of neuronal function. The four main laboratory requirements are: (1) a controlled Environment to keep the biological preparation healthy; (2) Optics for visualizing the preparation; (3) Mechanics for stably positioning the microelectrode; and (4) Electronics for amplifying and recording the signal [24]. A standard rig consists of a microscope with a micromanipulator, an amplifier, a digitizer, and a computer with acquisition software, all housed on an anti-vibration table within a Faraday cage to shield from external interference [24]. The following sections break down the key components in detail.
Detailed Equipment Analysis
Table 1: Key Equipment for Neuronal Electrophysiology
| Equipment Category | Primary Function | Key Specifications | Considerations for Researchers |
|---|---|---|---|
| Microscope with Micromanipulator | Optical magnification and precise electrode positioning | • 300-400x magnification• Contrast enhancement (DIC, Phase, Hoffman)• Nanometer-precision 3D movement | An inverted microscope is preferable for easier electrode access from above [24]. |
| Amplifier | Measures electrical currents or changes in membrane potential | • Low-noise performance• Variable gain control• Capable of voltage-clamp and current-clamp | Amplifies signals from the headstage; some models allow customization of gain and filter settings [24] [26]. |
| Micropipette Puller | Fabricates glass microelectrodes for recording | • Programmable heat, force, and pull parameters• Multiple pull stages for consistency | The type of glass, ambient temperature, and humidity all affect the final pipette shape [27]. |
| Faraday Cage | Enclosure to block external electromagnetic interference | • Wire mesh or solid conductive material• Grounded to dissipate currents | Essential for low-current measurements (e.g., below 1 µA); must be properly grounded to the instrument [24] [28]. |
| Digitizer | Converts analog signals from the amplifier into digital data | • High sampling rate (e.g., 500 kHz)• Features for noise reduction (e.g., HumSilencer) | Positioned between the amplifier and computer; determines the quality of the signal for analysis [24]. |
| Headstage | Holds the micropipette and transmits electrical signals to the amplifier | • Critical electric circuitry to reduce noise• Specifically tuned for the amplifier | The headstage is mounted onto the micromanipulator, which controls its position [24]. |
Research Reagent Solutions
The following table lists essential materials and reagents required for a typical electrophysiology experiment, such as at the C. elegans neuromuscular junction [29].
Table 2: Essential Research Reagents and Materials
| Item | Function/Application | Example Specifications |
|---|---|---|
| Borosilicate Glass Capillaries | Used to fabricate recording, stimulus, and cutting pipettes. | Outer diameter: 1.0 - 1.5 mm; Inner diameter: 1.1 mm [29] [30]. |
| Internal Pipette Solution | Fills the recording pipette to establish electrical continuity with the cell interior. | Contains ions (e.g., CsCl, CsF), pH buffered to 7.2 with CsOH [29]. |
| Extracellular Solution | Maintains the biological preparation in a healthy, physiological state during recording. | Bubbled with 5% CO₂ and 95% O₂; contains salts (NaCl, KCl, CaCl₂, MgCl₂, glucose) [29]. |
| Collagenase Solution | Enzyme used to assist in the dissection and preparation of tissue. | 1 mg/mL stock solution in extracellular solution [29]. |
| Sylgard 184 | An elastomer used to coat pipettes, decreasing capacitance and improving noise characteristics. | Cured overnight at 60°C [29] [30]. |
| Histoacryl Blue Tissue Adhesive | Used to immobilize the dissected preparation for stable recording. | A blue-colored surgical glue for easy visualization during dissection [29]. |
Experimental Protocols
Workflow for Electrophysiological Recording and Correlation Microscopy
The following diagram outlines a comprehensive protocol that integrates electrophysiological recording with subsequent electron microscopy analysis, enabling researchers to correlate neuronal function with ultrastructural anatomy [29] [31].
Protocol: Pipette Pulling and Preparation
The creation of high-quality glass microelectrodes is a critical first step for successful electrophysiology. The process is both a science and an art, requiring an understanding of material properties and puller mechanics [27].
Detailed Steps for Pipette Preparation:
Pulling Pipettes:
- Capillary Selection: Use clean, dust-free borosilicate glass capillaries. For standard patch-clamp recording, capillaries with an outer diameter of 1.0 mm to 1.5 mm are typical [30].
- Program Design: Use a programmable puller (e.g., Sutter P-97) with a multi-step program. A common approach is a 4-5 step program with descending heat and velocity at each step, and a small pull on the final step [30].
- Parameter Adjustment: The final pipette geometry is fine-tuned by adjusting key parameters [27]:
- Increase Heat: Results in a longer taper.
- Increase Force: Produces smaller tips and a longer taper.
- Increase Pull Distance: Yields smaller tips.
- Environmental Control: Note that room temperature and humidity can affect pull consistency and must be kept stable [27].
Pipette Finishing (Optional but Recommended):
- Coating: Coat the pipette shank with an insulator like Sylgard 184 or dental wax to decrease electrical capacitance and improve noise characteristics [30]. Apply air pressure to the back of the pipette during dipping to prevent the insulator from entering the tip.
- Fire Polishing: Use a microforge with a heated filament to smooth the pipette tip. A brief heat pulse of 1-2 seconds is sufficient to smooth the glass and remove any insulator from the tip opening [30].
Quality Control and Storage:
Protocol: In Vivo Electrophysiology at the Neuromuscular Junction
This protocol details the steps for performing electrophysiological recordings at the C. elegans neuromuscular junction (NMJ), a common model system [29].
Timing: Approximately 3 hours for preparation and recording.
Steps:
Preparation (Day Before Recording):
- Transfer 20-30 well-fed L4-stage worms to a new NGM plate for use the next day [29].
- Prepare, aliquot, and freeze the internal pipette stock solution. Adjust the pH to 7.2 before freezing [29].
- Prepare and freeze aliquots of collagenase digestion solution (1 mg/mL in extracellular solution) [29].
- Prepare Sylgard 184-coated circular coverslips and cure them overnight at 60°C [29].
Preparation (Day of Recording):
- Make 500 mL of fresh extracellular solution and bubble continuously with a mixture of 5% CO₂ and 95% O₂ for at least 20 minutes [29].
- Prepare an ice bottle to immobilize worms.
- Pull all required pipettes: recording pipettes (which must be polished), stimulus pipettes, and sharp cutting pipettes [29].
- Thaw one aliquot each of collagenase and internal pipette solution [29].
Dissection and Recording:
- Immobilization: Place worms on an agarose pad on a Sylgard-coated coverslip and cool on ice to immobilize them [29].
- Gluing and Dissection: Glue the worms to the coverslip using Histoacryl Blue tissue adhesive. Perform a longitudinal cut along the body wall using a sharp pipette to expose the neuromuscular junctions [29].
- Establishing Recording: Place the dissected preparation into the recording chamber, continuously perfused with oxygenated extracellular solution. Under visual guidance using the microscope, maneuver the recording pipette (filled with internal solution) onto a muscle cell using the micromanipulator. Apply gentle suction to form a tight seal (giga-ohm seal) [29].
- Data Acquisition: Use the amplifier and software to record postsynaptic currents. Signals are acquired through the headstage, amplified, digitized, and stored on a computer for subsequent analysis [29] [24].
Technical Considerations and Troubleshooting
The Science of Pulling Micropipettes
Creating consistent and high-quality micropipettes is foundational. Several factors influence the process [27]:
- Heat Transfer: The primary heat source is radiation from the filament. The distance between the glass and filament is critical for even heating. Convection from ambient air and conduction to filament holders also affect the glass transition and must be managed by allowing cool-down time between pulls [27].
- Filament Aging: The platinum/iridium filament slowly oxidizes with use, changing its heating properties over time and eventually burning out, which necessitates replacement [27].
- Glass Type: Different types of glass capillaries have different softening points. Even different manufacturing lots of the same product can show slight variations, requiring fine-tuning of pulling programs [27].
Principles and Proper Use of a Faraday Cage
A Faraday cage is an enclosure made of conductive material or mesh that blocks external electromagnetic fields [32]. It works by redistributing electrical charges on its exterior, which cancels out the effect of the external field inside the enclosure [28]. For electrophysiologists, its proper use is non-negotiable for high-fidelity recordings.
- When to Use: A Faraday cage should be used whenever possible, but it is absolutely essential for experiments involving low currents (below 1 µA) or high frequencies. The small electrical currents measured during patch-clamp experiments (in the picoamp range) can be easily distorted by external noise sources like radio waves or mains power lines [24] [28].
- Critical Grounding: Simply placing equipment inside a cage is insufficient. The cage must be grounded to the instrument's ground reference. An ungrounded cage can act as an antenna, capacitively coupling noise into the electrodes. Most potentiostats/amplifiers require the cage to be earth grounded, though some floating-ground instruments are exceptions [28].
- Design and Integrity: The cage's effectiveness depends on the conductivity of the material and the size of any holes. openings should be smaller than 1/10th the wavelength of the noise to be blocked. Special attention must be paid to doors and lids to ensure good electrical continuity across the seams [28]. A common and effective DIY solution is a wood-frame cage covered with copper or aluminum mesh [28].
The precise measurement of neuronal activity hinges on the correct selection, operation, and integration of core electrophysiology equipment. Microscopes with micromanipulators enable the visualization and precise placement of electrodes. Amplifiers and digitizers are crucial for faithfully detecting and converting minuscule biological signals. The art and science of pulling micropipettes provide the essential interface with the neuron itself. Finally, the Faraday cage creates the quiet electronic environment necessary for these sensitive measurements. By following the detailed application notes and protocols outlined in this document, researchers and drug development professionals can establish a robust foundation for investigating the mechanisms of neuronal function, synaptic transmission, and the effects of pharmacological compounds with high accuracy and reliability.
Core Techniques and Their Transformative Applications in Research and Drug Discovery
Patch-clamp electrophysiology represents the gold standard technique for high-resolution recording of ionic currents across biological membranes, enabling the functional study of ion channels at the level of single molecules to entire cellular networks [33]. Since its initial development by Neher and Sakmann in 1976 and subsequent refinement to include whole-cell configuration by Hamill et al. in 1981, this technique has revolutionized neurophysiology and drug discovery research [34]. The method's unparalleled sensitivity allows researchers to observe the conformational changes that individual ion channel proteins undergo during gating, providing critical insights into neuronal excitability, synaptic transmission, and the mechanisms of neurological diseases [33] [35]. For drug development professionals, patch-clamp electrophysiology serves as an essential tool for screening compounds that modulate ion channel function, offering direct assessment of drug efficacy and kinetics. This article details the core configurations, experimental protocols, and technical considerations that establish patch-clamp recording as an indispensable methodology in neuroscience research and pharmaceutical development.
Technical Configurations and Their Applications
The patch-clamp technique encompasses several configurations, each tailored to address specific experimental questions by providing access to different levels of electrophysiological information.
Table 1: Comparison of Primary Patch-Clamp Configurations
| Configuration | Key Feature | Primary Applications | Typical Pipette Resistance | Signal Resolution |
|---|---|---|---|---|
| Cell-Attached | Intact cell; records single-channel currents from a membrane patch | Single-channel kinetics, ligand-gated or mechanosensitive channel activity [33] | 12-24 MΩ [33] | Single-channel currents (pA range) |
| Whole-Cell | Direct electrical access to cell interior; records macroscopic currents | Neuronal excitability, action potentials, synaptic currents [35] [34] | 3-6 MΩ [34] | Macroscopic currents (nA range) |
| Inside-Out | Isolated intracellular membrane face | Modulation of channels by intracellular messengers [34] | 5-10 MΩ | Single-channel currents |
| Outside-Out | Isolated extracellular membrane face | Rapid solution exchange studies of ligand-gated channels [34] | 5-10 MΩ | Single-channel currents |
Each configuration provides unique experimental advantages. The cell-attached mode permits long observation periods of single-channel activity in their native membrane environment without disrupting intracellular content, making it ideal for studying baseline channel kinetics [33]. Conversely, the whole-cell configuration allows comprehensive assessment of a neuron's integrative properties, including synaptic inputs and action potential generation, by providing electrical access to the entire cell [35]. The excised patch configurations (inside-out and outside-out) enable precise control of the solution environment on either side of the membrane, facilitating studies of channel modulation by second messengers or pharmaceuticals.
Experimental Protocols
Cell-Attached Single-Channel Recording
This protocol outlines the procedure for obtaining one-channel cell-attached recordings, optimized for NMDA receptors or mechanosensitive channels like PIEZO1 [33].
Materials and Equipment:
- Patch-clamp amplifier and data acquisition system (e.g., with QuB software)
- Vibration isolation table, Faraday cage
- Inverted microscope with phase-contrast and fluorescence capabilities
- Pipette puller and polisher
- Borosilicate glass capillaries
- HEK293 cells or cortical neurons expressing the channel of interest
Step-by-Step Procedure:
Cell Preparation: Maintain HEK293 cells (passages 22-40) in DMEM with 10% FBS and 1% penicillin/streptomycin. For transfection, plate cells at ~10⁵ cells/35 mm dish and transfect with appropriate channel cDNA (e.g., GluN1, GluN2A for NMDA receptors) using a calcium phosphate method. Use cells for recording 24-48 hours post-transfection [33].
Pipette Preparation: Pull borosilicate glass capillaries to produce tips with 1.4-1.6 μm outer diameter, yielding resistances of 12-24 MΩ when filled with pipette solution. Fire-polish to optimize seal formation [33].
Pipette Solution: For NMDA receptors, use a solution containing (in mM): 1 glutamate, 0.1 glycine, 150 NaCl, 2.5 KCl, 1 EDTA, and 10 HEPES (pH 8.0 with NaOH). This provides saturating agonist concentrations and physiologic permeant ions [33].
Seal Formation: Select a fluorescently identified, healthy cell. Apply slight positive pressure to the pipette while lowering it into the bath solution. Once the pipette contacts the cell membrane, release positive pressure and apply gentle negative pressure to achieve a giga-ohm seal (resistance >1 GΩ) [33].
Data Acquisition: Set the amplifier to voltage-clamp mode with applied voltage typically between +60 to +100 mV. Acquire data at 40 kHz sampling rate with a 10 kHz low-pass filter. Record continuous stretches of activity for kinetic analysis [33].
Whole-Cell Patch-Clamp Recording in Brain Slices
This protocol details the steps for whole-cell recording from neurons in acute brain slices, enabling assessment of neuronal excitability and synaptic function [35].
Materials and Equipment:
- Vibratome for slice preparation
- Carbogen (95% O₂/5% CO₂) delivery system
- aCSF and intracellular solutions
- Micromanipulator, amplifier, and data acquisition software
Step-by-Step Procedure:
Acute Slice Preparation: Prepare cutting solution containing (in mM): 220 glycerol, 2.5 KCl, 1.25 NaH₂PO₄, 25 NaHCO₃, 0.5 CaCl₂, 7 MgCl₂, and 20 D-glucose [35]. Rapidly dissect and section brain tissue (300-400 μm thickness) in ice-cold cutting solution to minimize excitotoxicity.
Slice Recovery: Transfer slices to artificial cerebrospinal fluid (aCSF) containing (in mM): 125 NaCl, 2.5 KCl, 25 NaHCO₃, 1.25 NaH₂PO₄, 2.5 CaCl₂, 1.3 MgCl₂, and 10 D-glucose [35]. Incubate at 32-35°C for 30 minutes, then maintain at room temperature for at least 1 hour before recording.
Intracellular Solution: Prepare potassium gluconate-based internal solution containing (in mM): 135 KCl, 0.5 EGTA, 10 HEPES, 2 Mg-ATP, 0.2 Na-GTP, and 4 Na₂-phosphocreatine (pH 7.25 with KOH, 280-290 mOsm) [35]. For synaptic current recordings, use CsCl-based solutions to block potassium channels.
Whole-Cell Establishment: Approach target neurons under visual guidance using DIC or fluorescence microscopy. Contact the cell membrane with 3-6 MΩ pipettes while applying positive pressure. Upon seal formation (>1 GΩ), compensate pipette capacitance and apply brief negative pressure or voltage pulses to rupture the membrane patch, establishing whole-cell access [34].
Recording Parameters: For current-clamp recordings of action potentials, maintain cells near their resting potential. For voltage-clamp recordings of synaptic currents, hold at -70 mV for AMPA receptor-mediated currents or +40 mV for NMDA receptor-mediated currents. Add tetrodotoxin (TTX, 1 μM) to isolate miniature postsynaptic currents [35].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful patch-clamp experimentation requires carefully formulated solutions and quality materials to maintain cellular health and ensure recording stability.
Table 2: Essential Research Reagents and Materials for Patch-Clamp Electrophysiology
| Category | Component | Typical Concentration | Function and Importance |
|---|---|---|---|
| Extracellular Solutions | Artificial Cerebrospinal Fluid (aCSF) | 125 mM NaCl, 2.5 KCl, 25 NaHCO₃, 1.25 NaH₂PO₄, 2.5 CaCl₂, 1.3 MgCl₂, 10 D-glucose [35] | Maintains physiological ionic environment and osmolarity during recordings |
| Cutting Solution for Slices | 220 mM glycerol, 2.5 KCl, 0.5 CaCl₂, 7 MgCl₂, 20 D-glucose [35] | Protects cells during slice preparation; low Ca²⁺/high Mg²⁺ reduces excitotoxicity | |
| Intracellular Solutions | Potassium Gluconate-based | 126 mM K-gluconate, 4 KCl, 10 HEPES, 0.3 EGTA, 4 Mg-ATP, 0.3 GTP, 10 phosphocreatine [34] | Maintains physiological K⁺ gradient; suitable for current-clamp recordings |
| CsCl-based | 130 mM CsCl, 5 KCl, 0.5 EGTA, 10 HEPES, 2 Mg-ATP, 0.2 Na-GTP [35] | Blocks K⁺ channels; improves voltage control for synaptic current measurements | |
| Pharmacological Agents | Tetrodotoxin (TTX) | 1 μM [35] | Voltage-gated sodium channel blocker; isolates miniature synaptic events |
| DNQX and AP-5 | 10 μM DNQX, 20 μM AP-5 [35] | Glutamate receptor antagonists; blocks excitatory synaptic transmission | |
| Picrotoxin | 100 μM [35] | GABAA receptor antagonist; blocks inhibitory synaptic currents | |
| Technical Materials | Borosilicate Glass Capillaries | - | Fabrication of recording pipettes with optimal electrical and mechanical properties |
| Biocytin | 0.5% [34] | Cell filler for post-hoc morphological reconstruction of recorded neurons |
Advanced Applications and Integration with Other Techniques
Modern electrophysiology increasingly combines patch-clamp recording with other methodologies to provide multidimensional insights into neuronal function, creating powerful hybrid approaches for comprehensive investigation.
The Patch2MAP technique exemplifies this integration, combining whole-cell patch-clamp electrophysiology with epitope-preserving magnified analysis of the proteome (eMAP) for correlative functional and structural investigation [36]. This method involves filling patched neurons with biocytin during recording, followed by chemical fixation, tissue-gel hybridization, and super-resolution imaging. This enables precise correlation of physiological properties with subcellular protein expression, such as demonstrating that functional AMPA-to-NMDA receptor ratios tightly correspond to respective protein expression levels in human cortical neurons [36].
Similarly, patch-clamp recordings integrated with two-photon glutamate uncaging allow researchers to measure functional receptor properties at individual dendritic spines while subsequently quantifying protein distribution at the same synapses [36]. These advanced applications highlight how patch-clamp electrophysiology serves as a foundation for multimodal investigation of neuronal function, from molecular mechanisms to network-level processes. For drug development, these integrated approaches provide unprecedented insight into how pharmacological compounds affect not only ion channel function but also downstream signaling pathways and structural plasticity.
Automated planar patch-clamp (APC) technology represents a transformative advancement in electrophysiology, enabling direct, high-throughput interrogation of ion channel activity for drug discovery. This method addresses a critical bottleneck in neuroscience and cardiac research, where traditional manual patch-clamp techniques, while considered the gold standard for accuracy, are prohibitively slow and labor-intensive for large-scale compound screening [37] [38]. By replacing the glass micropipette with a planar substrate containing a microscopic aperture, the process of achieving a high-resistance seal (giga-seal) on a cell membrane can be automated, dramatically increasing data output and reproducibility while reducing operator-dependent variability [38]. This Application Note details the implementation of APC for drug screening, providing specific protocols and quantitative data to facilitate its adoption in research and development.
Key Principles and Technological Advantages
The core principle of planar patch-clamp involves integrating a microscopic aperture into a chip or multi-well plate. A cell suspension is added, and negative pressure draws a single cell onto the aperture, forming a high-resistance seal. Subsequent membrane rupture establishes the whole-cell configuration for electrophysiological recording [38] [39]. This fundamental design enables several key advantages over conventional methods:
- High Throughput: APC systems can simultaneously record from 384 or more cells, generating hundreds of data points in the time a manual patch-clamp experiment would yield a single recording [37] [40].
- Enhanced Reproducibility: Automation minimizes experimenter bias and variability. Assay robustness is quantifiable, with Z-factor analyses consistently showing good to excellent values, making the technique ideal for standardized screening [37].
- Direct and Quantitative Measurement: Unlike indirect fluorometric methods, APC provides direct, real-time measurement of ion channel kinetics and pharmacology with high resolution and accuracy [40] [39].
Quantitative Performance Data
The following tables summarize key performance metrics from recent applications of APC in different experimental contexts.
Table 1: Performance of APC on Native Cardiomyocytes Data derived from swine atrial and ventricular cardiomyocytes recorded on a 384-well APC system [37].
| Parameter | Atrial Cardiomyocytes | Ventricular Cardiomyocytes | Overall Performance |
|---|---|---|---|
| Patching Success Rate | ~16.1% (estimated) | ~11.7% (estimated) | 13.9 ± 1.7% |
| Seal Resistance | >100 MΩ | >100 MΩ | Stable during acquisition |
| L-type Ca²⁺ Current (I_Ca,L) Density | -4.29 ± 0.17 pA/pF | -8.65 ± 1.2 pA/pF | Comparable to manual patch-clamp |
| Pharmacology (Nifedipine EC₅₀) | 6.08 ± 1.14 nM | 3.41 ± 0.71 nM | Appropriate concentration-dependent block |
Table 2: Application of APC for Screening ENaC Modulators Data from a high-throughput screen using HEK293 cells stably expressing human αβγ-ENaC [40].
| Experimental Measure | Result / Value | Significance |
|---|---|---|
| Cell Preparation | Enzymatic detachment (TrypLE Express) | High success rate for APC recordings |
| Key Reagents | Amiloride (inhibitor), S3969 (activator), γ-inhibitory peptide | Validation of inhibitory and stimulatory effects |
| Functional Outcome | Robust, amiloride-inhibitable ENaC currents | Confirmation of reliable current measurement |
Detailed Experimental Protocols
Protocol 1: High-Throughput Screening of L-type Calcium Channel Modulators in Native Cardiomyocytes
This protocol is adapted from studies on isolated swine cardiomyocytes and is designed for screening compounds affecting I_Ca,L [37].
I. Cell Preparation
- Cardiomyocyte Isolation: Isolate atrial and ventricular cardiomyocytes from mammalian heart tissue using a standard enzymatic digestion procedure (e.g., collagenase/protease). The expected yield is approximately 7,200-8,800 viable cells per heart.
- Cell Suspension: Resuspend the freshly isolated cells in appropriate physiological saline solution (e.g., Tyrode's solution). Keep the suspension at room temperature and use within 6-8 hours.
II. Automated Planar Patch-Clamp Recording
- System Setup: Use a 384-well fixed-well format APC platform. Prime the system with appropriate internal and external solutions.
- Internal Solution: (Example) CsCl, EGTA, HEPES, Mg-ATP to isolate Ca²⁺ currents by blocking K⁺ currents.
- External Solution: (Example) Tyrode's solution with 1.8-2.0 mM CaCl₂ to carry the I_Ca,L.
- Cell Loading: Dispense the cell suspension into the wells of the APC plate. Cells settle via gravity and suction onto the patch-clamp apertures.
- Seal Formation and Whole-Cell Access: The system automatically applies gentle negative pressure to form giga-ohm seals (>100 MΩ) and subsequently ruptures the membrane patch to establish whole-cell configuration. Monitor seal quality via capacitance and series resistance (Rseries).
III. Electrophysiology and Drug Application
- Voltage Protocol for I_Ca,L:
- Holding potential: -50 mV (to inactivate Na⁺ channels).
- Depolarizing step: A series of 200-ms steps from -40 mV to +60 mV in 10-mV increments.
- Inter-pulse interval: 5 seconds to allow for recovery from inactivation.
- Data Acquisition: Record the resulting currents. Peak I_Ca,L is typically observed at +10 mV. Analyze current density (pA/pF) by normalizing to cell capacitance.
- Drug Application:
- Establish a stable baseline recording of I_Ca,L.
- Apply increasing concentrations of the test compound (e.g., nifedipine at 1, 5, 25 nM, and 5 µM) via the automated fluidics system.
- At each concentration, re-run the voltage protocol after a set incubation period (e.g., 2-3 minutes).
- Include a positive control (e.g., 5 µM nifedipine for full block) and a vehicle control.
IV. Data Analysis
- Plot concentration-response curves by normalizing the peak I_Ca,L at each drug concentration to the baseline current.
- Fit the data with a suitable equation (e.g., Hill equation) to determine the half-maximal inhibitory concentration (IC₅₀).
Protocol 2: Identification of Epithelial Sodium Channel (ENaC) Modulators
This protocol outlines the use of APC for screening activators and inhibitors of ENaC, a key therapeutic target [40].
I. Cell Culture and Preparation
- Cell Line: Use a HEK293 cell line stably transfected with human α-, β-, and γ-ENaC subunits. Maintain cells in culture medium supplemented with selection antibiotics and 50 µM amiloride to prevent sodium overload.
- Cell Detachment: To prepare for APC, detach cells using a standard enzymatic reagent like TrypLE Express.
- Critical Recovery Step: After detachment, incubate the cell suspension in culture medium for a prolonged period (e.g., several hours) to allow for recovery from partial proteolytic activation of ENaC induced by the enzymes. This step enhances the sensitivity for detecting channel activators.
- Final Resuspension: Wash and resuspend the cells in the appropriate bath solution for recording.
II. APC Recording of ENaC Currents
- Solutions: Use symmetrical Na⁺ conditions to maximize ENaC currents. The external and internal solutions should contain a comparable high Na⁺ concentration (e.g., 135-150 mM).
- Voltage Protocol:
- A continuous voltage-ramp protocol (e.g., from -100 mV to +100 mV over 500 ms) can be used to observe the current-voltage relationship of ENaC.
- Alternatively, a holding potential of -60 or -70 mV can be maintained, and the steady-state current can be monitored.
- Validation and Screening:
- Validate the recorded current as ENaC-mediated by applying a known inhibitor, 10 µM amiloride, which should block >80% of the current.
- For screening, apply test compounds and monitor changes in the amiloride-sensitive current.
- To identify activators mimicking proteolytic cleavage, test the effect of compounds in the presence and absence of a prototypical serine protease like chymotrypsin.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for APC Experiments
| Item | Function / Application | Example & Notes |
|---|---|---|
| Stable Cell Line | Recombinant expression of target ion channel. | HEK293 cells stably expressing human αβγ-ENaC [40]. |
| Native Cells | Physiologically relevant model system. | Freshly isolated swine or rodent cardiomyocytes [37]. |
| Enzymatic Detachment Reagent | Harvesting adherent cells for suspension. | TrypLE Express; less harsh than trypsin-EDTA, improves cell health and recording success [40]. |
| Internal/External Solutions | Ionic environment for current isolation. | Cs⁺-based internal and Ca²⁺-containing external for I_Ca,L; symmetrical Na⁺ for ENaC [37] [40]. |
| Reference Agonist | Positive control for channel activation. | S3969 (small molecule ENaC activator) [40]. |
| Reference Antagonist | Positive control for channel blockade. | Nifedipine (L-type Ca²⁺ channel blocker) [37]; Amiloride (ENaC blocker) [40]. |
| Inhibitory Peptide | Tool for mechanistic studies. | γ-inhibitory peptide (Acetyl-RFSHRIPLLIF-Amide) for blocking ENaC [40]. |
Workflow and Data Analysis Visualization
The following diagram illustrates the standard workflow for a high-throughput drug screening campaign using an automated planar patch-clamp system.
Diagram 1: Automated Patch-Clamp Drug Screening Workflow.
Automated planar patch-clamp technology has firmly established itself as an indispensable tool in modern ion channel research and drug discovery. By providing high-throughput, high-quality, and reproducible electrophysiological data, it bridges the gap between molecular biology and functional phenotyping. The protocols and data outlined herein demonstrate its successful application across target classes, from cardiac ion channels to neuronal and epithelial targets, enabling the rapid identification and characterization of novel therapeutic compounds with enhanced efficiency and predictive power.
High-density microelectrode arrays (HD-MEAs) have emerged as a powerful tool for the functional characterization of electrogenic cells, enabling researchers to infer cellular phenotypes and elucidate fundamental mechanisms underlying cellular function [41]. These platforms allow for the study of cellular function across spatial and temporal scales, from subcellular compartments to entire intact networks, and from microseconds to months [41]. The technology is particularly valuable in interdisciplinary work at the intersection of biomedical engineering, computer science, and artificial intelligence (AI), finding applications in neurodevelopmental research, stem cell biology, and pharmacology [41]. For drug development professionals, HD-MEAs provide a powerful platform for assessing compound effects on neural network function in vitro, bridging the gap between traditional electrophysiology and clinical translation [42] [43].
HD-MEA Technology and Quantitative Specifications
Advances in complementary metal-oxide-semiconductor (CMOS) technology have enabled the miniaturization of electrode arrays and the integration of electronic components directly on-chip, overcoming the "connectivity problem" of traditional low-density MEAs [41]. This integration has significantly enhanced the number of electrodes, array area, spatial density, and number of readout channels while improving the signal-to-noise ratio (SNR) by avoiding long signal paths that introduce parasitic capacitance and thermal noise [41].
Table 1: Key Specifications of Advanced HD-MEA Platforms
| Parameter | Representative Specification | Application Significance |
|---|---|---|
| Array Sensing Area | 5.51 × 5.91 mm² [41] | Suitable for large networks and tissue slices |
| Total Electrodes | 236,880 [41] | High spatial sampling for detailed activity mapping |
| Electrode Density | >3000 electrodes per mm² [41] | Enables subcellular resolution and single-cell tracking |
| Simultaneous Readout Channels | 33,840 channels [41] | Massive parallel recording capability |
| Sampling Rate | Up to 70 kHz [41] | Adequate for capturing precise action potential waveforms |
| Electrode Size | 11.22 × 11.22 μm² [41] | Compatible with individual neurons and processes |
| Electrode Spacing | 0.25 μm [41] | Minimizes spatial aliasing |
Experimental Protocols
Protocol: Simultaneous Measurement of Field Potential and Glutamate Release
This protocol enables direct investigation of the relationship between synaptic signaling dynamics and neuronal excitation, which is particularly relevant for studying diseases like Alzheimer's, schizophrenia, and epilepsy where glutamate dysregulation occurs [44].
Key Materials:
- Enzyme-modified CNT-MEA: 64-channel indium tin oxide (ITO) microelectrode array with electroplated cup-stacked carbon nanotubes (CNTs) [44]
- Enzyme Solution: Glutamate oxidase (Glu-Ox) and osmium polymer/horseradish peroxidase (Os-HRP) with glutaraldehyde crosslinker [44]
- Preparation of Enzyme-modified CNT-MEA:
Experimental Procedure:
- Tissue Preparation: Prepare acute hippocampal brain slices (300-400 μm thickness) from experimental animals using standard procedures [44]
- System Setup: Place the enzyme-modified CNT-MEA in the recording chamber and continuously perfuse with oxygenated artificial cerebrospinal fluid (aCSF) at 32°C [44]
- Simultaneous Recording:
- Acquire field potential (FP) signals through standard MEA recording channels
- Measure electrochemical (EC) signals for glutamate detection simultaneously [44]
- Pharmacological Validation:
- Data Analysis:
- Correlate FP spike patterns with glutamate concentration changes
- Calculate glutamate release kinetics from EC signals [44]
Protocol: Functional Connectivity Analysis of Neuronal Networks
This protocol describes the use of the MEA-NAP (MEA Network Analysis Pipeline) for extracting functional connectivity and network topology from MEA recordings, applicable to both 2D cultures and 3D cerebral organoids [45] [46].
Key Materials:
- MEA-NAP Software: MATLAB-based pipeline for network analysis (open-source) [45]
- Neuronal Cultures: 2D human iPSC-derived neurons, murine cortical cultures, or 3D human cerebral organoids [45]
- Recording System: Single- or multi-well MEA systems with appropriate data export capabilities [45]
Experimental Procedure:
- Data Acquisition:
- Spike Detection:
- Functional Connectivity Mapping:
- Network Analysis:
- Pharmacological Perturbation (Optional):
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for MEA Experiments
| Item | Function/Application | Example Use Case |
|---|---|---|
| Enzyme-modified CNT-MEA | Simultaneous measurement of field potentials and neurotransmitter release [44] | Real-time monitoring of glutamate dynamics in hippocampal slices during depolarization [44] |
| Glutamate Oxidase (Glu-Ox) | Enzyme for electrochemical detection of glutamate; converts glutamate to α-ketoglutarate and H₂O₂ [44] | Key component of biosensor for measuring glutamate release in disease models [44] |
| Os-HRP Polymer | Electron mediator for enhanced electrochemical signal detection [44] | Amplification of H₂O₂ signal generated in glutamate detection assay [44] |
| MEA-NAP Software | MATLAB-based pipeline for analyzing functional connectivity and network topology [45] [46] | Tracking network development in human iPSC-derived cultures and identifying hub nodes [45] |
| Human iPSC-Derived Neurons | Physiologically relevant human cellular models for disease modeling and drug screening [45] | Studying neurodevelopmental disorders and screening therapeutic compounds [45] |
| Cerebral Organoids | 3D human stem cell-derived models that recapitulate aspects of brain development [45] | Investigating network formation in complex 3D environments modeling human brain development [45] |
Data Analysis and Interpretation
Quantitative Analysis of MEA Data
Table 3: Quantitative Analysis Methods for MEA Data
| Analysis Type | Appropriate Quantitative Methods | Biological Interpretation |
|---|---|---|
| Univariate Analysis | Descriptive statistics (mean, median, standard deviation of firing rates, burst parameters) [47] | Basic assessment of network activity levels and excitability [45] |
| Functional Connectivity | Spike Time Tiling Coefficient (STTC), probabilistic thresholding for significant connections [45] | Mapping of information flow pathways and functional interactions between neurons [45] |
| Network Topology | Graph theory metrics (modularity, clustering coefficient, path length, efficiency) [45] | Assessment of network organization, efficiency of information transfer, and resilience [45] |
| Node Cartography | Classification of nodes based on connectivity patterns (hubs, peripherals, connectors) [45] | Identification of critical elements that control network stability and information integration [45] |
| Dimensionality Reduction | PCA, t-SNE, UMAP for visualizing network developmental trajectories [45] | Tracking network maturation and classifying network states across development or treatment [45] |
Integration with Other Modalities
The combination of HD-MEAs with other experimental techniques enables multimodal investigation of cellular function, providing more comprehensive biological insights [41]. Recent innovations have focused on adding other readout modalities to HD-MEAs and introducing innovative electrode designs for intracellular-like measurements at scale [41]. These integrated approaches are particularly valuable for translational applications, including functional phenotyping of human cellular models and drug screening, where they provide insights often inaccessible through single-method characterization techniques [41].
Electrophysiology serves as a cornerstone technique in neuroscience and drug discovery, enabling researchers to decipher the electrical properties of neurons and other excitable cells. At the heart of this field lie two fundamental recording configurations: voltage-clamp and current-clamp. These techniques empower scientists to measure the ion channel activity and electrical excitability that underpin neuronal signaling, from basic sensory transduction to complex cognitive processes. The voltage-clamp technique, pioneered by Cole, Hodgkin, and Huxley in the mid-20th century using squid giant axons, was instrumental in revealing the ionic basis of the action potential [48] [49]. The subsequent development of the patch-clamp technique by Sakmann and Neher refined these approaches, allowing study of single ion channels and smaller cells [50]. Today, these methods remain essential tools for understanding neuronal function in health and disease, and for screening potential neuroactive pharmaceuticals in drug development pipelines [51] [52]. This application note details the principles, methodologies, and applications of both techniques within the context of contemporary neuronal research.
Fundamental Principles and Comparisons
The Voltage-Clamp Technique
The voltage-clamp technique is designed to maintain a pre-determined, or "clamped," membrane potential in a cell while measuring the transmembrane ionic currents required to maintain that voltage [53] [54] [48]. This is achieved through a negative feedback circuit. The amplifier continuously compares the measured membrane potential (Vm) to the desired command voltage (Vcmd). Any difference between these values (error signal) drives the injection of current (I) into the cell, equal in magnitude but opposite in direction to the sum of the ionic currents flowing through the cell's membrane channels. This feedback occurs almost instantaneously, preventing the membrane potential from changing [48] [49]. The recorded current is thus a direct reflection of the net ionic flux through activated channels at a fixed membrane potential, allowing for precise quantification of ion channel kinetics and conductance [53] [54].
Table 1: Core Components of a Voltage-Clamp System
| Component | Function |
|---|---|
| Voltage-Sensing Electrode | Measures the instantaneous membrane potential [54]. |
| Current-Passing Electrode | Injects current to maintain the membrane at the command voltage [54]. |
| Feedback Amplifier | Compares measured voltage to command voltage and drives the corrective response [54] [48]. |
| Command Voltage Source | Sets the desired membrane potential for the experimenter [48]. |
A key application of voltage-clamp in neuronal research is the study of voltage-gated sodium channels (NaV), which are crucial for action potential initiation and propagation. Under voltage-clamp, a family of depolarizing voltage steps can be applied, and the resulting fast, inward sodium currents can be recorded and analyzed for activation and inactivation kinetics [52]. This is vital for investigating the effects of disease-causing mutations or for screening compounds that modulate sodium channel activity.
The Current-Clamp Technique
In contrast, current-clamp mode is used to record changes in membrane potential while injecting a defined amount of current into the cell [53] [50]. Here, the amplifier is configured to pass a set current (which can be zero, constant, or a complex waveform) through the recording electrode and measure the resulting voltage across the membrane [53] [55]. This mode is ideal for studying the innate electrical excitability of a cell, as it allows the membrane potential to fluctuate freely in response to injected current or synaptic input. The most significant readout in current-clamp is the action potential. By injecting depolarizing current steps, researchers can elicit and record action potentials, analyzing key parameters such as threshold, amplitude, duration, and firing frequency [53] [55]. This provides direct insight into the cell's overall health and synaptic integration capabilities.
Table 2: Key Differences Between Voltage-Clamp and Current-Clamp Techniques
| Parameter | Voltage-Clamp | Current-Clamp |
|---|---|---|
| Controlled Variable | Membrane Potential (Voltage) [53] | Injected Current [53] |
| Measured Variable | Transmembrane Ionic Current [53] [54] | Membrane Potential [53] |
| Primary Application | Study of ion channel kinetics, conductance, and pharmacology [53] [48] | Study of cellular excitability, action potentials, and synaptic potentials [53] [56] |
| Output Reveals | Properties of specific ion channel populations (e.g., Na⁺, K⁺) [53] | Integrated response of all active conductances in the cell [53] |
| Best Suited For | Isolating and quantifying specific ionic currents [54] | Observing natural cellular signaling and firing patterns [53] [56] |
Research Reagent Solutions and Essential Materials
Successful electrophysiology requires precise instrumentation and reagent preparation. The following table outlines core components of a modern patch-clamp setup, applicable to both voltage-clamp and current-clamp experiments on neurons.
Table 3: Essential Research Reagents and Equipment for Neuronal Patch-Clamp Electrophysiology
| Item | Function / Description | Example / Note |
|---|---|---|
| Patch-Clamp Amplifier | Core instrument for signal amplification, feedback control, and mode switching [57]. | Axon Instruments models, EPC-7/EPC-10 amplifiers [56] [57]. |
| Data Acquisition System | Converts analog signals to digital for recording and analysis; outputs command waveforms [57]. | Axon Digidata systems interfaced with acquisition software [57]. |
| Micromanipulator | Precisely positions the glass pipette onto the cell membrane. | Motorized or piezo-driven manipulators for fine control. |
| Pipette Puller | Fabricates recording pipettes with consistent tip diameter and resistance [50]. | Pipette resistance typically 3-7 MΩ for neuronal cell-attached/whole-cell [56]. |
| Internal Pipette Solution | Replaces intracellular fluid; contains specific ions, ATP, and buffering agents [50] [55]. | e.g., KCl-based (145 mM KCl) or K-gluconate-based solutions [55]. |
| External Bath Solution | Mimics extracellular environment; provides ions, nutrients, and pH buffering [54] [55]. | e.g., Artificial Cerebrospinal Fluid (aCSF) or Tyrode's solution [55]. |
| Enzyme Solutions | For tissue cleaning; used in brain slice preparation to improve seal success. | e.g., Proteases (optional, for cleaning membrane). |
| Pharmacological Agents | To isolate, block, or activate specific ion channels or receptors [54] [55]. | e.g., TTX (NaV blocker), TEA (K⁺ channel blocker), CNQX (AMPA receptor antagonist) [56] [55]. |
Detailed Experimental Protocols
Protocol: Voltage-Clamp Recording of Voltage-Gated Sodium Currents in Neurons
Application: This protocol is used to isolate and characterize the fast sodium current (INa) in neurons, which is essential for action potential upstroke. This is critical for studying channelopathies or the effects of potential neurotherapeutics [52].
Materials:
- Cells: Freshly isolated neurons or neurons in acute brain slices [51].
- Solutions:
- Internal (Pipette) Solution: CsF-based solution to block potassium currents and improve voltage control.
- External (Bath) Solution: Standard physiological solution (e.g., aCSF). To isolate INa, add K⁺ channel blockers (e.g., TEA, 4-AP) and Ca²⁺ channel blockers (e.g., Cd²⁺, Co²⁺).
- Drugs: Tetrodotoxin (TTX) as a selective sodium channel blocker for confirmation.
Method:
- System Setup: Establish a whole-cell voltage-clamp configuration on the target neuron. For automated systems, follow the manufacturer's high-throughput protocol [51].
- Capacitance and Series Resistance Compensation: Use the amplifier's compensation circuitry to correct for the cell's capacitance and the series resistance (Rs) between the pipette and cell interior. Inadequate Rs compensation is a major source of error and voltage clamp artifacts, especially for large, fast currents like INa [52].
- Leak Subtraction: Apply a P/N or other leak subtraction protocol to remove linear capacitive and leak currents from the records.
- Voltage Protocol:
- Hold the cell at a hyperpolarized potential (e.g., -90 mV) to ensure sodium channels are available for activation.
- Apply a series of depolarizing voltage steps (e.g., from -80 mV to +60 mV in 10 mV increments) of a fixed duration (e.g., 20-50 ms).
- Data Acquisition: Record the elicited transmembrane currents. The fast, transient inward current is INa.
- Pharmacological Validation: Apply TTX (e.g., 1 µM) to the bath. Repeat the voltage protocol; the abolition of the transient inward current confirms it is INa.
- Data Analysis: Plot the peak INa against the test voltage to generate a current-voltage (I-V) relationship. Analyze activation and inactivation kinetics from the current traces.
Protocol: Current-Clamp Recording of Neuronal Excitability and Synaptic Potentials
Application: This protocol is used to assess the intrinsic excitability of a neuron and to record synaptic potentials, providing a direct measure of neuronal output and integration [53] [56].
Materials:
- Cells: Neurons in acute brain slices to preserve native circuitry.
- Solutions:
- Internal (Pipette) Solution: K-gluconate or KCl-based solution.
- External (Bath) Solution: Standard oxygenated aCSF.
- Drugs: Synaptic receptor agonists/antagonists (e.g., CNQX, AP5, Bicuculline) to characterize synaptic events.
Method:
- Recording Configuration: Establish a whole-cell or cell-attached current-clamp configuration. For stable resting membrane potential (RMP) recordings without disturbing intracellular content, a tight-seal (>1 GΩ) cell-attached configuration in current-clamp mode can be used [56].
- Measure Resting Membrane Potential (RMP): With zero current injection (I=0), record the stable membrane potential.
- Input Resistance (Rin) Test: Inject a small hyperpolarizing current step (e.g., -20 pA, 500 ms). Measure the resulting steady-state voltage change (ΔV). Rin = ΔV / I.
- Action Potential (AP) Evocation: Inject a series of depolarizing current steps of increasing magnitude (e.g., 5-30 pA increments) [55]. Record the resulting action potentials.
- Synaptic Potential Recording: To record postsynaptic potentials (PSPs), stimulate afferent fibers while in I=0 mode. Excitatory (EPSP) and inhibitory (IPSP) postsynaptic potentials will appear as depolarizing or hyperpolarizing deflections, respectively. Cell-attached current-clamp is particularly valuable for determining the true polarity of GABAergic potentials without the risk of shifting the chloride reversal potential, as can happen in whole-cell mode [56].
- Data Analysis:
- From AP traces: Calculate firing threshold, AP amplitude, afterhyperpolarization (AHP) amplitude, and adaptation index.
- From PSP traces: Measure amplitude, latency, and rise/decay time constants.
Advanced Applications and Integrated Approaches
Modern electrophysiology often leverages the strengths of both techniques to gain a comprehensive understanding of neuronal function. A powerful approach is the sequential or combined application of voltage-clamp and current-clamp on the same cell. For instance, voltage-clamp can first be used to characterize the density and kinetics of specific sodium, potassium, and calcium currents in a neuron. Immediately afterward, the configuration can be switched to current-clamp to investigate how these specific ionic conductances shape the cell's action potential waveform, firing patterns, and response to synaptic inputs [51]. This combined methodology is instrumental in linking molecular properties of channels (measured under voltage-clamp) to their direct functional role in cellular computation and signaling (observed under current-clamp).
High-throughput automated patch-clamp systems have been developed that can perform both voltage-clamp and current-clamp recordings, dramatically increasing the screening capacity for drug discovery and basic research [51] [55]. These systems are advancing to include features like temperature control and dynamic clamp, further bridging the gap between controlled experiments and physiological conditions [55]. Furthermore, computational modeling is increasingly used to interpret and correct for inherent artifacts in voltage-clamp recordings, such as those arising from incomplete series resistance compensation, ensuring more accurate biophysical characterization of ion channels, particularly those with fast kinetics like NaV1.5 [52].
Modern neuroscience research into neuronal activity measurement increasingly relies on the multimodal integration of complementary techniques. Electrophysiology provides high-temporal-resolution readouts of electrical signals, calcium imaging offers spatially resolved monitoring of population activity, and optogenetics enables precise, cell-type-specific manipulation of neural circuits. Used in isolation, each method provides a limited view of neural function; however, their combined application offers a more comprehensive picture of brain activity. This Application Note details current protocols and technical solutions for successfully integrating these advanced methods, framed within the context of a broader thesis on electrophysiology methods for neuronal activity measurement research. The content is designed for researchers, scientists, and drug development professionals seeking to implement these powerful combinatorial approaches in their experimental workflows.
The Scientist's Toolkit: Core Technologies and Reagents
Successful integration of optogenetics, calcium imaging, and electrophysiology requires careful selection of hardware, software, and biological reagents. The table below summarizes essential components for establishing a multimodal experimental pipeline.
Table 1: Research Reagent Solutions and Essential Materials for Multimodal Neuroscience
| Item Category | Specific Examples | Function & Application |
|---|---|---|
| Optogenetic Actuators | Channelrhodopsin-2 (ChR2), Chrimson, ChRmine [58] | Light-sensitive ion channels for neuronal excitation; ChR2 (blue light-activated) for millisecond-scale control, red-shifted variants (Chrimson, ChRmine) for deeper tissue penetration and dual-wavelength experiments. |
| Calcium Indicators | GCaMP6s, GCaMP7 [59] [60] [61] | Genetically Encoded Calcium Indicators (GECIs); fluorescence changes correspond to neuronal activity, enabling population-wide activity monitoring. |
| Integrated Electrophysiology-Optogenetics Probes | Neuropixels Opto [58] | Combines 960 electrical recording sites with 28 integrated light emitters (14 blue @ 450nm, 14 red @ 638nm) on a single shank for simultaneous recording and spatially addressable optogenetic manipulation. |
| High-Density Recording Systems | High-Density Microelectrode Arrays (HD-MEAs) [41] | In vitro platforms with thousands of electrodes for large-scale, long-term recording of neural networks at subcellular to network scales. |
| Implantable Wireless Systems | FIMOSS [62] | Fully Implantable Multisite Optogenetic Stimulation System; a wireless, battery-free, chronic implant for long-term optogenetic studies in behaving mice. |
| Real-Time Software Platforms | Improv [61] | A modular software platform for orchestrating adaptive, closed-loop experiments by integrating real-time data acquisition, analysis, and experimental control. |
Quantitative Comparison of Integrated Methodologies
Different experimental goals require specific technical approaches. The quantitative profiles of leading technologies for integrated measurement and manipulation are detailed below.
Table 2: Quantitative Profile of Integrated Electrophysiology-Optogenetics Platforms
| Parameter | Neuropixels Opto Probe [58] | FIMOSS (Chronic Implant) [62] | HD-MEA (in vitro) [41] |
|---|---|---|---|
| Primary Use Case | Large-scale in vivo recording & manipulation | Chronic wireless stimulation in behaving mice | High-throughput in vitro screening & network analysis |
| Recording Sites | 960 (384 simultaneously recorded) | N/A (Stimulation-focused) | Up to 236,880 electrodes (e.g., 5.51x5.91 mm² area) |
| Stimulation Capability | 28 emitters (14 blue, 14 red) | 4-channel μLED cuff | Electrical stimulation via electrodes |
| Spatial Resolution | 100 μm emitter spacing, 20 μm vertical site spacing | Sub-nerve fascicle resolution (~250 μm) | Subcellular (electrode pitch < 12 μm) |
| Key Innovation | On-chip photonic waveguides for dual-color light delivery | Fully implantable, wireless, and programmable | Massive parallelization for "electrical imaging" |
| Typical Experiment Duration | Acute or semi-chronic | Long-term (validated for 12+ weeks) | Long-term (days to months) |
Table 3: Performance Characteristics of Calcium Imaging Components
| Component | Parameter | Value / Description | Notes |
|---|---|---|---|
| GCaMP6s Indicator [59] [61] | Signal-to-Noise | High | Standard for detecting individual action potentials |
| Kinetics | Moderate-Fast | Suitable for tracking population dynamics in vivo | |
| Deep Generative Models (e.g., SVAE, GPVAE) [59] | Primary Function | Dimensionality reduction & batch effect correction | Enables integration of data across sessions and specimens |
| Advantage vs. PCA | Preserves biological variability while mitigating technical artifacts | Superior for clustering and visualizing single-neuron dynamics | |
| Real-Time Analysis (Improv + CaImAn) [61] | Processing Speed | Up to 3.6 Hz frame rate demonstrated | Enables closed-loop experimental designs |
Experimental Protocols
Protocol: Integrated In Vivo Electrophysiology and Optogenetics with Neuropixels Opto
This protocol describes the simultaneous acquisition of high-resolution neural activity and cell-type-specific manipulation in the mouse brain using the Neuropixels Opto probe.
Materials:
- Neuropixels Opto probe (Version 2) [58]
- Transgenic mouse line with Cre-dependent opsin expression (e.g., Ai32 for ChR2)
- Viral vector for targeted opsin delivery (e.g., AAV5-EF1a-DIO-ChRmine) [58]
- Stereotaxic surgical apparatus
- Lasers (450 nm blue and 638 nm red) with fiber coupling
- Data acquisition system (SpikeGLX or Open Ephys GUI) [58]
Method:
- Animal Preparation and Viral Injection:
- Anesthetize the mouse and secure it in a stereotaxic frame.
- Inject 200-500 nL of AAV5-EF1a-DIO-ChRmine into the target brain region (e.g., striatum) at a rate of 100 nL/min. Allow 3-6 weeks for robust opsin expression.
Probe Implantation and Setup:
- Calibrate the photonic switching tree of the Neuropixels Opto probe. For high-intensity, precise experiments, prioritize the red light emitters due to their greater stability [58].
- Position the probe for the target brain region. The 1.4 mm span of emitters allows manipulation across multiple anatomical layers or structures.
- Connect the optical fiber cable (for lasers) and the digital data cable to the headstage.
Data Acquisition and Optogenetic Manipulation:
- In the acquisition software (e.g., SpikeGLX), configure the recording settings: 30 kHz sampling for the Action Potential (AP) band and 2.5 kHz for the Local Field Potential (LFP) band.
- Define the stimulation protocol. For optotagging: deliver 1-2 second light pulses (1-5 mW per emitter) through selected emitters while recording. For causal testing: use patterned stimulation (e.g., 10-50 ms pulses) during specific behavioral epochs.
- Simultaneously record extracellular activity from 384 selected channels while executing the light delivery protocol.
Data Analysis:
- Sort spikes from recorded data to isolate single units.
- Identify optotagged neurons by calculating the change in firing rate in response to light stimulation across trials. A short-latency, reliable response confirms direct opsin expression.
- Analyze how stimulation of specific neuronal populations alters the firing patterns of non-tagged cells across the recorded network to infer circuit-level effects.
Protocol: Real-Time Closed-Loop Experiments with Calcium Imaging and Optogenetics
This protocol leverages the Improv software platform to create an adaptive experiment where real-time analysis of calcium imaging data dictates optogenetic intervention.
Materials:
- Two-photon or epifluorescence microscope
- Improv software platform [61]
- Optogenetic setup (laser and targeting system)
- Animal model (e.g., larval zebrafish or mouse) expressing GCaMP6s and an opsin.
Method:
- System Configuration:
- Install and configure the Improv platform. Define the processing pipeline using a text-based configuration file.
- Key "Actors" to include in the pipeline: an "Image Acquirer" to stream calcium images, "CaImAn Online" for real-time ROI extraction and trace deconvolution, a "Model Fitting" actor (e.g., for LNP models), and a "Stimulation Controller" actor that triggers the laser based on model output [61].
Real-Time Processing and Model Fitting:
- Stream calcium images into Improv. The "CaImAn Online" actor will identify active neurons and extract their fluorescence traces.
- The "Model Fitting" actor will continuously receive these traces. For example, fit a Linear-Nonlinear-Poisson (LNP) model to the most recent 100 frames of data to estimate each neuron's visual receptive field or functional connectivity [61].
- The model's parameters are updated in real-time using stochastic gradient descent as new data arrives.
Closed-Loop Control:
- Define the control logic within the "Stimulation Controller" actor. For instance: "If Neuron N's activity exceeds threshold X, deliver a 100 ms optogenetic pulse to Population Y within 50 ms."
- The actor receives the real-time activity and model data from the shared data store and sends commands to the laser driver.
- This allows for interventions such as silencing neurons the moment they become part of a specific assembly or testing the causal role of a newly identified functional connection.
Monitoring and Validation:
- Use Improv's integrated GUI to monitor raw data streams, processed traces, and model outputs in real time.
- After the experiment, validate the real-time analysis against offline benchmarks to ensure fidelity.
Protocol: Chronic Peripheral Nerve Interfacing with FIMOSS
This protocol outlines the use of a fully implantable wireless system for long-term optogenetic evaluation of nerve function and recovery in mice, suitable for studies modeling nerve injury or surgical repair.
Materials:
- Thy1-ChR2-EYFP transgenic mouse
- FIMOSS implant [62]
- Surgical equipment for nerve exposure and implantation
Method:
- Device Preparation:
- Ensure the FIMOSS implant is sterilized and functionally tested. The device should be wirelessly powered and respond to command programming.
Surgical Implantation:
- Anesthetize the mouse and perform a pectoralis major incision to access the brachial plexus.
- Carefully place the MOSD II cuff optrode around the target nerve trunk (e.g., C7 nerve). The cuff should encircle the nerve without constriction.
- Position the driver module subcutaneously on the ipsilateral chest wall. Suture the device in place to prevent migration.
- Close the surgical incision.
Long-Term Evaluation:
- Over 12 weeks, periodically wirelessly program the implant to stimulate different nerve fascicles using the four integrated μLEDs.
- Record compound muscle action potentials (CMAPs) via electromyography and observe forelimb movements to assess functional output.
- In nerve transfer models, track the temporal changes in innervation patterns of the transferred and adjacent nerves to map functional reorganization [62].
Integrated Workflow and Data Integration Strategy
The true power of these methods is realized when they are combined into a single, cohesive experimental and analytical workflow. The following diagram and description outline a comprehensive strategy for a causal in vivo circuit analysis.
This workflow begins with large-scale calcium imaging (e.g., using GCaMP6s) to monitor thousands of neurons simultaneously in a behaving animal, identifying populations correlated with a specific behavior or cognitive state [60] [61]. The functional properties of these candidate neurons (e.g., tuning to sensory stimuli) are further characterized. Subsequently, high-density electrophysiology, such as with a Neuropixels Opto probe, is employed to record the same neurons with superior temporal resolution and to identify network interactions [58]. Based on this functional map, a causal hypothesis is formulated. Finally, optogenetic manipulation is applied—using the integrated emitters on the Neuropixels Opto probe or a separate FIMOSS implant—to activate or inhibit the identified populations while continuing electrophysiological recording to observe the direct causal effects on both local circuit dynamics and behavior [62] [58]. This iterative process of observation, perturbation, and measurement leads to robust, causally supported circuit models.
Electrophysiology provides a direct window into the electrical communication of neurons, making it indispensable for understanding the mechanisms underlying neurological diseases. By measuring ion fluxes, action potentials, and local field potentials, these techniques enable researchers to decode how neural signaling becomes disrupted in pathological conditions. The ability to record from single neurons to entire networks across temporal scales from milliseconds to months allows for comprehensive investigation of disease progression and therapeutic interventions [63] [64]. This application note details specific protocols and experimental designs employing electrophysiology to study epilepsy, Parkinson's disease, and neuropathic pain, providing a standardized framework for researchers in academic and drug development settings.
Epilepsy Research
Background and Pathophysiology
Epilepsy is characterized by recurrent, spontaneous seizures resulting from abnormal, hyper-synchronous neuronal activity. Focal epilepsies originate in a restricted brain region, the epileptic focus (EF), but frequently involve the recruitment of remote brain regions into a large-scale epileptic network (EN). Research using high-density electrophysiology has demonstrated that during epileptogenesis, the brain undergoes significant functional reorganization. Beyond the EF, generalized spikes (GSs) emerge that propagate across the brain in a highly stable spatiotemporal pattern [65]. Furthermore, pathological fast ripples, once considered specific to the EF, also appear in remote cortical regions. Crucially, these remote interictal activities are dependent on the focus early in the disease but become self-sustaining after the chronic stage is established, continuing even after focus silencing [65]. This network perspective is essential for understanding why surgical resection of the preoperatively identified focus may not always control seizures [65].
Key Experimental Findings and Quantitative Data
Table 1: Key Electrophysiological Findings in the Kainate Mouse Model of Temporal Lobe Epilepsy
| Electrophysiological Event | Spatial Localization | Disease Stage | Dependence on EF | Associated Behavioral Manifestation |
|---|---|---|---|---|
| Focal Spikes | Injected Hippocampus (EF) | Latent & Chronic | Always dependent | None directly observed |
| Generalized Spikes (GSs) | Bilateral Hippocampus & Frontal Cortices | Emerges during latent phase | Early: DependentChronic: Independent | Often concomitant with muscular twitches |
| Fast Ripples (FRs) | EF and Remote Cortical Regions (e.g., Frontal) | Chronic | Early: DependentChronic: Independent (in remote areas) | Not specified |
Detailed Protocol: In Vivo Investigation of Epileptic Networks
Objective: To characterize the development of large-scale epileptic networks in a mouse model of unilateral temporal lobe epilepsy (TLE) using combined high-density surface EEG and intracortical recordings [65].
Materials and Reagents:
- Animals: Adult male C57BL/6j mice.
- Anesthesia: Isoflurane system (induction 2.5%, maintenance 1–1.5%).
- Stereotaxic Frame: With heating pad and rectal temperature probe.
- Kainate: Unilateral injection into the dorsal hippocampus to induce status epilepticus and subsequent TLE.
- Electrodes: High-density epicranial electrode grids and intracortical depth electrodes.
- Head-Holder: Custom aluminum ring fixed with dental cement.
- Recording System: Amplifiers and software for simultaneous video and multi-channel electrophysiology.
Procedure:
- Surgical Preparation: Anesthetize the mouse and secure it in a stereotaxic frame. Maintain body temperature at 37°C.
- Electrode Implantation: Retract the skin and mark electrode positions on the skull. Apply a thin layer of Loctite to the skull. After drying, drill small patches (500 µm diameter) at each electrode location to improve electrical contact.
- Head-Holder Fixation: Fix an aluminum ring-like head-holder to the occipital and nasal bones using dental cement. Fill the center of the ring with silicon and allow the animal to recover.
- Kainate Injection: Perform a unilateral injection of kainate into the dorsal hippocampus to induce status epilepticus.
- Longitudinal Recording: Conduct repeated recording sessions from pre-injection (control) to chronic stages (e.g., D7, D14, D28 post-injection) in awake, behaving animals.
- Pharmacological Silencing: At selected time points (e.g., D7 and D28), pharmacologically silence the EF to test the dependence of remote network activities.
- Data Analysis:
- Identify and classify interictal epileptic discharges (IEDs): Focal Spikes vs. Generalized Spikes (GSs).
- Detect pathological fast ripples in the EF and remote regions.
- Analyze the spatiotemporal propagation patterns of GSs.
- Correlate electrophysiological events with simultaneous video recordings of behavior.
Visualizing the Epileptic Network Workflow
Parkinson's Disease Research
Background and Pathophysiology
Parkinson's disease (PD) is a neurodegenerative disorder characterized by the loss of dopaminergic neurons in the substantia nigra pars compacta. From an electrophysiological perspective, PD is viewed as a disorder of deranged neural rhythms in the cortico-subcortical re-entrant loops [66]. A central element is the subthalamic nucleus (STN), which exhibits a pathologically excessive burst discharge pattern in the dopamine-deprived state. These bursts are not fully autonomous but often rely on glutamatergic synaptic inputs from the motor cortex (MC) via the "hyperdirect" pathway, constituting a "relay burst mode" [66]. This aberrant activity contributes to both hypokinetic (bradykinesia, rigidity) and hyperkinetic (tremor) symptoms, and is a primary target for deep brain stimulation (DBS) therapy.
Key Experimental Findings and Quantitative Data
Research utilizing combined magnetoencephalography (MEG) and local field potential (LFP) recordings from DBS electrodes in the STN has provided unique insights into subcortico-cortical networks in PD. This approach allows for the simultaneous capture of cortical and deep brain activity, facilitating the study of network dynamics [67]. Furthermore, in vitro models using patient-derived neurons have begun to reveal early electrophysiological alterations, such as hyperexcitability in medium spiny neurons with GBA-N370S mutations [68].
Table 2: Electrophysiological Signatures in Parkinson's Disease Models
| Model / Approach | Key Electrophysiological Finding | Technical Method | Therapeutic / Pathophysiological Insight |
|---|---|---|---|
| In Vivo (Patients) | Excessive burst discharges in STN; Enhanced beta power in LFP; ~4-6 Hz coherence for tremor. | Simultaneous MEG & STN-LFP [67], DBS recording [66] | DBS ameliorates symptoms by disrupting pathological rhythms. |
| In Vitro (Patch-Clamp) | DA depletion downregulates HCN channels in GPe [66]; αSyn aggregation increases AP threshold [68]; GBA mutation causes early hyperexcitability. | Patch-clamp on slices, SH-SY5Y cells, hiPSC-derived neurons [68] | Identifies early cellular dysfunction and potential ion channel targets. |
| In Vitro (MEA) | Network-level synchrony and oscillation disruptions. | MEA on hiPSC-derived neural cultures & organoids [68] | Enables drug screening on patient-specific neural networks. |
Detailed Protocol: Combined MEG and Deep Brain LFP Recording in PD Patients
Objective: To investigate the functional connectivity between the subthalamic nucleus (STN) and the cortex in individuals with Parkinson's disease during rest and motor tasks, in both medicated and unmedicated states [67].
Materials and Reagents:
- Participants: PD patients implanted with STN DBS electrodes (e.g., 20 patients, median age 63).
- MEG System: 306-channel whole-head MEG system (e.g., VectorView, MEGIN).
- LFP Recording Setup: Custom, non-ferromagnetic extension cables for DBS electrodes to connect to MEG amplifiers.
- Physiological Monitoring: Electro-oculogram (EOG) electrodes, electromyogram (EMG) for forearm flexor/extensor muscles.
- Software: Pre-processing and source analysis software (e.g., FieldTrip in MATLAB).
Procedure:
- Patient Preparation: Conduct recordings the day after DBS electrode implantation, before stimulator implantation. Withdraw dopaminergic medication on the evening before the OFF-state recording.
- Sensor Setup: Connect the externalized DBS electrodes to the MEG system's amplifiers via the custom extensions. Attach EOG and EMG electrodes according to standard placements.
- Medication OFF State Recording:
- Verify the OFF state using the Unified Parkinson's Disease Rating Scale (UPDRS) part III.
- Record resting-state brain activity for several minutes.
- Perform task-based recordings:
- HOLD Task: Patient elevates the more affected forearm and holds the position for multiple trials (~300s total).
- MOVE Task: Patient performs self-paced repetitive fist-clenching with the more affected hand (~300s total).
- Medication ON State Recording:
- Administer 1.5 times the patient's usual levodopa morning dose.
- Wait for clear motor improvement (≥30 minutes, confirmed by UPDRS items).
- Repeat the resting-state and task-based recordings (HOLD and MOVE).
- Data Acquisition: Acquire data at a sampling rate of 2 kHz. Apply online band-pass filtering (MEG: 0.03–660 Hz; LFP/EMG: 0.1–660 Hz).
- Data Pre-processing:
- Visually inspect data and discard artifact-contaminated segments.
- Re-reference LFP signals using a bipolar scheme (subtracting signals from neighboring contacts on the same electrode).
- Apply a 1 Hz high-pass filter to remove slow drift.
- Down-sample data as needed for specific analyses.
Visualizing PD Circuit Dysfunction and Recording Setup
Neuropathic Pain Research
Background and Pathophysiology
Neuropathic pain (NP) arises from a lesion or disease of the somatosensory nervous system. Electrophysiology serves as a core technology to resolve the mechanisms of aberrant signal generation and transmission at molecular, cellular, and network levels [69]. Key research areas include the investigation of ion channel function, neuronal excitability, and neuroplasticity in dorsal root ganglia and sensory neurons. Recent bibliometric analyses show a shift in research focus toward "plasticity" and "connectivity," signaling a move to understand network mechanisms and develop precise interventions [69]. The emergence of concepts like the "dynamic pain connectome" and the use of computational modeling reflect a trend of multidisciplinary integration in the field.
Key Experimental Findings and Research Trends
Studies employing advanced electrophysiological techniques like patch-clamp recording have been pivotal in linking ion channel dysfunction and neuronal hyperexcitability to neuropathic pain states. Research published in high-impact journals has utilized these methods to deeply explore alterations in ion channel function associated with neuralgia, laying the foundation for precise interventions based on electrophysiological phenotypes [69]. The field is increasingly moving toward individualized treatment strategies based on specific electrophysiological signatures.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Neurological Disease Electrophysiology
| Item | Function / Application | Example Context |
|---|---|---|
| Neuropixels Probes | High-density silicon probes for large-scale, single-neuron recording across many brain areas. | Brain-wide neural activity mapping in behaving mice [70]. |
| High-Density Microelectrode Arrays (HD-MEAs) | In vitro platform for non-invasive, long-term recording of extracellular field potentials and spike activity from neural networks. | Drug screening and network analysis in hiPSC-derived models of PD [63] [68]. |
| Deep Brain Stimulation (DBS) Electrodes | Provide direct access to record local field potentials (LFPs) from deep brain structures in human patients. | STN LFP recording in PD patients [67] [66]. |
| Induced Pluripotent Stem Cells (hiPSCs) | Generate patient-specific neurons and organoids for in vitro disease modeling. | Studying electrophysiological properties of PD neurons with LRRK2 or GBA mutations [68]. |
| Kainic Acid | Glutamate receptor agonist used to induce status epilepticus and temporal lobe epilepsy in rodent models. | Mouse model of TLE for studying epileptogenesis [65]. |
| Patch-Clamp Rig | Gold-standard technique for high-resolution recording of ionic currents and action potentials from single cells. | Characterizing intrinsic excitability and synaptic transmission in pain pathways and PD models [69] [68]. |
Cardiac safety pharmacology is a critical discipline in drug development, dedicated to identifying compounds with potential adverse effects on the heart, particularly those increasing the risk of lethal arrhythmias such as Torsade de Pointes (TdP) [71]. For decades, the assessment of a drug's potential to block the human Ether-à-go-go-Related Gene (hERG) potassium channel has been the cornerstone of this field, as hERG block is the most common mechanism underlying drug-induced QT interval prolongation [72]. However, reliance solely on hERG data has led to the discontinuation of potentially valuable drugs because the assay possesses limitations in specificity.
The Comprehensive in vitro Proarrhythmia Assay (CiPA) initiative represents a paradigm shift from this single-target approach. Launched in 2013 and overseen by an international consortium of regulators, academics, and industry representatives [73], CiPA aims to engineer a more holistic and physiologically relevant assessment of proarrhythmic potential [74]. This new framework integrates multiple sources of information, including multi-ion channel screening, in silico modeling of human ventricular electrophysiology, and verification using human stem cell-derived cardiomyocytes [73] [74]. This application note details the established protocols for the hERG assay and situates them within the innovative, integrated framework of the CiPA initiative, highlighting its relevance for researchers using electrophysiological methods across fields, including neuronal activity measurement.
The hERG Assay: Application Notes and Protocols
Background and Principles
The hERG channel mediates the rapid delayed rectifier potassium current (IKr), which is essential for the repolarization phase of the cardiac action potential [74]. Pharmacological blockade of this channel delays repolarization, prolonging the QT interval on the surface electrocardiogram (ECG), and can precipitate TdP [72]. Consequently, the ICH S7B guideline mandates testing for hERG block for all new chemical entities [72]. The manual patch-clamp technique remains the gold-standard method for assessing compound effects on hERG channel current due to its high fidelity and direct measurement of ionic currents.
Detailed Experimental Protocol
The following protocol for manual patch-clamp hERG assays is based on multi-laboratory studies conducted in accordance with ICH S7B Q&A 2.1 best practices [72].
Key Research Reagent Solutions
Table 1: Essential Reagents and Materials for hERG Assay
| Item | Specification/Composition | Function/Purpose |
|---|---|---|
| Cell Line | hERG1a-transfected HEK 293 or CHO cells | Provides a consistent, high-expression system for studying hERG channel pharmacology. |
| External Solution | 130 mM NaCl, 5 mM KCl, 1 mM MgCl₂, 1 mM CaCl₂, 10 mM HEPES, 12.5 mM Dextrose; pH 7.4 with NaOH | Mimics the extracellular ionic environment to maintain physiological channel gating. |
| Internal (Pipette) Solution | 120 mM K-gluconate, 20 mM KCl, 10 mM HEPES, 5 mM EGTA, 1.5 mM MgATP; pH 7.3 with KOH | Mimics the intracellular environment and provides essential components for channel function. |
| Drug Stock Solutions | Prepared in DMSO or appropriate vehicle, with final vehicle concentration ≤ 0.3% | Enables solubilization and application of test compounds at known concentrations. |
| Positive Control | e.g., Cisapride, Dofetilide | A known hERG blocker used to validate assay sensitivity and performance. |
Step-by-Step Methodology
- Cell Preparation: Culture hERG-transfected cells (e.g., HEK 293) using standard procedures. On the day of recording, harvest cells using gentle dissociation reagents to ensure viable, single cells with intact ion channels.
- Electrophysiology Setup: Transfer a cell suspension to the recording chamber continuously perfused with pre-warmed (35–37°C) external solution. Place the recording chamber on the stage of an inverted microscope.
- Patch-Clamp Establishment: Fire-polish a borosilicate glass pipette (2-4 MΩ resistance) and fill it with internal solution. Use a micromanipulator to position the pipette onto a cell membrane. Apply gentle suction to form a high-resistance seal (>1 GΩ), then rupture the membrane patch beneath the pipette tip to achieve whole-cell configuration.
- Voltage Protocol and Baseline Recording: Continuously perfuse the cell with external solution at a flow rate of 1-2 mL/min. Apply a standard voltage-clamp protocol to elicit hERG current. A common protocol involves:
- Holding at -80 mV.
- Stepping to +20 mV for 2 seconds to activate and inactivate the channels.
- Stepping to -50 mV for 4 seconds to elicit the large, characteristic tail current as channels recover from inactivation.
- Repeat this protocol every 10-15 seconds. Record a stable baseline for at least 3-5 minutes.
- Compound Application: After obtaining a stable baseline, apply the test compound sequentially in increasing concentrations. For each concentration, perfuse the cell for a sufficient duration to reach a steady-state block (typically 3-5 minutes). It is critical to verify final drug concentrations in the recording chamber via bioanalysis where possible, as drug loss to tubing and chambers can occur [72].
- Data Acquisition and Analysis: Record the hERG tail current amplitude at -50 mV for each sweep. Normalize the current amplitude in the presence of drug to the baseline amplitude. Plot the normalized current against the log of the drug concentration and fit the data with a Hill equation to calculate the half-maximal inhibitory concentration (IC50).
Data Interpretation and Variability
A key outcome of the hERG assay is the calculation of a safety margin, defined as the IC50 divided by the maximum free therapeutic plasma concentration (or relevant clinical exposure) [72]. Multi-laboratory studies have quantified the inherent variability of the manual patch-clamp hERG assay. When standardized protocols and best practices are followed, the within-laboratory variability for testing the same drug is approximately 5-fold [72]. Therefore, hERG block potency values (IC50) differing by less than 5-fold should not be considered biologically significant, as they fall within the assay's natural data distribution.
Table 2: Key Sources of Variability in hERG Assays
| Factor | Impact on hERG IC50 | Best Practice Recommendation |
|---|---|---|
| Recording Temperature | Room temperature increases IC50 vs. physiological (35-37°C) | Record at near-physiological temperature (35-37°C) [72]. |
| Stimulation Frequency | Different pacing rates can alter state-dependent block | Use a physiologically relevant stimulation frequency [72]. |
| Voltage Protocol | Waveform design affects channel state occupancy | Adopt a standardized protocol (e.g., FDA-recommended). |
| Drug Loss/Adsorption | Can lead to overestimation of IC50 | Verify chamber concentrations via bioanalysis [72]. |
| Cell Line & Culture | Different expression systems can influence pharmacology | Use a well-characterized, stable cell line. |
The CiPA Initiative: An Integrated Framework
From Single Target to Systems-Level Assessment
While hERG block is a common risk factor, it is not solely predictive of clinical TdP risk. The CiPA initiative was proposed to address this limitation by evaluating a compound's integrated electrophysiological effects across multiple key cardiac ion channels [73]. The core hypothesis is that a drug's overall proarrhythmic potential depends on the net effect of its ion channel block profile, which can be accurately predicted using in silico models of human ventricular cardiomyocytes [74].
The Four Components of CiPA
The CiPA strategy is built on four synergistic work streams [73] [74]:
- Ion Channel Profiling: Quantitatively assess the effects of a drug on multiple human cardiac ion currents (e.g., hERG/IKr, late INa, ICaL, IKs, IK1) at physiological temperature using high-throughput automated patch-clamp systems.
- In Silico Modeling: Integrate the concentration-response data from ion channel profiling into a computer model (a "virtual cardiac myocyte") to simulate the drug's effect on the human ventricular action potential. The model predicts whether the ion channel profile is likely to be proarrhythmic.
- Human Stem Cell-Derived Cardiomyocytes (hSC-CMs): Experimentally verify the in silico predictions using in vitro cultures of hSC-CMs. These cells express the full complement of human ion channels and can provide a holistic, physiologically relevant readout of compound effects on field potentials and/or action potentials.
- Clinical ECG Analysis: Re-evaluate existing clinical ECG data from new and legacy drugs to validate and refine the overall CiPA paradigm.
CiPA Workflow and Electrophysiological Integration
The following diagram illustrates how the components of CiPA integrate electrophysiological data across scales, from single channels to cellular networks—a concept highly familiar to neuroscientists mapping neuronal activity.
Advanced Tools and Cross-Disciplinary Relevance
The evolution of cardiac safety screening shares a strong technological synergy with modern neuroscience. Both fields rely on advanced electrophysiological tools to decode complex cellular and network-level communication.
- High-Density Microelectrode Arrays (HD-MEAs): Originally driven by neuroscience and brain-computer interface research [63], HD-MEAs are now pivotal in CiPA's verification phase. These arrays, featuring thousands of electrodes, allow for non-invasive, long-term recording of field potentials and spike propagation in hSC-CM cultures or even 3D cardiac tissues with single-cell resolution [63]. This is directly analogous to their use in mapping neural activity in brain organoids [75].
- In Silico Modeling: The mechanistic models of cardiac electrophysiology used in CiPA have a rich heritage, originating from the Hodgkin-Huxley equations developed for neuronal axons [74]. These models provide a quantitative framework to integrate data and predict emergent behavior, whether it's a cardiac action potential or neuronal spiking.
- Standardized Graphical Representations: Just as the neuroscience community has proposed "Neural Schematics" to unify the graphical representation of neural network structures [76], the cardiac safety field benefits from standardized workflows and data representation to ensure clarity and reproducibility across disciplines and laboratories.
The journey from the targeted hERG assay to the integrated CiPA framework exemplifies the evolution of safety pharmacology towards a more comprehensive and mechanistic paradigm. For drug development professionals, adhering to standardized hERG protocols while embracing the multi-parametric CiPA approach will lead to more accurate prediction of clinical cardiac risk. For researchers specializing in electrophysiology, the tools and concepts highlighted—from HD-MEAs to in silico modeling—demonstrate a powerful cross-pollination between cardiac and neural sciences, enabling deeper insights into the function of all electrogenic tissues.
#LabHacks: Proven Strategies for Robust and High-Quality Recordings
Within the field of neuronal activity measurement research, the quality of electrophysiological data is fundamentally constrained by the health of the ex vivo tissue preparations from which recordings are made. Achieving high-quality patch-clamp recordings or obtaining clear signals on high-density microelectrode arrays (HD-MEAs) begins long before the electrode is positioned; it starts with the meticulous preparation of acute brain slices [63] [77]. A well-prepared slice ensures that neurons remain viable, maintain their physiological properties, and are suitable for sophisticated experimental interrogation. This application note details standardized, optimized protocols for the dissection, slicing, and incubation of acute brain slices, framing them within the context of a broader methodology for reliable neuronal electrophysiology.
The primary challenge in maintaining brain tissue ex vivo is meeting its high metabolic demand, particularly its need for oxygen, without the support of intact vasculature [78]. Furthermore, the process of dissection and slicing induces significant trauma, leading to cellular damage, excitotoxicity, and the release of inflammatory mediators, all of which can compromise tissue health and experimental outcomes. The protocols described herein are designed to systematically minimize this damage at each stage, from rapid and careful dissection to optimized incubation using advanced perfusion techniques, thereby providing a foundation for robust and reproducible research.
Comprehensive Protocols for Tissue Preparation
Protocol 1: Mouse Brain Dissection and Slicing for Electrophysiology
This protocol provides a step-by-step guide for the preparation of acute brain slices, a critical foundation for electrophysiological investigations such as patch-clamp recording [77].
Key Solutions and Reagents:
- Carbogen (95% O₂ / 5% CO₂): Used for bubbling solutions to maintain proper oxygenation and pH (approximately 7.4) [77].
- Ice-cold Cutting Solution: A sucrose-based solution containing low Ca²⁺ (0.1 mM) and high Mg²⁺ (3 mM) to suppress synaptic activity and reduce excitotoxicity during the slicing process [77].
- Artificial Cerebrospinal Fluid (ACSF): Used for incubation and recording. Its ionic composition mimics that of native CSF.
Methodology:
- Preparation: Prepare and thoroughly bubble the ice-cold cutting solution with carbogen for at least 15-20 minutes prior to dissection. Pre-cool all necessary tools and the stage of the vibratome (e.g., a Compresstome). Fill the incubation chamber with the chosen incubation solution and pre-warm it to 37°C [77].
- Rapid Dissection: Euthanize the mouse according to approved institutional guidelines. Quickly decapitate and remove the brain into a petri dish containing ice-cold, carbogenated cutting solution. The entire process from decapitation to brain immersion should be completed in less than 60 seconds to minimize anoxia.
- Embedding and Sectioning: Gently affix the brain to the vibratome stage using cyanoacrylate glue. Submerge the tissue in the ice-cold, carbogenated cutting solution. Cut brain slices to the desired thickness (typically 300-400 μm for patch-clamp) using a slow, controlled advance speed and appropriate vibration frequency. These parameters must be optimized to balance slice yield with minimal tissue damage [77].
- Slice Transfer: Immediately after cutting, use a wide-bore transfer pipette (e.g., a modified plastic pipette) to gently move the slices to the pre-warmed incubation chamber filled with standard ACSF [77].
Troubleshooting:
- Poor Neuronal Viability: Ensure solutions are correctly prepared and vigorously bubbled with carbogen. Minimize the time between dissection and slice incubation.
- Torn or Compressed Slices: Check the sharpness of the vibratome blade and ensure the brain is securely and correctly mounted to prevent movement during sectioning.
Protocol 2: Advanced Bubble Perfusion Incubation for Ex Vivo Tissue
For extended experiments requiring precise control of the cellular microenvironment, traditional static incubation can be superseded by advanced microfluidic perfusion systems [78]. The following protocol describes a "bubble perfusion" system, which uses segmented flows of media droplets separated by oxygen bubbles to simultaneously deliver nutrients and high concentrations of oxygen to ex vivo brain slices.
Key Solutions and Reagents:
- Warm ACSF (36.8 ± 0.13 °C): Serves as the perfusion media [78].
- Hydrogel Glue (Chitosan hydrochloride / Dextran dialdehyde): A biocompatible adhesive used to immobilize tissue slices on coverslips within the perfusion chamber, preventing movement during fluid flow [78].
- Propidium Iodide: A fluorescent dye used for end-point assessment of cell membrane integrity and tissue health [78].
Methodology:
- Device Preparation: The bubble perfusion device, which can be fabricated using consumer-grade 3D printing technology (e.g., using BioMed Clear resin), must be thoroughly rinsed and sterilized prior to use [78].
- Tissue Immobilization: Immobilize the acute brain slice (400-500 μm thick) on a GelBond film coverslip using the two-part hydrogel glue. Seal the coverslip onto the device's tissue chamber, which has a typical internal volume of 19 μL [78].
- System Operation: Utilize a custom valving system to deliver on-demand, metered volumes of oxygen bubbles and warm ACSF droplets (e.g., 30 μL volume) to the tissue chamber. The oxygen bubbles act as temporary reservoirs of gas, enhancing oxygen diffusion into the tissue [78].
- Viability Assessment: After the experiment (e.g., up to 12 hours of perfusion), assess tissue health by performing propidium iodide staining. Healthy tissue preparations have demonstrated that approximately 60% of cells in entorhinal cortex and suprachiasmatic nucleus tissue show no sign of membrane damage after 12 hours of perfusion [78].
Troubleshooting:
- Inconsistent Perfusion: Check for blockages in the microfluidic channels and ensure the valving system is functioning correctly.
- Temperature Instability: Verify the temperature of the prewarming chambers and the circulating water system that maintains the device at physiological temperature.
Quantitative Data and Analysis
Table 1: Key Quantitative Parameters from the Bubble Perfusion Protocol [78]
| Parameter | Value | Significance |
|---|---|---|
| Tissue Chamber Volume | 19 μL | Defines the microenvironment volume surrounding the slice. |
| Droplet Volume | 30 μL | Volume of media delivered per perfusion event. |
| Perfusion Temperature | 36.8 ± 0.13 °C | Maintains physiological temperature for cellular function. |
| Temperature Drift (over 60s) | 0.5 ± 0.09 °C | Indicates high thermal stability during droplet exposure. |
| Viable Cells after 12h (PI stain) | ~60% | Demonstrates the system's efficacy for long-term tissue maintenance. |
Table 2: Electrophysiology Tools for Functional Validation of Tissue Health
| Technology | Key Feature | Application in Tissue Health Validation |
|---|---|---|
| High-Density Microelectrode Arrays (HD-MEAs) [63] | High spatiotemporal resolution; can record from thousands of sites simultaneously. | Monitoring network-wide action potential and local field potential dynamics to assess functional connectivity and health. |
| Neuropixels Ultra Probes [79] | Ultra-high site density (6 μm spacing). | Improved detection of single neurons and classification of cell types based on waveform features in healthy tissue. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Acute Brain Slice Preparation
| Item | Function / Application |
|---|---|
| Carbogen (95% O₂ / 5% CO₂) [77] | Oxygenates slicing and incubation solutions while maintaining physiological pH. |
| Sucrose-based Cutting Solution [77] | Provides osmotic support and reduces excitotoxicity (via low Ca²⁺/high Mg²⁺) during slicing. |
| Artificial Cerebrospinal Fluid (ACSF) [77] | Ionic solution mimicking cerebrospinal fluid for incubation and electrophysiological recording. |
| Hydrogel Glue (ChitHCl/DDA) [78] | Biocompatible adhesive for immobilizing tissue slices in perfusion devices without toxicity. |
| Propidium Iodide [78] | Fluorescent viability stain for end-point assessment of cell membrane integrity. |
| 3D Printed Microfluidic Perfusion Device [78] | Customizable platform for advanced bubble perfusion incubation of ex vivo tissues. |
Workflow and Signaling Pathway Diagrams
Diagram 1: Experimental workflow for tissue preparation.
Diagram 2: Signaling pathways for functional validation.
The patch-clamp technique stands as a cornerstone of modern electrophysiology, providing an unparalleled window into the function of ion channels and neuronal excitability. The quality of this sophisticated measurement is fundamentally dependent on the interface between the instrument and the cell: the glass micropipette. The process of fabricating these pipettes, a precise science of heating and pulling glass capillaries, directly determines their electrical and physical characteristics. This application note details the critical protocols for mastering micropipette fabrication, focusing on the interplay between pulling parameters, resultant tip resistance, and the ultimate goal of forming high-resistance gigaohm seals. Mastery of these elements is essential for any researcher in neuroscience or drug development aiming to acquire low-noise, high-fidelity recordings of neuronal activity.
The Science of Pulling Micropipettes
Key Pulling Parameters and Their Effects
Micropipette pullers use controlled heat and mechanical force to draw glass capillaries into finely tapered tips. The geometry of the tip—specifically its length, taper, and final diameter—is meticulously governed by the puller's program settings. This geometry, in turn, defines the pipette's electrical resistance, which must be optimized for different experimental configurations [80]. Understanding and adjusting these parameters is both a scientific and an artisanal process [81].
The table below summarizes how adjustments to key parameters on a programmable puller influence the physical characteristics of the resulting pipette.
Table 1: The Effect of Puller Parameters on Micropipette Geometry
| Parameter | Effect of Increasing the Parameter | Effect of Decreasing the Parameter |
|---|---|---|
| Heat | Creates a longer, more gradual taper [81] | Creates a shorter, steeper taper [81] |
| Force | Produces a smaller tip diameter and a longer taper [81] | Produces a larger tip diameter and a shorter taper [81] |
| Distance | Produces a smaller tip diameter [81] | Produces a larger tip diameter [81] |
| Delay | Creates a shorter taper [81] | Creates a longer taper [81] |
Optimizing Pipette Resistance for Experimental Goals
The resistance of the pipette (Rpip) is a critical, easily measurable proxy for its tip diameter and is a primary indicator of its suitability for specific experiments. Consistency in Rpip is a key marker of a well-optimized and reproducible pulling protocol.
Table 2: Target Pipette Resistances for Common Electrophysiology Configurations
| Experimental Configuration | Target Pipette Resistance (MΩ) | Rationale |
|---|---|---|
| Whole-Cell (Somatic) | 2 - 5 MΩ [80] | Lower resistance minimizes series resistance, improving electrical access to the cell interior and voltage control [80]. |
| Single-Channel / Cell-Attached | 5 - 10 MΩ [80] | Higher resistance facilitates the formation of high-resistance seals and reduces pipette tip noise, which is crucial for resolving tiny single-channel currents [80]. |
| Dendritic Recording or In Vivo | 8 - 15 MΩ [82] | Sharper, higher-resistance tips are better suited for accessing small neuronal structures or for navigating tissue in vivo [82]. |
Environmental and Material Considerations
Beyond the programmed parameters, several external factors can affect pull consistency and must be controlled:
- Glass Type: Different types of borosilicate glass capillaries have varying softening points, which will require adjustments to the heat parameter [81]. Even different manufacturing lots of the same glass can exhibit slight variations [81].
- Filament Condition: A puller's filament slowly oxidizes over time, changing its heating characteristics and necessitating periodic recalibration of programs [81].
- Ambient Conditions: Room temperature and humidity can affect heat transfer via convection, meaning a stable laboratory environment is required for reproducible results day-to-day [81].
Protocol for Pipette Pulling and Seal Formation
Workflow for Pipette Preparation and Sealing
The following diagram illustrates the integrated workflow, from initial setup to successful seal formation, highlighting the logical relationships between each stage.
Detailed Experimental Methodology
Part A: Pulling Reproducible Micropipettes
- Program Selection: Based on your experimental goal (Table 2), select a pre-established program on your micropipette puller or begin with a manufacturer-recommended "cookbook" program for your specific glass type [81].
- Parameter Fine-Tuning:
- Pull a test pipette and measure its resistance. If the Rpip is too high, consult Table 1 and consider slightly decreasing the Force or Distance to achieve a larger tip. If Rpip is too low, consider increasing Heat or Force for a smaller tip [81].
- Make only one parameter adjustment at a time and pull 2-3 pipettes to assess consistency before making further changes.
- Document the final parameters for each glass type and lot to ensure long-term reproducibility.
- Quality Control: Measure the resistance of each pipette by immersing the tip in the standard bath solution and applying a small voltage pulse (e.g., 5 mV). Accept pipettes where the resistance is within a 10% coefficient of variation of your target value [80].
Part B: Achieving a Gigaohm Seal
- Solution Preparation: Prepare and filter (0.2 µm) the internal pipette solution. Critical parameters to control are osmolarity (must match the bath solution to ~5 mOsm), pH (buffered to 7.2-7.4), and ionic composition tailored to the channels under study [80].
- Pipette Preparation: Back-fill the micropipette with the filtered internal solution, avoiding bubbles. Gently tap or centrifuge to bring the solution to the tip.
- Approach and Seal Formation:
- Apply light positive pressure to the pipette interior to prevent contamination of the tip as it is immersed in the bath and advanced toward the cell [80].
- Advance the pipette slowly using a micromanipulator until a slight increase in resistance is observed, indicating contact with the cell membrane [80].
- Immediately release the positive pressure and apply a gentle, continuous negative pressure (suction). Monitor the resistance until it jumps to a stable value ≥ 1 GΩ, forming the "gigaohm seal" essential for low-noise recording [80].
Advanced Technique: Ultrasonic Pipette Cleaning for Reuse
A recent groundbreaking method allows for the automated cleaning and reuse of patch-clamp pipettes, dramatically increasing throughput, especially in automated setups. This protocol involves using a piezo-element to sonicate the pipette tip at 40 kHz within the bath solution, coupled with cycles of high positive and negative pressure to dislodge membrane residues [82].
Key Findings and Protocol:
- Efficiency: Pipettes can be reused at least ten consecutive times with no negative impact on seal resistance (RGS) or access resistance (Ra) [82].
- Cleaning Protocol: The pipette is moved to a "cleaning position" (1-5 mm from the tissue). Sonication (40 kHz) is applied for a short duration along with alternating pressure cycles [82].
- Validation: Scanning electron microscopy confirms that the tip of a cleaned pipette is similar to a fresh one, and success rates for achieving a whole-cell configuration can exceed 90% even after ten reuses [82].
- Stability: When performed at a sufficient distance (5 mm), the cleaning process does not affect the resting membrane potential or membrane resistance of other neurons being recorded simultaneously in the same chamber [82].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful patch-clamp electrophysiology relies on a suite of specialized materials and reagents. The following table details the key items and their functions.
Table 3: Essential Materials for Patch-Clamp Electrophysiology and Micropipette Fabrication
| Item | Function / Application |
|---|---|
| Programmable Micropipette Puller | Instrument for fabricating glass micropipettes with consistent, application-specific tip geometries [81]. |
| Borosilicate Glass Capillaries | Raw material for pulling micropipettes; selected for specific properties like softening point and OD/ID [81]. |
| Patch-Clamp Amplifier | The central electronic component for measuring minute ionic currents and controlling membrane potential [80]. |
| Internal Pipette Solution | Chemical environment dialyzed into the cell; composition (ions, ATP, GTP, buffers) is tailored to the experiment [80]. |
| Vibration Isolation Table | A non-negotiable requirement to decouple the recording rig from environmental vibrations that can disrupt fragile seals [80]. |
| Positive & Negative Pressure System | For applying precise pressure to clear the tip, form gigaohm seals, and rupture the membrane patch [80]. |
| Ultrasonic Cleaning System (with Piezo) | For automated cleaning and reuse of patch-clamp pipettes, significantly improving recording throughput [82]. |
In neuronal activity measurement research, the integrity of electrophysiological data is paramount. The accurate capture of neural signals, which often involve microvolt-scale potentials and millisecond-scale temporal dynamics, is critically dependent on the effective mitigation of noise. Noise, defined as any unwanted interference that obscures the target signal, originates from two primary sources: electrical interference from external electromagnetic fields and mechanical vibrations transmitted through the physical setup. This document provides detailed application notes and protocols for researchers, scientists, and drug development professionals to identify, understand, and mitigate these disruptive forces, thereby ensuring the reliability and quality of electrophysiological data in the context of advanced techniques such as high-density microelectrode arrays (HD-MEAs) [41].
Understanding and Mitigating Electrical Interference
Electrical interference, particularly at the 50/60 Hz mains frequency and its harmonics, is a pervasive challenge that can severely degrade signal quality. The following sections outline its sources and proven mitigation strategies.
Electrical noise in an electrophysiology rig can be categorized as follows:
- Mains Hum (50/60 Hz): The fundamental interference from AC power lines, often exacerbated by ground loops [83].
- Electromagnetic Interference (EMI): Radiated noise from fluorescent lights, computer monitors, motors, and other electronic devices [84] [85] [86].
- Thermal Noise: Inherent noise generated by the random thermal motion of electrons in resistive components [85].
- Shot Noise: Noise arising from the discrete nature of electrical charge as it crosses a junction [85].
Core Mitigation Strategies: A Protocol
A systematic approach is required to eliminate electrical interference. The following protocol, summarized in Table 1, should be executed sequentially.
Table 1: Quantitative Impact of Electrical Noise Mitigation Strategies
| Strategy | Noise Reduction Estimate | Key Action | Primary Effect |
|---|---|---|---|
| Star Grounding | Significant reduction (Qualitative) | Connect all grounds to a single point [83] [86]. | Eliminates ground loops and differing potentials. |
| Faraday Cage | Near-elimination of external EMI (Qualitative) | Enclose setup in conductive mesh grounded via star point [84] [86]. | Blocks external electromagnetic fields. |
| Driven Guard/Shield | Prevents signal attenuation (Qualitative) | Use amplifiers with driven guard circuitry on cables [83]. | Ensures shield voltage matches signal voltage. |
| Notch Filtering | Eliminates 50/60 Hz fundamental (Qualitative) | Apply hardware or software 50/60 Hz notch filters [83]. | Removes persistent mains frequency noise. |
| Rig Simplification | Identifies dominant noise source (Qualitative) | Remove all non-essential equipment, reintroduce one-by-one [84]. | Isolates and identifies noise-generating devices. |
Protocol 1: Systematic Elimination of Electrical Interference
Initial Setup and Grounding:
- Implement a star-grounding system. Connect the chassis grounds of all instruments, the Faraday cage, and the master power strip to a single, common ground point [83] [86]. This prevents "ground loops," which create differing electrical potentials and are a major source of 60 Hz hum [83].
- Use the ground port on a central device (e.g., an acquisition system like the XDAQ) as the common star node [86].
- Ensure all equipment is plugged into the same master power strip to consolidate ground pathways [83].
Shielding with a Faraday Cage:
- Construct or utilize a Faraday cage around the recording apparatus. This can be made from conductive materials like aluminum foil, copper mesh, or steel sheets [84] [86].
- Critically, ground the entire cage to the central star ground point, not directly to a facility earth, to avoid creating new ground loops [86].
- Pay close attention to door seams and cable entry points, using conductive gaskets or mesh sleeves to maintain shielding integrity [86].
Headstage and Animal Grounding:
- Establish a stable reference (REF) and ground (GND) point at the animal. This is typically achieved via a bone screw or Ag/steel wire with verified contact to cerebrospinal fluid or tissue [86].
- Ensure the animal has no other path to ground (e.g., from a grounded stereotaxic frame or heating pad) other than the headstage reference leads [86].
- Short all unused headstage channels to the headstage ground to prevent stray signal pickup [86].
Troubleshooting and Filtering:
- Perform a rig simplification procedure. Strip the setup down to the absolute essentials (microscope, manipulators, headstage) and reintroduce devices (cameras, monitors, perfusion systems) one by one while monitoring noise on an oscilloscope to identify culprits [84].
- As a final measure, employ a 50/60 Hz notch filter, available in hardware on many amplifiers (e.g., A-M Systems) or in software, to remove any residual mains frequency noise [83].
Understanding and Mitigating Mechanical Vibration
Mechanical vibration can cause relative motion between the preparation and the recording electrode, leading to low-frequency drift and movement artifacts that disrupt long-term or sensitive recordings.
Vibrations are transmitted through the building structure and can originate from:
- External sources: Building HVAC systems, nearby machinery, and foot traffic.
- Internal sources: Refrigerators, centrifuges, and perfusion pumps within the laboratory [84].
- Experimental equipment: Un-damped motors or stages on the rig itself.
While the therapeutic application of vibration (e.g., whole-body vibration therapy) is a subject of neuroscience research [87] [88], uncontrolled mechanical vibration in an experimental context is a significant source of artifact and instability.
Core Mitigation Strategies: A Protocol
The following protocol, with strategies summarized in Table 2, provides a method to isolate the electrophysiology rig from mechanical vibration.
Table 2: Vibration Mitigation Solutions and Their Applications
| Solution | Typical Application | Mechanism of Action | Considerations |
|---|---|---|---|
| Anti-Vibration Table | Foundation of all rig setups | Uses pneumatic or damping elements to absorb floor-borne vibrations [84]. | Essential base component. |
| Vibration Dampeners | Mounting for specific noise sources (e.g., pumps, fans) | Incorporates rubber, sorbothane, or other viscoelastic materials to absorb energy [89]. | Can be applied at the source or between rig components. |
| Structural Isolation | Physical separation of the rig | Locating the rig away from obvious vibration sources like elevators or HVAC units. | A simple but highly effective planning consideration. |
| Rigid Mounting | Securing cables and components | Prevents sympathetic vibration of loose components (cables, tubing) [84]. | Complements isolation strategies. |
Protocol 2: Mitigation of Mechanical Vibration
Foundation with Anti-Vibration Table:
- Place the entire electrophysiology rig, including the microscope and manipulators, on a high-quality anti-vibration (air) table. This is the single most important step for isolating the experiment from floor-borne vibrations [84].
Identify and Isolate Internal Vibration Sources:
- Identify all moving parts on or near the rig, such as cooling fans, pumps, or cameras.
- Where possible, mount these devices on vibration-dampening pads or isolator mounts made of rubber or sorbothane to prevent their vibrations from coupling into the main rig structure [89].
Secure and Streamline the Experimental Arena:
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key materials and solutions required for implementing the noise mitigation strategies described in this document.
Table 3: Research Reagent and Material Solutions for Noise Mitigation
| Item | Function/Application | Specific Examples/Notes |
|---|---|---|
| Faraday Cage Materials | Blocks external electromagnetic interference. | Aluminum foil, copper mesh, steel sheets, or commercial cages. Conductive gaskets for doors [86]. |
| Star Grounding Cables | Creates a single-point ground to prevent ground loops. | Low-resistance, shielded cabling to connect all equipment to a common ground point [83] [86]. |
| Headstage & Adapters | Interfaces neural probes with acquisition system. | KonteX v2 headstage adapters for flexible GND/REF configuration [86]. |
| Driven Guard Amplifier | Amplifies signals while minimizing cable-borne noise. | A-M Systems amplifiers with driven guard technology [83]. |
| Notch Filter | Removes 50/60 Hz line noise from the signal. | Hardware filter on amplifier or software filter in acquisition system (e.g., SciWorks Discovery) [83]. |
| Anti-Vibration Table | Isulates the rig from floor-borne vibrations. | Pneumatic or passive damping optical tables [84]. |
| Vibration Dampening Pads | Isolates specific vibrating components (pumps, fans). | Pads made of rubber, sorbothane, or other viscoelastic materials [89]. |
| Bone Screw / Ag Wire | Establishes a stable electrical reference at the animal. | Used with verification of contact to CSF or tissue [86]. |
| Ethanol & Cleaning Tools | For maintaining conductivity. Clean pipette holders and contacts. | Removes oxidation from grounding wires and electrodes [84]. |
In electrophysiological research, the fidelity of neuronal activity measurements is profoundly influenced by the physicochemical environment of the living preparation. The composition of extracellular and intracellular solutions is not merely a technical consideration but a fundamental determinant of experimental success and biological relevance. Solution integrity—maintained through precise control of osmolarity, pH buffering, and oxygenation—ensures the preservation of native neuronal physiology, thereby yielding data that accurately reflect in vivo conditions. This application note details the critical principles and protocols for preparing and validating physiological solutions essential for reliable electrophysiology, particularly in the context of whole-cell patch-clamp recordings and acute brain slice experiments.
The complex interplay of these factors sustains cellular homeostasis. Osmolarity maintains cell volume and prevents osmotic stress-induced artifacts. pH buffering regulates hydrogen ion concentration, critically influencing protein function, enzymatic activity, and the operational state of ion channels and receptors. Oxygenation meets the high metabolic demands of neuronal tissue, preventing anoxic depolarization and preserving synaptic transmission. Neglecting any single component compromises cellular viability and introduces confounding variables, ultimately questioning experimental validity. This document provides a consolidated framework for researchers to standardize these crucial parameters, enhancing reproducibility and physiological relevance in studies of neuronal function and drug discovery.
Theoretical Foundations
Osmolarity and Osmotic Balance
Osmolarity, expressed in milliosmoles per liter (mOsm/L), is a measure of the total solute concentration in a solution. It is a colligative property, dependent on the number of osmotically active particles per unit volume of solvent. In biological systems, osmosis—the movement of water across a semi-permeable membrane from an area of low solute concentration to an area of high solute concentration—is a primary determinant of cell volume [90].
Physiological Range and Importance: The osmolarity of mammalian cerebrospinal fluid and plasma is approximately 290-310 mOsm [91]. Maintaining this osmotic balance in experimental solutions is paramount. Hypotonic solutions (lower osmolarity) cause water influx, leading to neuronal swelling, while hypertonic solutions (higher osmolarity) cause water efflux, resulting in shrinkage. Both states alter channel gating properties, disrupt synaptic connectivity, and can induce apoptosis. For intracellular (pipette) solutions used in whole-cell patch-clamp, a slightly hypotonic value (typically 10-20 mOsm lower than the extracellular solution) is often used to promote seal formation and maintain stable recordings, though significant deviations must be avoided to prevent cell swelling [92].
Adjusting Osmolarity: The osmolarity of a solution is primarily established by its major ionic components (e.g., Na⁺, K⁺, Cl⁻). Fine-tuning to the target osmolarity is typically achieved by adding an osmotically active, metabolically inert solute such as sucrose, glucose, or mannitol [93]. The use of impermeant anions like gluconate or lactobionate in intracellular solutions also contributes to osmolarity while helping to prevent cell swelling [94] [92].
Principles of pH Buffering
A buffer is a solution that resists changes in pH upon the addition of small amounts of acid or base. Biological processes are highly sensitive to fluctuations in extracellular and intracellular pH, which can alter the charge state of amino acids, thereby affecting protein structure, ion channel gating, and synaptic receptor function.
The Bicarbonate/CO₂ Buffer System: In vivo, the primary extracellular buffer is the bicarbonate/CO₂ system, which is highly effective and physiologically authentic. A typical Artificial Cerebrospinal Fluid (ACSF) contains ~25 mM NaHCO₃ and is equilibrated with 95% O₂ / 5% CO₂ to maintain a stable pH of 7.4 [95]. The relevant equilibrium is: [ \text{CO}2 + \text{H}2\text{O} \rightleftharpoons \text{H}2\text{CO}3 \rightleftharpoons \text{H}^+ + \text{HCO}_3^- ] Carbonic anhydrase accelerates the interconversion between CO₂ and carbonic acid. A key advantage of this system is its connection to cellular metabolism and its role in transporting CO₂ waste.
Artificial Buffers: For solutions not equilibrated with CO₂, such as intracellular pipette solutions or simplified extracellular media, synthetic buffers are essential. HEPES (pKa ~7.5) is the most common, offering good buffering capacity in the physiological pH range (7.2-7.4) [93] [92]. It is highly soluble, membrane-impermeant, and relatively inert. Other buffers like PIPES and MOPS are used for specific pH ranges. A critical consideration is that HEPES can diminish the amplitude of activity-dependent extracellular alkaline transients, which are dependent on the bicarbonate buffer system [95]. Therefore, the choice of buffer must align with the experimental goals.
The Critical Role of Oxygenation
The brain consumes a disproportionate amount of the body's oxygen for ATP production. In vitro, acute brain slices and neuronal cultures remain metabolically active and are highly vulnerable to hypoxia.
Consequences of Hypoxia: Oxygen deprivation rapidly depletes ATP stores, leading to failure of energy-dependent processes. The Na⁺/K⁺ ATPase pump ceases to function, resulting in depolarization of the resting membrane potential, inactivation of voltage-gated sodium channels, and ultimately, anoxic depolarization. Synaptic transmission fails, and irreversible cell death begins within minutes.
Oxygenation Practice: Continuous carbogenation (95% O₂ / 5% CO₂) of ACSF is the gold standard. The 5% CO₂ maintains the bicarbonate buffer system at pH 7.4. The high oxygen tension ensures sufficient O₂ diffusion to cells within the several-hundred-micrometer-thick slice. Solutions should be bubbled for at least 15-20 minutes before use and continuously during experiments. A recent study highlights that solution composition, including osmolarity, can influence the oxygenation state of hemoglobin, underscoring the interplay between these parameters [91]. Maintaining solutions at the correct temperature (typically ~32-34°C for recordings) also optimizes oxygen solubility and metabolic function.
Research Reagent Solutions Toolkit
Table 1: Key components of electrophysiology solutions and their functions.
| Reagent | Category | Primary Function | Key Considerations |
|---|---|---|---|
| NaCl | Extracellular Ionic | Major contributor to extracellular osmolarity and action potential propagation. | Baseline concentration ~124 mM in ACSF [95]. |
| KCl | Ionic | Sets resting membrane potential; higher in intracellular solutions [92]. | High extracellular K⁺ can depolarize neurons. |
| NaHCO₃ | Buffer / Ionic | Primary physiological pH buffer in CO₂-equilibrated ACSF [95]. | Requires carbogen (95% O₂/5% CO₂) saturation. |
| HEPES | Buffer | Maintains pH in non-CO₂ systems (e.g., pipette solutions) [92]. | Can interfere with certain biological pH transients [95]. |
| K-gluconate / KMeSO₄ | Intracellular Ionic | Major impermeant anion in pipette solutions; reduces chloride-mediated effects [92]. | K-gluconate may weakly chelate Ca²⁺; KMeSO₄ may preserve excitability better [92]. |
| CaCl₂ | Ionic / Signaling | Critical for synaptic transmission and second messenger signaling. | Concentration must be carefully balanced with Mg²⁺. |
| MgCl₂ | Ionic / Channel Blocker | Modulates neuronal excitability and NMDA receptor function. | |
| D-Glucose / Sucrose | Metabolic / Osmotic | Energy source (glucose) and osmotic agent (both) [93]. | Sucrose is often used in dissection solutions for osmotic substitution. |
| EGTA / BAPTA | Ca²⁺ Chelator | Buffers intracellular Ca²⁺ in pipette solutions to study signaling or prevent toxicity [92]. | BAPTA has faster kinetics than EGTA. |
| ATP / GTP | Energetic | Fuel for kinases, pumps, and GTP-binding proteins in the recorded cell [92]. | Thermolabile; aliquots should be stored frozen. |
| CsOH / CsCl | Ionic / Channel Blocker | Used in pipette solutions to block K⁺ channels and improve space clamp [92]. | Causes cell depolarization; not for current-clamp. |
Quantitative Data on Solution Parameters
Table 2: Comparison of common respiration buffer compositions and their impact on mitochondrial function. Adapted from [94].
| Buffer Name | Key Components | Relative ADP-Stimulated Respiration* | Key Characteristics & Impact |
|---|---|---|---|
| KCl-based (B1) | 130 mM KCl, 1 mM MgCl₂, 20 mM MOPS | Baseline | High Cl⁻ can inhibit transporters like ANT; standard but suboptimal. |
| K-lactobionate (B2) | 60 mM K-lactobionate, 110 mM Sucrose, 20 mM Taurine, 3 mM MgCl₂, 20 mM HEPES | +16% to +35% | Low Cl⁻; lactobionate is cytoprotective and prevents swelling. |
| K-gluconate (B3) | 130 mM K-gluconate, 1 mM MgCl₂, 20 mM MOPS | +26% (Average) | Low Cl⁻; gluconate has metal chelating properties. |
| K-gluconate-Sucrose (B4) | 60 mM K-gluconate, 110 mM Sucrose, 20 mM Taurine, 3 mM MgCl₂, 20 mM HEPES | +35% (Average) | Low Cl⁻ and ionic strength; superior for maximizing respiration. |
*Average increase across multiple substrate combinations compared to the KCl-based B1 buffer.
Table 3: The effect of osmolarity on red blood cell properties, demonstrating general osmotic principles applicable to neurons. Data from [91].
| Suspension Medium Osmolarity | Cell Status | Hemoglobin Concentration | Absorbance at 700 nm | Physiological/Experimental Correlation |
|---|---|---|---|---|
| 200-300 mOsm | Hypotonic / Swollen | Decreased | Lower | Increased light transmission due to cell swelling. |
| ~300 mOsm | Isotonic (Normal) | Normal (Physiological) | Baseline | Represents healthy physiological condition. |
| >300 mOsm (up to 900 mOsm) | Hypertonic / Shrunk | Increased | Higher | Increased light scattering due to cell shrinkage and higher internal refractive index. |
Detailed Experimental Protocols
Protocol 1: Preparation of Artificial Cerebrospinal Fluid (ACSF) for Acute Brain Slice Electrophysiology
This protocol outlines the preparation of 1 liter of standard ACSF for recording from acute rodent brain slices.
Materials:
- Ultrapure water (Type I, 18.2 MΩ·cm)
- Analytical balance
- pH meter
- Osmometer
- Magnetic stirrer and stir bar
- Carbogen tank (95% O₂ / 5% CO₂)
- Volumetric flask or graduated cylinder
- 0.22 µm sterile filter unit (optional, for aseptic preparation)
Reagents: NaCl, KCl, NaH₂PO₄, NaHCO₃, MgCl₂, CaCl₂, D-Glucose.
Procedure:
- Weighing and Dissolution: Measure out the following reagents and add them sequentially to approximately 800 mL of ultrapure water while stirring:
- 124 mM NaCl (7.23 g)
- 3.0 mM KCl (0.22 g)
- 1.0 mM NaH₂PO₄ (0.14 g)
- 26 mM NaHCO₃ (2.18 g)
- 1.5 mM MgCl₂ (0.30 g as MgCl₂·6H₂O)
- 2.5 mM CaCl₂ (0.37 g as CaCl₂·2H₂O)
- 10 mM D-Glucose (1.80 g) Note: Add CaCl₂ last, after all other components are fully dissolved, to prevent precipitation with phosphates.
pH Adjustment: Bring the final volume to 1 L with ultrapure water. Bubble the solution vigorously with carbogen gas for at least 20-30 minutes. The pH should stabilize at 7.4 ± 0.1 due to the bicarbonate buffer system. Do not adjust pH with acid or base unless necessary, as this alters ionic composition.
Osmolarity Verification: Withdraw a small sample of carbogenated ACSF and measure its osmolarity using a vapor pressure or freezing-point depression osmometer. The target value is 300 ± 5 mOsm. If the osmolarity is too high, add small amounts of water. If it is too low, add small amounts of sucrose to adjust.
Final Preparation and Storage: Filter the solution if sterility is required. ACSF should be used fresh on the same day. For recording, it should be continuously bubbled with carbogen and maintained at the appropriate temperature (32-34°C) using a perfusion system.
Protocol 2: Formulation and Quality Control of a K-gluconate-Based Intracellular Pipette Solution
This protocol describes the preparation of a standard intracellular solution for whole-cell patch-clamp recordings of neuronal firing.
Materials:
- Ultrapure water
- Analytical balance
- pH meter
- Osmometer
- Magnetic stirrer
- Ice bath
- 0.22 µm syringe filter
- Aliquot tubes
Reagents: K-gluconate, KCl, NaCl, MgCl₂, HEPES, EGTA, Mg-ATP, Na-GTP, KOH.
Procedure:
- Preparation of Stock and Base Solution: It is recommended to prepare a 1 M stock solution of K-gluconate. To make 100 mL of the final pipette solution, add the following to approximately 80 mL of ultrapure water:
- 120 mM K-gluconate (from 1M stock)
- 10 mM KCl (0.075 g)
- 5 mM NaCl (0.029 g)
- 1 mM MgCl₂ (0.020 g as MgCl₂·6H₂O)
- 10 mM HEPES (0.238 g)
- 1 mM EGTA (0.038 g)
pH Adjustment: Adjust the pH of the solution to 7.25-7.30 using concentrated (e.g., 1 M or 5 M) KOH. Using KOH maintains the desired high K⁺ concentration. Note that the pH of HEPES-buffered solutions is temperature-sensitive; adjust at the temperature at which it will be used (e.g., room temperature).
Osmolarity Adjustment and Final Additions: Measure the osmolarity of the base solution. The target is typically 280-290 mOsm, about 10-20 mOsm lower than the extracellular solution. Adjust if necessary by adding K-gluconate stock (to increase) or water (to decrease). Finally, add the labile components:
- 2 mM Mg-ATP (e.g., 0.121 g/100mL, but use from frozen stock)
- 0.3 mM Na-GTP (e.g., from frozen stock)
Aliquoting and Storage: Pass the solution through a 0.22 µm filter to remove particulates that could clog the pipette. Aliquot into small, single-use volumes (e.g., 0.5-1 mL) and store at -20°C or below. Avoid repeated freeze-thaw cycles. Thaw aliquots on ice immediately before use [92].
Signaling Pathways and Experimental Workflows
Diagram 1: Relationship between solution integrity and data quality. This diagram illustrates how the three core solution parameters directly influence cellular physiology, which in turn dictates the reliability of electrophysiological recordings. Maintaining each parameter within its optimal range (green arrows) promotes homeostasis and yields reliable data. Deviation in any parameter (red arrows) leads to cellular dysfunction and experimental artifacts.
Diagram 2: Electrophysiology solution preparation workflow. This flowchart provides a step-by-step guide for the preparation and quality control of both extracellular and intracellular solutions, highlighting key decision points and specialized steps for each solution type.
Improving Slice Viability and Cell Survival for Long-Duration Experiments
The study of neuronal network dynamics and synaptic function fundamentally relies on ex vivo brain slice preparations. For electrophysiology research, the transition from short-term acute slices to long-term organotypic cultures has been a pivotal advancement, enabling extended investigation of disease progression and therapeutic interventions [96]. A primary challenge in this field, however, is maintaining the structural integrity, cellular diversity, and functional viability of the living brain tissue over prolonged experimental durations [96]. This application note details established and emerging protocols designed to significantly enhance slice viability and cell survival, with a specific focus on supporting long-duration electrophysiological measurements of neuronal activity. The preservation of synaptic connections and native cellular environments in these models provides a more physiologically relevant system for translational research and drug development [96] [2].
Quantitative Assessment of Viability Enhancement Strategies
The following strategies have been quantitatively evaluated for their effectiveness in promoting neuronal health in vitro. The data are summarized in the table below for clear comparison.
Table 1: Quantitative Effects of Interventions on Neuronal Viability
| Intervention | Concentration / Type | Reported Effect on Viability | Key Measured Metrics |
|---|---|---|---|
| Human Cerebrospinal Fluid (hCSF) Supplementation [97] | 10% (v/v) in culture media | Significantly reduces cell death | SYTOX Green assay (dead cells); Calcein AM/EthD-2 dual-staining (live/dead ratio) |
| High-Density Microelectrode Arrays (HD-MEAs) [41] | Non-invasive CMOS-based platform | Enables long-term functional monitoring (> months) | Extracellular action potential (AP) propagation, local field potential (LFP) dynamics |
| Physiologically Rich Culture Media [96] | Organotypic slice culture protocol | Preserves structural integrity & cellular diversity | Tissue architecture, synaptic function, vascular networks |
Detailed Experimental Protocols
Protocol 1: Preparation of Organotypic Slice Cultures Supplemented with hCSF
This protocol is adapted for enhancing viability in primary neuronal cultures and organotypic slices using human cerebrospinal fluid (hCSF), a physiologically rich medium containing essential neurotrophic factors and metabolites [97].
Materials:
- Biological Source: Brain tissue from embryonic day 18 (E18) rat embryos or human surgical resections [96] [97].
- hCSF: Commercially sourced or ethically collected human cerebrospinal fluid.
- Basal Culture Medium: Standard neuronal culture medium (e.g., Neurobasal).
- Viability Assays: SYTOX Green nucleic acid stain, Calcein AM / Ethidium Homodimer-2 (EthD-2) live/dead viability kit.
Procedure:
- Slice Preparation: Prepare acute brain slices (200-400 µm thickness) using a vibratome in ice-cold, oxygenated (95% O₂ / 5% CO₂) slicing artificial cerebrospinal fluid (ACSF) [2].
- Culture Media Formulation: Prepare the optimized culture medium by supplementing the basal medium with 10% (v/v) hCSF [97].
- Culture Establishment: Transfer slices onto porous membrane inserts or into a roller-tube apparatus with the hCSF-supplemented medium.
- Maintenance: Maintain cultures in a humidified incubator at 35°C with 5% CO₂. Replace 50% of the culture medium with fresh hCSF-supplemented medium every 2-3 days.
- Viability Assessment (at endpoint):
- SYTOX Green Assay: Add SYTOX Green stain to the culture medium at a working concentration of 1 µM. Incubate for 15-30 minutes, then image. SYTOX Green selectively labels nuclei of dead cells.
- Calcein AM/EthD-2 Dual-Staining: Prepare a working solution containing 2 µM Calcein AM and 4 µM EthD-2. Incubate with slices for 30-45 minutes. Image to visualize live (Calcein-positive, green fluorescence) and dead (EthD-2-positive, red fluorescence) cells [97].
Protocol 2: Long-Term Functional Monitoring Using HD-MEAs
This protocol outlines the use of High-Density Microelectrode Arrays (HD-MEAs) for non-invasive, long-term electrophysiological recording from viable slice cultures, allowing for the assessment of network health and function over weeks to months [41].
Materials:
- HD-MEA Setup: A CMOS-based HD-MEA system with thousands of electrodes, integrated amplifiers, and data acquisition capabilities [41].
- Perfusion System: A calibrated system for continuous perfusion of oxygenated ACSF at a controlled temperature (32-34°C).
Procedure:
- System Setup: Place the HD-MEA chip in the recording chamber and calibrate the perfusion system. Ensure the ACSF is continuously bubbled with carbogen (95% O₂ / 5% CO₂) and maintained at the physiological temperature of 32-34°C.
- Slice Transfer: Carefully transfer a viable organotypic slice from the culture insert onto the center of the HD-MEA chip.
- Continuous Perfusion: Gently place a slice anchor (e.g., a harp) over the slice to secure it and begin continuous perfusion with oxygenated ACSF at a slow rate (1-2 mL/min).
- Signal Acquisition: Configure the HD-MEA system for full-frame or partial readout. Begin recording extracellular signals, which can include single-unit action potentials from individual neurons and local field potentials (LFPs) from neural populations [41].
- Data Analysis: Use specialized software to analyze the recorded data. Key analyses include:
- Spike Sorting: To isolate and track the activity of individual neurons over time.
- Spike-Triggered Averaging: To map the spatial propagation of action potentials across the array for a single neuron, providing subcellular resolution [41].
- Network Burst Analysis: To investigate synchronized network activity and its evolution over the culture period.
Experimental Workflow for Enhanced Slice Electrophysiology
The following diagram illustrates the integrated workflow, from slice preparation to data analysis, incorporating the viability-enhancing strategies detailed in this note.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of long-duration slice experiments requires a suite of specialized reagents and tools. The following table lists key materials and their critical functions in the protocol.
Table 2: Key Research Reagent Solutions for Slice Viability and Electrophysiology
| Item Name | Function / Application |
|---|---|
| Human Cerebrospinal Fluid (hCSF) | Physiologically relevant supplement providing neurotrophic factors, signaling molecules, and metabolites to significantly enhance neuronal survival in vitro [97]. |
| High-Density Microelectrode Array (HD-MEA) | CMOS-based platform for large-scale, long-term extracellular recording and stimulation of neural activity at cellular and subcellular resolution, from in vitro cultures and ex vivo tissue [41]. |
| Calcein AM / EthD-2 Viability Kit | Dual-fluorescence assay for simultaneous quantification of live (Calcein AM, green) and dead (EthD-2, red) cell populations in a culture [97]. |
| SYTOX Green Nucleic Acid Stain | High-affinity dead-cell stain that penetrates compromised membranes and becomes fluorescent upon binding to DNA, used for quantifying cell death [97]. |
| Oxygenated Artificial Cerebrospinal Fluid (ACSF) | Ionic and pH-balanced physiological salt solution, continuously oxygenated (95% O₂ / 5% CO₂) to maintain tissue health during experiments [2]. |
| Whole-Cell Patch Clamp Setup | Gold-standard technique for detailed intracellular recording of neuronal excitability, synaptic currents, and membrane properties in acute slices [2]. |
Ensuring Credibility: Validation Frameworks and Comparative Technique Analysis
Validated computational models and high-quality electrophysiological data are fundamental to advancing neuroscience research and drug development. The increasing complexity of artificial intelligence (AI) models and high-throughput screening technologies necessitates rigorous validation frameworks to ensure scientific reproducibility and translational success [98] [99]. This document outlines standardized protocols for model and data validation within neuronal electrophysiology, providing researchers with practical tools to establish trustworthiness in their experimental and computational workflows. These principles are critical for integrating computational neuroscience with experimental physiology, thereby supporting reliable biomarker identification and compound screening in neurological disease research.
Principles of Model Validation
Validation Framework and Performance Metrics
Model validation ensures that computational tools perform reliably across diverse datasets and experimental conditions. The European Heart Rhythm Association (EHRA) checklist, developed via a modified Delphi process, provides a structured 29-item framework for transparent reporting in electrophysiology research, emphasizing reproducibility [98]. This framework mandates clear reporting of trial registration, participant details, data handling, and training performance—areas currently underreported in scientific literature (<20% of papers) [98].
Performance metrics must be carefully selected based on the specific analytical task. For binary classification models, the Area Under the Receiver Operating Characteristic Curve (AUROC) measures class discrimination ability, while the Area Under the Precision-Recall Curve (AUPRC) is more appropriate for imbalanced datasets [98]. The F1 score, as the harmonic mean of precision and recall, provides a single metric balancing the trade-off between false positives and false negatives [98].
Table 1: Essential Performance Metrics for Model Validation
| Metric | Calculation | Optimal Value | Application Context |
|---|---|---|---|
| AUROC | Area under ROC curve | 1.0 (perfect discrimination) | Binary classification tasks |
| AUPRC | Area under precision-recall curve | 1.0 (perfect performance) | Imbalanced class distributions |
| F1 Score | 2 × (Precision × Recall)/(Precision + Recall) | 1.0 (perfect balance) | Classification with uneven class importance |
| Mean Absolute Error | Σ|Predicted - Actual|/n | 0 (perfect accuracy) | Regression tasks, parameter estimation |
Internal and External Validation Protocols
Robust validation requires both internal and external validation procedures. Internal validation involves testing models on data from the same source (e.g., same laboratory equipment, patient group) as the training data, providing an initial assessment of generalizability [98]. External validation tests model performance on data from entirely different sources (different institutions, equipment, or patient populations), which is critical for confirming robustness and readiness for clinical deployment [98].
Protocol: External Validation for Neuronal Classification Models
- Data Acquisition: Curate datasets from multiple independent sources (e.g., different research institutions, animal models, experimental conditions) [100].
- Preprocessing: Apply identical preprocessing pipelines (normalization, feature extraction) to all datasets to ensure consistency [101].
- Blinded Testing: Evaluate model performance on external datasets without retraining or fine-tuning.
- Performance Comparison: Compare key metrics (AUROC, F1 score) between internal and external validation cohorts. A performance drop of >15% indicates poor generalizability.
- Bias Assessment: Analyze performance variation across demographic variables, experimental conditions, and data sources.
Recent studies demonstrate that external validation rates for AI models in electrophysiology remain below 30%, representing a significant translational gap [102]. Furthermore, workflow integration of validated models is below 20%, highlighting the need for more robust validation frameworks [102].
Principles of Data Validation
Data Quality Assessment and Standardization
High-quality electrophysiological data forms the foundation of trustworthy research. Data validation begins with rigorous quality assessment and standardization protocols to minimize technical variability and enhance cross-study comparability. The NeuroElectro project demonstrates effective data curation through automated extraction of electrophysiological properties from published literature combined with expert manual validation [103]. This semi-automated approach balances scalability with accuracy, addressing the challenge of heterogeneous data reporting conventions across studies.
Protocol: Data Quality Control for Neuronal Electrophysiology Recordings
- Signal Quality Assessment:
- Calculate signal-to-noise ratio (SNR) for all recordings; exclude traces with SNR < 3:1
- Apply automated artifact detection algorithms to identify and flag contaminated segments
- Verify resting membrane potential stability (±5 mV baseline drift maximum)
Feature Extraction Validation:
- Implement consensus definitions for electrophysiological properties (e.g., action potential threshold, input resistance) [103]
- Extract 48 standardized electrophysiological features including resting membrane potential (vrest), average interspike intervals (avg_isi), and upstroke-downstroke ratios [100]
- Compute 24 morphological attributes including total volume, average diameter, and soma surface area for morpho-electrophysiological studies [100]
Metadata Documentation:
- Record complete methodological details: animal species, strain, recording solution, temperature [101]
- Document electrode properties and recording configurations
- Note pharmacological manipulations and experimental conditions
Table 2: Data Quality Thresholds for Electrophysiological Recordings
| Parameter | Acceptance Threshold | Exclusion Criteria | Validation Method |
|---|---|---|---|
| Signal-to-Noise Ratio | > 3:1 | ≤ 3:1 | Automated calculation from raw traces |
| Baseline Stability | < ±5 mV drift | ≥ ±5 mV drift | Statistical analysis of baseline periods |
| Action Potential Amplitude | > 50 mV | ≤ 50 mV | Peak-to-trough measurement |
| Input Resistance | Consistent within ±20% across measurements | Variations > 20% | Repeat hyperpolarizing step responses |
Synthetic Data Validation and Integration
Synthetic data generation addresses data scarcity, particularly for rare neuronal subtypes, but requires rigorous validation to ensure biological fidelity. Benchmarking studies compare classical approaches like SMOTE with deep generative models (GANs, VAEs, Normalizing Flows, DDPMs) for classifying electrophysiological and morpho-electrophysiological neuron types [100].
Protocol: Validating Synthetic Neuronal Data
- Feature Space Comparison:
- Generate synthetic data using multiple methods (SMOTE, GANs, VAEs)
- Compare distribution of synthetic features with original data using statistical distance metrics
- Calculate mean absolute errors between synthetic and real class profiles
Biological Plausibility Assessment:
- Ensure synthetic neurons respect natural phenotypic variability observed between real neuronal classes [100]
- Validate that synthetic action potentials maintain physiological characteristics (appropriate waveforms, thresholds)
- Verify morpho-electrophysiological relationships remain within biologically possible ranges
Downstream Utility Evaluation:
- Train classifiers on augmented datasets (real + synthetic data)
- Compare performance with classifiers trained on real data only
- Evaluate using cross-validated accuracy, precision, and recall
Studies demonstrate that SMOTE-based augmentation yields classification accuracy gains of 0.16 for electrophysiological types and 0.12 for morpho-electrophysiological types, outperforming many deep generative approaches [100]. However, GANs approach similar performance with proper hyperparameter optimization, offering greater flexibility for complex data distributions.
Experimental Protocols for Validation
Cross-Platform Electrophysiology Validation
Validation across different electrophysiology platforms ensures consistent results regardless of technological approach. Comparative studies examining hα3β4 and hα4β2 nicotinic receptors response to acetylcholine across Dynaflow (low-throughput), PatchXpress 7000A (medium-throughput), and IonWorks Barracuda (high-throughput) platforms demonstrate consistent EC₅₀ values despite methodological differences [99]. This cross-platform consistency validates each system's utility for screening nicotinic compounds.
Protocol: Cross-Platform Assay Validation
- System Calibration:
- Use standardized reference compounds with known efficacy and potency
- Validate each platform with control measurements before experimental runs
- Implement standardized data acquisition parameters across systems where possible
Dose-Response Characterization:
- Generate full dose-response curves for reference agonists
- Calculate EC₅₀ values using standardized curve-fitting algorithms
- Compare values across platforms; acceptable variation < 0.5 log units
Inhibition Assay Validation:
- Test both competitive (e.g., dihydro-beta-erythroidin) and uncompetitive (e.g., mecamylamine) antagonists [99]
- Implement custom algorithms for generating dose-response curves from multiple extrapolated current metrics
- Verify mechanism-specific inhibition patterns across platforms
Optimal Experimental Design for Parameter Estimation
Model-driven optimal experimental design reduces parameter uncertainty in cellular electrophysiology. For cardiac cellular electrophysiology, optimal designs have been developed that outperform commonly used protocols in identifying maximum conductance values, with shorter experiment durations and improved predictive power [104]. These approaches can be adapted to neuronal studies for creating cell-specific models.
Protocol: Optimal Design for Neuronal Parameter Estimation
- Voltage-Clamp Experiments:
- Design protocols that maximize information for parameter estimation
- Include both activation and inactivation voltage protocols
- Incorporate recovery from inactivation protocols
Current-Clamp Experiments:
- Design current injection protocols that elicit diverse firing patterns
- Include both subthreshold and suprathreshold stimuli
- Incorporate dynamic current injections (ramps, noise)
Protocol Optimization:
- Define parameter estimation goals a priori
- Use model-based approaches to design information-rich protocols
- Balance protocol duration with information content
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Electrophysiology Validation
| Tool/Reagent | Function | Application Context | Validation Consideration |
|---|---|---|---|
| High-Density Microelectrode Arrays (HD-MEAs) | Large-scale recording from electrogenic cells | Network-level electrophysiology, drug screening | Electrode density (>3000/mm²), simultaneous readout channels [41] |
| PatchXpress 7000A | Medium-throughput automated patch clamp | Ion channel screening, receptor characterization | Cross-platform consistency with low- and high-throughput systems [99] |
| IonWorks Barracuda | High-throughput electrophysiology screening | Compound screening, dose-response studies | Validation against conventional patch clamp methods [99] |
| NeuroElectro Database | Compendium of neuronal electrophysiological properties | Model constraint, experimental planning | Manual curation of literature-derived data [103] |
| Allen Cell Types Database | Public repository of neuronal properties | Neuronal classification, model development | Standardized feature extraction pipelines [100] |
| SMOTE Algorithm | Synthetic minority over-sampling technique | Addressing class imbalance in neuronal classification | Biological fidelity assessment against real data variability [100] |
Within the domain of human cognitive neuroscience and clinical neurophysiology, the non-invasive measurement of neuronal activity is paramount. Two predominant techniques for such measurements are Electroencephalography (EEG) and Magnetoencephalography (MEG). Both methods capture signals originating from the synchronized post-synaptic potentials of cortical pyramidal neurons, providing direct, millisecond-level temporal resolution of brain function, which is unattainable with hemodynamic-based methods like fMRI [105]. Despite this shared biophysical basis, the distinct physical principles governing the signals they measure—electrical potentials for EEG and magnetic fields for MEG—lead to significant differences in their sensitivity profiles, spatial resolution, and susceptibility to artifacts.
Framed within a broader thesis on electrophysiological methods, this analysis delineates the complementary strengths and limitations of EEG and MEG. It provides a detailed, practical guide for researchers and clinicians on their application, supported by contemporary comparative data and standardized protocols for multimodal integration. Understanding the synergistic relationship between these modalities is crucial for designing robust experiments, particularly in translational research and drug development where precise spatiotemporal characterization of brain network activity is essential.
Theoretical Foundations and Comparative Biophysics
The fundamental signal for both EEG and MEG is derived primarily from intracellular currents flowing in the apical dendrites of synchronously activated pyramidal neurons in the cortex [105]. When these neurons are activated, the configuration of the resulting current dipole and its relationship to the cortical geometry dictates how the signal is projected to the sensors.
EEG Principles: EEG measures the electrical potential differences on the scalp surface generated by these neuronal currents. The signal must propagate through various tissues (e.g., brain parenchyma, cerebrospinal fluid, skull, and scalp), each with different and often inhomogeneous electrical conductivity. The skull, in particular, has low conductivity, which smears and attenuates the electrical potentials, significantly blurring the spatial origin of the underlying neural activity [105].
MEG Principles: MEG measures the extracranial magnetic fields induced by the same intracellular currents. These magnetic fields are largely unaffected by the varying conductivity of biological tissues, passing through them virtually undistorted. Consequently, MEG provides a more spatially focal representation of the underlying brain activity compared to EEG [106]. However, MEG is predominantly sensitive to currents oriented tangentially to the scalp surface (those located in the sulcal walls), while it is relatively blind to radially oriented sources (on the gyral crowns). In contrast, EEG captures signals from both radial and tangential sources [105] [107].
Table 1: Fundamental Biophysical and Technical Comparison of EEG and MEG
| Feature | Electroencephalography (EEG) | Magnetoencephalography (MEG) |
|---|---|---|
| Measured Quantity | Electrical potential difference (µV) on scalp | Magnetic field (fT) outside head |
| Basis in Biophysics | Volume currents from post-synaptic potentials | Intracellular currents from post-synaptic potentials |
| Spatial Blurring | High (due to skull conductivity) | Low (minimal distortion by tissues) |
| Primary Source Orientation | Radial and tangential | Primarily tangential |
| Typical Temporal Resolution | Millisecond | Millisecond |
| Sensor Type | Passive electrodes | Superconducting Quantum Interference Devices (SQUIDs) or Optically Pumped Magnetometers (OPMs) |
| Noise Susceptibility | Sensitive to muscular, ocular, and movement artifacts | Sensitive to environmental magnetic noise |
Quantitative Comparative Analysis
Recent empirical studies provide a quantitative basis for the comparative performance of EEG and MEG. A 2025 comparative study that employed time-domain, time-frequency, and source-space analyses offers critical insights [106].
The study confirmed that MEG planar gradiometers capture the highest total information content, followed by magnetometers and then EEG. Specifically, for physiological signals such as vertex waves and K-complexes, the total information was significantly higher in MEG. Furthermore, mutual information analysis indicated that MEG-derived independent components exhibited greater topographical variability and higher information content for neurophysiological activity, whereas EEG components were more homogeneous [106].
In terms of artifact susceptibility, the study found that EEG was more sensitive to high-amplitude artifacts from sources like swallowing and muscle activity (EMG). This makes EEG data more vulnerable to contamination from common patient movements. Conversely, the fidelity of MEG for deep brain sources or those in regions like the orbitofrontal cortex can be limited by signal attenuation with distance, though it is less contaminated by myogenic artifacts [106].
Applications in brain-computer interfaces (BCIs) further highlight these differences. A 2025 BCI study on auditory attention reported that classification accuracy was highest (73.2%) using whole-scalp MEG (306 channels). Accuracy decreased to 69%, 66%, and 61% when using 64, 9, and 3 EEG channels, respectively. This demonstrates that while high-channel-count EEG can approach MEG's performance, low-channel-count setups result in a significant drop in accuracy, though they may remain usable for specific applications [108].
Table 2: Empirical Performance Comparison from Recent Studies
| Performance Metric | EEG Findings | MEG Findings |
|---|---|---|
| Signal-to-Noise Ratio (SNR) | Lower comparative SNR [106] | Highest SNR in planar gradiometers [106] |
| Information Content | More homogeneous components [106] | Higher information for neurophysiological patterns [106] |
| Artifact Sensitivity | Higher sensitivity to EMG, swallowing, eye blinks [106] | Less sensitive to myogenic artifacts [106] |
| BCI Classification Accuracy | 69% (64 ch), 66% (9 ch), 61% (3 ch) [108] | 73.2% (306 ch) [108] |
| Source Localization Accuracy | Broader, less spatially focal [106] | More spatially focal and precise [106] |
Application Notes and Experimental Protocols
Protocol 1: Simultaneous EEG-MEG Data Acquisition for Sensory Evoked Responses
This protocol is designed for studies requiring comprehensive spatiotemporal characterization of brain responses, such as in pharmaco-physiology or biomarker validation.
1. Research Reagent Solutions & Equipment Table 3: Essential Materials for Simultaneous EEG-MEG Acquisition
| Item | Function/Description |
|---|---|
| MEG System | A whole-head system (e.g., 306-channel TRIUX or CTF DSQ3500) housed in a magnetically shielded room (MSR) [107]. |
| EEG System | A compatible high-impedance amplifier and cap (e.g., 64-channel EasyCap) designed for simultaneous use inside an MEG dewar. |
| Electrophysiology Software | Software for stimulus presentation (e.g., PsychToolbox in MATLAB) and synchronized data acquisition (e.g., CTF acquisition software) [107]. |
| Conductive Gel & Abrasive Paste | For achieving and maintaining electrode-skin impedance below 5 kΩ for EEG, ensuring high-quality signal. |
| Anatomical Landmark Digitzer | To record the 3D position of nasion, pre-auricular points, and EEG electrodes relative to the MEG head position indicator coils. |
| Structural MRI Scanner | A 3T MRI system to acquire a high-resolution T1-weighted anatomical volume for source reconstruction. |
2. Procedure
- Step 1: Participant Preparation. Fit the participant with the EEG cap according to the 10-10 or 10-5 international system. Prepare the scalp at each electrode site with abrasive paste and apply conductive gel to achieve low impedance. Ensure the participant wears an MEG-compatible (non-magnetic) attire.
- Step 2: Positioning and Co-registration. Position the participant in the MEG dewar. Place the three head-position indicator (HPI) coils on the scalp (at nasion and pre-auricular points). Use the 3D digitizer to record the locations of the HPI coils, all EEG electrodes, and several hundred head shape points across the scalp.
- Step 3: Acquisition Parameters. Set the MEG sampling rate to 1000 Hz or higher (e.g., 1200 Hz [107]) with an online anti-aliasing filter. Configure the EEG system to sample at the same rate, with a compatible bandpass filter (e.g., 0.1-300 Hz). Ensure the systems share a common trigger interface for precise stimulus synchronization.
- Step 4: Data Recording. Begin simultaneous recording. Present sensory stimuli (e.g., auditory "Yes"/"No" words [108] or visual naturalistic images [107]) in a randomized, event-related paradigm. Record sufficient trials (e.g., 100+ per condition) to ensure an adequate signal-to-noise ratio for averaged responses.
- Step 5: Post-acquisition. Coregister the digitized head shape with the participant's structural MRI by aligning the fiduciary points and fitting the head surface to the MRI scalp surface.
Protocol 2: Presurgical Mapping of Interictal Epileptiform Discharges (IEDs)
This protocol outlines a clinical application for localizing the epileptogenic zone in patients with pharmacoresistant epilepsy.
1. Research Reagent Solutions & Equipment Table 4: Essential Materials for Epilepsy Presurgical Mapping
| Item | Function/Description |
|---|---|
| High-Density MEG/EEG | MEG (306 ch) or EEG (64-128 ch) systems for capturing detailed epileptiform activity. |
| Magnetically Shielded Room (MSR) | Essential for MEG to attenuate ambient environmental magnetic noise. |
| Source Imaging Software | Software capable of distributed source imaging (e.g., dSPM, sLORETA) and dipole fitting. |
| Clinical MRI & CT | High-resolution structural MRI and potentially a CT scan for identifying structural lesions. |
2. Procedure
- Step 1: Long-term Recording. Acquire at least 30-60 minutes of resting-state data to increase the probability of capturing interictal spikes. Include periods of drowsiness and sleep, as IEDs are often activated during these states.
- Step 2: Data Inspection and Spike Identification. An experienced clinical neurophysiologist reviews the data to identify and mark individual IEDs. Both EEG and MEG data should be inspected independently and then reviewed together to leverage their complementary sensitivity.
- Step 3: Forward Modeling. Construct a head model using the Boundary Element Method (BEM) [105] or Finite Element Method (FEM) [105] based on the patient's MRI. This model defines the volume conductor for calculating the signal transfer from source to sensor.
- Step 4: Inverse Solution. Use an inverse method (e.g., a dipole fitting algorithm for focal spikes or a distributed source model for extended sources) to estimate the generator locations of the averaged IEDs. MEG's strength lies in providing a more spatially focal estimate of the irritative zone, which can be crucial for surgical planning [109].
- Step 5: Clinical Integration. Overlay the estimated source localizations onto the patient's 3D MRI. These results are integrated with other data (e.g., semiology, video-EEG, fMRI, SPECT) at a multidisciplinary surgical conference to formulate a final treatment plan [109].
Emerging Technologies and Future Directions
The field of electromagnetic brain imaging is rapidly evolving, with several technologies poised to enhance the application of both EEG and MEG.
- Optically Pumped Magnetometers (OPMs): OPMs are a new generation of magnetic sensors that do not require cryogenic cooling. This allows for the development of wearable "MEG helmets" that enable natural movement during recording and are adaptable to a wider range of head sizes, including children [109] [110]. Early comparative studies show OPMs performing comparably to traditional SQUID-based MEG in detecting interictal epileptiform discharges [111].
- Multimodal Integration and Biomarkers: There is a strong push to integrate MEG with other modalities to identify early biomarkers for neurological and psychiatric disorders. For instance, MEG is being used to detect aberrant network signatures in conditions like Alzheimer's disease and traumatic brain injury, potentially years before overt symptoms appear [110]. The integration of MEG with diffusion tensor imaging (DTI) can also provide a more complete picture of brain structure-function relationships.
- AI and Foundation Models: A significant innovation is the development of foundation models like "BrainOmni," which is the first model to perform unified pretraining on both EEG and MEG signals [112]. By using a novel "Sensor Encoder" that incorporates physical sensor properties, these models can generalize across different devices and modalities, potentially revolutionizing data analysis and improving the scalability of neuroimaging applications.
EEG and MEG are not competing but fundamentally complementary technologies in the electrophysiology toolkit. The choice between them—or the decision to use them in tandem—should be guided by the specific research or clinical question. MEG excels in providing high-fidelity, spatially focal information for tangential cortical sources with less contamination from biological artifacts. In contrast, EEG offers a more accessible and robust method for capturing a broader range of brain activity, including radial sources, and is essential for long-term monitoring.
For the most comprehensive assessment of brain dynamics, particularly in translational research and drug development aimed at modulating specific neural circuits, a multimodal approach that leverages the strengths of both EEG and MEG is highly recommended. The ongoing development of wearable MEG systems, sophisticated analysis pipelines, and unified AI models promises to further democratize these powerful techniques, deepening our understanding of the human brain in health and disease.
Electroencephalography (EEG) is a fundamental, non-invasive tool for investigating brain function and neurological disorders, valued for its exceptional temporal resolution, portability, and cost-effectiveness [113]. The analysis of EEG signals presents a significant challenge because these signals are inherently non-stationary, meaning their statistical properties change over time [114] [115]. This non-stationarity is particularly evident during dynamic brain processes such as epileptic seizures [114], motor movements [116], or shifts in covert visual attention [117]. Consequently, traditional Fourier Transform (FT), which assumes signal stationarity, is often inadequate for a comprehensive analysis as it provides only the global frequency content without temporal localization [115].
To overcome this limitation, advanced time-frequency analysis techniques have been developed. The Short-Time Fourier Transform (STFT) and the Wavelet Transform (WT) are two prominent methods that map a signal into both time and frequency domains, allowing researchers to observe how the spectral components of an EEG signal evolve over time [114] [116]. This application note provides a structured comparison of these three techniques—FT, STFT, and WT—within the context of electrophysiology research. It includes quantitative performance comparisons, detailed experimental protocols, and essential toolkits to guide researchers and scientists in selecting the appropriate method for specific experimental inquiries in both basic neuroscience and drug development.
Core Methodological Principles
- Fourier Transform (FT): The Fast Fourier Transform (FFT) is a fundamental algorithm for computing the discrete Fourier transform. It decomposes a signal from the time domain into its constituent sinusoidal components in the frequency domain. The primary limitation of the FFT is its inherent assumption of signal stationarity. It is therefore most suitable for identifying dominant rhythmic activity, such as posterior-dominant alpha rhythms (8-13 Hz) in awake, relaxed individuals with eyes closed [115].
- Short-Time Fourier Transform (STFT): The STFT extends the concept of the FFT by introducing a sliding temporal window. The signal is divided into short, sequential, or overlapping segments (frames), and an FFT is applied to each segment. The succession of these FFTs produces a time-frequency representation of the signal, known as a spectrogram [114] [115]. A key trade-off in STFT is the uncertainty principle: a shorter window provides better temporal resolution but poorer frequency resolution, and vice-versa [116].
- Wavelet Transform (WT): The WT can be considered a multi-resolution extension of the FT. Instead of using a fixed-width window, it employs a "mother wavelet" function that is scaled (dilated or compressed) and translated in time. This allows for variable time-frequency resolution—high frequency resolution and low temporal resolution at low frequencies, and high temporal resolution with low frequency resolution at high frequencies [114]. The Continuous Wavelet Transform (CWT) is used for detailed time-frequency analysis, while the Discrete Wavelet Transform (DWT) is employed for efficient signal decomposition and reconstruction, often for feature extraction or compression [115] [117].
Quantitative Performance Comparison
The following table summarizes the performance of these techniques based on key studies analyzing EEG signals.
Table 1: Performance Comparison of Signal Processing Techniques in EEG Analysis
| Technique | Reported Classification Accuracy | Key Advantages | Key Limitations |
|---|---|---|---|
| FFT | Not specifically reported for non-stationary classification | Fast computation; simple interpretation; ideal for stationary signals [115]. | Lacks time localization; unsuitable for non-stationary signals; sensitive to noise [115]. |
| STFT | High accuracy in real-time seizure detection [114] | Shorter processing time, making it more suitable for real-time applications [114] [118]; simpler implementation and interpretation [116]. | Fixed time-frequency resolution due to window size constraint [114] [116]. |
| WT | 91.2% - 100% accuracy in seizure detection [119]; >90% in covert attention tasks [117] | Superior resolution for analyzing transient, non-stationary events [114]; multi-scale analysis capability; ability to compress signal into fewer features [114] [117]. | Higher computational cost and complexity than STFT [114] [115]. |
Qualitative Methodological Trade-offs
The choice between STFT and Wavelet Transform often involves a trade-off between computational efficiency and analytical flexibility.
- Suitability for Real-Time Processing: A direct comparison for determining epileptic seizure activity concluded that the STFT is more applicable for real-time processing due to its shorter computation time, despite the WT providing good resolution [114] [118]. This makes STFT a strong candidate for embedded clinical systems or brain-computer interfaces (BCIs) requiring rapid feedback.
- Handling of Complex Brain Dynamics: For decoding covert visual attention, a deep learning framework that used CWT-generated time-frequency representations as input achieved over 90% accuracy in complex four-class classification [117]. This demonstrates the WT's power in revealing intricate, time-varying neural patterns that might be obscured by the fixed window of the STFT.
- Analysis of Repetitive Movements: In studies of repetitive motor tasks, the STFT was recommended as the best compromise between spectral and temporal resolution for analyzing movement-related oscillations in the α- and β-bands [116]. This suggests that for rhythmic brain processes with predictable timing, the simplicity and clarity of the STFT are advantageous.
Experimental Protocols
This section provides detailed methodologies for implementing these transforms in a typical EEG analysis pipeline, from raw data to feature extraction.
Protocol 1: EEG Sub-band Extraction using STFT
Application Note: This protocol is ideal for applications where real-time capability is prioritized and the brain phenomena of interest have a relatively stable frequency content over short durations, such as monitoring sleep spindles or event-related desynchronization [115] [116].
Workflow Diagram:
Step-by-Step Procedure:
Data Acquisition & Preprocessing:
- Acquire EEG data according to international 10-20 electrode placement system [115] [117].
- Preprocess the raw signal using a Finite Impulse Response (FIR) bandpass filter (e.g., 1-60 Hz) to remove DC offset and high-frequency noise [117].
- Apply a notch filter (e.g., 50 Hz or 60 Hz) to suppress line interference [117].
- Remove artifacts (e.g., ocular, cardiac, muscle) using techniques like Independent Component Analysis (ICA) [117].
Signal Segmentation:
- Divide the continuous, preprocessed EEG signal into short, sequential epochs (trials) time-locked to an event (e.g., stimulus onset).
- Within each epoch, apply a sliding window (e.g., Hanning window) with a defined overlap (e.g., 50%) to create segments for FFT analysis [114].
STFT Calculation:
Sub-band Power Extraction:
- From the spectrogram, integrate the power within the standard clinical frequency bands to create time courses for each band:
- Delta (δ): 0.5 - 4 Hz
- Theta (θ): 4 - 8 Hz
- Alpha (α): 8 - 13 Hz
- Beta (β): 13 - 30 Hz
- Gamma (γ): 30 - 60 Hz [115].
- From the spectrogram, integrate the power within the standard clinical frequency bands to create time courses for each band:
Protocol 2: Feature Extraction using Discrete Wavelet Transform (DWT)
Application Note: This protocol is superior for analyzing signals with abrupt, transient components, such as epileptic spikes or sharp waves. It is highly effective for compressing EEG data into a small number of discriminative features for machine learning classifiers [114] [119].
Workflow Diagram:
Step-by-Step Procedure:
Preprocessing:
- Follow the same data acquisition and preprocessing steps outlined in Protocol 1 (Steps 1a-1d) to obtain a clean, continuous EEG signal.
Wavelet Decomposition:
- Select an appropriate mother wavelet (e.g., Daubechies 4 'db4' is commonly used for EEG) [119].
- Apply the DWT to the preprocessed EEG signal. The DWT functions as a filter bank, decomposing the signal into different frequency sub-bands.
- The first level of decomposition produces Approximation coefficients (A1) representing the low-frequency component and Detail coefficients (D1) representing the high-frequency component.
- Iteratively decompose the successive Approximation coefficients to achieve a multi-level decomposition tree. For example, a 5-level decomposition can be used to isolate the δ, θ, α, β, and γ bands [119].
Feature Calculation:
- From the derived coefficients at each decomposition level, calculate statistical features that characterize the signal. Common features include:
- Energy: The sum of squares of the coefficients in a sub-band.
- Entropy: A measure of the randomness or complexity of the signal within a sub-band.
- Standard Deviation: The dispersion of the coefficient values [119].
- From the derived coefficients at each decomposition level, calculate statistical features that characterize the signal. Common features include:
Classification:
- The computed features from all relevant sub-bands are assembled into a feature vector.
- This feature vector is then used as input to a classifier, such as a Support Vector Machine (SVM) or an Artificial Neural Network (ANN), to discriminate between different brain states (e.g., seizure vs. non-seizure) [119].
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for EEG Signal Processing
| Item / Technique | Function / Specification | Example Usage & Notes |
|---|---|---|
| Ag-AgCl Electrodes | Non-invasive scalp electrodes for detecting electrical brain activity. | Standard for clinical EEG; high conductivity and low noise [115]. |
| 10-20 Placement System | International standard for electrode positioning. | Ensures consistency and reproducibility across recordings and studies [115] [117]. |
| Data Acquisition Card | Converts analog EEG signals to digital data. | Requires a card with 12-bit resolution or higher; sampling frequency typically 250 Hz or higher [114] [117]. |
| FIR / IIR Filters | Digital filters for preprocessing. | FIR filters are preferred for their linear phase response [115] [117]. |
| Daubechies Wavelets | A family of orthogonal wavelets for DWT. | 'db4' is frequently selected for its similarity to EEG morphologies [119]. |
| Support Vector Machine (SVM) | A supervised machine learning model for classification. | Commonly used with wavelet-extracted features for high-accuracy seizure detection [119]. |
| Artificial Neural Network (ANN) | A non-linear classifier inspired by biological neural networks. | Effective for classifying complex patterns in EEG sub-bands [119]. |
The analysis of EEG signals demands sophisticated time-frequency techniques due to their non-stationary nature. The Fourier Transform remains a foundational tool for initial spectral assessment but is insufficient for detailed dynamic analysis. The choice between the Short-Time Fourier Transform (STFT) and the Wavelet Transform (WT) is not one of absolute superiority but of application-specific suitability. For real-time diagnostic systems and repetitive movement analysis where processing speed is critical, STFT offers a robust and efficient solution. Conversely, for the detailed analysis of transient, complex neurological events like epileptic seizures or for decoding covert cognitive states, the multi-resolution analytical power of the Wavelet Transform is unparalleled, often yielding higher classification accuracy at the cost of greater computational complexity. A firm grasp of the principles, trade-offs, and practical protocols outlined in this application note will empower electrophysiology researchers to effectively harness these powerful signal processing tools in their quest to decode brain activity.
Electrophysiology is the cornerstone of cellular excitability research, providing direct insight into the function of ion channels that govern neuronal communication and cardiac contraction [120]. The patch clamp technique, developed by Sakmann and Neher, remains the gold standard for ion channel research due to its exceptional data quality and informational content [121] [120]. However, this method suffers from inherent limitations in throughput and technical demands, prompting the development of automated electrophysiology platforms over the past two decades [121]. This application note provides a structured comparison of manual and automated patch clamp systems, detailing their respective capabilities in throughput, data quality, and application scope to guide researchers in selecting appropriate methodologies for neuronal activity measurement research.
Technical Comparison of Electrophysiology Platforms
Fundamental Operational Characteristics
Manual patch clamp techniques utilize glass micropipettes that form a tight seal (giga-ohm resistance) against the cell membrane, allowing precise measurement of ionic currents across the membrane [121] [120]. This approach offers multiple recording configurations including cell-attached, whole-cell, inside-out, and outside-out patches, each with specific applications for studying different aspects of ion channel function [121]. The manual method provides unparalleled flexibility but requires significant operator expertise and time, typically limiting output to a few cells per day [121].
Automated patch clamp (APC) systems employ either automated glass pipettes or planar electrode-based technologies [121]. Planar systems utilize microfabricated chips containing micron-sized holes where cells are captured by suction, forming seals for electrical recording [121]. These systems automate the patching process, enabling parallel recordings from multiple cells and dramatically increasing experimental throughput while reducing operator dependency [121] [37].
Quantitative Performance Metrics
Table 1: Throughput and Data Quality Comparison of Electrophysiology Platforms
| Platform Type | Data Points Per Day | Seal Resistance | Success Rate | Key Limitations |
|---|---|---|---|---|
| Manual Patch Clamp | Low (varies by operator) | >1 GΩ [121] | Not applicable (operator-dependent) | Low throughput, high personnel costs, requires significant expertise [121] |
| QPatch | 1,250-3,500 [121] | >1 GΩ [121] | Not specified | Limited to suspension cells, no intracellular perfusion [121] |
| IonWorks HT/Quatto | ~3,000 [121] | 50-100 MΩ [121] | Not specified | Moderate seal resistance, no compound washout [121] |
| PatchXpress | ~2,000 [121] | >1 GΩ [121] | Not specified | No intracellular perfusion or current clamp [121] |
| Fixed-well APC (Cardiomyocytes) | High (exact number not specified) | >100 MΩ [37] | 13.9 ± 1.7% [37] | Optimized for larger primary cells [37] |
Application Scope and Data Variability
Manual patch clamp remains essential for studying complex cellular systems, including primary neurons, tissue slices, and differentiated cells derived from induced pluripotent stem cells (iPSCs) or embryonic stem cells (ESCs) [121]. Its flexibility allows investigation of neuronal network dynamics and mixed cell populations where visual selection of specific cell types is required [121]. Recent multi-laboratory comparisons of manual patch clamp data using standardized protocols demonstrate that hERG block potency values within 5-fold should not be considered different, as this represents the natural variability of the assay even under controlled conditions [72].
Automated systems excel in high-throughput compound screening applications, particularly for drug discovery and safety pharmacology [121] [99]. These platforms are ideal for homogeneous cell lines stably expressing high levels of specific ion channels, such as those used in hERG cardiac safety screening [121] [72]. Recent advancements have extended APC applications to native cardiomyocytes, with studies demonstrating successful recordings of action potentials, L-type calcium currents (ICa,L), and inward rectifier currents in freshly isolated swine atrial and ventricular cells [37]. The reproducibility of these APC assays, as measured by Z-factor analysis, consistently shows good to excellent values, indicating robust suitability for high-throughput screening [37].
Experimental Protocols
Manual Patch Clamp Protocol for Neuronal Ion Channels
Cell Preparation:
- Utilize primary neuronal cultures, brain slices, or differentiated neurons from iPSCs.
- For primary cultures, plate cells on glass coverslips coated with poly-D-lysine or other appropriate substrates.
- Maintain cells in culture for 7-21 days to allow maturation of ionic currents, confirming functionality through the presence of tetrodotoxin (TTX)-sensitive sodium currents and specific potassium currents.
Solution Preparation:
- External Solution (Artificial Cerebrospinal Fluid): 130 mM NaCl, 3 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 10 mM HEPES, 10 mM glucose, pH 7.4 with NaOH, ~300 mOsm.
- Internal (Pipette) Solution: 120 mM K-gluconate, 20 mM KCl, 10 mM HEPES, 5 mM EGTA, 1.5 mM MgATP, 0.3 mM NaGTP, pH 7.3 with KOH, ~290 mOsm.
Recording Procedure:
- Pull borosilicate glass capillaries to obtain pipettes with resistance of 3-6 MΩ.
- Mount coverslip with cells in recording chamber and continuously perfuse with external solution.
- Approach cell surface with pipette using micromanipulator under visual guidance.
- Apply gentle suction to form giga-ohm seal (>1 GΩ).
- Apply additional brief suction or voltage zap to rupture membrane patch, achieving whole-cell configuration.
- Compensate series resistance (typically 60-80%) and capacitance.
- Implement appropriate voltage or current clamp protocols to characterize specific ion currents.
Data Analysis:
- For voltage-gated sodium channels, determine voltage-dependence of activation and inactivation using appropriate step protocols.
- Analyze neuronal action potential properties including threshold, amplitude, and afterhyperpolarization.
- For synaptic currents, measure amplitude, frequency, and kinetics of spontaneous postsynaptic currents.
Automated Patch Clamp Protocol for Compound Screening
Cell Preparation:
- Use suspension cells stably expressing the ion channel of interest.
- For hERG screening: HEK293 or CHO cells stably expressing hERG1a.
- Prepare cells at appropriate density (0.5-2 × 10^6 cells/mL) in external solution with viability >90%.
Solution Preparation:
- External Solution: 130 mM NaCl, 5 mM KCl, 1 mM MgCl2, 2 mM CaCl2, 10 mM HEPES, 12.5 mM dextrose, pH 7.4 with NaOH.
- Internal Solution: 120 mM K-gluconate, 20 mM KCl, 10 mM HEPES, 5 mM EGTA, 1.5 mM MgATP, pH 7.3 with KOH.
System Setup:
- Prime planar patch chip with internal solution.
- Dispense cell suspension into wells.
- Apply suction to capture cells on apertures and form seals.
- Monitor seal formation and proceed to whole-cell configuration.
Compound Application:
- Establish stable baseline recording.
- Apply test compounds sequentially with washout steps between concentrations.
- Include positive and negative controls on each plate.
- Verify compound exposure through bioanalysis when possible [72].
Data Acquisition and Analysis:
- Implement high-throughput analysis workflows for processing large datasets [122].
- For voltage-gated channels, analyze peak current, steady-state activation/inactivation, and time constants.
- Generate concentration-response curves to determine IC50/EC50 values.
- Apply quality control criteria including seal resistance, capacitance, and series resistance limits.
Workflow Visualization
Diagram 1: Comparative workflow of manual versus automated patch clamp experiments. Manual processes (blue) emphasize flexibility and single-cell precision, while automated processes (red) highlight parallel processing and standardization for increased throughput.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Electrophysiology Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Borosilicate Glass Capillaries | Formation of recording pipettes | For manual patch clamp, typically pulled to resistances of 2-6 MΩ; fire-polishing can improve seal success [120] |
| Planar Patch Chips | Microfabricated substrates for automated recordings | Contains micron-sized apertures for cell capture; composition varies (silicon, plastic, quartz) [121] |
| Ion Channel Cell Lines | Recombinant expression systems | HEK293 or CHO cells stably expressing specific ion channels (e.g., hERG, NaV1.1-1.9) enable standardized screening [121] [72] |
| Primary Neuronal Cultures | Native cellular environment | Maintain native channel composition and regulatory elements; essential for translational research [121] |
| External/Internal Recording Solutions | Ionic environment control | Composition varies based on ion channel studied; often include HEPES buffer, ions, and energy sources [72] [37] |
| Pharmacological Modulators | Channel-specific agonists/antagonists | Used for validation (e.g., nifedipine for L-type Ca2+ channels, TTX for voltage-gated Na+ channels) [37] |
| Enzymatic Isolation Kits | Primary cell preparation | Collagenase/hyaluronidase blends for isolating native cardiomyocytes or neurons [37] |
Manual and automated patch clamp platforms offer complementary strengths for electrophysiological research. Manual techniques provide unparalleled flexibility and access to complex cellular preparations, including primary neurons and stem cell-derived cultures, making them ideal for mechanistic studies and validation experiments. Automated systems deliver substantially higher throughput with reduced operator dependency, excelling in compound screening applications and standardized assays. Recent advancements in APC technology have expanded its applicability to native cardiomyocytes and complex current measurements, bridging the gap between throughput and physiological relevance [37]. The choice between platforms should be guided by specific research objectives, weighing factors of data content, throughput requirements, cell type compatibility, and available resources. Future developments in automated systems that improve flexibility with diverse cell types and enhance data quality will further broaden their applications in both academic research and drug discovery initiatives.
Validating in vitro models with electrophysiological profiling is a critical step in bridging the translational gap between preclinical drug discovery and clinical success, particularly for central nervous system (CNS) targets. Electrophysiological techniques provide a direct, functional readout of neuronal health and network activity, offering insights that complement molecular and biochemical data [123]. These methods are especially valuable for assessing the functional impact of compounds on neuronal ion channels, receptors, and transporters, which are common mediators of off-target CNS effects that account for a significant proportion of drug attrition [123]. The emergence of more complex human cell-based models and automated systems has positioned electrophysiology as an essential tool for creating more predictive preclinical safety and efficacy profiles.
Electrophysiological Techniques for Translational Validation
Two primary electrophysiological techniques are employed for the validation of in vitro models: patch-clamp recordings and microelectrode arrays (MEAs). Each offers unique advantages for different aspects of neuronal function assessment.
Patch-clamp is a highly sensitive technique considered the 'gold standard' for studying ionic currents and membrane potentials at the level of single cells [68]. It provides exceptional spatiotemporal precision and allows direct access to the intracellular environment, enabling researchers to explore sub-threshold signals and the fundamental mechanisms of neuronal excitability in both voltage-clamp and current-clamp modes [68]. Its application is well-demonstrated in Parkinson's disease (PD) research, where it has been used to show that alpha-synuclein (αSyn) accumulation increases the action potential threshold in neuronal models [68].
Microelectrode Arrays (MEAs), in contrast, enable non-invasive, multi-site, long-term recordings of extracellular field potentials and spike activity across neural networks [124] [68]. This technology is ideal for observing developmental dynamics, network synchronization, and the overall functional effects of pharmacological interventions or disease-specific mutations on network behavior. A key advancement is its application in human induced pluripotent stem cell (hiPSC)-derived neural models, which allows for the assessment of compound effects on human neuronal networks, as demonstrated in studies of opioid receptor modulation [124].
Table 1: Comparison of Key Electrophysiological Techniques
| Feature | Patch-Clamp Recording | Microelectrode Array (MEA) |
|---|---|---|
| Primary Application | Intracellular recording; single-cell analysis [68] | Extracellular recording; network-level analysis [124] [68] |
| Key Measured Parameters | Ionic currents, action potential threshold/frequency, membrane potential [68] | Network bursts, mean firing rate, synchrony, burst duration [124] |
| Throughput | Low to medium (manual); medium (automated) [123] | Medium to high [68] |
| Temporal Resolution | Very high (millisecond) [68] | High (millisecond) [68] |
| Key Advantage | Direct intracellular access; high-resolution sub-threshold signals [68] | Non-invasive; long-term network activity monitoring [68] |
Experimental Design & Workflow
A robust workflow for electrophysiological validation integrates human-relevant cellular models with defined experimental protocols and analytical endpoints. The use of hiPSC-derived neurons and astrocytes has become a cornerstone of this approach, providing a genetically relevant and physiologically responsive platform [124].
The experimental workflow begins with the culture of neural cells on a suitable platform, such as an MEA plate, allowing them to develop robust and synchronous baseline network activity patterns [124]. Once mature, the network is treated with the test agent across a range of concentrations. A positive control, such as a known opioid agonist, can be used to establish a baseline response, evidenced by a concentration-dependent modulation of electrophysiological activity [124]. The specificity of the observed response is then tested by co-application or subsequent application of a selective antagonist to demonstrate phenotypic reversal [124]. Data is continuously acquired and analyzed for parameters spanning from single-electrode to network-wide activity.
Diagram 1: Electrophysiological profiling workflow for compound testing.
Key Experimental Findings & Data Presentation
Electrophysiological profiling in hiPSC-derived neural models generates rich, quantitative data on the functional impact of pharmacological agents. The application of the μ-opioid receptor agonist DAMGO serves as a robust example, demonstrating concentration-dependent suppression of network activity that is reversible by the antagonist naloxone [124].
Critical parameters affected by opioid receptor activation include metrics of overall neural activity, single-electrode bursting, network bursting, and synchronicity [124]. Furthermore, DAMGO treatment has been shown to disrupt higher-order baseline neural patterns and synaptic network connectivity [124]. The baseline properties of the neural network itself can influence the magnitude of the drug-induced effects, highlighting the importance of characterizing the in vitro model's initial state [124].
Table 2: Quantitative Electrophysiological Parameters for Model Validation
| Parameter Category | Specific Metric | Example Change with Opioid Agonist (DAMGO) | Reversal by Naloxone |
|---|---|---|---|
| Overall Neural Activity | Mean Firing Rate | Decreased, concentration-dependent [124] | Yes [124] |
| Single Electrode Burst | Bursts per Minute | Decreased [124] | Yes [124] |
| Network Burst | Network Bursts per Minute | Decreased [124] | Yes [124] |
| Synchronicity | Synchronization Index | Disrupted [124] | Yes [124] |
| Higher-Order Patterns | Synaptic Network Connectivity | Disrupted [124] | Data needed |
Detailed Protocols
Protocol 1: MEA Assay for Pharmacological Profiling on hiPSC-Derived Neural Networks
This protocol details the steps for using microelectrode arrays to assess the functional response of a human iPSC-derived neural model to a compound and its specific reversal by an antagonist, based on a study investigating opioid effects [124].
Key Materials:
- hiPSC-derived neurons and astrocytes [124]
- Multielectrode Array (MEA) plates [124]
- µ-opioid receptor agonist (e.g., DAMGO) [124]
- Opioid antagonist (e.g., Naloxone) [124]
- Appropriate cell culture medium and reagents
Procedure:
- Cell Culture and Plating: Culture hiPSC-derived neurons and astrocytes according to established protocols. Plate the cells onto MEA plates pre-coated with a suitable substrate (e.g., poly-D-lysine, laminin) at a density that supports robust network formation.
- Network Maturation: Maintain the cultures for several weeks, replacing the medium periodically, to allow the development of mature, synchronous neural network activity characterized by stable baseline firing and bursting patterns [124].
- Baseline Recording: Place the MEA plate in the recording setup maintained at 37°C and 5% CO₂. Record spontaneous neural activity for at least 10 minutes to establish a pre-treatment baseline.
- Compound Treatment: Treat the networks with the agonist (e.g., DAMGO) across a range of concentrations (e.g., 1 nM to 10 µM). For each concentration, add the compound directly to the culture medium and mix gently.
- Post-Treatment Recording: Record neural activity for a defined period (e.g., 30-60 minutes) after each compound addition to capture the peak effect.
- Antagonist Application: Following agonist exposure, add the antagonist (e.g., 10 µM naloxone) to all wells [124].
- Reversal Recording: Record neural activity for an additional 30-60 minutes post-antagonist application to assess phenotypic reversal.
- Data Analysis: Analyze the recorded data for key parameters, including mean firing rate, burst properties, and network synchrony. Normalize data to the baseline recording period and plot concentration-response relationships for the agonist and the extent of reversal by the antagonist.
Protocol 2: Patch-Clamp Characterization of Neuronal Excitability in Disease Models
This protocol outlines the use of patch-clamp electrophysiology to investigate intrinsic neuronal properties and excitability changes in hiPSC-derived models of neurodegenerative disease, such as Parkinson's disease [68].
Key Materials:
- hiPSC-derived dopaminergic neurons (from healthy donors and patients with PD-associated mutations, e.g., SNCA, LRRK2-G2019S) [68]
- Patch-clamp rig (amplifier, micromanipulators, vibration isolation table, Faraday cage)
- Recording pipettes
- Extracellular and intracellular recording solutions
Procedure:
- Cell Preparation: Culture hiPSC-derived dopaminergic neurons on glass coverslips suitable for the recording chamber. Cells can be used as 2D monolayers or from more complex 3D organoids [68].
- Electrode and Solution Preparation: Pull borosilicate glass capillaries to create recording pipettes with appropriate resistance. Fill the pipette with a filtered intracellular solution matching the physiological ionic composition.
- Cell Identification: Transfer a coverslip with cells to the recording chamber perfused with oxygenated extracellular solution. Visualize neurons under a microscope and bring the pipette close to a cell of interest.
- Whole-Cell Formation: Apply gentle positive pressure to the pipette and advance it onto the cell membrane. Quickly release the positive pressure and apply gentle suction to achieve a high-resistance seal (giga-ohm seal). Compensate for pipette capacitance and rupture the membrane patch with a brief pulse of suction or voltage zap to establish the whole-cell configuration.
- Current-Clamp Recording: In current-clamp mode, set the holding current to zero. Record the cell's resting membrane potential. To probe excitability, inject a series of depolarizing current steps of increasing magnitude and record the resulting voltage changes, including the number and frequency of action potentials fired.
- Voltage-Clamp Recording: Switch to voltage-clamp mode to isolate specific ionic currents. Hold the cell at a set potential (e.g., -70 mV) and apply voltage steps or ramps to activate voltage-gated sodium, potassium, or calcium channels. The amplifier will measure the resulting ionic currents.
- Data Analysis: Analyze recordings for parameters such as resting membrane potential, action potential threshold, input resistance, and the magnitude of voltage-gated currents. Compare these properties between healthy control neurons and those carrying disease-related mutations to identify functional deficits [68].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful electrophysiological profiling relies on a suite of specialized reagents and tools. The following table details key components for establishing and running these assays.
Table 3: Research Reagent Solutions for Electrophysiological Profiling
| Item | Function/Application | Example/Note |
|---|---|---|
| hiPSC-Derived Neural Cells | Provides a genetically human-relevant, physiologically active model system for toxicity and efficacy testing [124]. | Co-cultures of hiPSC-neurons and hiPSC-astrocytes can develop robust, synchronous network activity [124]. |
| Multielectrode Array (MEA) System | Enables non-invasive, long-term, multi-site recording of extracellular field potentials and network activity [124] [68]. | Used for network-level analysis and pharmacological screening, as in opioid agonist studies [124]. |
| Patch-Clamp Setup | The "gold standard" for high-resolution recording of ionic currents and membrane potentials from single cells [68] [123]. | Applied to study disease-specific changes in neuronal excitability in PD models [68]. |
| Specific Receptor Agonists/Antagonists | Pharmacological tools to probe specific signaling pathways and validate model responsiveness [124]. | DAMGO (μ-opioid receptor agonist) and naloxone (antagonist) used to demonstrate specific, reversible network effects [124]. |
| 3D Organoid Culture Platforms | Advanced in vitro models that may more faithfully recapitulate the cellular complexity and structure of the native brain [68]. | Midbrain organoids derived from PD patients used for electrophysiological characterization [68]. |
Signaling Pathways and Network Impacts
Understanding how a compound or disease mutation impacts neural function requires mapping its effects onto specific signaling pathways and network-level outcomes. The pathway below illustrates the cascade of events triggered by μ-opioid receptor activation in a human neuronal network, culminating in measurable electrophysiological changes.
Diagram 2: Signaling pathway of μ-opioid receptor activation.
Conclusion
Electrophysiology remains the cornerstone of functional analysis in neuroscience, providing an unparalleled, direct measurement of neuronal activity. The journey from foundational single-cell patch-clamp recordings to high-throughput automated systems and network-level MEA analysis has dramatically expanded our capabilities in both basic research and drug discovery. As the field progresses, the integration of electrophysiology with other technologies—such as optogenetics, human induced pluripotent stem cells (iPSCs), organoids, and advanced computational models—paves the way for a new era of personalized medicine and deeper mechanistic understanding of neurological diseases. The future of electrophysiology lies in continuing to enhance the credibility of its models, refining high-content screening methods for ion channel drug targets, and further bridging the gap between preclinical findings and clinical applications to accelerate the development of novel therapeutics.
References
- 1. Unlocking Neuronal Secrets Excitability [https://www.numberanalytics.com/blog/ultimate-guide-neuronal-excitability-electrophysiology-techniques]
- 2. Whole-cell patch clamp and extracellular electrophysiology ... [https://www.sciencedirect.com/science/article/pii/S2666166725004149]
- 3. Protocol for extracellular recordings of mechanically ... [https://pubmed.ncbi.nlm.nih.gov/40378047/]
- 4. Quantum computing meets neural : modeling ion channels... excitability [https://www.aimspress.com/article/doi/10.3934/biophy.2025016]
- 5. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 6. NIH supports new research on ion channels, the 'hidden ... [https://news.utsa.edu/2025/10/nih-supports-new-research-on-ion-channels-the-hidden-drivers-of-health/]
- 7. Article Combined statistical-biophysical modeling links ion ... [https://www.sciencedirect.com/science/article/pii/S2666389925001710]
- 8. Linking ion channel gene expression to neuronal firing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546750/]
- 9. Recent advances in the pharmacology of voltage-gated ion ... [https://www.sciencedirect.com/science/article/pii/S0031699725074988]
- 10. Estimation of ionic currents and compensation ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1458878/full]
- 11. Review: Academic Ion Channels Drug Discovery ... [https://metrionbiosciences.com/ion-channels-drug-discovery-workshop-2025/]
- 12. Functional Characterization of Ion Channels in Planar Lipid ... [https://pubmed.ncbi.nlm.nih.gov/40304908/]
- 13. Functional Effect Predictions For Ion Channel Missense ... [https://www.medrxiv.org/content/10.1101/2025.10.16.25337735v1.full]
- 14. 2025 InnovatION Grant Program [https://ionbiosciences.com/2025-innovation-grant-program/]
- 15. Action potential [https://en.wikipedia.org/wiki/Action_potential]
- 16. Physiology, Resting Potential - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538338/]
- 17. Physiology, Neurotransmitters - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK539894/]
- 18. Pain Research Reveals New Detail of How Synapses ... [https://news.utdallas.edu/health-medicine/pain-research-synapses-strength-2025/]
- 19. Resting potential [https://en.wikipedia.org/wiki/Resting_potential]
- 20. Resting Membrane Potential - Nernst - Generation [https://teachmephysiology.com/nervous-system/synapses/resting-membrane-potential/]
- 21. What Is Action Potential? [https://www.simplypsychology.org/what-is-action-potential.html]
- 22. Synaptic transmission | Nature Neuroscience [https://www.nature.com/subjects/synaptic-transmission/neuro]
- 23. What is Action Potential, Membrane ... [https://www.moleculardevices.com/applications/patch-clamp-electrophysiology/what-action-potential]
- 24. Electrophysiology, Patch Clamp Technique, Cardiac ... [https://www.moleculardevices.com/technology/electrophysiology]
- 25. Neural electrophysiology: Measuring how neurons ... [https://cytotronics.com/resources_cpt/neural-electrophysiology/]
- 26. Neuroscience Instrumentation, Amplifiers, Stimulators, ... [https://www.a-msystems.com/s-1-instruments.aspx?srsltid=AfmBOorKesBezxI_oPP1nCYzidUvz1PD1KYGGl5PtuK0WnRV4EjDINLU]
- 27. Science and Art of Pulling Micropipettes [https://www.wpiinc.com/blog/post/Science-and-Art-of-Pulling-Micropipettes?srsltid=AfmBOoqxIG2XbNudOTkkhmcBWPHhDpIeQFQeQn3oujvSP4Qxjhx-lvNp]
- 28. Faraday Cage: What Is It? How Does It Work? [https://www.gamry.com/application-notes/instrumentation/faraday-cage/]
- 29. Protocols for electrophysiological recordings and electron ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8371263/]
- 30. Making Patch-pipettes and Sharp Electrodes with a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3233862/]
- 31. Protocol to correlate electron microscopy with ... [https://www.sciencedirect.com/science/article/pii/S2666166724001680]
- 32. Faraday cage [https://en.wikipedia.org/wiki/Faraday_cage]
- 33. One-channel Cell-attached Patch-clamp Recording - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4188217/]
- 34. Patch clamp | Spikes and bursts [https://spikesandbursts.wordpress.com/patch-clamp/]
- 35. Whole-cell patch clamp and extracellular electrophysiology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12337184/]
- 36. Patch2MAP combines patch-clamp electrophysiology with ... [https://www.nature.com/articles/s41598-025-18207-3]
- 37. A modern automated patch-clamp approach for high ... [https://www.nature.com/articles/s42003-022-03871-2]
- 38. The Role of Planar Patch-Clamp Array Chip Technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC3184600/]
- 39. Development of planar patch clamp technology and its ... [https://www.sciencedirect.com/science/article/pii/S1002007108003547]
- 40. Automated patch-clamp recordings for detecting activators ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12092551/]
- 41. Advances in large-scale electrophysiology with high-density ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00058k]
- 42. Electrophysiology Methods for Assessing of ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11205106/]
- 43. Biological application of microelectrode arrays in drug ... [https://pubmed.ncbi.nlm.nih.gov/12923608/]
- 44. Development of a microelectrode array system for ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325005706]
- 45. MEA-NAP: A flexible network analysis pipeline for neuronal ... [https://www.sciencedirect.com/science/article/pii/S2667237524002911]
- 46. MEA-NAP: A flexible network analysis pipeline for neuronal ... [https://pubmed.ncbi.nlm.nih.gov/39520988/]
- 47. Types of Quantitative Data Analysis and Presentation Format [https://pressbooks.bccampus.ca/undergradresearch/chapter/types-of-quantitative-data-analysis-and-presentation-format/]
- 48. Voltage Clamp - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/voltage-clamp]
- 49. Voltage clamp - Scholarpedia [http://www.scholarpedia.org/article/Voltage_clamp]
- 50. Current Clamp Technique - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/current-clamp-technique]
- 51. Article High-throughput combined voltage-clamp/current- ... [https://www.sciencedirect.com/science/article/pii/S2667237522002909]
- 52. Resolving Artifacts in Voltage‐Clamp Experiments with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376535/]
- 53. What’s the Difference Between a Voltage Clamp and a Current Clamp? | The Scientist [https://www.the-scientist.com/what-s-the-difference-between-a-voltage-clamp-and-a-current-clamp-72296]
- 54. Voltage Clamp Explained – Principles, Applications & How ... [https://physiologicinstruments.com/blogs/news/voltage-clamp-explained?srsltid=AfmBOoql-ZefUwJHxa4DOYumKwVbcbBF63D32-RI8e-vMwe7u2zikS-L]
- 55. Current clamps – Knowledge and References [https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Medical_technology_%26_engineering/Current_clamps/]
- 56. Cell-attached voltage-clamp and current-clamp recording and stimulation techniques in brain slices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2373773/]
- 57. Patch Clamp Electrophysiology, Action Potential, Voltage ... [https://www.moleculardevices.com/applications/patch-clamp-electrophysiology]
- 58. Neuropixels Opto: Combining high-resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11838571/]
- 59. INTEGRATION OF CALCIUM IMAGING TRACES VIA ... [https://arxiv.org/html/2501.14615v3]
- 60. Unraveling the neurobiological mechanisms of depression ... [https://pubmed.ncbi.nlm.nih.gov/40651214/]
- 61. A software platform for real-time and adaptive ... [https://www.nature.com/articles/s41467-025-64856-3]
- 62. A wireless optogenetic stimulation system for long-term ... [https://www.nature.com/articles/s41467-025-63746-y]
- 63. Advances in large-scale electrophysiology with high-density ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394932/]
- 64. Electrophysiology: Tapping Into the Wonders of the Brain [https://kids.frontiersin.org/articles/10.3389/frym.2025.1588454]
- 65. Electrophysiological Evidence for the Development of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6705908/]
- 66. An electrophysiological perspective on Parkinson's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8656091/]
- 67. Exploring the electrophysiology of Parkinson's disease with ... [https://www.nature.com/articles/s41597-024-03768-1]
- 68. In vitro electrophysiological characterization of Parkinson's ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1584555/full]
- 69. Electrophysiology in neuropathic pain: a bibliometric analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170604/]
- 70. A brain-wide map of neural activity during complex behaviour [https://www.nature.com/articles/s41586-025-09235-0]
- 71. Integration of electrophysiological and mechanical ... [https://www.sciencedirect.com/science/article/pii/S016926072500313X]
- 72. Multi-laboratory comparisons of manual patch clamp hERG ... [https://www.nature.com/articles/s41598-025-15761-8]
- 73. CiPA initiative [https://cipaproject.org/]
- 74. Recent developments in using mechanistic cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4909717/]
- 75. Advanced neural activity mapping in brain organoids via ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1634582/full]
- 76. Neural Schematics as a unified formal graphical ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2013.00022/full]
- 77. A Comprehensive Guide to Acute Brain Slices for ... [https://precisionary.com/a-comprehensive-protocol-guide-to-acute-brain-slices-for-electrophysiology/?srsltid=AfmBOor8-oN4rXpcjP-wgr2GgwgRUAdA6xx-QodYCVtL-2PoiAx1obKc]
- 78. Bubble Perfusion Brain Slice Culture with Single-Droplet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532049/]
- 79. Ultra-high-density Neuropixels probes improve detection ... [https://www.sciencedirect.com/science/article/pii/S0896627325006658]
- 80. Patch-Clamp Techniques: Choosing Equipment and ... [https://www.labx.com/resources/patch-clamp-techniques-choosing-equipment-and-optimizing-experiments/5621]
- 81. Science and Art of Pulling Micropipettes [https://www.wpiinc.com/blog/post/Science-and-Art-of-Pulling-Micropipettes?srsltid=AfmBOooTT6Vnbpwx0o9sJgkI0-l0u9Bf7546YkSHkmGHg1YhnLN80wAt]
- 82. Immediate reuse of patch-clamp pipettes after ultrasonic ... [https://www.nature.com/articles/s41598-024-51837-7]
- 83. How to Deal With Noise in Electrophysiology Rigs [https://blog.a-msystems.com/how-to-deal-with-noise-in-electrophysiology-rigs/]
- 84. How to reduce the noise around your electrophysiology rig [https://www.scientifica.uk.com/neurowire/labhacks-how-to-denoise-your-rig]
- 85. Electrical Noise Effects on Electronic Signal Interference [https://www.ai-futureschool.com/en/electrotechnics/understanding-electrical-noise-in-circuits.php]
- 86. Reducing Interference During Electrophysiology Recording ... [https://www.kontex.io/post/reducing-interference-during-electrophysiology-recording-sessions]
- 87. The effects of whole-body vibration therapy on immune and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11323691/]
- 88. 40 Hz vibrations reduce Alzheimer's pathology, symptoms in ... [https://picower.mit.edu/news/40-hz-vibrations-reduce-alzheimers-pathology-symptoms-mouse-models]
- 89. How to Implement Effective Noise Control for Battery Systems [https://blog.harbingerland.com/how-to-implement-effective-noise-control-for-battery-systems-a-step-by-step-guide/]
- 90. Osmolarity - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/osmolarity]
- 91. Change in Osmotic Pressure Influences the Absorption ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11011345/]
- 92. Electrophysiology: What goes on the inside? - Scientifica [https://www.scientifica.uk.com/neurowire/electrophysiology-what-goes-on-the-inside]
- 93. BUFFERS [https://www.ou.edu/research/electron/bmz5364/buffers.html]
- 94. The effect of respiration buffer composition on mitochondrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5665555/]
- 95. Rapid Rise of Extracellular pH Evoked by Neural Activity Is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2822688/]
- 96. Human brain slice cultures: translational applications and ... [https://www.life-science-alliance.org/content/8/12/e202403160]
- 97. Enhancing neuronal viability: The protective role of 10% ... [https://pubmed.ncbi.nlm.nih.gov/40517804/]
- 98. State of the Art of Artificial Intelligence in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123071/]
- 99. Validation of a High-Throughput, Automated ... [https://www.sciencedirect.com/science/article/pii/S2472555222074561]
- 100. Synthetic Data Generation for Classifying ... [https://arxiv.org/html/2508.06514v1]
- 101. Guidelines and best practices for electrophysiological data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4141903/]
- 102. Artificial Intelligence in Cardiac Electrophysiology [https://www.mdpi.com/2306-5354/12/10/1102]
- 103. NeuroElectro: a window to the world's neuron ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2014.00040/full]
- 104. Model-driven optimal experimental design for calibrating ... [https://www.sciencedirect.com/science/article/pii/S0169260723003553]
- 105. Electrophysiological Imaging of Brain Activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3241716/]
- 106. Qualitative and Quantitative Comparative Analysis of ... [https://pubmed.ncbi.nlm.nih.gov/41042404/]
- 107. A large-scale MEG and EEG dataset for object recognition ... [https://www.nature.com/articles/s41597-025-05174-7]
- 108. Comparing MEG and EEG measurement set-ups for a ... [https://pubmed.ncbi.nlm.nih.gov/40209163/]
- 109. A MEG powerhouse: How UTSW is pushing the limits of ... [https://www.utsouthwestern.edu/newsroom/articles/year-2025/aug-meg-powerhouse.html]
- 110. Highlights from MEG-TREC 2025 [https://fixel.ufhealth.org/2025/05/01/highlights-from-meg-trec-2025/]
- 111. A comparative study on the detection and localization of ... [https://www.sciencedirect.com/science/article/pii/S1053811925002356]
- 112. A Brain Foundation Model for Unified EEG and MEG Signals [https://arxiv.org/html/2505.18185v1]
- 113. EEG Signal Processing Techniques and Applications—2nd ... [https://www.mdpi.com/1424-8220/25/3/805]
- 114. Comparison of STFT and wavelet transform methods in ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482504000691]
- 115. Automated EEG Signal Processing: A Comprehensive ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027025002055]
- 116. Time-frequency analysis of movement-related spectral power ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2815165/]
- 117. Decoding covert visual attention of ... [https://www.nature.com/articles/s41598-025-21635-w]
- 118. Comparison of STFT and wavelet transform methods in ... [https://pubmed.ncbi.nlm.nih.gov/15809098/]
- 119. Wavelet Transform for Classification of EEG Signal using ... [https://biomedpharmajournal.org/vol10no4/wavelet-transform-for-classification-of-eeg-signal-using-svm-and-ann/]
- 120. Fundamentals, Membrane... | Technology Networks Electrophysiology [https://www.technologynetworks.com/neuroscience/articles/electrophysiology-fundamentals-membrane-potential-and-electrophysiological-techniques-359363]
- 121. A Comparison of the Performance and Application Differences... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3549544/]
- 122. An efficient and scalable data analysis solution for ... [https://pubmed.ncbi.nlm.nih.gov/35058183/]
- 123. The emerging role of in vitro electrophysiological methods ... [https://www.sciencedirect.com/science/article/pii/S1056871916300168]
- 124. Nonclinical Human Neural New Approach Methodologies ... [https://www.sciencedirect.com/science/article/pii/S3050620425000594]